Abstract
Early care and education settings, such as family child care homes (FCCHs), are important venues for children’s health promotion. Keys to Healthy Family Child Care Homes evaluated a FCCH-based intervention’s impact on children’s diet and physical activity. This study enrolled 496 children aged 1.5–4 years and 166 FCCH providers into a cluster-randomized control trial (intervention=242 children/83 FCCHs, control=254 children/83 FCCHs) conducted during 2013–2016. The 9-month intervention addressed provider health, health of the FCCH environment, and business practices, and was delivered through three workshops, three home visits, and nine phone calls. The attention control arm received a business-focused intervention. Primary outcomes were children’s diet quality (2 days of observed intakes summarized into Healthy Eating Index scores) and moderate to vigorous physical activity (3 days of accelerometry) at the FCCH. Secondary outcomes were child body mass index (BMI), FCCH provider health behaviors, and FCCH nutrition and physical activity environments and business practices. Repeated measures analysis, using an intent-to-treat approach, accounting for clustering of children within FCCHs and adjusting for child age, sex, and BMI, was used to evaluate change (completed in 2018). Compared to controls, intervention children significantly improved their diet quality (5.39, p=0.0002, CI=2.53, 8.26) but not MVPA (0.31, p = 0.195, CI=−0.16, 0.79). Intervention FCCH providers significantly improved their diet quality and several components of their FCCH environment (i.e., time provided for physical activity, use of supportive physical activity practices, and engagement in nutrition and physical activity education/professional development). FCCHs are malleable settings for health promotion, especially diet quality.
INTRODUCTION
A high-quality diet and regular physical activity improves young children’s weight, cardiometabolic health, skeletal/bone health, psychosocial health, and cognitive development.1–4 Unfortunately, young children are not meeting diet and physical activity recommendations.5 These behaviors are adopted early in life track into adolescence and adulthood, hence it is important to intervene early to shape behaviors.6
Early care and education (ECE) offers important opportunities to improve young children’s diet and physical activity.7 In Australia and the United States (US), 60–64% of children aged 3–5 years are enrolled in some type of ECE program.8,9 Many countries in Europe have enrollment rates above 90%.10 Most children, at least in the US, are in full-day care.8 Hence, ECE settings are where they get most of their meals/snacks and opportunities for physical activity.
Family child care homes (FCCHs) are the second largest provider of child care in the US.11 FCCHs are generally smaller, less formal, ECE programs. FCCHs have fewer regulations compared to center-based programs, including limited nutrition and physical activity requirements.12,13 FCCHs are an important target for intervention as they have poor nutrition and physical activity practices,14 and the children enrolled have poor diet quality, low physical activity, and increased risk of obesity.15–17
Unfortunately, FCCHs have been largely ignored in intervention research.14 The few existing FCCH-based intervention studies show promising results but many rely on quasi-experimental designs and focus on environmental outcomes.18–21
To address this research gap, we developed Keys to a Healthy Family Child Care Home (Keys), an intervention to improve FCCH environments and positively impact children’s diet quality and physical activity. This paper describes primary and secondary outcomes from this intervention.
METHODS
Keys used a cluster-randomized controlled trial to evaluate a 9-month FCCH-based intervention’s impact on children’s diet quality and physical activity while at child care. Study protocols and intervention development have been published,22,23 but are described briefly below. Protocols were approved by the Institutional Review Boards at the University of North Carolina at Chapel Hill and the Duke University Medical Center and registered at ClinicalTrials.gov (NCT01814215).
Participants and Recruitment
Participants included a convenience sample of FCCH providers in central North Carolina and children aged 1.5–4 years enrolled in these FCCHs, recruited in five cohorts over 2 years. Community partners shared information about the project with local FCCHs. Then, study staff followed up with FCCH providers via mail, email, and telephone to invite study participation. During telephone follow-ups, FCCHs were screened for eligibility (i.e., enrolling at least two children aged 1.5–4 years, providing at least one meal and snack per day, being open year-round, and having been in business for two years with no plans to close in the coming year). Study staff then visited eligible FCCH providers to explain study details and obtain written informed consent. Study staff worked through the FCCH provider to share study information with parents (including project contact information for questions) and collect informed consent. Parental consent for at least two children was required for the FCCH to participate.
Power
Calculations assumed two-sided tests of significance at α=0.025 (overall Type I error=0.05), clusters of three children per FCCH (on average), ICCs of 0.36 for Healthy Eating Index (HEI) score and 0.12 for moderate to vigorous physical activity (MVPA) (based on previous ECE work), and an effect size of 0.40 (+5 points in HEI score, +1 minute/hour in MVPA). The initial sample size of 150 FCCHs and 450 children 22 was revised following cohort 1 due to high child attrition (20% anticipated vs. 47% actual),24 due mainly to children no longer being enrolled in the FCCH because of change in parental employment, transition into center-based care, or moving out of the area. The updated sample size was 165 FCCHs and 495 children.
Randomization
Following baseline data collection, children were randomized in clusters, based on their FCCH. FCCHs were stratified based on FCCH provider weight (i.e., normal weight, overweight, obese), given that child care providers’ own health impacts their nutrition and physical activity practices and the behaviors of the children in their care.25,26 The study statistician used computerized block randomization to assign FCCHs into either the intervention or control arm (1:1) (SAS 9.3, Cary, NC). Participants were informed of randomization by the project manager, while investigators remained blinded.
Intervention
The Keys intervention was designed to help FCCH providers create environments that support children’s healthy eating and physical activity behaviors. The intervention was developed using Intervention Mapping.23 Drawing on the Socio-Ecologic Framework,27 the intervention targeted provider behaviors and practices that would address multiple levels of influence for children – intrapersonal (child), interpersonal (child-provider and child-parent interactions), and organizational (FCCH environment, provisions, and policies). Social Cognitive Theory28 and Self Determination Theory29 informed identification of psychological drivers of behavior change: behavioral capacity, self-efficacy, expectations and expectancies (attitudes and beliefs), autonomy, and relatedness (social support). Behavior change strategies included persuasive communication, guided practice, self-evaluation, autonomy building, physiological and affective change tools, and active learning.
The Keys intervention included three modules addressing FCCH provider health, the FCCH environment, and FCCH business practices. FCCH provider health and business practices were included as they are critical determinants of the FCCH environment. The FCCH environment module encouraged sharing educational materials with families to help parent adopt similar changes at home. Each module lasted three months and was delivered via a workshop, a home visit, and three telephone or email contacts by health coaches trained in adult learning principles30 and motivational interviewing.31 The 9-month duration allowed the intervention to run concurrent with a typical school-year.
Attention Control
The control program offered a similar dose of attention (replacing home visits with telephone calls) and focused solely on business practices. Content addressed record keeping, contracts, and marketing.
Measures
Measurement of FCCH providers and children occurred at two time points: baseline and post-intervention, approximately nine months apart. Given the multiple cohorts, data collection spread across 2013–2016. Data collectors, certified on all protocols and blinded to arm assignment, conducted a 2-day measurement visit with each FCCH, arriving before the first meal and staying until children left. Alternate day visits (e.g., Monday and Wednesday, Tuesday and Thursday) spread measurement across three days.
Primary Outcomes: Child Diet Quality and Physical Activity
Children’s diet quality at the FCCH was estimated from observed intakes of food and beverages collected via the Diet Observation in Child Care protocol.32 Data collectors observed all meals/snacks over two days and estimated the amount of food and beverages served and remaining for each child. Data were entered into the Nutrition Data System for Research (NDSR, University of Minnesota, 2016) to estimate intakes of energy, macro- and micronutrients, and food group servings. For each child, data were summed across the two days of intakes, then the HEI-2010 algorithm was applied.33 HEI scores assess compliance with national dietary guidelines, higher scores reflecting higher compliance. HEI scoring adjusts for total calories consumed, facilitating comparison across children who consumed different numbers of meals/snacks.
Children’s physical activity was assessed with ActiGraph GT3X+ accelerometers (ActiGraph, Pensacola, FL). Accelerometers were placed on children at the beginning of the first day and worn over the right hip until being collected at the end of the second day. Alternating day visits allowed accelerometers to be worn for three weekdays. Parents were instructed to remove the monitor at bedtime and replace it in the morning. Data were downloaded and processed (SAS v9.4) to assess wear and physical activity outcomes. FCCH start and end times collected in the FCCH environmental assessment (described below) were used to identify physical activity during the FCCH day. Minimum wear criteria (i.e., ≥1 day of wear, ≥3 hours of wear during the FCCH day) were established and age-appropriate cut-points applied to calculate minutes of MVPA (≥191counts/5s),34,35 active play (≥116counts/5s),34,36 and sedentary time (<8.3counts/5s)35 per day for each child. Day-level data for each child were averaged then standardized into minutes per hour to account for variation in the length of the FCCH day and children’s wear time.
Secondary Outcomes
Child Anthropometrics and Demographics.
Data collectors measured children’s height, weight, and waist circumference while children were in light clothing with shoes removed. Height was measured to the nearest 1/8 inch using a Seca stadiometer (Seca Corporation, Columbia, MD; generally as standing height, but six children under 2 years and unable to stand independently were measured lying down37); weight was measured to the nearest 0.1 pound using a Tanita 800BWB scale (Tanita Corporation, Tokyo, Japan); and waist circumference was measured to the nearest 0.1 cm using a Guilick II measuring tape. Height and weight were used to calculate BMI. BMI percentile and z-score were calculated using either the Centers for Disease Control and Prevention’s sex-specific growth charts38 for children 2 years or older or the World Health Organization’s growth standards39 for children under 2 years old. Parents completed a brief demographic survey for their child.
FCCH Provider Diet Quality, Physical Activity, Anthropometrics, and Demographics.
FCCH provider diet was assessed using the Block Brief Food Frequency Questionnaire (FFQ).40 FFQ data were used to calculate a modified HEI-2010 diet quality score.41 Physical activity was assessed using ActiGraph GT3X+ accelerometers worn for seven days (overlapping with children’s physical activity assessment). FCCH provider data were summarized into 60-second epochs. Minimum wear criteria (i.e., ≥3 days and ≥7 hours of wear per day) were established and standard adult cut-points were applied to calculate minutes of MVPA (>2020counts/min),42 lifestyle activity (>760counts/min),43 and sedentary time (<100counts/min).42 Average minutes of activity per day were calculated and standardized to a 14-hour day to account for differences in wear time. FCCH provider height and weight were measured using procedures similar to those used for children, which were then used to calculate BMI and weight status (normal weight, overweight, obese). FCCH providers also completed a demographic survey about themselves and their FCCH.
FCCH Nutrition and Physical Activity Environments.
FCCH nutrition and physical activity environments were assessed using the Environment and Policy Assessment and Observation modified for FCCHs (EPAO-FCCH).44 Data collectors conducted two non-consecutive days of observation and a document review. The EPAO-FCCH assesses compliance with 38 nutrition and 27 physical activity best practices, which are then used to calculate seven nutrition and 10 physical activity environmental sub-scores (range 0–3) as well as overall nutrition (range 0–21) and physical activity scores (range 0–30). Higher scores indicate better compliance with best practices.
FCCH Business Practices.
A modified version of the Business Administration Scale (BAS)45 was used to capture FCCH business practices. Modifications removed non-relevant sections (e.g., risk management) and items overlapping with demographic surveys and expanded items related to promoting children’s healthy eating and physical activity (e.g., communication with parents). Data were summarized into five sub-scores (i.e., income and benefits, work environment, record keeping, provider-parent communication, and marketing and public relations, each ranging from 1–7) and an overall score (range 5–35).
Process Evaluation
Intervention participation data were tracked by the health coaches using an Access database. Participation data included workshop completion (either in group as prescribed, or individually), number of coaching contacts (range 0–12) and length (in minutes), and number of completed self-monitoring logs (range 0–36). Knowledge of recommended behaviors and practices was evaluated following workshops with a brief quiz and summarized as passed (score of 55% or higher) or not passed. Satisfaction was evaluated with brief surveys rating various aspects of quality of the workshops and coaching contacts (1=poor to 5=excellent).
Statistical Analysis
Analyses were conducted under an intent-to-treat model using the Proc Mixed procedure (SAS v9.4) to perform the repeated measures analysis comparing intervention and control groups.46 Models specified an unstructured covariance matrix (comparisons based on change in the Akaike information criterion). Maximum likelihood estimation was applied, helping to account for missing data.47 Models of child-level outcomes accounted for clustering; included child age, sex, and BMI as covariates; and for primary outcomes (HEI score, MVPA/hr) used p values <0.025. Similar methods were used to evaluate secondary outcomes, but models with FCCH provider and environment outcomes did not account for clustering. Specific covariates were selected for FCCH provider outcomes (i.e., age, race, income, and BMI, as known determinants of adults diet and physical activity behaviors), FCCH environment outcomes (i.e., quality rating), and FCCH business outcomes (i.e., provider education, Child And Adult Care Food Program, CACFP). Since secondary outcomes were exploratory, a p-value of <0.05 was used.
To address missing child-level data, multiple imputation was used, models were re-run, and results were compared against the original. One hundred samples were imputed and analyzed in SAS (Proc MI) using available physical activity, HEI, and covariate data. Comparison of baseline data from completers and non-completers suggests that data are missing at random.
RESULTS
Participants
Participants included 496 children and 166 FCCH providers, of which 242 children from 83 FCCHs were assigned to the intervention arm and 254 children from 83 FCCHs were assigned to the control arm. See Figure 1 for the study’s CONSORT diagram. Demographics of children, FCCH providers, and FCCHs are presented in Table 1.
Figure 1:
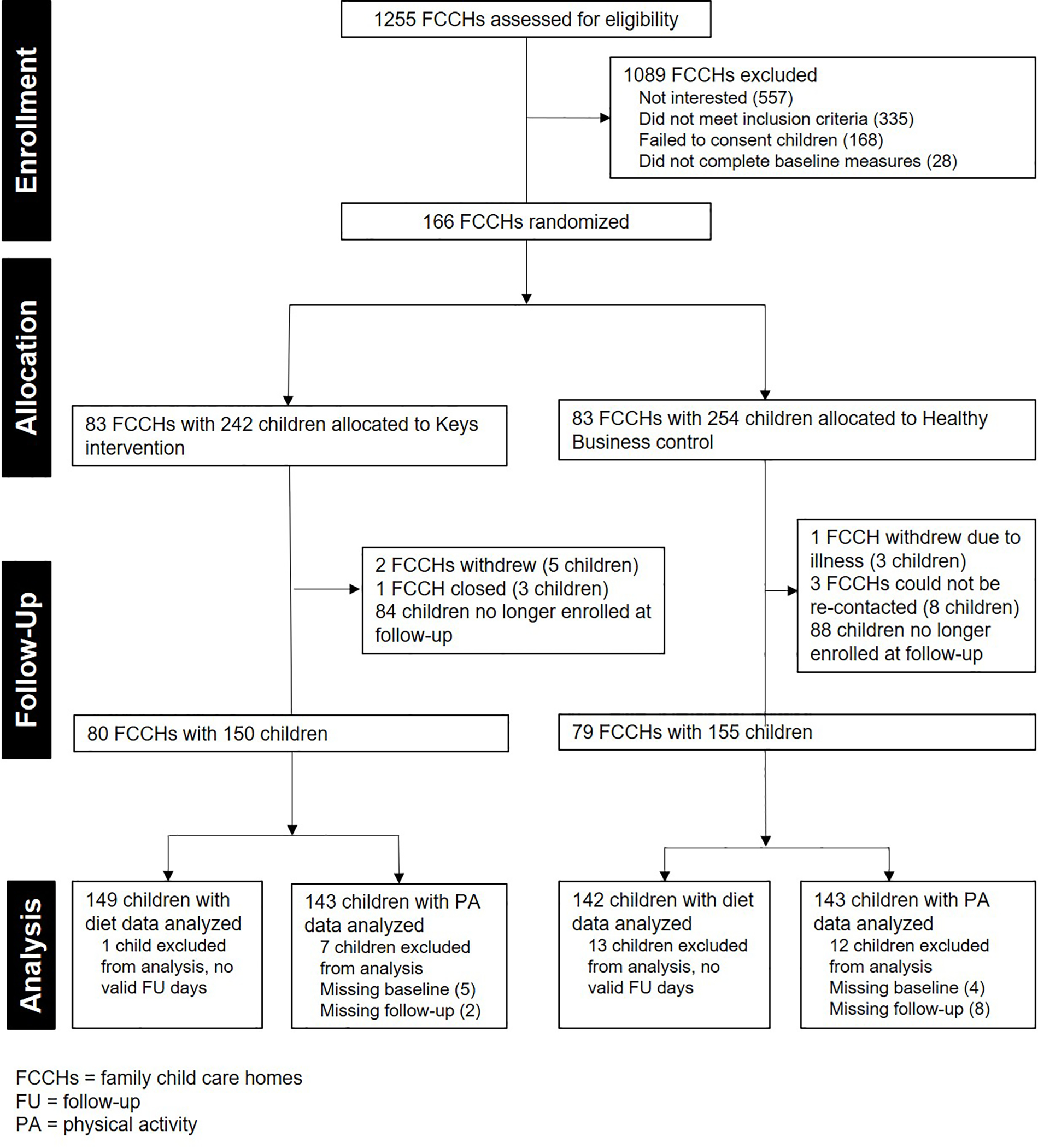
Keys to Healthy Family Child Care Homes CONSORT diagram
Table 1.
Characteristics of participating children, FCCH providers, and FCCHs
| Total Sample | ||
|---|---|---|
| Children | n=496 | |
| Age (months, mean (SD)) | 35.7 | (11.4) |
| Male | 246 | (49.6%) |
| Race | ||
| Black or African American | 314 | (63.3%) |
| White | 135 | (27.2%) |
| Other | 47 | (9.5%) |
| Hispanic or Latino | 20 | (4.1%) |
| Days per week in child care (mean (SD)) | 4.9 | (0.7) |
| FCCH Providers | n=166 | |
| Age (years, mean (SD)) | 49.3 | (9.1) |
| Race | ||
| Black or African American | 123 | (74.1%) |
| White | 30 | (18.1%) |
| Other | 13 | (7.8%) |
| Hispanic or Latino | 8 | (4.8%) |
| Education | ||
| High school diploma or GED | 41 | (24.7%) |
| Associate’s degree or 60 hrs college credit | 82 | (49.4%) |
| Bachelor’s degree or greater | 42 | (25.3%) |
| FCCH Programs | n=166 | |
| Quality Ratinga | ||
| 1 or 2 stars | 13 | (7.8%) |
| 3 stars | 40 | (24.1%) |
| 4 stars | 68 | (41.0%) |
| 5 stars | 45 | (27.1%) |
| Accepts CACFPb Subsidy | 151 | (91.0%) |
Quality Rating is a North Carolina program that assesses the quality of the child care program. Ratings can range between 1 and 5 stars, with more stars equating to higher quality care.
CACFP refers to the Child and Adult Care Food Program, a federally funded program that reimburses participating child care programs for providing eligible meals and snacks served to low-income and other children in their care.
FCCH, Family Child Care Home; GED, General Education Development; CACFP, Child and Adult Food Program
At post-intervention, there was a 38% loss-to-follow-up. The main reason was children no longer being enrolled in the FCCH (n=172 children) or FCCH providers refusing to participate in measures (n=19 children).
Primary Outcomes
Child Diet Quality and Physical Activity
Intervention children significantly improved their total HEI scores relative to control children (+5.39 points, p<0.001). Improvements were seen in whole grains, seafood/plant protein, refined grains, and sodium (for all p≤0.031), with small to medium effect sizes.48 Unexpectedly, a significant decrease was noted in total vegetables (−0.49 points, p=0.003). Children wore the accelerometers on average 2.7 days for 6.6 hours per FCCH day (no significant differences by time or arm). No significant differences were noted between arms for changes in children’s MVPA, active play minutes, or sedentary time. Also, no significant differences were noted between arms for change in children’s BMI or BMI percentile. Results with imputed data were similar (Supplemental Table 1). Child outcomes are presented in Table 2.
Table 2.
Child outcomes: Changes in diet, physical activity, and weight
| Intervention | Control | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | baseline | post-intervention | baseline | post-intervention | Diff in mean change | (95% CI)a | p-valuea | Effect sizeb | ICCc | ||||
| mean | (SD) | mean | (SD) | mean | (SD) | mean | (SD) | ||||||
| n=242 | n=149 | n=253 | n=142 | ||||||||||
| Child Diet | |||||||||||||
| HEI Score | 61.3 | (16.57) | 64.35 | (16.34) | 61.96 | (19.22) | 59.85 | (17.34) | 5.39 | (2.53, 8.26) | <0.001 | 0.29 | 0.61 |
| Adequacy: | |||||||||||||
| Total fruit | 4.46 | (1.64) | 4.38 | (1.4) | 4.47 | (1.31) | 4.30 | (1.66) | 0.03 | (−0.28, 0.33) | 0.859 | 0.06 | 0.38 |
| Whole fruit | 4.59 | (1.61) | 4.71 | (1.06) | 4.69 | (1.37) | 4.60 | (1.41) | 0.18 | (−0.10, 0.47) | 0.211 | 0.14 | 0.29 |
| Total vegetables | 2.01 | (2.12) | 1.84 | (1.51) | 1.89 | (1.88) | 2.08 | (1.80) | −0.49 | (−0.82, −0.17) | 0.003 | −0.18 | 0.46 |
| Greens and beans | 1.25 | (3.18) | 1.14 | (2.54) | 0.98 | (2.85) | 1.16 | (2.62) | −0.21 | (−0.71, 0.28) | 0.399 | −0.10 | 0.58 |
| Whole grains | 3.65 | (5.48) | 4.89 | (4.92) | 3.58 | (5.35) | 3.57 | (5.10) | 1.57 | (0.59, 2.55) | 0.002 | 0.23 | 0.66 |
| Dairy | 8.94 | (2.47) | 9.05 | (2.55) | 9.34 | (2.03) | 9.33 | (1.87) | 0.14 | (−0.36, 0.64) | 0.587 | 0.05 | 0.39 |
| Total protein | 3.61 | (2.30) | 3.41 | (2.53) | 3.60 | (2.25) | 3.31 | (2.62) | 0.01 | (−0.41, 0.42) | 0.972 | 0.03 | 0.47 |
| Seafood/plant protein | 1.57 | (3.50) | 1.79 | (3.10) | 1.72 | (3.69) | 1.57 | (3.23) | 0.67 | (0.06, 1.28) | 0.031 | 0.10 | 0.65 |
| Fatty acids | 4.7 | (5.05) | 4.56 | (5.00) | 4.47 | (5.19) | 4.30 | (5.07) | 0.04 | (−0.86, 0.93) | 0.938 | 0.01 | 0.53 |
| Moderation: | |||||||||||||
| Refined grains | 5.24 | (5.77) | 6.20 | (4.76) | 5.47 | (5.09) | 4.43 | (4.54) | 1.96 | (1.08, 2.84) | <0.001 | 0.37 | 0.6 |
| Sodium | 4.58 | (5.07) | 5.05 | (4.22) | 5.35 | (4.10) | 4.43 | (4.52) | 1.41 | (0.57, 2.25) | 0.001 | 0.31 | 0.58 |
| Empty calories | 16.70 | (6.63) | 17.34 | (4.80) | 16.40 | (6.56) | 16.78 | (6.05) | 0.03 | (−0.97, 1.03) | 0.948 | 0.04 | 0.68 |
| Child Physical Activity | |||||||||||||
| MVPA min/hrd | 4.77 | (2.63) | 5.48 | (2.80) | 4.72 | (3.05) | 5.15 | (2.60) | 0.31 | (−0.16, 0.79) | 0.195 | 0.10 | 0.31 |
| Active play min/hrd | 8.19 | (3.88) | 9.17 | (3.97) | 8.08 | (4.61) | 8.65 | (3.74) | 0.45 | (−0.25, 1.16) | 0.202 | 0.10 | 0.32 |
| Sedentary min/hrd | 38.31 | (7.02) | 37.37 | (6.32) | 38.74 | (8.06) | 38.40 | (6.55) | −0.75 | (−1.95, 0.45) | 0.219 | −0.08 | 0.34 |
| Child Weight | |||||||||||||
| BMI | 16.99 | (2.10) | 16.96 | (2.40) | 16.67 | (1.82) | 16.44 | (1.95) | 0.21 | (−0.02, 0.44) | 0.077 | 0.10 | 0.24 |
| BMI percentile | 65.57 | (29.41) | 66.10 | (30.74) | 62.59 | (30.76) | 62.24 | (30.25) | 1.42 | (−2.61, 5.45) | 0.489 | 0.03 | 0.03 |
Note: Boldface indicates statistical significance (p<0.05).
Difference in mean change, 95% CI, and p-value reflect the fully adjusted model, which controls for baseline values as well as child sex, age, and BMI.
Effect sizes calculated using Cohen’s d.
ICCs reported are for the difference scores using the entire sample.
Estimates of activity reflect only time spent at the FCCH.
HEI, Healthy Eating Index; MVPA, moderate to vigorous physical activity; BMI, body mass index
Secondary Outcomes
FCCH Provider Diet Quality, Physical Activity, and Anthropometrics
FCCH providers in the intervention arm significantly improved their total HEI scores compared to those in the control arm (+3.44 points, p=0.023). Improvements were seen in total fruit, total vegetables, whole grains, fatty acids, and sodium (for all p≤0.028), with medium effect sizes.48 No significant differences were noted for changes in FCCH providers’ MVPA or BMI. FCCH provider outcomes are presented in Table 3.
Table 3.
FCCH Provider and FCCH Outcomes
| Intervention | Control | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | baseline | post-intervention | baseline | post-intervention | Diff in mean change | (95% CI)a | p-valuea | Effect sizeb | ||||
| mean | (SD) | mean | (SD) | mean | (SD) | mean | (SD) | |||||
| n=83 | n=80 | n=83 | n=79 | |||||||||
| FCCH Provider Diet | ||||||||||||
| Modified HEI Score | 59.67 | (9.29) | 63.50 | (9.23) | 59.46 | (9.57) | 60.36 | (9.95) | 3.44 | (0.48, 6.39) | 0.023 | 0.31 |
| Adequacy: | ||||||||||||
| Total fruit | 3.97 | (1.47) | 4.42 | (1.09) | 4.34 | (1.15) | 4.32 | (1.26) | 0.48 | (0.05, 0.92) | 0.028 | 0.37 |
| Whole fruit | 4.3 | (1.31) | 4.71 | (0.74) | 4.46 | (1.09) | 4.52 | (1.21) | 0.37 | (−0.02, 0.76) | 0.060 | 0.29 |
| Total vegetables | 3.43 | (1.33) | 3.80 | (1.29) | 3.80 | (1.42) | 3.67 | (1.39) | 0.55 | (0.07, 1.04) | 0.026 | 0.36 |
| Greens and beans | 3.25 | (1.61) | 3.73 | (1.63) | 3.34 | (1.81) | 3.47 | (1.68) | 0.35 | (−0.20, 0.90) | 0.212 | 0.2 |
| Whole grains | 7.16 | (2.06) | 7.86 | (1.98) | 7.39 | (2.11) | 7.33 | (2.22) | 0.77 | (0.09, 1.45) | 0.026 | 0.36 |
| Dairy | 5.03 | (3.02) | 5.08 | (3.18) | 4.75 | (2.99) | 4.93 | (2.87) | −0.13 | (−1.09, 0.82) | 0.783 | −0.04 |
| Total protein | 2.68 | (0.97) | 2.78 | (1.02) | 2.48 | (0.84) | 2.62 | (1.01) | −0.02 | (−0.35, 0.32) | 0.917 | −0.04 |
| Seafood/plant protein | 3.84 | (1.43) | 4.05 | (1.34) | 3.76 | (1.47) | 3.72 | (1.52) | 0.27 | (−0.24, 0.79) | 0.296 | 0.17 |
| Fatty acids | 4.96 | (2.54) | 5.57 | (2.86) | 5.29 | (2.86) | 4.93 | (2.47) | 1.09 | (0.20, 1.98) | 0.017 | 0.36 |
| Moderation: | ||||||||||||
| Refined grains | 5.21 | (2.54) | 5.03 | (2.58) | 4.49 | (2.43) | 5.06 | (2.23) | −0.68 | (−1.46, 0.10) | 0.089 | −0.31 |
| Sodium | 7.81 | (1.87) | 8.19 | (1.59) | 8.45 | (1.63) | 7.94 | (1.94) | 0.84 | (0.14, 1.54) | 0.019 | 0.51 |
| Empty calories | 8.03 | (4.23) | 8.26 | (4.48) | 6.91 | (4.27) | 7.85 | (3.77) | −0.52 | (−1.90, 0.86) | 0.455 | −0.17 |
| FCCH Provider Physical Activity | ||||||||||||
| MVPA min/day | 15.51 | (11.97) | 14.94 | (12.99) | 17.36 | (15.89) | 15.32 | (14.59) | 1.16 | (−3.89, 6.22) | 0.650 | 0.11 |
| Lifestyle min/day | 120.10 | (47.33) | 113.77 | (55.57) | 121.80 | (55.14) | 108.87 | (48.74) | 3.92 | (−9.94, 17.77) | 0.577 | 0.13 |
| Sedentary min/day | 396.17 | (100.42) | 409.57 | (136.14) | 408.04 | (95.10) | 401.62 | (96.24) | 21.28 | (13.30, 55.86) | 0.226 | 0.2 |
| FCCH Provider Weight | ||||||||||||
| BMI | 33.57 | (7.61) | 33.50 | (7.66) | 33.05 | (7.24) | 33.18 | (7.39) | −0.13 | (−0.68, 0.41) | 0.631 | −0.03 |
| FCCH Environment | ||||||||||||
| Overall Nutrition Score | 9.30 | (1.70) | 9.42 | (1.77) | 9.09 | (1.83) | 9.06 | (1.73) | 0.24 | (0.01, 0.47) | 0.040 | 0.09 |
| Foods provided | 2.15 | (0.27) | 2.13 | (0.28) | 2.05 | (0.25) | 2.05 | (0.27) | −0.03 | (−0.12, 0.06) | 0.542 | −0.09 |
| Beverages provided | 2.01 | (0.28) | 2.10 | (0.26) | 1.95 | (0.31) | 1.95 | (0.27) | 0.10 | (−0.01, 0.20) | 0.084 | 0.31 |
| Feeding environment | 1.45 | (0.20) | 1.49 | (0.23) | 1.36 | (0.22) | 1.37 | (0.20) | 0.04 | (−0.04, 0.12) | 0.339 | 0.17 |
| Feeding practices | 1.43 | (0.26) | 1.37 | (0.26) | 1.43 | (0.28) | 1.33 | (0.27) | 0.04 | (−0.06, 0.13) | 0.466 | 0.12 |
| Menus | 0.64 | (1.20) | 0.65 | (1.21) | 0.79 | (1.30) | 0.82 | (1.32) | 0.00 | ------ | ------ | −0.02 |
| Educ/prof development | 0.68 | (0.35) | 0.74 | (0.32) | 0.68 | (0.33) | 0.67 | (0.32) | 0.09 | (0.01, 0.16) | 0.02 | 0.22 |
| Nutrition policy | 0.94 | (0.70) | 0.94 | (0.72) | 0.86 | (0.59) | 0.89 | (0.58) | 0.00 | 0.00 | ------ | −0.05 |
| Overall Physical Activity Score | 13.14 | (2.16) | 13.19 | (2.37) | 12.83 | (2.08) | 12.36 | (2.34) | 0.54 | (−0.21, 1.29) | 0.154 | 0.25 |
| Time provided | 1.37 | (0.59) | 1.41 | (0.60) | 1.49 | (0.59 | 1.27 | (0.51) | 0.26 | (0.03, 0.49) | 0.028 | 0.44 |
| Indoor play equipment | 1.39 | (0.45) | 1.40 | (0.45) | 1.39 | (0.54) | 1.37 | (0.53) | 0.02 | (−0.18, 0.22) | 0.818 | 0.05 |
| Physical activity practices | 1.65 | (0.29) | 1.65 | (0.27) | 1.67 | (0.32) | 1.51 | (0.32) | 0.16 | (0.04, 0.27) | 0.009 | 0.52 |
| Outdoor playtime | 1.22 | (0.65) | 1.20 | (0.64) | 1.25 | (0.77) | 1.16 | (0.78) | 0.08 | (−0.15, 0.32) | 0.493 | 0.11 |
| Outdoor play environment | 1.30 | (0.37) | 1.17 | (0.34) | 1.28 | (0.39) | 1.19 | (0.39) | −0.04 | (−0.18, 0.10) | 0.572 | −0.12 |
| Educ/prof development | 0.37 | (0.39) | 0.46 | (0.39) | 0.37 | (0.37) | 0.32 | (0.32) | 0.15 | (0.04, 0.27) | 0.011 | 0.38 |
| Physical activity policy | 0.80 | (0.75) | 0.79 | (0.74) | 0.76 | (0.73) | 0.78 | (0.73) | 0.00 | ------ | ------ | −0.05 |
| Screen time | 2.40 | (0.56) | 2.47 | (0.54) | 2.23 | (0.54) | 2.31 | (0.54) | −0.03 | (−0.22, 0.16) | 0.755 | −0.04 |
| Screen time practices | 2.65 | (0.49) | 2.65 | (0.53) | 2.39 | (0.65) | 2.43 | (0.63) | −0.04 | (−0.24, 0.15) | 0.649 | −0.06 |
| Screen time policy | 1.01 | (0.37) | 1.00 | (0.36) | 0.98 | (0.31) | 0.99 | (0.30) | 0.00 | ------ | ------ | −0.07 |
| Business Practices | ||||||||||||
| Overall Score | 13.95 | (4.91) | 14.56 | (4.68) | 13.96 | (4.60) | 14.25 | (4.14) | 0.61 | (−0.93, 2.14) | 0.437 | 0.07 |
| Income and benefits | 2.16 | (2.00) | 1.91 | (1.88) | 2.01 | (1.83) | 1.61 | (1.49) | 0.15 | (−0.48, 0.77) | 0.641 | 0.08 |
| Recordkeeping | 2.34 | (1.62) | 3.00 | (1.98) | 2.42 | (1.73) | 2.53 | (1.58) | 0.67 | (0.10, 1.25) | 0.022 | 0.33 |
| Work environment | 5.48 | (2.15) | 4.89 | (2.48) | 4.87 | (2.40) | 5.16 | (2.22) | −0.79 | (−1.66, 0.07) | 0.073 | −0.39 |
| Communication | 1.78 | (1.08) | 1.84 | (1.06) | 1.96 | (1.25) | 1.99 | (1.10) | 0.00 | (−0.44, 0.44) | 0.999 | 0.03 |
| PR and marketing | 2.33 | (1.74) | 2.93 | (1.98) | 2.70 | (1.94) | 2.96 | (2.10) | 0.42 | (−0.21, 1.06) | 0.189 | 0.18 |
Note: Boldface indicates statistical significance (p<0.05).
Difference in mean change, 95% CI, and p-value reflect the fully adjusted model, controlling for baseline values; provider age, race, income, and BMI for provider outcomes; FCCH quality rating for nutrition/physical activity environment scores; and provider education and acceptance of CACFP subsidy for business practices.
Effect sizes calculated using Cohen’s d.
HEI, Healthy Eating Index; MVPA, moderate to vigorous physical activity; BMI, body mass index; Educ., education; Prof., professional; PR, public relations
FCCH Nutrition and Physical Activity Environments and Business Practices
FCCHs in the intervention arm significantly increased their nutrition environment scores relative to controls (+0.24, p=0.040). A similar increase was noted in the overall physical activity score, but this difference was not significant (+0.54, p=0.15). Environmental sub-scores showed significant improvement in time provided for physical activity, daily physical activity practices, and nutrition and physical activity education/professional development (for all p<0.028), with small to medium effect sizes.48 FCCHs in the intervention arm also had significant improvements in record keeping relative to those in the control arm (+0.68, p=0.022). FCCH outcomes are presented in Table 3.
Process Evaluation
Intervention participation was high; FCCH providers completed, on average, 2.9 workshops (2.2 in the group setting), 11.3 coaching contacts (averaging 423.5 minutes total), and 22.7 self-monitoring logs. FCCH providers passed, on average, 2.8 of the 3 knowledge assessments. Satisfaction with workshops and coaching were also highly rated, with scores ranging between 4.6 and 4.9 (out of 5).
DISCUSSION
Keys is the first randomized controlled trial to evaluate a FCCH-based nutrition and physical activity intervention for children. Results demonstrated significant improvements in children’s diet quality but not physical activity. Results also demonstrated significant improvements in FCCH providers’ diet quality and several aspects of their FCCH environments. Four previous quasi-experimental intervention studies with FCCHs demonstrate similar improvements in nutrition and physical activity practices;18–20,49 hence, FCCHs appear to be a malleable setting that can be improved to benefit children’s health. More intervention studies are needed to confirm essential content and strategies necessary to overcome critical barriers. Even with Keys’ comprehensive program (addressing FCCH providers’ health, FCCH environments, and FCCH business practices) and intensive delivery model (in-person workshops, home visits, and coaching contacts), effects were small to moderate and sometimes mixed.
Keys’ positive dietary findings suggest that FCCH-based nutrition interventions can produce similar improvements in children’s diets as center-based interventions.50 Intervention children had a 9% increase in HEI score overall. HEI component scores generally changed in the right direction, but like other intervention studies, not all changes were significant.51 The decrease in the vegetable component score warrants attention as it suggests an unintended negative impact on vegetable consumption, possibly from failing to redirect FCCH providers to healthier vegetables when discouraging fried and pre-fried potatoes. Additionally, some food groups may be easier to change (e.g., whole grains) while others (e.g., vegetables) may require more focused or intense intervention.52 Further analyses are needed to explore mediational pathways driving these changes. Improvements in FCCH providers’ diet quality may help explain improvements in children’s diet quality despite limited changes in the FCCH nutrition environment.
The non-significant physical activity findings suggest that FCCH providers encounter additional challenges that limit intervention impact. These results contrast several reviews of ECE center-based interventions which generally demonstrate physical activity improvements.51,53 Significant improvements were observed in several aspects of the FCCH environment, including time provided, daily practices, and education/professional development. While these environmental aspects are associated with children’s physical activity,54–56 improvements appeared insufficient to impact children’s behaviors. Additional analyses may aid our understanding of these mixed findings and whether the low physical activity of FCCH providers, and lack of change, moderated the impact of environmental improvements.
A key lesson from this study is the need to refine content for future FCCH interventions. A 2018 systematic review identified 17 studies describing FCCH environments as they relate to child diet, physical activity, and weight.14 It noted several problematic areas, including frequent use of coercive feeding practices, suboptimal space for active play, reliance on television, inadequate training, and lack of written policies. It should not be assumed, however, that recommendations based largely on center-based studies apply directly to FCCHs. Uniqueness of FCCHs may impact how these practices work to influence children’s behaviors. For example, data from FCCH-based studies have demonstrated that adequate indoor space is significantly associated with children’s physical activity, even more so than outdoor play space.57,58 Interventions may need to prioritize reorganizing FCCHs’ indoor environments to allow for more gross motor activities.57 Also, data from this study suggest that screen use is positively associated with children’s MVPA,59 which contradicts center-based research showing screens to be associated with sedentary time.60 Intervention messages about screens may need to offer active screen time resources that help engage children of different ages in gross motor activities.59 The Keys intervention did not significantly impact either of these aspects of the FCCH environment; hence, the lack of change in children’s physical activity may be explained by a failure to address critical environmental elements.
Another lesson from the Keys study is the importance of FCCH provider health. Baseline data demonstrated that most FCCH providers had at least four of six key health risk behaviors (e.g., excess weight, insufficient activity, inadequate fruit/vegetable intake, inadequate sleep, high stress, no health insurance).61 Most alarming was that close to 90% were FCCH providers with overweight or obesity. Poor health behaviors and attitudes, including uncertainty in their physical abilities, dislike of healthy foods, and lack of nutrition and physical activity knowledge, impair FCCH providers’ ability to be healthy role models and to adopt recommended practices.25,26,62 The contrast between diet and physical activity outcomes suggest that changing FCCH providers’ behaviors will support children’s behavior change.
Future FCCH intervention research would benefit from strategies that address economic barriers, which exist at two levels – FCCH providers and the families they serve. FCCHs have low profit margins, and studies have documented that limited time and resources are barriers to their adoption of recommended diet and physical activity practices.25,26 FCCHs are an appealing form of child care for low-income families given their lower enrollment fees and flexible schedules (e.g., accommodating shift work). The high rates of acceptance of child care subsidies and participation in CACFP is evidence that Keys’ FCCHs were serving low-income families. The Healthy Business module represented at least a modest attempt to address a key “root cause” of obesity, namely economic disadvantage common to the FCCH industry 63). Record keeping may be an easier business practice to adopt while others, such as developing new contracts or marketing, may require more practical examples and tools to support their use.
One study limitation was high attrition, caused primarily by enrollment turnover. Close monitoring of attrition allowed for quick adjustment of the sample size. Children lost to follow-up were similar to completers, suggesting that attrition did not unduly bias the sample. Another limitation was the sample’s homogeneity – mostly female FCCH providers, with overweight/obesity, and modest incomes. While recruitment efforts effectively targeted a low-income population at increased risk for adverse health outcomes, the sample homogeneity may limit the generalizability of findings.
CONCLUSION
In summary, the Keys intervention improved diets of children and caregivers but not physical activity. Future research should investigate strategies for working within the restrictive environments of FCCHs and improving training opportunities to better support physical activity. Future research should also examine practical strategies for integrating effective FCCH-based interventions into child care systems (e.g., CACFP, quality rating and improvement systems) that serve predominantly child care centers.
Supplementary Material
Acknowledgements:
We thank Tom Copeland, Red Leaf Press, for his assistance developing the Healthy Business content. We also thank the FCCH providers, parents, and children who participated.
Funding: This work was supported by the National Heart, Lung, and Blood Institute (HL108390), the Centers for Disease Control and Prevention (U48-DP005017), and the National Institute of Diabetes and Digestive and Kidney Diseases (DK056350). Content is solely the responsibility of the authors and does not represent the official views of any funders.
Competing interest statement: Drs. Ward, Burney, Hales, Benjamin-Neelon, Tovar, Østbye, and Mrs. Vaughn have been funded by the National Heart, Lung, and Blood Institute (HL108390).
Abbreviations:
- BMI
body mass index
- CACFP
child and adult care food program
- ECE
early care and education
- EPAO
environment and policy assessment and observation
- FCCH
family child care home
- FFQ
food frequency questionnaire
- HEI
healthy eating index
- MVPA
moderate to vigorous physical activity
Footnotes
Data availability: Deidentified data will be shared following publication provided the investigator seeking the data has approval from an Institutional Review Board, Independent Ethics Committee, or Research Ethics Board, and executes a data use/sharing agreement with UNC.
Trial registration: This study is registered at www.clinicaltrials.gov NCT01814215.
REFERENCES
- 1.Emmett PM, Jones LR. Diet, growth, and obesity development throughout childhood in the Avon Longitudinal Study of Parents and Children. Nutrition Reviews. October 2015;73 Suppl 3:175–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaikkonen JE, Mikkila V, Magnussen CG, Juonala M, Viikari JS, Raitakari OT. Does childhood nutrition influence adult cardiovascular disease risk?--insights from the Young Finns Study. Annals of Medicine. March 2013;45(2):120–128. [DOI] [PubMed] [Google Scholar]
- 3.Berenson GS, Srinivasan SR, Nicklas TA. Atherosclerosis: a nutritional disease of childhood. American Journal of Cardiology. November 26 1998;82(10B):22T–29T. [DOI] [PubMed] [Google Scholar]
- 4.Carson V, Lee EY, Hewitt L, et al. Systematic Review of the relationships between physical activity and health indicators in the early years (0–4 years). BMC Public Health. 2017;17(Supp5):854–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kovacs E, Siani A, Konstabel K, et al. Adherence to the obesity-related lifestyle intervention targets in the IDEFICS study. International Journal of Obesity. September 2014;38 Suppl 2:S144–S151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ling J, Robbins LB, Wen F, Zhang N. Lifestyle Interventions in Preschool Children: A Meta-analysis of Effectiveness. American Journal of Preventive Medicine. July 2017;53(1):102–112. [DOI] [PubMed] [Google Scholar]
- 7.Story M, Kaphingst KM, French S. The role of child care settings in obesity prevention. Future of Children. Spring 2006;16(1):143–168. [DOI] [PubMed] [Google Scholar]
- 8.National Center for Education Statistics. Percentage of 3-, 4-, and 5-year-old children enrolled in preprimary programs, by level of program, attendance status, and selected child and family characteristics: 2016. 2017; https://nces.ed.gov/programs/digest/d17/tables/dt17_202.20.asp. Accessed May 8, 2019.
- 9.Baxter JA. Child care and early childhood education in Australia (Facts Sheet 2015). 2015; https://aifs.gov.au/publications/child-care-and-early-childhood-education-australia. Accessed October 16, 2019. [Google Scholar]
- 10.Bos JM, Phillips-Fain G, Rein E, Weinberg E, Chavez S. Connecting All Children to High-Quality Early Care and Education: Promising strategies from the international community. Washington, DC: American Institutes for Research.; October 2016. [Google Scholar]
- 11.Child Care Aware of America. Checking In: A Snapshot of the Child Care Landscape. 2017; https://usa.childcareaware.org/wp-content/uploads/2017/07/FINAL_SFS_REPORT.pdf. Accessed May 3,, 2018. [Google Scholar]
- 12.Benjamin SE, Copeland KA, Cradock A, et al. Menus in child care: a comparison of state regulations with national standards. Journal of the American Dietetic Association. January 2009;109(1):109–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duffey KJ, Slining MM, Benjamin Neelon SE. States lack physical activity policies in child care that are consistent with national recommendations. Childhood Obesity. December 2014;10(6):491–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Francis L, Shodeinde L, Black MM, Allen J. Examining the Obesogenic Attributes of the Family Child Care Home Environment: A Literature Review. Journal of Obesity. 2018;2018:3490651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trost SG, Messner L, Fitzgerald K, Roths B. Nutrition and physical activity policies and practices in family child care homes. American Journal of Preventive Medicine. December 2009;37(6):537–540. [DOI] [PubMed] [Google Scholar]
- 16.Christakis DA, Garrison MM. Preschool-aged children’s television viewing in child care settings. Pediatrics. December 2009;124(6):1627–1632. [DOI] [PubMed] [Google Scholar]
- 17.Black L, Matvienko-Sikar K, Kearney PM. The association between childcare arrangements and risk of overweight and obesity in childhood: a systematic review. Obesity reviews : an official journal of the International Association for the Study of Obesity. October 2017;18(10):1170–1190. [DOI] [PubMed] [Google Scholar]
- 18.Trost SG, Messner L, Fitzgerald K, Roths B A nutrition and physical activity intervention for family child care homes. American Journal of Preventive Medicine. 2011;41(4):392–398. [DOI] [PubMed] [Google Scholar]
- 19.Woodward-Lopez G, Kao J, Kuo ES, et al. Changes in Nutrition Policies and Dietary Intake in Child Care Homes Participating in Healthy Eating and Active Living Initiative. American Journal of Preventive Medicine. May 2018;54(5S2):S170–S177. [DOI] [PubMed] [Google Scholar]
- 20.Kao J, Woodward-Lopez G, Kuo ES, et al. Improvements in Physical Activity Opportunities: Results From a Community-Based Family Child Care Intervention. American Journal of Preventive Medicine. May 2018;54(5S2):S178–S185. [DOI] [PubMed] [Google Scholar]
- 21.Dinkel D, Dev D, Guo Y, et al. Improving the Physical Activity and Outdoor Play Environment of Family Child Care Homes in Nebraska Through Go Nutrition and Physical Activity Self-Assessment for Child Care. Journal of Physical Activity and Health. October 1 2018;15(10):730–736. [DOI] [PubMed] [Google Scholar]
- 22.Østbye T, Mann CM, Vaughn AE, et al. The Keys to Healthy Family Child Care Homes intervention: Study design and rationale. Contemporary clinical trials. January 2015;40:81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mann CM WD, Vaughn A, Benjamin Neelon SE, Long Vidal LJ, Omar S, Namenek Brouwer RJ, Østbye T. Application of the intervention mapping protocol to develop Keys, a family child care home intervention to prevent early childhood obesity. BMC Public Health. 2015;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ward DS, Vaughn AE, Burney RV, Østbye T. Recruitment of family child care homes for an obesity prevention intervention study. Contemporary Clinical Trials Communications. 2016;3:131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hughes CC, Gooze RA, Finkelstein DM, Whitaker RC. Barriers to obesity prevention in Head Start. Health Affairs. Mar-Apr 2010;29(3):454–462. [DOI] [PubMed] [Google Scholar]
- 26.Copeland KA, Kendeigh CA, Saelens BE, Kalkwarf HJ, Sherman SN. Physical activity in child-care centers: do teachers hold the key to the playground? Health Education Research. February 2012;27(1):81–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. Winter 1988;15(4):351–377. [DOI] [PubMed] [Google Scholar]
- 28.Bandura A. Social foundations of thought and action. A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 29.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist January 2000;55(1):68–78. [DOI] [PubMed] [Google Scholar]
- 30.Dunst CJ TC, Hamby DW. Meta-analysis of the effectiveness of four adult learning methods and strategies. International Journal of continuing education and lifelong learning. 2010;3(1):91–112. [Google Scholar]
- 31.Miller WR, Rollnick S. Motivational Interviewing : Preparing People for Change. New York: Guilford Press; 2002. [Google Scholar]
- 32.Ball SC, Benjamin SE, Ward DS. Development and reliability of an observation method to assess food intake of young children in child care. Journal of the American Dietetic Association. April 2007;107(4):656–661. [DOI] [PubMed] [Google Scholar]
- 33.Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. Journal of the Academy of Nutrition and Dietetics. April 2013;113(4):569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring). November 2006;14(11):2000–2006. [DOI] [PubMed] [Google Scholar]
- 35.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. Journal of Sports Sciences. December 2008;26(14):1557–1565. [DOI] [PubMed] [Google Scholar]
- 36.Reilly JJ, Coyle J, Kelly L, Burke G, Grant S, Paton JY. An objective method for measurement of sedentary behavior in 3- to 4-year olds. Obesity Research. October 2003;11(10):1155–1158. [DOI] [PubMed] [Google Scholar]
- 37.de Onis M, Onyango AW, Van den Broeck J, Chumlea WC, Martorell R, for the WHO Multicentre Growth Reference Study Group. Measurement and standardization protocols for anthropometry used in the construction of a new international growth reference. Food and Nutrition Buletin. 2004;25(Suppl 1):S27–S36. [DOI] [PubMed] [Google Scholar]
- 38.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000. CDC Growth Charts for the United States: methods and development. Vital and Health Statistics. Series 11: Data from the National Health Survey. 2002(246):1–190. [PubMed] [Google Scholar]
- 39.WHO Multicentre Growth Reference Study Group. WHO child growth standards based on length/height, weight, and age. Aca Paediatr Suppl 2006;450:76–85. [DOI] [PubMed] [Google Scholar]
- 40.Block G, Hartman AM, Naughton D. A reduced dietary questionnaire: development and validation. Epidemiology. January 1990;1(1):58–64. [DOI] [PubMed] [Google Scholar]
- 41.Tovar A, Vaughn A, Burney R, Fede J, Østbye T, Ward DS. Predictors of feeding practices among family child care home American Society for Nutrition Annual Meeting. Boston, MA: 2018. [Google Scholar]
- 42.Troiano RP. Translating accelerometer counts into energy expenditure: Advancing the quest. Journal of Applied Physiology. 2006;100(4):1107–1108. [DOI] [PubMed] [Google Scholar]
- 43.Matthews CE. Calibration of Accelerometer Output for Adults. Medicine and Science in Sports and Exercise. November 2005;37(11):S512–S522. [DOI] [PubMed] [Google Scholar]
- 44.Vaughn AE, Mazzucca S, Burney R, Østbye T, Benjamin-Neelon SE, Tovar A, Ward DS Assessment of nutrition and physical activity environments in family child care homes: Modification and psychometric testing of the Environment and Policy Assessment and Observation. BMC Public Health. 2017;17(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Talan TNB, Jorde P. Business Administration Scale for Family Child Care, BAS. New York, NY: Teachers College Press; 2009. [Google Scholar]
- 46.Moser EB. Repeated Measures Modeling with PROC MIXED, paper 188–29 presented at SAS Users’ Group International: SAS Institute Inc.; 2004:1–19. [Google Scholar]
- 47.Allison P. Handling Missing Data by Maximum Likelihood, paper 312–2012 presented at the SAS Global Forum: SAS Institute Inc.; 2012:1–21. [Google Scholar]
- 48.Cohen J. Statistical Power Analysis for the Behavioural Sciences. 2nd ed. New Jersey: Lawrence Earlbaum Associates, Inc.; 1988. [Google Scholar]
- 49.Dinkel D, Dev D, Guo Y, et al. Improving the Physical Activity and Outdoor Play Environment of Family Child Care Homes in Nebraska Through Go Nutrition and Physical Activity Self-Assessment for Child Care. Journal of physical activity & health. May 9 2018:1–7. [DOI] [PubMed] [Google Scholar]
- 50.Matwiejczyk L, Mehta K, Scott J, Tonkin E, Coveney J. Characteristics of Effective Interventions Promoting Healthy Eating for Pre-Schoolers in Childcare Settings: An Umbrella Review. Nutrients. March 1 2018;10(3):293–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ward DS, Welker E, Choate A, et al. Strength of obesity prevention interventions in early care and education settings: A systematic review. Preventive Medicine. February 2017;95 Suppl:S37–S52. [DOI] [PubMed] [Google Scholar]
- 52.Fisher JO, Dwyer JT. Next Steps for Science and Policy on Promoting Vegetable Consumption among US Infants and Young Children. Adv Nutr January 2016;7(1):261S–271S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sisson SB, Krampe M, Anundson K, Castle S. Obesity prevention and obesogenic behavior interventions in child care: A systematic review. Preventive Medicine. June 2016;87:57–69. [DOI] [PubMed] [Google Scholar]
- 54.Bower JK, Hales DP, Tate DF, Rubin DA, Benjamin SE, Ward DS. The childcare environment and children’s physical activity. American Journal of Preventive Medicine. January 2008;34(1):23–29. [DOI] [PubMed] [Google Scholar]
- 55.Gubbels JS, Kremers SP, van Kann DH, et al. Interaction between physical environment, social environment, and child characteristics in determining physical activity at child care. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. January 2011;30(1):84–90. [DOI] [PubMed] [Google Scholar]
- 56.Sugiyama T, Okely AD, Masters JM, Moore GT. Attributes of Child Care Centers and Outdoor Play Areas Associated with Preschoolers’ Physical Activity and Sedentary Behavior. Environment and Behavior 2012;44(3):334–349. [Google Scholar]
- 57.Neshteruk CD, Mazzucca S, Ostbye T, Ward DS. The physical environment in family childcare homes and children’s physical activity. Child: Care, Health and Development. June 6 2018;44(5):746–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gunter KB, Rice KR, Ward DS, Trost SG. Factors associated with physical activity in children attending family child care homes. Preventive Medicine. February 2012;54(2):131–133. [DOI] [PubMed] [Google Scholar]
- 59.Mazzucca S, Neshteruk C, Burney R, et al. Physical activity and sedentary behaviors of children in family child care homes: Are there opportunities for improvement? Pediatric Exercise Science. November 1 2018;30(4):529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vanderloo LM. Screen-viewing among preschoolers in childcare: a systematic review. BMC Pediatr August 16 2014;14:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tovar A, Vaughn AE, Grummon A, et al. Family child care home providers as role models for children: Cause for concern? Prev Med Rep March 2017;5:308–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sharma S, Dortch KS, Byrd-Williams C, et al. Nutrition-related knowledge, attitudes, and dietary behaviors among head start teachers in Texas: a cross-sectional study. Journal of the Academy of Nutrition and Dietetics. April 2013;113(4):558–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Child Care Aware of America. The US and the high cost of child care: A review of prices and proposed solutions for a broken system. Arlington, VA: 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


