Abstract
Introduction
The coronavirus disease 2019 (COVID-19) was defined as a species of beta coronavirus causing atypical respiratory disease in humans. The COVID-19 pandemic has resulted in an unprecedented health and economic crisis worldwide. Little is known about the specifics of its influence on people living with human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) (PLWHA). In this study, we aim to investigate the prevalence and mortality in PLWHA co-infected with COVID-19.
Methods
The databases PUBMED, EMBASE, BioRxiv, and medRxiv were searched up to 9 March 2021 to explore the prevalence and mortality rate of COVID-19 in PLWHA. Cohort studies and case series meeting the inclusion criteria were included in this review.
Results
We identified 14 eligible studies, 9 of which were cohort and 5 were case series. A total of 203,761 patients with COVID-19 were identified (7718 PLWHA vs. 196,043 non-PLWHA). Meta-analyses estimated the prevalence and mortality rate of COVID-19 in PLWHA was 0.774% [95% confidence interval (CI) 0.00393–0.01517] and 8.814% (95% CI 0.05766–0.13245) respectively. COVID-19 co-infected PLWHA do not seem to be associated with higher mortality, as compared to non-PLWHA [relative risk (RR) 0.96 (95% CI 0.88–1.06)]. The presence of comorbidities such as diabetes mellitus, RR 5.2 (95% CI 4.25–6.36), hypertension and chronic cardiac disease, RR 4.2 (95% CI 1.09–16.10), and chronic kidney disease, RR 8.43 (95% CI 5.49–12.93) were associated with an increased mortality in COVID-19 co-infected PLWHA.
Conclusion
The estimated prevalence and mortality rate of COVID-19 in PLWHA were 0.774% and 8.814%, respectively. Since most of the included studies used unmatched populations, comparisons between PLWHA and non-PLWHA should be interpreted with caution. Further investigations are needed for a more comprehensive understanding of the relationship between cluster of differentiation 4 cell count, HIV viral load, antiretroviral therapy, and COVID-19 related prognosis in PLWHA.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40121-021-00447-1.
Keywords: COVID-19, HIV, Meta-analysis, Prevalence, Prognosis, Systematic review
Key Summary Points
| Why carry out this study? |
| The coronavirus disease 2019 (COVID-19) pandemic has become a major public health crisis globally. The correlation between human immunodeficiency virus (HIV) and COVID-19 remains unclear. |
| People living with HIV/acquired immunodeficiency syndrome (AIDS) (PLWHA) are generally thought to be at a higher risk for developing a severe course and outcome of COVID-19 infection due to immunodeficiency. Therefore, there is an underlying interest to investigate the impact of COVID-19 on this population. |
| What was learned from the study? |
| This study defined a total of 203,761 patients with COVID-19 (7718 PLWHA vs. 196,043 non-PLWHA). Meta-analyses showed estimated prevalence and mortality rate of COVID-19 in PLWHA was 0.774% and 8.814%, respectively. |
| This study indicated increased mortality among COVID-19 co-infected PLWHA having co-morbid conditions such as diabetes mellitus, chronic kidney disease, hypertensionand chronic cardiac disease. |
| No statistical significance was observed in mortality between PLWHA and non-PLWHA. |
| Further studies are needed to address the role of cluster of differentiation 4 cells, HIV viral load, and antiretroviral therapy in COVID-19 co-infection. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14381498.
Introduction
Since coronavirus disease 2019 (COVID-19) emerged in China in late 2019, it has proven to be an urgent threat to global health. As of 21 March 2021, COVID-19 has affected 215 countries and territories, resulting in more than 100 million identified cases and 27 million confirmed deaths [1]. Global statistics from 2019 show approximately 38 million people chronically infected with human immunodeficiency virus (HIV) [2]; therefore, there has been a deep interest to explore the impact of COVID-19 infection among people living with HIV/acquired immunodeficiency syndrome (AIDS) (PLWHA). However, the prevalence and prognosis, as well as other clinical characteristics of COVID-19 co-infected PLWHA, have not been studied extensively. A recent cohort study by Had et al. of 404 HIV patients showed no statistical significance in mortality due to COVID-19 co-infection when compared to a matched control population [3]. Conversely, two cohort studies conducted by Boulle et al. [4] (3978 HIV patients) and Huang et al. [5] (6001 HIV patients) indicated that HIV was associated with higher mortality as compared to controls. However, the prevalence and prognosis of COVID-19 and the role of other characteristics [e.g., age, comorbidities, HIV viral load, cluster of differentiation 4 (CD4) cell count, and antiretroviral therapy (ART)] during infection in this population is not clear. Hence, a systematic review and meta-analysis will help to summarize the results.
Methods
Protocol and Registration
This meta-analysis was conducted in accordance with the statement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) [6]. The registration number for the international prospective register of systematic review (PROSPERO) is CRD42021231640. The primary outcome for this systematic review and meta-analysis is the prevalence and mortality rate of COVID-19 in PLWHA. Additional outcomes included mortality comparison in PLWHA and non-PLWHA due to COVID-19 co-infection, as well as the roles of comorbidity, CD4 cells, ART, and HIV viral load in COVID-19-related outcomes in PLWHA. Subgroup analyses were conducted based on the study population and country.
Eligibility Criteria
We included preprints to capture emerging evidence. Studies reporting the following data were considered for inclusion: (1) investigated clinical outcomes of COVID-19 co-infection in PLWHA, including prevalence, mortality, need for intensive care support, comorbidity, duration of hospitalization, and recovery; (2) laboratory findings: inflammation biomarkers during hospitalization, HIV viral load, and count of CD4 cells prior to the co-infection; and (3) validated diagnostic criteria of COVID-19 and accurate study dates.
Exclusion criteria were as follows: (1) studies without available data for synthesis; and (2) single case reports, case series with a reported number of participants less than 15, review editorials, and conference abstracts. There were no restrictions regarding age, sex, or duration of the study.
Detailed studies with large populations and multi-center involvement were preferred for this review as these reduced deviations and met requirements for studies conducted in the same region/country and having a population overlap.
Electronic Search
A systematic search was independently performed by two authors through electronic databases, including PUBMED, EMBASE, BioRxiv, and medRxiv, which were searched up to 9 March 2021 with the publication language restricted to English. Studies were retrieved by utilizing medical subject headings (MeSH) and MeSH-derived topical terms. Our search term for PUBMED was ((“COVID-19” OR “2019 novel coronavirus disease” OR “COVID19” OR “COVID-19 pandemic” OR “SARS-CoV-2 infection” OR “COVID-19 virus disease” OR “2019 novel coronavirus infection” OR “2019-nCoV infection” OR “coronavirus disease 2019” OR “coronavirus disease-19” OR “2019-nCoV disease” OR “COVID-19 virus infection”) AND (“HIV” OR “Human Immunodeficiency Virus*” OR “Human T Cell Lymphotropic Virus Type III” OR “Human T-Cell Leukemia Virus Type III” OR “LAV-HTLV-III” OR “Lymphadenopathy-Associated Virus*” OR “Human T Lymphotropic Virus Type III” OR “AIDS Virus*” OR “Acquired Immun* Deficiency Syndrome Virus” OR “HTLV-III”)).
Study Selection
Articles that were considered to be potentially relevant to the topic were obtained in full text. Two independent reviewers (Shivank, S. and Shantanu, S.) performed the search, two independent reviewers screened the titles, abstracts, and full texts (C.N.C. and M.F.C.), and disputes were resolved by consensus or consultation with the supervisors (M.L. and S.F.T.).
Data Collection Process
The following information was extracted from each included study: (1) first author’s name, year of publication; (2) location; (3) study design; (4) comparison or control; (5) sample size; (6) patient characteristics: median age; (7) ART; (8) confirmation method for COVID-19; and (9) outcome: mortality. Data were extracted by three authors (C.N.C, S.F.T, and N.L.) and validated by a fourth author (Shantanu. S.).
Risk of Bias of Individual Studies
The quality assessment for the case series was conducted in accordance with the Joanna Briggs Institute (JBI) checklist for case series [7]. The JBI checklist for case series rates the quality of selection, measurement, and comparability of studies, giving a score ranging from 0 to 10. For cohort studies, biases were assessed with the Newcastle–Ottawa scale, which included ratings of selection bias, comparability issues, and outcome reporting bias [8]. Two reviewers (C.N.C. and N.L.) assessed the risk of bias for each study independently. Any disagreement was resolved by consultation with the supervisors (M.L. and S.F.T.).
Statistical Methods
We calculated prevalence estimates using the variance of the ‘logit of accuracy indices’, since the weightage of inverse variance in meta-analysis is sub-optimum while dealing with data having non-normal distribution and low prevalence [9]. For dichotomous outcomes, we calculated the relative risk (RR) with 95% confidence interval (CI). We assessed for statistical heterogeneity by visual inspection of the forest plot and calculation of the Higgin's I2 statistic [10]. According to the Cochrane Handbook for Meta-analysis, when meta-analysis was possible because of acceptable clinical and methodological heterogeneity, we reported the fixed-effects model summary estimate for I2 < 25% and the random-effects model summary estimate for I2 > 25% [11]. We expected the existence of heterogeneity (I2 > 25%), due to concerns of study design, the number in the population, and varied statistical approaches in studies. Therefore, meta-analyses were performed based on a randomized effect model in this review. Meta-analyses and forest plots were performed in R (v.4.0.2; R Foundation for Statistical Computing, Vienna, Austria), using the meta-package [12].
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies of human participants or animals performed by any of the authors.
Results
Study Selection
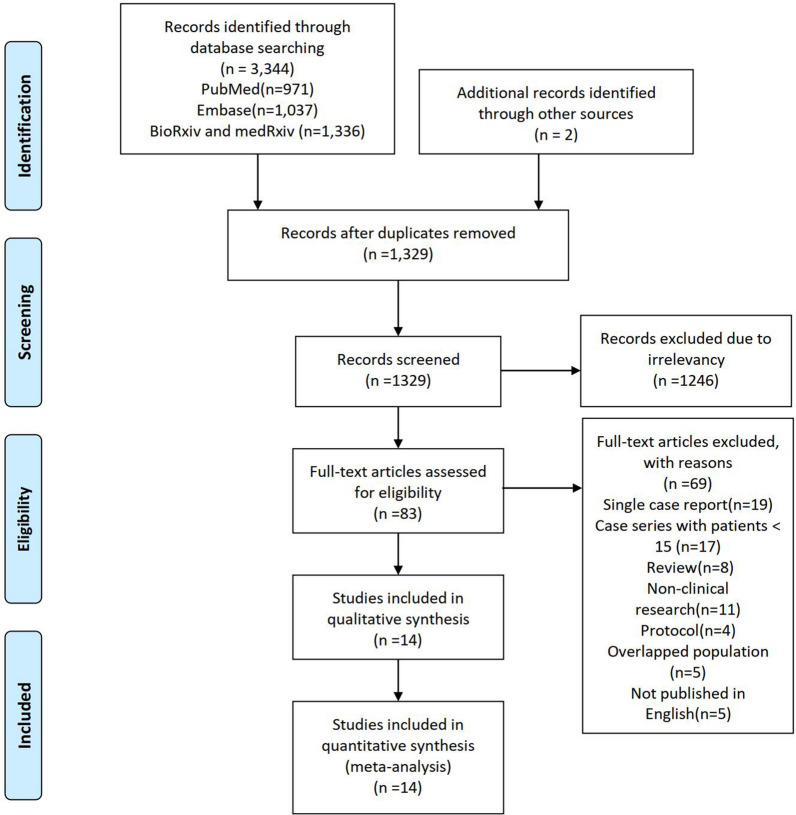
The primary outcome of interest for this review was the prevalence of COVID-19 in PLWHA and the mortality rate in those who were co-infected with COVID-19. A total of 3,344 articles were retrieved from electronic databases up to 9 March 2021. After the removal of irrelevancy and duplicates, 83 articles were taken for full-text screening, and, finally, 14 studies providing outcomes of interest were included for review [4, 5, 13–24]. Of these included studies 13 were peer-reviewed, while 1 case series was unpublished [19]. A PRISMA flow chart for the literature search is shown in Fig. 1.
Fig. 1.
PRISMA flowchart of literature search and study selection
Study Characteristics
A total of 203,761 patients with COVID-19 were identified (7,718 PLWHA vs. 196,043 non-PLWHA). To assess the prevalence of COVID-19 in PLWHA, a total of 757,103 patients were included. Table 1 outlines the characteristics and data extracted from the included studies. Nine studies were of cohort design [4, 5, 13, 15, 17, 18, 20–22] and the other five were case series [14, 16, 19, 23, 24]. Only one cohort study used matched population design while comparing PLWHA and non-PLWHA[21]. Seven of the studies were conducted in Europe (England, UK [18], Italy [14, 20], Spain [13], France [17]), Germany [24], and Central/East European countries [19]. The others were from Asia (China [5]), Africa (Western Cape [4]), North America (United States [16, 21–23]), and South America (Chile [15]), respectively. Four of the cohort studies used a mass database(provincial/national) for population recruitment [4, 5, 18, 22], another two had a multi-center involvement [13, 15], and three studies had a single-center involvement [17, 20, 21]. Four out of the five case series were of a multi-center design [14, 16, 19, 24]. For analysis of COVID-19 prevalence in PLWHA, we identified six studies with a population total of 757,103 patients. For analysis of mortality due to COVID-19 in PLWHA, 14 studies were included, with a total of 5626 patients. For comparison of mortality due to COVID-19 between PLWHA and non-PLWHA, six studies with a total number of 5,090 PLWHA and 195,812 non-PLWHA patients were included. Additionally, four studies provided data of comorbidities among PLWHA and non-PLWHA, which enabled us to perform a comparison for the risk of COVID-19 co-infection based on various comorbidities in the two groups. Only two of the included studies reported data of CD4 count and HIV viral load before/during hospitalization between COVID-19-infected and non-COVID-19-infected PLWHA [5, 20]. However, since the reported data of these two items were not standardized, this resulted in the infeasibility of determining the role of either of the two crucial factors in the risk of COVID-19 co-infection in this population. Also, due to insufficient data reported in studies, we failed to assess socio-demographic disparities (e.g., age, sex, ethnicity) of COVID-19 co-infection in PLWHA.
Table 1.
Characteristics of trials included in the systematic review and meta-analyses
| Source | Study design | Country/region | Data source | Identified case of COVID-19 (n) | Median age (IQR) | Diagnostic methods for COVID-19 | CD4 cells/HIV VL | Patient on ART (%) | Most reported comorbidities | Mortality patient (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Boulle [4] | Provincial-based cohort study | Western Cape province, South Africa | Using data from the WCPHDC of public sector, patients aged ≥ 20 years with documented sex and not known to have died before 1 March 2020 and follow-up through 9 June 2020 | 3978 PLWHA vs. 18,330 non-PLWHA | 41 years in PLWHA vs. 40.6 years in non-PLWHA | SARS-CoV-2 PCR test | 7.6% with VL > 1000 copies/ml or CD4 cell count < 200 cells/ml, 34.7% with VL unknown in past 15 months | Not reported in detail | DM; HTN; CKD; Chronic pulmonary disease / asthma | 115 (3%) PLWHA vs. 510 (2.8%) non-PLWHA |
| Geretti [18] | Prospective cohort study | England, UK | Using the ISARIC WHO CCP-UK database, people aged ≥ 18 years and admitted to participating hospital(207atthetime) with either laboratory-confirmed or highly likely COVID-19 infection | 122 PLWHA vs. 47,470 non-PLWHA | 56 years in PLWHA vs. 74 years in non-PLWHA | Either laboratory confirmed or highly likely infection | Not reported | 25 (83%) on ART deceased vs. 87 (94%) on ART alive | Chronic cardiac disease; Chronic pulmonary disease; CKD; DM; Obesity; Chronic neurological disorder; Dementia; Liver disease; Cancer; Chronic hematological disease; Rheumatological disease; Malnutrition | 30 (24.5%) PLWHA vs. 13,969 (29.4%) non-PLWHA |
| Huang [5] | Cohort | Wuhan City, China | Using systems of NNIDRS and CRIMS, PLWHA included with confirmed, clinically diagnosed, suspected, and asymptomatic cases | 35 PLWHA vs. 50,333non-PLWHA | 37 years in PLWHA | SARS-CoV-2 PCR test, suspected, clinically diagnosed | CD4 count: 200–499 cells/ml; 66% VL < 20 copies/ml | 32 (91.4%) on ART | Not reported | 2 (5.7%) PLWHA vs. 3869 (7.7%) non-PLWHA |
| Biagio [14] | Multi-center Case series | Italy | Using data from Infectious Diseases Departments participating in the CISAI study group, PLWHA referred to the centers with a diagnosis of COVID-19 | 69 PLWHA | 53 years | SARS-CoV-2 PCR test | Not reported | Not reported in detail | HTN; DM; CVD; | 7 patients deceased |
| Amo [13] | Multi-center Cohort | Spain | PLWHA referred to 60 Spain hospitals with COVID-19 diagnosis between 1 February and 15 April 2020 and data from the 2019 National HIV Hospital Survey | 236 PLWHA | 55.8 years | SARS-CoV-2 PCR test | Not reported | 100% on ART | Not reported | 20 patients deceased |
| Maggiolo [20] | Single center, prospective cohort | Italy | Not reported | 55 PLWHA | 54 (49–48) years | SARS-CoV-2 PCR test | CD4 count:904 (557–1110) cells/μl; 98% VL < 50 copies/ml | 100% on ART | CVD; HTN; Cancer; DM | 4 patients deceased |
| Etienne [17] | Single center, prospective cohort | Paris, France |
Consecutive PLWHA taken in care in the department and having developed COVID-19 clinical symptoms and/or hospi- talized for COVID-19 in the hospital |
54 PLWHA | 54 (47–60) years | Not reported | CD4 count: 583 (474–773) cells/μl; 96.2% VL < 40 copies/ml | 100% on ART | DM; HTN; CKD; Respiratory disease; Cirrhosis; Cancer; CVD | 1 patient deceased |
| Meyerowitz [23] | Single center Case series | Massachusetts, USA | PLWHA with confirmed COVID-19 infection hospitalized in a local hospital | 36 PLWHA | 53.4 years | SARS-CoV-2 nasopharyngeal swab PCR | CD4 count: 691 cells/μl; No report in VL | 35 (97.2%) on ART | DM, HTN, NASH, HLD, COPD | 2 patients deceased |
| Collins[16] | Multi-center Case series | Georgia, USA | PLWHA with confirmed COVID-19 infection in three of the local centers | 20 PLWHA | 57 (48–62) years | SARS-CoV-2 PCR test | CD4 count:425 (262–815) cells/μl; 90% VL < 200 copies/ml | 19 (95%) on ART | HTN, DM, Chronic lung disease, CKD | 3 patients deceased |
| Härter [24] |
Multi-center Case series |
Germany | PLWHA with confirmed COVID-19 infection in German HIV centers | 33 PLWHA | 48 years | SARS-CoV-2 PCR test | CD4 count: > 350 cells/μl; 94% virally suppressed | 100% on ART | DM; HTN; COPD; CVD; CKD; Hepatitis B infection | 3 patients deceased |
| Kase [19] | Case series | 12 countries in central and eastern Europe | PLWHA with confirmed COVID-19 infection in ECEE Network Group | 34 PLWHA | 42.7 years | SARS-CoV-2 PCR test | CD4 count:558 (312–719) cells/μl;53% VL < 50 copies/ml | 15 (44.1%) on ART |
CVD; Chronic lung disease; DM; Obesity; Hepatitis C infection; Hepatitis B infection |
3 patients deceased |
| Nagarakanti [21] | Single center, retrospective cohort, matched designed | New Jersey, USA | PLWHA with confirmed COVID-19 infection in a local medical center | 23 PLWHA vs. 254 non-PLWHA | 59 (51–67) years in PLWHA vs 62 (50–74) years in non-PLWHA | SARS-CoV-2 PCR test | Not reported | 15 (65.2%) on ART | HTN; DM; CKD; CAD; COPD | In hospital deceased: 3 (13%) PLWHA vs. 6 (2.4%) non-PLWHA |
| Tesoriero [22] | Multi-center, cohort | New York, USA | The NYS HIV surveillance registry, ECLRS, and SHIN-NY | 2988 PLWHA vs. 375,260 non-PLWHA | 54 years in PLWHA vs. 63 years in non-PLWHA | SARS-CoV-2 PCR test | Not reported | Not reported | Not reported | In hospital deceased: 207(23.1%) PLWHA vs 14,522(23.6%) non-PLWHA |
| Ceballos [15] | Multi-center, prospective cohort | Chile | PLWHA with confirmed COVID-19 infection hospitalized in 23 hospitals in Chile | 36 PLWHA vs. 4360 non-PLWHA | 44 (26–85) years in PLWHA; unavailable in non-PLWHA | SARS-CoV-2 PCR test | CD4 count:202 (168–446) cells/μl; 55% VL < 50 copies/ml | 30 (83%) on ART | DM; HTN; Obesity; COPD; Asthma; CKD; Chronic liver disease; CVD; Cancer; | 5(13.9%) PLWHA vs 4,360(23.8%) non-PLWHA |
-PLWHA People living with immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), IQR Interquartile range, WCPHDC Western Cape Provincial Health Data Center, ISARIC International severe acute respiratory and emerging infections consortium, WHO CCP-UK World Health Organization–clinical characterization protocol–United Kingdom, VL viral load, ART antiretroviral therapy, PCR polymerase chain reaction, NNIDRS national notifiable infectious disease report system, CRIMS China national HIV/AIDS comprehensive response information management, CISAI Coordinamento italiano per lo studiodell’infezione da HIV e Allergie, ECLRS Electronic clinical laboratory reporting system, SHIN-NY State health information network for New York, NYS New York State, ECEE Central and Eastern Europe, DM diabetes mellitus, HTN hypertension, NASH nonalcoholic steatohepatitis, HLD hyperlipidemia, COPD chronic obstructive pulmonary disease, CKD chronic kidney disease, CAD coronary artery disease, CVD cardiovascular diseases
Risk of Bias Within Studies
The risk of bias assessment of the included studies and reasons for judgment are presented in Tables 2 and 3. Overall, cohorts and case series were assessed to have a moderate risk of bias. The average score among cohort studies was 6 points out of 9 (varying between 5 and 9 points individually). Under-reporting of the non-exposed group, retrospective design, and inadequate follow-up contribute to various disadvantages of the cohort studies. The average score among case series was 6 points out of 10 (varying between 3 and 9 points of inter-agreement with risk of bias domains). The disadvantages of case-series studies were inadequate reporting of participant recruitment, their demographic presentation, and a short duration of follow-up.
Table 2.
The methodological quality score of included studies based on Newcastle–Ottawa quality assessment score
| Source | Selection | Comparability | Outcome | Total score | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the exposed group | Selection of the non-exposed group | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability of study on the basis of the design or analysis | Assessment of outcome | Was follow-up long enough for outcomes to occur? | Adequacy of follow-up of the groups | Out of 9 | |
| Boulle [4] | 1 | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 7 |
| Geretti [18] | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 7 |
| Huang [5] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 6 |
| Amo [13] | 1 | 0 | 1 | 0 | 2 | 1 | 0 | 0 | 5 |
| Maggiolo [20] | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 5 |
| Etienne [17] | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 5 |
| Nagarakanti [21] | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 5 |
| Tesoriero [22] | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 6 |
| Ceballos [15] | 1 | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 7 |
Table 3.
Quality appraisal of included case series employing Joanna Briggs Institute Case Series Checklist
| Meyerowitz [23] | Collins [16] | Harter [24] | Kase [19] | Biagio [14] | |
|---|---|---|---|---|---|
| Were there clear criteria for inclusion in the case series? | Y | Y | Y | Y | Y |
| Was the condition measured in a standard, reliable way for all participants included in the case series? | Y | Y | Y | N | Y |
| Were valid methods used for identification of the condition for all participants included in the case series? | Y | Y | N | N | Y |
| Did the case series have consecutive inclusion of participants? | Y | Y | Y | N | Y |
| Did the case series have complete inclusion of participants? | ? | Y | Y | N | ? |
| Was there clear reporting of the demographics of the participants in the study? | Y | Y | Y | N | N |
| Was there clear reporting of clinical information of the participants? | Y | Y | Y | Y | ? |
| Were the outcomes or follow-up results of cases clearly reported? | N | N | N | N | N |
| Was there clear reporting of the presenting site(s)/clinic(s) demographic information? | N | Y | N | N | N |
| Was statistical analysis appropriate? | Y | Y | Y | Y | Y |
| Score (Y or N/A = 1, N or? = 0) | 7 | 9 | 7 | 3 | 5 |
Results of Meta-Analyses
Primary Outcome
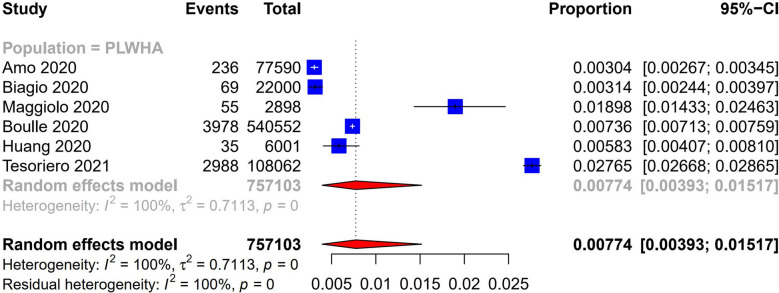
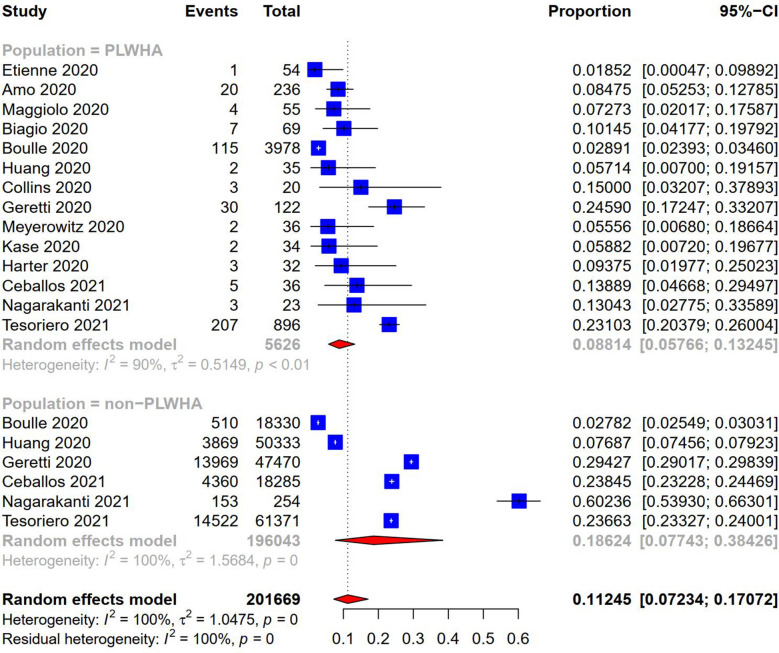
Findings of prevalence and mortality rate for COVID-19 infected PLWHA were of interest. Pooled results from six of the included studies showed the prevalence of co-infection with COVID-19 in PLWHA was 0.774% (95% CI 0.00393–0.01517) (Fig. 2). For the mortality rate of COVID-19 in PLWHA, pooled results from 14 included studies showed a rate of 8.814% (95% CI 0.05766–0.13245) (Fig. 3). Subgroup analyses categorized by country can be found in the Supplementary Material.
Fig. 2.
Prevalence of COVID-19 in PLWHA
Fig. 3.
The COVID-19 mortality rate in PLWHA and non-PLWHA
Additional Outcomes
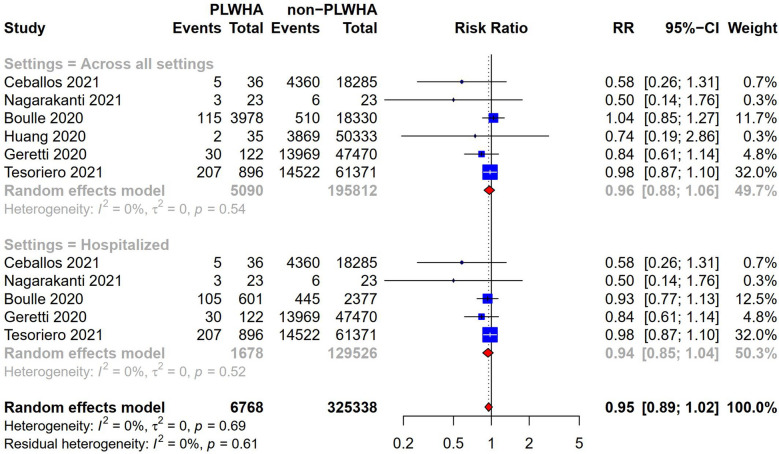
Additional outcomes include: (1) the risk of mortality in PLWHA due to COVID-19 infection compared to non-PLWHA; (2) the risk of COVID-19 co-infection grouped by various comorbidities between PLWHA and non-PLWHA; (3) comparison comorbidity in the risk of COVID-19 mortality in PLWHA; and (4) the role of CD4 count, HIV viral load, and ART in COVID-19 co-infection in PLWHA. Six studies reported outcomes of mortality in both populations. The pooled data indicated that, compared to non-PLWHA, a COVID-19 course in PLWHA having an estimated RR 0.96 (95% CI 0.88–1.06, I2 = 0%; Fig. 4) was not associated with higher mortality across all settings. Five studies were included in the subgroup analysis of hospitalized patients, which indicated that there is no evidence that HIV was associated with higher mortality due to COVID-19, RR 0.94 (95% CI 0.85–1.04, I2 = 0%, Fig. 4).
Fig. 4.
Comparison mortality between PLWHA and non-PLWHA due to COVID-19
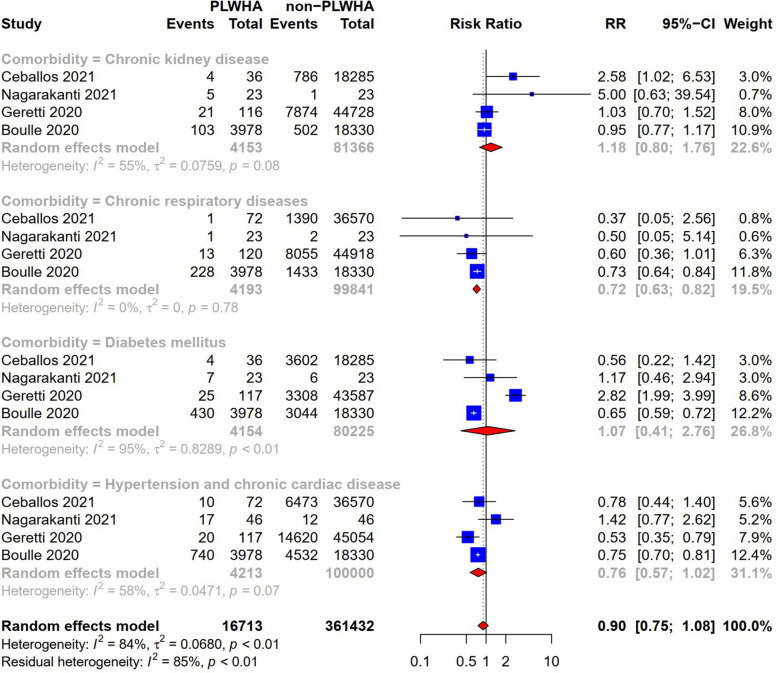
Data of comorbidities were available from four cohort studies, which reported chronic kidney disease, chronic respiratory disease, diabetes mellitus, and hypertension and chronic cardiac disease in both PLWHA and non-PLWHA. Pooled results showed that none of the comorbidities were associated with a higher risk of infection with COVID-19 when PLWHA and non-PLWHA were compared: for chronic kidney disease, RR 1.18 (95% CI 0.80–1.76, I2 = 55%; Fig. 5); for chronic respiratory disease, RR 0.72 (95% CI 0.63–0.82, I2 = 0%; Fig. 5); for diabetes mellitus, RR 1.07 (95% CI 0.41–2.76, I2 = 95%; Fig. 5); and for hypertension and chronic cardiac disease, RR 0.76 (95% CI 0.57–1.02, I2 = 58%; Fig. 5).
Fig. 5.
Comparison of comorbidity in the risk of COVID-19 co-infection between PLWHA and non-PLWHA
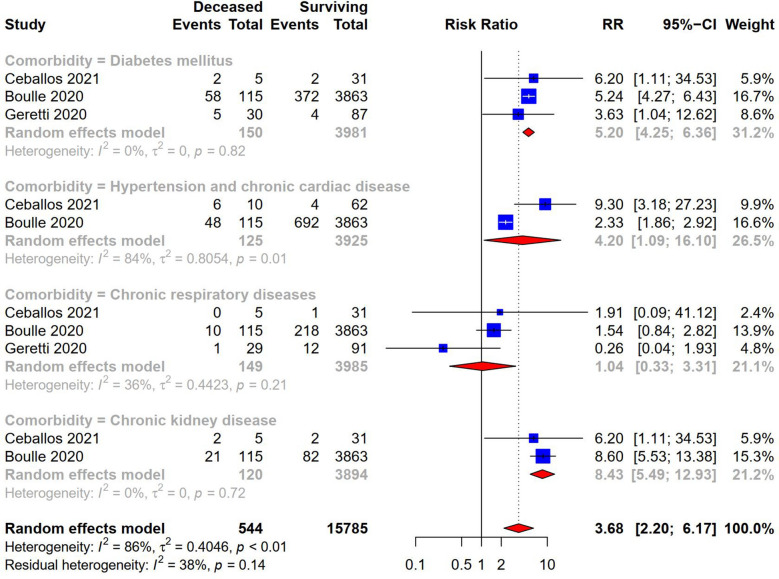
An analysis grouped by comorbidities was performed in PLWHA. Three studies were included in the analysis. The result indicated that chronic kidney disease, RR 8.43 (95% CI 5.49–12.93, I2 = 0%; Fig. 6), diabetes mellitus, RR 5.20 (95% CI 4.25–6.36, I2 = 0%; Fig. 6), hypertension and chronic cardiac disease, RR 4.20 (95% CI 1.09–16.10, I2 = 84%; Fig. 6) have a strong association with increased mortality due to COVID-19 in PLWHA.
Fig. 6.
Comparison comorbidity in the risk of COVID-19 mortality in PLWHA
The classification of HIV viral load, CD4 count, and ART was not standardized, hence we failed to estimate their impact in COVID-19 co-infected PLWHA.
Discussion
Several studies have reported the prevalence of COVID-19 among PLWHA, with an estimated rate ranging from 0.8 to 9.7% [25–27]. However, their conclusions were based on single studies and only a few systematic reviews and meta-analyses have estimated the odds comprehensively and quantitatively. A recent, unpublished systematic review and meta-analysis indicated that the prevalence and mortality rate of PLWHA hospitalized for COVID-19 was 1.22% and 12.35%, respectively [28]. Unfortunately, as only 573 PLWHA were included in the pooled analysis and seven out of nine included studies were conducted in New York City, the strength of the evidence presented in the unpublished review is possibly limited for reflecting the generalized population. As increased evidence has since been published, our review and meta-analysis uses a large sample size from multiple diverse regions. Our findings suggested that the prevalence and mortality rate of COVID-19 in PLWHA was 0.774% and 8.814%, respectively. The estimated prevalence rate is lower than the existing reports, possibly due to varying sample sizes across studies and the epidemiological characteristic difference between regions (Supplementary Material). Distinct examples of this are an included study, conducted in Wuhan, China, which estimated 0.583% COVID-19 prevalence out of 5966 PLWHA [5], and an excluded conference report, the Veterans Aging Cohort Study conducted in the USA, which estimated a 9.7% prevalence for COVID-19 out of 30,891 PLWHA [25]. True prevalence could be higher, as HIV remains disproportionately concentrated in low-income regions which also have the highest HIV-related morbidity and mortality [29, 30]. PLWHA in these regions might have poor disease management, which consequently results in an increased risk of contracting COVID-19 due to being immunocompromised. These patients might not be identified as COVID-19 co-infected due to inadequate detection capacity or the limitations of local governments.
There is also a growing interest regarding the characteristics and prognosis of COVID-19 between PLWHA and non-PLWHA. Some evidence from multiple European HIV/AIDS organizations acknowledged that there is not sufficient evidence showing a varying disease course or higher COVID-19 infection rates in PLWHA compared to non-PLWHA [31]. Consistent with these conclusions, a recently published systematic review and meta-analysis conducted by Sarkar et al. indicated no significant impact in COVID-19 mortality between PLWHA and non-PLWHA [RR 0.99 (95% CI 0.82–1.19)] [32]. However, this finding was in contrast to another study conducted by Mellor et al. [33], which suggested that PLWHA had a higher risk of COVID-19 mortality compared to the general population [HR 1.95 (95% CI 1.62–2.34)]. It is a much-debated topic whether HIV plays a pivotal role in COVID-19 prognosis, as the evidence has been derived from cohort studies that were performed in unmatched populations. The number of PLWHA having COVID-19 co-infection was relatively low in such cases (Table 1). On the other hand, both of the above-mentioned meta-analyses are suspected to have included studies having overlapping populations and periods between each other, which might have led to inappropriate interpretation [34]. Sarkar’s review used data collected from four studies conducted in the same region (New York City) and one study of a multi-center design [3]. In Mellor’s review, two of the included studies were conducted at national level in the UK [18, 35].
Despite having an unmatched population, our study showed insufficient evidence for a higher risk of COVID-19 mortality in PLWHA when compared to non-PLWHA across all settings (Fig. 4). This leads to a puzzling question: Why are PLWHA not at higher risk for developing a severe course and outcome of COVID-19 infection compared to the general population even though they might be immunosuppressed? A pharmacologic hypothesis might explain why this might be the case. PLWHA have usually prescribed ART for the management of HIV. Recent evidence suggests that widely prescribed anti-HIV medications, Tenofovir, Emtricitabine, Raltegravir, and Dolutegravir, have been proven to result in reduced in vivo SARS-CoV-2 proliferation [36–39]. It has been further found that, among COVID-19 infected PLWHA, those who took Tenofovir disoproxil fumarate therapy had better clinical outcomes compared to other ARTs [13, 40]. Another possible explanation for this outcome could be that most studies were performed in high-income countries where the majority of PLWHA were more likely to have well-controlled HIV on ART (Table 1). Outcomes in low-income areas having a high burden of HIV might be a little more complex. Another concern is that the patients undergoing ART might be more likely to experience treatment interruptions due to restrictions on non-emergency medical appointments related to physical distancing requirements. It is estimated that approximately 19% of PLWHA were unable to receive ART refills due to the pandemic [41]. Also, many HIV/AIDS prevention and control centers have been converted to COVID-19 centers and refused PLWHA of their ART [41, 42]. Effective action should be taken to help these patients receive their basic ART on time.
Correlation between comorbidities and COVID-19 has recently been in focus. It is reported that approximately two-thirds of COVID-19 co-infected PLWHA had multimorbid complications [43]. In our review, meta-analyses showed that PLWHA who had comorbidities such as- chronic kidney disease, diabetes mellitus, hypertension and chronic cardiac disease, were not associated with a higher risk of contracting COVID-19 compared to non-PLWHA. These results, however, differ from some published studies which showed comorbidities correlated to a higher incidence of COVID-19 in the general population [26, 44]. In fact, the issue of whether comorbidities should be considered the driver of poor outcomes from COVID-19 has been a controversial and much-disputed subject [16, 45], as evidence from most studies was of a single-arm design, not matched, and had a small sample size. The included population for analysis in our study was also not matched, so we might underestimate the magnitude of the effect. Interestingly, our analysis indicated a strong correlation between COVID-19 mortality and comorbidities of chronic kidney disease, diabetes mellitus, and hypertension and chronic cardiac disease in PLWHA (Fig. 6).
These findings contribute to our understanding of the prevalence and mortality rate of COVID-19 in PLWHA. Also, this study has been conducted to confirm that a few comorbidities might drive poor outcomes among COVID-19 co-infected PLWHA. However, this study’s strength is subject to the following disadvantages that possibly limit its external validation: (1) the overall risk of bias assessment for the cohort studies and case series was moderate; however, both types of studies were evaluated to have a high-risk bias in the duration of follow-up, which might likely result in decreased death reporting [46]; (2) most of the included studies used an unmatched population design in assessing the role of comorbidities in contracting COVID-19 between PLWHA and non-PLWHA; the magnitude of the effect might be an underestimate since the sample size of PLWHA in studies was originally small; and (3) few of the included studies were performed in low-income but high-HIV burden areas (e.g., Sub-Saharan Africa). PLWHA living in these areas appeared to have poor HIV management [47]. Since our study included patients from high-income areas with better HIV management, the overall prevalence and mortality for the general population might be underestimated. Careful interpretation of results is, therefore, necessary.
Given the rapid spread of the virus and an exponential increase in cases, a strategy of mass quarantine has been implemented globally. Despite these measures to aid healthcare, a resultant disturbing impact on mental health could arise among PLWHA [48]. It has been evidenced that psycho-social depression could have a negative impact on health and behavior, and is associated with poor health outcomes [49, 50]. None of the included studies investigated mental well-being. Additional research is required to probe psycho-social effects due to COVID-19 among PLWHA.
Limitations
Our analysis faced the following limitations: (1) due to a lack of standardized reporting in included studies, our review was unable to investigate the roles of CD4 count, HIV viral load as well as ART in COVID-19 infection and prognosis; and (2) insufficient data reported in studies led to an inability to gain an insight regarding the incidence of ICU admissions, the need for the use of mechanical ventilation, and the assessing of socio-demographic disparities in COVID-19 co-infection in PLWHA.
Conclusions
Our study gained some insights into the prevalence and mortality of COVID-19 in PLWHA. We also found that comorbidities such as chronic kidney disease, diabetes mellitus, and hypertension and chronic cardiac disease, are responsible for poor outcomes in COVID-19 co-infected PLWHA. Further studies need to be carried out to validate the relationship between COVID-19 outcomes and HIV viral load, CD4 count, ART in diverse settings.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank Mrs. Yunru Fan and Dr. Alexandra Lam for coordinating and supporting the development and preparation of the manuscript.
Funding
The funding for this study was provided by the High-level Hospital Construction Research Project of Maoming People’s Hospital, Maoming, China. The journal’s Rapid Service Fee was also funded by the sponsor. The funder had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
SFT, NL, SS and ML conceived the idea of this study. SS and SS managed the literature search. CNC and MFC screened the titles, abstracts, and full texts. CNC, SFT and NL assessed the bias and performed data extraction. Shivank.S performed the initial meta-analyses. Shantanu.S performed the final meta-analyses. SS, SS, NL, and ML wrote the manuscript. All authors provided critical insights and edits. All authors read and approved the final manuscript.
Disclosures
Min Liang, Ning Luo, Mafeng Chen, Chunna Chen, Shivank Singh, Shantanu Singh, and Shifan Tan declare that they have no competing interests.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies involving human participants or animals performed by any of the authors.
Data Availability
The datasets used and analyzed during this study are available from the corresponding author on reasonable request.
Footnotes
Min Liang, Ning Luo, Mafeng Chen have contributed equally to this work.
Contributor Information
Min Liang, Email: imtuaska@163.com.
Shifan Tan, Email: mmrytsf@163.com.
References
- 1.John Hopkins University. Coronavirus Resource Center 2020. https://coronavirus.jhu.edu/map.html. Accessed 21 Mar 2021
- 2.People living with HIV in all ages. https://aidsinfo.unaids.org/. Accessed 9 Mar 2021.(2019).
- 3.Hadi YB, Naqvi SFZ, Kupec JT, Sarwari AR. Characteristics and outcomes of COVID-19 in patients with HIV: a multicentre research network study. AIDS. 2020;34(13):F3–f8. doi: 10.1097/QAD.0000000000002666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boulle A, Davies MA, Hussey H, Ismail M, Morden E, Vundle Z, et al. Risk factors for COVID-19 death in a population cohort study from the Western Cape Province. South Africa. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang J, Xie N, Hu X, Yan H, Ding J, Liu P, et al. Epidemiological, virological and serological features of COVID-19 cases in people living with HIV in Wuhan City: A population-based cohort study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18(10):2127–2133. doi: 10.11124/JBISRIR-D-19-00099. [DOI] [PubMed] [Google Scholar]
- 8.Wells G, Shea B, O'Connell J. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Health Research Institute Web site; 2014. p. 7. [Google Scholar]
- 9.Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks: Sage Publications, Inc; 2001. p. ix. [Google Scholar]
- 10.Higgins J, Thompson S. Higgins JPT, Thompson SGQuantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.R Core Team (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/. Accessed 13 Jan 2021.
- 13.Del Amo J, Polo R, Moreno S, Díaz A, Martínez E, Arribas JR, et al. Incidence and severity of COVID-19 in HIV-positive persons receiving antiretroviral therapy: a cohort study. Ann Intern Med. 2020;173(7):536–541. doi: 10.7326/M20-3689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Di Biagio A, Ricci E, Calza L, Squillace N, Menzaghi B, Rusconi S, et al. Factors associated with hospital admission for COVID-19 in HIV patients. AIDS. 2020;34(13):1983–1985. doi: 10.1097/QAD.0000000000002663. [DOI] [PubMed] [Google Scholar]
- 15.Ceballos ME, Ross P, Lasso M, et al. Clinical characteristics and outcomes of people living with HIV hospitalized with COVID-19: a nationwide experience. Int J STD & AIDS. 2021;32(5):435–443. doi: 10.1177/0956462420973106. [DOI] [PubMed] [Google Scholar]
- 16.Collins LF, Moran CA, Oliver NT, Moanna A, Lahiri CD, Colasanti JA, et al. Clinical characteristics, comorbidities and outcomes among persons with HIV hospitalized with coronavirus disease 2019 in Atlanta. Georgia Aids. 2020;34(12):1789–1794. doi: 10.1097/QAD.0000000000002632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Etienne N, Karmochkine M, Slama L, Pavie J, Batisse D, Usubillaga R, et al. HIV infection and COVID-19: risk factors for severe disease. AIDS. 2020;34(12):1771–1774. doi: 10.1097/QAD.0000000000002651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geretti AM, Stockdale AJ, Kelly SH, Cevik M, Collins S, Waters L, et al. Outcomes of COVID-19 related hospitalization among people with HIV in the ISARIC WHO Clinical Characterization Protocol (UK): a prospective observational study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kase K, Skrzat-Klapaczyńska A, Vassilenko A, Harxhi A, Lakatos B, Lukić GD, et al. The case series of 34 patients with COVID-19 diagnosed with HIV infection from Central and Eastern European Countries—Euroguidelines in Central and Eastern Europe Network Group data. medRxiv. 2020:2020.09.16.20191528.
- 20.Maggiolo F, Zoboli F, Arosio M, Valenti D, Guarneri D, Sangiorgio L, et al. SARS-CoV-2 infection in persons living with HIV: A single center prospective cohort. J Med Virol. 2021;93(2):1145–1149. doi: 10.1002/jmv.26352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nagarakanti SR, Okoh AK, Grinberg S, Bishburg E. Clinical outcomes of patients with COVID-19 and HIV coinfection. J Med Virol. 2021;93(3):1687–1693. doi: 10.1002/jmv.26533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tesoriero JM, Swain CE, Pierce JL, Zamboni L, Wu M, Holtgrave DR, et al. COVID-19 outcomes among persons living with or without diagnosed HIV infection in New York State. JAMA Netw Open. 2021;4(2):e2037069. doi: 10.1001/jamanetworkopen.2020.37069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meyerowitz EA, Kim AY, Ard KL, Basgoz N, Chu JT, Hurtado RM, et al. Disproportionate burden of coronavirus disease 2019 among racial minorities and those in congregate settings among a large cohort of people with HIV. AIDS. 2020;34(12):1781–1787. doi: 10.1097/QAD.0000000000002607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Härter G, Spinner CD, Roider J, Bickel M, Krznaric I, Grunwald S, et al. COVID-19 in people living with human immunodeficiency virus: a case series of 33 patients. Infection. 2020;48(5):681–686. doi: 10.1007/s15010-020-01438-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park LS, Rentsch CT, Sigel K, et al. COVID-19 in the largest US HIV cohort. AIDS 2020: 23rd International AIDS Conference San Francisco/Oakland Virtual; July 6–10, 2020. Abstract LBPEC23.
- 26.Vizcarra P, Pérez-Elías MJ, Quereda C, Moreno A, Vivancos MJ, Dronda F, et al. Description of COVID-19 in HIV-infected individuals: a single-centre, prospective cohort. Lancet HIV. 2020;7(8):e554–e564. doi: 10.1016/S2352-3018(20)30164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ssentongo P, Heilbrunn ES, Ssentongo AE, Advani S, Chinchilli VM, Nunez JJ, et al. Prevalence of HIV in patients hospitalized for COVID-19 and associated outcomes: a systematic review and meta-analysis. medRxiv.2020:2020.07.03.20143628. doi: 10.1101/2020.07.03.20143628.
- 29.Dwyer-Lindgren L, Cork MA, Sligar A, Steuben KM, Wilson KF, Provost NR, et al. Mapping HIV prevalence in sub-Saharan Africa between 2000 and 2017. Nature. 2019;570(7760):189–193. doi: 10.1038/s41586-019-1200-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018 Nov 10;392(10159):1736-1788. 10.1016/S0140-6736(18)32203-7. Epub 2018 Nov 8. Erratum in: Lancet. 2019 Jun 22;393(10190):e44. Erratum in: Lancet. 2018 Nov 17;392(10160):2170. PMID: 30496103; PMCID: PMC6227606. [DOI] [PMC free article] [PubMed]
- 31.BHIVA, DAIG, EACS. GESIDA & the Polish AIDS Society Statement on risk of COVID-19 for people living with HIV (PLWH). British HIV association (BHIVA). 2020. https://www.bhiva.org/BHIVA-DAIG-EACS-GESIDA-Polish-Scientific-AIDS-Society-statement-on-risk-of-COVID-19-for-PLWH. Accessed 26 Oct 2020.
- 32.Sarkar S, Khanna P, Singh AK. Impact of COVID-19 in patients with concurrent co-infections: a systematic review and meta-analyses. J Med Virol. 2021;93:2385–2395. doi: 10.1002/jmv.26740. [DOI] [PubMed] [Google Scholar]
- 33.Mellor MM, Bast AC, Jones NR, Roberts NW, Ordóñez-Mena JM, Reith AJM, et al. Risk of adverse coronavirus disease 2019 outcomes for people living with HIV. AIDS. 2021;35(4):F1–f10. doi: 10.1097/QAD.0000000000002836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Higgins J, Green SR. Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, England. 2011.
- 35.Bhaskaran K, Rentsch CT, MacKenna B, Schultze A, Mehrkar A, Bates CJ, et al. HIV infection and COVID-19 death: a population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet HIV. 2021;8(1):e24–e32. doi: 10.1016/S2352-3018(20)30305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elfiky AA. Ribavirin, remdesivir, sofosbuvir, galidesivir, and tenofovir against SARS-CoV-2 RNA dependent RNA polymerase (RdRp): A molecular docking study. Life Sci. 2020;253:117592. doi: 10.1016/j.lfs.2020.117592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jockusch S, Tao C, Li X, Anderson TK, Chien M, Kumar S, et al. Triphosphates of the two components in DESCOVY and TRUVADA are inhibitors of the SARS-CoV-2 polymerase. bioRxiv. 2020:2020.04.03.022939. doi: 10.1101/2020.04.03.022939.
- 38.Indu P, Rameshkumar MR, Arunagirinathan N, Al-Dhabi NA, Valan Arasu M, Ignacimuthu S. Raltegravir, indinavir, tipranavir, dolutegravir, and etravirine against main protease and RNA-dependent RNA polymerase of SARS-CoV-2: a molecular docking and drug repurposing approach. J Infect Public Health. 2020;13(12):1856–1861. doi: 10.1016/j.jiph.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alavian G, Kolahdouzan K, Mortezazadeh M, Torabi ZS. Antiretrovirals for prophylaxis against COVID-19: a comprehensive literature review. J Clin Pharmacol. 2021;61:581–590. doi: 10.1002/jcph.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Laurence J. Why aren't people living with HIV at higher risk for developing severe coronavirus disease 2019 (COVID-19)? AIDS Patient Care STDS. 2020;34(6):247–248. doi: 10.1089/apc.2020.29005.com. [DOI] [PubMed] [Google Scholar]
- 41.Kanwugu ON, Adadi P. HIV/SARS-CoV-2 coinfection: a global perspective. J Med Virol. 2021;93:726–732. doi: 10.1002/jmv.26321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adadi P, Kanwugu ON. Living with HIV in the time of COVID-19: a glimpse of hope. J Med Virol. 2021;93:59–60. doi: 10.1002/jmv.26118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mirzaei H, McFarland W, Karamouzian M, et al. COVID-19 among people living with HIV: a systematic review. AIDS Behav. 2021;25:85–92. doi: 10.1007/s10461-020-02983-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lesko CR, Bengtson AM. HIV and SARS-CoV-2: Intersecting Epidemics with Many Unknowns. Am J Epidemiol. 2020;190(1):10–16. doi: 10.1093/aje/kwaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sigel K, Swartz T, Golden E, Paranjpe I, Somani S, Richter F, et al. Coronavirus 2019 and people living with human immunodeficiency virus: outcomes for hospitalized patients in New York City. Clin Infect Dis. 2020;71(11):2933–2938. doi: 10.1093/cid/ciaa880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ndlovu Z, Burton R, Stewart R, Bygrave H, Roberts T, Fajardo E, et al. Framework for the implementation of advanced HIV disease diagnostics in sub-Saharan Africa: programmatic perspectives. Lancet HIV. 2020;7(7):e514–e520. doi: 10.1016/S2352-3018(20)30101-6. [DOI] [PubMed] [Google Scholar]
- 48.Dyer J, Wilson K, Badia J, et al. The psychosocial effects of the covid-19 pandemic on youth living with HIV in Western Kenya. AIDS Behav. 2021;25:68–72. doi: 10.1007/s10461-020-03005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weinstein TL, Li X. The relationship between stress and clinical outcomes for persons living with HIV/AIDS: a systematic review of the global literature. AIDS Care. 2016;28(2):160–169. doi: 10.1080/09540121.2015.1090532. [DOI] [PubMed] [Google Scholar]
- 50.Yu L, Chiu CH, Lin YS, Wang HH, Chen JW. Testing a model of stress and health using meta-analytic path analysis. J Nurs Res. 2007;15(3):202–214. doi: 10.1097/01.JNR.0000387616.64812.60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during this study are available from the corresponding author on reasonable request.