Background
A novel coronavirus, SARS-CoV-2, emerged from Wuhan, China in December of 2019. This virus is responsible for an atypical respiratory illness. It has been shown to activate coagulation cascade resulting in both arterial and venous thromboembolism.
Case
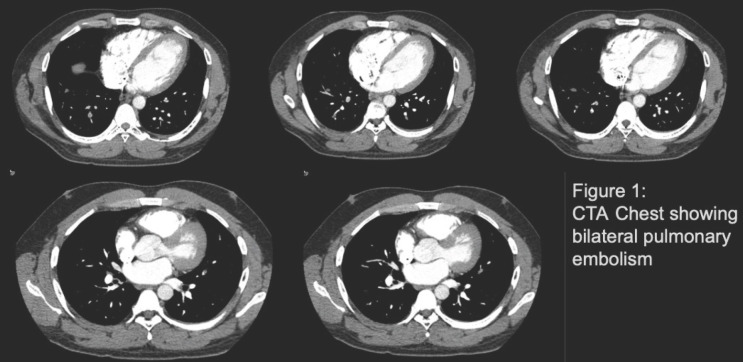
A healthy 34 yo male presents to the emergency department with chief complaint of progressively worsening SOB and sharp left-sided, non-radiating chest pain. The patient previously tested positive for COVID in May of 2020, but never required hospitalization and was treated supportively in the outpatient setting. Initial vitals were: BP 161/100, HR 77, RR 18, SpO2 98% and patient was afebrile. Initial studies included a CXR and EKG, which were negative for acute cardiopulmonary abnormality or right heart strain. A CTA Chest revealed bilateral PE involving the lower lobe regions of the lung, most prominently the right lower.
Decision-making
The patient was admitted for observation and to obtain TTE for evaluation of right heart abnormality/dysfunction. The echocardiogram findings did not show significant findings. Patient was placed on heparin drip and transitioned to DOAC therapy prior to discharge after symptomatic improvement.
Conclusion
There have been few case reports noting the late onset of PE, however, these cases have diagnosed PE days to weeks post-COVID-19 infection. Comparatively, this case reveals an otherwise healthy young male without predisposing factors presenting with PE after five months of initial COVID19 exposure.
Footnotes
Poster Contributions
Sunday, May 16, 2021, 1:15 p.m.-2:00 p.m.
Session Title: Complex Clinical Cases: FIT Pulmonary Vascular Disease 2
Abstract Category: FIT: Pulmonary Vascular Disease