Abstract
Purpose
To measure motor function improvements in patients with Parkinson’s disease (PD) using Health Qigong exercises.
Patients and Methods
Fifty-two PD patients (Hoehn and Yahr stages I to IV) were randomly divided into experimental and control groups. Twenty-six PD patients in the experimental group were intervened with routine medicine and fitness Qigong exercise. The other 26 PD patients as the control group were treated only with regular medication. Twelve-week intervention had been conducted for the study, and participants completed the scheduled exercises 4 times per week for 60 minutes each time. Data which included the one-legged blind balance, physical coordination, and gait was collected before, during, and after the intervention. Comparisons were made between the experimental and control groups through the repeated measures analysis of variance.
Results
A total of 40 participants (77% response rate) completed the study. There was no significant difference in baseline data. After 12 weeks of Health Qigong therapy, the length of time the one-legged blind balance test had increased (P < 0.01), and the time it took to TUG test was reduced (P < 0.01). Joint range of motion and gait significantly improved. The control group’s there were no significant differences in the above variables, except for joint range of motion, which decreased.
Conclusion
Health Qigong exercises can significantly improve physical functions in patients with PD, especially for the balance ability, gait, joint range of motion in patients with PD. It can reduce their activity risk factor and improve their quality of life.
Keywords: Parkinson’s disease, Health Qigong exercise, motor function, balance, gait
Introduction
Parkinson’s disease (PD) is a common age-related neurodegenerative disorder. PD symptoms vary: the most common symptoms are tremors at rest, slow movement, stiffness, and impaired balance.1 If there are no intervention measures, the behavior ability of patients with severe disease will be seriously affected, even including physical function. PD can also cause a range of non-motor symptoms, including sleep problems, constipation, language confusion, and mood disorders.2 PD occurs in middle-aged and older adults. The incidence of disease in people over 60 years old is 1%, and the incidence increases with age, imposing a heavy burden on families and society.3,4 Motor symptoms gradually worsen with the progression of the disease.
Although no cure or treatment can delay PD progression, several pharmacological and surgical therapies can improve symptoms.5 Because of the side-effects associated with pharmacotherapy and the risks of operative treatment, clinicians are paying increased attention to exercise interventions.6 According to recent studies, exercise improves clinical symptoms of PD, including postural instability, rigidity, muscle tremors, slow movement, and physical abilities such as muscle function and sense of balance.7–10 Several trials and meta-analyses showed that various exercises improve motor and non-motor (behavioral, emotional, cognitive) symptoms of PD.11,12 These include dance, yoga, tai chi, and Health Qigong.13–18 Especially for patients in the mild-to-moderate stage, exercise has a positive effect on physical and mental health. However, studies have shown that short-term exercise intervention can significantly improve PD patients, but if the exercise plan is combined with daily life, it will have a better and sustained impact.19
Health Qigong is a promising rehabilitation method that integrates mind, breath, and body movement and serves as an additional treatment for several neurodegenerative diseases. Health Qigong exercise is a structured, planned, and repetitive physical activity program prescribed by a doctor or rehabilitation specialist.20 It reduces pressure, adjusts mood, enhances exercise tolerance, improves balance, and regulates immune function.21 In recent years, investigators studied rehabilitation experiments on Health Qigong for PD.22 Li et al found that Health Qigong practice improved the ability to focus on the postural stability, and can enhance core muscle to stress weight-bearing joints and to increase proprioception input of trunk and lower limb joints.23 Others showed that Health Qigong exercise relieved sleep disorders and non-motor symptoms in patients with PD.24 The effect of Health Qigong on the mechanism of PD has attracted extensive attention from researchers worldwide. Parkinson’s exercise therapy is based on Health Qigong and is designed according to the dyskinesia symptoms of patients with PD.9 A systematic review and meta-analysis also pointed out that the current Parkinson’s patients affected by Health Qigong, Taiji needs to be better described, and more large-scale and strict experiments should be carried out, to guide individuals with different subtypes of Parkinson’s disease and symptom burden to choose the best dose and specific scheme.25 It seems that in most of the included studies, the effectiveness of Taiji and Qigong training was evaluated by functional test.26 Therefore, this paper aims to analyze the effect of Health Qigong exercise intervention on the motor function of patients with Parkinson’s disease. Through balance, Physical coordination, gait, joint range of motion and other aspects, the motor function and activity ability of PD patients were evaluated, and the influence mechanism of Health Qigong exercise on PD patients was analyzed.
Methods
Setting
We conducted this study in the rehabilitation center of Beijing Sport University from May 2019 to August 2019. The study was approved by the Ethics Committee of Beijing Sport University and Beijing Aerospace Central Hospital (Department of Neurology), and a written informed consent was obtained from every eligible subject.
Participants
We recruited a convenience sample of 52 patients with PD in a hospital in Beijing. We randomly divided patients into the experimental and control groups, with 26 patients in each group. The baseline information of gender, height and weight were collected. Before the intervention, one person independently completed the random assignment of the computer digital table and formed a sealed number. Due to the characteristics of intervention teaching, the distribution groups of researchers and subjects are known, but the subjects do not know the research hypothesis.
The inclusion criteria were as follows: (1) no obvious cognitive or mobility impairment, and no auxiliary equipment required for activities; (2) age 40–85 years; (3) Hoehn and Yahr scale: score 1–4; (4) UPDRS III: at least one limb score of tremor, stiffness, posture stability, or slow movement items ≥2 points; (5) stable medication doses; and (6) medical clearance to participate in the experiment.
Exclusion criteria were as follows: (1) history of non-Parkinson’s neurological impairments; (2) currently participation in other behavioral or pharmacological studies or coach-guided exercise programs; (3) mental status score of fewer than 24 points; (4) physical weakness, impaired vision, or inability to understand the test content.
Procedure
The intervention was a 12-week Health Qigong exercise therapy under the guidance of a professional Health Qigong coach. In the control group, the routine stable drug treatment was maintained within 12 weeks without any other intervention. According to the common clinical motor symptoms of PD patients, The whole set of Health Qigong exercises included ten movements which they are selected from Health Qigong Baduanjin, Health Qigong Wuqinxi, Health Qigong Yijinjing, Health Qigong Liuzijue, Health Qigong 12-step Daoyin Health Preservation Exercises and Health Qigong Mawangdui Daoyinshu. Each movement was to be practiced three to six times (three time for both side, six time for single side), taking approximately 12–16 minutes for the entire form, to improve PD’s physical coordination, stability, balance, and gait. The Health Qigong exercise program was conducted for 12 weeks, 4 days per week, with each session lasting for 60 minutes. Each session included 10 minutes of warm-up, 40 minutes of Health Qigong practice, and 10 minutes of relaxation at the end. During the test, the subjects were guaranteed enough time to rest and recover.
Measurement Procedure
Five instruments were used to measure the outcomes of the 12-week Health Qigong program. They included the reaction capacity, dynamic and static balance capacity test, joint range of motion test, gait test. This study is mainly concerned with the effect of Health Qigong on PD Physical Function; thus, the items such as balance capacity (the most common and main symptoms of PD) all needed to be measured and analyzed. The following instruments were used for collecting data: balance and reaction capacity were measured through (a) Reaction time test, (b) TUG test, and (c) one-legged blind balance test. In addition, the walking ability was measured by (d) gait test, and through (e) joint range of motion, test to measure the flexibility of the shoulder joint, knee, hip joint range of motion. All data were collected by the lab technicians and the project assistants.
Reaction time: The subject stands naturally, with a signal light about 1 meter in front of the abdomen. When the light comes on, the patient responds with a knee bend and jump up. We used a stopwatch to record the reaction time in seconds as the time required for the patient saw the light on to the moment he jumps up. The test was conducted twice and the average score was taken.
Balance: One-legged blind balance test. During the test, the subjects were prepared to stand naturally. When they heard the “start” command, they closed their eyes and raised their left foot at the same time. When the support foot moved (or raised the foot to contact the ground or opened their eyes), the test ended. In the same way, the right foot was raised. The left foot and the right foot were both tested twice respectively, and the average value was taken. We used a stopwatch to record the time of static balance in seconds.
Physical coordination: The Timed Up and Go (TUG) Test requires a chair with armrests and a stopwatch. During the assessment, the patient wears their usual shoes and sits on chair, leaning on the back of the chair, hands on the armrests. We place a thick colored line on the ground 3 m away from the seat. When the tester gives the “start” command, the patient stands up from the chair. After standing firmly, the patient walks as quickly as possible for 3 m, turns around after crossing a thick colored line, walks quickly back to the chair, then turns around and sits down, leaning on the back of the chair. We estimated dynamic balance, physical coordination ability and the possibility of falling by recording the time from when the patient’s back leaves the chair back to the time they sit down again.
Flexibility: sit-and-reach test. The subjects took off their shoes and sat on the flat ground, with their legs extended to the front of their bodies, their toes facing up, their feet slightly apart, and their soles resting on the flat ground. Two hands are folded and slowly extended forward, when reaching the maximum distance, hold for a few seconds, and measure the distance reached by the fingertips with a ruler. The best score was recorded, measured in centimeters beyond the sole of the subject’s foot, or how far away from the foot if it did not reach the toe (negative measurement score).
Joint Range of Motion: Knee joint flexion test. The subjects lie prone, and we place a protractor axis at the knee joint, and a fixed arm is parallel to the thigh. Bend your knee and slide your foot up close to your buttocks. Keep going until you reach the maximum point of your knee flexion abilities. We place a movable arm along the fibula to measure the angle formed by the horizontal line of a movable arm and fixed arm (0–135°, Figure 1). Then, repeat the measurement on your other knee.
Figure 1.
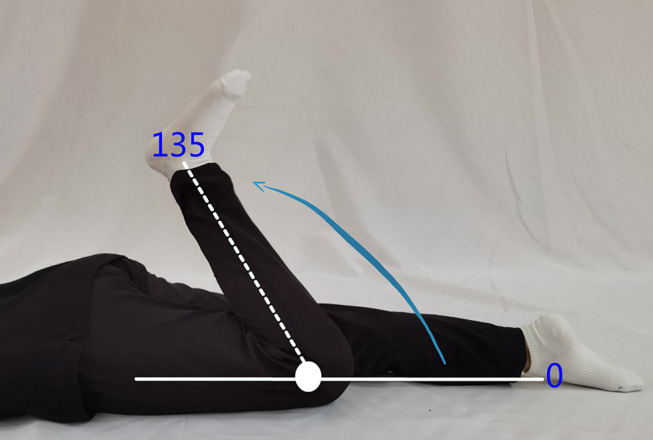
Knee joint flexion test chart.
Hip extension test. The subjects lie prone, hips were flat on the ground, legs straight. We fix the goniometer axis at the femur’s greater trochanter, and the fixed arm is horizontal with the ground. The patient actively extends the hip, keeps going until you reach the maximum point of your hip extension abilities. We place the movable arm upward along the middle of the femur to measure the angle of hip extension (0–15°, Figure 2).
Figure 2.
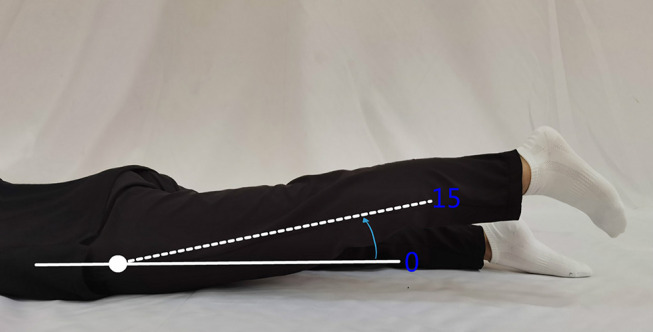
Hip extension test chart.
Hip flexion test. The subjects are supine with hips flat on the ground. The subject flexes the thigh and lower legs and brings them close to the chest. We fix the goniometer axis at the femur’s greater trochanter; the fixed arm was parallel to the ground; we place the movable arm along the middle of the femur. The Patient exerts the maximal effort of actively flex the hip and record the movement angle of hip flexion (0–135°, Figure 3).
Figure 3.

Hip flexion test chart.
Shoulder joint test. The subject stands naturally, the right arm is bent and grasps the long stick upward close to the back of the thoracic spine. The elbow is down, the back of the hand is close to the spine, the subject raises and bends the left arm, the elbow is up, and the left hand is close to the back of the head. The subject grasps the upper part of the long stick, and we measure the linear distance between the roots of the index fingers of both hands. When the left hand is up, it is to measure the activity value of the left shoulder joint (Figure 4).
Figure 4.
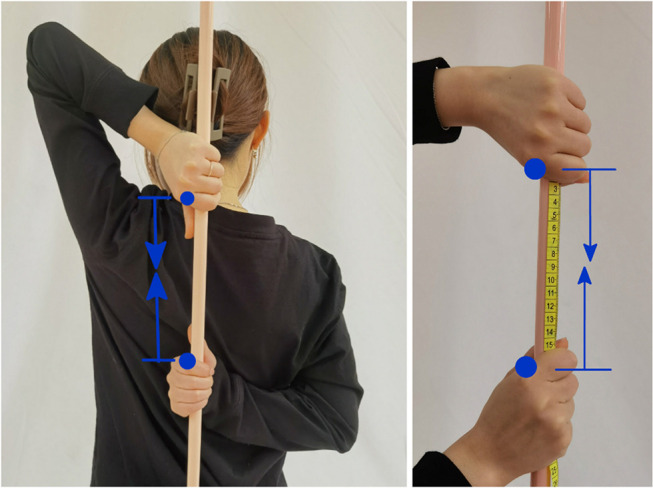
Shoulder joint test chart.
Gait: 10-m walking test (10MWT): The patient is asked to walk along a 14-meter straight line, marked at 2 m and 12 m. The patient starts at the 2 m marks and ends at the 12 m marks. We calculate and record the values of Stride length, Cadence, Gait velocity under normal speed-walking, and fast speed-walking the patient to walk between these marks. The gait velocity is monitored by using Smartspeed equipment (Fusion Sport, Australia). The recorded walking video that heel coordinates of a gait cycle are obtained by digitizing the heel points in the Vision System (Beijing Sport University). Gait cycle is defined as landing from one heel to the other. Gait cycle and gait velocity are calculated to get the cadence and stride length. In a gait cycle, the horizontal distance of the heel in the fore-and-aft direction is the stride length, the derivative of the stride length in time is the gait velocity, and the gait velocity divided by the stride length is the cadence. All gait parameters of normal speed-walking and fast speed-walking were tested twice, and at the last take the average of the two times.
Compliance: the evaluation was recorded based on the number of times the Parkinson’s patients participated in exercise therapy and the number of times they were tested, and finally recorded in the form of percentage.
Statistics and Data Analysis
We used SPSS 23.0 (SPSS Inc., Chicago, IL, USA) for all statistical tests. Baseline characteristics were summarized and presented using appropriate descriptive statistics. Baseline characteristics of experimental and control groups were compared using independent t-test, chi-square tests. The sensitive analysis was conducted to assess the robustness of the statistical results. We compared sample means using the Repeated Measures analysis of variance and represented measurement data as mean±SD. Three tests were conducted before, during, and after the intervention, and the results were compared and analyzed. The experimental design includes the comparison of the changes of the experimental group and the control group, as well as the comparison of the changes of the time before and after the two groups. We set statistical significance at P-value of <0.05.
Results
Of the 52 PD patients who participated in the study, four failed to complete the whole experiment due to illness. Another eight patients did not complete the study for personal reasons. The remaining 40 subjects completed the study program, and all patients received standard medical care during the study period. All tests were conducted in the morning when it was guaranteed that all subjects would stop taking anti-Parkinson drugs for at least 12 hours. The baseline data showed that there were no significant differences (P>0.05, Table 1).
Table 1.
Baseline Characteristics of Participants
| Characteristics | Experimental Group (n=20) | Control Group (n=20) | P-value |
|---|---|---|---|
| Age (years) | 64.95±7.83 | 67.03±7.47 | 0.730 |
| Height (cm) | 163.67±6.29 | 163.09±7.59 | 0.160 |
| Weight (kg) | 69.53±10.66 | 68.42±10.79 | 0.821 |
| Sex (male/female) | 8/12 | 11/9 | 0.527 |
| Years of PD (years) | 3.63±1.52 | 3.25±1.73 | 0.581 |
Notes: Data are shown as mean ± SD. Independent sample t-test of variance was used to compare the age, height, weight, and years of PD among groups, and the chi-square test was used to compare sex among groups. The significance level was set at p<0.05.
By the Repeated Measures analysis of variance, there was a no significantly different reaction time between groups (P>0.01, Table 2) before and after the experiment. At 6 weeks of treatment, there was no difference in reaction time between the experimental and control groups. After 12 weeks of intervention, the control group’s reaction time was significantly longer than that of the experimental group, which remained stable before, during, and after the experiment. Compared with before intervention, the experimental group had significant improvement in the one-legged blind balance test (left, P<0.001; right, P=0.001) and the TUG test (6 weeks after the intervention, P=0.046; 12 weeks after the intervention, P=0.002) were significantly improved (Table 2). After 12 weeks of intervention, there was a significant interaction in the TUG test between the control group and the experimental group (time by group interaction P=0.027) (Table 2).
Table 2.
Reaction Time, One-Legged Blind Balance and TUG Test
| Experimental Group (n=20) | Control Group (n=20) | ||||||
|---|---|---|---|---|---|---|---|
| Pre | Mid | Post | Pre | Mid | Post | ||
| Reaction time (s) | 0.35±0.11 | 0.34±0.11 | 0.34±0.11 | 0.35±0.13 | 0.35±0.12 | 0.40±0.12## | |
| One-legged blind balance test (s) | Left | 2.56±1.41 | 3.21±2.83 | 4.85±4.03## | 3.49±3.68 | 3.14±2.74 | 3.94±4.14 |
| Right | 2.31±0.92 | 3.65±3.31 | 5.22±5.02## | 4.58±5.53 | 3.37±3.37 | 2.97±2.90 | |
| TUG test (s) | 11.47±4.67 | 10.42±3.64# | 9.26±2.97##* | 11.77±5.52 | 12.16±5.61 | 12.71±6.02 | |
Notes: Data are shown as mean ± SD. *p<0.05, comparisons are significant between the control group and the experimental group. #p<0.05, ##p<0.01, comparisons are significant within groups.
Abbreviation: s, the unit is seconds.
As shown in Table 3, after the intervention, there was a significant difference in the normal speed-walking stride length of the experimental group (P=0.041). The gait velocity of the experimental group was significantly different after 6 weeks (normal speed-walking, P=0.006; fast speed-walking, P=0.006) and 12 weeks (normal speed-walking, P<0.001; fast speed-walking, P<0.001). Compared with the control group, the gait velocity (normal speed-walking, P=0.015; fast speed-walking, P=0.027) of the experimental group was significantly improved at 12 weeks, and the cadence of normal and fast speed-walking, and fast speed-walking stride length was improved, but there was no significant difference (P>0.05, Table 3). These data show that exercise therapy can improve the gait and walking ability of patients, so as to effectively prevent the occurrence of falls.
Table 3.
Gait Test
| Experimental Group (n=20) | Control Group (n=20) | ||||||
|---|---|---|---|---|---|---|---|
| Pre | Mid | Post | Pre | Mid | Post | ||
| Normal speed-walking | Stride length (m) | 1.059±0.14 | 1.066±0.18 | 1.175±0.16# | 1.047±0.28 | 1.076±0.35 | 1.077±0.34 |
| Cadence (steps/min) | 61.30±12.95 | 63.89±14.21 | 63.38±15.24 | 59.93±3.54 | 63.62±10.95 | 63.50±11.99 | |
| Gait velocity (m/s) | 0.566±0.17 | 0.741±0.14## | 0.841±0.28##* | 0.660±0.18 | 0.640±0.24 | 0.649±0.177 | |
| Fast speed-walking | Stride length (m) | 1.098±0.20 | 1.126±0.17 | 1.165±0.14 | 1.076±0.43 | 1.044±0.33 | 1.043±0.29 |
| Cadence (steps/min) | 67.10±12.65 | 68.52±12.72 | 68.76±13.62 | 66.53±4.97 | 67.08±4.93 | 66.38±4.58 | |
| Gait velocity (m/s) | 0. 715±0.18 | 1.004±0.35## | 1.118±0.26##* | 0.802±0.33 | 0.810±0.500 | 0.857±0.42 | |
Notes: Data are shown as mean ± SD. *p<0.05, comparisons are significant between the control group and the experimental group. #p<0.05, ##p<0.01, comparisons are significant within groups.
Abbreviations: m, the unit is meter; step/min, step per minter; m/s, meter per second.
The results of repeated measurement analysis of variance showed that after 12 weeks of exercise, the experimental group showed significantly improved sit-and-reach (P=0.002), knee flexion (left: P<0.001, right: P<0.001), hip flexion (left: P=0.024), hip extension (left: P<0.001, right: P<0.001), and ROM of shoulder joint (left: P<0.001, right: P=0.04) (Table 4). Compared with the control group, the experimental group of knee flexion (left, P<0.001; right, P<0.001), hip flexion (Compared with 6 weeks after the intervention, left, P=0.013; Compared with 12 weeks after the intervention, left, P=0.009), hip extension (left, P<0.001; right, P<0.001), shoulder joint (left, P=0.001; right, P=0.011) after 12 weeks of exercise therapy intervention, there were significant differences (Table 4). These findings suggest that the experimental group’s flexibility was better after 12 weeks of exercise therapy. The control group deteriorated in terms of hip extension (both left and right, Table 4) and shoulder joint (both left and right, Table 4).
Table 4.
Joint Range of Motion
| Experimental Group (n=20) | Contrast Group (n=20) | ||||||
|---|---|---|---|---|---|---|---|
| Pre | Mid | Post | Pre | Mid | Post | ||
| Sit-and-reach(cm) | −0.91±7.75 | 2.06±8.63 | 2.58±8.56## | 1.77±35.20 | 0.24±4.61 | 0.25±5.85 | |
| Knee flexion (°) | Left | 53.09±10.13 | 56.65±7.62 | 83.95±18.78##** | 57.40±5.46 | 61.25±7.84 | 58.10±13.17 |
| Right | 53.20±7.86 | 53.75±7.29 | 84.55±16.38##** | 55.25±6.62 | 58.15±8.74 | 55.30±16.43 | |
| Hip flexion (°) | Left | 84.20±14.61 | 85.20±12.23* | 84.85±13.08** | 80.15±12.55 | 76.00±10.09 | 74.75±9.96# |
| Right | 76.20±14.45 | 78.00±9.45 | 78.45±11.94 | 74.20±8.59 | 75.90±8.16 | 75.55±13.23 | |
| Hip extension (°) | Left | 7.40±4.03 | 6.60±5.37 | 12.25±5.87##** | 15.70±3.61 | 16.60±3.68 | 15.70±3.95 |
| Right | 7.15±7.89 | 6.30±4.74 | 12.45±7.13##** | 15.80±5.02 | 16.60±6.68 | 14.45±7.89 | |
| Shoulder joint (cm) | Left | 21.58±10.30 | 20.10±8.00 | 16.10±7.69##** | 23.85±8.37 | 23.60±8.52 | 25.30±8.50 |
| Right | 17.65±7.57 | 18.11±7.94 | 14.24±6.43##* | 19.38±8.22 | 19.38±8.34 | 20.65±8.50 | |
Notes: Data are shown as mean ± SD. *p<0.05, **p<0.01, comparisons are significant between the control group and the experimental group. #p<0.05, ##p<0.01, comparisons are significant within groups.
Abbreviations: cm, the unit is centimeter; °, the unit is degree.
Discussion
“Health Qigong” is defined as a compound term in China. On the one hand, it is for the purpose of health and has the significance of fitness; on the other hand, it is a standardized fitness method that takes Qigong as the means of exercise. Health Qigong is a kind of sport that aims at health and is based on gentle physical activities. Its physical and mental state tends to integrate body, breath, and heart adjustment.27 Through 12 weeks of exercise therapy intervention, we found that Health Qigong can improve the body coordination, dynamic and static balance ability, gait, joint activity ability of Parkinson’s patients. The monitoring of the number of patients who continuously participated in the exercise and test showed that the average attendance rate of Health Qigong was 89% (78–100%). Reasons for absence include medical treatment, forgetfulness or illness. Most Health Qigong participants (91%) had mastered the skills at the end of the project. During the project evaluation, participants said they liked the Health Qigong project very much and 90% of them would continue to practice. No injuries or discomfort were reported during the exercise, showing good compliance and acceptance. Compared with the previous intervention studies mostly involved in gait and balance function of patients with Parkinson’s disease, this study increased the monitoring of the physiological index of joint range of motion, which more comprehensively showed the effect of Health Qigong on motor function of patients with Parkinson’s disease. In the following sections, we further discuss and interpret the results.
Reaction and Balance
Reaction generally refers to the body by in vivo or in vitro stimulation caused by the corresponding activities. Balance refers to keeping body balance, keeping balance during and after body movement, and restoring balance. The more complex and faster the movements are, the higher the requirements for the body’s reaction ability and balance ability are. Because most Parkinson’s patients are elderly people, all parts of the body not only have natural physiological aging but also are affected by Parkinson’s movement disorder symptoms, resulting in the decline of reaction time and balance ability of patients. The results of exercise therapy showed that Health Qigong exercise therapy improves coordination, reaction ability, and balance.
Patients with PD are prone to falls because of movement disorders; this is one reason why many patients avoid going out and communicating with the outside world, aggravating their disease progression.28 Health Qigong exercise therapy for PD is based on the typical motor symptoms associated with PD disease. At the same time, the exercise environment and communication can promote the social communication ability of PD patients, which has a potentially positive impact on the psychological mood of PD patients.28,29 For patients who are susceptible to falls, strengthening static and dynamic balance abilities can enhance muscle strength of lower limbs and can help prevent falls. Squatting, clenching both fists, glaring, and twisting not only relieves nerve fatigue and relaxes the nervous system but also strengthens core muscles, improve the activity of joints, and improves proprioceptive input to the trunk and lower limbs, thereby improving motor performance in patients with PD.
Physical Coordination
The ability of physical coordination is the ability of the human brain to call on all parts of the body to cooperate with each other and finally complete the action. Of course, this ability is gradually developed in the process of growth and development, but it is also affected by age, sports ability, and other factors. Both strength, physical coordination, and cardiorespiratory capacity are shown to decline with aging, Compared with aerobic training, concurrent training, and multimodal training, functional training will have more potential to improve human physical coordination.30 Regular physical coordination exercises can not only improve the behavior and neurophysiological outcomes among older adults but also have a positive impact on their quality of life.31 Health Qigong comprehensive exercises set coordination, speed, balance ability, flexibility, and other physical qualities, which fully reflect the central nervous system’s function of controlling and regulating muscle activities. Sports such as yoga may be limited by the conditions of sports equipment and venues, and there may be hidden risks in sports such as antagonism sports, Health Qigong exercise is not limited to the venue and environment, and its movements are easy to learn and safe. In the process of exercise, more symmetrical exercises are used, such as the left and right alternation movements of Health Qigong Liuzijue, the change of body direction, which can fully mobilize the attention of PD patients and relax and breathe so that they can devote themselves to exercise. The physical coordination ability of PD patients was improved by the Health Qigong exercise, and the balance ability and reaction speed was improved simultaneously.
Gait Performance
Significant improvements in gait kinematic parameters (such as striding speed and step length) began in the 6th week of training, and there was no significant difference in gait speed. The movements selected from Health Qigong·Baduanjin can effectively increase the strength of leg muscles by emphasizing regular lower limb activities. In the process of practice, attention should be paid to breathing and the coordination of ideas, which can more effectively promote balance and walking ability.32 This is similar to the influence mechanism of Taiji, but comparatively speaking, the movements of Health Qigong are easier to learn.33 Studies have shown that gastrocnemius and tibialis anterior muscles have an important impact on gait in patients with PD; therefore, we need to exercise these two muscles. During movement, the patient’s body must rotate left and right, opening their step and moving the body’s center of gravity to exercise the waist and knee. Meanwhile, heel lifting effectively stimulates calf gastrocnemius and other muscle groups’ strength and lengthens the plantar muscles and ligaments. To exercise the anterior tibialis muscle, there is a “hook foot” exercise that can effectively exercise this muscle group at the warm-up stage. These movements improve gait stability, stride length, and walking speed.
Joint Range of Motion
With increased age, joint flexibility decreases, particularly in middle-aged and older adults. In the most severe cases, there is a decreased quality of life, leading to accelerated aging and limitation of daily activities. In patients with PD patients, these limitations are more pronounced. During exercise, we required patients to stretch their arms, move up and down, rotate their wrists and waist, bend and extend their lower limbs, and lift their heels and knees. All this improved their joints’ flexibility, increased their levels of physical activity ability, and possibly reduced the risk of injury.
Limitations
A potential limitation of the present study was the small sample size, at the beginning of the study, due to such as illness and personal various reasons, there was a loss of sample size. Twelve weeks of Health Qigong exercise improved various parameters; however, we did not perform a long-term survey, and therefore we cannot make definitive statements regarding the long-term effects. There are few studies regarding the mechanism of Health Qigong exercise on the motor function of patients with PD. Further research is needed to confirm our findings and to provide a comprehensive explanation using physiological and psychological evaluations.
Conclusion
Health Qigong exercise significantly improves physical functions in patients with PD, including balance, gait, and joint range of motion. Health Qigong exercise may reduce the risk of movement disorders in PD patients. As a safe and effective clinical alternative therapy, it is worthy of promotion.
Acknowledgments
We gratefully acknowledge the financial support from the Beijing Sport University International cooperation topics (Project number 2020046). Zhirong Wan and Xiaolei Liu are co-first authors.
Ethics Approval and Informed Consent
In addition, all mentioned procedures in our study were performed according to the declaration of Helsinki.
The study was approved by the Ethics Committee of Beijing Sport University and Beijing Aerospace Central Hospital (Department of Neurology), and a written informed consent was obtained from every eligible subject.
Disclosure
Dr Zhirong Wan reports grants from Beijing Sport University, during the conduct of the study. Dr Xiaolei Liu reports grants from Beijing Sport University, during the conduct of the study. Professor Hui Yang reports grants from Beijing Sport University, during the conduct of the study. Miss Fang Li reports grants from Beijing Sport University, during the conduct of the study. Miss Lei Li reports grants from Beijing Sport University, during the conduct of the study. Professor Yulin Wang reports grants from Beijing Sport University, during the conduct of the study. Dr Hao Jiang reports grants from Beijing Sport University, during the conduct of the study. Prof. Dr. Jichen Du reports grants from Beijing Sport University, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- 1.Thaut MH, Rice RR, Braun Janzen T, et al. Rhythmic auditory stimulation for reduction of falls in Parkinson’s disease: a randomized controlled study. Clin Rehabil. 2019;33(1):34–43. PMID: 30033755. doi: 10.1177/0269215518788615 [DOI] [PubMed] [Google Scholar]
- 2.Santos-García D, de Deus FT, Suárez CE, et al. Non-motor symptom burden is strongly correlated to motor complications in patients with Parkinson’s disease. Eur J Neurol. 2020;27(7):1210–1223. PMID: 32181979. doi: 10.1111/ene.14221 [DOI] [PubMed] [Google Scholar]
- 3.Debû B, De oliveira godeiro C, Lino JC, et al. Managing gait, balance, and posture in Parkinson’s Disease. Curr Neurol Neurosci Rep. 2018;18(5):23. PMID: 29623455. doi: 10.1007/s11910-018-0828-4 [DOI] [PubMed] [Google Scholar]
- 4.Mak MKY, Wong-Yu ISK. Exercise for Parkinson’s disease. Int Rev Neurobiol. 2019;147:1–44. PMID: 31607351. doi: 10.1016/bs.irn.2019.06.001 [DOI] [PubMed] [Google Scholar]
- 5.Du GQ, Fang BY, Xi JN, et al. Study on rehabilitation drug utilization in patients with Parkinson’s disease. China Med. 2020;15(11):1790–1794. doi: 10.3760/j.issn.1673-4777.2020.11.032 [DOI] [Google Scholar]
- 6.Tang L, Fang Y, Yin J. The effects of exercise interventions on Parkinson’s disease: a Bayesian network meta-analysis. J Clin Neurosci. 2019;70:47–54. PMID: 31526677. doi: 10.1016/j.jocn.2019.08.092 [DOI] [PubMed] [Google Scholar]
- 7.Borrione P, Tranchita E, Sansone P, et al. Effects of physical activity in Parkinson’s disease: a new tool for rehabilitation. World J Methodol. 2014;4(3):133–143. PMID: 25332912; PMCID: PMC4202452. doi: 10.5662/wjm.v4.i3.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang XX. Effect of exercise therapy on improving dyskinesia in patients with Parkinson’s disease. Guide China Med. 2014;12(25):224–225. doi: 10.15912/j.cnki.gocm.2014.25.462 [DOI] [Google Scholar]
- 9.Liu XL, Chen S, Wang Y. Effects of Health Qigong Exercises on relieving symptoms of Parkinson’s disease. Evid Based Complement Alternat Med. 2016;2016:5935782. PMID: 27891159; PMCID: PMC5116525. doi: 10.1155/2016/5935782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodwin VA, Richards SH, Taylor RS, et al. The effectiveness of exercise interventions for people with Parkinson’s disease: a systematic review and meta-analysis. Mov Disord. 2008;23(5):631–640. PMID: 18181210. doi: 10.1002/mds.21922 [DOI] [PubMed] [Google Scholar]
- 11.Li Z, Wang T, Liu H, et al. Dual-task training on gait, motor symptoms, and balance in patients with Parkinson’s disease: a systematic review and meta-analysis. Clin Rehabil. 2020;34(11):1355–1367. PMID: 32660265. doi: 10.1177/0269215520941142 [DOI] [PubMed] [Google Scholar]
- 12.Kwok JY, Choi KC, Chan HY. Effects of mind-body exercises on the physiological and psychosocial well-being of individuals with Parkinson’s disease: a systematic review and meta-analysis. Complement Ther Med. 2016;29:121–131. PMID: 27912936. doi: 10.1016/j.ctim.2016.09.016 [DOI] [PubMed] [Google Scholar]
- 13.Dos SDM, Komeroski IG, Monteiro EP, et al. Effects of dance practice on functional mobility, motor symptoms and quality of life in people with Parkinson’s disease: a systematic review with meta-analysis. Aging Clin Exp Res. 2018;30(7):727–735. PMID: 28980176. doi: 10.1007/s40520-017-0836-2 [DOI] [PubMed] [Google Scholar]
- 14.Kwok JYY, Kwan JCY, Auyeung M, et al. The effects of yoga versus stretching and resistance training exercises on psychological distress for people with mild-to-moderate Parkinson’s disease: study prxotocol for a randomized controlled trial. Trials. 2017;18(1):509. PMID: 29096672; PMCID: PMC5667474. doi: 10.1186/s13063-017-2223-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li F, Harmer P, Fitzgerald K, et al. Tai chi and postural stability in patients with Parkinson’s disease. N Engl J Med. 2012;366(6):511–519. PMID: 22316445; PMCID: PMC3285459. doi: 10.1056/NEJMoa1107911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Y, Li XY, Gong L, et al. Tai Chi for improvement of motor function, balance and gait in Parkinson’s disease: a systematic review and meta-analysis. PLoS One. 2014;9(7):e102942. PMID: 25047456; PMCID: PMC4105461. doi: 10.1371/journal.pone.0102942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wassom DJ, Lyons KE, Pahwa R, et al. Qigong exercise may improve sleep quality and gait performance in Parkinson’s disease: a pilot study. Int J Neurosci. 2015;125(8):578–584. PMID: 25233147. doi: 10.3109/00207454.2014.966820 [DOI] [PubMed] [Google Scholar]
- 18.Klein PJ, Baumgarden J, Schneider R. Qigong and Tai Chi as therapeutic exercise: survey of systematic reviews and meta-analyses addressing physical health conditions. Altern Ther Health Med. 2019;25(5):48–53. PMID: 31221939. [PubMed] [Google Scholar]
- 19.Alberts JL, Rosenfeldt AB. The universal prescription for Parkinson’s disease: exercise. J Parkinsons Dis. 2020;10(s1):S21–S27. PMID: 32925109; PMCID: PMC7592674. doi: 10.3233/JPD-202100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saint-Hilaire M, Ellis T. A prescription for physical therapy and exercise in Parkinson’s disease. Adv Parkinson’s Dis. 2013;2(04):118–120. doi: 10.4236/apd.2013.24023 [DOI] [Google Scholar]
- 21.Yang Y, Qiu WQ, Hao YL, et al. The efficacy of traditional Chinese Medical Exercise for Parkinson’s disease: a systematic review and meta-analysis. PLoS One. 2015;10(4):e0122469. doi: 10.1371/journal.pone.0122469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiao CM, Zhuang YC. Effect of health Baduanjin Qigong for mild to moderate Parkinson’s disease. Geriatr Gerontol Int. 2016;16(8):911–919. PMID: 26310941. doi: 10.1111/ggi.12571 [DOI] [PubMed] [Google Scholar]
- 23.Li Z, Zhuang J, Jiang Y, et al. Study protocol for a single-blind randomised controlled trial to evaluate the clinical effects of an Integrated Qigong exercise intervention on freezing of gait in Parkinson’s disease. BMJ Open. 2019;9(9):e028869. PMID: 31515419; PMCID: PMC6747653. doi: 10.1136/bmjopen-2018-028869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moon S, Sarmento CVM, Steinbacher M, et al. Can Qigong improve non-motor symptoms in people with Parkinson’s disease - A pilot randomized controlled trial? Complement Ther Clin Pract. 2020;39:101169. PMID: 32379638; PMCID: PMC7607921. doi: 10.1016/j.ctcp.2020.101169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Song R, Grabowska W, Park M, et al. The impact of Tai Chi and Qigong mind-body exercises on motor and non-motor function and quality of life in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism. Relat Disord. 2017;41:3–13. PMID: 28602515; PMCID: PMC5618798. doi: 10.1016/j.parkreldis.2017.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu PL, Lee M, Huang TT. Effectiveness of physical activity on patients with depression and Parkinson’s disease: a systematic review. PLoS One. 2017;12(7):e0181515. PMID: 28749970; PMCID: PMC5531507. doi: 10.1371/journal.pone.0181515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yu P, Li W, Li H, et al. The efficacy and safety of health qigong for anti-aging: protocol for a systematic review and meta-analysis. Medicine (Baltimore). 2020;99(49):e22877. PMID: 33285677; PMCID: PMC7717840. doi: 10.1097/MD.0000000000022877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schootemeijer S, van der Kolk NM, Ellis T, et al. Barriers and motivators to engage in exercise for persons with Parkinson’s disease. J Parkinsons Dis. 2020;10(4):1293–1299. PMID: 32925106; PMCID: PMC7739964. doi: 10.3233/JPD-202247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Šumec R, Filip P, Sheardová K, et al. Psychological benefits of nonpharmacological methods aimed for improving balance in Parkinson’s disease: a systematic review. Behav Neurol. 2015;2015:620674. PMID: 26236107; PMCID: PMC4508472. doi: 10.1155/2015/620674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lucas MN, Tiego AD, Fabrício ER, et al. The effect of different training modalities on physical fitness in women over 50 years of age. Motriz: Revista De Educação Física. 2017;22(4):319–326. doi: 10.1590/s1980-6574201600040016 [DOI] [Google Scholar]
- 31.Dunsky A. The effect of balance and coordination exercises on quality of life in older adults: a mini-review. Front Aging Neurosci. 2019;11:318. PMID: 31803048; PMCID: PMC6873344. doi: 10.3389/fnagi.2019.00318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zou L, Pan Z, Yeung A, et al. A review study on the beneficial effects of Baduanjin. J Altern Complement Med. 2018;24(4):324–335. PMID: 29227709. doi: 10.1089/acm.2017.0241 [DOI] [PubMed] [Google Scholar]
- 33.Deuel LM, Seeberger LC. Complementary therapies in Parkinson Disease: a review of acupuncture, Tai Chi, Qi Gong, Yoga, and Cannabis. Neurotherapeutics. 2020;17(4):1434–1455. PMID: 32785848;PMCID: PMC7851283. doi: 10.1007/s13311-020-00900-y [DOI] [PMC free article] [PubMed] [Google Scholar]


