Abstract
Background:
The United States (U.S.) is experiencing an ongoing opioid crisis. Economic burden estimates that describe the impact of the crisis are needed when considering federal and state resources devoted to addressing overdoses. In this study, we estimate the societal costs for opioid use disorder and fatal overdose from all opioids in 2017.
Methods:
We estimated costs of fatal overdose from all opioids and opioid use disorder based on the incidence of overdose deaths and the prevalence of past-year opioid use disorder for 2017. Incidence of fatal opioid overdose was obtained from the National Vital Statistics System; prevalence of past-year opioid use disorder was estimated from the National Survey of Drug Use and Health. Costs were estimated for health care, criminal justice and lost productivity. Costs for the reduced quality of life for opioid use disorder and life lost due to fatal opioid overdose were valued using U.S. Department of Health and Human Services guidelines for valuing reductions in morbidity and mortality.
Results:
Costs for opioid use disorder and fatal opioid overdose in 2017 were estimated to be $1.02 trillion. The majority of the economic burden is due to reduced quality of life from opioid use disorder and the value of life lost due to fatal opioid overdose.
Conclusions:
These estimates can assist decision makers in understanding the magnitude of opioid use disorder and fatal overdose. Knowing the magnitude and distribution of the economic burden can inform public policy, clinical practice, research, and prevention and response activities.
Keywords: Opioid, use disorder, overdose, costs
1. Introduction
The United States is experiencing an ongoing overdose crisis. The nature of the crisis is also changing rapidly. There have been three distinct waves of the crisis. A marked increase in overdoses involving prescription opioids began in the late 1990s. Heroin overdose death rates started to climb in 2010. Since 2013, there has been a marked increase in fatal overdoses involving synthetic opioids such as illicitly made fentanyl (Scholl et al., 2019), although rates of opioid use disorder have remained relatively stable (US Department of Health and Human Services, 2018). There is evidence that illicitly manufactured fentanyl, an extremely powerful opioid, is responsible for the recent increase in opioid overdose deaths (Dowell et al., 2017).
Economic burden estimates that describe the impact of the opioid crisis can be useful information for decision makers when considering the amount of resources devoted to addressing it. It is important for these estimates to demonstrate both the overall magnitude of the problem and how it effects specific parts of the economy. For example, decision makers in health care will need to know how they are impacted by increases in costs for treatment. Employers may be particularly interested in how the productivity of workers are affected. While these types of tangible financial considerations are important, to understand the broader impact of the crisis on society it is also necessary to attempt to quantify the impact of the crisis on the overall value lost from increased morbidity and mortality.
Several studies have estimated the economic impact of opioid use disorder and fatal opioid overdose (Birnbaum et al., 2006; Birnbaum et al., 2011; Rice et al., 2014). Most of these studies have focused on the component of the crisis related to prescription opioids. For example, Florence, et al. (2016) estimated that the economic burden of prescription opioid use disorder and fatal overdose in 2013 was $78.5 billion (Florence et al., 2016). The components of this estimate included health care, criminal justice, and lost productivity. A 2017 report from the President’s Council of Economic Advisers (CEA) (CEA, 2017) pointed out that the methods used in the Florence, et al. study did not measure the full social impact of fatal overdoses. In order to measure these costs, CEA included a value for lost life that incorporated the concept of “willingness to pay” for reductions in mortality risk - the value of a statistical life (VSL). The CEA report also expanded the valuation to all cases of opioid use disorder and opioid overdose and estimated an overall economic impact of approximately $500 billion for 2015. This report, however, did not measure the value of quality of life lost by opioid use disorder. Also, the number of fatal overdoses has risen substantially since 2015 (Scholl et al., 2019).
In this study, we estimate the costs for opioid use disorder and fatal overdose from all opioids (both prescription and illicit) for 2017. We extend the analysis to measure the value of reduced quality of life for opioid use disorder. These estimates provide an up-to-date understanding of the overall economic impact of the crisis. The expanded valuation methods used also provide the fullest accounting to date of the impact of the crisis.
2. Methods
2.1. Overview
We calculated cost estimates of fatal opioid overdose and opioid use disorder based on the incidence of opioid overdose deaths and the prevalence of past-year opioid use disorder for calendar year 2017 using a societal perspective. Societal costs include both the cost for persons experiencing overdose or use disorder, and costs incurred by society in general, such as criminal justice related costs. Costs calculated for opioid use disorder are annual costs, while costs for fatal cases are lifetime costs discounted to 2017 present value at a rate of 3%. We used the most recently available year of data for all cost components. When the most recent year of data available was earlier than 2017, costs were inflation-adjusted to 2017 dollars.
Our measure of the 2017 incidence of opioid overdose deaths came from the United States National Vital Statistics System mortality file (Centers for Disease Control and Prevention and National Center for Health Statistics, 2018). Cases were identified first using the underlying (X40-X44,X60-X64,X85,Y10-Y14) and then multiple cause of death (T40.0-T40.4, T40.6) International Classification of Diseases, Tenth Revision (ICD-10)codes. This includes all opioid-related overdose deaths regardless of intent (intentional, unintentional, homicide, or undetermined). Prevalence of past-year opioid use disorder was measured using the 2017 National Survey on Drug Use and Health (NSDUH) (Center for Behavioral Health Statistics and Quality, 2018). The NSDUH is a nationally representative sample of the U.S. civilian noninstitutionalized population ages 12 and older. The survey collects detailed information on substance use, including a questionnaire that identifies opioid use disorder (opioid abuse or dependence) based on questions similar to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) (American Psychiatric Association, 1994). The survey also collects detailed data on health insurance coverage during the year, and basic demographic information such as gender and age. This information was used in assigning health care costs and lost productivity costs to opioid use disorder cases, as described in more detail below. Survey weights were used to estimate nationally representative population totals for cases of opioid use disorder. Details of all calculations presented below may be found in the electronic appendix that accompanies this study.
2.2. Health Care Costs
Health care costs were taken from estimates in a previously published study and inflated to 2017 dollars (Florence et al., 2016). The original source study used a matched case-control design to estimate the impact of opioid use disorder diagnoses on health care spending. This design was implemented using the de-identified IBM MarketScan® Research Databases (IBM, 2013) for commercial, Medicaid and Medicare health plan enrollees for the years 2012–2013. Matching controlled for basic demographic variables, health status was matched based on the Charlson comorbidity index and health care costs prior to use disorder diagnosis, and regression models controlled for skewness in the expenditure data. The resulting cost estimate is the increase in annual health care costs associated with opioid use disorder. This includes direct treatment costs for the disorder (such as medically-treated nonfatal overdoses) as well as more general health care costs associated with the disorder (e.g. increased office visits).
The increased medical cost associated with opioid use disorder was then multiplied by the relevant number of persons with opioid use disorder derived from the NSDUH for each insurance coverage category reported in the survey data (Private, Medicare, Medicaid, CHAMPUS/VA, other and uninsured). CHAMPUS/VA and other categories were assigned costs for private coverage. Costs for the uninsured were imputed using the method described in a previously issued report from the Kaiser Family Foundation (Coughlin et al., 2014).
Not all treatment for substance use disorder is funded by health insurance, so additional costs of treatment for other programs such as Substance Abuse and Mental Health Services Administration (SAMHSA) block grants and private foundation funding were estimated by identifying non-insurance-based federal (e.g. SAMHSA block grants, Department of Veterans Affairs, etc.), state and local (e.g. non-Medicaid programs funded through mental health and substance abuse agencies), and private (e.g. philanthropic and other nonpatient revenue sources) expenditures on treatment for substance use disorder (Substance Abuse and Mental Health Services Administration, 2014). These costs were multiplied by the share of past-year opioid use disorder cases as a share of all past-year substance use disorder cases in the 2017 NSDUH.
2.3. Crime Related Costs
We updated the criminal justice costs using identical methods to those in Florence, et al. (2016), but using more recent data sources. This method consists of using reported criminal justice spending for drug crimes and multiplying that number by the share of past-year opioid use disorder cases from NSDUH. Criminal justice costs consisted of four components: (1) police protection, (2) legal and adjudication, (3) correctional facilities, and (4) property lost due to crimes. We obtained spending data on police protection, legal and adjudication activities, and correctional facilities from the Justice Expenditure and Employment Extracts, 2015 – Preliminary (Bronson, 2018) and data on property lost due to crimes from the Crime in the United States 2016 (United States Department of Justice, 2016). We estimated the ratio of arrests for the components of police protection and legal and adjudication (Drug Enforcement Administration, 2018; Harwood et al., 2004; United States Department of Justice, 2016; Substance Abuse and Mental Health Services Administration, 2018), the ratio of incarcerations for the correctional facilities component (Carson, 2018), and the ratio for the component of property lost due to crimes.
2.4. Lost Productivity Costs
To value lost productivity, we followed the same methodology as Florence, et al. (2016), but extend the analysis to both illicit and prescription opioids. We measure lost productivity costs from: (1) premature death from opioid overdose, (2) reduced productive hours for opioid use disorder, and (3) incarceration related to opioids. Costs for overdose deaths were estimated in the CDC’s WISQARS™ (Web-based Injury Statistics Query and Reporting System) cost module (Centers for Disease Control Prevention, 2015). Lost productivity from fatal overdoses was estimated using the costs of all poisoning deaths in WISQARS™. Lost productivity in WISQARS includes the value of lost salary and fringe benefits, and well as the loss of household production (Lawrence et al., 2014).
In calculating lost productivity for opioid use disorder, we used an approach that values the loss of “productive hours” and employs updated estimates of the value of productive hours for the U.S. population (Gross et al., 2018). This value then was multiplied by the percentage reduction in productivity attributable to opioid use disorder (17% for males and 18% for females (National Drug Intelligence Center, 2011)), and finally summed over values across all gender and age groups. The prevalence of opioid use disorder cases for each gender and age group were tabulated from the 2017 NSDUH, then multiplied by the corresponding per person annual production value of U.S. population (Gross et al., 2018) which was inflated to 2017 dollars.
To calculate lost productivity due to incarceration, we first used the numbers of inmates incarcerated for crimes attributed to opioid use disorder at federal, state, and local levels in 2016 (Carson, 2018; Drug Enforcement Administration, 2018), following the same apportionment method described above for criminal justice costs. After estimating the numbers of federal, state, and local inmates incarcerated for crimes attributed to opioid use disorder, we then multiplied those numbers by the per person annual production value of the U.S. population inflated to 2017 dollars.
2.5. Valuation of Lost Quality of Life and Life Lost
To estimate the value of lost quality of life due to opioid related morbidity and life lost due to fatal opioid overdose, we followed recently issued guidelines for regulatory impact analysis by the U.S. Department of Health and Human Services (HHS) (Office of the Assistant Secretary for Planning and Evaluation, 2016). These guidelines were issued to assist agencies that are required to evaluate the overall costs and benefits of proposed regulations. The guidelines recommend using measures of lost quality of life and the VSL that are specific to the outcome being analyzed, when feasible. The rationale for this is that the preferences of the U.S. population for reducing the risk of morbidity and mortality may differ by the cause and population affected. However, the guidelines provide consensus estimates of a VSL, discounted to present value at a rate of 3%.
For opioid use disorder, we calculated the lost health-related quality of life (HRQOL) per person compared to a person without opioid use disorder based on weights developed to estimate the effect on HRQOL for persons with opioid use disorder (Wittenberg et al., 2016). These HRQOL weights are based on a survey of 1,178 participants from the US population to assess the reduction in quality of life based on whether or not a person with opioid use disorder was currently using opioids either by injection or prescription opioid misuse (medication assisted treatment is not considered drug use), was currently in the initiation stage of treatment for opioid use disorder, was in the stabilization stage of treatment, or was in remission. Since the stage of treatment is not available in the NSDUH survey responses, we used the mean HRQOL weight across the treatment categories to assign weights to the “in treatment” group. HRQOL weights are defined on a scale from 0 (death) to 1 (perfect health). The reference study assigned a weight of 1 to a person with no history of opioid use disorder, and estimated weights for each defined category of treatment status, drug use, and injection status. Specific HRQOL weights used and detailed calculations are available in the electronic appendix.
We estimated the number of persons that met each category for the HRQOL weights using 2017 data from the NSDUH. We estimated the number of opioid use disorder cases and defined four stratification categories of users by treatment status, current opioid use (excluding medication assisted use disorder treatment), and injection drug use status, within the previous 12 months. We multiplied the value of the HRQOL decrease by the VSLY value provided in the HHS Guidelines, updated for income growth and inflation to 2017 dollars (VSLY=$517,324; details included in electronic appendix).
The value of life lost due to opioid overdose was determined by multiplying the number of overdose cases by the consensus VSL estimates for 2017 (VSL=$10.1 million). Our total valuation of economic burden of opioid use disorder and fatal overdose is therefore the sum of the HRQOL/VSL valuation, health care and substance use disorder treatment cost, criminal justice and lost productivity. Detailed data and calculations for all estimates are available in the electronic appendix.
2.6. Sensitivity Analysis
Calculation of the economic burden in this study uses data from a variety of sources, so it is not possible to directly estimate a traditional confidence interval for the estimates. In order to demonstrate the sensitivity of our analysis to changes in model parameters, we conducted probabilistic simulations of the various cost categories. Cost categories that used estimates of the number of persons with opioid use disorder used a Pert distribution centered at the estimated number of persons, and the 2.5% and 97.5% cutoffs based on the confidence interval for the estimate. Components that used published results with a reported standard error or confidence interval, such as the QALY weights for opioid use disorder, assumed a normal distribution with the reported estimate as the mean and the variance defined by the reported standard error or confidence interval. For model inputs that did not have a reported confidence interval, we assumed a Pert distribution that varied the input by +/− 10%. We then conducted a simulation with 10,000 replications and report a 95% prediction interval [PI] that is at the 2.5% and 97.5% cutoffs of the distribution of estimates in the simulation. Distribution assumptions were made to provide a simulation using a range of plausible values of the model parameters but are not necessarily the actual distributions of the underlying variables.
We also examined the sensitivity of our results to the use of a number of alternative assumptions and data sources. For example, a number of recent studies have examined the impact of opioid use disorder on health care spending. We used results from a recent study that estimates health care costs across a variety of health care payers to examine how these more recent estimates affect our results{Davenport et al., 2019}.
To examine the sensitivity of our results to various estimates of a VSL, we calculated a range for HRQOL lost and life lost using the low and high values of a VSL provided in the HHS Guidelines. We also estimate the burden using alternative weights of the HRQOL lost. The alternative weights were chosen by reviewing a range of estimates of HRQOL estimates for study subjects with opioid use disorder in studies of the cost effectiveness of various types of use disorder treatment. The weights used were chosen to represent the range of reductions to HRQOL in these studies. The low end of these alternative measures compared scores on the EQ-5D for persons with opioid use disorder who were in treatment to those who were not (Woody et al, 2008). The high end of these measures used the Australian Quality of Life instrument (AQoL), and compares study subjects at baseline to their scores taken at various intervals over the course of treatment{Harris et al., 2005}. We use these alternative measures as a sensitivity analysis, and not as our primary results, because both instruments lacks specificity to the condition being studied, and the populations studied were limited to subsets of the population of persons with opioid use disorder (e.g. only those who use heroin). Finally, previous research has shown that both fatal opioid overdose (Ruhm, 2017) and opioid use disorder (Barocas et al., 2018) is likely undercounted in the data sources we used. To examine the sensitivity of our results to the undercount of fatal overdose cases, we estimated costs using results of a recent study that used contributing cause of death data to classify opioid overdose deaths, which showed this increased the number of deaths by 28% (Boslett et al., 2020).
Opioid use disorder can be undercounted because the NSDUH surveys the noninstitutionalized population, which will exclude incarcerated persons. The homeless population will also likely be missed by household-based surveys. Both of these populations have been shown to have high rates of substance use disorder (Barocas et al., 2018). We examine the sensitivity of our results to including these populations in our estimate of opioid use disorder costs. We estimated the number of incarcerated persons by using data on the incarcerated population (Bronson and Carson, 2017) and the share of this population estimated to have substance use disorders (National Institute on Drug Abuse, 2020). We estimated the number of homeless persons by using estimates of the homeless population (Addiction Center, 2020) and the share of this populations with substance use disorders. For both the incarcerated and homeless populations with substance use disorder, we attributed the share with opioid use disorder by using the share of opioid use disorder as a share of all substance use disorders from the 2017 NSDUH.
3. Results
Table 1 reports the estimated number of persons with past-year opioid use disorder, and the number of fatal overdoses involving opioids (prescription and illicit) in 2017. There were approximately 2.1 (95% confidence interval [CI] 1.9 to 2.4) million persons ages 12 years and older with an opioid use disorder, and 47,600 fatal opioid overdoses.
Table 1.
Prevalence of Opioid Use Disorder and Fatal Opioid Overdose, United States 2017
| Outcome | Cases in 2017 (95% Confidence Interval) |
|---|---|
| Opioid Use Disorder* (Millions) |
2.129 (1.874, 2.385) |
| Fatal Overdose** (Number of Deaths) |
47,600 |
National Survey of Drug Use and Health, 2017, for U.S. non-institutional population age 12 and over.
National Vital Statistics System mortality data; Opioid Overdose deaths identified based on International Classification of Diseases, Tenth Revision codes for drug overdoses: X40–X44, X60–X64, X85, and Y10–Y14; the type of drug involved was based on ICD-10 codes for opioids (all T40.0–T40.4 and T40.6).
The economic burden of opioid use disorder and fatal opioid overdose is presented in Table 2. The overall economic burden totaled approximately $1,020.7 billion (95% PI $967.2 to $1,075.7 billion) in 2017. Slightly less than half of these costs were attributable to opioid use disorder ($471.0 billion (95% PI $417.8 to $525.7billion)). Almost $35 billion of the costs were associated with health care ($31.3 billion (95% PI $25.2 to $37.4 billion)) and opioid use disorder treatment ($3.5 billion (95% PI $3.4 to $3.7 billion)). Approximately $23 billion are related to criminal justice spending ($14.8 billion) and lost productivity of incarcerated individuals ($7.8 billion). Lost productivity, for individuals with opioid use disorder ($23.5 billion) and fatal opioid overdose ($68.7 billion), together accounts for over $92 billion.
TABLE 2.
Estimated Costs of Opioid Use Disorder and Fatal Overdose, United States 2017 (Millions of 2017$)
| Nonfatal Costs | Aggregate Costs (95% Prediction Interval) | Percentage of Aggregate Costs |
|---|---|---|
| Health Care | ||
| Private Insurance | $12,902 | 1.3% |
| Medicare | $3,170 | 0.3% |
| Medicaid | $11,142 | 1.1% |
| Champus/VA | $1,124 | 0.1% |
| Other | $820 | 0.1% |
| Uninsured | $2,151 | 0.2% |
| Total | $31,308 | 3.1% |
| ($25,171, $37,444) | ||
| Substance Abuse Treatment | ||
| Federal | $844 | 0.1% |
| State and Local | $2,326 | 0.2% |
| Private | $365 | 0.0% |
| Total | $3,534 | 0.3% |
| ($3,355, $3,714) | ||
| Criminal Justice | ||
| Police protection | $6,209 | 0.6% |
| Legal and adjudication | $2,819 | 0.3% |
| Correctional facilities | $5,445 | 0.5% |
| Property lost due to crime | $347 | 0.0% |
| Total criminal justice costs | $14,819 | 1.5% |
| ($14,181, $15,462) | ||
| Lost Productivity | ||
| Reduced productive time/increased disability | $23,479 | 2.3% |
| Production lost for incarcerated individuals | $7,832 | 0.8% |
| Total Lost Productivity | $31,311 | 3.1% |
| ($26,681, $35,954) | ||
| Value of Reduced Quality of Life | $390,003 | 38.2% |
| ($337,693, $444,278) | ||
| Total Non Fatal Costs | $470,975 | 46.1% |
| ($417,783, $525,692) | ||
| Fatal Costs | ||
| Lost Productivity | $68,694 | 6.7% |
| Health Care | $260 | 0.0% |
| Value of Statistical Life Lost | $480,737 | 47.1% |
| Total Fatal Costs | $549,691 | 53.9% |
| ($544,835, $554,546) | ||
| Total of Nonfatal and Fatal | $1,020,666 | 100.0% |
| ($967,244, $1,075,680) | ||
Source: Author’s calculations using the National Survey of Drug Use and Health, the National Vital Statistics System mortality data; Opioid Overdose deaths identified based on International Classification of Diseases, Tenth Revision codes for drug overdoses: X40-X44, X60-X64, X85, and Y10-Y14; the type of drug involved was based on ICD-10 codes for opioids (all T40.0-T40.4 and T40.6), IBM MarketScan® Research Databases (Health Care Costs); Substance Abuse and Mental Health Services Administration. Projections of National Expenditures for Treatment of Mental and Substance Use Disorders, 2010–2020. (Use Disorder Treatment Costs), Bureau of Justice Statistics. Justice Expenditure and Employment Extracts, 2015 – Preliminary., United States Department of Justice, Federal Bureau of Investigation. Crime in the United States 2015., Office of National Drug Control Policy. The economic costs of drug abuse in the United States: 1992–2002., Drug Enforcement Administration. National Forensic Laboratory Information System: 2012 Annual Report., Carson EA. Prisoners in 2016. Bureau of Justice Statistics 2018, (Reduced Quality of Life) Wittenberg, E., Bray, J.W., Aden, B., Gebremariam, A., Nosyk, B., Schackman, B.R., 2016. Measuring benefits of opioid misuse treatment for economic evaluation: health-related quality of life of opioid-dependent individuals and their spouses as assessed by a sample of the US population. Addiction 111(4), 675–684., (Lost productivity: non-fatal) Krueger, K.V.G., Scott D. Pike, Jamison, 2018. Estimated annual and lifetime labor productivity in the United States, 2016: implications for economic evaluations Journal of Medical Economics, 1–8. (Value of statistical life and year) Office of the Assistant Secretary for Planning and Evaluation. Guidelines for regulatory impact analysis. Washington, DC: U.S. Department of Health and Human Services; 2016 and the (Health care costs and lost productivity: fatal) Web-based injury statistics query and reporting system (WISQARS). Prediction intervals are based on probabilistic simulations.
By far the largest components of the overall economic burden, however, are the value of reduced quality of life from opioid use disorder ($390.0 billion) and life lost to opioid overdose ($480.7 billion). These two cost components account for over 85% of the total economic burden.
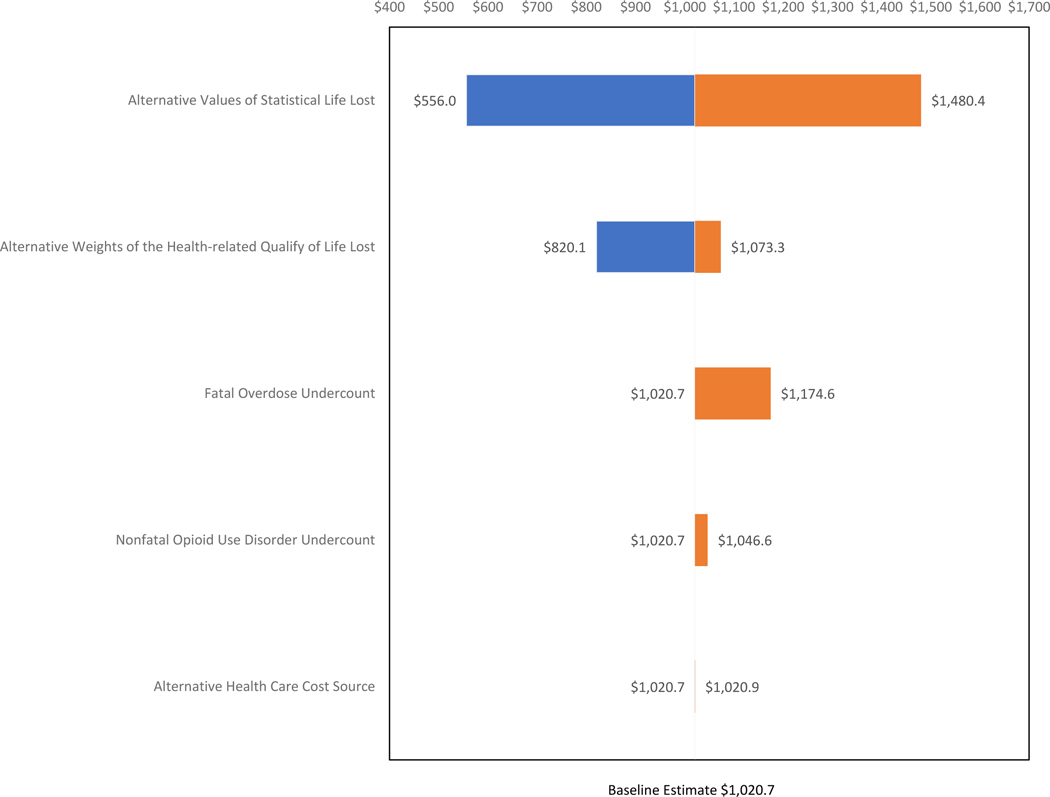
The results of our sensitivity analysis are presented in the Figure. The figure is arranged to show the relative impact of different scenarios on our estimates. Using and alternative source of health care cost data has the smallest impact on the estimates (from $1,020.7 billion to $1,020.9 billion). Including estimates of the incarcerated and homeless populations with opioid use disorder has a smaller impact ($1,020.7 billion to $1,046.6 billion) than adjusting for the undercount of fatal cases ($1,020.7 billion to $1,174.6 billion). Our baseline estimates fall within the range of estimates produced by using HRQoL weights from generic instruments ($820.1 billion to $1,073.3 billion). Our results are most sensitive to the choice of values for the VSL and VSLY. At the low estimate of a VSL/VSLY from the HHS guidelines, the overall economic burden is $556.0 billion, and at the high value of the VSL/VSLY, the overall burden is over $1,480.4 billion.
Figure. Sensitivity Analysis.
Source: Author’s calculations using the National Survey of Drug Use and Health, the National Vital Statistics System, mortality data; Opioid Overdose deaths identified based on International Classification of Diseases, Tenth Revision codes for drug overdoses: X40-X44, X60-X64, X85, and Y10-Y14; the type of drug involved was based on ICD-10 codes for opioids (all T40.0-T40.4 and T40.6), and (Value of Statistical Life) Office of the Assistant Secretary for Planning and Evaluation. Guidelines for regulatory impact analysis. Washington, DC: U.S. Department of Health and Human Services; 2016. (Health Related Quality of Life) Woody GE, Poole SA, Subramaniam G, et al. Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial. JAMA. 2008;300(17):2003–2011. Harris, A. H., Gospodarevskaya, E., & Ritter, A. J. (2005). A randomised trial of the cost effectiveness of buprenorphine as an alternative to methadone maintenance treatment for heroin dependence in a primary care setting. Pharmacoeconomics, 23(1), 77–91. (Fatal Overdose Undercount) Barocas, J., White, L., Jianing Wang, J., Walley, A., LaRochelle, M., Bernson, D., Land, T., Morgan, J., Samet, J., and Linas, B., 2018:Estimated Prevalence of Opioid Use Disorder in Massachusetts, 2011–2015: A Capture-Recapture Analysis. American Journal of Public Health 108, 1675–1681. (Nonfatal Use Disorder Undercount) Bronson, J. and Carson, E. Prisoners in 2017. 2019. U.S. Department of Justice, Washington, D.C.; Criminal Justice DrugFacts. 2020. National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services.; The Connection Between Homelessness and Addiction. 2020. Additions Center. (Health care costs) Davenport, S., A., Weaver, M., Caverly. 2019. Costs and Comorbidities of Opioid Use Disorder. Society of Actuaries. Milliman.
4. Discussion
This study identified a substantial amount of economic value lost due to the opioid crisis in 2017. Slightly more than one-half of the cost is associated with fatal overdoses. This is a change from previously published estimates, where a large share of costs was attributable to opioid use disorder (Birnbaum et al., 2011; Florence et al., 2016; Rice et al., 2014). This difference with previous estimates is primarily because this study uses the value of a statistical life to value the loss of life from fatal overdose. The current study also expands on the previous literature by assessing the value of lost quality of life from opioid use disorder. This is a broader range of outcomes, and a more comprehensive estimate, than the most recent studies (Davenport et al., 2019). Based on the results presented here, substantial economic benefits could be realized by reducing the rate of fatal overdoses and preventing opioid use disorder.
Several effective strategies have been identified to improve opioid prescribing consistent with clinical guidelines, treat opioid use disorder and prevent fatal overdose. Naloxone distribution programs have been shown to reduce opioid mortality rates (Walley et al., 2013). Mandatory provider review of prescription drug monitoring programs before prescribing opioids and laws that govern the ownership and operation of pain clinics have been shown to reduce the amount of opioids prescribed and prescription overdose death rates (Dowell et al., 2016). Medication-assisted treatment for opioid use disorder has been shown to reduce the rate of opioid misuse among patients with opioid use disorder and the rate of fatal opioid overdose (Mattick et al., 2009, 2014; Schwartz et al., 2013). However, the population requiring treatment has been estimated to be much larger than the current treatment capacity (Jones et al., 2015). Expanded implementation of effective strategies to prevent and treat opioid use disorder, and prevent fatal overdose is needed. The results of this study can assist decision makers by allowing them to compare the cost of implementing these strategies to the expected benefits from reduced opioid use disorder and overdose cases.
This study is subject to some limitations. Many of the cost estimation methods used methods from a previous study, so the limitations of that study are also present in these results. A primary limitation of our methodology is that we only measure the cost of opioid use disorder in a single year. To estimate the overall economic costs of a condition like opioid use disorder, it would be necessary to observe cases of disorder from their inception through the course of a person’s life. That would allow an understanding of the lifetime impacts of developing these disorders, and the associated outcomes could then have costs estimated that would identify the full lifetime cost of the condition and the benefit of preventing the disorder from occurring. However, there is still not sufficient information to develop lifetime costs of opioid use disorder.
There are also limitations to the source data used to estimate the costs. Health care costs were estimated with a convenience sample of health insurers and public insurance beneficiaries and may not be representative of the U.S. population. These costs are also only estimated for diagnosed cases of opioid use disorder in persons age 12+, so we do not estimate costs to other persons, such as in the case of neonatal abstinence syndrome. Criminal justice costs were apportioned from government budget data and may not reflect the costs of all criminal justice activity related to opioids. We also use a budget apportionment method for attributing non-health insurance expenditures for substance use disorder treatment. In both cases, we used the share of opioid use disorder cases as a percentage of all substance abuse cases to apportion these costs. However, some types of drug use may generate a dipropionate share of criminal justice or substance abuse treatment costs, which our methods would not account for. Lost productivity estimates used data based on average earnings for the U.S. population, which may not be representative of the population of those with opioid use disorder or fatal overdose.
There are also several limitations of the data and methods used to estimate the HRQL and VSL. We did not have a VSL value specific to the willingness to pay to prevent an opioid overdose death and instead used a general-purpose set of values based on results from studies that examined the value of risk reduction over a diverse set of risks. If the societal average willingness to pay to prevent an opioid overdose fatality is different from these values, this could cause our valuation to be inaccurate. We also only value lost HRQL for individuals with opioid use disorder. There is likely a substantial reduction in quality of life for friends and family members who care for loved with use disorder, and lose loved ones to overdose (Wittenberg et al., 2016). Using a nationally representative sample of the non-institutional U.S. population from the NSDUH will not account for cases of opioid use disorder in incarcerated and homeless populations. Finally, mortality data for opioid overdose may also understate the true number of cases, as some overdose death certificates do not contain information on specific drugs(Ruhm, 2017). As shown in our sensitivity analysis, this would imply that our estimates are conservative. Despite these limitations, these estimates provide an up-to-date understanding of the overall economic impact of the crisis. These estimates can assist decision makers in understanding the magnitude of opioid use disorder and fatal overdose. Knowing the magnitude and distribution of the economic burden can inform public policy, clinical practice, research, and prevention and response activities.
Supplementary Material
References
- Addiction Center. 2020. The Connection Between Homelessness and Addiction. https://www.addictioncenter.com/addiction/homelessness/ (Accessed August 20, 2020)
- American Psychiatric Association, 1994. Diagnostic and statistical manual of mental disorders. 4th ed. American Psychiatric Association, Washington (DC). [Google Scholar]
- Barocas JA, White LF, Wang J, Walley AY, LaRochelle MR, Bernson D, Land T, Morgan JR, Samet JH, Linas BP, 2018. Estimated prevalence of opioid use disorder in Massachusetts, 2011–2015: A capture–recapture analysis. Am. J. Public Health, 108(12),1675–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum HG, White AG, Reynolds JL, Greenberg PE, Zhang M, Vallow S, Schein JR, Katz NP, 2006. Estimated costs of prescription opioid analgesic abuse in the United States in 2001: a societal perspective. Clin. J. Pain 22(8), 667–676. [DOI] [PubMed] [Google Scholar]
- Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL, 2011. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 12(4), 657–667. [DOI] [PubMed] [Google Scholar]
- Boslett AJ, Denham A, and Hill EL (2020) Using contributing causes of death improves prediction of opioid involvement in unclassified drug overdoses in US death records. Addiction, 115: 1308–1317. 10.1111/add.14943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronson J 2018. Justice expenditure and employment extracts, 2015—preliminary. Washington, DC: Bureau of Justice Statistics, US Department of Justice, NCJ, 248628. https://www.bjs.gov/index.cfm?ty=pbdetail&iid=6310. (Accessed January 20, 2019) [Google Scholar]
- Bronson J, Carson E, 2019. Prisoners in 2017. U.S. Department of Justice, Washington, D.C. https://www.bjs.gov/content/pub/pdf/p17.pdf (Accessed August 20, 2020) [Google Scholar]
- Carson EA, 2018. Prisoners in 2016. Bureau of Justice Statistics, NCJ251149. US Department of Justice; https://www.bjs.gov/index.cfm?ty=pbdetail&iid=6187. (Accessed January 20, 2019) [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2018. 2017 National Survey on Drug Use and Health Final Analytic File Codebook. Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Health Statistics, 2018. Multiple Cause of Death 1999–2017 on CDC WONDER online database released 2018. http://wonder.cdc.gov/mcd-icd10.html. (Accessed January 25, 2019) [Google Scholar]
- Centers for Disease Control Prevention, National Center for Injury Prevention and Control, 2015. Web- based injury statistics query and reporting system (WISQARS). [Google Scholar]
- Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, Fry-Smith A, Day E, Lintzeris N, Roberts T, Burls A, 2007. Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation. In NIHR Health Technology Assessment programme: Executive Summaries. NIHR Journals Library. [DOI] [PubMed] [Google Scholar]
- Coughlin T, Holahan J, Caswell K, 2017. Uncompensated care for the uninsured in 2013: a detailed examination. 2014. The Henry J. Kaiser Family Foundation: The Kaiser Commission on Medicaid and the Uninsured. [Google Scholar]
- Council of Economic Advisers (US), 2017. The underestimated cost of the opioid crisis. Executive Office of the President of the United States, Council of Economic Advisers. [Google Scholar]
- Davenport S, Weaver A, & Caverly M, 2019. Costs and Comorbidities of Opioid Use Disorder. Milliman White Paper. https://milliman-cdn.azureedge.net/-/media/milliman/importedfiles/uploadedfiles/insight/2019/costs-comorbidities-opioid-use-disorder.ashx (Accessed August 20, 2020) [Google Scholar]
- Dowell D, Zhang K, Noonan RK, Hockenberry JM, 2016. Mandatory provider review and pain clinic laws reduce the amounts of opioids prescribed and overdose death rates. Health Aff. 35(10), 1876–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell D, Noonan RK, Houry D, 2017. Underlying factors in drug overdose deaths. Jama, 318(23), 2295–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drug Enforcement Administration, 2018. National Forensic Laboratory Information System: 2012 Annual Report. Washington, DC. [Google Scholar]
- Florence C, Luo F, Xu L, Zhou C, 2016. The economic burden of prescription opioid overdose, abuse and dependence in the United States, 2013. Med. Care, 54(10), 901–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosse SD, Krueger KV, Pike J, 2019. Estimated annual and lifetime labor productivity in the United States, 2016: implications for economic evaluations. J. Med. Econ, 22(6), 501–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris AH, Gospodarevskaya E, Ritter AJ, 2005. A randomised trial of the cost effectiveness of buprenorphine as an alternative to methadone maintenance treatment for heroin dependence in a primary care setting. Pharmacoeconomics, 23(1), 77–91. [DOI] [PubMed] [Google Scholar]
- Harwood HJ, Bouchery E, 2004. The economic costs of drug abuse in the United States, 1992–2002. Executive Office of the President, Office of National Drug Control Policy. [Google Scholar]
- IBM, 2013. IBM MarketScan® Research Databases. https://www.ibm.com/us-en/marketplace/marketscan-research-databases/details. (Accessed July 15, 2013)
- Jones CM, Campopiano M, Baldwin G, McCance-Katz E, 2015. National and state treatment need and capacity for opioid agonist medication-assisted treatment. Am. J. Public Health, 105(8), e55–e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence BA, Miller TA., 2014. Medical and work loss cost estimation methods for the WISQARS cost of injury module. Final Report to the Centers for Disease Control and Prevention. Pacific Institute for Research and Evaluation. Calverton, MD. http://www.pire.org/documents/WisqarsCostMethods.pdf (Accessed August 22, 2020) [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M, 2009. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst. Rev, (3). [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M, 2014. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst. Rev, (3). [DOI] [PubMed] [Google Scholar]
- National Drug Intelligence Center, 2011. The economic impact of illicit drug use on American society. United States Department of Justice, Washington D.C. [Google Scholar]
- National Institute on Drug Abuse. 2020. Criminal Justice Drug Facts. National Institutes of Health; U.S. Department of Health and Human Services. https://www.drugabuse.gov/publications/drugfacts/criminal-justice (Accessed August 22, 2020) [Google Scholar]
- Office of the Assistant Secretary for Planning and Evaluation, 2016. Guidelines for regulatory impact analysis. U.S. Department of Health and Human Services, Washington, DC. [Google Scholar]
- Rice JB, Kirson NY, Shei A, Enloe CJ, Cummings AKG, Birnbaum HG, Holly P, Ben-Joseph R, 2014. The economic burden of diagnosed opioid abuse among commercially insured individuals. Postgrad. Med 126(4), 53–58. [DOI] [PubMed] [Google Scholar]
- Ruhm CJ, 2017. Geographic variation in opioid and heroin involved drug poisoning mortality rates. Am. J. Prev. Med 53(6), 745–753. [DOI] [PubMed] [Google Scholar]
- Scholl L SP, Kariisa M, Wilson N, Baldwin G, 2019. Drug and Opioid-Involved Overdose Deaths-United States, 2013–2017. MMWR Morb. Mortal. Wkly. Rep 67, 1419–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz RP, Gryczynski J, O’grady KE, Sharfstein JM, Warren G, Olsen Y, Mitchell SG, Jaffe JH, 2013. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995–2009. Am. J. Public Health, 103(5), 917–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2014. Projections of national expenditures for treatment of mental and substance use disorders, 2010–2020. HHS Publication No. SMA-14–4883. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18–5068, NSDUH Series H-53. [Google Scholar]
- US Department of Justice, 2016. Uniform crime report: Crime in the United States, 2015. [Google Scholar]
- Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, Ruiz S,Ozonoff A, 2013. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ, 346. [DOI] [PMC free article] [PubMed]
- Wittenberg E, Bray JW, Aden B, Gebremariam A, Nosyk B, Schackman BR, 2016. Measuring benefits of opioid misuse treatment for economic evaluation: health‐related quality of life of opioid‐dependent individuals and their spouses as assessed by a sample of the US population. Addiction, 111(4), 675–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woody GE, Poole SA, Subramaniam G, Dugosh K, Bogenschutz M, Abbott P, Patkar A, Publicker M, McCain K, Potter JS, Forman R, 2008. Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial. JAMA, 300(17), 2003–2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.