Abstract
We sought to undertake a systematic review to assess the current research and to provide a platform for future research on the psychological health impact of chronic environmental contamination (CEC). CEC is the experience of living in an area where hazardous substances are known or perceived to be present in air, water, or soil at elevated levels for a prolonged and unknown period of time. We employed a systematic review approach to assess the psychological health impact of CEC in literature from 1995 to 2019, and conducted a meta-analysis of available findings (k = 60, N = 25,858) on the impact of CEC on anxiety, general stress, depression, and PTSD. We also present a narrative synthesis of findings that suggest risk factors for the experience of psychological health impacts in the wake of CEC. Likely factors increasing risk for elevated psychological health impact from CEC experience are institutional delegitimization of community concerns and the real or perceived presence of health effects from CEC. The meta-analyses observed small-to-medium effects of experiencing CEC on anxiety, general stress, depression, and PTSD. However, there was also evident risk of bias in the data. Our review suggests that psychological health in the context of CEC is an important potential public health burden and a key area for future improved research.
Keywords: Chronic environmental contamination, Mental health, Stress
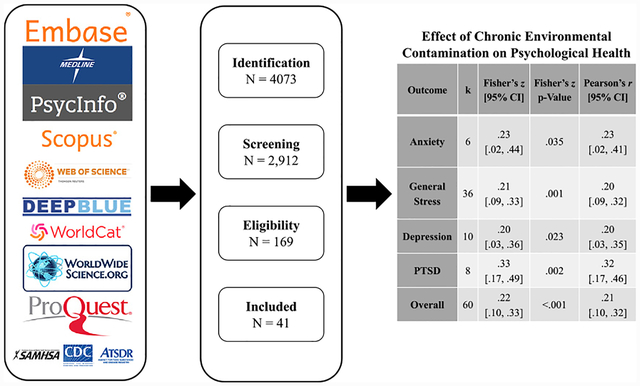
GRAPHICAL ABSTRACT
1. Introduction
Chronic environmental contamination (CEC) is the experience of living in an area where hazardous substances are known or perceived to persist over time in air, water, or soil at elevated levels. This contamination may be chemical or radiological, and the result of prior or current industrial processes or a technological accident (Couch and Coles, 2011). CEC may pose toxicological health risks if someone is exposed. The experience of long-term exposure to environmental contamination can also be psychologically stressful for some members of an affected community (Baum and Flemming, 1993; Havenaar and Van den Brink, 1997; Tucker, 1998). Chronic stress can have a variety of deleterious physical health effects such as immune suppression or dysregulation (Dhabhar, 2011), risk of obesity, Type II diabetes, atherosclerosis, and early cognitive decline (McEwen, 2008). Stress and its associated health effects may interact with toxicant exposure to negatively impact already vulnerable populations (Segal et al., 2015).
Addressing psychological health impacts in communities living with CEC is therefore important for improving their health (Hoover et al., 2015). We define psychological health impacts broadly in this review, so as to encompass the wide range of psychological health variables assessed across this literature. Psychological health impacts can be thought of as the various emotional, psychological, and behavioral effects that experiencing CEC may have on an individual or community that can strain their ability to cope (Gerhardstein et al., 2019). It is crucial to consider both individual psychological effects as well as psychosocial effects – community-level factors through which broader structural forces impact residents. These issues underscore the importance of the central question of this review: What is the impact of experiencing CEC on psychological health? As part of a project initiated by the Agency for Toxic Substances and Disease Registry (ATSDR), we undertook a systematic review assessing the psychological health impact of chronic contamination experience.
The existing literature that has assessed the psychological health impact of CEC is limited due to the many research barriers inherent to CEC events. The systematic review and meta-analysis presented here serve to synthesize the existing literature in order to assess the extent of the psychological health impact of CEC, to understand the limitations of the literature and the barriers to conducting research, and to suggest future research topics and methods in this area.
1.1. Previous research on CEC and psychological health
Early psychological studies used a range of comparative designs and methods to determine that CEC experience was stressful for extended temporal periods, although not necessarily at levels indicative of clinical impairment (Baum and Flemming, 1993; Havenaar and Van den Brink, 1997; Bowler et al., 1994). Theoretical models suggested similarities between symptoms of CEC-induced chronic stress and posttraumatic stress disorder (PTSD), particularly in regard to the chronic ambiguity, invisibility, and subsequent hypervigilance associated with exposure and potential health effects (Edelstein, 2018; Vyner, 1988). Researchers highlighted that the stage sequence in CEC is often of a cyclical nature, differing from the linear trajectory of natural disaster stages (Edelstein, 2018).
Past literature suggests that the material dimension of impact (e.g., real or perceived health effects, property loss or devaluation) is a significant contributor to the stress of the CEC experience (Edelstein, 2018). Further, Vyner (1988) proposed that the social dimension of responses to CEC was the most important factor for determining the risk of severe psychological health outcomes. Specifically, he identified three social risk factors that we designate processes of institutional delegitimization: (1) denial (or framing as a “non-issue” (Reich, 1991; Calloway et al., 2020)) of the severity and potential impact of CEC by corporations, government, or public health professionals; (2) problematic relationships with healthcare providers who are unfamiliar with local histories of CEC and may attribute patient concerns to somatic symptom or illness anxiety disorders (Calloway et al., 2020); and (3) indirect or direct victim-blaming processes such as attributing health effects to lifestyles choices rather than CEC (Checker, 2007).
Beyond variation of these situational factors, studies have consistently documented diverging psychological responses to CEC. Some community members exhibit a “maximalist” reaction of distress, and others a “minimalist” reaction of little impact (Fowlkes and Miller, 1987). It has been noted that women often display more pronounced stress reactions to CEC and technological disasters than men (Gibbs, 1989).
Evidence that CEC exposure is stratified by race/ethnicity and socioeconomic status is provided in U.S. national-level longitudinal studies of hazardous waste facility sitings (Mohai and Saha, 2015), national- and state-level studies of Superfund site locations (Kramar et al., 2018), and case studies of metropolitan areas (Pulido, 2000). An exposure-disease paradigm suggests that disadvantaged groups are at greater risk for suffering physical health consequences when exposed to contaminants because they are chronically subjected to greater stressors (Gee and Payne-Sturges, 2004; Morello-Frosch and Shenassa, 2006). Exposures to stress and environmental contaminants can interact, leading to worse health risks than either exposure on its own (McEwen and Tucker, 2011). Some scholars have called this interaction a “double jeopardy” for disadvantaged communities (Morello-Frosch and Shenassa, 2006).
Social and environmental stressors are associated with higher allostatic load, a form of physiological wear measured as a composite of physical biomarkers (McEwen and Tucker, 2011). Through allostatic overload, chronic stress can lead to several health risks, including hypertension, coronary heart disease, and autoimmune disorders, which may also make individuals more susceptible to the effects of contaminants (Dhabhar, 2011). Chronic stress may interact with toxicant exposure to produce worse health outcomes, in part by amplifying the adverse effects of a toxicant (e.g., by compromising the immune system, especially if contaminants independently impair immune functioning (Gee and Payne-Sturges, 2004)).
To summarize what is known from the existing literature, the experience of CEC can have negative impacts on psychological health, with qualities that differentiate it from the experience of natural disasters, and women and members of disadvantaged social groups are disproportionately vulnerable to negative psychological and physical health impacts. However, a central question has not been previously addressed using a systematic review method: What is the severity of the psychological health impacts caused by CEC, and what risk factors may contribute to psychological health impacts?
2. Methods
We conducted a systematic review and meta-analysis of available quantitative findings from 1995 to 2019 as a synthesis of what is already known and impetus to future research. Given natural barriers to research in this area, it was anticipated that the relevant quantitative empirical evidence would be somewhat limited with an acknowledged risk of bias.
2.1. Study selection and data extraction
The available quantitative literature was examined using a systematic review protocol (PRISMA-P checklist) that was developed iteratively a priori (Moher et al., 2009). Due to project time constraints associated with federal government scientific clearance processes, the protocol for this review was not registered, but is available in Supplemental Materials (Appendix A). The present systematic review and meta-analysis adhered to this protocol, but only represent one part of the broader project carried out by ATSDR. Specifically, the present review only reports methods and results pertinent to Research Question 2 (Item #7) in the a priori PRISMA-P checklist. Literature searching occurred from June to August of 2019. We searched Embase, Medline, PsycINFO, Scopus, TOXNET, and Web of Science for peer-reviewed literature. We searched Deep Blue, WorldCat, WorldWide Science, and PROQUEST, as well as the ATSDR, CDC, and SAMHSA websites for grey literature (see Appendix B in Supplemental Materials for all search terms).
Studies needed to include quantitative analyses on the psychological stress impacts of experiencing CEC (including living near contaminated sites), provide findings that examined an identified community (or set of communities), and be conducted within a developed nation (Human Development Index 2018 ≥0.90). All quantitative study designs were allowed. Further, studies had to include an operationalization of the exposure/contamination experience, a measure of psychological health including anxiety, stress, depression, or post-traumatic stress, and had to be conducted from 1995 to 2019 (in order to update a major synthesis of this literature conducted in 1995 by an ATSDR-convened expert panel (Tucker, 1998)).
The research team decided to narrowly focus the operationalization of CEC, which resulted in excluding occupational exposures and major catastrophic events. While occupational exposures can be chronic in nature, these studies do not typically address the psychosocial impact of CEC as a community-level hazard. Occupational exposures also tend overall to induce less psychological stress compared to involuntary community exposures (Lebovits et al., 1986). Well-researched, major catastrophic events (e.g., September 11 terrorist attacks, Fukushima disaster, Deepwater Horizon oil spill) present highly unique aspects that might influence psychosocial outcomes to a degree that would be atypical for most communities’ CEC experience. We excluded such events because (1) they were characterized by heavily-mediatized, widespread social narratives, and (2) they had clearly catastrophic and traumatic impacts on a large number of lives or livelihoods. Consequently, they could be expected to have large psychological effects, which we would not expect to generalize to CEC experiences which lack these aspects. Furthermore, because there are large bodies of extant literature on each of these events, we believed that searching for studies of other, lesser-known experiences would make a more important scientific contribution.
Articles were screened by five researchers at the title, abstract, and full-text level using DistillerSR software (Evidence Partners, Ottawa, Ontario). One researcher screened each article at the title level and abstract level. Hand searching was done on reference lists of all studies that made it past abstract screening. We also reached out to corresponding authors of included papers published in the past 5 years for clarification on effect size statistics when necessary. This resulted in the inclusion of 2 effect sizes from 2 separate papers that had appeared in the systematic review, but that did not report enough information to calculate the effect sizes. One author that we reached out to alerted us of a paper that we did not find in our initial literature search, but that fit our inclusion criteria. We included this paper in the systematic review and included one effect size from this paper in the meta-analysis. Relevant hand-searched empirical studies and grey literature were included into the full-text screen, though no grey literature ended up being included in the present review. For the full-text screen, two researchers screened each article. Screening disagreements were discussed among the group until consensus was reached. Relevant qualitative, theoretical, review, and non-empirical grey literature papers were flagged during searching and retained separately for inclusion in a separate narrative review project (Sullivan et al., under review). Relevant data were extracted from all articles that made it past full-text screening using data extraction forms created in DistillerSR. The full evidence table with all extracted data is available upon request, but a simplified version can be found in Table 1 (Behbod et al., 2014; Bevc et al., 2007; Cline et al., 2014; Couch and Mercuri, 2007; Cutchin et al., 2008; Downey and Van Willigen, 2005; Elliott et al., 1997; Elliott et al., 2018; Fitzgerald et al., 2008; Fortenberry et al., 2018; Ginsberg et al., 2012; Grasmück and Scholz, 2005; Greve et al., 2005; Greve et al., 2007; Ha et al., 2018; Hastrup et al., 2007; Korol et al., 1999; Kruger et al., 2017a; Kruger et al., 2017b; Kruger et al., 2017c; Levy et al., 2004; Matthies et al., 2000; McCarron et al., 2000; McIntyre et al., 2018; Peek et al., 2009; Rehner et al., 2000; Reif et al., 2003; Sansom et al., 2017; Santiago-Rivera et al., 2007; Schade et al., 2015; Schade et al., 2016; Song et al., 2018; Ushijima et al., 2004; Vandermoere, 2006; Vandermoere, 2008; Verschuur et al., 2007; Verschuur et al., 2008; Weinert et al., 2011; Whiteman et al., 1995; Zierold et al., 2004; McComas and Trumbo, 2001).
Table 1.
Empirical quantitative studies on psychological stress as a function of chronic environmental contamination, selected through the systematic review.
| Publication | Contamination event/source | Region | Study design | Independent variable (s) | Dependent variable (s) | Risk of bias | n | r |
|---|---|---|---|---|---|---|---|---|
| Behbod et al. (2014) | Tert-butyl mercaptan exposure, tank leak | Prichard, AL, US | Cross-sectional | Distance | General stress | Low | 204 | 0.24 |
| Bevc et al. (2007)b | Landfill/waste site | Ft. Lauderdale, FL, US | Cross-sectional | Subjective | Depression, | Low | 223 | 0.230 |
| PTSD | .26 | |||||||
| Cline et al. (2014) | Asbestos exposure, industrial activity | Libby, MT, US | Cross-sectional | Proxy measure | General stress | High | 208 | 0.39 |
| Couch and Mercuri (2007)b | Benzene exposure from industrial activity | Houston, TX, US | Case-control | Objective | General stress | Low | 341 | 0.580 |
| 550 | .430 | |||||||
| 386 | .340 | |||||||
| 405 | .31 | |||||||
| Cutchin et al. (2008) | Industrial activity and refinery explosion | Texas City, TX, US | Before-and-after | Distance | General stress | Low | 315 | 0.15 |
| Downey and Van Willigen (2005)b | Proximity to chronic industrial activity | Chicago & neighboring counties in IL, US | Cross-sectional | Objective | General stress | Low | 1210 | 0.230 |
| .190 | ||||||||
| Depression | .11 | |||||||
| Elliott et al. (1997)a | Landfill | Milton, ON, CA | Before-and-after | High | ||||
| Elliott et al. 2018 | Proximity to unconventional oil & gas wells | Belmont County, OH, US | Cross-sectional | Objective | General stress | Low | 66 | 0.16 |
| Fitzgerald et al. (2008) | Polychlorinated biphenyl exposure, water, industrial activity | Hudson River Area, NY, US | Cross-sectional | Objective | Depression | Low | 243 | 0.16 |
| Fortenberry et al. (2018)a | Lead exposure, water | Flint, MI, US | Cross-sectional | High | ||||
| Ginsberg et al. (2012) | Chlorine exposure, railway accident | Graniteville, SC, US | Cross-sectional | Health | PTSD | Low | 225 | 0.45 |
| Grasmück and Scholz (2005) | Heavy metal exposure, soil, industrial activity | Dornach, Switzerland | Case-control | Subjective | General stress | High | 57 | 0.63 |
| Greve et al. (2005)b | Toxic waste cloud, railway accident | Eunice, LA, US | Case-control | Objective | General stress | Low | 78 | 0.370 |
| Depression | .370 | |||||||
| PTSD | .37 | |||||||
| Greve et al. (2007)b | Toxic waste cloud, railway accident | Eunice, LA, US | Case-control | Objective | Anxiety | Low | 51 | .17c |
| General Stress | .30c | |||||||
| PTSD | .34c | |||||||
| Anxiety | 51 | .36d | ||||||
| Depression | .18d | |||||||
| Ha et al. (2018)b | Heavy traffic roads contaminated by radiation | Seoul, South Korea | Cross-sectional | Subjective | Anxiety | Low | 8826 | 0.220 |
| General stress | .19 | |||||||
| Hastrup et al. (2007)b | Hazardous dumping, historic industrial activity | Anonymous | Case-control | Objective | General stress | Low | 290 | 0.280 |
| Appalachian | .340 | |||||||
| Community | Depression | .47 | ||||||
| Korol et al. (1999) | Nuclear waste, government activities | Fernald, OH, US | Cross-sectional | Distance | PTSD | High | 91 | 0.54 |
| Kruger et al. (2017a) | Lead exposure, water | Flint, MI, US | Cross-sectional | Subjective | PTSD | High | 786 | 0.25 |
| Kruger et al. (2017b)b | Lead exposure, water | Flint, MI, US | Cross-sectional | Subjective | General stress | High | 834 | 0.250 |
| .16 | ||||||||
| Kruger et al. (2017c) | Lead exposure, water | Flint, MI, US | Cross-sectional | Subjective | General stress | High | 277 | 0.22 |
| Levy et al. (2004)a | Environmental exposures, public housing | Boston, MA, US | Cross-sectional | High | ||||
| Matthies et al. (2000)b | Benzo(a)pyrene exposure, soil, industrial activity | Dortmund-Dorstfeld, Germany | Case-control | Subjective | General stress | Low | 152 | 0.460 |
| Objective | 415 | .17 | ||||||
| McCarron et al. (2000)b | Landfill, chromium waste | Glasgow, Scotland | Case-control | Health | General stress | Low | 398 | 0.080 |
| Objective | 798 | .001 | ||||||
| McComas and Trumbo (2001)a | Landfills, chronic industrial activity | Various communities, NY State, US | Cross-sectional | High | ||||
| McIntyre et al. (2018) | Chronic industrial activity | Various communities, Australia | Cross-sectional | Distance | General stress | Low | 2009 | 0.03 |
| Peek et al. (2009)b | Chronic industrial activity | Texas City, TX, US | Cross-sectional | Subjective | General stress | Low | 2604 | 0.060 |
| Depression | .13 | |||||||
| Rehner et al. (2000) | Methyl parathion exposure, pesticide use | Jackson County, MS, US | Follow-up cohort | Time | Depression | Low | 115 | 0.25 |
| Reif et al. (2003)a | Trichloroethylene exposure, water | Denver, CO, US | Cross-sectional | Low | ||||
| Sansom et al. (2017) | Waste sites and industrial activity | Houston, TX, US | Cross-sectional | Time | General stress | High | 109 | 0.08 |
| Santiago-Rivera et al. (2007) | Polychlorinated biphenyl exposure, water | Akwasasne Mohawk reservation, NY, US | Cross-sectional | Objective | General stress | Low | 353 | 0.18 |
| Schade et al. (2015)a | 4-methylcyclohexane methanol exposure, solvent spill | Charleston, WV, US | Retrospective follow-up | High | ||||
| Schade et al. (2016) | 4-methylcyclohexane methanol exposure, solvent spill | Charleston, WV, US | Retrospective follow-up | Health | General stress | High | 489 | 0.47 |
| Song et al. (2018)a | Hydrogen fluoride exposure, spill/transport accident | Gumi, South Korea | Cross-sectional | Low | ||||
| Ushijima et al. (2004) | Methylmercury exposure, water, industrial activity | Minamata City, Japan | Follow-up cohort | Health | General stress | High | 133 | 0.47 |
| Vandermoere (2006) | Heavy metal exposure, soil, industrial activity | Kouterwijk, Belgium | Cross-sectional | Subjective | General stress | High | 98 | 0.38 |
| Vandermoere (2008)b | Heavy metal exposure, soil, industrial activity | Kouterwijk, Belgium | Case-control | Objective | General stress | High | 300 | 0.420 |
| .190 | ||||||||
| Anxiety | .11 | |||||||
| Verschuur et al. (2007)b | Rumored uranium exposure, airplane accident | Amsterdam, Netherlands | Before-and-after | Health | General stress | High | 1074 | 0.260 |
| .390 | ||||||||
| Anxiety | .340 | |||||||
| PTSD | .36 | |||||||
| Verschuur et al. (2008)b | Rumored uranium exposure, airplane accident | Amsterdam, Netherlands | Follow-up cohort | Health | Anxiety | High | 168 | 0.120 |
| General Stress | .040 | |||||||
| PTSD | .09 | |||||||
| Weinert et al. (2011)b | Asbestos exposure, industrial activity | Libby, MT, US | Cross-sectional | Distance | General stress | High | 386 | 0.090 |
| Depression | .03 | |||||||
| Whiteman et al. (1995)a | Lead/chemical exposure, mining and industry | Kinston, Australia | Follow-up cohort | High | ||||
| Zierold et al. (2004) | Arsenic exposure, water | Sinnipee/St. Peter, WI, US | Cross-sectional | Objective | Depression | High | 1185 | 0.38 |
| k = 60 | N = 25,858 | r = 0.26 |
Studies not included in the meta-analysis.
Includes multiple effects from the same participants.
Effects from child participants.
Effects for parents of child participants.
2.2. Risk of Bias
Risk of Bias assessments for the included literature were made using the Risk of Bias Assessment Tool for Nonrandomized Studies (RoBANS) (Kim et al., 2013). However, the findings were not weighted based on the risk of bias assessment. Many well-established and widely-used tools for assessing risk of bias in systematic reviews are specifically designed to assess randomized controlled trials (e.g., the Cochrane Collaboration tool (Higgins and Thomas, 2019)). However, the area of research reviewed here does not permit this methodology. Alternatively, the RoBANS was designed to assess risk of bias in a variety of non-randomized study designs. The RoBANS assesses risk of bias in 6 domains: selection of participants, consideration of confounding variables, measurement of exposure, blinding of outcome assessments, handling of incomplete outcome data, and selective outcome reporting. Due to variation in reporting standards, it was difficult to judge most studies in this literature for the last three domains; accordingly, low versus high risk scores were assigned to studies based on their majority score for the first 3 domains. Overall RoBANS assessment scores for each study can be found in Table 1. The findings were not weighted based on the risk of bias assessment for two reasons. First, there are limitations to the RoBANS as a tool for grading evidence in this specific research area. Second, this is an emerging and challenging field where most studies are expected to have a relatively high risk of bias due to inherent challenges.
2.3. Methods of analysis
We conducted meta-analyses to assess the impact of CEC on the experience of negative psychological health outcomes. Studies from the systematic review were included in the meta-analysis if they reported sufficient statistical information in order to extract effect sizes, had an independent variable that assessed objective or subjective experience of contamination, and had a dependent variable that assessed psychological stress. We also reached out to corresponding authors from papers published in since 2015 for clarification on statistics where necessary to compute effect sizes. We conducted a meta-analysis of random effects using a multilevel linear model of mixed effects. All effect sizes were converted to Pearson’s r correlation coefficients. We calculated summary estimates for each dependent variable separately, as well as for all effect sizes together. Further, we present a narrative synthesis of important findings from the systematic review on potential risk factors that could not be included in the meta-analysis.
Independent variables utilized for the meta-analysis fell into six categories assessing (extent of) CEC experience: Objective exposure (k = 27), time (k = 2), distance (k = 6), health (k = 11), subjective exposure (k = 13), and proxy measures (k = 1). Objective exposure measures included indicators such as the amount of a given contaminant in a water source. Objective exposure independent variables also included studies that compared an “exposed” case group to a “non-exposed” control group. Time included measures of how long an individual was exposed to a given contaminant. Distance measures assessed how far an individual was from the contaminated site/event. Health included both objective measures of health effects experienced by individuals that were associated with contamination (e.g., prevalence of Minamata disease, lung function), and subjective measures of perceived connections between health and contamination. Subjective exposure measures included subjective concerns and uncertainties about the given contamination event, or subjective assessments of how much of the contaminant the participant was exposed to. The proxy measure for contamination used in one study was the perceived deleterious impacts of CEC on social relationships.
Dependent variables fell into 4 categories: anxiety (k = 6), general stress (k = 36), depression symptoms (k = 10), and PTSD symptoms (k = 8). The Anxiety measures included such scales as the State-Trait Anxiety Scale (STAS) and various health anxiety scales. The General Stress measures varied widely, including the Perceived Stress Scale (PSS), various versions of the General Health Questionnaire (GHQ), sleep quality and duration measures, and other more event-specific measures for concern about the impacts of the contamination. Depression measures included the Beck Depression Inventory (BDI), the Center for Epidemiological Studies Depression Scale (CES—D), and other non-specified measures. PTSD measures included the Impact of Events scale (IES), the Short Screening Survey for PTSD, and other non-specified or interview measures.
3. Results
Fig. 1 depicts our selection process, which ultimately yielded 41 studies for inclusion in the systematic review. See Table 1 for an evidence table of all studies included in the systematic review. Of these, 33 studies met the above criteria to be included in the meta-analysis, including 60 effect sizes. Most studies examined communities in the United States, although 32% came from either Australia, Canada, Europe, or South Korea. The majority of studies (59%) examined communities experiencing CEC in the form of (potential) exposures due to historic or ongoing industrial activity (e.g., Superfund site communities), although a number also examined exposures that occurred in the wake of technological accidents (24%) or due to proximity to a landfill/waste site (12%). Only 2 of the studies (5%) examined exposures due to radiation or nuclear activity.
Fig. 1.

Screening and selection process for the systematic review.
The majority of studies (61%) were cross-sectional in design. Evaluating the studies using the RoBANS tool, this literature clearly exhibits a risk of bias, indexed (for instance) by the fact that 46% of the studies either relied on self-reported indices of exposure or had no index of individual exposure levels, and only about one-quarter of studies used either a case-control design (17%) or a before-and-after design (7%). One small but notable advance over the earlier literature is that at least one study established an effect of CEC on psychological stress while controlling for potential secondary gains and strategic over-reporting in the context of litigation (Greve et al., 2005). Overall, the characteristics of the studies reflect methodological challenges often inherent to the study of psychological outcomes of CEC. While due caution should be used when extrapolating from these findings, this body of literature still offers valuable lessons to inform future research and practice.
Less than half of studies reported physical health outcomes. Among these, many are limited by self-report. Despite these limitations, there is some suggestive evidence supporting allostatic load theory in the context of CEC. A study of the CEC-impacted, racial minority Wingate community in Fort Lauderdale observed bidirectional links between physical and psychological health (Bevc et al., 2007); a study of the Texas City community yielded an association between contamination concerns and physical health specifically in Black participants (Cutchin et al., 2008); and a survey of 19 Wisconsin towns found that higher levels of arsenic in private well water were associated both with higher reported levels of depression and adverse cardiac effects (Zierold et al., 2004). At least one of the present studies directly established CEC effects on physiological stress indicators, such as inflammation and viral reactivation (Peek et al., 2009).
3.1. Possible risk factors
Earlier literature suggests there are several factors that moderate the likelihood of psychological stress among community members. Our review offers further support for two primary risk factors identified in earlier studies. Along the material dimension, the presence (versus absence) of health effects and concerns in the individual, family, or community appears to be a risk factor for negative psychological health outcomes. 29% of studies reported a significant association between health effects or concerns and psychological health. Of these, 6 studies reported sufficient statistical information, allowing us to calculate 11 effect sizes for the effect of contamination-related health concerns on all psychological health outcomes. As a supplementary analysis to the main meta-analyses reported below, we conducted a meta-analysis of random effects using a multilevel linear model of mixed effects to assess the impact of health concerns on psychological health (see Table 2 and Fig. 2 for summaries of the results). Pearson’s r effect sizes ranged from 0.04 to 0.47 with a raw mean of 0.28 (SD = 0.17, median = 0.34). The meta-analysis revealed a small-to-medium effect of health concerns on all psychological health outcomes: z = 0.33, se = 0.14, 95% CI [0.02, 0.65], p = .040. A Fisher’s z of 0.33 is roughly equivalent to a Pearson’s r of 0.32 (95% CI [0.02, 0.57]).
Table 2.
Summary of meta-analysis of the effect of contamination-related health concerns on all psychological health dependent variables.
| Independent variable | k | Fisher’s z [95% CI] | Fisher’s z p-Value | Pearson’s r [95% CI] | Cochrane’s Q | Cochrane’s Q p-Value | I2 |
|---|---|---|---|---|---|---|---|
| Health | 11 | 0.33 [0.02, 0.65] |
0.040 | 0.32 [0.02, 0.57] |
93.98 | <0.0001 | 95.30% |
Note. This table presents a summary of the meta-analysis for the effect of contamination-related health concerns on all psychological health dependent variables. All Fisher’s z estimates were attained from multilevel linear models of mixed effects. Each Fisher’s z was converted to Pearson’s r for ease of interpretation.
Fig. 2.
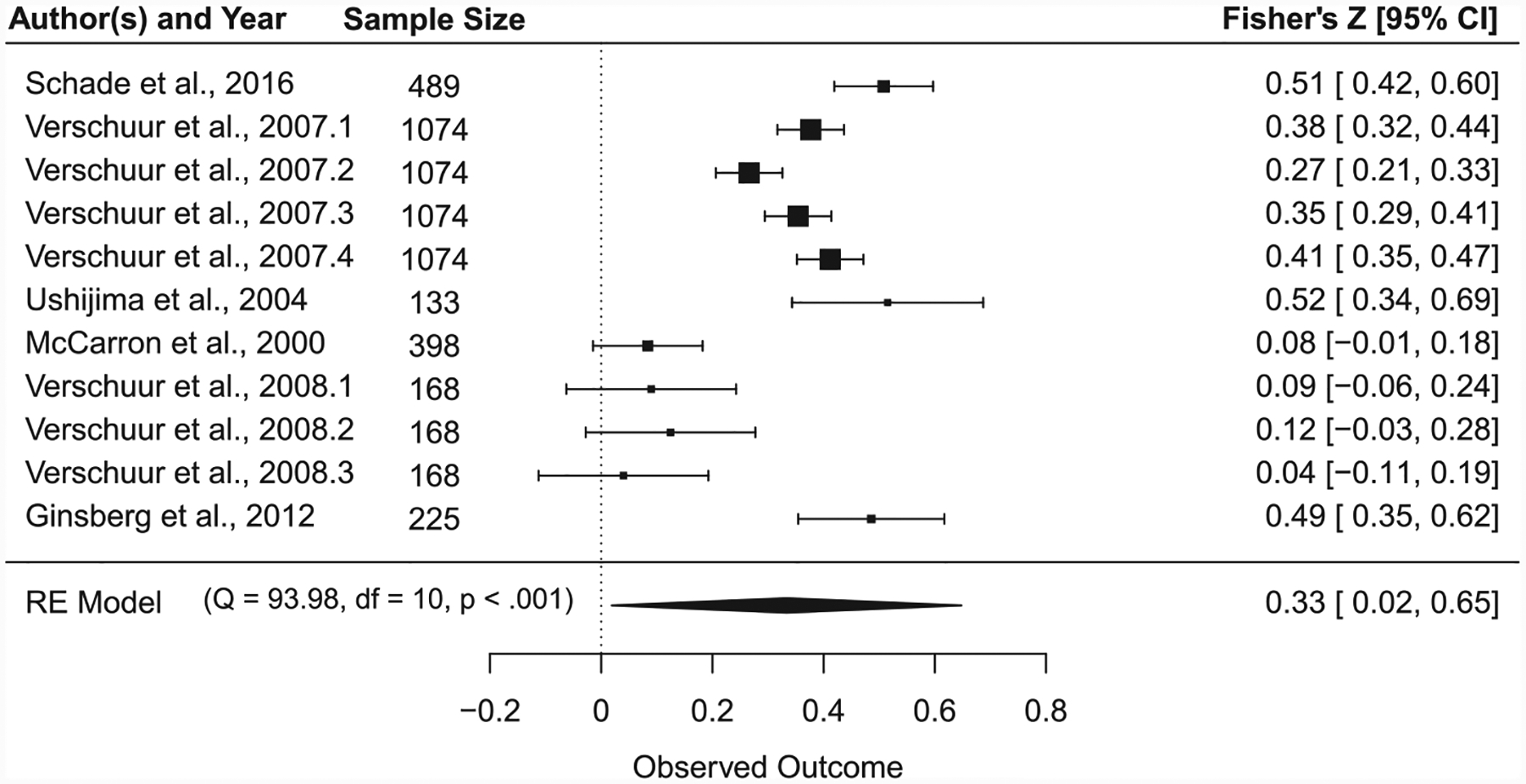
Effect size forest plot for meta-analysis of the effect of contamination-related health concerns on all psychological health dependent variables. Note. Each individual Fisher’s z effect size is presented as a black square with 95% CI error bars. Size of the square for each individual effect size represents relative weight based on sample size. The large black rhombus represents the aggregated Fisher’s z effect size. The width of the rhombus represents the 95% CI around the effect size.
Along the social dimension, an important moderator is the experience of various processes of institutional delegitimization: feeling that responsible or socially protective institutions have denied or misattributed one’s concerns about CEC-related health effects. Perceived poor communication from officials (Schade et al., 2016) and credibility of public health, media, and industry (McComas and Trumbo, 2001) significantly impacted distress. Notably, 50% of sampled residents in Flint, MI reported that feeling overlooked by responsible institutions was a major stressor (Fortenberry et al., 2018).
In the accumulated literature, women (compared to men) displayed statistically significantly worse psychological health impacts in 24% of the total studies. Although these studies do not speak to the mechanism(s) behind this effect, women may be at greater risk for stress along both the material dimension – women often have the caregiver role for health issues within the family and may be more alert and aware of new problems – and the social dimension – they may be especially likely to experience delegitimization through dismissal of their concerns as “irrational” (Brown and Ferguson, 1995).
3.2. Effects of chronic contamination on psychological stress
See Table 3 for a summary of results and Fig. 3 for a forest plot of these meta-analyses. Pearson’s r effect sizes ranged considerably from <0.002 to 0.63. The raw mean of effect sizes was 0.26 (SD = 0.15, median = 0.25). We converted the Pearson’s r correlations into Fisher’s z to conduct the meta-analysis (M = 0.28, SD = 0.17, median = 0.26). The final overall N in the 33 studies was 25,858. However, it is important to note that over 34% (n = 8826) came from a single study on community radiation impacts in South Korea (Ha et al., 2018). Removing this study from the meta-analysis did not substantively change the outcome (Δ Fisher’s z < 0.01).
Table 3.
Summary of meta-analyses split by dependent variable.
| Outcome | k | Fisher’s z [95% CI] | Fisher’s z p-Value | Pearson’s r [95% CI] | Cochrane’s Q | Cochrane’s Q p-Value | I2 |
|---|---|---|---|---|---|---|---|
| Anxiety | 6 | 0.23 [0.02, 0.44] |
0.035 | 0.23 [0.02, 0.41] |
24.69 | <0.001 | 83.46% |
| General Stress | 36 | 0.21 [0.09, 0.33] |
0.001 | 0.20 [0.09, 0.32] |
473.45 | <0.0001 | 94.40% |
| Depression | 10 | 0.20 [0.03, 0.36] |
0.023 | 0.20 [0.03, 0.35] |
110.32 | <0.0001 | 91.67% |
| PTSD | 8 | 0.33 [0.17, 0.49] |
0.002 | 0.32 [0.17, 0.46] |
29.52 | <0.001 | 82.12% |
| Overall | 60 | 0.22 [0.10, 0.33] |
<0.001 | 0.21 [0.10, 0.32] |
679.42 | <0.0001 | 94.21% |
Note. This table presents summaries of the meta-analyses for Anxiety, General Stress, Depression, PTSD, and all outcomes combined. All Fisher’s z estimates were attained from multilevel linear models of mixed effects. Each Fisher’s z was converted to Pearson’s r for ease of interpretation.
Fig. 3.
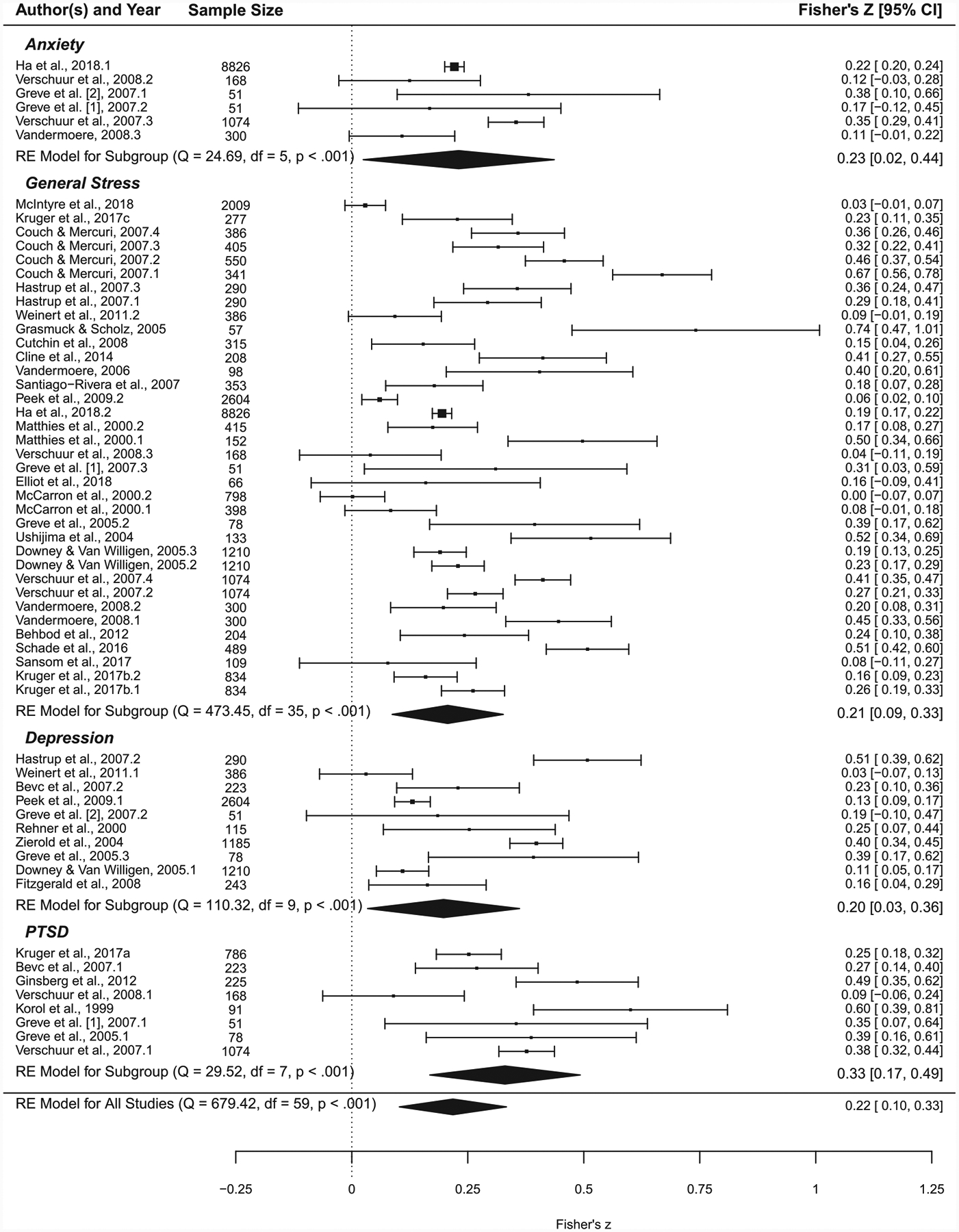
Effect size forest plot for meta-analyses, separated by psychological health outcome. Note. Each individual Fisher’s z effect size is presented as a black square with 95% CI error bars. Size of the square for each individual effect size represents relative weight based on sample size. Large black rhombuses represent the aggregated Fisher’s z effect sizes for Anxiety, General Stress, Depression, PTSD, and all outcomes combined. The width of each rhombus represents the 95% CI around the effect size.
We conducted a meta-analysis of random effects using a multilevel linear model of mixed effects in order to account for nonindependence of effect sizes from the same studies. We found a small-to-medium effect of contamination on all psychological outcomes, including anxiety, general stress, depression, and PTSD: z = 0.22, se = 0.06, 95% CI [0.10, 0.33], p < .001. A Fisher’s z of 0.22 is roughly equivalent to a Pearson’s r of 0.21 (95% CI [0.10, 0.32]).
We also conducted the meta-analyses separately for each of the different dependent variables. We found a small-to-medium effect of chronic contamination on anxiety (z = 0.23, se = 0.08, 95% CI [0.02, 0.44], p = .035), a small-to-medium effect of chronic contamination on general stress (z = 0.21, se = 0.06, 95% CI [0.09, 0.33], p = .001), a small-to-medium effect of chronic contamination on depression symptoms (z = 0.20, se = 0.07, 95% CI [0.03, 0.36], p = .023), and a medium effect of chronic contamination on PTSD symptoms (z = 0.33, se = 0.07, 95% CI [0.17, 0.49], p = .002). We conducted Bayesian Information Criterion model comparisons of random effects models that either did or did not account for nonindependence to find the best fitting model. In all cases, the models presented above were the best fit for the data (ΔBIC >7).
3.3. Analysis of heterogeneity
Each of the meta-analyses showed considerable heterogeneity of effect sizes. For the effect size of chronic contamination on all psychological outcomes, there was substantial heterogeneity: Q = 679.42, p < .001, I2 = 94.21%. More of this heterogeneity was due to within-study variation (I2 = 62.89%) than between-study variation (I2 = 31.33%). The higher within-study variation likely reflects the inclusion of multiple different independent and dependent variables. In order to assess between-study variation more meaningfully, we ran separate tests of heterogeneity on subsets for each of the three dependent variables. There was also substantial heterogeneity for the pooled effect size of chronic contamination on only anxiety (Q = 24.69, p < .001, I2 = 83.46%), on only general stress (Q = 473.45, p < .001, I2 = 94.40%), on only depression (Q = 110.32, p < .001, I2 = 91.67%), and on only PTSD (Q = 29.52, p < .001, I2 = 82.12%). The substantial heterogeneity of each of these analyses is not surprising, given the broad range of methods used to measure the dependent variables and the heterogeneity inherent to each of the CEC events represented by this literature. It is important to interpret the results of these meta-analyses with caution, maintaining awareness of the unique nature of each of the CEC events represented in these analyses, as well as the lack of consistency in how exposure to CEC and psychosocial health consequences are measured in this literature. Funnel plot summaries of the heterogeneity of the pooled effect sizes are available in the Supplemental Materials (Fig. S1).
4. Discussion
Our review suggests that CEC has a robust impact on anxiety, general stress, depression symptoms, and PTSD symptoms. Despite limitations, it seems unlikely, based on the meta-analysis, that there is a null or negligible average effect of CEC on psychological health. Further, the assembled studies indicate that the presence of concerns about possible health impacts or actual health impacts (attributed to contamination) on the individual or their family members is a robust risk factor for the psychological health impacts of CEC. This finding is meaningful considering that not all of the studies assessed these variables. As prior studies have suggested (Lebovits et al., 1986), our findings reinforce the notion that, within a community experiencing CEC, those with health problems they attribute to contamination are the most likely to experience negative psychological outcomes. Our review provides evidence that social processes of institutional delegitimization of concerns may act as secondary impacts of CEC, and may in some instances have a greater influence on psychological health than the material dimension of health concerns. In sum, our review supports the conclusion that those individuals who attribute physical health effects to exposure, and who feel that their concerns are being de-legitimized by culpable or responsible institutions, are most at risk for psychological health impacts as a consequence of CEC.
As noted, this review represents a major update to a synthesis of the literature based on an ATSDR-convened expert panel in 1995 (Tucker, 1998). Results from the present review support a number of findings from this report, though the former is somewhat more limited in scope due to the exclusive inclusion of quantitative literature. Specifically, the original expert panel report and the present review converge in the findings that (1) experiencing CEC can have negative effects on psychological health, (2) the perceived presence of physical health impacts from CEC can contribute to worse psychological health impacts, and (3) institutional delegitimization of community concerns can further exacerbate psychological health impacts of CEC. One new finding from the present review is that women may be particularly susceptible to the psychological health impacts of CEC. The present review represents an important advancement beyond the original expert panel report as the first systematic review and meta-analysis of the psychological health impacts of CEC.
One of the major advances in the literature on psychological health impacts of CEC in recent decades has been the documentation of environmental injustice. The literature accumulated for the present review does not provide substantial additional documentation of such effects, simply because the studies were generally not designed to test for them: most study samples were racially homogenous and hence inadequate for tests of moderation. However, qualitative studies that were separately gathered as part of the systematic review documented perceived experiences of institutional delegitimization that are attributed to indirect or even direct racism (Sullivan et al., under review). There are well-documented health disparities based on both race/ethnicity and lower socioeconomic status, and recent evidence that the effect of socioeconomic status on mental health is environmental in origin (Nuru-Jeter et al., 2018). These findings, combined with the systematic review results presented here, suggest that the risk of psychological health impacts is elevated for disadvantaged group members (racial/ethnic minorities and lower socioeconomic status) due to: (1) increased likelihood of experiencing CEC; (2) increased likelihood of adverse health effects that may be attributed to CEC; and (3) increased likelihood of experiencing institutional delegitimization.
4.1. State of the literature
The findings of this systematic review and exploratory meta-analysis must be interpreted with caution given the methodological limitations present in the existing literature in this area of research. Five factors influencing heterogeneity and/or risk of bias should be considered. First, the independent variable of CEC experience and the dependent variable of psychological health were assessed in highly diverse ways across the studies, often using measures that have not been well validated. This reflects the variability inherent in the CEC events represented in the literature reviewed here. Second, in many studies, self-report was used for either the independent variable, the dependent variable, or both. This may present limitations particularly in situations where an impacted community perceives that they may gain from over-reporting exposures or health consequences. Third, sampling limitations occurred in many studies, with almost all studies using convenience samples. Participants were often recruited via word-of-mouth, in clinics, or at community meetings among individuals more likely to already be concerned about CEC. These selection biases could artificially inflate observed effect sizes. Fourth, the relative lack of case-control, longitudinal, or pre-post designs limits the ability to make causal inferences. This suggests that many of these studies did not have a meaningful comparison group or baseline estimate of the psychosocial health of an impacted community prior to contamination. This is a common methodological challenge in research on different types of environmental disasters (Norris, 2006). Fifth, many studies used only bivariate analyses, so potentially confounding variables (e.g., socioeconomic status) may not be sufficiently addressed in the literature. Due to such limitations of the literature, it is important to interpret the meta-analysis presented here with caution, and as an impetus for future improved research.
Still, we interpret the presence of small-to-medium effects in the exploratory meta-analysis as reinforcing prior research and further supporting that there is a robust, detectable impact of CEC on individual psychological health in an impacted community. Much of the research indicates that residents of CEC communities show variable psychological responses, and it is important to bear in mind that our meta-analytic approach averages across these variable responses. The small-to-medium effects observed are consistent with the interpretation that while many people’s psychological health is at least somewhat impacted by CEC, only a subset are likely to experience major psychological difficulties; and in many of the reviewed studies a subset of participants met screening criteria (as indicated by self-report measures) for a clinical diagnosis. The relatively larger effect for PTSD outcomes is notable but possibly due to the fact that the majority of PTSD effects came from studies in which a technological disaster was the source of CEC. The effect of CEC on depression (r = 0.20) is also notable. By comparison, in a meta-analytic investigation of the effect of negative life events on depression in older adults, bereavement, severe illness, and financial strain all had relatively smaller effects (Kraaij et al., 2002); and a methodologically rigorous pre/post study showed that a natural disaster had a smaller effect (r = 0.15) on depression rates (Ginexi et al., 2000).
4.2. Future directions
Looking forward, we suggest a number of methodological considerations for future research in this area. More rigorous study designs, especially prospective cohort, longitudinal, and comparative designs ranging across multiple, demographically heterogeneous communities, would better establish the true extent of the psychological health impact of CEC and its moderating factors. Relatedly, future studies should consider more rigorous sampling methodologies that reduce selection biases, such as random sampling in an impacted area or stratified sampling to compare impacted and control communities. In general, greater consistency in measurement of constructs such as experienced stress and PTSD symptoms would also be desirable. It would be beneficial if future research could better triangulate on psychological health outcomes using both self-report and physiological methods. Despite the established importance of allostatic load and the physical health effects of chronic stress (McEwen and Tucker, 2011), we did not find many studies in our systematic review that permit determination of toxicant-stress interactions on health. This is because few studies simultaneously and adequately assess (1) actual and perceived toxicant exposure, (2) both physical and psychological health outcomes, and (3) longitudinal processes in the context of a CEC-impacted community. Future studies should consider other secondary sources of stress faced by these communities (e.g., community conflict, financial losses from dropping property values or the destruction of arable land). Finally, future studies should assess other social determinants of health (e.g., socioeconomic status, education, neighborhood characteristics, access to healthcare) and either control for these factors in analyses, or assess the moderating role that these factors may play in the association between CEC and psychological health outcomes.
To summarize our recommendations for addressing the shortcomings of the extant literature, we suggest that future work should operationalize exposure both objectively and subjectively, operationalize psychological health using physiological indicators as well as self-report measures, assess exposure, psychological health, and physical health outcomes simultaneously, and sample more rigorously from multiple communities simultaneously in order to generalize across experiences or employ longitudinal methods to assess temporal trends in CEC experience.
4.3. Conclusion
The literature we have assembled for this review has broad implications for the psychological health impacts of CEC. We suggest that any successful public health assessment or intervention in communities impacted by CEC must take seriously the psychological health impacts that individuals may face. Of equal import is an understanding of the potential risk factors for worse psychological health outcomes: institutional delegitimization and real or perceived health impacts. It is pivotal that public health officials and local community leaders validate the psychological experiences of impacted communities to adequately address the impact of CEC.
Supplementary Material
HIGHLIGHTS.
Psychological health impact of chronic environmental contamination is understudied.
Contamination was associated with anxiety, general stress, depression, and PTSD.
Institutional delegitimization and physical health impacts may be risk factors.
Acknowledgments
This research was funded by the Agency for Toxic Substances and Disease Registry. Guidehouse Inc. provided project management support.
Footnotes
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2021.145025.
References
- Baum A, Flemming I, 1993. Implications of psychological research on stress and technological accidents. Am Psychol. 48 (6), 665. [DOI] [PubMed] [Google Scholar]
- Behbod B, Parker EM, Jones EA, et al. , 2014. Community health assessment following mercaptan spill: Eightmile, Mobile County, Alabama, September 2012. J Public Health Manag Pract. 20 (6), 632–639. 10.1097/PHH.0000000000000024. [DOI] [PubMed] [Google Scholar]
- Bevc CA, Marshall BK, Picou JS, 2007. Environmental justice and toxic exposure: toward a spatial model of physical health and psychological well-being. Soc. Sci. Res 36 (1), 48–67. [Google Scholar]
- Bowler RM, Mergler D, Huel G, Cone JE, 1994. Psychological, psychosocial, and psychophysiological sequelae in a community affected by a railroad chemical disaster. J. Trauma. Stress 7 (4), 601–624. [DOI] [PubMed] [Google Scholar]
- Brown P, Ferguson FI, 1995. “MAKING A BIG STINK” Women’s work, women’s relationships, and toxic waste activism. Gend. Soc 9 (2), 145–172. [Google Scholar]
- Calloway EE, Chiappone A, Schmitt HJ, et al. , 2020. Exploring community psychosocial stress related to per- and poly-fluoroalkyl substances (PFAS) contamination: lessons learned from a qualitative study. Int. J. Environ. Res. Public Health 17 (23), 8706. 10.3390/ijerph17238706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Checker M, 2007. “But i know it’s true”: environmental risk assessment, justice, and anthropology. Hum. Organ 66 (2), 112–124. [Google Scholar]
- Cline RJ, Orom H, Chung JE, Hernandez T, 2014. The role of social toxicity in responses to a slowly-evolving environmental disaster: the case of amphibole asbestos exposure in Libby, Montana. USA. Am J Community Psychol. 54 (1–2), 12–27. [DOI] [PubMed] [Google Scholar]
- Couch SR, Coles CJ, 2011. Community stress, psychosocial hazards, and EPA decision-making in communities impacted by chronic technological disasters. Am. J. Public Health 101 (Suppl. 1), S140–S148. 10.2105/AJPH.2010.300039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couch SR, Mercuri AE, 2007. Toxic water and the anthill effect: the development of a subculture of distress in a once contaminated community. Cult Contam Legacies Pollut Russ US. 14, 117–137. [Google Scholar]
- Cutchin MP, Martin KR, Owen SV, Goodwin JS, 2008. Concern about petrochemical health risk before and after a refinery explosion. Risk Anal Int J. 28 (3), 589–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhabhar FS, 2011. Effects of stress on immune function: Implications for immunoprotection and immunopathology. Handb Stress Sci Biol Psychol Health. Published online 47–63. [Google Scholar]
- Downey L, Van Willigen M, 2005. Environmental stressors: the mental health impacts of living near industrial activity. J. Health Soc. Behav 46 (3), 289–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelstein M, 2018. Contaminated Communities: Coping with Residential Toxic Exposure. Routledge. [Google Scholar]
- Elliott SJ, Taylor SM, Hampson C, et al. , 1997. ‘It’s not because you like it any better…’: residents’ reappraisal of a landfill site. J. Environ. Psychol 17 (3), 229–241. [Google Scholar]
- Elliott EG, Ma X, Leaderer BP, et al. , 2018. A community-based evaluation of proximity to unconventional oil and gas wells, drinking dwater contaminants, and health symptoms in Ohio. Environ. Res 167, 550–557. 10.1016/j.envres.2018.08.022. [DOI] [PubMed] [Google Scholar]
- Fitzgerald EF, Belanger EE, Gomez MI, et al. , 2008. Polychlorinated biphenyl exposure and neuropsychological status among older residents of upper Hudson River communities. Environ. Health Perspect 116 (2), 209–215. 10.1289/ehp.10432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortenberry GZ, Reynolds P, Burrer SL, et al. , 2018. Assessment of behavioral health concerns in the community affected by the flint water crisis - Michigan (USA) 2016. Prehospital Disaster Med. 33 (3), 256–265. 10.1017/S1049023X18000250. [DOI] [PubMed] [Google Scholar]
- Fowlkes MR, Miller PY, 1987. Chemicals and Community at Love Canal. The Social and Cultural Construction of Risk. Springer, In, pp. 55–78. [Google Scholar]
- Gee GC, Payne-Sturges DC, 2004. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ. Health Perspect 112 (17), 1645–1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhardstein B, Tucker PG, Rayman J, Reh CM, 2019. A fresh look at stress and resilience in communities affected by environmental contamination. J. Environ. Health 82 (4), 36–38. [PMC free article] [PubMed] [Google Scholar]
- Gibbs MS, 1989. Factors in the victim that mediate between disaster and psychopathology: a review. J. Trauma. Stress 2 (4), 489–514. [Google Scholar]
- Ginexi EM, Weihs K, Simmens SJ, Hoyt DR, 2000. Natural disaster and depression: a prospective investigation of reactions to the 1993 Midwest floods. Am. J. Community Psychol 28 (4), 495–518. [DOI] [PubMed] [Google Scholar]
- Ginsberg JP, Holbrook JR, Chanda D, Bao H, Svendsen ER, 2012. Posttraumatic stress and tendency to panic in the aftermath of the chlorine gas disaster in Graniteville. South Carolina. Soc Psychiatry Psychiatr Epidemiol 47 (9), 1441–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasmück D, Scholz RW, 2005. Risk perception of heavy metal soil contamination by high-exposed and low-exposed inhabitants: the role of knowledge and emotional concerns. Risk Anal Int J. 25 (3), 611–622. [DOI] [PubMed] [Google Scholar]
- Greve KW, Bianchini KJ, Doane BM, Love JM, Stickle TR, 2005. Psychological evaluation of the emotional effects of a community toxic exposure. J. Occup. Environ. Med 47 (1), 51–59. 10.1097/01.jom.0000150386.33867.f9. [DOI] [PubMed] [Google Scholar]
- Greve KW, Bianchini KJ, Stickle TR, Love JM, Doane BM, Thompson MD, 2007. Effects of a community toxic release on the psychological status of children. Child Psychiatry Hum. Dev 37 (4), 307–323. 10.1007/s10578-006-0036-3. [DOI] [PubMed] [Google Scholar]
- Ha M, Ju Y-S, Lee WJ, et al. , 2018. Cesium-137 contaminated roads and health problems in residents: An epidemiological investigation in Seoul, 2011. J Korean Med Sci. 33 (9). 10.3346/jkms.2018.33.e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastrup JL, Thomas SN, Edelstein MR, 2007. Fear of cancer in a rural Appalachian community following notification of an environmental hazard. Res Soc Probl Public Policy. 14, 93–115. [Google Scholar]
- Havenaar JM, Van den Brink W, 1997. Psychological factors affecting health after toxicological disasters. Clin. Psychol. Rev 17 (4), 359–374. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thomas J, 2019. Chandler J, et al. John Wiley & Sons, Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
- Hoover E, Renauld M, Edelstein MR, Brown P, 2015. Social science collaboration with environmental health. Environ. Health Perspect 123 (11), 1100–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SY, Park JE, Lee YJ, et al. , 2013. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J. Clin. Epidemiol 66 (4), 408–414. [DOI] [PubMed] [Google Scholar]
- Korol M, Green BL, Gleser GC, 1999. Children’s responses to a nuclear waste disaster: PTSD symptoms and outcome prediction. J. Am. Acad. Child Adolesc. Psychiatry 38 (4), 368–375. 10.1097/00004583-199904000-00008. [DOI] [PubMed] [Google Scholar]
- Kraaij V, Arensman E, Spinhoven P. Negative life events and depression in elderly persons: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2002;57(1):P87–P94. [DOI] [PubMed] [Google Scholar]
- Kramar DE, Anderson A, Hilfer H, Branden K, Gutrich JJ, 2018. A spatially informed analysis of environmental justice: analyzing the effects of gerrymandering and the proximity of minority populations to US superfund sites. Environ Justice. 11 (1), 29–39. [Google Scholar]
- Kruger DJ, Cupal S, Franzen SP, et al. , 2017a. Toxic trauma: household water quality experiences predict posttraumatic stress disorder symptoms during the Flint, Michigan, water crisis. J Community Psychol. 45 (7), 957–962. [Google Scholar]
- Kruger DJ, Kodjebacheva GD, Cupal S, 2017b. Poor tap water quality experiences and poor sleep quality during the Flint. Michigan Municipal Water Crisis. Sleep Health. 3 (4), 241–243. [DOI] [PubMed] [Google Scholar]
- Kruger DJ, Cupal S, Kodjebacheva GD, Fockler TV, 2017c. Perceived water quality and reported health among adults during the Flint, MI water crisis. Californian J Health Promot. 15 (1), 56–61. [Google Scholar]
- Lebovits AH, Baum A, Singer JE, 1986. Exposure to Hazardous Substances: Psychological Parameters. Lawrence Erlbaum. [Google Scholar]
- Levy JI, Welker-Hood LK, Clougherty JE, Dodson RE, Steinbach S, Hynes HP, 2004. Lung function, asthma symptoms, and quality of life for children in public housing in Boston: a case-series analysis. Environ Health Glob Access Sci Source. 3. 10.1186/1476-069X-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthies E, Höger R, Guski R, 2000. Living on polluted soil: determinants of stress symptoms. Environ. Behav 32 (2), 270–286. 10.1177/00139160021972522. [DOI] [Google Scholar]
- McCarron P, Harvey I, Brogan R, Peters TJ, 2000. Self reported health of people in an area contaminated by chromium waste: interview study. Br. Med. J 320 (7226), 11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McComas KA, Trumbo CW, 2001. Source credibility in environmental health–risk controversies: application of Meyer’s credibility index. Risk Anal. 21 (3), 467–480. [DOI] [PubMed] [Google Scholar]
- McEwen BS, 2008. Central effects of stress hormones in health and disease: understanding the protective and damaging effects of stress and stress mediators. Eur. J. Pharmacol 583 (2–3), 174–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS, Tucker P, 2011. Critical biological pathways for chronic psychosocial stress and research opportunities to advance the consideration of stress in chemical risk assessment. Am. J. Public Health 101 (S1), S131–S139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre E, Prior J, Connon ILC, Adams J, Madden B, 2018. Sociodemographic predictors of residents worry about contaminated sites. Sci. Total Environ 643, 1623–1630. 10.1016/j.scitotenv.2018.06.261. [DOI] [PubMed] [Google Scholar]
- Mohai P, Saha R, 2015. Which came first, people or pollution? A review of theory and evidence from longitudinal environmental justice studies. Environ. Res. Lett 10 (12), 125011. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, 2009. Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6 (7), e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Shenassa ED, 2006. The environmental “riskscape” and social inequality: implications for explaining maternal and child health disparities. Environ. Health Perspect 114 (8), 1150–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, 2006. Methods for Disaster Mental Health Research. Guilford Press. [Google Scholar]
- Nuru-Jeter AM, Michaels EK, Thomas MD, Reeves AN, Thorpe RJ Jr., LaVeist TA, 2018. Relative roles of race versus socioeconomic position in studies of health inequalities: a matter of interpretation. Annu. Rev. Public Health 39, 169–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peek MK, Cutchin MP, Freeman D, Stowe RP, Goodwin JS, 2009. Environmental hazards and stress: evidence from the Texas City stress and health study. J. Epidemiol. Community Health 63 (10), 792–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulido L, 2000. Rethinking environmental racism: white privilege and urban development in Southern California. Ann. Assoc. Am. Geogr 90 (1), 12–40. [Google Scholar]
- Sullivan D, Schmitt HJ, Calloway E, Clausen W, Tucker P, Rayman J, & Gerhardstein B (under review). Chronic Environmental Contamination: A Narrative Review of Psychosocial Health Consequences, Risk Factors, and Pathways to Community Resilience. [DOI] [PubMed]
- Rehner TA, Kolbo JR, Trump R, Smith C, Reid D, 2000. Depression among victims of south Mississippi’s methyl parathion disaster. Health Soc. Work 25 (1), 33–39. [DOI] [PubMed] [Google Scholar]
- Reich MR, 1991. Toxic Politics: Responding to Chemical Disasters. Cornell University Press. [Google Scholar]
- Reif JS, Burch JB, Nuckols JR, Metzger L, Ellington D, Anger WK, 2003. Neurobehavioral effects of exposure to trichloroethylene through a municipal water supply. Environ. Res 93 (3), 248–258. 10.1016/S0013-9351(03)00131-2. [DOI] [PubMed] [Google Scholar]
- Sansom G, Parras J, Parras A, et al. , 2017. The impacts of exposure to environmental risk on physical and mental health in a small geographic community in Houston. TX. J Community Health. 42 (4), 813–818. 10.1007/s10900-017-0322-y. [DOI] [PubMed] [Google Scholar]
- Santiago-Rivera AL, Morse GS, Haase RF, McCaffrey RJ, Tarbell A, 2007. Exposure to an environmental toxin, quality of life and psychological distress. J. Environ. Psychol 27 (1), 33–43. [Google Scholar]
- Schade CP, Wright N, Gupta R, Latif DA, Jha A, Robinson J, 2015. Self-reported household impacts of large-scale chemical contamination of the public water supply, Charleston, West Virginia, USA. PLoS ONE 10 (5). 10.1371/journal.pone.0126744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schade CP, Gupta R, Jha A, Wright N, 2016. Persistent distress after water contamination. W V Med J. 112 (5), 40–47. [PubMed] [Google Scholar]
- Segal D, Lin Y-S, Ginsberg G, Sonawane B, 2015. A conceptual framework for evaluating the interaction of a chemical and nonchemical stressor in human health risk assessments: a case study for lead and psychosocial stress. Hum Ecol Risk Assess Int J. 21 (7), 1840–1868. [Google Scholar]
- Song JY, Jeong K-S, Choi K, Kim M, Ahn Y-S, 2018. Psychological risk factors for post-traumatic stress disorder in workers after toxic chemical spill in Gumi. South Korea. Workplace Health Saf. 66 (8), 393–402. [DOI] [PubMed] [Google Scholar]
- Tucker P, 1998. Report of the Expert Panel Workshop on the Psychological Responses to Hazardous Substances. U.S. Department of Health and Human Services. https://www.atsdr.cdc.gov/hec/prhs/psych5ed.pdf. (Accessed 1 October 2019). [Google Scholar]
- Ushijima K, Kitano T, Shono M, et al. , 2004. Social factors associated with psychological distress among inhabitants in a methyl-mercury polluted area in rural Japan. Environ Sci Int J Environ Physiol Toxicol 11 (3), 151–162. [PubMed] [Google Scholar]
- Vandermoere F, 2006. The process of soil excavation in a community: site-specific determinants of stress perception. Environ. Behav 38 (5), 715–739. [Google Scholar]
- Vandermoere F, 2008. Psychosocial health of residents exposed to soil pollution in a Flemish neighbourhood. Soc. Sci. Med 66 (7), 1646–1657. 10.1016/j.socscimed.2007.12.031. [DOI] [PubMed] [Google Scholar]
- Verschuur M, Spinhoven P, Emmerik A.v., Rosendaal F, 2007. Making a bad thing worse: effects of communication of results of an epidemiological study after an aviation disaster. Soc. Sci. Med 65 (7), 1430–1441. 10.1016/j.socscimed.2007.05.014. [DOI] [PubMed] [Google Scholar]
- Verschuur MJ, Spinhoven P, Rosendaal FR, 2008. Offering a medical examination following disaster exposure does not result in long-lasting reassurance about health complaints. Gen. Hosp. Psychiatry 30 (3), 200–207. 10.1016/j.genhosppsych.2008.02.006. [DOI] [PubMed] [Google Scholar]
- Vyner HM, 1988. The psychological dimensions of health care for patients exposed to radiation and the other invisible environmental contaminants. Soc. Sci. Med 27 (10), 1097–1103. [DOI] [PubMed] [Google Scholar]
- Weinert C, Hill WG, Winters CA, et al. , 2011. Psychosocial health status of persons seeking treatment for exposure to libby amphibole asbestos. ISRN Nurs. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteman DC, Dunne MP, Burnett PC, 1995. Psychological and social correlates of attrition in a longitudinal study of hazardous waste exposure. Arch. Environ. Health 50 (4), 281–286. 10.1080/00039896.1995.9935955. [DOI] [PubMed] [Google Scholar]
- Zierold KM, Knobeloch L, Anderson H, 2004. Prevalence of chronic diseases in adults exposed to arsenic-contaminated drinking water. Am. J. Public Health 94 (11), 1936–1937. 10.2105/AJPH.94.11.1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


