Abstract
BACKGROUND:
Despite cardiac rehabilitation (CR) being shown to improve health outcomes among patients with heart disease, its use has been suboptimal. In response, the Million Hearts Cardiac Rehabilitation Collaborative developed a road map to improve CR use, including increasing participation rates to ≥70% by 2022. This observational study provides current estimates to measure progress and identifies the populations and regions most at risk for CR service underutilization.
METHODS AND RESULTS:
We identified Medicare fee-for-service beneficiaries who were CR eligible in 2016, and assessed CR participation (≥1 CR session attended), timely initiation (participation within 21 days of event), and completion (≥36 sessions attended) through 2017. Measures were assessed overall, by beneficiary characteristics and geography, and by primary CR-qualifying event type (acute myocardial infarction hospitalization; coronary artery bypass surgery; heart valve repair/replacement; percutaneous coronary intervention; or heart/heart-lung transplant). Among 366 103 CR-eligible beneficiaries, 89 327 (24.4%) participated in CR, of whom 24.3% initiated within 21 days and 26.9% completed CR. Eligibility was highest in the East South Central Census Division (14.8 per 1000). Participation decreased with increasing age, was lower among women (18.9%) compared with men (28.6%; adjusted prevalence ratio: 0.91 [95% CI, 0.90–0.93]) was lower among Hispanics (13.2%) and non-Hispanic blacks (13.6%) compared with non-Hispanic whites (25.8%; adjusted prevalence ratio: 0.63 [0.61–0.66] and 0.70 [0.67–0.72], respectively), and varied by hospital referral region and Census Division (range: 18.6% [East South Central] to 39.1% [West North Central]) and by qualifying event type (range: 7.1% [acute myocardial infarction without procedure] to 55.3% [coronary artery bypass surgery only]). Timely initiation varied by geography and qualifying event type; completion varied by geography.
CONCLUSIONS:
Only 1 in 4 CR-eligible Medicare beneficiaries participated in CR and marked disparities were observed. Reinforcement of current effective strategies and development of new strategies will be critical to address the noted disparities and achieve the 70% participation goal.
Keywords: cardiac rehabilitation, coronary artery bypass, heart diseases, myocardial infarction, percutaneous coronary intervention
Outpatient cardiac rehabilitation (CR) is a multidisciplinary, evidence-based intervention shown to improve health outcomes and quality of life when used among patients who have suffered an acute myocardial infarction (AMI), undergone a cardiac procedure (eg, coronary artery bypass surgery [CABG]) or have a persistent cardiac condition that would benefit from structured exercise and focused disease management (eg, chronic heart failure).1–4 Typically, a complete course of CR is considered attending ≥36 supervised sessions over a period of around 12 weeks. There is a positive association reported between the number of sessions used and improved health outcomes.5–7 Despite national guidelines supporting its use8,9 and CR being a commonly covered benefit within health insurance plans,10–12 historically, only around 20% of eligible patients participate in CR13 and the number of sessions used by patients who do initiate CR is often suboptimal.5,6 Furthermore, considerable disparities in CR use exist by geography, patient characteristics, and qualifying event type.14–18
In response, the Million Hearts Cardiac Rehabilitation Collaborative (Collaborative), representing over 100 organizations and agencies, developed a road map in 2016 with the goal to increase CR participation (≥1 CR session attended) from 20% to ≥70% by 2022.13 This goal was established based on the participation rates attained by some high-performing CR programs.13 Achieving it would support the Million Hearts 2022 overall aim of preventing 1 million heart attacks, strokes, and other cardiovascular events (https://millionhearts.hhs.gov)19,20 by saving an estimated 25 000 lives and preventing 180 000 hospitalizations annually in the United States.13 The purpose of this article is to provide current estimates among Medicare fee-for-service (FFS) beneficiaries aged ≥65 years—a group that historically has had similar CR participation rates as those described using national survey data5,13,16—that will serve as a baseline to measure the Collaborative’s progress in achieving their 5-year participation goal, as well as to provide estimates for other important CR-related measures. Furthermore, this article identifies the populations most at risk for underutilization of CR services. These findings can be used to inform efforts at minimizing disparities and potentially unwarranted variation in CR use by geography and qualifying event type to improve cardiovascular health outcomes.
METHODS
We analyzed Medicare Part A and Part B claims data collected during 2016 to 2017 within the Centers for Medicare and Medicaid Services Chronic Conditions Warehouse database for FFS beneficiaries aged ≥65 years. The Medicare data sets used can be obtained for a fee by external researchers; see https://www.resdac.org for additional information. In alignment with Medicare’s benefit guidance,10,11 beneficiaries were considered eligible for outpatient CR if they experienced ≥1 of the following events during 2016 (referred to collectively as primary qualifying events): AMI hospitalization; CABG; heart valve repair or replacement; percutaneous coronary intervention; or heart or heart-lung transplant. Events were identified based on beneficiaries’ receipt of specified International Classification of Disease, Tenth Revision, Clinical Modification diagnosis (first- or second-listed code) or procedural codes (any location) on inpatient claims or current procedural terminology codes (any location) on outpatient or provider claims (Table in the Data Supplement).
In separate analyses, beneficiaries without a primary qualifying event were considered CR eligible if they had documented current stable angina pectoris (angina) or stable, chronic heart failure (heart failure) during 2016 (referred to collectively as secondary qualifying events). Angina was defined as having a specified International Classification of Disease, Tenth Revision, Clinical Modification code (any location) on ≥2 outpatient claims (Table in the Data Supplement). Heart failure was defined in 2 ways in an attempt to match Medicare’s clinical eligibility criteria.11 Diagnosis-based heart failure was defined as having a specified International Classification of Disease, Tenth Revision, Clinical Modification code (any location) for chronic systolic (or systolic/diastolic) heart failure on ≥2 outpatient claims or on an inpatient claim with no subsequent cardiovascular disease-related hospitalization occurring within 6 weeks (Table in the Data Supplement). Procedure-based heart failure was defined as having a specified International Classification of Disease, Tenth Revision, Clinical Modification procedure code or current procedural terminology code in an inpatient or outpatient encounter for either insertion of an implantable ventricular assist device or biventricular pacemaker (Table in the Data Supplement).
To be included in the analyses, beneficiaries had to be alive for >21 days after their qualifying event; have continuous Medicare Part A and Part B enrollment for ≥12 months after their qualifying event unless they died; not be a nursing home resident—defined as ≥90 consecutive days of skilled nursing facility care—nor receive hospice care either before the qualifying event or ≤21 days after discharge for the initial qualifying event; and not be entitled to Medicare benefits due to having end-stage renal disease. Among beneficiaries with >1 primary qualifying event, the first event was considered the index event. Beneficiaries with multiple primary qualifying events occurring within 21 days were recoded as combinations (eg, AMI with CABG). Additional steps were taken to identify the index date among beneficiaries meeting the angina and heart failure criteria (Methods in the Data Supplement). An outpatient CR session was defined as having a Healthcare Common Procedure Coding System code for physician services for outpatient CR without (93 797) or with (93 798) continuous electrocardiographic monitoring or intensive CR with or without continuous ECG monitoring and with (G0422) or without (G0423) exercise in combination with a place of service code of 11 (office), 19 (off-campus outpatient hospital), or 22 (on-campus outpatient hospital).
Multiple CR utilization-related factors were assessed. Eligibility was defined as a beneficiary having a qualifying CR event during January 1, 2016, to December 31, 2016, and was expressed as the number of beneficiaries with qualifying events per 1000 beneficiaries. Participation was defined as a CR-eligible beneficiary participating in ≥1 CR sessions within 365 days of the qualifying event date and was measured as the percentage of eligible beneficiaries who participated in CR. Time to participation was defined as the number of days from the event date until CR initiation and was measured as mean days to participation and via 3 categorical variables: initiated participation in ≤21, ≤42, or ≤90 days. CR participation in ≤21 days was termed timely initiation, which aligns with the current quality measure.21 Utilization describes the number of sessions used by participants within 36 weeks of CR initiation and was measured as mean sessions used and via 2 categorical variables: participation in ≥25 sessions (an important threshold for conveying health benefits5) or ≥36 sessions (termed completion).
The CR utilization-related factors were assessed by age; sex; race/ethnicity; dual Medicare and Medicaid coverage status; comorbidity status, defined as the count of meeting the specifications22 for ever having any of 9 chronic conditions while a Medicare FFS beneficiary (Table 1); chronic kidney disease status; post-acute care use after the qualifying event; death status during the observation year; CR-qualifying event type (summarized as AMI only, AMI with procedure, and procedure only), and US Census Division and hospital referral region (HRR) of the beneficiary’s primary residence. To compare findings within strata, adjusted prevalence ratios (aPRs) were calculated instead of odds ratios because of the high prevalence of cases and the potential for overestimation using odds ratios.23 The aPRs were calculated using PROC GENMOD (SAS Enterprise Guide version 7.1 Cary, NC) and adjusted, as appropriate, for age, sex, race-ethnicity, dual status, comorbidity count category, qualifying event type, and death status. Convergence of the model was achieved using a log link and a Poisson distribution and the relative Hessian convergence criterion was <0.0001. HRR-level maps were developed for the CR utilization factors, displaying unadjusted values and aPRs. Overall and patient CR-related costs were captured. This research was considered exempt from Institutional Review Board review under 45 Code of Federal Regulations 46.101[b] [5] which covers Department of Health and Human Services research and demonstration projects which are designed to study, evaluate, or examine public benefit or service programs.
Table 1.
Cardiac Rehabilitation Eligibility, Participation, and Utilization Among Medicare Fee-for-Service Beneficiaries Aged ≥65 Years Who Had a Primary Qualifying Event Type, 2016–2017
| CR Eligible | Participation Among Eligible | Sessions Used Among Participants | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Rate/1000 | N | % | aPR* (95% CI) | Mean No. of Sessions (SD) | ≥25 Sessions, % | ≥36 Sessions | ||
| % | aPR* (95% CI) | ||||||||
| Total | 366 103 | 13.0 | 89 327 | 24.4 | NA | 24.8 (12.0) | 56.7 | 26.9 | NA |
| 65–74 y | 151 392 | 10.0 | 48 037 | 31.7 | Referent | 24.8 (12.0) | 56.4 | 26.8 | Referent |
| 75–84 y | 134 699 | 15.6 | 33 436 | 24.8 | 0.93 (0.92–0.95) | 25.2 (11.8) | 57.9 | 27.6 | 1.08 (1.05–1.11) |
| ≥ 85 y | 80 012 | 18.0 | 7854 | 9.8 | 0.57 (0.56–0.59) | 23.6 (12.4) | 53.5 | 23.9 | 0.98 (0.93–1.03) |
| Sex | |||||||||
| Male | 207 911 | 16.9 | 59 462 | 28.6 | Referent | 25.4 (11.8) | 58.7 | 28.3 | Referent |
| Female | 158 192 | 10.0 | 29 865 | 18.9 | 0.91 (0.90–0.93) | 24.5 (12.2) | 56.5 | 26.1 | 0.87 (0.85–0.90) |
| Race-ethnicity | |||||||||
| Non-Hispanic white | 313 251 | 13.5 | 80 884 | 25.8 | Referent | 25.4 (11.9) | 56.4 | 26.8 | Referent |
| Non-Hispanic black | 22 865 | 11.0 | 3113 | 13.6 | 0.70 (0.67–0.72) | 24.4 (12.5) | 56.4 | 26.9 | 1.07 (1.00–1.14) |
| Hispanic | 16 182 | 11.1 | 2130 | 13.2 | 0.63 (0.61–0.66) | 23.1 (12.9) | 52.6 | 23.7 | 0.97 (0.89–1.06) |
| Asian | 6342 | 8.6 | 1033 | 16.3 | 0.80 (0.75–0.85) | 24.3 (12.6) | 55.6 | 26.3 | 1.06 (0.94–1.20) |
| Other/unknown | 7463 | 10.2 | 2167 | 29.0 | 0.96 (0.92–1.00) | 25.4 (11.8) | 58.7 | 27.5 | 1.00 (0.92–1.08) |
| Dual Medicare/Medicaid coverage | |||||||||
| No | 324 167 | 12.8 | 86 449 | 26.7 | Referent | 25.0 (11.9) | 57.2 | 27.2 | Referent |
| Yes | 41 936 | 14.9 | 2878 | 6.9 | 0.40 (0.39–0.42) | 19.6 (13.3) | 40.7 | 16.8 | 0.65 (0.59–0.71) |
| Comorbidities† | |||||||||
| 0–2 | 54 874 | 4.6 | 20 619 | 37.6 | Referent | 25.3 (11.8) | 57.5 | 29.0 | Referent |
| 3–4 | 108 397 | 11.9 | 33 634 | 31.0 | 1.01 (0.99–1.03) | 25.5 (11.7) | 58.8 | 28.0 | 0.97 (0.94–1.00) |
| 5–6 | 133 522 | 24.8 | 27 066 | 20.3 | 0.87 (0.85–0.88) | 24.4 (12.1) | 55.6 | 25.5 | 0.89 (0.86–0.92) |
| 7–9 | 69 310 | 37.0 | 8008 | 11.6 | 0.65 (0.63–0.67) | 22.5 (12.6) | 49.6 | 21.3 | 0.76 (0.72–0.80) |
| Chronic kidney disease‡ | |||||||||
| No | 138 877 | 6.9 | 44 883 | 32.3 | Referent | 25.2 (11.8) | 57.6 | 27.9 | Referent |
| Yes | 227 226 | 28.0 | 44 444 | 19.6 | 0.86 (0.85–0.87) | 24.4 (12.1) | 55.8 | 25.8 | 0.94 (0.91–0.96) |
| PAC use§ | |||||||||
| None | 322 843 | NA | 84 076 | 26.1 | Referent | 24.9 (11.9) | 53.7 | 25.5 | Referent |
| Any PAC use | 43 260 | NA | 5251 | 12.1 | 0.61 (0.60–0.63) | 25.1 (11.9) | 58.3 | 26.7 | 1.03 (0.98–1.09) |
| Home health only | 25 034 | NA | 3743 | 15.0 | 0.71 (0.68–0.73) | 25.1 (11.9) | 58.7 | 26.8 | 1.03 (0.96–1.09) |
| Any institutional PAC‖ | 18 226 | NA | 1508 | 8.3 | 0.46 (0.44–0.49) | 25.1 (12.0) | 57.4 | 26.5 | 1.04 (0.94–1.15) |
| Died >21 d of discharge | |||||||||
| No | 317 377 | NA | 88 494 | 27.9 | Referent | 24.9 (11.9) | 57.0 | 27.1 | Referent |
| Yes | 48 726 | NA | 833 | 1.7 | 0.11 (0.11–0.12) | 14.4 (11.5) | 22.9 | 5.6 | 0.22 (0.17–0.30) |
aPR indicates adjusted prevalence ratio; CR, cardiac rehabilitation; NA, not applicable; and PAC, post-acute care.
Adjusted, as appropriate, by age, sex, race-ethnicity, dual status, comorbidity count category, qualifying event type, and death status.
Count of the following: documented evidence of heart failure, atrial fibrillation, stroke/transient ischemic attack, endocrine or renal dysfunction, cancer, musculoskeletal or joint dysfunction, pulmonary dysfunction, cognitive or mental impairment, or ophthalmic dysfunction.
Covariates included in the adjusted model were modified by removing chronic kidney disease from one of the conditions included in the comorbidity count variable.
Covariates included in the adjusted model were modified by excluding qualifying event type because of collinearity with the PAC use variables.
Any use of a long-term care facility, skilled nursing facility, or inpatient rehabilitation facility with or without home health after the initial qualifying event occurred.
RESULTS
In 2016, 366 103 Medicare beneficiaries had a primary CR-eligible event (13.0 per 100 000 beneficiaries), with eligibility rates increasing with age and numbers of comorbidities, and being highest among men (16.9 per 100 000), non-Hispanic whites (13.5 per 100 000), and beneficiaries dual-eligible for Medicare and Medicaid (14.9 per 100 000; Table 1).
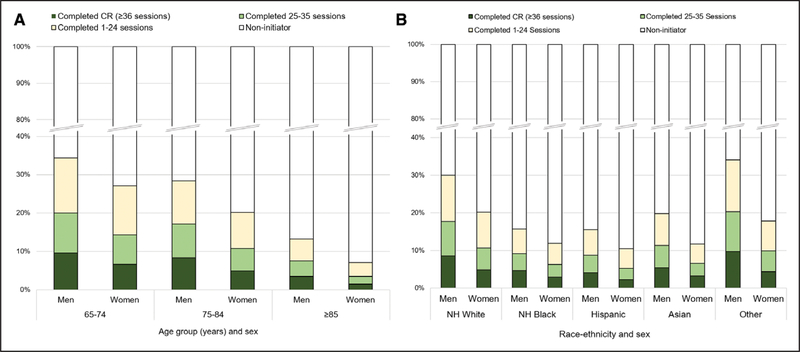
Overall, 89 327 (24.4%) of eligible beneficiaries participated in CR (Table 1), accounting for $227.6 million in total costs (mean of $103 per CR session used), including $51.8 million in beneficiary out-of-pocket costs paid by beneficiaries or through supplemental insurance (mean of $23 per CR session used; data not shown). Participation decreased with increasing age and was lower in women compared with men (18.9% versus 28.6%; aPR: 0.91 [95% CI, 0.90–0.93]); disparities by sex increased with increasing age (Figure 1A). Non-Hispanic whites had the highest participation rate (25.8%), with Hispanics (13.2%) being 0.63 times as likely (aPR 95% CI, 0.61–0.66) and non-Hispanic blacks (13.6%) being 0.70 times as likely (aPR 95% CI, 0.67–0.72) as whites to participate (Table 1). Hispanic (10.4%), non-Hispanic black (11.9%), and Asian (11.7%) women had particularly low rates, with the rate among Asian men (19.8%) being almost 70% higher than that among Asian women (Figure 1B). Dual-eligible beneficiaries were 0.40 (aPR 95% CI, 0.39–0.42) times as likely as non-dual-eligible beneficiaries to participate (6.9% versus 26.7%), and rates were considerably lower among beneficiaries with ≥5 comorbidities compared with 0 to 2 comorbidities (Table 1). Using PAC services after the qualifying event was associated with decreased participation, especially if institutional PAC was used (8.3% versus 26.1% [no PAC use]; aPR: 0.46 [95% CI, 0.44–0.49]).
Figure 1.
Cardiac rehabilitation participation and completion among eligible* Medicare fee-for-service beneficiaries aged ≥65 y, by (A) age and sex and (B) race-ethnicity and sex, 2016–2017.
CR indicates cardiac rehabilitation; and NH, non-Hispanic. *Includes primary CR-qualifying event types only.
Overall, the mean number of sessions used by CR participants was 24.8 (SD: 12.0), with 56.7% of participants using ≥25 sessions and 26.9% using ≥36 sessions, or completing CR (Table 1). Completion rates were highest among beneficiaries aged 75 to 84 years (27.6%; aPR: 1.08 [95% CI, 1.05–1.11]) compared with adults aged 65–74 years]), lower in women compared with men (26.1% versus 28.3%; aPR: 0.87 [95% CI, 0.85–0.90]), and had minimal variation by race-ethnicity or PAC use. Dual-eligible beneficiaries were 35% less likely (aPR: 0.65 [95% CI, 0.59–0.71]) as non-dual-eligible beneficiaries to complete CR (16.8% versus 27.2%), and completion rates were lower among beneficiaries with ≥5 comorbidities (representing 55% of CR-eligible beneficiaries) compared with 0 to 2 comorbidities (15% of CR-eligible beneficiaries).
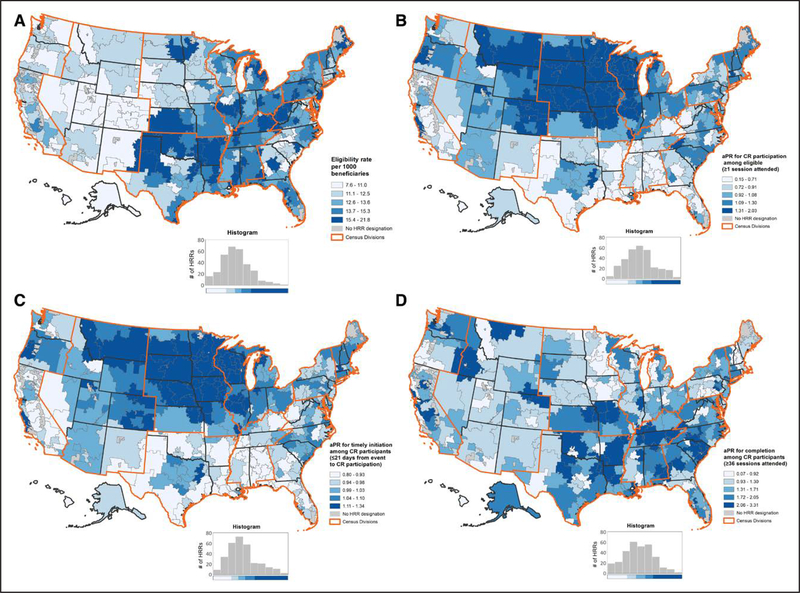
Table 2 shows the CR measures summarized by Census Division, which are then mapped by HRR in Figure 2 (unadjusted eligibility rates and aPRs for participation, timely initiation, and completion) and Figure I in the Data Supplement (unadjusted participation, timely initiation, and completion rates). CR eligibility ranged across Census Divisions from 10.7 (Mountain) to 14.8 (East South Central) per 1000 beneficiaries and ranged from 7.6 to 21.8 per 1000 beneficiaries across HRRs. Using the New England division (participation rate: 26.5%) as the referent, CR participation ranged from a low of 18.6% in the East South Central division (aPR: 0.62 [95% CI, 0.59–0.64]) to a high of 39.1% in the West North Central division (aPR: 1.24 [95% CI, 1.20–1.29]); range of 3.6% to 57.7% across HRRs (aPR range of 0.15–2.03; referent: Boston, Massachusetts HRR). Overall, the mean days from the qualifying event until CR participation was 47.0 (SD: 38.6) days, with 24.3% of participants initiating CR within 21 days, or having timely initiation. Timely initiation was lowest in the Middle Atlantic division (11.9%; aPR: 0.76 [95% CI, 0.69–0.82]) and greatest in the West North Central division (50.2%; aPR: 3.11 [95% CI, 2.90–3.34]); range of 3.0% to 84.8% across HRRs (aPR range of 0.80–1.34). Nationally, 58.0% of participants initiated CR within 42 days and 89.5% within 90 days. Slight variation in completion rates was observed by Census Division, with the highest rate occurring in the East South Central division (33.2%; aPR: 1.43 [95% CI, 1.33–1.54]); range of 5.0% to 57.9% across HRRs (aPR range of 0.07–3.31). Maps of the unadjusted rates and aPRs for the CR-related measures at the HRR level showed similar patterns.
Table 2.
Cardiac Rehabilitation Eligibility,* Participation, Timely Initiation, and Utilization by US Census Division Among Medicare Fee-for-Service Beneficiaries Aged ≥65 Years, 2016–2017
| Census Division | CR Eligible | Participation Among Eligible | Days From Event to CR Participation | Sessions Used Among Participants | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Rate/ 1000 | N | % | aPR† (95% CI) | Mean No. of Days (SD) | ≤21 Days | ≤42 Days, % | ≤90 Days, % | Mean No. of Sessions (SD) | ≥25 Sessions, % | ≥36 Sessions | |||
| % | aPR† (95% CI) | % | aPR† (95% CI) | |||||||||||
| New England | 21 202 | 13.4 | 5624 | 26.5 | Referent | 55.3 (41.1) | 16.7 | Referent | 47.2 | 84.3 | 24.3 (11.3) | 51.7 | 23.1 | Referent |
| Middle Atlantic | 49 504 | 13.8 | 9623 | 19.4 | 0.71 (0.69–0.74) | 58.5 (41.5) | 11.9 | 0.76 (0.69–0.82) | 42.1 | 84.0 | 25.4 (11.7) | 59.6 | 25.4 | 1.10 (1.03–1.18) |
| East North Central | 61 247 | 14.0 | 18 967 | 31.0 | 1.06 (1.03–1.09) | 44.4 (37.0) | 26.2 | 1.63 (1.52–1.75) | 61.2 | 90.9 | 24.6 (11.8) | 55.6 | 24.6 | 1.07 (1.01–1.14) |
| West North Central | 26 140 | 13.1 | 10 218 | 39.1 | 1.24 (1.20–1.29) | 30.4 (30.1) | 50.2 | 3.11 (2.90–3.34) | 79.7 | 95.8 | 23.6 (11.8) | 49.5 | 24.8 | 1.07 (1.00–1.15) |
| South Atlantic | 78 374 | 12.7 | 17 864 | 22.8 | 0.76 (0.74–0.78) | 52.4 (38.8) | 15.2 | 0.97 (0.90–1.04) | 49.6 | 88.3 | 25.7 (11.9) | 61.1 | 31.1 | 1.34 (1.26–1.42) |
| East South Central | 28 534 | 14.8 | 5317 | 18.6 | 0.62 (0.59–0.64) | 46.5 (36.7) | 21.0 | 1.34 (1.23–1.46) | 59.5 | 90.5 | 25.5 (12.0) | 59.6 | 33.2 | 1.43 (1.33–1.54) |
| West South Central | 42 353 | 13.9 | 8548 | 20.2 | 0.65 (0.63–0.67) | 41.9 (37.8) | 30.8 | 2.01 (1.86–2.17) | 66.9 | 91.6 | 25.5 (12.5) | 60.7 | 31.4 | 1.36 (1.27–1.45) |
| Mountain | 20 384 | 10.7 | 5852 | 28.7 | 0.88 (0.85–0.92) | 40.7 (36.2) | 32.5 | 2.02 (1.87–2.19) | 66.1 | 92.2 | 23.3 (12.3) | 51.8 | 22.6 | 0.97 (0.90–1.05) |
| Pacific | 37 533 | 10.8 | 7274 | 19.4 | 0.73 (0.70–0.75) | 53.4 (40.4) | 15.8 | 1.00 (0.91–1.09) | 50.7 | 86.5 | 24.2 (12.4) | 56.3 | 23.5 | 1.02 (0.95–1.10) |
| Missing | 832 | 6.4 | 40 | 4.8 | 0.24 (0.18–0.33) | 57.1 (52.5) | ‡ | ‡ | 52.5 | 85.0 | 14.7 (11.3) | ‡ | ‡ | ‡ |
| Total | 366 103 | 13.0 | 89 327 | 24.4 | NA | 47.0 (38.6) | 24.3 | NA | 58.0 | 89.5 | 24.8 (12.4) | 56.7 | 26.9 | NA |
aPR indicates adjusted prevalence ratio; CR, cardiac rehabilitation; and NA, not applicable.
Includes primary qualifying event types only; rate per 1000 Medicare Fee-for-service beneficiaries.
Adjusted by age, sex, race-ethnicity, dual status, qualifying event type, comorbidity count category, and death status.
Suppressed because of small cell size.
Figure 2.
Cardiac rehabilitation unadjusted eligibility rates and adjusted* prevalence ratios for participation, timely initiation, and completion among Medicare fee-for-service beneficiaries aged ≥65 y, by hospital referral region and US Census Division, 2016–2017.
aPR indicates adjusted prevalence ratio; CR, cardiac rehabilitation; and HRR, hospital referral region. *Adjusted, as appropriate, by age, sex, race-ethnicity, dual status, comorbidity count category, qualifying event type, and death status. The Boston, Massachusetts HRR was used as the referent.
CR participation varied considerably by primary qualifying event type (Table 3). For beneficiaries with an AMI, the overall participation rate was 16.5% but varied considerably depending on if a CR-qualifying cardiac procedure was performed within 21 days of the AMI: 7.1% (no cardiac procedure) to 34.5% (cardiac procedure). Among beneficiaries who had a CR-qualifying cardiac procedure performed, participation rates ranged from 23.1% for percutaneous coronary intervention with no AMI to 55.3% for CABG with no AMI. Timely initiation occurred among 32.1% of CR participants who had an AMI and was higher among those who did not have a cardiac procedure (38.3%) compared to those who did (29.6%). Among CR participants who had a cardiac procedure, timely initiation was lowest for CABG and heart valve repair/replacement (10.6%) and highest for percutaneous coronary intervention with AMI (33.8%). For CR participants with an AMI, the overall completion rate was 26.5%, ranging from 25.3% to 27.0% for those without and with a cardiac procedure, respectively. Among those who had a cardiac procedure, completion rates ranged from 23.9% for heart transplant to 29.7% for CABG with AMI.
Table 3.
Cardiac Rehabilitation Eligibility, Participation, and Utilization by Primary Qualifying Event Type Among Medicare Fee-for-Service Beneficiaries Aged ≥65 y, 2016–2017
| Eligible Condition/Procedure* | CR Eligible | CR Participation Among Eligible | Days From Event to CR Participation | Sessions Used Among Participants | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Rate/ 1000 | N | % | Mean No. of Days | SD | ≤21 Days, % | ≤42 Days, % | ≤90 Days, % | Mean No. of Sessions | SD | ≥25 Sessions, % | ≥36 Sessions, % | |
| AMI | 222 589 | 7.9 | 36 635 | 16.5 | 43.2 | 39.7 | 32.1 | 64.3 | 90.1 | 24.6 | 12.1 | 56.0 | 26.5 |
| With no procedure | 146 831 | 5.2 | 10 492 | 7.1 | 45.0 | 47.3 | 38.3 | 63.8 | 86.6 | 24.2 | 12.2 | 55.2 | 25.3 |
| With any procedure | 75 758 | 2.7 | 26 143 | 34.5 | 42.7 | 35.8 | 29.6 | 64.5 | 91.6 | 24.8 | 49.5 | 56.4 | 27.0 |
| Procedures | |||||||||||||
| CABG | 43 441 | 1.5 | 23 059 | 53.1 | 50.2 | 34.6 | 13.5 | 51.0 | 90.0 | 25.9 | 11.4 | 60.5 | 29.6 |
| With AMI | 10 251 | 0.4 | 4708 | 45.9 | 51.2 | 36.2 | 14.1 | 49.9 | 88.9 | 25.9 | 11.6 | 61.0 | 29.7 |
| No AMI | 33 190 | 1.2 | 18 351 | 55.3 | 49.9 | 34.2 | 13.3 | 51.3 | 90.2 | 25.9 | 11.4 | 60.4 | 29.6 |
| PCI | 120 665 | 4.3 | 33 836 | 28.0 | 41.5 | 38.1 | 33.7 | 68.0 | 91.2 | 24.0 | 12.4 | 53.8 | 25.5 |
| With AMI | 63 249 | 2.2 | 20 577 | 32.5 | 40.1 | 35.7 | 33.8 | 68.6 | 92.3 | 24.5 | 12.2 | 55.2 | 26.3 |
| No AMI | 57 416 | 2.0 | 13 259 | 23.1 | 43.6 | 41.9 | 33.5 | 65.9 | 89.4 | 23.2 | 12.7 | 51.6 | 24.1 |
| Heart valve procedure | 40 614 | 1.4 | 15 117 | 37.2 | 52.4 | 37.2 | 15.9 | 48.7 | 88.2 | 24.8 | 11.7 | 56.7 | 26.0 |
| With AMI | 300 | <0.1 | 77 | 25.7 | 57.2 | 40.9 | 16.9 | 42.9 | 85.7 | 24.0 | 12.0 | 54.5 | 26.0 |
| No AMI | 40 314 | 1.4 | 15 040 | 37.3 | 52.4 | 37.2 | 15.9 | 48.8 | 88.2 | 24.8 | 11.7 | 56.8 | 26.0 |
| Heart transplant† | 525 | <0.1 | 201 | 38.3 | 65.9 | 50.4 | 17.4 | 38.8 | 75.6 | 24.5 | 12.0 | 54.2 | 23.9 |
| Combination procedure | 14 027 | 0.5 | 6622 | 47.2 | 54.1 | 36.6 | 11.2 | 45.6 | 88.0 | 26.1 | 11.2 | 60.7 | 29.0 |
| With AMI | 1957 | 0.1 | 781 | 39.9 | 53.6 | 37.3 | 13.8 | 45.5 | 88.3 | 25.6 | 11.8 | 59.9 | 26.9 |
| No AMI | 12 070 | 0.4 | 5841 | 48.4 | 54.2 | 36.5 | 10.8 | 45.6 | 87.9 | 26.1 | 11.2 | 60.8 | 29.3 |
| CABG and heart valve‡ | 11 495 | 0.5 | 5600 | 48.7 | 54.3 | 36.3 | 10.6 | 45.3 | 87.8 | 26.3 | 11.1 | 61.3 | 29.4 |
AMI indicates acute myocardial infarction; CABG, coronary artery bypass graft; CR, cardiac rehabilitation; and PCI, percutaneous coronary intervention.
Eligible conditions/procedures that occurred in combination had to occur within 21 days of each other.
With or without AMI (collapsed due to small cell sizes); includes both heart and heart-lung transplants.
Both a CABG and heart valve procedure were performed within the first 21 days of the initial qualifying event with or without an AMI occurring
Among beneficiaries identified as only having a secondary CR-qualifying event type, 141 642 were identified as having stable angina and 362 282 as having a heart failure-related qualifying condition/event (totals are not mutually exclusive; Table 4). CR participation was low for both (stable angina: 7.1%; heart failure: 2.9%). For heart failure, participation rates were 2.7% for those identified by diagnosis codes, 6.5% for beneficiaries who had a biventricular pacemaker procedure, and 41.8% for those with a ventricular assist device procedure. Both heart failure procedure groups had significant delays between the procedure date and CR initiation (mean days [SD]: 96.3 [65.3] and 139.8 [74.8], respectively). Completion rates were 22.4% for beneficiaries with stable angina, 19.1% for those with heart failure by diagnosis code, 23.3% for those with biventricular pacemaker procedures, and 32.5% for those with ventricular assist device procedures.
Table 4.
Cardiac Rehabilitation Eligibility, Participation, Timely Initiation, and Utilization Among Medicare Fee-for-Service Beneficiaries Aged ≥65 Years Who Had Secondary Qualifying Event Type, 2016–2017
| Eligible Condition/Procedure* | CR Eligible | CR Participation Among Eligible | Days From Event to CR Participation | Sessions Used Among Participants | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Rate/ 1000 | N | % | Mean No. of Days | SD | ≤21 days, % | ≤42 Days, % | ≤90 Days, % | Mean No. of Sessions | SD | ≥25 Sessions, % | ≥36 Sessions, % | |
| Stable angina | 141 642 | 5.0 | 10 065 | 7.1 | NA | NA | NA | NA | NA | 22.4 | 13.4 | 48.5 | 22.4 |
| Heart failure, overall | 362 282 | 12.9 | 10 345 | 2.9 | NA | NA | NA | NA | NA | 21.7 | 13.6 | 46.7 | 19.8 |
| Diagnosis based | 352 883 | 12.5 | 9536 | 2.7 | NA | NA | NA | NA | NA | 21.4 | 13.5 | 46.0 | 19.1 |
| Procedure based | 9399 | 0.3 | 809 | 8.6 | 109.3 | 71.1 | 6.7 | 18.3 | 48.9 | 24.1 | 13.8 | 52.9 | 26.0 |
| VAD | 562 | <0.1 | 235 | 41.8 | 139.8 | 74.8 | 5.3 | 11.0 | 29.8 | 27.8 | 15.0 | 61.0 | 32.5 |
| BiV pacer | 8837 | 0.3 | 574 | 6.5 | 96.3 | 65.3 | 7.3 | 21.4 | 57.0 | 22.6 | 13.0 | 49.5 | 23.3 |
BiV pacer indicates biventricular pacemaker; CR, cardiac rehabilitation; NA, not applicable; and VAD, (implantable) ventricular assist device.
The stable angina and heart failure categories are not mutually exclusive.
DISCUSSION
Based on the findings of this study among Medicare FFS beneficiaries aged ≥65 years, considerable gains will be required to achieve the national CR participation goal of ≥70% among eligible patients.13 Overall, approximately one-fourth (24.4%) of the 366 000 Medicare FFS beneficiaries identified as having a primary qualifying event in 2016 participated in outpatient CR, with important disparities observed by age, sex, and race/ethnicity. There was also considerable variation by qualifying event type and geography. Moreover, among the almost 90 000 beneficiaries who participated in CR, only 24.3% initiated in a timely manner and only 26.9% completed a full course. The low participation and completion rates observed in this study translate to upwards of 7 million missed opportunities to potentially improve health outcomes had 70% of eligible beneficiaries participated in CR and completed 36 sessions.
Previous reports have described multiple factors potentially responsible for the disparities in CR use observed in this study. For example, inadequate CR education and referral and competing demands, such as caregiver responsibilities, have been identified as significant factors leading to women having lower CR use compared to men.16,17,24 In this study—even after adjustment for age and other covariates—women were 9% less likely than men to participate in CR and were 13% less likely to complete CR after initiation. The degree of disparity between the sexes increased with age and varied by race/ethnicity, with the greatest difference occurring between Asian men and women. Furthermore, as observed in other studies,16,25 participation rates varied considerably by race-ethnicity, with Hispanics and non-Hispanic blacks being 37% and 30% less likely to participate in CR compared with non-Hispanic whites, respectively, which may be a result of them having greater risk for receiving inadequate CR education and referral and experiencing financial barriers.26 In our study, Medicare beneficiaries were responsible for around 20% of cost sharing for CR services, which, on average, would require $828 in copays for a full course of 36 sessions. This amount, in addition to ancillary costs associated with transportation, missed employment, or arranging for alternative caregiving for family members, could serve as financial barriers for CR use, especially among beneficiaries without supplemental insurance and with low socioeconomic status.15,27
We observed an important paradox pertaining to the relationship between comorbidity status and CR eligibility and participation. Specifically, eligibility rates were highest among beneficiaries with the greatest number of comorbidities; however, participation rates were simultaneously lowest among these same groups. This highlights an important opportunity because over half of CR-eligible beneficiaries had ≥5 comorbidities. While the care beneficiaries seek and receive can be influenced by the number, types, and characteristics of the comorbidities they have,28 use of CR and its multidisciplinary approach could confer benefits for the management of their comorbid conditions in addition to decreasing their cardiovascular disease risk. For example, CR use has been shown to improve renal function,29 which, in and of itself, can place those who have had an AMI at lower risk for having another event.30 Over 60% of the CR-eligible beneficiaries had chronic kidney disease—a condition responsible for a considerable amount of Medicare spending31—but only 20% participated in CR. Improving CR use among this population could improve both renal and cardiovascular health and decrease healthcare costs.
Two unique findings presented in this article are the comparison of CR utilization measures stratified by qualifying event type and by HRR. There was around an 8-fold difference in CR participation observed across primary qualifying event types. Participation was highest among beneficiaries who had a cardiac procedure-based qualifying event and lowest among those who had an AMI-related hospitalization without a procedure. Furthermore, these differences appear to be widening. For example, compared to the findings of Suaya et al17 among Medicare beneficiaries in 1997, our study found that CR participation increased among beneficiaries who had an AMI with CABG from 20.9% (Suaya et al) to 45.9% (our study), CABG alone from 31.0% to 55.3%, and AMI with percutaneous coronary intervention from 20.9% to 32.5%. However, participation decreased among beneficiaries who had an AMI with no accompanying cardiac procedure from 11.1% to 7.1%. In addition, we observed that CR use among beneficiaries with non-procedure-related secondary qualifying events was low. For example, although CR referral rates among beneficiaries with heart failure are reportedly increasing,32 we found that only 2.7% of beneficiaries with heart failure as their CR-qualifying condition used CR. Much of the variation in participation observed across primary and secondary qualifying event types is likely unwarranted, as CR has been shown to improve health outcomes for each type.1–4,10,11
In addition, depicting the CR measures by HRR provides a more granular understanding of the geographic variation described in other studies14,17 and may allow groups such as hospitals and CR programs to better appreciate the CR-related needs of the Medicare population within their healthcare market. While eligibility rates follow similar established patterns for the greatest heart disease burden occurring in the southeastern United States and throughout Appalachia,32 HRR-level rates for the CR measures described in this study followed interesting patterns. Most notably, HRRs in the Southeast and Appalachia tended to have the lowest participation but the highest completion. Conversely, HRRs in the Midwest tended to have the highest participation, but the lowest completion. While additional work is needed to better understand these findings, it has been suggested that much of the regional variation in CR use can be addressed by hospitals and community-based practices integrating systematic CR referrals and other pro-CR processes within standardized treatment protocols, improving the capacity within existing CR programs, and addressing shortages in available programs, especially in rural areas.33–36 One strategy for addressing shortages in CR program availability could be to increase the use of home-based CR or tele-CR, modes of providing CR that achieve similar health outcomes as those attained using center-based CR.37,38 However, health insurance coverage for receiving these types of services are currently limited, including for Medicare FFS beneficiaries.10,11
Recent activities at the national level could help support health systems in working with eligible patients to initiate and complete CR. In addition to the Collaborative’s road map,13 the Centers for Disease Control and Prevention and the American Association of Cardiovascular and Pulmonary Rehabilitation released the Million Hearts Cardiac Rehabilitation Change Package, a menu of options from which hospital quality improvement teams and CR program staff can select specific interventions and strategies to improve CR referral, enrollment, participation, and adherence.39 Examples include using an inpatient CR liaison to schedule eligible patients before hospital discharge40; striving to establish first CR visits within 21 days of hospital discharge regardless of qualifying event type, which should decrease the variation in timely initiation observed in this study21,41; offering an accelerated CR program option for select patients42; and using text messaging and mobile applications to engage with patients and track participation.43 Finally, the systematic collection and reporting of the measures reported in this study (an adapted version of this study’s methodology is available for application among other health insurance plan members or patient populations44) and the clinical performance and quality measures that were recently updated and expanded by the American College of Cardiology and American Heart Association are important for quality improvement efforts.21,45 Their use may be key in improving and minimizing disparities in CR use regionally and nationally.
This study has at least 5 limitations. First, the administrative claims-based definitions used have not been validated through chart review; this likely most greatly affects the definitions used for identifying beneficiaries eligible for CR solely based on heart failure status. Second, despite use of our exclusion criteria, we likely were unable to exclude all beneficiaries for whom CR is not appropriate and thus we potentially underestimate participation rates. Third, we were unable to assess rates of CR referral using the available administrative data; receiving a referral is an integral step for promoting CR use.40 Fourth, this study was restricted to assessing CR use among older patients with Medicare FFS coverage; therefore, it may not be generalizable to Medicare Advantage members or to younger patients who may have different CR use rates and require different types of support to initiate and complete CR.12,15 Fifth, we may not have adequately controlled for all confounders in our analyses. This includes not controlling for the potential effect of CR site availability and accessibility (eg, drive-time between beneficiaries’ homes and CR sites) on the disparities and geographic variation observed for CR use.46 Future analyses could assess the impact of these factors.
Despite the importance of CR use to improve health outcomes after a qualifying cardiac event, participation and completion remain low among eligible Medicare FFS beneficiaries. Furthermore, disparities and considerable geographic variability persist. A wealth of guidance exists that identifies the evidence-based strategies that can be used to increase CR use. Hospitals, CR programs, and other stakeholders can consider systematically integrating these strategies into their processes and tracking the effects of their implementation using established quality and performance measures. Continued innovation in delivery of services may help meet the needs of the groups most underserved, as well as to increase capacity to provide care for all those who qualify. The findings in this article and future analyses can be used to assess the impact these collective efforts have on achieving national CR utilization goals.
Supplementary Material
WHAT IS KNOWN?
Outpatient cardiac rehabilitation is a multidisciplinary, evidence-based intervention shown to improve health outcomes and quality of life when used among patients who have had a qualifying heart disease event or procedure.
Historically, participation in cardiac rehabilitation among eligible patients and completion of 36 or more sessions among those who initiate it has been low, with considerable disparities observed by geography and patient characteristics.
WHAT THE STUDY ADDS?
In 2016, approximately one-fourth (24.4%) of the 366 000 Medicare fee-for-service beneficiaries eligible for outpatient cardiac rehabilitation participated, and among those who participated, only 24.3% initiated within 21 days and 26.9% completed a full course of 36 or more sessions.
The low participation and completion rates observed in this study translate to upwards of 7 million missed opportunities to potentially improve health outcomes had 70% of eligible beneficiaries participated in cardiac rehabilitation and completed 36 sessions.
Considerable gains are required to achieve the national goal established by the Million Hearts Cardiac Rehabilitation Collaborative of ≥70% participation among eligible patients and to overcome the disparities and geographic variation by hospital referral region observed for cardiac rehabilitation use.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Medicare & Medicaid Services or the Centers for Disease Control and Prevention.
Footnotes
Disclosures
None.
The Data Supplement is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCOUTCOMES.119.005902.
Contributor Information
Matthew D. Ritchey, Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta, GA.
Sha Maresh, Center for Medicare and Medicaid Innovation, Centers for Medicare and Medicaid Services, Baltimore, MD.
Jessica McNeely, Center for Medicare and Medicaid Innovation, Centers for Medicare and Medicaid Services, Baltimore, MD.
Thomas Shaffer, Center for Medicare and Medicaid Innovation, Centers for Medicare and Medicaid Services, Baltimore, MD.
Sandra L. Jackson, Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta, GA.
Steven J. Keteyian, Division of Cardiovascular Medicine, Henry Ford Hospital, Detroit, Michigan.
Clinton A. Brawner, Division of Cardiovascular Medicine, Henry Ford Hospital, Detroit, Michigan.
Mary A. Whooley, School of Medicine, University of California, San Francisco.
Tiffany Chang, Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta, GA; IHRC, Inc..
Haley Stolp, Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta, GA; IHRC, Inc..
Linda Schieb, Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta, GA.
Janet Wright, Office of the Surgeon General, US Department of Health and Human Services, Washington, DC.
REFERENCES
- 1.Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;CD001800. doi: 10.1002/14651858. CD001800.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJ, Dalal H, Lough F, Rees K, Singh S. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014;CD003331. doi: 10.1002/14651858.CD003331.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sibilitz KL, Berg SK, Tang LH, Risom SS, Gluud C, Lindschou J, Kober L, Hassager C, Taylor RS, Zwisler AD. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev. 2016;CD010876. doi: 10.1002/14651858.CD010876.pub2 [DOI] [PubMed] [Google Scholar]
- 4.Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med. 2001;345:892–902. doi: 10.1056/NEJMra001529 [DOI] [PubMed] [Google Scholar]
- 5.Suaya JA, Stason WB, Ades PA, Normand SL, Shepard DS. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33. doi: 10.1016/j.jacc.2009.01.078 [DOI] [PubMed] [Google Scholar]
- 6.Martin BJ, Hauer T, Arena R, Austford LD, Galbraith PD, Lewin AM, Knudtson ML, Ghali WA, Stone JA, Aggarwal SG. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation. 2012;126:677–687. doi: 10.1161/CIRCULATIONAHA.111.066738 [DOI] [PubMed] [Google Scholar]
- 7.Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121:63–70. doi: 10.1161/CIRCULATIONAHA.109.876383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–e239. doi: 10.1016/j.jacc.2013.05.019 [DOI] [PubMed] [Google Scholar]
- 9.Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW, Lloyd-Jones DM, Minissian M, Mosca L, Peterson ED, Sacco RL, Spertus J, Stein JH, Taubert KA. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58:2432–2446. doi: 10.1016/j.jacc.2011.10.824 [DOI] [PubMed] [Google Scholar]
- 10.Centers for Medicare and Medicaid Services. Decision Memo for Cardiac Rehabilitation Programs. CAG-00089R. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=164&NcaName=Cardiac+Rehabilitation+Programs&DocID=CAG-00089R. 2006. Accessed November 11, 2019.
- 11.Centers for Medicare and Medicaid Services. Decision Memo for Cardiac Rehabilitation Programs - Chronic Heart Failure. CAG-00437N. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=270. 2014. Accessed November 11, 2019.
- 12.Gaalema DE, Savage PD, Rengo JL, Cutler AY, Elliott RJ, Priest JS, Higgins ST, Ades PA. Patient characteristics predictive of cardiac rehabilitation adherence. J Cardiopulm Rehabil Prev. 2017;37:103–110. doi: 10.1097/HCR.0000000000000225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ades PA, Keteyian SJ, Wright JS, Hamm LF, Lui K, Newlin K, Shepard DS, Thomas RJ. Increasing cardiac rehabilitation participation from 20% to 70%: a road map from the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017;92:234–242. doi: 10.1016/j.mayocp.2016.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beatty AL, Truong M, Schopfer DW, Shen H, Bachmann JM, Whooley MA. Geographic variation in cardiac rehabilitation participation in Medicare and Veterans Affairs populations: opportunity for improvement. Circulation. 2018;137:1899–1908. doi: 10.1161/CIRCULATIONAHA.117.029471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bachmann JM, Huang S, Gupta DK, Lipworth L, Mumma MT, Blot WJ, Akwo EA, Kripalani S, Whooley MA, Wang TJ, Freiberg MS. Association of neighborhood socioeconomic context with participation in cardiac rehabilitation. J Am Heart Assoc. 2017;6:e006260. doi: 10.1161/JAHA.117.006260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fang J, Ayala C, Luncheon C, Ritchey M, Loustalot F. Use of outpatient cardiac rehabilitation among heart attack survivors - 20 states and the district of Columbia, 2013 and four states, 2015. MMWR Morb Mortal Wkly Rep. 2017;66:869–873. doi: 10.15585/mmwr.mm6633a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466 [DOI] [PubMed] [Google Scholar]
- 18.Park LG, Schopfer DW, Zhang N, Shen H, Whooley MA. Participation in cardiac rehabilitation among patients with heart failure. J Card Fail. 2017;23:427–431. doi: 10.1016/j.cardfail.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frieden TR, Berwick DM. The “Million Hearts” initiative–preventing heart attacks and strokes. N Engl J Med. 2011;365:e27. doi: 10.1056/NEJMp1110421 [DOI] [PubMed] [Google Scholar]
- 20.Ritchey MD, Loustalot F, Wall HK, Steiner CA, Gillespie C, George MG, Wright JS. Million Hearts: description of the national surveillance and modeling methodology used to monitor the number of cardiovascular events prevented during 2012–2016. J Am Heart Assoc. 2017;6:e006021. doi: 10.1161/JAHA.117.006021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomas RJ, Balady G, Banka G, Beckie TM, Chiu J, Gokak S, Ho PM, Keteyian SJ, King M, Lui K, Pack Q, Sanderson BK, Wang TY. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2018;11:e000037. doi: 10.1161/HCQ.0000000000000037 [DOI] [PubMed] [Google Scholar]
- 22.U.S. Centers for Medicare and Medicaid Services. Chronic Conditions Data Warehouse Condition Algorithms. https://www.ccwdata.org/web/guest/condition-categories. 2019. Accessed November 11, 2019.
- 23.Tamhane AR, Westfall AO, Burkholder GA, Cutter GR. Prevalence odds ratio versus prevalence ratio: choice comes with consequences. Stat Med. 2016;35:5730–5735. doi: 10.1002/sim.7059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Supervia M, Medina-Inojosa JR, Yeung C, Lopez-Jimenez F, Squires RW, Perez-Terzic CM, Brewer LC, Leth SE, Thomas RJ. Cardiac rehabilitation for women: a systematic review of barriers and solutions. Mayo Clin Proc. 2017;92:565–577. doi: 10.1016/j.mayocp.2017.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prince DZ, Sobolev M, Gao J, Taub CC. Racial disparities in cardiac rehabilitation initiation and the effect on survival. PM R. 2014;6:486–492. doi: 10.1016/j.pmrj.2013.11.016 [DOI] [PubMed] [Google Scholar]
- 26.Mochari H, Lee JR, Kligfield P, Mosca L. Ethnic differences in barriers and referral to cardiac rehabilitation among women hospitalized with coronary heart disease. Prev Cardiol. 2006;9:8–13. doi: 10.1111/j.1520-037x.2005.3703.x [DOI] [PubMed] [Google Scholar]
- 27.Pack QR, Squires RW, Valdez-Lowe C, Mansour M, Thomas RJ, Keteyian SJ. Employment status and participation in cardiac rehabilitation: does encouraging earlier enrollment improve attendance? J Cardiopulm Rehabil Prev. 2015;35:390–398. doi: 10.1097/HCR.0000000000000140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zulman DM, Asch SM, Martins SB, Kerr EA, Hoffman BB, Goldstein MK. Quality of care for patients with multiple chronic conditions: the role of comorbidity interrelatedness. J Gen Intern Med. 2014;29:529–537. doi: 10.1007/s11606-013-2616-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Takaya Y, Kumasaka R, Arakawa T, Ohara T, Nakanishi M, Noguchi T, Yanase M, Takaki H, Kawano Y, Goto Y. Impact of cardiac rehabilitation on renal function in patients with and without chronic kidney disease after acute myocardial infarction. Circ J. 2014;78:377–384. doi: 10.1253/circj.cj-13-0779 [DOI] [PubMed] [Google Scholar]
- 30.Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, White HD, Nordlander R, Maggioni A, Dickstein K, Zelenkofske S, Leimberger JD, Califf RM, Pfeffer MA. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295. doi: 10.1056/NEJMoa041365 [DOI] [PubMed] [Google Scholar]
- 31.Honeycutt AA, Segel JE, Zhuo X, Hoerger TJ, Imai K, Williams D. Medical costs of CKD in the Medicare population. J Am Soc Nephrol. 2013;24:1478–1483. doi: 10.1681/ASN.2012040392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vaughan AS, Ritchey MD, Hannan J, Kramer MR, Casper M. Widespread recent increases in county-level heart disease mortality across age groups. Ann Epidemiol. 2017;27:796–800. doi: 10.1016/j.annepidem.2017.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gurewich D, Prottas J, Bhalotra S, Suaya JA, Shepard DS. System-level factors and use of cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2008;28:380–385. doi: 10.1097/HCR.0b013e31818c3b5b [DOI] [PubMed] [Google Scholar]
- 34.Pack QR, Squires RW, Lopez-Jimenez F, Lichtman SW, Rodriguez-Escudero JP, Zysek VN, Thomas RJ. The current and potential capacity for cardiac rehabilitation utilization in the United States. J Cardiopulm Rehabil Prev. 2014;34:318–326. doi: 10.1097/HCR.0000000000000076 [DOI] [PubMed] [Google Scholar]
- 35.Bachmann JM, Klint ZW, Jagoda AM, McNatt JK, Abney LR, Huang S, Liddle DG, Frontera WR, Freiberg MS. Group enrollment and open gym format decreases cardiac rehabilitation wait times. J Cardiopulm Rehabil Prev. 2017;37:322–328. doi: 10.1097/HCR.0000000000000255 [DOI] [PubMed] [Google Scholar]
- 36.Valencia HE, Savage PD, Ades PA. Cardiac rehabilitation participation in underserved populations. Minorities, low socioeconomic, and rural residents. J Cardiopulm Rehabil Prev. 2011;31:203–210. doi: 10.1097/HCR.0b013e318220a7da [DOI] [PubMed] [Google Scholar]
- 37.Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;102:1183–1192. doi: 10.1136/heartjnl-2015-308966 [DOI] [PubMed] [Google Scholar]
- 38.Anderson L, Sharp GA, Norton RJ, Dalal H, Dean SG, Jolly K, Cowie A, Zawada A, Taylor RS. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6:CD007130. doi: 10.1002/14651858.CD007130.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention (CDC). Cardiac Rehabilitation Change Package. Atlanta, GA: CDC, US Dept of Health and Human Services; 2018. [Google Scholar]
- 40.Grace SL, Russell KL, Reid RD, Oh P, Anand S, Rush J, Williamson K, Gupta M, Alter DA, Stewart DE; Cardiac Rehabilitation Care Continuity Through Automatic Referral Evaluation (CRCARE) Investigators. Effect of cardiac rehabilitation referral strategies on utilization rates: a prospective, controlled study. Arch Intern Med. 2011;171:235–241. doi: 10.1001/archinternmed.2010.501 [DOI] [PubMed] [Google Scholar]
- 41.Pack QR, Mansour M, Barboza JS, Hibner BA, Mahan MG, Ehrman JK, Vanzant MA, Schairer JR, Keteyian SJ. An early appointment to outpatient cardiac rehabilitation at hospital discharge improves attendance at orientation: a randomized, single-blind, controlled trial. Circulation. 2013;127:349–355. doi: 10.1161/CIRCULATIONAHA.112.121996 [DOI] [PubMed] [Google Scholar]
- 42.American Association of Cardiovascular and Pulmonary Rehabilitation. Cardiac rehabilitation enrollment strategy: accelerated use of cardiac rehabilitation. Available at: https://www.aacvpr.org/Portals/0/Million%20Hearts%20Change%20Package/4.24.2018%20Files/EP-30-CRCP-Turn-key-Accelerated-Usage%20of%20CR.pdf?timestamp=1524594116056. Accessed May 7, 2019.
- 43.Lounsbury P, Elokda AS, Gylten D, Arena R, Clarke W, Gordon EEI. Text-messaging program improves outcomes in outpatient cardiovascular rehabilitation. Int J Cardiol Heart Vasc. 2015;7:170–175. doi: 10.1016/j.ijcha.2015.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention (CDC). Million Hearts® Outpatient Cardiac Rehabilitation Use Surveillance Methodology. Atlanta, GA: CDC, US Dept of Health and Human Services; 2019. Available at: https://millionhearts.hhs.gov/files/Cardiac-Rehab-Use-Surveillance-Guidance.pdf. Accessed May 7, 2019. [Google Scholar]
- 45.Pack QR, Squires RW, Lopez-Jimenez F, Lichtman SW, Rodriguez-Escudero JP, Lindenauer PK, Thomas RJ. Participation rates, process monitoring, and quality improvement among cardiac rehabilitation programs in the United States: a national survey. J Cardiopulm Rehabil Prev. 2015;35:173–180. doi: 10.1097/HCR.0000000000000108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ruano-Ravina A, Pena-Gil C, Abu-Assi E, Raposeiras S, van ‘t Hof A, Meindersma E, Bossano Prescott EI, González-Juanatey JR. Participation and adherence to cardiac rehabilitation programs. A systematic review. Int J Cardiol. 2016;223:436–443. doi: 10.1016/j.ijcard.2016.08.120 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.