Abstract
Acute Respiratory Distress Syndrome (ARDS) accounts for 10% of all intensive care unit admissions and mortality remains exceedingly high ranging from 35 to 46%. Prone positioning has demonstrated benefit as a treatment option in the moderate to severe subset of ARDS patients. Referral to an extracorporeal membrane oxygenation (ECMO) center remains the standard of care for patients with refractory hypoxemia. Transfer of these already critically ill patients is high risk but there is a possibility for improved oxygenation on transport with prone positioning. Currently there is limited data on the safe transportation of prone patients to ECMO centers. Herein we describe a case of an ARDS patient safely transported prone with minimal ad hoc adjustments to standard ambulance transport.
Keywords: Critical care, Extracorporeal membrane oxygenation, Prone position, Respiratory distress syndrome, Referral and consultation
1. Introduction
Acute Respiratory Distress Syndrome (ARDS) accounts for approximately 10% of all intensive care unit admissions and globally affects 3 million patients annually [1]. Despite large research efforts, mortality remains exceedingly high ranging from 35 to 46% [2]. Prone positioning improves outcomes in patients with moderate/severe ARDS, defined as PaO2/FiO2 below 150 mm Hg [3]. For patients with refractory hypoxemia, extracorporeal membrane oxygenation (ECMO) has become increasingly utilized. Transport to an expert ECMO center alone (with or without cannulation) has been demonstrated to improve outcomes [4,5]. ECMO centers are comprised of highly specialized health care staff and resources and therefore have led to the development of regional centers rather than being available at community hospitals [4,5]. For patients who improve in the prone position it is advantageous to maintain this position during transfer to an ECMO center. Prone positioning has the potential for increased adverse events in transport due to lack of access to IV lines, endotracheal tube and the anterior chest for standard cardiopulmonary resuscitation [9]. There is limited data on the safety of transporting patients in the prone position. Herein we present a case of a patient safely transported in the prone position using minimal ad hoc adjustments to standard ambulance transport.
2. Case
A 54-year-old male (BMI: 30 kg/m2) with past medical history of only rheumatoid arthritis treated with plaquenil presented to a local emergency department (ED) with cough, fever and body aches for 7 days. At presentation the patient's vital signs were: heart rate 109 bpm, respiratory rate 20 breaths/min, blood pressure 134/74 mmHg, oxygen saturation of 92% and a temperature of 38.2 °C. A chest CT demonstrated bibasilar alveolar consolidations. The patient was given escalating treatment for refractory hypoxia including high-flow nasal cannula, antibiotics and a course of pulse steroids (Methylprednisolone 1 g for 3 days). The patient was subsequently intubated due to worsening hypoxemia and supported with a lung protective mechanical ventilation strategy. The ECMO team was contacted after the referring center felt their trial of prone positioning showed no improvement in gas exchange (PaO2/FiO2 ratio of 50).
The patient was assessed by the ECMO team with vital signs as follows: heart rate 140 bpm, systolic blood pressure 123 mmHg without vasopressors, and oxygen saturation of 92%. The patient was mechanically ventilated with a driving pressure of 14 cmH20, positive end expiratory pressure (PEEP) of 14cmH2 and 100% FiO2. Prone positioning was again attempted after further sedation and paralysis. Once prone the patient's PEEP was able to be reduced to 10 cmH20 and driving pressure to 11 cmH2O while maintaining volumes of 400 cc (4.32 ml/kg). Oxygen saturations improved to 94%. The decision was then made to transfer the patient prone.
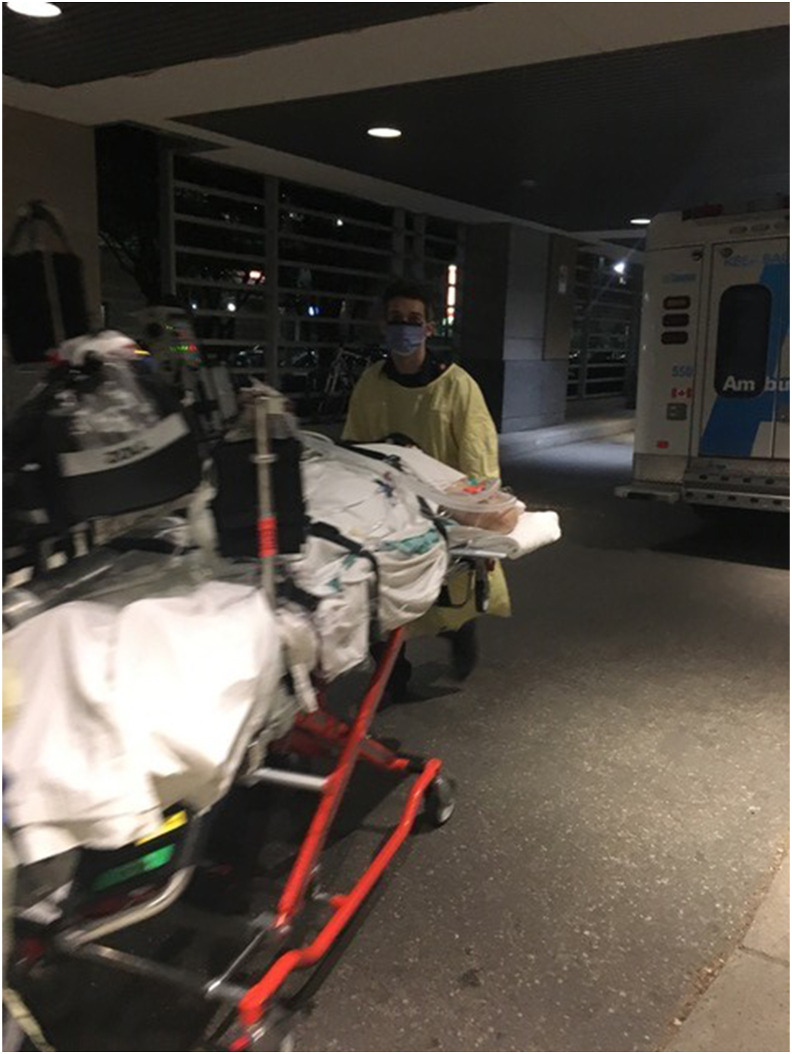
The transport team consisted of two critical care physicians, a perfusionist and two critical care paramedics. To facilitate the maintenance of the patient in prone position on the ambulance stretcher, the paramedic team was able to fashion side rests from an available spine board placed perpendicular to the stretcher (Fig. 1 ). The side rests allowed the patient to be placed in a swimmer's position to allow for access to IV lines and help maintain the patient's infusions. Careful consideration was given to maintaining endotracheal tube position and eye protection. The patient was transported 14.6 km by ground ambulance and the transfer was well tolerated without adverse events. The patient's hemodynamics and saturation were stable throughout. The patient adequately improved with prone positioning initially but required ECMO cannulation on day 7 due to worsening hypoxemia. The patient eventually improved with ECMO and was decannulated 7 days after initiation and transferred 14 days later to his home hospital.
Fig. 1.
Transportation of patient in prone position.
3. Discussion
Our case demonstrates the ease and safety of transporting patients in the prone position. The team responsible for the transport had no specialized equipment for transporting patients prone but were successful with minor adjustments.
Although there have been a number of cases of prone transfers both by land and air demonstrating safety and reliability there has been little adoption in general practice [[6], [7], [8]]. Hersey et al., developed a checklist for prone transportation as a safety mechanism and described their technique of positioning the patient for transport [9]. Unfortunately, further studies need to be done to determine the efficacy of the checklist. Although there have not been any reported adverse events with prone transport – only a small number of cases have been reported [[6], [7], [8], [9], [10]]. We believe our case is unique in the use of an ad hoc method in transporting a patient prone safely and demonstrates the ease with which it can be done. Given the COVID-19 pandemic and increased incidence of severe ARDS, we hope that the ease of our method will allow more practitioners to consider prone transportation for these critically ill patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author statement
Anton Nikouline: Investigation, Writing – original draft, Writing – review & editing. John T. Granton: Writing – review & editing, Supervision. Lorenzo Del Sorbo: Conceptualization, Writing – review & editing, Supervision.
Declaration of competing interest
None.
References
- 1.Ranieri V.M., Rubenfeld G.D., Thompson B.T., et al. ARDS definition task force. Acute respiratory distress syndrome: the berlin definition. J. Am. Med. Assoc. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 2.Bellani G., Laffey J.G., Pham T., et al. LUNG SAFE Investigators; ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. J. Am. Med. Assoc. 2016;315(8):788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 3.Munshi L., Del Sorbo L., Adhikari N.K., et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc. 2017 Oct;14(Supplement 4):S280–S288. doi: 10.1513/AnnalsATS.201704-343OT. [DOI] [PubMed] [Google Scholar]
- 4.Peek G.J., Mugford M., Tiruvoipati R., et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009 Oct 17;374(9698):1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 5.Mendes P.V., de Albuquerque Gallo C., Besen B.A., et al. Transportation of patients on extracorporeal membrane oxygenation: a tertiary medical center experience and systematic review of the literature. Ann. Intensive Care. 2017 Dec;7(1):14. doi: 10.1186/s13613-016-0232-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uusaro A., Parviainen I., Takala J., et al. Safe long-distance interhospital ground transfer of critically ill patients with acute severe unstable respiratory and circulatory failure. Intensive Care Med. 2002 Aug 1;28(8):1122–1125. doi: 10.1007/s00134-002-1348-9. [DOI] [PubMed] [Google Scholar]
- 7.Flabouris A., Schoettker P., Garner A. ARDS with severe hypoxia—aeromedical transportation during prone ventilation. Anaesth. Intensive Care. 2003 Dec;31(6):675–678. doi: 10.1177/0310057X0303100613. [DOI] [PubMed] [Google Scholar]
- 8.DellaVolpe J.D., Lovett J., Martin-Gill C., et al. Transport of mechanically ventilated patients in the prone position. Prehosp. Emerg. Care. 2016 Sep 2;20(5):643–647. doi: 10.3109/10903127.2016.1162888. [DOI] [PubMed] [Google Scholar]
- 9.Hersey D., Witter T., Kovacs G. Transport of a prone position acute respiratory distress syndrome patient. Air Med. J. 2018 May 1;37(3):206–210. doi: 10.1016/j.amj.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Cornejo R., Ugalde D., Llanos O., et al. Prone position ventilation used during a transfer as a bridge to ecmo therapy in hantavirus-induced severe cardiopulmonary syndrome. Case Rep Crit Care. 2013;2013 doi: 10.1155/2013/415851. [DOI] [PMC free article] [PubMed] [Google Scholar]