Abstract
Background
The burden of life-threatening conditions requiring intensive care units has grown substantially in low-income countries related to an emerging pandemic, urbanization, and hospital expansion. The rate of ICU mortality varied from region to region in Ethiopia. However, the body of evidence on ICU mortality and its predictors is uncertain. This study was designed to investigate the pattern of disease and predictors of mortality in Southern Ethiopia.
Methods
After obtaining ethical clearance from the Institutional Review Board (IRB), a multi-center cohort study was conducted among three teaching referral hospital ICUs in Ethiopia from June 2018 to May 2020. Five hundred and seventeen Adult ICU patients were selected. Data were entered in Statistical Package for Social Sciences version 22 and STATA version 16 for analysis. Descriptive statistics were run to see the overall distribution of the variables. Chi-square test and odds ratio were determined to identify the association between independent and dependent variables. Multivariate analysis was conducted to control possible confounders and identify independent predictors of ICU mortality.
Results
The mean (±SD) of the patients admitted in ICU was 34.25(±5.25). The overall ICU mortality rate was 46.8%. The study identified different independent predictors of mortality. Patients with cardiac arrest were approximately 12 times more likely to die as compared to those who didn't, AOR = 11.9(95% CI:6.1 to 23.2).
Conclusion
The overall mortality rate in ICU was very high as compared to other studies in Ethiopia as well as globally which entails a rigorous activity from different stakeholders.
Keywords: Mortality, Intensive care unit, Hospital, Predictor
Abbreviations: APACHE, Acute Physiologic and Chronic Health Evaluation; AOR, Adjusted Odds Ratio; ACLS, advanced cardiac life support; ARDS, Acute Respiratory Distress Syndrome; BMI, Body Mass Index; CI, Confidence Interval; CT, Computerized Tomography; DURH, Dilla University referral hospital; GCS, Glasgow Coma Scale; HURH, Hawassa university referral hospital; ICU, Intensive Care Unit; IRB, Institutional Review Board; IQR, Inter Quartile e Range; LOS, Length of Stay; SAPS, Simplified Acute Physiology Score; SD, Standard Deviation; SOFA, Sequential Organ Failure Assessment; STROBE, Strengthening the Reporting of Observational Studies in Epidemiology; WURH, Wolaita Sodo referral hospital
Highlights
-
•
The incidence rate of mortality among ICU patients was approximately fifty percent.
-
•
The main causes of ICU mortality were Trauma, Congestive heart failure, ARDS, and stroke respectively.
-
•
The cardiovascular and respiratory disorders were the commonest comorbidity among ICU patients.
-
•
All patients admitted to ICU experienced at least one complication during ICU stay.
1. Introduction
The modern intensive care medicine emerged during the Polio epidemics in the 1950s, which was pioneered by a Danish anesthetist, Bjorn Ibsen at the Kommune hospital of Copenhagen in 1953 [1,2].
The Intensive Care Unit (ICU) is a specially staffed, well equipped, separate, and self-contained area of a hospital dedicated to providing aggressive therapy using state-of-the-art technology and both invasive and noninvasive monitoring for critically ill and high-risk patients [[3], [4], [5], [6]].
The burden of life-threatening conditions requiring management in the intensive care unit has grown substantially in the last couple of decades in low and middle-income countries because of an emerging pandemic, motorization, urbanization, and hospital expansion [[7], [8], [9], [10], [11], [12]]. However, the advancement of ICU care is very limited in these countries due to the high cost of infrastructure, training medical staff, failure to incorporate international guidelines for evidence-based care, and availing medical supplies([9,11,[13], [14], [15], [16]]).
Intensive care unit comprises only 10% of hospital bed but it costs more than 30% of acute hospital care which is equivalent to 20% of the hospital budget and this cost becomes higher in a patient with a severe critical illness which hinders the low resource setting to establish intensive care units(3, 17).
Critical ill patients are admitted to ICU for some reasons including but not limited to respiratory failure, severe infectious diseases, multiple trauma and shock, myocardial infarction, heart failure, renal failure, poisoning, postoperative care, and therapeutic [[18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37]].
Evidence showed that the incidence of ICU admission ranged from 1 to 54% globally [17,35,[37], [38], [39], [40]]. The cause of ICU admission is not consistent across the globe and the majority of available evidence showed that cardiovascular and respiratory disorders were the commonest causes of admission in middle and high-income countries accounting for 27–41% of admission [17,35,[37], [38], [39], [40]] while trauma and postoperative care were the main reasons for ICU admission in low-income countries which varied from 10 to 50% [6,37,38,41].
Evidence revealed that the outcomes of patients in ICU is greatly related to different factors including but not limited to the pattern of diseases, the severity of the disease, infrastructure, trained medical staff, nursing care, medical supplies, age of patient, presence of comorbidities and multiorgan failure, pre-hospital and emergency care trauma score, mechanical ventilation, length of ICU stay, complications in ICU, dissemination of antimicrobial-resistant microorganisms and inappropriate or suboptimal use of antibiotics [6,9,18,[24], [25], [26], [27], [28],30,34,36,37,[40], [41], [42], [43], [44], [45], [46], [47], [48]].
The global prevalence of mortality in ICU roughly ranges from 9 to 61%. An international study recruiting 13, 796 participants from Africa, Asia, America, Europe, and Oceania revealed that the prevalence of mortality in ICU was 18.2% [49].
Other evidence from Sub-Saharan Africa showed that mortality in ICU was ranged from 27% to 61% [38,41,50,51]. A systematic review and meta-analysis by Vincent et al. showed that ICU mortality related to septic shock in Europe and North America was 37.3% (95% CI:35.5–43.5%) [52].
The mortality is very high in the low-income country which is as high as 61% as compared to developed countries which varied from 9 to 18% [28,38,41,50,51,53].
The rate of ICU mortality in Ethiopia varied from region to region ranging from 27 to 38% [4,6,28,32,46,53]. However, the pattern of disease and predictors of mortality in the Southern part of Ethiopia is not well investigated. This multicenter observational study was designed to investigate the pattern of disease and predictors of mortality in selected Southern Ethiopia ICUs.
2. Materials and methods
2.1. Protocol and registration
This study was conducted in compliance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies and strengthening the reporting of cohort studies in surgery (STROCSS) [54,55]. The study was registered retrospectively in research registry with Unique Identifier Number (UIN:: researchregistry6641) and available at: https://www.researchregistry.com/browse-the-registry#home/
2.2. Study design and setting
This is a multi-center retrospective Cohort study conducted in three teaching and referral hospitals in Southern Ethiopia; namely, X University referral hospital, Y University referral hospital, and Z referral hospital from June 20, 2018, to May 20, 2020. These teaching and referral hospital are administered by the Federal Ministry of health and education of Ethiopia. The ICUs are providing a similar level of care with almost similar staff profiles, monitoring modalities, ICU infrastructure, medical supplies, and admission patterns. The care of patients in these ICUs is to the minimum standard because of lack of medical supplies (mechanical ventilator, integrated monitors, vasopressor/inotropes, nutritional support), lack of well-trained staff (lack of intensivist, dentition/nutritionist, physiotherapist). Besides, Y University referral hospital and Z University hospital ICUs didn't have Computerized Tomography (CT), portable chest X-ray Machine, Spirometer, and appropriate Biochemical tests.
2.3. Eligibility
The inclusion criteria for this observational study were all adult patients who were 12 years and above admitted to ICUs of the three referral and teaching hospital during the study period. All patients with incomplete data greater than 15% were excluded. The incomplete date in less than five percent of the records was entertained with the assumption of multiple imputations.
2.4. Variables
2.4.1. Dependent variables
The dependent variables were the clinical outcomes in ICU including 30-day mortality, length of ICU stay, the incidence of cardiac arrest, and complications in ICU.
2.4.2. Independent variables
Socio-demographic characteristics (age and gender), causes of admission, presence of comorbid illness, category of admission, the vital sign at admission, intervention during ICU stay were the independent variables.
2.5. Sample size and sampling procedure
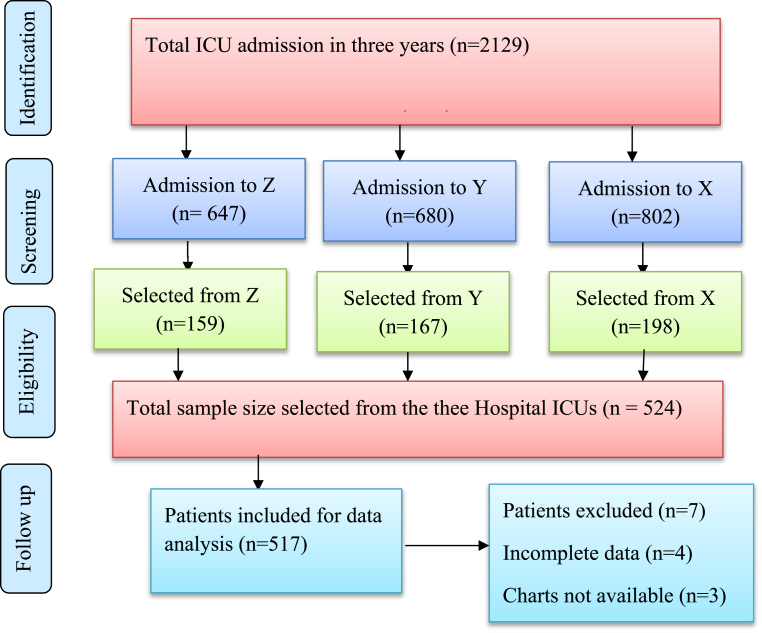
The sample size (n) was determined using a single population proportion formula with the following assumptions: level of confidence (α) was taken as 0.05; Zα/2 = 1.96, a 4.6% margin of error (d = 0.46), and proportion of mortality 46% was taken from a study conducted in Jimma University(46). Therefore, the total sample size was 524 with a 15% contingency for the non-response rate. As shown with a strobe flow diagram (Fig. 1), the total ICU admission in three centers was (N = 2129) patients. The total ICU admission in Z, Y, and X Universities were 647, 680, and 802 respectively. The study populations were taken from each ICU with a proportion allocation formula by dividing the admission in each ICU by the total admission of the three ICUs multiplied by the sample size (n = 524). Z = n1/N * n, Y = n2/N* n, and X = n3/N*n where n1, n2, and n3 were the total admission in Z, Y, and X respectively. Then, the required number of participants were selected with systematic random sampling with a skip interval of (k = 4).
Fig. 1.
Strobe flow chart.
2.6. Data collection procedures
The data was collected by three trained bachelors Anesthetist with standardized questionnaire adapted from previous literature [28,32,36,41,44,49,50,[56], [57], [58]]. A total of 524 patient charts were recruited from 2119 patients admitted in ICU from June 20, 2018, to 2020 in three hospitals with systematic allocation proportion based on the number of patients admitted during the study period (Fig. 1).
The data extraction includes Socio-demographic characteristics (age of the patient, gender, weight, Height, BMI); Admission variables (admission category, causes of category, vital sign at admission; intervention in ICU (mechanical ventilation, vasopressor requirement); complication in ICU (cardiac arrest, infection, aspiration) and outcomes (mortality, length of ICU stay and some mechanical ventilator).
2.7. Data analysis
The data was checked, coded, and entered into Epi-info version 7.0 and imported to SPSS version 22 and STATA version 16 for analysis. Descriptive statistics were summarizing with tables and figures. The categorical variables were reported in Frequency and percentage and the statistical difference was determined by Chi-square and Fisher exact test where appropriate. The numerical data were reported in mean ± SD for symmetric and median (Interquartile range) for asymmetric numeric data. The outlier of the data was checked with standardized residual while Shapiro Wilk tests were employed for the normality test. The multicollinearity among independent variables was checked by the Variance inflation factor and tolerance.
Association of demographic characteristics, admission category, causes of admission, and intervention in ICU, a complication in ICU and mortality in ICU was analyzed by using binary logistic regression. The Model fitness was checked using Hosmer-Lemeshow goodness of fitness test, Pseudo R2, and Pearson chi-square statistics. All Variables that were significant on bivariate analysis at a p-value less than 0.25 were taken to multivariate analysis one after the other to investigate model prediction and independent predictors of the explanatory variables. In multivariate analysis, a p-value of less than 0.05 was considered for the statistical association. The finding of this study was reported in compliance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies [54,55].
2.8. Ethical statement
This study was reviewed and approved by the Institutional Review Board (IRB) of XXXXXXX and was given a reference number (007/19-10). The study was conducted in compliance with the Helsinki declaration for observational studies. A formal letter was written to each University hospital ICU director to get permission to access the patients’ data and all the patient identifiers were kept anonymous.
3. Results
A total of 2119 patients were admitted to the three teaching referral Hospitals’ ICU from June 2018 to May 2020. Five Hundred and twenty-four patients were selected with systematic proportion allocation from three ICUs. Finally, Five hundred and seventeen were included in the analysis, and the rest seven were excluded due to incomplete data.
3.1. Admission characteristics
The mean (±SD) of the patients admitted in ICU was 34.25(±5.25). The majority of patients were in the age range of 19–39 years while the lowest was in the less than 18 years range. Among 517 patients, the majority 274(53%) were female while males accounted for 247(47%).
The majority of Admissions were from the emergency department 223(43.1%) followed by Medical ward 180(34.8%), gynecology/Obstetrics ward 50(9.7%) while the lowest were from operation theatre 47(9.1%) and surgical ward 17(3.3%). The commonest causes of ICU admissions were acute respiratory distress syndrome, Congestive heart failure, and severe pneumonia, stroke, myocardial infarction, and acute kidney injury respectively.
The majority of patients had a respiratory rate greater than twenty breaths per minute while less than twenty-three of patients had respiratory rate less than twelve breaths per minute. Seventy percent of the patients had a pulse rate greater than a hundred beats per minute while only six percent of patients had no palpable pulse at admission. More than half 272(53.2) of patients had a GCS score of less than eight while 197(37.1%) of the patients were hypoxemic (PSO2 less than 90%) at admission.
This study identified different causes of ICU admission among 517 cohorts. The majority causes of ICU admission were Trauma 185(35.5%) followed by others 90(17.4%), ARDS 57(11%), and congestive heart failure 55(10.6%) (Table1).
Table 1.
Admission characteristics of patients admitted to Teaching and Referral Hospitals’ ICUs in Southern Ethiopia, June 2018 to May 2020.
| Characteristics | All admissions (n = 517) | survivors (n = 275) | Non-survivors (n = 242) | P-value |
|---|---|---|---|---|
|
Age range (years) <18 19 to 39 >40 |
102(19.7) 233(45.1) 182(35.2) |
39(35.3) 117(50.2) 86(47.3) |
63(64.7) 116(49.8) 96(52.7) |
>0.05 |
|
Gender Female Male |
274(53.0) 243(47.0) |
149(54.4) 126(51.9) |
125(45.6) 117(48.1) |
>0.05 |
| Admission vital sign Respiratory rate <12 12 to 20 >20 Pulse rate >100 60 to 100 <60 Not palpable Oxygen Saturation (PS02, %) >90 <90 Glasgow coma scale <8 9–12 >12 |
23(4.4) 119(23.0) 375(72.5) 330(63.8) 141(27.3) 13(2.5) 33(6.4) 325(62.9) 197(37.1) 272(53.2) 196(37.9) 46(8.9) |
20(86.9) 42(35.3) 180(48.0) 169(51.2) 36(25.5) 9(69.2) 28(84.8) 184(56.6) 58(29.4) 184(67.6) 51(26.0) 7(15.2) |
3(13.1) 77(64.7) 195(52.0) 161(48.8) 105(74.5) 4(30.8) 5(15.2) 141(43.4) 134(70.6) 91(32.4) 145(74.0) 39(84.8) |
<0.0001** <0.0001** <0.0001** <0.0001** |
| Sources of admission Emergency department Medical ward Surgical ward Gynecology/obstetrics ward Operation Room |
223(43.1) 180(34.8) 17(3.3) 50(9.7) 47(9.1) |
109(48.9) 79(43.9) 8(47.1) 21(42.0) 25(53.2) |
114(51.1) 101(56.1) 9(52.9) 29(58.0) 22(46.8) |
>0.05 |
| Causes of admission Trauma Myocardial infarction Congestive heart failure Septic shock HIV/AIDS ARDS Diabetic ketoacidosis stroke Acute kidney injury Severe Pneumonia Others |
185(35.8) 33(6.4) 55(10.6) 30(5.8) 18(3.5) 57(11.0) 19(3.7) 40(7.7) 31(6.0) 45(8.7) 90(17.4) |
121(65.4) 10(30.3) 21(38.2) 22(73.3) 8(44.4) 29(50.9) 7(36.8) 14(35.0) 16(51.6) 23(51.1) 9(10) |
64(34.6) 23(69.7) 34(61.8) 8(26.7) 10(55.6) 28(49.1) 12(63.2) 26(70.0) 15(48.4) 22(48.9) 81(90) |
<0.001** 0.036* >0.05 0.02* >0.05 >0.05 >0.05 >0.05 >0.05 >0.05 <0.05 |
Note: ** very significant; *significant; ARDS: Acute Respiratory Distress Syndrome; PSO2: percutaneous oxygen saturation.
3.2. Comorbidity, intervention, and outcomes
All Patients admitted to ICU had some comorbidity. The cardiovascular disorders were the commonest comorbidity 183(35.4%) followed by respiratory disorders 153(29.6%), neurologic disorders 133(25.7%), and infectious disorders 59(11.4%). However, none of the comorbidities didn't show a significant association with 60 days of mortality (P > 0.05). The majority 278(53.8%) of patients admitted to ICU were on a mechanical ventilator where 187(67.3%) of them died during follow-up. One-hundred eighty-five patients were on inotropes while 236(45.6%) of them were on a fluid challenge.
All patients admitted to ICU experienced at least one complication during ICU stay. One hundred twenty-five sustained cardiac arrest and 102(81.6%) of them in time during follow up while 15(2.9%) had aspiration and from which 11(73.3%) of them died. The median and IQR of the length of ICU stay was 5(0.2–40) days where the minimum and Maximum ICU stays were 4 h–40 days respectively.
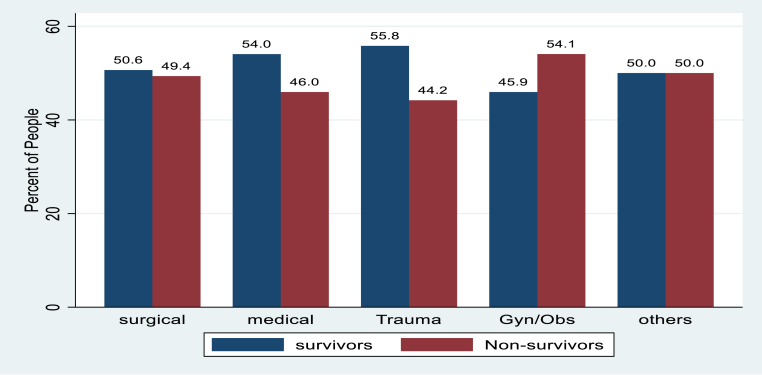
The incidence rate of mortality among ICU patients was 46.8%. The major causes of mortality among patients admitted to ICU in Southern Ethiopia were trauma 64(12.4%), Congestive heart failure 34(6.6%), ARDS 28(5.4%0 and stroke 26(5%)) (Table2). The mortality of patients in ICU among admission categories was the highest in gynecology/obstetrics followed by other and surgical categories (Fig. 2).
Table 2.
Prevalence of comorbidities, Intervention, complication, and outcomes of patients admitted to Teaching Referral Hospitals’ ICUs in Southern Ethiopia, June 2018 to May 2020.
| Characteristics | All admissions (n = 517) | survivors (n = 275) | Non-survivors (n = 242) | P-value |
|---|---|---|---|---|
| Comorbidities, n (%) Cardiovascular disease Respiratory disease Renal disease Infectious disease Neurological disease Endocrine disease Gastrointestinal Hematological disease Rheumatic disease Others |
183(35.4) 153(29.6) 31(6.0) 59(11.4) 133(25.7) 29(5.6) 35(6.8) 27(5.2) 5(1.0) 30(5.8) |
97(53.0) 79(51.6) 15(48.4) 25(42.4) 77(57.9) 15(51.7) 16(45.7) 14(51.9) 3(60.0) 15(50.0) |
86(47.0) 74(48.4) 16(51.6) 34(57.6) 56(42.1) 14(48.3) 19(54.3) 13(48.1) 2(40.0) 15(50.0) |
>0.05 |
| Intervention Mechanical Ventilation Inotropes Vasopressors Fluid Blood Transfusion Feeding Surgery GIT prophylaxis Antibiotics others |
278(53.8) 185(35.8) 274(53.0) 236(45.6) 20(3.9) 78(15.1) 9(1.7) 35(6.8) 324(62.7) 248(48.0) |
91(32.7) 86(46.5) 145(52.9) 123(25.1) 8(40.0) 38(48.7) 5(55.6) 16(45.7) 142(43.8) 139(56.0) |
187(67.3) 99(53.5) 129(47.1) 113(47.9) 12(60.0) 40(51.3) 4(44.4) 19(54.3) 51(56.2) 109(44.0) |
<0.0001** 0.027* >0.05 >0.05 >0.05 >0.05 >0.05 >0.05 <0.05* <0.0001** |
| Complications Cardiac arrest Anemia Arrhythmia Infection Hypotension Hypertension Aspiration |
125()24.2) 177(34.2) 43(8.3) 99(19.1) 332(64.2) 94(18.2) 15(2.9) |
23(18.4) 93(52.5) 24(55.8) 44(44.4) 176(53.0) 54(57.4) 4(26.7) |
102(81.6) 84(47.5) 19(44.2) 55(55.6) 156(47.0) 40(42.6) 11(73.3) |
<0.0001** >0.05 >0.05 0.034* >0.05 >0.05 0.033* |
Note: ** very significant; *significant; ARDS: Acute Respiratory Distress Syndrome; PSO2: percutaneous oxygen saturation.
Fig. 2.
Mortality by category of admission in Southern Ethiopia Teaching and Referral Hospitals' ICU from June 2018 to May 2020.
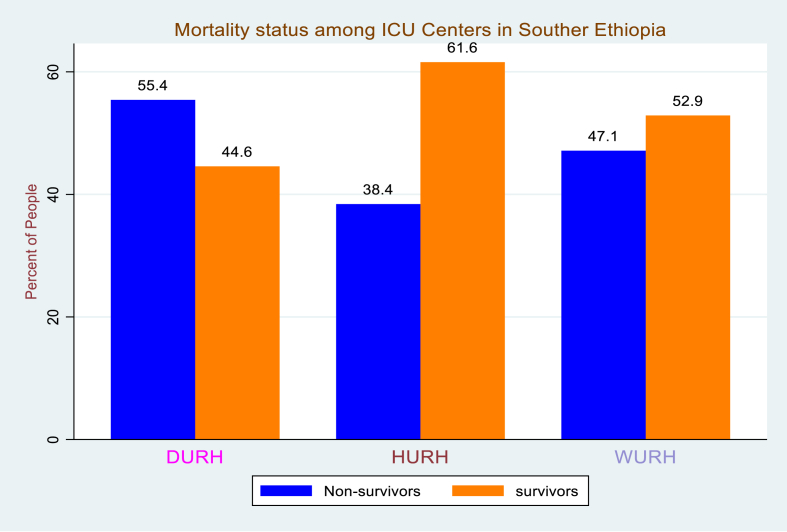
The mortality of patients among patients admitted to ICU in Southern Ethiopia teaching referral hospital's Intensive care unit was very high, 242/517 admission where the mortality was very high in Dilla University (55.4%) followed by Wolaita Sodo University (47.1%), and Hawassa University (38.4%) (Fig. 3).
Fig. 3.
Kaplan Meier survival plot on the influence of Cardiac arrest on 60-day survival during ICU stay.
Fig. 3: Mortality status among ICU centers in Southern Ethiopia from June 20, 2018, to May 20, 2020.
3.3. Determinants of ICU mortality
The variables showing a p-value of less than 0.25 in bivariate analysis were entered in multivariate analysis with a forward selection method as the explanatory variables were more than fifteen. The model fitness was estimated with Pearson chi-square statistics(X2 = 282, DF = 9, p = 0.0001) and Pseudo R2 = 0.561 and insignificant Hosmer –Lemeshow goodness of fit (p = 0.412). Fifty-six percent of the variation of ICU mortality was explained by the independent variables entered in the final regression model and the rest forty-four percent of the variation may be due to chance or other factors.
The variables that showed a significant difference in multivariate analysis were cardiac arrest, GCS score, aspiration, antibiotic use, mechanical ventilation, hypoxia, infection, and ICU length of stay. The multivariate analysis revealed that Patients who sustained cardiac arrest in ICU were approximately 12 times more likely to die as compared to those who didn't have a cardiac arrest, OR = 11.9(95% confidence interval(CI): 6.1 to 23.2). The Multivariate analysis also showed that patients whose GCS score less than eight were 8 times more likely to die, OR = 8.2(95% confidence interval(CI): 2.7 to 25.5) (Table 3).
Table 3.
Bivariate and multivariate analysis of 60-days mortality among patients admitted to ICU in Southern Ethiopia Teaching referral hospitals (N = 517), 2020.
| Variables | All admission (n=517) | Survivors (n = 275) | Non-survivors (n=242) | COR(95% CI) | AOR(95% CI) |
|---|---|---|---|---|---|
| Cardiac arrest, n (%) | 125(24.2) | 102(81.6) | 23(18.4) | 7.9[4.9, 13.1] | 11.9(6.1, 23.2)*** |
| Antibiotics(yes), | 192(37.3) | 51(26.4) | 142(73.6) | 3.9[2.7, 5.9] | 5.7(3.2, 10.2)*** |
| Aspiration(yes) | 15(2.9) | 11(73.3) | 4(26.7) | 3.2[1.0, 10.3] | 5.6(1.1, 29.4) |
| Infection(yes) | 99(19.1) | 55(55.6) | 44(44.4) | 1.5[0.9, 2.4] | 3.1(1.6, 5.9)** |
| MV(yes) | 278(53.8) | 187(67.3) | 91(32.7) | 6.9[4.6, 10.2] | 5.8(3.3, 10.3)*** |
| Hypoxia (Ps02<90) | 325(62.9) | 184(56.6) | 141(43.4) | 3.0[2.1,4.4] | 1.9(1.1, 3.3) |
|
GCS below 8 9 to 12 Above 12 |
275(53.2) 196(37.9) 46(8.9) |
184(66.9) 51(26.0) 7(37.0) |
91(33.1) 145(74.0) 39(63.0) |
11.3[4.8, 26.2] 1.9[0.83, 4.7] Ref |
8.2(2.7, 25.5)** 1.9(0.6, 6.1) Ref |
| Septic shock(yes) | 30(5.8) | 8(26.7) | 22(73.3) | 0.3[0.13, 0.7] | 0.6(0.2, 2.0) |
|
ICU LOS < 1 week 1 to 2 weeks > 2 weeks |
383(74.1) 85(16.4) 49(9.5) |
202(52.7) 27(31.8) 36(73.5) |
181(47.3) 58(68.2) 13() |
Ref 1.3[0.6,2.8] 3.1[1.6,6.0] |
Ref 1.5(0.6, 4.1) 8.7(3.6, 20.1)*** |
Note: ***: very significant (p-value <0.000; **: significant (p-value <0.0001); ICU LOS: Intensive Care Unit Length of stay; MV: Mechanical Ventilation; Ps02: Percutaneous Oxygen saturation; Ref: reference; GCS: Glasgow Coma Scale.
4. Discussion
This multi-center observational study revealed that the majority of patients admitted to ICU were female and younger productive age groups, 19–39 years old which are in line with other studies conducted in Sub-Saharan African countries [6,19,28,32,38,41,46]. The possible explanation for this difference in this age group in low-income countries might be due to engagement in violence, road traffic accident and relatively educated with high health-seeking behavior. On the contrary, the rate of admission to ICU in developed nations was among older patients that might be due to a sedentary lifestyle and high prevalence of a non-communicable disease among these patients [23,27,33,35].
The commonest causes of ICU admissions in our study were cardiovascular and respiratory disorders which are comparable with studies conducted globally [2,6,20,28,32,45,48,49,52,53,58,59]. However, there are discrepancies on the causes of admission to intensive care unit where studies conducted in Kenya, Tanzania, Uganda, Nigeria revealed postoperative events were the major causes of Admission [38,41,56] while studies were done from Jimma University referral hospital and Addis Ababa Black Lion hospital was due to trauma [46,53]. An international study from six continents including 10069 patients and another study from Belgium and the UK showed that the major causes of admission were cardiovascular and respiratory disease [20,40,45]. This difference may be explained by the types of ICU, level of care of the hospital, types of study design, and socio-demographic characteristics of the population.
This study revealed that the majority of patients were hypotensive, septic, comatose, and hypoxemic with unstable vital signs which were strongly associated with 30-days ICU mortality. In our study, more than fifty percent of patients were on a mechanical ventilator and from which more than sixty percent died during follow up. This high rate of mortality in patients with mechanical ventilator may be related to a frequent power cut, improper nursing care as they were not trained formally, lack of medication, malnutrition as there was no standard nutrition supplement, and ventilator-associated complications.
The overall ICU mortality rate of this study was higher than studies done in a different region of Ethiopia such as Addis Ababa (39%), Gondar (38.7%), Jimma (37.7%), Mekelle (27%) [32,46,60,61] and other studies conducted in sub-Saharan Africa namely: Nigeria (34.6%), Uganda (40.1%), and Tanzania (41.1%) [38,41,62]. On the other hand, it is lower than studies conducted in Jimma (50.4%), National Hospital of Abuja (68.4%), and Burkina Faso 60% [[63], [64], [65]]. This discrepancy might be due to differences in sample size, level of ICU care, availability of medical supplies, and stratification of skilled staff.
In this study, cardiac arrest, aspiration, being on a mechanical ventilator, hypoxemia at admission, and low GCS, and the use of antibiotics and length of stay were independent predictors of mortality. This study revealed that patients who sustained cardiac arrest were approximately 12 times more likely to die as compared to those who didn't, AOR = 11.9(95% CI:6.1 to 23.2). This high risk of death might be related to inadequate resuscitation drugs and equipment, lack of well-trained staff in advanced cardiac life support (ACLS), inappropriate post-cardiac arrest care, and compliance with ACLS protocol.
The study also revealed that patients with aspiration were 5.6 times more likely to die, AOR = 5.6(95% CI: 1.1. to 29.4) and patients on antibiotics for a prolonged period were still 5.7 times more likely to die as compared to those who didn't have, AOR = 5.7(95% CI: 3.2 to 10.2) which was in line with an observational and systematic review [33,47,66,67]. The possible explanation might be the rapid emergence and dissemination of antimicrobial-resistant microorganisms, administering unnecessary broad-spectrum antibiotics, and undue antibiotics for a prolonged period.
This study showed that ICU mortality was strongly associated with trauma, congestive heart failure, ARDS, and stroke which are comparable to studies conducted in Sab-Saharan African countries [2,6,46,53]. The possible explanation might be lack of Emergency medical care System (EMS) in pre-hospital, inadequate specialists, lack of well-trained ICU staffs, well-equipped integrated monitors, and drugs. Besides, the cost of ICU is very high for low and middle-income countries to establish modern well-equipped ICU because ICU requires a huge investment for training medical staff, purchasing medical supplies, and establishing ICU infrastructures.
4.1. Limitation of the study
This is a multi-center observational study with more than one month follow up and a relatively large sample size. However, this study is not without limitations. The nature of data handling management, unavailability of biochemical tests to determine the severity and prognostic score such as acute physiologic and chronic health evaluation (APACHE), sequential organ failure assessment (SOFA), Simplified Acute Physiology Score (SAPS) was the possible limitations.
4.2. Political implication
This multi-center observational study revealed that the overall mortality rate in ICU was very high as compared to other studies in Ethiopia as well as globally. The main independent predictors of mortality were traced and this entails a rigorous activity from different stakeholders. The majority of predictors could be prevented by availing emergency drugs for management of shock, cardiac arrest, aspiration, intracranial hypertension, arrhythmia, pain management, and sedation; integrative patient monitors as most of the monitors were not functional; training of ICU nurse because most of the nurses didn't have formal intensive care training; provision of adequate calories; availing bedside tests including portable X-ray, ultrasound, and biochemical tests.
4.3. The implication for further research
It has been known that retrospective study has its limitations as some important parameters may not be available. Besides, we didn't assess the severity and prognostic scores due to the unavailability of biochemical tests in some centers. Therefore, a multi-center prospective cohort study is in demand.
5. Conclusion
The overall ICU mortality rate was very high. The majority of independent predictors were cardiac arrest, aspiration, infection, unstable vital signs at admission, and being on a mechanical ventilator which could be minimized by implementing appropriate ICU care with a set of guidelines and protocols.
Ethics approval and consent to participate
Ethical clearance and approval were obtained from the ethical review board of the College of Health Science and Medicine.
Consent for publication
Not applicable.
Availability of data and materials
Data and material can be available where appropriate.
Registration of Research Studies
The study was registered retrospectively in research registry with Unique Identifier Number(UIN:researchregistry6641) and available at: https://www.researchregistry.com/browse-the-registry#home/
Guarantor
Semagn Mekonnen Abate, Corresponding Author
Assistant professor of Anesthesiology
Department of Anesthesiology
College of Health Sciences and Medicine
Dilla University
Tel:+251913864605
Provenance and peer review
Not commissioned, externally peer-reviewed.
Funding
This research was funded a total of USD 833 by Dilla University postgraduate program.
Author contribution
Please specify the contribution of each author to the paper, e.g. study concept or design, data collection, data analysis or interpretation, writing the paper, others, who have contributed in other ways, should be listed as contributors.
Declaration of competing interest
The authors declare that there are no competing interests.
Acknowledgments
The authors would like to acknowledge Dilla University for financial and technical support encouragement to carry out the project.
References.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102318.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Berthelsen P., Cronqvist M. The first intensive care unit in the world: Copenhagen 1953. Acta Anaesthesiol. Scand. 2003;47(10):1190–1195. doi: 10.1046/j.1399-6576.2003.00256.x. [DOI] [PubMed] [Google Scholar]
- 2.Okafor U. Challenges in critical care services in Sub-Saharan Africa: perspectives from Nigeria. Indian J. Crit. Care Med.: Peer-reviewed. 2009;13(1):25. doi: 10.4103/0972-5229.53112. Official Publication of Indian Society of Critical Care Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brilli R.J., Spevetz A., Branson R.D., Campbell G.M., Cohen H., Dasta J.F. Critical care delivery in the intensive care unit: defining clinical roles and the best practice model. Crit. Care Med. 2001;29(10):2007–2019. doi: 10.1097/00003246-200110000-00026. [DOI] [PubMed] [Google Scholar]
- 4.Haftu H., Hailu T., Medhaniye A. Assessment of pattern and treatment outcome of patients admitted to pediatric intensive care unit, Ayder Referral Hospital, Tigray, Ethiopia. BMC Res. Notes. 2015;11(1):1–6. doi: 10.1186/s13104-018-3432-4. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marshall J.C., Bosco L., Adhikari N.K., Connolly B., Diaz J.V., Dorman T. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J. Crit. Care. 2017;37:270–276. doi: 10.1016/j.jcrc.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Obsa M.S., Adem A.O., Gete G.B. Clinical outcomes of patients admitted in intensive care units of nigist eleni mohammed memorial hospital of hosanna, southern Ethiopia. Int. J. Med. Med. Sci. 2017;9(6):79–85. [Google Scholar]
- 7.Adhikari N.K., Fowler R.A., Bhagwanjee S., Rubenfeld G.D. Critical care and the global burden of critical illness in adults. Lancet. 2010;376(9749):1339–1346. doi: 10.1016/S0140-6736(10)60446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abhulimhen-Iyoha B.I., Pooboni S.K., Vuppali N.K.K. Morbidity pattern and outcome of patients admitted into a pediatric intensive care unit in India. Indian J. Clin. Med. 2014;5:S13902. IJCM. [Google Scholar]
- 9.Firth P., Ttendo S. Intensive care in low-income countries—a critical need. N. Engl. J. Med. 2012;367(21) doi: 10.1056/NEJMp1204957. 1974-6. [DOI] [PubMed] [Google Scholar]
- 10.Fowler R.A., Adhikari N.K., Bhagwanjee S. Clinical review: critical care in the global context–disparities in burden of illness, access, and economics. Crit. Care. 2008;12(5):225. doi: 10.1186/cc6984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murthy S., Leligdowicz A., Adhikari N.K. Intensive care unit capacity in low-income countries: a systematic review. PloS One. 2015;10(1) doi: 10.1371/journal.pone.0116949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Razzak J.A., Hyder A.A., Akhtar T., Khan M., Khan U.R. Assessing emergency medical care in low income countries: a pilot study from Pakistan. BMC Emerg. Med. 2008;8(1):8. doi: 10.1186/1471-227X-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dondorp A., Dünser M., Schultz M. 2019. Infrastructure and Organization of Adult Intensive Care Units in Resource-Limited Settings--Sepsis Management in Resource-Limited Settings. [PubMed] [Google Scholar]
- 14.Papali A., Adhikari N.K., Diaz J.V., Dondorp A.M., Dünser M.W., Jacob S.T. Sepsis Management in Resource-Limited Settings. Springer; Cham: 2019. Infrastructure and organization of adult intensive care units in resource-limited settings. 31-68. [PubMed] [Google Scholar]
- 15.Tumukunde J., Sendagire C., Ttendo S.S. Development of intensive care in low-resource regions. Current Anesthesiology Reports. 2019;9(1) 15-7. [Google Scholar]
- 16.Arabi Y.M., Schultz M.J., Salluh J.I. Springer; 2017. Intensive Care Medicine in 2050: Global Perspectives. [DOI] [PubMed] [Google Scholar]
- 17.Rosenberg A.L., Watts C. Patients readmitted to ICUs: a systematic review of risk factors and outcomes. Chest. 2000;118(2):492–502. doi: 10.1378/chest.118.2.492. [DOI] [PubMed] [Google Scholar]
- 18.Abhulimhen-Iyoha B.I., Pooboni S.K., Vuppali N.K.K. Morbidity pattern and outcome of patients admitted into a pediatric intensive care unit in India. Indian J. Clin. Med. 2014;5:S13902. IJCM. [Google Scholar]
- 19.Agalu A., Woldie M., Ayele Y., Bedada W. Reasons for admission and mortalities following admissions in the intensive care unit of a specialized hospital, in Ethiopia. Int. J. Med. Med. Sci. 2014;6(9):195–200. [Google Scholar]
- 20.Arulkumaran N., Harrison D., Brett S. Association between day and time of admission to critical care and acute hospital outcome for unplanned admissions to adult general critical care units: cohort study exploring the ‘weekend effect’. Br. J. Addiction: Br. J. Anaesth. 2017;118(1):112–122. doi: 10.1093/bja/aew398. [DOI] [PubMed] [Google Scholar]
- 21.Auld S., Caridi-Scheible M., Blum J.M., Robichaux C.J., Kraft C.S., Jacob J.T. medRxiv; 2020. ICU and Ventilator Mortality Among Critically Ill Adults with COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bellani G., Laffey J.G., Pham T., Fan E., Brochard L., Esteban A. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. Jama. 2016;315(8):788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 23.Cardoso L.T., Grion C.M., Matsuo T., Anami E.H., Kauss I.A., Seko L. Impact of delayed admission to intensive care units on mortality of critically ill patients: a cohort study. Crit. Care. 2011;15(1):1–8. doi: 10.1186/cc9975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Y.-C., Lin S.-F., Liu C.-J., Jiang D.D.-S., Yang P.-C., Chang S.-C. Risk factors for ICU mortality in critically ill patients. J. Formos. Med. Assoc. 2001;100(10):656–661. [PubMed] [Google Scholar]
- 25.Depuydt P.O., Vandijck D.M., Bekaert M.A., Decruyenaere J.M., Blot S.I., Vogelaers D.P. Determinants and impact of multidrug antibiotic resistance in pathogens causing ventilator-associated-pneumonia. Crit. Care. 2008;12(6):R142. doi: 10.1186/cc7119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fowler R.A., Sabur N., Li P., Juurlink D.N., Pinto R., Hladunewich M.A. Sex-and age-based differences in the delivery and outcomes of critical care. CMAJ (Can. Med. Assoc. J.) 2007;177(12):1513–1519. doi: 10.1503/cmaj.071112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gayat E., Cariou A., Deye N., Vieillard-Baron A., Jaber S., Damoisel C. Determinants of long-term outcome in ICU survivors: results from the FROG-ICU study. Crit. Care. 2018;22(1):8. doi: 10.1186/s13054-017-1922-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gidey K., Hailu A., Bayray A. Pattern and outcome OF medical intensive care unit admissions to ayder comprehensive specialized hospital IN tigray, Ethiopia. Ethiop. Med. J. 2017;56 [Google Scholar]
- 29.Groenland C.N., Termorshuizen F., Rietdijk W.J., van den Brule J., Dongelmans D.A., de Jonge E. Emergency department to ICU time is associated with hospital mortality: a registry analysis of 14,788 patients from six university hospitals in The Netherlands. Crit. Care Med. 2019;47(11):1564. doi: 10.1097/CCM.0000000000003957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khalil M.M., Salem H.M., El Tohamy M.F. Characteristics and clinical outcome of patients treated in the respiratory ICU of Abbassia Chest Hospital. Egypt. J. Bronchol. 2019;13(1):93. [Google Scholar]
- 31.Knaus W.A., Wagner D.P., Zimmerman J.E., Draper E.A. Variations in mortality and length of stay in intensive care units. Ann. Intern. Med. 1993;118(10):753–761. doi: 10.7326/0003-4819-118-10-199305150-00001. [DOI] [PubMed] [Google Scholar]
- 32.Lema G., Tessema H., Mesfin N., Fentie D., Arefaynie N. A retrospective cross-sectional study; 2019. Admission Pattern, Clinical Outcomes and Associated Factors Among Patients Admitted in Medical Intensive Care Unit at University of Gondar Comprehensive and Specialized Hospital, Northwest Ethiopia. 2019. [Google Scholar]
- 33.Liang C.-A., Lin Y.-C., Lu P.-L., Chen H.-C., Chang H.-L., Sheu C.-C. Antibiotic strategies and clinical outcomes in critically ill patients with pneumonia caused by carbapenem-resistant Acinetobacter baumannii. Clin. Microbiol. Infect. 2018;24(8):e1–e7. doi: 10.1016/j.cmi.2017.10.033. 908. [DOI] [PubMed] [Google Scholar]
- 34.Mendez-Tellez P.A., Dorman T., editors. Mayo Clinic Proceedings. Elsevier; 2005. Predicting patient outcomes, futility, and resource utilization in the intensive care unit: the role of severity scoring systems and general outcome prediction models. [DOI] [PubMed] [Google Scholar]
- 35.Moran J.L., Bristow P., Solomon P.J., George C., Hart G.K., Australian Mortality and length-of-stay outcomes, 1993–2003, in the binational Australian and New Zealand intensive care adult patient database. Crit. Care Med. 2008;36(1):46–61. doi: 10.1097/01.CCM.0000295313.08084.58. [DOI] [PubMed] [Google Scholar]
- 36.Ongóndi M., Mwachiro M., Ranketi S. Predictors of mortality in a critical care unit in south western Kenya. Annals of African Surgery. 2016;13(1) [Google Scholar]
- 37.Onyekwulu F., Anya S. Pattern of admission and outcome of patients admitted into the intensive care unit of university of Nigeria teaching hospital enugu: a 5-year review. Niger. J. Clin. Pract. 2015;18(6):775–779. doi: 10.4103/1119-3077.163291. [DOI] [PubMed] [Google Scholar]
- 38.Sawe H.R., Mfinanga J.A., Lidenge S.J., Mpondo B.C., Msangi S., Lugazia E. Disease patterns and clinical outcomes of patients admitted in intensive care units of tertiary referral hospitals of Tanzania. BMC Int. Health Hum. Right. 2014;14(1):26. doi: 10.1186/1472-698X-14-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sjoding M.W., Prescott H.C., Wunsch H., Iwashyna T.J., Cooke C.R. Longitudinal changes in intensive care unit admissions among elderly patients in the United States. Crit. Care Med. 2016;44(7):1353. doi: 10.1097/CCM.0000000000001664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vincent J.-L., Marshall J.C., Ñamendys-Silva S.A., François B., Martin-Loeches I., Lipman J. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. lancet .Respir. Med. 2014;2(5):380–386. doi: 10.1016/S2213-2600(14)70061-X. [DOI] [PubMed] [Google Scholar]
- 41.Ilori I.U., Kalu Q.N. Intensive care admissions and outcome at the university of calabar teaching hospital, Nigeria. J. Crit. Care. 2012;27(1):e1–e4. doi: 10.1016/j.jcrc.2011.11.011. 105. [DOI] [PubMed] [Google Scholar]
- 42.Diaz J.V., Riviello E.D., Papali A., Adhikari N.K., Ferreira J.C. Global critical care: moving forward in resource-limited settings. Annals of global health. 2019;85(1) doi: 10.5334/aogh.2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lone N.I., Gillies M.A., Haddow C., Dobbie R., Rowan K.M., Wild S.H. Five-year mortality and hospital costs associated with surviving intensive care. Am. J. Respir. Crit. Care Med. 2016;194(2):198–208. doi: 10.1164/rccm.201511-2234OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murthy S., Adhikari N.K. Global health care of the critically ill in low-resource settings. Ann. Am.Thorac. Soc. 2013;10(5):509–513. doi: 10.1513/AnnalsATS.201307-246OT. [DOI] [PubMed] [Google Scholar]
- 45.Sakr Y., Moreira C.L., Rhodes A., Ferguson N.D., Kleinpell R., Pickkers P. The impact of hospital and ICU organizational factors on outcome in critically ill patients: results from the Extended Prevalence of Infection in Intensive Care study. Crit. Care Med. 2015;43(3):519–526. doi: 10.1097/CCM.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 46.Smith Z., Ayele Y., McDonald P. Outcomes in critical care delivery at Jimma university specialised hospital, Ethiopia. Anaesth. Intensive Care. 2013;41(3):363–368. doi: 10.1177/0310057X1304100314. [DOI] [PubMed] [Google Scholar]
- 47.Paul M., Shani V., Muchtar E., Kariv G., Robenshtok E., Leibovici L. Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob. Agents Chemother. 2010;54(11):4851–4863. doi: 10.1128/AAC.00627-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Navarrete-Navarro P., Rivera-Fernández R., López-Mutuberría M.T., Galindo I., Murillo F., Dominguez J.M. Outcome prediction in terms of functional disability and mortality at 1 year among ICU-admitted severe stroke patients: a prospective epidemiological study in the south of the European Union (Evascan Project, Andalusia, Spain) Intensive Care Med. 2003;29(8):1237–1244. doi: 10.1007/s00134-003-1755-6. [DOI] [PubMed] [Google Scholar]
- 49.Vincent J.-L., Rello J., Marshall J., Silva E., Anzueto A., Martin C.D. International study of the prevalence and outcomes of infection in intensive care units. Jama. 2009;302(21):2323–2329. doi: 10.1001/jama.2009.1754. [DOI] [PubMed] [Google Scholar]
- 50.Dünser M., Towey R., Amito J., Mer M. Intensive care medicine in rural sub‐Saharan Africa. Anaesthesia. 2017;72(2):181–189. doi: 10.1111/anae.13710. [DOI] [PubMed] [Google Scholar]
- 51.Henry O., Amata A. A two-year review of admissions to the intensive care unit of the georgetown public hospital corporation. Guyana. West Indian Med J. 2017;66(6):628. [Google Scholar]
- 52.Vincent J.-L., Jones G., David S., Olariu E., Cadwell K.K. Frequency and mortality of septic shock in Europe and North America: a systematic review and meta-analysis. Crit. Care. 2019;23(1):1–11. doi: 10.1186/s13054-019-2478-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Haile S. Addis Ababa University; 2014. One Year Retrospective Review of Disease Patterns and Clinical Outcomes of Patients Admitted in Intensive Care Units of Armed Force General Teaching Hospital in Addis Ababa, Ethiopia. [Google Scholar]
- 54.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The strengthening the reporting of observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int. J. Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 55.Agha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G. STROCSS 2019 Guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 56.Lalani H.S., Waweru-Siika W., Mwogi T., Kituyi P., Egger J.R., Park L.P. Intensive care outcomes and mortality prediction at a national referral hospital in Western Kenya. Ann. Am.Thorac. Soc. 2018;15(11):1336–1343. doi: 10.1513/AnnalsATS.201801-051OC. [DOI] [PubMed] [Google Scholar]
- 57.Riviello E.D., Kiviri W., Fowler R.A., Mueller A., Novack V., Banner-Goodspeed V.M. Predicting mortality in low-income country ICUs: the Rwanda mortality probability model (R-MPM) PloS One. 2016;11(5) doi: 10.1371/journal.pone.0155858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tomlinson J., Haac B., Kadyaudzu C., Lee C., Muyco A., Charles A. 205: Critical care IN SUB-saharan africa: outcomes IN the midst OF austerity. Crit. Care Med. 2011;39(12):52. [Google Scholar]
- 59.Melaku Z., Alemayehu M., Oli K., Tizazu G. Pattern of admissions to the medical intensive care unit of Addis Ababa university teaching hospital. Ethiop. Med. J. 2006;44(1):33–42. [PubMed] [Google Scholar]
- 60.Bayisa T., Berhane A., Kedir S., Wuletaw T. Admission patterns and outcomes IN the medical intensive care unit OF ST. Paul’s hospital millennium medical college, addis ababa, Ethiopia. Ethiop. Med. J. 2017;55(1) [PubMed] [Google Scholar]
- 61.Gidey K., Hailu A., Bayray A. Pattern and outcome of medical intensive care unit admissions to ayder comprehensive specialized hospital in Tigray, Ethiopia. Ethiop. Med. J. 2018;56(1) [Google Scholar]
- 62.Kwizera A., Dünser M., Nakibuuka J. National intensive care unit bed capacity and ICU patient characteristics in a low income country. BMC Res. Notes. 2012;5(1):475. doi: 10.1186/1756-0500-5-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Agalu A., Mirkuzie W., Ayele Y., Bedada W. Reasons for admission and mortalities following admissions in the intensive care unit of a specialized hospital, Ethiopia. Int. J. Med. Med. Sci. 2014;6(9):195–200. [Google Scholar]
- 64.Ohaegbulam S., Okafor U., Ihekire O., Elumelu E. Using the revised trauma score to predict outcome in severely head injured patients in a developing nation–A pilot study. Int. J. Med.Health Dev. 2007;12(2):51–55. [Google Scholar]
- 65.Dao B., Rouamba A., Ouedraogo D., Kambou T., Bazié A. Transfer of obstetric patients in a pregnant and postpartum condition to an intensive care unit: eighty-two cases in Burkina Faso. Gynecol. Obstet. Fertil. 2003;31(2):123–126. doi: 10.1016/s1297-9589(03)00006-7. [DOI] [PubMed] [Google Scholar]
- 66.Luyt C.-E., Bréchot N., Trouillet J.-L., Chastre J. Antibiotic stewardship in the intensive care unit. Crit. Care. 2014;18(5):480. doi: 10.1186/s13054-014-0480-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roberts J.A., Paul S.K., Akova M., Bassetti M., De Waele J.J., Dimopoulos G. DALI: defining antibiotic levels in intensive care unit patients: are current β-lactam antibiotic doses sufficient for critically ill patients? Clin. Infect. Dis. 2014;58(8):1072–1083. doi: 10.1093/cid/ciu027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and material can be available where appropriate.