Abstract
Objectives:
Estimate the point prevalence of COVID-19 vaccine acceptability among US firefighters and Emergency Medical Services (EMS) workers.
Methods:
A cross-sectional study design was used to administer an anonymous online survey to a national non-probabilistic sample of firefighter and EMS workers.
Results:
Among the 3169 respondents, 48.2% expressed high acceptability of the COVID-19 vaccine when it becomes available, while 24.2% were unsure and 27.6% reported low acceptability. Using the “high COVID-19 vaccine acceptability” group as the reference category, the groups with greater odds of reporting low acceptability included those: 30 to 39 years of age (odds ratio = 3.62 [95% confidence interval = 2.00 to 6.55]), Black race (3.60 [1.12 to 11.53]), Hispanic/Latinx ethnicity (2.39 [1.45 to 3.92]), with some college education (2.06 [1.29 to 3.27]), married (1.65 [1.03 to 2.65]), of current rank firefighter/EMS (2.21 [1.60 to 3.08]).
Conclusions:
Over half of US firefighters and EMS workers were uncertain or reported low acceptability of the COVID-19 vaccine when it becomes available.
Keywords: COVID-19 vaccine, emergency medical services (EMS) workers, firefighters, vaccine acceptability
Firefighters and Emergency Medical Services (EMS) workers provide a critical role in maintaining the functionally of the United States (US) health care system. These first responders are at high risk of exposure to patients who have COVID-19 as well as at risk of transmitting the SARS-CoV-2 virus to others, including their family members.1 The National Academies of Sciences, Engineering, and Medicine consensus study advises a four-phased equitable-allocation framework for the COVID-19 vaccine.2 Phase 1a includes vaccine coverage for approximately 5% of the US population including front-line workers such as firefighters and EMS personnel. Similarly, the CDC's Advisory Committee on Immunization Practices’ has considered high priority groups for vaccine administration including paid and unpaid health care personnel and other essential workers who have the potential for direct or indirect exposure to patients or infectious materials.3 Ongoing community spread of SARS-CoV-2 will require frontline workers in patient-facing roles to continue close personal exposure to patients with the virus, placing them at high risk for infection.4 The COVID-19 vaccine holds promise as a public health tool to reduce the risk of transmission.
There is limited information on vaccine acceptability among first responders, however insight from a recent national Pew Research Center poll from early September 2020 suggests that the proportion of Americans who say they would get vaccinated for the coronavirus has declined since the start of the year.5 The survey finds approximately 77% of Americans believe it's very or somewhat likely a COVID-19 vaccine will be approved in the US before its safety and effectiveness are fully understood. Among the approximate 50% of respondents who stated they would not get a COVID-19 vaccine, 76% expressed concern about side effects as a major reason not to get vaccinated. Despite our growing knowledge of American outlook on a COVID-19 vaccine, including potential facilitators and barriers to receipt, little is known about the perceptions and the acceptability of the COVID-19 vaccine among first responders. In the present study, we estimate the point prevalence of COVID-19 vaccine acceptability among a sample of US firefighters and Emergency Medical Service Workers.
MATERIALS AND METHODS
Study Design, Study Sample, and Participant Recruitment
A cross-sectional study design was used to estimate COVID-19 vaccine acceptability rates in a non-probabilistic sample of first responders who included incumbent US firefighters, paramedics and emergency medical technicians located across all 50 states and US territories. An anonymous web-based survey was administered via REDCap between October 1 and October 31, 2020.6 To recruit first responder using established firefighters, paramedics and EMT e-mail Listservs, a recruitment e-mail describing the study was sent to e-mail lists of demographically diverse professional first responder organizations across the United States. The recruitment e-mail included a brief description of the goal of the survey study along with a link to the online survey. Because professional organizations were asked to forward the recruitment message, it is not possible to know how many first responders were reached, however 3598 (88.1% consent rate) first responders opened and read the consent form of whom 3169 completed the consent and study survey. All 50 US and five territories (American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, and the US Virgin Islands) were also represented in the sample.
Survey Instrument and Measures
The main study outcome measure was self-reported COVID-19 vaccine acceptability. The acceptability measure used a 10-item questionnaire t adapted to the COVID-19 context from a validated general vaccine acceptability survey.7 Responses to each acceptability scale item was measured on a 7-point Likert scale, where 1 indicated “strongly disagree,” 4 is “not sure,” and 7 was “strongly agree.” Five of the 10 COVID-19 acceptability questionnaire response items were reverse coded prior to analysis in order to reduce the acquiescence effect. We classified each survey respondent into one of three categories (ie, low acceptability with scores ranging from 1.00 to 3.99; unsure with scores from 4.00 to 4.99, and high acceptability with scores from 5.00 to 7.00). In addition to the COVID-19 vaccine acceptability questions, we included measures on work characteristics, employment, and sociodemographic characteristics. One survey question assessed the first responder's state of employment that was used to categorize respondents into one of 10 Federal Emergency Management Agency (FEMA) geographical regions.
Data Analysis
We calculated descriptive statistics for continuous variables, expressed as means with its standard deviation (sd), and for categorical variables, expressed as frequency and percent of the sample. We examined the main outcome of COVID-19 vaccine acceptability (high/unsure/low) by sociodemographic and work characteristics, by COVID-19 infection, and 2019 seasonal influenza vaccine receipt. For categorical data, we conducted Fisher exact test to compare groups. A polychotomous logistic regression model tested the association between COVID-19 vaccine acceptability and first responder age groups controlling for select socio-demographic and worker characteristics. P values <0.05 were considered statistically significant. We performed all data management and statistical analyses using IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, NY). The study protocol was reviewed and approved by the Institutional Review Board of the University.
RESULTS
Among the 3169 respondents, 48.2% expressed high acceptability of the COVID-19 vaccine when it becomes available, while 24.2% were unsure and 27.6% reported low acceptability (Table 1). Respondents who expressed low COVID-19 vaccine acceptability, compared with those who expressed high acceptability, were significantly more likely to be 30 to 39 years (31.3% vs 19.7%; P ≤ 0.001), of Black race (1.8% vs 0.3%; P ≤ 0.001), multi-race (5.4% vs 1.7%; P ≤ 0.001), other race (5.1% vs 3.2%; P ≤ 0.001), of Hispanic/Latinx ethnicity (6.5% vs 3.3%; P < 0.001), had some college education (56.1% vs 35.5; P < 0.001); be divorced, widowed, separated (8.3% vs 7.8%), of normal weight (18.5% vs 13.2%), and have a current rank of Firefighter/Paramedic/EMT (38.2% vs 28.0%). Furthermore, respondents who were unsure about vaccine acceptability were more likely to not have received the influenza vaccine in the prior 2019 season (36.4% vs 15.2%; P ≤ 0.001), and to have worked less years as a first responder (22.5 years vs 24.6 years; P < 0.001).
TABLE 1.
COVID-19 Vaccine Acceptability Stratified by Socio-Demographic and Work Characteristics, Prior Influenza Vaccination Receipt, and Prior COVID-19 Infection Among Firefighters, Paramedics, and Emergency Services Technicians Participating in the National Firefighter Acceptability of COVID-19 Vaccine Timing Study (FACTS), October 2020 (N = 3169)
| COVID-19 Vaccine Acceptability | |||||
| Low Vaccine Acceptability | Unsure | High Vaccine Acceptability | |||
| Sociodemographic Characteristics | Total Sample | n (%)∗ | n (%)∗ | n (%)∗ | P-Value† |
| Total | 3,169 (100.0) | 976 (27.6) | 767 (24.2) | 1,526 (48.2) | |
| Age groups | <0.001 | ||||
| 21–29 yrs | 186 (6.1) | 61 (7.2) | 59 (8.0) | 66 (4.4) | |
| 30–39 yrs | 713 (23.2) | 265 (31.3) | 156 (21.3) | 292 (19.7) | |
| 40–49 yrs | 1,009 (32.9) | 279 (32.9) | 272 (37.1) | 458 (30.8) | |
| 50–59 yrs | 858 (28.0) | 205 (24.2) | 199 (27.1) | 454 (30.6) | |
| 60 yrs and older | 301 (9.8) | 37 (4.4) | 48 (6.5) | 216 (14.5) | |
| Gender | 0.106 | ||||
| Male | 2893 (92.5) | 779 (91.6) | 721 (94.2) | 1393 (92.2) | |
| Female | 233 (7.5) | 71 (8.4) | 44 (5.8) | 118 (7.8) | |
| Race | <0.001 | ||||
| White | 2,876 (92.2) | 743 (87.7) | 705 (91.9) | 1428 (94.8) | |
| Black | 30 (1.0) | 15 (1.8) | 10 (1.3) | 5 (0.3) | |
| Multi-Race | 83 (2.7) | 46 (5.4) | 12 (1.6) | 25 (1.7) | |
| Other | 131 (4.2) | 43 (5.1) | 40 (5.2) | 48 (3.2) | |
| Ethnicity | <0.001 | ||||
| Hispanic/Latinx | 151 (4.9) | 55 (6.5) | 47 (6.2) | 49 (3.3) | |
| Non-Hispanic/non-Latinx | 2928 (95.1) | 796 (93.5) | 712 (93.8) | 1420 (96.7) | |
| Educational attainment | <0.001 | ||||
| High School/GED | 204 (6.5) | 46 (5.4) | 58 (7.6) | 100 (6.6) | |
| Some College | 1344 (43.0) | 480 (56.1) | 326 (42.9) | 538 (35.5) | |
| College Graduate | 1581 (50.5) | 329 (38.5) | 376 (49.5) | 876 (57.9) | |
| Marital status | 0.030 | ||||
| Married/Unmarried couple | 2586 (82.8) | 717 (84.1) | 605 (79.1) | 1264 (84.0) | |
| Divorced, widowed, separated | 264 (8.5) | 71 (8.3) | 76 (9.9) | 117 (7.8) | |
| Single | 272 (8.7) | 65 (7.6) | 84 (11.0) | 123 (8.2) | |
| Body mass index | 0.002 | ||||
| Normal weight | 442 (13.2) | 151 (18.5) | 99 (13.7) | 192 (13.2) | |
| Overweight | 1421 (49.8) | 368 (45.2) | 329 (45.4) | 724 (49.8) | |
| Obese | 1130 (37.8) | 296 (36.3) | 297 (41.0) | 537 (37.0) | |
| Firefighter current rank | <0.001 | ||||
| Firefighter/Paramedic/EMT | 941 (31.3) | 320 (38.2) | 216 (30.1) | 405 (28.0) | |
| Driver/Operator | 262 (8.7) | 103 (12.3) | 39 (5.4) | 120 (8.3) | |
| Inspector/Fire Investigator | 58 (1.9) | 15 (1.8) | 13 (1.8) | 30 (2.1) | |
| Lieutenant | 393 (13.1) | 144 (17.2) | 70 (9.7) | 179 (12.4) | |
| Captain | 490 (16.3) | 113 (13.5) | 162 (22.6) | 215 (14.8) | |
| Battalion/Deputy/Division Chief | 859 (28.6) | 142 (17.0) | 218 (30.4) | 499 (34.5) | |
| Had Flu Vaccine 2019 season | <0.001 | ||||
| Yes | 2115 (67.1) | 343 (39.4) | 483 (63.6) | 1289 (84.8) | |
| No | 1035 (32.9) | 527 (60.6) | 277 (36.4) | 231 (15.2) | |
| Been infected with COVID-19 | <0.001 | ||||
| Yes, confirmed | 203 (6.4) | 66 (7.6) | 34 (4.4) | 103 (6.8) | |
| Yes, but not test confirmed | 339 (10.7) | 142 (9.4) | 72 (9.4) | 125 (8.2) | |
| No | 2331 (73.7) | 569 (73.7) | 565 (73.7) | 1197 (78.6) | |
| Don’t know | 290 (9.2) | 97 (12.5) | 96 (12.5) | 97 (6.4) | |
| Firefighter tenure | <0.001 | ||||
| Years (mean ± standard deviation) | 22.9 ± 11.2 | 20.2 ± 9.7 | 22.5 ± 10.8 | 24.6 ± 11.9 | |
Differences in sub-total population sample due to item non-response or missing.
P-value for significance testing comparing all three COVID-19 acceptability groups (low, high, and unsure).
Low COVID-19 Acceptability and Unsure Stance
In the polytomous multiple logistic regression (Table 2), using the high COVID-19 vaccine acceptability group as the referent category, the strongest associations with report of low COVID-19 acceptability was being 30 to 39 years of age relative to respondents 60 years and older (OR = 3.62 [95% confidence interval = 2.00 to 6.55]), being Black race relative to White (3.60 [1.12 to 11.53]), being multi-race (2.98 [1.61 to 5.51]), having some college education relative to a high school diploma (2.06 [1.29 to 3.27]), being married or an unmarried couple relative to being single (1.65 [1.03 to 2.65]), being obese (0.63 [0.46 to 0.88]) relative to normal weight, being a driver/operator (2.40 [1.58 to 3.65]), reporting non-receipt of the 2019 influenza vaccine (0.13 [0.11 to 0.17]), and having not been previously infected with COVID-19 (0.54 [0.38 to 0.76]).
TABLE 2.
Polytomous Logistic Regression for Predictors of COVID-19 Vaccine Acceptability Among Firefighters, Paramedics, and Emergency Services Technicians Participating in the National Firefighter Acceptability of COVID-19 Vaccine Timing Study (FACTS), October 2020 (N = 3169)
| Low Acceptability | Unsure About Acceptability | |
| Predictors | AOR∗ [95% Confidence Interval] | AOR∗ [95% Confidence Interval] |
| Age groups (ref = 60 yrs and older) | ||
| 21–29 yrs | 3.38 [1.49–7.63] | 2.98 [1.40–6.34] |
| 30–39 yrs | 3.62 [2.00–6.55] | 2.22 [1.30–3.80] |
| 40–49 yrs | 2.51 [1.48–4.26] | 2.43 [1.54–3.86] |
| 50–59 yrs | 1.95 [1.19–3.19] | 1.72 [1.13–2.64] |
| Gender (ref = female) | ||
| Male | 1.15 [0.76–1.72] | 1.51 [1.00–2.30] |
| Race (ref = White) | ||
| Black | 3.60 [1.12–11.53] | 3.43 [1.11–10.67] |
| Multi-race | 2.98 [1.61–5.51] | 1.05 [0.49–2.22] |
| Other | 1.15 [0.67–1.98] | 1.33 [0.81–2.19] |
| Ethnicity (ref = Non-Hispanic/non-Latinx) | ||
| Hispanic/Latinx | 2.39 [1.45–3.92] | 2.35 [1.47–3.77] |
| Educational attainment (ref = High School/GED) | ||
| Some College | 2.06 [1.29–3.27] | 1.10 [0.71–1.72] |
| College Graduate | 1.20 [0.75–1.91] | 0.86 [0.55–1.34] |
| Marital status (ref = single) | ||
| Married/Unmarried couple | 1.65 [1.03–2.65] | 0.71 [0.47–1.08] |
| Divorced, widowed, separated | 1.67 [0.93–3.02] | 1.26 [0.75–2.10] |
| Body mass index (ref = normal weight) | ||
| Overweight | 0.60 [0.44–0.83] | 0.76 [0.56–1.04] |
| Obese | 0.63 [0.46–0.88] | 0.96 [0.70–1.32] |
| Firefighter current rank (ref = Chiefs) | ||
| Firefighter/Paramedic/EMT | 2.21 [1.60–3.08] | 0.87 [0.64–1.18] |
| Driver/Operator | 2.40 [1.58–3.65] | 0.61 [0.39–0.95] |
| Inspector/Fire Investigator | 1.16 [0.52–2.60] | 0.62 [0.28–1.36] |
| Lieutenant | 2.36 [1.62–3.42] | 0.77 [0.53–1.11] |
| Captain | 1.44 [1.01–2.05] | 1.35 [1.01–1.80] |
| Influenza vaccine receipt in 2019 (ref = No) | ||
| Yes | 0.13 [0.11–0.17] | 0.35 [0.28–0.44] |
| Been infected with COVID-19 (ref = Don’t know) | ||
| Yes, confirmed | 0.61 [0.36–1.04] | 0.45 [0.26–0.79] |
| Yes, but not test confirmed | 1.52 [0.97–2.38] | 0.82 [0.52–1.31] |
| No | 0.54 [0.38–0.76] | 0.57 [0.41–0.80] |
AOR, adjusted odds ratio, its 95% CI is shown in this table.
Reference group = high COVID-19 vaccine acceptability.
The strongest associations with report of uncertainty for the COVID-19 vaccine, compared with high COVID-19 vaccine acceptability was being 21 to 29 years of age relative to respondents 60 years and older (2.98 [1.40 to 6.34]), being male relative to female (1.51 [1.00 to 2.30]), being Black race relative to White (3.43 [1.11 to 10.67]), being Hispanic/Latinx (2.35 [1.47 to 3.77]), being of rank Captain relative to the battalion, deputy and division chiefs (1.35 [1.01 to 1.80]), reporting non-receipt of the 2019 influenza vaccine (0.35 [0.28 to 0.44]), and having not been previously infected with COVID-19 (0.57 [0.41 to 0.80]). Across all 10 geographic FEMA regions, states in region 4, Southeast (43.1%), region 6, Southwest (32.7%), and region 9, West (34.1%) had the top three highest proportion of first responders who expressed low COVID-19 vaccine acceptability (Fig. 1).
FIGURE 1.
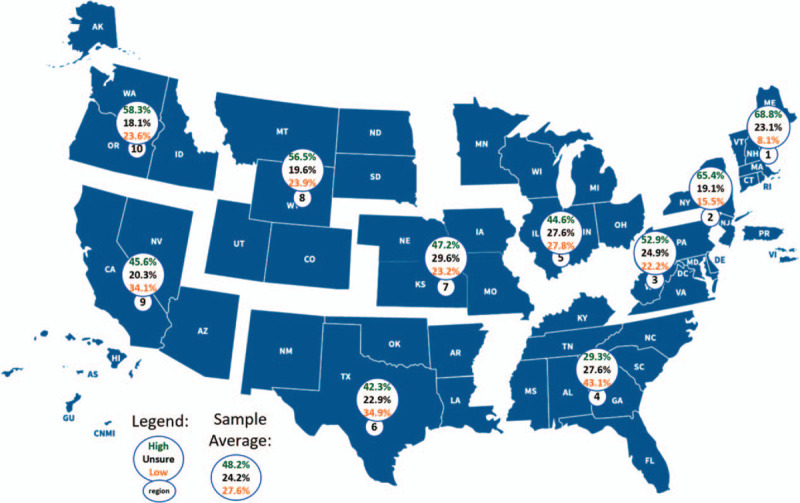
Frequency of unsure, high, and low COVID-19 vaccine acceptability stratified by FEMA region among firefighters, paramedics, and emergency services technicians participating in the national Firefighter Acceptability of COVID-19 vaccine Timing Study (FACTS), October 2020 (N = 3169). FEMA, Federal Emergency Management Agency.
DISCUSSION
In this study of US firefighters, paramedics and emergency medical technicians, we estimated the point prevalence (October 2020) for COVID-19 vaccine acceptability. Our data indicate that over half of US firefighters and EMS workers were uncertain or reported low acceptability of the COVID-19 vaccine when it becomes available to them. Among first responders who were unsure about accepting the vaccine, significantly more were of male sex, Black race, Hispanic/Latinx ethnicity, being a captain, reported not having the influenza vaccine during the 2019 season and had worked fewer years as a first responder. Our study findings have some similarities to research examining H1N1 influenza vaccine receipt in firefighters and emergency medical service workers.8–10 A study among Fire Department of New York City (FDNY) firefighters and EMS workers found that first responders who reported influenza vaccine receipt in the prior year, were more likely to receive the vaccine in the current year.10 This strong significant positive association between prior flu vaccine receipt in 2019 and willingness to accept the COVID-19 vaccine suggests opportunities to improve knowledge and education about vaccine effectiveness, illness/side effects, fears, and even enhance fire department organizational culture to improve vaccination rates. Similarly, first responders of Hispanic ethnicity were less likely to report acceptance of the H1N1 influenza vaccine compared with their non-Hispanic white counterparts.
Our study does differ by first responder rank and years of service such that our study respondents who were unsure or expressed low COVID-19 acceptability were of lower rank or worked fewer years as first responder. Caution should be used when interpreting firefighter rank as a predictor of COVID-19 acceptability (ie, Captain) given variability in the proportion of firefighters who reported being unsure versus having low acceptability of the COVID-19 vaccine. While the focus of this analysis was career firefighters and EMS workers, volunteer firefighters are estimated to comprise approximately 67% of the US fire service workforce and may express differences in COVID-19 acceptability.11 Public health campaigns should be tailored for educating those sub-groups of firefighters and emergency medical service workers who identified as unsure or expressed low COVID-19 acceptability.
Acknowledgments
The authors would like to thank the National Volunteer Fire Council, the International Association of Fire Chiefs, the International Association of Fire Firefighters, FirefighterCloseCall.com, home to the secret list, and all the US firefighters and emergency medical service workers who took the time to participate in this research study.
Footnotes
Institution at which the work was performed: Department of Public Health Sciences, Leonard M. Miller School of Medicine, University of Miami, Miller School of Medicine, 1120 N.W. 14th Street, Room #1025, Miami, FL 33136.
Authors’ contributions: A.J.C.M., C.A.S., K.M.S., P.L.F., J.L.B., D.L.S., S.J., G.P.H., and J.G., conceived the study, participated in its design, coordination, performed statistical analyses, and co-drafted the manuscript. A.J.C.M., P.L.F., K.M.S., and C.A.S. collected field data, entered study data, performed data analysis, and interpretation of study results. A.J.C.M., C.A.S., K.M.S., P.L.F., J.L.B., D.L.S., S.J., G.P.H., and J.G. interpreted study results and helped with the manuscript draft. All authors read, revised, and approved the final manuscript.
Funding: This research work was supported by the National Cancer Institute of the National Institutes of Health under Award Number P30CA240139. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Institution and Ethics approval and informed consent: This study research protocol was reviewed and approved by the University of Miami's Institutional Review Board (#20201201).
The authors declare no potential conflicts of interest.
Disclaimers: The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the University of Miami, University of Arizona, Yale University, Skidmore College, Center for Fire, Rescue and EMS Health Research in the National Development & Research Institutes, Underwriters Laboratories, Inc., or Rutgers University.
Clinical Significance: In a national sample (N = 3169) of U.S. first responders, 48.2% expressed high acceptability of the COVID-19 vaccine when it becomes available, while 24.2% were unsure and 27.6% reported low acceptability. Respondents unsure about vaccine acceptability were more likely to have not received the influenza vaccine in the prior 2019 season.
REFERENCES
- 1.Yang BY, Barnard LM, Emert JM, et al. Clinical characteristics of patients with coronavirus disease 2019 (COVID-19) receiving emergency medical services in King County, Washington. JAMA Netw Open 2020; 3:e2014549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kahn B, Brown L, Foege W, Gayle H. National Academies of Sciences E, Medicine. A framework for equitable allocation of COVID-19 vaccine. Framework for Equitable Allocation of COVID-19 Vaccine. US: National Academies Press; 2020. [PubMed] [Google Scholar]
- 3. McClung N, Chamberland M, Kinlaw K, et al. The Advisory Committee on Immunization Practices’ ethical principles for allocating initial supplies of COVID-19 vaccine—United States, 2020; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jun JFMAMJVSDAPwDHI, United States, COVID-19 Stats; 2020:1753. [Google Scholar]
- 5. Center PR. Republicans, democrats move even further apart in coronavirus concerns; 2020. [Google Scholar]
- 6.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sarathchandra D, Navin MC, Largent MA, McCright AM. A survey instrument for measuring vaccine acceptance. Prev Med 2018; 109:1–7. [DOI] [PubMed] [Google Scholar]
- 8.Rebmann T, Wright KS, Anthony J, Knaup RC, Peters EB. Seasonal and H1N1 influenza vaccine compliance and intent to be vaccinated among emergency medical services personnel. Am J Infect Control 2012; 40:632–636. [DOI] [PubMed] [Google Scholar]
- 9.Hubble MW, Zontek TL, Richards ME. Predictors of influenza vaccination among emergency medical services personnel. Prehosp Emerg Care 2011; 15:175–183. [DOI] [PubMed] [Google Scholar]
- 10.Glaser MS, Chui S, Webber MP, et al. Predictors of acceptance of H1N1 influenza vaccination by FDNY firefighters and EMS workers. Vaccine 2011; 29:5675–5680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evarts B, Stein GP. US Fire Department Profile 2017. MA: National Fire Protection Association Quincy; 2019. [Google Scholar]


