Abstract
Hoarding disorder (HD), characterized by difficulty parting with possessions and functionally impairing clutter, affects 2–6% of the population. Originally considered part of Obsessive-Compulsive Disorder (OCD), HD became a distinct diagnostic entity in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013. While sleep impacts OCD, little is known about sleep in HD. As HD patients often report poor sleep in clinical settings, understanding global subjective sleep quality and disturbances may lead to novel therapeutic targets. To address this gap, the authors used a sample of convenience: an existing data set designed to screen research study eligibility and explore the psychopathology and phenomenology of OCD and HD. The data set included information collected from individuals with HD (n=38), OCD (n=26), and healthy participants (n=22) about insomnia, sleep quality, and mood using interviews and structured instruments including the Insomnia Severity Index (ISI), Pittsburgh Sleep Quality Index (PSQI), and Depression Anxiety Stress Scales (DASS). In this data set, HD and OCD groups reported significantly greater insomnia symptoms and poorer sleep quality compared with healthy controls while controlling for depression, age, and gender. A sizable minority of HD and OCD individuals met criteria for comorbid sleep disorders. OCD and HD groups differed in delayed sleep phase prevalence. To our knowledge, this is the first study examining subjective sleep quality and insomnia in HD as compared to healthy individuals and those with OCD, while controlling for relevant clinical characteristics. Given that there are evidence-based treatments for insomnia and other sleep disorders, our study raises the possibility that treatment interventions targeting sleep may improve HD outcomes.
Introduction
Insufficient or poor quality sleep is associated with impairments in functioning and mental health, including higher rates of chronic pain and illness (Luyster et al., 2012; Taylor et al., 2007), increased risk for depression (Baglioni et al., 2011; Li et al., 2016), and suicide (Bernert et al., 2014, 2015). Sleep also impacts cognition, decision-making, and emotional processing (Bernert et al., 2014; Deliens et al., 2014; Haack & Mullington, 2005; Palmer & Alfano, 2017; Scullin & Bliwise, 2015; Stubbs et al., 2016). Despite its negative effects, sleep disturbances remain underdiagnosed and undertreated in the general population and in individuals with mental illness (Benca, 2005; Kallestad et al., 2011; Krystal et al., 2008).
Hoarding disorder (HD) is a common disorder, with a prevalence of 2–6% (Timpano et al., 2011). HD is characterized by persistent difficulty discarding possessions—regardless of their actual value—and distress associated with discarding, such that clutter compromises use of living areas in the home (American Psychiatric Association, 2013). In DSM-IV, hoarding symptoms were exclusively attributed to obsessive-compulsive disorder (OCD). However, in DSM-5, HD is now considered a discrete diagnostic entity within the Obsessive-Compulsive and Related Disorders category due to distinct patterns of risk, vulnerability, and treatment response (American Psychiatric Association, 2013; Mataix-Cols et al., 2010; Timpano et al., 2016).
Little is known about sleep in HD. A small study (n=24) using the Insomnia Severity Index (ISI) found that hoarding severity of individuals with HD correlated with insomnia severity (Raines et al., 2015). Due to past nosological overlap, evidence of sleep disturbance in OCD is important to note. In one study of treatment-seeking individuals with OCD, 70% reported subjective sleep quality disturbances as measured by the Bergen Insomnia Scale (Nordahl et al., 2018). In a nationally representative sample, sleep disturbance as measured by the Chronic Conditions section of the CIDI 3.0 was associated with obsessions and compulsions severity, even when controlling for depression (Cox & Olatunji, 2016). A systematic review of OCD and sleep found evidence for poorer sleep quality (e.g., reduced sleep duration and lower sleep efficiency) and associations between poor sleep quality and higher OCD severity (Paterson et al., 2013). Sleep disturbance may interfere with effective OCD treatment (Donse et al., 2017; Paterson et al., 2013). However, the precise relationship between sleep and OCD remains unclear given negative findings, contributions of comorbid depression to sleep disturbance, and methodological challenges (Bobdey et al., 2002; Díaz-Román et al., 2015; Marcks et al., 2010). One robust finding is the higher incidence of delayed sleep phase in OCD, which may also be associated with poor treatment response (Donse et al., 2017). To the best of our knowledge, however, no study has previously examined sleep quality and sleep phase in hoarding disorder. Comparing sleep quality between HD, OCD, and healthy controls may shed light on the converging and diverging relevance of sleep disorder to one or both disorders, which in turn may impact our mechanistic understanding of the Obsessive-Compulsive and Related Disorders category, as well as impact our treatments for these disorders.
To examine sleep quality, symptoms of insomnia, and prevalence of delayed sleep phase in HD, we contrasted self-reports of individuals with HD, OCD, and healthy controls using DSM-5 criteria in a sample of convenience (i.e., individuals being screened for clinical study participation). Based on previous findings, we hypothesized that individuals with HD and individuals with OCD would self-report poorer sleep quality and greater symptoms of insomnia as compared to healthy controls. We also explored the prevalence of delayed sleep phase in the three groups (HD, OCD, healthy controls). Two sleep questionnaires assessing global subjective sleep quality and disturbances over a specified period of time were used: the Pittsburgh Sleep Quality Index (PSQI)—the most extensively studied self-report measure of sleep quality (Devine et al., 2005)—and the Insomnia Severity Index, a brief, reliable measure of perceived insomnia commonly used in research and clinical practice (Bastien et al., 2001).
Methods
Data Set
The authors used an existing data set designed to explore OCD and HD psychopathology and phenomenology and to screen eligibility of individuals interested in OCD- and HD-specific research studies between June 2016 and April 2018. All data collection procedures were approved by the Stanford Institutional Review Board. The data set included information collected from individuals with HD (n=38), OCD (n=26), and healthy participants (n=22) about insomnia, sleep quality, and mood using clinical interviews, structured diagnostic scales and self-report measures including the Insomnia Severity Index, Pittsburgh Sleep Quality Index, and Depression Anxiety Stress Scales. Participants met DSM-5 criteria for hoarding disorder or OCD, as assessed using a structured interview (Structured Clinical Interview for DSM-5; SCID; First et al., 2015). Exclusion criteria for the OCD and HD groups included comorbid HD or OCD, respectively, and diagnosis with a psychotic disorder. Of the 26 OCD participants, two (8%) reported current hoarding obsessions and compulsions as target symptoms on the Y-BOCS checklist. An additional three of 26 OCD participants reported either hoarding obsessions or compulsions as Y-BOCS target symptoms. No OCD participants met DSM-5 criteria for hoarding disorder. Healthy participants were excluded if diagnosed with any neuropsychiatric disorder.
Measures
Insomnia Severity Index (ISI).
The Insomnia Severity Index is a brief and reliable measure of perceived insomnia symptoms over the preceding two weeks (Bastien et al., 2001). The ISI is comprised of seven items and assesses severity of sleep onset and maintenance problems, satisfaction with current sleep patterns, interference with functioning, noticeability of related impairment, and concern or distress related to sleep (Bastien et al., 2001). Scores range from 0 to 28, with higher scores indicating more severe insomnia symptoms (Bastien et al., 2001).
Pittsburgh Sleep Quality Index (PSQI).
The Pittsburgh Sleep Quality Index is a self-report measure of sleep quality and sleep disturbances over a one-month period (Buysse et al., 1989). The PSQI is comprised of 19 items and generates a global score with seven subscale scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The global scores range from 0 to 21, with higher scores indicating poorer sleep quality (Buysse et al., 1989). The PSQI is the most extensively studied self-report measure of sleep problems (Devine et al., 2005). It has acceptable psychometric properties, including good internal reliability and test-retest reliability (Buysse et al., 1989). Relevant PSQI items (i.e., Items 1, 2, and 3) were used to determine an individual’s typical sleep phase during the past month and identify delayed sleep phase, analogous to Delayed Sleep Phase Disorder (DSPD). Delayed sleep phase was operationally defined as a pattern of falling asleep after 1 a.m. and awakening after 10 a.m. during the past month (Turner et al., 2007).
Depression Anxiety Stress Scales (DASS).
The Depression Anxiety Stress Scales is a 21-item, self-report measure assessing depression, anxiety, and stress over the past week. Responses are provided on a 4-point scale (0–3). The DASS shows very good psychometric properties in clinical and non-clinical cohorts (Crawford & Henry, 2003). The depression subscale has a range of 0–42, with higher scores indicating higher symptoms of depression.
Data Analysis
Descriptive statistics were computed for all measures. Sociodemographic differences between groups were tested with chi-square or Fisher’s exact test where appropriate for nominal measures, and with one-way analysis of variance (ANOVA) for scale variables (i.e., DASS depression scores). To test the hypotheses regarding group differences in ISI and PSQI scores, two one-way Analysis of Covariance (ANCOVA) were conducted with ISI and PSQI scores as dependent variables, group (HD, OCD, healthy control) as an independent variable, and depressive symptoms (i.e., DASS depression subscale scores) and age as continuous covariates. We controlled for depressive symptoms, age, and gender for the following reasons. We controlled for depression due to the associations between depression and sleep impairment (Baglioni et al., 2011; Li et al., 2016), differing rates of comorbid depression between OCD and HD (Frost et al., 2011), and previous meta-analyses suggesting that depression affects sleep in OCD (Díaz-Román et al., 2015). We controlled for age given the robust findings on age-related sleep changes (Scullin & Bliwise, 2015), due to increases in severity of hoarding symptoms with each decade of life and individually in mid-life (Ayers et al., 2010; Dozier et al., 2016; Frost et al., 2000), and since research participants with hoarding disorder are typically older than other clinical samples (Wheaton et al., 2016). Similarly, although there are no clear gender differences in hoarding disorder (Postlethwaite et al., 2019), gender as well as sex-specific steroid hormones may alter different sleep properties (Adan & Natale, 2002; Manber & Armitage, 1999). Additionally, clinical hoarding research samples have a higher average percentage of female participants (77%) compared to community samples (55%) (Woody et al., 2020). We explored delayed sleep phase prevalence in each group (HD, OCD, healthy control) using the PSQI (Turner et al., 2007). Due to observed gender differences in our sample, we conducted two post-hoc ANCOVAs with depression severity, age, and gender as covariates, which did not alter our findings. Self-identified gender was coded into female, male, and non-binary to be inclusive of both binary and non-binary participants. To calculate the sample size without a prior study of hoarding with either ISI or PSQI, we first reviewed the literature and found a study comparing groups including OCD and HC participants and contrasted only these groups, revealing a large effect size in PSQI (Bobdey et al., 2002). With this assumption, using G*Power 3.1 (Faul et al., 2007), we calculate that the current sample allowed for examination of our main ANCOVAs at a power > 95% to test large size effects with a Type 1 error α < 0.05).
Results
Participant Characteristics
Participants from OCD, HD, and healthy control groups differed significantly by age (p < .001), depression severity (F = 17.09, p < .0001), and gender (p = .001), but did not differ significantly by race (p = .08) or ethnicity (p = .21) (Table 1). Concomitant medications and psychiatric comorbidities are presented in Supplementary Tables 1 and 2, respectively.
Table 1.
Participants
| HD | OCD | HC | |
|---|---|---|---|
| n=38 | n=26 | n=22 | |
| n | n | n | |
| Self-Reported Gender (M/F/NB)* | 7/31/0 | 16/9/1 | 11/11/0 |
| Race (C/AF/NH-PI/AI-AN/A/M/U/O) | 31/1/1/0/3/0/2/0 | 19/0/0/0/2/2/3/0 | 11/0/1/0/4/1/2/3 |
| Ethnicity (H/NH/U) | 2/35/1 | 5/21/0 | 4/17/1 |
| Age, years (SD| Range) * | 58.58 (9.06| 35–75) | 36.15 (10.91| 21–58) | 36.09 (14.04| 21–72) |
Sociodemographic summary.
indicates statistically significant differences between groups p < .05; OCD – obsessive-compulsive disorder; HD – hoarding disorder; HC – healthy controls; SD – standard deviation. M – male; F – female; NB – non-binary; C – Caucasian; AF – African American/Black; NH/PI – Native Hawaiian/Pacific Islander; AS-AN – American Indian/Alaska Native; A – Asian; M – Mixed; U – Unknown; O – Other; H – Hispanic; NH – non-Hispanic
Self-Reported Symptoms of Insomnia and Sleep Quality
Insomnia Severity Index (ISI).
Mean ISI scores significantly differed between the groups, F = 5.5, p = .006 (Table 2; Figure 1). Planned pairwise comparisons indicated that HD and OCD groups each had higher ISI total scores than the HC group (F = 8.96, p = .004; F = 7.56, p = .007, respectively), whereas HD and OCD groups did not differ (F = .143, p = .706). Item-level data is presented in Supplementary Table 3.
Table 2.
Descriptive Statistics
| HD group (n=38) | OCD group (n=26)c | Healthy controls (n=22) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | Range | M | SD | Range | M | SD | Range | |
| ISI total score | 7.08 | 5.34 | 0–21 | 7.92 | 5.73 | 0–20 | 0.82 | 2.26 | 0–21 |
| PSQI global score | 6.26 | 3.00 | 0–14 | 6.72 | 3.87 | 0–14 | 2.32 | 2.32 | 0–10 |
| DASS depression score | 8.95 | 8.0 | 14.69 | 12.41 | 0.09 | 0.43 | |||
| n | % | n | % | N | % | ||||
| Hypersomnolence Disordera | 3 | 8 | 2 | 8 | 0 | ||||
| Insomnia Disordera | 3 | 8 | 3 | 12 | 0 | ||||
| Delayed Sleep Phaseb | 0 | 3 | 12 | 0 | |||||
Descriptive Statistics summary. ISI – Insomnia Severity Index; PSQI – Pittsburgh Sleep Quality Global Score.
Determined with SCID.
Identified with PSQI (Turner et al., 2007).
26 OCD participants completed the ISI, and 25 OCD participants completed the PSQI.
Fig. 1.
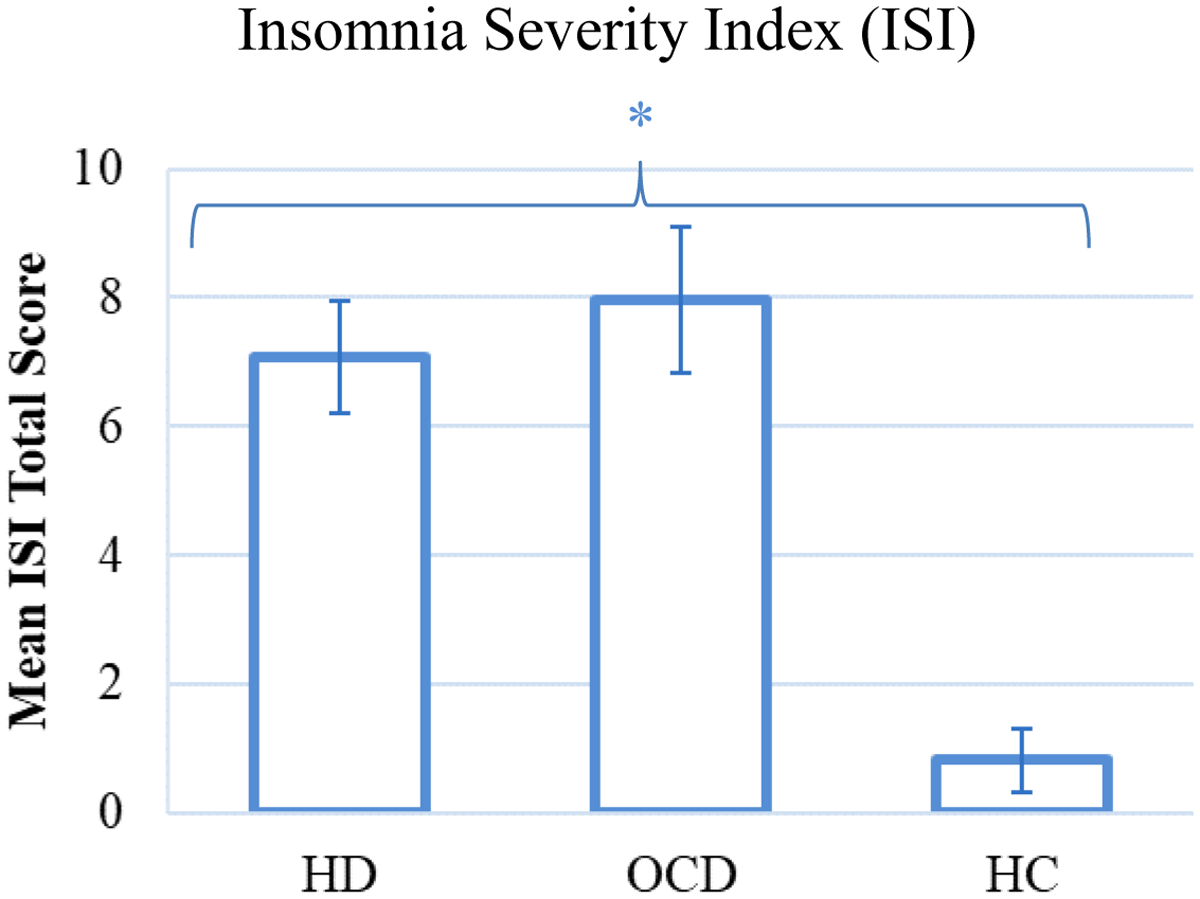
Mean ISI total scores in OCD, HD, and Healthy Controls. *significance at .01 level. Error bars represent one standard error from the mean.
Pittsburgh Sleep Quality Index (PSQI).
Mean PSQI scores statistically differed between HD, OCD, and healthy controls, F = 3.34, p = .04 (Table 2; Figure 2). Planned pairwise comparisons indicated that HD and OCD groups both had higher scores than healthy controls (F = 4.52, p = .037; F = 5.38, p = .023, respectively), whereas OCD and HD groups did not differ (F = 0.02, p = .9). Item-level data is presented in Supplementary Table 4.
Fig. 2.
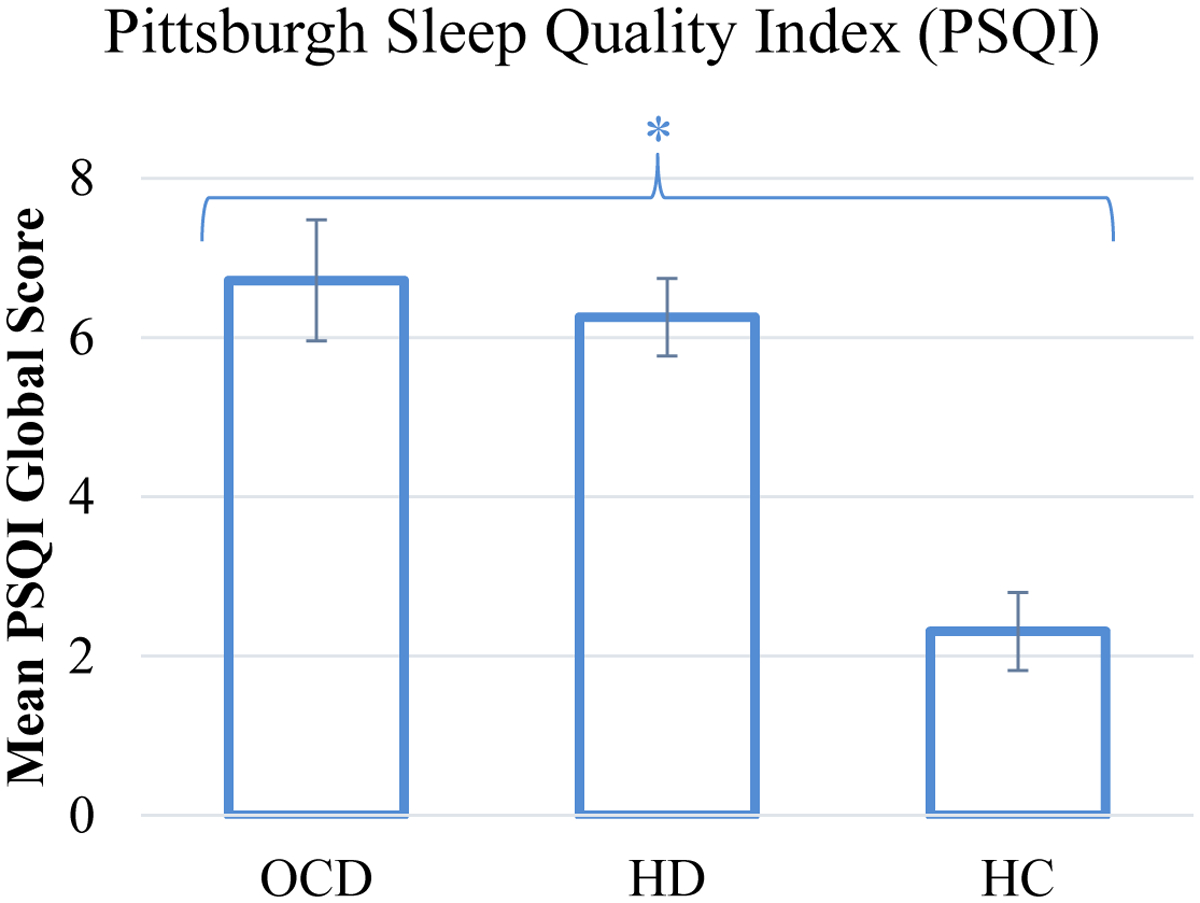
Mean PSQI global scores in OCD, HD, and Healthy Controls. *significance at .05 level. Error bars represent one standard error from the mean.
Delayed Sleep Phase Prevalence.
Three members of the OCD group (12%) met criteria for delayed sleep phase as operationally defined. No individuals with HD and no healthy controls met criteria for delayed sleep phase.
Discussion
This is the first study to 1) investigate self-reported sleep quality in individuals with HD, 2) compare insomnia symptoms and sleep quality among HD, OCD, and healthy controls, and 3) explore frequency of delayed sleep phase in a clinical sample of individuals with HD. The study used two sleep questionnaires assessing global subjective sleep quality and disturbances over a specified period of time: the Pittsburgh Sleep Quality Index (PSQI)—the most-extensively studied self-report measure of sleep quality (Devine et al., 2005)—and the Insomnia Severity Index (ISI), a brief, reliable measure of perceived insomnia which is the gold standard for insomnia assessment and a primary outcome measure in clinical trials (Bastien et al., 2001; Buysse et al., 2006). We found that OCD and HD groups reported comparably elevated insomnia symptoms and poorer sleep quality compared to healthy controls, when adjusting for age, gender, and depression. Second, a sizable minority of both OCD and the HD groups met criteria for a sleep disorder. Third, three out of 25 individuals with OCD (12%), and none in the HD or HC groups, reported a pattern of late bedtime and late rise time consistent with delayed sleep phase.
Our finding of worsened sleep quality and elevated insomnia symptoms in OCD and HD compared to healthy controls while adjusting for age, gender, and depression severity suggests that sleep is an area of clinical concern for individuals with both OCD and HD. Regarding sleep disturbances in HD, our findings are consistent with preliminary findings indicating that HD symptoms may interfere with sleep quality (Raines et al., 2015). Furthermore, OCD and HD participants’ higher levels of sleep impairment even when controlling for depression severity is consistent with previous findings of sleep impairment independent of depression severity (Nota et al., 2015; Paterson et al., 2013). Our finding that sleep impairment is associated with HD and OCD despite controlling age and depression is striking, as sleep-related complaints increase with age (Neikrug & Ancoli-Israel, 2010), and there are robust and well-established connections between depression and impaired sleep.
In this study, three out of 26 individuals with OCD reported a pattern of late bedtime and late rise times consistent with delayed sleep phase. This finding is consistent with evidence that individuals with OCD experience higher rates of circadian dysregulation resulting in delayed sleep phase (Coles et al., 2012; Mukhopadhyay et al., 2008; Paterson et al., 2013). Three out of 25 individuals with OCD reported delayed sleep phase (12%). This percentage is higher than estimated rates of 0.13–10% in the general population (Magee et al., 2016), but lower than previously reported estimates of 17–42% delayed sleep prevalence in OCD patients (Mukhopadhyay et al., 2008; Turner et al., 2007). These previous studies utilized inpatients and objective sleep logging over several days, while we utilized a self-report measure—suggesting our findings may underreport specific sleep patterns. In our study, none of the individuals with HD reported bedtimes and rising times consistent with delayed sleep phase. The absence of delayed sleep phase in our HD sample suggests differences in the nature of sleep impairments between OCD and HD. As the etiology of delayed sleep phase in OCD remains unclear (Paterson et al., 2013), the difference we found between OCD and HD patients could indicate group differences and warrants replication.
Our findings of poorer sleep quality and elevated insomnia symptoms in individuals with OCD and HD compared with healthy controls have important clinical implications. First, for individuals with HD and OCD experiencing disordered sleep, sleep disturbances may increase functional impairment and hinder effective treatment through negative effects on cognition and emotion regulation (Deliens et al., 2014; Durmer & Dinges, 2005; Krystal et al., 2008; Linkovski et al., 2019; Ramsawh et al., 2009). We suggest that screening for sleep disturbances may influence treatment of choice and impact treatment response among patients. Second, both HD and OCD have high comorbidity with depression (Brakoulias et al., 2017; Frost et al., 2011). Evidence from other populations indicates that sleep disturbances may increase the risk for the onset and reoccurrence of depressive episodes (Baglioni et al., 2011). Moreover, sleep disturbances may increase risk for suicide, independent of depressed mood. Indeed, this finding has been replicated using multiple measurements of sleep disturbance as well as objective sleep parameters (Bernert et al., 2014, 2015; Bernert, Hom, et al., 2017; Bernert, Luckenbaugh, et al., 2017; Turvey et al., 2002).
Our findings suggest that HD and OCD patients experience sleep disturbance. Addressing HD and OCD patients’ sleep difficulties in our treatments may improve patients’ lives. There are effective interventions to reduce symptoms of patients suffering from sleep disorders. Cognitive Behavioral Therapy for Insomnia (CBT-i) is a highly effective treatment that can lead to meaningful reductions in insomnia symptoms sustained over 6 months (Trauer et al., 2015). Current treatments for delayed sleep phase include chronotherapy (sleep scheduling), photic (exposure to bright morning light), chronobiotic (e.g., administration of melatonin), or other approaches (e.g., exercise, sleep hygiene) (Magee et al., 2016). Applying these treatments for OCD and HD patients may improve their sleep and possibly reduce their clinical symptoms.
Initial treatment efforts have addressed sleep disturbance in OCD and HD. In a case study of a patient with treatment-resistant OCD, CBT for OCD with adjunct chronotherapy (i.e., behavioral techniques to adjust sleep phase) led to a reduction in OCD symptoms and successful shifting of a patient’s sleep schedule (Coles & Sharkey, 2011). Furthermore, OCD inpatient programs with a set lights-out time have a higher rate of treatment response compared to programs without a set lights-out time (Coles & Stewart, 2019). Effective OCD treatment may also reduce sleep disturbance in some individuals affected by OCD and related disorders. In a small study (n=36), concentrated exposure treatment for OCD (i.e., intensive four-day treatment in a group setting) not only reduced OCD symptoms, but also reduced comorbid sleep disturbance, with improvements in sleep maintained at 6-month follow-up (Nordahl et al., 2018). These improvements in sleep were not linked to reductions in depression (Nordahl et al., 2018). In HD, different groups are testing novel treatments (Arch et al., 2012; Ayers et al., 2014; Chou et al., 2019; Diefenbach et al., 2015; Levy et al., 2019; Linkovski et al., 2018; Mathews et al., 2018; Moulding et al., 2017) that might be further enhanced by addressing patients’ disturbed sleep. Exploring specific sleep components (e.g., onset, maintenance, latency vs. duration) may impact treatment implications. Further, the presence of specific sleep difficulties may serve as prognostic indicators of treatment impact or treatment resistance (Donse et al., 2017; Manber et al., 2011).
Our study has several limitations, including our cross-sectional design, a relatively small sample size, use of self-report assessments, excluding individuals with comorbid OCD and HD, screening for sleep disorders using the SCID, and examining only primary sleep measures to conserve statistical power. In addition, while we did control for age in our analyses, the average ages of the groups were significantly different. Of note, our HD sample showed lower comorbidity with depression than typical samples, and at the same time, it also supports our finding that the high incidence of sleep disturbance observed in our sample is not attributable to mood disorder. Our results warrant replication and extension using objective sleep measures (e.g., polysomnography, actigraphy), which may allow assessment of additional sleep disorders (e.g., narcolepsy) potentially associated with OCD and HD. Using larger patient cohorts may elucidate the contribution of sleep to OCD and HD patients’ symptom presentation and severity, while incorporating sleep measures within clinical trials may facilitate exploration of sleep as a predictor treatment response. Our study demonstrates the presence of similar and distinct patterns of sleep disruption in HD and OCD. The potential role of an adjunct sleep intervention in improving response to existing treatments is recommended for further investigation.
Supplementary Material
Funding Support:
This study was supported by an Innovator Grant from Department of Psychiatry and Behavioral Sciences (Dr. Rodriguez) and National Institutes of Mental Health R01MH105461 (Dr. Rodriguez). Dr. Linkovski is supported by the Israeli Ministry of Science and Technology. Dr. van Roessel is supported by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs.
Financial disclosures:
In the last three years, Dr. Rodriguez has served as a consultant for Epiodyne, received research grant support from Biohaven Pharmaceuticals, and a stipend from APA Publishing for her role as Deputy Editor at The American Journal of Psychiatry. The other authors report no additional financial or other relationships relevant to the subject of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adan A, & Natale V (2002). Gender Differences in Morningness–Eveningness Preference. Chronobiology International, 19(4), 709–720. 10.1081/CBI-120005390 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (Ed.). (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed). American Psychiatric Association. [Google Scholar]
- Arch JJ, Eifert GH, Davies C, Vilardaga JCP, Rose RD, & Craske MG (2012). Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders. Journal of Consulting and Clinical Psychology, 80(5), 750–765. 10.1037/a0028310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers CR, Saxena S, Espejo E, Twamley EW, Granholm E, & Wetherell JL (2014). Novel Treatment for Geriatric Hoarding Disorder: An Open Trial of Cognitive Rehabilitation Paired with Behavior Therapy. The American Journal of Geriatric Psychiatry, 22(3), 248–252. 10.1016/j.jagp.2013.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers CR, Saxena S, Golshan S, & Wetherell JL (2010). Age at onset and clinical features of late life compulsive hoarding. International Journal of Geriatric Psychiatry, 25(2), 142–149. 10.1002/gps.2310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Lombardo C, & Riemann D (2011). Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders, 135(1–3), 10–19. 10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallières A, & Morin CM (2001). Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. [DOI] [PubMed] [Google Scholar]
- Benca RM (2005). Diagnosis and Treatment of Chronic Insomnia: A Review. Psychiatric Services, 56(3), 332–343. 10.1176/appi.ps.56.3.332 [DOI] [PubMed] [Google Scholar]
- Bernert RA, Hom MA, Iwata NG, & Joiner TE (2017). Objectively Assessed Sleep Variability as an Acute Warning Sign of Suicidal Ideation in a Longitudinal Evaluation of Young Adults at High Suicide Risk. The Journal of Clinical Psychiatry, 78(6), e678–e687. 10.4088/JCP.16m11193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Kim JS, Iwata NG, & Perlis ML (2015). Sleep disturbances as an evidence-based suicide risk factor. Current Psychiatry Reports, 17(3), 554. 10.1007/s11920-015-0554-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Luckenbaugh DA, Duncan WC, Iwata NG, Ballard ED, & Zarate CA (2017). Sleep architecture parameters as a putative biomarker of suicidal ideation in treatment-resistant depression. Journal of Affective Disorders, 208, 309–315. 10.1016/j.jad.2016.08.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Turvey CL, Conwell Y, & Joiner TE (2014). Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: A longitudinal, population-based study of late life. JAMA Psychiatry, 71(10), 1129–1137. 10.1001/jamapsychiatry.2014.1126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobdey M, Fineberg N, Gale TM, Patel A, & Davies HA (2002). Reported sleep patterns in obsessive compulsive disorder (OCD). International Journal of Psychiatry in Clinical Practice, 6(1), 15–21. 10.1080/136515002753489371 [DOI] [PubMed] [Google Scholar]
- Brakoulias V, Starcevic V, Belloch A, Brown C, Ferrao YA, Fontenelle LF, Lochner C, Marazziti D, Matsunaga H, Miguel EC, Reddy YCJ, do Rosario MC, Shavitt RG, Shyam Sundar A, Stein DJ, Torres AR, & Viswasam K (2017). Comorbidity, age of onset and suicidality in obsessive–compulsive disorder (OCD): An international collaboration. Comprehensive Psychiatry, 76, 79–86. 10.1016/j.comppsych.2017.04.002 [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, & Morin CM (2006). Recommendations for a standard research assessment of insomnia. Sleep, 29(9), 1155–1173. 10.1093/sleep/29.9.1155 [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF III, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Chou C, Tsoh JY, Shumway M, Smith LC, Chan J, Delucchi K, Tirch D, Gilbert P, & Mathews CA (2019). Treating hoarding disorder with compassion-focused therapy: A pilot study examining treatment feasibility, acceptability, and exploring treatment effects. British Journal of Clinical Psychology, bjc.12228. 10.1111/bjc.12228 [DOI] [PubMed] [Google Scholar]
- Coles ME, Schubert JR, & Sharkey KM (2012). Delayed bedtimes and obsessive-compulsive symptoms. Behavioral Sleep Medicine, 10(4), 258–265. 10.1080/15402002.2011.634939 [DOI] [PubMed] [Google Scholar]
- Coles ME, & Sharkey KM (2011). Compulsion or chronobiology? A case of severe obsessive-compulsive disorder treated with cognitive-behavioral therapy augmented with chronotherapy. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine, 7(3), 307–309. 10.5664/JCSM.1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coles ME, & Stewart E (2019). Circadian zeitgebers and treatment outcome in inpatient programs for obsessive compulsive disorder (OCD): A pilot study. Chronobiology International, 36(9), 1190–1193. 10.1080/07420528.2019.1624563 [DOI] [PubMed] [Google Scholar]
- Cox RC, & Olatunji BO (2016). Sleep disturbance and obsessive-compulsive symptoms: Results from the national comorbidity survey replication. Journal of Psychiatric Research, 75, 41–45. 10.1016/j.jpsychires.2016.01.007 [DOI] [PubMed] [Google Scholar]
- Crawford JR, & Henry JD (2003). The Depression Anxiety Stress Scales (DASS): Normative data and latent structure in a large non-clinical sample. The British Journal of Clinical Psychology, 42(Pt 2), 111–131. 10.1348/014466503321903544 [DOI] [PubMed] [Google Scholar]
- Deliens G, Gilson M, & Peigneux P (2014). Sleep and the processing of emotions. Experimental Brain Research, 232(5), 1403–1414. 10.1007/s00221-014-3832-1 [DOI] [PubMed] [Google Scholar]
- Devine EB, Hakim Z, & Green J (2005). A systematic review of patient-reported outcome instruments measuring sleep dysfunction in adults. PharmacoEconomics, 23(9), 889–912. [DOI] [PubMed] [Google Scholar]
- Díaz-Román A, Perestelo-Pérez L, & Buela-Casal G (2015). Sleep in obsessive–compulsive disorder: A systematic review and meta-analysis. Sleep Medicine, 16(9), 1049–1055. 10.1016/j.sleep.2015.03.020 [DOI] [PubMed] [Google Scholar]
- Diefenbach GJ, Tolin DF, Hallion LS, Zertuche L, Rabany L, Goethe JW, & Assaf M (2015). A Case Study of Clinical and Neuroimaging Outcomes Following Repetitive Transcranial Magnetic Stimulation for Hoarding Disorder. American Journal of Psychiatry, 172(11), 1160–1162. 10.1176/appi.ajp.2015.15050602 [DOI] [PubMed] [Google Scholar]
- Donse L, Sack AT, Fitzgerald PB, & Arns M (2017). Sleep disturbances in obsessive-compulsive disorder: Association with non-response to repetitive transcranial magnetic stimulation (rTMS). Journal of Anxiety Disorders, 49, 31–39. 10.1016/j.janxdis.2017.03.006 [DOI] [PubMed] [Google Scholar]
- Dozier ME, Porter B, & Ayers CR (2016). Age of onset and progression of hoarding symptoms in older adults with hoarding disorder. Aging & Mental Health, 20(7), 736–742. 10.1080/13607863.2015.1033684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durmer JS, & Dinges DF (2005). Neurocognitive consequences of sleep deprivation. Seminars in Neurology, 25(1), 117–129. 10.1055/s-2005-867080 [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. 10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, & Spitzer RL (2015). Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV). American Psychiatric Association. [Google Scholar]
- Frost RO, Steketee G, & Tolin DF (2011). Comorbidity in Hoarding Disorder. Depression and Anxiety, 28(10), 876–884. 10.1002/da.20861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost RO, Steketee G, & Williams L (2000). Hoarding: A community health problem. Health & Social Care in the Community, 8(4), 229–234. 10.1046/j.1365-2524.2000.00245.x [DOI] [PubMed] [Google Scholar]
- Haack M, & Mullington JM (2005). Sustained sleep restriction reduces emotional and physical well-being. Pain, 119(1–3), 56–64. 10.1016/j.pain.2005.09.011 [DOI] [PubMed] [Google Scholar]
- Kallestad H, Hansen B, Langsrud K, Ruud T, Morken G, Stiles TC, & Gråwe RW (2011). Differences between patients’ and clinicians’ report of sleep disturbance: A field study in mental health care in Norway. BMC Psychiatry, 11(1), 186. 10.1186/1471-244X-11-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krystal AD, Thakur M, & Roth T (2008). Sleep disturbance in psychiatric disorders: Effects on function and quality of life in mood disorders, alcoholism, and schizophrenia. Annals of Clinical Psychiatry: Official Journal of the American Academy of Clinical Psychiatrists, 20(1), 39–46. 10.1080/10401230701844661 [DOI] [PubMed] [Google Scholar]
- Levy HC, Frost RO, Offermann EA, Steketee G, & Tolin DF (2019). A Comparison of Cognitive Restructuring and Thought Listing for Excessive Acquiring in Hoarding Disorder. Cognitive Therapy and Research, 43(6), 1065–1074. 10.1007/s10608-019-10022-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Wu C, Gan Y, Qu X, & Lu Z (2016). Insomnia and the risk of depression: A meta-analysis of prospective cohort studies. BMC Psychiatry, 16(1), 375. 10.1186/s12888-016-1075-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linkovski O, Weinbach N, Edelman S, Feldman MW, Lotem A, & Kolodny O (2019). Beyond uncertainty: A broader scope for “incentive hope” mechanisms and its implications. Behavioral and Brain Sciences, 42, e44. 10.1017/S0140525X18002029 [DOI] [PubMed] [Google Scholar]
- Linkovski O, Zwerling J, Cordell E, Sonnenfeld D, Willis H, La Lima CN, Baker C, Ghazzaoui R, Girson R, Sanchez C, Wright B, Alford M, Varias A, Filippou-Frye M, Shen H, Jo B, Shuer L, Frost RO, & Rodriguez CI (2018). Augmenting Buried in Treasures with in-home uncluttering practice: Pilot study in hoarding disorder. Journal of Psychiatric Research, 107, 145–150. 10.1016/j.jpsychires.2018.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luyster FS, Strollo PJ, Zee PC, & Walsh JK (2012). Sleep: A Health Imperative. Sleep, 35(6), 727–734. 10.5665/sleep.1846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee M, Marbas EM, Wright KP, Rajaratnam SMW, & Broussard JL (2016). Diagnosis, Cause, and Treatment Approaches for Delayed Sleep-Wake Phase Disorder. Sleep Medicine Clinics, 11(3), 389–401. 10.1016/j.jsmc.2016.05.004 [DOI] [PubMed] [Google Scholar]
- Manber R, & Armitage R (1999). Sex, Steroids, and Sleep: A Review. Sleep, 22(5), 540–541. 10.1093/sleep/22.5.540 [DOI] [PubMed] [Google Scholar]
- Manber R, Bernert RA, Suh S, Nowakowski S, Siebern AT, & Ong JC (2011). CBT for Insomnia in Patients with High and Low Depressive Symptom Severity: Adherence and Clinical Outcomes. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine, 7(6), 645–652. 10.5664/jcsm.1472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcks BA, Weisberg RB, Edelen MO, & Keller MB (2010). The relationship between sleep disturbance and the course of anxiety disorders in primary care patients. Psychiatry Research, 178(3), 487–492. 10.1016/j.psychres.2009.07.004 [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Frost RO, Pertusa A, Clark LA, Saxena S, Leckman JF, Stein DJ, Matsunaga H, & Wilhelm S (2010). Hoarding disorder: A new diagnosis for DSM-V? Depression and Anxiety, 27(6), 556–572. 10.1002/da.20693 [DOI] [PubMed] [Google Scholar]
- Mathews CA, Mackin RS, Chou C-Y, Uhm SY, Bain LD, Stark SJ, Gause M, Vigil OR, Franklin J, Salazar M, Plumadore J, Smith LC, Komaiko K, Howell G, Vega E, Chan J, Eckfield MB, Tsoh JY, & Delucchi K (2018). Randomised clinical trial of community-based peer-led and psychologist-led group treatment for hoarding disorder. BJPsych Open, 4(4), 285–293. 10.1192/bjo.2018.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulding R, Nedeljkovic M, Kyrios M, Osborne D, & Mogan C (2017). Short-Term Cognitive-Behavioural Group Treatment for Hoarding Disorder: A Naturalistic Treatment Outcome Study. Clinical Psychology & Psychotherapy, 24(1), 235–244. 10.1002/cpp.2001 [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay S, Fineberg NA, Drummond LM, Turner J, White S, Wulff K, & Ghodse H (2008). Delayed sleep phase in severe obsessive-compulsive disorder: A systematic case-report survey. CNS Spectrums, 13(5), 406–413. [DOI] [PubMed] [Google Scholar]
- Neikrug AB, & Ancoli-Israel S (2010). Sleep Disorders in the Older Adult – A Mini-Review. Gerontology, 56(2), 181–189. 10.1159/000236900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordahl H, Havnen A, Hansen B, Öst L-G, & Kvale G (2018). Sleep disturbances in treatment-seeking OCD-patients: Changes after concentrated exposure treatment. Scandinavian Journal of Psychology, 59(2), 186–191. 10.1111/sjop.12417 [DOI] [PubMed] [Google Scholar]
- Nota JA, Sharkey KM, & Coles ME (2015). Sleep, arousal, and circadian rhythms in adults with obsessive–compulsive disorder: A meta-analysis. Neuroscience & Biobehavioral Reviews, 51, 100–107. 10.1016/j.neubiorev.2015.01.002 [DOI] [PubMed] [Google Scholar]
- Palmer CA, & Alfano CA (2017). Sleep and emotion regulation: An organizing, integrative review. Sleep Medicine Reviews, 31, 6–16. 10.1016/j.smrv.2015.12.006 [DOI] [PubMed] [Google Scholar]
- Paterson JL, Reynolds AC, Ferguson SA, & Dawson D (2013). Sleep and obsessive-compulsive disorder (OCD). Sleep Medicine Reviews, 17(6), 465–474. 10.1016/j.smrv.2012.12.002 [DOI] [PubMed] [Google Scholar]
- Postlethwaite A, Kellett S, & Mataix-Cols D (2019). Prevalence of Hoarding Disorder: A systematic review and meta-analysis. Journal of Affective Disorders, 256, 309–316. 10.1016/j.jad.2019.06.004 [DOI] [PubMed] [Google Scholar]
- Raines AM, Portero AK, Unruh AS, Short NA, & Schmidt NB (2015). An Initial Investigation of the Relationship Between Insomnia and Hoarding. Journal of Clinical Psychology, 71(7), 707–714. 10.1002/jclp.22161 [DOI] [PubMed] [Google Scholar]
- Ramsawh HJ, Stein MB, Belik S-L, Jacobi F, & Sareen J (2009). Relationship of anxiety disorders, sleep quality, and functional impairment in a community sample. Journal of Psychiatric Research, 43(10), 926–933. 10.1016/j.jpsychires.2009.01.009 [DOI] [PubMed] [Google Scholar]
- Scullin MK, & Bliwise DL (2015). Sleep, Cognition, and Normal Aging: Integrating a Half-Century of Multidisciplinary Research. Perspectives on Psychological Science : A Journal of the Association for Psychological Science, 10(1), 97–137. 10.1177/1745691614556680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubbs B, Wu Y-T, Prina AM, Leng Y, & Cosco TD (2016). A population study of the association between sleep disturbance and suicidal behaviour in people with mental illness. Journal of Psychiatric Research, 82, 149–154. 10.1016/j.jpsychires.2016.07.025 [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, & Bush AJ (2007). Comorbidity of Chronic Insomnia With Medical Problems. Sleep, 30(2), 213–218. 10.1093/sleep/30.2.213 [DOI] [PubMed] [Google Scholar]
- Timpano KR, Exner C, Glaesmer H, Rief W, Keshaviah A, Brähler E, & Wilhelm S (2011). The epidemiology of the proposed DSM-5 hoarding disorder: Exploration of the acquisition specifier, associated features, and distress. The Journal of Clinical Psychiatry, 72(6), 780–786. 10.4088/JCP.10m06380 [DOI] [PubMed] [Google Scholar]
- Timpano KR, Muroff J, & Steketee G (2016). A Review of the Diagnosis and Management of Hoarding Disorder. Current Treatment Options in Psychiatry, 3(4), 394–410. 10.1007/s40501-016-0098-1 [DOI] [Google Scholar]
- Trauer JM, Qian MY, Doyle JS, Rajaratnam SMW, & Cunnington D (2015). Cognitive Behavioral Therapy for Chronic Insomnia: A Systematic Review and Meta-analysis. Annals of Internal Medicine, 163(3), 191–204. 10.7326/M14-2841 [DOI] [PubMed] [Google Scholar]
- Turner J, Drummond LM, Mukhopadhyay S, Ghodse H, White S, Pillay A, & Fineberg NA (2007). A prospective study of delayed sleep phase syndrome in patients with severe resistant obsessive-compulsive disorder. World Psychiatry, 6(2), 108. [PMC free article] [PubMed] [Google Scholar]
- Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, & Wallace R (2002). Risk factors for late-life suicide: A prospective, community-based study. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 10(4), 398–406. [PubMed] [Google Scholar]
- Wheaton MG, Abramowitz JS, Jacoby RJ, Zwerling J, & Rodriguez CI (2016). An investigation of the role of intolerance of uncertainty in hoarding symptoms. Journal of Affective Disorders, 193, 208–214. 10.1016/j.jad.2015.12.047 [DOI] [PubMed] [Google Scholar]
- Woody SR, Lenkic P, Bratiotis C, Kysow K, Luu M, Edsell-Vetter J, Frost RO, Lauster N, Steketee G, & Tolin DF (2020). How well do hoarding research samples represent cases that rise to community attention? Behaviour Research and Therapy, 126, 103555. 10.1016/j.brat.2020.103555 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


