Abstract
OBJECTIVE:
Migraine headaches affect about approximately 15% of the population and some notable efforts have been made to develop meditation interventions to address pain and mood among this population. However, key active ingredients and the necessary duration of meditation interventions to produce an effect are still unknown. The purpose of this study is to assess key meditation ingredients that positively impact mood and headache factors across different meditation techniques and to establish an initial time or ”dose” needed to reach proactive treatment efficacy.
METHOD:
In this longitudinal study, three active management forms of meditation were compared to a cognitive distraction meditation to assess the effects on migraine headaches and emotions over a 30 day period when practiced 20 minutes per day.
RESULTS:
The active group showed significant decreases in anger (p=.005) and migraine pain (p=.002) over time. Further analysis showed that the bulk of the change for the active management group occurred in the final 10 days, after 20 days of practice of the technique (p<.05).
CONCLUSION:
This suggests that cognitively active forms of meditation are more effective in reducing migraine headache pain and negative mood than distraction techniques. However, individuals engaging in these strategies need to consistently practice these techniques for approximately 20 days to proactively reduce migraine headache pain and negative mood.
Keywords: Migraine, Headache, Mood, Pain, Longitudinal, Meditation, Intervention
1.1. Introduction
Migraine headache is a pain disorder that impacts people across multiple cultures and ethnicities. Migraine headaches are identified by the intense, unilateral, throbbing pain that often co-occurs with photophobia and/or phonophobia.1 Migraineurs report migraines cause significant pain (100%), negatively impact relationships (60%), and interfere with home life (85%).2 It has also been demonstrated that migraineurs have an increased sensitivity to pain even between headache attacks.3,4
Epidemiological studies indicate a high prevalence of migraine in the US. According to a recent American Migraine Study, approximately 18% of women and 6% of men in the United States suffer from migraine headaches every year.5 Migraine headaches are also associated with negative impact on individuals’ social functioning and relationships as well as decreased quality of life.6,7,8,9 In sum, the physical, psychological, emotional, and cost burden of migraine is substantial.10,11
Individuals who experience frequent migraines also have an increased prevalence of other physical and psychiatric comorbidities and appear to have greater psychosomatic reactivity to stress, increased depression, and anxiety.12,13,14 Further, migraineurs are more likely to report that irritation, worry, and anxiety are frequent triggers for migraine headaches.15 Since negative emotions can trigger and prolong migraine headaches, treatments that can address this issue may reduce the frequency and severity of migraine headaches.
In addition to pharmaceutical treatment, migrainuers also make use of complementary and alternative medicine (CAM) approaches.16 Adults with migraine in a nationally representative sample of US (n = 23,393) were more likely to use CAM therapies than those without migraine (AOR = 1.29, 95% CI = 1.15–1.45).17 Mind-body therapies such as progressive relaxation, yoga, and meditation were some of the most frequently used techniques. While certainly these are different practices, they all contain an element of cognitive focus or cognitive control as part of the technique that may influence the psychoogical and physical benefits that have been found from using these techniques. Psychophysiological interventions aimed at increasing positive emotions can improve pain tolerance18 decrease negative emotions and improve migraine frequency.19 Since disrupted mood and anxiety symptoms increase migraine headache frequency,20 meaningful cognitive focus may be a form of stress reduction that canreduce the psychophysiological impact of stress on the body.21 Neuromodulating pain using mind-body techniques may help individuals with chronic migraine.22 For example, progressive muscle relaxation can result in a 35–40% decline in frequency of headaches.23 Meditation is also emerging as an efficient preventative therapy for individuals who suffer from chronic pain and stress.24,25 Meditation, one form of cognitive control, has proven effective in reducing physiological and psychological arousal to stress.21 However, it appears that the daily practice of multiple types of meditation may help alleviate psychological and physical symptoms of migraine headaches.26,27
Meditation practice has been associated with improved pain and decreased migraine headaches frequency in previous studies. 21,25,26,27 Tonelli &Wachholtz (2014) showed that a single exposure of compassion based meditation to meditation naïve migraineurs (n = 27, Mage = 54.5 years SD = 11.1) led to a significant decline in patient-reported pain and emotional tension post intervention.26 There was as much as a 33% decrease in pain and 43% decrease in emotional tension from pre-to-post intervention period. Previous research by Wachholtz & Pargament (2005) also showed that spiritual meditation practice for 20 minutes a day for two weeks led to significant reduction in anxiety, negative mood, and increased pain tolerance compared to secular meditation and relaxation.21 It is possible that meaningful cognitive control that occurs through the practice of meditation can also impact frequency of headaches, even when there is not an explicit effort to reduce headache pain.28 However, it is unknown if all forms of cognitive control, both those that contain meaningful practices for the participant (e.g. meditation, relaxation) and meaningless practices (e.g. simple distraction) would be equally effective in reducing migraine headache frequency or pain levels.
By enhancing meaningful cognitive control as a stress reduction strategy, patients may increase their ability to improve both the frequency of migraine headaches and pain tolerance. However, very few studies have focused on comparing the impact of specific types of meditation on migraine outcomes. Previous research has focused on meditation practices such as mantra-based practices, and mindfulness practices but few have done head-to-head studies comparing meditation techniques for specific medical illnesses. To our knowledge no studies have assessed differences between meaningful cognitive focus exercises and cognitive distraction practices.
Some of these meditation techniques use a meaningful phrase, mantra, or cognitive focus to direct the mental exercise while other techniques rely solely on the benefits from the repetitive nature of saying a “any soothing, mellifluous sound,” regardless of its meaning to the individual29. Other researchers have found that meaningful phrases are better and later research has shown that having a meaningful component to mental focus can improve outcomes. 21,30,31,32 There appears to be a difference in mental and physical health outcomes when an intentional, meaningful focus of attention is used to reduce stress. However, this concept has not been explicitly tested in the context of frequent migraineurs. It is unknown whether a meaningful cognitive focus results in different outcomes than basic distraction with regard to negative emotions or migraine headache pain.
Gonzalez and team33 found that the post-headache experiences, particularly life limitations, are a serious concern for individuals with frequent migraines. Therefore, it is both headache pain, and the negative life impact even after the pain recedes, that impacts migraineurs. In a choice format conjoint analysis of adults aged 18 years or older, hypothetical treatments that limited the duration of headache symptoms without allowing them to resume their daily activities for 16 hours after a headache, on average, were viewed as less than half as good as treatments that limited both headache and post-headache symptoms. Therefore, patients with migraines were far more focused on perceived impact of post-headache symptoms on social functioning and daily activities than the migraine headache itself.
Current Study
All of these factors suggest the quality of life of individuals suffering from migraines may benefit from a psychological treatment designed to reduce the frequency of migraine headaches, while still allowing individuals to function in their daily lives. The current study aims to compare meditations using focused and meaningful cognitive practices (Spiritual meditation, Internally-focused secular meditation, and Progressive muscle relaxation practices) to a cognitive distraction technique on migraine related pain and emotional outcomes after a one hour training and practice session in the participant’s randomly assigned technique and then independent practice of the technique for 30 days to assess for differences in trajectories of migraine headache frequency, or severity. The groups were categorized into two domains: Active management group (Spiritual meditation, Internally-focused secular meditation, and Progressive muscle relaxation) and cognitive distraction group (Externally focused distraction phrases). As previous research has not explicitly tested the required “dose” for these types of meditation techniques, we will also be exploring the duration of time needed to practice the techniques prior to seeing significant changes in migraine headache, frequency, or severity.
Specific Aims
We hypothesized that the active management group that used meaningful cognitive control strategies would have better migraine frequency or severity outcomes after engaging in the technique for a 30 day practice period compared to those who used only cognitive distraction techniques for migraine headaches after a single one hour training session in the participant’s randomly assigned technique.
2.1. Method
This study is a reanalysis of data from a longitudinal randomized controlled trial study examining the impact of meditation techniques and migraine headaches.27
Participants
Participants were recruited from psychology classes at a large mid-western university and the local community through flyers and advertisements in the local community surrounding the university. Participation was completely voluntary and participants did not receive any financial compensation. All research procedures were approved by the university’s Institutional Review Board. The study was not registered at clinicaltrials.gov as recruitment began prior to mandated registration. The inclusion criterion was a minimum age requirement of 18 years and experience of at least two migraine headaches1 in the previous month. Those with a history of diabetes or Raynaud’s syndrome were excluded from the study due to possible altered perception of pain. The participants were screened for migraine headaches using the ID Migraine Screener.34 Two or more positive responses to three yes/no questions qualify as a migraine headache. This measure has been previously used and has an established sensitivity of 0.81, specificity of 0.75, and a positive predictive value of 0.93.34
Procedures
After completing informed consent, participants were randomly assigned to a group meeting of 5–7 individuals using a random number generator using the RANDBETWEEN function in Microsoft Excel to develop a random order of numbers between 1 and 4 by an undergraduate Research Assistant who was blinded as to which intervention was designated by each number (which intervention was taught in group #1, group #2, etc). The blinded RA placed the group assignments in an envelope with the participant’s name on it to be given to the participant upon completion of their initial survey and basic study training. In the initial group meeting, participants received basic education about the study and informed consent was reviewed again. Participants then completed the initial survey (demographic, psychological, spiritual, health assessments), and taught how to use the daily headache logs. All data collection was completed by assessment RAs who were blinded to study hypotheses. After submitting their initial survey, participants received their envelope with their technique group number and directed to go to the designated room for their technique group. Technique training was a single one hour education and practice session that occurred immediately after the initial group meeting. Participants were not aware of the different types of techniques being taught in the study outside if their assigned technique. Classes were taught by post-bac Research Assistants who were trained on the study protocols by the study psychologists but were blinded as to the hypotheses of the study. They were supervised for adherence to the protocol scripts by the study psychologists via audiotapes of the education sessions. Participants in the meditation techniques were allowed to choose one of four phrases that they would meditate on throughout the next 30 days. Data collection was tied to a confidential participant number and group number so that data collection and assessment RAs were blinded as to the technique that the participant had been assigned. There was no overlap between the post-bac RAs that taught the intervention, the undergraduate RAs that completed the data collection procedures, and the RA that completed the randomization procedures.
Participants reported names and dosages of all headache related analgesic medication they took during the course of the study. This information was reported and submitted in their daily diaries. No participants were treated with preventative migraine medication; all migraine medication among study completers was commercially available analgesic medications. Two participants had frequent use of prescription abortive medication and benzodiazepines; both of these participants dropped out of the study prior to assessment Session 2 and were not included in the final data analysis. No participant had any changes to their medication regimens during the study.
Meditation Training
Each participant was trained in how to perform their assigned meditation/relaxation task using a training protocol script by a research assistant in a single one hour education and practice session immediately subsequent to the initial group session. RAs that taught the classes were blinded to the study hypotheses. With the training protocol script, participants were taught to sit in a quiet room, without any distractions (e.g. no television, radio). They were taught to wear comfortable clothing and told that they could sit in any position they would like, as long as they would not fall asleep. They were encouraged to pick a time during the day that they could use for their regular relaxation/meditation time. During the training and practice session, participants discussed problems that frequently arise among new practitioners of relaxation/meditation (e.g. losing focus) and how to solve the problem and continue relaxing/meditating.
Meditation practice consisted of repeating their choice of one of the optional phrases provided within their randomly assigned meditation type. Participants were asked to use the phrase to focus their meditation and to meditate 20 minutes/daily for 30 days and complete daily headache diaries. The emphasis was that they would repeat the phrase mentally rather than verbally, but if they felt it helped them enter the cognitive focus, they could speak the phrase out loud a few times to help them focus or re-focus their mind during their practice. Additional information about the study research methodology and the original analyses can be found in Wachholtz & Pargament.27
Using a random number generator, the participants were randomly assigned to one of the following four groups. In the Spiritual Meditation group (Group 1), participants were allowed to choose to focus on one of the four spiritual meditative phrases ‘‘God is peace,’’ ‘‘God is joy,’’ ‘‘God is good,’’ and ‘‘God is love.’’* In the Internal Secular Meditation group (Group 2), participants were allowed to choose from four internally focused positive self-reinforcement phrases: ‘‘I am content,’’ ‘‘I am joyful,’’ ‘‘I am good,’’ ‘‘I am loved.” In the External Secular Meditation group, participants were allowed to choose from four externally focused secular meditation phrases: ‘‘Grass is green,’’ ‘‘Sand is soft,’’ ‘‘Cotton is fluffy,’’ ‘‘Cloth is smooth.’, In the Relaxation group (Group 4), participants were taught progressive muscle relaxation with cognitive control of muscle tension, relaxation, and repeated body scans.27 The relaxation group was not provided a meditation phrase and instead instructed to focus their thoughts on identifying and reducing muscle tension in the body.
In each group, the participants were asked to practice the technique for 20 minutes per day for 30 days in a quiet environment, avoiding all possible distractions. Participants completed daily headache and practice logs. Groups 1, 2, & 4, were identified as active management groups that taught the participants an active emotional or physiological approach to migraine management. Group 3 was conceptualized as a cognitive distraction group. Group 3 provided cognitive activity, but it was not meaningfully focused. No adverse effects were reported during the study, including no increases in negative mood, headaches, or medication use.
Manipulation checks were made during this process to assess how participants perceived the intervention. Participants rated their relaxation level due to their assigned technique on a 5 point Likert scale (0–5), with higher levels indicating greater relaxation.
Daily Diaries
The participants logged their daily practice of technique, and reported whether they performed the technique for 20 minutes and submitted the logs daily via email.
Measures
Headache logs.
Participants completed daily headache diaries during each of the 30 days of the study. They submitted the diaries daily via email. Daily diaries consisted of questions including 1) migraine headache in the past 24 hours (Yes/No), 2) if yes, the severity of the migraine headache (0–10), and 3) if the participant consumed abortive or analgesic medications for a migraine headache including medication and dosage. Relative equi-analgesic doses and the effective analgesic dosage relationships among the participants’ migraine medications were assessed using the Oxford League Table of Analgesics in Acute Pain35. As none of the participants that completed the study used opioids, the relationships were normed to the equivalent of 1 gram of acetaminophen.
Emotions.
The participants also recorded their emotions on a daily basis on a 7 point scale where 1 represented “not at all” and 7 represented “very much”. The participants recorded their ratings on: happiness, sadness, calm, and anger. Participants also rated their general mood ranging from 1 (negative) to 7 (positive).
Analysis Plan
The present study expanded our analyses from our previous study utilized multi-level hierarchical linear growth modeling to examine change over time in participants’ self-reported level of pain across the 30 days of the diary study with adjustments for frequency of headache and medication use27. Data were organized in IBM SPSS 20.0 and analyzed in SSI’s HLM 7.2. Multi-level analysis was used because it can account for clustering of data within individuals and is robust against problems arising from issues of unequal cells sizes and independence of errors. Mixed effects models also can accommodate missing data points (individuals who did not provide data on one or more days during the duration of the diary study).
Predictors of change in self-reported pain and felt emotions over time were examined in several models. First, linear growth models were run to examine change in participants’ self-reported emotions (anger and happiness) over the 30 days of the intervention. Additional analyses examined group differences (active management vs. cognitive distraction) in anger and happiness intercepts and slopes. Primary analyses examined change in participants’ self-reported pain scores over the 30 days of the intervention. An initial model was run to examine the amount of clustering in the data as captured in the intra-class correlation (ICC). Next, a growth model was run with linear trend coefficients to examine the total amount of variance in intercepts and time slopes, and meditation group was added as a level 2 predictor of pain intercepts and linear slopes. Then participants’ emotions were added to the model as time-varying covariates along with time and group. Finally, piecewise growth models were run, which examined change in the self-reported pain over three-separate periods of the diary study: first 10 days, second 10 days, and final 10 days. Group was included in these models as a level 2 predictor.
3.1. Results
Descriptive Statistics
Initially, ninety-two individuals consented to participate in the study. Nine participants did not complete the study citing that the study took up too much time. Three participants did not submit logs for at least 15 days and were excluded from the analyses. The remaining participants created an analytical sample size of N = 80 (see Figure 1). The final sample consisted of 4 groups: Spiritual meditation (n = 18), internal secular meditation (n = 20), external secular meditation (n =21), and relaxation group (n = 21).
Figure 1.
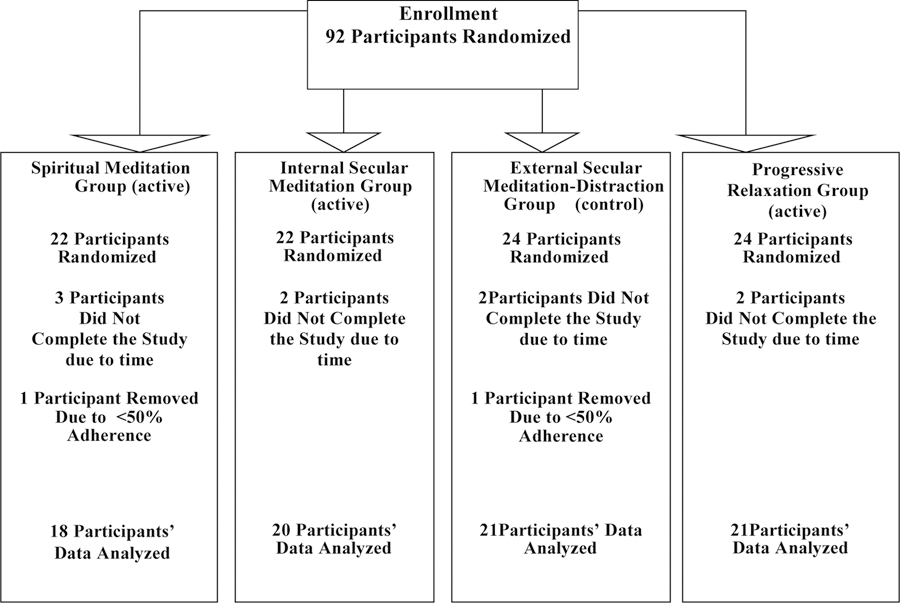
CONSORT Diagram of Participant Enrollment and Procedures
There was no difference in attrition across groups. One individual difference was identified between completer and non-completers; those who did not complete the study reported fewer headaches at pre-test as compared to completers.27 For further data on completers and non-completers, please see reference 27. Eighty participants completed the study (see Table 1; Figure 1). Power analyses utilizing an average effect/variance sizes from studies where participants meditated for less than or equal to 1 month indicate that 20 participants per cell are required to achieve statistical significance for a power level of .921.
Table 1.
Sample Description by Demographics
| Spiritual Meditation | Internal Secular Meditation | External Secular Meditation | Relaxation | |||
|---|---|---|---|---|---|---|
| All N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Gender | ||||||
| Male | 8 (10%) | 2 (11.1%) | 2 (10%) | 2 (9.5%) | 2 (9.5%) | |
| Female | 72 (90%) | 16 (88.9%) | 18 (90%) | 19 (90.5%) | 19 (90.5%) | |
| Pre-Study Headache/Mon | 12.1 (5.72) | 13.7 (6.36) | 12.8 (5.10) | 11.1 (5.24) | 11.4 (6.25) | |
| Race/Ethnicity | ||||||
| Non-Hispanic White | 58(73.4%) | 13 (72.2%) | 15 (78.9%) | 13 (61.9%) | 17 (81%) | |
| Non-Hispanic Black | 9 (11.4%) | 0 (0%) | 2 (10.5%) | 6 (28.6%) | 1 (4.8%) | |
| Hispanic | 5 (6.3%) | 1 (5.6%) | 1 (5.3%) | 1 (4.8%) | 2 (9.5%) | |
| Other/Multiracial | 7 (8.9%) | 4 (22.2%) | 1 (5.3%) | 1 (4.8%) | 1 (4.8%) | |
| Prayer | ||||||
| Never | 8 (10%) | 3 (16.7%) | 3 (15%) | 2 (9.5%) | 0 (0%) | |
| Formal | 8 (10%) | 2 (11.1%) | 3 (15%) | 1 (4.8%) | 2 (9.5%) | |
| During Stress | 29 (36.3%) | 6 (33.3%) | 8 (40%) | 7 (33.3%) | 8 (38.1%) | |
| Regularly | 35 (43.7%) | 7 (38.9%) | 6 (30%) | 11 (52.4%) | 11 (52.4%) | |
| Religion | ||||||
| Protestant | 34 (42.5%) | 7 (38.9%) | 6 (30%) | 9 (42.9%) | 12 (57.1%) | |
| Catholic | 31 (38.7%) | 8 (44.4%) | 11 (55%) | 5 (23.8%) | 7 (33.3%) | |
| Other | 9 (11.3%) | 2 (11.1%) | 2 (10%) | 5 (23.8%) | 0 (0%) | |
| Agnostic | 6 (7.5%) | 1 (5.6%) | 1 (5%) | 2 (9.5%) | 2 (9.5%) | |
| Religious Person | ||||||
| Not Religious | 11 (13.7%) | 4 (22.2%) | 2 (10%) | 4 (19%) | 1 (4.8%) | |
| Slightly | 19 (23.7%) | 4 (22.2%) | 7 (35%) | 3 (14.3%) | 5 (23.8%) | |
| Moderately Religious | 37 (46.3%) | 9 (50%) | 9 (45%) | 9 (42.9%) | 10 (47.6%) | |
| Very Religious | 13 (16.3%) | 1 (5.6%) | 2 (10%) | 5 (23.8%) | 5 (23.8%) | |
| Spirituality | ||||||
| Not Spiritual | 5 (6.3%) | 2 (11.1%) | 1 (5%) | 2 (9.5%) | 0 (0%) | |
| Slightly | 26 (32.5%) | 5 (27.8%) | 6 (30%) | 7 (33.3%) | 8 (38.1%) | |
| Moderately Spiritual | 39 (48.8%) | 10 (55.6%) | 11 (55%) | 10 (47.6%) | 8 (38.1%) | |
| Very Spiritual | 10 (12.5%) | 1 (5.6%) | 2 (10%) | 2 (9.5%) | 5 (23.8%) | |
Note: All group differences were insignificant at alpha 0.05 level. Fischer exact tests were run for variables with zero cells.
Description of the study sample (n = 80) with significant study variables are presented in Table 1. The study participants were primarily women (n = 72) with a mean age of 19 years (SD = 1.06), White race (n = 58), and slightly-to-moderately spiritual (n = 65). There were no significant differences between the groups on monthly headache frequency or severity.
Manipulation Check
No subjective difference was observed on the level of relaxation experienced between the groups during their assigned tasks. On an average participants rated the tasks ‘‘moderately’’ relaxing (F (3, 71) = 0.19, p = NS, η2 = .01; M = 3.4, SD = .97, range 3.4–3.5).
Self-reported emotions: Anger and happiness
Examining change in anger and happiness.
Separate linear growth models were run to examine change over the 30-day meditation intervention in participants’ self-reported levels of anger and happiness. Models indicated that participants’ self-reported levels of anger decreased (B = −.01, SE = .003, t(78) = −2.90, p = .005) while self-reported happiness increased (B = .015, SE = .003, t(78) = 4.05, p < .001) over the 30 days of the intervention.
Active Management group and emotion.
Active Management group (active management vs. cognitive distraction group) was added to these linear models as a level-2 predictor of intercepts and linear time slopes. The active management and cognitive distraction groups did not significantly differ in their happiness either their linear happiness slopes (B = −.009, SE = .008, t(77) = −1.009, p = .317) or linear anger slopes (B = .006, SE = .008, t(77) = −.766, p = .47) over the 30 days. While the active management group displayed significant decreases in self-reported anger (B = −.012, SE = .004, t(77) = −2.86, p = .005), however the cognitive distraction group’s reported anger did not change over the 30 days (B = −.005, SE = .007, t(77) = −.847, p = .40).
Self-reported pain models
Linear time models.
Baseline model.
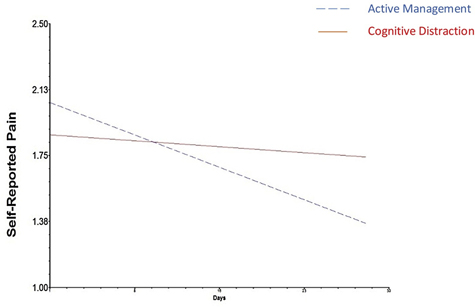
An initial linear growth model indicated that participants’ self-reported pain scores were moderately clustered within individuals (ICC = 0.11). In addition, there was a significant amount of inter-individual variance in self-reported pain intercepts (variance =.881, χ2= 167.34, p < .001) and time linear slopes (variance =.001, χ2 = 104.84, p = .027). Participants’ self-reported pain scores indicated a linear decrease over the 30-days of the meditation intervention (see Figure 2).
Fig. 2.
Linear change in self-reported pain for active management and cognitive distraction groups.
Active Management group and pain.
Similar to the model for emotions, Active Management group (active management vs. cognitive distraction group) was added to the model as a level-2 (individual level) predictor of self-reported pain intercepts and. Group accounted for 1% of the variance in self-reported pain intercepts and 6% of the variance in linear slopes. Although the slopes for the two groups did not significantly differ, the self-reported pain scores for the active management group significantly decreased over time, but it should be noted that the pain reports of the cognitive distraction group did not significantly change over time (Table 2).
Table 2.
Mixed Effects Models on Impact of Groups on Self-Reported Pain over a 30 Day Period
| Coefficient | Std. Err. | t-ratio | Sig. | |
|---|---|---|---|---|
| Intercept | 2.02 | .14 | 14.02 | <.001 |
| Linear Time slope | −.02 | .01 | −2.94 | .004 |
| Adding Management Group to the model | ||||
| Linear time X management group interaction | .020 | .016 | 1.18 | .182 |
| -Active Management Group slope | −.025 | 0.008 | −3.23 | .002 |
| -Cognitive Distraction Group slope | .004 | 0.013 | −0.35 | .725 |
Note: The hierarchical mixed effects models were run on respondents (n = 80) with migraine.
Std. Err.: Standard Errors; Sig.: Significance level
Including self-reported emotion.
Next, two separate models were run in which anger and happiness were added as time-varying covariates. Group remained in the model as an individual predictor. Both daily happiness (B = −.815 SE = .056, t(77) = −14.53, p < .001) and daily anger (B = .30 SE = .083, t(77) = 10.79, p < .001) scores were significant predictors of pain scores. However, with emotions in the model, pain scores no longer indicated significant linear change across time, and the linear self-reported pain slopes for both the cognitive distraction and the active management groups were both non-significant.
Piece-wise linear time models.
Baseline model (Table 3).
Table 3.
Piecewise Linear Models Predicting Self-Reported Pain for 10 Day Segments
| Coefficient | Std. Err. | t-ratio | Sig. | |
|---|---|---|---|---|
| First 10 days slope | −0.02 | 0.03 | −0.92 | 0.362 |
| Second 10 days slope | −0.01 | 0.02 | −0.39 | 0.702 |
| Third 10 days slope | −0.04 | 0.02 | −1.64 | 0.106 |
Note: The 30 day daily diaries period was divided into segments of 10 days for respondents (n = 80) with migraine. Std. Err.: Standard Errors; Sig.: Significance level.
A second series of models was run in which self-reported pain scores were examined in piece-wise linear models with time divided into three 10-day segments. Pain scores did not demonstrate significant linear change within any of the three separate 10-day segments.
Active Management Group (Table 4).
Table 4.
Mediation Group Predicting Time Piecewise (10-day) Time Slopes
| Coefficient | Std. Err. | t-ratio | Sig. | |
|---|---|---|---|---|
| First Segment | ||||
| Cognitive Distraction Group | .020 | .050 | .49 | .629 |
| Active Management Group | −.061 | 0.06 | −1.11 | .271 |
| Second Segment | ||||
| Cognitive Distraction Group | −.040 | 0.038 | −1.04 | .302 |
| Active Management Group | .003 | 0.022 | .17 | .875 |
| Third Segment | ||||
| Cognitive Distraction Group | .031 | 0.046 | .69 | .493 |
| Active Management Group | −.063 | 0.027 | −2.32 | .023 |
Note: The 30 day daily diaries period was divided into segments of 10 days for respondents (n = 80) with migraine. Std. Err.: Standard Errors; Sig.: Significance levels.
Similar to the linear time model, active management group was added to the model as a level-2 (individual level) predictor of self-reported pain intercepts and slopes with active management group compared to the cognitive distraction group. The pain scores for the cognitive distraction group did not significantly change during any of the 3 10-day segments. The pain scores for active management group did not significantly change across the first 10 day or the second 10-day segment. However, during the final 10-day segment, the active management group reported significant decreases in pain. The final 10-day slope for the active management group was different from the final 10-day slope segment for the cognitive distraction group (B = −.09, SE = .053, t (78) = −1.775, p = .05). Group accounted for 6.6% of the variance in the third 10-day time segment.
4.1. Discussion
Our study focused on examining the impact of meaningful cognitive focus during meditation and relaxation on pain and associated emotions among frequent migraineurs. While the four groups were initially conceptualized as having unique properties that would result in unique trajectories, the role of active vs distraction cognitive activities was a stronger distinction than specific types of active control. The results indicate that there was a significant decrease in self-reported pain over the course of 30 days among migraineurs practicing active management with the most significant change occurring after 20 days of practice. In our study, we identified that a cognitive distraction group using meaningless phrases had less efficacy to reduce self-reported pain or improve mood over 30 days of practice while the active management group using meaningful cognitive focus that included body-focused, self-esteem focused, or spiritually focused forms of meditation showed significant intra-group changes over the same 30 day period. We found that despite rating their daily practice of any meditation as equally relaxing, frequent migraineurs in the active management group reported significant reduction in self-reported pain over the 30 day period although the cognitive distraction group did not. In addition, the participants in the active management group also reported significant reduction in anger, however the cognitive distraction group, indicated no improvements in participant’s anger over the 30 day period. Stress is one of the frequent triggers of migraine,12,14 so reducing daily levels of experienced anger may be a key mechanism through which meditation interventions are able to alleviate migraine symptoms. In this study, daily experienced emotions (both anger and happiness) were significantly associated with daily self-reported pain with no difference among groups. In addition the effect of time on migraine pain was lost after addition of anger and happiness in the model. This finding may hint at the possible role of emotions that explain reduction in migraine pain. Also, the practice of daily meditation which is known to reduce stress and elevate mood can help improve the perceptions of extent of pain.
Overall, the results indicated that the active management was more effective at reducing pain symptoms over the 30 days of the study compared to the cognitive distraction group with significant group differences occurring after 20 days of practice. This could mean that meditation and relaxation techniques that provide meaningful and active management of the headaches may be more successful in relieving pain as compared to using techniques such as external secular meditation that focus more on mental distraction. We examined the impact of 30 day practice of meditation/relaxation on migraine outcomes and found that the active management group shows a better pain control in the final 10 days of the practice, as compared to cognitive distraction which shows no association with migraine pain outcomes.
The findings of our study are similar to previous research on use of meaningful phrases during meditation practice. Herbert Benson’s work on the difference between meaningful and meaningless mantra phrases as outlined in his book “Beyond the Relaxation Response”.30 This also echo’s other work 32,36 on use of mantra meditation among individuals with post-traumatic stress disorder. Lang et al. (2012) suggested that mantra repetition (with meaningful phrases) may induce a feeling of better wellbeing which can be attributed to personal perception/importance of the chosen spiritual word or phrase.37 In relation to the current study, this could mean that within the domains of techniques that elicit mindful distractions, the meaning of the phrase may hold greater power to relax the mind, as compared to meaningless phrases.36
On the other hand, a large body of Transcendental Meditation research has established that meaningful phrases are not necessary to elicit a relaxation response or beneficial effects. TM, a technique that helps in reducing stress with a daily practice of 20 minutes twice a day, has a evidence base for improvement in stress,38,39 anxiety,40 blood pressure reduction.41 TM studies have shown that despite the individual’s lack of knowledge of the meaning of the repetitive phrase (“mantra”), individuals show significant improvements in health and well-being.
The differential finding of TM using a “meaningless” phrase yet showing powerful outcomes, may be related to the definition of “meaning”. While the individual may not know the translation of their assigned mantra in his/her spoken language, there is an imbued spiritual meaning to the phrase which provides meaning for the practice to the individual. Thus the concept of “meaning” may not need to be a verbal translation, but an imbued meaning (spiritual or secular) may also suffice in making a practice meaningful to an individual.
Therefore this may account for the observation in our study that a simple cognitive distraction technique is not enough. It suggests that distraction-only pain management strategies, such as television etc. that do not provide intentional cognitive or physical stress management, will do very little over the long term to reduce the frequency or severity of migraine headaches. Simple cognitive distraction may have minimal long-term benefit to the practitioner, and is limited to the immediate effect of not concentrating on the pain.
The critical component of active management appears to be the consistent practice of the active management technique for approximately 20 days. The piece-wise models showed that repeated practice of the active management technique for 20 minutes per day for 20 days allows the individual to develop a skill that affects the individual’s psychological mood, and physiological response to stress that, in turn, changes the trajectory of migraine headache pain and negative mood. Simple cognitive distraction reduces the immediate pain of migraine headaches, but does not allow the individual to learn a skill to reduce the long-term frequency of headaches. Our study shows that the consistent practice of an active management technique may be the key component to reducing the negative impact of migraine headaches.
Limitations and Future Directions
The current study had a few limitations. The sample size was small (n = 80) and was restricted to primarily young adults (Mean = 19 years, SD = 1.10). This study also had a higher proportion of female participants (n = 72, 90 %), which may have led to overrepresentation of female gender. However, gender differences in the current study may not be associated with bias, since the prevalence of migraine in the general population is also higher in females than males (80%).33 The study also lacked verification of clinical indicators by a headache specialist. In this study, the Migraine ID screener (with well-established validity and reliability in a primary care setting) was used to assess presence of migraine, as was a self-reported diagnosis of migraine by their physician, but this was not validated with a full physical by a headache specialist in the context of the study. Additionally, it should be noted that the measures used were not PROMIS measures and were based on self-report. A notable strength of the study is the large number of waves which allowed for powerful intrapersonal analyses and allowed for the piecewise analyses. However, the groups were small, which limited our ability to fully capture potential individual differences. Thus, many of the between group analyses were significant, but some were only marginal, which potentially means the study was under-powered. The separate forms of meditation (e.g. spiritual meditation, internal secular meditation, and relaxation groups) may have separate pain and mood trajectories over a 30 day time period that could be identified by a larger study with more power. In a previous study, spiritual meditation was found to be more effective in increasing pain tolerance, reducing negative mood, among migraineurs in pre-post test results,50 however, the intent of the study was to differentiate between meaningful and non-meaningful phrases during meditation and their association with migraine outcomes over a 30 day period.
Future studies should focus on examining the impact of non-theistic spiritual, secular, and open-focus forms of meditation techniques that may help to better understand the critical components of meditation to include for individuals using meditation to reduce the severity, frequency or duration of migraine headaches. In addition, a wider spectrum of demographics with a larger sample size and a longer follow up time will help in better understanding of the long-term impact of different types of meditation techniques and provide a basis to clinically match specific techniques to specific patients.
Implications
Meditation and relaxation techniques are beneficial psycho-social therapies with minimal side effects, multiple psycho-physiological benefits, and reduced cost compared to pharmacological treatments. The active management group reported a significantly greater pain reduction over a period of 30 days with the greatest impact occurring after 20 days. The use of active management techniques may not only be responsible for clearing dysfunctional thought process but also help in addressing relieving other issues such as co-occurring stress. Primary and specialty care providers such as physicians, nurses, and mental health professionals who work with frequent migraineurs can encourage a simple to learn, free, low daily commitment (20 minutes), to engage in a meditation technique that can impact the frequency and severity of migraine headaches, as well as daily mood and reduction of anger levels very quickly. The providers should also make an effort to understand the preferences of the patients with migraine who may show better symptom relief with non-pharmacological therapies such as meditation as compared to taking medications. It should also be underlined that such therapies can be added as an alternative medicine to the pharmaceutical treatment.
Conclusions
Simple cognitive distraction techniques, such as mental distractions with phrases that do not provide cognitive or physical stress management may reduce immediate migraine headache pain, but may have limited long-term impact on migraine headache pain or negative mood. However, when practiced 20 minutes per day for at least 20 days, active cognitive-focus techniques using meaningful practices among frequent migraineurs may effectively reduce migraine headache pain.
Highlights.
There are many studies examining a single form of meditation, but few examine multiple meditation techniques to compare key ingredients that make a technique “successful” for patient’s pain management
In a longitudinal assessment, we found that meditative techniques integrating active cognitive controls work better to reduce migraine frequency, severity, and negative mood compared to passive or distraction techniques
Across active engagement meditation types, 30 minutes of daily practice for 20 days appeared necessary to reach efficacy
Acknowledgments
Funding: Funding for this study was provided by a NIH-NIDA grant (#K23DA030397) to AW.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
COI Statement: The authors have no conflicts of interest to declare.
Participants who did not feel that the term “God” reflected their spirituality could change the term to signify the focus of their spirituality. One participant chose to change the term to “Mother Earth.”
References
- 1.The International Headache Society. (2004). The international classification of headache disorders. Cephalalgia, 24 (Suppl 1) (2nd Edition), 1–160. [DOI] [PubMed] [Google Scholar]
- 2.Stewart WF, Wood GC, Razzaghi H, Reed ML, & Lipton RB (2008). Work impact of migraine headaches. Journal of Occupational and Environmental Medicine/American College of Occupational and Environmental Medicine. 50(7):736–745. doi: 10.1097/JOM.0b013e31818180cb [doi] [DOI] [PubMed] [Google Scholar]
- 3.Main A, Vlachonikolis I, & Dowson A The wavelength of light causing photophobia in migraine and tension-type headache between attacks. Headache. 2000;40(3):194–199. [DOI] [PubMed] [Google Scholar]
- 4.Rojahn J, & Gerhards F Subjective stress sensitivity and physiological responses to an aversive auditory stimulus in migraine and control subjects. Journal of Behavioral Medicine. 1986;9(2):203–212. [DOI] [PubMed] [Google Scholar]
- 5.Bigal ME, & Lipton RB The epidemiology, burden, and comorbidities of migraine. Neurologic Clinics. 2009;27(2):321–334. doi:10.1016/j.ncl.2008.11.011 ; 10.1016/j.ncl.2008.11.01110.1016/j.ncl.2008.11.011; 10.1016/j.ncl.2008.11.011 [DOI] [PubMed] [Google Scholar]
- 6.Arslantas D, Tozun M, Unsal A, & Ozbek Z Headache and its effects on health-related quality of life among adults. Turkish Neurosurgery. 2013;23(4):498–504. doi:10.5137/1019-5149.JTN.7304-12.0 ; 10.5137/1019-5149.JTN.7304-12.010.5137/1019-5149.JTN.7304-12.0; 10.5137/1019-5149.JTN.7304-12.0 [DOI] [PubMed] [Google Scholar]
- 7.Donovan E, Mehringer S, & Zeltzer LK A qualitative analysis of adolescent, caregiver, and clinician perceptions of the impact of migraines on adolescents’ social functioning. Pain Management Nursing: Official Journal of the American Society of Pain Management Nurses. 2013;14(4):e135–41. doi:10.1016/j.pmn.2011.09.002 ; 10.1016/j.pmn.2011.09.00210.1016/j.pmn.2011.09.002; 10.1016/j.pmn.2011.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kernick D, & Campbell J Measuring the impact of headache in children: A critical review of the literature. Cephalalgia: An International Journal of Headache. 2009;29(1):3–16. doi:10.1111/j.1468-2982.2008.01693.x ; 10.1111/j.1468-2982.2008.01693.x10.1111/j.1468-2982.2008.01693.x; 10.1111/j.1468-2982.2008.01693.x [DOI] [PubMed] [Google Scholar]
- 9.Tkachuk GA, Cottrell CK, Gibson JS, O’Donnell FJ, & Holroyd KA Factors associated with migraine-related quality of life and disability in adolescents: A preliminary investigation. Headache. 2003;43(9):950–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF, & AMPP Advisory Group. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–349. doi: 10.1212/01.wnl.0000252808.97649.21 [DOI] [PubMed] [Google Scholar]
- 11.Bloudek LM, Stokes M, Buse DC, Wilcox TK, Lipton RB, Goadsby PJ, … Martelletti P Cost of healthcare for patients with migraine in five European countries: Results from the international burden of migraine study (IBMS). The Journal of Headache and Pain. 2012;13(5):361–378. doi:10.1007/s10194-012-0460-7 ; 10.1007/s10194-012-0460-710.1007/s10194-012-0460-7; 10.1007/s10194-012-0460-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huber D, & Henrich G Personality traits and stress sensitivity in migraine patients. Behavioral Medicine (Washington, D.C.). 2003;29(1):4–13. doi: 10.1080/08964280309596169 [DOI] [PubMed] [Google Scholar]
- 13.Sadeghniiat K, Rajabzadeh A, Ghajarzadeh M, & Ghafarpour M Sleep quality and depression among patients with migraine. ActaMedicaIranica. 2013;51(11):784–788. [PubMed] [Google Scholar]
- 14.Waldie KE, & Poulton R Physical and psychological correlates of primary headache in young adulthood: A 26 year longitudinal study. Journal of Neurology, Neurosurgery, and Psychiatry. 2002;72(1):86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanteri-Minet M, Auray JP, El Hasnaoui A, Dartigues JF, Duru G, Henry P, … Gaudin AF Prevalence and description of chronic daily headache in the general population in france. Pain 2003;102(1–2):143–149. [DOI] [PubMed] [Google Scholar]
- 16.Adams J, Barbery G, & Lui CW Complementary and alternative medicine use for headache and migraine: A critical review of the literature. Headache. 2013;53(3):459–473. doi:10.1111/j.1526-4610.2012.02271.x ; 10.1111/j.1526-4610.2012.02271.x10.1111/j.1526-4610.2012.02271.x; 10.1111/j.1526-4610.2012.02271.x [DOI] [PubMed] [Google Scholar]
- 17.Wells RE, Bertisch SM, Buettner C, Phillips RS, & McCarthy EP Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. 2011;51(7):1087–1097. doi: 10.1111/j.1526-4610.2011.01917.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lecci L, & Wirth RJ Investigating the effects of physical discomfort on laboratory-induced mood states. Journal of Behavior Therapy and Experimental Psychiatry. 2000;31(3–4):231–247. [DOI] [PubMed] [Google Scholar]
- 19.Fan AY,Gu RJ, & Zhou AN MMPI changes associated with therapeutic intervention: A migraine control study. Headache. 1999;39(8):581–585. [DOI] [PubMed] [Google Scholar]
- 20.Zwart JA, Dyb G, Hagen K, Odegard KJ, Dahl AA, Bovim G, & Stovner LJ Depression and anxiety disorders associated with headache frequency. The nord-trondelag health study. European Journal of Neurology: The Official Journal of the European Federation of Neurological Societies. 2003;10(2):147–152. [DOI] [PubMed] [Google Scholar]
- 21.Wachholtz AB, & Pargament KI Is spirituality a critical ingredient of meditation? Comparing the effects of spiritual meditation, secular meditation, and relaxation on spiritual, psychological, cardiac, and pain outcomes. Journal of Behavioral Medicine. 2005.28(4):369–384. doi: 10.1007/s10865-005-9008-5 [DOI] [PubMed] [Google Scholar]
- 22.Perini F, & De Boni A Peripheral neuromodulation in chronic migraine. Neurological Sciences: Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2012;33 Suppl 1:S29–31. doi:10.1007/s10072-012-1039-4 ; 10.1007/s10072-012-1039-410.1007/s10072-012-1039-4; 10.1007/s10072-012-1039-4 [DOI] [PubMed] [Google Scholar]
- 23.Penzien DB, Rains JC, & Andrasik F Behavioral management of recurrent headache: Three decades of experience and empiricism. Applied Psychophysiology and Biofeedback. 2002;27(2):163–181. [DOI] [PubMed] [Google Scholar]
- 24.Marchand WR Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and zen meditation for depression, anxiety, pain, and psychological distress. Journal of Psychiatric Practice. 2012;18(4):233–252. doi:10.1097/01.pra.0000416014.53215.86 ; 10.1097/01.pra.0000416014.53215.8610.1097/01.pra.0000416014.53215.86; 10.1097/01.pra.0000416014.53215.86 [DOI] [PubMed] [Google Scholar]
- 25.Oberg EB, Rempe M,& Bradley R Self-directed mindfulness training and improvement in blood pressure, migraine frequency, and quality of life. Global Advances in Health and Medicine: Improving Healthcare Outcomes Worldwide. 2013;2(2):20–25. doi:10.7453/gahmj.2013.006 ; 10.7453/gahmj.2013.00610.7453/gahmj.2013.006; 10.7453/gahmj.2013.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tonelli ME, & Wachholtz AB Meditation-based treatment yielding immediate relief for meditation-naive migraineurs. Pain Management Nursing: Official Journal of the American Society of Pain Management Nurses. 2014;15(1):36–40. doi:10.1016/j.pmn.2012.04.002 ; 10.1016/j.pmn.2012.04.00210.1016/j.pmn.2012.04.002; 10.1016/j.pmn.2012.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wachholtz AB, & Pargament KI Migraines and meditation: Does spirituality matter? Journal of Behavioral Medicine. 2008;31(4):351–366. doi:10.1007/s10865-008-9159-2 ; 10.1007/s10865-008-9159-210.1007/s10865-008-9159-2; 10.1007/s10865-008-9159-2 [DOI] [PubMed] [Google Scholar]
- 28.Blanchard EB, Appelbaum KA, Radnitz CL, Morrill B, Michultka D, Kirsch C, … Jaccard J A controlled evaluation of thermal biofeedback and thermal biofeedback combined with cognitive therapy in the treatment of vascular headache. Journal of Consulting and Clinical Psychology. 1990;58(2):216–224. [DOI] [PubMed] [Google Scholar]
- 29.MacLean CR, Walton KG, Wenneberg SR, Levitsky DK, Mandarino JP, Waziri R, … Schneider RH Effects of the transcendental meditation program on adaptive mechanisms: Changes in hormone levels and responses to stress after 4 months of practice. Psychoneuroendocrinology. 1997;22(4):277–295. [DOI] [PubMed] [Google Scholar]
- 30.Benson H, & Proctor W Beyond the Relaxation Response. New York: Times Books. 1984. [Google Scholar]
- 31.Bormann JE, Becker S, Gershwin M, Kelly A, Pada L, Smith TL, et al. Relationship of Frequent Mantram Repetition to Emotional and Spiritual Well-Being in Healthcare Workers. The Journal of Continuing Education in Nursing. 2006;37(5). [DOI] [PubMed] [Google Scholar]
- 32.Bormann JE, Smith TL, Becker S, Gershwin M, Pada L, Grudzinski AH, & Nurmi EA Efficacy of frequent mantram repetition on stress, quality of life, and spiritual well-being in veterans: A pilot study. Journal of Holistic Nursing: Official Journal of the American Holistic Nurses’ Association. 2005;23(4):395–414. doi: 10.1177/0898010105278929 [DOI] [PubMed] [Google Scholar]
- 33.Gonzalez JM, Johnson FR, Runken MC, & Poulos CM Evaluating migraineurs’ preferences for migraine treatment outcomes using a choice experiment. Headache. 2013;53(10):1635–1650. doi:10.1111/head.12142 ; 10.1111/head.1214210.1111/head.12142; 10.1111/head.12142 [DOI] [PubMed] [Google Scholar]
- 34.Lipton RB, Dodick D, Sadovsky R, Kolodner K, Endicott J, Hettiarachchi J, … ID Migraine validation study. A self-administered screener for migraine in primary care: The ID migraine validation study. Neurology. 2003;61(3):375–382. [DOI] [PubMed] [Google Scholar]
- 35.Oxford Pain Site. (2007). Oxford League Table of Analgesics in Acute Pain. Retrieved May 12, 2007, from http://www.jr2.ox.ac.uk/bandolier/booth/painpag/Acutrev/Analgesics/Leagtab.html
- 36.Vujanovic AA, Niles B, Pietrefesa A, Schmertz SK, & Potter CM Mindfulness in the treatment of post-traumatic stress disorder among military veterans. Professional Psychology: Research and Practice. 2011;42:24–31. [Google Scholar]
- 37.Lang AJ, Strauss JL, Bomyea J, Bormann JE, Hickman SD, Good RC, & Essex M The theoretical and empirical basis for meditation as an intervention for PTSD. Behavior Modification. 2012;36(6):759–786. doi:10.1177/0145445512441200 ; 10.1177/014544551244120010.1177/0145445512441200; 10.1177/0145445512441200 [DOI] [PubMed] [Google Scholar]
- 38.Elder C, Nidich S, Moriarty F, & Nidich R Effect of transcendental meditation on employee stress, depression, and burnout: A randomized controlled study. The Permanente Journal. 2014;18(1):19–23. doi: 10.7812/TPP/13-102 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schneider RH, Grim CE, Rainforth MV, Kotchen T, Nidich SI, Gaylord-King C, … Alexander CN Stress reduction in the secondary prevention of cardiovascular disease: Randomized, controlled trial of transcendental meditation and health education in blacks. Circulation Cardiovascular Quality and Outcomes. 2012;5(6):750–758. doi:10.1161/CIRCOUTCOMES.112.967406 ; 10.1161/CIRCOUTCOMES.112.96740610.1161/CIRCOUTCOMES.112.967406; 10.1161/CIRCOUTCOMES.112.967406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Orme-Johnson DW, & Barnes VA Effects of the transcendental meditation technique on trait anxiety: A meta-analysis of randomized controlled trials. Journal of Alternative and Complementary Medicine (New York, N.Y.). 2013.doi: 10.1089/acm.2013.0204 [DOI] [PubMed] [Google Scholar]
- 41.Nidich SI, Rainforth MV, Haaga DA, Hagelin J, Salerno JW, Travis F, … Schneider RH A randomized controlled trial on effects of the transcendental meditation program on blood pressure, psychological distress, and coping in young adults. American Journal of Hypertension. 2009;22(12):1326–1331. doi:10.1038/ajh.2009.184 ; 10.1038/ajh.2009.18410.1038/ajh.2009.184; 10.1038/ajh.2009.184 [DOI] [PMC free article] [PubMed] [Google Scholar]