Abstract
Purpose of review:
The purpose of this review is to 1) illuminate prevalent methodological approaches and estimates of association between mental health diagnoses and suicide from the meta-analytic literature; 2) discuss key internal and external validity concerns with these estimates; and 3) highlight some of the unique attributes and challenges in US-based suicide research and opportunities to move the evidence base forward.
Recent findings:
Globally, there is considerable variability in measures of association between mental health disorders and suicide and a growing debate over methodological approaches to this research. A high suicide incidence makes the US an outlier, and the decentralized nature of US administrative data poses a unique challenge to data linkage that could otherwise advance this research.
Summary:
We offer methodological considerations for future research and discuss opportunities made possible by the recent expansion of the US National Violent Death Reporting System to a nationwide registry.
Keywords: suicide, mental health disorder, validity, generalizability
Introduction
Suicide is a leading cause of death internationally and within the United States (US). While global suicide mortality trends have declined over the last several years,(1) the US suicide rate increased 35% between 1999 and 2018, from 10.5 to 14.2 deaths per 100,000 population.(2) Suicide is now the 10th leading cause of death in the US, accounting for 48,344 deaths in 2018.(3)
Acknowledging this concerning trend, in 2012 the US Surgeon General released a National Strategy for Suicide Prevention Plan, which advocated for a comprehensive approach to suicide prevention involving both community and clinical action.(4) The Plan highlighted the widespread consensus that mental health disorders (MHDs), including mood disorders, anxiety disorders, borderline personality disorder, schizophrenia, and substance use disorders (SUD), are leading risk factors for suicide and suicidal behavior.(4)
The MHD-suicide association is widely assumed to be established and strong. Perhaps as a result, many publications in this area adopt a seemingly relaxed approach to the methods used to estimate the MHD-suicide association in the literature, with little attention to study specifics (e.g., populations studied, exposure definitions) and variability in magnitudes of associations. For example, it is quite common to find an introductory paragraph in suicide-related studies citing one eye-catching finding that 90% of suicide decedents had a diagnosable MHD, despite the literature’s wide variability in estimates and debate generated by this statistic.(5–10)
While estimate variability is not automatically a research shortcoming, it becomes problematic when 1) estimates are biased due to internal validity issues or 2) consumers of research attempt to generalize findings that may hold in certain populations, contexts, and circumstances and not others (e.g., external validity issues). Therefore, as researchers and practitioners develop and discuss suicide prevention interventions and policies, it is critical to have a clear understanding of the population characteristics, design assumptions, analytic methodologies, and potential biases underlying the estimates utilized. As such, the purpose of this review is to 1) illuminate some of the prevalent methodological approaches and estimates of association between MHDs and suicide, as captured in the meta-analytic literature, and 2) discuss key internal and external validity concerns with these estimates. Moreover, because the US has an increasing suicide trend characterized by unique risk factors, like firearm ownership and availability, we 3) also highlight some of the unique attributes and challenges in US-based suicide research and opportunities to move the evidence base forward.
Mental health disorders and suicide: findings from the meta-analytic literature
Many meta-analyses have examined the relationship between MHDs and suicide or suicidal behavior (Table 1). While these studies have contributed considerably to the field, they also illuminate some key limitations in the evidence base.
Table 1.
Select meta-analyses and large cohort studies examining associations between mental health and substance use disorders and suicide
| Source | Study design | Inclusion criteria | Exposure | Measure of Association (95% CI) | Effect Measure |
|---|---|---|---|---|---|
| Meta-analyses | |||||
| Harris et al. 1997 (11) | International Meta-analysis 249 studies |
• Cohort must have a defined disorder with two years of follow up • Less than 10% lost to follow up • Published observed suicide number and expected number, or sufficient information to estimate the expected number |
Major depression | 20.35 (18.27, 22.58) | SMR |
| Opioid use | 14.00 (10.79, 17.88) | ||||
| Any SUD | 5.47 (5.41, 6.09) | ||||
| Anxiety neurosis | 6.29 (5.33, 7.38) | ||||
| OCD | 11.54 (2.38, 33.72) | ||||
| Panic disorder | 10.00 (4.57, 18.98) | ||||
| Chesney et al. 2014 (12) | International Meta-review 20 studies |
• Included the most recent meta-analysis or review, or if not available then the most recent large (N>1000) study reporting risks for suicide | Depression | 19.7 (12.2, 32.0) | SMR |
| Opioid use | 13.5 (10.5, 17.2) | ||||
| Anxiety disorders | 3.3 (2.1, 5.3) | OR | |||
| Too et al. 2019 (15) | International Meta-analysis of linkage studies 13 studies |
• Comparisons of individuals with and without mental disorders based on a general population sample | Mood disorders | 12.3 (8.9, 17.1) | IRR |
| SUDs | 4.4 (2.9, 6.8) | ||||
| Anxiety disorders | 4.1 (2.4, 6.9) | ||||
| Conner et al. 2019 (40) | Meta-analysis: Psychological autopsies 35 studies |
• Living or dead controls • Descriptive data on mood disorders and/or alcohol or drug use disorders • In-person proxy interviews using a diagnostic instrument • Controls can be interviewed or a proxy can be interviewed for controls • Must include all suicides in a population or an age, sex, and/or location subgroup |
Major depression |
26.87 (15.58, 46.36) |
OR |
| Asia Europe North America |
7.95 (3.30, 19.16) 7.68 (2.60, 22.70) |
||||
| SUDs | |||||
| Asia Europe North America |
3.35 (2.00, 5.61) 6.54 (3.76, 11.39) 3.97 (1.99, 7.90) |
||||
| Large Cohort Studies | |||||
| Mortensen et al. 2000 (21) | Retrospective longitudinal record linkage case-control study (1980–1994) | • Population: Danish psychiatric inpatients • 811 cases, 79,871 controls • Exposure ascertainment: Psychiatric diagnosis (ICD-9) at most recent inpatient discharge from the Danish Psychiatric Central Register |
Reactive psychosis | 1.80 (1.28, 2.53) | IRR |
| Drug abuse | 1.08 (0.82, 1.42) | ||||
| Other psychiatric disorder | 1 (reference) | ||||
| Sonderman et al. 2014 (73) | Prospective longitudinal cohort survey-based study (2002–2009) | • Population: Black and White residents in Southeastern US • N=85,000 • Exposure ascertainment: “Has a doctor ever told you that you have depression or have you been treated for depression?” |
Depression | 3.05 (1.70, 5.48) | HR |
| Boggs et al. 2018 (29) | Retrospective longitudinal health-systems-based case-control study (2010–2013) | • Population: 8 US health systems (Mental Health Research Network) • 2,674 cases (1,298 firearm cases), 267,400 controls • Exposure ascertainment: ICD-9 codes within the previous 12 months of suicide for cases and matched index date for controls |
Any psychiatric disorder | OR | |
| Firearm Other |
5.51 (4.92, 6.14) 9.04 (8.06, 10.15) |
||||
| Anxiety disorder |
6.53 (5.68, 7.50) |
||||
| Firearm Other |
7.74 (6.84, 8.75) | ||||
| Depression | |||||
| Firearm Other |
7.29 (6.46, 8.23) 12.28 (10.96, 13.74) |
||||
OR=odds ratio; SMR=standardized mortality ratio; IRR=incidence rate ratio; SUD=substance use disorder; OCD=obsessive compulsive disorder
In an early example, Harris et al. (1997) reported standardized mortality ratios (SMRs) for suicide based on 249 studies from a range of countries dating back to the 1950s, with the majority published in the 1980s and 1990s.(11) This study appears regularly in suicide-related literature, with over 3,000 citations. Despite its landmark status, the lack of specificity in methods exemplifies common deficiencies in this literature. In explaining the inclusion and exclusion criteria for the study, the authors state that they selected papers with “defined disorders” without giving a clear source of the definitions. While it appears that these disorders are likely based on International Classification of Disease, version 9 (ICD-9-CM) codes, the ICD-9-CM codes utilized by individual investigators may not have been consistent across studies and information is lacking on when the patients were diagnosed or the setting of diagnosis. Although the authors suggest that they only included longitudinal designs, more specific information on the study populations and the rigor of the study designs is warranted. Without this synthesized information, it is difficult to form an impression of which patients are at highest risk or how these associations have trended over time and populations.
Meta-analyses and reviews published since Harris et al. (1997) have generally focused on the associations between specific MHDs, SUDs, and other conditions and suicide, often with highly divergent results.(12) Chesney et al. (2014) reviewed 20 such meta-analyses and published results for many MHDs and SUDs, along with a score reflecting the rigor of the publication in question (Table 1). Unfortunately, Chesney fails to distinguish between analyses of secondary (e.g., specialist) vs. primary care or general population samples, though suicide risks and associations may be quite different across these populations.(13) For example, in another meta-analysis, this one examining MHD prevalence among suicide victims, Bertolote et al. (2004) reported that among those who suicided, the risk of a mood disorder was higher in general population samples than in studies of psychiatric inpatients (44.4% vs. 20.8%).(14) This was also true of SUDs (19.2% vs 9.8%) but not of anxiety/somatoform disorders (2.7% vs 2.5%).(14) While attention to study population sources in this analysis is thorough, the authors included studies with extremely diverse methods of MHD ascertainment, which might also explain some of the population-level variability in their findings.(14)
Another common limitation of these meta-analyses is that they reflect data almost exclusively from “Western,” industrialized countries. Too et al. (2019) acknowledged evidence suggesting that MHD-suicide associations may be different in Asian countries, and further found that in their meta-analysis of mostly Scandinavian countries, the study location accounted for a great deal of the heterogeneity in effect estimates.(15) This underscores the importance of context in interpreting these estimates. In the following sections, we delve more deeply into these issues, highlighting common internal and external validity considerations in the MHD and suicide literature.
Internal validity concerns
Internal validity refers to the amount of systematic error in a study’s effect estimate(s). Estimates that have little or no systematic error are described as internally valid. There are three general categories of systematic error that can reduce a study’s internal validity: confounding, selection bias, and measurement or misclassification bias.(16) Below, we highlight key concerns prevalent in the MHD-suicide literature within each of these general categories.
Confounding control
Confounding occurs when effects of extraneous factors are blended with the actual effect of the exposure.(16) There are a number of factors that can and do get blended when attempting to estimate the effect of MHDs on suicide, and these factors can be illuminated using Directed Acyclic Graphs (DAGs).(17, 18) DAGs are graphs that make explicit researchers’ assumptions about relationships between the outcome, exposure, and covariates.
Figure 1 illustrates a possible DAG for the causal relationship between MHD and suicide, which is informed by scientific findings and underlying suicide theory—the Stress-Diathesis Model is a popular theory that explains suicide as the result of an interaction between 1) distal factors and personal vulnerabilities and 2) proximal stressors from life events.(19, 20) While DAGs, like the example in Figure 1, can and should be shaped by the best available evidence and theory, even when they illuminate a minimally sufficient set of factors that should be accounted for in the study design or analyses in order to remove bias, measurement of such factors (e.g., “personality traits”) might be very difficult or impossible to achieve on a population scale. Despite these limitations, DAGs support analysts in pinpointing and addressing known, measured confounders (e.g., by adjusting for them in a statistical model); in thinking through potential quantitative bias analyses for unmeasured confounders; and in helping identify mediators (e.g., factors on a causal pathway between the exposure and outcome) that if included in the model, could induce bias. In the DAG in Figure 1, “history of self-harm” and “history of suicide attempts” are considered mediators.
Figure 1.
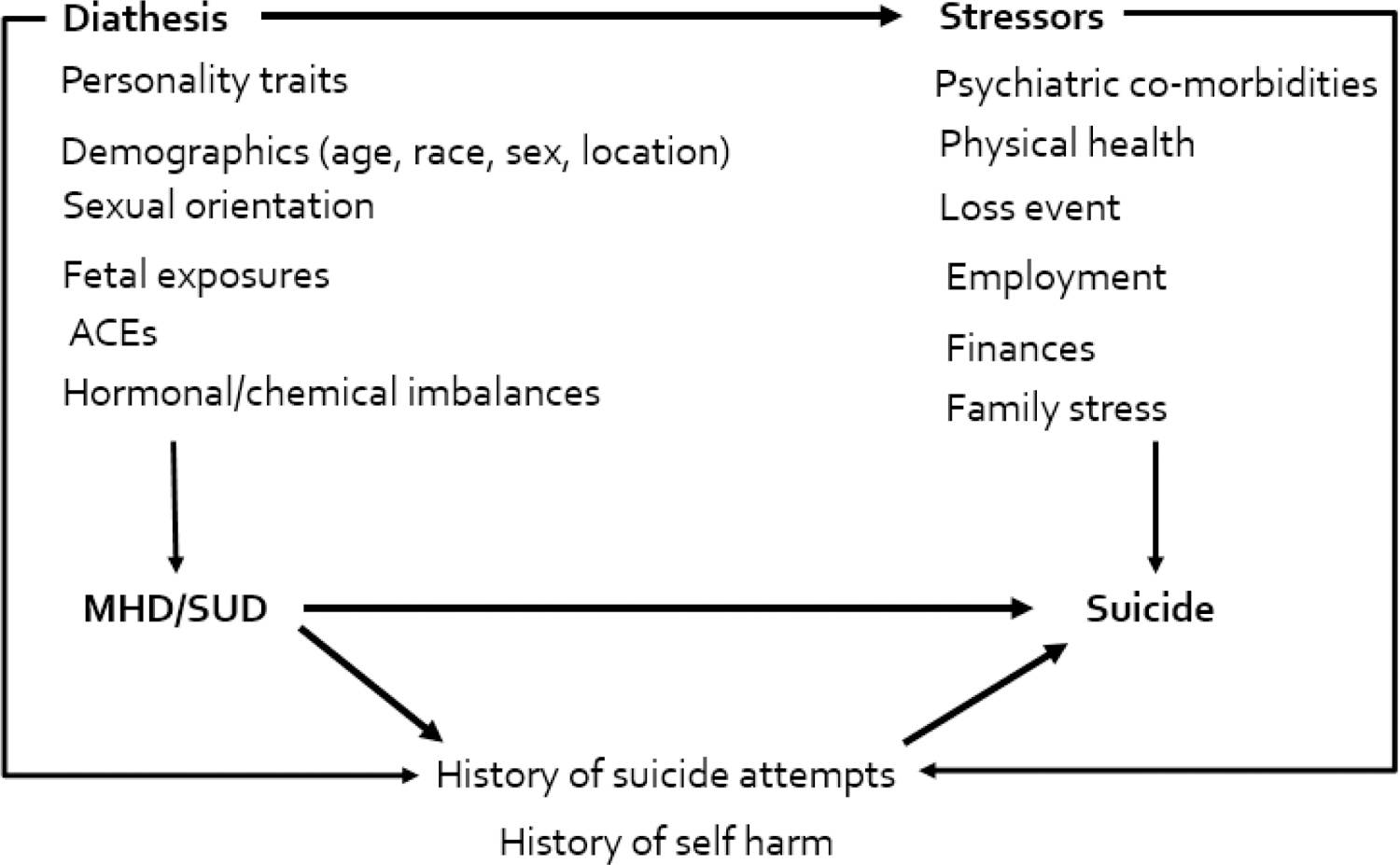
Example Directed Acyclic Graph (DAG) depicting potential causal and biasing pathways between mental health and substance use disorders and suicide
ACEs=Adverse Childhood Experiences; MHD=Mental Health Disorder; SUD=Substance Use Diagnosis
Unfortunately, to date, suicide models generally have not taken advantage of the abundant theory regarding causal pathways between MHDs and suicide. This may be due to at least two reasons: unfamiliarity with robust causal inference methods, such as DAGs, and/or an inability to adjust for a minimally sufficient set of factors because they are not measured in the data sources most commonly used, such as administrative data. Instead, it is the norm for MHD-suicide studies to report SMRs that adjust estimates to reflect solely the age and gender distribution of some broader population of interest and to ignore other confounders, such as socioeconomic status, race, or comorbidities.(12) This common reliance on age/sex-adjusted SMRs has hindered the research community’s conversation on confounding control. Moreover, the lack of causal inference theory underlying much of this research may make it more likely for mediators to be considered appropriate members of the adjustment set.(21) While inherent restrictions exist by data source, a much greater degree of attention needs to be paid to the topic of robust confounding control and causal inference in MHD-suicide research in order to inform future data collection, estimation approaches, and quantitative bias analyses meant to address the issue of residual confounding.
Selection bias
Selection bias occurs when the exposure-outcome relationship for a population under study differs from the population that should have been eligible for the study. It results from selecting the study population based on factors related to the exposure and/or outcome and can create a distortion in effect estimates.(16) Many MHD-suicide studies rely on diagnosis codes in health insurance administrative data and medical records to measure both the exposure and outcome. These may be problematic for many reasons. For example, in the US, where health insurance is largely privatized, different populations may have different levels of consistency in their health care coverage and utilization, which means some persons are more likely to be diagnosed (and therefore selected into the study) than others. Additionally, because suicidal behaviors and nonfatal suicide injuries are more likely to trigger a medical visit, the outcome can also increase the chance of selection in some studies. This differential selection according to exposure and outcome is commonly referred to as Berkson’s bias.(22) Tools are available to assess the magnitude of such bias,(16) and researchers should carefully consider how the population they are including in their study might differ from the population they are trying to make inferences about.
Measurement bias or misclassification
Measurement of the exposure and outcome can be a third challenge to internal validity in estimating the effect of MHDs on suicide. Below, we highlight some common sources of exposure and outcome misclassification in this research.
Exposure measurement
As noted above, diagnosis codes are an extremely common means of assessing MHDs and suicidal behaviors; however, in addition to the role they can play in selection bias, researchers should also evaluate their potential measurement bias. First, healthcare providers can be subject to social desirability bias and stigma surrounding MHDs and at times may not be willing to “label” a patient with a MHD, leading to under ascertainment of exposure in diagnosis codes. Second, for those with a diagnosable MHD, patients’ records are not always linked across providers, so a diagnosis such as a MHD, which is often treated in an outpatient setting, may not be present in hospital or primary care records. In this scenario, combining claims with medical records may address some of the missingness in MHD exposure. However, even in this case, because diagnoses are not associated with reimbursement, providers are poorly incentivized to be accurate and specific in their claims documentation. Finally, not all diagnosed illnesses are associated with a claim.
Another likely source of measurement error arises from the use of psychological autopsy (PA) methods for ascertaining MHD history. PA involves conducting interviews with a “proxy” (e.g., next of kin) following a death and is an extremely common study design in suicide research.(8) Several PA meta-analyses have been conducted (Table 1). The PA approach was first developed to assist medical examiners and coroners in their work and was never standardized for research purposes. It is vulnerable to inconsistencies and biases, including inconsistent numbers and types of proxies, lack of standardized proxy interview tools, and a lack of consensus on the source of controls (living or dead) for decedent suicide cases.(8) Recall bias, including bias introduced by interviewing people close to the recently deceased, has not been fully evaluated in these studies, and the time lapse between the death and interviews is often inconsistent or lengthy.(8, 13) The PA approach was used by Cavanah et al. (2003) to support the previously discussed (and debated) claim that 90% of people who suicide had a diagnosable MHD.(5) In a critique of the PA approach, Hjelmeland et al. (2012) question the reliability and validity of the approach, calling for the use of other, more systematic approaches for interviewing a high number of key informants around each suicide and taking into account the relationship with the deceased during data collection and analysis stages.(10)
Finally, exposure misclassification may be more common for specific types of suicide, such as firearm-related suicides. Studies show that individuals with easy access to highly lethal means are more likely to suffer a fatal outcome in the event of a suicide attempt. For example, research indicates that firearm owners are at increased risk of suicide,(23–27) often attributed to the fact that firearms are extremely lethal (85% of people who attempt suicide with a firearm die).(28) On average, very little time lapses between the decision to self-inflict lethal force and the act of suicide and time may be even shorter for those with access to highly lethal means. Boggs et al. (2018), using a linkage between US medical records and death records, found that out of 35 MHD and general medicine diagnoses thought to be predictive of suicide, 32 were more predictive of non-firearm suicide than firearm suicide (Table 1).(29) However, this could be a function of opportunities for accurate exposure measurement and, therefore, potential exposure misclassification. Because the time from onset of suicide ideation until death may be shorter among those using firearms, there may be a shorter window of time for these individuals to be seen by health professionals and diagnosed with MHD-related conditions. In a population like the US, where about half of suicides are by firearm, the effects of MHDs on suicide may, therefore, look different than in a country with a different distribution of methods used.
Outcome measurement
The outcome of suicide also may be prone to misclassification for several reasons. First, there may not be enough evidence to determine intent of death (e.g., unintentional overdose vs. suicide by overdose).(30) Second, deaths may be misclassified due to social desirability bias because suicide is stigmatized, and officials may rule them accidental or of undetermined intent to avoid causing embarrassment or financial penalty to family members. Third, officials may be less likely to classify the death as a suicide if the decedent does not fit the typical race and gender profile. The likelihood for suicide among minorities to be classified as “undetermined” is well-documented.(31)
External validity concerns
In addition to internal validity concerns, there are a number of external validity concerns that researchers and practitioners should note when trying to apply or “transport” study findings from one context to another. External validity refers to the generalizability of a study to the population of interest. The population of interest may be clinic-based, hospital-based, health systems-based, or geographically-based.
The presence of national health registries and more lenient policies surrounding personal health information in European countries often allow for study designs and results that are applicable to larger populations, such as an entire nation.(15, 21, 32–39) In comparison, investigators in countries like the US, which lack similar national health registries, tend to focus on subpopulations, such as the military or members of a common health insurance plan. Relatedly, the majority of suicide research appears to take place in European countries. For instance, in Berotlote et al.’s (2004) international meta-analysis, 45% of the suicide deaths came from the United Kingdom, and an additional 26% were contributed by Denmark.(14) As is commonly observed in meta-analyses on this topic, the US contributed just 4% of deaths.
However, as noted earlier, effect estimates of the association between MHDs and suicide vary considerably by population, highlighting the importance of context-specific studies and inferences, as opposed to smoothing over estimates from heterogeneous populations. Connor et al. (2019), demonstrated that major depression was much more predictive of suicide in Asia than in Western regions, while SUDs were less predictive (Table 1).(40) With that in mind, we agree with Rothman that, taken too far, “the pursuit of representativeness can defeat the goal of validly identifying causal relationships.”(16) Thus, some balance must be achieved between these two tensions, and researchers should consider that a small well-defined population with strong internal validity may be of more use than an estimate of effect for a larger population but with little confounding control.
United States-based research challenges
The US faces several distinct challenges in its suicide research and prevention efforts, given its unique firearm culture and fragmented data structures. The increasing rate of suicide in this country is likely attributable to a confluence of factors and could benefit from a larger body of rigorous research. We highlight key characteristics and challenges of US suicide-related research and follow with a discussion of promising paths forward.
Recent suicide research from the US is summarized in a review by Steele et al. (2018)(41), which underscores that US studies frequently focus on suicide risk factors for very specific populations (e.g., youth,(42–44) people of advanced age,(45, 46) prisoners,(47) veterans,(48–54) patients with specific diagnoses,(55) twins,(56) patients who otherwise screen as high risk for suicide(57–61), or Medicaid beneficiaries(58, 59, 62, 63)). Because national registries do not exist and the capacity to link data is often limited, much US research has targeted such smaller, high risk populations. Sources such as schools, prisons, the Veterans’ Health Administration, medical records, and senior care programs facilitate easier study population sampling and data collection than studies of the general population. As a result, relatively few US studies reflect the general population. However, the US suicide rate is increasing among a diverse range of demographic groups, not just these specialized populations.(64) Thus, there is a critical need for studies that assess relationships between MHDs and other risk factors and suicide in a wider swath of the population.
Another characteristic of US suicide research is a focus on risk factors for suicidal behavior (e.g., suicidal ideation, attempts, plans), as opposed to suicide itself. Again, this reflects the available data: while probabilistic linkages between medical records or claims data and death data certainly exist,(44, 58, 59, 63, 65–67) they do not approach the scope or detail available in other countries.(21, 34, 37) Meanwhile, US resources such as the National Comorbidity Survey(68–71) and The National Epidemiologic Survey on Alcohol and Related Conditions(72) offer nationally representative survey data but investigate non-fatal outcomes.
While US suicide-related research is generally typified by studies of smaller, specific populations and risk factors for suicidal behaviors, there are a few notable exceptions of larger, population-based suicide studies. The Southern Community Cohort Study was a longitudinal prospective study from 2002–2009 of 85,000 low income Black and White American patients in the Southeast and between the ages of 40–79 years.(73) In this sample, patients who reported that they had been diagnosed with or treated for depression had a hazard ratio for suicide of 3.05 (95% confidence interval (CI): 1.70, 5.48) compared to those who had not. Unfortunately, other MHDs were not assessed, and given depression assessment procedures, measurement of depression may have been subject to recall bias (Table 1).
The Mental Health Research Network is a more recent example of the potential for large, longitudinal, civilian data linkages in the US.(74) Using 2,674 suicides cases and 100 matched controls per case in eight health care systems,(75) the authors estimated associations between different healthcare settings and suicide based on the timing, number of visits, and history of MHD or SUD diagnoses. Results indicated an increased odds of suicide in every sub-category; for example, the adjusted odds of suicide within one week of being discharged from the hospital with a SUD diagnosis was 103.68 (95% CI: 66.38, 161.92) times the odds of suicide among outpatients who did not have an SUD.(75) While these examples constitute important suicide research efforts in the US, predictors of suicide are still vastly understudied, relative to the considerable public health burden of suicide.
Data linkage studies utilizing the National Violent Death Reporting System: A promising path forward
The National Violent Death Reporting System (NVDRS) is a unique US surveillance system with linkage potential that offers an opportunity to substantially strengthen the suicide-related evidence base. The NVDRS was developed by the US Centers for Disease Control and Prevention (CDC) in 2002, beginning with 6 states (Massachusetts, Maryland, New Jersey, Oregon, South Carolina, and Virginia).(76) It gradually expanded to include all 50 states, Puerto Rico, and the District of Columbia by 2018. The purpose of the system is to integrate detailed proximal death information on violent deaths, including suicide, homicide, deaths caused by law enforcement, deaths of undetermined intent, and unintentional firearm deaths in order to inform prevention efforts. For these deaths, death certificates, law enforcement reports, medical examiner reports, and toxicology reports are collected and linked, and detailed data from each of these sources is mined by state-level abstractors.
Linkages to NVDRS data offer the potential to overcome several of the biases discussed previously. Because it offers general population surveillance data, there is the potential to link NVDRS to general population controls from other surveillance systems (such as statewide hospital discharge data), which may reduce selection bias while affording sufficient power to evaluate for heterogeneity of effects. The rigorous data design instituted by NVDRS make this resource robust to outcome misclassification; however, for some exposures and confounders (i.e., those based on police statements collected from living associates), this resource is likely subject to the same bias introduced by PA studies.
Studies have linked health data to state VDRS data sources to more fully capture risk factors and trajectories leading to violent deaths, like suicides (Table 2). One Oregon study linked VDRS records on 112 veterans who suicided in 2000–2005 to Veteran’s Health Administration records in order to better understand health contacts in the year prior to death.(65) Rather than diagnoses, the researchers searched for screenings for depression, SUD, post-traumatic stress disorder, or suicidal ideation. They found that 68% of veterans were screened for depression and 81% for a SUD in the year prior to death. The authors also described health care utilization before the suicide, noting that almost half had a mental health-related contact and 55% were seen in a primary care setting in the year prior to death, revealing potentially important opportunities for intervention. In another notable example, Weis et al. (2006) linked South Carolina VDRS data to state hospital inpatient and emergency room billing records, as well as State Department of Mental Health data and criminal justice data.(66) Key findings indicated that 57% of suicide victims were hospitalized or had an emergency department visit, and 19% were seen by the Department of Mental Health in the year prior to death. As a final example, a study using Kentucky’s VDRS linked to statewide emergency department visit data (2008–2010) described events leading up to the suicide and estimated the impact of critical risk factors, like MHDs, on suicide.(77) Results indicated that the odds of suicide among those with MHDs was 1.93 (95% CI: 1.52, 2.45) times the odds of suicide among those without MHDs.
Table 2.
Studies involving linkage with state Violent Death Reporting System data
| Source | Linked databases | Sample | What VDRS added | Findings |
|---|---|---|---|---|
| Denneson et al. 2010 (65) | Oregon VDRS to Veterans Integrated Service Network 20 Data Warehouse | All veterans aged ≥18 who suicided in Oregon between 2000–2005 who had health care-related contact with a Department of Veterans Affairs Medical Center in the 12 months before death n=112 | Patient identifiers (name, DOB, DOD, last 4 of SSN), cause of death, veteran status, sex, race-ethnicity, education, marital status | • 63% had ≥1 primary care contact, 48% had ≥1 VA mental health-related contact in the year before death • 68% were screened for depression, and 41% for SI in year before death • Median number of days between last contact and death = 42 (range 0–358) • The majority who were screened denied SI |
| Basham et al. 2011(53) | Oregon VDRS to Veterans Integrated Service Network 20 Data Warehouse | All veterans aged ≥18 who suicided in Oregon between 2000–2005 n=968 | Patient identifiers (name, DOB, DOD, last 4 of SSN), cause of death, veteran status, sex, race-ethnicity, education, marital status | • 21.9% had any type of VA encounter • Of the patients with a psychiatric inpatient stay, 38.7% had their suicide within 30 days of discharge • 48% of decedents were prescribed antidepressants within 12 month of death |
| Weis et al. 2006 (66) | South Carolina VDRS to South Carolina Data Warehouse: inpatient and outpatient charges, Department of Mental Health records, and arrest data | All South Carolina suicide decedents in 2004 n=491 | Patient identifiers, law enforcement and coroner narratives (used to validate criminal history) | • 57.4% had a hospital or emergency room discharge in 2003 or 2004, with an average of 3 visits per person • 24.8% had a suicide attempt in 2003 or 2004 • 47.5% of the suicide attempt encounters were firearm-related • 16.7% died within 30 days of the final hospital encounter • Median number of days between last contact and death = 110 (many patients had more than 12 months of records linked) • 91 decedents had a median of 8 (range 1–1800+) visits with the Department of Mental Health, where depression was the most common diagnosis |
| Cerel et al. 2016 (77) | Kentucky VDRS to Kentucky Outpatient Services Claims Files | All Kentucky homicide (n=569) and suicide (n=1,599) decedents from 2008–2010 + ED controls (4/case) | Patient identifiers | • 10.7% of suicide decedents visited an ED in the 6 weeks prior to death • 22% of suicides occurred within 2 days of an ED visit • 9.9% of suicides had a self-injury code within 6 weeks of death • The odds of suicide among those with a mental disorder diagnosis was 1.93 (95% CI 1.52, 2.45) times the odds in those without a mental disorder diagnosis |
VDRS=Violent Death Reporting System; DOB=date of birth; DOD=date of death; SSN=social security number; VA=Veterans Administration; SI=suicidal ideation; ED=emergency department; CI=confidence interval
In sum, these examples demonstrate the feasibility of linking state-level VDRS data to health data. In doing so, they have provided a template, including linkage variables and approaches for “fuzzy” linkages, which can be replicated in future studies. However, one limitation of these studies is that they generally have not made use of the rich circumstantial information that VDRS provides surrounding suicides. VDRS data captures (in many cases) the decedent’s recent struggles, mental state, and conflicts prior to death. While this PA-like data come with limitations, these data could be leveraged strategically to flesh out or validate health care backgrounds provided through linkage. Presumably, similar circumstantial information could be collected from controls, or a selection of controls, in order to provide comparisons that could yield a more internally valid measure of association.
Conclusions
Suicide is a leading cause of death around the world, with increasing rates in the US. This likely stems from the US’s firearm culture, which has contributed to high availability of this extremely lethal option. In addition to ease of access to lethal force means, MHDs have long been recognized as key risk factors in the global setting. However, estimates of association between MHDs and suicide have typically been generated by studies situated in other countries. Moreover, many of these studies suffer from a variety of internal validity issues, including inappropriate confounding control, selection bias concerns, and potential exposure and outcome mismeasurement. This is due in part to limitations in population-level data resources globally and particularly in the US.
The NVDRS holds considerable potential for US-based research, offering the potential for larger study populations and more complete variable measurement and corresponding confounding control, particularly when linked with other large health-related databases (e.g., Medicaid, Medicare, medical records, etc.). Understanding unbiased, context-specific relationships between MHDs and death by suicide can help researchers and practitioners identify and appropriately customize interventions for populations at greatest risk.
Acknowledgements:
Financial support for this work was provided by the University of North Carolina at Chapel Hill Injury Prevention Research Center through an award (R49/CE0042479) from the Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. In addition, this research was partially supported by a National Research Service Award Pre-Doctoral/Post-Doctoral Traineeship from the Agency for Healthcare Research and Quality sponsored by The Cecil G. Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, Grant No. T32-HS000032.
Footnotes
COI:
Josie Caves Sivaraman has nothing to disclose.
Dr. Naumann has nothing to disclose.
Human and animal rights: This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Naghavi M, Global Burden of Disease Self-Harm C. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ. 2019;364:l94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hedegaard H, Curtin SC, Warner M. Suicide Mortality in the United States, 1999–2017. NCHS Data Brief. 2018(330):1–8. [PubMed] [Google Scholar]
- 3.Suicide: National Institute of Mental Health; [Available from: https://www.nimh.nih.gov/health/statistics/suicide.shtml.
- 4.2012 National Strategy for Suicide Prevention: Goals and Objectives for Action: A Report of the US Surgeon General and of the National Action Alliance for Suicide Prevention. Publications and Reports of the Surgeon General. Washington (DC) 2012. [PubMed] [Google Scholar]
- 5.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405. [DOI] [PubMed] [Google Scholar]
- 6.Hjelmeland H, Knizek BL. Suicide and mental disorders: A discourse of politics, power, and vested interests. Death Stud. 2017;41(8):481–92. [DOI] [PubMed] [Google Scholar]
- 7.Pridmore S Mental disorder and suicide: a faulty connection. Aust N Z J Psychiatry. 2015;49(1):18–20. [DOI] [PubMed] [Google Scholar]
- 8.Pouliot L, De Leo D. Critical issues in psychological autopsy studies. Suicide Life Threat Behav. 2006;36(5):491–510. [DOI] [PubMed] [Google Scholar]
- 9.Haw C, Hawton K. Suicide is a complex behaviour in which mental disorder usually plays a central role. Aust N Z J Psychiatry. 2015;49(1):13–5. [DOI] [PubMed] [Google Scholar]
- 10.Hjelmeland H, Dieserud G, Dyregrov K, Knizek BL, Leenaars AA. Psychological autopsy studies as diagnostic tools: are they methodologically flawed? Death Stud. 2012;36(7):605–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–28. [DOI] [PubMed] [Google Scholar]
- 12.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kapur N Suicide in the mentally ill. Psychiatry. 2009;8(7):257–60. [Google Scholar]
- 14.Bertolote JM, Fleischmann A, De Leo D, Wasserman D. Psychiatric diagnoses and suicide: revisiting the evidence. Crisis. 2004;25(4):147–55. [DOI] [PubMed] [Google Scholar]
- 15.Too LS, Spittal MJ, Bugeja L, Reifels L, Butterworth P, Pirkis J. The association between mental disorders and suicide: A systematic review and meta-analysis of record linkage studies. J Affect Disord. 2019;259:302–13. [DOI] [PubMed] [Google Scholar]
- 16.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 2008.
- 17.Howards PP, Schisterman EF, Poole C, Kaufman JS, Weinberg CR. “Toward a clearer definition of confounding” revisited with directed acyclic graphs. Am J Epidemiol. 2012;176(6):506–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rothman KJ, Greenland S, Lash TL. 3 ed2008. [Google Scholar]
- 19.Hamza CA, Stewart SL, Willoughby T. Examining the link between nonsuicidal self-injury and suicidal behavior: a review of the literature and an integrated model. Clin Psychol Rev. 2012;32(6):482–95. [DOI] [PubMed] [Google Scholar]
- 20.Hawton K, van Heeringen K. Suicide. Lancet. 2009;373(9672):1372–81. [DOI] [PubMed] [Google Scholar]
- 21.Mortensen PB, Agerbo E, Erikson T, Qin P, Westergaard-Nielsen N. Psychiatric illness and risk factors for suicide in Denmark. Lancet. 2000;355(9197):9–12. [DOI] [PubMed] [Google Scholar]
- 22.Westreich D Berkson’s bias, selection bias, and missing data. Epidemiology. 2012;23(1):159–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anglemyer A, Horvath T, Rutherford G. The accessibility of firearms and risk for suicide and homicide victimization among household members: a systematic review and meta-analysis. Ann Intern Med. 2014;160(2):101–10. [DOI] [PubMed] [Google Scholar]
- 24.Brent DA, Perper JA, Allman CJ, Moritz GM, Wartella ME, Zelenak JP. The presence and accessibility of firearms in the homes of adolescent suicides. A case-control study. JAMA. 1991;266(21):2989–95. [PubMed] [Google Scholar]
- 25.Brent DA, Perper JA, Moritz G, Baugher M, Schweers J, Roth C. Firearms and adolescent suicide. A community case-control study. Am J Dis Child. 1993;147(10):1066–71. [DOI] [PubMed] [Google Scholar]
- 26.Kellermann AL, Rivara FP, Somes G, Reay DT, Francisco J, Banton JG, et al. Suicide in the home in relation to gun ownership. N Engl J Med. 1992;327(7):467–72. [DOI] [PubMed] [Google Scholar]
- 27.Miller M, Azrael D, Hemenway D. Firearm availability and unintentional firearm deaths, suicide, and homicide among 5–14 year olds. J Trauma. 2002;52(2):267–74; discussion 74–5. [DOI] [PubMed] [Google Scholar]
- 28.Fowler KA, Dahlberg LL, Haileyesus T, Annest JL. Firearm injuries in the United States. Prev Med. 2015;79:5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boggs JM, Beck A, Hubley S, Peterson EL, Hu Y, Williams LK, et al. General Medical, Mental Health, and Demographic Risk Factors Associated With Suicide by Firearm Compared With Other Means. Psychiatr Serv. 2018;69(6):677–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bohnert ASB, Ilgen MA. Understanding Links among Opioid Use, Overdose, and Suicide. N Engl J Med. 2019;380(1):71–9. [DOI] [PubMed] [Google Scholar]
- 31.Huguet N, Kaplan MS, McFarland BH. Rates and correlates of undetermined deaths among African Americans: results from the National Violent Death Reporting System. Suicide Life Threat Behav. 2012;42(2):185–96. [DOI] [PubMed] [Google Scholar]
- 32.O’Neill S, Graham B, Ennis E. Prescribed pain and mental health medication prior to suicide: A population based case control study. J Affect Disord. 2019;246:195–200. [DOI] [PubMed] [Google Scholar]
- 33.Weiser M, Goldberg S, Werbeloff N, Fenchel D, Reichenberg A, Shelef L, et al. Risk of completed suicide in 89,049 young males assessed by a mental health professional. Eur Neuropsychopharmacol. 2016;26(2):341–9. [DOI] [PubMed] [Google Scholar]
- 34.de la Cruz LF, Rydell M, Runeson B, D’Onofrio B, Brander G, Rück C, et al. Suicide in obsessive–compulsive disorder: a population-based study of 36 788 Swedish patients. Molecular psychiatry. 2017;22(11):1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Qin P, Agerbo E, Westergard-Nielsen N, Eriksson T, Mortensen PB. Gender differences in risk factors for suicide in Denmark. Br J Psychiatry. 2000;177:546–50. [DOI] [PubMed] [Google Scholar]
- 36.Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: a national register-based study of all suicides in Denmark, 1981–1997. Am J Psychiatry. 2003;160(4):765–72. [DOI] [PubMed] [Google Scholar]
- 37.Madsen T, Agerbo E, Mortensen PB, Nordentoft M. Predictors of psychiatric inpatient suicide: a national prospective register-based study. J Clin Psychiatry. 2012;73(2):144–51. [DOI] [PubMed] [Google Scholar]
- 38.Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Arch Gen Psychiatry. 2005;62(4):427–32. [DOI] [PubMed] [Google Scholar]
- 39.Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Arch Gen Psychiatry. 2011;68(10):1058–64. [DOI] [PubMed] [Google Scholar]
- 40.Conner KR, Bridge JA, Davidson DJ, Pilcher C, Brent DA. Metaanalysis of Mood and Substance Use Disorders in Proximal Risk for Suicide Deaths. Suicide Life Threat Behav. 2019;49(1):278–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Steele IH, Thrower N, Noroian P, Saleh FM. Understanding Suicide Across the Lifespan: A United States Perspective of Suicide Risk Factors, Assessment & Management. J Forensic Sci. 2018;63(1):162–71. [DOI] [PubMed] [Google Scholar]
- 42.Sheftall AH, Asti L, Horowitz LM, Felts A, Fontanella CA, Campo JV, et al. Suicide in Elementary School-Aged Children and Early Adolescents. Pediatrics. 2016;138(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roche AM, Giner L, Zalsman G. Suicide in early childhood: a brief review. Int J Adolesc Med Health. 2005;17(3):221–4. [DOI] [PubMed] [Google Scholar]
- 44.Fontanella CA, Warner LA, Steelesmith DL, Bridge JA, Brock GN, Campo JV. A National Comparison of Suicide Among Medicaid and Non-Medicaid Youth. Am J Prev Med. 2019;56(3):447–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10(4):398–406. [PubMed] [Google Scholar]
- 46.Bartels SJ, Coakley E, Oxman TE, Constantino G, Oslin D, Chen H, et al. Suicidal and death ideation in older primary care patients with depression, anxiety, and at-risk alcohol use. Am J Geriatr Psychiatry. 2002;10(4):417–27. [PubMed] [Google Scholar]
- 47.Blaauw E, Kerkhof AJ, Hayes LM. Demographic, criminal, and psychiatric factors related to inmate suicide. Suicide Life Threat Behav. 2005;35(1):63–75. [DOI] [PubMed] [Google Scholar]
- 48.Bohnert KM, Ilgen MA, Louzon S, McCarthy JF, Katz IR. Substance use disorders and the risk of suicide mortality among men and women in the US Veterans Health Administration. Addiction. 2017;112(7):1193–201. [DOI] [PubMed] [Google Scholar]
- 49.Copeland LA, Finley EP, Bollinger MJ, Amuan ME, Pugh MJ. Comorbidity Correlates of Death Among New Veterans of Iraq and Afghanistan Deployment. Med Care. 2016;54(12):1078–81. [DOI] [PubMed] [Google Scholar]
- 50.Zivin K, Yosef M, Miller EM, Valenstein M, Duffy S, Kales HC, et al. Associations between depression and all-cause and cause-specific risk of death: a retrospective cohort study in the Veterans Health Administration. J Psychosom Res. 2015;78(4):324–31. [DOI] [PubMed] [Google Scholar]
- 51.Conner KR, Bohnert AS, McCarthy JF, Valenstein M, Bossarte R, Ignacio R, et al. Mental disorder comorbidity and suicide among 2.96 million men receiving care in the Veterans Health Administration health system. J Abnorm Psychol. 2013;122(1):256–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Conner KR, Bossarte RM, He H, Arora J, Lu N, Tu XM, et al. Posttraumatic stress disorder and suicide in 5.9 million individuals receiving care in the veterans health administration health system. J Affect Disord. 2014;166:1–5. [DOI] [PubMed] [Google Scholar]
- 53.Basham C, Denneson LM, Millet L, Shen X, Duckart J, Dobscha SK. Characteristics and VA health care utilization of U.S. Veterans who completed suicide in Oregon between 2000 and 2005. Suicide Life Threat Behav. 2011;41(3):287–96. [DOI] [PubMed] [Google Scholar]
- 54.Shepardson RL, Kosiba JD, Bernstein LI, Funderburk JS. Suicide risk among Veteran primary care patients with current anxiety symptoms. Fam Pract. 2019;36(1):91–5. [DOI] [PubMed] [Google Scholar]
- 55.Jones JE, Hermann BP, Barry JJ, Gilliam FG, Kanner AM, Meador KJ. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy Behav. 2003;4 Suppl 3:S31–8. [DOI] [PubMed] [Google Scholar]
- 56.Glowinski AL, Bucholz KK, Nelson EC, Fu Q, Madden PA, Reich W, et al. Suicide attempts in an adolescent female twin sample. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1300–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Arias SA, Miller I, Camargo CA Jr., Sullivan AF, Goldstein AB, Allen MH, et al. Factors Associated With Suicide Outcomes 12 Months After Screening Positive for Suicide Risk in the Emergency Department. Psychiatr Serv. 2016;67(2):206–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Olfson M, Wall M, Wang S, Crystal S, Bridge JA, Liu SM, et al. Suicide After Deliberate Self-Harm in Adolescents and Young Adults. Pediatrics. 2018;141(4). [DOI] [PubMed] [Google Scholar]
- 59.Olfson M, Wall M, Wang S, Crystal S, Liu SM, Gerhard T, et al. Short-term Suicide Risk After Psychiatric Hospital Discharge. JAMA Psychiatry. 2016;73(11):1119–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68(3):371–7. [PubMed] [Google Scholar]
- 61.Black DW, Winokur G, Warrack G. Suicide in schizophrenia: the Iowa Record Linkage Study. J Clin Psychiatry. 1985;46(11 Pt 2):14–7. [PubMed] [Google Scholar]
- 62.Fontanella CA, Saman DM, Campo JV, Hiance-Steelesmith DL, Bridge JA, Sweeney HA, et al. Mapping suicide mortality in Ohio: A spatial epidemiological analysis of suicide clusters and area level correlates. Prev Med. 2018;106:177–84. [DOI] [PubMed] [Google Scholar]
- 63.Fontanella CA, Warner LA, Hiance-Steelesmith DL, Sweeney HA, Bridge JA, McKeon R, et al. Service Use in the Month and Year Prior to Suicide Among Adults Enrolled in Ohio Medicaid. Psychiatr Serv. 2017;68(7):674–80. [DOI] [PubMed] [Google Scholar]
- 64.Web-based Injury Statistics Query and Reporting System (WISQARS): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2005. [Available from: www.cdc.gov/injury/wisqars.
- 65.Denneson LM, Basham C, Dickinson KC, Crutchfield MC, Millet L, Shen X, et al. Suicide risk assessment and content of VA health care contacts before suicide completion by veterans in Oregon. Psychiatr Serv. 2010;61(12):1192–7. [DOI] [PubMed] [Google Scholar]
- 66.Weis MA, Bradberry C, Carter LP, Ferguson J, Kozareva D. An exploration of human services system contacts prior to suicide in South Carolina: an expansion of the South Carolina Violent Death Reporting System. Inj Prev. 2006;12 Suppl 2:ii17–ii21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Becker M, Brown L, Ochshorn E, Diamond R. Risk for suicide among medicaid beneficiaries. Suicide Life Threat Behav. 2009;39(2):172–81. [DOI] [PubMed] [Google Scholar]
- 68.Pan YJ, Stewart R, Chang CK. Socioeconomic disadvantage, mental disorders and risk of 12-month suicide ideation and attempt in the National Comorbidity Survey Replication (NCS-R) in US. Soc Psychiatry Psychiatr Epidemiol. 2013;48(1):71–9. [DOI] [PubMed] [Google Scholar]
- 69.Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J Abnorm Psychol. 2006;115(3):616–23. [DOI] [PubMed] [Google Scholar]
- 71.Nock MK, Kazdin AE, Hiripi E, Kessler RC. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National Comorbidity Survey Replication. Psychol Med. 2006;36(5):699–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hoertel N, Franco S, Wall MM, Oquendo MA, Kerridge BT, Limosin F, et al. Mental disorders and risk of suicide attempt: a national prospective study. Mol Psychiatry. 2015;20(6):718–26. [DOI] [PubMed] [Google Scholar]
- 73.Sonderman JS, Munro HM, Blot WJ, Tarone RE, McLaughlin JK. Suicides, homicides, accidents, and other external causes of death among blacks and whites in the Southern Community Cohort Study. PLoS One. 2014;9(12):e114852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rossom RC, Simon GE, Beck A, Ahmedani BK, Steinfeld B, Trangle M, et al. Facilitating Action for Suicide Prevention by Learning Health Care Systems. Psychiatr Serv. 2016;67(8):830–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ahmedani BK, Westphal J, Autio K, Elsiss F, Peterson EL, Beck A, et al. Variation in patterns of health care before suicide: A population case-control study. Prev Med. 2019;127:105796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Blair JM, Fowler KA, Jack SP, Crosby AE. The National Violent Death Reporting System: overview and future directions. Inj Prev. 2016;22 Suppl 1:i6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cerel J, Singleton MD, Brown MM, Brown SV, Bush HM, Brancado CJ. Emergency Department Visits Prior to Suicide and Homicide: Linking Statewide Surveillance Systems. Crisis. 2016;37(1):5–12. [DOI] [PubMed] [Google Scholar]


