Abstract
Background
Transfusion-associated circulatory overload (TACO) is a rare life-threatening event associated with transfusion. This study aimed to identify any case of TACO in a large cohort of highly transfused patients with gastrointestinal tract (GI) bleeding.
Materials and methods
Data from patients who underwent an oesophago-gastro-duodenoscopy (OGD) were collected over one year from the gastroenterology service of a regional hospital.
Results
A total of 278 patients were identified, of which 81 required transfusion. In total, 811 blood components were transfused (red cell concentrate, platelets, plasma), leading to a cumulative TACO incidence of 12.3%. The probability of developing TACO was greater for patients aged ≥80 years (OR=3.9%; p=0.0058), with renal disease (OR=1.9%, p=not significant) and with cardiac disease (OR 11.1%; p=0.003). Patients with TACO had a lower overall survival (52 vs 20% at 3 years, p=0.034, HR=2.19, 95% CI: 1.04–4.63) compared to patients with cirrhosis without TACO (57 vs 28% at 3 years, p=0.003, HR=2.20, 95% CI: 1.30–3.72). Patients with an advanced stage of liver cirrhosis (Child Pugh c10 or more) were most likely to develop TACO.
Discussion
This study shows that within the GI setting TACO may be markedly under-reported. Clinical awareness for potential TACO development in GI patients with cardiac or renal disease or age >80 years is now required.
Keywords: TACO, gastroenterology, GI bleeding, transfusion, cardiac failure, fluid overload, incidence
INTRODUCTION
Transfusion-associated circulatory overload (TACO) is an important cause of morbidity and mortality according to the UK Serious Hazards of Transfusion (SHOT) scheme1 and is now considered to be one of the leading causes of transfusion-related fatalities2. TACO was the most common cause of transfusion-related deaths reported to the US Food and Drug Administration in 20183.
Transfusion-associated circulatory overload still remains under-reported; this is possibly due to a lack of awareness of the condition or because of sub-optimal haemovigilance3. TACO is characterised by acute pulmonary oedema which develops during or shortly after transfusion, and is associated with symptoms and signs of congestive cardiac failure. The pathophysiology of this condition is believed to be caused by increased hydrostatic blood pressure (due to fluid volume overload) leading to fluid leakage into the alveolar space, emulating congestive cardiac failure4. Cardiac or renal impairment and positive fluid balance, and advanced age, can be seen as a first-hit, whereas suboptimal fluid management or other components in the transfusion product may elicit the second hit, with both hits together resulting in the onset of TACO5,6.
The clinical signs and symptoms of TACO include dyspnoea, orthopnoea associated with tachycardia, hypertension, elevated central venous pressure, and pulmonary and/or sacral or ankle oedema7–10. Pulmonary oedema is apparent on chest X-ray and may be accompanied by cardiomegaly. TACO may be difficult to differentiate from transfusion-related acute lung injury (TRALI), as hypoxaemia and bilateral infiltrates on chest X-ray are features of both conditions5. For these reasons, TACO cases are often reported as TRALI, and TRALI as TACO. TACO treatment includes oxygen therapy, diuretics, continuous positive airway pressure (CPAP) and, in exceptional cases, therapeutic phlebotomy7.
Diseases of the gastrointestinal (GI) tract are likely to cause bleeding (melena, haematemesis, etc). Furthermore, patients with liver disease have haemostatic imbalance due to portosystemic venous shunting, resulting in engorged gastric and oesophageal varices prone to bleeding. In addition, these patients have a disturbed coagulation system, in tenuous equilibrium between pro- and anti-coagulant factors. Patients with liver cirrhosis have reduced albumin production and may be prone to develop fluid retention, ankle oedema and ascites. Some of these patients are on prophylactic beta blockade for the treatment of oesophageal varices. Porto-pulmonary hypertension (PPHTN) may exacerbate right heart failure due to a reduction in right ventricle cardiac output and increase in pulmonary vascular resistance (PVR). For these reasons, we also investigated patients within the GI setting with and without liver cirrhosis who developed TACO to further understand this transfusion-associated complication.
MATERIALS AND METHODS
We performed a retrospective review of all patients admitted to the GI department of a large regional hospital in northern Italy serving a population of over 500,000 people. All patients had a GI bleed requiring an oesophago-gastro-duodenoscopy (OGD). In addition, we conducted a review of serious transfusion-related adverse events (SAEs) notified to the local Transfusion Hospital Service, which has been a mandatory requirement in Italy since 200611.
We performed a further analysis of patients with a diagnosis of liver cirrhosis to determine the incidence of TACO in this subgroup.
All patients admitted consecutively to the Gastroenterology Department of the hospital over a one-year period (from 1st January 2015 to 31st December 2015) with an acute sudden upper GI bleed (haematemesis or melena) requiring an urgent OGD ± transfusion(s) of blood components were included in the review.
Haemoglobin (Hb), mean cell volume (MCV), haematocrit (HCT), red blood cell (RBC) count, white cell count, neutrophils, platelet (PLT) count, creatinine, prothrombin time (PT) and partial thromboplastin time (PTT) were recorded at admission (t0), 24 hours (h) post transfusion (t1) and 48 h post transfusion (t2): Information collected on SAE forms included: biochemistry, treatment and patient outcome, and, where TACO or TRALI were suspected, the rate of transfused blood products, total volume of blood products and other intravenous (IV) fluids transfused, and the use and timing of diuretics.
Transfusion-associated circulatory overload was defined in accordance with the criteria defined by the International Society of Blood Transfusion (ISBT) working party on haemovigilance12–14 (Table I). All patients recorded as having TACO were found to fulfill those criteria. The incidence of TACO per type of blood component issued was calculated using data made available by the local Transfusion Service of the South Tirol Region (Table II). Physiological parameters (oxygen saturation, blood pressure, heart rate), diuretic, total IV fluids administered, OGD data, causes of bleeding, and co-morbidities were also recorded.
Table I.
TACO criteria according to the International Society of Blood Transfusion (ISBT 2010)
| Patients classified with a TACO should exhibit: |
|---|
|
Definition: all patients should fulfill criteria “1)” and two or more of listed criteria in group “2)”. TACO: transfusion-associated circulatory overload.
Table II.
Total number and type of blood component transfused
| Component issued | TACO cases | Incidence per component | |
|---|---|---|---|
| RCC only | 675 | 10 | 1.48% |
| RCC and Plasma | 89 | 1 | 1.12% |
| RCC and Platelets | 47 | 1 | 2.12% |
| Total | 811 | 10 |
TACO: transfusion-associated circulatory overload; RCC: red cell components.
Statistical analysis
Continuous variables were summarised as median and interquartile range (IQR), while categorical covariates were summarised as absolute and percentage frequencies. Association between baseline characteristics of patients and presence of TACO or cirrhosis was estimated by means of logistic regression, and the effect of covariate was reported as odds ratio (OR) with 95% confidence interval (95% CI). Repeated measures of haematological parameters were analysed by means of ANOVA; p-values are as reported for the conservative F-test of Greenhouse-Geisser. Overall survival (OS) was defined from the date of first clinical evaluation to date of last clinical follow up or date of death from any cause. OS was estimated using the Kaplan-Meier method, and the association between survival and covariate was estimated utilizing the Cox proportional hazard regression model, with 95% CI. As this study was a retrospective clinical audit on regional transfusion SAEs, we did not plan a sample size. We considered a p-value <0.05 as moderate strength against the null hypothesis. All statistical tests were two-sided.
Serious transfusion-related adverse events
According to the Joint United Kingdom (UK) Blood Transfusion and Tissue Transplantation Services Professional Advisory Committee, SAE is defined as any untoward occurrence associated with the procurement, testing, processing, storage and distribution of tissues and cells that might lead to the transmission of a communicable disease, to death or life-threatening, disabling or incapacitating conditions for patients or which might result in, or prolong, hospitalisation or morbidity15.
RESULTS
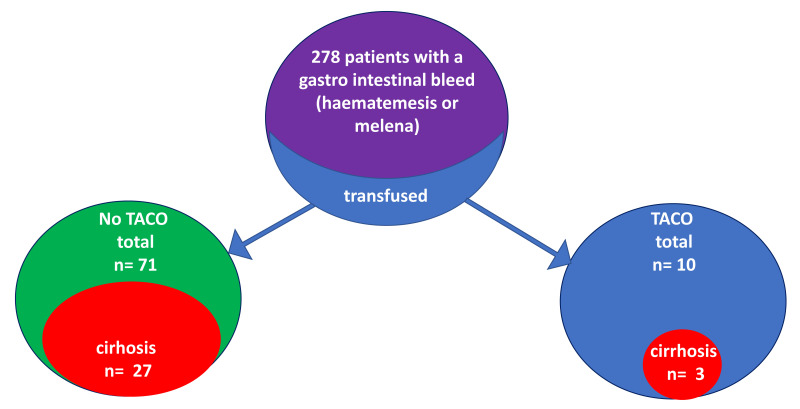
A total of 278 patients with GI bleeding (haematemesis or melena) requiring an OGD were admitted to the Gastroenterology Department during the study period. Of these, 116 patients were admitted with active GI bleeding, and 81 required transfusion of blood components (Figure 1). Of the 81 transfused, 10 developed TACO. Of the 71 who did not develop TACO, 38 (53%) were admitted because of melena, 27 (38%) because of haematemesis, and 6 (9%) with both. The data were analysed to further study TACO. A total number of 811 units of blood component were transfused over the study period. This was mainly red cell concentrate (RCC); however, combinations of RCC and plasma (n=89) or PLT (n=47) were also given (Table I). Of the 81 patients transfused, 10 (12.3%) fulfilled the criteria for TACO diagnosis. Of these, 60% (n=6) were male, 50% (n=5) were admitted with cardiovascular disease, 70% had co-existing renal failure, and 30% (n=3) had liver cirrhosis. Anticoagulant in the form of low molecular weight subcutaneous heparin (LMWH) was given to one patient with cirrhosis, a platelet-anti-aggregation agent (aspirin) to another and one patient received neither anticoagulant nor anti-aggregant therapy. The median period of time from hospital admission to TACO development was 4.5 days (range 1–22).
Figure 1.
Patient grouping
A total of 278 patients with gastrointestinal bleeding were studied. Out of these, only 81 required transfusions. Transfusion-associated circulatory overload (TACO) was identified in 10 cases (T-group); within this group only 3 cases also had liver cirrhosis (TL-group). Of the transfused patients, 71 had no evidence of TACO and 27 had liver cirrhosis. Patients without TACO and without liver cirrhosis were used as a second control (n=44).
All blood counts for patients who developed TACO (n=10) and for the control group (n=71) are before transfusion, at 24 h and at 48 h after transfusion; these were recorded and studied. The parameters of TACO patients did not show any statistically significant difference before and after transfusion (Table III). An ANOVA test for repeated measured comparing TACO and control group showed a statistical significance difference for PLT (p=0.001) with a lower number of PLT in the TACO group.
Table III.
Shown blood counts values, creatine and the coagulation times of patients before any transfusion, at 24 hour and at 48 hours after transfusion
| TACO | WBC×103/μL | RBC×106/μL | Neutrophils (%) | MCV (80–99 fl) | Hb (g/dL) | Ht (%) | PLT×103/μL | Creatinin (mg/dL) | PT (secs) | PTT (secs) |
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | 9.95±5.61 | 2.96±0.85 | 75.36+10.64 | 88.1±11.50 | 8.37±2.25 | 25.74±6.98 | 95±6.33 | 1.67±1.47 | 1.33±0.19 | 0.99±0.09 |
| 24h post | 7.53±5.95 | 3.40±0.52 | 75.12+12.67 | 88.67±7.45 | 9.63±1.21 | 29.99±4.17 | 87±4.23 | 1.56±1.46 | 1.32±0.07 | 1.09±0.05 |
| 48h post | 7.37±4.40 | 3.38±0.44 | 67.53+12.14 | 87.42±7.55 | 9.46±0.97 | 29.38±2.56 | 91±6.32 | 1.39±1.30 | 1.43±0.32 | 1.03±0.08 |
| pvalue | p=0.142 | p=0.137 | p=0.233 | p=0.506 | p=0.139 | p=0.097 | p=0.436 | p=0.261 | p=0.393 | p=0.455 |
Note, an ANOVA test for repeated measured comparing data of transfusion-associated circulatory overload (TACO) patients versus control identified a statistical significance difference for platelets only (p=0.001). WBC: white blood cell count; RBC: red blood cell count; MCV: mean cell volume; Hb: haemoglobin; Ht: haematocrit; PLT: platelet count; PT: prothrombin time; PTT: partial thromboplastin time; secs: seconds; h: hours.
No statistical significance was noted between the transfused patients who developed TACO and those who did not across a number of physiological parameters including: blood pressure, O2 saturation, heart rate and diuretic administration. However, patients who developed TACO were significantly older and had a high incidence of cardiac disease (Table IV) (Online Supplementary Content, Table SI). The probability of developing TACO was higher for those patients aged ≥80 years (OR=3.9%; p=0.0058) and with cardiac disease (OR 11.1%; p=0.003). Patients with cirrhosis were less likely to present with melena (25 vs 52%; p=0.012) than haematemesis (62 vs 30%; p=0.002) and were mostly <80 years of age (49 vs 27%; p=0.029).
Table IV.
Demographic data and comorbidities of transfusion-associated circulatory overload (TACO) cases
| Case | Gender | Age years | Liver cirrhosis | Dyspnoea | Cardiac disease | Hypertension | Renal failure | Melena | Haematemesis | Alive or † |
|---|---|---|---|---|---|---|---|---|---|---|
| #1 | M | 82 | no | no | none | yes | yes | yes | no | † |
| #2 | F | 75 | yes | yes | cardiac failure | no | no | yes | yes | alive |
| #3 | M | 79 | no | no | MI | no | yes | yes | no | alive |
| #4 | M | 86 | no | yes | cardiac failure | no | yes | yes | no | † |
| #5 | F | 81 | no | no | MI | no | no | yes | no | † |
| #6 | F | 81 | yes | no | none | yes | yes | yes | no | † |
| #7 | F | 85 | no | yes | AF | yes | yes | yes | no | † |
| #8 | M | 84 | yes | no | none | yes | yes | yes | no | † |
| #9 | M | 91 | no | no | none | yes | yes | no | yes | † |
| #10 | M | 64 | no | yes | none | yes | no | no | yes | † |
MI: myocardial infarction; F. Female; M: male.
During the study period, a total of 811 blood components (RCC, PLT, plasma) were issued to the Gastroenterology Department of the hospital, resulting in a cumulative TACO incidence of 12.3%.
Liver cirrhosis
Of the 81 patients transfused, 30 had liver cirrhosis and 3 of these developed TACO. Of these patients, 2 presented with melena and the third with haematemesis. At endoscopy, all 3 had bleeding oesophageal varices requiring band ligation or sclerosing therapy and received a median infusion of 700 mL of albumin (or 14 vials, where 1 vial=50 mL of human albumin 20%). One patient received 10 RBC units and 1 unit of PLT but no plasma before TACO. Another patient received 6 RBC units, but no PLT or plasma, and the third patient received 4 RBC units and no PLT or plasma before decompensation. Median number of RBC units transfused was 3 (range 2–10). Median serum albumin level was 3.0 (range 1.7–3.6) g/dL. Median Hb level at admission was 8.8 g/dL (range 2.7–14.8); median Hb level at the TACO event was 8.9 (range 4.1–11.6) g/dL. Median value of creatinine levels at TACO time was 1.9 mg/dL (range 0.6–7.0). Patients with liver cirrhosis developed TACO earlier after 1–2 days, compared to patients without liver cirrhosis who developed TACO within a median of 9 days (exact Mann-Whitney test, p=0.008). All patients with stage F2 liver cirrhosis were also on prophylactic treatment with beta blockers to protect against oesophageal varices rupture.
Of the 27 with cirrhosis who were transfused, but who did not develop TACO, bleeding was due to melena (n=3; 12%), haematemesis (n=16; 59%), or both (n=8, 29%). At endoscopy, 19 patients (73%) had an esophageal or gastric variceal bleeding and 8 patients (29%) had gastric or duodenal bleeding caused by ulcerative lesions. Of this group, 6 received albumin infusions. The median dose of albumin infused was 450 mL (human albumin 20% 10 g/50 mL). Hb level at admission was 8.3 g/dL (range 4.9–11.7). Median value of creatinine levels was 1.3 mg/dL (range 0.6–3.2). Cardiac disease was documented in 3 out of the 27 patients: 2 with heart failure and one with atrial fibrillation. One patient was already receiving anti-aggregation treatment. No patient was started on anticoagulation. Serum creatinine level did not change over time (p=0.322). There was no significant difference in creatine levels in transfused patients with cirrhosis who developed TACO compared with those patients with cirrhosis who were transfused yet did not develop TACO (p=0.240).
Of the 71 patients transfused who did not develop TACO, 44 did not have liver cirrhosis. Median RBC units administered was 2.8±3.6 standard deviation; none of these patients received albumin infusions and data on serum albumin levels of this group are not available. Median Hb levels at admission was 8.6 g/dL (range 4.9–11.7); median creatinine level was 1.2 mg/dL (range 0.6–3.2).
Overall clinical co-morbidities
Of the 81 patients transfused, 33 (41%) had a pre-existing comorbidity, mainly cardiovascular, liver cirrhosis, respiratory or renal condition (Table V). Some patients presented with more than one comorbidity.
Table V.
Pre-existing conditions of all 81 transfused patients
| Pre-existing condition | Examples | n | % of patients |
|---|---|---|---|
| Cardiovascular | Angina, Myocardial infarction, Valve incompetence, Atrial fibrillation, Hypertension | 15 | 18% |
| Respiratory | Chronic obstructive airways disease, Respiratory infection, Pleural effusion, Asthma | 3 | 4% |
| Renal | Renal impairment, Renal failure | 7 | 8% |
| Malignancy | Both solid tumour and leukaemia | 4 | 5% |
| Surgical | Abdominal surgery, Mastectomy, Above knee amputation | 4 | 5% |
| Miscellaneous | Diabetes, Sepsis, Gastritis, Hepatic dysfunction | 4 | 5% |
| None | No reported underlying history | 48 | 59% |
Cardiovascular, respiratory or renal conditions were most frequently represented. Some patients had more than one underlying comorbidity.
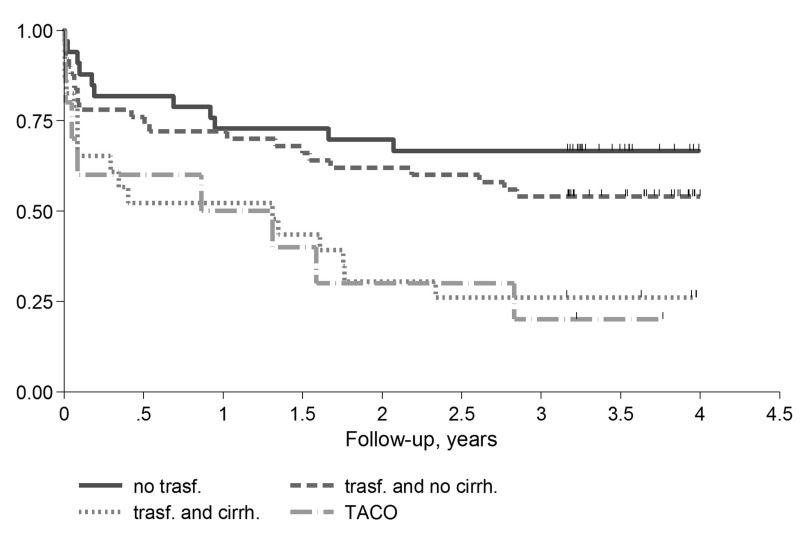
Outcome
Of the 116 patients admitted because of active GI bleeding, 59 deaths were identified over a median follow-up time of 3.5 years. OS at 3 years was 49% (95% CI: 40–58%) with a median OS of 2.8 years. The 3-year OS for patients not transfused was 67% (95% CI: 48–80%), 54% (95% CI: 39–67%) for patients transfused without cirrhosis or TACO, 26% (95% CI: 11–45%) for patients transfused with cirrhosis and 20% (95% CI: 3–47) for patients with TACO, respectively (p=0.002). Patients not transfused and those patients transfused without cirrhosis showed similar OS (HR 1.49, 95% CI: 0.73–33.06, p=0.275), while patients transfused with cirrhosis and TACO showed a higher risk of death (HR 3.15, 95% CI: 1.47–6.73, p=0.003; and HR 3.55, 95% CI: 1.42–8.81, p=0.007; respectively) (Figure 2 and Online Supplementary Table SI).
Figure 2.
Overall survival of 116 patients grouped according to: a) not transfused (no trasf.); b) transfused without cirrhosis (trasf. and no cirrh); c) transfused with cirrhosis (trasf. and cirrh.); d) transfusion-associated circulatory overload (TACO)
Overall, patients with TACO had a lower survival (20 vs 5 2% at 3 years, p =0.034, H R=2.19 9 5% C I: 1 .04–4.62) compared with patients without TACO. Similarly, patients with cirrhosis had a lower survival compared with patients without cirrhosis (28 vs 57% at 3 years, p=0.002, HR=2.20 95% CI: 1.30–3.72). TACO with liver cirrhosis had the highest mortality risk (HR=2.44, 95% CI: 1.46–4.08, p=0.001). Other covariates negatively affecting OS were age >80 years (HR=1.82, 95% CI: 1.09–3.05, p=0.023) and diuretic use before TACO (HR 2.02, 95% CI: 1.18–3.45, p=0.010). Of the 30 patients treated with diuretics before transfusion, 93% (n=28) also received diuretics post-transfusion. Furthermore, patients treated with diuretics either pre- or post-transfusion were shown to have an increased risk of mortality on multiple regression analysis (HR 2.02, 95% CI: 1.18–3.45, p=0.010, and HR 2.61, 95% CI: 1.56–4.37, p<0.001, respectively). Transfusion with plasma, was marginally negatively associated with OS, although this was not statistically significant (HR=2.17, 95% CI: 0.86–5.44, p=0.099). No statistically significant difference in the median volume of IV fluids administered to the TACO patients and those patients transfused who did not develop TACO was noted.
Serious transfusion-related adverse events
In addition to the 10 TACO cases reported by the unit during the study period, other SAEs recorded were: i) febrile non-haemolytic transfusion reaction n=4; ii) allergic reaction n=5. However, only the febrile non-haemolytic transfusion reactions had been correctly reported to the transfusion service.
DISCUSSION
This study, primarily, highlights the relevance of TACO within the GI setting. It is important to comment on the TACO definition used in our study. The study was designed in 2014 and carried out in 2015. Therefore, the TACO cases were identified using the definition made available by the ISBT in 201014. Comparing this TACO definition with the more recent definition produced in 2018 by the ISBT, a key difference is the time to develop any TACO event, which has been increased from 6 h to 12 h after transfusion2. Our study suffers from this limitation, and perhaps our data might be under-representative of all possible TACO cases occurring within 12 h.
Out of the 10 patients who developed TACO, it appears that in 9 of these TACO was triggered by cardiac or renal impairment or advanced age (>70 years); these are recognised to be first hit factors for TACO development. Only patient #10 did not have any cardiac or renal impairment and was aged <70 years. Taken together, this indicates that there may not be a direct pathophysiological relation between the GI setting and TACO, apart from the need for transfusion due to bleeding. However, this study clearly shows that clinicians should be aware of potential TACO development in GI patients with cardiac or renal impairment or age >80 years.
The high TACO incidence (12.3%) reported in this study might prompt gastroenterologists to be particularly vigilant when transfusing patients, especially the elderly, as TACO is associated with a very high mortality. Other studies using active surveillance15 have reported a TACO incidence of 1% (4:382) in orthopaedic patients6 and an incidence of 2% (1:356) in intensive care unit (ICU) settings16. Though the findings in this study might sensitise clinicians to the important risk associated with the use of blood transfusion, they should be interpreted carefully and merit further validation. The finding of higher TACO incidence in elderly patients is consistent with clinical observation and with previous reports17.
TACO and diuretics
The finding of a statistically significant association with TACO and the administration of diuretics is to be expected. However, we also showed a strong relationship between diuretics given pre-transfusion and TACO. These data may simply indicate that patients with an uncontrolled fluid balance are more likely to develop TACO. Murphy et al.4 suggest that slowing blood product infusion and prophylactic diuretic therapy may ameliorate the clinical status of TACO patients4. The same authors showed that TACO was most commonly reported in ICU patients or in patients with increased length of hospital stay, suggesting that TACO simply represents an epiphenomenon of further compromised cardiovascular status rather than a distinct clinical condition18. Nevertheless, this may be a real finding. Loop or thiazide diuretics drugs may cause hypovolaemia and hypokalaemia, which have been linked with cardiac arrhythmias and risk of death18. In addition, the ESCAPE trial19 and the study by Butler et al.20 have also highlighted a direct relationship between the use of highdose diuretics and mortality. It is also important to stress that, at present, pre-transfusion diuretics should not be withheld in high-risk patients due to our data, which is retrospective in nature. Continuous infusion of loop diuretics for the treatment of volume overload20 may also be preferable than pre-transfusion bolus injection to avoid electrolyte and fluid imbalances. However, this requires further investigation and validation, preferably within clinical trials.
TACO and cirrhosis
The development of TACO in patients with liver cirrhosis may be a consequence of an unstable haemodynamic circulation due to portal hypertension21. In particular, patients with cirrhosis are more likely to suffer from porto-pulmonary hypertension (PPHT). Although we do not have sufficient data to prove the presence of PPTH, we believe that this might in part be the reason for the worse outcome observed in patients with cirrhosis and also TACO. Furthermore, all patients with grade F2 oesophageal varices were also on beta blocker treatment but we were not be able to prove a link between this treatment and TACO (data not shown). Our finding that patients with advanced liver cirrhosis were more likely to develop TACO needs further confirmation in a larger study. Furthermore, this finding should be adjusted in larger series for the presence of cardiac or renal impairment and age >80 years. We suggest that increased vigilance may be warranted before transfusing any cirrhotic patient.
Study limitations
The incidence of TACO in our study has been calculated on component issues from a single centre retrospectively over one year. Patients were followed up over a period of only three years. For this reason, these data are limited and require further validation.
CONCLUSIONS
Clinicians should be aware of the increased risk of TACO in the elderly, and ensure that accurate fluid balance and/or body weight are recorded in all critically ill patients before transfusion and that diuretics are promptly administered where TACO is suspected. The majority of cases of TACO associated with transfusion of large volumes were also associated with older age and with underlying cardiovascular conditions22. Failure to recognise TACO and its associated complications is not uncommon and may result in under-reporting. These findings emphasise the importance of the role of haemovigilance and of training and education in transfusion medicine in hospitals to minimise the morbidity and mortality associated with TACO. Prospective, preferably multicentric, studies are now required to explore whether patients with liver cirrhosis are more likely to develop TACO.
Supplementary Information
ACKNOWLEDGEMENTS
We are deeply grateful to Ms Birgith Wirth from the Onlus Butterfly and Ms Sara Endrizzi from the Charity Association Onlus Chernobil Alto Adige for helping to raise research funding. We are also grateful to Dr Luigi Marcheselli (Department of Diagnostic, Clinical and Public Health Medicine, University of Modena and Reggio Emilia, Italy) for his kind advice and suggestions on statistics.
Footnotes
AUTHORSHIP CONTRIBUTIONS
MA designed the study, analysed data, performed data collection and wrote the paper. PA analysed data and wrote the paper. PM, RP, SG, VC, FA and AL reviewed data and the article, and approved the final version of the manuscript.
The Authors declare no conflicts of interest.
REFERENCES
- 1.SHOT [internet] Transfusion-associated circulatory overload (TACO) [Accessed on 06/04/2020.]. Available at: https://www.shotuk.org/wp-content/uploads/myimages/TACO-reporting-criteria_draft-Nov-2016-2.pdf.
- 2.Wiersum-Osselton JC, Whitaker B, Grey S, et al. Revised international surveillance case definition of transfusion-associated circulatory overload: a classification agreement validation study. Lancet Haematol. 2019;6:e350–8. doi: 10.1016/S2352-3026(19)30080-8. [DOI] [PubMed] [Google Scholar]
- 3.Food and Drug Administration (FDA) Fatalities reported to fda following blood collection and transfusion annual summary for fiscal year 2016. [Accessed on 06/04/2020.]. Available at: https://www.fda.gov/media/111226/download.
- 4.Murphy EL, Kwaan N, Looney MR, et al. TRALI Study Group. Risk factors and outcomes in transfusion-associated circulatory overload. Am J Med. 2013;126:357.e29–38. doi: 10.1016/j.amjmed.2012.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Semple JW, Rebetz J, Kapur R. Transfusion-associated circulatory overload and transfusion-related acute lung injury. Blood. 2019;133:1840–53. doi: 10.1182/blood-2018-10-860809. [DOI] [PubMed] [Google Scholar]
- 6.Semple JW, Rebetz J, Kapur R. Transfusion-associated circulatory overload (TACO): time to shed light on the pathophysiology. ISBT Science Series. 2019;14:136–9. [Google Scholar]
- 7.Popovsky MA. Transfusion-associated circulatory overload. ISBT Science Series. 2008;3:166–9. [Google Scholar]
- 8.Popovsky MA, Audet AM, Andrzejewski C., Jr Transfusion-associated circulatory overload in orthopedic surgery patients: a multi-institutional study. Immunohematology. 1996;12:87–9. [PubMed] [Google Scholar]
- 9.Gajic O, Gropper MA, Hubmayr RD. Pulmonary edema after transfusion: how to differentiate transfusion-associated circulatory overload from transfusion-related acute lung injury. Crit Care Med. 2006;34(Suppl 5):109–13. doi: 10.1097/01.CCM.0000214311.56231.23. [DOI] [PubMed] [Google Scholar]
- 10.Popovsky MA. Transfusion and lung injury. Transfus Clin Biol. 2001;8:272–7. doi: 10.1016/s1246-7820(01)00111-2. [DOI] [PubMed] [Google Scholar]
- 11.Gazzetta Ufficiale della Repubblica Italiana. 300. Dec 28, 2015. Decreto del Ministero della Salute 2 novembre 2015. [In Italian.] [Google Scholar]
- 12.Lin Y, Cohen R, Armali C, et al. Transfusion-associated circulatory overload prevention: a retrospective observational study of diuretic use. Vox Sang. 2018;113:386–92. doi: 10.1111/vox.12647. [DOI] [PubMed] [Google Scholar]
- 13.Parmar N, Pendergrast J, Lieberman L, et al. The association of fever with transfusion-associated circulatory overload. Vox Sang. 2017;112:70–8. doi: 10.1111/vox.12473. [DOI] [PubMed] [Google Scholar]
- 14.ISBT [internet] Transfusion-associated circulatory overload (TACO) Definition. 2018. [Accessed on 06/04/2020.]. Available at: https://www.isbtweb.org/fileadmin/user_upload/TACO_2018_definition_March_2019.pdf.
- 15.Gosmann F, Nørgaard A, Rasmussen MB, et al. Transfusion-associated circulatory overload in adult, medical emergency patients with perspectives on early warning practice: a single-centre, clinical study. Blood Transfus. 2018;16:137–44. doi: 10.2450/2017.0228-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rana R, Fernández-Pérez ER, Khan SA, et al. Transfusion-related acute lung injury and pulmonary edema in critically ill patients: a retrospective study. Transfusion. 2006;46:1478–83. doi: 10.1111/j.1537-2995.2006.00930.x. [DOI] [PubMed] [Google Scholar]
- 17.Piccin A, Cronin M, Brady R, et al. Transfusion-associated circulatory overload in Ireland: a review of cases reported to the National Haemovigilance Office 2000 to 2010. Transfusion. 2015;55:1223–30. doi: 10.1111/trf.12965. [DOI] [PubMed] [Google Scholar]
- 18.Cooper HA, Dries DL, Davis CE, et al. Diuretics and risk of arrhythmic death in patients with left ventricular dysfunction. Circulation. 1999;100:1311–5. doi: 10.1161/01.cir.100.12.1311. [DOI] [PubMed] [Google Scholar]
- 19.Hasselblad V, Gattis Stough W, Shah MR, et al. Relation between dose of loop diuretics and outcomes in a heart failure population: results of the ESCAPE trial. Eur J Heart Fail. 2007;9:1064–9. doi: 10.1016/j.ejheart.2007.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Butler J, Forman DE, Abraham WT, et al. Relationship between heart failure treatment and development of worsening renal function among hospitalized patients. Am Heart J. 2004;147:331–8. doi: 10.1016/j.ahj.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 21.Nair H, Berzigotti A, Bosch J. Emerging therapies for portal hypertension in cirrhosis. Expert Opin Emerg Drugs. 2016;21:167–81. doi: 10.1080/14728214.2016.1184647. [DOI] [PubMed] [Google Scholar]
- 22.Leto L, Aspromonte N, Feola M. [Continuous infusion versus bolus injection of loop diuretics in acute heart failure: a literature review]. G Ital Cardiol (Rome) 2012;13:263–72. doi: 10.1714/1056.11558. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.