Abstract
Aims:
We aimed to evaluate the readiness and predictors of diabetes service capability at the level of primary care in Bangladesh as an illustrative instance of readiness for diabetes care in low- and middle-income countries (LMICs).
Methods:
We used data from the 2014 Bangladesh Health Facility Survey (BHFS), a cross-sectional, nationally representative survey (n = 1596 health facilities). We constructed a diabetes-specific readiness index to assess diabetes service readiness in facilities with outpatient capability and used multivariable regression analysis to evaluate contextual predictors of diabetes service readiness.
Results:
Three-hundred and forty-five facilities with outpatient and diabetes service capability were included. Mean readiness for diabetes service capability on a scale of 0–100 was 24.9 (95%CI: 20.8–28.9) and was lowest in rural settings, districts with high social deprivation, and public facilities, where diabetes diagnostic equipment and medications were largely unavailable. Facility type was the strongest, independent predictor of diabetes service readiness.
Conclusions:
Diabetes service readiness in outpatient facilities in Bangladesh was low, particularly in public facilities, rural settings, and districts with high social deprivation. .These findings could inform policies aimed at improving diabetes care in areas of high unmet need and may serve as a model to assess diabetes service readiness in other LMICs.
Keywords: Diabetes service readiness, Low- and middle-income countries, Disparities in diabetes care, Diabetes in Bangladesh
1. Introduction
Globally, an estimated 463 million adults are living with diabetes mellitus, a number projected to grow to 700 million by 2045 [1]. While the rise in diabetes prevalence has been a worldwide phenomenon, the rate of increase in prevalence over the past decade has been fastest in low- and middle-income countries (LMICs)— a trend projected to continue [1,2]. Despite this growing burden, health systems in these lower resource settings are also expected to be least prepared for the demands posed by this condition [3]. Yet, little is known about health system preparedness (hereafter “readiness”) for diabetes service provision at the level of primary care in LMICs, which hinders priority setting and efficient resource allocation.
Among LMICs, Bangladesh has emerged as an important focus of the diabetes pandemic in South Asia, recently ranked as one of the ten countries with the highest number of people with diabetes worldwide—a figure projected to double by 2045 [4]. Despite demonstrating exceptional health progress over the past few decades [5], the growing burden of diabetes has become a major challenge for the health system in Bangladesh and for the introduction of Universal Health Coverage [6,7]. Although a national plan for tackling non-communicable diseases (NCDs) exists, current activities for the management of NCDs have been largely fragmented and have not been commensurate with the scope and complexity of the problem [8].
While several studies have described diabetes service readiness of health systems in LMICs [7,9–13], an important gap in the available literature is the identification of contextual predictors of outpatient diabetes service readiness in low resource settings, such as urban/rural location, area social deprivation level, and facility type [7]. Since health inequalities are known to vary along social gradients [14] and given that primary care is the front-line of diabetes management [15], identifying predictors of diabetes service readiness at the level of primary care can help guide policies and steer investment to areas of greatest need of improvement in LMICs. In this study, we: (1) construct a diabetes-specific readiness index using standard health system metrics; (2) geographically map outpatient readiness for diabetes in Bangladesh; and (3) evaluate contextual predictors of outpatient diabetes service readiness in Bangladesh as an illustrative instance of readiness for diabetes care in LMICs.
2. Materials and methods
2.1. Data source and study sample
We used data from the 2014 Bangladesh Health Facility Survey (BHFS), a cross-sectional, nationally and regionally representative, probabilistic and facility-based survey that was implemented by the National Institute of Population Research and Training (NIPORT) of the Ministry of Health and Family Welfare in Bangladesh [16]. The BHFS-2014 survey utilized standardized questionnaires from the service provision assessment (SPA) component of the U.S. Agency for International Development (USAID) Demographic and Health Surveys (DHS) Program [17]. The goal of the SPA surveys is to provide a comprehensive overview of a country’s health service delivery and availability, which are based on the World Health Organization’s (WHO) service readiness indicators [18]. The aim of the 2014 BHFS was to assess the availability of basic and essential health care services and the readiness of health facilities to provide quality services to patients.
The 2014 BHFS was conducted on a random sample of 1596 health facilities selected from a total of 19,184 registered facilities [16]. Trained interviewers carried out standardized, direct, structured face-to-face interviews with key health facility informants. Since the focus of our analysis was outpatient diabetes service provision and given that only a subset of health facilities in Bangladesh are equipped for the provision of diabetes services, we included only health facilities with outpatient capability that answered “yes” to the question “Do providers in this facility diagnose and/or manage diabetes?” (n = 345 sampled health facilities, which corresponded to a population of 2524 health facilities when considering complex survey design). Among these 345 facilities, 201 facilities also had inpatient capability. A flow diagram of the sample selection process is provided in Supplemental Online Appendix, p. 2.
2.2. Health facility type categorization
Ten facility types were listed on the 2014 BHFS [16]. A list and categorization details of these facilities are presented in Supplemental Online Appendix, p 3. We sub-categorized all facilities into three general categories: public facilities, private facilities, and NGOs. Public facilities were further categorized according to the 2014 BHFS report into District (District hospital and Mother and Child Welfare Center), Upazila Health Complex, Union, and Community clinic. Within the tiered health system of Bangladesh, District hospitals function as urban referral centers for primary care facilities and are equipped for the provision of both inpatient and outpatient services [19]. Upazila Health Complexes at the upazila (subdistrict) level also provide inpatient and outpatient services but are primarily designed for care delivery in rural areas [20]. Union level facilities and Community clinics correspond to the lowest levels of care delivery, mostly outpatient care, in rural areas.
2.3. Definitions of health facility readiness
We defined readiness according to the WHO Service Availability and Readiness Assessment (SARA) reference manual as the availability of components required to provide health services [21]. We considered two different aspects of readiness: basic amenities and diabetes-specific readiness. Basic amenity readiness is defined as the overall capacity of health facilities to provide seven basic amenities: power, improved water source inside or within the ground of the facility, room with auditory and visual privacy for patient consultations, access to adequate sanitation facilities for clients, communication equipment, access to a computer with email/internet, and emergency transportation. Diabetes-specific readiness refers to the ability of health facilities to offer diabetes services and the capacity to provide that service measured through presence of diabetes tracer items (Table 1). These definitions formed the basis for the construction of the readiness indices described below.
Table 1 —
Proportion of health facilities with outpatient and diabetes service capability, according to the 2014 Bangladesh Health Facility Survey (BHFS), by facility type.
| 2014 BHFS question/variable | Outpatient health facilities with provision of diabetes services (N=2,524) | Facility Type |
||||||
|---|---|---|---|---|---|---|---|---|
|
Public facilities (N=1,799) |
||||||||
| District (N=336) | Upazila (N=621) | Union (N=542) | Community clinic (N=300) | NGO (N=374) | Private (N=351) | |||
| Response | N (%) | % [95% CI] | ||||||
| Does this facility routinely provide inpatient care?*** | Yes | 631 (25.1) | 97.8 [86.0, 99.7) | 99.1 [96.6, 99.7] | 7.0 [2.3, 19.4] | ncr | 31.0 [19.2, 46.1] | 100 |
| Basic Amenities: Does this facility have any of the following? | ||||||||
| Central supply electricity grid or an alternative fuel source?*** | Yes | 977 (38.7) | 93.5 [81.5, 97.9] | 78.2 [66.1, 86.8] | 35.8 [22.4, 51.8] | 9.8 [3.3, 26.0] | 77.4 [61.2, 87.9] | 97.0 [81.3, 99.6] |
| Water source on site?* | Yes | 2,130 (84.4) | 100 | 95.6 [88.6, 98.4] | 82.1 [67.7, 91.0] | 76.1 [54.4, 89.5] | 95.6 [83.9, 98.9] | 97.0 [81.3, 99.6] |
| Room with auditory/visual privacy for pt. consultations?*** | Yes | 737 (29.2) | 30.4 [19.1, 44.8] | 25.4 [16.5, 36.9] | 35.0 [22.1, 50.6] | 10.3 [3.6, 26.1] | 61.6 [46.3, 74.9] | 78.3 [62.7, 88.6] |
| Toilet for clients? | Yes | 1,950 (81.5) | 100 | 99.6 [97.0, 99.9] | 77.8 [60.0,89.1] | 70.7 [51.4, 84.6] | 100 | 100 |
| Landline or cell phone?*** | Yes | 933 (37.0) | 89.1 [76.3, 95.4] | 86.2 [77.8, 95.1] | 10.9 [5.0, 222] | 16.8 [6.4, 37.4] | 66.0 [49.9, 79.1] | 95.6 [83.3, 98.9] |
| Working computer?** | Yes | 1,815 (71.9) | 93.5 [81.6, 97.9] | 99.6 [97.0, 99.9] | 43.4 [29.1, 58.9] | 71.4 [51.8, 85.3] | 72.0 [57.1, 83.2] | 99.6 [96.9, 99.9] |
| Access to email/internet at least 2 hrs/day?*** | Yes | 1,080 (42.8) | 78.3 [64.0, 87.9] | 90.6 [81.0, 95.7] | 23.6 [13.3, 38.4] | 33.3 [18.9, 51.6] | 64.9 [49.9, 77.4] | 46.5 [31.3, 62.3] |
| Ambulance?*** | Yes | 396 (15.7) | 80.4 [66.4, 89.5] | 81.5 [70.3, 89.2] | ncr | ncr | 17.7 [9.1, 31.6] | 50.3 [34.6, 65.9] |
| General equipment for diabetes care: Does this facility have any of the | ||||||||
| A manual or digital blood pressure apparatus? | Yes | 2,246 (89.0) | 92.9 [75.3, 98.2] | 97.5 [84.1, 99.7] | 85.7 [68.6, 94.2] | 85.9 [68.0, 94.6] | 100 | 76.0 [40.8, 93.6] |
| A stethoscope? | Yes | 2,335 (92.5) | 97.8 [86.0, 99.7] | 97.7 [90.6, 99.5] | 89.1 [76.4, 95.4] | 89.9 [69.5, 97.2] | 100 | 97.0 [81.3, 99.6] |
| A functioning adult scale?* | Yes | 1,983 (78.6) | 76.1 [61.7, 86.3] | 72.5 [59.7, 82.4] | 52.2 [37.3, 66.8] | 88.2 [66.1, 96.6] | 87.0 [73.7, 94.1] | 74.8 [57.4, 86.7] |
| A measuring tape (for waist circumference) | Yes | 1,212 (48.0) | 56.5 [42.0, 70.0] | 43.7 [32.1, 56.0] | 28.6 [16.7, 44.5] | 52.9 [34.9, 70.2] | 61.5 [45.6, 75.2] | 47.4 [32.2, 63.1] |
| A stadiometer* | Yes | 683 (53.1) | 54.4 [39.9, 68.1] | 53.8 [41.5, 65.8] | 25.5 [15.3, 39.3] | 64.3 [44.9, 80.0] | 59.1 [43.5, 73.0] | 38.4 [24.7, 54.3] |
| Diabetes-specific items: How many providers in this facility? | ||||||||
| Diagnose and/or manage diabetes*** | Dx & Tx | 1,767 (70.0) | 26.1 [15.4, 40.7] | 35.6 [22.0, 45.3] | 54.7 [39.3, 69.2] | 98.9 [95.4, 99.7] | 51.6 [36.6, 66.3] | 17.0 [8.1, 32.1] |
| Dx only | 124 (0.05) | 2.2 [0.3, 14.0] | 8.2 [3.6, 17.5] | 19.5 [10.2, 34.2] | 0.5 [0.07, 3.7] | 2.1 [0.3, 13.7] | ncr | |
| Tx only | 633 (25.1) | 71.7 [57.4, 82.9] | 59.2 [46.7, 70.7] | 25.8 [14.0, 42.6] | 0.6 [0.8, 4.4] | 46.3 [31.8, 61.5] | 83.0 [67.9, 91.9] | |
| Have had diabetes training in the last 2 years?** | 0 | 2,007 (79.5) | 91.3 [78.9, 96.7] | 83.5 [72.5, 90.7] | 98.5 [94.9, 99.6] | 67.8 [48.5, 82.5] | 88.6 [76.0, 95.0] | 85.7 [71.0, 93.6] |
| 1 | 497 (19.7) | 4.4 [1.1, 15.8] | 14.4 [7.8, 25.2] | 1.5 [0.4, 5.1] | 32.2 [17.6, 51.5] | 11.1 [4.7, 23.8] | 9.4 [3.4, 23.1] | |
| >1 | 20 (0.008) | 4.4 [1.1, 15.9] | 2.1 [0.4, 10.1] | ncr | ncr | 0.3 [0.04, 2.3] | 4.9 [1.2, 18.4] | |
| Diabetes-specific items: Does this facility have any of the following items? | ||||||||
| National or other diabetes guidelines?* | Yes | 979 (38.9) | 63.0 [48.7, 75.7] | 61.9 [49.2, 73.1] | 29.5 [17.5, 45.1] | 30.4 [16.5, 49.1] | 57.6 [42.1, 71.8] | 48.9 [33.4, 64.7] |
| A working order** glucometer? | Yes | 1,799 (71.3) | 36.8 [23.3, 52.8] | 47.3 [33.0, 62.1] | ncr | 100 | 78.0 [60.9, 89.0] | 74.1 [56.0, 86.5] |
| Unexpired glucometer test strips??*** | Yes | 813 (32.2) | 36.8 [23.3, 52.8] | 36.9 [24.3, 51.6] | ncr | 100 | 75.4 [58.1, 87.1] | 72.0 [54.1, 84.9] |
| Good sharps waste storage and disposal? | Yes | 1,018 (67.5) | 56.5 [42.1, 69.9] | 59.1 [46.7, 70.4] | 56.9 [41.6, 71.0] | 62.1 [43.1, 78.0] | 66.8 [51.4, 793] | 62.9 [46.5, 76.9] |
| Offer or do any blood glucose testing?*** | Yes | 421 (31.0) | 82.6 [68.9, 91.1] | 75.8 [65.3, 83.9] | ncr | 9.1 [4.0, 19.2] | 79.5 [63.7, 89.5] | 90.0 [75.1, 96.4] |
| A chemistry analyzer?*** | Yes | 1,920(76.1) | 50.0 [32.0, 68.1] | 49.3 [28.0, 70.9] | ncr | ncr | 62.4 [38.8, 81.3] | 97.8 [85.6, 99.7] |
| Do or use urine protein testing?*** | Yes | 1,874 (74.3) | 57.6 [40.6, 72.9] | 54.8 [38.8, 69.9] | ncr | ncr | 84.9 [68.1, 93.7] | 95.7 [78.5, 99.3] |
| Do or use urine glucose testing?* | Yes | 1,855 (73.5) | 57.6 [40.3, 73.2] | 55.8 [39.8, 70.6] | ncr | 40.6 [5.3, 89.4] | 78.5 [61.1, 89.5] | 91.9 [74.1, 97.8] |
| Metformin*** | Yes | 243 (9.6) | 28.3 [17.1, 42.9] | 8.0 [3.8, 15.8] | ncr | ncr | 16.5 [8.1, 30.8] | 73.2 [5.8, 84.6] |
| Glibenclamide*** | Yes | 169 (6.7) | 21.7 [12.1, 36.0] | 16.1 [8.8, 27.5] | 0.31 [0.023, 0.04] | ncr | 2.9 [0.6, 12.9] | 50.3 [33.9, 66.7] |
| Insulin*** | Yes | 162 (16.4) | 15.2 [7.4, 28.8] | 0.7 [0.1, 5.2] | ncr | ncr | 6.3 [1.8, 20.0] | 62.4 [45.3, 76.9] |
| Injectable glucose*** | Yes | 207(8.2) | 34.8 [22.4, 49.6] | 11.9 [5.7, 23.3] | ncr | ncr | 10.1 [4.1, 22.6] | 60.1 [43.1, 75.0] |
| General Medications (for reference) | ||||||||
| Paracetamol | Yes | 2,436 (96.5) | 100 | 99.1 [96.6, 99.8] | 97.1 [88.8, 99.3] | 98.0 [92.2, 99.5] | 93.2 [80.8, 97.8] | 87.8 [71.9, 95.3] |
| Amoxicillin | Yes | 2,251 (89.2) | 91.3 [78.9, 96.7] | 95.5 [87.8, 96.7] | 88.3 [74.3, 95.2] | 92.4 [74.0, 98.1] | 81.3 [67.1, 90.3] | 77.1 [60.1, 88.2] |
n corresponds to the sample size and N corresponds to the population of health facilities represented when considering complex survey design. ncr: no cases reported. P values for chi-square testing across facility types-:
: ≤ 0.05;
: ≤0.01;
:< 0.001.
Variables not formally outlined on WHO SARA manual but deemed important in the equipment category to provide diabetes services. Urine-ketones tracer indicator not assessed in the 2014 BHFS.
2.4. Readiness index for basic amenities
We constructed a basic amenities index using factor analysis (FA) [22] based on a set of conceptual correlates to health facility readiness for basic amenity provision [18]. Briefly, FA is a type of multivariate analysis and a statistical simplification technique applied to observed and correlated data that approximates one or more underlying characteristics. We included the eight variables categorized under the seven basic amenities domain on the WHO SARA reference manual described above [21]. To assess the internal consistency and reliability of the readiness index constructed, we calculated Cronbach’s Alpha (α) (α = 0.744 suggested index reliability). Following the Dalenius & Hodges stratification method [23], we rescaled the index from 0 to 100 (0 being lowest readiness and 100 being highest readiness) and when used as a categorical variable, the index was expressed at three levels: low, medium, and high. Through this categorization, the variance obtained is minimal within each group and maximum between groups.
2.5. Readiness index for provision of diabetes care
We constructed a diabetes-specific index using the methodology outlined above. Following the WHO SARA manual [21], we reviewed all variables according to the four diabetes domains of service readiness: trained staff and guidelines, equipment, diagnostics, and medicines and commodities. Nineteen variables related to diabetes service provision were identified (Table 1 and Supplemental Online Appendix, p 4). Sharps and waste storage and disposal and urine glucose testing were considered important variables according to standard clinical diabetes guidelines and, hence, were included in our analysis despite not being specifically outlined in the WHO SARA diabetes tracer item guideline [21]. Cronbach’s Alpha (α) of 0.875 suggested index reliability [24]. Missing data were predominantly concentrated in 11 out of the 27 variables (Supplemental Online Appendix, p. 4) included in the construction of the readiness indices. Given the conceptual relevance of these variables, and in order to construct an unbiased index, we replaced the original missing data with a number 1 and we generated a dummy variable that retained the missing variable information. This resulted in a total of 38 variables included in the multivariate analysis, which incorporated the variability of both existing and missing data.
2.6. District social deprivation index
To assess the relationship between area social deprivation and health facility readiness, we constructed a multivariate district social deprivation index using data from the Bangladesh Interactive Poverty Maps Project at the World Bank [25]. We included all districts in the analytical sample (58 districts out of 64 in total). This index combined the population density (total population per km2), the share of the rural population, the percentage of the population that lives below the official national lower poverty line, the percentage of the working population in the agricultural sector, percentage of households without access to electricity, flush toilet and tap water, the percentage of children (<5y) who are severely underweight, and the percentage of adults with low literacy. Cronbach’s α = 0.881 suggested index reliability.
2.7. Analysis
All analyses were performed on Stata (College Station, Texas) version 15.1 considering complex survey design. We first conducted a descriptive analysis of the selected variables, categorized as either basic amenities or diabetes-specific services. For reference, we included paracetamol and amoxicillin as general medication variables and evaluated their availability across facility types. Distributional independence of each tracer item by facility type was assessed using chi-square testing. We then calculated the mean readiness (and 95% CI) of basic and diabetes-specific services and performed unadjusted linear regression by each predictor variable (urban/rural setting, district social deprivation, inpatient service capability, and facility type). We subsequently estimated three additive linear regression models with independent variables added in two categories: contextual predictors (urban/rural setting, district social deprivation) and internal facility predictors (facility type, basic amenities index, and inpatient capability). Lastly, utilizing the GPS dataset available through the DHS, we mapped the regional geographic distribution of the health facilities included in this study according to their crude diabetes service readiness score (low, medium, high). To understand the regional diabetes prevalence context of each facility, we also included regional age-adjusted diabetes prevalence estimates from the literature [26]. Since the unit of analysis in our study is the health facility and the unit of analysis of the published prevalence estimates is the individual, the geographic illustration of these health facilities in the context of regional diabetes prevalence is qualitative and does not imply correlation.
3. Results
Of the 345 facilities included in this analysis, 71% were public, 13.9% were NGOs, and 14.8% were private. Table 1 summarizes the inpatient capability, basic amenities and diabetes-specific services among health facilities with diabetes service provision in the 2014 BHFS, according to facility type. The availability of basic amenities was significantly different across facility types, with highest availability in District, Upazila, NGO, and private facilities and lowest availability in Union and Community clinics. General equipment items were distributed more evenly across facilities. Blood pressure apparatus and stethoscopes were reported as available across all facility types (76.0% to 100% of facilities for blood pressure apparatus availability and 89.1% to 100% for stethoscope availability). Measurement equipment for height, weight, and waist circumference was also available across all facility types, with more than 50% of facilities having an adult scale but a lower percentage of facilities having measuring tape for waist circumference or a stadiometer.
4. Availability of diabetes-specific services and items across facilities
Union facilities and Community clinics had the highest percentage of providers diagnosing and treating diabetes (54.7% and 98.9%, respectively) compared with all other facilities. However, all facility types had a low percentage of providers with diabetes training in the last 2 years, particularly Union facilities, where only 1.5% of their providers met this qualification. Availability of diabetes guidelines was variable across all facilities, with the highest availability in District facilities (63.0% [48.7, 75.7]) and the lowest availability in Union facilities (29.5% [17.5, 45.1]). Availability of working glucometers also differed significantly across facilities, with good availability in Community clinics and private facilities, low availability in District and Upazila facilities, and no availability in Union facilities. A similar trend was observed for unexpired glucometer test strips.
With the exception of private facilities, medication availability for diabetes treatment was low across all facility categories. Metformin was reported available in 73.2% of private facilities, whereas availability was reported in only 28.3% of District, 8.0% of Upazila, 16.5% of NGOs, and in none of Union facilities and Community clinics. Insulin was reported available in 62.4% of private facilities whereas availability was reported in only 15.2% of District, 6.3% of NGOs and was nearly absent in Upazila, Union, and Community clinics. A similar trend was observed for glibenclamide and injectable glucose. In contrast to medications for diabetes, paracetamol and amoxicillin were available in greater than 87.8% [71.9, 95.3] and 77.1% [60.1, 88.2] of facilities, respectively.
4.1. 2.2. Readiness index for basic amenities and diabetes service provision according to contextual and internal facility variables
Fig. 1 illustrates the mean readiness (0–100 scale, 100 being highest readiness) for basic amenities and for diabetes service provision overall and by each contextual predictor (urban/rural context and district social deprivation) and each internal facility predictor (inpatient service capability and facility type). Overall, mean readiness for basic amenities was 58.5 [95% CI: 53.8, 63.2] and mean readiness for diabetes services was 24.9 [20.8, 28.9]. Statistically significant differences were observed for the diabetes readiness index when stratified by each predictor variable. Mean diabetes service readiness was lowest in rural versus urban settings (rural, 13.6 [10.8, 16.5]; urban, 60.0 [55.6, 64.4]), and facilities with medium versus low district social deprivation (medium, 15.7 [11.0, 32.3]; low, 41.0 [25.4, 56.6]). Diabetes service readiness was also lowest in facilities with no inpatient capability (14.1 [11.1, 17.1]) compared with facilities with inpatient capability (57.1 [52.1, 62.0]). Diabetes service readiness was lowest in public facilities, primarily Union facilities (6.2 [5.2, 7.2]) and Community clinics (10.5 [7.6, 13.3]) and highest in NGOs (53.1 [44.9, 61.4)] and private facilities (75.0 [69.1, 82.3]). Statistically significant differences for the basic amenity readiness index were only observed when stratified by urban/rural setting and inpatient capability.
Fig. 1 —
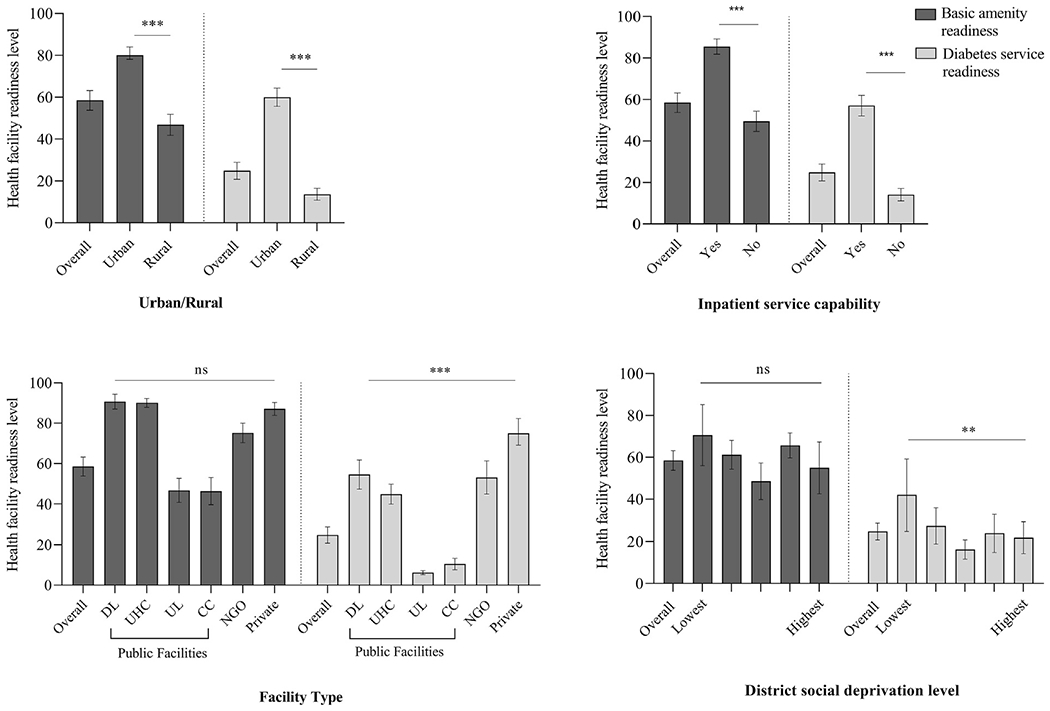
Readiness level for basic amenities and diabetes service provision in outpatient facilities in the 2014 BHFS, by urban/rural setting, inpatient capability, facility type, and district social deprivation level. Facility type abbreviations: District level (DL), Upazila Health Complex (UHC), Union level (UL), Community clinic (CC). District social deprivation levels were ranked from 1 (lowest-richest) to 5 (highest-poorest). P values for unadjusted univariable linear regression: **: ≤0.01; ***:≤ 0.001.
4.2. 2.2. Regional map of health facility diabetes service readiness and regional age-adjusted diabetes prevalence
Fig. 2 illustrates the map of Bangladesh and the regional distribution of health facilities included in this analysis, categorized according to each facility’s diabetes-specific readiness level. The map also depicts the regional prevalence of diabetes according to published estimates, stratified into low, medium and high [26]. Since the unit of analysis of the readiness index (health facility) and the unit of analysis of diabetes prevalence (individuals) were not the same, the illustration is qualitative and does not imply correlation. Most of the facilities had low diabetes service readiness (67.8% of all facilities), 16.3% had medium readiness and 15.9% had high readiness. Khulna, Rajshani, and Barishal had more than 70% of their facilities categorized as low-readiness and less than 10% of their facilities categorized as high-readiness. Among these three regions, Barishal has the second highest age-adjusted diabetes prevalence in Bangladesh [26]. Dhaka, Rangpur and Sylhet had the highest proportion of facilities with medium and high diabetes service readiness.
Fig. 2 —
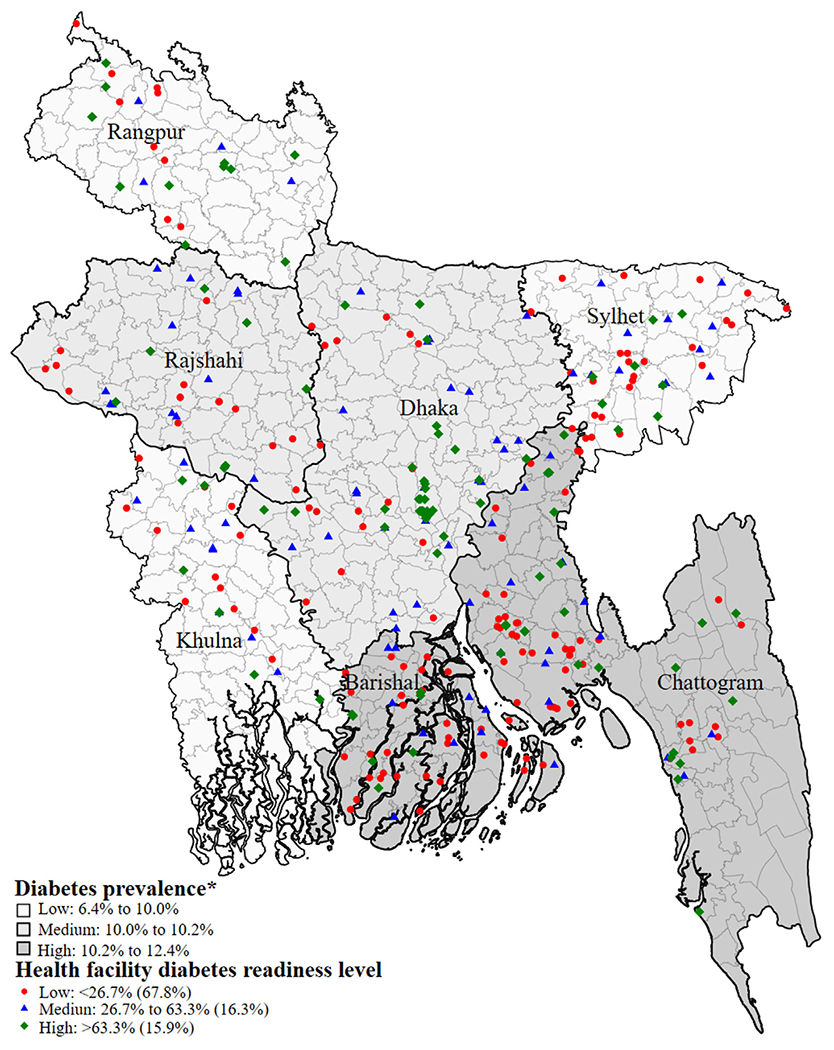
Map of health facilities with diabetes service provision capacity in the 2014 BHFS according to diabetes service readiness level and regional age-adjusted diabetes prevalence. *Published age-adjusted diabetes prevalence in Bangladesh, by region. †Diabetes service readiness index was adapted to a 0–100 scale and was derived from the World Health Organization Service and Availability Readiness Assessment tracer items for diabetes care.
4.3. 2.2. Multivariable regression models
Additive adjusted linear regression models for the relationship between diabetes service readiness and predictors are presented in Table 2. After adjusting for facility type, basic amenity index, inpatient capability, urban/rural setting, and district social deprivation level, facility type and basic amenity readiness level were strongly associated with diabetes service readiness. Specifically, compared with District facilities, all public facilities were negatively associated with health facility diabetes service readiness, with the lowest coefficients corresponding to Union facilities and Community clinics (Union coeff. -36.4 [-53.7, -19.1], Community clinics coeff. -32.4 [-50.1, -14.1]). In contrast, when compared with District facilities, private facilities were positively associated with diabetes service readiness (coeff. 21.0 [11.3, 30.8]). Compared with low basic amenities index, facilities with higher basic amenity index were positively associated with diabetes service readiness.
Table 2 —
Multivariable regression models of the relationship between health facility diabetes service readiness and predictors in the 2014 BHFS.
| Predictor Variable | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Coeff. and [95%CI] | |||
| Facility Type | |||
| District | Ref. | Ref. | |
| Upazila Health Complex | −9.8 [‒18.4, ‒1.2]* | −9.6 [‒19.0, ‒0.11]* | |
| Union | −37.4 [‒50.4, ‒24.4]*** | −36.4 [‒53.7, ‒19.1]*** | |
| Community clinic | −32.9 [‒46.7, ‒19.1]*** | −32.4 [‒50.1, ‒14.1]** | |
| NGO | 4.4 [‒7.4, 16.3] | 5.2 [‒7.0, 17.4] | |
| Private | 20.9 [11.2, 30.7]*** | 21.0 [11.3, 30.8]*** | |
| Basic Amenities Index | |||
| Low | Ref. | Ref. | |
| Medium | 5.8 [1.9, 9.7]** | 6.0 [2.3, 9.7]** | |
| High | 7.9 [0.1, 15.6]* | 8.2 [‒0.01, 16.3]* | |
| Inpatient capability | |||
| Yes | 7.3 [‒3.8, 18.5] | 7.2 [‒3.8, 17.9] | |
| No | Ref. | Ref. | |
| Urban | Ref. | Ref. | |
| Rural | −44.4 [‒50.5, 38.2]*** | −0.9 [‒12.5, 10.7] | |
| District Social Deprivation Level | |||
| Lowest (richest) | Ref. | Ref. | |
| Low | −4.7 [‒16.8, 7.4] | 3.3 [‒3.9, 10.4] | |
| Middle | −10.6 [‒22.0, 0.8] | 0.11 [‒5.9, 6.2] | |
| High | −10.2 [‒21.7, 1.2] | −1.1 [‒8.0, 5.8] | |
| Highest (poorest) | −7.1 [‒19.0, 4.8] | 3.1 [‒4.2, 10.4] | |
| N° of facilities | 2,524 | 2,524 | 2,524 |
| n of facilities | 345 | 345 | 345 |
| Goodness of fit | |||
| F | 73.3 | 115.1 | 75 |
| P value | <0.001 | 0.001 | <0.001 |
| R2 | 0.52 | 0.72 | 0.72 |
Model 1 adjusted for contextual predictors: urban/rural setting and district social deprivation level. Model 2 adjusted for internal health facility predictors: facility type, basic amenities index, inpatient capability. Model 3 adjusted for contextual and internal facility predictors. n corresponds to the sample size and N corresponds to the population of health facilities represented when considering complex survey design. P values:
: < 0.05;
: <0.01;
:< 0.001.
5. Discussion
We assessed primary care facility readiness for diabetes service delivery in Bangladesh, a LMIC with a rapidly growing diabetes prevalence. We found that diabetes service readiness in outpatient facilities was low, particularly in rural settings, areas with high district social deprivation, and in public facilities. Upazila Health Complexes (which serve primarily rural populations), Union facilities and Community clinics (the smallest units of public outpatient care delivery) were negatively associated with diabetes service readiness when compared with District facilities (the most robust units of public outpatient care delivery in Bangladesh). In contrast, private facilities were positively associated with diabetes service readiness. This relationship was observed even after adjusting for urban/rural setting, district social deprivation level, inpatient capability, and basic amenity readiness level. Since diabetes has been proposed as a tracer of health systems [27] and given that the WHO SARA tracer items have been standardized for the assessment of health facilities across LMICs, the diabetes readiness index presented in our study could serve as a tool to identify important gaps in diabetes delivery capability in other LMICs.
Several important policy implications emerged from our analysis. First, the finding that public facilities, primarily Union and Community clinics, were least prepared for diabetes service provision and had critical gaps in diagnostic equipment and medication availability for diabetes treatment highlights important areas of improvement across the public health sector in Bangladesh. While availability of general basic medications, such as paracetamol and amoxicillin, was robust across all facilities, medications for diabetes treatment had low availability in all but private facilities and were largely unavailable in Union facilities and Community clinics. Metformin, glibenclamide, and insulin are included in the Essential Medicines List and should be available in facilities that provide diabetes services [28]. Insufficient funds for health facilities, weak procurement processes, delays in receiving drugs, and increased drug and medical supply prices are common factors that contribute to drug and medical supply shortages and could potentially explain this deficit [29]. The stark contrast in widespread availability of acute medications and the limited availability of medications for diabetes across facilities is consistent with prior studies in LMICs [30]. This finding suggests either lack of prioritization of diabetes treatment in these facilities or a misalignment between supply and demand, which has been associated with sub-optimal service utilization and poor health outcomes [31]. Since public health facilities are the most accessible units of care for most of the population, these findings also highlight an important gap in the public primary care sector of Bangladesh and could help guide supply chain policy for improving availability of medications for the treatment of diabetes.
Second, the finding that primary care facilities in rural areas and in areas of higher district social deprivation were least prepared for the care provision of patients with diabetes suggests inequities in care delivery of diabetes in Bangladesh. This is particularly relevant when considering that undiagnosed diabetes in Bangladesh is most prevalent among the most socioeconomically vulnerable groups in the country [32]. In these areas of higher district social deprivation, patients with diagnosed diabetes may lack the resources to travel to seek care in other, better equipped facilities. Moreover, people with undiagnosed diabetes who live in these areas, and who may remain asymptomatic for several years, are likely to experience a significant delay in appropriate screening, diagnosis, treatment, linkage to care and consequently develop adverse sequelae related to uncontrolled diabetes [33]. Additionally, we found that while NGOs were generally better prepared for diabetes care provision, they were geographically distributed along areas of lower district social deprivation (Supplemental Online Appendix, p. 5). Although NGOs, such as the Diabetic Association of Bangladesh, have significantly increased their service provision since 2014 [34], it is important to assess whether this has resulted in an increased availability of diabetes services in highly socially deprived areas in Bangladesh.
Third, as illustrated in Fig. 2, some of the regions with the highest diabetes prevalence, such as Barishal and Chattogram, had a high proportion of their facilities categorized as having low diabetes service readiness. Although this finding is qualitative, it highlights a possible mismatch in the availability of primary care facilities equipped for the provision of diabetes services, the regional burgeoning demand for these services, and the need for targeted investments to strengthen service provision in areas of high prevalence. We also observed that differences in readiness across facility type and deprivation level were significant for the diabetes-specific readiness index but not for the basic amenity index. This suggests that results derived from the construction of the diabetes readiness index highlight elements within the health system that are specific to diabetes service provision and may not be solely explained by limited basic resources.
Our findings are consistent with several studies on health facility readiness in LMICs. In their systematic review, Nuche-Berenguer and Kupfer identified critical gaps in the capacity to diagnose diabetes, medication access, and training of healthcare workers caring for patients with diabetes in Sub-Saharan Africa [13]. Single-country studies in South Asia have presented similar findings [11,12]. In their health facility survey study in two Indian communities, Gabert et al. showed that lower-level health facilities had limited capacity to measure blood glucose as well as significant gaps in the availability of first-line pharmaceuticals for diabetes management [11]. In a mixed methods study in south India, Elias et al showed that the majority of households depended on private facilities for diabetes care because of lack of laboratory facilities and frequent medicine stockouts at government primary health centers [12]. Similarly, in a multi-country analysis, Moucheraud showed that fewer than half of surveyed facilities across five LMICs were ready for the management of diabetes [9]. Overall, our findings expand on this literature and add an important level of complexity by investigating predictors of health facility readiness and by qualitatively illustrating the geographic distribution of outpatient readiness for diabetes service provision in Bangladesh.
Our study has several limitations. First, although the BHFS is a high-quality, nationally representative survey, this is a cross-sectional study and we report associations, not causal effects. Secondly, we focused on a subsample of facilities reporting the provision of diabetes services. We expect this subsample to be representative of the facilities providing this service nationwide assuming that diabetes facilities have a random probability of selection within the total group of facilities. However, we cannot confirm that the sample is nationally representative due to the absence of a census of facilities providing diabetes services. Third, our study included only facilities that provided outpatient services and those facilities that responded “yes” to diabetes service capability. Since most facilities surveyed had missing information on diabetes service capacity (Supplemental Online Appendix, p. 2), resulting in their exclusion from our sample population, our findings are only applicable to the smaller percentage of facilities with complete information.
Fourth, since there is no literature on the relative weight of each diabetes tracer item on the WHO SARA instrument, we utilized equal weights for each item used in the construction of the diabetes-specific readiness index. This could have under- or overestimated the readiness level for diabetes service provision. Future studies to strengthen the validation of a diabetes readiness metric may consider consulting diabetes healthcare experts (i.e. using Delphi methods) [35], benchmarking these results against those of countries with a similar demographic, social and economic profile, and comparing our estimates with population-level surveys that are similar in time period and design. Lastly, while the WHO SARA tracer items used for the construction of the diabetes readiness index allow for the general evaluation of diabetes service capability, items related to screening of microvascular complications, such as retinopathy and neuropathy, were not included. Since early detection of these conditions is essential for optimal diabetes care [36], inclusion of questions relevant to these complications in future health facility surveys may allow for the construction of more comprehensive tools for measuring diabetes-specific service readiness.
As health systems and individuals in LMICs face the unprecedented burden posed by diabetes in the coming decades, it is vital to understand the readiness and contextual predictors of health system readiness for diabetes management in these settings. In this study, we found that overall readiness for diabetes service provision at the primary care level in Bangladesh was low, particularly in public facilities, rural settings, and districts with high social deprivation. Since diabetes management represents an important challenge to the introduction of Universal Health Care in Bangladesh and other LMICs, our findings could help guide policies for the prioritization of resource allocation that could strengthen care delivery for diabetes in low resource settings and steer investment towards areas of highest unmet need.
Supplementary Material
Acknowledgments
The authors acknowledge the efforts of the Ministry of Health and Family Welfare in Bangladesh, NIPORT for the implementation of the 2014 BHFS, ICF International for technical assistance, Associates for Community and Population Research (ACPR) for data collection as well as the funders of the 2014 BHFS: Government of the People’s Republic of Bangladesh and U.S. Agency for International Development (USAID).
Funding
Jacqueline Seiglie was supported by Grant Number T32DK007028 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Footnotes
Declaration of Competing Interest
DJW reports serving on a data monitoring committee for Novo Nordisk. All other authors declare no competing interests.
Ethics approval
The 2014 BHFS data files were obtained from the Demographic and Health Survey’s Program following standard protocol. All authors directly involved in the data analysis were included in the data request form. The study was exempt from collecting ethical approval since the survey protocols were reviewed and approved by the Nepal Research Council and the ICF Institutional Review Board in Calverton, Maryland, USA.
REFERENCES
- [1].International Diabetes Federation Diabetes Atlas 9th edition 2019 [Internet]. [cited 2019 Nov 18]. Available from: https://diabetesatlas.org/en/.
- [2].Risk Factor NCD. Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387 (10027):1513–30. 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ali MK, Rabadá;n-Diehl C, Flanigan J, Blanchard C, Narayan KMV, Engelgau M. Systems and Capacity to Address Noncommunicable Diseases in Low- and Middle-Income Countries. C O M M E N TA R Y:5. [DOI] [PubMed] [Google Scholar]
- [4].Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract 2019;1(157):107843. 10.1016/j.diabres.2019.107843. [DOI] [PubMed] [Google Scholar]
- [5].Chowdhury AMR, Bhuiya A, Chowdhury ME, Rasheed S, Hussain Z, Chen LC. The Bangladesh paradox: exceptional health achievement despite economic poverty. Lancet 2013;382(9906):1734–45. 10.1016/S0140-6736(13)62148-0. [DOI] [PubMed] [Google Scholar]
- [6].Biswas T, Islam A, Rawal LB, Islam SMS. Increasing prevalence of diabetes in Bangladesh: a scoping review. Public Health. 2016;1(138):4–11. https://doi.org/10.1136/bmjopen-2018-022817. [DOI] [PubMed] [Google Scholar]
- [7].Biswas T, Haider MM, Das Gupta R, Uddin J. Assessing the readiness of health facilities for diabetes and cardiovascular services in Bangladesh: a cross-sectional survey. BMJ Open 2018. 10.1136/bmjopen-2018-022817. Oct 31;8 (10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Health system preparedness for responding to the growing burden of non-communicable disease — a case study of Bangladesh (WP25) | Health Care | Public Health [Internet]. Scribd. [cited 2019 Dec 18]. Available from: https://www.scribd.com/document/129234322/Health-system-preparedness-for-responding-to-the-growing-burden-of-non-communicable-disease-a-case-study-of-Bangladesh-WP25.
- [9].Moucheraud C Service readiness for noncommunicable diseases was low in five countries In 2013–15. Health Aff (Millwood). 2018;37(8):1321–30. 10.1377/hlthaff.2018.0151. [DOI] [PubMed] [Google Scholar]
- [10].Jacobs B, Hill P, Bigdeli M, Men C. Managing noncommunicable diseases at health district level in Cambodia: a systems analysis and suggestions for improvement. BMC Health Services Res 2016;16(1):32. 10.1186/s12913-016-1286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gabert R, Ng M, Sogarwal R, Bryant M, Deepu RV, McNellan CR, et al. Identifying gaps in the continuum of care for hypertension and diabetes in two Indian communities. BMC Health Services Res 2017;17(1):846. 10.1186/s12913-017-2796-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Elias MA, Pati MK, Aivalli P, Srinath B, Munegowda C, Shroff ZC, et al. Preparedness for delivering non-communicable disease services in primary care: access to medicines for diabetes and hypertension in a district in south India. BMJ Glob Health 2017;2(Suppl 3). 10.1136/bmjgh-2017-000519 e000519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Nuche-Berenguer B, Kupfer LE. Readiness of Sub-Saharan Africa healthcare systems for the new pandemic, diabetes: a systematic review. J Diabet Res 2018;18(2018):1–12. 10.1155/2018/9262395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res. 2013;48(2 Pt 1):539–59. 10.1111/j.1475-6773.2012.01449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Davidson JA. The increasing role of primary care physicians in caring for patients with type 2 diabetes mellitus. Mayo Clin Proc. 2010;85(12 Suppl):S3–4. 10.4065/mcp.2010.0466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].National Institute of Population Research and Training/Bangladesh NI of PR and T-, ACPR/Bangladesh A for C and PR-, International ICF. Bangladesh Health Facility Survey 2014. 2016. Mar 1 [cited 2019 Dec 18]; Available from: https://dhsprogram.com/publications/publication-SPA23-SPA-Final-Reports.cfm. [Google Scholar]
- [17].The Demographic Health Surveys Program - Service Provision Assessments (SPA) [Internet]. [cited 2019 Sep 23]. Available from: https://dhsprogram.com/What-We-Do/Survey-Types/SPA.cfm.
- [18].Service Readiness Indicators Version 2.2 (English) [Internet]. [cited 2019 Sep 23]. Available from: https://dhsprogram.com/publications/publication-spaq5-spa-questionnaires.cfm.
- [19].Ahmed S, Hasan MZ, Laokri S, Jannat Z, Ahmed MW, Dorin F, et al. Technical efficiency of public district hospitals in Bangladesh: a data envelopment analysis. Cost Eff Resour Alloc 2019;17(1):15. 10.1186/s12962-019-0183-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ahmed S, Siddique AK, Iqbal A, Rahman FKMN, Islam MdN, Sobhan MdA, et al. Causes for Hospitalizations at Upazila Health Complexes in Bangladesh. J Health Popul Nutr. 2010. Aug;28(4):399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].World Health Organization | Service Availability and Readiness Assessment (SARA): an annual monitoring system for service delivery. World Health Organization. Accessed December 22, 2019. https://www.who.int/healthinfo/systems/sara_reference_manual/en/ [Google Scholar]
- [22].Cudeck R Exploratory factor analysis. In: Handbook of applied multivariate statistics and mathematical modeling. San Diego, CA, US: Academic Press; 2000. p. 265–96. [Google Scholar]
- [23].Dalenius T, Jr JLH. Minimum Variance Stratification. Journal of the American Statistical Association. 1959. March 1;54 (285):88–101. [Google Scholar]
- [24].Knoke D, Bohrnstedt GW, Mee AP. Statistics for social data analysis [Internet]. Itasca, Ill.: F.E. Peacock Publishers; 2002. [cited 2019 Dec 18]. Available from: http://books.google.com/books?id=1wNHAAAAMAAJ. [Google Scholar]
- [25].Bangladesh Interactive Poverty Maps [Internet]. World Bank. [cited 2019 Dec 18]. Available from: https://www.worldbank.org/en/data/interactive/2016/11/10/bangladesh-poverty-maps. [Google Scholar]
- [26].Akter S, Rahman MM, Abe SK, Sultana P. Prevalence of diabetes and prediabetes and their risk factors among Bangladeshi adults: a nationwide survey. Bull World Health Organ 2014;92(3):204–213A. 10.2471/BLT.13.128371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Nolte E, Bain C, McKee M. Diabetes as a tracer condition in international benchmarking of health systems. Diabetes Care 2006;29(5):1007–11. 10.2337/dc05-1550. [DOI] [PubMed] [Google Scholar]
- [28].World Health Organization | Bangladesh. World Health Organization. Accessed January 22, 2020. https://www.who.int/selection_medicines/country_lists/bgd/en/ [Google Scholar]
- [29].Ahmed S-G, Begum T, Smith OK. Diagnostic Study of Public Financial Management : To Strengthen Health Financing and Service Delivery in Bangladesh [Internet]. The World Bank; 2019. Apr [cited 2020 Jan 22] p. 1–66. Report No.: 137120. Available from: http://documents.worldbank.org/curated/en/856271558671301506/Diagnostic-Study-of-Public-Financial-Management-To-Strengthen-Health-Financing-and-Service-Delivery-in-Bangladesh. [Google Scholar]
- [30].World Health Organization | Differences in the availability of medicines for chronic and acute conditions in the public and private sectors of developing countries. World Health Organization. Accessed December 18, 2019. https://www.who.int/bulletin/volumes/89/6/10-084327/en/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Greenwald BC, Stiglitz J. Externalities in economies with imperfect information and incomplete markets. QJ Econ 1986;101(2):229–64. [Google Scholar]
- [32].Hasan MdM, Tasnim F, Tariqujjaman Md, Ahmed S. Socioeconomic Inequalities of Undiagnosed Diabetes in a Resource-Poor Setting: Insights from the Cross-Sectional Bangladesh Demographic and Health Survey 2011. Int J Environ Res Public Health. 2019. January 3; 16 (1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Manne-Goehler J, Geldsetzer P, Agoudavi K, Andall-Brereton G, Aryal KK, Bicaba BW, et al. Health system performance for people with diabetes in 28 low- and middle-income countries: a cross-sectional study of nationally representative surveys. PLoS Med 2019;16(3). 10.1371/journal.pmed.1002751 e1002751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Diabetic Association of Bangladesh [Internet]. [cited 2020 Jan 22]. Available from: https://www.dab-bd.org/publication.php.
- [35].Hsu C-C, Sandford BA. The Delphi Technique: Making Sense Of Consensus. 12(10):8. [Google Scholar]
- [36].Association AD 10. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes—2018. Diabetes Care 2018;41(Supplement 1):S105–18. 10.2337/dc18-S010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


