Abstract
There are a limited number of studies on postoverdose clinical findings of mirtazapine in the literature. Our case presented an unlikely junctional rhythm, which we have not seen in the previous studies, in a patient who had bradycardia and hypotension following mirtazapine intake. A 37-year old male was admitted to the emergency department (ED) after his suicide attempt with 300 mg PO of mirtazapine tablets. He took the drug 2 h prior to his ED visit. He did not have any complaints after the mirtazapine intake. His complete physical examination and electrocardiography (ECG) revealed no pathological findings. He was observed in the ED. The results were in the normal range in his blood test and he has 0 mg/dl of blood ethanol. He experienced dizziness after 5 h and 30 min. The blood pressure was 60/30 mmHg. The heart rate was 34 beats/min. The simultaneous ECG showed junctional bradycardia. 0.5 mg atropine IV was given two times at intervals. Norepinephrine infusion was initiated after normal saline therapy. Forty-five minutes later, he did not have any clinically significant complaint. There are no pathological findings in his follow-up ECG and physical examination. He was discharged of his own accord 10 h after his ED admission. His initial mirtazapine level was 145 ng/ml when he came to the ED. Mirtazapine was known to have a safe cardiac profile both for regular dose and overdose. However, physicians should consider that it might induce a life-threatening bradyarrhythmia.
Keywords: Electrocardiography, life-threatening rhythm, overdose
Introduction
Mirtazapine, as an atypical antidepressant, affects the central nervous system as it blocks presynaptic alpha-2 adrenergic and postsynaptic 5-HT2/5-HT3 receptors.[1] Consequently, it causes an increase in neuronal norepinephrine and serotonin levels.[2] In the literature, many studies have stated its reliability regarding its effectiveness in clinical use and its side effect profile.[3,4] The data about its postoverdose clinical findings are limited.[2,5]
We presented a patient who had hypotension and bradycardia after he took mirtazapine to commit suicide in our case because of an unlikely junctional rhythm detected in his electrocardiography (ECG). We have not seen a similar case in the literature before.
Case Report
A 37-year old male (weight: 80 kg, height: 178 cm) was admitted to the emergency department (ED) after his suicide attempt with 300 mg PO of mirtazapine tablets. He had been using the prescribed drug for 45 days and he took the tablets to commit suicide approximately 2 h before his hospital visit. He stated that he had alcohol, but he did not take any additional drugs. He also added that he did not have any clinically relevant complaints after taking the medication. The patient's relatives and the prehospital emergency medical personnel, who brought the patient to the hospital, stated that there was no evidence of additional medicine intake (empty medicine boxes, empty blister packs, etc) at the incident scene. The patient's medical history revealed that he had a depression diagnosis concurrent with the drug use and he used sertraline and mirtazapine together. He also stated that he had no additional disease or drug use. His family medical history had no related health issues. On admission, in his physical examination, the blood pressure (BP) was 150/80 mmHg, the heart rate was 66 beats/min, the breath count was 18 breaths/min, and the temperature was 36.0°C. His complete physical examination did not show another pathological finding. His blood sugar level in the fingertip was 93 mg/dl. There was no pathological finding in his ECG. The patient was placed in observation in the ED. Activated charcoal and gastric lavage therapy was not administered as a result of a consultation with the National Poison Management Center. 40 mg omeprazole IV was administered. The results of blood gas, electrolytes, renal function tests, liver and cardiac enzymes, and complete blood count were all normal. The ethanol level was 0 mg/dl in his blood. At the 5th h of the observation, the patient did not have any clinically relevant complaint, and his BP was 100/60 mmHg, heart rate was 56 beats/min, breath count was 18 breaths/min, and temperature was 36.0°C. Thirty minutes later, the patient complained of feeling faint and his BP was measured 60/30 mmHg and his heart rate was 34 beats/min. The simultaneous ECG showed junctional bradycardia [Figure 1]. 0.5 mg atropine IV was given to the patient two times at intervals. Norepinephrine infusion was initiated at a dose of 8 mcg/min after a normal saline therapy. After 45 min, his BP was 105/60 mmHg and the heart rate was 58 beats/min. The patient did not have another clinically relevant complaint and his physical examination did not reveal another pathological finding. ECG for rhythm control showed no pathological findings. The patient's concurrent follow-up blood tests demonstrated changes only in white blood cells (from 6.8 × 109 /ul to 9.1 × 109 /ul) and in base deficit (from − 0.8 mmol/L to −1.8 mmol/L) compared with his initial values. We did not encounter any additional problems during the observation. Under normal conditions, the standard treatment and observation period for an asymptomatic patient after mirtazapine intake is 8–10 h. An extension in observation time was planned because the patient developed a life-threatening rhythm at the 5th h and 45th min of his admission. However, the patient left the ED of his own accord 10 h after his admission. The patient's mirtazapine level was measured as 145 ng/ml at the time of his admission (therapeutic range is 5–100 ng/ml).
Figure 1.
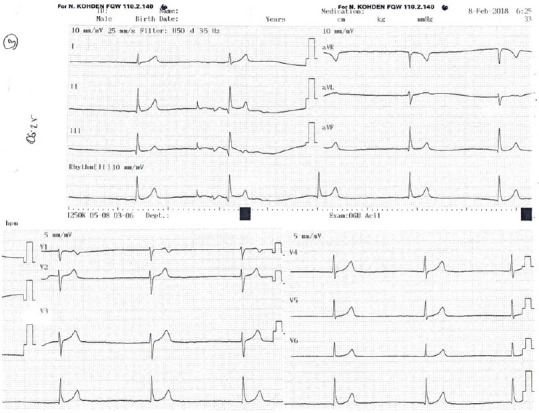
Electrocardiography (5th h and 30th min of observation in the emergency department)
Discussion
Mirtazapine is identified as a noradrenergic and specific serotonergic antidepressant due to its mechanism of action acts as alpha-2 adrenergic antagonist and 5-HT2 and 5-HT3 agonist. It does not have an antimuscarinic effect or does not block sodium channel; thus, an evident effect on the cardiac conduction is not anticipated.[6] The daily dose is established as 20–30 mg/day (range: 5–60 mg) to achieve optimal efficacy.[6] A range of 5–100 ng/mL is the therapeutic reference range for concentrations of mirtazapine in plasma.[7,8]
Many clinical studies demonstrated the efficacy of mirtazapine at a therapeutic dose and its safe side effect profile.[9,10] The most frequently seen and reportedly temporary side effects are dry mouth, increased appetite, weight gain, and sedation.[4] As a side effect, no clinically significant cardiovascular incident was reported.[10,11] However, the available data on the mirtazapine's clinical features after an overdose are not sufficient. The mirtazapine-related cases with serotonin toxicity, agitation, confusion, cogwheel rigidity, and rhabdomyolysis were reported,[5] but these findings were mostly associated with additional drug intake instead of mirtazapine. In addition, in the cases with isolated mirtazapine overdose, impact on the heart rate (mostly tachycardia) and mild hypotension was also reported.[1,5,6,12,13] A retrospective study stated that after mirtazapine overdose (median dose 450 mg), 72.8% of the cases were asymptomatic at the time of admission and those with clinically relevant complaints took an additional drug.[1] While in 3 out of 23 cases with isolated mirtazapine intake, the heart rate was <61 beats/min (P < 0.05), in all 23 cases, a decline was observed in BP levels. In only one of the cases with isolated mirtazapine intake, PR >200 ms was detected in ECG. QRT and QT prolongation, severe arrhythmia, and blockage were not observed.[1] Another retrospective study reported bradycardia and hypotension in one out of 33 patients after isolated mirtazapine intake.[6] The ECGs of these patients did not show any conduction disturbances. In a study conducted by Berling et al., isolated mirtazapine intake (median dose: 420 mg) was detected in 33% of the patients.[5] Nine out of 89 patients had a heart rate <61 beats/min and in 2 of them, BP was reported as <90 mmHg. They mentioned that these cases did not require inotropic support therapy. In 81 patients with ECGs, QRS and QT prolongation or arrhythmia was not detected.[5] Unlike the cases with bradycardia and hypotension in these studies,[5,6] in our case, the junctional rhythm was observed in ECG.
Furthermore, in our study, mirtazapine overdose was validated with the plasma concentration values, unlike these studies.[1,5,6,12,13] We examined the mirtazapine level in plasma and it was detected over the therapeutic level range.
Its effects on receptors and an evident cardiac conduction disorder due to mirtazapine intake are not anticipated.[6] However, in the literature, there are studies which associate the cases of torsades de pointes with mirtazapine[13] and mention the incidence of QTc prolongation (3%).[14] In our case, we also detected clinical findings related to an impact on the heart and a conduction disorder in ECG.
Alterations in autonomic tone on the SA node might cause its inconvenient deceleration.[15] The junctional rate might be reduced to a level <40 beats/min as a result of enhanced vagal tone, dysfunctional pacemakers in organic heart disease, or hyperkalemia originated from the digoxin toxicity.[16] The pacemaker is naturally above the bifurcation of the bundle branches; thus, junctional rhythm is a regular narrow QRS complex rhythm. Yet, the QRS may be wide in case there is a conduction disturbance distal to the pacemaker, a dominant subjunctional pacemaker, or a dominant ventricular pacemaker.[16] Our case, which had no pathological findings on the ECG at the time of admission, developed tone alteration in the SA node and ECG changes. On the ECG of our case, there was a steady rhythm with an undetected P wave and a ventricular rhythm of 33/min. The QRS complex was 96 ms and had normal morphology. The QTc was identified as 368 ms.
Junctional rhythm may be either asymptomatic or come with malaise, palpitation, or presyncope.[15] The vital symptoms of our case also reached the normal limits and he became asymptomatic with the treatment. There was no additional drug intake; thus, the clinical signs and symptoms were associated with isolated mirtazapine intake. The mirtazapine plasma level of the case also supported the diagnosis.
Conclusion
Mirtazapine, which was considered safe from cardiac side effects even in overdoses, might cause serious life-threatening bradyarrhythmia. There is a need of vigilance on serious cardiovascular adverse events in patients on mirtazapine.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Waring WS, Good AM, Bateman DN. Lack of significant toxicity after mirtazapine overdose: A five-year review of cases admitted to a regional toxicology unit. Clin Toxicol (Phila) 2007;45:45–50. doi: 10.1080/15563650601005837. [DOI] [PubMed] [Google Scholar]
- 2.Christine M. Stork, serotonin reuptake inhibitors and atypical antidepressants. In: Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR, editors. Goldfrank's Toxicologic Emergencies. 10th ed. New York: McGraw-Hill Education; 2015. pp. 1698–713. [Google Scholar]
- 3.Kasper S. Clinical efficacy of mirtazapine: A review of meta-analyses of pooled data. Int Clin Psychopharmacol. 1995;10(Suppl 4):25–35. doi: 10.1097/00004850-199512004-00005. [DOI] [PubMed] [Google Scholar]
- 4.Biswas PN, Wilton LV, Shakir SA. The pharmacovigilance of mirtazapine: Results of a prescription event monitoring study on 13554 patients in England. J Psychopharmacol. 2003;17:121–6. doi: 10.1177/0269881103017001716. [DOI] [PubMed] [Google Scholar]
- 5.Berling I, Isbister GK. Mirtazapine overdose is unlikely to cause major toxicity. Clin Toxicol (Phila) 2014;52:20–4. doi: 10.3109/15563650.2013.859264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.LoVecchio F, Riley B, Pizon A, Brown M. Outcomes after isolated mirtazapine (Remeron) supratherapeutic ingestions. J Emerg Med. 2008;34:77–8. doi: 10.1016/j.jemermed.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Grasmäder K, Verwohlt PL, Kühn KU, Frahnert C, Hiemke C, Dragicevic A, et al. Relationship between mirtazapine dose, plasma concentration, response, and side effects in clinical practice. Pharmacopsychiatry. 2005;38:113–7. doi: 10.1055/s-2005-864120. [DOI] [PubMed] [Google Scholar]
- 8.Baumann P, Hiemke C, Ulrich S, Eckermann G, Gaertner I, Gerlach M, et al. The AGNP-TDM expert group consensus guidelines: Therapeutic drug monitoring in psychiatry. Pharmacopsychiatry. 2004;37:243–65. doi: 10.1055/s-2004-832687. [DOI] [PubMed] [Google Scholar]
- 9.Timmer CJ, Sitsen JM, Delbressine LP. Clinical pharmacokinetics of mirtazapine. Clin Pharmacokinet. 2000;38:461–74. doi: 10.2165/00003088-200038060-00001. [DOI] [PubMed] [Google Scholar]
- 10.Watanabe N, Omori IM, Nakagawa A, Cipriani A, Barbui C, Churchill R, et al. Mirtazapine versus other antidepressive agents for depression. Cochrane Database Syst Rev. 2011;12:CD006528. doi: 10.1002/14651858.CD006528.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anttila SA, Leinonen EV. A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev. 2001;7:249–64. doi: 10.1111/j.1527-3458.2001.tb00198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waring WS. Clinical use of antidepressant therapy and associated cardiovascular risk. Drug Healthc Patient Saf. 2012;4:93–101. doi: 10.2147/DHPS.S28804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poluzzi E, Raschi E, Moretti U, De Ponti F. Drug-induced torsades de pointes: Data mining of the public version of the FDA Adverse Event Reporting System (AERS) Pharmacoepidemiol Drug Saf. 2009;18:512–8. doi: 10.1002/pds.1746. [DOI] [PubMed] [Google Scholar]
- 14.Kyoung HC, Kyoung-Uk L. Over-Sedation, the main toxic effect of mirtazapine overdose? Clin Psychopharmacol Neurosci. 2010;8:167–9. [Google Scholar]
- 15.Beinart SC. Junctional Rhythm. WebMd: Medscape; 2018. [Last accessed on 2018 Dec 18]. Available from: https://emedicine.medscape.com/article/155146-overview#a4 . [Google Scholar]
- 16.Goldberger AL. Cardiac Arrhythmias Due to Digoxin Toxicity, October 12, 2017. [Last accessed on 2018 Dec 18]. Available from : https://www.uptodate.com/contents/cardiac-arrhythmias-due-to-digoxin-toxicity#H24718286 .


