Abstract
Background
Bladder dysfunction is a common complication following radical hysterectomy, caused by the damage to pelvic autonomic nerves that innervate the muscles of the bladder, urethral sphincter, and pelvic floor fasciae. Bladder dysfunction increases the rates of urinary tract infection, hospital visits or admission, and patient dissatisfaction. In addition, bladder dysfunction can also negatively impact patient quality of life (QoL). Several postoperative interventions have been proposed to prevent bladder dysfunction following radical hysterectomy. To our knowledge, there has been no systematic review evaluating the effectiveness and safety of these interventions for preventing bladder dysfunction following radical hysterectomy in women with cervical cancer.
Objectives
To evaluate the effectiveness and safety of postoperative interventions for preventing bladder dysfunction following radical hysterectomy in women with early‐stage cervical cancer (stage IA2 to IIA2).
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 4) in the Cochrane Library, MEDLINE via Ovid (1946 to April week 2, 2020), and Embase via Ovid (1980 to 2020, week 16). We also checked registers of clinical trials, grey literature, conference reports, and citation lists of included studies.
Selection criteria
We included randomised controlled trials (RCTs) evaluating the effectiveness and safety of any type of postoperative interventions for preventing bladder dysfunction following a radical hysterectomy in women with stage IA2 to IIA2 cervical cancer.
Data collection and analysis
Two review authors independently selected potentially relevant RCTs, extracted data, assessed risk of bias, compared results, and made judgments on the quality and certainty of the evidence. We resolved any disagreements through discussion or consultation with a third review author. Outcomes of interest consisted of spontaneous voiding recovery one week after the operation, quality of life (QoL), adverse events, post‐void residual urine volume one month after the operation, urinary tract infection over the one month following the operation, and subjective urinary symptoms.
Main results
We identified 1464 records as a result of the search (excluding duplicates). Of the 20 records that potentially met the review criteria, we included five reports of four studies. Most of the studies had unclear risks of selection and reporting biases. Of the four studies, one compared bethanechol versus placebo and three studies compared suprapubic catheterisation with intermittent self‐catheterisation. We identified two ongoing studies.
Bethanechol versus placebo The study reported no information on the rate of spontaneous voiding recovery at one week following the operation, QoL, adverse events, urinary tract infection in the first month after surgery, and subjective urinary symptoms for this comparison. The volume of post‐void residual urine, assessed at one month after surgery, among women receiving bethanechol was lower than those in the placebo group (mean difference (MD) ‐37.4 mL, 95% confidence interval (CI) ‐60.35 to ‐14.45; one study, 39 participants; very‐low certainty evidence).
Suprapubic catheterisation versus intermittent self‐catheterisation The studies reported no information on the rate of spontaneous voiding recovery at one week and post‐void residual urine volume at one month following the operation for this comparison. There was no difference in risks of acute complication (risk ratio (RR) 0.77, 95% CI 0.24 to 2.49; one study, 71 participants; very low certainty evidence) and urinary tract infections during the first month after surgery (RR 0.77, 95% CI 0.53 to 1.13; two studies, 95 participants; very‐ low certainty evidence) between participants who underwent suprapubic catheterisation and those who underwent intermittent self‐catheterisation. Available data were insufficient to calculate the relative measures of the effect of interventions on QoL and subjective urinary symptoms.
Authors' conclusions
None of the included studies reported rate of spontaneous voiding recovery one week after surgery, time to a post‐void residual volume of urine of 50 mL or less, or post‐void residual urine volume at 6 and 12 months after surgery, all of which are important outcomes for assessing postoperative bladder dysfunction.
Limited evidence suggested that bethanechol may minimise the risk of bladder dysfunction after radical hysterectomy by lowering post‐void residual urine volume. The certainty of this evidence, however, was very low. The effectiveness of different types of postoperative urinary catheterisation (suprapubic and intermittent self‐catheterisation) remain unproven.
Plain language summary
Postoperative interventions for preventing bladder dysfunction after radical hysterectomy in women with early‐stage cervical cancer
The issue Radical hysterectomy with pelvic lymphadenectomy (removal of the uterus (womb) with its surrounding tissues and lymph glands in the pelvis) is the treatment for early‐stage cervical cancer (when cancer is still within the cervix and upper vagina, without spread into nearby tissues). Bladder dysfunction (problems with the way the bladder holds and releases urine) is a common problem following radical hysterectomy, caused by the damage to the nerves controlling urination.
The aim of the review To assess the usefulness and safety of treatment to prevent bladder dysfunction following radical hysterectomy in women with early‐stage cervical cancer. We searched the scientific databases for randomised controlled trials (studies in which people or groups of people are allocated by chance to two or more groups, treating them differently) published to April 2020.
Main findings We found four studies that met the inclusion criteria. One study compared a medication called bethanechol to placebo (a substance that has no therapeutic effect, used as a control in testing drugs). Three studies compared suprapubic catheterisation (insertion of a flexible tube (catheter) into the bladder through a cut in the lower abdomen to drain urine) with intermittent self‐catheterisation (insertion of a catheter via the urethra, into the bladder at intervals throughout the day).
Bethanechol versus placebo
Bethanecol may reduce the chance of bladder dysfunction by lowering the volume of post‐void residual urine, assessed at one month after surgery. However, the certainty of this evidence is very low and further studies have the potential to better inform this outcome.
Suprapubic catheterisation versus intermittent self‐catheterisation There was insufficient evidence to indicate the effectiveness of suprapubic catheterisation and intermittent self‐catheterisation for preventing bladder dysfunction. Very‐low certainty evidence noted no difference between these two treatments in the risk of an unfavourable result and urinary tract infections during the first month after surgery.
Conclusions
None of the included studies reported rate of spontaneous voiding recovery one week after surgery, time to a post‐void residual volume of urine of 50 mL or less, or post‐void residual urine volume at 6 and 12 months after surgery, all of which are important outcomes for assessing postoperative bladder dysfunction. Limited evidence suggested that bethanechol may prevent bladder dysfunction after radical hysterectomy by lowering post‐void residual urine volume. The certainty of this evidence, however, was very low. The effectiveness of different types of postoperative urinary catheterisation (suprapubic and intermittent self‐catheterisation) remains unproven.
Summary of findings
Background
Please see Appendix 1 for a glossary of terms.
Description of the condition
Cervical cancer is the fourth most common cancer affecting women worldwide, with an estimated 569,847 new cases and 311,365 cervical cancer‐related deaths globally in 2018 (Bray 2018). Cervical cancer is a major health problem among women in developing countries, with almost 70% of the global burden and 90% of cervical cancer‐related deaths occurring in these regions (Ferlay 2015; Bray 2018). The high burden of cervical cancer among less economically developed settings is secondary to the failure to provide effective, large‐scale screening programmes (Torre 2015; Bray 2018).
Treatment of cervical cancer depends on the extent of the disease. Appendix 2 displays a 2018 International Federation of Gynecology and Obstetrics (FIGO) staging system for cervical cancer (Bhatla 2019), which was revised from the 2009 FIGO staging system (Appendix 3). Women with early‐stage cervical cancer (FIGO stage IA2 to IIA2) can be treated with either radical hysterectomy with pelvic lymphadenectomy (removal of the uterus with its surrounding tissues and lymph glands in the pelvis) or pelvic chemoradiation (radiation therapy to lower abdomen being given at the same time as chemotherapy) (Landoni 1997). In premenopausal women, radical hysterectomy with pelvic lymphadenectomy may be preferable to pelvic radiation in order to preserve ovarian function and vaginal elasticity, as well as prevent the long‐term risks of pelvic radiation (Cull 1993; Viswanathan 2014).
The aim of radical hysterectomy is to remove the primary tumour with an adequate margin of normal tissue to ensure complete resection (Piver 1974; Querleu 2008; Verleye 2009). Appendix 4 lists details of the three systems for the classification of radical hysterectomy (Piver‐Rutledge‐Smith, Gynecological Cancer Group of the European Organization for Research and Treatment of Cancer, and Querleu and Morrow). The stage of cervical cancer is the fundamental factor to be taken into consideration when considering radical hysterectomy. Women with early‐stage cervical cancer are traditionally treated with Piver type III radical hysterectomy. However, a previous randomised controlled trial (RCT) demonstrated that women with early‐stage cervical cancer who underwent Piver type II hysterectomy (also called modified radical hysterectomy) had comparable oncological outcomes to those who underwent type III hysterectomy (Landoni 2001). Pelvic lymphadenectomy is performed to look for metastatic lesions in the pelvic lymph nodes. The survival of women with early‐stage cervical cancer who undergo radical hysterectomy with pelvic lymphadenectomy is excellent. Estimated five‐year survival rates range between 70% and 90% (Kim 2000; Suprasert 2010; Srisomboon 2011; Mahawerawat 2013).
One of the most distressing morbidities that can occur following radical hysterectomy is bladder dysfunction (problems with the way the bladder holds and releases urine) (Lin 1998; Plotti 2011; Laterza 2015). The incidence of bladder dysfunction after radical hysterectomy varies from 12% to 85% depending on the method used in evaluating bladder dysfunction and the duration of follow‐up (Zullo 2003; Wit 2014). In addition, the risk of bladder dysfunction depends on the extent of surgery. Women undergoing type II radical hysterectomy are at lower risk of postoperative bladder dysfunction than those who undergo type III radical hysterectomy (Landoni 2001; Raspagliesi 2006). By magnifying anatomical structures in the pelvis, laparoscopic approaches may help reduce the denervation of pelvic nerves during radical hysterectomy. However, it has yet to be shown that these approaches have a significant effect on the prevention of bladder dysfunction (Laterza 2015; Kietpeerakool 2019). Minimally invasive radical hysterectomy, however, is associated with inferior survival to laparotomy radical hysterectomy in women with early‐stage cervical cancer. Consequently, a minimally invasive radical hysterectomy is not recommended. Although there may be a selective group of women for whom minimally invasive radical hysterectomy remains safe, further studies are needed (Ramirez 2018; Cusimano 2019; Chen 2020).
Causes of bladder dysfunction following radical hysterectomy are secondary to the damage of pelvic autonomic nerves that innervate the muscles of the bladder (detrusor muscle), urethral sphincter and pelvic floor fasciae (Zullo 2003; Sellers 2012). Bladder dysfunction following radical hysterectomy includes various functional disorders of the lower urinary tract, such as urinary retention, voiding difficulty, urinary hesitancy, urinary tract infection, and urinary stress incontinence (Chen 2002). Bladder dysfunction increases the rates of urinary tract infection, hospital visits or admission, patient dissatisfaction, and the need for intermittent self‐catheterisation (Manchana 2010). Bladder dysfunction can also negatively impact patient quality of life (QoL), which can lead to embarrassment or even social isolation (Zhou 2016).
Description of the intervention
Postoperative interventions for preventing bladder dysfunction after radical hysterectomy can be classified broadly into two groups: pharmacological interventions and non‐pharmacological interventions. Pharmacological interventions use parasympathomimetic agents to stimulate contraction of the smooth muscles of the detrusor muscle and can improve the symptoms associated with bladder hypotonia (Sellers 2012). The drugs frequently used in treating bladder dysfunction following radical hysterectomy are bethanechol chloride and cisapride (Kemp 1997; Madeiro 2006). A wide range of non‐pharmacological interventions have been used to reduce bladder dysfunction following radical hysterectomy, including postoperative suprapubic catheterisation, intermittent self‐catheterisation, bladder training and acupuncture (Fernandez 2005; Naik 2005; Geller 2014; Kidd 2015).
How the intervention might work
Previous studies have demonstrated that a malfunctioning bladder detrusor muscle is a major cause of bladder dysfunction following radical hysterectomy (Plotti 2011; Laterza 2015). Contraction of the detrusor muscle of the urinary bladder is stimulated by parasympathetic nerve impulses mediated by the neurotransmitter acetylcholine (Sellers 2012). Pharmacological therapy for voiding disorders consists of drugs that improve detrusor muscle contraction and those that reduce urethral resistance, which may have a role in the prevention of postoperative bladder dysfunction.
Bethanechol, a cholinergic agent, is a synthetic ester, and is structurally and pharmacologically related to acetylcholine. Bethanechol increases the tone of the detrusor muscle by stimulating the parasympathetic nervous system (Kemp 1997; Madeiro 2006).
Cisapride is a prokinetic agent. It is principally prescribed for treating gastro‐oesophageal reflux in children. The mechanism of action of cisapride is to stimulate the release of acetylcholine, thus promoting detrusor muscle contractility. Hence, as a result of its parasympathomimetic effect, cisapride may be effective for treating bladder hypotonia after surgery (Madeiro 2006). Cisapride, however, has been restricted to a limited access programme in the USA and Europe because it is associated with serious side effects, including cardiac arrhythmias (irregular heart rhythms) and death (Henney 2000).
Suprapubic catheterisation (SPC), an insertion of a catheter via postoperative suprapubic cystostomy, has been proposed to hasten the recovery of bladder function compared with an indwelling urethral catheter, by minimising the risks of a urinary tract infection and asymptomatic bacteriuria, which can impede bladder function activity returning to normal (Kidd 2015).
Bladder training is an important form of behaviour therapy that can be effective in treating bladder dysfunction following radical hysterectomy (Goldfarb 1967). Bladder training targets the detrusor muscle and aims to promote bladder filling and emptying according to a normal pattern (Oberst 1981). As bladder training has been acknowledged as an effective intervention for managing individuals with neurogenic bladder (Wallace 2004), this intervention may be effective for managing bladder dysfunction following radical hysterectomy.
Acupuncture is a treatment derived from traditional Chinese medicine. Fine needles are inserted at certain sites in the body for either therapeutic or preventative purposes. A small electrical current passing between pairs of acupuncture needles may be used at the same time, a technique called electroacupuncture (Yi 2011). Previous studies have reported the efficacy of acupuncture for the treatment of postoperative urinary retention after gynaecological surgery (Wang 2007; Geller 2014). However, the actual mechanism of action remains unknown.
Why it is important to do this review
Although survival outcomes of women with early‐stage cervical cancer after radical hysterectomy with pelvic lymphadenectomy are excellent, surgery is frequently associated with postoperative complications (an unfavourable result of the operation), particularly bladder dysfunction (Suprasert 2010). As bladder dysfunction diminishes QoL and is one of the most distressing complications following radical hysterectomy (Zhou 2016), effective interventions are needed in order to prevent or reduce the severity of the symptoms of this condition. Several postoperative interventions have been proposed to prevent bladder dysfunction following radical hysterectomy. To our knowledge, there has been no systematic review evaluating the effectiveness and safety of postoperative interventions for preventing bladder dysfunction following a radical hysterectomy in women with cervical cancer.
Objectives
To evaluate the effectiveness and safety of postoperative interventions for preventing bladder dysfunction following radical hysterectomy in women with early‐stage cervical cancer (FIGO stage IA2 to IIA2).
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs).
Types of participants
Women aged 18 years or over with early‐stage cervical cancer who have undergone radical hysterectomy (Piver type II, Piver type III, Querleu‐Morrow class B2, or class C1). Early‐stage cervical cancer was defined as cervical cancer stage IA2 to IIA2 by either the 2009 or 2018 FIGO staging system. If studies included women with other types of gynaecological cancer (i.e. endometrial cancer), we planned to contact the trial authors to retrieve data related to participants with cervical cancer only. If this was not possible, we planned to include the study only if at least 80% of participants were diagnosed with cervical cancer.
Types of interventions
We planned to include any trial that attempted to compare the following.
A pharmacological agent and placebo or standard care.
A non‐pharmacological intervention and a standard care. Specific non‐pharmacological interventions include postoperative suprapubic catheterisation, bladder training and acupuncture.
A pharmacological agent and a non‐pharmacological intervention.
A pharmacological agent and another agent.
A non‐pharmacological intervention and another intervention.
Combinations of intervention and placebo or standard care.
Combinations of intervention and single intervention.
Combinations of intervention and other combinations.
Types of outcome measures
Primary outcomes
Rate of spontaneous voiding recovery at one week after surgery. We defined spontaneous voiding recovery as a voluntary void that has 50 mL or less of urine remaining in the bladder, measured by clean intermittent catheterisation after the woman feels as though her bladder is empty.
Quality of life (QoL), determined using a scale that has been validated in accordance with the norms reported in a peer‐reviewed publication (i.e. the European Organisation for Research and Treatment of Cancer (EORTC) QLQ‐CX24 cervical cancer‐specific QoL questionnaire (Greimel 2006)).
Secondary outcomes
Time after surgery to a post‐void residual urine volume of 50 mL or less (days). Post‐void residual urine was defined as the amount of urine retained in the bladder after a voluntary void, measured by clean intermittent catheterisation after the participant feels as though bladder is empty.
Time after surgery to a post‐void residual urine volume of 75 mL or less (days). See Differences between protocol and review
Time after surgery to a post‐void residual urine volume of 100 mL or less (days). See Differences between protocol and review
Adverse events (excluding bladder dysfunction). We categorised the severity of the following adverse events according to the Common Terminology Criteria for Adverse Events (CTCAE 2010). (A) Acute complications including postoperative mortality; digestive complications (e.g. bowel injuries, bowel obstruction); urological injuries; haematological complications (e.g. anaemia from acute blood loss); and cardiovascular and thromboembolic complications (e.g. myocardial infarction, arterial thrombosis, venous thrombosis, pulmonary embolism). (B) Late complications including symptomatic lymphocysts; incisional hernia; digestive complications (e.g. intestinal obstruction and fistula formation); and urological complications (e.g. ureteral stenosis and fistulae).
Post‐void residual urine volume (amount of urine measured by clean intermittent catheterisation after the participant feels that her bladder is empty) at 1, 6 and 12 months after surgery (mL)
Rate of urinary tract infections in the first month after surgery, diagnosed by urine culture
Subjective urinary symptoms, determined using a standard questionnaire (i.e. International Prostate Symptom Score (Barry 1992))
Flow rate (mL per second), obtained by urodynamic measurement
Maximum flow rate (mL per second) and number of women with low maximum flow rate (< 15 mL per second, as defined by Abrams 2003), obtained by urodynamic measures
Detrusor pressure at maximum flow and number of women with low detrusor pressure at maximum flow (< 25 cmH2O)
Bladder compliance (mL/cmH2O). See Differences between protocol and review
Poor bladder compliance, defined as bladder compliance less than 10 mL/cmH2O following the guidelines of the International Continence Society (Cho 2009)
We planned to present a 'Summary of findings' table reporting the following outcomes listed in order of priority.
Rate of spontaneous voiding recovery at one week after surgery.
QoL.
Time after surgery to a post‐void residual urine volume of 50 mL or less (days).
Adverse events.
Post‐void residual urine volume one month after surgery.
Urinary tract infections in the first month after surgery.
Subjective urinary symptoms.
Search methods for identification of studies
We included only randomised controlled trials (RCTs), irrespective of the language of publication, publication status or sample size.
Electronic searches
We searched the following electronic databases on 20 April 2020.
The Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 4) in the Cochrane Library;
MEDLINE via Ovid (1946 to April week 2 2020);
Embase via Ovid (1980 to 2020 week 16).
Appendix 5, Appendix 6, and Appendix 7 display the search strategies for CENTRAL, MEDLINE, and Embase, respectively.
Searching other resources
We searched the World Health Organization International Clinical Trials Registry Platform (who.int/ictrp/en/) and ClinicalTrials.gov to identify any ongoing trials. If we identified ongoing trials that had not been published, we planned to approach the principal investigators and major co‐operative groups active in this area to ask for relevant data. We searched the following databases for grey literature: Open‐Grey (opengrey.eu/) and Index to theses (proquest.com/products-services/pqdt_uk_ireland.html).
Hand searching
We handsearched reports of conferences from the following sources.
Annual Meeting of the Society of Gynecologic Oncology.
Annual Meeting of the International Gynecologic Cancer Society.
Annual Meeting of the European Society of Medical Oncology.
Annual Meeting of the British Gynaecological Cancer Society.
Biennial Meeting of the Asian Society of Gynecologic Oncology.
Biennial Meeting of Asia and Oceania Federation of Obstetrics and Gynaecology.
Biennial Meeting of the European Society of Gynaecologic Oncology.
We checked the citation lists of the included studies and key textbooks for potentially relevant references. We searched for papers in all languages and translated them, if necessary. We planned to include unpublished trials only if trial data and methodological descriptions were provided in written form or through direct contact with the trial authors.
Data collection and analysis
Selection of studies
We downloaded all titles and abstracts retrieved via an electronic search of the Endnote reference management database. After duplicates were removed, we transferred these data to Covidence (covidence.org). Two review authors (AA and CK) examined the remaining references independently. We excluded those studies which clearly did not meet the inclusion criteria, and we obtained full‐text copies of potentially relevant references. Two review authors (AA and CK) independently assessed the eligibility of the retrieved reports or publications. We resolved any disagreement through discussion or, if required, we planned to consult a third review author (KG or PL). We identified and excluded duplicates and collated multiple reports of the same study so that each study, rather than each report, is the unit of interest in the review. We used the details obtained from the selection process in Covidence to complete a PRISMA flow diagram and 'Characteristics of excluded studies' table (Liberati 2009).
Data extraction and management
Two review authors (AA and CK) independently extracted study characteristics and outcome data from included studies using Covidence. We noted in the 'Characteristics of included studies' table if outcome data were not reported in a usable way. We resolved disagreements by consensus or by involving a third review author (KG or TT). One review author (CK) checked study characteristics for accuracy against the trial report.
For included studies, we extracted the following data.
Author, year of publication, and journal citation (including language).
Country.
Setting.
Inclusion and exclusion criteria.
Study methodology.
-
Study population and disease characteristics:
total number enrolled;
participant characteristics;
age;
co‐morbidities;
other baseline characteristics;
percentage of participants with non‐cervical cancer (only RCTs involving mixed gynaecologic malignancies);
FIGO stage of cervical cancer;
the histopathological subtype of cervical cancer;
tumour size (largest tumour diameter);
the radicality of surgery (Piver or Querleu‐Morrow).
-
Intervention details:
schedule of bladder training;
suprapubic cystostomy technique;
acupuncture;
cholinergic agents (dose, duration).
-
Comparison:
placebo;
no intervention.
Risk of bias in the study (see below).
Duration of follow‐up.
Outcomes: for each outcome, we extracted the outcome definition and unit of measurement (if relevant); for adjusted estimates, we recorded variables adjusted for in analyses.
Results: we extracted the number of participants allocated to each intervention group, the total number analysed for each outcome, and the missing participants.
Notes: funding for trial and notable conflicts of interest of trial authors.
Assessment of risk of bias in included studies
We assessed and reported on the methodological quality and risk of bias in included studies in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019), which recommends the explicit reporting of the following individual elements for RCTs.
Selection bias: random sequence generation and allocation concealment.
Performance bias: blinding of participants and personnel (treatment providers).
Detection bias: blinding of outcome assessment.
Attrition bias: incomplete outcome data.
Reporting bias: selective reporting of outcomes.
Other possible bias.
We considered outcome data as complete if at least 80% of participants underwent follow‐ups and were assessed for primary outcomes. Two review authors (AA and CK) independently applied the 'Risk of bias' tool and resolved differences by discussion or by appeal to a third review author (KG or PL). We judged each item as being at high, low or unclear risk of bias as set out in the criteria displayed in Appendix 8. We provided a quote from the study report or a statement, or both, as justification for our judgement for each item in the 'Risk of bias' table. We summarised results in both a 'Risk of bias' graph and a 'Risk of bias' summary. When interpreting treatment effects and meta‐analyses, we took into account the risk of bias in the studies that contribute to that outcome. Where information on risk of bias relates to unpublished data or correspondence with trial authors, we planned to note this in the table.
Measures of treatment effect
We used the following measures of the effect of treatment.
For dichotomous outcomes (e.g. rate of spontaneous voiding recovery one week after surgery, rate of urethral catheter removal, rate of urinary tract infections, number of participants with normal detrusor pressure at maximum flow, adverse events), we analysed data based on the number of events and the number of women assessed in the intervention and comparison groups. We used these to calculate the risk ratio and 95% confidence interval.
For continuous outcomes (e.g. duration of postoperative retained urethral catheterisation, post‐void residual urine volume and QoL measures), we analysed data based on the means, standard deviations and number of women assessed for both the intervention and comparison groups to calculate the mean differences between treatment arms with their 95% confidence intervals. If the mean difference was reported without individual group data, we used this to report the study results. If more than one study measured the same outcome using different tools, we calculated the standardised mean difference and 95% confidence interval using the inverse variance method.
For time‐to‐event data (e.g. time after surgery to a post‐void residual urine volume of 50 mL or less), we planned to extract the log of the hazard ratio (logHR) and its standard error from trial reports. If these were not reported, we planned to estimate the logHR and its standard error using the methods of Parmar 1998.
Unit of analysis issues
We included studies in which individual women were randomised. In a study with multiple intervention groups, we planned to combine all relevant experimental intervention groups into a single group to create a single pair‐wise comparison, where possible (Higgins 2019).
Dealing with missing data
We planned to contact the original investigators to request missing data. If we could not contact the investigators or could not obtain the requested missing data, we planned to analyse only the available data and not to impute missing outcome data for any of the outcomes.
Assessment of heterogeneity
We clinically assessed heterogeneity by visual inspection of forest plots. We assessed statistical heterogeneity in each meta‐analysis using the I2 statistic and Chi2 test (Higgins 2003). We regarded heterogeneity as substantial if the I2 statistic value was greater than 50% or there was a low P value (< 0.10) in the Chi2 test for heterogeneity (Deeks 2001; Higgins 2019). If there was substantial statistical heterogeneity, we planned to carry out subgroup analyses to assess differences among the included studies. However, if there was both clinical and methodological heterogeneity across included studies, we planned to not report pooled results from meta‐analysis, but instead use a narrative approach to data synthesis.
Assessment of reporting biases
See Differences between protocol and review.
We were unable to assess reporting bias, as only four studies met our inclusion criteria.
Data synthesis
We applied the random‐effects model with inverse variance weighting for all meta‐analyses (DeSimonian 1986). We performed statistical analysis using Review Manager 5.4 (Review Manager 2014).
For time‐to‐event data, we planned to pool hazard ratios using the generic inverse variance.
For any dichotomous outcomes, we calculated the risk ratios for each study and then pooled them.
For continuous outcomes, we pooled the mean differences among the treatment arms, if all trials measure the outcome on the same scale; otherwise we planned to pool standardised mean differences
Subgroup analysis and investigation of heterogeneity
See Differences between protocol and review.
We intended to carry out subgroup analyses in order to assess the effect of the following factors.
Tumour size (2 cm or less versus more than 2 cm).
Surgical approach (laparotomy versus minimally invasive surgery).
Nerve‐sparing approach during a radical hysterectomy (yes versus no).
Radicality of surgery (Piver type II versus Piver type III, or Querleu‐Morrow class B2 versus class C1).
Extent of pelvic lymph node dissection determined by the number of lymph nodes removed.
We planned to assess subgroup differences using the interaction tests available within Review Manager 2014. We planned to report the results of subgroup analyses by quoting the Chi2 statistic and P value, the interaction test, and the I2 statistic. However, we did not perform subgroup analysis, as most analyses were based on only one or two included studies. Nevertheless, we acknowledged these factors in the interpretation of review findings.
Sensitivity analysis
See Differences between protocol and review.
We were unable to conduct any of the planned sensitivity analyses due to insufficient data. If more studies are included in a future update, we plan to perform sensitivity analyses in order to assess the effect of the following factors.
Repeating the analysis excluding unpublished studies (if any).
Repeating the analysis excluding studies judged to be at 'high' or 'unclear' risk of bias for allocation concealment.
Summary of findings and assessment of the certainty of the evidence
We created Summary of findings tables to summarise the results of the meta‐analyses conducted for each of the outcomes, as outlined in the section Types of outcome measures. We graded the overall certainty of the evidence for each outcome according to the GRADE approach, which takes into account issues related not only to internal validity (risk of bias, inconsistency, imprecision, publication bias) but also to external validity, such as directness of results (Langendam 2013). We created a 'Summary of findings' table based on the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011), and used GRADEpro GDT (Table 1; Table 2).
Summary of findings 1. Bethanechol compared to placebo for preventing bladder dysfunction after radical hysterectomy in women with early‐stage cervical cancer.
| Comparison 1: Bethanechol versus placebo | ||||||
| Patients: women with early‐stage cervical cancer undergoing radical hysterectomy Setting: tertiary hospital Intervention: bethanechol Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
|
Assumed risk: placebo |
Corresponding risk: bethanechol |
|||||
| Rate of spontaneous voiding recovery 1 week after surgery | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Quality of life (QoL) | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Time after surgery to post‐void residual volume of urine ≤ 50 mL (days) | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Adverse events | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Post‐void residual urine volume (mL) at 1 month after surgery | Mean 98.4 | MD 37.4 lower (60.35 lower to 14.45 lower) | ‐ | 39 participants (1 RCT) | ⊕⊝⊝⊝ Very low a,b | |
| Urinary tract infections in the first month after surgery | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Subjective urinary symptoms | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
aThe evidence was downgraded by two levels due to imprecision (combination of sparse data and a low number of events). bThe evidence was downgraded by one level due to unclear risk of selection bias.
Summary of findings 2. Suprapubic catheterisation compared to intermittent self‐catheterisation for preventing bladder dysfunction after radical hysterectomy in women with early‐stage cervical cancer.
| Comparison 2: Suprapubic catheterisation versus intermittent self‐catheterisation | ||||||
| Patients: women with early‐stage cervical cancer Setting: tertiary hospital Intervention: suprapubic catheterisation (SPC) Comparison: intermittent self‐catheterisation (ISC) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk: suprapubic catheterisation | Corresponding risk: intermittent catheterisation | |||||
| Rate of spontaneous voiding recovery 1 week after surgery | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Quality of life (QoL) | ‐ | ‐ | No differences of QoL between the comparison groups. See comment | ‐ | ‐ | Data were insufficient for calculating the relative measures |
| Time after surgery to post‐void residual volume of urine ≤ 50 mL (days) | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Adverse events (acute complication after surgery) | 12 per 100 | 9 per 100 fewer (3 fewer to 30 more) | RR 0.77 (0.24 to 2.49) | 71 participants (1 RCT) | ⊕⊝⊝⊝ Very low a,b | 4 of 33 in SPC group versus 6 of 38 in ISC group |
| Post‐void residual urine volume (mL) at 1 month after surgery | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Urinary tract infections in the first month after surgery | 35 per 100 | 27 per 100 (18 fewer to 39 more) | RR 0.77 (0.53 to 1.13) | 95 participants (2 RCTs) | ⊕⊝⊝⊝ Very low a,c |
Nwabineli 1993: 7 of 10 in SPC group versus 13 of 14 in ISC group Suprasert 2002: 8 of 33 in SPC group versus 11 of 38 in ISC group |
| Subjective urinary symptoms | ‐ | ‐ | No differences between the comparison group See comment | ‐ | ‐ | Available data were insufficient to calculate the relative measures of the effect of interventions. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
aThe evidence was downgraded by two levels due to serious imprecision (small sample size and wide CI crossing the line of no effect). bThe evidence was downgraded by one level due to indirectness (reporting adverse events of unclear severity and unclear their association with the intervention). cThe evidence was downgraded by one level due to unclear risk of selection bias.
High certainty: the true effect lies close to that of the estimate of the effect.
Moderate certainty: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low certainty: the true effect may be substantially different from the estimate of the effect.
Very low certainty: the true effect is likely to be substantially different from the estimate of effect.
We downgraded the evidence from 'high' certainty by one level for each serious (or by two for each very serious) limitation.
Results
Description of studies
Results of the search
An extensive search of the literature databases in April 2020 yielded the following results: CENTRAL (71 references), MEDLINE (758 references), and Embase (1055 references). After eliminating duplicates, we screened titles and abstracts of 1464 references and excluded 1444 that obviously did not meet the review inclusion criteria. Of the 20 references that potentially met the review inclusion criteria, we excluded ‐ with reasons ‐ 15 reports after reviewing the full texts (see Characteristics of excluded studies). The search found two ongoing studies (Boonthongtho 2016; Sun 2017; see Characteristics of ongoing studies), and one study awaiting classification (Cheng 2017; see Characteristics of studies awaiting classification). Figure 1 shows the PRISMA flow chart for study selection.
1.
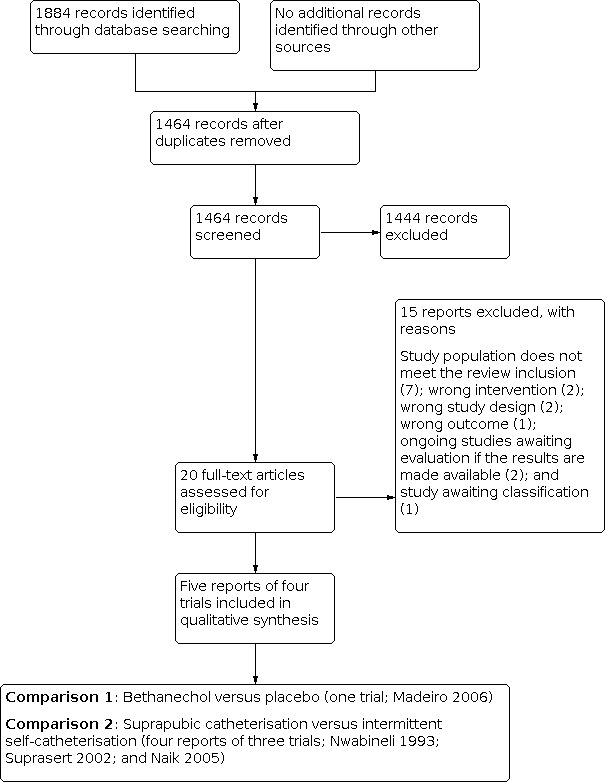
Study flow diagram.
Included studies
Four studies (five reports) met the inclusion criteria (Nwabineli 1993; Suprasert 2002; Naik 2005; Madeiro 2006). One report (Roberts 2006) described updated results of Naik 2005. See Characteristics of included studies table for details of each study.
Participants
Nwabineli 1993 was a two‐armed parallel RCT conducted between September 1989 and February 1990. Participants were 24 women with cervical cancer stage IB or IIA who underwent type II or type III radical hysterectomy. Inclusion criteria were age less than 50 years, no history of voiding problems, and no previous radiotherapy. Exclusion criteria were a history of tricyclic antidepressants or anticholinergics used.
Suprasert 2002 was a two‐armed parallel RCT conducted between September 1998 and June 1999. Participants were 71 women with cervical cancer stage IB1 or IIA with normal bladder function and urinary analysis who underwent type III radical hysterectomy following bilateral pelvic lymphadenectomy. Women were considered ineligible if they had a history of urinary tract infection more than two times per year, or a history of renal stone or bladder calculi, or previous urinary incontinence, or intraoperative bowel or urinary tract complication, or inability to perform intermittent self‐catheterisation.
Naik 2005 was a two‐armed parallel RCT undertaken between July 1999 and June 2002. Participants were 40 women with cervical cancer stage IB1 who underwent type III radical hysterectomy. Updated data of this report were subsequently published in 2006 (Roberts 2006).
Madeiro 2006 was a four‐armed parallel RCT conducted between March 2002 and February 2003. Participants were 79 women with cervical cancer stage IB who underwent a standard class III hysterectomy with bilateral pelvic lymphadenectomy via laparotomy approach. An indwelling urethral catheter remained postoperatively in all patients for 10 days. Exclusion criteria were previous pelvic radiation therapy, or recurrent urinary tract infections, or urinary calculi, or uncontrolled diabetes mellitus, or bronchial asthma, or potential risk factors for cisapride use such as heart disease and family history of sudden death. We excluded two arms that administered cisapride and cisapride plus bethanechol due to the fact that cisapride now has been restricted in the USA and Europe because of its serious side effects.
Surgical procedure
Radical hysterectomies performed in Nwabineli 1993, Suprasert 2002, and Naik 2005 were carried out via laparotomy approach. The type of surgical approach for radical hysterectomy in Madeiro 2006 was unknown.
Interventions
Madeiro 2006 compared bethanechol versus placebo. Dosage of oral bethanechol was 10 mg repeated every 8 hours.
Nwabineli 1993, Suprasert 2002, and Naik 2005 compared suprapubic catheterisation (SPC) versus intermittent self‐catheterisation (ISC). Suprapubic catheterisation consisted of insertion of a Bonanno suprapubic catheter at the time of surgery, followed by free drainage, followed by catheter removal at five to seven days after the surgery.
Outcomes reported
None of the included studies reported rate of spontaneous voiding recovery at one week after surgery, time to a post‐void residual urine volume of 50 mL or less, post‐void residual urine volume at 6 and 12 months after surgery, and poor bladder compliance.
Nwabineli 1993 reported time after surgery to a post‐void residual urine volume of less than 100 mL, adverse events, and rate of urinary tract infections in the first month after surgery.
Suprasert 2002 reported time after surgery to a post‐void residual urine volume of less than 75 mL, adverse events, and rate of urinary tract infections in the first month after surgery.
Naik 2005 reported QoL, time after surgery to a post‐void residual urine volume of less than 100 mL, adverse events, rate of urinary tract infections in the first month after surgery, and subjective urinary symptoms.
Madeiro 2006 reported post‐void residual urine volume one month after surgery, flow rate, maximum flow rate, number of women with low maximum flow rate, number of women with low detrusor pressure at maximum flow, and bladder compliance.
Excluded studies
See Characteristics of excluded studies, Characteristics of ongoing studies, and Characteristics of studies awaiting classification.
We excluded seven reports because their participants were not the population that this review aimed to assess (Kuo 2005; Dy Echo 2011; Manchana 2011; Dy Echo 2012; Fanfani 2015; Wang 2015; Gong 2016). We excluded Pengsaa 1992 and Wells 2008 because their studies were not RCTs. We excluded Chen 2012 and Chen 2014 because of wrong intervention. We excluded Li 2019 because of wrong outcomes. In addition, we excluded two ongoing studies (Boonthongtho 2016; Sun 2017), and one conference proceeding awaiting classification (Cheng 2017).
Risk of bias in included studies
See Characteristics of included studies table, Figure 2, and Figure 3 for full details.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Suprasert 2002 stated that the participants were randomised by drawing a sealed envelope that contained computer‐generated random numbers thus indicating a low risk of selection bias.
Madeiro 2006 stated that the participants were allocated using a computerised randomisation schedule. However, they did not state the concealment process. This trial therefore was at unclear risk of selection bias.
Naik 2005 stated that the participants were randomised by drawing a sealed envelope that developed from an independent administrator, but did not state the methods of random sequence generation. Consequently, this trial was judged as having an unclear risk of selection bias.
Nwabineli 1993 stated that the participants were randomised using random sampling numbers. However, they did not state the allocation concealment process. This trial therefore was at unclear risk of selection bias.
Blinding
Madeiro 2006 stated that all medications were provided in packages of identical appearance. Identification was only made by a standardised code. Randomisation was only revealed at the end of the trial and was controlled by an independent investigator. This trial, therefore, was at low risk of performance and detection biases.
Blinding of participants and personnel was not feasible in Nwabineli 1993, Suprasert 2002, and Naik 2005, which compared suprapubic catheterisation versus intermittent self‐catheterisation. However, the outcomes of interest (i.e. time after surgery to a post‐void residual urine volume less than 75 mL, adverse events, and rate of urinary tract infections in the first month after surgery) were unlikely to be affected by lack of blinding of participants and personnel. Hence, we considered these studies as having a low risk of bias for this domain.
Incomplete outcome data
All included studies were at low risk of attrition bias as they had low percentages of withdrawals and dropouts (Nwabineli 1993; Suprasert 2002; Naik 2005; Madeiro 2006). See Characteristics of included studies for the proportion of participants analysed.
Selective reporting
None of the included studies reported the rate of spontaneous voiding recovery one week after surgery, or post‐void residual urine volume at 6 and 12 months after surgery. Quality of life (QoL), adverse events and subjective urinary symptoms, which are important outcomes, were rarely reported. An adverse event was assessed only in Suprasert 2002. Naik 2005 reported QoL and subjective urinary symptoms but available data, however, were insufficient to calculate the relative measures of the effect of interventions. Due to a lack of reported outcomes that are the elements necessary for decision‐making, all included studies thus were at high risk of reporting bias (Higgins 2017).
Other potential sources of bias
There was no Information indicating other important risks of bias. Accordingly, all included studies were judged as having a low risk of bias for this domain.
Effects of interventions
None of the studies reported the rate of spontaneous voiding recovery one week after surgery, time after surgery to a post‐void residual urine volume of 50 mL or less, post‐void residual urine volume at 6 and 12 months after surgery, and poor bladder compliance. Consequently, we added time after surgery to a post‐void residual urine volume of 75 mL or less, and 100 mL or less, respectively, and bladder compliance, as additional secondary outcomes (see Differences between protocol and review).
Madeiro 2006 compared bethanechol with placebo. Nwabineli 1993, Suprasert 2002, and Naik 2005 compared suprapubic catheterisation (SPC) with intermittent self‐catheterisation (ISC).
Comparison 1: Bethanechol versus placebo
Madeiro 2006 reported four‐arm comparisons including placebo; bethanechol alone given 10 mg orally every eight hours; cisapride alone given 10 mg orally every eight hours; and a combination of 10 mg of bethanechol and cisapride given orally every eight hours. As cisapride has been restricted in the USA and Europe due to its serious side effects, including cardiac arrhythmias (irregular heart rhythms) and death, we, therefore, included only the data obtained from participants allocated to placebo and bethanechol alone in the analyses.
Primary outcomes
Rate of spontaneous voiding recovery at one week after surgery
No data were reported for this outcome.
Quality of life
No data were reported for this outcome.
Secondary outcomes
Time after surgery to a post‐void residual urine volume of 50 mL or less (days)
No data were reported for this outcome.
Time after surgery to a post‐void residual urine volume of 75 mL or less (days)
No data were reported for this outcome.
Time after surgery to a post‐void residual urine volume of 100 mL or less (days)
No data were reported for this outcome.
Adverse events
No data were reported for this outcome.
Post‐void residual urine volume at one month after surgery
Post‐void residual urine volume assessed at one month after surgery among participants receiving bethanechol was lower than those in the placebo group (MD ‐37.4 mL, 95% CI ‐60.35 to ‐14.45; 39 participants; very low certainty evidence; Analysis 1.1).
1.1. Analysis.

Comparison 1: Bethanechol versus placebo, Outcome 1: Post‐void residual urine volume one month after surgery
Post‐void residual urine volume at six months after surgery
No data were reported for this outcome.
Post‐void residual urine volume at 12 months after surgery
No data were reported for this outcome.
Rate of urinary tract infections in the first month after surgery
No data were reported for this outcome.
Subjective urinary symptoms
No data were reported for this outcome.
Flow rate (mL per second)
Flow rate at one month after surgery among participants receiving bethanechol was higher than that noted among participants allocated to placebo (MD 1.20, 95% CI 0.25 to 2.15; 39 participants; Analysis 1.2).
1.2. Analysis.

Comparison 1: Bethanechol versus placebo, Outcome 2: Flow rate (mL per second)
Maximum flow rate (mL per second)
The maximum flow rate at one month after surgery among participants receiving bethanechol was higher compared to those who were assigned to the placebo group (MD 3.20, 95% CI 1.82 to 4.58; 39 participants; Analysis 1.3).
1.3. Analysis.

Comparison 1: Bethanechol versus placebo, Outcome 3: Maximum flow rate (mL per second)
Number of women with low maximum flow rate (< 15 mL per second)
Participants receiving bethanechol had a lower risk of having a low maximum flow rate than those given placebo (RR 0.36, 95% 0.18 to 0.72; 39 participants; Analysis 1.4).
1.4. Analysis.

Comparison 1: Bethanechol versus placebo, Outcome 4: Number of women with low maximum flow rate (< 15 mL per second)
Detrusor pressure at maximum flow (cmH2O)
Detrusor pressure at maximum flow, assessed at one month after surgery among participants receiving bethanechol was higher than that noted among participants receiving placebo (MD 8.4, 95% CI 4.92 to 11.88; 39 participants; Analysis 1.5).
1.5. Analysis.

Comparison 1: Bethanechol versus placebo, Outcome 5: Detrusor pressure at maximum flow (cmH2O)
Number of women with low detrusor pressure at maximum flow (< 25 cmH2O)
Participants receiving bethanechol had a lower risk of encountering low detrusor pressure at maximum flow than those given placebo (RR 0.25, 95% CI 0.10 to 0.63; 39 participants; Analysis 1.6).
1.6. Analysis.

Comparison 1: Bethanechol versus placebo, Outcome 6: Number of women with low detrusor pressure at maximum flow
Bladder compliance (mL per cmH2O)
See Differences between protocol and review.
The trial did not report poor bladder compliance but reported bladder compliance assessed at one month after surgery. There was no difference in bladder compliance evaluated at one month following surgery between the two comparison groups (MD 8.90, 95% CI ‐0.33 to 18.13; 39 participants; Analysis 1.7).
1.7. Analysis.

Comparison 1: Bethanechol versus placebo, Outcome 7: Bladder compliance
Comparison 2: Suprapubic catheterisation (SPC) versus intermittent self‐catheterisation (ISC)
Four reports of Nwabineli 1993, Suprasert 2002, and Naik 2005 compared SPC versus ISC.
Primary outcomes
Rate of spontaneous voiding recovery at one week after surgery
None of the studies reported the rate of spontaneous voiding recovery one week after surgery.
Quality of life
Naik 2005 and their update report assessed QoL among 36 participants at 3 weeks, 6 weeks and 12 weeks after surgery, using EORTC QLQ C30 questionnaires. The trial found no significant differences between the two groups. Nevertheless, data were insufficient for calculating MD of QoL scores among the comparison groups.
Secondary outcomes
Time after surgery to a post‐void residual urine volume 50 mL or less (days)
None of the studies reported this outcome.
Time after surgery to a post‐void residual urine volume of 75 mL or less (days)
See Differences between protocol and review.
Suprasert 2002, assessing 71 participants, found that women given SPC went a longer time to a post‐void residual urine volume of 75 mL or less than women given ISC (MD 4.2 days, 95% CI 1.17 to 7.23; Analysis 2.1).
2.1. Analysis.

Comparison 2: Suprapubic catheterisation versus intermittent self‐catheterisation, Outcome 1: Time to post‐void residual volume of urine < 75 mL after surgery (days)
Time after surgery to a post‐void residual urine volume of 100 mL or less (days)
See Differences between protocol and review.
Nwabineli 1993 and Naik 2005 reported time after surgery to a post‐void residual urine volume of 100 mL or less. A meta‐analysis assessing 64 women showed that women given SPC went a shorter time after surgery to a post‐void residual urine volume of 100 mL or less than women given ISC (MD ‐11.02 days, 95% CI ‐17.78 to ‐4.26; two studies, very low certainty evidence; Analysis 2.2). The percentage of variability in effect estimates due to heterogeneity rather than to chance was not important (I2 = 0%).
2.2. Analysis.

Comparison 2: Suprapubic catheterisation versus intermittent self‐catheterisation, Outcome 2: Time to post‐void residual volume of urine < 100 mL after surgery (days)
Adverse events
Suprasert 2002, assessing 71 participants, reported acute complications after surgery. The trial showed no difference in risk of acute complications after surgery (RR 0.77, 95% CI 0.24 to 2.49; very low certainty evidence; Analysis 2.3) between participants who underwent SPC (four events in 33 participants) and those who underwent ISC (six events in 38 participants).
2.3. Analysis.

Comparison 2: Suprapubic catheterisation versus intermittent self‐catheterisation, Outcome 3: Adverse events; acute complications
Post‐void residual urine volume at 1, 6 and 12 months after surgery
None of the studies reported this outcome.
Rate of urinary tract infections in the first month after surgery
In Nwabineli 1993, 7 of 10 participants assigned to the SPC group and 13 of 14 participants assigned to the ISC group experienced urinary tract infection. In Suprasert 2002, 8 of 33 participants and 11 of 38 participants assigned to the SPC and ISC groups, respectively, experienced urinary tract infection.
A meta‐analysis of Nwabineli 1993 and Suprasert 2002, assessing 95 participants, showed no difference in risk of the rate of urinary tract infections during the first month after surgery (RR 0.77, 95% CI 0.53 to 1.13; very low certainty evidence; Analysis 2.4). The percentage of variability in effect estimates due to heterogeneity rather than to chance was not important (I2 = 0%).
2.4. Analysis.

Comparison 2: Suprapubic catheterisation versus intermittent self‐catheterisation, Outcome 4: Urinary tract infections during the one‐month period following surgery
Subjective urinary symptoms
Naik 2005 and their update publication reported subjective urinary symptoms using a urinary symptoms questionnaire (USQ). This trial found no differences in terms of subjective urinary symptoms between participants undergoing suprapubic catheterisation and those who underwent intermittent self‐catheterisation. Available data, however, were insufficient to calculate the relative measures of the effect of interventions. We were unable to obtain additional data by contacting the authors of the trial.
Flow rate (mL per second)
None of the studies under this comparison reported this outcome.
Maximum flow rate (mL per second)
None of the studies under this comparison reported this outcome.
Number of women with low maximum flow rate (< 15 mL per second)
None of the studies under this comparison reported this outcome.
Detrusor pressure at maximum flow (cmH2O)
None of the studies under this comparison reported this outcome.
Number of women with low detrusor pressure at maximum flow (< 25 cmH2O)
None of the studies under this comparison reported this outcome.
Bladder compliance
None of the studies under this comparison reported this outcome.
Discussion
The findings of this review were based on five reports of four included studies (see Figure 1). One trial compared bethanechol versus placebo (Madeiro 2006). Three studies compared SPC versus ISC (Nwabineli 1993; Suprasert 2002; Naik 2005).
Summary of main results
No information on the rate of spontaneous voiding recovery at one week following operation was reported in any of the included studies. QoL, adverse events, and subjective urinary symptoms were rarely assessed in the current evidence.
-
In a comparison of bethanechol versus placebo, participants given bethanechol:
probably had lower amounts of post‐void residual urine volume at one month after surgery (MD ‐37.4 mL, 95% CI ‐60.35 to ‐14.45; one trial, 39 participants; Analysis 1.1); and
probably had better bladder functions, assessed at one month after operation, including higher flow rate (MD 1.20, 95% CI 0.25 to 2.15; 1 trial, 39 participants; Analysis 1.2); higher maximum flow rate (MD 3.20, 95% CI 1.82 to 4.58; 1 trial, 39 participants; Analysis 1.3); lower risk of having a low maximum flow rate (RR 0.36, 95% CI 0.18 to 0.72; 1 trial, 39 participants; Analysis 1.4); and higher detrusor pressure at maximum flow (MD 8.4, 95% CI 4.92 to 11.88; 1 trial, 39 participants; Analysis 1.5).
Results of the comparison between SPC and ISC among the included studies are contradictory. Meta‐analysis assessing 64 women noted that compared to ISC, SPC may shorten time after surgery to post‐void residual urine volume of 100 mL or less (MD ‐11.02 days, 95% CI ‐17.78 to ‐4.26; 2 studies, 64 participants; Analysis 2.2). However, another included study reported a longer time after surgery to post‐void residual urine volume of 75 mL or less among women receiving SPC than those who were allocated to the ISC group (MD 4.2 days, 95% CI 1.17 to 7.23; 1 trial, 71 participants; Analysis 2.1). There may have been little or no difference in the risks of short‐term complication (RR 0.77, 95% CI 0.24 to 2.49; 1 trial, 71 participants; Analysis 2.3), and urinary tract infections in the first month after surgery (RR 0.77, 95% CI 0.53 to 1.13; 2 studies, 95 participants; Analysis 2.4).
Overall completeness and applicability of evidence
We identified five published reports from four RCTs that included two comparisons of the interventions given to prevent bladder dysfunction after radical hysterectomy for cervical cancer including bethanechol versus placebo and SPC versus ISC. The primary outcomes of this review were the rate of spontaneous voiding recovery at one week after surgery and QoL. However, none of the studies reported the rate of spontaneous voiding recovery one week after surgery. In addition, only one trial assessed QoL, but data were insufficient for assessing the effect of the intervention.
Applicability of evidence is limited by the quantity and certainty of the review results. The lack of data regarding primary outcomes of interest in almost all included studies and the very low certainty of available evidence may impede the applicability of the review findings. It is thus difficult to make any adequate judgements regarding the effectiveness of the interventions assessed in this review. Additionally, it is important to note that the surgical techniques applied in almost all of the participants were conventional laparotomy radical hysterectomy. Therefore, the results may not be fully applicable to other surgical techniques (i.e. laparoscopic radical hysterectomy or nerve‐sparing radical hysterectomy).
Quality of the evidence
In the protocol, we planned to assess the certainty of evidence by eleven relevant outcomes including the rate of spontaneous voiding recovery at one week after surgery, QoL, time after surgery to a post‐void residual urine volume of 50 mL or less, adverse events, post‐void residual urine volume at one month after surgery, rate of urinary tract infection in the first month after surgery, and subjective urinary symptoms (Aue‐aungkul 2017).
As the review included only four studies, we obtained evidence from few studies and small number of participants for each comparison. Using GRADE assessments, we graded the certainty of the evidence as follows.
Bethanechol versus placebo: information on post‐void residual urine volume assessed at one month after surgery was downgraded to very low certainty evidence due to important imprecision (combination of sparse data and a low number of events) and unclear risk of selection bias. No information on the rate of spontaneous voiding recovery at one week following the operation, QoL, adverse events, urinary tract infection in the first month after surgery, and subjective urinary symptoms were reported under this comparison (see Table 1).
Suprapubic catheterisation versus intermittent self‐catheterisation: information on adverse events was downgraded to very low certainty evidence because of serious imprecision (small sample size and wide CI crossing the line of no effect) and indirectness. Evidence regarding the rate of urinary tract infection in the first month after surgery was downgraded to very low certainty because of serious imprecision and unclear risk of selection bias. Available data were insufficient to calculate the relative measures of the effect of interventions on QoL and subjective urinary symptoms. No information on the rate of spontaneous voiding recovery at one week and post‐void residual urine volume at one month were reported under this comparison (see Table 2).
Potential biases in the review process
With assistance from the Information Specialist of the Cochrane Gynaecological, Neuro‐oncology and Orphan Cancers Group, we were able to conduct a comprehensive literature search, including a search of the grey literature, conference proceedings and abstracts, citation lists of included studies, and registered databases of ongoing studies. In addition, bias was minimised in terms of the overall review process by following the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019).
As this review included only four studies, there remains the possibility of publication bias. We did not perform a funnel plot, as the analyses were limited to only one or two studies. Because of the small number of included studies, we did not carry out sensitivity and subgroup analyses as planned in the review protocol (Aue‐aungkul 2017). None of the review authors have any links to drug companies or financial interest in the prescription of the drug under evaluation, nor did they participate in the conduct of any of the included trials. Therefore, there were no known conflicts of interest of the authors of this review.
Agreements and disagreements with other studies or reviews
Interventions for preventing bladder dysfunction after radical hysterectomy can be classified as intraoperative and postoperative interventions. Nerve‐sparing radical hysterectomy is an example of an intraoperative intervention. Postoperative interventions include administration of parasympathomimetic agents to stimulate contraction of the detrusor muscle, SPC, bladder training, and acupuncture (see Description of the intervention).
Kietpeerakool 2019 recently reported a Cochrane Review and meta‐analysis assessing the effectiveness and potential harms of nerve‐sparing radical hysterectomy in women with early‐stage cervical cancer. Nerve‐sparing radical hysterectomy is a modified surgical technique developed to permit surgical removal (resection) of oncologically relevant tissues surrounding the cervical cancer lesion while preserving pelvic autonomic nerves. This review noted that the nerve‐sparing technique may lessen the risk of postoperative bladder dysfunction compared to the conventional radical hysterectomy. Nerve‐sparing radical hysterectomy reduced postoperative bladder dysfunctions in terms of a shorter time to post‐void residual urine volume of 50 mL or less (mean difference (MD) ‐13.21 days, 95% CI ‐24.02 to ‐2.41; low certainty evidence) and lower volume of post‐void residual urine measured one month following operation (MD ‐9.59 days, 95% CI ‐16.28 to ‐2.90; low certainty evidence).
To date, our review is the first systematic review evaluating the effectiveness and safety of various postoperative interventions for preventing bladder dysfunction after radical hysterectomy for early‐stage cervical cancer. Limited evidence suggested that bethanechol may minimise the risk of bladder dysfunction after radical hysterectomy by means of lower post‐void residual urine volume assessed one month after surgery and better results of urodynamic assessment. The effectiveness of different types of postoperative urinary catheterisation (suprapubic and intermittent self‐catheterisation), however, remained unproven by available evidence obtained from RCTs. In a retrospective cohort study conducted among women with early‐stage cervical cancer who underwent radical hysterectomy, postoperative SPC was associated with shorter time to trial of voiding and lower urinary tract infection compared to transurethral catheterisation (Wells 2008).
There are no RCTs assessing the effectiveness of bladder training for preventing bladder dysfunction following radical hysterectomy with a focus on women with early‐stage cervical cancer. Three reports of two RCTs assessing bladder training following radical hysterectomy which included women with early‐stage and locally advanced‐stage cervical cancer failed to note the effectiveness of this intervention (Santaguida 2012; Fanfani 2015; Gong 2016). One RCT reported in Santaguida 2012 and Fanfani 2015 found that the median duration of time after surgery to a post‐void residual urine volume of 100 mL or less was four days in the bladder training group (range 1 day to 40 days) and three days in the control group (range 1 day to 30 days). Gong 2016 reported no difference in the risk of urinary tract infections during the first month after surgery between the women assigned to bladder training (22.9%) and women in the control group (20.3%). Based on these findings, the effectiveness of bladder training for preventing bladder dysfunction following radical hysterectomy for cervical cancer, therefore, remained unconfirmed.
Authors' conclusions
Implications for practice.
In general, the studies included in this review are very small, and thus make inferences challenging in the face of very low certainty evidence. None of the included studies reported the primary outcomes and various important secondary outcomes that this review aimed to assess (i.e. rate of spontaneous voiding recovery one week after surgery, time to a post‐void residual urine volume of 50 mL or less, and post‐void residual urine volumes at 6 and 12 months after surgery.
Very low‐certainty evidence obtained from one small RCT indicated that bethanechol may minimise the risk of bladder dysfunction after radical hysterectomy by means of lower post‐void residual urine volume assessed at one month after surgery and better results of the urodynamic assessment. However, there was a lack of data regarding clinically important outcomes (i.e. rate of spontaneous voiding recovery, QoL, adverse events, urinary tract infection, and subjective urinary symptoms). There was insufficient evidence to indicate whether SPC lessens the risk of bladder dysfunction following radical hysterectomy.
Implications for research.
In light of the results of this review, bethanechol may be an option for the treatment of bladder dysfunction following radical hysterectomy. However, the benefits and harms of this cholinomimetic drug need to be reassessed in further adequately powered, high‐quality RCTs. If this pharmacological intervention can be shown to prevent bladder dysfunction, additional information regarding optimal dose and duration of treatment are required.
In addition, particular attention should be paid to an assessment of a combination therapy with bethanechol and an alpha‐adrenergic blocker, which was shown to be more effective than bethanechol alone in a previous RCT conducted among patients with various causes of underactive bladder (Yamanishi 2004; Kim 2017).
Importantly, any further studies should encompass an evaluation of the rate of spontaneous voiding recovery, QoL, time to a post‐void residual urine volume of 50 mL or less, post‐void residual urine volume, adverse events, and urinary tract infections which are clinically important outcomes for clinical‐decision making.
History
Protocol first published: Issue 11, 2017 Review first published: Issue 1, 2021
Acknowledgements
We would like to thank Jo Morrison for clinical and editorial advice; Jo Platt for designing the search strategy and Gail Quinn, Clare Jess and Tracey Harrison for their contributions to the editorial process.
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure, Cochrane Programme Grant or Cochrane Incentive funding to the Cochrane Gynaecological, Neuro‐oncology, and Orphan Cancers Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service or the Department of Health.
The authors and Cochrane Gynaecological, Neuro‐oncology and Orphan Cancers team are grateful to the following peer reviewers for their time and comments: Andrew Bryant, Jonathan Frost, Sonali Kaushik and Monique Spillman and some who wish to remain anonymous.
Appendices
Appendix 1. Glossary
Pelvic chemoradiation: a combination of medication and radiotherapy given at the same time to destroy cancer cells.
Radical hysterectomy: the surgical removal of the womb, the cervix, the upper part of the vagina and the tissues around the cervix.
Pelvic lymphadenectomy: the surgical removal of the lymph glands found in the pelvis.
Bladder dysfunction (also referred to as voiding dysfunction): a general term to describe abnormalities in either the filling or emptying of the bladder (e.g. urinary retention, voiding difficulty and urgency).
Detrusor muscle: the smooth muscle of the urinary bladder.
Bladder hypotonia: the bladder does not press strongly enough to become completely empty.
Postoperative suprapubic catheterisation: a procedure that creates a connection between the urinary bladder and the skin to drain urine from the bladder.
Acetylcholine: the chemical substance released by the distal part of the nervous system to activate muscles.
Parasympathomimetic agents (also referred to as cholinergic drugs): substances that provoke the autonomic nervous system to promote contraction of the smooth muscle of the urinary bladder.
Prokinetic agent: a drug which enhances gastrointestinal motility by increasing the frequency of contractions in the small intestine.
Poor bladder compliance: a significant increase in bladder pressure with small increments in bladder volume, as measured in a urodynamic study.
Appendix 2. Revised FIGO staging for carcinoma of the cervix uteri (2018)
| Stage I: The carcinoma is strictly confined to the cervix uteri (extension to the corpus should be disregarded) | |
| IA: Invasive carcinoma that can be diagnosed only by microscopy, with maximum depth of invasion < 5 mma | |
| IA1: Measured stromal invasion < 3 mm in depth | |
| IA2: Measured stromal invasion ≥ 3 mm and < 5 mm in depth | |
| IB Invasive carcinoma with measured deepest invasion ≥ 5 mm (greater than stage IA), lesion limited to the cervix uterib | |
| IB1: Invasive carcinoma ≥ 5 mm depth of stromal invasion and < 2 cm in greatest dimension | |
| IB2: Invasive carcinoma ≥ 2 cm and < 4 cm in greatest dimension | |
| IB3: Invasive carcinoma ≥ 4 cm in greatest dimension | |
| Stage II: The carcinoma invades beyond the uterus, but has not extended onto the lower third of the vagina or to the pelvic wall | |
| IIA Involvement limited to the upper two‐thirds of the vagina without parametrial involvement | |
| IIA1: Invasive carcinoma < 4 cm in greatest dimension | |
| IIA2: Invasive carcinoma ≥ 4 cm in greatest dimension | |
| IIB With parametrial involvement but not up to the pelvic wall | |
| Stage III: The carcinoma involves the lower third of the vagina and/or extends to the pelvic wall and/or causes hydronephrosis or non‐functioning kidney and/or involves pelvic and/or paraaortic lymph nodesc | |
| IIIA: Carcinoma involves the lower third of the vagina, with no extension to the pelvic wall | |
| IIIB: Extension to the pelvic wall and/or hydronephrosis or non‐functioning kidney (unless known to be due to another cause) | |
| IIIC: Involvement of pelvic and/or para‐aortic lymph nodes, irrespective of tumour size and extent (with r and p notations)c | |
| IIIC1 Pelvic lymph node metastasis | |
| IIIC2 Para‐aortic lymph node metastasis | |
| Stage IV: The carcinoma has extended beyond the true pelvis or has involved (biopsy proven) the mucosa of the bladder or rectum. A bullous edema, as such, does not permit a case to be allotted to stage IV | |
| IVA: Spread of the growth to adjacent organs | |
| IVB: Spread to distant organs | |
|
Remark FIGO, International Federation of Gynecology and Obstetrics aImaging and pathology can be used, when available, to supplement clinical findings with respect to tumour size and extent, in all stages. | |
| bThe involvement of vascular/lymphatic spaces does not change the staging. The lateral extent of the lesion is no longer considered. | |
| cAdding notation of r (imaging) and p (pathology) to indicate the findings that are used to allocate the case to stage IIIC. For example, if imaging indicates pelvic lymph node metastasis, the stage allocation would be stage IIIC1r and, if confirmed by pathological findings, it would be Stage IIIc1p. The type of imaging modality or pathology technique used should always be documented. When in doubt, the lower staging should be assigned. | |
Appendix 3. FIGO Staging for carcinoma of the cervix uteri (2009)
| Stage I: The carcinoma is strictly confined to the cervix uteri (extension to the corpus should be disregarded) | |
| IA: Invasive carcinoma that can be diagnosed only by microscopy. Invasion is limited to measured stromal invasion with a maximum depth of 5 mm and no wider than 7 mm | |
| IA1: Measured stromal invasion ≤ 3 mm in depth and ≤ 7 mm width | |
| IA2: Measured stromal invasion > 3 mm and ≤ 5 mm in depth and ≤ 7 mm width | |
| IB Clinical lesions limited to the cervix uteri, or preclinical lesions greater than stage IA | |
| IB1: Invasive carcinoma ≤ 4 cm | |
| IB2: Invasive carcinoma > 4 cm | |
| Stage II: The carcinoma invades beyond the uterus, but has not extended onto the lower third of the vagina or to the pelvic wall | |
| IIA Involvement limited to the upper two‐thirds of the vagina without parametrial involvement | |
| IIA1: Invasive carcinoma ≤ 4 cm in greatest dimension | |
| IIA2: Invasive carcinoma > 4 cm in greatest dimension | |
| IIB With parametrial involvement but not up to the pelvic wall | |
| Stage III: The carcinoma involves the lower third of the vagina and/or extends to the pelvic wall and/or causes hydronephrosis or non‐functioning kidney | |
| IIIA: Carcinoma involves the lower third of the vagina, with no extension to the pelvic wall | |
| IIIB: Extension to the pelvic wall and/or hydronephrosis or non‐functioning kidney (unless known to be due to another cause) | |
| Stage IV: The carcinoma has extended beyond the true pelvis or has involved (biopsy proven) the mucosa of the bladder or rectum. A bullous edema, as such, does not permit a case to be allotted to stage IV | |
| IVA: Spread of the growth to bladder and/or rectum | |
| IVB: Spread to distant organs | |
|
Remark FIGO, International Federation of Gynecology and Obstetrics | |
Appendix 4. Classification of radical hysterectomies
| Piver‐Rutledge‐Smith | GCG‐EORTC* | Querleu and Morrow | ||||
| Class I | Extrafascial hysterectomy Deflection and retraction of the ureters without dissection of the ureteral bed Uterine artery, uterosacral ligament and cardinal ligament are not removed No vaginal cuff removed |
Type I | Simple hysterectomy | Type A | Extrafascial hysterectomy Visualisation or palpation, or both, of the ureters without dissection of the ureteral bed Uterine artery, uterosacral ligament and cardinal ligament are not transected at a distance from the uterus Minimal vaginal cuff removed (< 10 mm) |
|
| Class II | Modified radical hysterectomy (Wertheim) Ureters are freed from the paracervical position but are not dissected out of the pubovesical ligament Uterine arteries divided just medial to the ureter Uterosacral ligaments resected midway between the uterus and their sacral attachments Medial half of the cardinal ligaments removed Upper one‐third of the vagina removed Elective pelvic lymphadenectomy |
Type II | Modified radical hysterectomy The uterus, paracervix and upper vagina (10 mm to 20 mm) are removed after dissection of the ureters to the point of their entry to the bladder Uterine arteries are cut off and ligated Medial half of parametria and proximal uterosacral ligaments are transected |
Type B | Ureters are unroofed and rolled laterally Partial removal of uterosacral and vesicouterine ligaments Transection of the paracervix at the level of the ureteral tunnel At least 10 mm of the vagina from the cervix or tumour is resected |
|
| B1 | Without removal of lateral paracervical lymph nodes | |||||
| B2 | With additional removal of lateral paracervical lymph nodes | |||||
| Class III | Classic radical hysterectomy (Meigs) Complete dissection of the ureter from the pubovesical ligament to entry in the bladder except a small lateral part so that the superior vesicle artery is conserved Uterine vessels divided at origin from the internal iliac artery Uterosacral ligaments resected at their sacral attachments Cardinal ligaments resected at the pelvic wall Upper half of the vagina removed Routine pelvic lymphadenectomy |
Type III | Radical hysterectomy En bloc removal of the uterus with the upper third of the vagina along with the paracervical and paravaginal tissues Uterine arteries are cut off and ligated at their origin The entire width of the parametria is resected bilaterally The entire uterosacral ligament is resected |
Type C | Ureters are completely mobilised Transection of the uterosacral ligament at the rectum Transection of the vesicouterine ligament at the bladder Complete transection of the paracervix 15 mm to 20 mm of the vagina from the cervix or tumour and the corresponding paracolpos is resected routinely |
|
| C1 | With preservation of autonomic nerves | |||||
| C2 | Without preservation of autonomic nerves | |||||
| Class IV | More radical than class III in three aspects: (i) Complete dissection of the ureter from the pubovesical ligament (ii) The superior vesicle artery is sacrificed (iii) Upper three‐quarters of the vagina removed |
Type IV | Extended radical hysterectomy Differs from class III in that three‐fourths of the vagina and paravaginal tissues are resected |
Type D | D1 | Resection of the entire paracervix at the pelvic side wall together with the hypogastric vessels, exposing the roots of the sciatic nerve |
| D2 | Type D1 plus resection of the entire paracervix with the hypogastric vessels and adjacent fascial or muscular structures | |||||
| Class V | More radical than class IV Excision of involved portion of distal ureter or bladder and reimplantation of ureter into the bladder |
Type V | Partial exenteration Terminal ureters or segments of bladder or rectum are resected along with the uterus and parametria |
|||
| For all types, lymphadenectomy is described separately according to four levels (external and internal iliac, common iliac, aortic inframesenteric and aortic infrarenal) and radicality (sentinel node sampling, random sampling, removal of enlarged nodes only, systematic lymph node dissection or debulking) | ||||||
* Gynecological Cancer Group of the European Organization for Research and Treatment of Cancer
Appendix 5. CENTRAL search strategy
#1. MeSH descriptor: [Uterine Cervical Neoplasms] this term only
#2. (cervi* near/5 (cancer* or tumor* or tumour* or neoplas* or carcinoma* or adenocarcinoma* or malignan*))
#3. #1 or #2
#4. MeSH descriptor: [Hysterectomy] explode all trees
#5. hysterectom*
#6. ((uter* or womb) near/5 (remov* or excis*))
#7. #4 or# 5 or #6
#8. MeSH descriptor: [Urinary Bladder] this term only
#9. MeSH descriptor: [Urinary Catheterization] this term only
#10. MeSH descriptor: [Urinary Bladder Diseases] explode all trees
#11. MeSH descriptor: [Lower Urinary Tract Symptoms] explode all trees
#12. MeSH descriptor: [Urination Disorders] explode all trees
#13. MeSH descriptor: [Urinary Tract Infections] explode all trees
#14. MeSH descriptor: [Urination] this term only
#15. ((bladder* or urethra* or ureter* or urin* or urologic*) near/5 (dysfunction* or disorder* or disease* or infect* or incontinence* or urgency* or injur* or damage* or hypotonia* or resist* or malfunction*))
#16. (suprapubic near/3 (cystostomy* or catheter*))
#17. MeSH descriptor: [Acupuncture Therapy] this term only
#18. MeSH descriptor: [Cholinergic Agents] explode all trees
#19. ((bladder* or detrusor muscle* or urin*) near/3 (train* or fill* or empty* or pattern* or intervention*))
#20. #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19
#21. #3 and #7 and #20
Appendix 6. MEDLINE Ovid search strategy
1. Uterine Cervical Neoplasms/ 2. (cervi* adj5 (cancer* or tumor* or tumour* or neoplas* or carcinoma* or adenocarcinoma* or malignan*)).mp. 3. 1 or 2 4. exp Hysterectomy/ 5. hysterectom*.mp. 6. ((uter* or womb) adj5 (remov* or excis*)).mp. 7. 4 or 5 or 6 8. Urinary Bladder/ 9. Urinary Catheterization/ 10. exp Urinary Bladder Diseases/ 11. exp Lower Urinary Tract Symptoms/ 12. exp Urination Disorders/ 13. exp Urinary Tract Infections/ 14. Urination/ 15. ((bladder* or urethra* or ureter* or urin* or urologic*) adj5 (dysfunction* or disorder* or disease* or infect* or incontinence* or urgency* or injur* or damage* or hypotonia* or resist* or malfunction*)).mp. 16. (suprapubic adj3 (cystostomy* or catheter*)).mp. 17. Acupuncture Therapy/ 18. exp Cholinergic Agents/ 19. ((bladder* or detrusor muscle* or urin*) adj3 (train* or fill* or empty* or pattern* or intervention*)).mp. 20. 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 21. 3 and 7 and 20
Key:
mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier pt=publication type sh=subject heading ab=abstract
Appendix 7. Embase Ovid search strategy
1. uterine cervix tumor/ 2. (cervi* adj5 (cancer* or tumor* or tumour* or neoplas* or carcinoma* or adenocarcinoma* or malignan*)).mp. 3. 1 or 2 4. exp hysterectomy/ 5. hysterectom*.mp. 6. ((uter* or womb) adj5 (remov* or excis*)).mp. 7. 4 or 5 or 6 8. bladder/ 9. bladder catheterization/ 10. exp bladder disease/ 11. exp lower urinary tract symptom/ 12. exp micturition disorder/ 13. exp urinary tract infection/ 14. micturition/ 15. ((bladder* or urethra* or ureter* or urin* or urologic*) adj5 (dysfunction* or disorder* or disease* or infect* or incontinence* or urgency* or injur* or damage* or hypotonia* or resist* or malfunction*)).mp. 16. (suprapubic adj3 (cystostomy* or catheter*)).mp. 17. acupuncture/ 18. exp cholinergic receptor stimulating agent/ 19. ((bladder* or detrusor muscle* or urin*) adj3 (train* or fill* or empty* or pattern* or intervention*)).mp. 20. 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 21. 3 and 7 and 20
Key:
mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier pt=publication type sh=subject heading ab=abstract
Appendix 8. 'Risk of bias' assessment
Assessment of risk of bias will be based on chapter 8 of Higgins 2011.
-
Random sequence generation
Low risk of bias, e.g. participants assigned to treatments on the basis of a computer‐generated random sequence or a table of random numbers.
High risk of bias, e.g. participants assigned to treatments on the basis of date of birth, clinic ID number or surname, or no attempt to randomise participants.
Unclear risk of bias, e.g. not reported, information not available.
-
Allocation concealment
Low risk of bias, e.g. where the allocation sequence could not be foretold.
High risk of bias, e.g. allocation sequence could be foretold by participants, investigators or treatment providers.
Unclear risk of bias, e.g. not reported.
-
Blinding of participants and personnel
Low risk of bias if participants and personnel were adequately blinded.
High risk of bias if participants were not blinded to the intervention that the participant received.
Unclear risk of bias if this was not reported or unclear.
-
Blinding of outcomes assessors
Low risk of bias if outcome assessors were adequately blinded.
High risk of bias if outcome assessors were not blinded to the intervention that the participant received.
Unclear risk of bias if this was not reported or is unclear.
-
Incomplete outcome data: we will record the proportion of participants whose outcomes were not reported at the end of the study. We will code a satisfactory level of loss to follow‐up for each outcome as:
Low risk of bias, e.g. if fewer than 20% of participants were lost to follow‐up and reasons for loss to follow‐up were similar in both treatment arms.
High risk of bias, e.g. if more than 20% of participants were lost to follow‐up or reasons for loss to follow‐up differed between treatment arms.
Unclear risk of bias, e.g. if loss to follow‐up was not reported.
-
Selective reporting of outcomes
Low risk of bias, e.g. review reports all outcomes specified in the protocol.
High risk of bias, e.g. it is suspected that outcomes have been selectively reported in the study.
Unclear risk of bias, e.g. it is unclear whether outcomes have been selectively reported.
-
Other bias
Low risk of bias, e.g. the review authors do not suspect any other source of bias and the trial appears to be methodologically sound.
High risk of bias, e.g. the review authors suspect that the trial was prone to an additional bias.
Unclear risk of bias, e.g. the review authors are uncertain whether an additional bias may have been present.
Data and analyses
Comparison 1. Bethanechol versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Post‐void residual urine volume one month after surgery | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.2 Flow rate (mL per second) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.3 Maximum flow rate (mL per second) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.4 Number of women with low maximum flow rate (< 15 mL per second) | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.5 Detrusor pressure at maximum flow (cmH2O) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.6 Number of women with low detrusor pressure at maximum flow | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.7 Bladder compliance | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only |
Comparison 2. Suprapubic catheterisation versus intermittent self‐catheterisation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Time to post‐void residual volume of urine < 75 mL after surgery (days) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.2 Time to post‐void residual volume of urine < 100 mL after surgery (days) | 2 | 64 | Mean Difference (IV, Random, 95% CI) | ‐11.02 [‐17.78, ‐4.26] |
| 2.3 Adverse events; acute complications | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.4 Urinary tract infections during the one‐month period following surgery | 2 | 95 | Risk Ratio (IV, Random, 95% CI) | 0.77 [0.53, 1.13] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Madeiro 2006.
| Study characteristics | ||
| Methods | Study design: a randomised, double‐blind, placebo‐controlled study Study setting: the Sao Marcos Hospital–Piauı Cancer Society in Brazil Study duration: March 2002 to February 2003 |
|
| Participants | Seventy‐nine patients with stage IB (FIGO) cervical cancer underwent a class III hysterectomy. Exclusion criteria were previous pelvic radiation therapy, recurrent urinary tract infections, urinary calculi, uncontrolled diabetes mellitus, bronchial asthma and risk factors for cisapride use, such as heart disease and family history of sudden death. An indwelling urethral catheter remained postoperatively in all patients for 10 days. All participants were randomised to the following groups: A‐placebo (19); B‐bethanechol, in a 10 mg oral dose every 8 hours (20); C‐cisapride, in a 10 mg dose every 8 hours (20); D‐bethanechol combined with cisapride (20). | |
| Interventions | Control group: placebo Intervention groups: ‐ Bethanechol 10 mg oral dose every 8 hours ‐ Cisapride 10 mg dose every 8 hours ‐ Bethanechol 10 mg oral dose every 8 hours and cisapride 10 mg dose every 8 hours All medication was administered during 30 consecutive days, starting from the first postoperative day. |
|
| Outcomes | ‐ Urodynamic study prior to surgery ‐ Urodynamic study at 30 day post operation By the same investigator |
|
| Notes | Urodynamic study was conducted with a 4‐channel Urodynamic System including uroflowmetry to determine post‐void residual volume, cystometry, urethral pressure profile and pressure‐flow study. Micturition dysfunction was defined as low maximum flow rate (600 mL), presence of detrusor instability, low bladder compliance and stress urinary incontinence (when urine leakage was observed after coughing or Valsalva maneuver during cystometery). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computerised randomisation schedule |
| Allocation concealment (selection bias) | Unclear risk | No statement regarding the method used to conceal the allocation sequence |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | All medication was provided in capsules, which were identical in appearance. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Randomisation was only revealed at the end of the study, controlled by an independent investigator. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants lost to follow‐up |
| Selective reporting (reporting bias) | High risk | No data on rate of spontaneous voiding recovery one week after surgery, quality of life, adverse events, time after surgery to post‐void residual volume of urine ≤ 50 mL, urinary tract infections in the first month after surgery, post‐void residual urine volume at 6 and 12 months after surgery, and subjective urinary symptoms were reported. |
| Other bias | Low risk | No information indicating an important risk of other bias |
Naik 2005.
| Study characteristics | ||
| Methods | Study design: a prospective randomised controlled trial Study setting: Queen Elizabeth Hospital in United Kingdom Study duration: July 1999 to June 2002 |
|
| Participants | 40 women treated by radical hysterectomy for early stage cervical cancer were randomised to intermittent self‐catheterisation (N = 21) and suprapubic catheterisation (N = 19). | |
| Interventions | Control group: intermittent self‐catheterisation (ISC) Intervention group: suprapubic catheterisation (SPC) |
|
| Outcomes | ‐ Mid‐stream specimen of urine for culture and sensitivity at 3 weeks, 6 weeks and 12 weeks following surgery ‐ Residual urine volume (RUV) at 3 weeks, 6 weeks and 12 weeks following surgery ‐ Ability to manage ISC following training at 3 weeks, 6 weeks and 12 weeks following surgery ‐ Urinary symptoms questionnaire (USQ) at 3 weeks, 6 weeks and 12 weeks following surgery ‐ Quality of life (EORTC QLQ C30) questionnaire at 3 weeks, 6 weeks and 12 weeks following surgery |
|
| Notes | ‐ The ISC protocol consisted of insertion of a transurethral indwelling catheter at the time of surgery which remained on free drainage until day 5, at which time it was withdrawn and the patient commenced ISC. ISC was continued until satisfactory frequency/volumes and RUVs were achieved (minimum 200 mL of urine, at least four hourly during the day, with residual urine volumes of < 100 mL). ‐ The SPC protocol consisted of insertion of a Bonanno suprapubic catheter at the time of surgery followed by free drainage until day 5 at which time it was clamped. Patients were then requested to pass urine at least every 4 hours during the day following which the RUV was measured by releasing the clamp. SPC was continued until satisfactory frequency/volumes and RUVs as described above were achieved. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No statement regarding the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed via sealed envelopes and an independent administrator. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Patients randomised to ISC were instructed and assessed in the use of ISC prior to surgery. However, the outcomes of interest were unlikely to be affected by lack of blinding of participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No statement regarding the blinding of outcome assessment. However, the outcomes of interest were unlikely to be affected by lack of blinding of outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 40 participants randomised, 4 were excluded (1 developed a ureteric fistula; 1 developed postoperative confusion; 1 suffered a perioperative cerebrovascular accident; and 1 participant died). This corresponds to a rate of incomplete outcome data of approximately 10%. Thus, this is unlikely to influence the effect of treatment assigned. |
| Selective reporting (reporting bias) | High risk | No data on rate of spontaneous voiding recovery one week after surgery, and adverse events were reported. |
| Other bias | Low risk | No information indicating an important risk of other bias |
Nwabineli 1993.
| Study characteristics | ||
| Methods | Study design: a randomised pilot study Study setting: St James's Hospital in the Republic of Ireland Study duration: September 1989 to February 1990 |
|
| Participants | 24 patients with stage IB or IIA carcinoma who underwent radical hysterectomy and pelvic node dissection for cervical carcinoma were randomised in this study to compare continuous postoperative drainage by urethral (N=14) and suprapubic catheters (N=10). Exclusion criteria included more than 50 year of age, preoperative voiding problems, treated by radiotherapy, and taking drugs likely to affect bladder function (e.g. tricyclic antidepressants and anticholinergics). | |
| Interventions | During the operation, all patients had an indwelling free draining Foley's catheter. At the end of the operation, a Becton‐Dickenson Bonanno catheter was inserted if randomisation had indicated a suprapubic catheter and the urethral catheter was removed. In those patients randomised to receive urethral catheters, this was left in situ. Control group: urinary drainage by urethral route Intervention group: urinary drainage by suprapubic route |
|
| Outcomes | ‐ Duration of continuous catheter drainage before the return of spontaneous voiding ‐ The incidence of urinary tract infection |
|
| Notes | Trial of voiding started on the fifth postoperative day. Catheters were removed when the residual urine was ≤ 100 mL. Antibiotics were not administered routinely in the postoperative period. Daily catheter specimens of urine were examined bacteriologically daily until the catheters were removed except in patients who went home with their catheters in situ. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using random numbers which were obtained from random sampling numbers |
| Allocation concealment (selection bias) | Unclear risk | No statement regarding the method used to conceal the allocation |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were not blinded to the intervention that they received. However, the outcomes of interest were unlikely to be affected by lack of blinding of participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No statement regarding the blinding of outcome assessment. However, the outcomes of interest were unlikely to be affected by lack of blinding of outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants lost to follow‐up |
| Selective reporting (reporting bias) | High risk | No data on rate of spontaneous voiding recovery one week after surgery, QoL, adverse events, post‐void residual urine volume at 1, 6 and 12 months after surgery, and subjective urinary symptoms were reported. |
| Other bias | Low risk | No information indicating an important risk of other bias |
Suprasert 2002.
| Study characteristics | ||
| Methods | Study design: a prospective randomised study Study setting: Chiang Mai University Hospital in Thailand Study duration: September 1998 to June 1999 |
|
| Participants | 81 stage IB1‐IIA cervical cancer patients who underwent radical hysterectomy with pelvic lymphadenectomy (RHPL). At the end of the RHPL operation, the participants were allocated immediately into the intermittent self‐catheterisation (N=38) or the suprapubic catheterisation (N=33) group before abdominal closure. Exclusion criteria included abnormal preoperative bladder function or urinary analysis, urinary tract infection more than 2 times per year, history of renal stone, bladder calculi, urinary incontinence, intraoperative bowel or urinary tract complication, and inability to perform Intermittent self‐catheterisation (ISC). |
|
| Interventions | ‐ Control group: suprapubic catheterisation Suprapubic catheter was placed through a small bladder incision and exited through a separated skin incision. The catheter in this group was clamped on day 7 postoperatively for 4 hours and was released after self‐voiding to check the post voiding residual (PVR) urine. ‐ Intervention group: intermittent self‐catheterisation (ISC) The ISC group was managed by indwelling transurethral Foley’s catheter for 7 days. On day 6, the patient was instructed to do ISC until she could confidently perform by herself. When the Foley’s catheter was removed on day 8, the ISC was performed every 4 hours after each voiding and the PVR urine was recorded. ‐ In both groups, ISC and SPC were discontinued when the PVR was < 75 ml for 2 consecutive voids. |
|
| Outcomes | ‐ Febrile morbidity ‐ The voiding time (days) ‐ Rate of urinary tract infection |
|
| Notes | ‐ Urine analysis was performed weekly until the ISC or SPC was discontinued. ‐ Bacteriuria was defined as urinary culture showed the organism more than 105 colonies/mL. ‐ Prolonged bladder dysfunction was defined as the voiding time was longer than 30 days. ‐ Febrile morbidity was defined as two consecutive oral temperatures ≥ 38˚ C, at least 6 hours apart excluding the first 24 hours after operation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Assigned by computerised randomisation |
| Allocation concealment (selection bias) | Low risk | Sealed in the envelope |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were not blinded to the intervention that they received. However, the outcomes of interest were unlikely to be affected by lack of blinding of participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No statement regarding the blinding of outcome assessment. However, the outcomes of interest were unlikely to be affected by lack of blinding of outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants lost to follow‐up |
| Selective reporting (reporting bias) | High risk | No data on rate of spontaneous voiding recovery 1 week after surgery, QoL, post‐void residual urine volume at 1, 6 and 12 months after surgery, or subjective urinary symptoms were reported. |
| Other bias | Low risk | No information indicating an important risk of other bias |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Chen 2012 | Wrong intervention Details: this study evaluated histopathology and clinical outcome of autonomic nerve trauma and vessels removal within the cardinal ligament (CL) during nerve‐sparing radical hysterectomy (NSRH) compared with radical hysterectomy (RH). |
| Chen 2014 | Wrong intervention Details: this randomised study was conducted to evaluate the impact of two types of hysterectomy (laparoscopic nerve‐sparing radical hysterectomy versus classical laparoscopic radical hysterectomy) on the bladder and intestinal functions among 65 patients with IA2 to IIA cervical cancer |
| Dy Echo 2011 | Study population does not meet inclusion criteria Details: this non blinded, no placebo, randomised controlled trial was conducted to determine the efficacy and safety of solifenacin succinate in decreasing duration of indwelling catheterisation among 16 patients who underwent radical hysterectomy for gynaecologic malignancies (early stage cervical cancer and clinical stage II endometrial cancer). |
| Dy Echo 2012 | Study population does not meet inclusion criteria Details: this prospective randomised study was conducted to evaluate the efficacy and safety of solifenacin succinate in the decreasing mean duration of indwelling catheterisation after radical hysterectomy among 36 patients with IA2 to IIA cervical cancer or endometrial cancer stage II. 26 patients (72.22%) were diagnosed with cervical cancer; 15 patients in the control arm, and 11 patients in the treatment arm. There were 10 (27.78%) endometrial cancer patients; 3 in the control arm, and 7 in the treatment arm. |
| Fanfani 2015 | Study population does not meet inclusion criteria (some were in locally advanced‐stage of cervical cancer) This trial was a two‐armed parallel RCT conducted between April 2009 and November 2011. Participants were 111 women with cervical cancer stage IB‐IIB (93 participants; 83.8%), FIGO stage II endometrial cancer (17 participants; 15.0%), and uterine sarcoma (1 participant; 0.9%) who underwent Querleu‐Morrow type B2 or type C1 radical hysterectomy. |
| Gong 2016 | Study population does not meet inclusion criteria (some were in locally advanced‐stage of cervical cancer) This trial was a two‐armed parallel RCT conducted between February 2012 and April 2015. Participants were 198 women with stage IB‐IIB cervical cancer who underwent type C radical hysterectomy. 111 participants (56.1%) with stage IB2 or IIB received neoadjuvant platinum‐based chemotherapy or chemoradiation. Women were considered ineligible if they had urinary incontinence, interstitial cystitis, cognitive impairment, or difficulty in completing the training program. |
| Kuo 2005 | Study population does not meet inclusion criteria Details: this prospective non‐randomised study was conducted to evaluate the effectiveness of urethral injection of Botulinum A toxin in the treatment of voiding dysfunction after radical hysterectomy. All participants had symptoms of severe difficult urination, abdominal straining to void, and a moderate to large post‐void residual. |
| Li 2019 | Wrong outcome Details: this RCT was conducted to evaluate the clinical significance of low‐frequency electrical stimulation in preventing urinary retention after radical hysterectomy. Outcomes were urinary retention (defined as when the patient cannot urinate smoothly, bladder residual urine volume was ≥ 100 mL as determined by B ultrasound, or cannot self‐discharge and need to reset the catheter) and pelvic floor muscle strength which are not the outcomes that this review aims to assess. |
| Manchana 2011 | Study population does not meet inclusion criteria Details: this prospective randomised study was conducted to evaluate the efficacy of bethanechol chloride compared with placebo for the prevention of bladder dysfunction after type III radical hysterectomy among 66 patients with early‐stage cervical cancer (N=37, 56%) or endometrial cancer stage II (N=29, 44%). |
| Pengsaa 1992 | Non‐randomised study Details: this prospective non‐randomised study was conducted to evaluate rate of lower urinary tract complications in both suprapubic and transurethral catheterisation groups after class III (Piver) radical hysterectomy among 66 patients with stage IB‐IIA cervical cancer or endometrial cancer stage II. |
| Wang 2015 | Study population does not meet inclusion criteria Details: this randomised controlled prospective double‐blinded trial was carried out in 107 patients who encountered urinary retention following a type III radical hysterectomy. |
| Wells 2008 | Non‐randomised study Details: this retrospective cohort study using the records of women with stage IA1 with lymphovascular invasion (LVSI) , 1A2, and IB1 cervical cancer who underwent radical hysterectomy with pelvic lymphadenectomy. Patients were assigned to one of two groups (transurethrally or suprapubically on the basis of the method of catheterisation used at the time of surgery. |
Characteristics of studies awaiting classification [ordered by study ID]
Cheng 2017.
| Methods | Title: The effect of TENS on postoperative urinary function in early cervical cancer Study design: a multicentre, randomised controlled clinical trial Study setting: China Source: abstract presentation in 42nd Annual Meeting – Vancouver, Canada during June 20 – 24, 2017 Published in: International Urogynecology Journal; Volume 28 (supplement 1). Springer London. |
| Participants | 68 patients with early stage cervical squamous cell carcinoma who underwent Piver III hysterectomy were recruited and randomised to study group (N=30) and control group (N=29). |
| Interventions | Control group: remove Foley on the 14th postoperative day Intervention: Transcutaneous electrical nerve stimulation (TENS) started on the 7th day after operation, lasting two to three courses, with 7 days for each course. Patients whose residual urine volume less than 100 ml on 14th received two courses of TENS with urinary catheter removed on 14th day post operation, while the rest of them completed three courses whose urinary catheter were keeping till residual urine volume less than 100ml. |
| Outcomes | ‐ Proportion of residual urine more than 100 mL on day 14 post operation ‐ Proportion of participants keeping urinary catheter more than 21 days ‐ Uroflowmetry ‐ Urogenital Distress Inventory‐6 (UDI‐6) score |
| Notes | The maximum current of TENS was adjusted according to patients' pain intensity, no more than 100 mA. |
Characteristics of ongoing studies [ordered by study ID]
Boonthongtho 2016.
| Study name | Effectiveness of Bethanechol Chloride and Early Bladder Training for Prevention of Bladder Dysfunction After Radical Hysterectomy in Cervical Cancer Stage IB ‐ IIA |
| Methods | Randomised |
| Participants | Women with cervical cancer stage IB ‐ IIA underwent standard type III radical hysterectomy, both open and laparoscopic approach |
| Interventions | Early bladder training and/or bethanechol chloride |
| Outcomes | Duration of retained urethral catheterisation (day) after standard type III radical hysterectomy |
| Starting date | October 2016 |
| Contact information | narisa.x@gmail.com; myanaran@hotmail.com |
| Notes | ClinicalTrials.gov Identifier: NCT02910596 Recruitment status was: not yet recruiting Last update posted: 3 October 2016 |
Sun 2017.
| Study name | Effect of transcutaneous electrical stimulation treatment on lower urinary tract symptoms after class III radical hysterectomy in cervical cancer patients: study protocol for a multicentre, randomised controlled trial |
| Methods | Multicentre, randomised controlled trial |
| Participants | Cervical cancer FIGO stage IA2 ‐ IIA1 patients who underwent class III radical hysterectomy |
| Interventions | Transcutaneous electrical stimulation treatment plus conventional clinical care |
| Outcomes | Self‐urination status and residual urine at postoperative 14 days, 21 days, 28 days, 3 months, 6 months and 12 months |
| Starting date | April 2015 |
| Contact information | wjianliu1203@163.com |
| Notes | The study is registered to Clinical Trials.gov (NCT02492542) on 25 June 2015. Recruitment status was: recruiting Last update posted: 14 March 2018 Estimated study completion date: December 2019 |
Differences between protocol and review
Types of outcome measures
In the protocol, we stated that our primary outcomes of interest were rate of spontaneous voiding recovery one week after surgery and QoL. However, none of the included studies reported the rate of spontaneous voiding recovery one week after surgery. In addition, only one included study reported QoL at 3 weeks, 6 weeks, and 12 weeks after surgery but the data were insufficient to calculate the relative measures of the effect of interventions.
In the protocol, we stated that we planned to assess the effect of interventions on the time after surgery to post‐void residual urine volume of 50 mL or less, and poor bladder compliance. However, none of the included studies reported these outcomes. We therefore added (1) time after surgery to post‐void residual urine volume of 100 mL or less; (2) time after surgery to post‐void residual urine volume of 75 mL or less; and (3) bladder compliance, as additional secondary outcomes.
In the review, we additionally stated the definition of spontaneous voiding recovery at one week after surgery.
Measures of treatment effect
In the review protocol, we planned to measure the time after surgery to post‐void residual urine volume of 50 mL or less as a time‐to‐event outcome. However, the available data did not permit us to estimate HRs for this outcome. We therefore determined the effects of intervention on the time to post‐void residual urine volume by applying mean difference with 95% CI.
Assessment of reporting biases
As most analyses were based on limited numbers of included studies, we were unable to construct funnel plots to determine the possibility of publication bias as planned in the review protocol. In future updates of this review, we will examine funnel plots corresponding to meta‐analysis of the primary outcome to assess the potential for small study effects such as publication bias, if we identify more than 10 studies. We plan to assess funnel plot asymmetry visually (Sterne 2011).
Subgroup analysis and investigation of heterogeneity
In the protocol, we planned to performed subgroup analysis in order to assess the effect of the following factors.
Tumour size (2 cm or less versus more than 2 cm).
Surgical approach (laparotomy versus minimally invasive surgery).
Nerve‐sparing approach during radical hysterectomy (yes versus no).
Radicality of surgery (Piver type II versus Piver type III, or Querleu‐Morrow class B2 versus class C1).
Extent of pelvic lymph node dissection determined by number of lymph nodes removed.
However, we did not perform subgroup analysis in this review, as most analyses were based on limited numbers of included studies. Nevertheless, we acknowledged these factors in the interpretation of review findings.
Sensitivity analysis
We planned in our protocol to perform sensitivity analysis in order to assess the effect of the following factors.
Repeating the analysis excluding unpublished studies (if any).
Repeating the analysis excluding studies judged to be at 'high' or 'unclear' risk of bias for allocation concealment
Howver, we were unable to conduct this sensitivity analysis because of the limited numbers of included studies.
Contributions of authors
Apiwat Aue‐aungkul: conceived review question, developed, and completed the review Chumnan Kietpeerakool: conceived review question, developed, co‐ordinated, and completed the review Siwanon Rattanakanokchai: developed and completed the review Khadra Galaal: conceived review question, edited the review and played an advisory role Teerayut Temtanakitpaisan: edited review Chetta Ngamjarus: edited review and acted in an advisory role Pisake Lumbiganon: edited review and acted in an advisory role
Sources of support
Internal sources
-
Department of Obstetrics and Gynaecology, Faculty of Medicine, Khon Kaen University, Thailand
Technical support
-
Department of Gynaecological Oncology, Princess Alexandra Wing, Royal Cornwall Hospital, UK
Technical support
-
Department of Epidemiology and Biostatistics, Faculty of Public Health, Khon Kaen University, Thailand
Technical support
-
Cochrane Thailand, Thailand
Technical support
External sources
No sources of support supplied
Declarations of interest
Apiwat Aue‐aungkul: none known Chumnan Kietpeerakool: none known Siwanon Rattanakanokchai: none known Khadra Galaal: none known Teerayut Temtanakitpaisan: none known Chetta Ngamjarus: none known Pisake Lumbiganon: none known
New
References
References to studies included in this review
Madeiro 2006 {published data only}
- Madeiro AP, Rufino AC, Sartori MG, Baracat EC, DeLima GR, Girao MJ. The effects of bethanechol and cisapride on urodynamic parameters in patients undergoing radical hysterectomy for cervical cancer. A randomized, double-blind, placebo-controlled study. International Urogynecology Journal and Pelvic Floor Dysfunction 2006;17(3):248-52. [DOI] [PubMed] [Google Scholar]
Naik 2005 {published data only}
- Naik R, Maughan K, Nordin A, Lopes A, Godfrey KA, Hatem MH. A prospective randomised controlled trial of intermittent self-catheterisation vs. supra-pubic catheterisation for post-operative bladder care following radical hysterectomy. Gynecologic Oncology 2005;99:437-42. [DOI] [PubMed] [Google Scholar]
- Roberts K, Naik R. Catheterization options following radical surgery for cervical cancer. British Journal of Nursing 2006;15(19):1038-44. [DOI] [PubMed] [Google Scholar]
Nwabineli 1993 {published data only}
- Nwabineli NJ, Walsh DJ, Davis JA. Urinary drainage following radical hysterectomy for cervical carcinoma - a pilot comparison of urethral and suprapubic routes. International Journal of Gynecological Cancer 1993;3(4):208-10. [DOI] [PubMed] [Google Scholar]
Suprasert 2002 {published data only}
- Suprasert P, Srisomboon J, Phongnarisorn C. A prospective randomized study comparing voiding time between suprapubic catheterization and intermittent self-catheterization following radical hysterectomy and pelvic lymphadenectomy for cervical cancer. Thai Journal of Obstetrics and Gynaecology 2002;14(1):73-9. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Chen 2012 {published data only}
- Chen C, Li W, Li F, Liu P, Zhou J, Lu L, et al. Classical and nerve-sparing radical hysterectomy: an evaluation of the nerve trauma in cardinal ligament. Gynecologic Oncology 2012;125:245-51. [DOI] [PubMed] [Google Scholar]
Chen 2014 {published data only}
- Chen L, Zhang WN, Zhang SM, Yang ZH, Zhang P. Effect of laparoscopic nerve-sparing radical hysterectomy on bladder function, intestinal function recovery and quality of sexual life in patients with cervical carcinoma. Asian Pacific Journal Cancer Prevention 2014;15(24):10971-5. [DOI] [PubMed] [Google Scholar]
Dy Echo 2011 {published data only}
- Dy Echo AV and Luna JT. The role of solifenacin succinate in the management of bladder dysfunction in post-radical hysterectomy patients: an interim report. International Journal of Gynecological Cancer 2011;21(12):321. [Google Scholar]
Dy Echo 2012 {published data only}
- Dy Echo AV, Luna JT, Quirapas GQ. The role of solifenacin succinate in the management of bladder dysfunction in radical hysterectomy patients. Philippine Journal of Obstetrics & Gynecology 2012;30(1):1-10. [Google Scholar]
Fanfani 2015 {published data only}
- Fanfani F, Costantini B, Mascilini F, Vizzielli G, Gallotta V, Vigliotta M, et al. Early postoperative bladder training in patients submitted to radical hysterectomy: is it still necessary? A randomized trial. Archives of Gynecology and Obstetrics 2015;291:883-8. [DOI] [PubMed] [Google Scholar]
- Santaguida S, Tortorella L, Vigliotta M, Margariti PA, Moruzzi MC, Scambia G, et al. Bladder training after nerve-sparing radical hysterectomy in cervical cancer patients: Is it necessary? In: International Journal of Gynecology & Obstetrics. Vol. 119. 2012:472.
Gong 2016 {published data only}
- Gong Y, Zhao L, Wang L, Wang F. The effect of clamping the indwelling urinary catheter before removal in cervical cancer patients after radical hysterectomy. Journal of Clinical Nursing 2016;26(7-8):1131-6. [DOI] [PubMed] [Google Scholar]
Kuo 2005 {published data only}
- Kuo HC. Effectiveness of urethral injection of botulinum a toxin in the treatment of voiding dysfunction after radical hysterectomy. Urologia Internationalis 2005;75(3):247-51. [DOI] [PubMed] [Google Scholar]
Li 2019 {published data only}
- Li H, Zhou CK, Song J, Zhang WY, Wang SM, Gu YL, et al. Curative efficacy of low frequency electrical stimulation in preventing urinary retention after cervical cancer operation. World Journal of Surgical Oncology 2019;17(1):141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Manchana 2011 {published data only}
- Manchana T, Prasartsakulchai C. Bethanechol chloride for the prevention of bladder dysfunction after radical hysterectomy in gynecologic cancer patients: a randomized controlled trial study. International Journal of Gynecological Cancer 2011;21(4):730-6. [DOI] [PubMed] [Google Scholar]
Pengsaa 1992 {published data only}
- Pengsaa P, Pothinam S, Udomthavornsok B. Urinary drainage following radical hysterectomy. Thai Journal of Obstetrics and Gynaecology 1992;4(2):125-8. [Google Scholar]
Wang 2015 {published data only}
- Wang HF, Wang DB, Chen YH, Zhou MY. Relief of urinary retention after radical hysterectomy for cervical cancer patients by acupressure: a randomized controlled trial. Chinese Journal of Integrated Traditional and Western Medicine 2015;35(4):425-8. [PubMed] [Google Scholar]
Wells 2008 {published data only}
- Wells TH, Steed H, Capstick V, Schepanksy A, Hiltz M, Faught W. Suprapubic or urethral catheter: what is the optimal method of bladder drainage after radical hysterectomy? Journal of Obstetrics & Gynaecology Canada: JOGC 2008;30(11):1034-8. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Cheng 2017 {published data only}
- Cheng W, Wang S, Sun X, Wang, J. The effect of TENS on postoperative urinary function in early cervical cancer (42nd Annual Meeting – Vancouver, Canada, June 20 – 24, 2017). In: International Urogynecology Journal. Vol. 28. Springer London, 2017:Supplement 1.
References to ongoing studies
Boonthongtho 2016 {published data only}
- Effectiveness of Bethanechol Chloride and Early Bladder Training for Prevention of Bladder Dysfunction After Radical Hysterectomy in Cervical Cancer Stage IB - IIA. Ongoing study. October 2016. Contact author for more information.
Sun 2017 {published data only}
- Effect of transcutaneous electrical stimulation treatment on lower urinary tract symptoms after class III radical hysterectomy in cervical cancer patients: study protocol for a multicentre, randomised controlled trial. Ongoing study. April 2015. Contact author for more information. [DOI] [PMC free article] [PubMed]
Additional references
Abrams 2003
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003;61(1):37-49. [DOI] [PubMed] [Google Scholar]
Aue‐aungkul 2017
- Aue-aungkul A, Kietpeerakool C, Galaal K, Temtanakitpaisan T, Ngamjarus C, Lumbiganon P. Postoperative interventions for preventing bladder dysfunction after radical hysterectomy in women with early-stage cervical cancer. Cochrane Database of Systematic Reviews 2017, Issue 11. Art. No: CD012863. [DOI: 10.1002/14651858.CD012863] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barry 1992
- Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. Journal of Urology 1992;148(5):1549–57. [DOI] [PubMed] [Google Scholar]
Bhatla 2019
- Bhatla N, Berek JS, Cuello Fredes M, Denny LA, Grenman S, Karunaratne K, et al. Revised FIGO staging for carcinoma of the cervix uteri. International Journal of Gynecology & Obstetrics 2019;145(1):129-35. [DOI] [PubMed] [Google Scholar]
Bray 2018
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians 2018;68(6):394-424. [DOI] [PubMed] [Google Scholar]
Chen 2002
- Chen GD, Lin LY, Wang PH, Lee HS. Urinary tract dysfunction after radical hysterectomy for cervical cancer. Gynecologic Oncology 2002;85(2):292-7. [DOI] [PubMed] [Google Scholar]
Chen 2020
- Chen X, Zhao N, Ye P, Chen J, Nan X, Zhao H, et al. Comparison of laparoscopic and open radical hysterectomy in cervical cancer patients with tumor size ≤ 2 cm. International Journal of Gynecologic Cancer 2020;30(5). [DOI] [PubMed] [Google Scholar]
Cho 2009
- Cho SY, Yi JS, Oh SJ. The clinical significance of poor bladder compliance. Neurourology and Urodynamics: Official Journal of the International Continence Society 2009;28(8):1010-4. [DOI] [PubMed] [Google Scholar]
CTCAE 2010
- US Department of Health and Human Services (National Institutes of Health, National Cancer Institute). Common Terminology Criteria for Adverse Events (CTCAE) Version 4.03. evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf (accessed 16 October 2017).
Cull 1993
- Cull A, Cowie VJ, Farquharson DI, Livingstone JR, Smart GE, Elton RA. Early stage cervical cancer: psychosocial and sexual outcomes of treatment. British Journal of Cancer 1993;68(6):1216-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cusimano 2019
- Cusimano MC, Baxter NN, Gien LT, Moineddin R, Liu N, Dossa F, et al. Impact of surgical approach on oncologic outcomes in women undergoing radical hysterectomy for cervical cancer. American Journal of Obstetrics and Gynecology 2019;221(6):619.e1-619.e24. [DOI] [PubMed] [Google Scholar]
Deeks 2001
- Deeks J, Altman D, Bradburn M. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. 2nd edition. London (UK): BMJ Publication Group, 2001. [Google Scholar]
DeSimonian 1986
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177-88. [DOI] [PubMed] [Google Scholar]
Endnote [Computer program]
- Endnote. Version X7. New York (NY): Thomas Reuters, 2015.
Ferlay 2015
- Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. International Journal of Cancer 2015;136(5):E359-86. [DOI] [PubMed] [Google Scholar]
Fernandez 2005
- Fernandez RS, Griffiths RD. Clamping short-term indwelling catheters: a systematic review of the evidence. Journal of Wound, Ostomy and Continence Nursing 2005;32(5):329-36. [DOI] [PubMed] [Google Scholar]
Geller 2014
- Geller EJ. Prevention and management of postoperative urinary retention after urogynecologic surgery. International Journal of Women's Health 2014;6:829-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldfarb 1967
- Goldfarb M, Medina-Cue R. Urologic complications of abdominoperineal surgery. Diseases of the Colon and Rectum 1967;10(5):379-83. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version accessed 3 November 2017. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Greimel 2006
- Greimel ER, Kuljanic Vlasic K, Waldenstrom AC, Duric VM, Jensen PT, Singer S. The European Organization for Research and Treatment of Cancer (EORTC) Quality-of-Life questionnaire cervical cancer module: EORTC QLQ-CX24. Cancer 2006;107(8):1812-22. [DOI] [PubMed] [Google Scholar]
Henney 2000
- Henney JE. Withdrawal of Troglitazone and Cisapride. JAMA 2000;283(17):2228. [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS (editors). Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0. (updated June 2017). The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook.
Higgins 2019
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019) Cochrane, 2019. Available from www.training.cochrane.org/handbook. [DOI] [PMC free article] [PubMed]
Kemp 1997
- Kemp B, Kitschke HJ, Goetz M, Heyl W. Prophylaxis and treatment of bladder dysfunction after Wertheim-Meigs operation: the positive effect of early postoperative detrusor stimulation using the cholinergic drug betanecholchloride. International Urogynecology Journal 1997;8(3):138-41. [DOI] [PubMed] [Google Scholar]
Kidd 2015
- Kidd EA, Stewart F, Kassis NC, Hom E, Omar MI. Urethral (indwelling or intermittent) or suprapubic routes for short-term catheterisation in hospitalised adults. Cochrane Database of Systematic Reviews 2015, Issue 12. Art. No: CD004203. [DOI: 10.1002/14651858.CD004203.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kietpeerakool 2019
- Kietpeerakool C, Aue-Aungkul A, Galaal K, Ngamjarus C, Lumbiganon P. Nerve-sparing radical hysterectomy compared to standard radical hysterectomy for women with early stage cervical cancer (stage Ia2 to IIa). Cochrane Database of Systematic Reviews 2019, Issue 2. Art. No: CD012828. [DOI: 10.1002/14651858.CD012828] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2000
- Kim SM, Choi HS, Byun JS. Overall 5-year survival rate and prognostic factors in patients with stage IB and IIA cervical cancer treated by radical hysterectomy and pelvic lymph node dissection. International Journal of Gynecologic Cancer 2000;10(4):305-12. [DOI] [PubMed] [Google Scholar]
Kim 2017
- Kim DK. Current pharmacological and surgical treatment of underactive bladder. Investigative and Clinical Urology 2017;58(Suppl 2):S90–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Landoni 1997
- Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet 1997;350(9077):535-40. [DOI] [PubMed] [Google Scholar]
Landoni 2001
- Landoni F, Maneo A, Cormio G, Perego P, Milani R, Caruso O, et al. Class II versus class III radical hysterectomy in stage IB-IIA cervical cancer: a prospective randomized study. Gynecologic Oncology 2001;80(1):3-12. [DOI] [PubMed] [Google Scholar]
Langendam 2013
- Langendam MW, Akl EA, Dahm P, Glasziou P, Guyatt G, Schünemann HJ. Assessing and presenting summaries of evidence in Cochrane Reviews. Systematic Reviews 2013;2:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Laterza 2015
- Laterza RM, Sievert KD, Ridder D, Vierhout ME, Haab F, Cardozo L, et al. Bladder function after radical hysterectomy for cervical cancer. Neurourology and Urodynamics 2015;34(4):309-15. [DOI] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gotzsche P, Ioannidis J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. BMJ 2009;339:2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lin 1998
- Lin HH, Sheu BC, Lo MC, Huang SC. Abnormal urodynamic findings after radical hysterectomy or pelvic irradiation for cervical cancer. International Journal of Gynecology and Obstetrics 1998;63(2):169-74. [DOI] [PubMed] [Google Scholar]
Mahawerawat 2013
- Mahawerawat S, Charoenkwan K, Srisomboon J, Khunamornpong S, Suprasert P, Sae-Teng CT. Surgical outcomes of patients with stage IA2 cervical cancer treated with radical hysterectomy. Asian Pacific Journal of Cancer Prevention 2013;14(9):5375-8. [DOI] [PubMed] [Google Scholar]
Manchana 2010
- Manchana T, Prasartsakulchai C, Santingamkun A. Long-term lower urinary tract dysfunction after radical hysterectomy in patients with early postoperative voiding dysfunction. International Urogynecology Journal and Pelvic Floor Dysfunction 2010;21(1):95-101. [DOI] [PubMed] [Google Scholar]
Oberst 1981
- Oberst MT, Graham D, Geller NL, Stearns MW Jr, Tiernan E. Catheter management programs and postoperative urinary dysfunction. Research in Nursing & Health 1981;4(1):175-81. [DOI] [PubMed] [Google Scholar]
Parmar 1998
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Statistics in Medicine 1998;17(24):2815-34. [DOI] [PubMed] [Google Scholar]
Piver 1974
- Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstetrics & Gynecology 1974;44(2):265-72. [PubMed] [Google Scholar]
Plotti 2011
- Plotti F, Angioli R, Zullo MA, Sansone M, Altavilla T, Antonelli E, et al. Update on urodynamic bladder dysfunctions after radical hysterectomy for cervical cancer. Critical Reviews in Oncology Hematology 2011;80(2):323-9. [DOI] [PubMed] [Google Scholar]
Querleu 2008
- Querleu D, Morrow CP. Classification of radical hysterectomy. Lancet Oncology 2008;9(3):297-303. [DOI] [PubMed] [Google Scholar]
Ramirez 2018
- Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. New England Journal of Medicine 2018;379(20):1895-904. [DOI] [PubMed] [Google Scholar]
Raspagliesi 2006
- Raspagliesi F, Ditto A, Fontanelli R, Zanaboni F, Solima E, Spatti G, et al. Type II versus type III nerve-sparing radical hysterectomy: comparison of lower urinary tract dysfunctions. Gynecologic Oncology 2006;102(2):256-62. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan) Version 5.3. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Roberts 2006
- Roberts K, Naik R. Catheterization options following radical surgery for cervical cancer. British Journal of Nursing 2006;15(19):1038-44. [DOI] [PubMed] [Google Scholar]
Santaguida 2012
- Santaguida S, Tortorella L, Vigliotta M, Margariti PA, Moruzzi MC, Scambia G, et al. Bladder training after nerve-sparing radical hysterectomy in cervical cancer patients: Is it necessary? In: International Journal of Gynaecology and Obstetrics. Vol. 119. 2012:472.
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and ‘Summary of findings’ tables. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Sellers 2012
- Sellers DJ, Chess-Williams R. Muscarinic agonists and antagonists: effects on the urinary bladder. Handbook of Experimental Pharmacology 2012;208:375-400. [DOI] [PubMed] [Google Scholar]
Srisomboon 2011
- Srisomboon J, Kietpeerakool C, Suprasert P, Manopanya M, Siriaree S, Charoenkwan K, et al. Survival and prognostic factors comparing stage IB 1 versus stage IB 2 cervical cancer treated with primary radical hysterectomy. Asian Pacific Journal of Cancer Prevention 2011;12(7):1753-6. [PubMed] [Google Scholar]
Sterne 2011
- Sterne J, Sutton A, Ioannidis J, Terrin N, Jones D, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
Suprasert 2010
- Suprasert P, Srisomboon J, Charoenkwan K, Siriaree S, Cheewakriangkrai C, Kietpeerakool C, et al. Twelve years experience with radical hysterectomy and pelvic lymphadenectomy in early stage cervical cancer. Journal of Obstetrics Gynaecology 2010;30(3):294-8. [DOI] [PubMed] [Google Scholar]
Torre 2015
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA: A Cancer Journal for Clinicians 2015;65(2):87-108. [DOI] [PubMed] [Google Scholar]
Verleye 2009
- Verleye L, Vergote I, Reed N, Ottevanger PB. Quality assurance for radical hysterectomy for cervical cancer: the view of the European Organization for Research and Treatment of Cancer - Gynecological Cancer Group (EORTC-GCG). Annals of Oncology 2009;20(10):1631-8. [DOI] [PubMed] [Google Scholar]
Viswanathan 2014
- Viswanathan AN, Lee LJ, Eswara JR, Horowitz NS, Konstantinopoulos PA, Mirabeau-Beale KL, et al. Complications of pelvic radiation in patients treated for gynecologic malignancies. Cancer 2014;15(120):24. [DOI] [PubMed] [Google Scholar]
Wallace 2004
- Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No: CD001308. [DOI: 10.1002/14651858.CD001308.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2007
- Wang XY. Effect of acupuncture on bladder function in patients with radical hysterectomy. Zhen Ci Yan Jiu 2007;32(2):132-5. [PubMed] [Google Scholar]
Wit 2014
- Wit EM, Horenblas S. Urological complications after treatment of cervical cancer. Nature Reviews Urology 2014;11(2):110-7. [DOI] [PubMed] [Google Scholar]
Yamanishi 2004
- Yamanishi T, Yasuda K, Kamai T, Tsujii T, Sakakibara R, Uchiyama T, et al. Combination of a cholinergic drug and an alpha-blocker is more effective than monotherapy for the treatment of voiding difficulty in patients with underactive detrusor. International Journal of Urology 2004;11(2):88-96. [DOI] [PubMed] [Google Scholar]
Yi 2011
- Yi WM, Pan AZ, Li JJ, Luo DF, Huang QH. Clinical observation on the acupuncture treatment in patients with urinary retention after radical hysterectomy. Chinese Journal of Integrative Medicine 2011;17(11):860-3. [DOI] [PubMed] [Google Scholar]
Zhou 2016
- Zhou W, Yang X, Dai Y, Wu Q, He G, Yin G. Survey of cervical cancer survivors regarding quality of life and sexual function. Journal of Cancer Research and Therapeutics 2016;12(2):938-44. [DOI] [PubMed] [Google Scholar]
Zullo 2003
- Zullo MA, Manci N, Angioli R, Muzii L, Panici PB. Vesical dysfunctions after radical hysterectomy for cervical cancer: a critical review. Critical Reviews in Oncology/Hematology 2003;48(3):287-93. [DOI] [PubMed] [Google Scholar]


