Abstract
Background
Psychosis is an illness characterised by the presence of hallucinations and delusions that can cause distress or a marked change in an individual's behaviour (e.g. social withdrawal, flat or blunted affect). A first episode of psychosis (FEP) is the first time someone experiences these symptoms that can occur at any age, but the condition is most common in late adolescence and early adulthood. This review is concerned with first episode psychosis (FEP) and the early stages of a psychosis, referred to throughout this review as 'recent‐onset psychosis.'
Specialised early intervention (SEI) teams are community mental health teams that specifically treat people who are experiencing, or have experienced a recent‐onset psychosis. The purpose of SEI teams is to intensively treat people with psychosis early in the course of the illness with the goal of increasing the likelihood of recovery and reducing the need for longer‐term mental health treatment. SEI teams provide a range of treatments including medication, psychotherapy, psychoeducation, and occupational, educational and employment support, augmented by assertive contact with the service user and small caseloads. Treatment is time limited, usually offered for two to three years, after which service users are either discharged to primary care or transferred to a standard adult community mental health team. A previous Cochrane Review of SEI found preliminary evidence that SEI may be superior to standard community mental health care (described as 'treatment as usual (TAU)' in this review) but these recommendations were based on data from only one trial. This review updates the evidence for the use of SEI services.
Objectives
To compare specialised early intervention (SEI) teams to treatment as usual (TAU) for people with recent‐onset psychosis.
Search methods
On 3 October 2018 and 22 October 2019, we searched Cochrane Schizophrenia's study‐based register of trials, including registries of clinical trials.
Selection criteria
We selected all randomised controlled trials (RCTs) comparing SEI with TAU for people with recent‐onset psychosis. We entered trials meeting these criteria and reporting useable data as included studies.
Data collection and analysis
We independently inspected citations, selected studies, extracted data and appraised study quality. For binary outcomes we calculated the risk ratios (RRs) and their 95% confidence intervals (CIs). For continuous outcomes we calculated the mean difference (MD) and their 95% CIs, or if assessment measures differed for the same construct, we calculated the standardised mean difference (SMD) with 95% CIs. We assessed risk of bias for included studies and created a 'Summary of findings' table using the GRADE approach.
Main results
We included three RCTs and one cluster‐RCT with a total of 1145 participants. The mean age in the trials was between 23.1 years (RAISE) and 26.6 years (OPUS). The included participants were 405 females (35.4%) and 740 males (64.6%). All trials took place in community mental healthcare settings.
Two trials reported on recovery from psychosis at the end of treatment, with evidence that SEI team care may result in more participants in recovery than TAU at the end of treatment (73% versus 52%; RR 1.41, 95% CI 1.01 to 1.97; 2 studies, 194 participants; low‐certainty evidence).
Three trials provided data on disengagement from services at the end of treatment, with fewer participants probably being disengaged from mental health services in SEI (8%) in comparison to TAU (15%) (RR 0.50, 95% CI 0.31 to 0.79; 3 studies, 630 participants; moderate‐certainty evidence).
There was low‐certainty evidence that SEI may result in fewer admissions to psychiatric hospital than TAU at the end of treatment (52% versus 57%; RR 0.91, 95% CI 0.82 to 1.00; 4 studies, 1145 participants) and low‐certainty evidence that SEI may result in fewer psychiatric hospital days (MD ‐27.00 days, 95% CI ‐53.68 to ‐0.32; 1 study, 547 participants).
Two trials reported on general psychotic symptoms at the end of treatment, with no evidence of a difference between SEI and TAU, although this evidence is very uncertain (SMD ‐0.41, 95% CI ‐4.58 to 3.75; 2 studies, 304 participants; very low‐certainty evidence). A different pattern was observed in assessment of general functioning with an end of trial difference that may favour SEI (SMD 0.37, 95% CI 0.07 to 0.66; 2 studies, 467 participants; low‐certainty evidence).
It was uncertain whether the use of SEI resulted in fewer deaths due to all‐cause mortality at end of treatment (RR 0.21, 95% CI 0.04 to 1.20; 3 studies, 741 participants; low‐certainty evidence).
There was low risk of bias for random sequence generation and allocation concealment in three of the four included trials; the remaining trial had unclear risk of bias. Due to the nature of the intervention, we considered all trials at high risk of bias for blinding of participants and personnel. Two trials had low risk of bias and two trials had high risk of bias for blinding of outcomes assessments. Three trials had low risk of bias for incomplete outcome data, while one trial had high risk of bias. Two trials had low risk of bias, one trial had high risk of bias, and one had unclear risk of bias for selective reporting.
Authors' conclusions
There is evidence that SEI may provide benefits to service users during treatment compared to TAU. These benefits probably include fewer disengagements from mental health services (moderate‐certainty evidence), and may include small reductions in psychiatric hospitalisation (low‐certainty evidence), and a small increase in global functioning (low‐certainty evidence) and increased service satisfaction (moderate‐certainty evidence). The evidence regarding the effect of SEI over TAU after treatment has ended is uncertain. Further evidence investigating the longer‐term outcomes of SEI is needed. Furthermore, all the eligible trials included in this review were conducted in high‐income countries, and it is unclear whether these findings would translate to low‐ and middle‐income countries, where both the intervention and the comparison conditions may be different.
Keywords: Adult, Female, Humans, Male, Young Adult, Bias, Community Mental Health Services, Early Medical Intervention, Early Medical Intervention/methods, Hospitalization, Hospitalization/statistics & numerical data, Psychotic Disorders, Psychotic Disorders/therapy, Randomized Controlled Trials as Topic
Plain language summary
Is recent‐onset psychosis best treated by a specialist mental health team?
What is psychosis?
Psychosis describes conditions affecting the mind, in which people have trouble distinguishing what is real from what is not real. This might involve seeing or hearing things that other people cannot see or hear (hallucinations), or believing things that are not true (delusions). The combination of hallucinations and delusional thinking can cause severe distress and a change in behaviour. A first episode psychosis is the first time a person experiences an episode of psychosis. Recent‐onset psychosis is the first few years of the illness after someone experiences it for the first time.
Psychosis is treatable
Many people recover from a first episode and never experience another psychotic episode. Mental health professionals assess a person before recommending a specific treatment. Depending on the services available, they may send people for treatment to:
‐ a community mental health team: mental health professionals who support people with complex mental health conditions;
‐ a crisis resolution team: mental health professionals who treat people who would otherwise need treatment in hospital; or
‐ an early intervention team: mental health professionals who work with people who are currently or have recently experienced their first episode of psychosis.
Early intervention teams specialise in treating recent‐onset psychosis, and aim to treat it as quickly and intensively as possible.
Why we did this Cochrane Review
We wanted to find out whether specialist early intervention teams were more successful at treating recent‐onset psychosis than outpatient or community mental health teams that do not specialise in treating it.
What did we do?
We searched for studies that investigated the use of early intervention teams to treat recent‐onset psychosis compared with standard community mental health care.
We looked for randomised controlled studies, in which the treatments people received were decided at random. This type of study usually gives the most reliable evidence about the effects of a treatment.
We wanted to find out, at the end of the treatment:
‐ how many people recovered;
‐ how many people stopped their treatment too soon;
‐ how many people were admitted to a psychiatric hospital, and for how long;
‐ the state of people's general mental health and functioning (how well they coped with daily life); and
‐ how many people died.
Search date: we included evidence published up to 22 October 2019.
What we found
We found four studies in 1145 people (65% men; average age 23 to 26 years) with recent‐onset psychosis. The studies compared treatment by specialist early intervention teams against 'usual treatment' (treatment by community health or outpatient mental health teams).
The studies took place in community mental health services in high‐income countries: Denmark, Sweden, the UK and the USA. The studies lasted from 18 to 24 months.
What are the results of our review?
Compared with usual treatment, treatment by an early intervention team:
‐may help more people recover from psychosis (2 studies; 194 people);
‐ probably reduces how many people stop their treatment too soon (3 studies; 630 people);
‐ may reduce the number of people admitted to a psychiatric hospital (4 studies; 1145 people)
‐ may reduce the time spent in a psychiatric hospital (1 study; 547 people); and
‐ may moderately improve people's general functioning (2 studies; 467 people).
We were uncertain about whether treatment by an early intervention team affects general psychotic symptoms (2 studies; 304 people), or its effect on how many people died (3 studies; 741 people).
How reliable are these results?
We are moderately confident that treatment by an early intervention team probably reduces the number of people who stop treatment too soon, although this result may change when more evidence is available.
We are less confident about how many people recover from psychosis, or are admitted to a psychiatric hospital, how long they stay in hospital, and any improvements in people's general functioning. These results are likely to change when more evidence is available.
Key message
Using specialist early intervention teams to treat recent‐onset psychosis is likely to have benefits, such as more people continuing with their treatment, and increasing the number of people who recover.
Summary of findings
Summary of findings 1. Specialised early intervention (SEI) compared to treatment as usual (TAU) for recent‐onset psychosis at end of treatment.
| SEI compared to TAU for recent‐onset psychosis at end of treatment | ||||||
| Patient or population: recent‐onset psychosis (less than three years since the start of psychotic symptoms and either first or second psychotic episode) Setting: community mental health Intervention: specialised early intervention team care Comparison: treatment as usual | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with TAU | Risk with SEI | |||||
| Global state: recovery (assessed by proportion recovered, as defined by the study, at end of treatment) | Study population | RR 1.41 (1.01 to 1.97) | 194 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | ||
| 516 per 1000 | 728 per 1000 (521 to 1000) | |||||
| Service use: disengagement from services (assessed by proportion disengaged, as defined by the study, at end of treatment) | Study population | RR 0.50 (0.31 to 0.79) | 630 (3 RCTs) | ⊕⊕⊕⊝ Moderateb | ||
| 150 per 1000 | 75 per 1000 (47 to 119) | |||||
| Service use: admission to psychiatric hospital (assessed by proportion admitted at end of treatment) | Study population | RR 0.91 (0.82 to 1.00) | 1145 (4 RCTs) | ⊕⊕⊝⊝ Lowe | ||
| 566 per 1000 | 515 per 1000 (464 to 566) | |||||
| Service use: number of days in psychiatric hospital (assessed by mean number of days in hospital at end of treatment) | The mean number of days in psychiatric hospital (end of treatment) in the TAU group was 123 days | MD 27 days fewer (53.68 fewer to 0.32 fewer) | ‐ | 547 (1 RCT) | ⊕⊕⊝⊝ Lowe | |
|
Mental state: average endpoint score on a general mental state scale (general psychopathology, assessed by PANNS at end of treatment)g |
‐ | SMD 0.41 points lower (4.58 lower to 3.75 higher) | ‐ | 304 (2 RCTs) | ⊕⊝⊝⊝ Very lowc,d,e | SMD of 0.50 represents a moderate effect size (Cohen 1988) |
| Death: all‐cause mortality (assessed by proportion deceased at end of treatment) | Study population | RR 0.21 (0.04 to 1.20) | 741 (3 RCTs) | ⊕⊕⊝⊝ Lowf | ||
| 19 per 1000 | 4 per 1000 (1 to 23) | |||||
| Functioning: average endpoint score on general functioning scale (global functioning, assessed by questionnaire at end of treatment) | ‐ | SMD 0.37 points higher (0.07 higher to 0.66 higher) | ‐ | 467 (2 RCTs) | ⊕⊕⊝⊝ Lowc,d | SMD of 0.50 represents a moderate effect size (Cohen 1988) |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardised mean difference; RCT: randomised controlled trial; RR: risk ratio; SEI: specialised early intervention; TAU: treatment as usual | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level due to indirectness. Use of surrogate outcome. Outcome assessment differs between trials. bDowngraded one level due to imprecision. Wide confidence intervals. cDowngraded one level due to risk of bias. Non‐blinded trials with subjective outcome, where outcomes assessor was either not blinded or allocation could easily be guessed by assessor. dDowngraded one level due to indirectness. Average scores from scales used to measure outcome instead of clinically important change. eDowngraded two levels due to imprecision. Few events, wide confidence intervals and small sample size. fDowngraded one level due to imprecision. Few events and wide confidence intervals. g Both studies used the PANNS scale to measure general psychopathology, but the LEO trial used an edited version with a smaller score range.
Background
Description of the condition
The lifetime prevalence of psychotic illness is estimated to be 4 per 1000 of the population, with first episode psychosis (FEP) incidence estimated at 34 new cases per 100,000 person‐years (Kirkbride 2012; Kirkbride 2017). Psychosis can occur at any age, but most people develop it in late adolescence and early adulthood, with a mean age of onset in the early twenties (Kirkbride 2017). Features of psychosis include hallucinations, delusions and disordered thinking (referred to as positive symptoms) and social withdrawal, flat or blunted affect, and poverty of speech (referred to as negative symptoms) (APA 2013). Psychotic illness encompasses a range of diagnoses, including schizophrenia and schizoaffective disorder, bipolar affective disorder and psychotic depression (WHO 2018). The impact on the individual is often significant; a psychotic illness has wide‐ranging implications on quality of life and disability, including effects on physical health, social functioning, social inclusion, and education and employment (Mason 1995; Meltzer 2002).
There is no consensus on the definition of FEP (Breitborde 2009). There may be a considerable delay between the onset of a person's symptoms and their being referred to, and treated by, mental health services (Birchwood 2013). The pathways to care for people with psychosis can also often involve multiple failed attempts at obtaining treatment before mental health services are able to successfully start a treatment regime (Lincoln 1998). As a result, clinical services and research studies use proxy measures for FEP. These are most commonly a 'duration criteria' (e.g. less than three years since first onset of symptoms), a 'contact with mental health services' criteria (e.g. first contact with mental health services), or an initiation of antipsychotic medication criteria (e.g. no more than 6 months of antipsychotic prescriptions). In this review, we will refer to FEP and the early stages of a psychosis as 'recent‐onset psychosis' in order to capture this uncertainty.
Schizophrenia and related psychotic illnesses are major contributors to the global burden of disease, with the associated annual economic costs estimated to range between USD 94 million and USD 102 billion by country (Chong 2016; Murray 1996). People with recent‐onset psychosis can reach remission of psychotic symptoms and functional recovery following an episode of psychosis, but many relapse, and as the number of relapses increases, the likelihood of remission decreases (Morgan 2014; Wiersma 1998). Recent studies have challenged the historically orthodox view that the course of a psychotic illness is deteriorating and progressive. A meta‐analysis on recovery after a first episode of psychosis estimated a 58% rate of remission and a 38% rate of recovery (Lally 2017). Long‐term outcome studies have also shown high rates of symptomatic recovery and (to a lesser extent) functional and social recovery in people being treated for recent‐onset psychosis (Revier 2015).
The growing optimism of remission and recovery following a psychotic episode has been complemented by services with a strong recovery‐oriented purpose that aim to intensively and assertively treat those with early psychosis in order to improve and enhance this recovery (Singh 2017).
Description of the intervention
A specialised early intervention (SEI) service is a phase‐specific multidisciplinary community mental health team that treats people experiencing, or who have recently experienced, their first episode of a psychotic illness (Fusar‐Poli 2017). The objectives of SEI services are two‐fold: first, they aim to intervene at an early stage of the illness, reducing the duration of untreated psychosis; second, they aim to provide a comprehensive package of treatment including medication, psychological therapies, and patient and family education, all backed by assertive case management (NICE 2014). The service model is of standalone, multidisciplinary community teams that provide an assertive outreach model of care, with care co‐ordinators having a restricted caseload size to enable them to work intensively with patients and engage them in treatment (RCPsych 2016). The aim of SEI is to reduce impairment and facilitate recovery, and in turn, improve prognosis.
SEI services are time‐limited to two or three years of treatment (depending on region and health service provision), with the rationale that early intensive treatment will preclude the need for such intensive treatment on an ongoing basis (i.e. a secondary prevention approach).
How the intervention might work
One of the most vocal arguments for the development of early phase treatments is that there is evidence of a 'critical period' in FEP (Birchwood 1998). This period, during the first few years of a psychotic illness, is potentially a period of rapid biological, psychological, and social changes, after which is followed by an eventual plateau of illness severity and functioning (Birchwood 1998). This trajectory of fluctuation of illness in the early years, followed by gradual deterioration has been found to be strongly predictive of later outcomes (Harrison 2001; Wiersma 1998). Standard community mental health teams had particular difficulty engaging this population, making it more challenging to deliver treatment (Birchwood 2014). SEI was developed primarily to improve engagement through assertive outreach, reducing the time to treatment (thereby reducing the duration of untreated psychosis) and potentially minimising the long‐term burden of the illness (Fusar‐Poli 2017). It is not clear however, whether SEI prevents poor outcomes, or alternatively, prevents poor outcomes only as long as SEI treatment is given.
Why it is important to do this review
SEI services are now considered the gold standard of care for people with recent‐onset psychosis in the UK, USA, Europe, and Australasia. In the UK it is the recommended treatment by the National Institute for Health and Care Excellence (NICE 2014), and timely access to SEI was the first National Health Service (NHS) waiting time standard for mental health care (NHS England 2015). Despite their widespread use, a previous Cochrane Review of early interventions for psychosis only found one eligible randomised control trial (RCT) of specialist team interventions for recent‐onset psychosis (Marshall 2011). A number of new RCTs comparing various forms of SEI to treatment as usual (TAU) have since been published (for example, GET UP PIANO 2013 and Kane 2016), and a recent meta‐analysis of SEI in the treatment of 'early phase psychosis', which included trials that recruited participants with multiple acute psychotic episodes or people who had already had lengthy community treatment (e.g. up to five years), found SEI superior to standard community mental health care in reducing treatment discontinuation, admission to psychiatric hospital, and psychotic symptoms (Correll 2018). It is important to do this review to ensure that new evidence for SEI services is evaluated.
Objectives
To compare specialised early intervention (SEI) teams to treatment as usual (TAU) for people with recent‐onset psychosis.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) regardless of blinding, but excluded quasi‐randomised studies, such as those that allocated interventions by alternate days of the week. Given the nature of the intervention, it would have been difficult to blind participants and clinicians from whether they were receiving the intervention or control condition and so we included both single‐ and double‐blinded studies. Where people were given additional treatments as well as specialised early intervention (SEI) for recent‐onset psychosis, we only included data if the adjunct treatment was evenly distributed between groups and it was only the SEI teams that were randomised. We did not exclude studies offering alternative models of care, such as step‐down care, following discharge from the early intervention team.
Types of participants
SEI services are designed to treat people in the early stages of psychosis. Exact eligibility criteria for services often differ both within and between regions and countries, but generally have a ‘time since onset' criterion and a ‘number of onsets’ criterion. We included participants who were within three years of the onset of their first psychotic episode (time since onset) with a first or second episode of psychosis (number of onsets). We included participants who were exhibiting symptoms that matched the criteria for primary psychotic diagnoses according to standardised criteria, such as the Diagnostic and Statistical Manual of Mental Disorders: DSM‐III (APA 1980), DSM‐III‐R (APA 1987), DSM‐IV (APA 1994), DSM‐IV‐TR (APA 2000), DSM‐5 (APA 2013), ICD‐10 (WHO 2004), ICD‐11 (WHO 2018) or Melbourne Criteria (Yung 2008). We excluded trials where participants had organic psychoses or head injury, and studies that recruited participants with prodromal symptoms (also known as 'at‐risk mental states') who had not yet transitioned to a psychotic episode. We also excluded trials that included participants whose onset of illness is longer than three years, unless we could extract data on only the eligible participants.
Types of interventions
Specialised early intervention (SEI) team care
These are multidisciplinary, standalone, community‐based mental health teams that take referrals for patients who have recent‐onset psychosis. SEI teams are an alternative, rather than an addition, to standard psychiatric care.
In order to be defined as a SEI service, the intervention had to provide the following.
Be multidisciplinary, standalone community‐based mental health teams that take referrals for patients who have recent‐onset psychosis and which is an alternative to, rather than an addition to, standard psychiatric care. Teams can share facilities with other health providers (for example, a community mental health team) but must operate independently from them. For example, having a separate caseload, separate team meetings, and a dedicated programme specifically aimed at the recent‐onset psychosis caseload.
Provide a package of treatment options that could include (but is not limited to) medication, psychological therapies, psychoeducation to the service user and carers, employment support, and physical health interventions (e.g. smoking cessation, physical health checks). These should be structured around regular, assertive outreach.
Accept service users on to the caseload who are in the first or second episode of psychosis and are within three years of the onset of their psychosis.
Treatment as usual (TAU)
TAU for people with recent‐onset psychosis differs by country, but usually consists of a community‐based or outpatient mental health team that does not provide specialist, phase‐specific (i.e. centred on the early phase of a psychotic illness) treatment.
Types of outcome measures
Timing of outcome assessment
We recorded post‐treatment outcomes and any available outcomes reported at follow‐up time points. Where appropriate, and if the data were available, we aimed to categorise treatment outcomes into end of treatment, medium‐term follow‐up (1 to 60 months post‐intervention), and long‐term follow‐up (longer than 60 months post‐intervention).
Primary outcomes
-
Global state
Recovery, as defined by the study
-
Service use
Disengagement from services, as defined by the study
Secondary outcomes
-
Service use
Admission to psychiatric hospital
Readmission to psychiatric hospital
Number of days in psychiatric hospital
-
Global state
Relapse, as defined by the study
-
Mental state
-
General
Clinically important change in general mental state
Any change in general mental state
Average endpoint/change score on a general mental state scale
-
Specific
Clinically important change in positive symptoms (delusions, hallucinations, disordered thinking), as defined by individual studies
Any change in positive symptoms (delusions, hallucinations, disordered thinking), as defined by individual studies
Clinically important change in negative symptoms (avolition, poor self‐care, blunted affect), as defined by individual studies
Any change in negative symptoms (avolition, poor self‐care, blunted affect), as defined by individual studies
Clinically important change in depression, as defined by individual studies
Any change in depression, as defined by individual studies
Average endpoint/change score on specific symptoms mental state scale/subscale
-
-
Behaviour
Specific
Occurrence of violent incidents (to self, others or property)
-
Adverse effects/events
-
General
At least one adverse effect/event
Average endpoint/change score on adverse effect scale
-
Specific
Incidence of any specific adverse effects, as defined by individual studies
-
-
Leaving the study early
For any reason
Due to adverse effect
-
Quality of life (recipient or informal carers or professional carers)
-
Overall
Clinically important change in overall quality of life
Average endpoint/change score on quality of life scale
-
-
Functioning
-
General
Clinically important change in general functioning
Average endpoint/change score on general functioning scale
-
Specific (including social, cognitive, life skills)
Clinically important change in specific functioning
Average endpoint/change score on specific functioning scale
Any change in educational status
Any change in employment status
-
-
Satisfaction with care (including subjective well‐being and family burden)
-
Recipient
Recipient satisfied with care
Average endpoint/change score on satisfaction scale
-
Carers
Carer satisfied with care
Average endpoint/change score on satisfaction scale
-
'Summary of findings' table
We used the GRADE approach to interpret findings (Schünemann 2011); and used GRADEpro GDT to export data from Review Manager 5 (RevMan 5) to create a 'Summary of findings' table. A 'Summary of finding' table provides outcome‐specific information concerning the overall certainty of evidence from each included study in the comparison, the magnitude of effect of the interventions examined, and the sum of available data on all outcomes we rate as important to patient care and decision making. We selected the following main outcomes for inclusion in the 'Summary of findings' table.
Global state: recovery, as defined by each study (at end of treatment).
Service use: disengagement from services, as defined by each study (at end of treatment).
Service use: admission to psychiatric hospital (at end of treatment).
Service use: number of days in psychiatric hospital (at end of treatment).
Mental state: clinically important change in general mental state (at end of treatment).
Adverse effects/events: death ‐ all‐cause mortality (at end of treatment).
Functioning: specific ‐ clinically important change in social functioning (at end of treatment).
If data were not available for these prespecified outcomes but were available for ones that are similar, we presented the closest outcome to the prespecified one in the table but took this into account when grading the finding.
Search methods for identification of studies
Electronic searches
Cochrane Schizophrenia's study‐based register of trials
On 3 October 2018, the Information Specialist searched the register using the search strategy described below. An update of this search strategy was conducted on 22 October 2019.
(*Early Intervention* AND *Special*) in Intervention Field of STUDY
In such study‐based registers, searching the major concept retrieves all the synonyms and relevant studies because all the studies have already been organised based on their interventions and linked to the relevant topics (Shokraneh 2017; Shokraneh 2018).
This register is compiled by systematic searches of major resources (AMED, BIOSIS, CENTRAL, CINAHL, ClinicalTrials.Gov, Embase, MEDLINE, PsycINFO, PubMed, WHO ICTRP) and their monthly updates, ProQuest Dissertations and Theses A&I and its quarterly update, Chinese databases (CBM, CNKI, and Wanfang) and their annual updates, handsearches, grey literature, and conference proceedings. There are no language, date, document type, or publication status limitations for inclusion of records into the register. For the full search strategies used to build Cochrane Schizophrenia's study‐based register of trials, please see: schizophrenia.cochrane.org/register-trials.
Searching other resources
Reference searching
We inspected references of all included studies for further relevant studies.
Personal contact
We contacted known experts in the field for information regarding unpublished trials. We noted the outcome of this contact in the 'Characteristics of included studies' and 'Characteristics of ongoing studies' tables.
Data collection and analysis
Selection of studies
Review authors SP and AM independently inspected citations from the searches and identified relevant abstracts; FDC independently re inspected a random 20% sample of the abstracts to ensure reliability of selection. Where disputes arose, we acquired the full report for more detailed scrutiny. SP and AM obtained and inspected full reports of the abstracts or reports meeting the review criteria. FDC re‐inspected a random 20% of these full reports in order to ensure reliability of selection. In case of disagreement, we involved another member of the review team (BL) to reach a final decision. We resolved all disagreements by discussion, and therefore did not need to attempt to contact the authors of the study concerned for clarification.
Data extraction and management
Extraction
Review authors SP, AM, and RH independently extracted data from all included studies. We attempted to extract data presented only in graphs and figures whenever possible, but included the data only if two review authors independently obtained the same result. SP and AM discussed any disagreement and documented our decisions. If necessary, we attempted to contact authors through an open‐ended request in order to obtain missing information, or for clarification. AC and BL helped clarify issues regarding any remaining problems and we documented these final decisions.
Management
Forms
We extracted data onto standard, predesigned, simple forms.
Scale‐derived data
We included continuous data from rating scales only if:
the psychometric properties of the measuring instrument had been described in a peer‐reviewed journal (Marshall 2000);
the measuring instrument had not been written or modified by one of the trialists for that particular trial; and
the instrument should have been a global assessment of an area of functioning and not subscores which are not, in themselves, validated or shown to be reliable.
However there were exceptions; we included subscores from mental state scales measuring positive and negative symptoms of schizophrenia where subscales had been previously validated in the empirical literature and were commonly used. Ideally, the measuring instrument should have either been i) a self‐report; or ii) completed by an independent rater or relative (not the therapist). We realise that this is not often reported clearly; in 'Description of studies' we noted if this was the case or not.
Endpoint versus change data
There are advantages of both endpoint and change data: change data can remove a component of between‐person variability from the analysis; however, calculation of change needs two assessments (baseline and endpoint) that can be difficult to obtain in unstable and difficult‐to‐measure conditions such as schizophrenia. We decided primarily to use endpoint data, and only used change data if the former were not available (Deeks 2011).
Skewed data
Continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data, we applied the following standards to relevant continuous data before inclusion.
Endpoint data from studies with fewer than 200 participants
When a scale started from the finite number zero, we subtracted the lowest possible value from the mean, and divided this by the standard deviation (SD). If this value was lower than one, it strongly suggested that the data are skewed and we excluded these data. If this ratio was higher than one but less than two, there was a suggestion that the data are skewed: we entered these data and tested whether their inclusion or exclusion would change the results substantially. If such data changed the results we entered them as 'other data'. Finally, if the ratio was larger than two we included these data, because it is less likely that they are skewed (Altman 1996).
If a scale started from a positive value (such as the Positive and Negative Syndrome Scale (PANSS), which can have values from 30 to 210 (Kay 1986), we modified the calculation described above to take the scale starting point into account. In these cases skewed data are present if 2 SD > (S − S min), where S is the mean score and 'S min' is the minimum score.
Please note: we entered all relevant data from studies of more than 200 participants in the analysis irrespective of the above rules, because skewed data pose less of a problem in large studies. We also entered all relevant change data, as when continuous data are presented on a scale that includes a possibility of negative values (such as change data), it is difficult to tell whether or not data are skewed.
Common measurement
To facilitate comparison between trials we aimed, where relevant, to convert variables that can be reported in different metrics, such as days in hospital (mean days per year, per week or per month) to a common metric (e.g. mean days per month).
Direction of graphs
Where possible, we entered data in such a way that the area to the left of the line of no effect indicates a favourable outcome for SEI. Where keeping to this made it impossible to avoid outcome titles with clumsy double‐negatives (e.g. 'not unimproved') we reported data where the left of the line indicated an unfavourable outcome and noted this in the relevant graphs.
Assessment of risk of bias in included studies
All included studies had two independent 'Risk of bias' assessments. Review authors SP, AM, and RH worked independently to assess risk of bias by using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions to assess trial quality (Higgins 2011a).
If the raters disagreed, we made the final rating by consensus. We reported non‐concurrence in quality assessment, but if disputes arose regarding the category to which a trial is to be allocated, we resolved this by discussion.
We note the level of risk of bias in both the text of the review, Figure 1 and Figure 2, and the 'Risk of bias' tables.
1.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Measures of treatment effect
Binary data
For binary outcomes we calculated a standard estimation of the risk ratio (RR) and its 95% confidence interval (CI). For binary data presented we calculated illustrative comparative risks (Hutton 2009).
Continuous data
For continuous outcomes we attempted to estimate the mean difference (MD) between groups if the measurement scales were the same, otherwise we used standardised mean difference (SMD).
Unit of analysis issues
Cluster trials
Studies increasingly employ 'cluster randomisation' (such as randomisation by clinician or practice), but analysis and pooling of clustered data poses problems. Authors often fail to account for intraclass correlation in clustered studies, leading to a unit of analysis error whereby P values are spuriously low, CIs unduly narrow and statistical significance overestimated (Divine 1992). This causes type I errors (Bland 1997; Gulliford 1999).
Where clustering had been incorporated into the analysis of primary studies, we presented these data as if from a non‐cluster randomised study, but adjusted for the clustering effect.
Where clustering had not been accounted for in primary studies, we presented data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. We sought to contact first authors of studies to obtain intraclass correlation coefficients for their clustered data and to adjust for this by using accepted methods (Gulliford 1999).
We have sought statistical advice and have been advised that the binary data from cluster trials presented in a report should be divided by a 'design effect'. This is calculated using the mean number of participants per cluster (m) and the intraclass correlation
coefficient (ICC): thus design effect = 1 + (m − 1) * ICC (Donner 2002). If the ICC was not reported we assumed it to be 0.1 (Ukoumunne 1999).
If cluster studies have been appropriately analysed and taken intraclass correlation coefficients and relevant data documented in the report into account, synthesis with other studies is possible using the generic inverse variance technique.
Cross‐over trials
A major concern of cross‐over trials is the carry‐over effect. This occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence, participants can differ significantly from their initial state at entry to the second phase, despite a washout phase. For the same reason cross‐over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both carry‐over and unstable conditions are very likely in severe mental illness, we only used data from the first phase of cross‐over studies.
Studies with multiple treatment groups
Where a study involved more than two treatment arms, if relevant, we presented the additional treatment arms in comparisons. If data were binary, we simply added these and combined them within the two‐by‐two table. If data were continuous, we combined data following the formula in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). Where additional treatment arms were not relevant, we did not reproduce these data.
Dealing with missing data
Overall loss of credibility
At some degree of loss of follow‐up, data must lose credibility (Xia 2009). We chose that, for any particular outcome, should more than 50% of data be unaccounted for we would not reproduce these data or use them within analyses. If, however, more than 50% of those in one arm of a study were lost, but the total loss was less than 50%, we addressed this within the 'Summary of findings' table by downgrading certainty. Finally, we also downgraded certainty within the 'Summary of findings' table if the loss was between 25% to 50% in total.
Binary
In the case where attrition for a binary outcome was between 0% and 50% and where these data were not clearly described, we presented data on a 'once‐randomised‐always‐analyse' basis (an intention‐to‐treat analysis (ITT)). Those leaving the study early were all assumed to have the same rates of negative outcome as those who completed. We used the rate of those who stayed in the study ‐ in that particular arm of the trial ‐ and applied this to those who did not. We undertook sensitivity analyses to test how prone the primary outcomes were to change when data only from people who completed the study to that point were compared to the ITT analysis using the above assumptions.
Continuous
Attrition
We used data where attrition for a continuous outcome was between 0% and 50%, and data only from people who completed the study to that point were reported.
Standard deviations (SDs)
If SDs were not reported, we tried to obtain the missing values from the authors. If these were not available, where there were missing measures of variance for continuous data, but an exacted standard error (SE) and CIs available for group means, and either P value or t value available for differences in mean, we calculated SDs according to the rules described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). When only the SE was reported, SDs were calculated by the formula SD = SE * √(n). The Cochrane Handbook for Systematic Reviews of Interventions presents detailed formulae for estimating SDs from P, t or F values, CIs, ranges or other statistics (Higgins 2011b). If these formulae did not apply, we calculated the SDs according to a validated imputation method which was based on the SDs of the other included studies (Furukawa 2006). If studies used different scales to measure the same construct, rather that calculate SDs according to the imputation methods, we followed the rules of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b) and carried the baseline SDs forward to the missing SDs. Although some of these imputation strategies can introduce error, the alternative would have been to exclude a given study's outcome and thus to lose information.
Assumptions about participants who left the trials early or were lost to follow‐up
Various methods are available to account for participants who left the trials early or were lost to follow‐up. Some trials just present the results of study completers; others use the method of last observation carried forward (LOCF); while more recently, methods such as multiple imputation or mixed‐effects models for repeated measurements (MMRM) have become more of a standard. While the latter methods seem to be somewhat better than LOCF (Leon 2006), we felt that the high percentage of participants leaving the studies early and differences between groups in their reasons for doing so is often the core problem in randomised schizophrenia trials. We therefore did not exclude studies based on the statistical approach used. However, by preference we used the more sophisticated approaches, i.e. we preferred to use MMRM or multiple imputation to LOCF, and we only presented completer analyses if some kind of ITT data were not available at all. Moreover, we addressed this issue in the item 'Incomplete outcome data' of the 'Risk of bias' tool.
Assessment of heterogeneity
Clinical heterogeneity
We considered all included studies without seeing comparison data to judge clinical heterogeneity. We inspected all studies for participants who were outliers or situations that we had not predicted would arise and, where found, discussed such situations or participant groups.
Methodological heterogeneity
We considered all included studies initially, without seeing comparison data, to judge methodological heterogeneity. We inspected all studies for clearly outlying methods that we had not predicted would arise and discussed any such methodological outliers.
Statistical heterogeneity
Visual inspection
We inspected graphs visually to investigate the possibility of statistical heterogeneity.
Employing the I² statistic
We investigated heterogeneity between studies by considering the I² statistic alongside the Chi² P value. We interpreted an I² estimate greater than or equal to 50% and accompanied by a statistically significant Chi² statistic as evidence of substantial heterogeneity (Deeks 2011). Where substantial levels of heterogeneity were found in the primary outcome, we explored reasons for heterogeneity (Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results (Egger 1997). These are described in section 10.1 of the Cochrane Handbook for Systemic reviews of Interventions (Sterne 2011).
Protocol versus full study
We attempted to locate protocols of included RCTs. If the protocol was available, we compared outcomes in the protocol and in the published report. If the protocol was not available, we compared outcomes listed in the methods section of the trial report with actually reported results.
Funnel plot
We are aware that funnel plots may be useful in investigating reporting biases but are of limited power to detect small‐study effects. We did not use funnel plots for outcomes where there were 10 or fewer studies, or where all studies were of similar size.
Data synthesis
We understand that there is no closed argument for preference for use of fixed‐effect or random‐effects models. The random‐effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This often seems to be true to us and the random‐effects model takes into account differences between studies, even if there is no statistically significant heterogeneity. There is, however, a disadvantage to the random‐effects model: it puts added weight onto small studies, which often are the most biased ones. Depending on the direction of effect, these studies can either inflate or deflate the effect size. We chose to use a random‐effects model for analyses.
Subgroup analysis and investigation of heterogeneity
Subgroup analyses
Standard SEI treatment duration
One of the most vocal arguments for the development of early phase treatments is that there is evidence of a 'critical period' in the early stages of psychosis (Birchwood 1998). This implies that there may be a dose‐response effect for treatment of recent‐onset psychosis (EASY_Extended). The most common duration of SEI treatment given in clinical scenarios is two years, but the duration of treatment given in studies may differ. As a subgroup analysis, where the duration of SEI treatment differed by more than six months from the standard two‐year duration of SEI care, we aimed to include only standard duration SEI trials in a subgroup analysis, however all trials were within six months duration of the standard SEI duration, so we did not perform any subgroup analysis.
Investigation of heterogeneity
We reported if inconsistency was high. Firstly, we investigated whether data had been entered correctly. Secondly, if data were correct, we inspected the graph visually and removed outlying studies successively to see if homogeneity was restored. For this review we decided that should this occur with data contributing to the summary finding of no more than 10% of the total weighting, we presented data. If not, we did not pool these data and discussed any issues.
When unanticipated clinical or methodological heterogeneity was obvious, we simply stated hypotheses regarding these for future reviews or versions of this review.
Sensitivity analysis
We carried out sensitivity analyses for primary outcomes only. If there were substantial differences in the direction or precision of effect estimates in any of the sensitivity analyses listed below, we did not add data from the lower‐quality studies to the results of the higher‐quality trials, but presented these data within a subcategory. If their inclusion did not result in a substantive difference, they remained in the analyses.
Implication of randomisation
If trials were described in some way as to imply randomisation, we aimed to compare data from the implied trials with trials that were randomised. However, all our included trials were randomised and therefore we did not conduct this sensitivity analysis.
Assumptions for lost binary data
Where assumptions had to be made regarding people lost to follow‐up (see Dealing with missing data) we compared the findings when we used our assumption and where we made the comparison with completer data only. If there was a substantial difference, we reported results and discussed them but continued to employ our assumption.
Assumptions for lost continuous data
Where assumptions had to be made regarding missing SDs (see Dealing with missing data), we aimed to compare the findings when we used our assumption and where we made the comparison with data that were not imputed. If there was a substantial difference, we aimed to report results and discuss them but continued to employ our assumption. However, we did not need to make any assumptions for lost continuous data and therefore did not conduct this sensitivity analysis.
Risk of bias
We aimed to analysed the effects of excluding trials that were at high risk of bias across one or more of the domains (see Assessment of risk of bias in included studies), however all trials included at least one domain at high risk of bias so we did not conduct this sensitivity analysis.
Imputed values
We aimed to undertake a sensitivity analysis to assess the effects of including data from trials where we used imputed values for ICC in calculating the design effect in cluster‐randomised trials, but this was not necessary as we did not impute values for ICC in any of the trials.
Fixed‐ and random‐effects
We synthesised data using a random‐effects model; however, we also synthesised data for the primary outcome using a fixed‐effect model to evaluate whether this altered the significance of the results.
Results
Description of studies
For substantive descriptions of the studies please see Included studies, Excluded studies, and Ongoing studies.
Results of the search
The first electronic search on 3 October 2018 identified 3321 references comprising 1854 studies. The second, updated search on 22 October 2019 identified a further 88 references. We further identified four references but no further studies through a cross‐referencing check of relevant papers. After duplicates were removed, 3335 references remained for screening. We excluded 3063 references through inspection of titles and abstracts, and obtained the full texts for the remaining 272 references, comprising 54 studies, to further assess eligibility. We excluded 49 studies; the reasons for exclusion are described in Excluded studies. One trial with three references is in the Ongoing studies list as the primary outcomes from this study have yet to be published (JCEP 2010). Overall, we included four trials with 144 references in this review. Figure 3 presents the flow chart of the study screening process.
3.
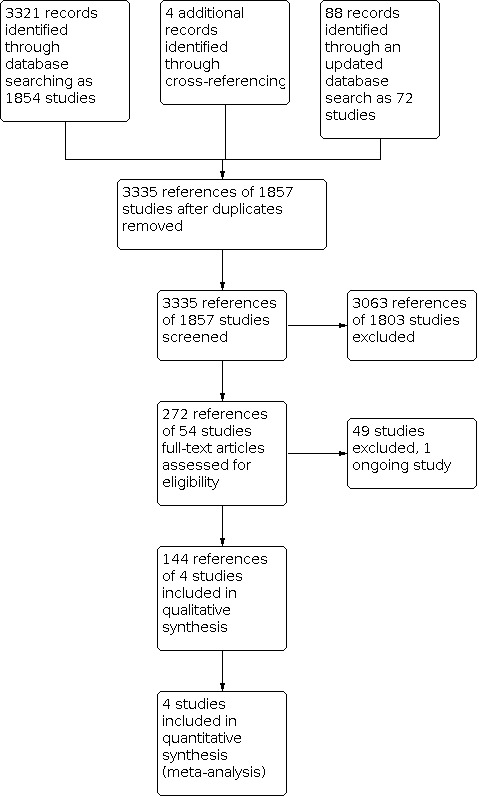
Study flow diagram.
Included studies
We included four studies with a total of 1145 participants.
Design and duration
Three studies were individually‐randomised controlled trials (RCTs) (LEO; OPUS; OTP), and one was a cluster‐RCT (RAISE). The total treatment duration was 18 months in LEO and 24 months in OPUS, OTP and RAISE.
Participants
Diagnosis
In LEO,participants had to meet the diagnostic criteria for non‐affective psychotic disorders and they had to be presenting to mental health services for the first time, or presenting to services a second time if on the first presentation they disengaged without receiving treatment.
In OPUS, participants had to meet diagnostic criteria for schizophrenia spectrum disorders, and could not have had more than 12 weeks continuous mental health treatment.
In OTP participants had to meet the diagnostic criteria for schizophrenia, schizoaffective, or schizophreniform disorders, having only presented to mental health services once (or twice without receiving proper treatment on the first occasion) and having a duration of untreated psychosis of less than 24 months.
In RAISE,participants had to meet diagnostic criteria for non‐affective psychosis, excluding substance induced psychotic disorders. They had to be in their first episode of psychosis with less than six months of lifetime antipsychotic prescriptions.
Age and gender
Age limit criteria were as follows: LEO 16 to 40 years; OPUS 18 to 45 years; OTP 18 to 35 years; RAISE 15 to 40 years. The mean age range in the trials was between 23.1 years (RAISE) and 26.6 years (OPUS). The included participants were 405 females (35.4%) and 740 males (64.6%).
Size
The sample size of the included trials ranged from 50 in OTP to 547 in OPUS, with a total of 1145 participants.
Setting
All four trials took place in community mental health settings in high‐income countries (LEO in England, OPUS in Denmark, OTP in Sweden, and RAISE in the USA).
Interventions
Specialised early intervention (SEI)
LEO was a SEI service with a multidisciplinary team providing an assertive outreach model of care. It provided an extended hours service (including weekend hours), case management with a case manager/service user ratio of 1:15, and offered a low‐dose atypical antipsychotic medication regimen, cognitive behaviour therapy (CBT), family counselling and vocational strategies, all from manualised protocols.
OPUS was a SEI service with a multidisciplinary team providing an 'enhanced' assertive outreach model of care. The service provided case management for two years, with a caseload ratio of 1:10. The service offered antipsychotic treatment, family psychoeducation, and social skills training.
OTP was a SEI service with a multidisciplinary treatment team. Case management was offered with a caseload ratio of 1:10 and intensive crisis management if needed. In addition, service users were offered low‐dose antipsychotic treatment, structured family psychoeducation, CBT, CBT‐based family communication and problem solving skills training.
RAISE was a standalone SEI service integrated within standard community mental health centres. Treatment was based on four core interventions: medication management, family psychoeducation, resilience‐focused individual therapy, and supported employment and education.
Outcomes
Non‐scale data
We were able to report dichotomous data on recovery, disengagement, leaving the study for any reason, relapse, admission to psychiatric hospital, number of readmissions to psychiatric hospital, number of days in psychiatric hospital, all‐cause mortality, employment, and violent offending.
Recovery was measured in three different ways in the three trials that reported data for the outcome: LEO defined recovery based on two clinicians' independent review of clinical notes over the course of the 18 months. OPUS defined recovery as not being psychotic based on the Life Chart Schedule for the two years prior to the five‐year follow‐up interview. OTP defined recovery through a clinical composite index based on the absence of 1) psychiatric hospital admissions, minor or major psychotic episode and persistent psychotic symptoms (i.e. four or more on the Brief Psychiatric Rating Scale (BPRS), hallucination or unusual thought content item for six or more consecutive weeks), 2) no suicide attempts, and 3) no poor compliance with treatment, throughout the two‐year follow‐up period.
Disengagement was measured in three different ways in the three trials that reported data for the outcome: LEO defined disengagement as having no contact with any mental health service at the 18‐month follow‐up. OPUS defined disengagement as stopping treatment despite clinical need according to clinical note review. OTP defined disengagement as receiving "little or no treatment" throughout the 24‐month follow‐up period.
We used data for participants leaving the study early for any reason in four trials (LEO; OPUS; OTP; RAISE). Leaving the study early was defined by any drop out from the study for any reason, including loss to follow‐up as reported in the study consort diagram and other supplementary materials. Disengagement relates to leaving treatment from mental health services, while leaving the study for any reason specifically relates to leaving the research study.
Relapse was reported in two studies. LEO defined relapse based on two clinicians' independent review of clinical notes over the course of the18 months of treatment from the SEI service. OTP defined a relapse as either a "major" or a “minor" reoccurrence. We used only major reoccurrence for our data. A major reoccurrence was defined as a two‐point increase in the Target Symptom rating scale and a score of six or seven on one of the key psychotic symptom items on the BPRS scale. In addition, this relapse had to be confirmed by an independent person from the rater (clinical team, or family member) as a significant worsening.
Psychiatric hospital admission was reported in all four trials (LEO; OPUS; OTP; RAISE). Psychiatric hospital admission was collected at multiple time points in LEO and OPUS however, we only used data for time periods measured from randomisation. Results reported in the cluster‐RCT RAISE were adjusted for both site and patient‐level random effects and we synthesised these data using the generic inverse variance technique.
The number of admissions was reported as mean psychiatric hospital admissions from randomisation in two trials (LEO; OTP). The number of psychiatric hospital admission was collected at multiple time points in LEO; however, we only used data for time periods measured from randomisation.
Number of days in psychiatric hospital was reported as mean hospital days per year in three trials (LEO; OPUS; OTP).
Death ‐ through suicide and natural causes was reported in three studies (LEO; OPUS; OTP).
Proportion in employment was measured in two studies (OPUS; RAISE). Results reported in the cluster‐RCT RAISE were adjusted for both site‐ and patient‐level random effects, and we synthesised these data using the generic inverse variance technique.
Violent offending was measured in one study (OPUS). It measured violent offending by the proportion of 'guilty' verdicts for a violent criminal offence during the two‐year and five‐year periods of follow‐up.
Outcome scales providing usable data
We were able to report outcome scale data on general psychopathology, positive psychotic symptoms, negative psychotic symptoms, depressive symptoms, general functioning, quality of life and service satisfaction.
Mental state scales
Positive and Negative Syndrome Scale ‐ PANSS (Kay 1986)
PANSS is a 30‐item scale including three subscales for measuring the severity of general psychopathology, positive symptoms, and negative symptoms. Each item is rated on a seven‐point scale, with higher scores indicating worse outcome. The Positive and Negative sub scales (with seven questions each) have a range of 7 to 49, whilst the general psychopathology subscale (with 16 questions) has a score range of 16 to 112. Two trials reported outcomes on this scale (LEO; RAISE). Results reported in the cluster‐RCT RAISE were adjusted for both site‐ and patient‐level random effects and we synthesised these data using the generic inverse variance technique.
Scale for the Assessment of Negative Symptoms ‐ SANS (Andreasen 1984)
The SANS is a valid instrument to assess the negative symptoms of schizophrenia. Each item, of which there are 25, is based on six‐point scale, with each domain symptoms rated from 0 (absent) to 5 (severe). Higher scores indicate more symptoms. OPUS reported outcomes on this scale, using the mean of the five global domain scores (range 0 to 5).
Scale for the Assessment of Positive Symptoms ‐ SAPS (Andreasen 2004)
SAPS is a rating scale to measure positive symptoms in schizophrenia. The scale is split into four domains, and within each domain separate symptoms are rated from 0 (absent) to 5 (severe). There are a total of 34 items. OPUS reported outcomes on this scale, using the mean of the four global domain scores (range 0 to 5).
Brief Psychiatric Rating Scale ‐ BPRS (Overall 1962)
The BPRS is a 24‐item scale that measures psychiatric symptoms. Each item is marked on a seven‐point Likert scale ranging from one to seven with one being ‘not present’ and seven being ‘extremely severe’. Possible scores range from 24 to 168 with lower scores representing less severe symptoms. Individual questions can be categorised into positive and negative symptoms. OTP reported outcomes on this scale.
Calgary Depression Scale ‐ CDS (Addington 1993)
CDS is a 9‐item scale designed to measure depression in schizophrenia patients without negative symptoms. The possible score ranges from 0 to 27 with higher scores indicating poor depression state. One trial reported outcomes on this scale (LEO).
Social functioning scales
Global Assessment of Functioning ‐ GAF (Jones 1995)
The GAF is a scale to assess psychological, social, and occupational functioning. It is rated on a 100‐point scale with lower scores indicating poorer functioning. Three trials report outcomes on this scale (LEO; OPUS; OTP).
Quality of life scales
Manchester Short Assessment of Quality of Life ‐ MANSA (Priebe 1999)
MANSA is a self‐report questionnaire that comprises 12 items on a seven‐point rating scale (range from 12 to 84) assessing satisfaction with life ‘in general’, with lower scores representing worse functioning. LEO reported outcomes on this scale; however, items are reversed scored, with lower scores representing better quality of life.
Heinrichs‐Carpenter Quality of Life Scale ‐ QLS (Heinrichs 1984)
The QLS has 21 items rated from semi‐structured interview, with each item rated on a seven‐point scale, for a total range of 0 to 126. Lower scores represent poorer quality of life. RAISE reported outcomes on this scale. Results reported in the cluster‐RCT RAISE were adjusted for both site‐ and patient‐level random effects and we synthesised these data using the generic inverse variance technique.
Service satisfaction scales
The Client Satisfaction Questionnaire ‐ CSQ‐8 (De Wilde 2005)
The CSQ‐8 is an eight‐item self‐report of global measure of patient satisfaction with services. The CSQ is substantially correlated with treatment dropout, number of therapy sessions attended, and with change in client‐reported symptoms. The CSQ‐8 consists of eight items rated on a four‐point Likert scale. The items are concerned with quality of services received, how well services met the client’s needs and general satisfaction. The total score ranges from eight to 32. Higher scores indicate greater satisfaction of the responders. OPUS reported outcomes on this scale.
Verona service satisfaction scale ‐ VSSS (Ruggeri 1993)
The VSSS is a 32‐item self‐report Likert scale (scored 1 to 5 ) addressing patients’ satisfaction with community‐based psychiatric services. Higher scores represent greater satisfaction. LEO used an eight‐item subscale of the VSSS to determine satisfaction with professionals' skills and behaviour, and reverse‐scored items so that greater satisfaction was represented by lower scores (scored 8 to 40).
Missing outcomes
The following prespecified outcome was not reported: mental state ‐ clinically important change in general mental state.
Excluded studies
We excluded 47 trials from this review. We have summarised them in Characteristics of excluded studies. The most common reasons for exclusion were that studies did not compare a SEI service in 15 (31.9%) studies, that there was no treatment as usual (TAU) condition in 11 (23.4%) studies, and that the intervention was a psychiatric inpatient‐only intervention in six (13.0%) studies.
Ongoing studies
We identified one ongoing trial whose results have not yet been published. Please refer to Ongoing studies for more details.
Awaiting assessment
No studies were awaiting assessment.
Risk of bias in included studies
See also Figure 1 and Figure 2.
Allocation
We graded three of the four eligible trials (3/4, 75%) as low risk of bias in relation to sequence generation (LEO; OPUS; OTP). The methods used for sequence generation were either independent or computer‐generated sequencing. We graded RAISE unclear for sequence generation, as it did not describe a method of sequence generation.
Three of the four eligible trials (3/4), 75%) had low risk of bias for allocation concealment (LEO; OPUS; OTP). All three described some form of allocation concealment through either pre‐numbered sealed envelopes or independent central allocation. We graded RAISE unclear for allocation concealment, as it did not describe a method of allocation concealment.
Blinding
Team‐based, long‐term treatment interventions are complex care interventions and would be difficult to mask. Therefore, none of the four trials blinded participants and the treatment team from the treatment arm allocation. We judged that outcome assessment was unlikely to influence results if the primary outcome was an objective outcome (i.e. not a clinical assessment or patient‐reported outcome), or if the primary outcome was subjective (i.e. self‐rated or interviewer‐rated) but those assessing the outcome were blind to the treatment allocation.
We graded all of the four eligible studies as high risk of bias for blinding of the participants. We graded two studies at high risk of bias for blinding of outcome assessments. In LEO, outcome assessors were blind to treatment allocation, however the primary outcome was a subjectively rated outcome made from reading clinical notes of which the outcome assessors were able to guess allocation with 60% accuracy. In OPUS, the primary outcome was an assessor‐rated symptom scale and assessors were not blind to treatment allocation.
Incomplete outcome data
We graded three of the four eligible trials (3/4, 75%) as low risk of bias in relation to incomplete outcome data (LEO; OPUS; OTP). LEO and OTP had a low proportion of incomplete outcome data, while OPUS had 25% missing data at two‐year (end of treatment) follow‐up in the SEI group and 40% missing data in TAU, but accounted for this using appropriate statistics and sensitivity analyses on the missing data. We rated RAISE at high risk of bias due to incomplete outcome data. The authors do not report on the exact figures for missing data but 54% in the intervention group and 68% in the TAU group were considered to have missing data either through exiting the study (34% and 53%, respectively), or completing the study with an assessment gap or gaps by missing more than three consecutive assessments in a row (19% and 13%, respectively). While the authors conducted appropriate analyses to account for missing data, we consider that these data were unlikely to be missing at random. We also consider that the difference in missingness between SEI and TAU would likely lead to bias, and no sensitivity analyses were reported in any published literature to test the assumptions of missingness.
Selective reporting
We considered LEO and RAISE at low risk of bias for selective reporting. Both trials reported prespecified outcomes from a protocol and there is a consistency of reported outcomes in the protocol, primary papers and follow‐up papers. We graded OTP as unknown risk of bias; we were unable to locate a published protocol, and the trial was registered with a trial registry only after the trial was completed. We graded OPUS at high risk of bias for selective reporting; their primary outcome is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not prespecified.
Other potential sources of bias
We did not think there was a high risk of other potential sources of bias within the included trials.
Effects of interventions
See: Table 1
Specialised early intervention (SEI) compared to treatment as usual (TAU)
Global state: recovery, as defined by the study
End of treatment
Two trials reported end of treatment recovery data. There was a clear difference between SEI and TAU care groups, favouring SEI (risk ratio (RR) 1.41, 95% confidence interval (CI) 1.01 to 1.97; 2 studies, 194 participants; I2 = 18%; low‐certainty evidence; Analysis 1.1).
1.1. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 1: Global state: recovery
Medium‐term SEI follow‐up (1 to 60 months post‐treatment)
OPUS reported medium‐term recovery data. There was no clear difference between SEI and TAU care groups (RR 0.96, 95% CI 0.71 to 1.30; 1 study, 547 participants; Analysis 1.1).
Sensitivity analysis, end of treatment
We found no substantive differences when we used data for completers only in a sensitivity analysis (RR 1.40, 95% CI 0.93 to 2.11; 2 studies, 181 participants), or when we used a fixed‐effect model instead of a random‐effects model (RR 1.41, 95% CI 1.01 to 1.97; 2 studies, 194 participants; Analysis 1.1).
Service use: disengagement from services, as defined by the study
End of treatment
Three trials reported data on disengagement at the end of treatment. There was a clear difference between SEI and TAU care groups, favouring SEI (RR 0.50, 95% CI 0.31 to 0.79; 3 studies, 630 participants; I2 = 0%; moderate‐certainty evidence; Analysis 1.2).
1.2. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 2: Service use: disengagement from services
Sensitivity analysis, end of treatment
We found no differences when we used data for completers only in a sensitivity analysis (RR 0.50, 95% CI 0.31 to 0.79; 3 studies, 630 participants), or when we used a fixed‐effect model instead of a random‐effects model in our analysis (RR 0.50, 95% CI 0.31 to 0.79; 3 studies, 630 participants; Analysis 1.2).
Service use: admission to psychiatric hospital
End of treatment
Four trials reported end of treatment follow‐up data for admission to psychiatric hospital. The point estimate suggests a difference between SEI and TAU care groups, favouring SEI, but the 95% confidence interval ranged between favouring SEI and no difference (RR 0.91, 95% CI 0.82 to 1.00; 4 studies, 1145 participants; low‐certainty evidence; Analysis 1.3).
1.3. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 3: Service use: admission to psychiatric hospital
Long‐term follow‐up (more than 60 months post‐treatment)
OTP reported on long‐term follow‐up data for admission to psychiatric hospital. There was no clear difference between SEI and TAU care groups (RR 0.77, 95% CI 0.48 to 1.24; 1 study, 50 participants).
Service use: readmission to psychiatric hospital
End of treatment
LEO reported data on this outcome. Data for this outcome were presented as 'other data' because of marked skew (Analysis 1.4), which makes it difficult to interpret the findings.
1.4. Analysis.
Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 4: Service use: readmission to psychiatric hospital ‐ skewed data
| Service use: readmission to psychiatric hospital ‐ skewed data | |||||
| Study | Intervention | Mean | SD | N | Notes |
| end of treatment | |||||
| LEO | SEI | 0.4 | 0.7 | 69 | Reported a difference |
| TAU | 0.8 | 1.0 | 67 | Reported a difference | |
| long term | |||||
| OTP | SEI | 4.4 | 7.9 | 28 | Reported no difference |
| TAU | 6 | 5.7 | 17 | Reported no difference | |
Long‐term follow‐up (more than 60 months post‐treatment)
OTP reported data on this outcome. Data for this outcome were presented as 'other data' because of marked skew (Analysis 1.4), which makes it difficult to interpret the findings.
Service use: number of days in psychiatric hospital
End of treatment
Two trials reported data on this outcome. Data for this outcome from the LEO trial were skewed and we excluded it from the analysis. There was a clear difference between SEI and TAU, favouring SEI (mean difference (MD) ‐27.00, 95% CI ‐53.68 to ‐0.32; 1 study, 547 participants; low‐certainty evidence; Analysis 1.5).
1.5. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 5: Service use: number of days in psychiatric hospital
Medium‐term SEI follow‐up (1 to 60 months post‐treatment)
OTP reported data on this outcome. We excluded data for this outcome from the analysis.
Global state: relapse, as defined by study
End of treatment
Two trials reported end of treatment relapse data. There was no clear difference between SEI and TAU care groups (RR 0.71, 95% CI 0.47 to 1.08; 2 studies, 194 participants; I2 = 0%; low‐certainty evidence; Analysis 1.6).
1.6. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 6: Global state: relapse
Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, general psychotic symptoms
End of treatment
Two trials reported data on this outcome. There was no clear difference between SEI and TAU care groups (standardised mean difference (SMD ‐0.41, 95% CI ‐4.58 to 3.75; 2 studies, 304 participants; very low‐certainty evidence; Analysis 1.7).
1.7. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 7: Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, general psychotic symptoms
Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, positive psychotic symptoms
End of treatment
Four trials reported data for average endpoint scores on specific symptom mental state scales. There was a clear difference between SEI and TAU groups, favouring SEI (SMD ‐0.18, 95% CI ‐0.33 to ‐0.03; 4 studies, 723 participants; Analysis 1.8).
1.8. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 8: Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, positive psychotic symptoms
Medium‐term SEI follow‐up (1 to 60 months post‐treatment)
OPUS reported medium‐term endpoint score data on positive psychotic symptoms. There was no clear difference between SEI and TAU care groups (SMD 0.06, 95% CI ‐0.16 to 0.29; 1 study, 301 participants).
Long‐term follow‐up (more than 60 months post‐treatment)
OPUS reported long‐term endpoint score data on positive psychotic symptoms. There was no clear difference between SEI and TAU care groups (SMD 0.02, 95% CI ‐0.15 to 0.19; 1 study, 547 participants).
Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, negative psychotic symptoms
End of treatment
Four trials reported data for average endpoint scores on specific symptom mental state scales. There was a clear difference between SEI and TAU groups, favouring SEI (SMD ‐0.32, 95% CI ‐0.53 to ‐0.11; 4 studies, 723 participants; Analysis 1.9).
1.9. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 9: Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, negative psychotic symptoms
Medium‐term SEI follow‐up (1 to 60 months post‐treatment)
OPUS reported medium‐term endpoint score data on negative psychotic symptoms. There was no clear difference between SEI and TAU care groups (SMD ‐0.07, 95% CI ‐0.29 to 0.16; 1 study, 301 participants).
Long‐term follow‐up (more than 60 months post‐treatment)
OPUS reported long‐term endpoint score data on negative psychotic symptoms. There was no clear difference between SEI and TAU care groups (SMD 0.05, 95% CI ‐0.12 to 0.21; 1 study, 547 participants).
Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, depressive symptoms
End of treatment
LEO reported data on this outcome. There was no clear difference between SEI and TAU care groups (MD 0.00, 95% CI ‐1.35 to 1.35; 1 study, 99 participants; very low‐certainty evidence; Analysis 1.10).
1.10. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 10: Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, depressive symptoms
Behaviour: specific, occurrence of violent incidents (to self, others or property)
End of treatment
OPUS reported data on occurrence of violent incidents at end of treatment. There was no clear difference between SEI and TAU care groups (RR 0.99, 95% CI 0.38 to 2.60; 1 study, 547 participants; very low‐certainty evidence; Analysis 1.11).
1.11. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 11: Behaviour: specific, occurrence of violent incidents (to self, others or property)
Medium‐term SEI follow‐up (1 to 60 months post‐treatment)
OPUS reported data on occurrence of violent incidents at medium‐term follow‐up. There was no clear difference between SEI and TAU care groups (RR 0.93, 95% CI 0.47 to 1.84; 1 study, 547 participants).
Adverse effects/events: death, suicide or natural cause
End of treatment
Three trials reported on all‐cause mortality at end of treatment. There was no clear difference between SEI and TAU care groups (RR 0.21, 95% CI 0.04 to 1.20; 3 studies, 741 participants; I2 = 0%; low‐certainty evidence; Analysis 1.12).
1.12. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 12: Adverse effects/events: death, suicide or natural cause
Medium‐term SEI follow‐up (1 to 60 months post‐treatment)
Two trials reported on all‐cause mortality at medium‐term follow‐up. There was no clear difference between SEI and TAU care groups (RR 0.56, 95% CI 0.22 to 1.46; 2 studies, 691 participants; I2 = 0%).
Long‐term follow‐up (more than 60 months post‐treatment)
OTP reported data on all‐cause mortality at long‐term follow‐up. There was no clear difference between SEI and TAU care groups (RR 0.23, 95% CI 0.01 to 5.28; 1 study, 50 participants).
Leaving the study early: for any reason
End of treatment
Four trials reported end of treatment data on leaving the study early. There was a clear difference between SEI and TAU care groups, favouring SEI (RR 0.63, 95% CI 0.54 to 0.74; 4 studies, 1145 participants; I2 = 0%; moderate‐certainty evidence; Analysis 1.13).
1.13. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 13: Leaving the study early: for any reason
Medium‐term SEI follow‐up (1 to 60 months post‐treatment)
OPUS reported medium‐term follow‐up data on leaving the study early. There was no clear difference between SEI and TAU (RR 1.00, 95% CI 0.86 to 1.16; 1 study, 547 participants).
Quality of life: recipient, overall, average endpoint score on quality of life scale
End of treatment
Two trials reported end of treatment data on average endpoint scores on quality of life scales. There was no clear difference between SEI and TAU (SMD 0.26, 95% CI ‐0.08 to 0.60; 2 studies, 300 participants; Analysis 1.14).
1.14. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 14: Quality of life: recipient, overall, average endpoint score on quality of life scale
Functioning: general, average endpoint score on general functioning scale
End of treatment
Two trials reported on end of treatment data on average endpoint score on a general functioning scale. There was a clear difference between SEI and TAU, favouring SEI (SMD 0.37, 95% CI 0.07 to 0.66; 2 studies, 467 participants; I2 = 45%; low‐certainty evidence; Analysis 1.15).
1.15. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 15: Functioning: general, average endpoint score on general functioning scale
Medium‐term SEI follow‐up (1 to 60 months post‐treatment)
OPUS reported on medium‐term follow‐up data on average endpoint score on a general functioning scale. There was no clear difference between SEI and TAU (SMD 0.07, 95% CI ‐0.16 to 0.29; 1 study, 301 participants).
Long‐term SEI follow‐up (more than 60 months post‐treatment)
OPUS reported on long‐term follow‐up data on average endpoint score on a general functioning scale. There was no clear difference between SEI and TAU (SMD ‐0.02, 95% CI ‐0.19 to 0.14; 1 study, 547 participants).
Functioning: specific, any change in education or employment status
End of treatment
Two trials reported end of treatment data on change in employment statues. There was no clear difference between SEI and TAU (RR 1.21, 95% CI 0.94 to 1.55; 2 studies, 951 participants; Analysis 1.16).
1.16. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 16: Functioning: specific, any change in education or employment status
Satisfaction with care: recipient, average endpoint score on satisfaction scale
End of treatment
Two trials reported end of treatment data on an average endpoint score on a satisfaction scale. There was a clear difference between SEI and TAU, favouring SEI (SMD 0.69, 95% CI 0.51 to 0.88; 2 studies, 463 participants; I2 = 0%; low‐certainty evidence; Analysis 1.17).
1.17. Analysis.

Comparison 1: Specialised early intervention (SEI) versus treatment as usual (TAU, Outcome 17: Satisfaction with care: recipient, average endpoint score on satisfaction scale
Discussion
Summary of main results
This review included three individually‐randomised controlled trials (RCTs) (LEO; OPUS; OTP), and one cluster‐RCT (RAISE), that investigated the effectiveness of standalone community mental health teams called specialised early intervention (SEI) in improving outcomes for people with first and early psychosis in comparison to treatment as usual (TAU).
Overall we found low‐certainty evidence that SEI increased the number of people considered recovered at the end of treatment, and moderate‐certainty evidence that fewer people had disengaged from SEI treatment than TAU. At medium‐term follow‐up of between 1 and 60 months after treatment had ended, we did not find any clear difference in recovery between SEI and TAU, although this included data from only one trial. No trials published data on medium‐term disengagement or long‐term (longer than 60 months after the intervention had ended) recovery or disengagement.
We found a number of differences between SEI and TAU for our secondary outcomes at end of treatment, although most of these were of between very low‐ and moderate‐certainty evidence. There was a clear, but small, effect of fewer admissions to psychiatric hospital favouring SEI, and small effects for fewer reported positive (hallucinations, delusions and disordered thinking) and negative (social withdrawal, flat or blunted affect, and poverty of speech) psychotic symptoms and better general functioning, all favouring SEI. Participants in SEI treatment also reported higher satisfaction with their care. Where trials reported medium‐term (positive and negative symptoms, general functioning) or long‐term (admission to hospital, positive and negative symptoms, and general functioning) data, we no longer found a difference between SEI and TAU. We found no clear differences at end of treatment, or medium‐ or long‐term outcomes (where reported), for relapse, general psychotic symptoms, depressive symptoms, occurrence of violent incidents, death from suicide or natural causes, quality of life, or change in employment or educational status.
Overall completeness and applicability of evidence
Completeness
We know of no further trials of SEI planned or underway other than the one identified in the Ongoing studies. There were a limited number of eligible trials for this review, although included trials did tend to collect similar outcome measures at end of treatment. There was a lack of completeness in the medium (1 ‐ 60 months after intervention ended) or long‐term (more than 60 months after intervention ended) follow‐ups, with only a single trial available for most outcome comparisons. There were a number of other trials of SEI which were ineligible due to their sample, which did not meet our criteria for a service to be considered 'early intervention' (a duration of untreated psychosis of less than three years and equal to or fewer than two episodes of psychosis). Another well‐known trial of SEI was not eligible as it did not offer a standalone SEI service (GET UP PIANO 2013).
Applicability
All four included trials recruited participants with early psychosis who would be eligible for SEI services. There were slight differences in recruitment criteria, with two trials specifically recruiting 'first episode' patients with little or no previous treatment (OPUS; RAISE), and two trials recruiting from an 'early psychosis' population who had one or two episodes of psychosis, but with minimal treatment for the first episode. Duration of untreated psychosis differed markedly between trials, and with large variation within each trial, but this would also be expected in everyday clinical practice. Each trial differed slightly in the treatment given, but all adhered to an assertive outreach approach within a standalone team.
All trials were conducted in high‐income countries. Therefore this evidence may not apply to SEI given in low‐ or middle‐income countries.
Certainty of the evidence
The certainty of evidence ranged between moderate and very low across our collected outcomes. When all four trials reported data on the same outcome, the evidence became of far higher certainty and met the optimal information size criteria. When there were fewer data to pool, this led to outcomes with imprecise estimates or outcomes being below the threshold for optimal information size. All four included trials were at high risk of bias in at least one domain of the Cochrane 'Risk of bias' tool. We downgraded all trials on risk of bias due to lack of blinding. This may be considered a controversial decision, as being able to blind participants in a complex intervention health services trial would be difficult, if not impossible. This risk could be minimised by appropriately blinding the assessment of outcomes, of which only two of the four trials adequately achieved. Finally, incomplete reporting of trial characteristics, such as randomisation procedures limited our ability to rate risk of bias in the two trials.
Potential biases in the review process
We have used a comprehensive search strategy with no language, date, or publication restrictions. However, there is always a possibility that eligible trials were missed. The SEI team construct is not stringently defined, and as such, disagreement about what qualifies as SEI treatment is possible. We aimed to adhere to a strict interpretation of SEI, including stringent eligibility criteria for participants and for the team structure.
Finally, we were unable to obtain some missing outcome data from eligible studies, as they were not reported or not available from study authors on request, which may have biased the results.
Agreements and disagreements with other studies or reviews
There is one previous review from the Cochrane Library, that included a comparison between SEI and TAU for early psychosis. Marshall 2011 included one eligible trial and found preliminary evidence for the effectiveness of SEI services. The Marshall 2011 trial differed markedly in scope to our current review. They reviewed all treatments for early psychosis, including early detection studies and treatments for those in the prodromal phase of psychosis, along with treatments for people with a first episode of psychosis. In comparison, our review only compared SEI community health services for people with recent‐onset psychosis. They included one eligible trial and found preliminary evidence for the effectiveness of SEI services.
There is one other notable review of SEI. Correll 2018 conducted a systematic review and meta‐analysis of SEI versus TAU for early phase psychosis and included 10 studies. Our review included fewer studies due to different eligibility criteria. We specified both a time since onset criteria and a number of psychotic episodes criteria for study participants. We also only included studies that evaluated SEI interventions that operated as an independent team, rather than as an enhanced care package within an existing community mental health team. Treatment given by SEI teams within the 10 included studies in the Correll 2018 review differed markedly. Results of our review and Correll 2018 were similar; with both finding more service users in recovery in SEI, fewer discontinuing treatment, fewer hospitalised at end of treatment, lower reported positive and negative psychotic symptoms, and better global functioning. Correll 2018 found no difference in general psychotic symptoms and depressive symptoms at the 18‐ to 24‐month end of treatment time points, results that are similar to our own end of treatment findings. Our results differed to Correll 2018 in regards to quality of life, numbers in work, and relapse, all outcomes of which they found differences between SEI and TAU (in favour of SEI) but we did not.
Authors' conclusions
Implications for practice.
For people with psychosis
There is some support for the effectiveness of SEI services while a person is being treated by them. There is low‐certainty evidence that treatment from a SEI team in comparison to TAU results in fewer admissions to psychiatric hospital and moderate‐certainty evidence it leads to fewer disengagements from community mental health treatment. There is also moderate‐certainty evidence that SEI treatment results in fewer positive (hallucinations, delusions and disordered thinking) and negative (social withdrawal, flat or blunted affect, and poverty of speech) psychotic symptoms and low‐certainty evidence of greater satisfaction with care during treatment. There is low‐certainty evidence that it also improves general functioning and the likelihood of recovery during treatment. Apart from disengagement from services and satisfaction with services, these effects are generally small and may not be clinically meaningful. There is also no evidence that after the treatment has finished, that these benefits are maintained.
As it is generally accepted that people in the early stages of psychosis require mental health treatment and there is no evidence of harm from SEI treatment in comparison to TAU, nor evidence of superior models of health care, SEI may provide some benefit.
For clinicians
There is low‐certainty evidence for the use of SEI services in comparison to TAU for a small reduction in psychiatric hospitalisation, and moderate‐certainty evidence of a large effect of reduction in disengagement from mental health services. There is moderate‐certainty evidence that SEI results in a small reduction of positive (hallucinations, delusions and disordered thinking) and negative symptoms (social withdrawal, flat or blunted affect, and poverty of speech) and low‐certainty evidence that it greatly increases satisfaction in care, while there is low‐certainty evidence that it improves general functioning and the likelihood of recovery. These effects were only observed during treatment and there was no evidence that outcomes are improved after the treatment has finished, although these were based on only one trial.
The evidence described here only applies for people with first‐ or second‐episode psychosis treated within three years of start of their symptoms, who have had little or no previous treatment for their psychosis. This evidence also only applies to SEI services that provide a standalone service as an independent package of care, rather than an add‐on to the currently available community mental health care (TAU).
For policy makers
For policy makers with the ability to implement SEI treatment programmes, there is between low‐ and moderate‐certainty evidence that there are short‐term clinical benefits to implementing SEI services in high‐income countries. Service‐level benefits include a reduction in admissions to psychiatric hospital and low‐certainty evidence of a reduction in the number of days spent in psychiatric hospital. Implementing SEI may improve service efficiency and reduce costs, although this review did not attempt to measure the economic impact of SEI services.
All four included trials came from high‐income countries. There is no evidence for SEI compared to TAU services in middle‐ and low‐income countries.
Implications for research.
General
While there were a small number of eligible trials, the size of the trials meant that optimal information criteria was generally met. All trials were at high risk of bias in at least one 'Risk of bias' item, in particular ‘blinding of participants and personnel’ in all four trials and ‘blinding of outcome assessment’ in two. As it is unlikely that one could find a suitable method of blinding SEI treatment from participants and personnel, it makes blinding the outcomes assessment all the more important. Participants leaving the study early was also high across trials, between 0% and 53.6% by trial arm (overall participants leaving the study early across all studies 34.5%, n = 1145). There were also no trials of SEI conducted in middle‐ or lower‐income countries, and both SEI and TAU probably differ in middle‐ or lower‐income countries, as well as potential differences in referral to these services (and therefore the types of participants who would be recruited for trials of SEI versus TAU). We did not collect outcome data on compulsory treatment or use of mental health legislation, which is an important outcome and should be included in any future studies and reviews. We have included a suggested design of a future trial of SEI in Table 2.
Specific
If further trials of SEI are conducted, we would recommend large, high‐quality trials that minimise risk of bias according to CONSORT, and trials in lower‐ or middle‐income countries. The priority for any trial should be establishing the medium‐ and long‐term outcomes of SEI after treatment has ended, as there is currently insufficient data to make any inference on these outcomes. Trials would need to be conducted in regions where there was still clinical equipoise as it is unlikely this equipoise exists in regions with well‐established SEI services.
1. Suggested future study design.
| Methods | Allocation: randomised Blinding: n/a. There is a very low likelihood of blinding being maintained in a such a complex intervention. Duration: two or three years intervention period, at least > 1‐year follow‐up period |
| Participants | Diagnosis: psychosis and related diagnoses N = 440* Gender: men and women Age: 14 ‐ 65 |
| Interventions | SEI comprised of recommended set of interventions: assertive community contact, small caseload size, offer of cognitive behaviour therapy for psychosis, family intervention, individual placement and support. |
| Outcomes | Global state: recovery** Global state: relapse Service use: disengagement from services Service use: admission to psychiatric hospital Functioning: clinically important change in functioning Quality of life: clinically important change in quality of life Economics: cost of care |
| Notes | * Sample size suggested relates to the size of a study with sufficient power to highlight a 10% difference between groups for the primary outcome if recovery in the intervention arm is 35% ** Primary outcome |
What's new
| Date | Event | Description |
|---|---|---|
| 17 February 2021 | Amended | Amended "blunted effect" to "blunted affect" in abstract text |
History
Protocol first published: Issue 3, 2019 Review first published: Issue 11, 2020
Acknowledgements
We would like to thank Dr Liu Shi from the Department of Psyhiatry, University of Oxford, for assisting us with translation of the Chinese‐language papers.
We would like to thank Clive Adams, Rebecca Syed, Claire Irving, Ghazaleh Aali, Farhad Shokraneh, Mahesh Jayaram and Irene Bighelli at the Cochrane Schizophrenia Group editorial base for their continued advice and support, as well as Robert Boyle, Senior Network Editor. Thanks to Nuala Livingstone and Clare Dooley from the Cochrane Editorial and Methods Department. Thanks to Heather Maxwell for copyediting the review and Carolyn Hughes for drafting the Plain Language Summary. We would like to thank peer reviewers Masahiro Banno and Dr Vidya Giri Shankar.
Cochrane Schizophrenia’s editorial base at The University of Nottingham, Nottingham, UK, produces and maintains standard text for use in the Methods section of their reviews. We have used this text as the basis of what appears here and adapted it as required.
Stephen Puntis is supported by the National Institute for Health Research (NIHR) through a NIHR Postdoctoral Fellowship Grant (PDF‐2017‐10‐029). The views expressed are those of the authors and not necessarily those of the UK National Health Service (NHS), the NIHR, or the UK Department of Health.
Andrea Cipriani is supported by the National Institute for Health Research (NIHR) Oxford Cognitive Health Clinical Research Facility, by an NIHR Research Professorship (grant RP‐2017‐08‐ST2‐006) and by the NIHR Oxford Health Biomedical Research Centre (grant BRC‐1215‐20005). The views expressed are those of the authors and not necessarily those of the UK National Health Service (NHS), the NIHR, or the UK Department of Health.
Data and analyses
Comparison 1. Specialised early intervention (SEI) versus treatment as usual (TAU.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Global state: recovery | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.1.1 end of treatment | 2 | 194 | Risk Ratio (IV, Random, 95% CI) | 1.41 [1.01, 1.97] |
| 1.1.2 medium term | 1 | 547 | Risk Ratio (IV, Random, 95% CI) | 0.96 [0.71, 1.30] |
| 1.1.3 Sensitivity analysis (lost binary data) ‐ end of treatment | 2 | 181 | Risk Ratio (IV, Random, 95% CI) | 1.40 [0.93, 2.11] |
| 1.1.4 Sensitivity analysis (lost binary data) ‐ medium term | 1 | 301 | Risk Ratio (IV, Random, 95% CI) | 0.96 [0.74, 1.26] |
| 1.1.5 Sensitivity analysis (fixed‐effect model) ‐ end of treatment | 2 | 194 | Risk Ratio (IV, Random, 95% CI) | 1.41 [1.01, 1.97] |
| 1.1.6 Sensitivity analysis (fixed‐effect model) ‐ medium term | 1 | 547 | Risk Ratio (IV, Random, 95% CI) | 0.96 [0.71, 1.30] |
| 1.2 Service use: disengagement from services | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.2.1 end of treatment | 3 | 630 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.31, 0.79] |
| 1.2.2 Sensitivity analysis (lost binary data) ‐ end of treatment | 3 | 630 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.31, 0.79] |
| 1.2.3 Sensitivity analysis (fixed‐effect model) ‐ end of treatment | 3 | 630 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.31, 0.79] |
| 1.3 Service use: admission to psychiatric hospital | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.3.1 end of treatment | 4 | 1145 | Risk Ratio (IV, Random, 95% CI) | 0.91 [0.82, 1.00] |
| 1.3.2 long term | 1 | 50 | Risk Ratio (IV, Random, 95% CI) | 0.77 [0.48, 1.24] |
| 1.4 Service use: readmission to psychiatric hospital ‐ skewed data | 2 | Other data | No numeric data | |
| 1.4.1 end of treatment | 1 | Other data | No numeric data | |
| 1.4.2 long term | 1 | Other data | No numeric data | |
| 1.5 Service use: number of days in psychiatric hospital | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.5.1 end of treatment | 1 | 547 | Mean Difference (IV, Random, 95% CI) | ‐27.00 [‐53.68, ‐0.32] |
| 1.5.2 long term | 1 | 45 | Mean Difference (IV, Random, 95% CI) | ‐56.00 [‐410.26, 298.26] |
| 1.6 Global state: relapse | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.6.1 end of treatment | 2 | 194 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.47, 1.08] |
| 1.7 Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, general psychotic symptoms | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.7.1 end of treatment | 2 | 304 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐4.58, 3.75] |
| 1.8 Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, positive psychotic symptoms | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.8.1 end of treatment | 4 | 723 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.33, ‐0.03] |
| 1.8.2 medium term | 1 | 301 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.16, 0.29] |
| 1.8.3 long term | 1 | 547 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.15, 0.19] |
| 1.9 Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, negative psychotic symptoms | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.9.1 end of treatment | 4 | 723 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.53, ‐0.11] |
| 1.9.2 medium Term | 1 | 301 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.29, 0.16] |
| 1.9.3 long term | 1 | 547 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.12, 0.21] |
| 1.10 Mental state: specific, average endpoint score on specific symptoms mental state scale/subscale, depressive symptoms | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.10.1 end of treatment | 1 | 99 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐1.35, 1.35] |
| 1.11 Behaviour: specific, occurrence of violent incidents (to self, others or property) | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.11.1 end of treatment | 1 | 547 | Risk Ratio (IV, Random, 95% CI) | 0.99 [0.38, 2.60] |
| 1.11.2 medium term | 1 | 547 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.47, 1.84] |
| 1.12 Adverse effects/events: death, suicide or natural cause | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.12.1 end of treatment | 3 | 741 | Risk Ratio (IV, Random, 95% CI) | 0.21 [0.04, 1.20] |
| 1.12.2 medium term | 2 | 691 | Risk Ratio (IV, Random, 95% CI) | 0.56 [0.22, 1.46] |
| 1.12.3 long term | 1 | 50 | Risk Ratio (IV, Random, 95% CI) | 0.23 [0.01, 5.28] |
| 1.13 Leaving the study early: for any reason | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.13.1 end of treatment | 4 | 1145 | Risk Ratio (IV, Random, 95% CI) | 0.63 [0.54, 0.74] |
| 1.13.2 medium term | 1 | 547 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.86, 1.16] |
| 1.14 Quality of life: recipient, overall, average endpoint score on quality of life scale | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.14.1 end of treatment | 2 | 300 | Std. Mean Difference (IV, Random, 95% CI) | 0.26 [‐0.08, 0.60] |
| 1.15 Functioning: general, average endpoint score on general functioning scale | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.15.1 end of treatment | 2 | 467 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [0.07, 0.66] |
| 1.15.2 medium term | 1 | 301 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.16, 0.29] |
| 1.15.3 long term | 1 | 547 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.19, 0.14] |
| 1.16 Functioning: specific, any change in education or employment status | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.16.1 end of treatment | 2 | 951 | Risk Ratio (IV, Random, 95% CI) | 1.21 [0.94, 1.55] |
| 1.17 Satisfaction with care: recipient, average endpoint score on satisfaction scale | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.17.1 end of treatment | 2 | 463 | Std. Mean Difference (IV, Random, 95% CI) | 0.69 [0.51, 0.88] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
LEO.
| Study characteristics | ||
| Methods | Study design: individually‐RCT Duration: intervention of 18 months, follow‐up until end of treatment at 18 months, and 5‐year follow‐up Setting: community‐based mental health team, England Recruitment method: patients who had presented to secondary mental health services (either through inpatient psychiatric services or community referrals) for first time, or presenting for a second time after a first presentation but subsequent disengagement |
|
| Participants | Diagnosis: diagnosis of non‐affective psychosis N = 144 Age: median age at baseline = 25 (IQR = 21.0 to 25.0) Sex: n = 93 (64.6%) male Inclusion criteria: aged 16 to 40, first or second presentation to mental health services specifically for treatment of non‐affective psychosis Exclusion criteria: organic psychosis, primary substance misuse diagnosis, asylum seekers liable to enforced dispersal |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Funding source: Directorate of Health and Social Care London research and development organisation and management programme (grant number RDC 01567) Conflicts of interest: TC and PP have received support from Eli Lilly, AstraZeneca, Janssen‐Cilag and Novartis for AstraZeneca, Janssen‐Cilag and Novartis for attending and speaking at conferences. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible patients were randomised to specialised care or standard care by permuted random blocks of between two and six. Group allocation was concealed in sealed envelopes. The trial statistician (GD) independently carried out the randomisation and concealment of results." Judgement: random permuted blocks |
| Allocation concealment (selection bias) | Low risk | Quote: as above Judgement: sealed envelopes, suggestive of adequate allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind to allocation, and subjective primary outcome rated by assessors who were able to guess allocation arm with above chance accuracy. Raters conducting participant interviews were not blind to allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Group allocation remained concealed until completion of the ratings. To test the success of blinding, assessors guessed the group allocation of each patient. The two raters correctly guessed the allocation of 60% (95% confidence interval 52% to 63%) of the patients (κ 0.20)" Judgement: assessors blinded and carried out ratings on extracts from notes with information about group allocation had been removed but could guess with above chance 60% accuracy. Secondary outcomes data from participant interviews were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement: low proportion of missing outcome data, carried out intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | Judgement: primary outcomes reported according to trial registry ISRCTN73679874 |
| Other bias | Low risk | None |
OPUS.
| Study characteristics | ||
| Methods | Study design: individually‐RCT Duration: intervention of 24 months, follow‐up until end of treatment at 24 months, and 5‐year and 10‐year follow‐up Setting: community‐based mental health team, Denmark Recruitment method: patients who had presented to secondary mental health services (either through inpatient psychiatric services or community referrals) for the first time and having no more than 12 weeks of antipsychotic treatment |
|
| Participants | Diagnosis: diagnosis of schizophrenia spectrum disorders, with diagnosis of schizophrenia comprising n = 382 (69%) of sample N = 547 Age: mean age at baseline 26.6 (SD = 6.4) and 26.6 (SD = 6.3) for intervention and TAU, respectively Sex: n = 323 (59.0%) male Inclusion criteria: aged 18 to 45 years, first contact with mental health services Exclusion criteria: prescribed antipsychotic medication for more than 12 weeks of continuous treatment |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Funding source: Danish Ministry of Health (jr.nr. 96‐0770‐71), Danish Ministry of Social Affairs, University of Copenhagen, Copenhagen Hospital Corporation, Danish Medical
Research Council (jr.nr. 9601612 and 9900734), and Slagtermester Wørzners Foundation. Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The included patients were centrally randomised to integrated treatment or standard treatment. In Copenhagen, randomisation was carried out through centralised telephone randomisation at the Copenhagen Trial Unit. The allocation sequence was computer generated, 1:1, in blocks of six, and stratified for each of five centres. In Aarhus, the researchers contacted a secretary by telephone when they had finished the entry assessment of each patient. The secretary then drew one lot from among five red and five white lots out of a black box. When the block of 10 was used, the lots were redrawn. Block sizes were unknown to the investigators." Judgement: randomly allocated by independent researcher |
| Allocation concealment (selection bias) | Low risk | Quote: as above Judgement: central allocation, adequate concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel not blind to allocation, and subjective primary outcome rated by assessors who were not blind to allocation arm. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Only independent investigators (PiJ, MA, PK, RM, LP,AT, TC, JØ) were involved in follow‐up interviews. For practical reasons, they could not be kept blind to treatment allocation" Judgement: no blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding due to it being an assessment by interviewer. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement: missing data have been imputed using appropriate methods |
| Selective reporting (reporting bias) | High risk | One or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not prespecified. Specifically the change in specified primary outcome was reported, but the original primary outcome result not reported. |
| Other bias | Low risk | None |
OTP.
| Study characteristics | ||
| Methods | Study design: individually‐RCT Duration: intervention of 24 months, follow‐up until end of treatment at 24 months, 10‐year follow‐up Setting: community‐based mental health team, Norway Recruitment method: consecutive referrals to secondary mental health services (either through inpatient psychiatric services or community referrals) for the first time and having no more than 24 months of previous psychiatric treatment |
|
| Participants | Diagnosis: diagnosis of schizophrenia and related disorders as per DSM‐IV N = 50 Age: mean age at baseline = 25.4 (SD = 4.6) Sex: n = 31 (62%) male Inclusion criteria: aged 18 to 35, first or second episode of psychosis Exclusion criteria: more than two years duration since first onset of symptoms, primary substance misuse diagnosis, mental retardation, not residing in service area during the study |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Funding source: Norwegian Research Council and the Norwegian Ministry of Health Conflict of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A secretary who was not part of the clinical service opened prenumbered envelopes with treatment group assignment according to random numbers provided by the central Optimal Treatment Project administration. Blocks were of variable size (8–12), stratified according to sex and with a ratio of IT to ST of 3: 2 to ensure that the majority of cases received the experimental treatment." Judgement: the investigators adequately describe a randomly allocated sequence by independent researcher |
| Allocation concealment (selection bias) | Low risk | Quote: "patients were randomly allocated to Integrated Treatment (IT), or ST, by an independent assistant with no knowledge of the referred patients" Judgement: low risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Judgement: participants and personnel not blind to allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Ratings were made by an independent rater who was blind to treatment conditions and trained to obtain a 0.8 kappa coefficient of inter‐rater reliability on all rating scales." Judgement: low risk of detection bias, although authors do not report on number of participants who's blinding could be guessed by assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote "Missing data were less than 10%"; Judgement: for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate; For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size |
| Selective reporting (reporting bias) | Unclear risk | No available registered protocol, trial registry lacks complete outcome information, trial registry entry after trial complete. Therefore unable to determine whether selective reporting occurred. |
| Other bias | Low risk | None |
RAISE.
| Study characteristics | ||
| Methods | Study design: cluster‐RCT, with clusters at the team level Duration: intervention of 24 months, follow‐up until end of treatment at 24 months Setting: community‐based mental health team, USA Recruitment method: participants who were taken on to the caseloads of the community teams who met eligibility criteria and consented to the intervention |
|
| Participants | Diagnosis: DSM‐IV diagnoses of schizophrenia n = 214 (52.9%), schizoaffective disorder, schizophreniform disorder, brief psychotic disorder, or psychotic disorder not otherwise specified were included N = 404; 34 randomised community teams (SEI = 17 team, TAU = 17 teams) Age: mean age at baseline 23.2 (SD = 5.2) and 23.1 (SD = 4.9) for intervention and TAU, respectively Sex: n = 293 (72.5%) male Inclusion criteria: aged 15 to 40, a first episode of psychosis, less than six months of lifetime psychotic medications Exclusion criteria: diagnosis of affective psychosis, substance‐induced psychotic disorder, organic psychosis, clinically significant head trauma or serious medical condition, non‐English language The participants in the SEI team differed from those in the TAU team by sex (77.6% male in comparison to 66.2%), had fewer participants with a previous hospitalisation (76.3% versus 81.6%) and worse symptom scores and fewer attending school than those in the TAU teams. |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Funding source: American Recovery and Reinvestment Act, NIMH (grant number HHSN271200900019C), NIMH Advanced Centers for Intervention and/or Services
Research award (P30MH090590). Conflicts of Interest: Dr. Kane has been a consultant for Alkermes, Amgen, Bristol‐Myers Squibb, Eli Lilly, EnVivo Pharmaceuticals (Forum), Forest, Genentech, H. Lundbeck, Intra‐Cellular Therapies, Janssen Pharmaceutica, Johnson and Johnson, Merck, Novartis, Otsuka, PierreFabre, Reviva, Roche, Sunovion, and Teva; he has received honoraria for lectures from Bristol‐Myers Squibb, Genentech, Janssen, Lundbeck, and Otsuka; and he is a shareholder in MedAvante and in Vanguard Research Group. Dr. Robinson has been a consultant to Asubio, Otsuka, and Shire; and he has received grants from Bristol‐Myers Squibb, Janssen, and Otsuka. Dr. Schooler has served on advisory boards or as a consultant for Abbott, Alkermes, Amgen, Eli Lilly, Forum (formerly EnVivo), Janssen Psychiatry, Roche, and Sunovion; she has received grant or research support from Genentech, Neurocrine, and Otsuka; and she has served on a data monitoring board for Shire and on the faculty of the Lundbeck International Neuroscience Foundation. Dr. Brunette has received grant support from Alkermes. Dr. Correll has been a consultant or adviser to or has received honoraria fromAbbVie, Actavis, Actelion, Alexza, Alkermes, Bristol‐Myers Squibb, Cephalon, Eli Lilly, Genentech, Gerson Lehrman Group, Intra‐Cellular Therapies, Janssen, Johnson and Johnson, Lundbeck, MedAvante, Medscape, Merck, Otsuka, Pfizer, ProPhase, Reviva, Roche, Sunovion, Supernus, Takeda, Teva, and Vanda; and he has received grant support from Bristol‐Myers Squibb, Janssen, Johnson and Johnson, Novo Nordisk, Otsuka, and Takeda. Ms Marcy is a shareholder in Pfizer. Mr Robinson has received grant support from Otsuka and is a shareholder in Pfizer. Dr Kurian has received grant support from Evotec, Forest, Johnson and Johnson,Naurex, Pfizer, Rexahn, and Targacept. Dr Miller has received payments for serving on a data monitoring committee for a study sponsored by Otsuka. The authors and their associates provide training and consultation about implementing NAVIGATE treatment that can include compensation. Dr Meyer‐Kalos, Dr Glynn, and Dr Robinson had received compensation for these activities. The other authors report no financial relationships with commercial interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Clinics were randomly assigned to the experimental intervention (N=17) or to standard care (N=17). None withdrew after randomisation" Judgement: authors state that clusters were randomly allocated but provide no detail on the method of sequence generation in protocol or outcome papers. |
| Allocation concealment (selection bias) | Unclear risk | Judgement: no text detailing allocation concealment in protocol or outcome papers. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Judgement: participants and personnel not blind to allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Centralized assessors, who were masked to individual treatment assignments and overall study design, administered..." Judgement: we considered that these centralised assessors conferred a low risk of bias for blinding of outcome assessment, however the authors do not detail whether there was any unbinding by assessors. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Judgement: analysis corrects for missing data, however there were extensive missing data: 51% of sample completed follow‐up, 55% in TAU and 45% in SEI respectively. Authors do not state overall proportion of missing data for repeated measures. It is likely that this missing data are not missing at random and missingness is likely to produce bias. We could find no evidence of sensitivity analyses examining missing data assumptions. |
| Selective reporting (reporting bias) | Low risk | Consistency of stated outcomes in trial registry and outcome papers. |
| Other bias | Low risk | None |
BPRS: Brief Psychiatric Rating Scale CBT: cognitive behaviour therapy CDG: congenital disorders of glycosylation GAF: Global Assessment of Functioning IQR: interquartile range MANSA: Manchester Short Assessment of Quality of Life NAVIGATE: A comprehensive early treatment program for people with first episode psychosis PANSS: Positive and Negative Syndrome Scale RCT: randomised controlled trial SAPS: Scale for the Assessment of Positive Symptoms SANS: Scale for the Assessment of Negative Symptoms SD: standard deviation SEI: specialised early intervention TAU: treatment as usual
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alaghband‐Rad 2006 | Intervention: not a SEI service |
| Cai 2013 | Intervention: medication trial |
| Carpenter 1982 | Intervention: medication trial |
| Cechnicki 2017 | Intervention: no minimum duration of untreated psychosis. Not a standalone service |
| Chen 2013 | Intervention: inpatient population, not community healthcare team intervention |
| COAST 2004 | Intervention: not within three years of onset of illness |
| Dai 2007 | Intervention: inpatient population, not community healthcare team intervention |
| EASY_Extended | Comparator: no TAU |
| Fan 2005c | Intervention: not a SEI service |
| GET UP PIANO 2013 | Intervention: not a standalone service |
| Hansen 2012 | Comparator: no TAU |
| Hou 2007 | Intervention: inpatient population, not community healthcare team intervention |
| ISRCTN58681229 | Comparator: no TAU |
| J‐CAP 2014 | Intervention: not within three years of onset of illness |
| LEO‐CAT 2004 | Intervention: not a SEI service evaluation, early detection only |
| Li 2012a | Intervention: inpatient population, not community healthcare team intervention |
| Li 2012b | Intervention: not a SEI service |
| Linszen 1994 | Comparator: no TAU |
| Linszen 2002 | Comparator: no TAU |
| Linszen 2003 | Comparator: no TAU |
| Linszen 2006 | Comparator: no TAU |
| Linszen 2007 | Comparator: no TAU |
| Liu 2012a | Intervention: medication trial |
| Liu 2012b | Intervention: not a SEI service |
| Malla 2000 | Randomisation: not a RCT |
| Malla 2017 | Intervention: extended SEI versus standard SEI, no TAU |
| NCT01783457 | Comparator: no TAU |
| NCT01936220 | See Linszen 2007 |
| NCT02037581 | Randomisation: not a RCT |
| NCT02751632 | Comparator: no TAU |
| NCT03409393 | Intervention: not a SEI service |
| OPUS II | Intervention: extended SEI versus standard SEI, no TAU |
| Pan 2012 | Intervention: not a SEI service |
| Qi 2006 | Intervention: not a SEI service |
| Qu 2012 | Intervention: medication trial |
| Rosenbaum 2002 | Randomisation: not a RCT |
| Santos 2008 | Intervention: not a SEI service |
| Sharivar 2010 | Intervention: not a SEI service |
| Sheng 2009 | Intervention: inpatient population, not community healthcare team intervention |
| STEP 2012 | Intervention: not within three years of onset of illness |
| Sun 2010 | Intervention: not a SEI service |
| Tang 2012 | Intervention: inpatient population, not community healthcare team intervention |
| Valencia 2010 | Intervention: not a SEI service |
| Valencia 2012 | Intervention: not a SEI service |
| Valencia 2013 | Intervention: not a SEI service |
| Wan 2012 | Intervention: medication trial |
| Wang 2012 | Intervention: not a SEI service |
| Zhang 2009 | Intervention: not a SEI service |
| Zipursky 2004 | Comparator: no TAU |
RCT: randomised controlled trial SEI: specialised early intervention TAU: treatment as usual
Characteristics of ongoing studies [ordered by study ID]
JCEP 2010.
| Study name | Stage‐specific case management for early psychosis |
| Methods | Study design: individually‐randomised controlled trial Country: Hong Kong Setting: community‐based mental health team |
| Participants | Eligiblility criteria: 22 ‐ 25 years of age, with a diagnosis of:
|
| Interventions | Components of treatment included:
|
| Outcomes | Functioning (social and occupational) |
| Starting date | 2009 |
| Contact information | christy@lmhui.com |
| Notes | Funding source: Hong Kong Jockey Club Charities Trust |
Differences between protocol and review
In the protocol the title of the review was 'Specialised early intervention teams for first episode psychosis'; in the review we changed the title to: 'Specialised early intervention teams for recent‐onset psychosis.' We have explained our decision to use the term 'recent‐onset psychosis' rather than 'first episode psychosis' in the Description of the condition.
In the protocol we used the following intervention term: 'early intervention in psychosis' (EIP); in the review we changed this to: 'specialised early intervention' (SEI).
In the protocol we used the following terms for the comparator: 'usual community mental health care' or 'standard care' or 'treatment as usual'; in the review we standardised this to 'treatment as usual' (TAU).
Timing of outcome assessment: in the protocol, we categorised timing of outcome assessments into short term (up to 12 months post‐treatment), medium term (13 to 60 months post‐treatment), and long term (longer than 60 months post‐treatment). In the review we have grouped these outcome assessments into end of treatment, medium term (1 to 60 months post treatment) and long term (longer than 60 months post‐treatment).
We have included relapse as an outcome in the full review. Relapse was measured as the proportion of participants who had relapsed, as defined by the study. We did not include relapse as an outcome in our protocol due to researcher error after a version edit of the protocol. We have added relapse to Types of outcome measures, Effects of interventions and Data and analyses sections.
We have used standardised mean difference (SMD) where different scales which assessed the same construct were comparable, while we have used mean difference (MD) where the construct was measured with the same scale. In our protocol we aimed to only use MD.
Contributions of authors
Stephen Puntis: development and writing of the review, study selection, statistical analysis
Amedeo Minichino: development and writing of the review, study selection, statistical analysis
Franco De Crescenzo: development and writing of the review, study selection, statistical analysis
Rachael Harrison: study selection, writing of the review
Andrea Cipriani: development and writing of the review, advised with study selection and statistical analysis
Belinda Lennox: development and writing of the review, advised with study selection and statistical analysis
Sources of support
Internal sources
-
University of Oxford, Oxford, UK
Employs review authors Stephen Puntis, Amedeo Minichino, Andrea Cipriani, and Belinda Lennox
-
NIHR Post Doctoral Fellowship Scheme ‐ Grant number PDF‐2017‐10‐029, UK
Funds review author Stephen Puntis
-
MRC‐Clarendon, UK
Funds review author Amedeo Minichino for DPhil
-
NIHR, UK
Provides additional funding to review author Belinda Lennox as clinical director for NIHR CRN: Thames Valley and South Midlands
-
Department of Epidemiology of the Regional Health Service, Italy
Provides funding for review author Franco De Crescenzo for the development of national clinical guidelines
-
NIHR Research Professorship, UK
Provides funding to Andrea Cipriani through a NIHR Professorship (RP‐2017‐08‐ST2‐006)
-
NIHR Oxford Health Biomedical Research Centre, UK
Provides support to Andrea Cipriani through grant (BRC‐1215‐20005)
External sources
None, Other
Declarations of interest
Stephen Puntis: SP currently receives research grants for the purpose of investigating the effectiveness of early intervention in psychosis services
Amedeo Minichino: AM currently receives Medical Research Council funding for a DPhil studentship
Franco De Crescenzo: none
Rachael Harrison: none
Andrea Cipriani: Andrea Cipriani has received research grants and consultancy fees from INCiPiT (Italian Network for Paediatric Trials), CARIPLO Foundation and Angelini Pharma, outside the submitted work.
Belinda Lennox: I work clinically in an early intervention in psychosis service, and am clinical lead for early intervention in psychosis for NHS England. I am an investigator on a pending NIHR HTA award examining extended early intervention services. I have received travel expenses from Lundbeck and Alkermes, fees for consultancy work for Astellas, and share income from GlaxoSmithKline, all outside the submitted work. No other declarations of interest.
Edited (no change to conclusions)
References
References to studies included in this review
LEO {published data only}
- Craig T, Garety P, Power P, Rahaman N, Colbert S, Fornells-Ambrojo M. Lambeth early onset service: a randomised controlled trial. Schizophrenia Research 2004;70(1):145-6. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig T. Brixton early psychosis project. http://www.controlled-trials.com 2004. [MEDLINE]
- Craig T. Brixton early psychosis project. National Research Register 2001;3. [MEDLINE]
- *.Craig TK, Garety P, Power P, Rahaman N, Colbert S, Fornells-Ambrojo M, et al. The Lambeth Early Onset (LEO) Team: randomised controlled trial of the effectiveness of specialised care for early psychosis. BMJ 2004;329(7474):1067-70. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig TK. Brixton early psychosis project. National Research Register 2000. [MEDLINE]
- Fornells-Ambrojo M, Craig T, Garety P. Occupational functioning in early non-affective psychosis: the role of attributional biases, symptoms and executive functioning. Epidemiology and Psychiatric Sciences 2014;23(1):71-84. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gafoor R, Nitsch D, Craig T, Garety P, Power P, McGuire P. Does Early Intervention (EI) in schizophrenia improve long term outcome? Results from 5 year follow-up study (South London Interventions in First Episode psychosis - LIFE). Early Intervention in Psychiatry 2008;2(Suppl 1):A51. [MEDLINE] [Google Scholar]
- Gafoor R, Nitsch D, McCrone P, Craig TK, Garety PA, Power P, et al. Effect of early intervention on 5-year outcome in non-affective psychosis. British Journal of Psychiatry 2010;196(5):372-6. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Garety P. Randomised controlled trial of early psychosis in Lambeth. National Research Register 2001;1. [MEDLINE]
- Garety PA, Craig TK, Dunn G, Fornells-Ambrojo M, Colbert S, Rahaman N, et al. "Specialised care for early psychosis: symptoms, social functioning and patient satisfaction: randomised controlled trial": corrigenda. British Journal of Psychiatry 2006;188(3):295. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Garety PA, Craig TK, Dunn G, Fornells-Ambrojo M, Colbert S, Rahaman N, et al. Specialised care for early psychosis: symptoms, social functioning and patient satisfaction: randomised controlled trial. British Journal of Psychiatry 2006;188(1):37-45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Knapp M. Brixton early psychosis study project #432. National Research Register 2004;1. [MEDLINE]
- McCrone P, Craig TK, Power P, Garety PA. Cost-effectiveness of an early intervention service for people with psychosis. British Journal of Psychiatry 2010;196(5):377-82. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Power P, Craig T, Garety P, Rahaman N, Colbert S, Fornells-Ambrojo M. Lambeth early onset (LEO) trial: a randomised controlled trial of assertive community follow-up in early psychosis: initial 6 month data. In: Unknown Source. 1994. [MEDLINE]
- Power P, Craig T, Garety P, Rahaman N, Fornells-Ambrojo M, Colbert S. A randomised controlled trial of assertive community follow-up in early psychosis: preliminary results. Schizophrenia Research 2002;53(3 Suppl 1):42. [MEDLINE] [Google Scholar]
- Power P, McGuire P, Iacoponi E, Garety P, Morris E, Valmaggia L, et al. Lambeth early onset (leo) and outreach & support in south london (oasis) service. Early Intervention in Psychiatry 2007;1(1):97-103. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Tempier R, Balbuena L, Garety P, Craig TJ. Does assertive community outreach improve social support? Results from the Lambeth study of early-episode psychosis. Psychiatric Services 2012;63(3):216-22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Tempier R, Balbuena L, Lepnurm M, Craig TK. Perceived emotional support in remission: results from an 18-month follow-up of patients with early episode psychosis. Social Psychiatry and Psychiatric Epidemiology 2013;48(12):1897-904. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Van Meijel B. Early intervention has no effect on symptoms in people with first episode, non-affective psychosis, although it may improve overall function and medication adherence. Evidence-Based Mental Health 2006;9(3):69. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
OPUS {published data only}
- Øhlenschlæger J, Thorup A, Petersen L, Jeppesen P, Abel M, Nordentoft M. Coercion in first episode psychosis. In: Proceedings of the 3rd International Conference on Early Psychosis; 2002 Sep 25-28; Copenhagen, Denmark. 2002:89-90. [MEDLINE]
- Albert N, Jensen H, Melau M, Hjorthoj C, Nordentoft M. How long should a specialized assertive early intervention program last? Early Intervention in Psychiatry 2014;8:10. [MEDLINE] [Google Scholar]
- Archie S. Integrated care improves one year outcomes in first episode psychosis. Evidence-Based Mental Health 2006;9(2):46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Austin S, Seche R, Hagen R, Mors O, Nordentoft M. Remission, metacognitive processes and quality of life-outcomes from opus trial. A 10 year follow-up of a randomized multi-center trial of intensive early intervention vs. Standard treatment for patients with first episode schizophrenia spectrum disorder. Schizophrenia Bulletin 2011;37:258. [MEDLINE] [Google Scholar]
- Austin S, Secher RG, Mors O, Nordentoft M. Course of illness in first-episode psychosis-outcomes from opus trial. Early Intervention in Psychiatry 2012;6:15. [MEDLINE] [Google Scholar]
- Austin S. An investigation of metacognitive beliefs and psychopathology within the opus cohort at 10 year follow up. Early Intervention in Psychiatry 2010;4(Suppl 1):144. [MEDLINE] [Google Scholar]
- Bergh S, Hjorthoj C, Sorensen HJ, Fagerlund B, Austin S, Secher RG, et al. Predictors and longitudinal course of cognitive functioning in schizophrenia spectrum disorders, 10years after baseline: the OPUS study. Schizophrenia Research 2016;175(1-3):57-63. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Bertelsen M, Jeppesen P, Petersen L, Thorup A, Ohlenschlaeger J, Le Quach P, et al. Course of illness in a sample of 265 patients with first-episode psychosis--five-year follow-up of the Danish OPUS trial. Schizophrenia Research 2009;107(2-3):173-8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Bertelsen M, Jeppesen P, Petersen L, Thorup A, Ohlenschlaeger J, le Quach P, et al. First episode of psychosis intensive early intervention programme versus standard treatment-secondary publication. Ugeskrift for Laeger 2009;171(41):2992-5. [MEDLINE: ] [PubMed] [Google Scholar]
- Bertelsen M, Jeppesen P, Petersen L, Thorup A, Ohlenschlaeger J, le Quach P, et al. Five-year follow-up of a randomized multicenter trial of intensive early intervention vs standard treatment for patients with a first episode of psychotic illness: the OPUS trial. Archives of General Psychiatry 2008;65(7):762-71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Bertelsen M, Jeppesen P, Petersen L, Thorup A, Ohlenschlaeger J, le Quach P, et al. Suicidal behaviour and mortality in first-episode psychosis: the OPUS trial. British Journal of Psychiatry. Supplements 2007;191(Suppl 51):s140-6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Bertelsen M, Jeppesen P, Petersen L, Thorup A, Ohlenschlaeger J, Quach P, et al. The OPUS-trial; a randomised multicentre single-blinded trial of integrated versus standard treatment for patients with a first episode of psychotic illness - five-years follow-up. Early Intervention in Psychiatry 2008;2(Suppl 1):A6. [MEDLINE] [Google Scholar]
- Bertelsen M, Nordentoft M, Jeppesen P, Petersen L, Thorup A, Le Quach P. The OPUS trial: results from the five-years follow-up. Schizophrenia Bulletin 2007;33(2):421. [MEDLINE] [Google Scholar]
- Bertelsen M, Thorup A, Petersen L, Jeppesen P, Oehlenschlager J, Joergensen P, et al. The OPUS trial: results from the five-year follow-up. Schizophrenia Research 2006;86(Suppl 1):S43. [MEDLINE] [Google Scholar]
- Bertelsen M. Randomized controlled trial of two years integrated treatment versus standard treatment of patients with first-episode of schizophrenia or psychosis, five years follow-up. The opus trial. Schizophrenia Bulletin 2005;31:519-20. [MEDLINE] [Google Scholar]
- Bertelsen M. Rct of integrated treatment versus standard treatment of patients with first-episode of schizophrenia - 5 years follow up. Schizophrenia Research 2004;70(1):32. [MEDLINE] [Google Scholar]
- Bertensen M, Le Quach P, Jeppesen P, Petersen L, Thorup A, Ohlenschlaeger J, et al. The OPUS trial: a randomised multi-centre trial of intensive early-intervention programme versus standard treatment for 547 first-episode psychotic patients - a five-year follow up. In: Proceedings of the International Congress on Schizophrenia Research; 2009 Mar 28 - Apr 1; San Diego, California, USA. 2009. [MEDLINE]
- Ellersgaard D, Mors O, Thorup A, Jorgensen P, Jeppesen P, Nordentoft M. A prospective study of the course of delusional themes in first episode non-affective psychosis. Early Intervention in Psychiatry 2012;6:67. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Ellersgaard D, Mors O, Thorup A, Jorgensen P, Jeppesen P, Nordentoft M. Prospective study of the course of delusional themes in first-episode non-affective psychosis. Early Intervention in Psychiatry 2014;8(4):340-7. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Hastrup LH, Kronborg C, Bertelsen M, Jeppesen P, Jorgensen P, Petersen L, et al. Cost-effectiveness of early intervention in first-episode psychosis: economic evaluation of a randomised controlled trial (the OPUS study). British Journal of Psychiatry 2013;202(1):35-41. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Hastrup LH, Kronborg C, Nordentoft M, Simonsen E. Cost-effectiveness of a randomized multicenter trial in first-episode psychosis (opus) in Denmark. Journal of Mental Health Policy and Economics 2011;14:S10. [MEDLINE] [Google Scholar]
- Hjorthoj C, Secher G, Austin S, Mors O, Nordentoft M. Ten-year follow-up of the Opus trial for first-episode psychosis. Early Intervention in Psychiatry 2014;8:16. [MEDLINE] [Google Scholar]
- Jørgensen P, Jeppesen P, Abel MB, Kassow P, Krarup G, Hemmingsen R, et al. Early intervention in schizophrenia. Nordic Journal of Psychiatry 2002;56(2):8. [MEDLINE] [Google Scholar]
- Jørgensen P, Nordentoft M, Abel MB, Gouliaev G, Jeppesen P, Kassow P. Early detection and assertive community treatment of young psychotics: the Opus study rationale and design of the trial. Social Psychiatry and Psychiatric Epidemiology 2000;35(7):283-7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Jeppesen P, Abel M B, Krarup G, Jorgensen P, Nordentoft M. Family burden and expressed emotion in first episode psychosis. The OPUS-trial. In: Proceedings of the 3rd International Conference on Early Psychosis; 2002 Sep 25-28; Copenhagen, Denmark. 2002:59. [MEDLINE]
- Jeppesen P, Hemmingsen R, Jírgensen P, Reisby N, Abel M-B, Nordentoft M. Opus project: impact of mental disorder on caregivers. Proceedings of the 11th World Congress of Psychiatry; 1999 Aug 6-11; Hamburg, Germany 1999;2:157. [MEDLINE] [Google Scholar]
- Jeppesen P, Hemmingsen R, Reisby N, Jørgensen P, Nordentoft M, Abel M-B. The impact of mental disorder on caregivers. Proceedings of the 11th World Congress of Psychiatry; 1999 Aug 6-11; Hamburg, Germany 1999;2:187. [MEDLINE] [Google Scholar]
- Jeppesen P, Nordentoft M, Abel M, Hemmingsen RP, Joergensen, Kassow P. Opus-project: a RCT of integrated psychiatric treatment for recent onset psychotic patients. Schizophrenia Research 2001;49(1-2):262. [MEDLINE] [Google Scholar]
- Jeppesen P, Nordentoft M, Jorgensen P, Abel MB, Reisby N, Hemmingsen R, et al. Opus-project: better compliance? A randomised-controlled trial of integrated care of first-episode psychotic patients conference abstract. Schizophrenia Research 1999;36(1-3):327. [MEDLINE] [Google Scholar]
- Jeppesen P, Petersen L, Thorup A, Abel M-B, Oehlenschlaeger J, Christensen TO, et al. Integrated treatment of first-episode psychosis: effect of treatment on family burden: OPUS trial. British Journal of Psychiatry 2005;48(Suppl):s85-90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Jeppesen P, Petersen L, Thorup A, Abel M-B, Ohlenschlaeger J, Christensen TO, et al. The association between pre-morbid adjustment, duration of untreated psychosis and outcome in first-episode psychosis. Psychological Medicine 2008;38(8):1157-66. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Madsen T, Karstoft KI, Secher RG, Austin SF, Nordentoft M. Trajectories of suicidal ideation in patients with first-episode psychosis: secondary analysis of data from the OPUS trial. Lancet Psychiatry 2016;3:443-50. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- NCT00157313. Randomised clinical trial of integrated treatment versus standard treatment in first episode psychosis. www.ClinicalTrials.gov/ct/show/ (first received 12 September 2005). [MEDLINE]
- Nordentoft M, Bertelsen M, Albert N, Jeppesen P, Petersen L, Thorup A, et al. The opus trial: A randomized multicentre single-blinded trial of specialized assertive early intervention (opus treatment) versus standard treatment for patients with a first episode of psychotic illness - five-year follow-up. Early Intervention in Psychiatry 2010;4(Suppl 1):24. [MEDLINE] [Google Scholar]
- Nordentoft M, Bertelsen M, Jeppesen P, Thorup A, Petersen L, Ohlenschlaeger J, et al. OPUS trial: a randomised multicentre trial of integrated versus standard treatment for patients with a first episode of psychotic illness. Nordic Journal of Psychiatry 2007;61(6):488. [MEDLINE] [Google Scholar]
- Nordentoft M, Bertelsen M, Thorup A, Jeppesen P, Petersen L. The opus-trial; a randomised multi-centre trial of integrated versus standard treatment for patients with a first episode of psychotic illness-five-years follow-up. In: Proceedings of the 12th International Congress on Schizophrenia Research; 2009 Mar 28-Apr 1; San Diego, CA. San Diego, CA, USA: Oxford Univ Press, 2009:370. [MEDLINE]
- Nordentoft M, Bertelsen M, Thorup A, Petersen L. Two versus 5 years of early intensive intervention in first episode psychosis. Early Intervention in Psychiatry 2008;2(Suppl 1):A7. [MEDLINE] [Google Scholar]
- Nordentoft M, Jeppesen P, Abel M, Kassow P, Petersen L, Thorup A, et al. OPUS study: suicidal behaviour, suicidal ideation and hopelessness among patients with first-episode psychosis. One-year follow-up of a randomised controlled trial. British Journal of Psychiatry. Supplements 2002;181(Suppl 43):S98-106. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Jeppesen P, Abel M, Petersen L, Thorup A, Christensen T, et al. Opus-project: a randomised controlled trial of integrated psychiatric treatment in first-episode psychosis - clinical outcome improved. In: Proceedings of the 3rd International Conference on Early Psychosis; 2002 Sep 25-28; Copenhagen, Denmark. 2002:56. [MEDLINE]
- Nordentoft M, Jeppesen P, Abel M B, Hemmingsen R, Reisby N. Can duration of untreated psychosis be shortened and does optimal treatment program improve outcome? A randomized controlled study. Nordisk Psykiatrisk Tidsskrift 1998;52(41):76. [MEDLINE] [Google Scholar]
- Nordentoft M, Jeppesen P, Jørgensen P, Abel MB, Kassow P, Reisby N, et al. OPUS - project: a randomised controlled trial of first episode psychotic patients better compliance. In: Proceedings of the 2nd International Conference on Early Psychosis; 2000 Mar 31 - Apr 2; New York, New York, USA. 2000. [MEDLINE]
- Nordentoft M, Jeppesen P, Jorgensen P, Abel M, Kassow P, Reisby N, et al. Opus-project: A randomised controlled trial of first episode psychotic patients: better compliance. Schizophrenia Research 2000;41(1):B145. [MEDLINE] [Google Scholar]
- Nordentoft M, Jeppesen P, Jorgensen P, Abel MB, Kassow P, Reisby N, et al. OPUS-project: a randomised controlled trial of first episode psychotic patients: better compliance. Nordic Journal of Psychiatry 2000;54:16. [MEDLINE] [Google Scholar]
- Nordentoft M, Jeppesen P, Kassow P, Abel M, Petersen L, Thorup A, et al. Opus-project: a randomised controlled trial of integrated psychiatric treatment in first-episode psychosis-clinical outcome improved. Schizophrenia Research 2002;53(3 Suppl 1):51. [MEDLINE] [Google Scholar]
- Nordentoft M, Jeppesen P, Kassow P, et al. OPUS project: a randomised controlled trial of integrated psychiatric treatment in first episode psychosis - clinical outcome improved. Schizophrenia Research 2002;53(Suppl. 1):51. [MEDLINE] [Google Scholar]
- Nordentoft M, Jeppesen P, Petersen L, Thorup A, Abel M, Ohlenschlaeger JK, et al. OPUS project: A randomised controlled trial of integrated psychiatric treatment in first episode psychosis. Schizophrenia Research 2003;60:297. [MEDLINE] [Google Scholar]
- Nordentoft M, Jeppesen P, Petersen L, Thorup A, Jorgensen P. Duration of untreated psychosis predicts psychotic symptoms but not negative symptoms. Schizophrenia Bulletin 2005;31:234. [MEDLINE] [Google Scholar]
- Nordentoft M, Jeppesen P, Petersen L, Thorup a, Krarup G, Abel M, et al. The Danish opus-trial: a randomised controlled trial of integrated treatment among 547 first-episode psychotic patients. One and two years follow-up. Schizophrenia Research 2004;67(1):35-6. [MEDLINE] [Google Scholar]
- Nordentoft M, Jeppesen P, Petersen L, Thorup a, Ohlenschaeger J, Christensen T, et al. Duration of untreated psychosis. Results from the opus trial. Schizophrenia Research 2004;70(1):31. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Jeppesen P, Petersen L, Thorup A, Ohlenschlaeger J, Christensen T, et al. The OPUS trial: a randomised multi-centre trial of integrated versus standard treatment for 547 first-episode psychotic patients. In: Proceedings of the 12th Biennial Winter Workshop on Schizophrenia; 2004 Feb 7-13; Davos, Switzerland. 2004. [MEDLINE]
- Nordentoft M, Jeppesen P, Petersen L, Thorup A, Ohlenschlaeger J, Christensen T, et al. Transition rates from schizotypal disorder to psychotic disorder for first-contact patients included in the opus trial. A randomized clinical trial of integrated treatment and standard treatment. European Psychiatry 2007;22:S129-S. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Jeppesen P, Ventegodt AT, Joergensen P, Abel M, Petersen L, et al. Opus-project: a randomised controlled trial of first episode psychotic patients: patient satisfaction, depression and suicidal behaviour. Schizophrenia Research 2001;49(1-2):265. [MEDLINE] [Google Scholar]
- Nordentoft M, Jorgensen P, Jeppesen P, Kassow P, Abel MB, Resiby N, et al. Opus-project: differences in clinical and social outcome of a randomized controlled trial of integrated care of first-episode psychotic patients. Schizophrenia Research 1999;36(1-3):330. [MEDLINE] [Google Scholar]
- Nordentoft M, Melau M, Iversen T, Petersen L, Jeppesen P, Thorup A, et al. From research to practice: How OPUS treatment was accepted and implemented throughout Denmark. Early Intervention in Psychiatry 2015;9(2):156-62. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Melau M, Jeppesen P, Petersen L, Thorup A, Ohlenschlager J, et al. The OPUS - trial; a randomised single-blinded trial of integrated versus standard treatment for patients with a first episode of psychotic illness - results of five-years follow-up and presentation of a new trial. Schizophrenia Research 2010;117(2-3):116. [MEDLINE] [Google Scholar]
- Nordentoft M, Ohlenschlaeger J, Thorup A, Petersen L, Jeppesen P, Bertelsen M. Deinstitutionalization revisited: A 5-year follow-up of a randomized clinical trial of hospital-based rehabilitation versus specialized assertive intervention (opus) versus standard treatment for patients with first-episode schizophrenia spectrum disorders. Psychological Medicine 2010;40(10):1619-26. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Petersen L, Jeppesen P, Thorup AAE, Abel MB, Ohlenschlaeger J, et al. OPUS: a randomized, multicenter clinical trial of integrated treatment compared with standard treatment before the first episode psychosis - secondary publication. Ugeskrift for Laeger 2006;168(4):381-4. [MEDLINE] [PubMed] [Google Scholar]
- Nordentoft M, Reisby N, Jeppesen P, Abel M-B, Kassow P, Jírgensen P. Opus-project: differences in treatment outcome of a randomised controlled trial of integrated psychiatric treatment of first-episode psychotic patients. In: Proceedings of the 11th World Congress of Psychiatry; 1999 Aug 6-11; Hamburg, Germany. Vol. 2. 1999:165. [MEDLINE]
- Nordentoft M, Secher G, Bertelsen M, Thorup A, Austin S, Albert N, et al. Opus: Concept and recent findings. European Archives of Psychiatry and Clinical Neuroscience 2011;261:S37-S8. [MEDLINE] [Google Scholar]
- Nordentoft M, Secher G, Hjorthoj CR, Austin S, Thorup A, Jeppesen P, et al. Ten-year follow-up of the OPUS specialized early intervention trial for patients with a first episode of psychosis. Schizophrenia Bulletin 2015;41:S149. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordentoft M, Thorup A, Petersen L, Jeppesen P, Krarup G, Christensen T, et al. The opus trial: A randomised multi-centre trial of integrated versus standard treatment for 547 first-episode psychotic patients. In: Proceedings of the 13th Biennial Winter Workshop on Schizophrenia Research; 2006 Feb 4-10; Davos, Switzerland. Davos, Switzerland: Elsevier Science Bv, 2006:8. [MEDLINE]
- Nordentoft M, Thorup A, Petersen L, Ohlenschlaeger J, Melau M, Christensen TO, et al. Transition rates from schizotypal disorder to psychotic disorder for first-contact patients included in the OPUS trial. A randomized clinical trial of integrated treatment and standard treatment. Schizophrenia Research 2006;83(1):29-40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Thorup A, Petersen L, Ohlenschlaeger J, Melau M, Christensen TO, et al. Transition rates from schizotypal disorder to psychotic disorder for first-contact patients included in the opus trial. A randomized clinical trial of integrated treatment and standard treatment. Schizophrenia Research 2006;86(Suppl 1):S44. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Nugent KL, Mortensen PB, Nordentoft M. Investigation of how known risk factors for schizophrenia incidence impart risk for specific schizophrenia subtypes. Schizophrenia Bulletin 2011;37:59. [MEDLINE] [Google Scholar]
- Ohlenschlaeger J, Nordentoft M, Køster A, Poulsen HD, Bredkjær S. Effect of person continuity on the use of coercion: the Danish opus-project. Schizophrenia Research 2002;53(3 Suppl 1):52. [MEDLINE] [Google Scholar]
- Ohlenschlaeger J, Nordentoft M, Thorup A, Jeppesen P, Petersen L, Christensen TO, et al. Effect of integrated treatment on the use of coercive measures in first-episode schizophrenia-spectrum disorder. A randomized clinical trial. International Journal of Law and Psychiatry 2008;31(1):72-6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Ohlenschlaeger J, Thorup A, Petersen L, Jeppesen P, Koster A, Munkner R, et al. Intensive treatment models and coercion. Nordic Journal of Psychiatry 2007;61(5):369-78. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- *.Petersen L, Jeppesen P, Thorup A, Abel MB, Ohlenschlaeger J, Christensen TO, et al. A randomised multicentre trial of integrated versus standard treatment for patients with a first episode of psychotic illness. BMJ 2005;331(7517):602-8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen L, Jeppesen P, Thorup A, Ohlenschlaeger J, Christensen T, Krarup G, et al. Substance abuse in first-episode schizophrenia-spectrum disorders. Schizophrenia Research 2006;86(Suppl 1):S44. [MEDLINE] [Google Scholar]
- Petersen L, Jeppesen P, Thorup A, Ohlenschlaeger J, Krarup G, Ostergard T, et al. Substance abuse and first-episode schizophrenia-spectrum disorders The Danish OPUS trial. Early Intervention in Psychiatry 2007;1(1):88-96. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Petersen L, Jeppesen P, Ventegodt AT, Abel M, Nordentoft M, Kassow P, et al. Opus-project: a randomised controlled trial of first episode psychotic patients: predictors of outcome. Schizophrenia Research 2001;49(1-2):266. [MEDLINE] [Google Scholar]
- Petersen L, Nordentoft M, Bertelsen M, Thorup A. Does cannabis abuse determine outcome among patients with first episode psychosis. Results from the opus-trial. Schizophrenia Bulletin 2007;33(2):453. [MEDLINE] [Google Scholar]
- Petersen L, Nordentoft M, Jeppesen P, Ohlenschaeger J, Thorup A, Christensen TO, et al. Improving 1-year outcome in first-episode psychosis: OPUS trial. British Journal of Psychiatry 2005;48(Suppl):s98-103. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Petersen L, Nordentoft M, Thorup A, Oehlenschlaeger J, Jeppesen P, Christensen T, et al. The OPUS trial: a randomised multi - centre trial of integrated versus standard treatment for 547 first-episode psychotic patients. Schizophrenia Bulletin 2005;31:531. [MEDLINE] [Google Scholar]
- Petersen L, Thorup a, Jeppesen P, Ohlenschaeger J, Krarup G, Christensen T, et al. Predictors of poor outcome. The opus-trial. Schizophrenia Research 2004;70(1):32. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Secher RG, Austin SF, Ole Mors NP, Nordentoft M. The opus-trial: Intensive, early, psycho-social intervention versus treatment as usual for first-episode psychosis patients. Results from the 10-year follow-up. European Archives of Psychiatry and Clinical Neuroscience 2011;261:S59. [MEDLINE] [Google Scholar]
- Secher RG, Hjorthoj CR, Austin SF, Thorup A, Jeppesen P, Mors O, et al. Ten-year follow-up of the OPUS specialized early intervention trial for patients with a first episode of psychosis. Schizophrenia Bulletin 2015;41(3):617-26. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secher RG, Nordentoft M, Austin S, Mors O. The opus trial: Intensive, early, psychosocial intervention versus treatment as usual for people with a first episode within the schizophrenic spectrum. Results from the 10-year follow-up. Early Intervention in Psychiatry 2012;6:21. [MEDLINE] [Google Scholar]
- Stevens H, Agerbo E, Dean K, Mortensen PB, Nordentoft M. Reduction of crime in first-onset psychosis: a secondary analysis of the OPUS randomized trial. Journal of Clinical Psychiatry 2013;74(5):e439-44. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Thorup A, Albert N, Bertelsen M, Petersen L, Jeppesen P, Le Quack P, et al. Gender differences in first-episode psychosis at 5-year follow-up -- two different courses of disease? Results from the OPUS study at 5-year follow-up. European Psychiatry 2013;29(1):44-51. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Thorup A, Albert N, Mette B, Petersen L, Jeppesen P, Le Quarck P, et al. Gender differences in first episode psychosis at 5-year follow-up: Two different courses of disease? European Archives of Psychiatry and Clinical Neuroscience 2013;263(Suppl. 1):S62. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Thorup A, Nordentoft M, Petersen L, Oehlensschlaeger J, Abel M, Jeppesen P, et al. The Danish OPUS-project: psychopathology and gender differences in first episode psychotic patients. In: Proceedings of the 3rd International Conference on Early Psychosis; 2002 Sep 25-28; Copenhagen, Denmark. 2002:59. [MEDLINE]
- Thorup A, Petersen L, Jeppesen P, Christensen T, Nordentoft M. The OPUS trial: gender differences in a sample of 547 first-episode psychotic patients. Schizophrenia Bulletin 2005;31:505. [MEDLINE] [Google Scholar]
- Thorup A, Petersen L, Jeppesen P, Nordentoft M. The quality of life among first-episode psychotic patients in the opus trial. Schizophrenia Research 2010;116(1):27-34. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Thorup A, Petersen L, Jeppesen P, Ohlenschlaeger J, Christensen T, Krarup G, et al. Integrated treatment ameliorates negative symptoms in first episode psychosis-results from the Danish OPUS trial. Schizophrenia Research 2005;79(1):95-105. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Thorup A, Petersen L, Jeppesen P, Ohlenschlaeger J, Christensen T, Krarup G, et al. Social network among young adults with first-episode schizophrenia spectrum disorders: results from the Danish OPUS trial. Social Psychiatry and Psychiatric Epidemiology 2006;41(10):761-70. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Thorup A. Gender differences in first-episode psychosis at five-year follow up - results from the Danish OPUS study gender differences have been found. Early Intervention in Psychiatry 2010;4(Suppl 1):53. [MEDLINE] [Google Scholar]
- Thorup A. The influence of social network, dup, age, gender and treatment on negative symptoms in first-episode psychosis. Schizophrenia Research 2004;70(1):89-90. [MEDLINE] [Google Scholar]
- Ventegodt AT, Jeppesen P, Petersen L, Abel M, Nordentoft M, Kassow P, et al. Opus-project: a randomised controlled trial of first episode psychotic patients: gender differences, social network and negative symptoms. Schizophrenia Research 2001;49(1-2):267. [MEDLINE] [Google Scholar]
- Vesterager L, Nordentoft M, Christensen T. Cognitive training integrated in opus treatment of patients with first episode schizophrenia. Schizophrenia Bulletin 2007;33(2):464. [MEDLINE] [Google Scholar]
OTP {published data only}
- *.Grawe RW, Falloon IR, Widen JH, Skogvoll E. Two years of continued early treatment for recent-onset schizophrenia: a randomised controlled study. Acta Psychiatrica Scandinavica 2006;114(5):328-36. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Grawe RW, Widen JH. Result of two years optimal out-patient treatment of first episode schizophrenia: a controlled study. Nordisk Psykiatrisk Tidsskrift 1998;52(41):76. [MEDLINE] [Google Scholar]
- Morken G, Grawe RW, Widen JH. A randomized controlled trial in recent-onset schizophrenia. Effects on compliance of two years of continued intervention. European Neuropsychopharmacology 2005;15(Suppl 3):S521. [MEDLINE] [Google Scholar]
- Morken G, Grawe RW, Widen JH. Effects of integrated treatment on antipsychotic medication adherence in a randomized trial in recent-onset schizophrenia. Journal of Clinical Psychiatry 2007;68(4):566-71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Morken G, Wide J, Grawe R. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry 2008;8(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00184509. Continued early intervention for recent-onset schizophrenia. A randomized controlled study. www.ClinicalTrials.gov/ct/show/NCT00184509 (first received 16 September 2005). [MEDLINE]
- Sigrunarson V, Grawe RW, Lydersen S, Morken G. Predictors of long term use of psychiatric services of patients with recent-onset schizophrenia: 12 years follow-up. BMC psychiatry 2017;17(1):18. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigrunarson V, Grawe RW, Morken G. Integrated treatment vs. treatment-as-usual for recent onset schizophrenia; 12 year follow-up on a randomized controlled trial. BMC Psychiatry 2013;13:200. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
RAISE {published data only}
- Alcover KC, Oluwoye O, Kriegal L, McPherson S, McDonell MG. Impact of first episode psychosis treatment on heavy cannabis use: Secondary analysis on RAISE-ETP study. Schizophrenia Research 2019;211:86-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azorin JM, Adida M, Belzeaux R, Fakra E. A model of care for first-episode psychosis: the RAISE-ETP project. L'Encephale 2016;42(Suppl 3):S13-7. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Brown B, Alphs L, Turkoz I, Yue Y. Baseline demographics and characteristics from a paliperidone palmitate study in subjects with recent-onset schizophrenia or schizophreniform disorder. Psychopharmacology Bulletin 2017;47(3):8-16. [MEDLINE] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Brunette MF. Facilitators and barriers to implementation of coordinated specialty care in US community mental health clinic. Schizophrenia Bulletin 2015;41:S304. [MEDLINE] [Google Scholar]
- Cadenhead K, Addington J, Bearden C, Cannon T, Cornblatt B, Mathalon D, et al. Metabolic abnormalities prior to the onset of psychosis: another risk factor for psychosis? Neuropsychopharmacology 2015;40:S565. [MEDLINE] [Google Scholar]
- Correll CU, Robinson DG, Schooler NR, Brunette MF, Mueser KT, Rosenheck RA, et al. Cardiometabolic risk in patients with first-episode schizophrenia spectrum disorders: baseline results from the RAISE-ETP study. JAMA Psychiatry 2014;71(12):1350-63. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Glynn S, Gingerich S, Meyer-Kalos P, Mueser K, Chan-Golston A, Sugar C, et al. Who participated in family work in the us raise-ETP first episode sample? Schizophrenia Bulletin 2018;44(Suppl. 1):S216-7. [MEDLINE] [Google Scholar]
- Glynn SM, Gingerich S, Mueser KT, Cather C, Penn D. The role of family intervention in coordinated specialty care for first episode psychosis. Schizophrenia Bulletin 2015;41:S173. [MEDLINE] [Google Scholar]
- Kane J, Schooler N, Robinson D, Addington J, Kane JM. The NIMH RAISE ETP (Early Treatment Program): Initial results. Early Intervention in Psychiatry 2014;8:1. [MEDLINE] [Google Scholar]
- *.Kane JM, Robinson DG, Schooler NR, Mueser KT, Penn DL, Rosenheck RA, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE Early Treatment Program. American Journal of Psychiatry 2016;173:362-72. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane JM, Schooler NR, Marcy P, Correll CU, Brunette MF, Mueser KT, et al. The RAISE Early Treatment Program for first-episode psychosis: background, rationale, and study design. Journal of Clinical Psychiatry 2015;76(3):240-6. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane JM. RAISE-ETP: Navigate vs usual care-two year outcomes. Schizophrenia Bulletin 2015;41:S317. [MEDLINE] [Google Scholar]
- Kane JM. The RAISE ETP study: initial results. Early Intervention in Psychiatry 2014;8:2. [MEDLINE] [Google Scholar]
- Mueser KT, Penn DL, Addington J, Brunette MF, Gingerich S, Glynn SM, et al. The NAVIGATE program for first-episode psychosis: rationale, overview, and description of psychosocial components. Psychiatric Services 2015;66(7):680-90. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueser KT. Description and implementation of the RAISE-ETP study psychosocial treatment model: the navigate program. Schizophrenia Bulletin 2015;41:S325-6. [MEDLINE] [Google Scholar]
- Robinson DG, Schooler NR, Correll CU, John M, Kurian BT, Marcy P, et al. Psychopharmacological treatment in the RAISE-ETP study: outcomes of a manual and computer decision support system based intervention. American Journal of Psychiatry 2018;175(2):169-79. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson DG, Schooler NR, John M, Correll CU, Marcy P, Addington J, et al. Prescription practices in the treatment of first-episode schizophrenia spectrum disorders: data from the national RAISE-ETP study. American Journal of Psychiatry 2015;172(3):237-48. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson DG, Schooler NR, Rosenheck RA, Lin H, Sint K, Marcy P et al. Predictors of hospitalization of individuals with first-episode psychosis: data from a 2-year follow-up of the RAISE-ETP. Psychiatric Services 2019;70:569-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson DG. Randomized comparison of comprehensive versus usual community care for first-episode psychosis: the RAISE-ETP study. Journal of the American Academy of Child and Adolescent Psychiatry 2017;56(10):S340. [MEDLINE] [Google Scholar]
- Rosenheck R, Leslie D, Sint K, Lin H, Robinson DG, Schooler NR, et al. Cost-effectiveness of comprehensive, integrated care for first episode psychosis in the NIMH RAISE Early Treatment Program. Schizophrenia Bulletin 2016;42:896-906. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenheck R, Mueser KT, Sint K, Lin H, Lynde DW, Glynn SM, et al. Supported employment and education in comprehensive, integrated care for first episode psychosis: Effects on work, school, and disability income. Schizophrenia Research 2017;182:120-8. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Rosenheck RA, Estroff SE, Sint K, Lin H, Mueser KT, Robinson DG, et al. Incomes and outcomes: Social Security Disability Benefits in first-episode psychosis. American Journal of Psychiatry 2017;174(9):886-94. [MEDLINE] [DOI] [PubMed] [Google Scholar]
- Schooler N, Khan A, Keefe R, Marcy P, Robinson D, Kane J. Cognitive functioning in first episode psychosis: Comparison of a two-year coordinated specialty care program to community care. Neuropsychopharmacology 2016;41:S593. [MEDLINE] [Google Scholar]
- Schooler N, Khan A, Keefe R, Robinson D, Kane J. Cognitive functioning in first-episode psychosis:-X000B- Comparison of a 2-year coordinated specialty care program to community care. Schizophrenia Bulletin 2017;43:S24. [MEDLINE] [Google Scholar]
- Schooler N. RAISE-ETP study design, site selection and implementation model. Early Intervention in Psychiatry 2014;8:1. [MEDLINE] [Google Scholar]
- Schooler NR. The RAISE-ETP study design, research and implementation model. Schizophrenia Bulletin 2015;41:S332-3. [MEDLINE] [Google Scholar]
- Sint K, Rosenheck R, Robinson DG, Schooler NR, Marcy P, Kane JM, et al. Accounting for group differences in study retention in a randomized trial of specialized treatment for first episode psychosis. Schizophrenia Research 2018;195:481-7. [MEDLINE] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Alaghband‐Rad 2006 {published data only}
- *.Alaghband-Rad J, Shahrivar Z, Mahmoodi J, Salesian N. First episode psychoses among Iranian adolescents. Schizophrenia Research 2006;86(Suppl 1):S65. [Google Scholar]
- Alaghband-Rad J, Shahrivar Z, Mahmoudi-gharaei J, Sharifi V, Amini H, Mottaghipour Y, et al. Integrated vs usual treatment model in first episode - psychosis among Iranian adolescents. Early Intervention in Psychiatry 2008;2(Suppl 1):A92. [Google Scholar]
- Alaghband-Rad J, Sharifi V, Amini H, Shahrivar Z, Mottaghipour Y, Mahmoodi J, et al. Management of first episode psychoses in Iran: unique features and challenges. Schizophrenia Research 2006;86(Suppl 1):S42. [Google Scholar]
Cai 2013 {published data only}
- Cai C. Comparison of different treatment methods affect the quality of life of patients with first-episode schizophrenia. Journal of Medical Theory and Practice 2013;26(3):341-2. [Google Scholar]
Carpenter 1982 {published data only}
- Carpenter WT, Stephens JH, Rey AC. Early intervention vs. continuous pharmacotherapy of schizophrenia. Psychopharmacology Bulletin 1982;18(1):21-3. [Google Scholar]
Cechnicki 2017 {published data only}
- Cechnicki A, Bielanska A. The influence of early psychosocial intervention on the long-term clinical outcomes of people suffering from schizophrenia. Psychiatria Polska 2017;51(1):45-61. [DOI] [PubMed] [Google Scholar]
Chen 2013 {published data only}
- Chen L. Application of comprehensive nursing intervention in first-episode schizophrenia patients. China Contemporary Medicine 2013;7(20):156-7. [Google Scholar]
COAST 2004 {published data only}
- Kuipers E, Holloway F, Rabe-Hesketh S, Tennakoon L. An RCT of early intervention in psychosis: Croydon Outreach and Assertive Support Team (COAST). Social Psychiatry and Psychiatric Epidemiology 2004;39(5):358-63. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Dai 2007 {published data only}
- Dai M, Liu F, Fan J. A study on influence of early comprehensive interventions on prognosis of incipient schizophrenia patients. Chinese Nursing Research 2007;21(9B):2393-4. [Google Scholar]
EASY_Extended {published data only}
- Chan GH, Jim OT, AuYang CW, Hui CL, Wong GH, Lam MM, et al. Effects of extended case management on functioning in people with early psychosis-preliminary findings of the EASY3 randomised controlled study. Schizophrenia Research 2012;136:S176. [Google Scholar]
- *.Chang WC, Chan GH, Jim OT, Lau ES, Hui CL, Chan SK, et al. Optimal duration of an early intervention programme for first-episode psychosis: randomised controlled trial. British Journal of Psychiatry 2015;206(6):492-500. [DOI] [PubMed] [Google Scholar]
- Chang WC, Chan HK, Jim TT, Wong HY, Hui LM, Chan KW, et al. Randomized controlled trial evaluating 1-year extended case management for first-episode psychosis patients discharged from EASY program in Hong Kong. Schizophrenia Bulletin 2013;39:S324-5. [Google Scholar]
- Chang WC, Kwong VW, Chan GH, Jim OT, Lau ES, Hui CL, et al. Prediction of functional remission in first-episode psychosis: 12-month follow-up of the randomized-controlled trial on extended early intervention in Hong Kong. Schizophrenia Research 2016;173:79-83. [DOI] [PubMed] [Google Scholar]
- Chang WC, Kwong VW, Chan GH, Jim OT, Lau ES, Hui CL, et al. Prediction of motivational impairment: 12-month follow-up of the randomized-controlled trial on extended early intervention for first-episode psychosis. European Psychiatry 2017;41:37-41. [DOI] [PubMed] [Google Scholar]
- Chang WC, Kwong VW, Lau ES, So HC, Wong CS, Chan GH, et al. Sustainability of treatment effect of a 3-year early intervention programme for first-episode psychosis. British Journal of Psychiatry 2017;211(1):37-44. [DOI] [PubMed] [Google Scholar]
- Chang WC, Kwong VW, OR Chi Fai P, Lau ES, Chan GH, Jim OT, et al. Motivational impairment predicts functional remission in first-episode psychosis: 3-Year follow-up of the randomized controlled trial on extended early intervention. Australian and New Zealand Journal of Psychiatry 2018;52(12):1194-201. [DOI] [PubMed] [Google Scholar]
- Chen EY, Chang WC, Chan SK, Lam MM, Hung SF, Chung DW, et al. Three-year community case management for early psychosis: a randomised controlled study. Hong Kong Medical Journal 2015;21 Suppl. 2:23-6. [PubMed] [Google Scholar]
- HKCTR-1001. Community case management for early psychosis: is two year an optimal duration? A randomized controlled study. www.hkClinicaltrials.com/trial_details.aspx?trialID=abe8d577-1d54-466a-9d41-28498efe70c6 (first received 2009).
- Ho RW, Chang WC, Kwong VW, Lau ES, Chan GH, Jim OT, et al. Prediction of self-stigma in early psychosis: 3-Year follow-up of the randomized-controlled trial on extended early intervention. Schizophrenia Research 2017;195:463-8. [DOI] [PubMed] [Google Scholar]
- Kwong VW, Chang WC, Chan GH, Jim OT, Lau ES, Hui CL, et al. Clinical and treatment-related determinants of subjective quality of life in patients with first-episode psychosis. Psychiatry Research 2017;249:39-45. [DOI] [PubMed] [Google Scholar]
- NCT01202357. Optimal duration of early intervention for psychosis. www.ClinicalTrials.gov/ct/show/NCT01202357 (first received 15 September 2010.
Fan 2005c {published data only}
- Fan X-H. The effects of community nursing intervention on the recovery of patients with primary schizophrenia. Journal of the Linyi Medical College 2005;27(6):419-21.
GET UP PIANO 2013 {published data only}
- Lasalvia A, Bonetto C, Lenzi J, Rucci P, Iozzino L, Cellini M, et al. Predictors and moderators of treatment outcome in patients receiving multi-element psychosocial intervention for early psychosis: results from the GET UP pragmatic cluster randomised controlled trial. British Journal of Psychiatry 2017;210(5):342-9. [DOI] [PubMed] [Google Scholar]
- Lenzi J, Iozzino L, De Girolamo G, Rucci P, Tosato S, Lasalvia A, et al. Predictors of 9-month hospitalization in patients with first-episode affective and non-affective psychosis. Results from the GET UP pragmatic cluster randomized controlled trial. Schizophrenia Research 2017;190:187-8. [DOI] [PubMed] [Google Scholar]
- NCT01436331. A large pragmatic cluster randomized controlled trial of a multi-element psychosocial intervention for early psychosis. ClinicalTrials.gov/show/NCT01436331 (first received 19 September 2011).
- Ruggeri M, Bonetto C, Lasalvia A, De Girolamo G, Fioritti A, Rucci P, et al. A multi-element psychosocial intervention for early psychosis (get up piano trial) conducted in a catchment area of 10 million inhabitants: Study protocol for a pragmatic cluster randomized controlled trial. Trials 2012;13(1):73. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ruggeri M, Bonetto C, Lasalvia A, Fioritti A, Girolamo G, Santonastaso P, et al. Feasibility and effectiveness of a multi-element psychosocial intervention for first-episode psychosis: results from the cluster-randomized controlled GET UP PIANO trial in a catchment area of 10 million inhabitants. Schizophrenia Bulletin 2015;41(5):1192-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggeri M, Lasalvia A, Santonastaso P, Pileggi F, Leuci E, Miceli M, et al. Family burden, emotional distress and service satisfaction in first episode psychosis. Data from the GET UP Trial. Frontiers in Psychology 2017;8:721. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hansen 2012 {published data only}
- *.Hansen JP, Ostergaard B, Nordentoft M, Hounsgaard L. Cognitive adaptation training combined with assertive community treatment: A randomised longitudinal trial. Schizophrenia Research 2012;135(1-3):105-11. [DOI] [PubMed] [Google Scholar]
- Hansen JP, Ostergaard B, Nordentoft M, Hounsgaard L. Cognitive adaptation training in an assertive community treatment setting for outpatients with schizophrenia. European Psychiatry 2013;28(Suppl. 1):1. [Google Scholar]
- Hansen J P, Ostergaard B, Nordentoft M, Hounsgaard L. The feasibility of cognitive adaptation training for outpatients with schizophrenia in integrated treatment. Community Mental Health Journal 2013;49(6):630-5. [DOI] [PubMed] [Google Scholar]
Hou 2007 {published data only}
- Hou D-Q, Zeng Z-X, Wang H-Y. Effect of insight education and self-confidence training on the quality of life and well-being rating in first episode schizophrenia. Chinese Journal of Rehabilitation Theory and Practice 2007;13(5):479-81. [Google Scholar]
ISRCTN58681229 {published data only}
- *.ISRCTN58681229. Cluster randomised trial comparing outcomes of early psychosis care by a specialist team and augmented community mental health teams (CMHTs). www.isrctn.com/ISRCTN58681229 (first received 31 January 2005).
- Johnson S, Hinton M, Pilling S, Bebbington P, Hobbs L, Cohen S. Strategies for implementation of early intervention for psychosis in a catchment area mental health system: A mixed methods comparison. Psychiatrische Praxis 2011;38:OP15_EC. [Google Scholar]
J‐CAP 2014 {published data only}
- *.Ando S, Nishida A, Koike S, Yamasaki S, Maegawa S, Ichihashi K, et al. Comprehensive early intervention for patients with first-episode psychosis in Japan (J-CAP): nine-month follow-up of randomized controlled trial. Early Intervention in Psychiatry 2014;8:82. [Google Scholar]
- Koike S, Nishida A, Yamasaki S, Ichihashi K, Maegawa S, Natsubori T, et al. Comprehensive early intervention for patients with first-episode psychosis in japan (J-CAP): study protocol for a randomised controlled trial. Trials 2011;12:156. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishida A, Ando S, Yamasaki S, Koike S, Ichihashi K, Miyakoshi Y, et al. A randomized controlled trial of comprehensive early intervention care in patients with first-episode psychosis in Japan: 1.5-year outcomes from the J-CAP study. Journal of Psychiatric Research 2018;102:136-41. [DOI] [PubMed] [Google Scholar]
- Nishida A, Koike S, Yamasaki S, Ando S, Nakamura T, Harima H, et al. Comprehensive early intervention for patients with first-episode psychosis in Japan (J-CAP): Study protocol for a randomised controlled trial. Early Intervention in Psychiatry 2012;6:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
LEO‐CAT 2004 {published data only}
- *.Power P, Craig T, Mcguire P, Iacoponi E, Garety P, Russell M. A randomised controlled trial of an early detection team in first episode psychosis: the LEO CAT trial. Schizophrenia Research 2004;67(1):36. [Google Scholar]
- Power P, Iacoponi E, Reynolds N, Fisher H, Russell M, Garety P, et al. The Lambeth Early Onset Crisis Assessment Team Study: general practitioner education and access to an early detection team in first-episode psychosis. British Journal of Psychiatry. Supplements 2007;191(Suppl 51):s133-9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Power P, Iacoponi E, Russell M, Fisher H, Mcguire P, Garety P, et al. A randomised controlled trial of an early detection team in first- episode psychosis: provisional findings of the leo cat study. Schizophrenia Research 2004;70(1):131. [Google Scholar]
- Power P, Monteiro E, Pobee I, Burnside A, Pugh C, Reynolds N, et al. 18 months outcome of first episode psychosis patients attending the LEO service in south London. Early Intervention in Psychiatry 2008;2(Suppl 1):A6. [Google Scholar]
Li 2012a {published data only}
- Li C, Zhang S, Cao H. Application of clinical nursing pathways in the nursing of first-time hospitalized patients with schizophrenia. Chinese Journal of Modern Medicine 2012;6(14):113-5. [Google Scholar]
Li 2012b {published data only}
- Li Z. Influence of first-episode schizophrenia cognitive function by prevention and treatment of community comprehensive measures. China Contemporary Medicine 2012;19(33):164-5. [Google Scholar]
Linszen 1994 {published data only}
- Lenior ME, Dingemans PM, Schene AH, Hart AA, Linszen DH. The course of parental expressed emotion and psychotic episodes after family intervention in recent-onset schizophrenia. A longitudinal study. Schizophrenia Research 2002;57(2-3):183-90. [DOI] [PubMed] [Google Scholar]
- Linszen D, Dingemans P, Lenior M, Scholte W. Early individual and family intervention in schizophrenia. In: Proceedings of the 10th World Congress of Psychiatry; 1996 Aug 23-28; Madrid, Spain. 1996.
- Linszen D, Dingemans P, Lenior M. Early intervention and a five year follow up in young adults with a short duration of untreated psychosis: ethical implications. Schizophrenia Research 2001;51(1):55-61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Linszen D, Dingemans P, Scholte W, Lenior M, Goldstein M. Early recognition, intensive intervention and other protective and risk factors for psychotic relapse in patients with first psychotic episodes in schizophrenia. International Clinical Psychopharmacology 1998;13(Suppl 1):S7-S12. [DOI] [PubMed] [Google Scholar]
- Linszen D, Dingemans P, Van der Does JW, Nugter A, Scholte P, Lenior R, et al. Treatment, expressed emotion and relapse in recent onset schizophrenic disorders. Psychological Medicine 1996;26(2):333-42. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Linszen D, Dingemans PM, Lenior ME, Scholte WF, Goldstein M. Early family and individual interventions and relapse in recent-onset schizophrenia and related disorders. Italian Journal of Psychiatry and Behavioural Sciences 1998;8:77-84. [Google Scholar]
- *.Linszen D, Lenior M, De-Haan L, Dingemans P, Gersons B. Early intervention, untreated psychosis and the course of early schizophrenia. British Journal of Psychiatry. Supplements 1998;172(33):84-9. [MEDLINE: ] [PubMed] [Google Scholar]
- Linszen DH, Dingemans PM, Lenior ME, Nugter MA, Scholte WF, Van der Does AJ. Relapse criteria in schizophrenic disorders: different perspectives. Psychiatry Research 1994;54(3):273-81. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Linszen H, Lenior RM, Dingemans PM. Early intervention in first episode psychoses and the critical period. Schizophrenia Research 2001;49(1-2):264. [Google Scholar]
- Nugter A, Dingemans P, Van der Does JW, Linszen D, Gersons B. Family treatment, expressed emotion and relapse in recent onset schizophrenia. Psychiatry Research 1997;72(1):23-31. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Nugter MA, Dingemans PM, Linszen DH, Van der Does AJ, Gersons BP. Parental communication deviance: its stability and the effect of family treatment in recent-onset schizophrenia. Acta Psychiatrica Scandinavica 1997;95(3):199-204. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Linszen 2002 {published data only}
- Linszen DH, Dingemans PM. Early intervention in recent onset schizophrenia preliminary results. In: Proceedings of the 3rd International Conference on Early Psychosis; 2002 Sep 25-28; Copenhagen, Denmark. 2002:13.
- *.Linszen DH, Dingemans PM. Sustained intervention in recent onset schizophrenia: three year results of a controlled clinical trial. Schizophrenia Research 2002;53(3 Suppl 1):14. [Google Scholar]
Linszen 2003 {published data only}
- *.Linszen D, Wouters L, Dingemans P, De Haan L, Nieman D. Early and 3-year sustained intervention in first episode schizophrenia: relapse, stabilization and its predictors. Schizophrenia Research 2004;67(1):18. [Google Scholar]
- Linszen D. Early and critical period intervention in first episode schizophrenia: relapse, chronicity, early stabilisation, predictors over 4 years and new research. Schizophrenia Research 2004;70(1):66. [Google Scholar]
- Linszen DH, De Haan L, Dingemans P, Van Bruggen M, Hofstra N, Van Engelsdorp H, et al. Treatment reluctance in first episode schizophrenia: lack of insight, non-compliance and cannabis abuse predict bad outcome after eighteen months intervention. Schizophrenia Research 2003;60:325. [Google Scholar]
Linszen 2006 {published data only}
- Linszen D, De Haan L, Dingemans P, Lenior R, Van Amelsvoort T, Wouters L. The Amsterdam critical period intervention in the early phase of schizophrenia-like psychoses. Schizophrenia Research 2006;86(Suppl 1):S61. [Google Scholar]
Linszen 2007 {published data only}
- *.Linszen D, De Haan L, Wouters L, Dingemans P, Van Amelsvoort T, Lenior M. A five year randomized controlled trial of specialised care and parent groups vs standard care for first episode patients. Schizophrenia Bulletin 2007;33(2):442. [Google Scholar]
- Linszen D, Wouters L, Krikke M, Nieman D, Amelsvoort TV, Lenior M, et al. Continuity of treatment and supporting parent groups in early phase schizophrenia: a 5 year randomised trial. In: Proceedings of the 12th International Congress on Schizophrenia Research; 2009 Mar 28-Apr 1; San Diego, CA. San Diego, CA, USA: Oxford Univ Press, 2009:346.
Liu 2012a {published data only}
- Liu M. Curative effect observation on 60 cases of first-episode schizophrenia treated by integrated Traditional Chinese and Western medicine. Journal of Guiyang College of Traditional Chinese Medicine 2012;2(24):47-8. [Google Scholar]
Liu 2012b {published data only}
- Liu M, Zhang L, Xie Y, Tang Q, Jiang C, Lu Q, et al. Study on the rehabilitation effect of community supervision and programmed training on first-episode schizophrenia. Journal of Psychiatry 2012;3:200-3. [Google Scholar]
Malla 2000 {published data only}
- Malla A, Norman R, McLean T, Manchanda R, Townsend L, Cortese L, et al. Development of a community focussed early intervention program for psychosis: combining service, research and public education. In: Proceedings of the 2nd International Conference on Early Psychosis; 2000 Mar 31 - Apr 2; New York, New York, USA. 2000.
Malla 2017 {published data only}
- Albert N, Melau M, Jensen H, Hastrup LH, Hjorthoj C, Nordentoft M. When should early intervention start, and for how long should it last? Schizophrenia Bulletin 2018;44(Suppl. 1):S129. [Google Scholar]
- ISRCTN11889976. Comparison between extension of specialised early intervention for first episode psychosis and regular care: a randomised controlled trial. www.isrctn.com/ISRCTN11889976 (first received 20 March 2009).
- Lutgens D, Iyer S, Joober R, Brown TG, Norman R, Latimer E, et al. A five-year randomized parallel and blinded clinical trial of an extended specialized early intervention vs. regular care in the early phase of psychotic disorders: Study protocol. BMC Psychiatry 2015;15:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutgens D, Joober R, Iyer S, Lepage M, Norman R, Schmitz N, et al. Progress of negative symptoms over the initial 5 years of a first episode of psychosis. Psychological Medicine 2018;InPress:InPress. [DOI] [PubMed] [Google Scholar]
- Lutgens D, Joober R, Iyer S, Lepage M, Norman R, Schmitz N, et al. Progress of negative symptoms over the initial 5 years of a first episode of psychosis - CORRIGENDUM. Psychological medicine 2018;InPress:InPress. [DOI] [PubMed] [Google Scholar]
- Malla A, Abadi S, Joober R, Latimer E, Schmitz N, Brown T, et al. A randomized controlled evaluation of "extended specialized early intervention service" vs. "regular care" for long-term management of early psychosis: a pilot study. Early Intervention in Psychiatry 2008;2(Suppl 1):A5. [Google Scholar]
- Malla A, Abadi S, Joober R, Latimer E, Schmitz N, Brown T, et al. A randomized controlled evaluation of "extended specialized early intervention service" vs. "regular care" for long-term management of early psychosis: a pilot study. Schizophrenia Research 2010;117(2-3):115. [Google Scholar]
- Malla A, Joober R, Iyer S, Lutgens D, Abadi S. The optimal duration of early intervention services for psychosis: Two Canadian studies. European Archives of Psychiatry and Clinical Neuroscience 2015;1:S48. [Google Scholar]
- *.Malla A, Joober R, Iyer S, Norman R, Schmitz N, Brown T, et al. Comparing three-year extension of early intervention service to regular care following two years of early intervention service in first-episode psychosis: a randomized single blind clinical trial. World Psychiatry 2017;16(3):278-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malla A, Joober R, Iyer S, Schmitz N, Norman R, Brown T, et al. Challenges of altering pathways to care and length of adequate EI services: Two controlled trials from Canada. Early Intervention in Psychiatry 2014;8:10. [Google Scholar]
- Malla A, Norman R, Iyer S, Joober R, Brown T, Schmitz N, et al. Extending specialized early intervention service from 2 to 5 years: A randomized controlled trial. Early Intervention in Psychiatry 2012;6:36. [Google Scholar]
- Malla A. A pilot randomized controlled evaluation of extended specialized early intervention service vs. regular care for longterm management of early psychosis. Proceedings of the 17th European Psychiatric Association, EPA Congress; 2009 Jan 24-28; Lisbon Portugal 2009:S112.
- Rondeau MC, Iyer S, Joober R, Schmitz N, Latimer E, Brown T, et al. A randomized controlled evaluation of 'extended specialized early intervention service' vs. 'regular care' for long-term management of early psychosis. Early Intervention in Psychiatry 2010;4(Suppl 1):74. [Google Scholar]
- Rondeau MC, Rho A, Iyer S, Joober R, Schmitz N, Latimer E, et al. A randomized controlled evaluation of 'extended specialized early intervention service' vs. 'Regular care' for long-term management of early psychosis. Early Intervention in Psychiatry 2012;6:72. [Google Scholar]
NCT01783457 {published data only}
- Barbeito S, Vega P, Ruiz de Azua S, Balanza-Martinez V, Colom F, Lorente E, et al. Integrated treatment of first episode psychosis with online training (e-learning): study protocol for a randomised controlled trial. Trials 2014;15:416. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT01936220 {published data only}
- NCT01936220. Relapse prevention in first episode of schizophrenia and related psychotic disorders: a 5 year randomized controlled trial. clinicaltrials.gov/ct2/show/NCT01936220 (first received 6 September 2013).
NCT02037581 {published data only}
- Lambert M, Schottle D, Sengutta M, Ludecke D, Nawara AL, Galling B, et al. Early detection and integrated care in adolescents and young adults with severe psychotic illnesses. Psychiatrische Praxis 2015;42:S49-53. [DOI] [PubMed] [Google Scholar]
- *.NCT02037581. Integrated care in early psychosisTI - Integrated Care in Early Psychosis (ICEP Study): a 12-month quasi experimental study with historic control group. clinicaltrials.gov/show/NCT02037581 (firs received 16 January 2014).
NCT02751632 {published data only}
- *.ACTRN12616000098437. Staged Treatment in Early Psychosis (STEP): a sequential multistage randomized clinical trial (SMART) of interventions for Ultra High Risk (UHR) of psychosis patients. apps.who.int/trialsearch/Trial2.aspx?TrialID=ACTRN12616000098437 2016.
- NCT02751632. The staged treatment in early psychosis study. clinicaltrials.gov/show/NCT02751632 (first received 26 April 2016).
NCT03409393 {published data only}
- NCT03409393. Feasibility and relevance of high-intensity functional training in patients with first-episode psychosis. clinicaltrials.gov/show/NCT03409393 (first received 14 September 2018).
OPUS II {published data only}
- Albert N, Glenthoj LB, Melau M, Jensen H, Hjorthoj C, Nordentoft M. Course of illness in a sample of patients diagnosed with a schizotypal disorder and treated in a specialized early intervention setting. Findings from the 3.5year follow-up of the OPUS II study. Schizophrenia Research 2017;182:24-30. [DOI] [PubMed] [Google Scholar]
- *.Albert N, Melau M, Jensen H, Emborg C, Jepsen JR, Fagerlund B, et al. Five years of specialised early intervention versus two years of specialised early intervention followed by three years of standard treatment for patients with a first episode psychosis: randomised, superiority, parallel group trial in Denmark (OPUS II). BMJ 2017;356:i6681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert N, Melau M, Jensen H, Hastrup LH, Hjorthøj C, Nordentoft M. The effect of duration of untreated psychosis and treatment delay on the outcomes of prolonged early intervention in psychotic disorders. NPJ Schizophrenia 2017;3(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymous. Five years of specialised early intervention versus two years of specialised early intervention followed by three years of standard treatment for patients with a first episode psychosis: randomised, superiority, parallel group trial in Denmark (OPUS II). BMJ 2017;356:j1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melau M, Bertelsen M, Jeppesen P, Krarup G, Nordentoft M, Thorup A, et al. A randomised clinical trial of the effect of five-years versus two-years specialised assertive intervention for first episode psychosis - the OPUS-II trial. Schizophrenia Research 2010;117(2-3):526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melau M, Jeppesen P, Thorup A, Bertelsen M, Petersen L, Gluud C, et al. The effect of five years versus two years of specialised assertive intervention for first episode psychosis - OPUS II: Study protocol for a randomized controlled trial. Trials 2011;12:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melau M, Thorup A, Bertelsen M, Jeppesen P, Krarup G, Nordentoft M. Does extended specialized intervention for patients with first episode psychosis improve outcome in the critical period.The OPUS II trial. Schizophrenia Bulletin 2011;37:315. [Google Scholar]
- Melau M. Treatment response, working alliance and patients' perspective: Results from opus i and opus ii. Early Intervention in Psychiatry 2010;4(Suppl 1):152. [Google Scholar]
- NCT00914238. Extended specialized assertive intervention for first episode psychosis. www.ClinicalTrials.gov/ct/show/NCT00914238 (first received 4 June 2009).
- Nordentoft M, Melau M, Jeppesen P, Petersen L, Thorup A, Ohlenschlager J, et al. The OPUS - trial; a randomised single-blinded trial of integrated versus standard treatment for patients with a first episode of psychotic illness - results of five-years follow-up and presentation of a new trial. Schizophrenia Research 2010;117(2-3):116. [Google Scholar]
Pan 2012 {published data only}
- Pan S. Application of cognitive therapy in nursing care of schizophrenia with depression. Xià bànyuè bǎn 2012;7:206-7. [Google Scholar]
- *.Pan S. Application of cognitive therapy in patients with schizophrenia and depressive disorder. Qilu Nursing Journal 2015;21(18):29-30. [Google Scholar]
Qi 2006 {published data only}
- Qi G. Comprehensive intervention on the rehabilitation of the community first episode schizophrenia. Chinese Journal of Rehabilitation Medicine 2006;21(4):356-7. [Google Scholar]
Qu 2012 {published data only}
- Qu Y. Study on the efficacy and safety of clozapine combined with ziprasidone in the treatment of schizophrenia. Chugai Medical Research 2012;31:14-5. [Google Scholar]
Rosenbaum 2002 {published data only}
- *.Rosenbaum B, Valbak K, Harder S, Knudsen P, Koster A, Lajer M, et al. The Danish National Schizophrenia Project: prospective, comparative longitudinal treatment study of first-episode psychosis. British Journal of Psychiatry 2005;186:394-9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Rosenbaum B, Valbak K, Lajer M, Harder S, Knudsen P, Køster A, et al. The Danish National Schizophrenia Project: background, design and baseline data. In: Proceedings of the 3rd International Conference on Early Psychosis; 2002 Sep 25-28; Copenhagen, Denmark. 2002:65.
Santos 2008 {published data only}
- Santos L, Gago J, Levy P, Mateus P, Robalo P, Ferreira R, et al. Cognitive-behavioural case management in first-episode schizophrenia and related psychotic disorders - the Portuguese experience. Early Intervention in Psychiatry 2008;2(Suppl 1):A21. [Google Scholar]
Sharivar 2010 {published data only}
- Shahrivar Z, Alaghband-Rad J, Gharaie JM, Seddigh A, Salesian N, Roodsari MJ, et al. The efficacy of an integrated treatment in comparison with treatment as usual in a group of children and adolescents with first-episode psychosis during a two -year follow-up. Iranian Journal of Psychiatry and Clinical Psychology 2012;18(2):124-7. [Google Scholar]
- *.Shahrivar Z, Alaghband-Rad J, Mahmoudi-Gharaei J, Sharifi V, Amini H, Roudsari MJ, et al. Integrated standard program in comparison to the usual treatment in adolescents with first episode psychosis: A randomized clinical trial. Early Intervention in Psychiatry 2010;4(Suppl 1):143. [Google Scholar]
- Shahrivar Z, Alaghband-Rad J, Mahmoudi Gharaie J, Seddigh A, Salesian N, Jalali Roodsari M, et al. The efficacy of an integrated treatment in comparison with treatment as usual in a group of youths with first-episode psychosis. Neuropsychiatrie de L'Enfance et de L'Adolescence 2012;60:S284-5. [Google Scholar]
- Sharifi V, Alaghband-rad J, Amini H, Mottaghipour Y, Jalali M, Seddigh A, et al. Towards models for aftercare of patients with a first episode of psychosis in Iran as a developing country. Schizophrenia Research 2006;86(Suppl 1):S164-5. [Google Scholar]
- Sharifi V, Alaghband-rad J, Mottaghipour Y, Shahrivar Z, Amini H, Mahmoudi-gharaei J, et al. Effectiveness of specialized services for first-episode psychosis in Iran: a 12-month randomized controlled trial. Early Intervention in Psychiatry 2008;2(Suppl 1):A30. [Google Scholar]
Sheng 2009 {published data only}
- Sheng WU. Effect of bio-psychosocial intervention on first-episode schizophrenia patients. Chongqing Medical Journal 2009;38(6):665-6.
STEP 2012 {published data only}
- NCT00309452. Randomized trial of usual care versus specialized, phase-specific care in the public sector for first episode psychosis. clinicaltrials.gov/ct2/show/NCT00309452 (first received 31 March 2006).
- Srihari V, Phutane V, Breitborde N, Tek C, Woods S. Early intervention for psychosis in the U.S. Public sector: a pragmatic randomized controlled trial. Early Intervention in Psychiatry 2012;6:106. [Google Scholar]
- Srihari V. Developing early intervention service for the us public sector: the STEP clinic. Early Intervention in Psychiatry 2012;6:17. [Google Scholar]
- *.Srihari VH, Tek C, Kucukgoncu S, Phutane VH, Breitborde NJ, Pollard J, et al. First-episode services for psychotic disorders in the U.S. public sector: a pragmatic randomized controlled trial. Psychiatric Services 2015;66(7):705-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srihari VH, Woods SW, Walsh B, Saksa JR, Pollard J, Hyman L, et al. Specialized Treatment Early in Psychosis (STEP): a pragmatic randomized controlled trial in the US public sector. Schizophrenia Research 2006;86(Suppl 1):S165. [Google Scholar]
- Woods SW, Srihari VH, Breitborde NJ, Saksa JK, McGlashan TH. STEP: Pragmatic randomized pilot trial of integrated treatment for first episode psychosis vs usual care in the United States. In: Proceedings of the 12th International Congress on Schizophrenia Research; 2009 Mar 28-Apr 1; San Diego, CA. San Diego, CA, USA: Oxford Univ Press, 2009:129-30.
Sun 2010 {published data only}
- Sun X, Li Z. Multi-disciplinary rehabilitation team of discharged patients with schizophrenia relapse prevention. Journal of Qilu Nursing 2010;16(25):13-5. [Google Scholar]
Tang 2012 {published data only}
- Tang X. The influence of open management training on patients with schizophrenia. Qilu Nursing Journal 2012;25:46-7. [Google Scholar]
Valencia 2010 {published data only}
- Valencia M, Luisa Rascon M, Juarez F, Escamilla R, Saracco R, Liberman RP. Application in Mexico of psychosocial rehabilitation with schizophrenia patients. Psychiatry 2010;73(3):248-63. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Valencia 2012 {published data only}
- Valencia M, Juarez F, Ortega H. Integrated treatment to achieve functional recovery for first-episode psychosis. Schizophrenia Research and Treatment 2012 May 10 [Epub ahead of print]. [DOI: 10.1155/2012/962371] [DOI] [PMC free article] [PubMed]
Valencia 2013 {published data only}
- Valencia M, Fresan A, Juarez F, Escamilla R, Saracco R. The beneficial effects of combining pharmacological and psychosocial treatment on remission and functional outcome in outpatients with schizophrenia. Journal of Psychiatric Research 2013;47(12):1886-92. [DOI] [PubMed] [Google Scholar]
Wan 2012 {published data only}
- Wan X. A comparative study of risperidone and olanzapine in the treatment of first-episode schizophrenia. Modern Diagnosis and Treatment 2012;6:627-8. [Google Scholar]
Wang 2012 {published data only}
- Wang J. The role of nursing intervention in the prevention of recurrence of schizophrenia. Chinese New Clinical Medicine 2012;5(7):650-1. [Google Scholar]
Zhang 2009 {published data only}
- Zhang R, Shen L, Xia J. Family nursing intervention of first-episode schizophrenia patients. Chinese Nursing Research 2009;23(2A):370-1. [Google Scholar]
Zipursky 2004 {published data only}
- Zipursky R. Home-based versus clinic-based care for first-episode psychosis: findings from the pilot phase of a randomized clinical trial. Schizophrenia Research 2004;70(1):16. [Google Scholar]
References to ongoing studies
JCEP 2010 {published data only}
- Hui CL, Chang WC, Chan SK, Lee EH, Tam WW, Lai DC, et al. Early intervention and evaluation for adult-onset psychosis: the JCEP study rationale and design. Early Intervention in Psychiatry 2014;8(3):261-8. [DOI] [PubMed] [Google Scholar]
- Hui CL, Lau WWY, Leung CM, Chang WC, Tang JYM, Wong GH, et al. Clinical and social correlates of duration of untreated psychosis among adult-onset psychosis in Hong Kong Chinese: The JCEP study. Early Intervention in Psychiatry 2015;9(2):118-25. [DOI] [PubMed] [Google Scholar]
- *.NCT00919620. Stage-specific case management for early psychosis. www.clinicaltrials.gov/ct/show/NCT00919620 (first received 12 June 2009).
Additional references
Addington 1993
- Addington D, Addington J, Matickatyndale E. Assessing depression in schizophrenia: the Calgary Depression Scale. British Journal of Psychiatry 1993;163(Suppl):39-44. [PubMed] [Google Scholar]
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313(7066):1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andreasen 1984
- Andreasen NC. Scale for the Assessment of Negative Symptoms. Iowa City: University of Iowa, 1984. [Google Scholar]
Andreasen 2004
- Andreasen NC. Scale for the Assessment of Positive Symptoms. Iowa: Iowa City, 2004. [Google Scholar]
APA 1980
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Third Edition. Washington, DC: American Psychiatric Association, 1980. [Google Scholar]
APA 1987
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Third Edition Revised. Washington, DC: American Psychiatric Association, 1987. [Google Scholar]
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Fourth Edition. Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Fourth Edition Text Revision. Washington, DC: American Psychiatric Association, 2000. [Google Scholar]
APA 2013
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Fifth Edition. Arlington, VA: American Psychiatric Association, 2013. [Google Scholar]
Birchwood 1998
- Birchwood M, Todd P, Jackson C. Early intervention in psychosis: the critical-period hypothesis. British Journal of Psychiatry 1998;172(S33):53-9. [PubMed] [Google Scholar]
Birchwood 2013
- Birchwood M, Connor C, Lester H, Patterson P, Freemantle N, Marshall M, et al. Reducing duration of untreated psychosis: care pathways to early intervention in psychosis services. British Journal of Psychiatry 2013;203:58-64. [DOI] [PubMed] [Google Scholar]
Birchwood 2014
- Birchwood M, Lester H, McCarthy L, Jones P, Fowler D, Amos T, et al. The UK national evaluation of the development and impact of Early Intervention Services (the National EDEN studies): study rationale, design and baseline characteristics. Early Intervention in Psychiatry 2014;8(1):59-67. [DOI] [PubMed] [Google Scholar]
Bland 1997
- Bland JM. Statistics notes. Trials randomised in clusters. BMJ 1997;315(7108):600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Breitborde 2009
- Breitborde JK, Srihari VH, Woods SW. Review of the operational definition for first-episode psychosis. Early Intervention in Psychiatry 2009;3(4):259-65. [DOI: 10.1111/j.1751-7893.2009.00148.x.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chong 2016
- Chong H, Teoh S, Wu D, Kotirum S, Chiou C, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatric Disease and Treatment 2016;12:357-73. [DOI] [PMC free article] [PubMed]
Cohen 1988
- Cohen J. Statistical Power Analysis in the Behavioral Sciences. 2 edition. Hillsdale (NJ): Lawrence Erlbaum Associates, Inc, 1988. [Google Scholar]
Correll 2018
- Correll C, Galling B, Pawar A, Krivko A, Bonetto C, Ruggeri M, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry 2018;75(6):555-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JP, Altman DG, editor(s). Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
De Wilde 2005
- De Wlide E, Hendricks V. The Client Satisfaction Questionnaire: psychometric properties in a Dutch addict population. European Addiction Research 2005;1(4):157-62. [DOI] [PubMed] [Google Scholar]
Divine 1992
- Divine GW, Brown JT, Frazier LM. The unit of analysis error in studies about physicians' patient care behavior. Journal of General Internal Medicine 1992;7(6):623-9. [DOI] [PubMed] [Google Scholar]
Donner 2002
- Donner A, Klar N. Issues in the meta-analysis of cluster randomized trials. Statistics in Medicine 2002;21(19):2971-80. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne D, Altman DG, Higgins JP, Curtina F, Worthingtond HV, Vaile A. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140-9. [DOI] [PubMed] [Google Scholar]
Furukawa 2006
- Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59(1):7-10. [DOI] [PubMed] [Google Scholar]
Fusar‐Poli 2017
- Fusar-Poli P, McGorry PD, Kane JM. Improving outcomes of first-episode psychosis: an overview. World Psychiatry 2017;16(3):251-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gulliford 1999
- Gulliford MC. Components of variance and intraclass correlations for the design of community-based surveys and intervention studies: data from the Health Survey for England 1994. American Journal of Epidemiology 1999;149(9):876-83. [DOI] [PubMed] [Google Scholar]
Harrison 2001
- Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J, et al. Recovery from psychotic illness: a 15-and 25-year international follow-up study. British Journal of Psychiatry 2001;178(6):506-17. [DOI] [PubMed] [Google Scholar]
Heinrichs 1984
- Heinrichs DW, Hanlon TE, Carpenter WT Jr. The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophrenia Bulletin 1984;10(3):388-98. [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JP, Deeks JJ, editor(s). Chapter 7: Selecting studies and collecting data. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hutton 2009
- Hutton JL. Number needed to treat and number needed to harm are not the best way to report and assess the results of randomised clinical trials. British Journal of Haematology 2009;146(1):27-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
Jones 1995
- Jones S, Thornicroft G, Coffey M, Dunn G. A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning. British Journal of Psychiatry 1995;166(5):654-9. [DOI] [PubMed] [Google Scholar]
Kane 2016
- Kane J, Robinson D, Schooler N, Mueser K, Penn D, Rosenheck R, et al. Comprehensive versus usual community care for First-Episode Psychosis: 2-Year outcomes from the NIMH RAISE Early Treatment Program. American Journal of Psychiatry 2016;173(4):362-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kay 1986
- Kay SR, Opler LA, Fiszbein A. Positive and Negative Syndrome Scale (PANSS) Manual. North Tonawanda (NY): Multi-Health Systems, 1986. [Google Scholar]
Kirkbride 2012
- Kirkbride JB, Errazuriz A, Croudace TJ, Morgan C, Jackson D, Boydell J, et al. Incidence of schizophrenia and other psychoses in England, 1950-2009: a systematic review and meta-analyses. PLOS One 2012;7(3):1-21. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirkbride 2017
- Kirkbride JB, Hameed Y, Ankireddypalli G, Ioannidis K, Crane CM, Nasir M, et al. The epidemiology of First-Episode Psychosis in Early Intervention in Psychosis services: Findings from the Social Epidemiology of Psychoses in East Anglia [SEPEA] Study. American Journal of Psychiatry 2017;174:143-53. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lally 2017
- Lally J, Ajnakina O, Stubbs B, Culllinane M, Murphy KC, Gaughran F, et al. Remission and recovery from first-episode psychosis in adults: systematic review and meta-analysis of long-term outcome studies. British Journal of Psychiatry 2017;211(6):350-8. [DOI: ] [DOI] [PubMed] [Google Scholar]
Leon 2006
- Leon AC, Mallinckrodt CH, Chuang-Stein C, Archibald DG, Archer GE, Chartier K. Attrition in randomized controlled clinical trials: methodological issues in psychopharmacology. Biological Psychiatry 2006;59(11):1001-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lincoln 1998
- Lincoln C, Harrigan S, McGorry P. Understanding the topography of the early psychosis pathways: An opportunity to reduce delays in treatment. British Journal of Psychiatry 1998;172(S33):21-5. [PubMed] [Google Scholar]
Marshall 2000
- Marshall M, Lockwood A, Bradley C, Adams C, Joy C, Fenton M. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. British Journal of Psychiatry 2000;176:249-52. [DOI] [PubMed] [Google Scholar]
Marshall 2011
- Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database of Systematic Reviews 2011, Issue 6. Art. No: CD004718. [DOI: 10.1002/14651858.CD004718.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mason 1995
- Mason P, Harrison G, Glazebrook C, Medley I, Dalkin T, Croudace T. Characteristics of outcome in schizophrenia at 13 years. British Journal of Psychiatry 1995;167(5):596-603. [DOI] [PubMed] [Google Scholar]
Meltzer 2002
- Meltzer H, Singleton N, Lee A, Bebbington P, Brugha T, Jenkins R. The Social and Economic Circumstances of Adults with Mental Disorders. London: Stationery Office, 2002. [Google Scholar]
Morgan 2014
- Morgan C, Lappin J, Heslin M, Donoghue K, Lomas B, Reuninghaus U, et al. Reappraising the long-term course and outcome of psychotic disorders: the AESOP-10 study. Psychological Medicine 2014;44(13):2713-26. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murray 1996
- Murray C, Lopez AD. Evidence-based health policy - lessons from the Global Burden of Disease Study. Science 1996;274(5288):740-3. [DOI] [PubMed] [Google Scholar]
NHS England 2015
- NHS England, National Collaborating Centre for Mental Health, National Institute for Health and Care Excellence. Implementing the Early Intervention in Psychosis Access and Waiting Time Standard (Guidance). 1 edition. NHS England, 2015. [Google Scholar]
NICE 2014
- National Institute for Health and Care Excellence. Psychosis and schizophrenia in adults: prevention and management (Clinical guideline). nice.org.uk/guidance/cg178 2014.
Overall 1962
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychological Reports 1962;10:799-812. [Google Scholar]
Priebe 1999
- Priebe S, Huxley P, Knight S, Evans S. Application and results of the Manchester Short Assessment of Quality of Life (MANSA). Internation Journal of Social Psychiatry 1999;45(1):7-12. [DOI] [PubMed] [Google Scholar]
RCPsych 2016
- Brightey-Gibbons F, Hodge S, Palmer L. Standards for Early Intervention in Psychosis Services. Pilot edition. London: Royal College of Psychiatrists, 2016. [Google Scholar]
Revier 2015
- Revier C, Reininghaus U, Dutta R, Fearon P, Murray R, Doody G, et al. Ten-year outcomes of first-episode psychoses in the MRC ÆSOP-10 study. Journal of Nervous and Mental Disease 2015;203:379. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ruggeri 1993
- Ruggeri M, Dali'Agnola R. The development and use of the Verona Expectations for Care Scale (VECS) and the Verona Service Satisfaction Scale (VSSS) for measuring expectations and satisfaction with community-based psychiatric services in patients, relatives and professionals. Psychological Medicine 1993;23(2):511-23. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JP, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Shokraneh 2017
- Shokraneh F, Adams CE. Study-based registers of randomized controlled trials: Starting a systematic review with data extraction or meta-analysis. BioImpacts 2017;7(4):209-17. [DOI: 10.15171/bi.2017.25] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shokraneh 2018
- Shokraneh F, Adams CE. Gallstone, snake venom and witchcraft for schizophrenia: the challenges of classifying [schizophrenia] trials. Evidence-Based Medicine 2018;23(Suppl 1):A18. [DOI: 10.1136/bmjebm-2018-111024.36] [DOI] [Google Scholar]
Singh 2017
- Singh S. Early intervention in psychosis: much done, much more to do. World Psychiatry 2017;16(3):276-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JA, Egger M, Moher D, editor(s). Chapter 10: Addressing reporting biases. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Intervention. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Ukoumunne 1999
- Ukoumunne OC, Gulliford MC, Chinn S, Sterne JA, Burney PG. Methods for evaluating area-wide and organisation-based intervention in health and health care: a systematic review. Health Technology Assessment 1999;3(5):iii-92. [PubMed] [Google Scholar]
WHO 2004
- World Health Organization. ICD-10: international statistical classification of diseases and related health problems: tenth revision. Geneva: World Health Organization, 2004. [Google Scholar]
WHO 2018
- World Health Organization. ICD-11: international statistical classification of diseases and related health problems: eleventh revision. Geneva: World Health Organization, 2018. [Google Scholar]
Wiersma 1998
- Wiersma D, Nienhuis F, Slooff C, Giel R. Natural course of schizophrenia disorders: a 15-year follow-up of a Dutch incidence cohort. Schizophrenia Bulletin 1998;24:75-85. [DOI] [PubMed] [Google Scholar]
Xia 2009
- Xia J, Adams CE, Bhagat N, Bhagat V, Bhoopathi P, El-Sayeh H, et al. Loss to outcomes stakeholder survey: the LOSS study. Psychiatric Bulletin 2009;33(7):254-7. [Google Scholar]
Yung 2008
- Yung AR, Nelson B, Stanford C, Simmons MG, Cosgrave EM, Killackey E et al. Validation of "prodromal" criteria to detect individuals at ultra high risk of psychosis: 2 year follow-up. Schizophrenia Research 2008;105(1-3):10-7. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Puntis 2019
- Puntis S, Minichino A, De Crescenzo F, Cipriani A, Lennox B. Specialised early intervention teams for first episode psychosis. Cochrane Database of Systematic Reviews 2019, Issue 3. Art. No: CD013288. [DOI: 10.1002/14651858.CD013288] [DOI] [PMC free article] [PubMed] [Google Scholar]


