Abstract
Background
Reported prevalence rates of asthma vary within and between countries around the world. These differences suggest environmental factors in addition to genetic factors in the cause of the disease and may provide clues for preventive strategies. We examined the variability of asthma-related symptoms and medication use among adults in 6 sites across Canada (Vancouver, Winnipeg, Hamilton, Montreal, Halifax and Prince Edward Island) and compared our findings with those from sites that had participated in a recent European survey.
Methods
We used the same sampling strategy and standardized questionnaire as those used in the European Community Respiratory Health Survey (ECRHS). The 6 Canadian sites were selected to represent different environments with respect to climate, air pollution and occupational exposure. Community-based samples of 3000 to 4000 people aged 20–44 years were randomly selected in each site. Subjects were asked to complete the questionnaire by mail between March 1993 and November 1994. Prevalence rates (and 95% confidence intervals [CIs]) of asthma symptoms, self-reported asthma attacks and use of asthma medication were compared across the Canadian sites and with sites that had participated in the ECRHS.
Results
The overall response rate of those selected to receive the questionnaire was 86.5% (range 74.5%–92.8%). The prevalence rates of most asthma symptoms varied significantly among the Canadian sites. For instance, 21.9% (Montreal) to 30.4% (Halifax) of the men and 24.0% (Vancouver) to 35.2% (Halifax) of the women reported wheezing in the year before the survey. Depending on the site, 4.4% to 6.3% of the men and 5.2% to 9.5% of the women reported an asthma attack in the last year, and 4.0% to 6.1% of the men and 4.9% to 9.7% of the women were currently using asthma medication. Prevalence rates of symptoms, asthma attacks and medication use did not change with age, but they were higher among women than among men. Compared with the results from the ECRHS sites, those from the Canadian sites were among the highest.
Interpretation
Significant variation in the prevalence of asthma symptoms, asthma attacks and use of asthma medication between Canadian sites and international sites suggests environmental influences. Different combinations of factors in different sites may be responsible for the high prevalence rates and should be the subject of further research to guide clinical management and public health intervention.
The increasing prevalence of asthma, frequency of hospital admissions and asthma-related mortality reported in many industrialized countries, including Canada,1,2,3 have led to concerns about the disease's medical and social costs.4 The rising prevalence may be due to increasing incidence or severity. Although the evidence for a genetic basis for asthma is strong, the environment also plays a major role in inducing and maintaining the asthmatic process.5,6
Differences in asthma prevalence among and within countries may provide clues for preventable risk factors.7 However, reported differences may also be due to the use of different definitions of asthma and of different instruments (e.g., questionnaires) for its measurement. In addition, there is no general consensus about its clinical definition,8 and less rigorous definitions are usually used for population-based studies.9 The International Union Against Tuberculosis and Lung Diseases sponsored the development of a standard questionnaire to be used in prevalence studies of asthma in adults.10 The validity and reproducibility of this questionnaire were found to be satisfactory.11,12 It was used in the European Community Respiratory Health Survey (ECRHS), a multicentre 2-stage prevalence study supported by the European Commission.13 The first stage assessed the variation in the prevalence of asthma symptoms across different study sites, and the second stage examined the prevalence of bronchial responsiveness and atopy. Forty-eight centres from 17 countries in Europe and 5 countries outside Europe completed the study between 1990 and 1995.14
Our objectives were to estimate the age- and sex-specific prevalence rates of asthma symptoms, self-reported asthma attacks and use of asthma medications among adults aged 20–44 years in 6 sites in Canada, to investigate the variation between these sites and to compare the results from the Canadian sites with those from the ECRHS sites.
Methods
Stage I of our study involved completion of a mailed questionnaire by randomly selected samples of the general population aged 20–44 years in 6 sites across Canada, selected to represent different environments with respect to climate, air pollution and occupational exposures. In Vancouver, Winnipeg, Hamilton and Montreal, the study was conducted between March 1993 and May 1994; in Halifax and Prince Edward Island it was conducted between September 1993 and November 1994. Sampling and data collection were evenly distributed throughout the year.
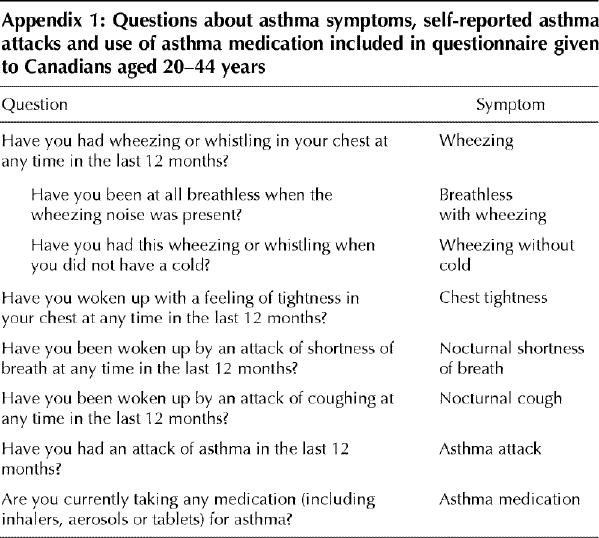
The overall sampling strategy and instruments were the same as those used in the ECRHS sites, to maximize the international comparability of the Canadian results.15 We used the ECRHS stage I questionnaire15 and added questions about non-asthma-related respiratory symptoms, smoking, occupational exposure to dust, fumes and gases, and residential history. The questions about asthma symptoms, self-reported asthma attacks and use of asthma medication are given in Appendix 1. The questionnaire was translated into French and translated back into English to check for accuracy. In Montreal, both the English and the French versions were mailed to all subjects to allow them to answer in their language of choice. A training workshop was organized for technical staff from all participating Canadian sites to standardize study procedures.
Each sample was drawn from a population of at least 150 000 people of all ages. We selected random samples of 3000 to 4000 adults aged 20–44 years in 5 urban sites (Vancouver, Winnipeg, Hamilton, Montreal and Halifax) and in PEI, where the rural–urban ratio was 1.5:1. In the 5 cities, random digit dialling was used to identify eligible individuals. For each city, a random sample of 18 000 telephone numbers, divided into 12 subsamples, was generated. Interviewers systematically called the generated numbers and, following an appropriate introduction, determined whether the number was residential and whether there were eligible individuals in the household. If nobody answered, the interviewer called up to 7 times, varying the day and time. If more than 1 household member was eligible, the interviewer identified the resident to be included using a predetermined sampling scheme. The subject's name and the postal address were recorded. Random digit dialling was not used in PEI because the sampling frame was the total province and the majority of telephone calls would have been long-distance, often using party telephone lines; we therefore selected a random sample of 3600 individuals from the population registry of the Provincial Health Insurance Plan. Otherwise the procedure for PEI was the same as that used in the 5 cities.
Individuals identified as eligible were mailed a questionnaire with a cover letter explaining the purpose of the study. The cover letter focused on general respiratory health and not on asthma. After 3 weeks a second questionnaire was sent to nonrespondents. Those who did not respond to the second mailing were telephoned after 3 weeks and encouraged to return the completed questionnaire by mail or to complete it by telephone.
Subjects were asked in which country they had been born and how long had they lived in the study site. Smoking status was classified as current (at the time of the survey), past or never. Those who answered Yes to the question “Have you ever been exposed to dust (gases or chemicals or fumes) at work?” were considered to have had occupational exposure. Another category included people who answered Yes to the question “Have you ever had to change or leave your job because it affected your breathing?”
Sex-specific prevalence rates and 95% confidence intervals (CIs) were estimated overall and for 5-year age groups. Age-related trends were examined using log-linear models.16 We used multiple logistic regression analysis to test differences between sites, controlling for smoking, birth outside Canada and occupational exposures. For international comparisons, sex- and age-specific prevalence rates were adjusted in the same manner as that used in the ECRHS;14,17 prevalence was adjusted to a standard population with an equal distribution by age and sex, without adjustment for nonresponse. Statistical significance was set at p < 0.05 or 95% CIs not overlapping 1.
The study was approved by ethics review boards from all participating institutions.
Results
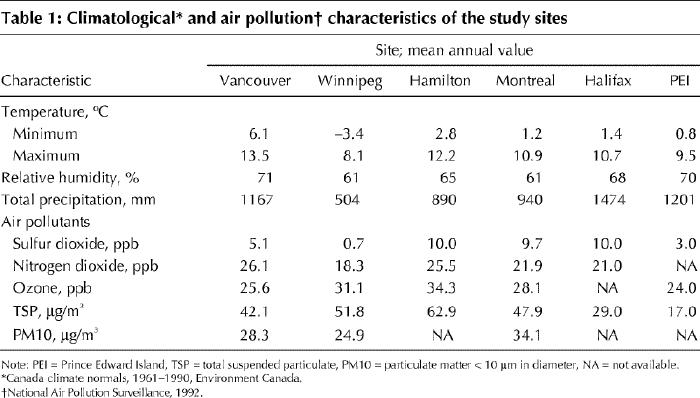
Table 1 shows selected climate and air pollution characteristics of the 6 sites. The average annual temperature and relative humidity were highest in Vancouver and lowest in Winnipeg, and the total precipitation was highest in Halifax and lowest in Winnipeg. The highest levels of sulfur dioxide were recorded in Hamilton, Montreal and Halifax, and the lowest in Winnipeg. The highest levels of total suspended particulate were recorded in Hamilton and Winnipeg and the lowest in PEI. There was less variability among sites with respect to nitrogen oxide and ozone.
Table 1
The response rate also varied by site. Overall, 21 449 eligible subjects were identified and 86.5% (range 74.5% [Halifax] to 92.8% [PEI]) completed the questionnaire. For 28.4% of the subjects the questionnaire was completed over the telephone. Age was calculated as of the date of completing the questionnaire. Subjects (n = 107) less than 1 year outside the selected age range for the study were included in the youngest and oldest groups. Responses from 18 616 individuals were included in the analysis.
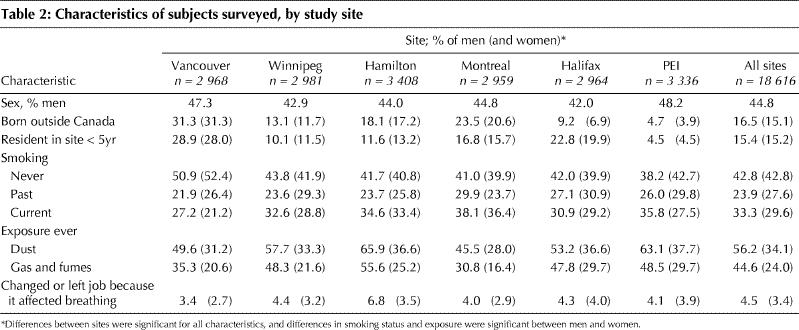
The subjects' characteristics varied between sites (Table 2). About 15% (range 3.9%–31.3%) were born outside Canada, and about 15% (range 4.5%–28.9%) resided for less than 5 years in the site of the interview. At all sites, more men than women reported being past or current smokers; overall, the difference in smoking between men and women was significant. The highest proportion of current smokers (men and women) was in Montreal and the lowest in PEI. The proportion of men who reported occupational exposure was highest in Hamilton; more women in Hamilton, Halifax and PEI than in the other 3 sites reported occupational exposure. More subjects in Hamilton than in the other sites changed or left their job because it had adversely affected their breathing. Overall, rates for reported occupational exposures and changing jobs were significantly higher among men than among women.
Table 2
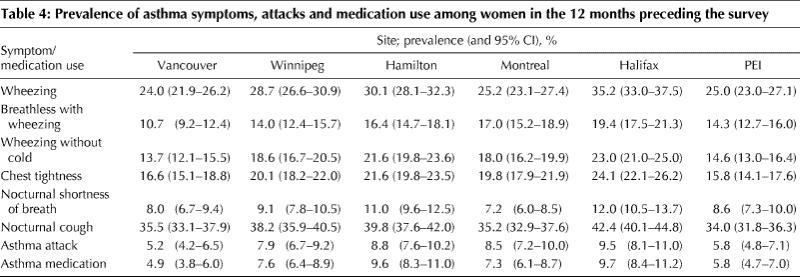
There was substantial variation between sites in the prevalences of asthma symptoms, self-reported asthma attacks and use of asthma medication among men (Table 3) and women (Table 4). For most symptoms and for both sexes, the highest prevalence rates were observed in Halifax and Hamilton, and the lowest in Vancouver and PEI. The ratio between the highest and the lowest prevalence rates by site varied by symptom and sex. For men and women, the variation in this ratio was the highest for use of asthma medication (1.5 for men and 2.0 for women) and the lowest for nocturnal cough (1.2 and 1.3 respectively). The prevalence rates varied significantly between sites for all symptoms among women and for wheezing, wheezing without a cold, chest tightness and nocturnal cough among men. In the multiple logistic regression analyses, these differences remained significant even after adjusting for between-site differences in the proportion of those born in Canada, were smokers, reported occupational exposure and changed jobs (details not shown).
Table 3
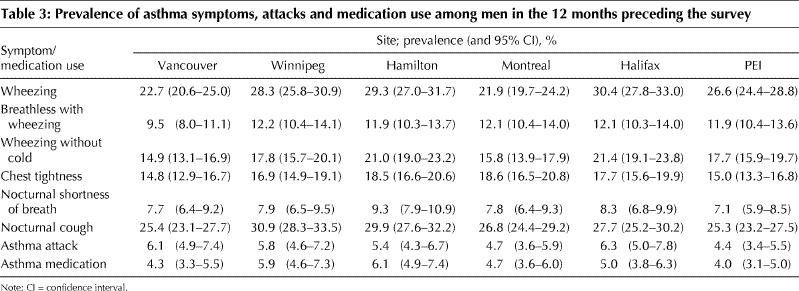
Table 4
To examine the relation of symptoms to age and sex, we pooled subjects from all sites (data not shown). The prevalence of asthma symptoms, self-reported asthma attacks and use of asthma medication changed little between ages 20 and 44 years in both men and women.
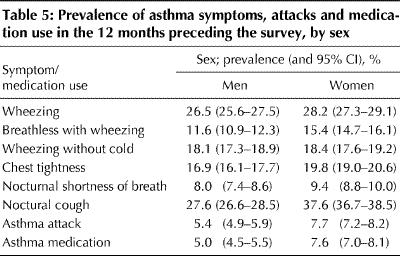
Of the asthma symptoms, all but wheezing and wheezing without a cold were significantly more prevalent among women than among men (Table 5). A significantly greater proportion of women than of men reported asthma attacks and were currently using asthma medication.
Table 5
In Fig. 1, the age- and sex-standardized prevalence rates of asthma symptoms, self-reported asthma attacks and use of asthma medication in the 6 Canadian sites are compared with the median and 75th percentile values for 48 sites that participated in the ECRHS.14 With 4 exceptions (breathlessness with wheezing in Vancouver, and nocturnal shortness of breath in Vancouver, Montreal and PEI), the lower limit of the 95% CI in all of the Canadian sites was higher than the ECRHS median for all symptoms, asthma attacks and use of asthma medication.14 In Halifax and Hamilton, the lower limit of the 95% CI was also higher than the ECRHS 75th percentile for all symptoms, asthma attacks and use of asthma medication. In Vancouver and PEI the prevalence rates of most symptoms were significantly higher than the ECRHS median but not higher than the 75th percentile.
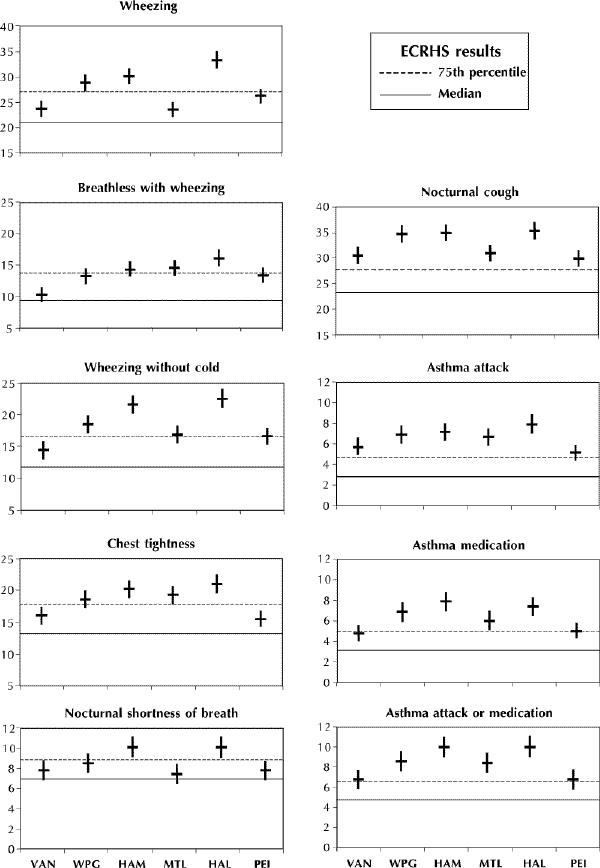
Fig. 1: Prevalence rates (and 95% confidence intervals) of asthma symptoms, attacks and medication use reported by subjects in 6 Canadian sites (Vancouver [VAN], Winnipeg [WPG], Hamilton [HAM], Montreal [MTL], Halifax [HAL] and Prince Edward Island [PEI]). In each graph, the solid horizontal line represents the median, and the broken line the 75th percentile, of the distribution of rates reported in 48 sites participating in the European Community Respiratory Health Survey (ECRHS).14 The category “asthma attack or medication” corresponds to the ECRHS category “diagnosed asthma.”14
Interpretation
To our knowledge, there have been no previous studies of prevalence of asthma and asthma-like symptoms among adults in Canada using a standardized questionnaire. A major strength of our study is that it allows comparisons between regions and between countries. Six sites across Canada were included, covering industrial and rural regions. Study limitations are the age limits (20–44 years) and the use of self-reported information. Nevertheless, our findings greatly extend previously available data on the epidemiology of asthma in Canada.
In the absence of an accepted definition of asthma, the burden of asthma in the population is best represented by the distribution of asthma symptoms and bronchial responsiveness. The ECRHS questionnaire15 has several advantages over previously used questionnaires: responses refer to symptoms, are independent of utilization of health services, not restricted to wheezing and cover the 12 months before the survey. The questions have been validated, although they may vary with respect to their sensitivity and specificity for asthma.18
We found that, for both men and women, the prevalence rates of asthma symptoms, self-reported asthma attacks and use of medication varied significantly across the Canadian sites, tending to be highest in Hamilton and Halifax and lowest in Vancouver and PEI. This variation was not explained by differences between the sites in the proportion of subjects born outside Canada, smokers or those reporting occupational exposures. The prevalence rates of asthma symptoms, asthma attacks and use of asthma medication did not vary by age. This may be due to the relatively narrow age group studied. All symptoms except wheezing and wheezing without a cold, as well as asthma attacks and use of asthma medication were more prevalent among women than among men. This is consistent with published information on differences in asthma incidence between men and women in their reproductive years.19
The variation in the proportion of subjects currently using any asthma medication (4.3%–6.1% of men and 4.9%–9.6% of women) followed the distribution of symptoms: the higher the prevalence of symptoms, the higher the proportion of participants using asthma medication. However, between-site variation in the use of asthma medication was even greater than the variation in symptoms, which suggests that other factors (e.g., physician practice) play a role in determining treatment patterns. We did not distinguish between use of medications for symptom relief and use for asthma prevention.
Significant variation in the prevalence rates of asthma symptoms among the Canadian sites suggests a role of environment, although it is unclear which factors may be responsible for the variation. Smoking and occupational exposures did not appear to explain the differences. It is unlikely that genetic determinants of susceptibility for asthma would vary substantially between the sites. The Canadian population is exposed to a variety of factors that may induce asthma or maintain the inflammatory process and trigger asthma attacks. These factors are likely to vary across the country. The lower prevalence rates in PEI than in the other sites are consistent with other observations that there is less asthma in rural than in urban areas,6,20,21,22 although other indicators of asthma morbidity, such as admissions to hospital, suggest that asthma is a major problem in PEI.2,23 The high prevalence of symptoms among adults in the industrialized city of Hamilton is consistent with a recent study showing higher rates of asthma among children in Hamilton than in the prairie city of Saskatoon.24 Specific occupational risks exist in some communities; for example, grain exposure in the prairies,25 and cedar, pulp mill, smelter and grain exposure in British Columbia.26
In all Canadian sites the prevalence rates of asthma attacks, use of asthma medication and asthma symptoms except nocturnal cough were above the median, and in most instances above the 75th percentile, of the ECRHS data.14 These comparisons were based on combined-sex rates because sex-specific rates are not available for ECRHS data. There was also substantial variation between the ECRHS sites (and within the ECRHS countries).14 We do not know how much of this variation was due to variation in smoking and occupational exposures, since these characteristics were not measured in stage 1 of the ECRHS.
In conclusion, the observed differences between the Canadian and international sites are unlikely to be due to methodological, cultural and linguistic differences.14,27 The same protocol and questionnaire were used, the training of Canadian technicians was carried out by those who had earlier participated in the ECRHS, and the sampling frame was defined similarly in all sites. The fact that random digit dialling was used in Canada and not in the ECRHS is unlikely to explain the differences. The high response rate (86.5% overall, with only 1 centre below 80%) compares favourably with that reported in the ECRHS (median 78%).14
The explanation for the high prevalence rates of asthma symptoms among Canadian adults in the 6 sites studied is not evident from our findings. For effective day-to-day management and public health interventions, further research is needed to determine population and individual risk factors for asthma-related morbidity in Canada.
Appendix 1.
Footnotes
This article has been peer reviewed.
Acknowledgements: We thank Dr. Peter Burney for his help in setting up the study, Ms. Susan Chinn for her help with the analysis, and Dr. Sonia Buist and her staff for training Canadian technicians in the ECRHS protocol.
This study was funded by grants from the National Health Research and Development Programme, Glaxo Canada and the Government of the Province of Prince Edward Island. The grant from Glaxo was to the University of Manitoba and not to a specific study site or investigator.
Competing interests: None declared.
Reprint requests to: Dr. Jure Manfreda Department of Medicine, Respiratory Hospital, 810 Sherbrook St., Winnipeg MB R3A 1R8; fax 204 787-2420; manfred@ms.umanitoba.ca
References
- 1.Mao Y, Semenciw R, Morrison H, MacWilliam L, Davies J, Wigle D. Increased rates of illness and death from asthma in Canada. CMAJ 1987;137:620-4. [PMC free article] [PubMed]
- 2.Wilkins K, Mao Y. Trends in rates of admission to hospital and death from asthma among children and young adults in Canada during the 1980s. CMAJ 1993;148:185-90. [PMC free article] [PubMed]
- 3.Manfreda J, Becker AB, Wang PZ, Roos LL, Anthonisen NR. Trends in physician-diagnosed asthma prevalence in Manitoba between 1980 and 1990. Chest 1993;103:151-7. [DOI] [PubMed]
- 4.Krahn MD, Berka C, Langlois P, Detsky AS. Direct and indirect costs of asthma in Canada, 1990. CMAJ 1996;154(6):821-31. Available: www.cma.ca/cmaj/vol-154/0821e.htm [PMC free article] [PubMed]
- 5.Burney P. Epidemiology of asthma. Allergy 1993;48:17-21. [DOI] [PubMed]
- 6.Becklake MR, Ernst P. The challenge of asthma. Environmental factors. Lancet 1997;350(Suppl 2):10-3. [DOI] [PubMed]
- 7.Burney P. Why study the epidemiology of asthma? Thorax 1988; 43:425-8. [DOI] [PMC free article] [PubMed]
- 8.Sears MR. The definition and diagnosis of asthma. Allergy 1993;48:12-6. [DOI] [PubMed]
- 9.Pekkanen J, Pearce N. Defining asthma in epidemiological studies. Eur Respir J 1999;14:951-7. [DOI] [PubMed]
- 10.Burney P, Chinn S. Developing a new questionnaire for measuring the prevalence and distribution of asthma. Chest 1987; 91:79s-83s. [DOI] [PubMed]
- 11.Burney PGJ, Chinn S, Britton JR, Tattersfield AE, Papacosta AO. What symptoms predict the bronchial response to histamine? Evaluation in a community survey of the Bronchial Symptoms Questionnaire (1984) of the International Union Against Tuberculosis and Lung Disease. Int J Epidemiol 1989;18:165-73. [DOI] [PubMed]
- 12.Burney PGJ, Laitinen LA, Perdrizet S, Huckauf H, Tattersfield AE, Chinn S, et al. Validity and repeatability of the IUATLD (1984) Bronchial Symptoms Questionnaire: an international comparison. Eur Respir J 1989;2:940-5. [PubMed]
- 13.Burney PGJ, Luczynska C, Chinn S, Jarvis D. The European Community Respiratory Health Survey. Eur Respir J 1994;7:954-60. [DOI] [PubMed]
- 15.European Commission, Directorate General XII. Protocol for the European Community Respiratory Health Survey. Luxembourg: Office for Official Publications; 1993.
- 14.European Community Respiratory Health Survey. Variations in the prevalence of respiratory symptoms, self-reported asthma attacks, and use of asthma medication in the European Community Respiratory Health Survey (ECRHS). Eur Respir J 1996;9:687-95. [DOI] [PubMed]
- 16.Kleinbaum DG, Kupper LL, Morgenstern H. Epidemiologic research: principles and quantitative methods. Belmont (CA): Lifetime Learning Publications; 1982.
- 17.Chinn S, Zanolin E, Lai E, Jarvis D, Luczynska CM, Burney PGJ. Adjustment of reported prevalence of respiratory symptoms for non-response in a multi-centre health survey. Int J Epidemiol 1995; 24:603-11. [DOI] [PubMed]
- 18.Abramson MJ, Hensley MJ, Saunders NA, Wlodarczyk JH. Evaluation of a new asthma questionnaire. J Asthma 1991;28:129-39. [DOI] [PubMed]
- 19.Becklake MR, Kauffmann F. Gender differences in airway behaviour over the human lifespan. Thorax 1999;54:1119-38. [DOI] [PMC free article] [PubMed]
- 20.Aberg N. Asthma and allergic rhinitis in Swedish conscripts. Clin Exp Allergy 1989;19:59-63. [DOI] [PubMed]
- 21.Nilsson L, Castor O, Lofman O, Magnusson A, Kjellman NIM. Allergic disease in teenagers in relation to urban or rural residence at various stages of childhood [published erratum appears in Allergy 1999 Nov; 54:1223] Allergy 1999;54:716-21. [DOI] [PubMed]
- 22.Ernst P, Cormier Y. Relative scarcity of asthma and atopy among rural adolescents raised on a farm. Am J Respir Crit Care Med 2000;161:1563-6. [DOI] [PubMed]
- 23.Sweet L, Fan JSK, O'Neill J. A validation study of asthma, Prince Edward Island, 1984–1988: hospitalizations. Chronic Dis Can 1992;13:19-23.
- 24.Habbick BF, Pizzichini MMM, Taylor B, Rennie D, Senthilselvan A, Sears MR. Prevalence of asthma, rhinitis and ezcema among children in 2 Canadian cities: the International Study of Asthma and Allergies in Childhood. CMAJ 1999;160(13):1824-8. Available: www.cma.ca/cmaj/vol-160/issue-13/1824.htm [PMC free article] [PubMed]
- 25.Senthilselvan A, Chen Y, Dosman JA. Predictors of asthma and wheezing in adults. Am Rev Respir Dis 1993;148:667-70. [DOI] [PubMed]
- 26.Siracusa A, Kennedy SM, DyBuncio A, Lin FJ, Marabini A, Chan-Yeung M. Prevalence and predictors of asthma in working groups in British Columbia. Am J Ind Med 1995;28:411-23. [DOI] [PubMed]
- 27.Osterman JW, Armstrong BG, Ledoux E, Sloan M, Ernst P. Comparison of French and English versions of the American Thoracic Society respiratory questionnaire in a bilingual working population. Int J Epidemiol 1991;20:138-43. [DOI] [PubMed]


