Abstract
Objective
We aimed to systematically identify the possible risk factors responsible for severe cases.
Methods
We searched PubMed, Embase, Web of science and Cochrane Library for epidemiological studies of confirmed COVID-19, which include information about clinical characteristics and severity of patients’ disease. We analyzed the potential associations between clinical characteristics and severe cases.
Results
We identified a total of 41 eligible studies including 21060 patients with COVID-19. Severe cases were potentially associated with advanced age (Standard Mean Difference (SMD) = 1.73, 95% CI: 1.34–2.12), male gender (Odds Ratio (OR) = 1.51, 95% CI:1.33–1.71), obesity (OR = 1.89, 95% CI: 1.44–2.46), history of smoking (OR = 1.40, 95% CI:1.06–1.85), hypertension (OR = 2.42, 95% CI: 2.03–2.88), diabetes (OR = 2.40, 95% CI: 1.98–2.91), coronary heart disease (OR: 2.87, 95% CI: 2.22–3.71), chronic kidney disease (CKD) (OR = 2.97, 95% CI: 1.63–5.41), cerebrovascular disease (OR = 2.47, 95% CI: 1.54–3.97), chronic obstructive pulmonary disease (COPD) (OR = 2.88, 95% CI: 1.89–4.38), malignancy (OR = 2.60, 95% CI: 2.00–3.40), and chronic liver disease (OR = 1.51, 95% CI: 1.06–2.17). Acute respiratory distress syndrome (ARDS) (OR = 39.59, 95% CI: 19.99–78.41), shock (OR = 21.50, 95% CI: 10.49–44.06) and acute kidney injury (AKI) (OR = 8.84, 95% CI: 4.34–18.00) were most likely to prevent recovery. In summary, patients with severe conditions had a higher rate of comorbidities and complications than patients with non-severe conditions.
Conclusion
Patients who were male, with advanced age, obesity, a history of smoking, hypertension, diabetes, malignancy, coronary heart disease, hypertension, chronic liver disease, COPD, or CKD are more likely to develop severe COVID-19 symptoms. ARDS, shock and AKI were thought to be the main hinderances to recovery.
1. Introduction
Coronavirus Disease 2019(COVID-19) which, was first identified in Wuhan, Hubei Province, China in December 2019, has already swept across the world. The World Health Organization (WHO) has officially declared the outbreak as a pandemic and a public health emergency [1]. As of 9th March 2021, according to WHO, the number of confirmed cases around the world has surged dramatically to 116,166,652 with 2,582,528 deaths, which suggests the general mortality rate is approximately 2.22% [2]. The severity of symptoms among patients infected with COVID-19 varies considerably from being varies considerably from being asymptomatic to being a critical illness with lethal complications [3, 4].
Some researchers have suggested that there are several factors possibly responsible for the severity of COVID-19, such as hypertension, diabetes and smoking [5–7]. Therefore, we performed this systematic review and meta-analysis to explore the potential risk posed by critical medical states in COVID-19 patients. Specifically, in this study we have compared the reported clinical characteristics of patients with non-severe and severe COVID-19 in eligible published literature.
2. Method
2.1 Search strategy
The literature search was performed using international databases PubMed, Embase, Web of science and Cochrane Library using the search terms: (“COVID-19” OR “SARS-Cov-2”) AND (“characteristics” OR “clinical”): The specific search strategy is listed in S1 Table. Included studies were published between December 2019 and February 2021. The meta-analysis was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [8].
2.2 Study selection
To minimize bias, two authors (LXY and ZXR) independently screened titles and abstracts and extracted potentially eligible articles. The full texts of selected articles were then carefully assessed according to the inclusion and exclusion criteria. Disagreements were resolved by discussion, with the third researcher (LQ) to reach a consensus.
2.3 Inclusion and exclusion criteria
Inclusion criteria:(1) case-control studies or cohort studies; (2) articles reporting the clinical characteristics and the severity of disease in patients diagnosed with COVID-19; (3) articles reporting the severity of COVID-19 and details of related factors; (4) articles reporting the specific grading standards of the severity of COVID-19.
The definition of severe disease was based on clinical symptoms, i.e., patients having severe dyspnea, extremely low oxygen saturation, respiratory distress or requiring mechanical ventilation, ICU admission or death.
The exclusion criteria: (1) review articles, letters, comments or opinions; (2) samples of less than 50; (3) incomplete information or full texts unavailable.
2.4 Quality assessment
All included studies were retrospective cohort studies so, the Newcastle-Ottawa Scale (NOS) was used to evaluate quality [9]. The major components include: representativeness of the exposed cohort, selection of the non- exposed cohort, ascertainment of exposure, demonstration that outcome of interest was not present at start of study, comparability, assessment of outcome, follow-up time and adequacy of follow up of cohorts. The quality rating is from 0 to 10 stars and the score≥7 stars indicates high-quality articles.
2.5 Data extraction
Two independent authors (LXY and ZXR) performed the data extraction by using standardized forms, which included date of publication, authors, region, number of included patients, sex, body mass index (BMI), smoking habits, comorbidities, complications, and severe or non-severe COVID-19.
2.6 Statistical analysis
We calculated odds ratios (ORs) in the dichotomous variables and standard mean difference (SMD) in the continuous variables with the 95% confidence intervals (CIs) and assessed publication bias using Stata 12.0. Heterogeneity was measured by I2 statistic. We used a Mantel-Haenszel random effects model to calculate effect sizes. In order to discover the potential sources of heterogeneity, we performed subgroup analyses and meta-regression analysis according to study location (Hubei province and outside Hubei province) and the median ages of patients. The stability of results was assessed by conducting a sensitivity analysis which omitted each study in turn. Funnel plots were used to assess for publication bias and asymmetry was taken to indicate bias. In this study, P values <0.05 were regarded as indicating statistical significance for the summary OR and SMD. In order to quantify the effects of risk factors on COVID-19 patients, we calculated population attributable fraction (PAF) by using the attributable fraction formula:
where Pc is the prevalence of the risk factors in the population [10]. In this analysis, the ORs were used as approximations of RRs.
3 Results
3.1 Study selection and characteristics
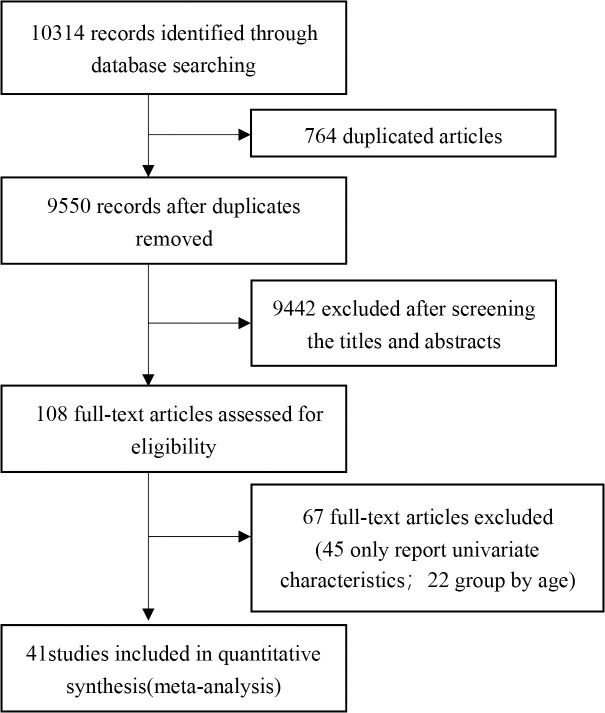
The complete literature-search process is displayed in Fig 1. The search strategy initially retrieved 10314 articles, 10273 of which were excluded by assessing the eligibility criteria. Of these studies, 764 papers were duplicates, 9442 were perceived as unrelated research and 67 articles were in line with exclusion criteria. Finally, 41 articles [11–51] published between February 7th, 2020 and March 13th, 2021 were included, all of which were retrospective cohort studies. In total, 21060 patients were included in the meta-analysis. The characteristics of all the included studies are shown in Table 1.
Fig 1. Flow diagram of literature selection.
Table 1. Characteristics of the included studies.
| Author | Publication Date | Study Location | Samples(M/F) | Severe | Non-severe | Overall age (Median age/Mean age, range/SD) | Adjustments |
|---|---|---|---|---|---|---|---|
| Wang et al. 2020a [11] | Feb 7,2020 | Wuhan, China | 138(75/63) | 36 | 102 | 56(42–68) | ①,②,④,⑤,⑥,⑦,⑧,⑨,⑩,⑪,⑫,⑬,⑭,⑮,⑯ |
| Zhang et al. 2020a [12] | Feb 19,2020 | Wuhan, China | 140(71/69) | 58 | 82 | 57(25–87) | ①,②,③,④,⑤,⑧,⑭,⑯ |
| Guan et al. 2020 [13] | Feb 28,2020 | China | 1099(640/459) | 173 | 926 | 47(35–58) | ①,②,③,④,⑤,⑥,⑦,⑧,⑨,⑩,⑪,⑫,⑬,⑭,⑰ |
| Wan et al. 2020 [14] | Mar 21,2020 | Chongqing, China | 135(73/62) | 40 | 95 | 47(36–55) | ①,②,④,⑤,⑧,⑨,⑩,⑫,⑬,⑮ |
| Hong et al. 2020 [15] | Apr 24,2020 | Daegu, Korea | 98(38/60) | 13 | 85 | 55.4(SD = 17.1) | ①,②,④,⑤,⑥,⑦,⑧,⑨,⑩,⑫,⑬,⑭,⑮ |
| Zhang et al. 2020b [16] | Apr 27,2020 | Guangdong, China | 1350(664/686) | 229 | 1121 | 44.1(SD = 17.9) | ①,②,④,⑤,⑧ |
| Chen et al. 2020 [17] | Apr 28,2020 | Zhejiang, China | 145(79/66) | 43 | 102 | 45.3(SD = 13.6) | ①,②,③,④,⑤,⑦,⑧,⑨,⑩,⑪,⑫,⑬ |
| Zhao et al. 2020 [18] | Apr 29,2020 | Hubei, China | 91(49/42) | 30 | 61 | 46* | ①,②,④,⑤,⑭,⑮,⑱ |
| Zheng et al. 2020 [19] | Apr 30,2020 | Hubei, China | 73 | 30 | 43 | 43(21–76) | ③,⑤ |
| Hu et al. 2020 [20] | May 3,2020 | Wuhan, China | 323(166/157) | 151 | 172 | 61(23–91) | ①,③,④,⑤,⑥,⑦,⑧,⑨,⑩,⑪,⑫,⑬,⑭,⑲ |
| Cai et al. 2020a [21] | May 14,2020 | Shenzhen, China | 383(183/200) | 91 | 292 | NA | ⑲ |
| Wang et al. 2020b [22] | May 19,2020 | Guangzhou, China | 275(134/141) | 45 | 230 | 49(34–62) | ①,②,③,④,⑤,⑥,⑦,⑧,⑩,⑪,⑫,⑬,⑰ |
| Buckner et al. 2020 [23] | May 22,2020 | Seattle, USA | 99(53/46) | 51 | 54 | 69(23–97) | ①,②,③,④,⑤,⑦,⑧,⑨,⑲ |
| Yang et al. 2020 [24] | May 25,2020 | Wuhan, China | 136(66/70) | 33 | 103 | 56(44–64) | ①,②,④,⑤,⑥,⑦,⑧,⑩,⑫,⑬,⑭,⑮ |
| Feng et al. 2020 [25] | Jun 1,2020 | China | 476(271/205) | 124 | 352 | 53(40–64) | ①,③,④,⑤,⑥,⑦,⑧,⑨,⑪ |
| Suleyman et al. 2020 [26] | Jun 16,2020 | Detroit, USA | 463(165/298) | 141 | 214 | 57.5(16.8) | ①,②,③,④,⑤,⑦,⑧,⑨,⑫,⑬,⑭,⑲,⑳ |
| Cao et al. 2020 [27] | Jun 17,2020 | Beijing, China | 80(38/42) | 27 | 53 | 53(SD = 20) | ①,③,④,⑤,⑧,⑨ |
| Shahriarirad et al. 2020 [28] | Jun 18,2020 | Iran | 113(71/42) | 11 | 102 | 53.75(20–99) | ①,④,⑤,⑥,⑦,⑨,⑪,⑳ |
| Nie et al. 2020 [29] | Jun 26,2020 | Henan, China | 671(367/304) | 72 | 583 | 44(31–53) | ①,②,③,④,⑤,⑧,⑨ |
| Zhang et al. 2020c [30] | Jul 8,2020 | Zhejiang, China | 771(394/337) | 61 | 710 | NA | ①,③,④,⑤,⑦,⑧,⑨,⑩,⑪,⑲ |
| Cai et al. 2020b [31] | Jul 11,2020 | Shenzhen, China | 298(145/153) | 240 | 58 | 47(33–61) | ①,②,④,⑤,⑦,⑧,⑩,⑲ |
| Gregoriano et al. 2020 [32] | Jul 15,2020 | Switzerland | 99(62/37) | 35 | 64 | 67(56–76) | ①,②,④,⑤,⑦,⑧,⑨,⑪ |
| Ghweil et al. 2020 [33] | Jul 17,2020 | Egypt | 66(48/18) | 30 | 36 | 55.5(SD = 10.1) | ①,②,③,④,⑤,⑧,⑲ |
| Yu et al. 2020 [34] | Jul 17,2020 | Wuhan, China | 1663(838/825) | 864 | 799 | 64(52–71) | ①,②,③,④,⑤,⑥,⑦,⑧,⑨,⑩,⑪ |
| Wang et al. 2020c [35] | Jul 18,2020 | Wuhan, China | 483(218/265) | 421 | 62 | 48.4(SD = 12.4) | ①,②,③,④,⑤,⑦,⑧,⑲, ⑳ |
| Lee et al.2020 [36] | Jul 21,2020 | Daegu, Korea | 694(212/482) | 137 | 557 | 52.1(SD = 18.29) | ①,④,⑤,⑦,⑧,⑨,⑩,⑪ |
| Xu et al. 2020 [37] | Jul 25,2020 | Wuhan, China | 88(36/52) | 41 | 47 | 57.11(SD = 15.39) | ①,④,⑤,⑦,⑧,⑨ |
| Wei et al. 2020 [38] | Jul 29,2020 | Wuhan, China | 276(155/121) | 14 | 262 | 51(41–58) | ①,②,③,④,⑤,⑥,⑦,⑧,⑨, ⑲, ⑳ |
| Liu et al. 2020 [39] | Aug 5,2020 | Jiangsu, China | 625(329/296) | 64 | 561 | 44.44(SD = 17.19) | ①,②,④,⑤ |
| Wang et al. 2020d [40] | Aug 25,2020 | Wuhan, China | 110(48/62) | 38 | 72 | NA | ①,③,④,⑤,⑥ |
| Ishii et al. 2020 [41] | Sep 10,2020 | Japan | 345(198/147) | 112 | 233 | 54(32–68) | ①,④,⑤,⑥,⑦,⑧,⑨,⑩, ⑪ |
| Shu et al. 2020 [42] | Sep 14,2020 | Wuhan, China | 293(135/158) | 86 | 207 | 57.1(SD = 15.6) | ①,②,④,⑤,⑥,⑧,⑪ |
| Du et al. 2020 [43] | Sep 21,2020 | Wuhan, China | 164(84/80) | 29 | 135 | 61.8(SD = 13.6) | ①,②,③,④,⑤,⑦,⑧,⑨, ⑪,⑲ |
| Xiong et al. 2020 [44] | Oct 22,2020 | Wuhan,China | 116(60/36) | 55 | 61 | 58.5(47–69) | ①,②,④,⑤,⑥,⑦,⑧,⑩, ⑫,⑬,⑭ |
| Lee et al. 2020b [45] | Nov 18,2020 | Korea | 7339(2970/4369) | 927 | 6412 | 47.1(SD = 19.0) | ①,②,④,⑤,⑦,⑧,⑨,⑪ |
| Kim et al. 2020 [46] | Nov 23,2020 | Uzbekistan | 843(480/363) | 150 | 693 | 36(26–47) | ①,②,④ |
| Ren et al. 2020 [47] | Dec 4,2020 | Wuhan, China | 129(62/67) | 40 | 89 | 50(34.5–61) | ①,②,④,⑤,⑦,⑧,⑪ |
| Vial et al. 2020 [48] | Dec 14.2020 | Santiago, Chile | 88(43/45) | 18 | 70 | 49(39.5–65) | ①,②,③,④,⑤,⑨ |
| Lv et al. 2021 [49] | Jan 1,2021 | Wuhan, China | 409(188/321) | 48 | 361 | 50.47(SD = 12.43) | ①,②,④,⑤,⑧,⑨ |
| Zhang et al. 2021a [50] | Jan 1,2021 | Jining, China | 78(50/28) | 6 | 72 | 43.82(SD = 15.91) | ①,②,③,④,⑤,⑥,⑦,⑧ |
| Zhang et al. 2021b [51] | Feb 13,2021 | Henan, China | 172(92/80) | 51 | 121 | 47.9(SD = 18.3) | ①,②,④,⑤,⑥,⑧,⑨,⑩, ⑪,⑫,⑭,⑮ |
* Zhao et al. 2020 [18] only reported median age without age range
①:sex ②:age ③:smoking history④:hypertension⑤:diabetes⑥:cerebrovascular disease ⑦:malignancy ⑧:coronary heart disease ⑨: chronic obstructive pulmonary disease (COPD)⑩:chronic liver disease ⑪: chronic kidney disease (CKD) ⑫: shock⑬: acute respiratory distress syndrome (ARDS) ⑭: acute kidney injury (AKI) ⑮: cardiac trauma ⑯: arrhythmia ⑰: disseminated intravascular coagulation (DIC) ⑱: digestive tract injury ⑲: body mass index (BMI) ⑳: asthma
NA: not available
3.2 Quality evaluation
The results of the quality evaluation of the included retrospective cohort studies are displayed in Table 2. Because of the urgent need for published results on COVID-19 during the outbreak, some studies [11–15, 18, 19, 22, 23, 27, 29, 30, 34, 40, 43, 48, 49, 51] had limited follow up times.
Table 2. Methodological quality evaluation of enrolled studies based on Newcastle-Ottawa (NOS).
| Author | Representativeness of the exposed cohort | Selection of the non- exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability | Assessment of outcome | Follow-up time | Adequacy of follow- up of cohorts | Total |
|---|---|---|---|---|---|---|---|---|---|
| Wang et al. 2020a [11] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Zhang et al. 2020a [12] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Guan et al. 2020 [13] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 6 | ||
| Wan et al. 2020 [14] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Hong et al. 2020 [15] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Zhang et al. 2020b [16] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Chen et al. 2020 [17] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Zhao et al. 2020 [18] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Zheng et al. 2020 [19] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 6 | ||
| Hu et al. 2020 [20] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Cai et al. 2020a [21] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Wang et al. 2020b [22] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Buckner et al. 2020 [23] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Yang et al. 2020 [24] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Feng et al. 2020 [25] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Suleyman et al. 2020 [26] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Cao et al. 2020 [27] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Shahriarirad et al. 2020 [28] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Nie et al. 2020 [29] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Zhang et al. 2020c [30] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Cai et al. 2020b [31] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Gregoriano et al. 2020 [32] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Ghweil et al. 2020 [33] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Yu et al. 2020 [34] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Wang et al. 2020c [35] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Lee et al.2020 [36] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Xu et al. 2020 [37] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Wei et al. 2020 [38] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Liu et al. 2020 [39] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Wang et al. 2020d [40] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Ishii et al. 2020 [41] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Shu et al. 2020 [42] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Du et al. 2020 [43] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Xiong et al. 2020 [44] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Lee et al. 2020b [45] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Kim et al. 2020 [46] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Ren et al. 2020 [47] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9 |
| Vial et al. 2020 [48] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 8 | |
| Lv et al. 2021 [49] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | 7 | ||
| Zhang et al. 2021a [50] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Zhang et al. 2021b [51] | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | 7 |
3.3 Summary of the meta-analysis for primary outcomes
We identified 15 risk factors in three categories (demographic characteristics, comorbidities, complications) that have impact on the severity of confirmed cases. All statistically significant factors in our analysis are summarized in Table 3.
Table 3. Results of the meta-analysis for primary outcomes.
| Risk Factors | Number of Studies | OR (95%CI) | I2 |
|---|---|---|---|
| Acute respiratory distress syndrome | 10 | 39.59 (19.99–78.41) | 48.7% |
| Shock | 11 | 21.50 (10.49–44.06) | 27.4% |
| Acute kidney injury | 10 | 8.84 (4.34–18.00) | 40.7% |
| Chronic kidney disease | 17 | 2.97 (1.63–5.41) | 68.4% |
| Chronic obstructive pulmonary disease | 24 | 2.88 (1.89–4.38) | 52.6% |
| Coronary heart disease | 33 | 2.87 (2.22–3.71) | 59.9% |
| Malignancy | 25 | 2.60 (2.00–3.40) | 11.9% |
| Cerebrovascular disease | 16 | 2.47 (1.54–3.97) | 28.4% |
| Hypertension | 39 | 2.42 (2.03–2.88) | 67.9% |
| Diabetes | 39 | 2.40 (1.98–2.91) | 55.6% |
| Obesity | 7 | 1.89 (1.44–2.46) | 0.0% |
| Advanced age | 30 | 1.73 (1.34–2.12) | 98.6% |
| Chronic liver disease | 15 | 1.51 (1.06–2.17) | 0.0% |
| Male | 39 | 1.51 (1.33–1.71) | 50.8% |
| Smoking history | 20 | 1.40 (1.06–1.85) | 30.6% |
3.4 Demographic characteristics
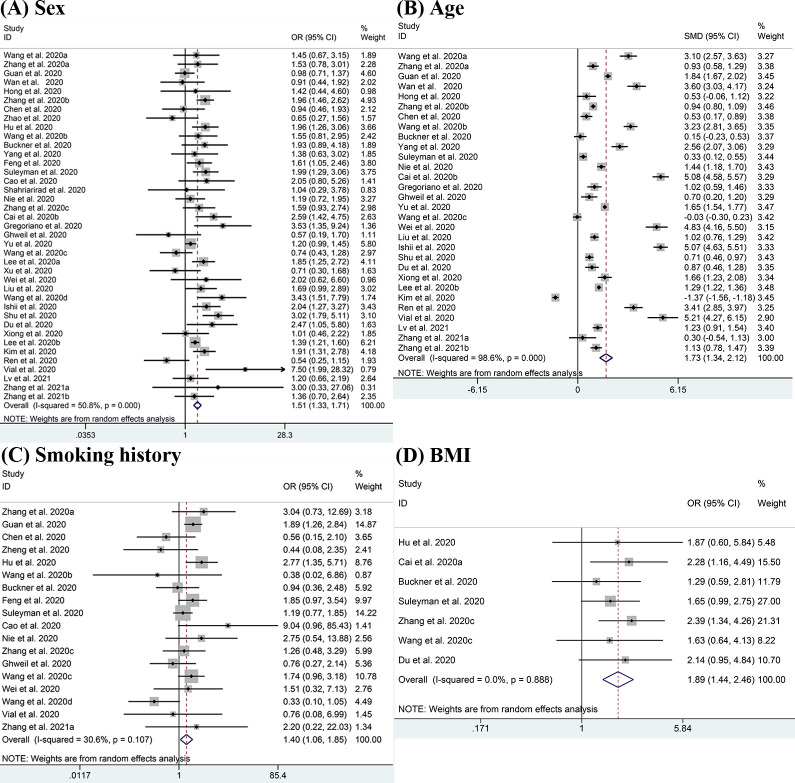
The demographic characteristics including sex, age, smoking history and BMI were pooled for meta-analysis and the results are displayed in Fig 2. There were 39 studies reporting on sex difference, and the pooled result showed that males were more likely to have severe disease than females (OR = 1.51, 95% CI:1.33–1.71; I2 = 50.8%) [11–18, 20, 22–51]. Advanced age (SMD = 1.73, 95% CI: 1.34–2.12; I2 = 98.6%) [11–17, 22–24, 26, 29, 31–35, 38, 39, 41–51] was also considered to be a risk factor for severe COVID-19. In all selected studies, the mean age of patients with severe conditions was older than those with non-severe conditions except for the studies from Wang 2020c [35] and Kim 2020 [46]. Patients with a history of smoking were also found to be positively associated with severe disease (OR = 1.40, 95% CI:1.06–1.85; I2 = 30.6%) [12, 13, 17, 19, 20, 22, 23, 25–27, 29, 30, 33, 35, 38, 40, 41, 43, 48, 50]. In studies which reported BMI, we observed higher rates of obesity (BMI≥30kg/m2) in patients with severe disease (OR = 1.89, 95% CI: 1.44–2.46; I2 = 0.0%) [20, 21, 23, 26, 30, 35].
Fig 2. Meta-analysis of the association between demographic characteristics and severe COVID-19 disease.
(A-D) Forest plots of the association between (A) sex, (B) age, (C) smoking history, (D) BMI and severe COVID-19 disease.
3.5 Comorbidities
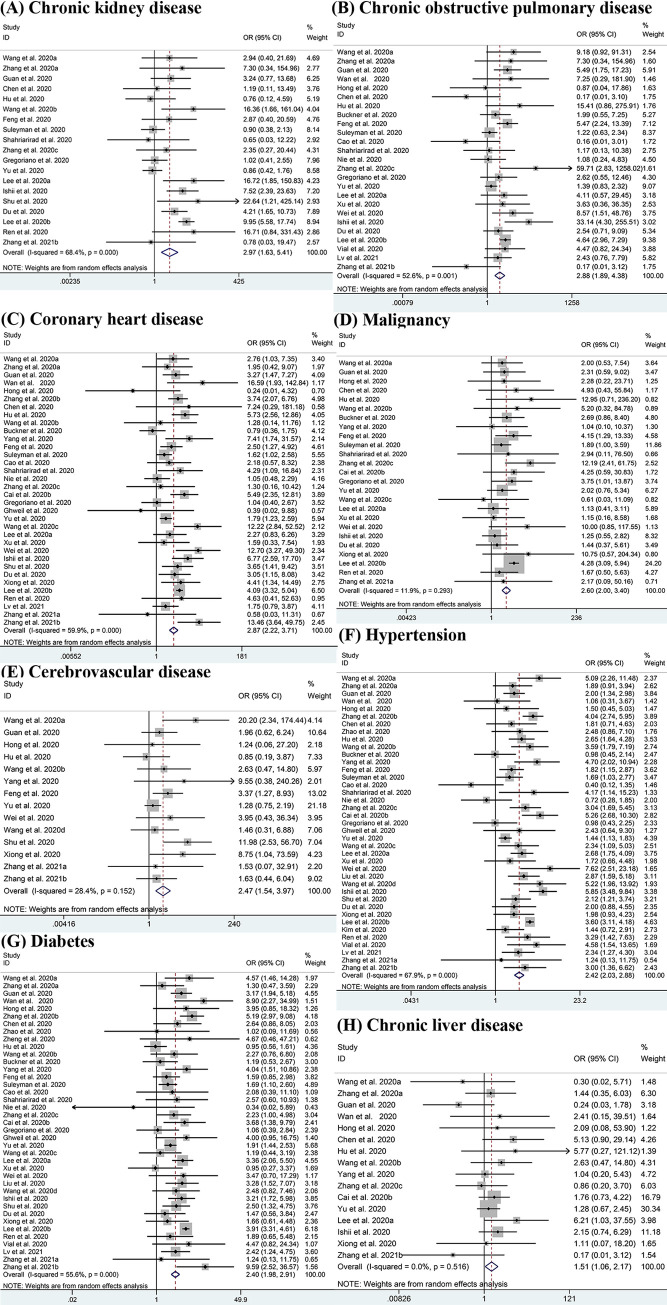
Fig 3 shows the potential association between seven comorbidities and the risk of severe COVID-19 using ORs. Compared with patients having non-severe disease, there was a higher potential for patients having severe conditions to have one or more comorbidities. Results show that CKD had the highest OR value at 2.97 (95% CI: 1.63–5.41; I2 = 68.4%) [11–13, 17, 20, 22, 25, 26, 28, 30, 32, 34, 36, 41–43, 45, 47, 51], followed by COPD with the OR of 2.88 (95% CI: 1.89–4.38; I2 = 52.6%) [11–15, 17, 20, 23, 25–30, 32, 34, 36–38, 41, 43, 45, 48, 49, 51]. Other significant outcomes included coronary heart disease (OR: 2.87, 95% CI: 2.22–3.71; I2 = 59.9%) [11–15, 17, 20, 22–38, 41–45, 47, 49–51], malignancy (OR = 2.60, 95% CI: 2.00–3.40; I2 = 11.9%) [11, 13, 15, 17, 20, 22–26, 28, 30–32, 34–38, 41, 43], cerebrovascular disease (OR = 2.47, 95% CI: 1.54–3.97; I2 = 28.4%) [11, 13, 14, 20, 22, 24, 25, 34, 38, 40, 42, 44, 50, 51], hypertension (OR = 2.42, 95% CI: 2.03–2.88; I2 = 67.9%) [11–18, 20, 22–51], diabetes (OR = 2.40, 95% CI: 1.98–2.91; I2 = 55.6%) [11–20, 22–45, 47–51] and chronic liver disease (OR = 1.51, 95% CI: 1.06–2.17; I2 = 0.0%) [11–15, 17, 20, 22–26, 28, 30–32, 34–38, 41, 43–44, 47, 50]. While the analyses of asthma (OR = 1.93, 95% CI: 0.81–4.61; I2 = 79.4%) [26, 28, 35, 38, 45] showed no significant differences between patients with severe and non-severe disease.
Fig 3. Meta-analysis of the association between comorbidities and severe COVID-19 disease.
(A-H) Forest plots of the association between (A) Chronic kidney disease, (B) Chronic obstructive pulmonary disease, (C) Coronary heart disease, (D) Malignancy, (E) Cerebrovascular disease, (F) Hypertension, (G) Diabetes, (H) Chronic liver disease and severe COVID-19 disease.
3.6 Complications
The results shown in Fig 4 indicate that ARDS (OR = 39.59, 95% CI: 19.99–78.41; I2 = 48.7%) [11, 13–15, 17, 20, 22, 24, 26, 44], shock (OR = 21.50, 95% CI: 10.49–44.06; I2 = 27.4%) [11, 13, 15, 17, 20, 22, 24, 43, 44, 51] and AKI (OR = 8.84, 95% CI: 4.34–18.00; I2 = 40.7%) [11, 13–15, 18, 20, 24, 26, 44, 51] which are potential life-threatening conditions, were clearly responsible for the ICU admissions. Additionally, some other complications like DIC (OR = 29.75, 95% CI: 3.41–259.68; I2 = 0.0%) [13, 22], secondary infection (OR = 10.03, 95% CI: 1.99–50.55; I2 = 39.0%) [14, 25], arrhythmia (OR = 9.80, 95% CI:3.91–24.60; I2 = 0.0%) [11, 12] and cardiac trauma (OR = 7.38, 95% CI:2.28–23.82; I2 = 75.0%) [11, 14, 15, 18, 24, 51] also potentially increase the severity of COVID-19. Though we lacked sufficient evidence to support the results for these other complications except for shock, ARDS and AKI, the data we already had were of high consistency. However, some complications such as hypohepatia (OR = 1.53, 95% CI: 0.71–3.30; I2 = 0.0%) [18, 24] did not show obvious association with the severity of patients’ conditions.
Fig 4. Meta-analysis of the association between complications and severe COVID-19 disease.
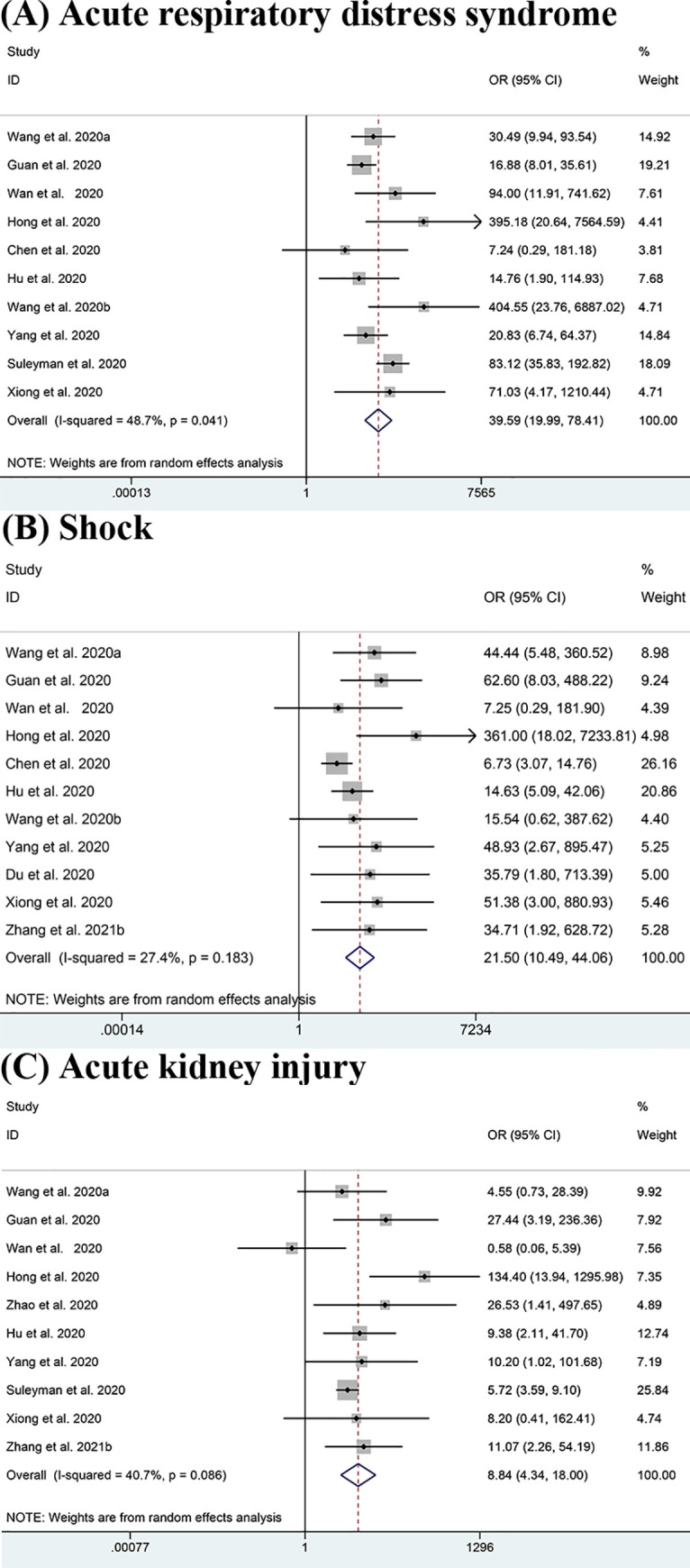
(A-C) Forest plots of the association between (A) Acute respiratory distress syndrome (ARDS), (B) Shock, (C) Acute kidney injury (AKI) and severe COVID-19 disease.
3.7 Population attributable risk
We calculated the population attributable risk (PAR) of the population infected with COVID-19. PAR reflects the proportion of severe COVID-19 that can be attributed to exposure to a risk factor. Table 4 shows that the PARs ranged from 0.9% to 11.3%, with the estimated attributable fraction in COVID-19 patients being 11.3% for hypertension and 7.1% for obesity. It is suggested that up to 11.3% and 7.1% of severe cases could have been avoided if the prevalences of hypertension and obesity were reduced.
Table 4. Population attributable risks of risk factors.
| Risk factor | Prevalence | OR | PAR |
|---|---|---|---|
| Smoking history | 0.1351 | 1.40 | 3.9% |
| Obesity | 0.1517 | 1.89 | 7.1% |
| Hypertension | 0.1926 | 2.42 | 11.3% |
| Diabetes | 0.1121 | 2.40 | 6.5% |
| Coronary heart disease | 0.0682 | 2.87 | 4.4% |
| Cerebrovascular disease | 0.0299 | 2.47 | 1.8% |
| Chronic obstructive pulmonary disease | 0.0227 | 2.88 | 1.5% |
| Chronic liver disease | 0.0278 | 1.51 | 0.9% |
| Chronic kidney disease | 0.0155 | 2.97 | 1.0% |
| Malignancy | 0.0256 | 2.60 | 1.6% |
| Shock | 0.0579 | 21.50 | 5.5% |
| Acute respiratory distress syndrome | 0.1033 | 39.59 | 10.7% |
| Acute kidney injury | 0.0838 | 8.84 | 7.4% |
3.8 Subgroup analysis and meta-regression analysis
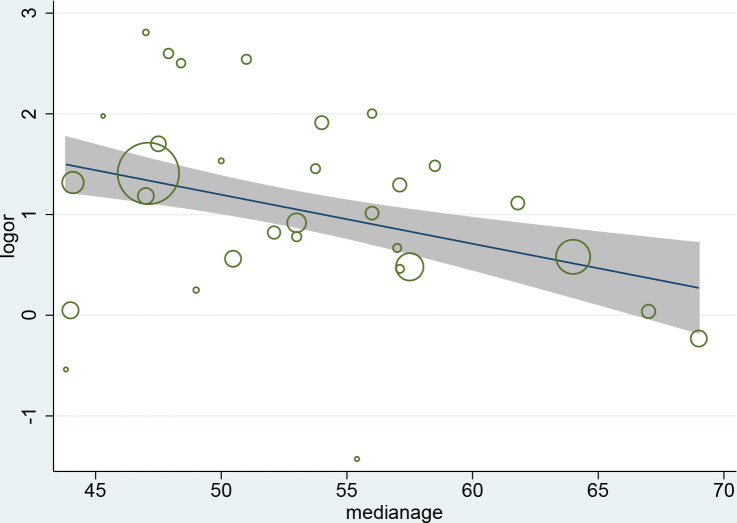
We performed subgroup analyses to identify the possible sources of heterogeneity of some outcomes. We tried to analyze several factors such as study location, publication date, sample size and patients’ average age of which study location gave a relatively meaningful result as shown in Table 5. This shows high consistency among the studies conducted in Hubei province but the heterogeneity of the studies outside Hubei province is also significant. Interestingly, the studies conducted in Hubei province show the ORs of ARDS was much lower than other regions. The meta-regression analysis demonstrates that the association between coronary heart disease and increased severity was influenced by age (P = 0.013), and the discrepancy between patients’ median ages in eligible studies partly contributed to the heterogeneity. (Fig 5)
Table 5. Subgroup analysis according to study location.
| Hubei Province | Outside Hubei Province | |||||||
|---|---|---|---|---|---|---|---|---|
| N | OR (95%CI) | I2 | P | N | OR (95%CI) | I2 | P | |
| COPD | 8 | 2.78(1.53,5.06) | 25.7% | 0.22 | 17 | 2.67(1.53,4.68) | 58.9% | 0.001 |
| CKD | 6 | 3.82(1.44,8.11) | 13.5% | 0.33 | 10 | 3.64(1.55,8.58) | 69.1% | 0.001 |
| ARDS | 5 | 25.25(12.32,51.74) | 0.0% | 0.80 | 6 | 61.22(19.03,196.94) | 67.8% | 0.008 |
| AKI | 5 | 8.65(3.42,21.85) | 0.0% | 0.90 | 5 | 9.77(2.65,36.01) | 71.1% | 0.08 |
Fig 5. Meta-regression by median age of patients.
3.9 Sensitivity analysis and publication bias
By excluding every article in turn, we conducted a sensitivity analysis and there was no evident change in either the significant outcomes or in heterogeneity. To assess the risk of publication bias, we drew a funnel plot for each factor. The results, displayed in S1 Fig, show that nearly all the funnel plots are symmetrical except for cerebrovascular disease, which suggests the risk of publication bias is low in our analysis.
4 Discussion
This study has examined the potential risk factors of severe COVID-19 such as demographic characteristics, comorbidities and complications to assist clinicians with allocation of medical resources. The higher the ORs of the risk factors, the greater the risks they bring. Our analysis has shown that males, obese patients (BMI ≥ 30kg/m2), patients with advanced age or a smoking history faced a greater risk of having severe COVID-19. This finding has also been supported by some previous studies [52–54]. However, some of the results of one meta-analysis were not consistent with our analysis, since they found gender irrelevant to the severity of COVID-19, which may possibly be due to the relatively small sample size [55]. The comorbidities including hypertension, diabetes, CKD, coronary heart disease, COPD, cerebrovascular disease and chronic liver disease could probably aggravate the illness and this outcome was consistent with other studies. [5, 7, 55–57] Complications including shock, AKI and ARDS were the main obstacles to recovery. Therefore, more attention should be paid to those obese elderly males with a history of smoking, and the above comorbidities or complications since they are more likely to develop the severe from of the disease. Although four previous studies [52, 53, 55, 57–59] have reported some risk factors for severe COVID-19, our analysis involved and reported on new factors obesity and chronic liver disease. In this study, the quality of evidence was higher since all the included studies were cohort studies rather than case-control studies, and we have included 41 eligible studies that were published from February,2020 to March, 2021, spanning a period of seven months.
Some studies have suggested that innate immunity and some factors associated with sex chromosomes may lead to the differences in susceptibility and inflammation between females and males. For instance, the X chromosome in the female has encoded some immune regulatory genes which caused lower viral load levels. TLR7, a Toll-like kind of receptor, which is higher in females than males, could enhance immune responses and boost the resistance to COVID-19 [60]. Besides, the circulating concentration of ACE2 (a functional cellular receptor of SARS-CoV-2) is higher in males than females, which could increase the susceptibility to SARS-CoV-2 [61]. Males also smoked at a higher rate than females [62] and that could result in a more vulnerable respiratory system. Therefore, it seems reasonable that women have been found to be more resistant to COVID-19. As for smoking, it suppresses the antiviral mechanisms and alters some cytokine patterns which play a role in the innate mucosal immunity [63]; the viral replication and the severity of COVID-19 would increase to some extent as a result. One study shows that smoking can also enhance the expression of ACE2 [64] and this would raise the susceptibility. With regard to age, it was evident that elderly people had a higher prevalence of comorbidities like diabetes [65] and complications like shock [66], but the OR was still significant when controlling for the above confounding factors. The natural decrease in functional reserve brought about by the physiological aging process could reduce elders’ capability to resist infections like COVID-19. Based on the analysis of an increasing number of studies reporting details of BMI, we considered obesity as a risk factor. Obesity could cause more endothelial dysfunction [67] and weaken the immunocompetent cells especially their cytotoxic cell responses [68]. The high level of ACE2 receptor expression in adipocytes may turn the adipose tissue into a viral carrier which could spread SARS-CoV-2 to other organs.
We also found some comorbidities were potentially high-risk factors for severe disease and this is consistent with other recent studies [53, 55, 57–59]. For example, as a chronic respiratory illness, COPD has already led to airflow blockage and so raises the risk of respiratory complications like ARDS. Psychologically, when patients with COPD get COVID-19, they seem to easily become very afraid and anxious [69]. Negative feelings may drive misbehavior and go against recovery, so psychological support is considered important. Though the degree varied, a large number of COVID-19 patients had hypoxaemia which may cause injury or apoptosis of cardiomyocytes [70]. As a result, patients with coronary heart disease were more likely to suffer from severer conditions like heart failure which can easily lead to death. For patients with hypertension, some kinds of blood pressure medications can enhance the expression of ACE2 and leave patients more susceptible to COVID-19 symptoms [71, 72]. However some other studies have shown that ACE2 plays an anti-inflammatory role in RAS and protect patients from ARDS [73, 74]. Therefore, the incidence of COVID-19 was lower but the severity was higher in patients with hypertension. Additionally, prolonged hypertension damages the vascular structure leaving the patients susceptible to serious infections. In terms of diabetes, this could compromise and weaken patients’ immune system thus worsening their conditions [75]. The dysfunctional pro-inflammatory cytokine responses due to diabetes could also increase the severity of COVID-19 [7]. Whether malignancy does affect the state of illness or lead to a poor prognosis is still controversial. Though our analysis showed there was a potential relationship between malignancy and severe condition, some articles had conflicting outcomes, and a few articles have even suggested that some patients with cancer may have better clinical outcomes since the possible emergence of cytokine storm was dampened because of their compromised immune systems [76, 77]. In addition to the above results, we have also found chronic renal disease (OR = 2.97, 95% CI: 1.63–5.41) was a potential risk factor for severe COVID-19, although a previous analysis had showed that it was not significantly associated with severe conditions [52]. It is likely that patients with CKD suffer from dysregulation of the immune system [78], which possibly contributed to the increase in severity. A study with similar results to ours has also reported a potential link between chronic liver disease and severe COVID-19 [79]. The hepatic insufficiency of COVID-19 patients could be worsened by potentially hepatotoxic drugs such as remdesivir, lopinavir and ritonavir used to treat the disease, causing more severe conditions [80]. More analyses need to be done in order to provide sufficient information and draw accurate conclusions about the controversial results above.
According to our analysis, ARDS, shock and AKI were the three major complications playing a role in severe conditions. Due to impaired gas exchange and serious inflammation in the alveolar space, patients with ARDS had significant need of ventilation [81]. Some studies [82, 83] suggested tissue plasminogen activator (tPA) may be useful in saving such patients’ lives in the face of lack of mechanic ventilation in some areas. AKI is prevalent among severe patients and can be fatal especially when patients required renal replacement therapy [84]. Similarly, shocked patients can die without timely treatment resulting from the lack of effective circulating blood volume. Therefore, it is essential to prevent the occurrence of the above complications and give prompt first aid treatment when such complications occur.
We believe the PAFs we calculated are meaningful for public health, because the risk of severe cases is likely to decrease in the wake of reduction in the prevalence of certain conditions. In our analysis, the top risk factor was hypertension with the score of 11.3%, indicating that though the OR of hypertension was not relatively high among all the factors, it did play a more important role than we had thought. The PAFs of ARDS (10.7%) and AKI (7.4%) were also high which showed that they possibly make a considerable contribution to the severity of COVID-19, but there are no specific clinical guidelines to prevent them. Therefore, more attention should be given to some other factors like obesity (7.1%) and diabetes (6.5%) since they can to some extent be prevented through practical guidelines [85] and public health campaigns. The other factors ranged from 0.9% to 5.5% and half of them were around 1.0%, suggesting that they exert less effects on the severity of COVID-19.
We should acknowledge that there are some limitations which may affect the accuracy of the outcomes and should be considered. First, some studies did not explicitly show their criteria for severe patients and non-severe patients, meaning the actual severity of patients with these two outcomes may not be consistent with those studies. Second, detecting significant heterogeneity in some analyses, we chose to use a random effects model to process data but did not identify the clear sources of heterogeneity through subgroup analyses. Third, the majority of the patients came from China, so they may not be representative of all patients across the world and so results should be carefully evaluated and accepted cautiously. The conclusion can be updated when more studies from outside China are published. Forth, we have tried to include studies from different cites but some articles may still include duplicated cases since they seldom mentioned the detailed composition of patient groups.
5 Conclusion
In summary, patients with COVID-19 who have the following characteristics: male gender, advanced age, a history of smoking, obesity, hypertension, diabetes, malignancy, coronary heart disease, hypertension, COPD, CKD and chronic liver disease, were more likely to develop the severe form of the disease. The emergence of complications like shock, ARDS, AKI generally increased the risk of the disease developing into the severe condition.
Supporting information
(DOC)
Funnel plot of (A) sex, (B) smoking history, (C)age, (D) BMI, (E) Chronic kidney disease, (F) Chronic obstructive pulmonary disease, (G) Coronary heart disease, (H) Malignancy, (I) Cerebrovascular disease, (J) Hypertension, (K)Diabetes, (L) Chronic liver disease, (M) Acute respiratory distress syndrome (ARDS), (N) Shock, (O) Acute kidney injury (AKI) and severe COVID-19 disease for the assessment of publication bias.
(TIF)
(DOCX)
Acknowledgments
We sincerely thank Associate Professor Yongzhen Yi for her professional opinion on statistical methods.
Abbreviations
- COVID-19
Coronavirus Disease 2019
- WHO
World Health Organization
- OR
odds ratio
- SMD
standard mean difference
- COPD
Chronic obstructive pulmonary disease
- CKD
Chronic kidney disease
- AKI
acute kidney injury
- ARDS
acute respiratory distress syndrome
- CI
confidence interval
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.World Health Organization. Coronavirus disease (COVID-19) outbreak, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#! (accessed 10 August 2020).
- 2.World Health Organization. Coronavirus disease (COVID-19) outbreak, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed 9 March 2021).
- 3.Zhang J, Wu S, Xu L. Asymptomatic carriers of COVID-19 as a concern for disease prevention and control: more testing, more follow-up. Biosci Trends. 2020/04/24. 2020;14: 206–208. 10.5582/bst.2020.03069 [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020/03/18. 2020;34: 101623. 10.1016/j.tmaid.2020.101623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lippi G, Henry BM. Chronic obstructive pulmonary disease is associated with severe coronavirus disease 2019 (COVID-19). Respir Med. 2020/05/19. 2020;167: 105941. 10.1016/j.rmed.2020.105941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berlin I, Thomas D, Le Faou AL, Cornuz J. COVID-19 and Smoking. Nicotine Tob Res. 2020/04/04. 2020;22: 1650–1652. 10.1093/ntr/ntaa059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodacki M. Severity of COVID-19 and diabetes mellitus: there is still a lot to be learned. Arch Endocrinol Metab. 2020/06/20. 2020;64: 195–196. 10.20945/2359-3997000000261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009/01/01. 2009;3: e123–30. [PMC free article] [PubMed] [Google Scholar]
- 9.Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020/03/01. 2020;7: 7. 10.1186/s40779-020-00238-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miettinen OS. Proportion of disease caused or prevented by a given exposure, trait or intervention. American journal of epidemiology. 1974;99(5):325–32. Epub 1974/05/01. 10.1093/oxfordjournals.aje.a121617 . [DOI] [PubMed] [Google Scholar]
- 11.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020/02/08. 2020;323: 1061–1069. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020/02/23. 2020;75: 1730–1741. 10.1111/all.14238 [DOI] [PubMed] [Google Scholar]
- 13.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020/02/29. 2020;382: 1708–1720. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wan S, Xiang Y, Fang W, Zheng Y, Li B, Hu Y, et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020/03/22. 2020;92: 797–806. 10.1002/jmv.25783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong KS, Lee KH, Chung JH, Shin KC, Choi EY, Jin HJ, et al. Clinical Features and Outcomes of 98 Patients Hospitalized with SARS-CoV-2 Infection in Daegu, South Korea: A Brief Descriptive Study. Yonsei Med J. 2020/05/12. 2020;61: 431–437. 10.3349/ymj.2020.61.5.431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang YT, Deng AP, Hu T, Chen XG, Zhuang YL, Tan XH, et al. [Clinical outcomes of COVID-19 cases and influencing factors in Guangdong province]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020/04/29. 2020;41: E057. 10.3760/cma.j.cn112338-20200318-00378 [DOI] [PubMed] [Google Scholar]
- 17.Chen Q, Zheng Z, Zhang C, Zhang X, Wu H, Wang J, et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Taizhou, Zhejiang, China. Infection. 2020/04/29. 2020;48: 543–551. 10.1007/s15010-020-01432-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao XY, Xu XX, Yin HS, Hu QM, Xiong T, Tang YY, et al. Clinical characteristics of patients with 2019 coronavirus disease in a non-Wuhan area of Hubei Province, China: a retrospective study. BMC Infect Dis. 2020/04/30. 2020;20: 311. 10.1186/s12879-020-05010-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zheng Y, Xiong C, Liu Y, Qian X, Tang Y, Liu L, et al. Epidemiological and clinical characteristics analysis of COVID-19 in the surrounding areas of Wuhan, Hubei Province in 2020. Pharmacol Res. 2020/05/04. 2020;157: 104821. 10.1016/j.phrs.2020.104821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu L, Chen S, Fu Y, Gao Z, Long H, Wang JM, et al. Risk Factors Associated with Clinical Outcomes in 323 COVID-19 Hospitalized Patients in Wuhan, China. Clin Infect Dis. 2020/05/04. 2020. 10.1093/cid/ciaa539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cai Q, Huang D, Ou P, Yu H, Zhu Z, Xia Z, et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020/04/03. 2020;75: 1742–1752. 10.1111/all.14309 [DOI] [PubMed] [Google Scholar]
- 22.Wang Y, Liao B, Guo Y, Li F, Lei C, Zhang F, et al. Clinical Characteristics of Patients Infected With the Novel 2019 Coronavirus (SARS-Cov-2) in Guangzhou, China. Open Forum Infect Dis. 2020/06/25. 2020;7: ofaa187. 10.1093/ofid/ofaa187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buckner FS, McCulloch DJ, Atluri V, Blain M, McGuffin SA, Nalla AK, et al. Clinical Features and Outcomes of 105 Hospitalized patients with COVID-19 in Seattle, Washington. Clin Infect Dis. 2020/05/24. 2020. 10.1093/cid/ciaa632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang Q, Xie L, Zhang W, Zhao L, Wu H, Jiang J, et al. Analysis of the clinical characteristics, drug treatments and prognoses of 136 patients with coronavirus disease 2019. J Clin Pharm Ther. 2020/05/26. 2020;45: 609–616. 10.1111/jcpt.13170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feng Y, Ling Y, Bai T, Xie Y, Huang J, Li J, et al. COVID-19 with Different Severities: A Multicenter Study of Clinical Features. Am J Respir Crit Care Med. 2020/04/11. 2020;201: 1380–1388. 10.1164/rccm.202002-0445OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit. JAMA Netw Open. 2020/06/17. 2020;3: e2012270. 10.1001/jamanetworkopen.2020.12270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cao Z, Li T, Liang L, Wang H, Wei F, Meng S, et al. Clinical characteristics of Coronavirus Disease 2019 patients in Beijing, China. PLoS One. 2020/06/20. 2020;15: e0234764. 10.1371/journal.pone.0234764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shahriarirad R, Khodamoradi Z, Erfani A, Hosseinpour H, Ranjbar K, Emami Y, et al. Epidemiological and clinical features of 2019 novel coronavirus diseases (COVID-19) in the South of Iran. BMC Infect Dis. 2020/06/20. 2020;20: 427. 10.1186/s12879-020-05128-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nie Y, Li J, Huang X, Guo W, Zhang X, Ma Y, et al. Epidemiological and clinical characteristics of 671 COVID-19 patients in Henan Province, China. Int J Epidemiol. 2020/06/27. 2020. 10.1093/ije/dyaa081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang SY, Lian JS, Hu JH, Zhang XL, Lu YF, Cai H, et al. Clinical characteristics of different subtypes and risk factors for the severity of illness in patients with COVID-19 in Zhejiang, China. Infect Dis Poverty. 2020/07/10. 2020;9: 85. 10.1186/s40249-020-00710-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cai Q, Chen F, Wang T, Luo F, Liu X, Wu Q, et al. Obesity and COVID-19 Severity in a Designated Hospital in Shenzhen, China. Diabetes Care. 2020/05/16. 2020;43: 1392–1398. 10.2337/dc20-0576 [DOI] [PubMed] [Google Scholar]
- 32.Gregoriano C, Koch D, Haubitz S, Conen A, Fux CA, Mueller B, et al. Characteristics, predictors and outcomes among 99 patients hospitalised with COVID-19 in a tertiary care centre in Switzerland: an observational analysis. Swiss Med Wkly. 2020/07/16. 2020;150: w20316. 10.4414/smw.2020.20316 [DOI] [PubMed] [Google Scholar]
- 33.Ghweil AA, Hassan MH, Khodeary A, Mohamed AO, Mohammed HM, Abdelazez AA, et al. Characteristics, Outcomes and Indicators of Severity for COVID-19 Among Sample of ESNA Quarantine Hospital’s Patients, Egypt: A Retrospective Study. Infect Drug Resist. 2020/08/09. 2020;13: 2375–2383. 10.2147/IDR.S263489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu C, Lei Q, Li W, Wang X, Li W, Liu W. Epidemiological and clinical characteristics of 1663 hospitalized patients infected with COVID-19 in Wuhan, China: a single-center experience. J Infect Public Heal. 2020/07/29. 2020;13: 1202–1209. 10.1016/j.jiph.2020.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang B, Wang Z, Zhao J, Zeng X, Wu M, Wang S, et al. Epidemiological and clinical course of 483 patients with COVID-19 in Wuhan, China: a single-center, retrospective study from the mobile cabin hospital. Eur J Clin Microbiol Infect Dis. 2020/07/20. 2020; 1–7. 10.1007/s10096-020-03927-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee JY, Hong SW, Hyun M, Park JS, Lee JH, Suh YS, et al. Epidemiological and clinical characteristics of coronavirus disease 2019 in Daegu, South Korea. Int J Infect Dis. 2020/07/24. 2020;98: 462–466. 10.1016/j.ijid.2020.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu X, Yu MQ, Shen Q, Wang LZ, Yan RD, Zhang MY, et al. Analysis of inflammatory parameters and disease severity for 88 hospitalized COVID-19 patients in Wuhan, China. Int J Med Sci. 2020/08/14. 2020;17: 2052–2062. 10.7150/ijms.47935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wei Y, Zeng W, Huang X, Li J, Qiu X, Li H, et al. Clinical characteristics of 276 hospitalized patients with coronavirus disease 2019 in Zengdu District, Hubei Province: a single-center descriptive study. BMC Infect Dis. 2020/07/31. 2020;20: 549. 10.1186/s12879-020-05252-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu S, Luo H, Wang Y, Cuevas LE, Wang D, Ju S, et al. Clinical characteristics and risk factors of patients with severe COVID-19 in Jiangsu province, China: a retrospective multicentre cohort study. BMC Infect Dis. 2020/08/09. 2020;20: 584. 10.1186/s12879-020-05314-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Y, Zhou Y, Yang Z, Xia D, Hu Y, Geng S. Clinical Characteristics of Patients with Severe Pneumonia Caused by the SARS-CoV-2 in Wuhan, China. Respiration. 2020/08/26. 2020; 1–9. 10.1159/000507940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ishii M, Terai H, Kabata H, Masaki K, Chubachi S, Tateno H, et al. Clinical characteristics of 345 patients with coronavirus disease 2019 in Japan: A multicenter retrospective study. J Infect. 2020/09/14. 2020. 10.1016/j.jinf.2020.08.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shu Z, Zhou Y, Chang K, Liu J, Min X, Zhang Q, et al. Clinical features and the traditional Chinese medicine therapeutic characteristics of 293 COVID-19 inpatient cases. Front Med. 2020/09/15. 2020; 1–16. 10.1007/s11684-020-0803-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Du H, Pan X, Liu N, Chen J, Chen X, Werring DJ, et al. The effect of vascular risk factor burden on the severity of COVID-19 illness, a retrospective cohort study. Respir Res. 2020/09/23. 2020;21: 241. 10.1186/s12931-020-01510-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiong S, Liu L, Lin F, Shi J, Han L, Liu H, et al. Clinical characteristics of 116 hospitalized patients with COVID-19 in Wuhan, China: a single-centered, retrospective, observational study. BMC infectious diseases. 2020;20(1):787. Epub 2020/10/24. 10.1186/s12879-020-05452-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee SG, Park GU, Moon YR, Sung K. Clinical Characteristics and Risk Factors for Fatality and Severity in Patients with Coronavirus Disease in Korea: A Nationwide Population-Based Retrospective Study Using the Korean Health Insurance Review and Assessment Service (HIRA) Database. International journal of environmental research and public health. 2020;17(22). Epub 2020/11/22. 10.3390/ijerph17228559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim K, Choi JW, Moon J, Akilov H, Tuychiev L, Rakhimov B, et al. Clinical Features of COVID-19 in Uzbekistan. Journal of Korean medical science. 2020;35(45):e404. Epub 2020/11/25. 10.3346/jkms.2020.35.e404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ren L, Yao D, Cui Z, Chen S, Yan H. Corona Virus Disease 2019 patients with different disease severity or age range: A single-center study of clinical features and prognosis. Medicine. 2020;99(49):e22899. Epub 2020/12/09. 10.1080/0886022X.2019.1605294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vial MR, Peters A, Pérez I, Spencer-Sandino M, Barbé M, Porte L, et al. Covid-19 in South America: clinical and epidemiological characteristics among 381 patients during the early phase of the pandemic in Santiago, Chile. BMC infectious diseases. 2020;20(1):955. Epub 2020/12/16. 10.1186/s12879-020-05665-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lv Z, Lv S. Clinical characteristics and analysis of risk factors for disease progression of COVID-19: A retrospective Cohort Study. International journal of biological sciences. 2021;17(1):1–7. Epub 2021/01/05. 10.7150/ijbs.50654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang N, Zhang H, Tang Y, Zhang H, Ma A, Xu F, et al. Risk factors for illness severity in patients with COVID-19 pneumonia: a prospective cohort study. International journal of medical sciences. 2021;18(4):921–8. Epub 2021/01/19. 10.7150/ijms.51205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang Q, Wang Z, Lv Y, Zhao J, Dang Q, Xu D, et al. Clinical features and prognostic factors of patients with COVID-19 in Henan Province, China. Human cell. 2021;34(2):419–35. Epub 2021/02/16. 10.1007/s13577-021-00499-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect. 2020/04/27. 2020;81: e16–e25. 10.1016/j.jinf.2020.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rahman A, Sathi NJ. Risk Factors of the Severity of COVID-19: a Meta-Analysis. medRxiv. 2020. 10.1111/ijcp.13916 [DOI] [PubMed] [Google Scholar]
- 54.Vardavas CI, Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis. 2020/03/25. 2020;18: 20. 10.18332/tid/119324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li J, He X, Yuan Y, Zhang W, Li X, Zhang Y, et al. Meta-analysis investigating the relationship between clinical features, outcomes, and severity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia. Am J Infect Control. 2020/06/17. 2020. 10.1016/j.ajic.2020.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lippi G, Wong J, Henry BM. Hypertension in patients with coronavirus disease 2019 (COVID-19): a pooled analysis. Pol Arch Intern Med. 2020/04/02. 2020;130: 304–309. 10.20452/pamw.15272 [DOI] [PubMed] [Google Scholar]
- 57.Liu H, Chen S, Liu M, Nie H, Lu H. Comorbid Chronic Diseases are Strongly Correlated with Disease Severity among COVID-19 Patients: A Systematic Review and Meta-Analysis. Aging Dis. 2020/06/04. 2020;11: 668–678. 10.14336/AD.2020.0502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhou Y, Yang Q, Chi J, Dong B, Lv W, Shen L, et al. Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: A systematic review and meta-analysis. Int J Infect Dis. 2020/07/30. 2020;99: 47–56. 10.1016/j.ijid.2020.07.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020/03/17. 2020;94: 91–95. 10.1016/j.ijid.2020.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Conti P, Younes A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection. J Biol Regul Homeost Agents. 2020/04/08. 2020;34: 339–343. 10.23812/Editorial-Conti-3 [DOI] [PubMed] [Google Scholar]
- 61.Sama IE, Ravera A, Santema BT, van Goor H, Ter Maaten JM, Cleland JGF, et al. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Hear J. 2020/05/11. 2020;41: 1810–1817. 10.1093/eurheartj/ehaa373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir Med. 2020/03/15. 2020;8: e20. 10.1016/S2213-2600(20)30117-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Silva A, Moreira JC, Martins SR. COVID-19 and smoking: a high-risk association. Cad Saude Publica. 2020/05/20. 2020;36: e00072020. 10.1590/0102-311x00072020 [DOI] [PubMed] [Google Scholar]
- 64.Brake SJ, Barnsley K, Lu W, McAlinden KD, Eapen MS, Sohal SS. Smoking Upregulates Angiotensin-Converting Enzyme-2 Receptor: A Potential Adhesion Site for Novel Coronavirus SARS-CoV-2 (Covid-19). J Clin Med. 2020/04/05. 2020;9. 10.3390/jcm9030841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Desai R, Singh S, Parekh T, Sachdeva S, Sachdeva R, Kumar G. COVID-19 and diabetes mellitus: A need for prudence in elderly patients from a pooled analysis. Diabetes Metab Syndr. 2020/05/22. 2020;14: 683–685. 10.1016/j.dsx.2020.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Desai R, Singh S, Parekh T, Sachdeva S, Kumar L, Sachdeva R, et al. COVID-19 and Shock: A Cautionary Tale for Elderly Patients From a Pooled Analysis. Ann Emerg Med. 2020/05/31. 2020;75: 789–791. 10.1016/j.annemergmed.2020.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sharma A, Garg A, Rout A, Lavie CJ. Association of Obesity With More Critical Illness in COVID-19. Mayo Clin Proc. 2020/08/31. 2020;95: 2040–2042. 10.1016/j.mayocp.2020.06.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hussain A, Mahawar K, Xia Z, Yang W, El-Hasani S. Obesity and mortality of COVID-19. Meta-analysis. Obes Res Clin Pr. 2020/07/15. 2020;14: 295–300. 10.1016/j.orcp.2020.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 69.Russell R. Covid-19 and COPD: A Personal Reflection. Int J Chron Obs Pulmon Dis. 2020/05/20. 2020;15: 883–884. 10.2147/COPD.S255101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020/03/13. 2020;109: 531–538. 10.1007/s00392-020-01626-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, Tallant EA, et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005/05/18. 2005;111: 2605–2610. 10.1161/CIRCULATIONAHA.104.510461 [DOI] [PubMed] [Google Scholar]
- 72.Klimas J, Olvedy M, Ochodnicka-Mackovicova K, Kruzliak P, Cacanyiova S, Kristek F, et al. Perinatally administered losartan augments renal ACE2 expression but not cardiac or renal Mas receptor in spontaneously hypertensive rats. J Cell Mol Med. 2015/03/15. 2015;19: 1965–1974. 10.1111/jcmm.12573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pranata R, Lim MA, Huang I, Raharjo SB, Lukito AA. Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: A systematic review, meta-analysis and meta-regression. J Renin Angiotensin Aldosterone Syst. 2020/05/16. 2020;21: 1470320320926899. 10.1177/1470320320926899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005/07/08. 2005;436: 112–116. 10.1038/nature03712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pal R, Bhansali A. COVID-19, diabetes mellitus and ACE2: The conundrum. Diabetes Res Clin Pr. 2020/04/03. 2020;162: 108132. 10.1016/j.diabres.2020.108132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Giannakoulis VG, Papoutsi E, Siempos II. Effect of Cancer on Clinical Outcomes of Patients With COVID-19: A Meta-Analysis of Patient Data. JCO Glob Oncol. 2020/06/09. 2020;6: 799–808. 10.1200/GO.20.00225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020/04/16. 2020;146: 110–118. 10.1016/j.jaci.2020.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Imig JD, Ryan MJ. Immune and inflammatory role in renal disease. Compr Physiol. 2013/05/31. 2013;3: 957–976. 10.1002/cphy.c120028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Oyelade T, Alqahtani J, Canciani G. Prognosis of COVID-19 in Patients with Liver and Kidney Diseases: An Early Systematic Review and Meta-Analysis. Trop Med Infect Dis. 2020/05/21. 2020;5. 10.3390/tropicalmed6010005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kulkarni A V, Kumar P, Tevethia H V, Premkumar M, Arab JP, Candia R, et al. Systematic review with meta-analysis: liver manifestations and outcomes in COVID-19. Aliment Pharmacol Ther. 2020/07/09. 2020;52: 584–599. 10.1111/apt.15916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Whyte CS, Morrow GB, Mitchell JL, Chowdary P, Mutch NJ. Fibrinolytic abnormalities in acute respiratory distress syndrome (ARDS) and versatility of thrombolytic drugs to treat COVID-19. J Thromb Haemost. 2020/04/25. 2020;18: 1548–1555. 10.1111/jth.14872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Choudhury R, Barrett CD, Moore HB, Moore EE, McIntyre RC, Moore PK, et al. Salvage use of tissue plasminogen activator (tPA) in the setting of acute respiratory distress syndrome (ARDS) due to COVID-19 in the USA: a Markov decision analysis. World J Emerg Surg. 2020/04/22. 2020;15: 29. 10.1186/s13017-020-00305-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK, Veress LA, et al. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): A case series. J Thromb Haemost. 2020/04/09. 2020;18: 1752–1755. 10.1111/jth.14828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gabarre P, Dumas G, Dupont T, Darmon M, Azoulay E, Zafrani L. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med. 2020/06/14. 2020;46: 1339–1348. 10.1007/s00134-020-06153-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes care. 2019;42(Suppl 1):S13–s28. Epub 2018/12/19. 10.2337/dc19-S002 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Funnel plot of (A) sex, (B) smoking history, (C)age, (D) BMI, (E) Chronic kidney disease, (F) Chronic obstructive pulmonary disease, (G) Coronary heart disease, (H) Malignancy, (I) Cerebrovascular disease, (J) Hypertension, (K)Diabetes, (L) Chronic liver disease, (M) Acute respiratory distress syndrome (ARDS), (N) Shock, (O) Acute kidney injury (AKI) and severe COVID-19 disease for the assessment of publication bias.
(TIF)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.