Abstract
Background
About 5% of cases of breast cancer and 10% of cases of ovarian cancer are due to an inherited predisposition. Since 1994 it has been possible to test some people at high risk for inherited mutations to the BRCA1 and BRCA2 genes. The purpose of our study was to explore how genetic testing had affected people found to have a BRCA mutation and their families, and to determine whether there was interest in a peer-support group.
Methods
All people given positive results of genetic testing for BRCA1 and BRCA2 mutations at either of 2 familial breast cancer clinics were invited to participate in a focus group and complete a questionnaire. Those who did not attend or who received positive results after the focus group were mailed the questionnaire. Information was sought on the effect of testing on cancer risk perception and worry about cancer, communication of test results to family members, attitudes toward surveillance and toward prevention options, satisfaction with clinical services, need for additional support and satisfaction with decision to undergo testing.
Results
Eight of the 27 people invited to participate in the focus group attended. Sixteen of the 26 who were mailed the questionnaire completed and returned it. Although cancer risk perception and worry increased after receipt of the test results, the participants did not regret their decision to undergo testing. Confidence in the efficacy of cancer surveillance was high. Prophylactic oophorectomy was much more acceptable than prophylactic mastectomy. Almost all (92% [22/24]) were satisfied with the clinical services they had received; however, all were dissatisfied with the lengthy wait for test results. Nine (38%) of the participants felt they would benefit from a support group.
Interpretation
Adequate resources must be made available to clinical programs providing BRCA1 and BRCA2 mutation testing to ensure appropriate pretest counselling and timely availability of results. Organization of support groups for people found to have the gene mutations should be a priority for these programs.
About 5% of cases of breast cancer and 10% of cases of ovarian cancer are due to an autosomal dominant inherited predisposition.1 The discovery of the BRCA1 gene in 1994 and the BRCA2 gene in 1995 has presented the opportunity to test appropriate people for inherited susceptibility to breast and ovarian cancer.2
Women with a mutation to the BRCA1 or BRCA2 gene have a 56% to 85% lifetime risk of acquiring breast cancer, which is often bilateral,3,4,5 and a 16% to 40% risk of ovarian cancer.3,4,5,6 Men with such a mutation have up to a 16% risk of acquiring prostate cancer,3,5 and a 6% risk of breast cancer with a BRCA2 mutation.7 Each child of a person with a BRCA mutation has a 50% chance of inheriting the mutation.
The decision whether to undergo genetic testing is very personal and complex. Our genetic testing protocols for hereditary breast cancer testing are based on the experience of the Canadian Collaborative Study of Predictive Testing for Huntington's disease.8 There is general consensus that testing be done in a supportive environment that includes counselling regarding the pros and cons of testing and the availability of formal psychological support. Once test results have been given, ongoing counselling should be available to mutation carriers.9
Results of genetic testing for BRCA1 and BRCA2 mutations have been given at the Toronto–Sunnybrook Regional Cancer Centre and North York General Hospital, Toronto, since 1996. There is little qualitative information in the literature about the experiences of people found to have a BRCA mutation and their specific needs. The objectives of our study were to obtain feedback about how genetic testing had affected people given positive results and their families, and to explore whether those with a mutation had any interest in a peer-support group in addition to routine follow-up in the familial breast cancer clinic.
Methods
Twenty-seven people with a BRCA1 or BRCA2 mutation to whom genetic test results had been given at the familial cancer clinics of the Toronto–Sunnybrook Regional Cancer Centre and North York General Hospital from February 1996 to July 1998 were contacted and asked to participate in a focus group to be held in August 1998. We did not contact subjects if they had known metastatic cancer (n = 2) or lived more than 60 km from the cancer centre (n = 3). Testing had been performed because of a strong family history of cancer, or because of Jewish ethnicity and a personal history of breast or ovarian cancer. Also in attendance at the focus group were the facilitator (a psychologist), an oncologist and 3 genetic counsellors. At the outset of the meeting, permission was obtained to audiotape the meeting, and a questionnaire was distributed to be completed as each topic was discussed.
The questionnaire, with an additional question regarding satisfaction with the decision to undergo genetic testing, was subsequently mailed to 26 people given positive test results who did not participate in the focus group: 19 who declined focus group participation, 3 who were not invited because of distance from the cancer centre, and 4 who received the results after the focus group was organized.
The questionnaire covered 9 topics: demographics, perception of cancer risk, worry about cancer, communication with immediate family members, attitudes toward surveillance, attitudes toward prevention options, satisfaction with clinical services, need for additional support, and satisfaction with decision to undergo genetic testing (mailed questionnaire only).
Subjects were asked to select from a range of risk from 0% to 100%, using increments of 10%, or from a scale from 0 (low confidence or importance) to 7 (high confidence or importance). Written comments were strongly encouraged throughout the questionnaire.
We used repeated-measures analysis of variance and the paired t-test to compare risk perception and worry about cancer in people with a previous cancer diagnosis and those without such a diagnosis from both study populations, before genetic counselling and after receiving positive genetic test results.
Results
Eight (30%) of the 27 people invited to participate in the focus group attended. Reasons for not attending included a desire to keep their genetic status a private matter or lack of interest in participating in such a group (n = 12) and logistics (n = 7). Sixteen (62%) of the 26 mailed questionnaires were completed and returned.
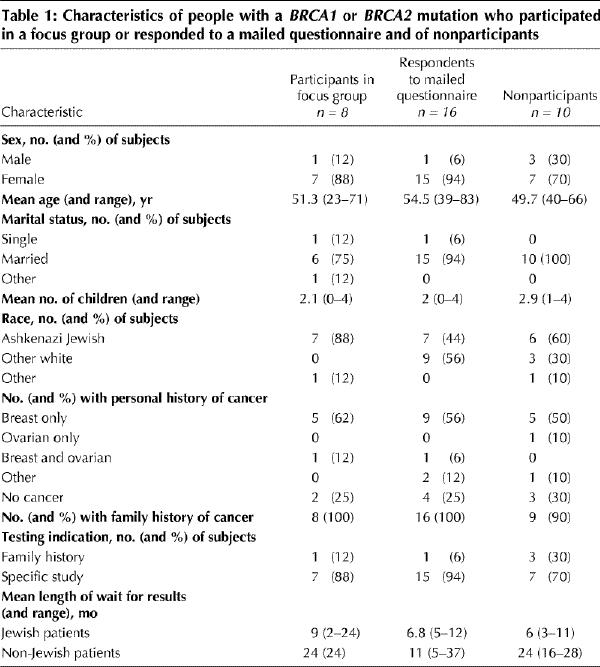
Table 1 shows the characteristics of the focus group participants, the respondents to the mailed questionnaire and the nonparticipants. The study population consisted mainly of married, middle-aged women with at least 1 child.
Table 1
Cancer risk perception
For the 18 subjects with a previous cancer diagnosis, the mean recalled estimated risk of acquiring a second cancer was 46% (range 10%–90%) before genetic counselling and 57% (range 30%–100%) after test results were received (p < 0.001, paired t-test). For the 6 participants and respondents who did not have a previous diagnosis of cancer, the mean recalled lifetime cancer risk estimate was 27.5% (range 10%–50%) before genetic counselling and 47.5% (range 15%–80%) after test results were received (p = 0.01, repeated-measures analysis of variance).
Worry about cancer
Of the 24 participants and respondents, 14 (58%) were not or a little worried about acquiring cancer, and 10 (42%) were moderately or very worried, before receiving their genetic test results. Eighteen subjects (75%) indicated that their distress level had increased after they received the test results (p = 0.002). Comments included: “Now I see cancer in my future whereas before I would have seen it in my past” and “I feel I am enveloped in a black cloud that never goes away. I fear for my children in a way I never did before.”
Communication with family members
One of the focus group participants, with a previous diagnosis of cancer, said that she had told no one in her family of her results because she “was not sure they'd want to know.” Another did not have any immediate living relatives to tell. The other 6 focus group participants and 12 (75%) of the respondents reported telling all their immediate family members of their test results. The remaining 4 respondents stated that they felt some relatives were too young to receive this sensitive information or that they did not feel close enough to certain relatives to share the results.
Reported reactions of family members were distributed fairly evenly as either “a little” (10/24 [42%]) or “moderately” (9/24 [38%]) worried about both the proband and their own risk.
Attitudes toward surveillance
Confidence in cancer surveillance was high among the 22 women: 18 (82%) indicated a confidence level of 5 to 7 for breast cancer screening, and 9 (90%) of the 10 who still had their ovaries indicated a confidence level of 5 to 7 for ovarian cancer screening. Of concern was that 1 woman with a previous diagnosis of cancer stated: “The increased vigilance has actually improved my chances of not having a recurrence ... . Prophylactic surgery will lessen the risk as well.” The 2 men indicated a confidence level of 4 and 5 for prostate cancer screening.
Attitudes toward prevention options
Only 1 subject had undergone prophylactic mastectomy, a decision made before she learned her genetic test results. Fifteen (68%) of the 22 women did not favour prophylactic mastectomy, but 9 of them would consider it if it were strongly recommended in the future.
Prophylactic oophorectomy was a much more acceptable option. Twelve (54%) of the 22 women had already had this surgery. Seven (70%) of the remaining 10 women indicated they would consider this option at a later time or were seriously considering it.
Twelve (71%) of the 17 women with a previous diagnosis of cancer were already taking tamoxifen or had completed their 5-year treatment. Thus, chemoprevention was not an option for them. However, 4 (80%) of the 5 women without a personal history of cancer reported that they would consider chemoprevention at a later date.
All of the subjects gave the highest confidence ratings to diet and lifestyle alterations (e.g., changes in exercise, alcohol consumption and smoking habits), with 77% assigning a confidence rating of 4 or greater.
Satisfaction with clinical services
Twenty-two subjects (92%) assigned a rating of 5 or greater for satisfaction with the clinical services they had received; however, all indicated their dissatisfaction with the lengthy wait for their genetic test results (Table 1).
Need for additional support
Five (62%) of the 8 focus group participants reported that they would favour a regular support group, meeting either monthly or semiannually. Most indicated that they would be happy with a peer-led group or a professionally led group. One subject commented:
It is good to listen to other experiences, to know others are feeling the same way, get helpful hints sometimes when you least expect it, sometimes a helpful book title. Also, sometimes groups help you to realize how well you are, and sometimes you help someone else just by a comment or sharing.
Only 4 (25%) of the 16 respondents indicated an interest in a support group. The other respondents felt that support from family and friends was meeting their needs.
Almost all of the subjects (22 [92%]) indicated an interest in follow-up with the genetic counselling team. The reasons stated included updates on new research studies or treatments, and an opportunity to have their psychological well-being assessed.
Satisfaction with decision to undergo genetic testing
All of the respondents indicated that they would undergo genetic testing once again, knowing everything they do now.
Interpretation
Although most of the participants in our study indicated that their perception of cancer risk and worry about cancer had increased after they learned their mutation status, none regretted the decision to undergo genetic testing. Almost 40% expressed an interest in attending an ongoing support group in addition to regular follow-up with the genetic counselling team.
A perceived benefit of genetic testing for our patients was the increased surveillance offered to those found to have a mutation. Julian-Reynier and colleagues10 found that 97% of the women in their study who participated in genetic testing perceived that their health surveillance would be improved after a positive test result. Are we providing a false sense of security? The benefits of breast cancer surveillance for women under the age of 50 years are unknown, as are the benefits of ovarian cancer surveillance for women of any age. The belief that surveillance may have any beneficial effect on the risk of occurrence or recurrence is clearly inappropriate.
Possible reasons for the much greater acceptability of prophylactic oophorectomy than of prophylactic mastectomy among the women surveyed include the issue of visible mutilation, the poorer prognosis of ovarian cancer than of breast cancer, and differences in confidence in the efficacy of breast versus ovarian cancer surveillance. These issues need further exploration.
Despite the lack of scientific evidence that diet or lifestyle changes can alter the risk of cancer in people with a BRCA mutation, our study population expressed high confidence in the effectiveness of such changes. The likely appeal of these measures is that they provide people with a feeling of some control over their destiny; moreover, such positive lifestyle changes are usually associated with a greater feeling of well-being.
The only negative comment made by the study participants about the clinical services they received was that the wait for test results was too long. The time from blood sampling to receiving results was up to 3 years. (The waiting time for the Jewish patients was significantly shorter [Table 1], since it is easier to test for specific mutations that are common in a particular ethnic group.) As testing moves from the research setting to become a clinical service, this is a concern that needs to be addressed by the allocation of appropriate human and financial resources.
Support groups have been beneficial in providing a wide range of services to individuals and families at risk for or affected with a genetic disease.11 They provide opportunities for people to share experiences about common physical or emotional health concerns, obtain emotional support and participate in collective problem-solving.12 Support groups for people with a BRCA mutation have not been reported in the literature. Our findings suggest that a significant minority of these people desire such a service.
Our results are based on a small sample and therefore should be interpreted with caution. Our subjects were mainly middle-aged white women with at least 1 child. We observed a lower perception of risk and lower distress level than reported in a review of US studies by Croyle and Lerman.13 The discrepancy may be due to the fact that most of our participants had a defined support system and were beyond the age of having to make life decisions based on their genetic results. Also, 3 issues that are not of concern in Canada may be of paramount importance in the United States: the cost of testing, potential loss of employment and insurability due to discrimination,14 and insurance coverage of surveillance and preventive surgery.
Our results can be used in future encounters with patients contemplating genetic testing. We can warn them of the unexpected negative effects that some of our patients have experienced, and perhaps better guide them in exploring the many complex issues involved. For some people the most appropriate option may be careful surveillance without testing. We must also be aware of the prevalence of misconceptions among some patients, such as exaggerated benefits of surveillance and lifestyle modification.
Since completing this study we have begun a series of facilitator-led support groups for women with a BRCA1 or BRCA2 mutation in the context of a multicentre study. The groups have the option of evolving to a peer-led group in the future.
Footnotes
This article has been peer reviewed.
Acknowledgement: We thank all the patients who gave generously of their time to participate in this study.
Competing interests: None declared.
Reprint requests to: Dr. Ellen Warner, Department of Medical Oncology, Toronto–Sunnybrook Regional Cancer Centre, 2075 Bayview Ave., Toronto ON M4N 3M5; fax 416 480-6002; Ellen.Warner@tsrcc.on.ca
References
- 1.Warner E, Heisey R, Goel V, Carroll J, McCready D. Hereditary breast cancer: risk assessment of patients with a family history of breast cancer. Can Fam Physician 1999;45:104-12. [PMC free article] [PubMed]
- 2.Heisey R, Carroll J, Warner E, McCready D. Hereditary breast cancer: identifying and managing BRCA1 and BRCA2 carriers. Can Fam Physician 1999; 45:114-24. [PMC free article] [PubMed]
- 3.Struewing JP, Hartge P, Wacholder S, Baker SM, Berlin M, McAdams M, et al. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med 1997;336:1401-8. [DOI] [PubMed]
- 4.Easton DF, Bishop DT, Ford D, Crockford GP. Breast Cancer Linkage Consortium. Genetic linkage analysis in familial breast and ovarian cancer: results from 214 families. Am J Hum Genet 1993;52:678-701. [PMC free article] [PubMed]
- 5.Ford D, Easton DF, Bishop DT, Narod SA, Goldgar DE. Breast Cancer Linkage Consortium. Risks of cancer in BRCA1 mutation carriers. Lancet 1994; 343:692-5. [DOI] [PubMed]
- 6.Ford D, Easton DF. The genetics of breast and ovarian cancer. Br J Cancer 1995;72:805-12. [DOI] [PMC free article] [PubMed]
- 7.Hoskins KF, Stopfer JE, Calzone KA, Merajver SD, Rebbeck TR, Garber JE, et al. Assessment and counseling for women with a family history of breast cancer. A guide for clinicians. JAMA 1995;273:577-85. [PubMed]
- 8.Wiggins S, Whyte P, Huggins M, Adams S, Theilmann J, Bloch M, et al. The psychological consequences of predictive testing for Huntington's disease. Canadian Collaborative Study of Predictive Testing. N Engl J Med 1992;327:1401-5. [DOI] [PubMed]
- 9.Stiefel F, Lehmann A, Guex P. Genetic detection: the need for psychosocial support in modern cancer prevention. Support Care Cancer 1997;5:461-5. [DOI] [PubMed]
- 10.Julian-Reynier C, Eisinger F, Vennin P, Chabal F, Aurran Y, Nogues C, et al. Attitudes towards cancer predictive testing and transmission of information to the family. J Med Genet 1996;33:731-6. [DOI] [PMC free article] [PubMed]
- 11.Black R, Weiss J. Genetic support groups in the delivery of comprehensive genetic services. Am J Hum Genet 1989;45:647-54. [PMC free article] [PubMed]
- 12.Peterkin A. Self-help movement experiencing rapid growth in Canada. CMAJ 1993;148(5):817-8. [PMC free article] [PubMed]
- 13.Croyle RT, Lerman C. Risk communication in genetic testing for cancer susceptibility. J Natl Cancer Inst Monogr 1999;25:59-66. [DOI] [PubMed]
- 14.Biesecker B. Psychological issues in cancer genetics. Semin Oncol Nurs 1997; 13:129-34. [DOI] [PubMed]


