Abstract
Background
Palliative care is a multidisciplinary team-based care for patients facing life-threatening illness and their families which addresses their physical, psychological, social, and spiritual needs to improve the quality of care. There is a strategy for an increase in palliative care services by integrating with the healthcare system. Therefore, this systematic review and meta-analysis was aimed to assess the overall pooled prevalence of nurses' knowledge towards palliative care in Ethiopia.
Method
PubMed/MEDLINE, HINARI, EMBASE, Scopus, Google Scholar, and African Journals OnLine (AJOL) were the databases used to search for articles. Cochrane I2 statistics and Egger's test were done to check heterogeneity and publication bias, respectively. Subgroup analysis by region, study period, and sample size was done due to the presence of heterogeneity. Sensitivity analysis was also done to detect the presence or absence of an influential study.
Result
Nine studies with a total of 2709 study participants were included in the final analysis. The overall pooled prevalence of nurses' knowledge towards palliative care was 45.57% (95% CI: 35.27–55.87). Educational status and palliative care training were significantly associated factors with the level of nurses' knowledge towards palliative care. B.S. degree holder nurses (AOR = 3.01; 95% CI: 1.50–6.02) and nurses who had palliative care training (AOR = 4.64; 95% CI: 2.37–9.08) were found to be significantly associated factors with the nurses' level of knowledge.
Conclusion
More than half of nurses had poor knowledge of palliative care. Educational status of nurses and palliative care training were significantly associated factors with the nurses' level of knowledge about palliative care. Therefore, palliative care training and improving nurses' careers through continuous professional development should be focused on regularly to improve nurses' knowledge about palliative care.
1. Introduction
Palliative care is the science of promoting the quality of life patients (adults and children) and their families, which is effective in the patient's late life and useful in relieving suffering from life-threatening terminal illness through early identification, correct assessment, treatment of pain, and other problems. It uses a team approach to address the needs of the patients and their families, including counseling, positively influencing the course of illness, and managing distressing clinical complications [1–3]. Palliative care has its standards that describe the systems and enablers necessary to deliver high-quality clinical care, and initial and ongoing assessments incorporate a patient's physical, psychological, cultural, social, and spiritual experiences and needs. The standards of palliative care also describe the explanation regarding quality management, quality improvement, and benchmarking [4]. Globally, 56,840,123 people require palliative care. It was needed for approximately 45% of all deaths in 2017 and 40% of patients in need of palliative care were aged 70 years and above [1]. Palliative care can benefit approximately 75% of people approaching the end of life. The growing number of older people and an increase of chronic illnesses in many countries including low-income settings make palliative care the center of focus [5]. Staff nurses should appropriately qualify and engage in continuous professional development and are supported in their role to provide palliative care. There are different roles of nurses regarding palliative care. These include being available on the patient's side. Nurses generally spent their time mostly with their patients to give basic care, even though the patient received care from other health professionals [6]. Nurses need to be equipped with palliative care knowledge to provide optimal care for patients suffering from chronic and serious illness and their families to improve their quality of life. However, a lack of nurses' knowledge regarding palliative care, which might be a lack of education in pain and symptom management and communication about goals of care, can result in a suboptimal and high cost of care [7]. Different studies revealed that the nurses' level of knowledge about palliative care was 44.5% in New York [8], 44.5% in Greece [9], 40% in Mongolia [10], and 43.5% in Pakistan [11], which was below the standards of the board [12]. As previous studies showed, lack of palliative care education, not participating in important aspects of health care, lack of experience, lack of proper training, few specialization units, and poor arrangement of a career ladder for nurses were found to be contributing factors for the poor knowledge of nurses about palliative care [8, 10, 12, 13]. Access to palliative care is a key quality metric that all health care organizations should improve [14].
Nurses have a prominent role in providing palliative care. Nurses must provide quality care to terminally ill and chronically sick patients. To improve the quality of life of the patients, nurses must have good knowledge of palliative care. However, little is known regarding palliative care preparedness among Ethiopian nurses. Thus, this systematic review and meta-analysis was designed to identify the level of knowledge about palliative care and associated factors among nurses in Ethiopia.
2. Methods and Materials
2.1. Study Protocol
Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) checklist for reporting of findings was used in this systematic review and meta-analysis, as shown in the supplementary file (Table S1) [15].
2.2. Databases and Search Strategies
In this systematic review and meta-analysis, PubMed/MEDLINE, HINARI, EMBASE, Google scholar, and African Journals OnLine (AJOL) searching databases were used. The published and unpublished articles from the repositories of Ethiopian universities were also searched. The searching date ranged from September 1 to September 23, 2020. Studies reporting knowledge on palliative care and associated factors among nurses in Ethiopia were included in the analysis. “Knowledge,” “awareness,” “palliative care,” “end of life care,” “caring terminally ill,” “factors,” “associated factors,” “determinant factors,” “nurses,” “hospital-based nurses,” and “Ethiopia” were searching items using “AND” and “OR” Boolean operators strings (Table 1).
Table 1.
Searches from different databases about the level of knowledge and associated factors regarding palliative care among nurses in Ethiopia.
| Databases | Searching terms | Number of studies |
|---|---|---|
| MEDLINE/PubMed | “Knowledge” OR “awareness” AND “palliative care” OR “end of life care” OR “caring terminally ill” AND “factors” OR “associated factors” OR “determinant factors” AND “nurses” OR “hospital-based nurses” AND “Ethiopia” | 88 |
| Google Scholar | “Knowledge” AND “palliative care” AND “associated factors” OR “determinant factors” AND “nurses” AND “Ethiopia” | 431 |
| Other databases | 7 | |
| Total retrieved articles | 526 | |
| Included studies | 9 |
2.3. Screening and Eligibility of Studies
After searching for accessible articles, all retrieved articles were exported into the “EndNote reference software version 8 (Thomson Reuters, Stamford, CT, USA) citation manager”. Then all articles were sorted and the duplications were removed. Two investigators (AG and AD) independently evaluated each study by title and abstracts using predetermined inclusion criteria. The eligibility of all studies for the final analysis was also assessed by critically reviewing the full text of the selected studies. In the extraction sheet, the first name of the authors, publication year, region where the study was conducted, sample size, study design, study period, level of knowledge, and factors affecting the level of knowledge were extracted. There was no discrepancy between the authors during the process of extraction, evaluation, and reviewing of the articles.
2.4. Inclusion and Exclusion Criteria
All published and unpublished cross-sectional studies conducted from January 1, 2010, to September 23, 2020, on nurses' level of knowledge about palliative care and associated factors in Ethiopia were included in this systematic review and meta-analysis. Articles that did not report outcome variables, different trials, review articles, case reports, and news were excluded from this review. Furthermore, qualitative studies, interventional studies, and studies without full text were also excluded from the final analysis.
2.5. Outcome Measurement of the Study
This systematic review and meta-analysis has two outcomes. The first outcome was the level of nurses' knowledge on palliative care, which was measured by the mean score of knowledge (good knowledge/poor knowledge) using knowledge assessing items. Thus, nurses who scored mean and above mean of knowledge assessing items were considered knowledgeable, whereas nurses who scored below the mean score of knowledge assessing items were considered not knowledgeable. The second outcome was the factors affecting the knowledge of nurses regarding palliative care.
2.6. Quality Assessment
The quality of the studies included in this systematic review was assessed using the Newcastle-Ottawa Scale (NOS) for cross-sectional studies [16] by two independent authors (AG and AD). The studies were included based on the Newcastle-Ottawa Scale's quality assessment criteria. The methodological quality, comparability, outcomes, and statistical analysis of the studies were the assessment tools used to declare the quality of studies. Studies scored on a scale of >7 out of 10 were considered as achieving high quality. All authors independently assessed the articles for consideration and inclusion in the final analysis.
2.7. Data Processing and Analysis
The inverse-variance random-effects model at 95% Cl was used to weigh the pooled prevalence of the level of knowledge regarding palliative care and its associated factors among nurses in Ethiopia [17]. We used a Microsoft Excel spreadsheet to extract and clean the data. Then, the extracted data were exported to STATA version 11 statistical software for analysis. Cochrane Q-test and I2 with its corresponding p values were used to assess the heterogeneity of studies [18]. Subgroup analysis by a region where the study was conducted, the study period, and the sample size was carried out to examine the source of heterogeneity. Sensitivity analysis was carried out to check the presence of an influential study. Egger's test was done to detect the presence of publication bias and was presented with a funnel plot [19]. A log odds ratio was used to decide the association between associated factors and the nurses' level of knowledge about palliative care. A statistical test with a p value < 0.05 was considered statistically significant.
3. Result
In this review, a total of 526 articles were retrieved using different searching databases. Of all retrieved articles, 147 articles were excluded from the analysis due to duplication. From the remaining 379 studies, 341 were further excluded after critically reviewing the titles and abstracts. Furthermore, 29 articles were excluded which did not fulfill the inclusion criteria. Finally, nine articles were included in the final analysis (Figure 1).
Figure 1.
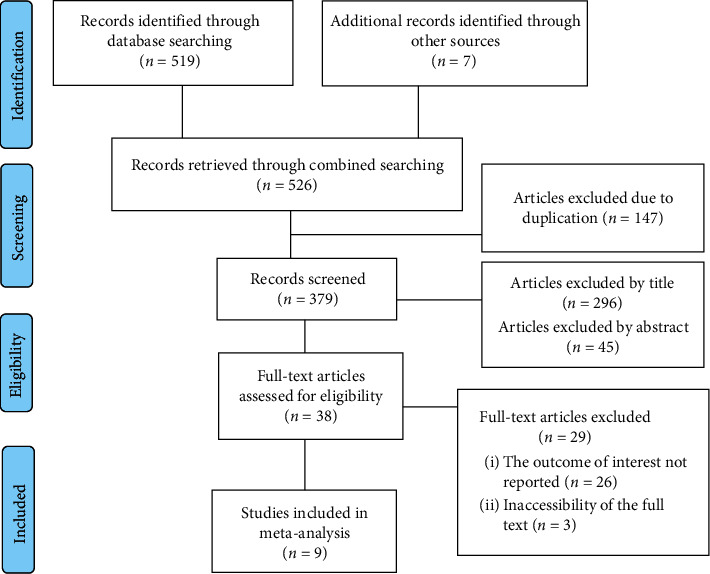
Flow chart of selection for systematic review and meta-analysis on the level of knowledge of nurses about palliative care and associated factors in Ethiopia.
3.1. Characteristics of the Studies and Study Participants
In this systematic review and meta-analysis, a total of nine articles were included with a total study population of 2709 (1137 males and 1572 females). The studies were three from the Amhara region [20–22], two from the Tigri region [23, 24], two from Addis Ababa city administration [25, 26], one from the Oromia region [27], and one from the Harar region [28]. All studies were cross-sectional in design and the sample size of the included studies ranged from 197 to 392 (Table 2).
Table 2.
Study characteristics included in the review and meta-analysis on nurse's knowledge about palliative care and associated factors in Ethiopia.
| Region | Sample size | Level of education | Experience in caring chronically ill patients | Palliative care training | Knowledge (%) | NOS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diploma | B.S. | Daily | Once/week | Once/month | Few/year | Never | Yes | No | ||||
| Tigri | 278 | 120 | 158 | 115 | 62 | 22 | 25 | 54 | — | — | 25.18 | 8 |
| Tigri | 355 | 169 | 186 | 165 | 79 | 17 | 40 | 54 | 267 | 88 | 62.82 | 8 |
| Addis Ababa | 341 | 170 | 171 | 186 | 70 | 27 | 33 | 25 | 74 | 267 | 30.50 | 9 |
| Amhara | 226 | 93 | 133 | 80 | 27 | 39 | 36 | 44 | 59 | 167 | 59.73 | 8 |
| Amhara | 331 | 45 | 286 | 153 | 78 | 48 | 4 | 48 | 62 | 269 | 38.97 | 7 |
| Amhara | 352 | 148 | 204 | — | — | — | — | — | — | — | 53.13 | 7 |
| Harar | 197 | — | — | — | — | — | — | — | 58 | 139 | 55.84 | 8 |
| Oromia | 237 | 106 | 131 | — | — | — | — | — | — | — | 58.23 | 8 |
| Addis Ababa | 392 | 57 | 335 | 271 | 56 | 18 | 37 | 10 | 112 | 280 | 26.53 | 8 |
NOS : Newcastle-Ottawa Scale; B.S. : Bachelor of Science.
3.2. Nurses' Knowledge about Palliative Care
This systematic review and meta-analysis revealed that the pooled prevalence of nurses' knowledge about palliative care in Ethiopia was 45.57% (95% CI: 35.27–55.87) (Figure 2).
Figure 2.
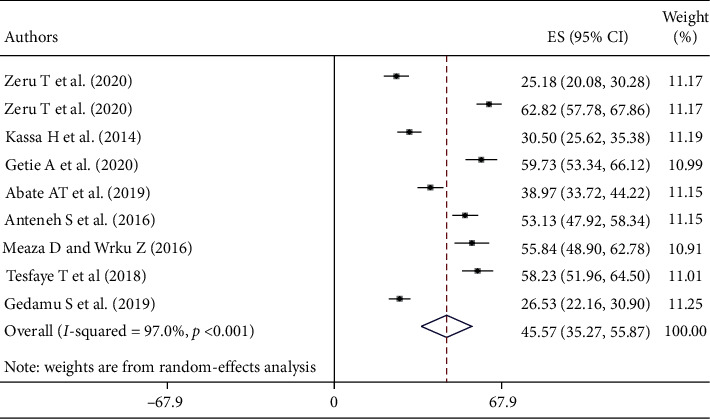
Forest plot of the pooled prevalence of nurses' knowledge about palliative care and associated factors in Ethiopia.
3.3. Heterogeneity and Subgroup Analysis
Heterogeneity was detected within the studies included in this review (I2 = 97.0%, p < 0.001). Therefore, subgroup analysis by a region where the study was conducted, the study period, and the sample size was carried out to detect the source of heterogeneity. The pooled prevalence of nurses' knowledge about palliative care was higher among nurses working in North Ethiopia, 47.93% (95% CI: 33.87–62.00). Similarly, the level of nurses' knowledge about palliative care was higher among studies conducted after 2017, 48.94% (95% CI: 34.01–63.87), and studies conducted before 2017, 41.37% (95% CI: 26.82–55.91). Higher prevalence of nurses' knowledge was reported among those studies with a sample size of <300, 49.67% (95% CI: 31.65–67.68) (Table 3).
Table 3.
Subgroup analysis on the level of nurse's knowledge about palliative care and associated factors in Ethiopia (n = 9).
| Variables | Subgroup | Studies (n) | Population | Prevalence (95% CI) | I 2 (%) | p value |
|---|---|---|---|---|---|---|
| Region | Northern Ethiopia | 5 | 1542 | 47.93 (33.87–62.00) | 97.1 | <0.001 |
| Southern Ethiopia | 4 | 1167 | 42.66 (26.78–58.45) | 97.0 | <0.001 | |
| Study period | ≥2017 | 5 | 1427 | 48.94 (34.01–63.87) | 97.2 | <0.001 |
| <2017 | 4 | 1282 | 41.37 (26.82–55.91) | 96.8 | <0.001 | |
| Sample size | <300 | 4 | 938 | 49.67 (31.65–67.68) | 97.1 | <0.001 |
| ≥300 | 5 | 1771 | 42.36 (28.71–56.01) | 97.4 | <0.001 |
Northern Ethiopia: Tigri region and Amhara region. Southern Ethiopia: Addis Ababa city administration, Oromia region, and Harar region.
3.4. Publication Bias
The results of this systematic review and meta-analysis showed that there is a symmetrical distribution of studies in the funnel plot and Egger's test was statistically insignificant (p=0.06), suggesting the absence of publication bias (Figure 3).
Figure 3.
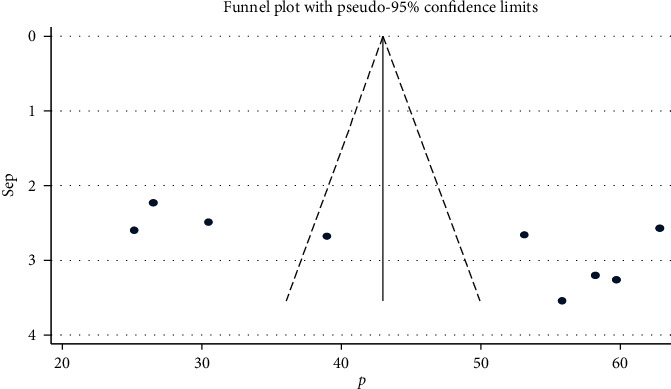
Funnel plot with 95% confidence limits of the pooled prevalence of nurses' knowledge about palliative care and associated factors in Ethiopia.
3.5. Sensitivity Analysis
The results of this study showed that none of the point estimates outside of the overall 95% confidence interval confirm that there is no influential study (Table 4).
Table 4.
Sensitivity analysis of nurse's knowledge about palliative care and associated factors in Ethiopia.
| Study omitted | Publication year | Estimated prevalence | (95% CI) |
|---|---|---|---|
| Zeru T et al. | 2020 | 48.13 | (37.62–58.64) |
| Zeru T et al. | 2020 | 43.38 | (33.22–53.55) |
| Kassa H et al. | 2014 | 47.47 | (36.31–58.64) |
| Getie a et al. | 2020 | 43.82 | (33.00–54.65) |
| Abate AT et al. | 2019 | 46.41 | (34.75–58.07) |
| Anteneh S et al. | 2016 | 44.63 | (33.27–55.99) |
| Meaza D and wrku Z | 2015 | 44.32 | (33.25–55.38) |
| Tesfaye T et al | 2018 | 44.01 | (33.07–54.94) |
| Gedamu S et al. | 2017 | 47.98 | (37.52–58.43) |
| Overall | 45.57 | (35.27–55.87) | |
CI : confidence interval.
3.6. Distribution of Nurses' Level of Education, Work Experience, and Training on Palliative Care
This systematic review and meta-analysis reported the pooled prevalence of level of education, work experience, the experience of giving care for chronically ill patients, and training on palliative care of nurses working in Ethiopia. Accordingly, more than half of the study participants were B.S. degree holder nurses, 68.96% (95% CI: 67.27–70.66). Regarding work experience, the majority of nurses had work experience of less than five years, 58.22% (95% CI: 56.52–59.92), and 50.87% (95% CI: 48.70–53. 05) of the nurses had the daily experience of giving care for chronically ill patients. Of all study participants included in this review, only 36.02% (95%CI: 34.06–37.98) were trained on palliative care (Table 5).
Table 5.
Distribution of nurse's level of education, work experience, and training on palliative care among nurses in Ethiopia.
| Valuables | Classifications | Studies | Population | Prevalence (95% CI) | I 2 (%) | p value |
|---|---|---|---|---|---|---|
| Level of education | Diploma | 8 | 908 | 31.04 (29.34–32.75) | 97.8 | <0.001 |
| B.S. | 8 | 1604 | 68.96 (67.27–70.66) | 97.8 | <0.001 | |
| Work experience | <5 years | 8 | 1398 | 58.22 (56.52–59.92) | 95.1 | <0.001 |
| 5–10 years | 8 | 648 | 25.57 (23.86–27.27) | 40.3 | 0.110 | |
| ≥10 years | 8 | 466 | 14.46 (13.12–15.79) | 95.7 | <0.001 | |
| Experience on giving care for chronically ill patient | Daily | 6 | 970 | 50.87 (48.70–53.05) | 95.1 | <0.001 |
| Once/week | 6 | 372 | 18.49 (16.76–20.21) | 80.5 | <0.001 | |
| Once/month | 6 | 171 | 07.18 (6.04–08.32) | 87.9 | <0.001 | |
| Few times/year | 6 | 175 | 04.72 (03.80–05.65) | 94.8 | <0.001 | |
| Never | 6 | 235 | 07.50 (06.36–08.65) | 96.6 | <0.001 | |
| Training on palliative care | Trained | 6 | 632 | 36.02 (34.06–37.98) | 98.9 | <0.001 |
| Not trained | 6 | 121 | 66.35 (64.40–68.29) | 98.8 | <0.001 |
3.7. Factors Associated with the Knowledge of Nurses about Palliative Care
This systematic review and meta-analysis showed that there is a significant association between training on palliative care and nurses' level of knowledge about palliative care. The odds of nurses' knowledge were 4.64 times more likely among nurses who were trained on palliative care than their counterparts (AOR = 4.64; 95% CI: 2.37–9.08) (Figure 4).
Figure 4.
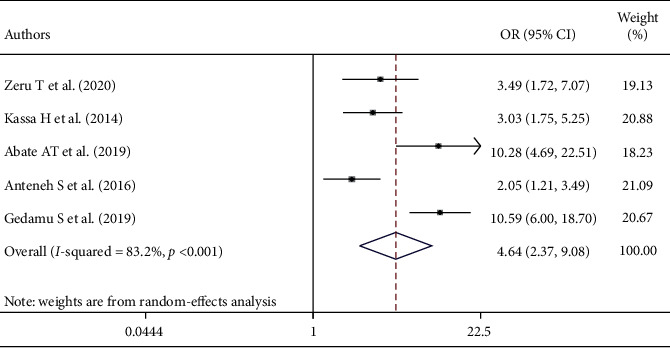
The overall pooled odds ratio of the association between training on palliative care and nurses' level of knowledge about palliative care in Ethiopia.
This study also showed that there is an association between the level of education and nurses' level of knowledge about palliative care. The odds of nurses' knowledge were 3.01 times more likely among B.S. degree holder nurses than diploma nurses (AOR = 3.01; 95% CI: 1.50–6.02) (Figure 5).
Figure 5.
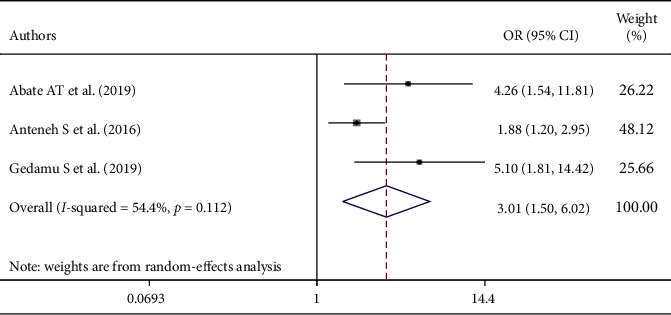
The overall pooled odds ratio of the association between educational status and nurses' level of knowledge about palliative care in Ethiopia.
4. Discussion
Providing palliative care should be a key component of the healthcare system that all healthcare organizations should strive to improve. Despite the understanding of the benefits of palliative care, many people living with chronic life-threatening illnesses do not receive palliative care. The primary challenges to apply palliative care are an overestimation of patient progress by health professionals and a low level of knowledge about palliative care. In this systematic review and meta-analysis, the pooled prevalence of the level of nurses' knowledge about palliative care in Ethiopia was 45.57% (95% CI: 35.27–55.87). This finding is almost similar to those in studies conducted in Pakistan (43.5%) [11], Greece (44.5%) [9], South Korea (48.3%) [29], Mongolia (40%) [10], Iran (39.3%) [3], Manipur (38%) [30], Saudi Arabia (36.5%) [31], India (38%) [2], Sudan (50.9%) [32], Spain (54%) [33], and South Iran (37.95%) [34]. Conversely, it is higher than those in studies done in Udupi district, India (20.5%) [35], Palestine (20.8%) [36], and Guwahati city, India (21%) [37]. The possible reason for this variation might be the integration of palliative care training with routine in the current study. The reason might be also the increase of chronic and life-threatening illness causing nurses to be exposed to giving palliative care or the variation in study participants in which the study participants of the previous studies were nursing students and all health professionals, whereas the current study includes nurses as a study subject. However, this finding is lower than that in a study done in India (67.6%) [38]. The reason might also be the variation in study setting, level of education, education about palliative care, and training on palliative care.
In the subgroup analysis, there was a variation in the level of nurses' knowledge about palliative care in the region where the studies were conducted, study period, and sample size. The higher prevalence of knowledge was reported among studies done in Northern Ethiopia, which might be due to the fact that most of the studies conducted in Northern Ethiopia were in referral hospitals. Similarly, the level of knowledge of nurses about palliative care was higher among studies conducted after 2017. This might be because the nurses included in the recent studies were trained about palliative care and most of them are B.S. degree holders.
Nurses with B.S. degree in their educational status were 3.01 times more likely knowledgeable about palliative care than diploma holders. This result is supported by studies conducted in the Northeastern region of the United States and Iran [3, 7]. This is because as the educational status of the nurses increases, their knowledge regarding palliative care is also increased due to an increment of professional knowledge, skills, and exposure to patients who need palliative care. The odds of nurses' knowledge were 4.64 times more likely among nurses who were trained on palliative care than those who were not trained on palliative care. This finding was in agreement with studies conducted in Iran, Greece, and Spain [3, 9, 31]. The possible reason might be the fact that getting updated training on palliative care raises the knowledge of nurses on palliative care.
5. Conclusion
This study revealed that more than half of the nurses had poor knowledge about palliative care. In this regard, the educational status of nurses and palliative care training were significantly associated factors with the nurses' level of knowledge about palliative care. Therefore, there should be incorporation of palliative care in the nursing curriculum. Furthermore, palliative care training and continuous education should be given regularly for nurses to improve their knowledge about palliative care.
5.1. Strength and Limitations of the Study
This review covers a wide area and accessed different articles making the review more accurate, and a subgroup and sensitivity analysis was carried out, which overcomes heterogeneity and checks the presence of influential studies. However, this study includes only studies with a cross-sectional design, which may be limited to generate a cause-effect link. It also sticks to the meta-analysis of observational studies in epidemiology.
Abbreviations
- AJO:
African Journals OnLine
- AOR:
Adjusted odds ratio
- B.S.:
Bachelor of Science
- CI:
Confidence Interval
- NOS:
Newcastle-Ottawa Scale
- PRISMA:
Preferred Reporting Items for Systematic Review and Meta-analysis.
Data Availability
All the related data have been presented within the manuscript. The dataset supporting the conclusions of this article is available from the authors upon request.
Conflicts of Interest
The authors declare that they have no competing interests to declare.
Authors' Contributions
AG and AD designed the study and designed and ran the literature search. All the authors (AG, AW, MB, GG, and AD) acquired the data, screened the records, extracted the data, and assessed the risk of bias. AG and AD carried out statistical analyses and wrote the report. All authors provided critical conceptual input, analyzed and interpreted the data, and critically revised the report. All authors read and approved the final manuscript.
Supplementary Materials
Table S1: Preferred Reporting Items for Systematic Review and Meta-analysis guideline for reporting of the findings.
References
- 1.World health organization, Connor S. R. Global Atlas of Palliative Care. 2nd. Geneva, Switzerland: World Health Organization; 2020. [Google Scholar]
- 2.Gopal K. S., Archana P. S. Awareness, knowledge and attitude about palliative care, in general, population and health care professionals in tertiary care hospital. International Journal of Scientific Study. 2016;3(10):31–35. [Google Scholar]
- 3.Paknejadi F., Hasavari F., Khaleghdoost Mohammadi T., Kazemnejad Leili E. Nurses’ knowledge of palliative care and its related factors. Journal of Holistic Nursing and Midwifery. 2019;29(4):236–242. doi: 10.32598/jhnm.29.4.236. [DOI] [Google Scholar]
- 4.Palliative Care Australia. National Palliative Care Standards. Canberra, Australia: Palliative Care Australia; 2018. [Google Scholar]
- 5.Etkind S., Bone A., Gomes B., et al. How many people will need palliative care in 2040? Past trends, future projections and implications for services. BMC Medicine. 2017;15(1):1–10. doi: 10.1186/s12916-017-0860-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sekse R. J. T., Hunskår I., Ellingsen S. The nurses’ role in palliative care: a qualitative meta‐synthesis. Journal of Clinical Nursing. 2018;27(1-2):e21–e38. doi: 10.1111/jocn.13912. [DOI] [PubMed] [Google Scholar]
- 7.Balicas D. The Effect of Palliative Care Nursing Education to Improve Knowledge in Palliative Care of Hospital-Based Nurses Caring for Patients with Chronic, Serious Illness. 2018. [Google Scholar]
- 8.Cleary A. S. Graduating nurses’ knowledge of palliative and end-of-life care. International Journal of Palliative Nursing. 2020;26(1):5–12. doi: 10.12968/ijpn.2020.26.1.5. [DOI] [PubMed] [Google Scholar]
- 9.Maria K., Evanthia V., Petros K. A., Dimitris N. Assessment of knowledge and associated factors towards palliative care among Greek nurses. Assessment. 2016;3(3) doi: 10.22158/wjssr.v3n3p381. [DOI] [Google Scholar]
- 10.Kim J. S., Kim J., Gelegjamts D. Knowledge, attitude and self-efficacy towards palliative care among nurses in Mongolia: a cross-sectional descriptive study. PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0236390.e0236390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parveen A., Sultana K., Waqas A., Tasneem S., Jabeen R., Faiz A. Knowledge and attitude of nurses about palliative care. Journal of Bioresource Management. 2020;7(1):p. 8. doi: 10.35691/jbm.0202.0122. [DOI] [Google Scholar]
- 12.Wi D. H., Kang S. J. Relationship among nurses’ knowledge, attitude towards palliative care and perception of death in neonatal intensive care units. Child Health Nursing Research. 2016;22(4):257–264. doi: 10.4094/chnr.2016.22.4.257. [DOI] [Google Scholar]
- 13.Fauziningtyas R., Widowati E. R., Indarwati R., Asmoro C. P. Determinants of knowledge and attitude related to palliative care nurses. International Journal of Psychosocial Rehabilitation. 2020;24(7) [Google Scholar]
- 14.Avati A., Jung K., Harman S., Downing L., Ng A., Shah N. H. Improving palliative care with deep learning. BMC Medical Informatics and Decision Making. 2018;18(4):p. 122. doi: 10.1186/s12911-018-0677-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D., Liberati A., Tetzlaff J., Altman D. G., Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine. 2009;6(7) doi: 10.1371/journal.pmed.1000097.e1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peterson J., Welch V., Losos M., Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Ottawa, Canada: Ottawa Hospital Research Institute; 2011. [Google Scholar]
- 17.Borenstein M., Hedges L. V., Higgins J. P. T., Rothstein H. R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 18.Rücker G., Schwarzer G., Carpenter J. R., Schumacher M. Undue reliance on I 2 in assessing heterogeneity may mislead. BMC Medical Research Methodology. 2008;8(1):p. 79. doi: 10.1186/1471-2288-8-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Egger M., Smith G. D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abate A. T., Amdie F. Z., Bayu N. H., Gebeyehu D. Knowledge, attitude and associated factors towards end of life care among nurses’ working in Amhara Referral Hospitals, Northwest Ethiopia: a cross-sectional study. BMC Research Notes. 2019;12(1):p. 521. doi: 10.1186/s13104-019-4567-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Getie A., Wondmieneh A., Mengesha A., Fitwi A., Gedefaw G., Demis A. Assessment of knowledge and attitude towards palliative care and associated factors among nurses working in North Wollo hospitals. Ethiopian Journal of Health Sciences. 2021;31(2):p. 393. doi: 10.1186/s13104-019-4567-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anteneh S., Kassa H., Demeke T., Guadu T. Assessment of nurses’ knowledge, attitude, practice and associated factors towards palliative care: in the case of Amhara region hospitals. Advances in Biological Research. 2016;10(2):110–123. [Google Scholar]
- 23.Zeru T., Berihu H., Gerensea H., Teklay G., Teklu T., Gebrehiwot H. Assessment of knowledge and attitude towards palliative care and associated factors among nurses working in selected Tigray hospitals, northern Ethiopia: a cross-sectional study. The Pan African Medical Journal. 2020;35(121) doi: 10.11604/pamj.2020.35.121.17820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeru T., Gerensea H., Berihu H., Zeru M., Wubayehu T. Nurses practice towards palliative care in Shire Endasilasie health facilities, Northern Ethiopia: a cross-sectional study. The Pan African Medical Journal. 2020;35(110) doi: 10.11604/pamj.2020.35.110.18648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kassa H., Murugan R., Zewdu F., Hailu M., Woldeyohannes D. Assessment of knowledge, attitude and practice and associated factors towards palliative care among nurses working in selected hospitals, Addis Ababa, Ethiopia. BMC Palliative Care. 2014;13(1):p. 6. doi: 10.1186/1472-684x-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gedamu S. Knowledge and Attitude of Nurses towards Palliative Care in Government Health Hospitals of Addis Ababa, Ethiopia. Addis Ababa, Ethiopia: Addis Ababa University; 2016. [Google Scholar]
- 27.Tesfaye T., Anbessie Y., Gizaw A. B. Palliative care practice and associated factors among nurses working in jimma university medical center south-west Ethiopia. Practice. 2017;18:p. 24. [Google Scholar]
- 28.Meaza D., Worku Z. Knowledge, attitude and practice of nurses towards palliative care in Harari national regional state, eastern Ethiopia. European Journal of Public Health. 2015;25(3):476–479. [Google Scholar]
- 29.Kim S., Hwang W. J. Palliative care for those with heart failure: nurses’ knowledge, attitude, and preparedness to practice. European Journal of Cardiovascular Nursing. 2014;13(2):124–133. doi: 10.1177/1474515113519521. [DOI] [PubMed] [Google Scholar]
- 30.Christina S., Shantibala K., Akoijam B. S., Pulu J. Knowledge of Palliative Care Among Nurses in a Tertiary Hospital in Manipur.
- 31.Khraisat O. M., Hamdan M., Ghazzawwi M. Palliative care issues and challenges in Saudi Arabia: knowledge assessment among nursing students. Journal of Palliative Care. 2017;32(3-4):121–126. doi: 10.1177/0825859717743229. [DOI] [PubMed] [Google Scholar]
- 32.Bilal M. The knowledge of palliative care and the attitude toward it among the nurses at Sabia General Hospital 2018. Sudan Journal of Medical Sciences. 2018;13(4):301–310. doi: 10.18502/sjms.v13i4.3606. [DOI] [Google Scholar]
- 33.Chover-Sierra E., Martínez-Sabater A., Lapeña-Moñux Y. Knowledge in palliative care of nursing professionals at a Spanish hospital. Revista latino-americana de enfermagem. 2017;25 doi: 10.1590/1518-8345.1610.2847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Iranmanesh S., Razban F., Tirgari B., Zahra G. Nurses’ knowledge about palliative care in Southeast Iran. Palliative and Supportive Care. 2014;12(3):203–210. doi: 10.1017/s1478951512001058. [DOI] [PubMed] [Google Scholar]
- 35.Karkada S., Nayak B., Malathi Awareness of palliative care among diploma nursing students. Indian Journal of Palliative Care. 2011;17(1):p. 20. doi: 10.4103/0973-1075.78445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ayed A., Sayej S., Harazneh L., Fashafsheh I., Eqtait F. The nurses’ knowledge and attitudes towards the palliative care. Journal of Education and Practice. 2015;6(4):91–99. [Google Scholar]
- 37.Sorifa B., Mosphea K. Knowledge and practice of staff nurses on palliative care. International Journal of Health Research and Medico-Legal Practice. 2015;1(2):41–45. [Google Scholar]
- 38.Storey S. L., Ziemba-Davis M. Knowledge of palliative care: an evaluation of oncology, intensive care, and heart failure nurses. Journal of Hospice and Palliative Nursing. 2013;15(5):307–315. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Preferred Reporting Items for Systematic Review and Meta-analysis guideline for reporting of the findings.
Data Availability Statement
All the related data have been presented within the manuscript. The dataset supporting the conclusions of this article is available from the authors upon request.


