Abstract
Background
All major guidelines for antihypertensive therapy recommend weight loss. Dietary interventions that aim to reduce body weight might therefore be a useful intervention to reduce blood pressure and adverse cardiovascular events associated with hypertension.
Objectives
Primary objectives
To assess the long‐term effects of weight‐reducing diets in people with hypertension on all‐cause mortality, cardiovascular morbidity, and adverse events (including total serious adverse events, withdrawal due to adverse events, and total non‐serious adverse events).
Secondary objectives
To assess the long‐term effects of weight‐reducing diets in people with hypertension on change from baseline in systolic blood pressure, change from baseline in diastolic blood pressure, and body weight reduction.
Search methods
For this updated review, the Cochrane Hypertension Information Specialist searched the following databases for randomised controlled trials up to April 2020: the Cochrane Hypertension Specialised Register, CENTRAL (2020, Issue 3), Ovid MEDLINE, Ovid Embase, and ClinicalTrials.gov. We also contacted authors of relevant papers about further published and unpublished work. The searches had no language restrictions.
Selection criteria
We included randomised controlled trials (RCTs) of at least 24 weeks' duration that compared weight‐reducing dietary interventions to no dietary intervention in adults with primary hypertension.
Data collection and analysis
Two review authors independently assessed risks of bias and extracted data. Where appropriate and in the absence of significant heterogeneity between studies (P > 0.1), we pooled studies using a fixed‐effect meta‐analysis. In case of moderate or larger heterogeneity as measured by Higgins I2, we used a random‐effects model.
Main results
This second review update did not reveal any new trials, so the number of included trials remains the same: eight RCTs involving a total of 2100 participants with high blood pressure and a mean age of 45 to 66 years. Mean treatment duration was 6 to 36 months. We judged the risks of bias as unclear or high for all but two trials. No study included mortality as a predefined outcome. One RCT evaluated the effects of dietary weight loss on a combined endpoint consisting of the necessity of reinstating antihypertensive therapy and severe cardiovascular complications. In this RCT, weight‐reducing diet lowered the endpoint compared to no diet: hazard ratio 0.70 (95% confidence interval (CI) 0.57 to 0.87). None of the trials evaluated adverse events as designated in our protocol. The certainty of the evidence was low for a blood pressure reduction in participants assigned to weight‐loss diets as compared to controls: systolic blood pressure: mean difference (MD) −4.5 mm Hg (95% CI −7.2 to −1.8 mm Hg) (3 studies, 731 participants), and diastolic blood pressure: MD −3.2 mm Hg (95% CI −4.8 to −1.5 mm Hg) (3 studies, 731 participants). We judged the certainty of the evidence to be high for weight reduction in dietary weight loss groups as compared to controls: MD −4.0 kg (95% CI −4.8 to −3.2) (5 trials, 880 participants). Two trials used withdrawal of antihypertensive medication as their primary outcome. Even though we did not consider this a relevant outcome for our review, the results of these RCTs strengthen the finding of a reduction of blood pressure by dietary weight‐loss interventions.
Authors' conclusions
In this second update, the conclusions remain unchanged, as we found no new trials. In people with primary hypertension, weight‐loss diets reduced body weight and blood pressure, but the magnitude of the effects are uncertain due to the small number of participants and studies included in the analyses. Whether weight loss reduces mortality and morbidity is unknown. No useful information on adverse effects was reported in the relevant trials.
Plain language summary
Do weight‐loss diets affect blood pressure, and reduce the effects of high blood pressure (hypertension)?
What is high blood pressure (hypertension)?
Blood pressure is a measure of the force that your heart uses to pump blood around your body. It is usually given as two figures: the pressure when your heart pushes blood out (systolic pressure), and the pressure when your heart rests between beats (diastolic pressure). Blood pressure is considered to be high when systolic pressure is over 140 and/or diastolic pressure is over 90, often written as '140 over 90' and measured in millimetres of mercury (mm Hg). The risk of developing high blood pressure increases as you get older.
High blood pressure is one of the main causes of early death and disability around the world. It can increase people's risk of developing serious long‐term health problems, such as heart attack or stroke. Lowering blood pressure in people with hypertension reduces the number of people who develop diseases of the heart and blood vessels (cardiovascular disease), which leads to fewer deaths and cardiovascular problems.
Weight and high blood pressure
High blood pressure is often related to unhealthy lifestyle habits, such as smoking, drinking too much alcohol, being overweight and not exercising enough. All treatment guidelines recommend keeping to a healthy weight and losing weight when needed. Some people choose to lose weight by following a diet, for example, by eating less fat, or by limiting the number of calories they eat.
Why we did this Cochrane Review
We wanted to find out if following a diet to lose weight has long‐lasting effects on blood pressure, and whether it could reduce the unwanted effects of high blood pressure on people's health.
What did we do?
We searched for studies that compared the effects of following a weight‐loss diet with not following a diet, in people with high blood pressure. We were interested in the effects of the diet on blood pressure and body weight. We also wanted to know how many people experienced any unwanted effects, how many people developed cardiovascular disease, and how many people died.
We looked for randomised controlled studies, in which the treatments people received were decided at random. This type of study usually gives the most reliable evidence about the effects of a treatment.
We assessed the reliability of the evidence we found. We considered factors such as: how the studies were conducted, how many people they involved, and whether their findings were consistent across studies.
Search date: we included evidence published up to April 2020.
What we found
We found eight studies in 2100 people with high blood pressure (average age 45 to 66 years). The studies were conducted in the USA (4 studies) and Europe (4 studies), and lasted 6 months to 36 months.
None of the studies reported useful information about any unwanted effects of following a weight‐loss diet.
What are the results of our review?
A weight‐loss diet probably enabled people to lose weight (5 studies, 888 people) and may have lowered their blood pressure (3 studies; 731 people), compared with people who did not follow a diet.
We did not find enough evidence about whether following a diet affected the number of people who died or developed cardiovascular disease. Three studies reported that no‐one died during the study; only one study looked at how many people developed a cardiovascular disease.
How reliable are these results?
We are moderately confident that people with high blood pressure lose weight after following a weight‐loss diet; however, these results might change if more evidence becomes available. We are less confident about whether a weight‐loss diet lowers blood pressure, because these results are based on a small number of studies; this result is likely to change if more evidence becomes available.
Key messages
Although people with high blood pressure lost weight and had lower blood pressure after following a weight‐loss diet, compared with people who did not follow the diet, we did not find enough reliable evidence to be certain about this result. We are uncertain whether following a weight‐loss diet could reduce cardiovascular disease because we did not find enough studies that looked at this.
Summary of findings
Summary of findings 1. Weight‐reducing diets versus no weight‐reducing diets for adults with essential hypertension.
| Weight‐reducing diets compared to no weight‐reducing diets for adults with essential hypertension | ||||
|
Patient or population: Men and non‐pregnant women ≥ 18 years old with essential hypertension Intervention: Weight‐reducing diets Comparison: No weight‐reducing diets | ||||
| Outcomes | Effect estimate (95% CI) | No of Participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Total mortality | 0 versus 0 | 845 (3 studies) | ⊕⊝⊝⊝ very lowa,b,c | No death occurred in 3 of the included RCT |
|
Cardiovascular morbidity Combined endpoint: necessity of reinstating antihypertensive therapy and severe cardiovascular complications Follow‐up: 30 months |
HR 0.70 (0.57 to 0.87) |
294 (1 study) |
⊕⊝⊝⊝ very lowa,d,e | Combined outcome includes events of very different severity |
| Adverse events | ‐ | ‐ | ‐ | No useable results reported |
|
Changes in systolic blood pressure [mm Hg] from baseline to end of study |
MD −4.49 (−7.20 to −1.78) |
731 (3 studies) | ⊕⊕⊝⊝ lowa,d | ‐ |
|
Changes in diastolic blood pressure [mm Hg] from baseline to end of study |
MD −3.19 (−4.83 to −1.54) |
731 (3 studies) | ⊕⊕⊝⊝ lowa,d | ‐ |
|
Changes in body weight [kg] from baseline to end of study |
MD −3.98 (−4.79 to −3.17) |
880 (5 studies) | ⊕⊕⊕⊝ moderatea | ‐ |
| CI: confidence interval; HR: hazard ratio; MD: mean difference | ||||
| GRADE Working Group grades of evidence High certainty: Further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: We are very uncertain about the estimate. | ||||
aHigh risk of bias in available randomised controlled trials. bLow number of studies. cNo predefined outcome. dWide confidence intervals. eOnly 1 randomised controlled trial.
Background
Description of the condition
Hypertension is a chronic non‐communicable disease associated with an increased risk of cardiovascular mortality and morbidity. High blood pressure is one of the leading causes of premature death and disability worldwide. In 2015, 7.8 million deaths or 14% of total deaths were estimated to be related to systolic blood pressure (SBP) at or above 140 mmHg globally (Forouzanfar 2017). Lowering blood pressure levels in people with hypertension has been shown to be an effective means of reducing cardiovascular morbidity and mortality (Brunström 2018; Ettehad 2016; Thomopoulos 2014).
Epidemiological investigations have consistently revealed a positive correlation between excess body weight and the risk of high blood pressure (Lelong 2019; Nguyen 2019; WHO 2020; Zhao 2017). Several published systematic reviews of randomised controlled trials (RCTs) also support this assumption, and show that weight‐loss interventions are well‐established strategies to lower blood pressure in people with hypertension (Akonobi 2019; Aucott 2005; Dickinson 2006; Gay 2016; Horvath 2008; Stelmach‐Mardas 2016). Furthermore, high body weight and hypertension independently contribute to cardiovascular diseases (GBD 2017). However, the observation that certain variables (for example, excess body weight, high blood pressure) are quantitatively related to more cardiovascular events does not necessarily mean that lowering these variables will automatically reduce the number of cardiovascular events. This may be due to the fact that the variable in question (for example, overweight) has no impact on aetiological pathways or that the damage to the cardiovascular system is already established and is only poorly or no longer reversible. It could also be the case that the treatment is effective and does lower cardiovascular events by reducing the risk factor, but at the same time increases cardiovascular or other risks through a different mechanism. An RCT is required to prove the effectiveness of an intervention, for which, ideally, a protocol was published prospectively. Many interventions that have been recommended on the basis of associations found in epidemiological studies eventually failed to show any beneficial effect, and sometimes even did harm in subsequent RCTs, for example a large dietary‐intervention study of 8.1 years duration in 48,835 obese postmenopausal women (40% having hypertension) resulted in only a modest reduction in diastolic blood pressure and no significant reduction in any cardiovascular outcomes (Allison 2016; Howard 2006).
Nevertheless, major hypertension guidelines underline the effect of lifestyle modification as a first‐step intervention to be considered in people with hypertension (ACC‐AHA 2017; ESH‐ESC 2018; Hypertension Canada 2018; NICE 2019). Weight reduction and weight loss maintenance are mandatory lifestyle changes. Body weight may be reduced by non‐pharmacological, pharmacological, or invasive interventions. A Cochrane Review of pharmacological interventions for weight reduction in adults with essential hypertension showed that participants under therapy with orlistat or phentermine/topiramate could reduce their weight and blood pressure levels to a statistically significantly greater degree than participants in the placebo group (Siebenhofer 2016). In case of ineffectiveness of drug treatment, device‐based therapies may be considered, principally targeting the treatment of resistant hypertension (ESH‐ESC 2018).
The aim of this systematic review is to evaluate the potential beneficial and harmful long‐term effects for people with hypertension who intend to reduce their body weight with non‐pharmacological dietary interventions.
Description of the intervention
This review covers dietary interventions (with a duration of at least 24 weeks) that aim to reduce body weight (for example, dietary counselling, caloric restrictions, reduction in fat intake). We did not include other interventions such as dietary interventions with no primary intention of weight reduction, increase of physical activity or other non‐drug approaches such as stress‐reduction techniques.
How the intervention might work
Observational studies of non‐pharmacological dietary measures in people with hypertension have suggested a positive association between body weight and blood pressure. One might therefore hypothesise that a dietary intervention with the aim of reducing body weight would reduce blood pressure and adverse cardiovascular events in people with hypertension.
Why it is important to do this review
For overweight people with established hypertension, it is commonly recommended that blood pressure should first be managed by non‐pharmacological interventions, including weight reduction (ACC‐AHA 2017; ESH‐ESC 2018; Hypertension Canada 2018; NICE 2019). Since dietary interventions might support the efforts of people to reduce body weight, it is important for the physician to be informed about the efficacy and potential harms of diets before recommending them.
Other reviews and meta‐analyses have shown that non‐pharmacological weight‐reducing interventions lead to a reduction in blood pressure (Akonobi 2019; Horvath 2008IQWiG 2006). However, empirical data on the long‐term effects of those interventions to lower the risk of mortality or cardiovascular morbidity are sparse.
This systematic review is the second update of the previously‐published Cochrane Review (Siebenhofer 2010; Siebenhofer 2011; Semlitsch 2016).
Objectives
Primary objectives
To assess the long‐term effects of weight‐reducing diets in people with hypertension on all‐cause mortality, cardiovascular morbidity, and adverse events (including total serious adverse events, withdrawal due to adverse events, and total non‐serious adverse events).
Secondary objectives
To assess the long‐term effects of weight‐reducing diets in people with hypertension on change from baseline in systolic blood pressure, change from baseline in diastolic blood pressure, and body weight reduction.
Methods
Criteria for considering studies for this review
Types of studies
We included RCTs of at least 24 weeks’ duration that compared weight‐reducing dietary interventions to no dietary intervention in adults with primary hypertension. Any additional pharmacological or non‐pharmacological co‐intervention must have been administered to all randomised participants and must not have been significantly different for the treatment and control groups at baseline or during the trial.
For example, we did not include a randomised trial with exercise plus diet versus no treatment. A trial in which all randomised participants exercised, and the only difference was a weight‐reducing diet versus no treatment or placebo would have met the inclusion criteria.
Types of participants
We included men and non‐pregnant women aged 18 years or older with essential hypertension (defined as baseline systolic blood pressure of at least 140 mm Hg or baseline diastolic blood pressure of at least 90 mm Hg, or both, or people on antihypertensive treatment).
Types of interventions
Dietary intervention with the intention to reduce body weight in comparison with no dietary intervention to reduce body weight.
Types of outcome measures
We included the following outcomes:
Primary outcomes
total mortality
cardiovascular morbidity
adverse events (including total serious adverse events, withdrawal due to adverse events, and total non‐serious adverse events)
Secondary outcomes
change from baseline in systolic blood pressure
change from baseline in diastolic blood pressure
change in body weight
Search methods for identification of studies
Electronic searches
The Cochrane Hypertension Information Specialist searched the following databases, without language, publication year or publication status restrictions:
the Cochrane Hypertension Specialised Register via the Cochrane Register of Studies (CRS‐Web) (searched 14 April 2020);
the Cochrane Central Register of Controlled Trials (CENTRAL 2020, Issue 3) via the Cochrane Register of Studies (CRS‐Web) (searched 3 April 2020);
MEDLINE Ovid (from 1946 onwards), MEDLINE Ovid Epub Ahead of Print, and MEDLINE Ovid In‐Process & Other Non‐Indexed Citations (searched 3 April 2020);
Embase Ovid (from 1974 onwards) (searched 3 April 2020);
ClinicalTrials.gov (www.clinicaltrials.gov) (searched 3 April 2020);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch) (searched 6 July 2018). It was not possible to run an updated search on the ICTRP website due to the COVID‐19 pandemic.
The Information Specialist modelled subject strategies for databases on the search strategy designed for MEDLINE. Where appropriate, they were combined with subject strategy adaptations of the sensitivity‐ and precision‐maximising search strategy designed by Cochrane for identifying randomised controlled (as described in the Cochrane Handbook for Systematic Reviews of Interventions Version 6, Chapter 4 (Lefebvre 2019)). We present search strategies for major databases in Appendix 1.
Searching other resources
The Cochrane Hypertension Information Specialist searched the Hypertension Specialised Register segment (which includes searches of MEDLINE, Embase, and Epistemonikos for systematic reviews) to retrieve existing reviews relevant to this systematic review, so that we could scan their reference lists for additional trials. The Specialised Register also includes searches for controlled trials in the Allied and Complementary Medicine Database (AMED), CAB Abstracts & Global Health, CINAHL, ProQuest Dissertations & Theses and Web of Science.
We checked the bibliographies of included studies and any relevant systematic reviews identified for further references to relevant trials.
Where necessary, we contacted authors of key papers and abstracts to request additional information about their trials.
Data collection and analysis
Selection of studies
Two review authors independently screened the title and abstract of each reference identified by the search and applied the inclusion criteria. We retrieved potentially relevant studies in full and again two review authors independently decided whether these studies met the inclusion criteria. In case of disagreement, we also obtained the full article, which the two review authors inspected independently. A third review author resolved disagreements. If a resolution of the disagreement was not possible, we added the article to those 'awaiting assessment' and contacted the authors of the study for clarification. We re‐assessed the articles after receiving the authors' replies.
Data extraction and management
Two review authors independently extracted data from each included study using a standardised data extraction form. We resolved differences in data extraction by consensus, referring back to the original article. If necessary, we sought information from the authors of the primary studies. We extracted, checked, and recorded the following data.
General information, including the sponsor of the trial (specified, known, or unknown) and country of publication.
All characteristics of the trial, participants, interventions, and outcome measures were summarised as reported in the publication.
Characteristics of the trial comprised the study design, duration of the trial, method of randomisation, allocation concealment, blinding (participants, people administering treatment, outcome assessors) and testing of blinding. We reported the characteristics of randomised participants at baseline and checked the similarity of groups at baseline.
Characteristics of participants are summarised in the Characteristics of included studies table and comprise the number of participants in each group, how the participants were selected (random), exclusion criteria used, and general characteristics (e.g. age, gender, nationality, ethnicity).
Relevant information about duration of the intervention, length of follow‐up (in months), and types of dietary weight‐reducing interventions.
Data on outcome measures, including total mortality, cardiovascular morbidity (including stroke, myocardial infarction, sudden death, heart failure, etc.), total serious adverse events, withdrawals due to adverse events, total non‐serious adverse events, mean change from baseline in systolic and diastolic blood pressure, as well as change in body weight.
Assessment of risk of bias in included studies
Two review authors independently assessed trials meeting the inclusion criteria to evaluate methodological quality. We resolved any differences in opinion by discussion with a third review author. We assessed all trials meeting the inclusion criteria using the 'Risk of bias' assessment tool under the categories of adequate sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other potential biases (Higgins 2019).
We carefully evaluated important numerical data such as screened, eligible, and randomised participants, as well as intention‐to‐treat (ITT) and per‐protocol (PP) populations. We investigated attrition rates, for example dropouts, losses to follow‐up, and withdrawals. We critically appraised issues of missing data, ITT, and PP, and compared them to specifications for primary outcome parameters and power calculation.
Measures of treatment effect
We used the risk ratio (RR) with a 95% confidence interval (CI) for dichotomous variables such as total mortality, cardiovascular morbidity, total withdrawals, and withdrawals due to adverse events. We calculated the mean difference (MD) for the mean change in systolic as well as diastolic blood pressure and body weight between the groups. If the standard deviation of the mean change was not explicitly given in the study, we calculated it from confidence intervals and the standard error of the mean, or estimated it from P values.
The position of the participant during blood pressure measurement may affect the blood pressure‐lowering effect. When measurements were reported for more than one position, the order of preference was: 1) sitting; 2) standing; and 3) supine (Musini 2009).
Unit of analysis issues
We intended to consider the level at which randomisation occurred, such as cross‐over trials, cluster‐randomised trials and multiple observations for the same outcome. If more than one comparison from the same trial was eligible for inclusion in the same meta‐analysis, we either combined groups to create a single pair‐wise comparison or appropriately reduced the sample size so that the same participants did not contribute more than once (splitting the 'shared' group into two or more groups). While the latter approach offers some solution to adjusting the precision of the comparison, it does not account for correlation arising because the same set of participants was included in multiple comparisons (Deeks 2019).
Dealing with missing data
If necessary, we contacted authors of trials reporting incomplete information to provide the missing information.
Assessment of heterogeneity
We assessed heterogeneity using Higgins I2 (Higgins 2003).
Assessment of reporting biases
We tested publication bias and small‐study effects in general using the funnel plot or other corrective analytical methods, depending on the number of clinical trials included in the systematic review.
Data synthesis
We summarised data statistically if they were available, sufficiently similar, and of adequate quality. We performed data synthesis and analyses using the Cochrane Review Manager 5 software (Review Manager 5). We performed statistical analysis according to the statistical guidelines referenced in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2019). We used a fixed‐effect model for the meta‐analyses. In case of moderate or larger heterogeneity as measured by Higgins I2, we used a random‐effects model.
Subgroup analysis and investigation of heterogeneity
We performed subgroup analyses where appropriate. Heterogeneity among participants could be related to, for example, sex, age, body mass index, concomitant diseases, ethnicity, blood pressure at baseline, blood pressure goals, concomitant antihypertensive therapy, and socioeconomic status. In the case of substantial heterogeneity (I2 greater than 50%), we had planned to perform sensitivity or subgroup analyses for the following items: study quality, PP versus ITT analyses, sex, age, body mass index, concomitant diseases, ethnicity, blood pressure at baseline, blood pressure goals, concomitant antihypertensive therapy, and socioeconomic status.
Sensitivity analysis
We tested the robustness of our results where appropriate, using several sensitivity analyses (for example study quality or PP versus ITT analyses, studies with large dropout rates and losses to follow‐up).
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach to assess the certainty of the evidence (Guyatt 2011). The main results of the study, including a summary of the data, the magnitude of the effect and the overall certainty of the evidence, are presented in Table 1.
We included all primary and secondary outcomes in Table 1, listed according to priority:
Total mortality
Cardiovascular morbidity
Adverse events
Change in systolic blood pressure
Change in diastolic blood pressure
Change in body weight
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
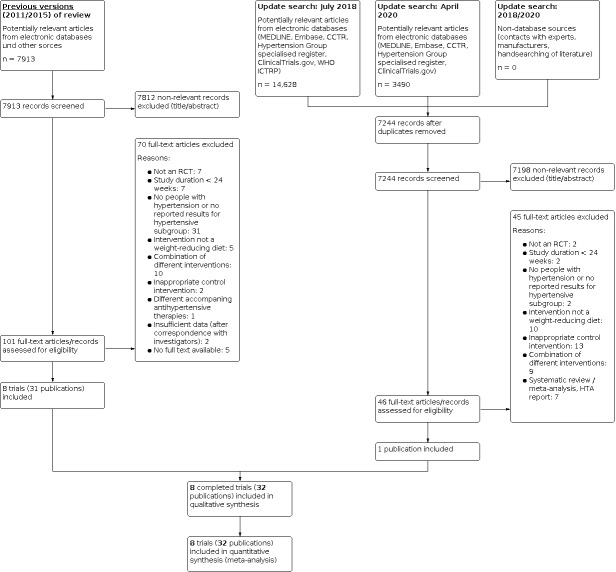
Our update searches of the electronic databases in 2018 and 2020 yielded 14,628 and 3490 records, respectively. After de‐duplication. 7244 records remained.
Of these 7244 publications, we excluded 7198 by consensus as not relevant to the question under study on the basis of their titles or abstracts, leaving 46 articles for further examination. After screening the full texts of these publications, we found only one publication that met the inclusion criteria. This article refers to a trial already included in the previous version of the review. We found no additional relevant trial for this review update. Finally, incorporating the additional publication to the 31 publications on eight trials from the previous version of the review, in this review update we include eight completed trials (32 articles/records) (see Figure 1 for details of the PRISMA statement (PRISMA 2009)).
1.
Flow diagram.
Included studies
We have provided details of the characteristics of the included trials in the Characteristics of included studies table and in Table 2; Table 3; Table 4. The following gives a brief overview of the comparisons between dietary interventions with an intention to reduce body weight and no dietary interventions to reduce body weight.
1. Overview of trial populations.
| Trial | Intervention(s) and comparator(s) | Description of power and sample size calculation | Screened/eligible (N) | Randomised (N) | Safety (N) | ITT (N) | Finishing trial (N) | Randomised finishing trial (%) | Follow‐up (extended follow‐up) |
| Cohen 1991 | diet | n.r. | 67 | 15 | n.r. | 15 | 15 | 100 | 12 months |
| no diet | 15 | n.r. | 15 | 15 | 100 | ||||
| Croft 1986 | diet | no power calculation was performed | n.r. | 66 | n.r. | 66 | 49 | 74 | 6 months |
| no diet | n.r. | 64 | n.r. | 64 | 61 | 95 | |||
| DISH 1985 | diet | n.r. | 584a | 87 | n.r. | n.r. | 67 | 77 | 13 months (56 weeks) |
| no diet | 89 | n.r. | n.r. | 77 | 87 | ||||
| Jalkanen 1991 | diet | n.r. | 25 | 25 | n.r. | n.r. | 24 | 96 | 12 months |
| no diet | 25 | 25 | n.r. | n.r. | 25 | 100 | |||
| ODES 1995 | diet | The planned sample size is 220 randomised participants. Ten per cent are expected to drop out, leaving about 200 participants to complete the 1‐year trial. The power will then be 80% for the detection of a standardized difference in response of 0.80 between two of the four randomised groups at the 5% two‐sided significance level. | 660b | 55 (n.r.)c | n.r. | n.r. | 52 (16)c | 95 (n.r.) | 12 months |
| no diet | 43 (n.r.)c | n.r. | n.r. | 43 (12)c | 100 (n.r.) | ||||
| diet + physical activity | 67 (n.r.)c | n.r. | n.r. | 65 (24)c | 97 (n.r.) | ||||
| no diet + physical activity | 54 (n.r.)c | n.r. | n.r. | 49 (20)c | 91 (n.r.) | ||||
| Ruvolo 1994 | diet | n.r. | n.r. | 16 | n.r. | n.r. | 14 | 88 | 6 months |
| no diet | 16 | n.r. | n.r. | 16 | 100 | ||||
| TAIM 1992 | diet + placebo | The sample size of about 195 within each drug group (587 total) for the weight loss component had 80% power to detect the following differences with a two‐sided α = 0.05: (1) placebo/usual failure rate of 90% vs placebo/weight loss failure rate of 60%, and (2) active drug/usual diet failure rate of 40% vs active drug/weight loss diet rate of 20%. These sample sizes also allowed for a 20% dropout rate by the end of the study. | 878b | 100d | n.r. | n.r. | 89d | 89 | 6 months (phase I) |
| no diet + placebo | 100d | n.r. | n.r. | 90d | 90 | ||||
| diet + atenolol | 96d | n.r. | n.r. | 88d | 92 | ||||
| no diet + atenolol | 99d | n.r. | n.r. | 87d | 89 | ||||
| diet + chlorthalidone | 95d | n.r. | n.r. | 86d | 91 | ||||
| no diet + chlorthalidone | 97d | n.r. | n.r. | 87d | 90 | ||||
| TONE 1998 | diet without salt restriction | The study is designed to provide greater than 80% statistical power for detecting a 30% reduction in the rate of return to antihypertensive medication associated with the weight loss intervention and a 25% reduction in the rate of return to antihypertensive medication associated with the reduced Na intervention. | 995b | 147d | 147d | 147d | n.r. | 96 to 99 | 15 to 36 months |
| no diet without salt restriction | 147d | 147d | 147d | n.r. | |||||
| diet + salt restriction | 147d | 147d | 147d | n.r. | |||||
| no diet + salt restriction | 144d | 144d | 144d | n.r. |
aParticipants in all seven study groups. bAll participants. cAll participants (hypertensive subgroup). dWeight loss component of the trial.
2. Baseline characteristics (I).
| Trial | Intervention(s) and comparator(s) | Description of participants | Nationality | Setting | Ethnic groups (%) | Duration of disease (mean years (SD)) | Antihypertensive treatment (%) |
| Cohen 1991 | diet | hypertensive and obese patients stratified by residents (residents not patients were randomised to intervention or control group) | USA | model family practice unit (Pittsburgh) | ‐ | ‐ | (number of medications: 1.6) |
| no diet | ‐ | ‐ | (number of medications: 1.2) | ||||
| Croft 1986 | diet | newly diagnosed hypertensive and obese patients | Great Britain | outpatient clinic (1 urban group practice) | ‐ | newly‐diagnosed patients | 0 |
| no diet | ‐ | 0 | |||||
| DISH 1985 | diet | people who were previously enrolled in the HDFP treated with antihypertensive drugs and who had sufficiently controlled hypertension. The dietary change on the return of hypertension after withdrawal of prolonged antihypertensive therapy (DISH) included 7 treatment arms; the results of 2 of those arms met the inclusion criteria for this review (hypertensive and obese patients with either dietary intervention or not) | USA | outpatient clinic | Black (62) | at least 5 years | 100 |
| no diet | Black (70) | 100 | |||||
| Jalkanen 1991 | diet | overweight hypertensive patients (selected from files) | Finland | outpatient clinic (2 hypertension clinics in Finland) | ‐ | ‐ | 50 |
| no diet | ‐ | ‐ | 50 | ||||
| ODES 1995 | diet | men and women ≥ 40 years old from screening programme for cardiovascular risk factors in Oslo (Norway) since 1981; participants were post‐hoc divided in tertiles according to DBP (tertile 1 DBP > 91 mm Hg, tertile 2 DBP 84 to 91 mm Hg, tertile 3 DBP < 84 mm Hg); only subgroups of tertile 1 (DBP > 91 mm Hg) will be reported here | Norwegian | outpatient clinic | ‐ | ‐ | 0 |
| no diet | ‐ | ‐ | 0 | ||||
| diet + physical activity | ‐ | ‐ | 0 | ||||
| no diet + physical activity | ‐ | ‐ | 0 | ||||
| Ruvolo 1994 | diet | overweight hypertensive patients on 10 mg amlodipine daily | Italian | outpatient clinic | ‐ | ‐ | 100 with amlodipine 10 mg |
| no diet | ‐ | ‐ | 100 with amlodipine 10 mg | ||||
| TAIM 1992 | diet + placebo | obese hypertensive patients | USA | outpatient clinic at 3 university hospitals (Bronx (New York), Birmingham (Alabama), Jackson (Mississippi)) | White (67) Black (33) |
‐ | 0 |
| no diet + placebo | White (65) Black (35) |
‐ | 0 | ||||
| diet + atenolol | White (67) Black (33) |
‐ | 100 | ||||
| no diet + atenolol | White (67) Black (33) |
‐ | 100 | ||||
| diet + chlorthalidone | White (67) Black (33) |
‐ | 100 | ||||
| no diet + chlorthalidone | White (67) Black (33) |
‐ | 100 | ||||
| TONE 1998 | diet without salt restriction | elderly, obese, and hypertensive patients; participants were assigned to active intervention: sodium reduction (S+), or weight loss, or sodium reduction (S+) and weight loss vs usual care | USA | outpatient clinic | White (73) African American (26) |
11.3 (9.2) | 100 |
| no diet without salt restriction | White (68) African American (32) |
11.6 (8.0) | 100 | ||||
| diet + salt restriction | White (76) African American (24) |
11.9 (9.5) | 100 | ||||
| no diet + salt restriction | White (70) African American (30) |
11.9 (9.3) | 100 |
3. Baseline characteristics (II).
| Trial | Intervention(s) and comparator(s) | Age (mean years (SD)) | Sex (female %) | BMI (mean kg/m² (SD)) | Body weight (mean kg (SD)) | Sitting systolic blood pressure (mean mmHg (SD)) | Sitting diastolic blood pressure (mean mmHg (SD)) | Comorbid conditions (%) |
| Cohen 1991 | diet | 59 | 73 | 34.2 | 91.8 | ‐ | ‐ | obesity (100) |
| no diet | 59.7 | 73 | 34 | 91.7 | ‐ | ‐ | obesity (100) | |
| Croft 1986 | diet | ‐ | 56 | ‐ | 86.7 (3.8) | 161 (3.5) | 98 (2.2) | obesity (100) |
| no diet | ‐ | 39 | ‐ | 82.2 (2.6) | 161 (3.5) | 96 (1.9) | obesity (100) | |
| DISH 1985 | diet | 56.1 | 68 | ‐ | 86 (17.3) | 127.6 | 80.9 | obesity (100) |
| no diet | 57.2 | 64 | ‐ | 89.8 (17.8) | 127.6 | 79.6 | obesity (100) | |
| Jalkanen 1991 | diet | ‐ | ‐ | ‐ | 86 (14) | 152 (17) | 101 (8) | ‐ |
| no diet | ‐ | ‐ | ‐ | 80 (11) | 155 (14) | 102 (7) | ‐ | |
| ODES 1995 | diet | ‐ | ‐ | 29.9 (0.7) | ‐ | 144.5 (4.5) | 97.3 (1.3) | ‐ |
| no diet | ‐ | ‐ | 30 (1.3) | ‐ | 137.5 (2.5) | 95.6 (1.1) | ‐ | |
| diet + physical activity | ‐ | ‐ | 29.6 (0.9) | ‐ | 142.8 (2.4) | 97 (0.9) | ‐ | |
| no diet + physical activity | ‐ | ‐ | 29.5 (0.8) | ‐ | 139.5 (2.0) | 96.4 (1.1) | ‐ | |
| Ruvolo 1994 | diet | ‐ | ‐ | 34 (4) | 98 (8) | 178 (8) | 107 (5) | obesity |
| no diet | ‐ | ‐ | 34 (3) | 97 (8) | 176 (8) | 106 (5) | obesity | |
| TAIM 1992 | diet + placebo | 48.6 | 41 | ‐ | 90 | 142.1 | 93.9 | Smokers (14) Alcohol use (≥ 1 drink/week) (35) |
| no diet + placebo | 46.8 | 59 | ‐ | 86 | 143.5 | 92.7 | Smokers (15) Alcohol use (≥ 1 drink/week) (37) |
|
| diet + atenolol | 48 | 48 | ‐ | 86 | 143.6 | 94.1 | Smokers (13.5) Alcohol use (≥ 1 drink/week) (36.5) |
|
| no diet + atenolol | 47.5 | 36 | ‐ | 89 | 140.5 | 92.7 | Smokers (20.2) Alcohol use (≥ 1 drink/week) (44.4) |
|
| diet + chlorthalidone | 47.4 | 51 | ‐ | 87 | 138 | 91.6 | Smokers (17.9) Alcohol use (≥ 1 drink/week) (38.9) |
|
| no diet + chlorthalidone | 48.8 | 40 | ‐ | 89 | 141.9 | 92.4 | Smokers (13.4) Alcohol use (≥ 1 drink/week) (42.3) |
|
| TONE 1998 | diet without salt restriction | 66 (5) | 51 | 31 (2.3) | 87 (10) | 130 (9) | 72 (8) | Smokers (3) Alcohol use (≥ 1 drink/week) (35) |
| no diet without salt restriction | 66 (4) | 59 | 31.3 (2.3) | 86 (10) | 128 (10) | 72 (7) | Smokers (5) Alcohol use (≥ 1 drink/week) (32) |
|
| diet + salt restriction | 66 (4) | 44 | 31.2 (2) | 86 (10) | 129 (9) | 72 (7) | Smokers (7) Alcohol use (≥ 1 drink/week) (43) |
|
| no diet + salt restriction | 66 (4) | 56 | 31.2 (2.5) | 88 (11) | 129 (9) | 72 (8) | Smokers (5) Alcohol use (≥ 1 drink/week) (36) |
All eight included trials had a parallel and open design (Cohen 1991; Croft 1986; DISH 1985; Jalkanen 1991; ODES 1995; Ruvolo 1994; TAIM 1992; TONE 1998), and three of them had a factorial design (ODES 1995; TAIM 1992; TONE 1998). Four studies were performed as single‐centre trials (Cohen 1991; Croft 1986; ODES 1995; Ruvolo 1994), and three did not mention any industry sponsoring (Cohen 1991; Jalkanen 1991; Ruvolo 1994).
Participants and duration
The included trials involved a total of 2100 hypertensive participants with a mean age of 45 to 66 years, a baseline systolic blood pressure of 128 to 178 mm Hg, and a baseline diastolic blood pressure of 72 to 107 mm Hg. Mean treatment duration was 6 to 36 months (see Table 3; Table 4).
Interventions
In all trials, participants received either a dietary intervention with the aim of reducing body weight or no dietary intervention to reduce body weight.
Outcomes
Primary outcomes
Only one trial included the occurrence of clinical cardiovascular disease complications during follow‐up as a predefined outcome (TONE 1998). Three trials reported mortality rates during the study period (ODES 1995; Ruvolo 1994; TONE 1998). Two studies reported adverse events (DISH 1985; TONE 1998).
Secondary outcomes
Except for three trials (Cohen 1991; DISH 1985; TONE 1998), all included trials described the mean change in systolic and diastolic blood pressure. All but two trials (ODES 1995; TONE 1998) described mean change in body weight.
Excluded studies
The main reason for exclusion was a lack of sufficient results for the hypertensive subgroup in trials including normotensive as well as hypertensive participants. We excluded some studies because they were not randomised controlled trials, did not include participants with essential hypertension, did not aim for weight reduction or examined a combined intervention, provided an inappropriate control intervention or different accompanying therapies, had a duration of intervention less than 24 weeks, or full text was not available. We excluded two studies after personal communication (Curzio 1989; Haynes 1984). Both studies were performed in the 1980s, and electronic records or hard copies or both were no longer available to further clarify whether the studies were suitable for inclusion in our review. We have provided reasons for excluding each trial in the Characteristics of excluded studies table.
Risk of bias in included studies
Our judgements of the risks of bias for all included trials are shown in the 'Risk of bias' summary figures (Figure 2; Figure 3). For details, see the 'Risk of bias' tables in Characteristics of included studies. The following gives a brief overview.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Only two trials reported the method of randomisation (TAIM 1992; TONE 1998), and both of them had a factorial design. Only two trials described the method of concealment (ODES 1995; TAIM 1992). Cohen 1991 was a cluster‐randomised trial in family practices, but without providing any information on allocation. In addition, the trial featured stratified randomisation of investigators instead of participants, with very small cluster size.
Blinding
All included trials had an open design in terms of participants and study personnel. In one trial (TONE 1998), an independent committee masked to intervention assignment evaluated the endpoints. In TAIM 1992, blood pressure endpoint assessment was blinded in only one out of three clinical centres due to logistical and budgetary considerations.
Incomplete outcome data
In Cohen 1991, the description of the outcome data was complete because there were no losses to follow‐up. In DISH 1985, no withdrawals were reported for the endpoint of successful withdrawal from antihypertensive medication, but between 13% and 23% of values were missing for body weight at follow‐up. In Jalkanen 1991 and Ruvolo 1994, only one to two participants were missing, but no reason for withdrawal was given. In TAIM 1992 and ODES 1995, study withdrawals were only reported for the whole study population, and no intention‐to‐treat analysis was performed. In TONE 1998, numbers of and reasons for withdrawals were missing, but 96% to 99% of participants were included in the follow‐up analysis.
Selective reporting
There was a risk of selective reporting bias in one trial in which post hoc analyses of blood pressure were calculated, and results were not reported for all predefined outcomes (ODES 1995).
Other potential sources of bias
We could identify other potential sources of bias in three trials (DISH 1985; ODES 1995; TAIM 1992). In DISH 1985, participants were randomised before consent was obtained, and in two studies (ODES 1995; TAIM 1992) treatment in the intervention group seemed to be more intensive. For further details, please see the 'Risk of bias' tables and Figure 2 and Figure 3.
Effects of interventions
See: Table 1
See: Table 1
Primary outcomes
Mortality
None of the included trials was designed to evaluate the effects of weight‐loss diet versus no diet on mortality. Three trials (ODES 1995; Ruvolo 1994; TONE 1998) reported that no participant died during the follow‐up periods.
Cardiovascular morbidity
Only one trial evaluated the effects of dietary weight‐loss intervention versus no dietary intervention, with a combined endpoint including cardiovascular complications (TONE 1998). After 30 months, the hazard ratio for participants in the dietary group to reach the combined endpoint, consisting of the necessity of reinstating antihypertensive therapy and severe cardiovascular complications, was 0.70 (95% confidence interval (CI) 0.57 to 0.87) compared with participants in the usual‐care group. Altogether, there were 145 cardiovascular events during the study period, with 21 events (14.3%) in the weight‐loss group, 23 events (15.6%) in the weight loss + sodium reduction group, 57 events (16.7%) in the usual‐care group, and 44 events (12.9%) in the sodium‐reduction group, respectively. There was no statistically significant difference between weight loss and no weight loss (P = 0.35).
Adverse events
None of the included trials evaluated the endpoint of adverse events as described in our protocol (including total serious adverse events, withdrawal due to adverse events, and total non‐serious adverse events).
TONE 1998 classified adverse events by type (primary cardiovascular events) and time of occurrence (before, during, or after attempted antihypertensive drug withdrawals). However, no usable results were reported for the overweight subgroups with and without dietary interventions. DISH 1985 reported adverse events as withdrawals due to the need to resume antihypertensive medication; this was the case in 40.5% of participants in the intervention group and 64.7% of participants in the control group (P = 0.0015).
Secondary outcomes
For details on secondary outcome data, see Table 5, Table 6, and Table 7. Due to between‐study variability, we have presented results from random‐effects models in the following analyses.
4. Body weight.
| Trial | Body weight [kg]a | |||||
| Intervention(s) and comparator(s) | Baseline | 6 months | 12 months | > 12 months | Change (baseline to endpoint) | |
| Cohen 1991 | diet | 92b | n. r. | n. r. | ‐c | −0.9 (4.0) |
| no diet | 92b | n. r. | n. r. | ‐c | +1.3 (3.0); P < 0.1 | |
| Croft 1986 | diet | 87 (4) | 80 (4) | ‐c | ‐c | −6.5b |
| no diet | 82 (3) | 82 (3) | ‐c | ‐c | −0.2b; P < 0.001 | |
| DISH 1985 | diet | 86 (17) | n. r. | n. r. | ‐c | −4.0 (5.0) |
| no diet | 90 (18) | n. r. | n. r. | ‐c | −0.5 (3.6); P < 0.05e | |
| Jalkanen 1991 | diet | 86 (14) | n. r. | 82 (13) | ‐c | −4.0d |
| no diet | 80 (11) | n. r. | 80 (11) | ‐c | 0.0d; P < 0.05 | |
| ODES 1995f | ‐ | n. r. | n. r. | n. r. | n. r. | n. r. |
| Ruvolo 1994 | diet | 98 (8) | 84 (9) | ‐c | ‐c | −14b,g |
| no diet | 97 (8) | 95 (8) | ‐c | ‐c | −2b,g; P = n. r. | |
| TAIM 1992 | diet + placebo | 90b | n. r. | n. r. | n. r.h | −4.4 (0.7)j |
| no diet + placebo | 86b | n. r. | n. r. | n. r.h | −0.7 (0.4)j; P = n. r. | |
| diet + atenolol | 86b | n. r. | n. r. | n. r.h | −3.0 (0.4)j | |
| no diet + atenolol | 89b | n. r. | n. r. | n. r.h | +0.5 (0.3)j; P = n. r. | |
| diet + chlorthalidone | 87b | n. r. | n. r. | n. r.h | −6.9 (0.5)j | |
| no diet + chlorthalidone | 89b | n. r. | n. r. | n. r.h | −1.5 (0.4)j; P = n. r. | |
| TONE 1998 | diet without salt restriction | 87 (10) | n. r. | n. r. | n. r. | n. r.k |
| no diet without salt restriction | 86 (10) | n. r. | n. r. | n. r. | n. r.k | |
| diet + salt restriction | 86 (10) | n. r. | n. r. | n. r. | n. r.k | |
| no diet + salt restriction | 88 (11) | n. r. | n. r. | n. r. | n. r.k | |
aMean (standard deviation), unless otherwise indicated. bData on variance missing. cObservation period ≤ 12 months. dNumbers calculated from the tables of publications. A mean weight reduction of 5 kg is stated in the text section.
eInformation on body weight was available for 77% of participants in the intervention group and 87% of participants in the control group. fNot mentioned for the hypertensive subgroup. gCalculated from table 1 in Ruvolo 1994. hOnly change in body weight reported for 24 months; since no other outcomes were reported for this time, and change in body weight is not a primary endpoint of this report, data were not extracted. jStandard error. kWeight reduction of 3.9 vs 0.9 kg (P < 0.001) in overweight participants of both intervention groups together (with and without salt restriction) vs control group.
[n. r.]: not reported.
5. Systolic blood pressure.
| Trial | Systolic blood pressure [mm Hg]a | |||||
| Intervention(s) and comparator(s) | Baseline | 6 months | 12 months | > 12 months | Change (baseline to endpoint) | |
| Cohen 1991 | diet | n. r.b | n. r. | n. r. | ‐c | n. r.b |
| no diet | n. r.b | n. r. | n. r. | ‐c | n. r.b | |
| Croft 1986 | diet | 161 (4) | 150 (4) | ‐c | ‐c | −11.0d |
| no diet | 161 (4) | 157 (4) | ‐c | ‐c | −4.0d; P < 0.01 | |
| DISH 1985 | ‐ | ‐e | ‐e | ‐e | ‐e | ‐e |
| Jalkanen 1991 | diet | 152 (17) | n. r. | 144 (20) | ‐c | −8.0d |
| no diet | 155 (14) | n. r. | 140 (16) | ‐c | −15.0d; P = n. r. | |
| ODES 1995 | diet | 145 (5)f | n. r. | n. r. | ‐c | −8.4 (3.3)f |
| no diet | 138 (3)f | n. r. | n. r. | ‐c | 2.9 (4.4)f; P < 0.05 | |
| diet + physical activity | 143 (2)f | n. r. | n. r. | ‐c | −8.3 (2.1)f | |
| no diet + physical activity | 140 (2)f | n. r. | n. r. | ‐c | −4.1 (1.8)f; P = n. r. | |
| Ruvolo 1994 | diet | 178 (8) | 145 (6) | ‐c | ‐c | −33d,g |
| no diet | 176 (8) | 144 (6) | ‐c | ‐c | −32d,g; P = n. r. | |
| TAIM 1992 | diet + placebo | 143d | n. r.h | n. r. | n. r. | −11.5d |
| no diet + placebo | 145d | n. r.h | n. r. | n. r. | −10.3d; P = n. r. | |
| diet + atenolol | 143d | n. r.h | n. r. | n. r. | −18.1d | |
| no diet + atenolol | 143d | n. r.h | n. r. | n. r. | −15.1d; P = n. r. | |
| diet + chlorthalidone | 141d | n. r.h | n. r. | n. r. | −21.7d | |
| no diet + chlorthalidone | 142d | n. r.h | n. r. | n. r. | −17.4d; P = n. r. | |
| TONE 1998 | ‐ | ‐e | ‐e | ‐e | ‐e | ‐e |
aMean (SD), unless otherwise indicated. bOnly the mean arterial blood pressure is reported (at baseline: IG and CG 106 mm Hg each; change from baseline to endpoint: IG +3.0 (SD 14.2) mm Hg and CG ‐0.7 (SD 11.3) mm Hg). cObservation period ≤ 12 months. dData on variance missing. ePurpose of the study was not the change in blood pressure, but the number of participants without any antihypertensive drug requirements at the end of the study after successful withdrawal of antihypertensives. fStandard error. gCalculated from table 1 in Ruvolo 1994. hOnly changes from baseline are reported, no absolute values. [n. r.]: not reported. [SD]: standard deviation.
6. Diastolic blood pressure.
| Study | Diastolic blood pressure [mm Hg]a | |||||
| Intervention(s) and comparator(s) | Baseline | 6 months | 12 months | > 12 months | Change (baseline to endpoint) | |
| Cohen 1991 | diet | n. r.b | n. r. | n. r. | ‐c | n. r.b |
| no diet | n. r.b | n. r. | n. r. | ‐c | n. r.b | |
| Croft 1986 | diet | 98 (2) | 91 (2) | ‐c | ‐c | −7.0d |
| no diet | 96 (2) | 95 (2) | ‐c | ‐c | −1.0d; P < 0.001 | |
| DISH 1985 | ‐ | ‐e | ‐e | ‐e | ‐e | ‐e |
| Jalkanen 1991 | diet | 101 (8) | n. r. | 90 (10) | ‐c | −11.0d |
| no diet | 102 (7) | n. r. | 91 (7) | ‐c | −11.0d; P = n. r. | |
| ODES 1995 | diet | 97 (1)f | n. r. | n. r. | ‐c | −7.1 (1.8)f |
| no diet | 96 (1)f | n. r. | n. r. | ‐c | −0.4 (3.6)f; ns | |
| diet + physical activity | 97 (1)f | n. r. | n. r. | ‐c | −7.1 (1.3)f | |
| no diet + physical activity | 96 (1)f | n. r. | n. r. | ‐c | −5.5 (1.7)f; P = n. r. | |
| Ruvolo 1994 | diet | 107 (5) | 84 (4) | ‐c | ‐c | −23d,g |
| no diet | 106 (5) | 85 (5) | ‐c | ‐c | −21d,g; P = n. r. | |
| TAIM 1992 | diet | n. r. | n. r.h | n. r. | n. r. | −12.8 (10.0) |
| no diet | n. r. | n. r.h | n. r. | −10.4 (7.8); P = 0.001 | ||
| TONE 1998 | ‐ | ‐e | ‐e | ‐e | ‐e | ‐e |
aMean (SD), unless otherwise indicated. bOnly the mean arterial blood pressure is reported (at baseline: IG and CG 106 mm Hg each; change from baseline to endpoint: IG +3.0 (SD 14.2) mm Hg and CG −0.7 (SD 11.3) mm Hg). cObservation period ≤ 12 months. dData on variance missing. ePurpose of the study was not the change in blood pressure, but the number of participants without any antihypertensive drug requirements at the end of the study after successful withdrawal of antihypertensives. fStandard error. gCalculated from table 1 in Ruvolo 1994. hOnly changes from baseline are reported, no absolute values. [n. r.]: not reported. [ns]: not significant. [SD]: standard deviation.
Changes in systolic blood pressure
Five trials investigating the effects of dietary versus no dietary intervention could not be included in the meta‐analysis for systolic blood pressure. In two trials (DISH 1985; TONE 1998), successful withdrawal from antihypertensives was the primary outcome. In another trial (Cohen 1991), only the mean blood pressure change was reported, and in the trials Jalkanen 1991 and Ruvolo 1994, estimators for variance and P values for the change in systolic blood pressure were missing. Therefore, only three trials remained for analysis (731 participants).
In the case of TAIM 1992, the overall standard deviation (SD) presented for the combined analyses could be used for the meta‐analysis. There was a significant reduction in systolic blood pressure, with a mean difference (MD) of −4.49 mm Hg (95% CI −7.20 to −1.78) in favour of dietary intervention. The test for heterogeneity gave a P value of 0.29, and Higgins I2 indicated only low heterogeneity between studies (I2 = 21%) (see Analysis 1.1; Figure 4). Differences in study quality could not explain heterogeneity. We could deduce no plausible explanation for heterogeneity from differences in study design, study duration, sample sizes, interventions, or characteristics of the included participants.
1.1. Analysis.

Comparison 1: Weight‐reducing diet versus no weight‐reducing diet, Outcome 1: Change in systolic blood pressure from baseline to endpoint
4.

Forest plot of comparison: 1 Weight‐reducing diet versus no weight‐reducing diet, outcome: 1.1 Change in systolic blood pressure from baseline to endpoint [mm Hg].
Changes in diastolic blood pressure
Five trials investigating the effects of dietary versus no dietary intervention could not be included in the meta‐analysis for diastolic blood pressure. In two trials (DISH 1985; TONE 1998), successful withdrawal from antihypertensives was the primary outcome. In Cohen 1991, only the mean blood pressure change was reported, and Jalkanen 1991 and Ruvolo 1994 do not include an estimator for variance and P values for the change in diastolic blood pressure. Therefore, only three trials remained for analysis (731 participants).
In the case of TAIM 1992, the SDs presented for the subgroup (atenolol, chlorthalidone, placebo) analyses could be used for the meta‐analysis. There was a significant reduction in diastolic blood pressure, with a MD of −3.19 mm Hg (95% CI −4.83 to −1.54) in favour of dietary intervention. The test for heterogeneity gave a P value of 0.18 (I2 = 35%) (see Analysis 1.2; Figure 5). Differences in study quality could not explain heterogeneity. We could deduce no plausible explanation for heterogeneity from differences in study design, study duration, sample sizes, interventions, or characteristics of included participants.
1.2. Analysis.

Comparison 1: Weight‐reducing diet versus no weight‐reducing diet, Outcome 2: Change in diastolic blood pressure from baseline to endpoint
5.

Forest plot of comparison: 1 Weight‐reducing diet versus no weight‐reducing diet, outcome: 1.2 Change in diastolic blood pressure from baseline to endpoint [mm Hg].
Body weight
Only three trials investigating the effects of dietary versus no dietary intervention could not be included in the meta‐analysis for body weight. In two trials (ODES 1995; TONE 1998), no values for changes in body weight were presented, and in Ruvolo 1994 an estimator for variance and P values for the change in body weight was missing. Five trials (880 participants) therefore remained for analysis. In TAIM 1992, we could use the SDs presented for the subgroup (atenolol, chlorthalidone, and placebo) analyses. Dietary intervention was found to lower body weight significantly more effectively, with a MD of −3.98 kg (95% CI −4.79 to −3.17) in favour of dietary intervention. The test for heterogeneity gave a P value of 0.17 (I2 = 34%) (see Analysis 1.3; Figure 6). Differences in study quality could not explain heterogeneity. We could deduce no plausible explanation for heterogeneity from differences in study design, study duration, sample sizes, interventions, or characteristics of included participants.
1.3. Analysis.

Comparison 1: Weight‐reducing diet versus no weight‐reducing diet, Outcome 3: Change in body weight from baseline to endpoint
6.

Forest plot of comparison: 1 Weight‐reducing diet versus no weight‐reducing diet, outcome: 1.3 Change in body weight from baseline to endpoint [kg].
Subgroup analyses
Not performed due to lack of data.
Sensitivity analyses
Not performed due to lack of data.
Publication and small‐study bias
A clear interpretation of the funnel plot was not possible, which we mainly attributed to the relatively small number of included studies.
Discussion
Summary of main results
This updated systematic review attempted to determine the long‐term effects of weight loss through dietary interventions on patient‐relevant endpoints, namely death, cardiovascular complications, and adverse events, in the antihypertensive therapy of people with essential hypertension. However, we found no currently‐available randomised controlled trials designed to answer this question. We identified no new trials as a result of the update, yielding eight relevant trials that intended to reduce body weight (for example dietary counselling, caloric restrictions, reduction in fat intake) versus no dietary interventions. Of the eight included trials, we judged only two as having minor deficiencies of study quality (TAIM 1992; TONE 1998), while the other six studies have major deficiencies. Only one trial reported on cardiovascular complications, as part of a combined primary outcome consisting of the necessity of reinstating antihypertensive therapy and severe cardiovascular complications, and was in favour of the dietary‐intervention group (TONE 1998). No valuable information on adverse effects was reported in any publications on the relevant trials. The meta‐analyses showed that participants under dietary therapy could reduce their systolic and diastolic blood pressure and body weight levels statistically significantly more than participants in the control groups.
Two trials did not aim for blood pressure reduction, but used successful withdrawal of antihypertensive medication as a primary outcome (DISH 1985; TONE 1998). In DISH 1985, about 35% of the participants in the control group and about 60% in the intervention group remained without antihypertensive medication after 56 weeks. In TONE 1998, 93% of the participants in the weight‐loss group and 87% in the control group could stop antihypertensive treatment. In the salt‐lowered groups, 93% of both the dietary weight‐loss intervention and the usual‐care group could successfully be taken off medication. Even though successful withdrawal of antihypertensive treatment was not included as a chosen outcome in our review, it further underscores the success of dietary weight‐loss interventions for reducing blood pressure.
In conclusion, in people with essential hypertension, therapy with dietary interventions to reduce body weight resulted in reductions in blood pressure and body weight. A reduction in body weight of approximately 4 kg was necessary to achieve a reduction of approximately 4.5 mm Hg systolic blood pressure and approximately 3.2 mm Hg diastolic blood pressure. However, the fact that only some of the studies could be included in the analyses weakens our conclusion. None of the studies provided data to answer the question of whether weight reduction can lower the risk of mortality or other patient‐relevant endpoints.
Overall completeness and applicability of evidence
For this update we searched four electronic databases and the clinical trials registry (ClinicalTrials.gov) until April 2020, and the WHO clinical trials registry ICTRP until July 2018. We also searched the reference lists of included trials and relevant systematic reviews and meta‐analyses. We assessed the quality of each study and summarised the results. The results of this review can therefore be taken to be complete and applicable. For full information, please see details in the relevant sections.
While the results of this review show that dietary interventions may be helpful in the antihypertensive therapy of overweight people with hypertension, major questions still remain. One point raised by Brian Haynes, a co‐author we contacted for further clarification on whether his paper was relevant for inclusion in the review, was whether any effect on blood pressure‐lowering persists when the participant's period of active weight loss ends. His clinical impression is that when weight loss stops (even if the weight loss is maintained?), the blood pressure goes back up (Haynes 2010 [pers comm]). However, there is still a lack of evidence about the long‐term effects of weight loss on hypertension, as we could identify no long‐term follow‐up trials for our review. Indirect evidence from this assumption can be derived from the Swedish Obese Subject Study (Sjöström 2004), where participants successfully reduced their body weight by means of bariatric surgery. This study showed that the postsurgical blood pressure reduction was still present two years after surgery, but increased again to baseline values after 10 years, despite continued weight loss. Secondly, it can be asked whether people with higher or lower blood pressure or higher or lower body weight at baseline might benefit in a different way from dietary intervention aiming to reduce body weight. It can, however, be assumed that the potential benefit on blood pressure might be greater in people with moderate‐to‐severe hypertension than in people with mild hypertension; in any case, we could find no correlation from the included studies. However, since the initial version of this review in 2011, no RCTs investigating the effect of weight‐reducing diets in people with hypertension with a follow‐up of at least six months were published,
Quality of the evidence
Of the eight trials included in our analyses, we judged only two as having minor deficiencies of quality (TAIM 1992; TONE 1998). All other trials have to be judged as having major deficiencies. The beneficial effects shown therefore reflect some degree of uncertainty. We have provided full details in the 'Risk of bias' tables in Characteristics of included studies.
Potential biases in the review process
A major limitation of this review is that, due to the lack of information in the included trials, we could draw no conclusions on the effects of the different dietary weight‐loss interventions on patient‐relevant long‐term outcomes.
The results for the change in blood pressure outcomes could also be considered uncertain, as we included data from only three trials in the analyses. These results were mainly based on the TAIM 1992 study, which we judged to have a low risk of bias and contributed more than 70% of all participants to the meta‐analyses. In addition, two of the trials that did not report results on blood pressure showed a reduction of antihypertensive medication as an indirect measure of blood pressure, which supports the findings of our meta‐analyses. Furthermore, inclusion of the remaining studies from which data on blood pressure were available but were insufficient would probably not have changed the results, because these trials were all small and rated at high risk of bias.
The findings on body weight may also be regarded as uncertain, as results from only five trials were available for the analysis. Again, the TAIM 1992 trial had the highest weight in the analysis. These results are supported by results from the ODES 1995 study, which did not report on body weight, but found body mass index to be reduced to a greater extent among participants in the intervention groups.
Agreements and disagreements with other studies or reviews
There are only a few published systematic reviews on the long‐term effects of weight‐reducing diets in people with hypertension. One systematic review, Effects of weight loss in overweight/obese individuals and long‐term hypertension outcomes (Aucott 2005), reached the same conclusion, i.e. that only short‐term trials were available. The authors also warned "that extrapolation of short‐term blood pressure changes with weight loss to the longer term is potentially misleading. The weight/hypertension relationship is complex and needs well‐conducted studies with long‐term follow‐up to examine the effects of weight loss on hypertension outcomes". In addition, we were involved in the preparation of the scientific report on the evaluation of the benefits and harms of non‐drug treatment strategies in people with essential hypertension (IQWiG 2006), and published a paper on this topic in 2008 (Horvath 2008). Since our last search for dietary interventions performed in February/March 2015 (Semlitsch 2016), we could identify no additional trials addressing our research question. We can therefore say with confidence that our findings are in agreement with other published reviews and studies in this field.
Some recent systematic reviews investigated the effect of weight‐reducing diets on blood pressure in people with or without hypertension. Gay 2016 reported significant reductions in systolic and diastolic blood pressure with low‐calorie diets after at least six months of follow‐up in a mixed population of people with normal or raised blood pressure. A second review investigating the effect of commercial weight‐loss programmes on cardiovascular risk factors in overweight or obese people with mostly normal blood pressure at baseline showed inconsistent results on blood pressure after six and 12 months of follow‐up (Metha 2016).
Authors' conclusions
Implications for practice.
Although trials on dietary interventions in people with elevated blood pressure demonstrated statistically significant decreases in weight loss and blood pressure, these findings are subject to a high risk of selective reporting bias. Furthermore, the available randomised controlled trial evidence provided no data on the effect of dietary interventions on mortality or morbidity, and none of the included trials reported valuable information on adverse events.
Implications for research.
Long‐term trials are needed, assessing the effect of dietary interventions to reduce body weight on mortality, morbidity, and adverse events in people with elevated blood pressure. Long‐term follow‐up data are also needed to determine the long‐term effects of weight‐reducing diets on blood pressure.
What's new
| Date | Event | Description |
|---|---|---|
| 11 May 2020 | New search has been performed | We updated the search for new studies in April 2020. We identified no new studies that met the inclusion criteria for this review. |
| 11 May 2020 | New citation required but conclusions have not changed | Update published with changed authors, update search, conclusion unchanged. |
History
Protocol first published: Issue 1, 2010 Review first published: Issue 9, 2011
| Date | Event | Description |
|---|---|---|
| 2 February 2016 | New search has been performed | We updated the search for new studies in February 2015. We identified no new studies that met the inclusion criteria of this review. We have added a 'Summary of findings' table. |
| 2 February 2016 | New citation required but conclusions have not changed | Update published with changed authors, updated search, conclusions not changed. |
Acknowledgements
The review authors would like to acknowledge Douglas Salzwedel for assisting in updating the literature search for the 2016 and 2020 update of this review.
The review authors would like to acknowledge the contributions of Eva Nagele, Nicole Posch, and Anika Maas in reviewing the data for the 2011 version of this review and Jutta Meschik, Nicole Posch and Stephanie Poggenburg in reviewing the data for the 2016 version of this review.
The review authors would like to acknowledge the contribution of Eugenia Lamont in the final editing of the manuscript for the 2011 version of this review.
The review authors would like to acknowledge the contributions of Andreas Waltering, Lars Hemkens, Christoph Pachler, and Reinhard Strametz in the selection of studies, quality assessment of trials, data extraction, and development of the final 2011 version of this review.
Appendices
Appendix 1. Search strategies
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Daily and Versions(R) <1946 to April 02, 2020> Search Date: 3 April 2020 ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 nutrition therapy/ 2 diet therapy/ 3 ((aliment$ or diet$ or nutrition) adj2 (chang$ or counsel$ or dash or health? or intervention? or overweight? or pattern? or program$ or therap$ or treatment? or weight?)).ti,kf. 4 ((aliment$ or diet$ or nutrition) adj3 (chang$ or counsel$ or dash or health? or intervention? or overweight? or pattern? or program$ or therap$ or treatment? or weight?)).ab. 5 ((bodyweight? or calor$ or overweight? or weight?) adj2 (chang$ or control$ or lose or losing or loss or manag$ or reduc$)).ti,ab,kf. 6 or/1‐5 7 hypertension/ 8 essential hypertension/ 9 blood pressure/ 10 (antihypertens$ or hypertens$).ti,ab,kf,ot. 11 ((chang$ or elevat$ or high or rais$ or reduc$) adj4 blood pressur$).ti,ab,kf,ot. 12 ((chang$ or elevat$ or high or rais$ or reduc$) adj4 (arterial pressur$ or bloodpressur$$ or bp)).ti,ab,kf,ot.
13 or/7‐12 14 randomized controlled trial.pt. 15 pragmatic clinical trial.pt. 16 controlled clinical trial.pt. 17 randomized.ab. 18 placebo.ab. 19 clinical trials as topic/
20 randomly.ab. 21 trial.ti. 22 or/14‐21 23 animals/ not (humans/ and animals/) 24 22 not 23 25 6 and 13 and 24 ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ Database: Cochrane Hypertension Specialised Register via Cochrane Register of Studies (CRS‐Web) Search Date: 14 April 2020 ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ #1 MESH DESCRIPTOR Nutrition Therapy AND INSEGMENT #2 MESH DESCRIPTOR Diet Therapy AND INSEGMENT #3 (chang* OR elevat* OR high OR rais* OR reduc*) NEAR3 (arterial pressur* OR blood pressur* OR bloodpressur* OR bp):TI,AB AND INSEGMENT #4 (#6 OR #7 OR #8 OR #9 OR #10) AND INSEGMENT #5 RCT:DE AND INSEGMENT #6 Review:ODE AND INSEGMENT #7 (#12 OR #13) AND INSEGMENT #8 #5 AND #11 AND #14 AND INSEGMENT #9 ((aliment* OR diet* OR nutrition) NEAR2 (chang* OR counsel* OR dash OR health* OR intervention* OR overweight* OR pattern* or program* OR therap* OR treatment* OR weight*)) AND INSEGMENT #10 (bodyweight* OR calor* OR overweight* OR weight*) AND (chang* OR control* OR lose OR losing OR loss OR manag* OR reduc*):TI AND INSEGMENT #11 (#1 OR #2 OR #3 OR #4) AND INSEGMENT #12 MESH DESCRIPTOR Hypertension AND INSEGMENT #13 MESH DESCRIPTOR Essential Hypertension AND INSEGMENT #14 MESH DESCRIPTOR Blood Pressure AND INSEGMENT #15 (antihypertens* OR hypertens*) AND INSEGMENT #16 ((aliment* OR diet* OR nutrition) NEAR2 (chang* OR counsel* OR dash OR health* OR intervention* OR overweight* OR pattern* or program* OR therap* OR treatment* OR weight*)) AND INSEGMENT #17 (bodyweight* OR calor* OR overweight* OR weight*) AND (chang* OR control* OR lose OR losing OR loss OR manag* OR reduc*):TI AND INSEGMENT #18 (#1 OR #2 OR #3 OR #4) AND INSEGMENT #19 MESH DESCRIPTOR Hypertension AND INSEGMENT #20 (chang* OR elevat* OR high OR rais* OR reduc*) NEAR3 (arterial pressur* OR blood pressur* OR bloodpressur* OR bp):TI,AB AND INSEGMENT #21 MESH DESCRIPTOR Essential Hypertension AND INSEGMENT #22 (#6 OR #7 OR #8 OR #9 OR #10) AND INSEGMENT #23 MESH DESCRIPTOR Blood Pressure AND INSEGMENT #24 RCT:DE AND INSEGMENT #25 Review:ODE AND INSEGMENT #26 (#12 OR #13) AND INSEGMENT #27 #5 AND #11 AND #14 AND INSEGMENT #28 (antihypertens* OR hypertens*) AND INSEGMENT #29 (chang* OR elevat* OR high OR rais* OR reduc*) NEAR3 (arterial pressur* OR blood pressur* OR bloodpressur* OR bp):TI,AB AND INSEGMENT #30 (#6 OR #7 OR #8 OR #9 OR #10) AND INSEGMENT #31 RCT:DE AND INSEGMENT #32 Review:ODE AND INSEGMENT #33 (#12 OR #13) AND INSEGMENT #34 #5 AND #11 AND #14 AND INSEGMENT ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ Database: Cochrane Central Register of Controlled Trials (Issue 3, 2020) via the Cochrane Register of Studies (CRS‐Web) Search Date: 3 April 2020 ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ #1 MESH DESCRIPTOR Nutrition Therapy AND CENTRAL:TARGET #2 MESH DESCRIPTOR Diet Therapy AND CENTRAL:TARGET #3 ((aliment* OR diet* OR nutrition) NEAR2 (chang* OR counsel* OR dash OR health* OR intervention* OR overweight* OR pattern* OR program* OR therap* OR treatment* OR weight*)) AND CENTRAL:TARGET #4 (bodyweight* OR calor* OR overweight* OR weight*) AND (chang* OR control* OR lose OR losing OR loss OR manag* OR reduc*):TI AND CENTRAL:TARGET #5 (#1 OR #2 OR #3 OR #4) AND CENTRAL:TARGET #6 MESH DESCRIPTOR Hypertension AND CENTRAL:TARGET #7 MESH DESCRIPTOR Essential Hypertension AND CENTRAL:TARGET #8 (antihypertens* OR hypertens*):TI,AB AND CENTRAL:TARGET #9 (chang* OR elevat* OR high OR rais* OR reduc*) NEAR3 (arterial pressur* OR blood pressur* OR bloodpressur* OR bp):TI,AB AND CENTRAL:TARGET #10 (#6 OR #7 OR #8 OR #9) AND CENTRAL:TARGET #11 #5 AND #10 AND CENTRAL:TARGET ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ Database: Embase <1974 to 2020 April 02> Search Date: 3 April 2020 ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 exp *diet therapy/ 2 ((aliment$ or diet$ or nutrition) adj2 (chang$ or counsel$ or dash or health? or intervention? or overweight? or pattern? or program$ or therap$ or treatment? or weight?)).ti. 3 ((aliment$ or diet$ or nutrition) adj3 (chang$ or counsel$ or dash or health? or intervention? or overweight? or pattern? or program$ or therap$ or treatment? or weight?)).ab. 4 ((bodyweight? or calor$ or overweight? or weight?) adj2 (chang$ or control$ or lose or losing or loss or manag$ or reduc$)).tw. 5 or/1‐4 6 exp hypertension/ 7 (antihypertens$ or hypertens$).ti,ab,ot. 8 exp *blood pressure/ 9 ((chang$ or elevat$ or high or rais$ or reduc$) adj3 (arterial pressur$ or bloodpressur$ or bp)).ti,ab,ot. 10 ((chang$ or elevat$ or high or rais$ or reduc$) adj3 blood pressur$).ti,ab,ot. 11 or/6‐10 12 randomized controlled trial/ 13 crossover procedure/ 14 double‐blind procedure/ 15 (randomi?ed or randomly).tw. 16 (crossover$ or cross‐over$).tw. 17 placebo.ab. 18 (doubl$ adj blind$).tw. 19 assign$.ab. 20 allocat$.ab. 21 or/12‐20 22 (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 23 21 not 22 24 5 and 11 and 23 ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ Database: ClinicalTrials.gov Search Date: 3 April 2020 ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ Condition or disease: Hypertension Other terms: randomized AND (bodyweight OR overweight OR weight) Study type: Interventional Studies (Clinical Trials) Intervention/treatment: (diet OR weight loss OR weight reduc*)
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
Database: WHO International Clinical Trials Registry Platform (ICTRP) Search Date: 6 July 2018 ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ hypertens* and diet* and bodyweight hypertens* and diet* and overweight hypertens* and diet* and weight hypertens* and weight loss hypertens* and weight reduc*
Data and analyses
Comparison 1. Weight‐reducing diet versus no weight‐reducing diet.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Change in systolic blood pressure from baseline to endpoint | 4 | 731 | Mean Difference (IV, Random, 95% CI) | ‐4.49 [‐7.20, ‐1.78] |
| 1.2 Change in diastolic blood pressure from baseline to endpoint | 6 | 731 | Mean Difference (IV, Random, 95% CI) | ‐3.19 [‐4.83, ‐1.54] |
| 1.3 Change in body weight from baseline to endpoint | 7 | 880 | Mean Difference (IV, Random, 95% CI) | ‐3.98 [‐4.79, ‐3.17] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cohen 1991.
| Study characteristics | ||
| Methods | Design: parallel, cluster‐randomised Date: not stated Duration: 12 months Number of study centres: 1 Setting: model family practice unit (Pittsburgh), USA | |
| Participants |
Who participated: 30 hypertensive and obese people stratified by residents (residents, not participants, were randomised to intervention or control group) Main inclusion criteria: age 20 to 75 years; BMI ≥ 28 kg/m2 (men); ≥ 27 kg/m2 (women); SBP ≥ 140 mm Hg, DBP ≥ 90 mm Hg in 2 or more readings Main exclusion criteria: not described in detail Subgroup analyses: weight losers vs weight gainer |
|
| Interventions |
Dietary intervention: physicians (n = 10) were taught by a behavioural psychologist; the goal of the dietary advice was to reduce the caloric content of the diet without radically changing the participant's lifestyle; monthly participant consultations and reviewing diet history sheet; the suggested diets were not specifically intended to be salt‐reducing (N = 15)
No dietary intervention: physicians (n = 8) received no special instructions or materials; the participants continued to be treated with their usual care (N = 15) Additional treatment: ‐ |
|
| Outcomes |
Primary outcomes: 1. Mortality: ‐ 2. Cardiovascular morbidity: ‐ 3. Adverse events: ‐ Secondary outcomes: 1. Changes in systolic blood pressure [mm Hg]: ‐ 2. Changes in diastolic blood pressure [mm Hg]: ‐ 3. Changes in body weight [kg]: Definition: body weight change from baseline to 6 months, from baseline to 12 months, and from 6 months to 12 months Additional outcome measured in the trial: 1. Mean arterial blood pressure change in mm Hg 2. Change in number of antihypertensive medications 3. Number of visits |
|
| Study details |
Length of follow‐up: 12 months Trial terminated before regular end (for benefit / because of adverse events): No Trial ID: ‐ |
|
| Publication details |
Language of publication: English Funding: ‐ Publication status: Full‐text journal publication |
|
| Study aim | Quote from publication: "...to determine whether this was an effective milieu for the treatment of hypertension by weight reduction using a low‐technology low‐cost approach and involving only the physician as the therapeutic medium." | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Comment: No details on sequence generation are provided; stratified randomisation of investigators instead of participants with very small cluster size Quote: "The residents were stratified by residency year and randomly assigned to either control or experimental groups. ... The experimental or control status of a patient was determined by the status of the physician, and great care was taken to avoid contamination." |
| Allocation concealment (selection bias) | Unclear risk | Comment: Method of concealment is not described |
| Blinding (performance bias and detection bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Change in blood pressure | High risk | Comment: Since the physicians assigned to the experimental group were taught about the weight‐reducing programme, knowledge of the allocation intervention was not prevented during study |
| Blinding (performance bias and detection bias) Change in body weight | High risk | Comment: Since the physicians assigned to the experimental group were taught about the weight‐reducing programme, knowledge of the allocation intervention was not prevented during study |
| Incomplete outcome data (attrition bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Change in blood pressure | Low risk | Comment: no withdrawals; all participants were analysed |
| Incomplete outcome data (attrition bias) Change in body weight | Low risk | Comment: No withdrawals; all participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | Comment: No study protocol available; no primary and secondary outcomes were defined in the publication |
| Other bias | Low risk | Comment: Non detected |
Croft 1986.
| Study characteristics | ||
| Methods | Design: parallel, randomised Date: not stated Duration: 6 months Number of study centres: 1 Setting: outpatient clinic (1 urban group practice), UK | |
| Participants |
Who participated: 176 newly‐diagnosed hypertensive and obese people Main inclusion criteria: age between 35 and 60 years; BMI > 25 kg/m2; SBP > 140 mm Hg or DBP > 90 mm Hg, or both, in 3 measurements Main exclusion criteria: SBP > 200 mm Hg; DBP > 114 mm Hg; previous antihypertensive medication; myocardial infarction or stroke within the previous 3 months; concurrent serious disease, conditions requiring diets, or medication likely to influence weight or blood pressure Subgroup analyses: none |
|
| Interventions |
Dietary intervention: active dietary advice for weight reduction by 2 experienced dietitians emphasising the importance of weight reduction for blood pressure control (N = 87)
No dietary intervention: visits at general practitioners, no active dietary advice; if participants indicated that they intended to lose weight, they were not discouraged but were given no specific advice or diet sheets (N = 89) Additional treatment: advice about modest restriction of salt use and reduction of excessive alcohol intake |
|
| Outcomes |
Primary outcomes:
1. Mortality: ‐
2. Cardiovascular morbidity: ‐
3. Adverse events: ‐ Secondary outcomes: 1. Changes in systolic blood pressure [mm Hg]: Definition: DBP change from baseline to endpoint visit 2. Changes in diastolic blood pressure [mm Hg]: Definition: DBP change from baseline to endpoint visit 3. Changes in body weight [kg]: Definition: body weight change from baseline to endpoint visit Additional outcomes measured in the study: 1. Start of antihypertensive medication |
|
| Study details |
Length of follow‐up: 6 months Trial terminated before regular end (for benefit / because of adverse events): No Trial ID: ‐ |
|
| Publication details |
Language of publication: English Funding: West Midlands Regional Research Committee; UK Publication status: Full‐text journal publication |
|
| Study aim | Quote from publication: "...to examine the effect of weight reduction on blood pressure in newly diagnosed obese hypertensive patients and to investigate whether weight reduction is more successful in hypertensive dieters than in normotensive dieters." | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: No details on sequence generation are provided, but according to IQWIG report adequate (IQWiG 2006) |
| Allocation concealment (selection bias) | High risk | Comment: Method of concealment is not described; not adequate according to IQWiG report (IQWiG 2006) |
| Blinding (performance bias and detection bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Change in blood pressure | Unclear risk | Comment: No information on blinding |
| Blinding (performance bias and detection bias) Change in body weight | Unclear risk | Comment: No information on blinding |
| Incomplete outcome data (attrition bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Change in blood pressure | Low risk |
Quote: “... The data was submitted to an ’intention to treat’ analysis which included all entrants and assumed that no further change in weight or blood pressure occurred for drop‐outs after the last occasion on which they attended.” Comment: Withdrawals: and reasons/descriptions (dietary intervention vs no dietary intervention): no reasons/descriptions reported: 17 vs 3 |
| Incomplete outcome data (attrition bias) Change in body weight | Low risk |
Quote: “... The data was submitted to an ’intention to treat’ analysis which included all entrants and assumed that no further change in weight or blood pressure occurred for drop‐outs after the last occasion on which they attended.” Comment: Withdrawals: and reasons/descriptions (dietary intervention vs no dietary intervention): no reasons/descriptions reported: 17 vs 3 |
| Selective reporting (reporting bias) | Unclear risk | Comment: No study protocol available; no primary and secondary outcomes were defined |
| Other bias | Low risk | Comment: None detected |
DISH 1985.
| Study characteristics | ||
| Methods | Design: parallel, randomised, open Date: not stated Duration: 13 months (56 weeks) Number of study centres: 4 Setting: outpatient clinic, USA | |
| Participants |
Who participated: 584 people who were previously enrolled in the HDFP treated with antihypertensive drugs and who had sufficiently controlled hypertension. The dietary change on the return of hypertension after withdrawal of prolonged antihypertensive therapy (dish) included 7 treatment arms; the results of 2 of those arms met the inclusion criteria for this review (hypertensive and obese patients with either dietary intervention or not) Main inclusion criteria: HDFP participants; DBP ≥ 95 mm hg on first screening, confirmed by second screening with DBP ≥ 90 mm hg; patients had received antihypertensive medication for at least 5 years; eligible participants had to be "controlled"; hypertensive persons defined by:
Main exclusion criteria: history of congestive heart failure; myocardial infarction; stroke or transient ischaemic attacks; creatinine level ≥ 2.5 mg/dl; ß‐blocker therapy for angina; glucocorticoid therapy for indefinite period Subgroup analyses: results from participants with mild and severe hypertension (not clear whether subgroups were predefined or post hoc) |
|
| Interventions |
Dietary intervention: according to revised "metropolitan life insurance" standards; intervention consisted of 8 initial weekly group sessions followed by monthly sessions plus individual consultation as needed (weight loss component of the trial: N = 87) No dietary intervention: no recommendations (weight loss component of the trial: N = 89) Additional treatment: discontinuation of antihypertensive treatment using a step‐down withdrawal programme; bi‐weekly consultations for BP measurement for 16 weeks followed by monthly consultations; no change in salt uptake |
|
| Outcomes |
Primary outcomes:
1. Mortality: ‐
2. Cardiovascular morbidity: ‐
3. Adverse events:
Definition: withdrawal due to the need to restart antihypertensive medication Secondary outcomes: 1. Changes in systolic blood pressure [mm Hg]: ‐ 2. Changes in diastolic blood pressure [mm Hg]: ‐ 3. Changes in body weight [kg]: Definition: body weight change from baseline to endpoint visit Additional outcomes measured in the study: 1. Number of participants without antihypertensive medication 2. Change in sodium excretion |
|
| Study details |
Length of follow‐up: 13 months (56 weeks ) Trial terminated before regular end (for benefit / because of adverse events): No Trial ID: ‐ |
|
| Publication details |
Language of publication: English Funding: grant from National Heart, Lung and Blood Institute; drugs were supplied by the following companies: Ayerst Laboratories, New York; Merck Sharp & Dohme, West Point, PA; Ciba‐Geigy Corp, Summit, NJ; Boehringer Ingelheim Ltd., Ridgefield, CT; USV Pharmaceutical Corp, Tuckahoe, NY; G.D. Searle & Co, Chicago Publication status: Full‐text journal publication |
|
| Study aim | Quote from publication: "... to determine whether long‐term aggressive antihypertensive therapy can be withdrawn in selected patients without relapse and if the substitution of dietary modification will reduce the recidivism rate." | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: No details on sequence generation are provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: Method of concealment is not described |
| Blinding (performance bias and detection bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Adverse events | Unclear risk | Comment: Open design; participants and investigators not blinded; no information on blinding for outcome assessors |
| Blinding (performance bias and detection bias) Change in blood pressure | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Change in body weight | Unclear risk | Comment: Open design; participants and investigators not blinded; no information on blinding for outcome assessors |
| Incomplete outcome data (attrition bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Adverse events | High risk | Comment: Only withdrawals due to the need to resume antihypertensive medication were reported; no other adverse events were reported |
| Incomplete outcome data (attrition bias) Change in blood pressure | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Change in body weight | High risk |
Comment: Withdrawals: and reasons/descriptions (dietary intervention vs no dietary intervention): concerning the endpoint success of withdrawal from antihypertensive medication: 0 vs 0; concerning body weight at week 56: 20 vs 12; although there were no losses to follow‐up in the relevant subgroups for success of discontinuing antihypertensive treatment, for 13% respectively 23% participants weight at week 56 is not reported |
| Selective reporting (reporting bias) | Unclear risk | Comment: No study protocol available; no primary and secondary outcomes were defined in the publications |
| Other bias | High risk | Comment: 1. Randomisation before consent of participants (possible selection bias) 2. Different body weight at baseline 3. Participants were in previous trial for 5 years (selected population may not be representative) |
Jalkanen 1991.
| Study characteristics | ||
| Methods | Design: parallel, randomised Date: not stated Duration: 12 months Number of study centres: 2 Setting: outpatient clinic (2 hypertension clinics ), Finland | |
| Participants |
Who participated: 50 overweight people with hypertensions (selected from files) Main inclusion criteria: age 35 to 59 years; BMI 27 to 34 kg/m2; DBP ≥ 95 mm Hg Main exclusion criteria: ‐ Subgroup analyses: none |
|
| Interventions |
Dietary intervention: individually‐planned energy‐restricted diet of 1000 to 1500 kcal a day, weekly (after 6 months every 3 weeks); sessions including discussions and lessons on behavioural modification, choice of food, physical exercise, and medical aspects of overweight and weight reduction; 1½ hour duration; total number of lectures about 40 hours; the participants received leaflets on the reduction of salt and fat consumption and on the increase of physical activity; lectures by different medical experts; nutritionists interview; laboratory tests (N = 25) No dietary intervention: visits every 3 months; no personal counselling; nutritionists interview; laboratory tests (N = 25) Additional treatment: participants' doctors were asked to keep the dosage of antihypertensive drugs at the initial level |
|
| Outcomes |
Primary outcomes:
1. Mortality: ‐
2. Cardiovascular morbidity: ‐
3. Adverse events: ‐ Secondary outcomes: 1. Changes in systolic blood pressure [mm Hg]: Definition: SBP change from baseline to endpoint visit 2. Changes in diastolic blood pressure [mm Hg]: Definition: DBP change from baseline to endpoint visit 3. Changes in body weight [kg]: Definition: body weight change from baseline to endpoint visit Additional outcomes measured in the study: 1. Change in lipid parameters 2. Change in potassium and sodium excretions 3. Change in dietary factors (fats and protein) |
|
| Study details |
Length of follow‐up: 12 months Trial terminated before regular end (for benefit / because of adverse events): No Trial ID: ‐ |
|
| Publication details |
Language of publication: English Funding: ‐ Publication status: Full‐text journal publication |
|
| Study aim | Quote from publication: "...to test a comprehensive but practical intervention program aimed for general use in the non‐pharmacological treatment of cardiovascular risk factors, especially overweight, hypertension and high serum lipids, in a primary health care setting." | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: No details on sequence generation are provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: Method of concealment is not described |
| Blinding (performance bias and detection bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Change in blood pressure | Unclear risk | Comment: Open design; participants and investigators not blinded; no information on blinding for outcome assessors |
| Blinding (performance bias and detection bias) Change in body weight | Unclear risk | Comment: Open design; participants and investigators not blinded; no information on blinding for outcome assessors |
| Incomplete outcome data (attrition bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Change in blood pressure | Unclear risk | Comment: ITT analysis unclear; Withdrawals: and reasons/descriptions (dietary intervention vs no dietary intervention): 1 (4%) vs 0; no reasons for withdrawals reported; No information on dealing with missing data |
| Incomplete outcome data (attrition bias) Change in body weight | Unclear risk | Comment: ITT analysis unclear; Withdrawals: and reasons/descriptions (dietary intervention vs no dietary intervention): 1 (4%) vs 0; no reasons for withdrawals reported; No information on dealing with missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: No study protocol available; no primary and secondary outcomes were defined in the publication |
| Other bias | Low risk | Comment: None detected |
ODES 1995.
| Study characteristics | ||
| Methods | Design: parallel, 2 x 2 factorial, randomised, open Date: not stated Duration: 12 months Number of study centres: unclear (probably 1, because all eligible participants were screened at the Ullevaal Hospital, Oslo) Setting: outpatient clinic, Norway | |
| Participants |
Who participated: 219 men and women ≥ 40 years old from screening programme for cardiovascular risk factors in Oslo (Norway) since 1981; participants were post hoc divided in tertiles according to DBP (tertile 1 DBP > 91 mm Hg, tertile 2 DBP 84 to 91 mm Hg, tertile 3 DBP < 84 mm Hg); only subgroups of tertile 1 (DBP > 91 mm Hg) will be reported in this review Main inclusion criteria: all criteria had to be fulfilled simultaneously (based on the screening performed 1 to 10 years before baseline examination): age 41 to 50 years + physical inactivity as measured by questionnaire (exercising at most once a week) + BMI > 24 kg/m2 + DBP 86 to 99 mm Hg + total serum cholesterol 5.20 to 7.74 mmol/l + HDL cholesterol < 1.20 mmol/l, fasting serum triglycerides > 1.4 mmol/l Main exclusion criteria: overt cardiovascular disease, diabetes, treatment with antihypertensive drugs or acetylsalicylic acid, lipid‐lowering diet Subgroup analyses: none |
|
| Interventions |
No‐exercise group: Dietary intervention: individual dietary counselling for each participant together with participant's spouse; main emphasis was a low‐calorie diet and a substantial increase in the intake of fish and fish products, an increase in the consumption of vegetables and fibre‐rich products of complex carbohydrates, and a reduction in intake of sugar and saturated fat; target body weight reduction was agreed upon, usually 0.5 to 1 kg monthly according to Anderssen 1995 and 0.5 to 2 kg according to the design paper Urdal 1993; hypertensive participants were also advised to reduce salt intake Follow‐up of dietary habits took place at months 3 and 9 (N = 122; hypertensive subgroup: N = not stated) No dietary intervention: no dietary counselling, no change in lifestyle (N = 97; hypertensive subgroup: N = not stated) Exercise group: Dietary intervention + exercise: individual counselling as mentioned above as well as additional supervised aerobic exercise programme consisting of circuit training and jogging for 1 hour 3 times a week No dietary intervention + exercise: no dietary counselling but same exercise programme as mentioned above Additional treatment: all participants were advised against smoking |
|
| Outcomes |
Primary outcomes:
1. Mortality: ‐
2. Cardiovascular morbidity: ‐
3. Adverse events: ‐ Secondary outcomes: 1. Changes in systolic blood pressure [mm Hg]: Definition: SBP change from baseline to endpoint visit 2. Changes in diastolic blood pressure [mm Hg]: Definition: DBP change from baseline to endpoint visit 3. Changes in body weight [kg]: Definition: changes in BMI from baseline to endpoint visit Additional outcomes measured in the study: 1. effect on haemostatic variables (primary study endpoint) |
|
| Study details |
Length of follow‐up: 12 months Trial terminated before regular end (for benefit / because of adverse events): No Trial ID: ‐ |
|
| Publication details |
Language of publication: English Funding: supported by grant from the Research Council of Norway, the Norwegian Council of Cardiovascular Diseases, and the insurance company Vital Friskvern Publication status: Full‐text journal publication |
|
| Study aim | Quote from publication: "...to test whether dietary changes, exercise, or the combination affects the haemostatic system." | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk |
Quote: "Each participant has a 25% chance of being allocated to each of the four treatment groups. The list is not blocked in any way, but randomization is stratified by sex." Comment: No details on sequence generation are provided |
| Allocation concealment (selection bias) | Low risk | Quote: "A sealed envelope is opened, revealing the randomization number and the name of the group to which the participant has been allocated." No information about numbered or opaque envelopes |
| Blinding (performance bias and detection bias) Total mortality | Low risk |
Quote: "Unmasked, but blinded objective blood analyse Comment: Participants, investigators and outcome assessors not blinded |
| Blinding (performance bias and detection bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Change in blood pressure | High risk |
Quote: "Unmasked, but blinded objective blood analyses" Comment: Participants, investigators and outcome assessors not blinded |
| Blinding (performance bias and detection bias) Change in body weight | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Total mortality | High risk |
Comment: No ITT analysis; withdrawals not reported for the hypertensive subgroup (tertile 1); withdrawals for the whole study population of normo‐ and hypertensives: No‐exercise subgroup (dietary intervention vs no dietary intervention): 3 vs 0 Exercise subgroup (dietary intervention vs no dietary intervention): 2 vs 5 reasons for dropouts:
|
| Incomplete outcome data (attrition bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Change in blood pressure | High risk |
Comment: No ITT analysis, although it was initially planned; withdrawals not reported for the hypertensive subgroup (tertile 1); withdrawals for the whole study population of normo‐ and hypertensives: No‐exercise subgroup (dietary intervention vs no dietary intervention): 3 vs 0 Exercise subgroup (dietary intervention vs no dietary intervention): 2 vs 5 reasons for dropouts:
|
| Incomplete outcome data (attrition bias) Change in body weight | Unclear risk | Comment: Outcome not reported |
| Selective reporting (reporting bias) | High risk | Comment: Post hoc analyses of blood pressure; not all predefined outcomes are reported for each tertile (e.g. quality of life) |
| Other bias | High risk | Comment: 1. Multiple testing was done without adjustment (e.g. Bonferroni correction) 2. Hypertensive participants in dietary‐intervention group advised to reduce salt intake (intervention bias) 3. Tertile 3 was defined as DBP < 84 mm Hg, whereas inclusion criteria was DBP > 86 mm Hg. In total, 68 participants (31%) were analysed in tertile 3 |
ODES 1995 no exercise.
| Study characteristics | ||
| Methods | see ODES 1995 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Study details | ||
| Publication details | ||
| Study aim | ||
| Notes | ||
ODES 1995 with exercise.
| Study characteristics | ||
| Methods | see ODES 1995 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Study details | ||
| Publication details | ||
| Study aim | ||
| Notes | ||
Ruvolo 1994.
| Study characteristics | ||
| Methods | Design: parallel, randomised Date: not stated Duration: 6 months Number of study centres: 1 Setting: outpatient clinic, Italy | |
| Participants |
Who participated: 32 overweight hypertensive patients on 10 mg amlodipine daily Main inclusion criteria: BMI > 30 kg/m2, DBP > 100 mm Hg Main exclusion criteria: heart failure, coronary artery disease, diabetes mellitus Subgroup analyses: ‐ |
|
| Interventions | Dietary intervention: weight‐reducing diet, no restriction on salt uptake (N = 16) No dietary intervention: no counselling (N = 16) Additional treatment: amlodipine 10 mg | |
| Outcomes |
Primary outcomes:
1. Mortality: ‐
2. Cardiovascular morbidity: ‐
3. Adverse events: reported: ‐ Secondary outcomes: 1. Changes in systolic blood pressure [mm Hg]: Definition: SBP change from baseline to endpoint visit 2. Changes in diastolic blood pressure [mm Hg]: Definition: DBP change from baseline to endpoint visit 3. Changes in body weight [kg]: Definition: body weight change from baseline to endpoint visit Additional outcomes measured in the study: 1. Change in left ventricular dimensions 2. Change in heart rate |
|
| Study details |
Length of follow‐up: 6 months Trial terminated before regular end (for benefit / because of adverse events): No Trial ID: ‐ |
|
| Publication details |
Language of publication: Italian Funding: ‐ Publication status: Full‐text journal publication |
|
| Study aim | Quote from publication: "Scopo di questo studio è valutare se l´impostazione di un regime dietetico ipocalorico possa determinare modificazioni significative a carico del ventricolo sinistro in pazienti obesi ed ipertesi trattati con amlodipina." | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: No details on sequence generation are provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: Method of concealment is not described |
| Blinding (performance bias and detection bias) Total mortality | Low risk | Comment: Participants not blinded; no information on blinding for investigators or outcome assessors |
| Blinding (performance bias and detection bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Change in blood pressure | Unclear risk | Comment: Participants not blinded; no information on blinding for investigators or outcome assessors |
| Blinding (performance bias and detection bias) Change in body weight | Unclear risk | Comment: Participants not blinded; no information on blinding for investigators or outcome assessors |
| Incomplete outcome data (attrition bias) Total mortality | High risk | Comment: ITT analysis unclear; withdrawals (dietary intervention vs no dietary intervention): 2 (13%) vs. 0; reasons for withdrawal not reported |
| Incomplete outcome data (attrition bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Change in blood pressure | High risk | Comment: ITT analysis unclear; withdrawals (dietary intervention vs no dietary intervention): 2 (13%) vs. 0 |
| Incomplete outcome data (attrition bias) Change in body weight | High risk | Comment: ITT analysis unclear; withdrawals (dietary intervention vs no dietary intervention): 2 (13%) vs. 0 |
| Selective reporting (reporting bias) | Unclear risk | Comment: No study protocol provided; no primary and secondary outcomes were defined in the publication |
| Other bias | Low risk | Comment: None detected |
TAIM 1992.
| Study characteristics | ||
| Methods | Design: 3x3 factorial, randomised, open Date: 1985 ‐ 1993 Duration: 6 months (phase I) Number of study centres: 3 Setting: outpatient clinic at 3 university hospitals (Bronx (New York), Birmingham (Alabama), Jackson (Mississippi)), USA | |
| Participants |
Who participated:878 obese hypertensive patients
The trial consisted of 2 phases. Phase I was performed in a 3 x 3 factorial design with follow‐up of 6 months. Phase II was performed in a 2 x 2 factorial design (usual care vs weight‐reducing diet). Since dropout in usual‐care group was 29% to 36% for phase II, only phase I will be analysed Main inclusion criteria: age 21 to 65 years; 110% to 116% of ideal body weight; sitting DBP (preliminary screened: treated ≤ 100 mm Hg, untreated 90 to 104 mm Hg; first clinic visit: 90 to 100 mm Hg; second clinic visit: < 115 mm Hg); no antihypertensive medication or discontinuation of current medication for at least 2 weeks before baseline BP measurement Main exclusion criteria: myocardial infarction within 1 year before study entry; medical history of stroke, bronchial asthma, insulin‐dependent diabetes mellitus, or allergy to thiazides or ß‐blockers; other major diseases (e.g. kidney disease, liver disease, or cancer); baseline creatinine ≥ 2 mg/dl; pregnancy; scheduled surgery Subgroup analyses: none |
|
| Interventions |
Dietary intervention: weight‐reducing diet (standard programme of diet counselling and nutrition education with the goal of a reduction of 10% of baseline weight or 4.54 kg, whichever was greater); 10 weekly group sessions within the first 6 months, subsequently individual or group counselling sessions with a nutritionist at least every 6 weeks, after 12 months dietary counselling on a quarterly basis (weight loss component of the trial: N = 291)
No dietary intervention: no diet and nutritional counselling or education (weight loss component of the trial: N = 296) Additional treatment: pharmacological antihypertensive treatment according to subgroup allocation (placebo or diuretic or ß‐blocker); medication was stepped up if BP reached predefined escape levels; regular monthly clinic visits for the first 6 months, every 3 months thereafter |
|
| Outcomes |
Primary outcomes:
1. Mortality: ‐
2. Cardiovascular morbidity: ‐
3. Adverse events: ‐ Secondary outcomes: 1. Changes in systolic blood pressure [mm Hg]: Definition: SBP change from baseline to endpoint visit 2. Changes in diastolic blood pressure [mm Hg]: Definition: DBP change from baseline to endpoint visit 3. Changes in body weight [kg]: Definition: body weight change from baseline to endpoint visit Additional outcomes measured in the study: 1. Change in sodium excretion 2. Change in potassium excretion 3. Quality of life (life satisfaction scale) 4. Symptoms and mental function (symptom checklist) 5. Expected side effects due to use of ß‐blocker (physical complaint inventory) |
|
| Study details |
Length of follow‐up: 6 months (phase I) Trial terminated before regular end (for benefit / because of adverse events): No Trial ID: ‐ |
|
| Publication details |
Language of publication: English Funding: National Heart, Lung and Blood Institute Publication status: Full‐text journal publication |
|
| Study aim | Quote from publication: "...to assess the 6‐month effectiveness of weight loss and low sodium/high potassium diets, alone or in combination with diuretics or ß‐blockers, in lowering diastolic blood pressure in persons with mild hypertension." | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: No details on sequence generation are provided in publications, but according to IQWIG report adequate (IQWiG 2006) |
| Allocation concealment (selection bias) | Low risk | Comment: Method of concealment is not described in publications, but according to IQWIG report adequate (IQWiG 2006) |
| Blinding (performance bias and detection bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Change in blood pressure | Unclear risk | Comment: Participants, study personnel were not blinded, but data collection staff was masked to intervention assignment |
| Blinding (performance bias and detection bias) Change in body weight | Unclear risk | Comment: Participants, study personnel were not blinded, but data collection staff was masked to intervention assignment |
| Incomplete outcome data (attrition bias) Total mortality | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Cardiovascular morbidity | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Change in blood pressure | High risk | Comment: No ITT analyses; withdrawals ranged from 1% to 12% in the study groups |
| Incomplete outcome data (attrition bias) Change in body weight | High risk | Comment: No ITT analyses; withdrawals ranged from 1% to 12% in the study groups |
| Selective reporting (reporting bias) | Low risk | Comment: Outcomes are reported as prespecified |
| Other bias | High risk | Comment: 1. Step‐up medication: 20% (placebo/usual diet) vs 10% (placebo/weight‐reducing diets); it is unclear how many participants required an additional open‐label antihypertensive treatment; indication for step‐up therapy is presented inconsistently between study‐related publications 2. Number of randomised participants (878) is below calculated sample size (918), although 1940 participants were eligible |
TAIM 1992 atenolol.
| Study characteristics | ||
| Methods | see TAIM 1992 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Study details | ||
| Publication details | ||
| Study aim | ||
| Notes | ||
TAIM 1992 chlorthalidone.
| Study characteristics | ||
| Methods | see TAIM 1992 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Study details | ||
| Publication details | ||
| Study aim | ||
| Notes | ||
TAIM 1992 combined.
| Study characteristics | ||
| Methods | see TAIM 1992 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Study details | ||
| Publication details | ||
| Study aim | ||
| Notes | ||
TAIM 1992 placebo.
| Study characteristics | ||
| Methods | see TAIM 1992 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Study details | ||
| Publication details | ||
| Study aim | ||
| Notes | ||
TONE 1998.
| Study characteristics | ||
| Methods | Design: parallel, 2 x 2 factorial, randomised, blinded endpoint evaluation Date: August 1992 ‐ December 1995 Duration: 15 to 36 months Number of study centres: 4 Setting:outpatient clinic, USA | |
| Participants |
Who participated: 975 elderly, overweight and non‐overweight, people with hypertension; participants were assigned to active intervention: sodium reduction (S+), or weight loss (only overweight participants), or sodium reduction (S+) and weight loss (only overweight participants) vs usual care Main inclusion criteria: age 60 to 80 years; BMI ≥ 27.8 kg/m2 (men), BMI ≥ 27.3 kg/m2 (women); SBP < 145 mm Hg and DBP < 85 mm Hg while taking 1 antihypertensive medication or 2 antihypertensive medications if 1 can be stopped during screening phase (combination of 1 diuretic and 1 non‐diuretic drug are considered as 1 drug) Main exclusion criteria: heart attack or stroke within preceding 6 months; angina; congestive heart failure; insulin‐dependent diabetes mellitus; BMI > 33 kg/m2 (men), BMI > 37 kg/m2 (women); unexplained or involuntary weight loss of 4.5 kg or greater during previous year; hypercreatinaemia; hyperkalaemia; hyperglycaemia; anaemia Subgroup analyses: age, gender, ethnicity |
|
| Interventions |
Dietary intervention: achieving and maintaining a weight loss of 4.5 kg or greater; structured programmes with dietary advice provided to participants mainly in small groups to change their eating behaviours and to motivate participants to achieve and maintain their desired reductions; participants were required to increase amount of physical activity, but no detailed information was provided (weight loss component of the trial: N = 294)
No dietary intervention: no study‐related counselling (weight loss component of the trial: N = 294) Additional treatment: Salt restriction (S+): achieving and maintaining a 24‐hour dietary sodium intake of 80 mmol or less (as measured by 24‐hour urine collection) |
|
| Outcomes |
Primary outcomes:
1. Mortality: reported
2. Cardiovascular morbidity: reported
3. Adverse events:
Definition: presumed adverse events were assessed using a standardised approach that included questioning of participants, family members, and physicians and a review of physicians' records with blinded evaluation Secondary outcomes: 1. Changes in systolic blood pressure [mm Hg]: ‐ 2. Changes in diastolic blood pressure [mm Hg]: ‐ 3. Changes in body weight [kg]: reported for the combined groups only (both intervention (IG‐S+ and IG‐S‐) vs both control (CG‐S+ and CG‐S‐) groups) Additional outcomes measured in the study: 1. Primary study endpoint: failure of antihypertensive drug withdrawal due to: a. occurrence of high blood pressure measured at 1 or more follow‐up visits according predefined values b. restart of treatment with antihypertensive medication due to other reasons or based on the decision of the treating doctors or study participants c. occurrence of clinical cardiovascular disease complications during follow‐up 2. Weight reduction |
|
| Study details |
Length of follow‐up: 15 to 36 months Trial terminated before regular end (for benefit / because of adverse events): No Trial ID: ‐ |
|
| Publication details |
Language of publication: English Funding: National Heart, Lung and Blood Institute and National Institute on Aging grants Publication status: Full‐text journal publication |
|
| Study aim | Quote from publication: "...to determine the feasibility, efficacy, and safety of sodium reduction and weight loss in older persons with hypertension." | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "using a computer program ... stratified by clinic and weight status ... blocking of variable length" |
| Allocation concealment (selection bias) | Low risk | Comment: Method of concealment is not described in publication, but according to IQWIG report supposable adequate (IQWiG 2006) |
| Blinding (performance bias and detection bias) Total mortality | Low risk | Comment: Participants, study personnel were not blinded, but an independent committee masked to intervention assignment evaluated the endpoints |
| Blinding (performance bias and detection bias) Cardiovascular morbidity | Unclear risk | Comment: Participants, study personnel were not blinded, but an independent committee masked to intervention assignment evaluated the endpoints |
| Blinding (performance bias and detection bias) Adverse events | Unclear risk | Comment: Participants, study personnel were not blinded, but an independent committee masked to intervention assignment evaluated the endpoints |
| Blinding (performance bias and detection bias) Change in blood pressure | Unclear risk | Comment: Outcome not reported |
| Blinding (performance bias and detection bias) Change in body weight | Unclear risk | Comment: Participants, study personnel were not blinded, but an independent committee masked to intervention assignment evaluated the endpoints |
| Incomplete outcome data (attrition bias) Total mortality | Low risk | Comment: Numbers of withdrawals and reasons are missing, but 96% to 99% of participants were included at follow‐up analysis |
| Incomplete outcome data (attrition bias) Cardiovascular morbidity | Low risk | Comment: Numbers of withdrawals and reasons are missing, but 96% to 99% of participants were included at follow‐up analysis |
| Incomplete outcome data (attrition bias) Adverse events | High risk | Comment: No usable results were reported |
| Incomplete outcome data (attrition bias) Change in blood pressure | Unclear risk | Comment: Outcome not reported |
| Incomplete outcome data (attrition bias) Change in body weight | Low risk | Comment: Numbers of withdrawals and reasons are missing, but 96% to 99% of participants were included at follow‐up analysis |
| Selective reporting (reporting bias) | Low risk | Comment: Outcomes are reported as prespecified |
| Other bias | Low risk | Comment: None detected |
BMI: body mass index BP: blood pressure DBP: diastolic blood pressure HDFP: Hypertension Detection an Follow‐up Program HDL: high‐density lipoprotein LOCF: last observation carried forward analysis SBP: systolic blood pressure
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| (no authors listed) 1993 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Abou‐Raya 2014 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| ACTRN12610000049077 | The study is not a randomised controlled trial |
| Allison 2016 | The intervention in this study is not a weight‐reducing diet |
| Andersen 1985 | The intervention in this study is not a weight‐reducing diet |
| Andrews 2011 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Angelico 2009 | Full text of this study is not available |
| Appel 2006 | The intervention in this study is not a weight‐reducing diet |
| Ard 2005 | The study is not a randomised controlled trial |
| Ard 2017 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Balas‐Nakash 2014 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Banos 2015 | The study includes a combination of different interventions |
| Bao 1999 | Full text of this study is not available |
| Bartels 1974 | The duration of the intervention is less than 24 weeks |
| Bazian 2004 | The study includes a combination of different interventions |
| Bennett 2018 | The study includes a combination of different interventions |
| Bouchonville 2014 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Cakir 2006 | The study includes a combination of different interventions |
| Cambien 1986 | Full text of this study is not available |
| Camhi 2010 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Chen 2009 | The intervention in this study is not a weight‐reducing diet |
| Childress 2008 | Full text of this study is not available |
| Chirinos 2016 | The study includes a combination of different interventions |
| Christensen 2013 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Coppell 2010 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Curzio 1989 | No electronic records and/or hard copies available, therefore insufficient data for inclusion (personal communication) |
| Cutler 1997 | The study includes a combination of different interventions |
| De Mello 2008 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Diaz 2014 | The study does not include participants with essential hypertension |
| Di Mauro 1998 | The control intervention in the study is inappropriate |
| Ebell 2013 | The study is not a randomised controlled trial |
| Fagerberg 1989 | The study includes different accompanying therapies |
| Gilliam 2012 | The study is not a randomised controlled trial |
| Gillum 1983 | The duration of the intervention is less than 24 weeks |
| Hall 2003 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Han 2017 | The control intervention in the study is inappropriate |
| Haynes 1984 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Hayward 2010 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| He 2000 | The study does not include participants with essential hypertension |
| Heinberg 2000 | The study includes a combination of different interventions |
| Heshka 2003 | The study is not a randomised controlled trial |
| Heyden 1974 | The study includes a combination of different interventions |
| Hsieh 2009 | The study is not a randomised controlled trial |
| Hua 2017 | The study includes a combination of different interventions |
| Hyden 1973 | The study includes a combination of different interventions |
| IRCT2015062422905N1 | The control intervention in the study is inappropriate |
| Jones 1999 | In this study the control group also includes a weight‐reducing dietary intervention |
| Kanke 2015 | The control intervention in the study is inappropriate |
| Karoff 1985 | The duration of the intervention is less than 24 weeks |
| Karvetti 1992 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Katzel 1995 | The study does not include participants with essential hypertension |
| Kawamura 1993 | The duration of the intervention is less than 24 weeks |
| Kittiskulnam 2014 | The study does not include participants with essential hypertension |
| Kolehmainen 2008 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Koopman 1990 | The intervention in this study is not a weight‐reducing diet |
| Korhonen 2003 | Full text of this study is not available |
| Larson‐Meyer 2010 | The study does not include participants with essential hypertension |
| Lindgarde 2001 | The intervention in this study is not a weight‐reducing diet |
| Mason 2013 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Masuo 2012 | The study includes a combination of different interventions |
| McCarron 2000 | The duration of the intervention is less than 24 weeks |
| Melchart 2015 | The study includes a combination of different interventions |
| Metz 2000 | In this study the control group also includes a weight‐reducing dietary intervention |
| Moore 2013 | The control intervention in the study is inappropriate |
| NCT00142649 | The control intervention in the study is inappropriate |
| NCT00661817 | The intervention in this study is not a weight‐reducing diet |
| NCT00783315 | The control intervention in the study is inappropriate |
| NCT01724645 | The duration of the intervention is less than 24 weeks |
| NCT02136264 | The control intervention in the study is inappropriate |
| NCT02445833 | The study is not a randomised controlled trial |
| NCT02454127 | The control intervention in the study is inappropriate |
| NCT03288142 | The intervention in this study is not a weight‐reducing diet |
| Neuhouser 2012 | The intervention in this study is not a weight‐reducing diet |
| Noble 1971 | The duration of the intervention is less than 24 weeks |
| Oshakbayev 2016 | The study includes a combination of different interventions |
| Poppitt 2002 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Prentice 2017 | The intervention in this study is not a weight‐reducing diet |
| Pritchard 2002 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Reisin 1978 | The duration of the intervention is less than 24 weeks |
| Rissanen 1985 | The study is not a randomised controlled trial |
| Rosas 2015 | The study includes a combination of different interventions |
| Salas‐Salvado 2008 | The intervention in this study is not a weight‐reducing diet |
| Salinardi 2012 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Samaha 2003 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Schwab 2008 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Sedjo 2016 | The study includes a combination of different interventions |
| Stamler 1985 | The study includes a combination of different interventions |
| Tate 2011 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Trepanowski 2014 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Tunyan 2007 | The study includes a combination of different interventions |
| Tuomilehto 2009 | The study does not include participants with essential hypertension |
| Ueki 2016 | The intervention in this study is not a weight‐reducing diet |
| UMIN000002967 | The control intervention in the study is inappropriate |
| UMIN000006582 | The duration of the intervention is less than 24 weeks |
| UMIN000029395 | The control intervention in the study is inappropriate |
| Vissers 2010 | The study does not include participants with essential hypertension |
| Weil 2016 | The control intervention in the study is inappropriate |
| Weiss 2016 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| WHO Europ.Coll.Grp. 1974 | The study is not a randomised controlled trial |
| Wright 2017 | The intervention in this study is not a weight‐reducing diet |
| Yamada 2013 | The study includes normotensive and hypertensive participants but reports no or insufficient results for the hypertensive subgroup |
| Zotova 2015 | The control intervention in the study is inappropriate |
Differences between protocol and review
Three new authors (Thomas Semlitsch, Christoph Pachler, and Reinhard Strametz) joined the team of review authors for the 2011 version of this review and provided substantive intellectual contributions that justify their inclusion as authors.
Nicole Pignitter changed her name to Nicole Posch due to marriage, and her new name was used in the 2016 update of this review.
Four authors (Andreas Waltering, Lars Hemkens, Christoph Pachler, and Reinhard Strametz) did not contribute to the 2016 update of this review and were removed from the list of authors.
Stephanie Poggenburg joined the team of authors for the 2016 update of this review and provided substantive intellectual contributions that justify her inclusion as author.
Two authors (Nicole Posch and Stephanie Poggenburg) did not contribute to the 2020 update of this review and were removed from the list of authors.
Cornelia Krenn joined the team of authors for the 2020 update of this review and provided substantive intellectual contributions that justify her inclusion as author.
Contributions of authors
Thomas Semlitsch: selection of studies, quality assessment of trials, data extraction, development of review updates, corresponding author.
Cornelia Krenn: selection of studies, development of review update.
Klaus Jeitler: protocol development, searching for trials for the initial version of the review, quality assessment of trials, data extraction.
Andrea Berghold: statistical analysis, development of final review.
Karl Horvath: protocol development, quality assessment of trials, data extraction, development of final review.
Andrea Siebenhofer: protocol development, quality assessment of trials, selection of studies, data extraction, development of final review and review update.
Sources of support
Internal sources
-
Medical University of Graz, Austria
Salary, office space, computer support, library resources
-
Institute of General Practice, Goethe University Frankfurt, Germany
Salary
External sources
No sources of support supplied
Declarations of interest
Andrea Siebenhofer, Klaus Jeitler, and Karl Horvath were involved in the preparation of a report on the evaluation of the benefits and harms of non‐drug treatment strategies in people with essential hypertension: weight reduction for IQWiG, (German Institute for Quality and Efficiency in Health Care (iqwig.de/)).
Andrea Berghold: No known conflicts of interest.
Thomas Semlitsch: No known conflicts of interest.
Cornelia Krenn: No known conflicts of interest.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Cohen 1991 {published data only}
- Cohen MD, D'Amico FJ, Merenstein JH. Weight reduction in obese hypertensive patients. Family Medicine 1991;23(1):25-8. [PMID: ] [PubMed] [Google Scholar]
Croft 1986 {published data only}
- Croft PR, Brigg D, Smith S, Harrison CB, Branthwaite A, Collins MF. How useful is weight reduction in the management of hypertension? Journal of the Royal College of General Practitioners 1986;36(291):445-8. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
DISH 1985 {published data only}
- Blaufox MD, Langford HG, Oberman A, Hawkins CM, Wassertheil-Smoller SW, Cutter GR. Effect of dietary change on the return of hypertension after withdrawal of prolonged antihypertensive therapy (DISH). Dietary Intervention Study of Hypertension. Journal of Hypertension. Supplement: Official Journal of the International Society of Hypertension 1984;2(3):S179-81. [PMID: ] [PubMed] [Google Scholar]
- Langford HG, Blaufox MD, Oberman A, Hawkins CM, Curb JD, Cutter GR, et al. Dietary therapy slows the return of hypertension after stopping prolonged medication. JAMA 1985;253(5):657-64. [PMID: ] [PubMed] [Google Scholar]
- Langford HG, Blaufox MD, Oberman A, Hawkins CM, Curb JD, Cutter GR, et al. Return of hypertension after withdrawal of prolonged antihypertensive therapy, effect of weight loss, sodium reduction, and baseline factors. Transactions of the Association of American Physicians 1984;97:190-6. [PMID: ] [PubMed] [Google Scholar]
Jalkanen 1991 {published data only}
- Jalkanen L. The effect of a weight reduction program on cardiovascular risk factors among overweight hypertensives in primary health care. Scandinavian Journal of Social Medicine 1991;19(1):66-71. [PMID: ] [DOI] [PubMed] [Google Scholar]
ODES 1995 {published data only}
- Anderssen S, Holme I, Urdal P, Hjermann I. Diet and exercise intervention have favourable effects on blood pressure in mild hypertensives: the Oslo Diet and Exercise Study (ODES). Blood Pressure 1995;4(6):343-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Anderssen SA, Carroll S, Urdal P, Holme I. Combined diet and exercise intervention reverses the metabolic syndrome in middle-aged males: Results from the Oslo Diet and Exercise Study. Scandinavian Journal of Medicine and Science in Sports 2007;17(6):687-95. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Anderssen SA, Hjermann I, Urdal P, Torjesen PA, Holme I. Improved carbohydrate metabolism after physical training and dietary intervention in individuals with the 'atherothrombogenic syndrome'. Oslo Diet and Exercise Study (ODES). A randomized trial. Journal of Internal Medicine 1996;240(4):203-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Jacobs DR Jr, Sluik D, Rokling-Andersen MH, Anderssen SA, Drevon CA. Association of 1-y changes in diet pattern with cardiovascular disease risk factors and adipokines: results from the 1-y randomized Oslo Diet and Exercise Study. American Journal of Clinical Nutrition 2009;89(2):509-17. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Torjesen PA, Birkeland KI, Anderssen SA, Hjermann I, Holme I, Urdal P. Lifestyle changes may reverse development of the insulin resistance syndrome. The Oslo Diet and Exercise Study: a randomized trial. Diabetes Care 1997;20(1):26-31. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Urdal P, Haaland A, Hjermann I, Gjesdal K, Christian C, Sorensen M, et al. The Oslo Diet and Exercise Study (ODES): Design and objectives. Controlled Clinical Trials 1993;14(3):229-43. [DOI] [PubMed] [Google Scholar]
ODES 1995 no exercise {published data only}
- Anderssen S, Holme I, Urdal P, Hjermann I. Diet and exercise intervention have favourable effects on blood pressure in mild hypertensives: the Oslo Diet and Exercise Study (ODES). Blood Pressure 1995;4(6):343-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
ODES 1995 with exercise {published data only}
- Anderssen S, Holme I, Urdal P, Hjermann I. Diet and exercise intervention have favourable effects on blood pressure in mild hypertensives: the Oslo Diet and Exercise Study (ODES). Blood Pressure 1995;4(6):343-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ruvolo 1994 {published data only}
- Ruvolo G, Greco E, Speziale G, Di Natale M, Marino B. The effect on left ventricular mass of treatment with amlodipine and diet therapy in obese patients with arterial hypertension [Effetti sulla massa ventricolare sinistra del trattamento con amlodipina e dietoterapia in pazienti obesi affetti da ipertensione arteriosa]. Minerva Cardioangiologica 1994;42(6):289-92. [PMID: ] [PubMed] [Google Scholar]
TAIM 1992 {published data only}
- Blaufox MD, Lee HB, Davis B, Oberman A, Wassertheil-Smoller S, Langford H. Renin predicts diastolic blood pressure response to nonpharmacologic and pharmacologic therapy. JAMA 1992;267(9):1221-5. [PMID: ] [PubMed] [Google Scholar]
- Davis BR, Blaufox MD, Hawkins CM, Langford HG, Oberman A, Swencionis C, et al. Trial of antihypertensive interventions and management. Design, methods, and selected baseline results. Controlled Clinical Trials 1989;10(1):11-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Davis BR, Blaufox MD, Oberman A, Wassertheil-Smoller S, Zimbaldi N, Cutler JA, et al. Reduction in long-term antihypertensive medication requirements. Effects of weight reduction by dietary intervention in overweight persons with mild hypertension. Archives of Internal Medicine 1993;153(15):1773-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Davis BR, Oberman A, Blaufox MD, Wassertheil-Smoller S, Hawkins CM, Cutler JA, et al. Effect of antihypertensive therapy on weight loss. The Trial of Antihypertensive Interventions and Management Research Group. Hypertension 1992;19(4):393-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Davis BR, Oberman A, Blaufox MD, Wassertheil-Smoller S, Zimbaldi N, Kirchner K, et al. Lack of effectiveness of a low-sodium/high-potassium diet in reducing antihypertensive medication requirements in overweight persons with mild hypertension. TAIM Research Group. Trial of Antihypertensive Interventions and Management. American Journal of Hypertension 1994;7(10 Pt 1):926-32. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Langford HG, Davis BR, Blaufox D, Oberman A, Wassertheil-Smoller S, Hawkins M, et al. Effect of drug and diet treatment of mild hypertension on diastolic blood pressure. The TAIM Research Group. Hypertension 1991;17(2):210-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Oberman A, Wassertheil-Smoller S, Langford HG, Blaufox MD, Davis BR, Blaszkowski T, et al. Pharmacologic and nutritional treatment of mild hypertension: changes in cardiovascular risk status. Annals of Internal Medicine 1990;112(2):89-95. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Wassertheil-Smoller S, Blaufox MD, Davis BR, Kirchner K, Langford HG, Oberman A. The trial of antihypertensive interventions and management (TAIM). Nieren- und Hochdruckkrankheiten 1994;23 (Suppl 1):S22-7. [Google Scholar]
- Wassertheil-Smoller S, Blaufox MD, Oberman AS, Langford HG, Davis BR, Wylie-Rosett J. The Trial of Antihypertensive Interventions and Management (TAIM) study. Adequate weight loss, alone and combined with drug therapy in the treatment of mild hypertension. Archives of Internal Medicine 1992;152(1):131-6. [PMID: ] [PubMed] [Google Scholar]
- Wassertheil-Smoller S, Davis BR, Oberman A. The TAIM Study: Sex-race differences in effects of diet and drugs on cardiovascular risk. Cardiovascular Risk Factors 1991;1(7):427-35. [Google Scholar]
- Wassertheil-Smoller S, Oberman A, Blaufox MD, Davis B, Langford H. The Trial of Antihypertensive Interventions and Management (TAIM) Study. Final results with regard to blood pressure, cardiovascular risk, and quality of life. American Journal of Hypertension 1992;5(1):37-44. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Wylie-Rosett J, Wassertheil-Smoller S, Blaufox MD, Davis BR, Langford HG, Oberman A, et al. Trial of antihypertensive intervention and management: greater efficacy with weight reduction than with a sodium-potassium intervention. Journal of the American Dietetic Association 1993;93(4):408-15. [PMID: ] [DOI] [PubMed] [Google Scholar]
TAIM 1992 atenolol {published data only}
- Davis BR, Blaufox MD, Oberman A, Wassertheil-Smoller S, Zimbaldi N, Cutler JA, et al. Reduction in long-term antihypertensive medication requirements. Effects of weight reduction by dietary intervention in overweight persons with mild hypertension. Archives of Internal Medicine 1993;153(15):1773-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
TAIM 1992 chlorthalidone {published data only}
- Davis BR, Blaufox MD, Oberman A, Wassertheil-Smoller S, Zimbaldi N, Cutler JA, et al. Reduction in long-term antihypertensive medication requirements. Effects of weight reduction by dietary intervention in overweight persons with mild hypertension. Archives of Internal Medicine 1993;153(15):1773-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
TAIM 1992 combined {published data only}
- Davis BR, Blaufox MD, Oberman A, Wassertheil-Smoller S, Zimbaldi N, Cutler JA, et al. Reduction in long-term antihypertensive medication requirements. Effects of weight reduction by dietary intervention in overweight persons with mild hypertension. Archives of Internal Medicine 1993;153(15):1773-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
TAIM 1992 placebo {published data only}
- Davis BR, Blaufox MD, Oberman A, Wassertheil-Smoller S, Zimbaldi N, Cutler JA, et al. Reduction in long-term antihypertensive medication requirements. Effects of weight reduction by dietary intervention in overweight persons with mild hypertension. Archives of Internal Medicine 1993;153(15):1773-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
TONE 1998 {published data only}
- Appel LJ, Espeland M, Whelton PK, Dolecek T, Kumanyika S, Applegate WB, et al. Trial of Nonpharmacologic Intervention in the Elderly (TONE). Design and rationale of a blood pressure control trial. Annals of Epidemiology 1995;5(2):119-29. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Bahnson JL, Whelton PK, Appel LJ, Espeland MA, Wofford JL, Rosen R, et al. Baseline characteristics of randomized participants in the trial of nonpharmacologic intervention in the elderly (TONE). Disease Management & Clinical Outcomes 1997;1(2):61-8. [Google Scholar]
- Espeland MA, Whelton PK, Kostis JB, Bahnson JL, Ettinger WH, Cutler JA, et al. Predictors and mediators of successful long-term withdrawal from antihypertensive medications. Archives of Family Medicine 1999;8(3):228-36. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Fessler B. Sodium reduction and weight loss instead of treatment with antihypertensive agents. Deutsche Apotheker Zeitung 1998;138(26):36-9. [Google Scholar]
- Kostis JB, Wilson AC, Shindler DM, Cosgrove NM, Lacy CR. Persistence of normotension after discontinuation of lifestyle intervention in the trial of TONE. Trial of Nonpharmacologic Interventions in the Elderly. American Journal of Hypertension 2002;15(8):732-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kumanyika SK, Espeland MA, Bahnson JL, Bottom JB, Charleston JB, Folmar S, et al. Ethnic comparison of weight loss in the Trial of Nonpharmacologic Interventions in the Elderly. Obesity Research 2002;10(2):96-106. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH Jr, Kostis JB, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA 1998;279(11):839-46. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
(no authors listed) 1993 {published data only}
- Hypertension Prevention Collaborative Research Group. The impact of weight loss on blood pressure. Patient Care 1993;27(17):16. [Google Scholar]
Abou‐Raya 2014 {published data only}
- Abou-Raya A, Abou-Raya S, Helmii M. Effect of exercise and dietary weight loss on symptoms and systemic inflammation in obese adults with psoriatic arthritis: randomized controlled trial. Annals of the Rheumatic Diseases 2014;73(Suppl 2):89-90. [Google Scholar]
ACTRN12610000049077 {published data only}
- ACTRN12610000049077. The Impact of Weight Loss on the Metabolic Syndrome. http://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12610000049077 (first received 3 December 2009).
Allison 2016 {published data only}
- Allison MA, Aragaki A, Eaton C, Wassertheil-Smoller S, Li W, Van Horn L, et al. Dietary intervention to reduce fat intake does not result in lower incident carotid artery disease: The women's health initiative diet modification trial. Circulation. Conference: American Heart Association 2013;128(22 Suppl. 1):A10374. [EMBASE: 71337690] [Google Scholar]
- Allison MA, Aragaki AK, Ray RM, Margolis KL, Beresford SA, Kuller L, et al. A randomized trial of a low-fat diet intervention on blood pressure and hypertension: tertiary analysis of the WHI Dietary Modification Trial. American Journal of Hypertension 2016;29(8):959-68. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Andersen 1985 {published data only}
- Andersen TR, Nielsen PE. Blood pressure lowering effect of weight reduction. Scandinavian Journal of Clinical and Laboratory Investigation. Supplementum 1985;176:7-14. [PMID: ] [PubMed] [Google Scholar]
Andrews 2011 {published data only}
- Andrews RC, Cooper AR, Montgomery AA, Norcross AJ, Peters TJ, Sharp DJ, et al. Diet or diet plus physical activity versus usual care in patients with newly diagnosed type 2 diabetes: the Early ACTID randomised controlled trial. Lancet 2011;378(9786):129-39. [PMID: ] [DOI] [PubMed] [Google Scholar]
Angelico 2009 {published data only}
- Angelico F, Del Ben M, Pacella A, Carnevale R, Loffredo L, Violi F. Low-fat, low-calorie, Mediterranean-style diet improves endothelial dysfunction in patients with the metabolic syndrome. Journal of Diabetes 2009;1(Suppl 1):A43. [Google Scholar]
Appel 2006 {published data only}
- Appel LJ, Sacks FM, Carey VJ, Conlin PR, Erlinger TP, Miller ER III. The effects of macronutrient intake on blood pressure: Subgroup analyses from the OmniHeart randomized feeding study. Journal of Hypertension 2006;24(Suppl 6):177. [Google Scholar]
Ard 2005 {published data only}
- Ard JD, Svetkey LP. Diet and blood pressure: applying the evidence to clinical practice. American Heart Journal 2005;149(5):804-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ard 2017 {published data only}
- Ard JD, Gower B, Hunter G, Ritchie CS, Roth DL, Goss A, et al. Effects of calorie restriction in obese older adults: the CROSSROADS randomized controlled trial. Journals of Gerontology Series A-Biological Sciences & Medical Sciences 2017;73(1):73-80. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Balas‐Nakash 2014 {published data only}
- Balas-Nakash M, Munoz-Manrique C, Legorreta-Legorreta J, Rodriguez-Cano A, Mier-Cabrera J, Aguilera-Perez JR. Structured hypocaloric diet is more effective than behavioral therapy in reducing metabolic syndrome in Mexican postmenopausal women: a randomized controlled trial. Menopause 2014;21(7):711-20. [PMID: ] [DOI] [PubMed] [Google Scholar]
Banos 2015 {published data only}
- Banos RM, Mensorio MS, Cebolla A, Rodilla E, Palomar G, Lison J, et al. An internet-based self-administered intervention for promoting healthy habits and weight loss in hypertensive people who are overweight or obese: a randomized controlled trial. BMC Cardiovascular Disorders 2015;15:83. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bao 1999 {published data only}
- Bao DQ, Mori TA, Burke V, Puddey IB, Beilin LJ. Dietary fish and weight reduction improves multiple risk factors in overweight, treated hypertensives. [abstract]. Australian and New Zealand Journal of Medicine 1999;29:148. [Google Scholar]
Bartels 1974 {published data only}
- Bartels RW, Bigalke C, Mollmann H, Schneeberger W, Wessels F. Influence of various hunger-cures on the behavior of body weight and blood pressure as well as on relevant blood parameters [Der Einfluss unterschiedlicher Fastenkuren auf das Gewichts- und Blutdruckverhalten sowie auf relevante metabolische Blutparameter]. Die Medizinische Welt 1974;25(17):725-35. [PMID: ] [PubMed] [Google Scholar]
Bazian 2004 {published data only}
- Bazian Ltd. Advice about diet and lifestyle does not reduce blood pressure in people with hypertension. Evidence-Based Healthcare and Public Health 2004;8(6):348-9. [Google Scholar]
Bennett 2018 {published data only}
- Bennett GG, Steinberg D, Askew S, Levine E, Foley P, Batch BC, et al. Effectiveness of an app and provider counseling for obesity treatment in primary care. American Journal of Preventive Medicine 2018;55(6):777-86. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bouchonville 2014 {published data only}
- Bouchonville M, Armamento-Villareal R, Shah K, Napoli N, Sinacore DR, Qualls C, et al. Weight loss, exercise or both and cardiometabolic risk factors in obese older adults: results of a randomized controlled trial. International Journal of Obesity 2014;38(3):423-31. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchonville M, Krupa S, Armamento-Villareal R, Sinacore DR, Qualls C, Villareal DT. Weight loss, exercise, or both and cardiometabolic risk factors in obese older adults: results of a randomized controlled trial. Endocrine Reviews 2012;33(Suppl 3):S18. [DOI: 10.1038/ijo.2013.122] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cakir 2006 {published data only}
- Cakir H, Pinar R. Randomized controlled trial on lifestyle modification in hypertensive patients. Western Journal of Nursing Research 2006;28(2):190-209. [DOI] [PubMed] [Google Scholar]
Cambien 1986 {published data only}
- Cambien F, Plouin PF, Safar M, Pequignot G, Guillanneuf MT, Dutemple C. Comparative study of a medical and a dietary intervention in overweight hypertensive patients [Essai comparant une intervention medicamenteuse et une intervention dietetique chez des patients ayant une hypertension associee a un surpoids]. Archives des Maladies du Coeur et des Vaisseaux 1986;79:1002. [Google Scholar]
Camhi 2010 {published data only}
- Camhi SM, Stefanick ML, Katzmarzyk PT, Young DR. Metabolic syndrome and changes in body fat from a low-fat diet and/or exercise randomized controlled trial. Obesity 2010;18(3):548-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2009 {published data only}
- Chen L, Appel LJ, Loria C, Lin PH, Champagne CM, Elmer PJ, et al. Reduction in consumption of sugar-sweetened beverages is associated with weight loss: the PREMIER trial. American Journal of Clinical Nutrition 2009;89(5):1299-306. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Childress 2008 {published data only}
- Childress S, Brubaker PH, Amico LA, Nesbit BA, Williams CM, Jack Rejeski W. Patterns of physical activity before and after an exercise intervention in overweight/obese older adults with CVD or the metabolic syndrome. Journal of Cardiopulmonary Rehabilitation and Prevention 2008;28(4):268. [Google Scholar]
Chirinos 2016 {published data only}
- Chirinos DA, Goldberg RB, Llabre MM, Gellman M, Gutt M, McCalla J, et al. Lifestyle modification and weight reduction among low-income patients with the metabolic syndrome: the CHARMS randomized controlled trial. Journal of Behavioral Medicine 2016;39(3):483-92. [EMBASE: 614987996] [DOI] [PubMed] [Google Scholar]
Christensen 2013 {published data only}
- Christensen P, Frederiksen R, Bliddal H, Riecke BF, Bartels EM, Henriksen M, et al. Comparison of three weight maintenance programs on cardiovascular risk, bone and vitamins in sedentary older adults. Obesity 2013;21(10):1982-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
Coppell 2010 {published data only}
- Coppell KJ, Kataoka M, Williams SM, Chisholm AW, Vorgers SM, Mann JI. Nutritional intervention in patients with type 2 diabetes who are hyperglycaemic despite optimised drug treatment - Lifestyle Over and Above Drugs in Diabetes (LOADD) study: randomised controlled trial. BMJ 2010;341:c3337. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Curzio 1989 {published data only}
- Curzio JL, Kennedy SS, Elliott HL, Farish E, Barnes JF, Howie CA, et al. Hypercholesterolaemia in treated hypertensives: a controlled trial of intensive dietary advice. Journal of Hypertension. Supplement: Official Journal of the International Society of Hypertension 1989;7(6):S254-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cutler 1997 {published data only}
- Cutler JA, Stamler J. Chapter 1. Introduction and summary of the dietary and nutritional methods and findings in the Multiple Risk Factor Intervention Trial. American Journal of Clinical Nutrition 1997;65(1 Suppl):184S-90S. [DOI] [PubMed] [Google Scholar]
De Mello 2008 {published data only}
- De Mello VD, Kolehmainen M, Pulkkinen L, Schwab U, Mager U, Laaksonen DE, et al. Downregulation of genes involved in NFB activation in peripheral blood mononuclear cells after weight loss is associated with the improvement of insulin sensitivity in individuals with the metabolic syndrome: The GENOBIN study. Diabetologia 2008;51(11):2060-7. [DOI] [PubMed] [Google Scholar]
Diaz 2014 {published data only}
- Diaz KM, Muntner P, Levitan EB, Brown MD, Babbitt DM, Shimbo D. The effects of weight loss and salt reduction on visit-to-visit blood pressure variability: results from a multicenter randomized controlled trial. Journal of Hypertension 2014;32(4):840-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Di Mauro 1998 {published data only}
- Di Mauro S, Spallina G, Leotta C, Giardina M, Di Fazio I, Malaguarnera M, et al. The effects of caloric restriction and controlled physical exercise on hypertension in the elderly. Archives of Gerontology and Geriatrics 1998;27(1):1-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ebell 2013 {published data only}
- Ebell MH. Intensive lifestyle intervention fails to improve patient-oriented outcomes in persons with obesity and diabetes. American Family Physician 2013;88(12):864A. [Google Scholar]
Fagerberg 1989 {published data only}
- Fagerberg B, Berglund A, Berglund G, Wikstrand J, Andersson OK. Food and health. Weight reduction and decreased sodium chloride intake depress blood pressure but not as much as drugs do [kost och halsa. Viktreduktion och minskat koksaltintag sanker blodtrycket mindre an lakemedel]. Lakartidningen 1989;86(51):4522-4. [PMID: ] [PubMed] [Google Scholar]
Gilliam 2012 {published data only}
- Gilliam ML. Long-term effects of weight-reducing diets in hypertensive patients. Obstetrics and Gynecology 2012;119(1):180-1. [Google Scholar]
Gillum 1983 {published data only}
- Gillum RF, Prineas RJ, Jeffery RW, Jacobs DR, Elmer PJ, Gomez O, et al. Nonpharmacologic therapy of hypertension: the independent effects of weight reduction and sodium restriction in overweight borderline hypertensive patients. American Heart Journal 1983;105(1):128-33. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hall 2003 {published data only}
- Hall WD, Feng Z, George VA, Lewis CE, Oberman A, Huber M, et al. Low-fat diet: effect on anthropometrics, blood pressure, glucose, and insulin in older women. Ethnicity & Disease 2003;13(3):337-43. [PMID: ] [PubMed] [Google Scholar]
Han 2017 {published data only}
- Han L, Zhang T, Sun D, Ma W, Wang T, Heianza Y, et al. Temporal relationship between changes in body weight and insulin resistance and its impact on blood pressure in response to 2-year weight-loss diet interventions: The pounds lost trial. Circulation. Conference: American Heart Association's Epidemiology and Prevention/Lifestyle and Cardiometabolic Health 2017;135(Suppl 1):P181. [EMBASE: 618428814] [Google Scholar]
Haynes 1984 {published data only}
- Haynes RB, Harper AC, Costley SR, Johnston M, Logan AG, Flanagan PT, et al. Failure of weight reduction to reduce mildly elevated blood pressure: a randomized trial. Journal of Hypertension 1984;2(5):535-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hayward 2010 {published data only}
- Hayward CS, Lockwood J, Williams CD, Cole RE, Torres DM, Harrison SA. Lifestyle modification and NAFLD: A prospective, randomized trial. Hepatology 2010;52:622A. [Google Scholar]
He 2000 {published data only}
- He J, Whelton PK, Appel LJ, Charleston J, Klag MJ. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension 2000;35(2):544-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Heinberg 2000 {published data only}
- Heinberg LJ, Haythornthwaite JA, Rosofsky W, McCarron P, Clarke A. Body image and weight loss maintenance in elderly African American hypertensives. American Journal of Health Behavior 2000;24(3):163-73. [1640739] [Google Scholar]
Heshka 2003 {published data only}
- Heshka S, Anderson J, Atkinson R, Gadde KM, Nanchahal K. Commercial weight reduction programme reduces weight more than self-help materials. Evidence-Based Healthcare 2003;7(4):179-81. [Google Scholar]
Heyden 1974 {published data only}
- Heyden S, Hames CG. Diet therapy of elevated blood pressure values in overweight persons. Hypertension-intervention study: 1 year's report from the Evans-County (Ga.) study [Diätbehandlung erhöhter blutdruckwerte bei übergewichtigen personen. Hypertonie-Interventionsstudie: 1-jahres-bericht aus der Evans-County (Ga.)-studie]. Die Medizinische Welt 1974;25(49):2041-3. [PMID: ] [PubMed] [Google Scholar]
Hsieh 2009 {published data only}
- Hsieh YC, Hung CT, Lien LM, Bai CH, Chen WH, Yeh CY, et al. A significant decrease in blood pressure through a family-based nutrition health education programme among community residents in Taiwan. Public Health Nutrition 2009;12(4):570-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hua 2017 {published data only}
- Hua K, Hao G, Li W. Cardiovascular outcomes of lifestyle intervention in hypertensive patients with antihypertensive agents. International Journal of Cardiology 2017;227:751-56. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hyden 1973 {published data only}
- Hyden S, Tyroler HA, Hames CG, Bartel A, Thompson JW, Krishan I, et al. Diet treatment of obese hypertensives. Clinical Science and Molecular Medicine. Supplement 1973;45 Suppl 1:209s-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
IRCT2015062422905N1 {published data only}
- IRCT2015062422905N1. Effects of low-calorie balanced diet containing wholegrain bread and wholegrain rice on indicators of metabolic syndrome in obese and overweight patients. en.irct.ir/trial/19659 (first received 25 September 2016).
Jones 1999 {published data only}
- Jones DW, Miller ME, Wofford MR, Anderson DC Jr, Cameron ME, Willoughby DL, et al. The effect of weight loss intervention on antihypertensive medication requirements in the Hypertension Optimal Treatment (HOT) study. American Journal of Hypertension 1999;12(12 Pt 1-2):1175-80. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kanke 2015 {published data only}
- Kanke S, Kawai T, Takasawa N, Mashiyama Y, Ishii A, Kassai R. Interventions for body weight reduction in obese patients during short consultations: an open-label randomized controlled trial in the Japanese primary care setting. Asia Pacific Family Medicine 2015;14(1):5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Karoff 1985 {published data only}
- Karoff C, Zidek W, Lange-Asschenfeldt H, Losse H, Vetter H. Blood pressure and intracellular electrolytes during weight reduction. Klinische Wochenschrift 1985;63 Suppl 3:129-31. [PMID: ] [PubMed] [Google Scholar]
Karvetti 1992 {published data only}
- Karvetti RL, Hakala P. A seven-year follow-up of a weight reduction programme in Finnish primary health care. European Journal of Clinical Nutrition 1992;46(10):743-52. [PMID: ] [PubMed] [Google Scholar]
Katzel 1995 {published data only}
- Katzel LI, Bleecker ER, Colman EG, Rogus EM, Sorkin JD, Goldberg AP. Effects of weight loss vs aerobic exercise training on risk factors for coronary disease in healthy, obese, middle-aged and older men. A randomized controlled trial. JAMA 1995;274(24):1915-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kawamura 1993 {published data only}
- Kawamura M, Akasaka T, Kasatsuki T, Nakajima J, Onodera S, Fujiwara T, et al. Blood pressure is reduced by short-time calorie restriction in overweight hypertensive women with a constant intake of sodium and potassium. Journal of Hypertension. Supplement: Official Journal of the International Society of Hypertension 1993;11(5):S320-1. [PMID: ] [PubMed] [Google Scholar]
Kittiskulnam 2014 {published data only}
- Kittiskulnam P, Kanjanabuch T, Tangmanjitjaroen K, Chancharoenthana W, Praditpornsilpa K, Eiam-Ong S. The beneficial effects of weight reduction in overweight patients with chronic proteinuric immunoglobulin a nephropathy: a randomized controlled trial. Journal of Renal Nutrition 2014;24(3):200-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kolehmainen 2008 {published data only}
- Kolehmainen M, Salopuro T, Schwab US, Kekalainen J, Kallio P, Laaksonen DE, et al. Weight reduction modulates expression of genes involved in extracellular matrix and cell death: the GENOBIN study. International Journal of Obesity 2008;32(2):292-303. [DOI] [PubMed] [Google Scholar]
Koopman 1990 {published data only}
- Koopman H, Spreeuwenberg C, Westerman RF, Donker AJ. Dietary treatment of patients with mild to moderate hypertension in a general practice: a pilot intervention study (1). The first three months. Journal of Human Hypertension 1990;4(4):368-71. [PMID: ] [PubMed] [Google Scholar]
- Koopman H, Spreeuwenberg C, Westerman RF, Donker AJ. Dietary treatment of patients with mild to moderate hypertension in a general practice: a pilot intervention study (2). Beyond three months. Journal of Human Hypertension 1990;4(4):372-74. [PMID: ] [PubMed] [Google Scholar]
Korhonen 2003 {published data only}
- Korhonen M, Kastarinen M, Uusitupa M, Stevens VJ, Worsley A. Advice from primary care physicians and nurses may improve diet in people with hypertension. Evidence-based Cardiovascular Medicine 2003;7:94-6. [Google Scholar]
Larson‐Meyer 2010 {published data only}
- Larson-Meyer DE, Redman L, Heilbronn LK, Martin CK, Ravussin E. Caloric restriction with or without exercise: the fitness versus fatness debate. Medicine and Science in Sports and Exercise 2010;42(1):152-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lindgarde 2001 {published data only}
- Lindgarde F. Orlistat with diet was effective and safe for weight loss and coronary risk reduction in obesity. Evidence-based Medicine 2001;6(2):54. [Google Scholar]
Mason 2013 {published data only}
- Mason C, Foster-Schubert KE, Imayama I, Xiao L, Kong A, Campbell KL, et al. History of weight cycling does not impede future weight loss or metabolic improvements in postmenopausal women. Metabolism: Clinical and Experimental 2013;62(1):127-36. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Masuo 2012 {published data only}
- Masuo K, Rakugi H, Ogihara T, Lambert G. Effects of weight loss on liver function in obese hypertensive patients. Journal of Hypertension 2012;30:e53-4. [Google Scholar]
- Masuo K, Rakugi H, Ogihara T, Lambert GW. Different mechanisms in weight loss-induced blood pressure reduction between a calorie-restricted diet and exercise. Hypertension Research - Clinical & Experimental 2012;35(1):41-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Masuo K, Rakugi H, Ogihara T, Lambert GW. The effects of weight loss on liver function in obese hypertensive patients. Circulation 2012;125(Suppl 1):P131. [Google Scholar]
McCarron 2000 {published data only}
- McCarron DA, Reusser ME. Cardiovascular risk reduction dietary intervention trial. Drug Benefit Trends 2000;12(5):42-8. [Google Scholar]
Melchart 2015 {published data only}
- Melchart D, Doerfler W, Eustachi A, Wellenhofer-Li Y, Weidenhammer W. The talent study: a multicentre randomized controlled trial assessing the impact of a 'tailored lifestyle self-management intervention' (talent) on weight reduction. BMC Obesity 2015;2:38. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Metz 2000 {published data only}
- Metz JA, Stern JS, Kris-Etherton P, Reusser ME, Morris CD, Hatton DC, et al. A randomized trial of improved weight loss with a prepared meal plan in overweight and obese patients: impact on cardiovascular risk reduction. Archives of Internal Medicine 2000;160(14):2150-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Moore 2013 {published data only}
- Moore RH, Diewald LK, Wadden TA, Sarwer DB, Berkowitz RI, Chittams J, et al. The impact of a primary care-based weight loss intervention on the quality of life. International Journal of Obesity 2013;37(Suppl. 1):S25-S30. [EMBASE: 369605264] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT00142649 {published data only}
- NCT00142649. Adherence to weight loss for hypertension in African American women. www.clinicaltrials.gov/ct2/show/nct00142649 (first received 2 September 2005).
NCT00661817 {published data only}
- NCT00661817. Integrated weight loss technologies for weight and blood pressure control in urban clinics. clinicaltrials.gov/ct2/show/nct00661817 (first received: 18 April 2008).
NCT00783315 {published data only}
- NCT00783315. Practice-based opportunities for weight reduction trial at Johns Hopkins. clinicaltrials.gov/ct2/show/nct00783315 (first received: 31 October 2008).
NCT01724645 {published data only}
- NCT01724645. Randomized, open label, parallel controlled trial, to evaluate the beneficial effects of Korean traditional diets in subjects with hypertension and type 2 diabetes. clinicaltrials.gov/ct2/show/nct01724645 (first received: 12 November 2012).
NCT02136264 {published data only}
- NCT02136264. Randomized controlled trial of a personalized dietary intervention approach for the control of essential hypertension. clinicaltrials.gov/ct2/show/nct02136264 (first received: 12 May 2014).
NCT02445833 {published data only}
- NCT02445833. Design, development and validation of an on-line intervention for promoting healthy habits and weight loss in hypertensive and risk for diabetes mellitus people with overweight and type I obesity. clinicaltrials.gov/ct2/show/nct02445833 (first received: 15 May 2015).
NCT02454127 {published data only}
- NCT02454127. Effectiveness of four dietary treatment strategies for metabolic syndrome: a prospective randomized trial. clinicaltrials.gov/ct2/show/nct02454127 (first received: 27 May 2015).
NCT03288142 {published data only}
- NCT03288142. Improving hypertension using a smartphone-enabled personal control program: the smart hypertension control study. clinicaltrials.gov/ct2/show/nct03288142 (first received: 19 September 2017).
Neuhouser 2012 {published data only}
- Neuhouser ML, Howard B, Lu J, Tinker LF, Van Horn L, Caan B, et al. A low-fat dietary pattern and risk of metabolic syndrome in postmenopausal women: the Women's Health Initiative. Metabolism: Clinical & Experimental 2012;61(11):1572-81. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Noble 1971 {published data only}
- Noble RE. A controlled study of a weight reduction regimen. Current Therapeutic Research, Clinical and Experimental 1971;13(11):685-91. [PMID: ] [PubMed] [Google Scholar]
Oshakbayev 2016 {published data only}
- Oshakbayev KP, Seidaliyeva AP, Togizbayeva GI, Gazaliyeva MA, Durmanova AK, Idrisov AS, et al. Clinical management with weight loss therapy in patients with type 2 diabetes: a randomised clinical trial. Diabetic Medicine 2016;1:32. [EMBASE: 72230636] [Google Scholar]
Poppitt 2002 {published data only}
- Poppitt SD, Keogh GF, Prentice AM, Williams DE, Sonnemans HM, Valk EE, et al. Long-term effects of ad libitum low-fat, high-carbohydrate diets on body weight and serum lipids in overweight subjects with metabolic syndrome. American Journal of Clinical Nutrition 2002;75(1):11-20. [PMID: ] [DOI] [PubMed] [Google Scholar]
Prentice 2017 {published data only}
- Prentice RL, Aragaki AK, Van Horn L, Thomson CA, Beresford SA, Robinson J, et al. Low-fat dietary pattern and cardiovascular disease: results from the Women's Health Initiative randomized controlled trial. American Journal of Clinical Nutrition 2017;106(1):35-43. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pritchard 2002 {published data only}
- Pritchard JE, Nowson CA, Billington T, Wark JD. Benefits of a year-long workplace weight loss program on cardiovascular risk factors. Nutrition and Dietetics 2002;59:87-96. [Google Scholar]
Reisin 1978 {published data only}
- Reisin E, Abel R, Modan M, Silverberg DS, Eliahou HE, Modan B. Effect of weight loss without salt restriction on the reduction of blood pressure in overweight hypertensive patients. New England Journal of Medicine 1978;298(1):1-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rissanen 1985 {published data only}
- Rissanen A, Pietinen P, Siljamaki-Ojansuu U, Piirainen H, Reissel P. Treatment of hypertension in obese patients: efficacy and feasibility of weight and salt reduction programs. Acta Medica Scandinavica 1985;218(2):149-56. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rosas 2015 {published data only}
- Rosas LG, Thiyagarajan S, Goldstein BA, Drieling RL, Romero PP, Ma J, et al. The effectiveness of two community-based weight loss strategies among obese, low-income US Latinos. Journal of the Academy of Nutrition & Dietetics 2015;115(4):537-50.e2. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Salas‐Salvado 2008 {published data only}
- Salas-Salvado J, Fernandez-Ballart J, Ros E, Martinez-Gonzalez MA, Fito M, Estruch R, et al. Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: One-year results of the PREDIMED randomized trial. Archives of Internal Medicine 2008;168(22):2449-58. [DOI] [PubMed] [Google Scholar]
Salinardi 2012 {published data only}
- Salinardi TC, Batra P, Roberts SB, Urban LE, Robinson LM, Pittas AG, et al. A lifestyle intervention reduces body weight and improves cardiometabolic risk factors in worksites. Circulation 2012;126(21 Suppl):A13112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Samaha 2003 {published data only}
- Samaha FF, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J, et al. A low-carbohydrate as compared with a low-fat diet in severe obesity. New England Journal of Medicine 2003;348(21):2074-81. [DOI] [PubMed] [Google Scholar]
Schwab 2008 {published data only}
- Schwab U, Seppanen-Laakso T, Yetukuri L, Agren J, Kolehmainen M, Laaksonen DE, et al. Triacylglycerol fatty acid composition in diet-induced weight loss in subjects with abnormal glucose metabolism - The GENOBIN study. PLoS ONE 2008;3(7):e2630. [DOI] [PMC free article] [PubMed]
Sedjo 2016 {published data only}
- Sedjo RL, Flatt SW, Byers T, Colditz GA, Demark-Wahnefried W, Ganz PA, et al. Impact of a behavioral weight loss intervention on comorbidities in overweight and obese breast cancer survivors. Supportive Care in Cancer 2016;24(8):3285-93. [EMBASE: 608873176] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stamler 1985 {published data only}
- Stamler R, Stamler J, Grimm R, Gosch FC, Dyer A. Control of hypertension by regulating nutrition. The 4-year results [Issledovanie po kontroliu gipertonii s pomoshch'iu regulirovaniia pitaniia. Rezul'taty za 4 goda.]. Terapevticheskii Arkhiv 1985;57(11):71-6. [PMID: ] [PubMed] [Google Scholar]
Tate 2011 {published data only}
- Tate DF, Turner-McGrievy G, Lyons E, Stevens J, Erickson K, Polzien K, et al. Replacing caloric beverages with water or diet beverages for weight loss in adults: main results of the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. American Journal of Clinical Nutrition 2012;95(3):555-63. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate DF, Turner-McGrievy G, Stevens J, Erickson K, Polzien K, Diamond M, et al. Replacing caloric beverages with water or diet beverages for weight loss in adults: results of a 6-month randomized controlled trial. Obesity 2011;19(Suppl 1):S68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Trepanowski 2014 {published data only}
- Trepanowski J, Kroeger C, Klempel M, Calvo Y, Varady K. Alternate day fasting versus daily calorie restriction for weight loss and cardio-protection. The FASEB Journal 2014;28(1 Suppl):120.6. [Google Scholar]
Tunyan 2007 {published data only}
- Tunyan AM. Cardioprotective effects of antihypertensive therapy with orlistat treatment and hypocaloric diet in combination in obese hypertensive patients. Circulation 2007;115(8):e248. [Google Scholar]
Tuomilehto 2009 {published data only}
- Tuomilehto HP, Seppa JM, Partinen MM, Peltonen M, Gylling H, Tuomilehto JO, et al. Lifestyle intervention with weight reduction: first-line treatment in mild obstructive sleep apnea. American Journal of Respiratory and Critical Care Medicine 2009;179(4):320-7. [DOI] [PubMed] [Google Scholar]
Ueki 2016 {published data only}
- Ueki K, Sasako T, Kato M, Okazaki Y, Okahata S, Katsuyama H, et al. Design of and rationale for the Japan Diabetes Optimal Integrated Treatment study for 3 major risk factors of cardiovascular diseases (J-DOIT3): a multicenter, open-label, randomized, parallel-group trial. BMJ Open Diabetes Research & Care 2016;4(1):e000123. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
UMIN000002967 {published data only}
- UMIN000002967. Effect of body weight measuring and advice by family doctors on body weight reduction for obese patients: a randomized controlled trial in a Japanese family practice. upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000003600 (first received: 13 December 2011).
UMIN000006582 {published data only}
- UMIN000006582. Lifestyle changes by delivery meals with dietitians: STYLIST Study. upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000007739 (first received: 22 October 2011).
UMIN000029395 {published data only}
- UMIN000029395. Investigation of effect on blood pressure and weight improvement by blood pressure measurement and dietary intervention. upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000033485 (first received: 3 October 2017).
Vissers 2010 {published data only}
- Vissers D, Verrijken A, Mertens I, Van Gils C, Van De Sompel A, Truijen S, et al. Effect of long-term whole body vibration training on visceral adipose tissue: a preliminary report. Obesity Facts 2010;3(2):93-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weil 2016 {published data only}
- Weil R, Kovacs B, Miller N, McDermott MP, Wall M, Kupersmith M, et al. A 6-month telephone-based weight loss intervention in overweight and obese subjects with idiopathic intracranial hypertension. Obesity Science & Practice 2016;2(2):95-103. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Weiss 2016 {published data only}
- Weiss EP, Albert SG, Reeds DN, Kress KS, McDaniel JL, Klein S, et al. Effects of matched weight loss from calorie restriction, exercise, or both on cardiovascular disease risk factors: a randomized intervention trial. American Journal of Clinical Nutrition 2016;104(3):576-86. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO Europ.Coll.Grp. 1974 {published data only}
- World Health Organization European Collaborative Group. An international controlled trial in the multifactorial prevention of coronary heart disease. International Journal of Epidemiology 1974;3(3):219-24. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wright 2017 {published data only}
- Wright N, Wilson L, Smith M, Duncan B, McHugh P. The BROAD study: a randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Nutrition & Diabetes 2017;7(3):e256. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yamada 2013 {published data only}
- Yamada S, Yamada Y, Irie J. A non-calorie-restricted non-ketogenic low-carbohydrate diet is effective as an alternative therapy for patients with type 2 diabetes. Diabetes 2013;62:A192-3. [DOI] [PubMed] [Google Scholar]
Zotova 2015 {published data only}
- Zotova AV, Desyatova IE, Bychenko SM, Sivertseva SA, Okonechnikova NS, Murav'ev SA. The efficacy of low calorie diet therapy in patients with arterial hypertension and chronic cerebral ischemia. Zhurnal Nevrologii i Psikhiatrii Imeni S.S. Korsakova 2015;115(10):25-28. [PMID: ] [DOI] [PubMed] [Google Scholar]
Additional references
ACC‐AHA 2017
- Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71(6):e13-115. [PMID: ] [DOI] [PubMed] [Google Scholar]
Akonobi 2019
- Akonobi A, Khan J. A systematic review of randomized controlled trials about some non-pharmacological interventions for treatment of hypertension: physical exercise, sodium restriction, weight and alcohol use reduction. Journal of Health and Social Sciences 2019;4(1):17-42. [Google Scholar]
Anderssen 1995
- Anderssen S, Holme I, Urdal P, Hjermann I. Diet and exercise intervention have favourable effects on blood pressure in mild hypertensives: the Oslo Diet and Exercise Study (ODES). Blood Pressure 1995;4(6):343-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Aucott 2005
- Aucott L, Poobalan A, Smith WC, Avenell A, Jung R, Broom J. Effects of weight loss in overweight/obese individuals and long-term hypertension outcomes: a systematic review. Hypertension 2005;45(6):1035-41. [PMID: ] [DOI] [PubMed] [Google Scholar]
Brunström 2018
- Brunström M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Internal Medicine 2018;178(1):28-36. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2019
- Deeks JJ, Higgins JP, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Dickinson 2006
- Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. Journal of Hypertension 2006;24(2):215-33. [PMID: ] [DOI] [PubMed] [Google Scholar]
ESH‐ESC 2018
- Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal 2018;39(33):3021-104. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ettehad 2016
- Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387(10022):957-67. [PMID: ] [DOI] [PubMed] [Google Scholar]
Forouzanfar 2017
- Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA 2017;317(2):165-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gay 2016
- Gay HC, Rao SG, Vaccarino V, Ali MK. Effects of different dietary interventions on blood pressure: Systematic review and meta-analysis of randomized controlled trials. Hypertension 2016;67(4):733-39. [EMBASE: 608644392] [DOI] [PubMed] [Google Scholar]
GBD 2017
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392(10159):1923-94. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383-94. [PMID: ] [DOI] [PubMed] [Google Scholar]
Haynes 2010 [pers comm]
- Haynes B. RE: Cochrane Review [personal communication]. Email to: A Siebenhofer. 10 December 2010.
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2019
- Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JAC. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Horvath 2008
- Horvath K, Jeitler K, Siering U, Stich AK, Skipka G, Gratzer TW, et al. Long-term effects of weight-reducing interventions in hypertensive patients: systematic review and meta-analysis. Archives of Internal Medicine 2008;168(6):571-80. [PMID: ] [DOI] [PubMed] [Google Scholar]
Howard 2006
- Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller S, et al. Low-fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 2006;295(6):655-66. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hypertension Canada 2018
- Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, et al. Hypertension Canada's 2018 Guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Canadian Journal of Cardiology 2018;34(5):506-25. [PMID: ] [DOI] [PubMed] [Google Scholar]
IQWiG 2006
- Institute for Quality and Efficiency in Health Care (IQWiG). IQWiG Reports - Commission No. A05-21A: Benefit assessment of non-drug treatment strategies in patients with hypertension: weight reduction [Abschlussbericht A05/21-A: Nutzenbewertung nichtmedikamentöser Behandlungsstrategien bei Patienten mit Bluthochdruck: A-Gewichtsreduktion]. iqwig.de/download/A05-21A_Abschlussbericht_Gewichtsreduktion_bei_Bluthochdruck_neu.pdf 2006.
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Lelong 2019
- Lelong H, Blacher J, Baudry J, Adriouch S, Galan P, Fezeu L, et al. Combination of healthy lifestyle factors on the risk of hypertension in a large cohort of French adults. Nutrients 2019;11(7):1687. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Metha 2016
- Mehta AK, Doshi RS, Chaudhry ZW, Jacobs DK, Vakil RM, Lee CJ, et al. Benefits of commercial weight-loss programs on blood pressure and lipids: a systematic review. Preventive Medicine 2016;90:86-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Musini 2009
- Musini VM, Wright JM. Factors affecting blood pressure variability: lessons learned from two systematic reviews of randomized controlled trials. PLoS ONE 2009;4(5):Article Number: e5673. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nguyen 2019
- Nguyen B, Bauman A, Ding D. Association between lifestyle risk factors and incident hypertension among middle-aged and older Australians. Preventive Medicine 2019;118:73-80. [PMID: ] [DOI] [PubMed] [Google Scholar]
NICE 2019
- National Institute for Health and Care Excellence (NICE). Hypertension in adults: diagnosis and management. www.nice.org.uk/guidance/ng136 2019 (last accessed 3 April 2020).
PRISMA 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine 2009;151(4):264-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Review Manager 5 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan). Version Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Siebenhofer 2016
- Siebenhofer A, Jeitler K, Horvath K, Berghold A, Posch N, Meschik J, et al. Long-term effects of weight-reducing drugs in people with hypertension. Cochrane Database of Systematic Reviews 2016, Issue 3. Art. No: CD007654. [DOI: 10.1002/14651858.CD007654.pub4] [DOI] [PubMed] [Google Scholar]
Sjöström 2004
- Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. New England Journal of Medicine 2004;351(26):2683-93. [PMID: ] [DOI] [PubMed] [Google Scholar]
Stelmach‐Mardas 2016
- Stelmach-Mardas M, Walkowiak J. Dietary interventions and changes in cardio-metabolic parameters in metabolically healthy obese subjects: a systematic review with meta-analysis. Nutrients 2016;8(8):455. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomopoulos 2014
- Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. Journal of Hypertension 2014;32(12):2285-95. [PMID: ] [DOI] [PubMed] [Google Scholar]
Urdal 1993
- Urdal P, Haaland A, Hjermann I, Gjesdal K, Christian C, Sorensen M, et al. The Oslo Diet and Exercise Study (ODES): Design and objectives. Controlled Clinical Trials 1993;14(3):229-43. [DOI] [PubMed] [Google Scholar]
WHO 2020
- World Health Organization (WHO). Fact Sheets: overweight and obesity. www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed 2 April 2020).
Zhao 2017
- Zhao Y, Zhang M, Luo X, Wang C, Li L, Zhang L, et al. Association of 6-year waist circumference gain and incident hypertension. Heart 2017;103(17):1347-52. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Semlitsch 2016
- Semlitsch T, Jeitler K, Berghold A, Horvath K, Posch N, Poggenburg S, et al. Long-term effects of weight-reducing diets in people with hypertension. Cochrane Database of Systematic Reviews 2016, Issue 3. Art. No: CD008274. [DOI: 10.1002/14651858.CD008274.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Siebenhofer 2010
- Siebenhofer A, Jeitler L, Berghold A, Hemkens LG, Waltering A, Horvath K. Long‐term effects of weight‐reducing diets in hypertensive patients. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD008274. [DOI: 10.1002/14651858.CD008274] [DOI] [PubMed] [Google Scholar]
Siebenhofer 2011
- Siebenhofer A, Jeitler K, Berghold A, Waltering A, Hemkens LG, Semlitsch T, et al. Long-term effects of weight-reducing diets in hypertensive patients. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No: CD008274. [DOI: 10.1002/14651858.CD008274.pub2] [DOI] [PubMed] [Google Scholar]