Abstract
Cardiorespiratory fitness (CRF) is now an established vital sign. CRF, along with muscle function and bone and joint health is related to functional independence and a higher quality of life. Wasserman and colleagues proposed a gear model illustrating the integrated role of the respiratory, cardiovascular, and skeletal muscle systems during aerobic exercise; in 2015, a revision to the original model was proposed. Our understanding of the effects and challenges associated with the coronavirus disease 2019 (COVID-19) are rapidly evolving. Initial evidence indicates higher levels of CRF, and muscle function protect individuals infected with COVID-19 from a complicated medical course. Moreover, for those individuals infected with COVID-19, there are initial signs of a reduction in CRF following the initial phase of recovery. We are also gaining an understanding of long COVID syndrome, where individuals who have recovered from the acute phase of viral infection present with lasting symptoms, which include but are not limited to reduced CRF, shortness of breath, and fatigue. Clearly, these individuals will require rehabilitation to restore and/or improve CRF, muscle function, bone and joint health, functional capacity (ie, the ability to perform activities of daily living), and quality of life. The importance of assessing the synergistic function of systems essential to performing activities that require physical exertion is a health care imperative. This graphical narrative provides an update to the gear model initially proposed by Wasserman and updated to a gear and circuit in 2015. External CRF, muscle function, and bone and joint health influencers and an approach to clinical assessment are also introduced.
Introduction
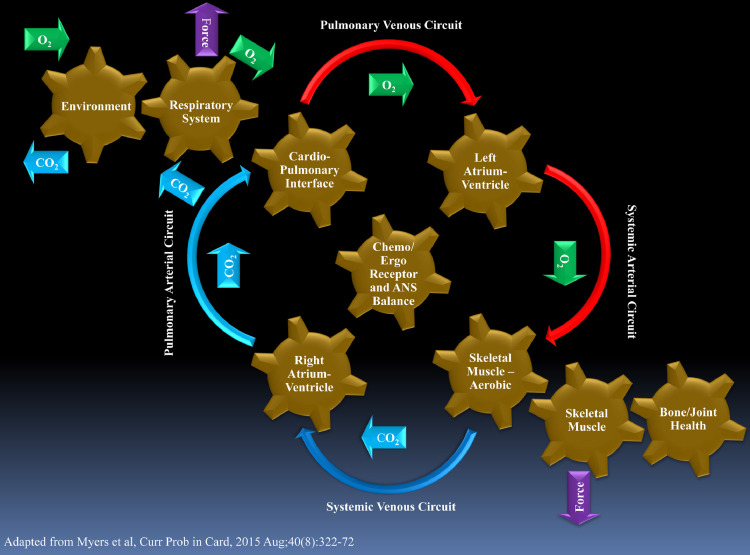
The importance of cardiorespiratory fitness (CRF), now recognized as a vital sign, muscle function, and bone and joint health to functional independence, quality of life and health trajectory are established – the evidence supporting these assertions spans decades and are beyond dispute.1, 2, 3 Wasserman and colleagues initially proposed a gear model that illustrated the integrated role of the respiratory, cardiovascular, and skeletal muscle systems during aerobic exercise.4 Normal, synergistic function of the respiratory, cardiovascular, and skeletal muscle systems are required for an appropriate response to a bout of aerobic exercise. Dysfunction in one or more of these systems leads to decreased CRF and functional capacity. In 2015, Myers et al.5 proposed a revision to the CRF-centric Wasserman gear model, adding arterial, and venous circuits to distinguish between right and left sided cardiac function and recognizing the role of chemo and/or egro receptors and autonomic nervous system balance. This revised model provided greater detail to the systems involved in oxygen consumption (O2) and carbon dioxide production (CO2) elimination, creating an opportunity to conceptualize physiologic dysfunction and determine the mechanisms for diminished CRF with enhanced precision.
Our understanding of the effects of the novel coronavirus disease 2019 (COVID-19) is rapidly evolving. From a global population standpoint, physical activity (PA) patterns are declining because of social distancing, remote working, and other local and/or state and/or federal restrictions put in place to reduce viral transmission.6, 7, 8, 9 These changes in PA may have lasting detrimental impacts on population CRF, leading to a further increase in risk for a multitude of poor health outcomes, posing global challenges for health care providers and policymakers. There are also concerns over the impact COVID-19 will have on muscle function and bone and joint health.10 , 11 Initial evidence indicates higher levels of CRF and muscle force production, as well as a physically active lifestyle, protect individuals infected with COVID-19 from more severe symptoms and a complicated medical course (eg, intensive care unit admission, mechanical ventilation, and mortality).12, 13, 14, 15 Moreover, for those individuals infected with COVID-19, there are initial signs of a reduction in CRF during the initial stages of recovery.16 We are also rapidly gaining an understanding of long COVID syndrome, where individuals who have recovered from the acute phase of viral infection continue to have lasting symptoms; exertional dyspnea, fatigue and reduced CRF and functional capacity are common characteristics of long COVID syndrome.17, 18, 19, 20 Clearly these individuals will require specialist and multidisciplinary rehabilitation to improve CRF, muscle function, functional capacity and quality of life.21 , 22 Consistent with the pre-COVID-19 pandemic era, the importance of assessing the synergistic function of systems essential to performing activities that require physical exertion, and prescribing interventions that target physiologic dysfunction in one or more systems when identified, is a health care priority. This graphical commentary provides an update to the gear and circuit model proposed by Myers et al.5 in 2015. External CRF and muscle influencers, as well as an approach to clinical assessment, are also introduced.
A Revised Gear and Circuit Model
Systems Involved in Oxygen Consumption, Carbon Dioxide Production, and Muscle Force Production
Figure 1 illustrates the systems involved in O2, CO2, and muscle force production. This illustration has been adapted from the model proposed by Myers et al.5 Primary modifications include: (1) The addition of gears for skeletal muscle and bone and joint health; and (2) Arrows to indicate force generation by the respiratory and skeletal muscle systems. Force generation varies in magnitude and duration, ideally meeting the need for a given bout of PA. An inability to generate and sustain the force needed for activities requiring physical exertion by the respiratory or skeletal muscle systems results in functional limitations. Bone and/or joint health is an indicator of both bone density and joint integrity, both of which can influence skeletal muscle force generation, which in turn impacts bone modelling and turnover, and its ability to provide mechanical integrity for locomotion and protection. Moreover, in addition to the importance of skeletal muscle force generation to perform anaerobic activities, the capacity for the respiratory and skeletal muscle systems to generate force at lower levels, repetitively, influences the capacity to perform aerobic activities and thus CRF. With these additions, Figure 1 provides a comprehensive illustration of all systems involved in performing tasks and/or activities that require physical exertion, from both an aerobic and anaerobic perspective. This model can be used by health care professionals in assessing these systems for potential dysfunction and subsequently guiding clinical decision making, which will be discussed in subsequent sections.
FIG 1.
Systems involved in oxygen consumption, carbon dioxide production and muscle force production. ANS, autonomic nervous system; CO2, carbon dioxide; O2, oxygen Adapted from: Myers J, Arena R, Cahalin LP, Labate V, and Guazzi M. Cardiopulmonary Exercise Testing in Heart Failure. Current problems in cardiology. 2015;40:322-372.
Numerous approaches exist to assess CRF, muscle function, and bone and joint health; the approach that is utilized is dependent upon resources and the expertise of personnel available. Cardiopulmonary exercise testing (CPX) is the gold standard approach to assessing CRF, providing the most comprehensive, non–invasive approach to assessing the integrity of the gears and circuits involved in physical exertion during aerobic activity,1 , 23 , 24 and is important in the post-COVID-19 period.25 Cardiorespiratory fitness is defined as the integrated function of multiple physiologic systems (eg respiratory, cardiovascular, and skeletal muscle), reflecting the interdependence of processes including pulmonary ventilation and/or perfusion, right and/or left ventricular (RV/LV) function, ventricular–arterial coupling, vascular accommodation of efficient blood transport to match O2 requirements, metabolic consumption of O2 and nutrients by muscle cells received from the blood, and communication of these metabolic demands to the cardiovascular control center.1 A primary subcomponent of CRF is exercise capacity, defined as the maximum amount of physical exertion that an individual can achieve during aerobic activity. Peak and/or maximal O2 is the primary measure of exercise capacity obtained from CPX. According to the Fick equation, variability in the peak and/or maximal O2 response is driven by left-sided cardiac output and is therefore an indicator of left ventricular function.26 However, there are additional systems that influence peak and/or maximal O2, such as the ability of working skeletal muscle to consume oxygen during PA. Ventilatory efficiency, primarily assessed through the minute ventilation and/or carbon dioxide production (E/CO2) slope and the partial pressure of end-tidal carbon dioxide production (PETCO2) during CPX, reflect right-sided cardiac function, pulmonary hemodynamics, and integrity of the cardiopulmonary interface.23 , 27 Other measures obtained during CPX provide additional insight into the circuits and gears illustrated in Figure 1 5 , 28 , 29 Readers are referred to previous publications on CPX that provide a comprehensive review of key measures as they relate to these systems. Respiratory muscle function is now recognized as having an important influence on CRF and exercise capacity.5 , 23 , 28 , 29 Assessment of respiratory muscle strength and endurance provides an indication of the ability of the respiratory musculature to generate maximal force during a single maneuver as well as sustain submaximal force repetitively; devices incorporating a pressure transducer and digital interface provide the most detailed assessment.30 , 31 The ability of skeletal muscle to generate maximal force during a single maneuver as well as sustain submaximal force repetitively is comprehensively determined through computerized isokinetic testing (eg, Biodex system). Lastly, lean body mass, a surrogate for muscle mass, and bone density can be assessed through a dual energy X-ray absorptiometry (DEXA) scan. In summary, combining CPX, respiratory muscle testing, isokinetic skeletal muscle testing, and a DEXA scan provides a technologically advanced, and comprehensive approach to assessing the systems illustrated in Figure 1.
Influencers of CRF, Muscle Function, and Bone and Joint Health
Several factors can impact CRF, muscle function, and bone and joint health. These influencers are illustrated in Figure 2 and Table 1 provides definitions of these influencers. These influencer interactions are complex and may present as varying phenotypes. Unfavorable influencer characteristics facilitate a higher likelihood for unhealthy lifestyle behaviors, including a sedentary lifestyle, which leads to lower CRF as well as poor muscle function, and bone and joint health.32, 33, 34, 35, 36, 37, 38, 39 Over a longer term, these influencers can increase the prevalence of risk factors for chronic diseases, and ultimately a confirmed diagnosis of one or more chronic diseases (eg, diabetes, cardiovascular disease, certain forms of cancer). Clinicians and exercise scientists assessing CRF, muscle function, and bone and joint health should be cognizant of these influencers and make efforts to improve and/or correct unfavorable influencer characteristics when possible.40
FIG 2.
Influencers of CRF, muscle function, and bone and joint health. CRF, cardiorespiratory fitness.
TABLE 1.
Definitions of CRF, muscle function, and bone/joint health influencers
|
Interpretation of CRF, Muscle, and Bone/Joint Assessments
A wealth of clinically relevant information is provided through the assessment of CRF, muscle function, and bone and joint health. Figure 3 illustrates clinically relevant areas to consider through these assessments. Direct assessments of the integrity, physiologic function, and signs of pathophysiology in the cardiovascular, pulmonary and/or respiratory, and skeletal muscle systems are all made from this battery of tests. While not directly assessed, higher levels of CRF and muscle function are associated with higher levels of immune function and reduced systemic inflammation, which are particularly relevant in the context of the COVID-19 pandemic.41, 42, 43, 44, 45 In those diagnosed with one or more chronic diseases affecting physiological function, assessments of disease severity can be made. CRF has been consistently shown to be highly prognostic and indicative of health trajectory in virtually all individuals, from those who are apparently healthy to patients diagnosed with one or more chronic diseases.1 As such, prognostic assessments should be performed in all individuals undergoing CPX. Respiratory and skeletal muscle force production also appears to have prognostic utility, where lower responses are indicative of an increased risk for a poor health trajectory.2 , 46 Balance and fall and/or fracture risk information can be obtained from skeletal muscle assessments and fracture risk from DEXA scanning.47 , 48 Lastly, this battery of assessments provide valuable information on prescribing individualized interventions targeting specific areas of dysfunction that have been identified as well as assessing treatment efficacy during follow-up assessments.
FIG 3.
Clinician Interpretation of CRF, muscle, and bone and joint assessments. CRF, cardiorespiratory fitness.
When should CRF, Muscle, and Bone and Joint Assessments be Performed?
Assessments related to the integrity of systems illustrated in Figure 1 are relevant at multiple timepoints across an individual's health trajectory. The medical conditions leading to the greatest burden, from an individual to the population level, are intricately related to CRF, muscle function, and bone and joint health.
Assessing CRF, muscle function, and bone and joint health prior to a medical event (eg, viral infection) can be used to quantify physiologic resiliency, stratify risk, and prescribe preventative interventions specifically directed toward systems that demonstrate dysfunction. Specific to the current viral pandemic, we are continually gaining an appreciation of those at highest risk for a complicated medical course (eg, hospitalization, mechanical ventilation) if infected with COVID-19; dysfunction in systems illustrated in Figure 1 as indicated by poor responses in the proposed battery of assessments appear to be indicative of increased risk.12 , 13 , 30 As such, routine CRF assessments included as part of an annual physical exam would provide information on the degree of physiologic resiliency an individual has if contracting a viral infection. Our group has recently proposed a CPX algorithm to assess health risks in the event of a viral infection and short- to long-term effects in patients who are diagnosed with a viral infection.49 Assessment of muscle function and bone and joint health are also a relevant part of a resiliency assessment, particularly for identifying individuals who demonstrate compromised muscle function and bone and joint prior to a viral infection. A complicated medical course requiring hospitalization and immobilization can further deteriorate muscle function and bone/joint health and significantly decrease mobility and increase the risk for fall and fracture at discharge.10 , 11 , 13 , 50
For patients infected with and recovering from COVID-19, CRF, muscle function, and bone and joint health assessments provide integral information pertaining to the trajectory of recovery and identifying systems with lasting dysfunction. Evidence has already emerged demonstrating a reduced peak O2 and an elevated E/VCO2 slope are common in patients recovering from COVID-19,19 , 20 both of which are primary CPX measures in the recently proposed algorithm.49 In patients suffering from long COVID syndrome, exertional fatigue and dyspnea are primary manifestations which can be quantified by this battery of assessments. The information obtained should also serve as the basis for prescribing individualized and bespoke COVID-19 interventions that address the identified dysfunction in one or more systems. Longitudinal assessments of CRF, muscle function and bone and joint health should be performed to track both changes in health status over time (ie, annual physical exam) as well as therapeutic efficacy when interventions are prescribed. Avoiding declines and, when dysfunction is identified, improving the function of systems illustrated in Figure 1 is essential to improving quality of life, functional capacity, and health trajectory.
Assessment of CRF, muscle function, and bone and joint health is also highly relevant to quantifying the likelihood for developing the risk factors for chronic disease as well as the risk for being diagnosed with one or more chronic diseases (ie, primary prevention).1 , 2 Moreover, these assessments remain relevant in those patients who develop chronic disease risk factors or are diagnosed with one or more chronic diseases to continually stratify risk for future adverse health events (ie, secondary prevention). This panel of assessments should likewise be used for developing interventions that specifically target dysfunction identified in one or more systems illustrated in Figure 1 and to gauge treatment efficacy longitudinally.
Value of Individual Assessments and Considerations for Lack of Resources
While individualized CRF, muscle function, and bone and joint health assessments, when performed together, provide the most comprehensive evaluation of the systems illustrated in Figure 1, it is not always indicated or feasible to perform the complete battery of assessments described herein. In this context, CPX, inspiratory muscle testing, isokinetic muscle testing and DEXA scans are all valuable as individual assessments, each providing insightful clinical information. Judgement should be exercised regarding which assessments should be ordered. For example, isokinetic skeletal muscle testing and DEXA scans are more indicated in post-menopausal women and elderly patients who present with decreased mobility and have indicators of increased fall and/or fracture risk. Moreover, though DEXA scans to monitor bone health are recommended in all adults aged ≥65 years51, both skeletal muscle and DEXA assessments may also be indicated in patients with one or more chronic disease diagnoses at an advanced stage regardless of age. Assessment of CRF is applicable across the lifespan regardless of an individual's health status given its robust, universal prognostic ability and, as such, should be assessed periodically as a clinical standard of care.1 Inspiratory muscle testing may be indicated in multiple situations, including patients with: (1) Unexplained dyspnea irrespective of age; (2) Chronic disease risk factors (eg, obesity) or one or more chronic disease diagnoses irrespective of age; and (3) Elderly individuals who are at risk for or present with frailty.30 In situations where all assessments are indicated but not feasible, thought should be given to prioritize the assessments that are of most importance.
We have presented an ideal, technologically advanced approach to assessing the systems illustrated in Figure 1. We do however acknowledge the ability to perform these assessments are not always feasible or practical due to a lack of equipment, personnel, expertise, or reimbursement. As highlighted in our previous work, we do encourage cross disciplinary collaboration between clinical and exercise scientists where resources, expertise, and access to specialist equipment is often routine and can broaden access to specialist services.40 In the instances where this is not possible, it is still important to assess CRF, muscle function and bone and joint health via alternative approaches. For example, timed walk tests, standard maximal and submaximal exercise testing without ventilatory expired gas, manual muscle testing, skin fold calipers, low-cost inspiratory muscle devices and functional and performance tests (eg, Romberg, Berg Balance Scale, BESTest52 , 53) are examples of viable options when resources are limited. While the precision of measurements related to the integrity of the systems illustrated in Figure 1 is reduced when resources are limited, clinically valuable information regarding physical function and health risks can still be obtained. Obtaining this information by all available resources should be a considered a clinical imperative.
Conclusion
Chronic disease and now viral pandemics are the two leading health crises on a global scale.54 Moreover, chronic disease risk factors and confirmed chronic disease diagnoses clearly increase the likelihood of adverse outcomes following COVID-19, and have thus led to a new global syndemic, defined as two or more health conditions or diseases that negatively interact with and affect the outcomes of one another.55 CRF, muscle function, and bone and joint health are key factors in both the chronic disease and viral pandemics we currently face. Favorable CRF, muscle function, and bone and joint health indicate resiliency to these health conditions while poor, below average characteristics associated with these assessments indicate a much higher risk for poor health outcomes. As such, performing CRF, muscle function and bone and joint health assessments should be considered a global standard of care and, when dysfunction is identified, employing evidence-based interventions to improve performance during these assessments is a health care priority. A primary approach to improving and maintaining higher CRF, muscle function, and bone and joint health is through healthy living behaviors, including being physically active throughout the day, participating in a structured exercise program, consuming a healthy diet, maintaining healthy body weight, and not smoking. In particular, being physically active has a significant positive impact on the responses to the CRF, muscle, and bone and joint health assessments described herein and significantly improve health trajectory. As such, it is imperative that health care professionals embrace the practice of healthy living medicine and promote leading a healthier lifestyle to all patients under their care.54 , 56
References
- 1.Ross R, Blair SN, Arena R, Church TS, Despres JP, Franklin BA, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: A scientific statement from the american heart association. Circulation. 2016;134:e653-e699. [DOI] [PubMed]
- 2.McLeod JC, Stokes T, Phillips SM. Resistance exercise training as a primary countermeasure to age-related chronic disease. Front Physiol. 2019;10:645. doi: 10.3389/fphys.2019.00645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thayer SW, Stolshek BS, Gomez Rey G, Seare JG. Impact of osteoporosis on high-cost chronic diseases. Value Health. 2014;17:43–50. doi: 10.1016/j.jval.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Wasserman K, Hansen JE, Sue DY, Stringer WW, Whipp BJ. 4th ed. Lippincott Williams & Wilkins; Philadelphia: 2005. Principles of exercise testing and interpretation: including pathophysiology and clinical applications. [Google Scholar]
- 5.Myers J, Arena R, Cahalin LP, Labate V, Guazzi M. Cardiopulmonary exercise testing in heart failure. Curr Probl Cardiol. 2015;40:322–372. doi: 10.1016/j.cpcardiol.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 6.Zheng C, Huang WY, Sheridan S, Sit CH, XK Chen, Wong SH. COVID-19 pandemic brings a sedentary lifestyle in young adults: A cross-sectional and longitudinal study. Int J Environ Res Public Health. 2020:17. doi: 10.3390/ijerph17176035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Consortium OBotE-C. Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients. 2020;12:1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis. 2021;64:108–110. doi: 10.1016/j.pcad.2020.04.005. Epub 2020 Apr 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sassone B, Mandini S, Grazzi G, Mazzoni G, Myers J, Pasanisi G. Impact of COVID-19 pandemic on physical activity in patients with implantable cardioverter-defibrillators. J Cardiopulm Rehabil. 2020;40:285–286. doi: 10.1097/HCR.0000000000000539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moro T, Paoli A. When COVID-19 affects muscle: effects of quarantine in older adults. Eur J Transl Myol. 2020;30:9069. doi: 10.4081/ejtm.2019.9069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Girgis CM, Clifton-Bligh RJ. Osteoporosis in the age of COVID-19. Osteoporos Int. 2020;31:1189–1191. doi: 10.1007/s00198-020-05413-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brawner CA, Ehrman JK, Bole S, Kerrigan DJ, Parikh SS, Lewis BK, et al. Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019. Mayo Clin Proc. 2021;96:32–39. doi: 10.1016/j.mayocp.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheval B, Sieber S, Maltagliati S, Millet GP, Formánek T, Chalabaev A, et al. Muscle strength is associated with COVID-19 hospitalization in adults 50 years of age and older. medRxiv: the preprint server for health sciences. 2021 doi: 10.1101/2021.02.02.21250909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salgado-Aranda R, Pérez-Castellano N, Núñez-Gil I, Orozco AJ, Torres-Esquivel N, Flores-Soler J, et al. Influence of baseline physical activity as a modifying factor on COVID-19 mortality: A single-center, retrospective study. Infect Dis Ther. 2021;10:801–810. doi: 10.1007/s40121-021-00418-6. Epub 2021 Mar 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamer M, Kivimäki M, Gale CR, Batty GD. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav Immun. 2020;87:184–187. doi: 10.1016/j.bbi.2020.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raman B, Cassar MP, Tunnicliffe EM, Filippini N, Griffanti L, Alfaro-Almagro F, et al. Vol. 31. 2021. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. (EClinicalMedicine). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat Med. 2021;27:626–631. doi: 10.1038/s41591-021-01292-y. Epub 2021 Mar 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Humphreys H, Kilby L, Kudiersky N, Copeland R. Long COVID and the role of physical activity: a qualitative study. BMJ open. 2021;11 doi: 10.1136/bmjopen-2020-047632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu M, Lv F, Huang Y, Xiao K. Follow-Up study of the chest CT Characteristics of COVID-19 survivors seven months after recovery. Front Med (Lausanne) 2021;8:636298. doi: 10.3389/fmed.2021.636298. eCollection 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Debeaumont D, Boujibar F, Ferrand-Devouge E, Artaud-Macari E, Tamion F, Gravier FE, et al. Cardiopulmonary exercise testing to assess persistent symptoms at 6 months in people with COVID-19 who survived hospitalization - A pilot study. Phys Ther. 2021;18 doi: 10.1093/ptj/pzab099. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silva RN, Goulart CDL, Oliveira MR, Tacao GY, Back GD, Severin R, et al. Cardiorespiratory and skeletal muscle damage due to COVID-19: making the urgent case for rehabilitation. Expert Rev Respir Med. 2021:1–14. doi: 10.1080/17476348.2021.1893169. [DOI] [PubMed] [Google Scholar]
- 22.Faghy MA, Ashton RE, Maden-Wilkinson TM, Copeland RJ, Bewick T, Smith A, et al. Integrated sports and respiratory medicine in the aftermath of COVID-19. Lancet Respir Med. 2020;8:852. doi: 10.1016/S2213-2600(20)30307-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, et al, American heart association exercise CR, prevention committee of the council on clinical C, council on E, prevention, council on peripheral vascular D, interdisciplinary council on quality of c and outcomes R. clinician's guide to cardiopulmonary exercise testing in adults: a scientific statement from the american heart association. Circulation. 2010;122:191-225. [DOI] [PubMed]
- 24.Kaminsky LA, Myers J, Arena R. Determining cardiorespiratory fitness with precision: Compendium of findings from the FRIEND registry. Prog Cardiovasc Dis. 2019;62:76–82. doi: 10.1016/j.pcad.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Faghy MA, Sylvester KP, Cooper BG, Hull JH. Cardiopulmonary exercise testing in the COVID-19 endemic phase. Br J Anaesth. 2020;125:447–449. doi: 10.1016/j.bja.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, et al. Exercise standards for testing and training: A scientific statement from the american heart association. Circulation. 2013;128:873-934. [DOI] [PubMed]
- 27.Guazzi M, Bandera F, Ozemek C, Systrom D, Arena R. Cardiopulmonary exercise testing: What is its value? J Am Coll Cardiol. 2017;70:1618–1636. doi: 10.1016/j.jacc.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 28.Guazzi M, Arena R, Halle M, Piepoli MF, Myers J, Lavie CJ. 2016 focused update: Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2016;133:e694–e711. doi: 10.1161/CIR.0000000000000406. [DOI] [PubMed] [Google Scholar]
- 29.Guazzi M, Adams V, Conraads V, Halle M, Mezzani A, Vanhees L, et al. European association for cardiovascular P, rehabilitation and american heart A. EACPR/AHA scientific statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2012;126:2261–2274. doi: 10.1161/CIR.0b013e31826fb946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Severin R, Arena R, Lavie CJ, Bond S, Phillips SA. Respiratory muscle performance screening for infectious disease management following COVID-19: A highly pressurized situation. Am J Med. 2020;133:1025–1032. doi: 10.1016/j.amjmed.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laveneziana P, Albuquerque A, Aliverti A, Babb T, Barreiro E, Dres M, et al. Vogiatzis I and Verges S. ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J. 2019;53 doi: 10.1183/13993003.01214-2018. [DOI] [PubMed] [Google Scholar]
- 32.García-Mayor J, Moreno-Llamas A, la Cruz-Sánchez E. High educational attainment redresses the effect of occupational social class on health-related lifestyle: Findings from four Spanish national health surveys. Ann Epidemiol. 2021;58:29–37. doi: 10.1016/j.annepidem.2021.02.010. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 33.Krishnaswami J, Sardana J, Daxini A. Community-engaged lifestyle medicine as a framework for health equity: Principles for lifestyle medicine in low-resource settings. Am J Lifestyle Med. 2019;13:443–450. doi: 10.1177/1559827619838469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Joseph RJ, Alonso-Alonso M, Bond DS, Pascual-Leone A, Blackburn GL. The neurocognitive connection between physical activity and eating behaviour. Obes Rev. 2011;12:800–812. doi: 10.1111/j.1467-789X.2011.00893.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blumenthal JA, Smith PJ, Mabe S, Hinderliter A, Welsh-Bohmer K, Browndyke JN, et al. Lifestyle and neurocognition in older adults with cardiovascular risk factors and cognitive impairment. Psychosom Med. 2017;79:719–727. doi: 10.1097/PSY.0000000000000474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Strauss RS, Rodzilsky D, Burack G, Colin M. Psychosocial correlates of physical activity in healthy children. Arch Pediatr. 2001;155:897–902. doi: 10.1001/archpedi.155.8.897. [DOI] [PubMed] [Google Scholar]
- 37.Xiao Y, Wang H, Zhang T, Ren X. Psychosocial predictors of physical activity and health-related quality of life among Shanghai working adults. Health Qual Life Outcomes. 2019;17:72. doi: 10.1186/s12955-019-1145-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.RE Lee, Cubbin C. Striding toward social justice: the ecologic milieu of physical activity. Exerc Sport Sci Rev. 2009;37:10–17. doi: 10.1097/JES.0b013e318190eb2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wardle J, Steptoe A. Socioeconomic differences in attitudes and beliefs about healthy lifestyles. J Epidemiol Community Health. 2003;57:440–443. doi: 10.1136/jech.57.6.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Faghy MA, Arena R, Stoner L, Haraf RH, Josephson R, Hills AP, et al. The need for exercise sciences and an integrated response to COVID-19: A position statement from the international HL-PIVOT network. Prog Cardiovasc Dis. 2021 doi: 10.1016/j.pcad.2021.01.004. S0033-0620(21)00013-X. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burtscher J, Millet GP, Burtscher M. Low cardiorespiratory and mitochondrial fitness as risk factors in viral infections: implications for COVID-19. Br J Sports Med. 2021;55:413–415. doi: 10.1136/bjsports-2020-103572. [DOI] [PubMed] [Google Scholar]
- 42.Filgueira TO, Castoldi A, Santos LER, de Amorim GJ, de Sousa Fernandes MS, Anastácio WdLdN, et al. The relevance of a physical active lifestyle and physical fitness on immune defense: Mitigating disease burden, with focus on COVID-19 consequences. Front Immunol. 2021;12:587146. doi: 10.3389/fimmu.2021.587146. eCollection 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Laddu DR, Lavie CJ, Phillips SA, Arena R. Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic. Prog Cardiovasc Dis. 2021;64:102–104. doi: 10.1016/j.pcad.2020.04.006. Epub 2020 Apr 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nieman DC. Coronavirus disease-2019: A tocsin to our aging, unfit, corpulent, and immunodeficient society. J Sport Health Sci. 2020;9:293–301. doi: 10.1016/j.jshs.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jae SY, Heffernan KS, Kurl S, Kunutsor SK, Kim CH, Johnson BD, et al. Cardiorespiratory fitness, inflammation, and the incident risk of pneumonia. J Cardiopulm Rehabil Prev. 2021;41:199–201. doi: 10.1097/HCR.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 46.van der Palen J, Rea TD, Manolio TA, Lumley T, Newman AB, Tracy RP, et al. Respiratory muscle strength and the risk of incident cardiovascular events. Thorax. 2004;59:1063–1067. doi: 10.1136/thx.2004.021915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pal C, Mani S, Pal AK, Ramuni K, Hassan HC. Assessment of risk factors and occurrence of osteoporotic fractures among low impact trauma clients in West Bengal, India. Enfermeria clinica. 2020;30 Suppl 5:6-11.
- 48.Veronese N, Smith L, Barbagallo M, Yang L, Zou L, Haro JM, et al. Sarcopenia and fall-related injury among older adults in five low- and middle-income countries. Exp Gerontol. 2021;147 doi: 10.1016/j.exger.2021.111262. [DOI] [PubMed] [Google Scholar]
- 49.Arena R, Myers J, Kaminsky L. Cardiopulmonary exercise testing algorithm for viral infection: Assessment of acute health risk and short- to long-term effects. J Cardiopulm Rehabil. 2021 doi: 10.1097/HCR.0000000000000614. In Press. [DOI] [PubMed] [Google Scholar]
- 50.Sagarra-Romero L, Viñas-Barros A. COVID-19: Short and long-term effects of hospitalization on muscular weakness in the elderly. Int J Environ Res Public Health. 2020:17. doi: 10.3390/ijerph17238715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Screening for osteoporosis to prevent fractures: us preventive services task force recommendation statement. Jama. 2018;319:2521–2531. doi: 10.1001/jama.2018.7498. [DOI] [PubMed] [Google Scholar]
- 52.Pérennou D, Decavel P, Manckoundia P, Penven Y, Mourey F, Launay F, et al. Evaluation of balance in neurologic and geriatric disorders. Ann Readapt Med Phys. 2005;48:317–335. doi: 10.1016/j.annrmp.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 53.Horak FB, Wrisley DM, Frank J. The balance evaluation systems test (BESTest) to differentiate balance deficits. Phys Ther. 2009;89:484–498. doi: 10.2522/ptj.20080071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arena R, Lavie CJ. The global path forward - Healthy Living for Pandemic Event Protection (HL - PIVOT) Prog Cardiovasc Dis. 2021;64:96–101. doi: 10.1016/j.pcad.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17:423–441. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- 56.Arena R, McNeil A, Sagner M, Lavie CJ. Healthy living: The universal and timeless medicine for healthspan. Prog Cardiovasc Dis. 2017;59:419–421. doi: 10.1016/j.pcad.2017.01.007. [DOI] [PubMed] [Google Scholar]