Abstract
The COVID-19 pandemic triggered abrupt challenges for health care providers, requiring them to simultaneously plan for and manage a rise of COVID-19 cases while maintaining essential health services. Since March 2020, the COVID-19 Health System Response Monitor, a joint initiative of the European Observatory on Health Systems and Policies, the WHO Regional Office for Europe, and the European Commission, has documented country responses to COVID-19 using a structured template which includes a section on provision of care. Using the information available on the platform, this paper analyzes how countries planned services for potential surge capacity, designed patient flows ensuring separation between COVID-19 and non-COVID-19 patients, and maintained routine services in both hospital and ambulatory settings. Despite very real differences in the organization of health and care services, there were many similarities in country responses. These include transitioning the management of COVID-19 mild cases from hospitals to outpatient settings, increasing the use of remote consultations, and cancelling or postponing non-urgent services during the height of the first wave. In the immediate future, countries will have to continue balancing care for COVID-19 and non-COVID-19 patients to minimize adverse health outcomes, ideally with supporting guidelines and COVID-19-specific care zones. Looking forward, policymakers will have to consider whether strategies adopted during the COVID-19 pandemic will become permanent features of care provision.
Keywords: COVID-19, Essential services, Service delivery, Prioritization of care
1. Introduction
The COVID-19 pandemic left health systems with the dual challenge of planning for and treating patients with COVID-19, while at the same time maintaining routine services and preventing the virus from spreading further in other care areas. Even the most well-resourced health systems faced pressures from new challenges brought on by COVID-19, and every country had to make difficult choices about how to maintain access to essential care while treating a novel communicable disease.
Even before the pandemic, comparing health services across countries had substantial limitations including but not limited to the lack of standardized definitions of terms (e.g., what is considered an essential service?), the variation in range of services attributed to each type of health care delivery (e.g., what services are provided in outpatient vs. inpatient settings?), and where the services are provided. For example, the number of physician consultations varies widely: in 2016, fewer than 3 consultations per person occurred in Cyprus and Sweden, with over 11 in the Slovak Republic and Hungary [4]. The number of hospital discharges per year also differs, even between closely neighboring countries: the Netherlands had 90 inpatient care discharges per 1000 population in 2018 while Germany had 255 in 2017 [5].
In the context of COVID-19, these variations have come into even starker contrast. Across countries—and over time—the pandemic has seen variation in the case definition [14], treatment for severe patients [1], medications used [13], and the location of COVID-19 treatment [11]. Moreover, the starting point for physical infrastructure and workforce proved crucial in defining the country response to COVID-19 [21].
This article reviews key themes in how health systems adapted the provision of health care during the early peaks of the pandemic. We discuss how countries compare in their approaches to planning services, managing cases, and maintaining essential services, highlighting country-specific innovations and preliminary lessons for policymakers.
2. Methods
The evidence presented in this article has been compiled from the methodology used and content reported in the Health System Response Monitor (HSRM), an online platform established in March 2020 in response to the COVID-19 outbreak to collect and organize up-to-date information on how countries in the WHO European region and Canada are responding to the crisis. The HSRM, available at https://www.covid19healthsystem.org/, focuses primarily on the responses of health systems but also captures wider public health initiatives. The HSRM is a joint undertaking of the European Observatory on Health Systems and Policies (Observatory), the WHO Regional Office for Europe, and the European Commission.
The HSRM content is broadly structured around the standard health system functions [16], and collects information about six broad areas of the country response to COVID-19: (1) preventing transmission, (2) ensuring sufficient physical infrastructure and workforce capacity, (3) providing health services effectively, (4) paying for services, (5) governance, and (6) measures in other sectors. The HSRM is authored by country experts, largely from the Health System and Policy Monitor network, and is edited by Observatory staff. The template for the HSRM has been used by the country experts to continuously update their country's response based on the latest measures taken in their countries. By using a structured questionnaire and having a team of Observatory staff editing the responses, information collected in the HSRM enables cross-country comparisons.
This article focuses on one of the six areas: “Providing health services effectively”. Within each country response, this section describes approaches for service delivery planning and patient pathways for suspected COVID-19 cases. It also considers efforts by countries to maintain other essential services during periods of excessive demand for health services.
Data collected from the HSRM between March 2020 and October 2020 serves as the primary source for this article, although some content has been supplemented with information from co-authors, Observatory editors, other country materials and documents. The absence of specific countries does not necessarily mean it did not adjust its provision of health services, but rather that limited information was available at the time of data collection. Additionally, the HSRM country pages contain varying levels of information, which means that the summary tables included in this analysis are not meant to be exhaustive.
This article does not aim to answer why some countries have responded better to the pandemic than others, but rather, to draw out interesting patterns, key contrasts, and innovative approaches in policy responses aimed at addressing common challenges across countries. Attributing any causal link between policy response and pandemic outcome presents a multitude of methodological challenges, so the analysis instead intends to describe and assess policy responses and draw out critical lessons. In turn, this can serve as a basis from which to begin discussions that eventually lead to an understanding of what seems to work, what does not work, and why. This analysis also presents some current gaps in policy knowledge that may open up areas for future research or provide a basis for further policy development.
3. Results
The COVID-19 pandemic presented immediate challenges to health care providers, and the countries studied in the HSRM show wide variations in response, but also significant overlap in spite of real differences in the organization of health care services. The continually changing situation created an unprecedented strain on health care providers to respond, with rapidly changing guidance for the COVID-19 case definition, management of COVID-19 contacts, infection prevention and control, occupational health, pregnancy and post-partum care, and more.
Regardless of the specific approaches taken, COVID-19 required health care providers to plan and implement measures to keep essential services running while managing an influx of COVID-19 suspected or confirmed cases. The following sections provide details about how countries planned services for potential surge capacity, designed patient flows ensuring separation between COVID-19 and non-COVID-19 patients, and maintained routine services in both hospital and ambulatory settings.
3.1. Planning services for COVID-19 patients in hospitals
In most countries, the initial pandemic response focused on planning services in hospitals, including ensuring sufficient physical infrastructure and workforce [21], as well as preventing transmission [15]. This article focuses on how hospitals planned services for treating and caring for COVID-19 patients. In some countries, central governments made national determinations for how resources should be allocated, and where and how patients with COVID-19 should flow through the system. Other countries left it up to regional bodies to determine the response. Still others gave guidance about measures to implement but left individual health care providers responsible for implementing the measures. This section describes each of these approaches, with country examples for each.
Particularly at the beginning of the pandemic, several countries organized the treatment of COVID-19 patients in designated hospitals, often those that specialized in treatments of infectious diseases or had intensive care capacities. Albania initially designated two hospitals for COVID-19 and transferred the medical services conducted at these hospitals to other public hospitals. Kyrgyzstan designated 24 hospitals for the observation of suspected cases and two hospitals for confirmed COVID-19 cases. On March 4th 2020, the Republic of Moldova designated four hospitals for the treatment of COVID-19 patients, two for severe cases, and two for mild and moderate cases. Greece created 13 COVID-19 reference hospitals across the country, with four hospitals dedicated solely to COVID-19 patients. In February, Serbia designated four hospitals as points of treatment for COVID-19 patients, although with increasing case numbers, five more were designated on March 16th 2020 to exclusively treat COVID-19 patients. The Ministry of Health in Slovakia designated three hospitals to serve uniquely for the treatment of COVID-19 patients, with other hospitals providing separate pavilions.
Other countries designated the hospitals in the largest cities to treat COVID-19 patients, but this quickly adapted as case numbers grew. Belgium designated two hospitals, in Brussels and Antwerp, as referral centers for the treatment of COVID-19 patients, but as the case numbers grew, all hospitals started admitting COVID-19 patients. In January, Cyprus initially designated the biggest hospital in the country as the reference hospital for COVID-19, but later changed this to a smaller hospital and a nursing ward, as well as an intensive care unit in each of the remaining five public hospitals in the country.
Other countries took a more regional approach. In Austria, each region designated specific hospitals or new hospital units to treat patients with suspected or confirmed COVID-19 cases. On March 27th 2020, the Bulgarian Minister of Health issued an ordinance on determining the hospitals, hospital wards, and number of beds determined for treatment of COVID-19 patients in each district describing that regions with higher infection rates identify designated COVID-19 hospitals. In Poland, each province (voivodeship) designated at least one hospital for COVID-19 patients, which serve as reference hospitals to which confirmed cases can be referred and treated. In addition, provinces have also selected hospitals with infectious disease departments that will be the second choice to admit patients at risk; these hospitals are required to be at the highest levels of readiness, with appropriate equipment and personal protective equipment (PPE). Switzerland's Federal Council took some measures in mid-March 2020 to ensure equitable distribution across cantons, such as requiring cantons to report on capacity, however in general cantons were able to organize individual responses to COVID-19.
Several other countries have not designated specific hospitals to exclusively treat COVID-19 patients, and provide national guidance while leaving the specifics to individual hospitals. Hospitals in Denmark designated departments and sections for treatment of COVID-19 patients. In France, initially all COVID-19 cases were referred to hospitals, while national recommendations for managing COVID-19 cases were first published in March 2020 and regularly updated on the Ministry of Health webpage. Ireland and the UK (England) required all hospitals to have a COVID-19 plan in place. The main acute hospital in Malta duplicated its emergency room so that one could treat COVID-19 patients and the other could treat non-COVID-19 patients. The Netherlands used open capacity due to postponements to support COVID-19 patients. In Sweden, hospitals on aggregate have doubled the system's capacity for intensive care, but different regions and hospitals have taken different measures.
Overall, the measures initially taken in hospitals influenced the subsequent response in managing cases and maintaining essential services. Even within one country, the initial approach could vary between regions, with Italy providing a clear example: as of April 8th 2020, the Lombardy region hospitalized 49% of positive cases while the Veneto hospitalized 21%. In contrast, in Germany, as of April 1st 2020, 85% of COVID-19 cases were treated by ambulatory physicians, mainly general practitioners (GPs), despite Germany having one of the largest acute care sectors in Europe. As more became known about COVID-19, countries increasingly transitioned their focus to manage cases outside of the hospital.
3.2. Managing COVID-19 cases–patient pathway and the role of ambulatory care
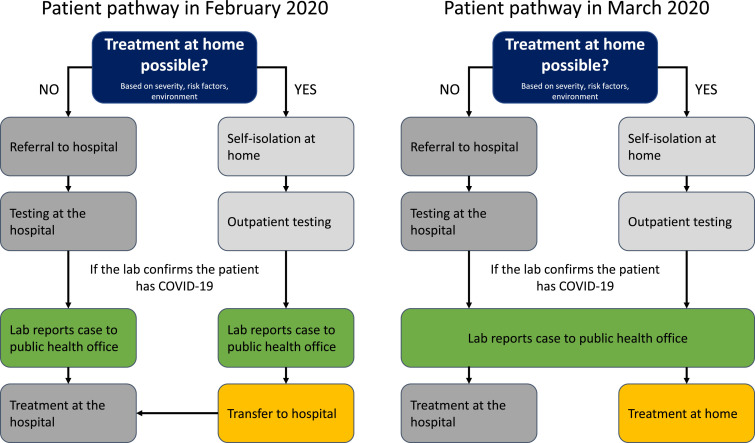
After a positive diagnosis of COVID-19, the patient pathway varied substantially across countries and sometimes even within countries. At the beginning of the pandemic, some countries hospitalized all patients with COVID-19. As more became known about the disease and to help manage capacity levels in hospitals, most countries advised mild cases of COVID-19 to self-isolate at home while only hospitalizing more severe cases. One example is provided in Fig. 1 , which compares the patient pathway recommended by the Robert Koch Institute (RKI) in Germany in February and March 2020. The guidance changed from hospitalizing all patients with COVID-19 to hospitalizing only those where treatment at home was not possible, with this change in the pathway indicated in yellow in the figure.
Fig. 1.
Testing criteria and measures for COVID-19 in Germany
Authors compilation based on RKI publications, latest available at [17]
In addition to the adapting process for managing cases changed over time, even within one country, the case definition could vary. In Israel, hospitals did not have a standard definition of “severely” ill COVID-19 patients, which not only caused confusion in reporting to the Ministry of Health, but also at times variations in treatment. On July 12th, 2020, the Ministry of Health issued a circular with a clear guidance in order to harmonize the definition and set standard paths of care and treatment guidelines.
As a result of the increased focus on treating mild COVID-19 patients outside of hospitals, primary care providers took on expanded responsibilities. In many countries, they served as the first point of contact for a suspected case, referred patients for testing, and diagnosed patients with COVID-19. Additionally, they supported surveillance teams in case detection and even in a few cases conducted contact tracing themselves, as described in more depth elsewhere (Rajan, 2020). Furthermore, they provided support and monitored conditions of those isolating at home to make sure they followed medical advice, initiated transfers to more intensive care if needed, and determined when the quarantine period can end.
Some countries, including Armenia, Belgium, France, and Germany, requested GPs to conduct home visits to perform tests or monitor COVID-19 patients. In the Czech Republic, GPs were advised to only conduct home visits with appropriate PPEs, and since many GPs did not have this in the beginning, some GPs were unwilling to see their patients in the first weeks of the outbreak. France advised GPs to group their consultations so that suspected cases of COVID-19 were seen in the same time period. However, more often countries discourage patients experiencing symptoms from visiting primary care providers or hospitals directly until after a phone consultation.
Some countries set up new models of care, such as ‘fever clinics’ in Georgia or ‘community assessment hubs’ in Ireland, which aimed at redirecting potential COVID-19 patients from other health care providers and preventing transmission to non-infected patients. During the last week of March 2020, Oslo, which had the highest infection rate in Norway, opened seven ‘fever clinics’ to receive patients referred by the GPs or the emergency out-of-hours clinics. Luxembourg similarly designated the ‘Maisons médicales’ (GP out-of-hour offices) as advanced care centers in order to contain the spread of the virus and concentrate these patients outside of emergency departments and general practices. The advanced care centers were supplied with testing materials for diagnosis of infections and appropriate protective equipment for staff. To manage the discharge process for COVID-19 patients, Belgium set up transition centers for patients who do not require hospitalization but are not yet able to return home.
In other countries, especially those with relatively newer primary care structures, it was possible to implement a broader redesign of primary health care operations in reaction to the pandemic. For example, Greece restructured its primary health centers along two main objectives. First, certain health centers operated on a 24-hour basis exclusively for the screening and management of mild COVID-19 cases. As of April 10th 2020, five centers were prepared to support the network of COVID-19 reference hospitals. Second, other health centers were transformed for care for non-COVID-19 patients with chronic diseases, emergency cases, and communication with patients in home isolation.
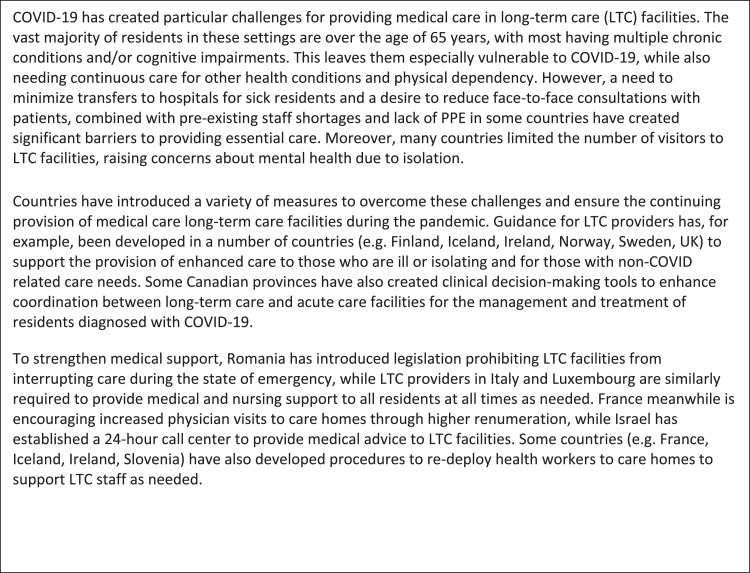
Other providers, including ambulance, home care, and long-term care providers, have taken various roles in managing cases. Several countries used ambulance providers to transport severe cases to the hospitals, including Belgium, Cyprus, Italy, Kazakstan, and the Republic of Moldova. In Hungary, the National Emergency Ambulance Service tested patients at home and delivered the test results to the lab. Care provided at home also faced changes as a result of COVID-19, particularly because health care providers may not have been equipped with the necessary PPE. A number of countries mobilized volunteers or organizations such as the Red Cross to provide services or deliver medications to vulnerable groups at home. For example, Croatia enabled immune-compromised patients to have blood samples taken at home. Across the world, many deaths attributed to COVID-19 took place in nursing homes, as many were not equipped to handle the pandemic, which is described in more depth in Fig. 2 .
Fig. 2.
Providing essential health services in care homes. [8], [20]
3.3. Remote consultations expanded both for monitoring of COVID-19 cases and teleconsultations
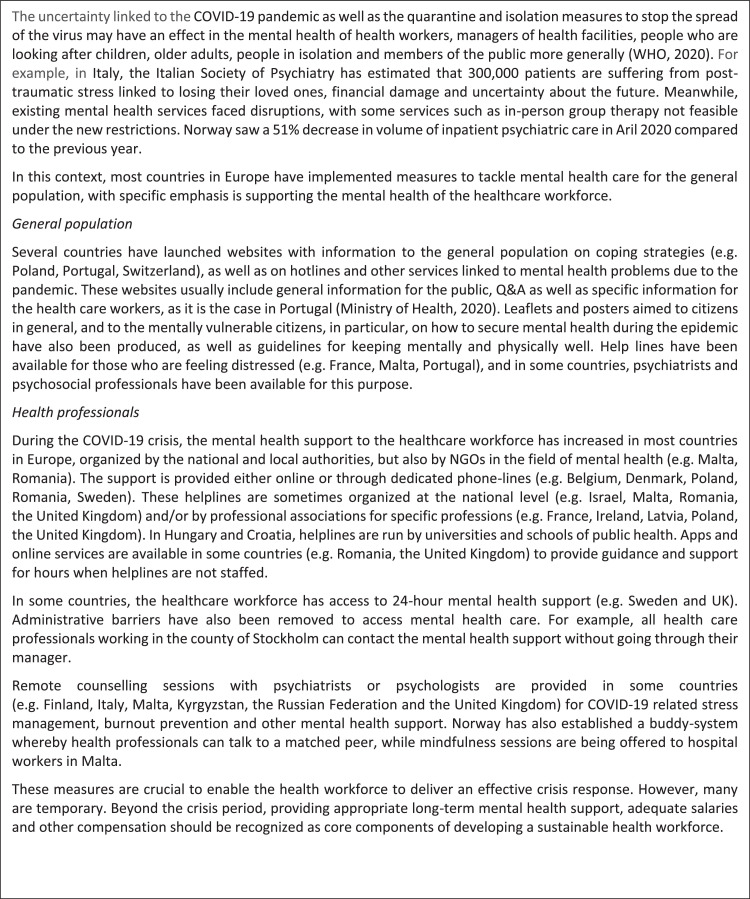
The use of remote consultations took a significant leap forward as providers searched for ways to continue to provide care while reducing the risk of transmission. In Germany, the Federal Association of SHI Physicians reported more than a ten-fold increase of teleconsultations in March 2020 (19,500) compared to January and February 2020 (1,700). Similarly, the number of doctors using remote consultations in France jumped from around 3,000 in February 2020 to 56,000 in April 2020, with GPs billing 80% of all teleconsultations. Lithuania's National Health Insurance Fund reported conducting 758,000 primary health care remote consultations in April 2020 compared to 11,000 in April 2019. In addition to conversations via telephone, video consultations have become more common. These support more advanced consultations that can involve simultaneous sharing of test results, imaging, or other files [23]. While primary care consultations often made up the majority of virtual consultations, they have also been adopted in specialty consultations including mental health (Fig. 3 ).
Fig. 3.
Mental health services.
To support remote consultations, many countries used existing or set up new telephone hotlines. Many countries use 112 as the emergency hotline, and have enhanced their screening procedures to determine whether a call is related to COVID-19. For example, Georgia forwarded calls related to COVID-19 to primary care doctors who have been specifically trained on COVID-19 protocols. In some cases, the supplementary lines were set up due to extraordinary demand on the regular emergency number. For example, Latvia set up a designated hotline for COVID-19 after the emergency number 113 started receiving an average of 4,000 calls a day instead of the regular 1,200 [7]. In Spain, initially the standard 24/7 emergency hotline was used for patients, but most regions have established a dedicated phone hotline separate from the 24/7 call center number to keep the standard emergency hotline for emergencies not related to COVID-19. Estonia and Germany both had pre-existing physician advisory lines in place, but Estonia set up a separate COVID-19 hotline to reduce the burden of calls to the GP helpline and 112.
Several countries reported setting up call lines for non-medical advice relating to COVID-19 information and procedures or chatbots on official websites (e.g., Ministry of Health or public health agencies). Norway established a helpline for general COVID-19 questions, not staffed by health care workers, while patient organizations have established additional helplines for patients with chronic diseases. Similarly, Switzerland operates a 24-hour COVID-19 hotline that provides recommendations on what to do based on symptoms, but does not provide medical advice. Austria set up a telephone helpline to guide patients to the right point of contact in order to avoid physical contacts with health care professionals and other patients. Latvia and Lithuania established special COVID-19 hotlines to provide current advice on conditions and testing.
3.4. Maintaining essential services
As an initial response to the pandemic, most countries prioritized essential services and cancelled or postponed non-urgent care (Table 1 ), although countries varied widely in which services they maintained and the duration of the restrictions. In the first wave of the COVID-19 pandemic, service disruption often occurred at the national level. As shown in Table 2 , the national restrictions on care provision ranged from 27 days (Poland) to 70 days (Iceland), with a median of 43.5 days. Nevertheless, a few commonalities can be observed, with the shared perspective that the mortality risk from postponing an intervention should not be higher than that of a severe COVID-19 case. In hospitals, essential services often included urgent consultations, necessary treatments (e.g., chemotherapy, dialysis), maternal services, and rehabilitation. In primary care, countries were more likely to continue treating chronic illnesses which would otherwise lead to deterioration of condition, neonatal screening, and infant vaccinations.
Table 1.
Countries cancelling or postponing non-urgent care and elective surgeries.
| Types of care adaptations | Countries |
|---|---|
| Non-urgent care and/or elective surgeries cancelled or postponed1 | Albania, Austria, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Cyprus, Denmark, Estonia, France, Georgia, Greece, Hungary, Ireland, Israel, Italy, Latvia, Lithuania, Luxembourg, Malta, North Macedonia, Norway, Poland, Portugal, Romania, Russian Federation, Serbia, Slovakia, Slovenia, Spain, Switzerland, Turkey, Ukraine, UK (England) |
| Physician or local decision about adaptations to care provision | Canada, Germany, the Netherlands, Spain, Sweden, Switzerland, US |
| Services maintained but potentially at reduced capacity | Armenia, Finland, Iceland |
1Countries vary in how they consider non-urgent care and whether this applies in ambulatory as well as inpatient settings. In some countries (e.g., Israel) the cancellations were only applicable to the public sector and not the private sector.
Table 2.
Duration of restrictions.
| Country | Date of restrictions | Date of reintroduction | Duration (days) |
|---|---|---|---|
| Albania | 11 March 2020 | 15 May 2020 | 65 |
| Austria | 12 March 2020 | 15 April 2020 | 34 |
| Belgium | 14 March 2020 | 4 May 2020 | 54 |
| Bulgaria | 13 March 2020 | 21 April 2020 | 39 |
| Croatia | 16 March 2020 | 27 April 20201 | 42 |
| Czech Republic | 17 March 2020 | 14 April 2020 | 28 |
| Denmark | 17 March 2020 | 13 April 2020 | 29 |
| Estonia | 17 March 20202 | 21 April 2020 | 35 |
| France | 6 March 2020 | 11 May 2020 | 67 |
| Greece | 23 March 2020 | 4 May 2020 | 36 |
| Hungary | 26 March 2020 | 4 May 2020 | 40 |
| Iceland | 23 March 2020 | 31 May 2020 | 70 |
| Ireland | 28 March 2020 | 19 May 20204 | 53 |
| Israel | 14 March 2020 | 27 April 2020 | 44 |
| Italy | 29 February 2020 | 4 May 2020 | 65 |
| Latvia | 14 March 2020 | 20 April 2020 | 38 |
| Lithuania | 16 March 2020 | 29 April 20205 | 44 |
| Luxembourg | 18 March 2020 | 4 May 2020 | 48 |
| Malta | 17 March 2020 | 22 May 2020 | 66 |
| Norway | 12 March 2020 | 14 April 2020 | 33 |
| Poland | 23 March 2020 | 18 April 2020 | 27 |
| Portugal | 17 March 2020 | 3 May 2020 | 47 |
| Romania | 23 March 2020 | 15 May 2020 | 53 |
| Russian Federation | 16 April 2020 | 25 May 2020 | 40 |
| Slovenia | 20 March 2020 | 9 May 2020 | 50 |
| Spain | 15 March 2020 | 17 May 20206 | 63 |
| Switzerland | 20 March 2020 | 27 April 2020 | 38 |
| UK (England) | 17 March 2020 | 29 April 2020 | 43 |
| Average | 46 days |
1: Croatia: Outpatient services reopened April 27th, while public hospitals inpatient services reopened May 4th.
2: Estonia: Elective inpatient and outpatient care only continues for those patients whose health situation does not allow for postponement of the treatment (made by the treating doctor). As of March 26th, dental care and private clinics can only provide emergency services.
3: Greece: As of May 4th, hospital doctors resumed non-emergency operations and afternoon outpatient appointments which had been suspended amid the peak of the coronavirus pandemic. Morning outpatient appointments resumed the week after, from May 11th.
4: Ireland: Screening programs restarted later, on July 6th.
5: Lithuania: Providers could only restart when they presented plans on how to do it safely, and then got the approval, plus they were not motivated to restart until July as they were paid anyway. Dental care reopened later, on May 18th.
6: Spain: reopening dates varied by region but end of lockdown provides national proxy.
Source: HSRM and [12]. Some countries had regional variations so the summary table captures the national guidance.
At the time of writing, limited data is available on the impact of these restrictions, as well as how this interacts with the approach taken in many countries to reserve bed and/or ICU capacities in case of a surge in cases. Further, after the initial restrictions, most countries used more local approaches to manage COVID-19 outbreaks, obscuring the situation at the national level. However, data from some countries already suggest alarming health trends for patients without COVID-19. Several countries observed drops in emergency room visits; Portugal experienced a 45% reduction in emergency room visits and five hospitals in Italy experienced a 73-83% drop in pediatric emergency department visits. Germany reported 30% fewer heart attacks and strokes, and registration of patients with suspected myocardial infarction has decreased by about 25% since the outbreak in Sweden. While reports of rationing care in hospitals were uncommon, several countries, including Estonia and Spain, developed ethical guidelines to guide clinical decision-making. In Armenia, on June 6th 2020, 200 patients were awaiting hospitalization due to shortage of beds.
In ambulatory care, countries saw a near-universal trend of decreased consultations in many specialties (largely due to the cancellation of services) combined with increased remote treatments, as described in the previous section. Norway provides a glimpse into this trend: compared to March 2019, in March 2020 Norway saw a 71% decline in outpatient consultations with chiropractors and a 55% decline in consultations with physiotherapists and dentists, while GP consultations increased by about 10%. The increase of GP consultations was driven by remote consultations, which constituted 58% of all consultations by week 12 since the introduction of physical distancing measures.
Routine public health activities, including cancer screenings and immunizations, were also affected in many countries. Some countries, including Bulgaria, Poland, and the Russian Federation, temporarily postponed some programs, while other countries considered them essential services. Slovenia paused cancer screenings, but resumed them in mid-May 2020, and expects that most cancer screening programs will meet usual targets by the end of 2020. April immunization data from Ukraine shows a decline, including a 30% reduction in measles-mumps-rubella vaccine coverage compared to 2018-2019 rates, as does population vaccination rates in Armenia, which has dropped by 27%. Further, Norway expressed concerns about the reduction in the number of new cancer cases, as the country saw a 24% drop in the number of new cases entering the cancer pathway, noting that it is not clear yet whether this reflects an actual decline in the number of cases or if the decline is caused by delayed reporting.
Overall, health systems faced a delicate balance of managing COVID-19 cases and maintaining essential services. Many countries expect to operate at lower capacity for routinely provided care, which will impact patient access and waiting times. For example, to protect patients from unnecessary contacts, health care providers used strategies such as reducing the number of people in waiting rooms, but this affected the number of patients a provider could see. The key strategies observed from the HSRM are summarized in Table 3 , with several country examples.
Table 3.
Common approaches used to maintain essential services with country examples.
| Approach | Country examples |
|---|---|
| Separate (confirmed and suspected) COVID-19 and non-COVID-19 patients |
|
| Increase the use of virtual treatments and digital services |
|
| Reduce capacity of waiting areas |
|
| Prioritize treatments |
|
| Provide staff with increased testing |
|
| Use private sector capacity |
|
4. Discussion
The provision of services is arguably the most visible health system function. In every country, the public primarily interacts with the health system through the delivery of care, from doctor's offices and hospitals to care provided at home, with provided services ranging from routine vaccinations to treatment of complex and rare diseases. While the pandemic has highlighted the visibility of other health system functions, in particular the public health measures necessary to prevent transmission of communicable diseases, COVID-19 has had unprecedented impacts on the provision of care.
While not the focus of this article, the initial starting point of each health system should not be understated. Health care provision varies widely across the countries studied in the HSRM, including the balance between primary and hospital care, the health workforce, and pre-existing digital tools. Some countries went into the pandemic with a relative advantage in certain areas, which both facilitated the country's initial response and eases their transition to resuming routine care. Pre-existing pandemic plans also may have contributed to the response, although all of these early advantages hinged on the governance and leadership within a particular country in how the COVID-19 response developed.
Several countries emphasized the role of the hospital in planning the response to COVID-19, but there are growing concerns about this approach. The focus on hospitals may create blind spots in the management of COVID-19 in other areas of care provision, including smaller hospitals, outpatient clinics, and long-term care facilities. Indeed, many countries experienced larger outbreaks in these settings without the accompanying support of personal protective equipment (PPE) and sufficient physical infrastructure and workforce needed to provide care; up to 47% of all COVID-19-related deaths have occurred among care home residents based on data as of June 2020 from 26 countries [3]. Additionally, the role of primary care providers in treating cases became more critical, but they may not have been supplied with the resources needed to provide the level of care required.
Some countries, such as Poland and Hungary, which initially saw low numbers of COVID-19 cases, underutilized the capacity set aside for treatment of COVID-19. During this time, however, little was known about the disease and how it would develop within the countries. Nevertheless, the decisions to dedicate capacity to COVID-19 not only affected the ability to provide care to non-COVID-19 patients, but also the capacity for specialized health professionals to conduct their training, as many were instead recruited to treat COVID-19 patients [22].
In terms of managing cases, many countries introduced new care pathways and mechanisms for patient triage and evolved their approach over time after more became known about the disease. Telephone hotlines, including new numbers specific to COVID-19 questions, were a particularly common approach due to the need of maintaining distance to reduce potential infections. However, the staffing of these lines is important. If the lines provide medical advice, they should be staffed by medical personnel, which calls into question whether there are appropriately trained personnel for this, who are also not urgently needed elsewhere. Additionally, having separately designated lines for COVID-19 reduces burden on normally operating emergency lines, but it may lead to confusion of the public if it is unclear where to seek advice.
Maintaining essential services while continuing to provide capacity to treat COVID-19 patients is perhaps the largest challenge facing health care providers during this pandemic. A survey of the WHO European Region found high levels of disruption in rehabilitation services and dental care (for both, 91% of surveyed countries indicated disruptions), non-communicable diseases diagnosis and treatment (76%), family planning and contraception (74%), and outreach services for routine immunizations (63%) [6]. Furthermore, nearly a fifth of countries reported a complete disruption of routine outreach for immunization and rehabilitation services. This is almost certainly related to the fact that these services are often conducted by the same personnel that are responsible for surveillance of COVID-19. Additionally, there are some indications that patients hesitate to contact emergency services for symptoms such as pain in the chest, if they perceive that the emergency department is treating COVID-19 patients and/or they fear contracting COVID-19 in the hospital [10], which could be linked to the reduced number of acute health events seen in some countries. While the cancellation or postponement of services in the initial months of the pandemic may have reduced unnecessary treatments or minimized induced health system demand, many patients are likely to have increased unmet needs for health care.
With many countries continuing to offer reduced services, the public may have to accept longer waiting times. This has already been observed in some countries including England, where in March 2020 3,097 patients were waiting more than 52 weeks for treatment, which exploded to 139,545 patients at the end of September 2020 [9]. While NHS England contracted with private sector providers to help alleviate this burden, different approaches to waiting list management and prioritization are likely to be essential to complement these initial efforts. It is important to note that not all countries have centralized datasets or routinely reported figures similar to that of the NHS, so the impact of the various measures taken—including reserving bed and/or ICU capacity, cancelling or postponing treatments—is not yet known.
A near-universal trend seen across the countries in the HSRM is an expansion in provision of virtual care, as it provides no risk of coronavirus transmission. Particularly for services such as prescription renewals and sick leave certificates, these options provide continuity of care with relatively low risk. However, it is not yet clear how the care-seeking behavior of patients may change and how the quality of care compares to care provided in-person, for example with mental health services. Furthermore, not all patients have access to video conferencing and other remote tools, which may lead to digital exclusion and inequitable care provision. Initial studies suggest that staff workload from remote consultations could increase by 25%, unless clinicians shorten consultation times, which has troubling implications for a workforce that is already stretched thin [19]. These impacts of the switch to remotely provided care require further evaluation and research.
At the time of writing, more is becoming understood about the disease, including the long-term implications, which has been referred to ‘long Covid’ or ‘long-haul Covid’ [2]. While some countries, including Ireland and the UK (England), have developed strategies for long Covid that acknowledge the chronic conditions accompanying some patients with the disease and provide some level of support, the larger impact to both health outcomes and health symptoms is not yet known.
While this article describes the adaptations countries have taken in planning services, managing COVID-19 cases, and maintaining essential services, the extent to which these will become permanent features of the health system is not yet known. Some specific measures, for example physically separating patient pathways to reduce transmission, may disappear while others, such as virtual consultations, may continue. Reflections on the permanence of health system changes can begin when the COVID-19 pandemic becomes a less acute feature in the provision of health care.
5. Conclusion
In the first wave, health systems included in the HSRM took varying measures in planning services for COVID-19 patients, managing cases, and maintaining essential services for all other conditions. While the implications of these measures are not yet fully clear, some experiences should be considered for future waves. Moreover, the COVID-19 pandemic has exposed areas where policymakers should focus future policy consideration and development.
First, guidelines on how to prioritize routine care with various COVID-19 scenarios provides essential clarity for health care providers in a rapidly changing epidemiological context. Ideally, the development of these guidelines would involve medical professionals, patient groups, and other stakeholders. Once these guidelines are available, they should adapt based on scientific findings rather than political considerations. A hybrid model, of maintaining routine procedures as far as possible, while also treating COVID-19 patients, is needed, but further definition of these parameters within the country and epidemiological context is required to operationalize this.
Second, the strategy already implemented in many countries to create specific COVID-19 care zones, for example by using separate buildings, having dedicated rooms for COVID-19 patients, or specific treatment times, should be maintained throughout the pandemic. While this places extreme burden on health systems and patients requiring non-COVID-19 care, it provides the only option for preventing the spread of the disease.
Third, providers and policymakers should consider the wider effects of using digital tools on patient access. While remote consultations offer certain advantages, they do not necessarily provide the same quality of care and require patients to adapt their care seeking behaviors. Furthermore, when relying on digital tools, policymakers must ensure that they are supported through reimbursements to health care providers, necessary infrastructure, training, and more.
Last, the pandemic has proven that it requires a whole system response, beyond the borders of hospital walls, the health system, and even countries. Going forward, the pandemic should be viewed as a whole system response, keeping in mind the transitions between treatment areas and balance between different care settings. This includes considerations such as avoiding overburdening GPs, avoiding over-reliance on hospitals, and care transitions for example between hospitals and long-term care facilities. The balance between care settings will also become crucial in the context of distributing COVID-19 vaccines, and requires consideration and planning from policymakers. Historically, strong boundaries around the provision of care exist between sectors and countries, and if COVID-19 teaches us one thing, a pandemic breaks these barriers down.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
We declare no competing interests.
Footnotes
Open Access for this article is made possible by a collaboration between Health Policy and The European Observatory on Health Systems and Policies.
References
- 1.Azoulay E., de Waele J., Ferrer R., et al. International variation in the management of severe COVID-19 patients. Crit Care. 2020;24:486. doi: 10.1186/s13054-020-03194-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Callard F., Perego E. How and why patients made Long COVID. Soc Sci Med. 2021;268:113426. doi: 10.1016/j.socscimed.2020.113426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Comas-Herrera A., Zalakaín J., Litwin C., et al. CPECLSE; 2020. Mortality associated with COVID-19 outbreaks in care homes: early international evidence. LTCcovid.org, International Long-Term Care Policy Network.https://ltccovid.org/wp-content/uploads/2020/06/Mortality-associatedwith-COVID-among-people-who-use-long-term-care26-June.pdf 26 June 2020. Available at. [Google Scholar]
- 4.Eurostat . 2020. Self-reported consultations of a medical professional by sex, age and degree of urbanisation.https://ec.europa.eu/eurostat/databrowser/view/hlth_ehis_am2u/default/table?lang=en Available at. [Google Scholar]
- 5.Eurostat . 2020. Hospital discharges by diagnosis, in-patients, per 100 000 inhabitants.https://ec.europa.eu/eurostat/databrowser/view/hlth_co_disch2/default/table?lang=en Available at: [Google Scholar]
- 6.Jakab M., et al. Managing health systems on a seesaw: balancing the delivery of essential health services whilst responding to COVID-19. Eurohealth 2020. 2020;26 [Google Scholar]
- 7.LSM.LV (2020). “Tālrunis pieteikumiem par Covid-19 analīzēm –8303” [phone for applications for COVID-19 analysis –8303 ]. 13 March 2020. Available at: https://www.lsm.lv/raksts/zinas/latvija/talrunis-pieteikumiempar-covid-19-analizem-8303.a352236/.
- 8.Ministry of Health. Programa Nacional para a Saúde Mental. National Mental Health Program. 2020 https://saudemental.covid19.min-saude.pt/ Available at. [Google Scholar]
- 9.NHS (2020). Statistical press notice: NHS referral to treatment (RTT) waiting times data March 2020. 14 May 2020. Available at: https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2020/05/Mar20-RTT-SPN-publication-version.pdf.
- 10.NOS (2020). “'Spoed is spoed: denk niet ze zijn vast te druk'” [‘'Speed is speed: don't think they are too busy"]. 28 March 2020. Available at: https://nos.nl/collectie/13838/artikel/2328656-spoed-is-spoed-denk-niet-ze-zijn-vast-te-druk.
- 11.Phua J., et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8:506–517. doi: 10.1016/S2213-2600(20)30161-2. 2020Published Online April 6, 2020 https://doi.org/10.1016/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reed S. Nuffield Trust; 2020. Resuming health services during the COVID-19 pandemic: what can the NHS learn from other countries? July 2020. [Google Scholar]
- 13.Tobaiqy M., et al. Therapeutic management of patients with COVID-19: a systematic review. Infect Prev Pract. 2020;2(3) doi: 10.1016/j.infpip.2020.100061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsang T., et al. Effect of changing case definitions for COVID-19 on the epidemic curve and transmission parameters in mainland China: a modelling study. Lancet Public Health. 2020;5(5):e289–e296. doi: 10.1016/S2468-2667(20)30089-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rajan S., et al. What have European countries done to prevent the spread of COVID-19? Lessons from the COVID-19 health system response monitor. Health Policy. 2021 doi: 10.1016/j.healthpol.2022.03.005. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rechel B., Maresso A., van Ginneken E. Health systems in transition: Template for Authors. World Health Organization (acting as the host for, and secretariat of, the European Observatory on Health Systems and Policies); Copenhagen, Denmark: 2019. [Google Scholar]
- 17.Robert Koch Institut (2020). “COVID-19-Verdacht: Testkriterien und Maßnahmen [COVID-19 suspicion: test criteria and measures]. Available at: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Massnahmen_Verdachtsfall_Infografik_DINA3.pdf?__blob=publicationFile.
- 19.Salisbury C., Murphy M., Duncan P. The impact of digital-first consultations on workload in general practice: modeling study. J Med Internet Res 2020. 2020;22(6):e18203. doi: 10.2196/18203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO (2020). Mental health & COVID-19. Available at: https://www.who.int/teams/mental-health-and-substance-use/covid-19.
- 21.Winkelmann J., et al. Countries responses in ensuring sufficient physical infrastructure and workforce capacity during the first COVID-19 wave. Health Policy. 2021 doi: 10.1016/j.healthpol.2021.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams G., et al. What strategies are countries using to expand health workforce surge capacity during the COVID-19 pandemic? 2nd ed. Eurohealth. 2020;26 [Google Scholar]
- 23.Richardson E., et al. Keeping what works: Remote consultations during the COVID-19 pandemic. Eurohealth. 2020;26(2):73–76. [Google Scholar]