Abstract
The “double barrel” technique has been a popular option in reconstituting the iliac-caval confluence in bilateral stenting. It has been mostly used with the Wallstent (Boston Scientific, Marlborough, Mass). The technique, although generally trouble-free, has a unique long-term complication. One stent barrel was found to compress the other from a late developing compliance mismatch. The complication is easily missed unless an intravascular ultrasound examination is performed. A cross-fenestration between the two barrels supported by a Z stent might provide clinical relief if the double barrel extension into the vena cava is relatively short in length.
Keywords: Iliac vein stent, stent compression, Z-stent fenestration, double barrel technique
The Wallstent (Boston Scientific, Marlborough, Mass) has been the mainstay in iliac-caval stenting until recently when a new generation of venous-specific stents were introduced. The Wallstent has enjoyed excellent long-term patency (>90%) in treating iliac-caval disease.1 However, ∼25% of limbs will require reintervention to correct nonthrombotic issues and improve stent functionality.2 The issue could be located at the inflow tract (new or missed stenosis), in the body of the stent itself (usually in-stent restenosis), or at the outflow tract in the inferior vena cava. Managing the iliac confluence is a potential problem area when simultaneous or staged bilateral iliac-caval stenting is required. In a previous report in 2010, we compared three different techniques of managing the iliac-caval confluence in bilateral stenting in our practice: (1) end to side apposition; (2) an end to side unsupported joint through a balloon-created fenestrum; and (3) a 3-cm extension of the Wallstents from both sides into the inferior vena cava to create a “double barrel” configuration.3 The double barrel technique appeared to be the best choice, with a significantly fewer number of reinterventions required to maintain stent functionality at a median follow-up of 12 months (range, 1-108 months). Although this favorable experience with the technique has generally prevailed in the subsequent decade, a unique late complication was noted in 8 of the 66 double barrel subset (12%) followed up. One of the stent barrels was found to have compressed the other, causing new outflow stenosis. We have described this complication and the technique we used to correct it. Updated long-term follow-up data for the double barrel cohort are also provided.
Methods
Patients
A total of 66 patients had undergone bilateral iliac vein stenting (from 2000 to 2016) using the double barrel technique of stent extension into the inferior vena cava. Bilateral stenting was performed simultaneously in 64 patients and was staged in 2 patients, both of the latter at outside hospitals.
Compression of one barrel
Of the 66 patients, 8, including the 2 patients in whom a second barrel had been added late, had presented with a recurrence of their symptoms. The median time of onset was 54 months (range, 11-117 months) after the original stenting. The stents were patent on duplex ultrasound examination, and the venography findings were unremarkable (Fig 1, A). The intravascular ultrasound (IVUS) findings were diagnostic of compression of one of the barrels by the opposite member (Fig 1, B).
Fig 1.
A, Double barrel stent deployment with compression of the left barrel. The compression was not apparent using bilateral venography. B, Intravascular ultrasound (IVUS) image of barrel compression. The larger barrel (Top) was 12 mm in diameter, and the compressed barrel (Bottom), 7 mm in diameter. The IVUS catheter was in the left-sided stent barrel.
Cross-fenestration technique
Access to the compressed barrel was obtained through the ipsilateral femoral vein (11F Pinnacle sheath; Terumo Interventional Systems, Tokyo, Japan) under ultrasound guidance. A 32/100 GLIDEWIRE (Terumo Interventional Systems) was used for IVUS diagnostics and other maneuvers. The GLIDEWIRE was maneuvered across the stents to the uncompressed barrel with appropriate catheter support. Passage can be difficult even with a thinner caliber guidewire if the Wallstent (Boston Scientific) has become fully encased in a tissue cover. The use of a Colapinto needle (Cook Medical Inc, Bloomington, Ind) might be necessary for the crossing (Fig 2, A). Once crossed, the putative fenestrum can be ballooned to size in a single stage with an 18F or 20F high-pressure (>14 atm) Atlas balloon (C.R. Bard, Tempe, Ariz). Predilatation with a dilator, a small caliber balloon, or the use of the “body floss” technique with bilateral femoral access could occasionally be necessary. The fenestrum should be supported by a Z stent to keep it open without recoil (Fig 2, B and C). Buckling or waisting of one or both of the barrels can occur at the upper or lower border of the fenestrum during creation and should be corrected by ballooning, followed by Z stent application, if needed. A completion IVUS examination was performed to ensure satisfactory caliber restoration of both barrels without irregularities. Finally, the anticoagulation and surveillance protocols for the procedure were the standard used for regular stenting.
Fig 2.
A, Needle puncture across the barrels using a Colapinto needle (Cook Medical Inc). The use of the needle within the double barrel stack carries little risk of arterial or other serious injury. B, Balloon dilatation of a putative fenestrum across the two barrels. C, Z-stent deployment supporting the fenestrum (see text for details).
Statistical analysis
The data were extracted from contemporaneously entered electronic medical records. Kaplan-Meier curves were used to determine stent patency and clinical improvement in swelling and pain. All analyses were performed using commercial software (Prism Corp, Irvine, Calif).
Permissions
All the patients provided written informed consent for the procedures. Our institutional review board approved the study and our report.
Results
The demographic data of the entire double barrel cohort and that of the barrel compression subset were similar (Table). Of the eight patients, five had had CEAP (clinical, etiologic, anatomic, pathophysiologic) clinical class 4 and three had had CEAP clinical class 3.
All eight patients with barrel compression had presented with a gradual onset of various combinations of swelling, pain, and tightness of the affected limb that affected their daily activities. All eight patients had experienced good or moderate relief of original symptoms after initial stenting. Swelling was dominant (grade 3) in six of eight patients, and pain was dominant in two patients (visual analog scale for pain score, 6 of 10 and 9 of 10, respectively) with grade 1 swelling. A good relief of symptoms was obtained after cross fenestration in three patients (no pain or swelling), moderate improvement in two patients (mild residual pain and swelling), and no improvement in three patients. The three patients who had been temporarily disabled were able to resume work on their feet.
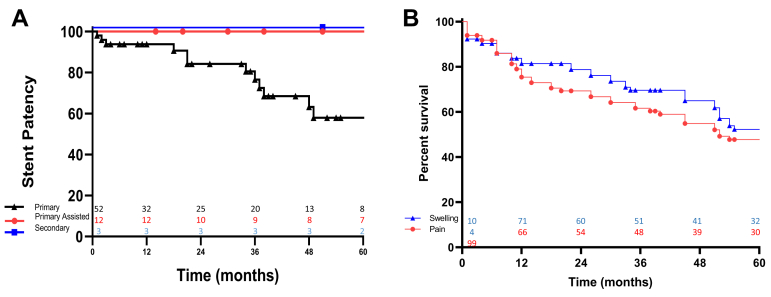
The remaining 58 patients with the double barrel configuration have been followed up for a median of 35 months (range, 1-199 months). The primary, assisted primary, and secondary patency (cumulative) in the group at 5 years was 58%, 86%, and 100%, respectively (Fig 3, A). Repeat intervention balloon dilatation to clear in-stent restenosis was required in 11 patients. The cumulative improvement (Kaplan-Meier curve) in swelling (≥1 grade) and visual analog scale for pain score (≥4 of 10) at 60 months after original stenting was 52% and 48%, respectively (Fig 3, B).
Fig 3.
A, Primary, primary-assisted, and secondary patency of bilateral stenting using the double barrel technique. Primary-assisted patency was defined as patency after reintervention to correct in-stent restenosis in 11 patients and barrel compression in 6 patients. The patency curves were determined by the number of patients, not the number of limbs. No unilateral stent occlusions had developed. B, Kaplan-Meier curves of symptom-free survival in limbs after the double barrel technique of stenting. The survival curve included limbs with improvement of at least one grade in swelling (grade 0, none; grade 1, pitting; grade 2, ankle edema; grade 3, gross swelling) after the stenting procedure. Pain relief was defined as improvement of ≥4 of 10 in the visual analog scale for pain score after stenting.
Discussion
The Wallstent (Boston Scientific) tends to lose its porosity over time owing to pseudo-endothelialization.4 This finding will not be visible on IVUS scanning. Barrel compression might be visible on computed tomography (not used in the present study). The loss of stent porosity will worsen the effects of the compressive stenosis by eliminating outflow sideways through the mesh. Barrel compression is associated with an exponentially greater resistance inversely related to the radius (Poiseuille's law). It appears that one of the barrels becomes stiffer owing to the greater accretion of tissue and, thus, compresses the more compliant barrel. We found no predilection for the left vs right side for barrel compression (Table). Delayed contralateral stenting might predispose to barrel compression owing to a compliance mismatch. Two such patients who had undergone stenting elsewhere were included in the present series.
Table.
Demographic data (n = 66)
| Variable | Double barrel (n = 58) | Barrel compression (n = 8) |
|---|---|---|
| Mean age, years | 59 | 58 |
| Sex, no. | ||
| Male | 1 | 1 |
| Female | 2 | 1 |
| Compressed barrel, no. | 0 | 8 |
| Right | 4 | |
| Left | 2 | |
| Bilateral | 2 | |
| Nonthrombotic, no. (%) | 24 (41) | 3 (38) |
| Post-thrombotic, no. (%) | 22 (38) | 3 (38) |
The double barrel is a satisfactory technique if performed properly. The usual minimal size of each iliac vein stent will be ≥16 mm in most cases.5 Therefore, the inferior vena cava should be dilated by kissing balloons to accommodate the double barrel without compression at the outset. The length of the double barrel should be as short (≤3 cm) as possible. The use of long double barrels will add to flow resistance in linear fashion (Poiseuille's equation). If compression were to develop, short double barrels can be easily corrected by placement of a Z stent to the top of both barrels. Reexpansion of the compressed barrel using a unilateral Z stent runs the risk of new compression of the contralateral unsupported Wallstent. In addition, the compression of long double barrels might not be as easily correctible using a single cross fenestration because a narrow segment will persist below the fenestrum. Some of the poor results in the present series might be related to this problem. Multiple fenestra might be required for effective decompression of long double barrels. The double barrel is not an appropriate technique for delayed contralateral stenting. An end to side fenestrum junction between the new and old stent supported by a Z stent would be a better option.6 The routine use of the Z stent to buttress the upper end of the Wallstent in unilateral stenting has significantly decreased the incidence of both contralateral and ipsilateral deep vein thrombosis with improved long-term patency.7,8 The technique will also result in significant clinical improvement in the contralateral limb, presumably because of off-loading of collateral vessels.9 This suggests that simultaneous bilateral stenting should be avoided. Contralateral stenting should be staged only when the opposite limb has failed to improve or the symptoms have worsened. The performance of the newer venous-specific stents in terms of barrel compression is unknown.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Raju S. Best management options for chronic iliac vein stenosis and occlusion. J Vasc Surg. 2013;57:1163–1169. doi: 10.1016/j.jvs.2012.11.084. [DOI] [PubMed] [Google Scholar]
- 2.Raju S., Tackett P., Jr., Neglen P. Reinterventions for nonocclusive iliofemoral venous stent malfunctions. J Vasc Surg. 2009;49:511–518. doi: 10.1016/j.jvs.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Neglen P., Darcey R., Olivier J., Raju S. Bilateral stenting at the iliocaval confluence. J Vasc Surg. 2010;51:1457–1466. doi: 10.1016/j.jvs.2010.01.056. [DOI] [PubMed] [Google Scholar]
- 4.Gloviczki P., Lawrence P.F. Iliac vein stenting and contralateral deep vein thrombosis. J Vasc Surg Venous Lymphat Disord. 2017;5:5–6. doi: 10.1016/j.jvsv.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Raju S., Buck W.J., Crim W., Jayaraj A. Optimal sizing of iliac vein stents. Phlebology. 2018;33:451–457. doi: 10.1177/0268355517718763. [DOI] [PubMed] [Google Scholar]
- 6.Raju S., Ward M., Jr., Kirk O. A modification of iliac vein stent technique. Ann Vasc Surg. 2014;28:1485–1492. doi: 10.1016/j.avsg.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 7.Murphy E.H., Johns B., Varney E., Buck W., Jayaraj A., Raju S. Deep venous thrombosis associated with caval extension of iliac stents. J Vasc Surg Venous Lymphat Disord. 2017;5:8–17. doi: 10.1016/j.jvsv.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Jayaraj A., Noel C., Kuykendall R., Raju S. Long term outcomes following use of a composite Wallstent-Z stent approach to iliofemoral venous stenting. J Vasc Surg Venous Lymphat Disord. 2020 Aug 20 doi: 10.1016/j.jvsv.2020.08.020. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Jayaraj A., Noel C., Raju S. Contralateral limb improvement after unilateral iliac vein stenting argues against simultaneous bilateral stenting. J Vasc Surg Venous Lymphat Disord. 2020;8:565–571. doi: 10.1016/j.jvsv.2020.03.010. [DOI] [PubMed] [Google Scholar]