Abstract
Background:
Infection Prevention and Control (IPC) practices have been established in home health care. Adherence to IPC practices has been suboptimal with limited available evidence. The study aim was to examine the impact of individual, home environment, and organizational factors on IPC practices using human factors model.
Methods:
Three hundred and fifty-three nurses were surveyed across two large home care agencies to examine the relationship between IPC adherence and individual, home environment, and organizational factors.
Results:
Nurses reported multiple barriers to IPC practices in patients’ homes (mean = 4.34, standard deviation = 2.53). Frequent barriers included clutter (reported by 74.5% of nurses) and a dirty environment (70.3%). Nurses also reported limited availability of some IPC supplies (mean = 7.76, standard deviation = 2.44), including personal protective equipment. Home environment factors were significant barriers, and availability of IPC supplies were significant enablers of IPC adherence. Agency-provided training and decision-making resources were not significant factors for IPC adherence in the presence of home environment barriers and IPC supplies.
Conclusions:
This study findings suggest that IPC adherence strategies point to addressing barriers in the home environment and increasing availability of IPC supplies. The relationship between the patient’s home environment, organizational factors, and IPC practices among home health care nurses warrants further study.
Keywords: Infection prevention and control, Home health care, Compliance
A growing number of older Americans with complex medical needs rely on home healthcare (HHC) services to age in place.1 HHC providers make home visits to deliver skilled nursing, rehabilitation, personal care, and social work services to patients who are not able to leave homes without assistance.2,3 Earlier hospital discharges, delivery of increasingly complex procedures outside of the hospital settings, and preferences of older adults to live at home as long as possible have contributed to the expansion of HHC services.3 From 2002 to 2018 the number of HHC users has increased by 35%, and in 2018, 3.4 million people were visited by HHC providers from 11,556 agencies.2 Increased use of HHC services has brought attention to patient safety measured by hospitalizations and emergency care use while receiving HHC services.2 Infections represent a serious threat to patient safety, causing 17% of unplanned hospitalizations.4 Although standards to prevent transmission of pathogens between patients and providers have been established,5,6 adherence to these standards was reported as suboptimal.8,9 Infection prevention has remained a priority patient safety goal in national health care settings,7 underscored by the recent COVID-19 outbreak.10 As human factors models have been increasingly applied to Infection Prevention and Control (IPC) strategies in the inpatient settings,11 only a few studies have applied these models to explorations of IPC practices in HHC settings.3 In an observation study followed by qualitative interviews with HHC nurses, researchers found that the unique role of home environment in regard to perceived patient infection risk was associated with nurses’ ability to carry out hand hygiene practices.9,12 A survey of HHC nurses identified that their knowledge of infection control practices was not associated with adherence, rather adherence was predicted by advanced certification in infection control, HHC work experience, and attitudes concordant with IPC practices.13 Another survey conducted in North Carolina reported nurses’ use of personal protective equipment was limited by its availability and conditions in home environment.14 Finally, in an Australian study, researchers found organizational resources, availability of supplies, home environment, and patients’ personal hygiene were associated with IPC practices of home care nurses.8 While each study examined individual, environmental, and organizational factors individually, primarily focusing on barriers in home environment, none of them examined all factors together. To address this gap, the aim of this study was to examine the impact of individual, home environment, and organizational factors on IPC adherence. We hypothesized that nurses reporting more barriers in patients’ homes were less likely to adhere to IPC practices; and that nurses reporting using more enabling organizational resources were more likely to adhere to IPC practices.
METHODS
An anonymous online survey was administered to nurses employed in two large Medicare-certified HHC agencies in the northeastern U.S. between April and August 2017. Registered or licensed practical nurses who were actively providing or managing direct patient care were eligible to take the survey. All study procedures had prior approval of the Institutional Review Board of Columbia University School of Nursing and both HHC agencies. Survey administration methods have been fully described elsewhere.13
Our selection and analysis of variables was guided by the Model of Human Factors of Health Care in the Home, based on the systems engineering approach increasingly applied in IPC research.3,11 The model examines characteristics of the 3 system components, (1) persons, (2) tasks, and (3) equipment or technology, interacting within the environments that may place barriers and enablers to system’s processes.3,11 The model was adapted to examine enablers and barriers in individual, home, and organizational environments relevant to the implementation of the IPC practices measured by adherence (Fig 1).
Fig 1.
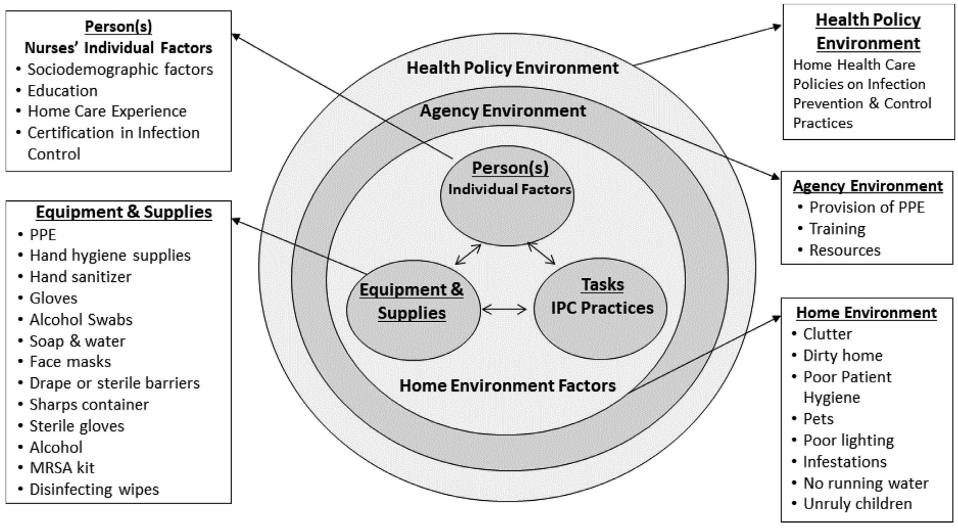
Conceptual Model of adherence to IPC practices in home health care.
IPC adherence
Adherence to IPC practices was assessed by 8 items adapted from existing instruments and agency policies and procedures.13,16 Examples of these items included performing hand hygiene (eg, I perform hand hygiene before and after patient care activities), using personal protective equipment appropriately (eg, I wear gloves when I am exposed to body fluids), practicing safe injection practices (eg, I dispose of needles in a sharps container), and disposing of waste appropriately (I dispose of all potentially contaminated materials into an impermeable bag). The responses were coded as adherent for the answer options “always” and “often,” and nonadherent, for the answer options “sometimes,” “rarely,” or “never.”13,16 A summary score measuring IPC adherence captured the proportion of items with self-reported adherence, ranging from 0 (nonadherence to any of the IPC practices) to 1 (adherence to all IPC practices).
Individual factors captured were nurses’ age, sex, race or ethnicity, nursing education level, years of HHC experience, and formal certification in infection control.
Home environment barriers were measured using a list of 8 barriers, which nurses rated the frequency that these barriers interfered with their ability to perform IPC practices (Fig 2). The list was developed based on a literature review and item selection was guided by the human factors model of items related to nurses’ ability to perform IPC practices. The barriers included poor lighting, clutter, infestations, unrestrained pets, absence of running water, unruly children, dirty environment, and poor patient hygiene.3,12,14,16-18,20-21 Each barrier was dichotomized as “present,” for the selected responses of “sometimes,” “often,” and “always”; or “absent,” for the responses of “rarely” and “never.”
Fig 2.
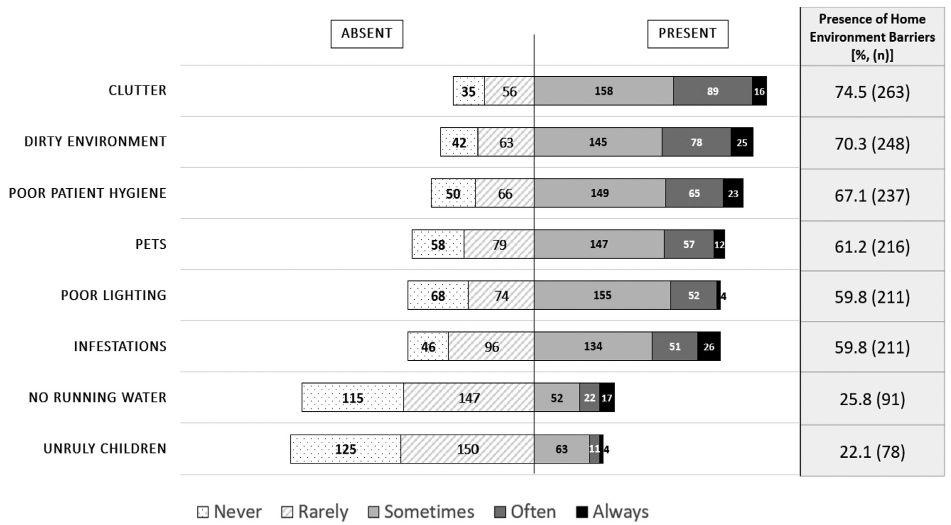
Frequency of home environment barriers encountered by nurses in patients’ homes (n = 353)*.
* NOTE: Barriers present in home environment were coded as responses of “always,” “often,” or “sometimes.”
Organizational factors were measured by 3 agency-provided resources that are directly related to IPC practice; IPC supplies, training, and resources for infection control decision-making. IPC training item assessed the timeframe of the last training the providers received, ranging from never to within the past 2 weeks. Responses were categorized as within 6 months, between 6 and 12 months, or over a year ago. The availability of IPC supplies was measured by the frequency with which nurses reported the supplies were available to them during home visits. The list of 13 supplies was selected based on agency policies and procedures and included soap, alcohol-based hand sanitizer, nonalcohol-based hand sanitizer, sharps container, Methicillin Resistant Staphylococcus Aureus supplies kit to use for patients diagnosed with Methicillin Resistant Staphylococcus Aureus, alcohol swabs, alcohol, face shields, face masks, sterile barriers, non-sterile gloves, sterile gloves, and chlorhexidine disinfectant wipes. Each supply was dichotomized as “available,” for the supplies reported available “always,” “often” and “sometimes,” and “absent,” for the supplies reported available “rarely” and “never.” A composite measure was created ranging from 0 to 13 summing the number of available IPC supplies, with low values indicating that there is usually a limited amount of supplies available for the home visit, and high values indicating the greater number of supplies usually available. Organizational resources use was measured using a list of 7 resources; policies and procedures, clinical practice guidelines, textbooks, scientific journals, electronic clinical decision support, professional consult, organizational websites, along with an option to enter the resources not listed. These resources were coded as either used or not used. A composite measure of the number of resources used was included in our analysis.
Data analysis
Bivariate statistics were used to summarize sociodemographic characteristics, availability IPC of supplies, use of organizational resources, and IPC adherence. A multivariable linear regression model was estimated to examine variation in IPC adherence as the dependent variable. Nurses’ individual factors, home environment factors, availability of IPC supplies, organizational IPC training, and organizational resources were included as independent variables. Statistical significance was set at an alpha level of <0.05. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
From the 1,134 administered surveys, 415 responses were returned (response rate, 36.6%). After excluding partial responses, the final analytic sample included 353 surveys, with 206 surveys from Agency 1 and 147 surveys from Agency 2.
Individual factors
Table 1 summarizes the individual characteristics of home health care nurses. Nurses were predominantly women (92.6%), aged over 40 years (mean age = 50, [standard deviation; SD] = 10.62), non-Hispanic white (43.9%) or black (23.2%). Most nurses were educated with bachelor’s (52.1%) or graduate (20.4%) degrees and were experienced in home care (mean years of home care experience = 13.6, [SD] = 9.4). A small proportion of nurses reported receiving specialized infection control certification (17.9%). Nurses reported high level of adherence to all 8 IPC practices (mean adherence score=0.88, [SD] = 0.16), ranging between 68.8% for wearing eye protection to 100% for wearing gloves when indicated.
Table 1.
Individual characteristics of nurses (n = 353)
| Characteristics | n (%) or mean (SD) |
|---|---|
| Age | 50.0 (10.62) |
| Sex | |
| Male | 26 (7.4) |
| Female | 327 (92.6) |
| Race/Ethnicity | |
| Non-Hispanic White | 155 (43.9) |
| Non-Hispanic Black | 82 (23.2) |
| Hispanic | 39 (11.1) |
| Other or mixed race/ethnicity | 77 (21.8) |
| Education | |
| Associate’s degree or some college | 97 (27.5) |
| Bachelor’s degree | 184 (52.1) |
| Graduate degree | 72 (20.4) |
| Years in home care nursing | 13.6 (9.4) |
| Certification in infection control | |
| Received certification | 63 (17.9) |
| Has not received certification | 290 (82.2) |
| Surveyed agency | |
| Agency 1 | 206 (58.4) |
| Agency 2 | 147 (41.6) |
| IPC adherence score (0-1) | 0.88 (0.16) |
SD, standard deviation.
Home environment barriers
Figure 2 illustrates the frequency of home environment barriers to IPC practices. Most nurses encountered multiple barriers to IPC practices in patients’ homes (mean number of barriers = 4.34, [SD] = 2.53) with 88.82% nurses encountering at least one barrier and 58.36% of nurses encountering 5-8 barriers. The most frequently reported barriers included clutter (74.5%) and a dirty environment (70.3%), while the least frequently reported barriers were unruly children (22.1%) and the absence of running water (25.8%).
Organizational factors
Table 2 presents organizational factors, including supplies, training, and decision-making resources related to IPC practices. Commonly available supplies were alcohol-based hand sanitizer (95.2%), soap (86.7%), gloves (94.5%), face masks (78.5%), and then face shields (50.4%). Of the disinfecting supplies, alcohol swabs were reported available by most nurses (91.8%), fewer nurses reported having alcohol solution (39.7%) and chlorhexidine wipes (20.4%). Most respondents (82.4%) reported receiving recent IPC training, with 38.2% of the nurses being trained within last 6 months and 44.2% within the last year. Among decision-making resources, most nurses reported using agency policies and procedures (97.7%), followed by the clinical practice guidelines (88.1%). Lesser used resources included scientific journals (21.3%) and electronic clinical decision support systems (16.4%).
Table 2.
Frequency of organizational resources available during home visits (n = 353)
| Infection prevention and control resources | n (%) |
|---|---|
| Infection prevention and control supplies | |
| Alcohol-based hand sanitizer | 336 (95.2) |
| Gloves | 337 (94.5) |
| Alcohol swabs | 324 (91.8) |
| Soap and water | 306 (86.7) |
| Face masks | 277 (78.5) |
| Drape or sterile barriers | 260 (73.7) |
| Sharps box/container | 182 (51.6) |
| Sterile gloves | 180 (51.0) |
| Alcohol | 140 (39.7) |
| Methicillin Resistant Staphylococcus Aureus (MRSA) supplies kit | 92 (26.1) |
| Nonalcohol-based hand sanitizer | 77 (21.8) |
| Chlorhexidine wipes | 72 (20.4) |
| Last received infection control training | |
| Less than 6 months | 135 (38.2) |
| More than 6 months, less than 1 year | 156 (44.2) |
| More than 1 year | 62 (17.6) |
| Resources used for IPC decision-making | |
| Agency policies and procedures | 345 (97.7) |
| Clinical practice guidelines | 311 (88.1) |
| Professional consult | 128 (36.3) |
| Textbooks | 100 (28.3) |
| Organizational websites | 97 (27.5) |
| Scientific journals | 75 (21.3) |
| Electronic clinical decision support | 58 (16.4) |
| Other resources not listed (eg, internet, personal experience, and infection control leadership) | 14 (4.0) |
Multivariable analyses of IPC adherence: relationships of personal, home environment, and organizational factors
Table 3 presents the results of the regression model of IPC adherence among home care nurses. The only individual factor associated with HHC nurses’ IPC practices was race/ethnicity. We found non-Hispanic Black nurses reported higher adherence to IPC practices than non-Hispanic White nurses (P < .001). Adjusting for other variables, nurses who reported encountering more home environment barriers had significantly (P < .001) lower IPC adherence scores. A one number increase in home environment barriers resulted in 0.10 unit decrease in the IPC adherence score, all other variables held constant.
Table 3.
Multivariable linear regression model of IPC adherence among home health care nurses(n = 353)
| Variable | IPC adherence Model 1: B (SE) |
|---|---|
| Individual factors | |
| Age | 0.013 (0.008) |
| Sex | |
| Men | reference |
| Women | −0.259 (0.244) |
| Race/Ethnicity | |
| Non-Hispanic White | reference |
| Non-Hispanic Black | 0.631 (0.172)*** |
| Hispanic | 0.366 (0.219) |
| Other or mixed race/ethnicity | 0.302 (0.176) |
| Education | |
| Associate’s degree or some college | Reference |
| Bachelor’s degree | 0.08 (0.155) |
| Graduate degree | −0.11 (0.192) |
| Years in home care nursing | 0.004 (0.009) |
| Certification in infection control | |
| Has not received certification | reference |
| Received certification | 0.326 (0.174) |
| Home environment factors | |
| The number of barriers | −0.104 (0.026)*** |
| Organizational factors | |
| Agency 1 | reference |
| Agency 2 | 0.402 (0.151)* |
| The number of available IPC supplies | 0.119 (0.029)*** |
| The number of resources used for IPC decision-making | 0.057 (0.046) |
| Last received IPC training | |
| Less than 6 months | Reference |
| More than 6 months, less than 1 year | −0.08 (0.143) |
| More than 1 year | 0.113 (0.188) |
| R2 | 0.186029 |
B, beta; SE, standard error.
P < .05.
P < .001.
Among organizational factors, only the availability of IPC supplies was significantly (P < .001) and positively associated with IPC adherence. A number increase in the available IPC supplies resulted in 0.12 unit increase in the average IPC adherence score, all other variables held constant. Together, these individual, home environment, and organizational resource factors explained 19% of the variance (R2) in self-reported IPC adherence among HHC nurses.
DISCUSSION
Overall, nurses reported high level of IPC adherence (88%), ranging between 68.8%, for wearing eye protection, to 100%, for wearing gloves when indicated. To our knowledge, this is the first study to investigate HHC nurses’ individual factors, home environment, and IPC practices. Most nurses encountered multiple barriers to IPC practices in patients’ homes. Moreover, the results of our study demonstrate that an increase in the number of home environment barriers was associated with decreased IPC adherence among HHC nurses.
The most commonly reported barriers in patients’ homes, clutter and a dirty home environment, are in line with prior studies linking clutter and unsanitary conditions to observed increase in the number of hand hygiene indications, nurses’ reports of feeling rushed or spending additional time to complete care tasks.8,9,12,15,17-20 Patients with severe conditions and functional deficits may be limited in their abilities to participate in personal and home hygiene activities. A recent study of infection-related hospitalizations in a national sample of HHC patients linked severe medical conditions and impaired physical functioning to increased risk of infection and hospitalization.21 Physical therapy or social work referral may be helpful to the patient. Home environments with numerous barriers may potentially contribute to the risk of adverse events for patients and should be further studied in relation to infection-related hospitalizations or use of emergency care. Since HHC nurses have limited tools at their disposal to address barriers present in the home environment, agencies may seek to involve home health aides in quality improvement strategies as members of interdisciplinary team to assist with managing personal and environmental hygiene. Such strategies may promote patient-centered care and reduce patient’s infection risk.
A quarter of the surveyed nurses (25.8%) reported the absence of running water as an environmental barrier. The absence of running water may present significant safety concerns for patients and caregivers. According to a recent study, HHC patients with unmet caregiver needs are at higher risk for wound-site infections leading to hospitalizations.21 Since training patients and caregivers to independently perform care tasks are part of the HHC plan,7 assessment of barriers in home environment, such as running water should be considered, especially important for patients with wounds and unmet caregiver needs. In our study, unruly children were the least frequent barrier in home environment reported by 22% of nurses. In a prior study of working conditions of home care nurses’ in North Carolina, 78% of nurses reported encountering unruly children in patients’ homes.19 In a randomized clinical trial of interventions on household transmission of respiratory viruses, school-aged children were linked to increased rates of household transmission and significantly protective intervention combined IPC education with the use of hand sanitizer and face masks.22 While our findings are not comparable with the previous report, the role of children in the HHC patients’ households should be explored further, specifically in relation to infection transmission, as both HHC patients and children may be at increased risk for severe infection. During outbreaks, the role of HHC nurses can be leveraged to extend IPC education and supplies to all members of patients’ household, including young children and their parents.
Our survey results suggest that: (1) the availability of IPC supplies in the home varies by the type of supply, and (2) that the number of available IPC supplies is significantly and positively associated with nurses’ IPC adherence. Approximately 78% of nurses reported face masks available to them during home visits. Face masks, indicated for respiratory protection from droplets, splashes, or sprays, are commonly used in the HHC settings.5 Face masks have been highlighted as critical equipment during the recent COVID-19 outbreak, as well as for transmission of other respiratory infections.22-24 Although we did not directly assess the availability of N95 respirator masks among nurses surveyed as part of our study, one recent study has reported a significant shortage of N95 respirator masks among HHC agencies amid the peak of the COVID-19 pandemic.24 Regular assessment of IPC practices for correct use should also improve emergency preparedness of HHC providers, frequently on the front lines of the outbreaks. Including HHC agencies in the local health care strategies for distribution of IPC supplies and training on prevention strategies may be essential to mitigate the risk of community transmission. In our study, neither resources used for IPC decision-making nor time since IPC training were found to be significantly associated with IPC adherence in the presence of home environment barriers. One possible explanation is that most nurses reported using at least one organizational resource and recent IPC training, so there was limited variability in these factors among our survey sample. The most frequently used resources to guide practice was the agency policies and procedures, which was used by almost all the nurses, indicating this resource as the ideal place to incorporate more information on how to assess home environment barriers and provide guidance on mitigation strategies. To complement traditional teaching of policies and procedures, organizations may also benefit from use of emerging adult learning innovations. Gaming simulation is currently being studied as a way to engage learners and may be a useful strategy to improve IPC adherence.25 Our findings of non-Hispanic Black reported higher adherence rates than non-Hispanic White nurses need to be explored in future studies.
This study is an important step to address the knowledge gap in factors for adherence to IPC practices in the home care settings. While causality cannot be established because of the cross-sectional study design, our findings provide preliminary evidence that barriers in home environment and insufficient IPC supplies may directly affect the nurses’ ability to adhere to IPC practices. Since our study identified barriers and enablers of IPC practices among home care nurses prior to COVID-19 pandemic, it will be interesting to test if these practices change over time.
Limitations
The limitations in our study are common to those in surveys. Self-report of adherence is known to be influenced by social desirability bias. However, the focus of the study was identification of relationships between adherence, home environment, organizational, and individual factors. Subsequent observation of the IPC practices, home environment, and supplies available during home visits would verify and supplement the findings. Additionally, the surveys were administered in 2 northeastern US agencies and the findings may not be generalizable to all HHC agencies. We also purposely surveyed nurses as they provide majority of home visits and are responsible for delivering IPC instruction to patients and caregivers. Further research may include other HHC providers.
CONCLUSIONS
Home environment barriers were associated with significantly lower self-report IPC practices. Among organizational factors, availability of IPC supplies were significant enablers of IPC practices, but organizational training and resources were not. These findings point to direction for addressing barriers in home environment and improving access to supplies during home visits for IPC adherence strategies. The relationship between home environment, organizational factors, and IPC practices warrants further study.
Acknowledgments
We would like to thank all the home health care nurses who participated in this study.
Funding source: This project was supported by the Agency for Healthcare Research and Quality (grant number R01HS024723). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Footnotes
Conflicts of interest: None to report.
References
- 1.Ornstein KA, Leff B, Covinsky KE, et al. Epidemiology of the homebound population in the United States. JAMA Inter Med. 2015;175:1180–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medicare Payment Advisory Commission, Report to the Congress: Medicare Payment Policy. (2020). Washington, D.C., March 2020. Available at: http://www.medpac.gov/docs/default-source/reports/mar20_medpac_ch9_sec.pdf?sfvrsn=0. Accessed September 17, 2020. [Google Scholar]
- 3.National Research Council. Health Care Comes Home: The Human Factors. Washington, DC: National Academies Press; 2011. [Google Scholar]
- 4.Shang J, Larson E, Liu J, Stone P. Infection in home health care: results from national outcome and assessment information set data. Am J Infect Control. 2015;43:454–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siegel JD, Rhinehart E, Jackson M, Chiarello L, Health Care Infection Control Practices Advisory Committee. 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35:S65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services (CMS), HHS. Medicare and medicaid program: conditions of participation for Home Health Agencies. Final rule. Fed Regist. 2017;82:4504. [PubMed] [Google Scholar]
- 7.The Joint Commission. National Patient Safety Goals Effective July 2020 for the Home Care Program. Oakbrook Terrace, IL: The Joint Commission on Accreditation of Healthcare Organizations; 2020. [Google Scholar]
- 8.Felembam O, John WS, Shaban RZ. Hand hygiene practices of home visiting community nurses: perceptions, compliance, techniques, and contextual factors of practice using the World Health Organization’s “Five Moments for Hand Hygiene”. Home Healthc Nurse. 2012;30:152–160. [DOI] [PubMed] [Google Scholar]
- 9.McDonald MV, Brickner C, Russell D, et al. Observation of hand hygiene practices in home health care. [e-pub ahead of print]. J Am Med Dir Assoc. 2020. 10.1016/j.jamda.2020.07.031, accessed November 9, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Center for Clinical Standards and Quality/Quality, Safety & Oversight Group Services, Centers for Medicare & Medicaid Services. Guidance for infection control and prevention concerning Coronavirus Disease 2019 (COVID-19) in Home Health Agencies (HHAs), QSO-20-18-HHA. 2020; 1–7. [Google Scholar]
- 11.Katz M, Gurses A. Infection prevention in long-term care: Re-evaluating the system using a human factors engineering approach. Infect Control Hosp Epidemiol. 2019;40:95–99. [DOI] [PubMed] [Google Scholar]
- 12.Dowding D, Russell D, Trifilio M, McDonald MV, Shang J. Home care nurses’ identification of patients at risk of infection and their risk mitigation strategies: a qualitative interview study. Int J Nurs Stud. 2020;107:103617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russell D, Dowding DW, McDonald MV, et al. Factors for compliance with infection control practices in home healthcare: findings from a survey of nurses' knowledge and attitudes toward infection control. Am J Infect Control. 2018;46:1211–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leiss JK, Sitzman KL, Kendra MA. Provision and use of personal protective equipment among home care and hospice nurses in North Carolina. Am J Infect Control. 2011;39:123–128. [DOI] [PubMed] [Google Scholar]
- 15.Felemban O, St John W, Shaban RZ. Infection prevention and control in home nursing: case study of four organisations in Australia. Br J Community Nurs. 2015;20:451–457. [DOI] [PubMed] [Google Scholar]
- 16.Gershon RR, Vlahov D, Felknor SA, et al. Compliance with universal precautions among health care workers at three regional hospitals. Am J Infect Control. 1995;23:225–236. [DOI] [PubMed] [Google Scholar]
- 17.Gershon RR, Pogorzelska M, Qureshi KA, et al. Home health care patients and safety hazards in the home: preliminary findings. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 1: Assessment). Rockville, MD: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- 18.Polivka BJ, Wills CE, Darragh A, Lavender S, Sommerich C, Stredney D. Environmental health and safety hazards experienced by home health care providers: a room-by-room analysis. Workplace Health Saf. 2015;63:512–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sitzman KL, Leiss JK. Documentation of incidental factors affecting the home healthcare work environment. Home Healthcare Now. 2009;27:516–521. [DOI] [PubMed] [Google Scholar]
- 20.Wills CE, Polivka BJ, Darragh A, Lavender S, Sommerich C, Stredney D. “Making Do” decisions: how home healthcare personnel manage their exposure to home hazards. West J Nurs Res. 2016;38:411–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shang J, Wang J, Adams V, Ma C. Risk factors for infection in home health care: analysis of national Outcome and Assessment Information Set data. Res Nurs Health. 2020;43:373–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Larson EL, Ferng YH, Wong-McLoughlin J, Wang S, Haber M, Morse SS. Impact of non-pharmaceutical interventions on URIs and influenza in crowded, urban households. Public Health Rep. 2010;125:178–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8:434–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shang J, Chastain AM, Perera UGE, et al. COVID-19 Preparedness in U.S. Home Health Agencies. J Ame Med Dir Assoc.. 2020;21:924–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Polivka BJ, Anderson S, Lavender SA, et al. Efficacy and usability of a virtual simulation training system for health and safety hazards encountered by healthcare workers. Games Health J. 2019;8:121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]


