Abstract
Background
Stereopsis is a valuable feature of human visual perception which is critically impaired in amblyopia, but can be improved through perceptual learning (PL). This article aims to determine the variables affecting the outcomes and intensity of a stereoacuity stimulation program.
Methods
Re-analysis of a previous study in stereodeficient subjects with a history of amblyopia. Sixteen subjects (12 females, 4 males) aged between 7 and 14 received stereopsis stimulation through a PL program at home. A correlation analysis evaluated whether treatment intensity or percentage improvement were related to age or baseline stereoacuity measurements. Further analysis was performed to assess whether the type of amblyopia conditioned the PL treatment (Fischer Statistical Test).
Results
No significant correlation was found between age and percentage improvement (rho = −0.08, p = 0.749), nor was age correlated with treatment intensity (rho = 0.170, p = 0.544). However, a correlation did exist between baseline stereoacuity levels and treatment intensity (rho = 0.734, p = 0.001). Baseline stereoacuity and percentage improvement had a negative correlation (rho = −0.748, p = 0.005), while treatment intensity showed only a weak association with the type of amblyopia (p = 0.064).
Conclusions
Present results suggest that perceptual learning in stereodeficient subjects is not influenced by either the subject's age or the type of amblyopia. Baseline stereoacuity, on the other hand, seems to be a predicting factor for perceptual learning outcomes. According to our study, subjects with poor basal stereoacuity needed more sessions to improve and their percentage improvement was lower. However, due to the reduced size of the sample, the results should be considered with caution.
Keywords: Amblyopia, Perceptual learning, Age, Baseline stereoacuity level, Computer video game
Introduction
Stereoanomaly is commonly associated with amblyopia1 and can be treated by means of Perceptual Learning. Stereopsis is a valuable feature of human visual perception.2 However, the research studies to improve stereoacuity in stereo-deficient subjects have been sporadic.3, 4, 5, 6 Recently, our research group described an innovative system of direct stimulation of stereopsis through gamified software (Computerized Stereoscopic Game) using random dot stimuli, in stereo-deficient subjects with a history of amblyopia.7 All subjects were treated following a protocol of 60 sessions of perceptual learning exclusively at home. That study concluded that stereoacuity measurements obtained from global stereopsis tests (Randot Preschool Stereoacuity Test) improved significantly with perceptual learning. Other recent studies used training based on games at home have been published.8, 9 In this previous research, the data of each training session stored the results in a database hosted on a remote server. This model of stimulation has several advantages; (I) the training sessions could be made at home without the inconvenience of going to the clinic regularly.10 (II) It is possible to know the real compliance.8, 9 (III) It is possible to know the evolution of each subject, session to session, and then know the exact moment when learning takes place. This last characteristic could allow us to know the doses necessary to achieve improvement in amblyopia. Different authors have studied this issue.11, 12 These studies have analyzed the doses in order to improve visual acuity in amblyopia, but the doses to improve stereoacuity were not analyzed.
Another interesting issue, is knowing if the subjects with refractive amblyopia get more improvement than subjects with strabismic amblyopia and if the subjects with strabismus need more sessions to achieve improvement. A study conducted by Webber et al.13 found that subjects with refractive amblyopia did in fact improve their stereoacuity by means of a dichoptic game. However, this improvement was not observed in the subjects with strabismic amblyopia.
The aim of the current study was to investigate whether or not the age, the basal level of stereopsis or the type of amblyopia were factors influencing the outcome (percentage of improvement) and intensity (the number of sessions required for learning). As far as the authors know, this analysis has yet to be performed.
Methods
This study is based on the outcomes obtained in the experimental group of a previous prospective, double blind and parallel study (Table 1).7 Subject had to work at home (60 prescribed sessions, 8 h, 4800 responses).
Table 1.
Results of the intervention in the 16 experimental group subjects. In the Perceptual Learning (PL) column, those subjects experiencing an improvement are marked as A–K. The measurements are in second arc. Abbreviations: RPST = Randot Preschool Stereo Acuity Test; CSG: Computer Stereogram Game. Previous treatment: VT = visual therapy; CL = contact lens; ES = esotropia surgery.
| n | History of amblyopia | Previous treatments | RPST baseline | RPST post-treatment | CSG baseline | CSG post-treatment | PL |
|---|---|---|---|---|---|---|---|
| 1 | Esotropia | VT/Occlusion/ES | 800 | 200 | 840 | 450 | A |
| 2 | Exotropia | VT/Occlusion | 200 | 100 | 240 | 60 | B |
| 3 | Esotropia | Occlusion | 800 | 800 | 840 | 840 | 01- |
| 4 | Isometropic | VT/Occlusion | 800 | 800 | 840 | 720 | 02- |
| 5 | Esotropia, anisometropic | VT/Occlusion | 800 | 800 | 840 | 720 | 03- |
| 6 | Esotropia | Occlusion/CL | 200 | 100 | 240 | 90 | C |
| 7 | Esotropia | Occlusion | 400 | 400 | 840 | 450 | 04- |
| 8 | Anisometropic | Occlusion/CL | 400 | 200 | 450 | 240 | D |
| 9 | Esotropia, anisometropic | VT/Occlusion | 400 | 100 | 420 | 210 | E |
| 10 | Esotropia | VT/Occlusion | 800 | 800 | 740 | 720 | 05- |
| 11 | Esotropia, anisometropic | VT/Occlusion | 200 | 60 | 240 | 90 | F |
| 12 | Isometropic | VT/Occlusion | 400 | 200 | 180 | 60 | G |
| 13 | Esotropia | VT/Occlusion/ES | 400 | 100 | 420 | 270 | H |
| 14 | Esotropia | VT/Occlusion/ES | 200 | 40 | 180 | 60 | I |
| 15 | Esotropia, anisometropic | VT/Occlusion | 400 | 100 | 360 | 60 | J |
| 16 | Anisometropic | Occlusion | 400 | 100 | 840 | 150 | K |
The sample was made up of stereo-deficient subjects who had previously undergone treatment for amblyopia (optical correction and posterior occlusion of the stronger fellow eye). In cases of strabismic amblyopia, prismatic correction and subsequent vergence therapy, using Anaglyph Random-Dot Stereogram software (VisionBuilder 2.7 for Windows by Haraldseth Software, Hamar, Norway), were needed. Although the treatment obtained good outcomes in visual acuity (monocular distance best corrected visual acuity in amblyopia eye equal to or greater than 0.1 logMAR) and binocular vision (with no evidence of any type of suppression or anomalous sensorial correspondence), the results in terms of stereoacuity were less than satisfactory (values between 800″ and 200″). This study is currently in the process of being published. The inclusion and exclusion criteria for the study can be found in the article by Portela et al.7 The study followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Basque Country. All participants signed a consent form before participating in the study.
In all subjects, a complete eye examination was performed by the same experienced optometrist, including measurement of best corrected distance visual acuity, monocular cover-uncover test, refractive error by autorefraction under cycloplegia, and evaluation of the anterior and posterior segment. Stereoacuity was measured with the Randot Preschool Stereoacuity Test (RPST). We had chosen the RPST as a reference test, because it shows an excellent test–retest reliability.14 Baseline and final stereoacuity measurements are used to calculate the outcome (percentage of improvement). Percentage of improvement was obtained using this formula:
The percentage of improvement was also calculated in log 10.
The Computer Stereoscopic Game (CSG) allowed a stimulation of stereopsis by means of a random dot hidden silhouette identification activity, in anaglyph format, following a protocol that has been previously described.7 In addition, the CSG provided a stereopsis value which determined the stimulation interval. The measurements of stereopsis provided by the CSG before perceptual learning had been added (Fig. 1). The CSG provided 23 different levels of stereopsis divided into three categories. To achieve a new level, the subject had to provide a correct response for three consecutive figures; the software automatically generated a random dot image with finer disparity. On the contrary, if the subject failed the response, the program maintained the same level of disparity.
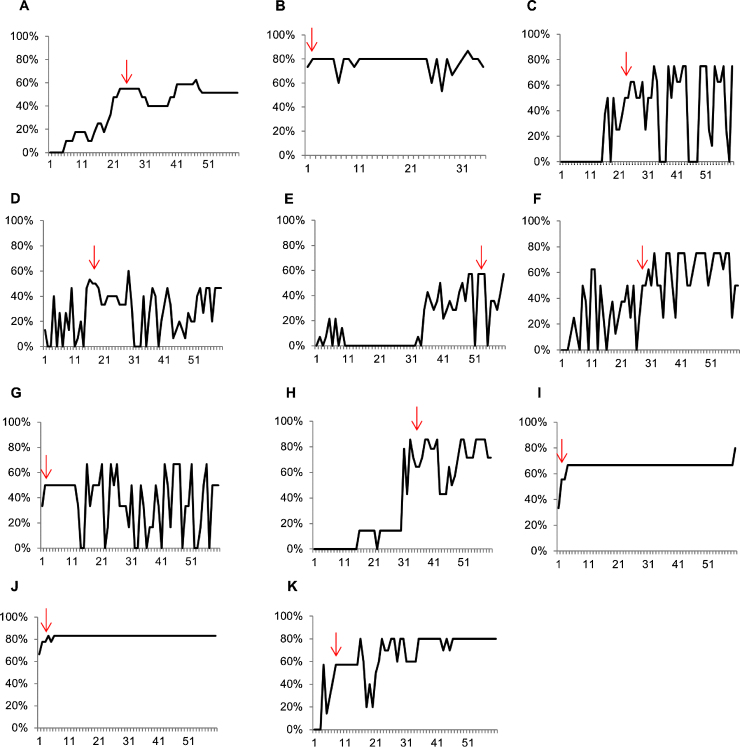
Figure 1.
Analysis of the outcomes obtained in the 11 subjects of the experimental group reaching a final successful outcome ≥50%. The y-axis shows the percentage of stereopsis learning expressed in second arc, whereas the x-axis shows the number of sessions. The arrow indicates the place where the learning occurred.
Characteristics of computerized stereoscopic game
The CSG has two main characteristics: game appearance (perceptual learning task) and design for home training. The game was a Windows application connected to the Internet that stored the results in a database hosted on a remote server. Access to this database allowed the clinician to follow the progression and to monitor the level of compliance on a daily basis. The initial and final levels of stereopsis after each training session were recorded. Hence, it was able to know the exact moment when the subject reached an improvement of 50% in three consecutive sessions.11 This was considered the outcome of success (Fig. 1). This criterion was chosen because an improvement of 50% could be transferred to the RPST. For example, to gain an improvement of stereopsis from 840″ to 420″ the subjects had to overcome 8 different levels of stereopsis; 24 hits in a row by chance is an unlikely outcome. Therefore, in this moment, the real perceptual learning took place, according to the criteria chosen in the study.
Agreement between computerized stereoscopic game and randot preschool stereoacuity test
In order to evaluate the agreement of measurements obtained with the CSG and RPST, two different analyses were made. Firstly, the Bland and Altman method was used at the beginning and after the treatment (32 measurements were compared). Secondly, it was analyzed if there were differences between the measurements of both tests by the Wilcoxon test.
Once detected in which period of the treatment the successful learning was achieved, we were able to analyze if the number of sessions was influenced by either age, baseline stereopsis or type of amblyopia.
Evaluation of age influence
To evaluate the effect of age on learning, two analysis were conducted with Spearman correlation test.
Firstly, we analyzed if older subjects needed more training sessions for learning (age vs intensity). To perform this analysis, we selected subjects who improved by at least 50% using the RPST (n = 11). In order to not eliminate any subject of statistical analysis, the five subjects that did not improve were assigned the arbitrary value of 80 sessions (in the study there were 60 sessions). Secondly, we analyzed if older subjects improved less than the younger subjects (age vs outcome).
Influence of baseline stereopsis
Once it was detected in which period of the treatment the successful learning was achieved, we were able to analyze if the number of sessions was influenced by the baseline stereopsis and type of amblyopia. The correlation (Spearman correlation test) between the initial stereoacuity value with RPST and the percentage of improvement was evaluated (baseline stereopsis vs outcome). The stereo data were log10 transformed. In addition, we analyzed if subjects with worse stereopsis needed a greater number of sessions for a 50% improvement in the value of stereopsis provided by the CSG (baseline stereopsis vs intensity). The five subjects whose perceptual learning did not improve, were assigned the value of 80 sessions.
In addition, to understand the speed of learning, an additional analysis was performed. The sample was divided in two groups according the baseline stereoacuity. One group with stereoacuity worse than 400″ with RPST and the other one better than 400″. The number of sessions to achieve for a 50% improvement was recorder in each group.
Influence of type of amblyopia
In order to assess if the type of amblyopia (anisometropic or strabismic) influenced the number of sessions necessary to obtain a successful outcome, the Mann–Whitney U test was used (type of amblyopia vs outcome).
Results
Ages of subjects ranged between 7 and 13 years old (mean 8.6 ± 1.9 years). Of the 16 patients who entered the study, 12 were females and 4 males. Four of them had a history of refractive amblyopia (two anisometropic and two isoametropic). 12 patients had a history of strabismic amblyopia, and eight of them were also anisometropic. Among subjects with a history of strabismic amblyopia, 11 had esotropia and one subject had exotropia. Table 1 summarizes the data of different clinical parameters at baseline examination.
All the participants had undergone previous amblyopic treatment and achieved good levels of visual acuity without presenting any type of sensory adaptation (suppression or anomalous sensorial correspondence), yet failed to achieve good levels of stereoacuity post-treatment. All patients, except for one who was emmetrope, were treated with optical correction. Two of the subjects used contact lenses as optical correction. Besides this, all patients were treated previously with occlusion, and 11 patients followed a vision therapy or orthoptic program. The orthoptic treatment consisted of prismatic correction of the strabismic deviation and the progressive reduction of the prismatic diopters as the vergence responses were improved. Three subjects received strabismus surgery to achieve binocular vision. Consequently, none of the sample had any strabismic deviation at baseline.
Agreement computerized stereoscopic game & randot preschool stereoacuity test
The measurements of the initial level of stereoacuity pre and post-therapy are shown in Table 2. Using the RPST, median at baseline was 400″ (IQ: 250″ to 800″) and post-therapy, it was 150″ (IQ: 100″ to 700″). The median value of stereopsis obtained by the CSG was 435″ (IQ: 270″ to 840″) and post-therapy it was 225″ (IQ: 67.50″ to 720″). The differences of measurements were not significant (p = 0.075 Wilcoxon test) between both tests.
Table 2.
Baseline clinical parameters. Abbreviations: BCVA = best corrected visual acuity; DE = dominant eye; AE = amblyopic eye.
| n | Age (years) | Sex | Age detection (years) | Refractive error |
BCVA | ||
|---|---|---|---|---|---|---|---|
| Sphere/cylinder AE |
Sphere/cylinder DE |
LogMAR AE DE |
|||||
| 1 | 7 | F | 3 | 3.75/−1.00 | 3.25 | −0.04 | −0.08 |
| 2 | 7 | F | 1 | 0.00 | 0.00 | 0.10 | 0.10 |
| 3 | 7 | M | 3 | 5.50 | 5.00 | 0.06 | −0.04 |
| 4 | 8 | F | 2 | 4.00/−1.50 | 4.00/−1.00 | 0.02 | 0.00 |
| 5 | 13 | F | 3 | 3.00 | 1.75 | 0.02 | 0.02 |
| 6 | 12 | M | 3 | 4.50/−0.75 | 4.00/−0.50 | 0.10 | 0.10 |
| 7 | 8 | M | 2 | 4.00/−2.75 | 4.00/−2.75 | 0.00 | 0.00 |
| 8 | 11 | F | 2 | 6.00/−0.50 | 1.50 | 0.07 | 0.00 |
| 9 | 7 | F | 4 | 3.00/−1.00 | 4.25/−1.00 | 0.10 | 0.07 |
| 10 | 9 | F | 3 | 6.50/−1.25 | 6.50/−2.00 | 0.10 | 0.00 |
| 11 | 8 | M | 3 | 3.50/−0.50 | 1.50/−0.50 | 0.10 | 0.00 |
| 12 | 9 | F | 4 | 2.75/−0.50 | 3.00/−0.50 | 0.02 | 0.02 |
| 13 | 10 | F | 2 | 8.00/−1.00 | 8.00/−0.75 | 0.07 | 0.00 |
| 14 | 7 | F | 3 | 5.50 | 5.50 | 0.05 | 0.05 |
| 15 | 7 | F | 2 | 5.50/−5.00 | 2.50/−1.00 | 0.05 | 0.00 |
| 16 | 8 | F | 2 | −5.75/−1.25 | −2.50/−1.75 | 0.05 | 0.00 |
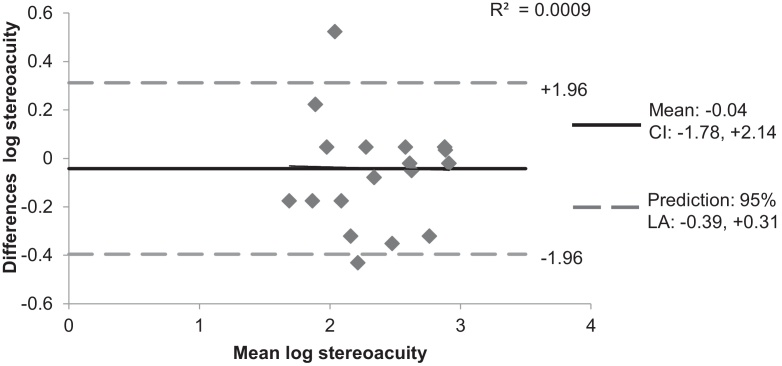
The Bland and Altman analysis revealed that data obtained with RPST showed a good agreement to data obtained with the CSG (Fig. 2). The mean of the difference of measurement was −0.04. The 93.75% of measurements were within agreement limits. Only two measurements were beyond agreement limits (upper limit = 0.31, lower limit = −0.39).
Figure 2.
Bland–Altman plot that compare stereoacuity logarithmic values measured with Randot Preschool Stereoacuity Test and Computerized Stereoscopic Game. The dashed lines show the limits of agreement (LA) for a 95% prediction of the population and the dotted line the mean difference between the methods compared and the confidence interval of the mean (CI).
Age influence
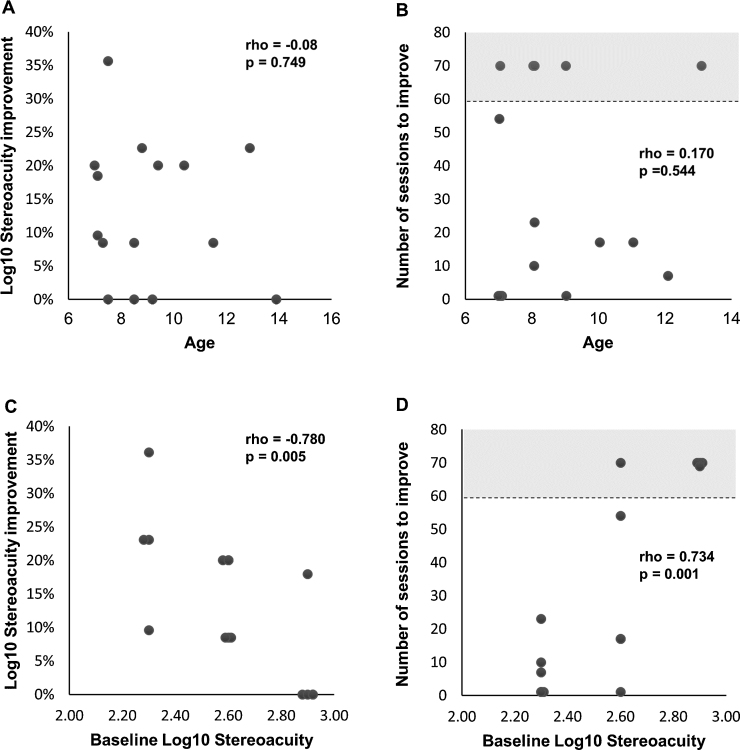
No correlation was found between age and the percentage of improvement achieved with perceptual learning (Fig. 3A) (rho = −0.08, p = 0.749). Likewise, no correlation was found between the number of sessions required and age (rho = 0.170, p = 0.544) (Fig. 3B).
Figure 3.
(A) Scattergram showing the relationship among percentage of improvement log stereoacuity and age. (B) Scattergram showing the relationship among age and the number of sessions necessary to achieve a 50% of improvement. (C) Scattergram showing the relationship among baseline log stereoacuity and the percentage of improvement. (D) Scattergram showing the relationship among baseline log stereoacuity and the number of sessions necessary to achieve a 50% improvement. In Fig. 3C and D, the gray areas represent the subjects who do not experience improvement (n = 5).
Learning threshold for each subject
In order to evaluate how learning had occurred throughout the 60 sessions, an analysis was performed throughout the treatment (Fig. 1). In four subjects (B, G, I, J), the learning took place during the first session (subjects B and J in the first session and subjects G and I in the second session). For the rest of the participants, successful learning was achieved afterwards: session 24 for Subject A, session 26 for Subject C, session 17 for Subject D, session 53 for Subject E, session 29 for Subject F, session 34 for subject H, and session 9 for subject K. Learning was stable for most of the subjects, though subjects C, D and G presented great variability.
Influence of baseline stereoacuity
Fig. 3C shows a strong inverse association (rho = −0.780, p = 0.005) between the initial stereoacuity measurements and the percentage of stereoacuity improvement. In addition, a positive association (rho = 0.734, p = 0.001) was found between the stereoacuity baseline value and the number of sessions required for successful learning (Fig. 3D).
Subjects with baseline stereoacuity worse than 400″ with RPST (subjects A, D, E, G, H, J and K) required 24, 17, 53, 2, 34, 1 and 9 sessions, respectively, to obtain an improvement of 50%. Subject D experienced a regression of the effect in session 33, returning to baseline levels of stereoacuity. In this subject, 50 sessions were necessary to obtain a 50% improvement. The median in this group was 53 sessions (IQ 17–80).
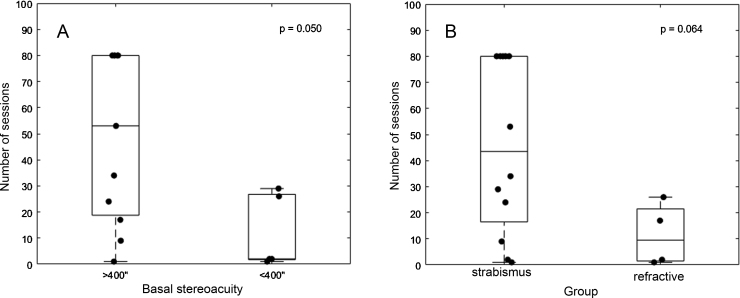
On the other hand, subjects with baseline stereoacuity better than 400″ with RPST (subjects B, C, F and I) required 1, 26, 29 and 2 sessions, respectively, to reach a 50% improvement. The median in this group was 2 sessions (IQ 1.50–17.50). Fig. 4A summarizes the number of sessions needed to achieve successful learning (50% improvement) in each group. The difference was significant (p = 0.050, Mann–Whitney U test).
Figure 4.
Number of sessions performed by subjects according to stereoacuity baseline value (A) or history of amblyopia (B). Boxes indicate 25th and 75th percentiles; dots represent number of sessions performed per subject.
Influence of the type of amblyopia
Finally, in order to evaluate whether the learning curve varied according to the type of amblyopia, the number of sessions needed for improvement was analyzed (Fig. 4B). Twelve subjects had a history of strabismic amblyopia (subjects A, B, E, F, H, I, J, O1–O5) and the remaining four had a history of refractive amblyopia (C, D, G, K). In the strabismic amblyopia group, a median of sessions was 26.50 (IQ 12.75–80), whereas in the group of refractive amblyopia, the median of sessions was 9.50 (IQ 1.25–23.75). Fig. 4B summarizes the number of sessions needed to achieve successful learning in each group. The difference was not significant (p = 0.064, Mann–Whitney U test).
Discussion
Fig. 1 displays the number of perceptual learning sessions that were necessary to improve the level of basal stereoacuity by 50% and to maintain stability for this improvement for at least three consecutive sessions. The aim of this analysis was to define when successful learning was achieved with treatment. The Bland and Altman analysis (Fig. 2) seems to indicate that the improvement observed with the CSG was transferred to the stereoacuity obtained from the RPST. Adams et al.15 considered that a gain of stereoacuity is real with the RPST when the improvement is two levels (to assess the variable test–retest). In our study, the stereoacuity remained stable after 6 months in the 11 subjects in whom stereoacuity improved, so that a gain of 50% with the CSG ensures that the improvement is real and stable.
In the group of 11 subjects experiencing successful learning, the number of sessions varied significantly, with four subjects achieving learning in the first two sessions (subjects B, G, I and J). These temporal differences have already been described by other researchers16 reporting a significant variation among subjects in the speed at which learning was established. Rapid improvements in performance, defined as those occurring within the first 200 trials, have been associated with procedural learning, where improvement results from generalization and the creation of templates. Stimulus-specific tasks, possibly potentiated by overnight consolidation, also result in rapid gains.16 In our study, rapid learning occurred in only four of eleven subjects, making generalization difficult. In any case, initial improvements cannot be attributed to adaptation to random-dot stimuli,17 because all the subjects had previously undergone vergence therapy training (previous treatment for amblyopia) using random-dot stereograms (with constant gross stereopsis demand).
Although most subjects achieved stable learning, some subjects (C, D, G) showed great variations in the threshold achieved between sessions. This could be attributed to the natural learning consolidation process as well as to lack of concentration on the part of our patients in certain sessions, since we were working with young patients whose attention levels were liable to fluctuate when their parents were not present. Executive control of attention plays a significant part in random-dot stereogram therapy, enabling the subject to select task-relevant signals (correlated dots) while filtering out task-irrelevant signals that conflict with these (decorrelated dots).18 Instances of poor attention, impulsive behavior or both led to the task being compromised on some occasions.
Nonetheless, the results overall demonstrate that attention levels were sufficient to allow perceptual learning to take place. Gamification of the task and compliance control are key to maintaining patient interest. Session duration may also play a role. Learning is an incremental function of practice, but session duration and minimum number of trials per session are still controversial.12 In our study, each session lasted 8 min, producing approximately 80 responses and values within the normal range compared with other studies. However, session duration was short enough to allow high attention levels in most cases.
Fig. 4B shows the difference in the number of sessions between subjects with a history of refractive and strabismic amblyopia. Statistically speaking, the difference was not significant (p = 0.064). The outcomes show that treatment response in subjects with a history of strabismic amblyopia was unpredictable, with some subjects behaving similarly to subjects with refractive amblyopia (subjects B, I, J), some requiring additional perceptual learning sessions, and others (O1–O5) in whom perceptual learning did not take place. One of the possible causes for a more intensive treatment in some subjects may be the presence of microstrabismus which is not detectable by cover test.19 Read concludes that normal stereoacuity may require alignment within 0.6 prism dioptres20 because the images of both eyes should be located within Panum's Area.21 Random dot stimuli therapy would improve stereopsis since perceptual learning improves fusion by itself.2 With perceptual learning, as the subject develops finer stereoacuity, the subtle deviation angle may be progressively reduced. It is expected that these subjects would require more sessions of perceptual learning to achieve a successful learning, rather than those with orthotropia or a history of refractive amblyopia. Another reason for the non-improvement may be the primary nature of the stereopsis deficit,21 which in some cases may be genetic; in others, it may be due to other factors, such as a perinatal event or anisometropia, which caused a stereopsis deficit prior to the onset of esotropia. Highly developed stereoacuity is dependent on a normal complement of binocular neurons in the visual cortex.21 A reduction of the functional binocular connections in the visual cortex may therefore be responsible for the stereopsis treatment failure.
The subjects with a history of refractive amblyopia experienced at least a 50% improvement in baseline stereopsis values in the first sessions. In the peer-reviewed literature, a successful learning in subjects with refractive amblyopia also occurred in the first sessions.3, 4, 5 That happen in the study of Ding and Levi,4 including five subjects (four with strabismus and one subject with anisometropia). In the subject with anisometropic amblyopia, stereopsis improved rapidly in the first 210 responses, which is a result similar to that found by Astle et al.3 and by Xi et al.5 However, in the strabismic subjects, between 3000 and 20,000 responses were necessary to re-establish binocular vision and improve stereopsis.4, 6
The initial conclusion of our results would be that perceptual learning of stereopsis is more effective in subjects with a history of refractive amblyopia than in subjects with a history of strabismic amblyopia. An analysis that would confirm this initial conclusion is the comparison of the number of sessions required for both types of amblyopes to achieve a successful outcome (Fig. 4B). This can be easily questioned since subjects with a history of strabismus in our study had poorer baseline levels of stereopsis (Table 1). Webber et al.13 stimulate the amblyopic visual system with a dichoptic game. They noticed that subjects with refractive amblyopia improved their stereoacuity, but his improvement was not observed in the subjects with strabismic amblyopia. Nevertheless, the subjects with refractive amblyopia had a baseline stereoacuity better than the subjects with strabismus amblyopia (null stereoacuity in baseline).
Li et al. in 200822 studied the number of sessions required to achieve a successful learning according to the depth of amblyopia. They concluded that the intensity of the treatment was closely related to the depth of amblyopia (the worse the level of basal visual acuity, the greater the number of treatment sessions that were required). This relationship could be transferred to stereo-deficient subjects. In the study of Ding and Levi in 2011,4 the subject with anisometropic amblyopia began with an initial stereoacuity of 70″, while the subjects with strabismus began with a null stereoacuity. Thus, the difference observed in the number of sessions may be due to differences in the depth of stereo-deficiency. In our series, there was a strong and direct correlation between the initial level of stereopsis and the number of sessions required (rho = 0.734, p = 0.001). This suggests that the baseline value of stereoacuity, and not the type of amblyopia, determines the intensity and duration of the treatment.
Finally, the relationship between basal stereoacuity and the percentage of improvement in stereopsis was studied. This analysis revealed the presence of a strong inverse association (rho = −0.780). This means that poorer levels of baseline stereoacuity were related to a lower percentage of improvement in stereoacuity. This type of analysis does not appear in studies on perceptual learning in stereo-deficient subjects, but has been reported in studies evaluating the baseline visual acuity in amblyopic subjects.10 In the aforementioned study, the baseline visual acuity values did not seem to condition the prognosis of treatment. However, our results suggest that the baseline value of stereoacuity and not the type of amblyopia determines the number of sessions of treatment required. Future studies with larger sample sizes are necessary to confirm if the baseline value of stereoacuity determines the intensity, duration and prognosis of perceptual learning treatment.
The effect of age on treatment was evaluated according to two types of analyses. Firstly, the correlation age-percentage of stereoacuity improvement was analyzed. In Fig. 3A, it can be seen how this association was almost null (rho = −0.08, p = 0.749). These results are consistent with those reported by other authors in stereo-deficient adults.3, 4, 5, 6 In all of these studies, age was not an obstacle for the improvement of stereoacuity. There are many studies that suggest that amblyopia can be treated with optical correction and occlusion or atropine beyond the sensitive period.23 Concerning perceptual learning, there are also some studies suggesting that this type of treatment is able to improve visual acuity11, 24 and stereoacuity4, 6 beyond the sensitive period, during the susceptible period. In addition, the Spearman Correlation Test (Fig. 3B) was used to determine if older subjects needed more sessions. To our knowledge, this analysis has not been previously performed. It showed that older subjects did not need more sessions of training compared to younger subjects (rho = 0.170, p = 0.544).
This research provides a value that is important to highlight. The data of the daily activity are hosted on a server that displays compliance and the daily performance. Compliance has been analyzed in previous studies with serious games,8, 9 but as far as the authors know, this is the first time that analysis of the performance has been conducted. However, the present investigation has some limitations that we would like to emphasize. The group of subjects with history of refractive amblyopia had a particularly small sample size, notwithstanding, the group with history of strabismus is comparatively very large. In addition, it would also have been interesting to analyze the effect of age in a broader range of ages. Future studies are necessary to continue investigating the factors that influence learning in stereo-deficient subjects.
Conclusion
Perceptual learning in stereo-deficient subjects is not influenced by age and does not appear to be influenced by type of amblyopia. However, there is a direct and strong association between the value of initial stereopsis and the number of sessions required to obtain successful learning. Finally, subjects with worse stereoacuity at baseline needed a greater number of sessions to achieve learning and reached a lower percentage of final improvement.
Conflicts of interest
Authors have to clearly state that at least 2 of the authors have commercial interests in the software, procedures or devices used. The computer-based test itself was developed at the University of Oviedo by the IdeasCAD research team (www.ideascad.es) under the direction of SM-G, coauthor of this manuscript, and partially founded by VISUALIA visual therapy clinic (www.visualia-coc.es), under agreement FUO-EM-104-12. After finishing this study, a private company name VISIONARY TOOL (www.visionarytool.com) has contacted both SM-G and JAP-C to participate in the development of a computerized visual training tool. This tool includes several games and tests. The one used in this article, based on random dot hidden silhouettes, is one of them.
Acknowledgements
This research was carried out thanks to a grant awarded by the European University of Madrid 2013/UEM20; to JR-A.
References
- 1.McKee S.P., Levi D.M., Movshon J.A. The pattern of visual deficits in amblyopia. J Vis. 2003;3:380–405. doi: 10.1167/3.5.5. [DOI] [PubMed] [Google Scholar]
- 2.Levi D.M., Knill D.C., Bavelier D. Stereopsis and amblyopia: a mini-review. Vis Res. 2015;114:17–30. doi: 10.1016/j.visres.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Astle A.T., McGraw P.V., Webb B.S. Recovery of stereo acuity in adults with amblyopia. BMJ Case Rep. 2011:1–4. doi: 10.1136/bcr.07.2010.3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ding J., Levi D.M. Recovery of stereopsis through perceptual learning in human adults with abnormal binocular vision. Proc Natl Acad Sci U S A. 2011;108:E733–E741. doi: 10.1073/pnas.1105183108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xi J., Jia W., Feng L. Perceptual learning improves stereoacuity in amblyopia. Invest Ophthalmol Vis Sci. 2014;55:2384–2391. doi: 10.1167/iovs.13-12627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vedamurthy I., Knill D.C., Huang S.J. Recovering stereo vision by squashing virtual bugs in a virtual reality environment. Philos Trans R Soc Lond (B) 2016;37:20150264. doi: 10.1098/rstb.2015.0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Portela-Camino J.A., Martín-González S., Ruiz-Alcocer J. A random dot computer video game improves stereopsis. Optom Vis Sci. 2018;95:523–535. doi: 10.1097/OPX.0000000000001222. [DOI] [PubMed] [Google Scholar]
- 8.Holmes J.M., Manh V.M., Lazar E.L. Effect of a binocular iPad game vs part-time patching in children aged 5 to 12 years with amblyopia: a randomized clinical trial. JAMA Ophthalmol. 2016;134:1391–1400. doi: 10.1001/jamaophthalmol.2016.4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manh V.M., Holmes J.M., Lazar E.L. A randomized trial of a binocular iPad game versus part-time patching in children aged 13 to 16 years with amblyopia. Am J Ophthalmol. 2018;186:104–115. doi: 10.1016/j.ajo.2017.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mansouri B., Singh P., Globa A., Pearson P. Binocular training reduces amblyopic visual acuity impairment. Strabismus. 2014;22:1–6. doi: 10.3109/09273972.2013.877945. [DOI] [PubMed] [Google Scholar]
- 11.Zhou Y., Huang C., Xu P. Perceptual learning improves contrast sensitivity and visual acuity in adults with anisometropic amblyopia. Vis Res. 2006;46:739–750. doi: 10.1016/j.visres.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 12.Levi D.M., Li R.W. Perceptual learning as a potential treatment for amblyopia: a mini-review. Vis Res. 2009;49:2535–2549. doi: 10.1016/j.visres.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Webber A.L., Wood J.M., Thompson B. Fine motor skills of children with amblyopia improve following binocular treatment. Invest Ophthalmol Vis Sci. 2016;57:4713–4720. doi: 10.1167/iovs.16-19797. [DOI] [PubMed] [Google Scholar]
- 14.Fawcett S.L., Birch E.E. Interobserver test–retest reliability of the Randot preschool stereoacuity test. J AAPOS. 2000;4:354–358. doi: 10.1067/mpa.2000.110340. [DOI] [PubMed] [Google Scholar]
- 15.Adams W.E., Leske D.A., Hatt S.R., Holmes J.M. Defining real change in measures of stereoacuity. Ophthalmology. 2009;116:281–285. doi: 10.1016/j.ophtha.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hussain Z., Sekuler A.B., Bennett P.J. How much practice is needed to produce perceptual learning? Vis Res. 2009;49:2624–2634. doi: 10.1016/j.visres.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 17.Julesz B. University of Chicago Press; Chicago: 1971. Foundations of Cyclopean Perception. [Google Scholar]
- 18.Yotsumoto Y., Watanabe T. Defining a link between perceptual learning and attention. PLoS Biol. 2008;6:e221. doi: 10.1371/journal.pbio.0060221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holmes J.M., Leske D.A., Hohberger G.G. Defining real change in prism-cover test measurements. Am J Ophthalmol. 2008;145:381–385. doi: 10.1016/j.ajo.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Read J.C.A. Stereo vision and strabismus. Eye. 2015;29:214–224. doi: 10.1038/eye.2014.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Birch E.E., Wang J. Stereoacuity outcomes after treatment of infantile and accommodative esotropia. Optom Vis Sci. 2009;86:647–652. doi: 10.1097/OPX.0b013e3181a6168d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li R.W., Klein S.A., Levi D.M. Prolonged perceptual learning of positional acuity in adult amblyopia: perceptual template retuning dynamics. J Neurosci. 2008;28:14223–14229. doi: 10.1523/JNEUROSCI.4271-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scheiman M.M., Hertle R.W., Beck R.W. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123:437–447. doi: 10.1001/archopht.123.4.437. [DOI] [PubMed] [Google Scholar]
- 24.Chen P.L., Chen J.T., Fu J.J. A pilot study of anisometropic amblyopia improved in adults and children by perceptual learning: an alternative treatment to patching. Ophthalmic Physiol Opt. 2008;28:422–428. doi: 10.1111/j.1475-1313.2008.00588.x. [DOI] [PubMed] [Google Scholar]