Abstract
Background:
Chronic obstructive pulmonary disease (COPD) is often accompanied by psychiatric problems, such as depression and anxiety, affecting both treatment outcomes and mortality. Evidence for the number of COPD patients using medication for these disorders is sparse. In this study, chronic antidepressant (ATD) and anxiolytic (ANX) drug use – to identify depression and anxiety – among COPD patients was compared with subjects with or without other chronic diseases.
Methods:
The NControl database containing prescription data of 800 pharmacies including 7 million individuals in The Netherlands was used. Patients of age 55+ years who received frequent prescriptions – at least two/year in 5 out of 6 years – for COPD medication, dermatological drugs, disease-modifying antirheumatic drugs (DMARDs), statins and oral glucose-lowering medication were analyzed for concomitant chronic use of ATDs and ANXs between 1 January 2013 and 1 January 2019. All other subjects aged 55+ years were included as a control group (control group 1). This group was further stratified into a group of subjects that received frequent prescriptions of any kind (control group 2).
Results:
15.2% of the patients that receive COPD treatment (n = 96,319), 15.3% of subjects that are treated for dermatological problems (n = 62,865), 13.2% of subjects that receive DMARDs (n = 7900), 11.6% of statins users (n = 422,376) and 11.4% of oral glucose-lowering medication users (n = 165,975) are also chronically treated for depression or anxiety, compared with 2.6% (control group 1; n = 3,290,608) and 11.4% (control group 2; n = 757,947). In general, female and 75+ years aged subjects showed a higher risk for using ATDs and ANXs chronically. In the COPD and the dermatological patient group the risk was the highest compared with the other patient groups.
Conclusions:
The rates of chronic ATD and ANX use and the risk of having depression and/or anxiety are especially high in COPD patients, indicating that psychiatric problems are more common in COPD than in most other chronic diseases. In general, age and gender strongly influence the risk of chronically using ATDs and ANXs.
The reviews of this paper are available via the supplemental material section.
Keywords: anti-anxiety agents, antidepressive agents, chronic disease, chronic obstructive, prescriptions, pulmonary disease
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic lung disorder characterized by the progression of airflow restriction associated with abnormal inflammatory responses to toxic particles or gases.1 The obstructive bronchiolitis and parenchymal destruction are progressive and not fully reversible. COPD is currently the third leading cause of death worldwide, representing a major concern for public health.2 Extrapulmonary comorbidities are highly prevalent in COPD, and it has been demonstrated these have a significant impact on quality of life and treatment outcomes.3 In COPD, the occurrence and severity of these extrapulmonary symptoms can be very heterogeneous and therefore there is a need for personalized treatment strategies in these patients.
There is an increased prevalence of psychiatric comorbidities, such as depression and anxiety, in COPD patients compared with non-COPD controls.3 For depression, two meta-analyses revealed a prevalence of 24.6% and 27.1% in COPD versus 11.7% and 10.0% in non-COPD subjects.4,5 The prevalence of anxiety in COPD was reported to be around 9–28% whereas in control subjects this was 4–6%.3 One study compared the prevalence of depressive symptoms in COPD patients to that in subjects having other chronic diseases, such as diabetes and arthritis.6 Around 40% of the COPD patients displayed symptoms of depression, which was the highest prevalence compared with almost all other chronic disease groups that were examined. The high prevalence of depression and anxiety is concerning because these problems are associated with reduced efficacy of COPD therapies partly due to physical activity avoidance, worsening of symptoms and increased mortality.3,7 Therefore, accurate diagnosis and treatment of depression and/or anxiety is vital for COPD patients.
The evidence for the use of anxiolytics (ANXs) and/or antidepressants (ATDs) in COPD patients is limited as well as inconsistent.3 The majority of studies have focused on the use of benzodiazepines as these have several safety issues in COPD patients, because of the potential adverse respiratory effects.8–10 In a study by Janssen and colleagues (2010), Dutch COPD patients were screened for symptoms of anxiety and depression before entering pulmonary rehabilitation.11 It appeared that 41.8% of the patients were experiencing clinically relevant symptoms of anxiety and/or depression, although only 24% of the patients were using ANXs and/or ATDs. As these patients were admitted for pulmonary rehabilitation, most patients had a severe disease state. Therefore, results might not represent the general COPD population. In the present study, the chronic use of ATDs and ANXs in subjects indicative of having COPD was evaluated and compared with subjects with and without chronic diseases in The Netherlands using a pharmacy prescription database.
Methods
Database
In a retrospective cohort study, data were obtained from the NControl database (2013–2018) including dispensing data from 800 pharmacies and over 7 million patients, located in different regions in The Netherlands. This database has been a source for multiple studies and includes information on patient demographics, including age and gender, and drug dispensing records from mainly community pharmacies and, to a lesser extent, outpatient pharmacies located in the hospitals.12,13
Ethical approval
Data protection is a central issue for research ethics and a fundamental human right.14 Use of prescription data in the database of NControl for research purposes is legally permissible. Patient data in the database are pseudonymized. It is impossible for researchers that work with the NControl database to re-identify any natural persons. As such, it is also not possible for researchers to ask patients’ permission to be included this study. NControl adheres to data protection and privacy regulations, as established in among others the Personal Data Protection Act in The Netherlands as well as The Netherlands Norm (NEN) 7510 standard on information protection in healthcare, which is derived from International Organisation for Standardization (ISO) norm 27001 and 27002.15
Subject and drug selection
Selection of subjects was performed using the NControl database between 1 January 2013 and 1 January 2019. Chronic patients were defined based on the frequency by and the duration for which patients received dispensions of chronic disease-specific medications. All medications were selected based on the WHO Anatomical Therapeutic Chemical (ATC) codes (Supplemental Table 1). COPD medication included (oral) glucocorticoids, adrenergics, anticholinergics and combinations between these drugs. Other medication groups included statins (cardiovascular disease), oral glucose-lowering medications (type 2 diabetes mellitus), disease-modifying antirheumatic drugs (DMARDs; rheumatoid arthritis) and dermatology medication consisting of emollients and protectives, antipruritics, antipsoriatics, dermatological corticosteroids and other dermatological preparations (eczema and psoriasis). The list of inclusion drugs with ATC codes is depicted in Supplemental Table 1.
Chronic use was defined as follows: at least two prescriptions of drugs within a category, in at least 5 out of 6 years of the study period. Patients may appear in more than one chronic disease group. Subjects who received only inhalation corticosteroids were excluded as COPD patients. We included subjects of age 55+ years. This age stratification was maintained for all analyses.
We included two control groups: control group 1 contained all subjects of age 55+ years who were not included in any of the five chronic disease groups. Control group 2 was a subset of group 1 containing subjects who received at least two prescriptions of any kind per year in 5 out of 6 years.
The groups were analyzed for concomitant chronic dispensing of ATDs and/or ANXs using the same conditions as the ones used to classify the chronic disease patient groups. We excluded hydroxyzine and z-hypnotics, as these are often prescribed for other indications than for anxiety/depression. ATC codes of the included drugs are depicted in Supplemental Table 1.
Statistical analysis
We used Microsoft SQL Server Management Studio and Microsoft Excel to extract the data from the database and perform our analyses. In this study, risk ratios (RRs) are used to describe the association between being a chronic patient in one of the chronic disease groups and using chronically ATDs and/or ANXs, compared with subjects in the control group. We further compared ratios in subgroups based on age and gender. For this, subgroups in the control group were compared with the corresponding subgroups in the chronic disease group.
Results
In total, 96,319 subjects indicated as having COPD were selected from the NControl database, of which 14,619 used ATDs and/or ANXs chronically (receiving ⩾2 prescriptions/year for at least 5 years) between 1 January 2013 and 1 January 2019 (Figure 1). Of the 62,865 chronic users of dermatological medication, 9627 used ATDs and/or ANXs chronically. The DMARDs user group consisted of 7900 subjects of which 1042 were chronic users of ATDs and/or ANXs. There were 422,376 patients that used statins, of which 49,203 also received ATDs and/or ANXs chronically. Of the 165,975 oral glucose-lowering drug users, 18,955 also displayed chronic use of ATDs and/or ANXs. In all chronic disease groups, chronic use of ATD and/or ANX drugs was higher as compared with control group 1 (86,407 out of 3,290,608) and, except for oral glucose-lowering medication users, with control group 2 (86,407 out of 757,947).
Figure 1.
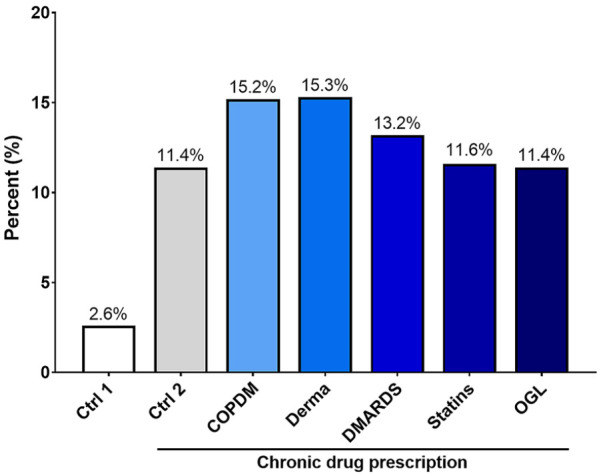
The percentage of chronic ATD and/or ANX users within the subject groups. Control (ctrl) group 1 includes all 55+ year-old subjects who were not included in any of the chronic disease groups. The subjects from control group 1 who received at least two prescriptions per year in 5 out of 6 years were included in control group 2.
ANX, anxiolytic; ATD, antidepressant; COPDM, chronic obstructive pulmonary disease (COPD) medication users; Derma, dermatological medication users; DMARDs, disease-modifying antirheumatic drugs users; OGL, oral glucose-lowering drug users.
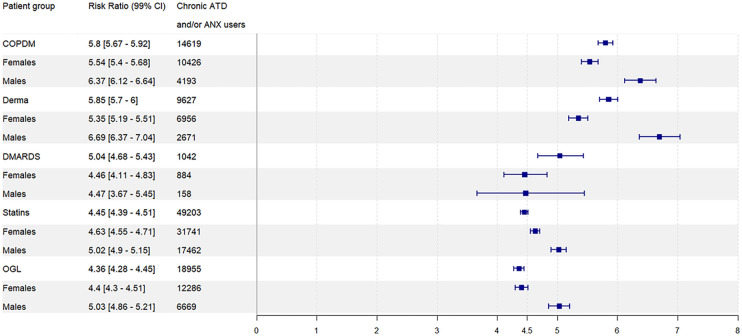
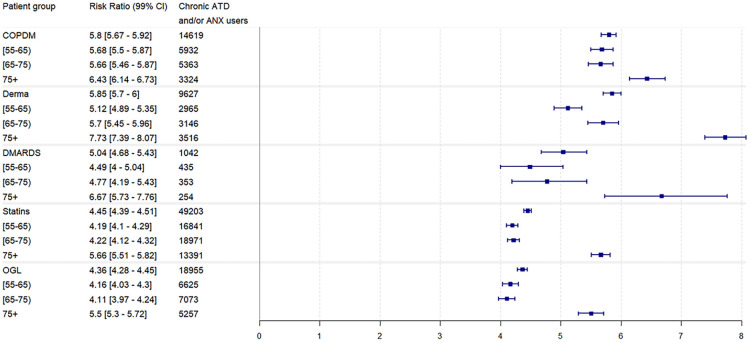
The RR for using ATDs and/or ANXs chronically in the COPD group was 5.80 (5.67–5.92) compared with control group 1 (Figure 2). The RR was higher in men than in women for the COPD group. Except for the dermatological medication user group, the RR in the other chronic disease subject groups was lower than in the COPD group (Figure 2). In the COPD group, subjects aged 75 years and older showed a higher RR (6.43 [6.14–6.73]) than other age groups (5.68 [5.5–5.87] and 5.66 [5.46–5.87] for ages 55–65 and 65–75 years, respectively; Figure 3). The higher RR in the 75+ years subgroup was even more pronounced in the other drug user groups. As compared with subjects aged 55–65 years, there was an increase in RR of 1.34 in the oral glucose-lowering drug user group to 2.61 in the dermatological medication user group (Figure 3).
Figure 2.
Chronic ATD and/or ANX use RRs of the chronic disease subject groups versus all other 55+ years old subjects (control group 1) overall and for each gender category.
ANX, anxiolytic; ATD, antidepressant; COPDM, chronic obstructive pulmonary disease (COPD) medication users; Derma, dermatological medication users; DMARDs, disease-modifying antirheumatic drugs users; OGL, oral glucose-lowering drug users.
Figure 3.
Chronic ATD and/or ANX use RRs of the chronic disease subject groups versus all other 55+ years old subjects (control group 1) for each age category.
ANX, anxiolytic; ATD, antidepressant; COPDM, chronic obstructive pulmonary disease (COPD) medication users; Derma, dermatological medication users; DMARDs, disease-modifying antirheumatic drugs users; OGL, oral glucose-lowering drug users.
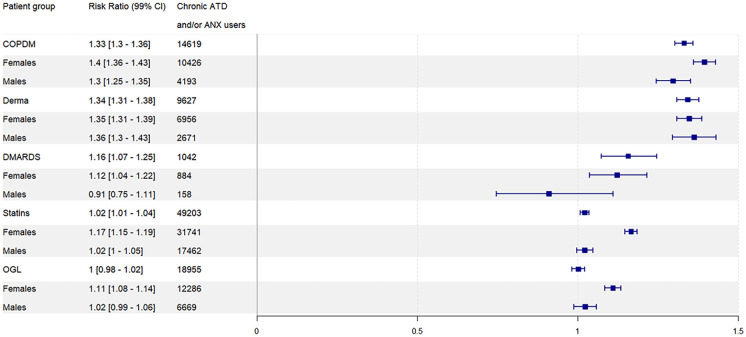
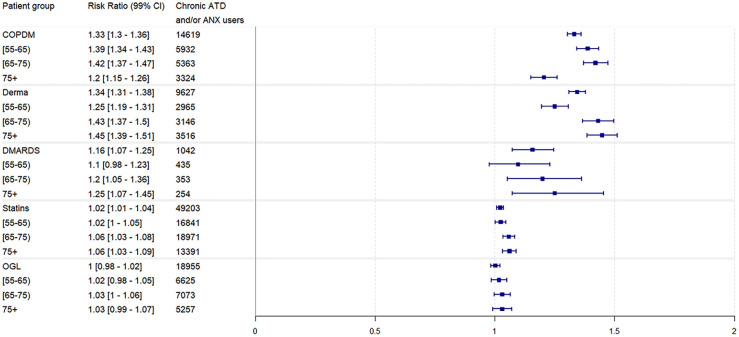
Compared with control group 2, the RR in the COPD subject group was 1.33 (1.30–1.36) (Figure 4). The RRs among the other chronic disease groups ranged between 1 and 1.34. No differences in RRs between women and men nor between the different age groups were observed for the chronic disease groups versus control group 2 (Figures 4 and 5).
Figure 4.
Chronic ATD and/or ANX use RRs of the chronic disease subject groups versus chronic users of any drugs from control group 1 (control group 2) overall and for each gender category.
ANX, anxiolytic; ATD, antidepressant; COPDM, chronic obstructive pulmonary disease (COPD) medication users; Derma, dermatological medication users; DMARDs, disease-modifying antirheumatic drugs users; OGL, oral glucose-lowering drug users.
Figure 5.
Chronic ATD and/or ANX use RRs of the chronic disease subject groups versus chronic users of any drugs from control group 1 (control group 2) for each age category.
ANX, anxiolytic; ATD, antidepressant; COPDM, chronic obstructive pulmonary disease (COPD) medication users; Derma, dermatological medication users; DMARDs, disease-modifying antirheumatic drugs users; OGL, oral glucose-lowering drug users.
Overall, there was an increased RR in women using ATDs and/or ANXs chronically compared with men for all the groups, ranging from 1.88 (1.78–1.99) in the dermatological medication user group to 2.36 (2.31–2.41) in control group 1 (Figure 6).
Figure 6.
Chronic ATD and/or ANX use RRs in women versus men for each subject group. Control group 1 includes all 55+ year-old subjects who were not included in any of the chronic disease groups. The subjects from control group 1 who received at least two prescriptions per year in 5 out of 6 years were included in control group 2.
ANX, anxiolytic; ATD, antidepressant; COPDM, chronic obstructive pulmonary disease (COPD) medication users; Derma, dermatological medication users; DMARDs, disease-modifying antirheumatic drugs users; OGL, oral glucose-lowering drug users.
Discussion
The use of ATDs and/or ANXs was higher in COPD patients and other selected chronic disease groups as compared with the non-users of chronic disease medication. This observation is in line with previous findings indicating a strong association between chronic diseases – such as diabetes and rheumatoid arthritis – and both anxiety and depression.16 More importantly, COPD patients had a 5.8 times higher risk of depression and/or anxiety medication use compared with all other subjects who were not included in any of the chronic disease groups. However, when this control group was stratified based on an increasing prescription rate of any drugs – identical to the criteria for chronic use – the risk of chronically using ATDs and/or ANXs was not different. One explanation for this is that mental health issues may affect health perception and increase somatization.17 Moreover, there are chronic disease patients in this group, other than the ones classified in this study. The chronic use of ATDs and/or ANXs might therefore be higher in this stratified group. In addition, our data show on average a two times higher risk of the chronic use of ATDs and/or ANXs for women compared with men among the chronic disease subject groups. This is in line with the risk in the control groups and the general population as there is in general almost a two-fold higher incidence of depression in women opposed to men.18
In the COPD group, the proportion of chronic users of ATDs and/or ANXs is lower compared with previous findings in an observational study including Dutch COPD patients (15.2% versus 24.3%, respectively).11 This discrepancy could be explained by the differences in population characteristics between the studies. The study of Janssen and coworkers11 included COPD patients who were admitted for pulmonary rehabilitation in a specialized center. This means that these COPD patients suffer from multiple symptoms affecting quality of life and, consequently, suffer more from depression and anxiety. The severity was reflected by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage of the population; almost 70% of the COPD patients had GOLD stage III or IV, severe to very severe COPD.1,11 A higher proportion of GOLD stage IV patients showed significant anxiety and depression than patients with other GOLD stages. Although disease severity has not been accounted for in the current study, a more general population of COPD subjects – with relatively mild to moderate COPD cases – has been studied as compared with the study of Janssen and coworkers.11 Furthermore, many studies investigating drug use prevalence have segregated any use of drugs into medication groups or investigated only a single medication group, such as benzodiazepines or solely ATDs or ANXs, which makes it more difficult to compare results. However, when comparing results with benzodiazepine use – a regularly investigated drug group in COPD – multiple publications indicate a higher incidence of use, ranging from 20.9% to 69%.8–10,19–21 This could partly be explained by the fact that in our study, only chronic users were selected to have a strong indication for the identification of depression and/or anxiety cases. In contrast, in other publications, the current use of ATDs and/or ANXs by patients using COPD medication was evaluated without accounting for the duration and frequency. Another important factor in our approach that may contribute to differences in ATD/ANX use in COPD is the exclusion of z-hypnotics, for example, zolpidem and zopiclone. Although these drugs have a similar binding site to benzodiazepines, z-hypnotics mainly have sedative effects and are therefore primarily used to treat insomnia. Sleep disturbances are very common in COPD and, although it is not recommended in severe COPD, z-hypnotics are prescribed to COPD patients.19,22–24
The relatively high rate of chronic ATD and/or ANX use in the patients suffering from dermatological problems, such as psoriasis and eczema, can be explained by the relationship between both skin and mental problems.25 Women with depression had an increased risk of developing psoriasis.26 Interestingly, the risk was especially high in women who were both depressed and using ATDs. The results indicate that there might be a bidirectional relation between mental health issues and skin problems. A bidirectional relation might also be applicable for the COPD patients as general anxiety and depression increase the likelihood of smoking and thus the risk of developing COPD. However, the prevalence of depression is higher in COPD patients as compared with smoking controls indicating that the disease itself plays an important role as well.27 Several factors are thought to contribute to the development of anxiety and depression in COPD specifically, including smoking, hypoxemia, systemic inflammation and the chronic use of corticosteroids.3
The present study has several limitations. Firstly, it is likely that there was the inclusion of asthma cases in the COPD subject group as there is overlap in pharmacological treatment between asthma and COPD. Although an age stratification was applied and the subjects using solely inhaled corticosteroids have been excluded, it was not possible to rule out the asthma cases completely. Besides, it is known that there can be an overlap in asthma and COPD, meaning that clinical features of both diseases can be present in one individual.28 Overlap in pharmacological treatment strategies hampers the total exclusion of asthma cases. It is important to consider this, because a relation between mental health and asthma has been demonstrated before represented by the high prevalence of anxiety and depression.29 Secondly, our findings have been based on a prescription database of pharmacies. Therefore, several confounding factors could not have been accounted for. These factors are mainly related to lifestyle such as diet and exercise. Besides, an unhealthy lifestyle is related to (the development of) depression.30 In addition, the index date of ATDs and/or ANXs in these subjects is not known. Knowledge about the index date could indicate whether there was anxiety/depression present prior to COPD diagnosis. In a follow-up cohort study, more research on incidence, causes and prognosis should be performed to, among other things, elaborate this.
The proportion of the identified COPD patients chronically using ATDs and/or ANXs in this study is lower compared with several prevalence studies of anxiety and depression.3 One reason for this could be the underdiagnosis and associated undertreatment of anxiety and/or depression in COPD patients. It was demonstrated that around 65% of COPD patients should be diagnosed with anxiety/depression whereas only 31% of these diagnosed patients were actually receiving treatment.31 A similar proportion of accurate treatment was found in people with depression in general.32 Although the physician may have legitimate reasons for declining pharmacological treatment of depression and/or anxiety in COPD patients because of adverse side effects, it is important to treat these symptoms in patients. Anxiety and depression in COPD have been related to worsened disease progression and increased mortality.3,7 Non-pharmacological treatment options, such as cognitive behavioral therapy, might be preferred in some patients because of the limited adverse effects. However, data on the proportion of COPD patients with depression and/or anxiety currently receiving non-pharmacotherapeutic treatment are lacking.
In conclusion, over a 6-year period, ATDs and/or ANXs were chronically prescribed to 15.2% of COPD patients. Compared with non-chronic medication users, the risk of depression and/or anxiety was increased in COPD patients. Among users of other chronic medication, the risk was also one of the highest. These data contribute to the awareness and acknowledgement of the increased risk of mental health issues in COPD patients which are known to hamper treatment outcomes significantly.
Supplemental Material
Supplemental material, sj-pdf-1-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-2-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-3-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-4-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-5-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-6-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Footnotes
Author contribution(s): Charlotte E. Pelgrim: Investigation; Project administration; Visualization; Writing-original draft.
Jan Maurik van den Heuvel: Data curation; Formal analysis; Methodology; Software; Validation; Visualization; Writing-original draft; Writing-review & editing.
Gert Folkerts: Conceptualization; Funding acquisition; Writing-review & editing.
Johan Garssen: Conceptualization; Funding acquisition; Writing-review & editing.
Anke H Maitland-van der Zee: Conceptualization; Data curation; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Writing-review & editing.
Aletta D. Kraneveld: Conceptualization; Funding acquisition; Investigation; Supervision; Validation; Writing-review & editing.
Conflict of interest: CEP, JMH, GF, AHM and ADK declare that they have no conflict of interst. JG is a part-time employee of Nutricia Research, Utrecht, The Netherlands.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work has been supported by the LSH-TKI-lung fund PPP allowance 10.2.16.119.
ORCID iD: Charlotte E. Pelgrim  https://orcid.org/0000-0003-1816-2705
https://orcid.org/0000-0003-1816-2705
Supplemental material: The reviews of this paper are available via the supplemental material section.
Contributor Information
Charlotte E. Pelgrim, Division of Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, Utrecht, The Netherlands.
Jan Maurik van den Heuvel, Department of Respiratory Medicine, Amsterdam University Medical Centers, University of Amsterdam, Amsterdam, The Netherlands.
Gert Folkerts, Division of Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, Utrecht, The Netherlands.
Johan Garssen, Division of Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, Utrecht, The Netherlands Danone Nutricia Research, Utrecht, The Netherlands.
Anke H. Maitland-van der Zee, Department of Respiratory Medicine, Amsterdam University Medical Centers, University of Amsterdam, Amsterdam, The Netherlands
Aletta D. Kraneveld, Division of Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, Utrecht, 3508 TC, The Netherlands.
References
- 1. Pauwels RA, Buist AS, Calverley PM, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001; 163: 1256–1276. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization. Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016. 2018. Geneva: World Health Organization. [Google Scholar]
- 3. Pelgrim CE, Peterson JD, Gosker HR, et al. Psychological co-morbidities in COPD: targeting systemic inflammation, a benefit for both? Eur J Pharmacol 2019; 842: 99–110. [DOI] [PubMed] [Google Scholar]
- 4. Matte DL, Pizzichini MM, Hoepers AT, et al. Prevalence of depression in COPD: a systematic review and meta-analysis of controlled studies. Respir Med 2016; 117: 154–161. [DOI] [PubMed] [Google Scholar]
- 5. Zhang MW, Ho RC, Cheung MW, et al. Prevalence of depressive symptoms in patients with chronic obstructive pulmonary disease: a systematic review, meta-analysis and meta-regression. Gen Hosp Psychiatry 2011; 33: 217–223. [DOI] [PubMed] [Google Scholar]
- 6. Schane RE, Woodruff PG, Dinno A, et al. Prevalence and risk factors for depressive symptoms in persons with chronic obstructive pulmonary disease. J Gen Intern Med 2008; 23: 1757–1762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maurer J, Rebbapragada V, Borson S, et al. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest 2008; 134: 43S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vozoris NT, Fischer HD, Wang X, et al. Benzodiazepine drug use and adverse respiratory outcomes among older adults with COPD. Euro Res J 2014; 44: 332–340. [DOI] [PubMed] [Google Scholar]
- 9. Halvorsen T, Martinussen PE. Benzodiazepine use in COPD: empirical evidence from Norway. Int J Chron Obstruct Pulmon Dis 2015; 10: 1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vozoris NT, Fischer HD, Wang X, et al. Benzodiazepine use among older adults with chronic obstructive pulmonary disease. Drugs Aging 2013; 30: 183–192. [DOI] [PubMed] [Google Scholar]
- 11. Janssen DJ, Spruit MA, Leue C, et al. Symptoms of anxiety and depression in COPD patients entering pulmonary rehabilitation. Chronic Respir Dis 2010; 7: 147–157. [DOI] [PubMed] [Google Scholar]
- 12. Garritsen FM, van den Heuvel JM, Bruijnzeel-Koomen CA, et al. Use of oral immunosuppressive drugs in the treatment of atopic dermatitis in the Netherlands. J Eur Acad Dermatol Venereol 2018; 32: 1336–1342. [DOI] [PubMed] [Google Scholar]
- 13. Van den Heuvel J, Hövels A, Büller HR, et al. NOACs replace VKA as preferred oral anticoagulant among new patients: a drug utilization study in 560 pharmacies in The Netherlands. Thromb J 2018; 16: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. European Commission DG Research and Innovation. Ethics and Data Protection, https://ec.europa.eu/info/sites/info/files/5._h2020_ethics_and_data_protection.pdf (2018).
- 15. van den Heuvel JM, Farzan N, van Hoek M, et al. Mining treatment patterns of glucose-lowering medications for type 2 diabetes in the Netherlands. BMJ Open Diabetes Res Care 2020; 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Australia 2009; 190: S54–S60. [DOI] [PubMed] [Google Scholar]
- 17. Williams ER, Guthrie E, Mackway-Jones K, et al. Psychiatric status, somatisation, and health care utilization of frequent attenders at the emergency department: a comparison with routine attenders. J Psychosom Res 2001; 50: 161–167. [DOI] [PubMed] [Google Scholar]
- 18. Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci 2015; 40: 219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cabibel V, Alexandre F, Oliver N, et al. Psychoactive medications in chronic obstructive pulmonary disease patients: from prevalence to effects on motor command and strength. Respir Med 2019; 159: 105805. [DOI] [PubMed] [Google Scholar]
- 20. Wang M-T, Tsai C-L, Lin CW, et al. Association between antipsychotic agents and risk of acute respiratory failure in patients with chronic obstructive pulmonary disease. JAMA Psychiatry 2017; 74: 252–260. [DOI] [PubMed] [Google Scholar]
- 21. Chen S-J, Yeh C-M, Chao T-F, et al. The use of benzodiazepine receptor agonists and risk of respiratory failure in patients with chronic obstructive pulmonary disease: a nationwide population-based case–control study. Sleep 2015; 38: 1045–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Roth T. Hypnotic use for insomnia management in chronic obstructive pulmonary disease. Sleep Med 2009; 10: 19–25. [DOI] [PubMed] [Google Scholar]
- 23. Omachi TA, Blanc PD, Claman DM, et al. Disturbed sleep among COPD patients is longitudinally associated with mortality and adverse COPD outcomes. Sleep Med 2012; 13: 476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McNicholas WT, Verbraecken J, Marin JM. Sleep disorders in COPD: the forgotten dimension. Euro Res Rev 2013; 22: 365–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dalgard FJ, Gieler U, Tomas-Aragones L, et al. The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol 2015; 135: 984–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dominguez P, Han J, Li T, et al. Depression and the risk of psoriasis in US women. J Eur Acad Dermatol Venereol 2013; 27: 1163–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hanania NA, Müllerova H, Locantore NW, et al. Determinants of depression in the ECLIPSE chronic obstructive pulmonary disease cohort. Am J Respir Crit Care Med 2011; 183: 604–611. [DOI] [PubMed] [Google Scholar]
- 28. Postma DS, Rabe KF. The asthma–COPD overlap syndrome. N Engl J Med 2015; 373: 1241–1249. [DOI] [PubMed] [Google Scholar]
- 29. Di Marco F, Santus P, Centanni S. Anxiety and depression in asthma. Curr Opin Pulm Med 2011; 17: 39–44. [DOI] [PubMed] [Google Scholar]
- 30. Van Gool CH, Kempen GI, Penninx BW, et al. Relationship between changes in depressive symptoms and unhealthy lifestyles in late middle aged and older persons: results from the Longitudinal Aging Study Amsterdam. Age Ageing 2003; 32: 81–87. [DOI] [PubMed] [Google Scholar]
- 31. Kunik ME, Roundy K, Veazey C, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest 2005; 127: 1205–1211. [DOI] [PubMed] [Google Scholar]
- 32. Simon GE. Evidence review: efficacy and effectiveness of antidepressant treatment in primary care. Gen Hosp Psychiatry 2002; 24: 213–224. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-2-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-3-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-4-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-5-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-6-tar-10.1177_1753466620961696 for Higher prescription of antidepressants and/or anxiolytics among chronic obstructive pulmonary disease patients by Charlotte E. Pelgrim, Jan Maurik van den Heuvel, Gert Folkerts, Johan Garssen, Anke H. Maitland-van der Zee and Aletta D. Kraneveld in Therapeutic Advances in Respiratory Disease