Abstract
The nuclear factor kappa B (NF-kB) family of transcription factors plays an essential role as stressors in the cellular environment, and controls the expression of important regulatory genes such as immunity, inflammation, death, and cell proliferation. NF-kB protein is located in the cytoplasm, and can be activated by various cellular stimuli. There are two pathways for NF-kB activation, as the canonical and non-canonical pathways, which require complex molecular interactions with adapter proteins and phosphorylation and ubiquitinase enzymes. Accordingly, this increases NF-kB translocation in the nucleus and regulates gene expression. In this study, the concepts that emerge in different cellular systems allow the design of NF-kB function in humans. This would not only allow the development for rare diseases associated with NF-kB, but would also be used as a source of useful information to eliminate widespread consequences such as cancer or inflammatory/immune diseases.
Keywords: Cancer, Immunity, Inflammation, NF-κB, Signaling
Introduction
The NF-kB transcription factor family consists of five distinct proteins as follows: RelA, RelB, c-Rel, p100, and p150 (Fig. 1A).1, 2, 3 They have rel homology domain (RHD), which is essential for dimerization, DNA binding, and interaction with lκB inhibitors. The domain is named for its sequence similarity with the v-rel oncogene from the T-strain of reticuloendotheliosis virus (REV), which causes the embryonic lymphatic tumor.4 Also, RelA, RelB, and c-Rel have transcription activation domain (TAD). Also, TADs are absent at p100 and p105, and these proteins are production Precursor of NF-kB, which after proteolysis, produces the p52 and p50 subunits.5, 6, 7 Therefore, NF-kB is a generic name and can be included in a family of dimeric proteins produced by different compounds.8, 9, 10 Moreover, all of them have the p50, p52, RelA, RelB, and c-Rel subunits. One of the widely studied NF-kB dimers is p50/RelA, which is expressed in most cells.3
Figure 1.
Protein family members and structure. (A) NF-kB family members. Proteins are shown based on their functional domain. The two serine residues (in the phosphorylation regions) and the lysine residues (in the ubiquitination region) participate in p100 processing to produce p52. (B) IkB family members. Proteins are shown with their functional domains. ANK: ankyrin Repeats. The involvement of serine residues (phosphorylation sites) and lysine residues (ubiquitination sites) in IkB dysregulation has been demonstrated.103
NF-κB main function
NF-kB proteins can regulate the expression of hundreds gene, which regulate important physiological processes such as inflammation, immunity, proliferation, and cell death.11 Since NF-kB activity is spontaneously regulated by a number of different stimuli, NF-kB proteins can be considered as regulators of cellular homeostasis.12, 13, 14
A key function of NF-κB is controlling the immune response at various stages. Immunity is associated with inflammation, and an appropriate and integrated functioning of both processes is essential.3 The first response is innate immune response, facilitated by specific cell types such as macrophages and dendritic cells, which recognize bacteria and viruses through pathogen-associated molecular patterns (PAMPS).19 Among these receptors are members of the toll-like receptor (TLR) family like TLR4, which is involved in the induction of NF-kB protein after recognition of bacterial lipopolysaccharide (LPS).20
One of the major activities of NF-kB proteins is controlling the inflammation process, which indicate that, they targeted the body's complex defense mechanisms under inflammation conditions.15 This is performed by positively and negatively regulating expressions of many important genes in the essential process including chemokines and pro-inflammatory cytokines. Cytokines such as tumor necrosis factor alpha (TNF-α) and interleukin 1 beta (IL-1β) are potent inducers of NF-kB.3,16 In addition, NF-κB also contributes to the resolution of inflammation, which then disrupts the function of NF-kB.17,18
The second response is adaptive immune response due to cell or humoral, and allow the identification of non-self-antigen and antibody synthesis.21 Cell-mediated immunity consists of T lymphocytes that, through their T-cell receptor (TCR), are able to identify antigens processed by antigen-presenting cells (APCs).3 These cells are those that are involved in innate immune response and require the activation of NF-kB.3 Accordingly, activation of T cells via TCR enables their proliferation and differentiation to obtain the effector function required for NF-kB.3 Humoral-mediated immune consists of B lymphocytes that directly detect B antigens through the B-cell receptor (BCR). Thus, NF-kB plays critical roles in the immune response as follows: first as a regulator of B cell lymphoid tissue formation and provides B cell differentiation and maturation; and second, it is targeted by BCR as an important element in B-cell survival, which ultimately controls NF-kB secondary lymphoid regeneration, whose poor progression has important consequences on lymphocyte activation. Due to the multifaceted role of NF-kB in immunity, malfunctioning of this transcription factor may decrease immunogenicity or autoimmunity.3
NF-kB transcription factors are also involved in cell proliferation and cell death. Regarding the case of cell proliferation, they have been reported to regulate the expression of several cell cycle regulators such as cyclin A, cyclin D1 or cyclin-dependent kinase 6 (CDK6).22 NF-kB activation is an essential step to protect the cell against the TNF-α-induced apoptosis. Also, these two functions are related to cancer.23 In most cases, cancer cells express NF-kB combination activation, unregulated proliferation or insensitivity to cell death.23,24
Finally, out of the functions of NF-kB as discussed in the following chapters, is the central nervous system (CNS). However, there is a controversy regarding the precise role of NF-kB in CNS progression, indicating that, NF-kB regulates neuronal plasticity through response to neurotrophic factors or synaptic transmission and participation in neuronal survival.25,26
Standard pathway activating NF-kB
One of the major features of NF-kB transcription factors is their association with members of the IKB inhibitor family in the cell cytoplasm. This protein family consists of three members (IkBα, IkBβ, and IkBε) having very similar structures (Fig. 1B).27, 28, 29 At the N-terminus, they have a conserved sequence containing two serine residues (DSGXXS) that can be altered by phosphorylation, in while half of their C-terminus contains a series of ankyrin repeats indicating their tendency for RHDs of NF-kB dimers.3
The cytoplasmic position of the NF-kB protein is determined by stimulation of its nuclear localization signal (NLS), which is achieved from IkB ankyrin repeats. After stimulation, IkBs are phosphorylated, and this change stimulates their ubiquitination and degradation by the 26S proteasome. Then, the released NF-kB dimers can enter the nucleus and bind to conserved DNA motifs for positive and negative regulations of gene expression (5ʹ-GGGRNYYYCC-3ʹ), in which R purine, Y pyrimidine, and N are any nucleotide type.3
It has been shown that, double-serine phosphorylation in the conserved IkB sequence is mediated by a kinase complex called IkB kinase (IKK).30 Also, its main components include two catalytic subunits, IKK1 and IKK2, and one regulatory subunit, as the NF-kB essential modulator. IKK activation is automatically regulated by phosphorylation.3,31, 32, 33 The kinase can be involved in IKK (via autophosphorylation) or the upstream TGFβ-activated kinase (TAK) complex.34, 35, 36, 37 This complex consists of a catalytic subunit of TAK1 and two regulatory subunits as follows: TAB1 and TAB2 or TAB3. In addition to IKK activating, the TAK complex can also activate MKKs and MAP kinases such as p38 and JNK.38,39
The domain components of IKK and TAK complexes represent their function in NF-kB signaling. Moreover, IKK1 and IKK2 are two related kinases, in which the domain kinase has phosphorylation activation sites at the N-terminus, the SSD mediates IKK1/IKK2 dimerization in the middle part, and the NEMO-binding domain (NBD) at the C-terminus.40, 41, 42 NBD is a helical dimeric protein containing the IKK interaction sequence at the N-terminus, which its first domain has a tendency toward ubiquitin in the middle part and a zinc finger (ZF) structure at the C-terminus.3,43 NEMO ubiquitin binding (NUB) and ZF domains have been shown to contribute to ubiquitin detection.44 TAK1 is a MEKK family kinase containing a kinase domain at N-terminus and a TAB2/TAB3 binding region at the C-terminus.3 The N-terminus kinase domain interacts with TAB1, which is a regulatory/scaffold protein containing a large helix at the N-terminus and a short sequence interacting with TAK1 at the C-terminus. Finally, TAB2 and TAB3 are similar regulatory proteins that have a coupling of ubiquitin conjugation to ER degradation (CUE) domain at the N-terminus and Npl4 zinc finger (NZF) at the C-terminus, which both of them tend to ubiquitin. In addition, they have twisted domains that have mediate interaction with TAK1.3
Ubiquitination
Ubiquitination plays an important role at different stages of the NF-kB activation process. These post-translational changes are involved in protein complex (Fig. 2).45,46 Ubiquitin is a small 8-kDa protein synthesized as a precursor for a polypeptide. In the first step, ubiquitin was activated by the ubiquitin-activating enzyme E1 through the ATP-dependent reaction. Then, the activated ubiquitin was transferred to the ubiquitin conjugation enzyme E2 to form the E2-ubiquitin thioester. Finally, in the presence of ubiquitin protein ligase E3, ubiquitin was covalently bound to the target protein by the isopeptide bonding between the carboxyl ubiquitin end and the ε-amine lysine group of the protein. Also, there are two E1 enzymes, tens of E2 enzymes, and hundreds of E3 enzymes that result in specific substrate specificity.3
Figure 2.
The ubiquitination process. The various steps required to change the substrate by mono and poly-ubiquitination are shown.104
In cells, proteins can be altered by one ubiquitin chain or several ubiquitin chains. In fact, ubiquitin contains seven lysines (K6, K11, K27, K29, K33, K48, and K63) that enable the poly-ubiquitination process.3 The type of chains synthesized from ubiquitin, named after the lysine residue, depends on E2 and also affects the fate of the modified protein. K48-associated polyubiquitin chains are identified by the recognition and degradation by the 26S proteasome.45 In the NF-kB signaling pathway, this polyubiquitination was observed at IkB levels after being phosphorylated by IKK, leading them to degrade. Other types of polyubiquitin chains like the K63-linked polyubiquitin chain, do not result in degradation; however, by interacting with substrates containing ubiquitin-binding domains alter the activity of the modified substrate.3 Ubiquitin-binding domains have been identified, most of which have identified a specific type or a limited number of polyubiquitin conformations.47 Accordingly, this provides another level of regulation of protein–protein interactions.3
Recently, it has been shown that, proteins can be altered by other types of polyubiquitin chains. A protein complex reported as linear ubiquitin chain assembly complex (LUBAC), results in the formation of “linear” chains or the chains associated with M1 polyubiquitin.48 In this case, diubiquitin occurs between the C-terminus (Gky76) and the N-terminus (Met1) of the remaining ubiquitin. Three different components of LUBAC include the followings: E3 ligase heme-oxidized IRP2 ubiquitin ligase-1 (HOIL-1), HOIL-1-interacting protein (HOIP) also called ring finger protein 31 (RNF31), and the SHANK associated RH domain interactor (SHARPIN) adapter.49,50 HOIL-1 contains UBL (pseudo-ubiquitin) domain at the N-terminus that interacts with several proteins, which among them HIOP, as a type of NZF (pseudo NplA zinc finger), binds to linear polyubiquitin and RBR and IBR domains.51, 52, 53 HOIP has a PUB domain that interacts with OTU deubiquitinase with linear linkage specificity (OTULIN), two NZF domains include the UBA domain responsible for interacting with HOIL-1 and the RBR catalytic domain.54,55 Sharpin contains a Pextrin homology highly twisted region at the N-terminus, which interacts with HOIP through the UBL domain. In addition, Sharpine has two NZF domains.3
As mentioned earlier, NEMO and TAB2/Tab3 have ubiquitin-binding domains. It has been shown that, the NUB domain/NEMO zinc finger segment identifies K63 polyubiquitin chains and linear chains,56 while the NZF-dependent TAB2/TAB3 chains identify K63-related chains.43,57,58
TNF-R1 signaling pathway
The first TNF-α signaling pathway requires the binding of TNF-α to TNFR1 (Fig. 3).59,60 This starts by connecting their death domain (DD) to the DD of TNFR-1, using TNF receptor-associated death domain protein (TRADD) and receptor interacting Serine/Threonine kinase 1 (RIPK-1) adapter molecules. Binding of E3 ligase of TRAF2/TRAF5 to TRADDcauses two other E3s c-IAP1 and c-IAP2 to modulate.3 RIPK-1 along with K63-linked polyubiquitin chains. Then, polyubiquitinated RIPK-1 with K63 via HOIL-1 subunit absorbs LUBAC, through TAB2/3 subunits absorb TAK complex, and through NEMO, they uptake IKK. Linear poly-ubiquitination of RIPK-1 and NEMO by LUBAC is more stable; and therefore, called messenger receptor complex (TNF-RSC), termed complex I.3,43 The masses induced by different compounds result in the phosphorylation of IKK by TAK1. The catalytic subunit of the TAK complex is involved, and IKK activation induces NF-kB release and stimulates transcription of its target genes.3,43
Figure 3.
TNF-R1 signaling pathway. The negative regulators of the ubiquitinated protein pathway have not been clearly shown.3
Ubiquitination events such as TNF-R1 signaling are regularly controlled through deubiquitinating enzymes (DUBs).
A20 is a protein with dual enzymatic activity (DUB/E3 ligase) encoded by the NF-kB induced gene TNF alpha induced protein 3 (TNFAIP3).61 A20 stops NF-κB activation by (1) deubiquitinating RIPK-1 and (2) polyubiquitinating RIP-1 to target it for degradation (proteolysis). CYLD lysine 63 deubiquitinase (CYLD) can hydrolyze the linear chain or chain associated with K63 and work on RIPK-1, NEMO, and TRAF-2.43,62, 63, 64 USP2 is another type of DUB that acts in level of RIPK-1.65 Finally, it has been shown that, OTULIN is a type of DUB tends to linear ubiquitin chains and inhibits LUBAC activity.66,67
TNF-α regulation of cell death
NF-kB activation in response to TNF-α also leads to an increase of cellular FLICE-like inhibitory protein (c-FLIP), which plays an important role in controlling the fate of cells.68 Immediately after TNF-RSC, TRADD, and RIPK-1 components were transferred to the cytoplasm via their DDs, they couple with the adapter fas-associated death domain (FADD) and caspase-8 primer, creating a new complex called complex IIa.68 In the case of NF-kB-induced c-FLIP synthesis, caspase-8/c-FILP dimer inhibits caspase-8 activity. If NF-kB activation does not occur, the activated caspase-8 in complex IIa through apoptosis targets cell death. Thus, activation of NF-kB in cells is stimulated by TNF-α and enables cell survival.3
It has been shown that, TNF-α can induce another form of cell death,69 termed necroptosis, which is controlled by components of the NF-kB pathway. Necroptosis contains another protein of complex IIa known as receptor-interacting protein kinase 3 (RIPK3). When apoptosis occurs, RIPK3 is proteolyzed by caspase-8. Also, in case of inhibition of caspase-8 enzymatic activity or lack of FADD; RIPK1 and RIPK3 are both stabilized and form a new complex (called complex IIb) leading to necroptosis. This state of cell death requires mixed lineage kinase domain like pseudokinase (MLKL),69 which is a substrate of RIPK3 kinase activity. After phosphorylation, MLKL induces pores in the cell membrane and releases cytoplasmic compounds into the extracellular environment, which destroys the cells.70,71 Accordingly, this release induce an inflammation reaction, which is a reaction that does not occur in apoptotic cell death. In this case, death involves nuclear accumulation and membrane organization changes, which eliminates non-leaky cell components.3
IL-1βR/TLR4 signaling pathway
The IL-1R and TLR signaling pathways are similar, due to the presence of a conserved domain called Toll/interleukin-1 receptor (TIR) domain that provides the conditions for creating the signaling complexes of several similar proteins in these receptors (Fig. 4).72 At the cell surface, IL-1R is associated with interleukin-1 receptor accessory protein (IL-1RacP), which is responsible for IL-1β detection and message transmission. TLR4 is selected as the TLR model linked to the MD-2 receptor, and represents the LPS (lipopolysaccharide) receptor, which is an outer wall component of gram-negative bacteria.3 Other TLRs tend to some compounds such as triacetylated lipoproteins (TLR1/TLR2); diacetylated lipoproteins; and peptidoglycans from gram-positive bacteria and lipoteichoic acid (TLR2/TLR6), dsRNA and polyI:C (TLR3) viral, flagellins (TLR5), single stranded RNA (TLR7 and TLR8), and bacterial and mycobacterial CpG-DNA (TLR9).3
Figure 4.
IL-1R and TLR4 signaling pathways.105
After utilizing their ligands, IL-1R/IL-1RacP and TLR4/MD-2 are used through TIR domains. The TIR domain contains Myd88 adapter that has also DD. This DD domain is involved in activation of interleukin-1 receptor-associated kinase (IRAK4, IRAK1), and TNF receptor associated factor (TRAF6) E3 ligase. After phosphorylation, IRAK1 is ubiquitinated by IRAK4, IRAK1, and TRAF6 and is released by K63 from receptor and absorbs TAK and IKK complexes.73, 74, 75 This is performed by ubiquitin-binding subunits (TAB2/TAB3 and NEMO, respectively) and induces phosphorylation and IKK activation. The E2 conjugation enzyme (Uev1AUbc13) is specifically involved in the production of these K63 ubiquitin chains and TRAF6-related E2,43,67 as well as through cellular features, which leads to synthesis of K63-related chains.76 However, a number of LUBAC samples are required for IL-1/TLR signaling.77,78 The compounds that are changed by linear chains are less well known. Also, NEMO may be one of these linear chains reported for the TNF-R1 pathway as well as IRAK1.3,43
BCR/TCR signaling pathway
Both, the BCR and the TCR, pathway overlap in NF-kB activation (Fig. 5).79,80 About TCR, α and β chains regarding TCR at the surface of T cells with ζ and ε/δ/γ chains related to CD3 molecules. Also, TCR signaling is targeted by major histocompatibility complex (MHC) molecules principal adaptation complex and antigenic peptides. Antigenic peptides are produced by APCs such as dendritic cells and macrophages.3
Figure 5.
BCR and TCR pathways.106
The onset of signaling has come from the activation of members of the tyrosine kinase family Src (sarcoma), Fyn, and Lck. Activation of these tyrosine kinases induces tyrosine phosphorylation of immune receptor tyrosine-based activation motifs (ITAMs) in CD3 and the utilization of zeta-chain-associated protein kinase-70 (ZAP70) by Src homology 2 (SH2) domains. Due to ZAP70 phosphorylation and activation, adapter proteins such as linker for activation of T cells (LAT) and SH2 domain-containing leukocyte protein of 76 kDa (SLP76) participate in phospholipase Cγ1 (PLCγ1) activation.3
BCR contains antigen-binding IgH heavy chain and antigen-binding IgL light chain and messages are transmitted by the message transfer section or CD79A/CD79B protein containing ITAMs. Tyrosine amino acid of these motifs are phosphorylated by Lyn kinase and other src kinases families such as Fyn and Blk. This allows Syk to be used by SH2 domains and activated.3 Signaling is expanded by BLNK and BTK, and activates and phosphorylates PLCγ2.
After activation of PLCγs, distal signaling is equally achieved in the TCR and BCR pathways. In fact, PLCγs hydrolyze inositol phospholipids (PIP2) to inositol triphosphate (IP3) and diacyl-glycerol (DAG). IP3 production stimulates intracellular calcium, and by DAG, maximizes protein kinase C (PKC) activation. PKCϴ represents the activated isoforms in the downstream section of TCR,81 whereas PKCβ is downstream of BCR.82 Afterwards, PKCs act on caspase recruitment domain-containing membrane-associated guanylate kinase protein-1 (CARMA1) and mucosa associated lymphoid tissue lymphoma translocation protein 1 (MALT1), and cause CARMA1/BCL10/MALT1 (CBM) complex formation.83 In this complex, interaction of the caspase recruitment domain (CARD) part of CARMA1 with the CARD part of Bc110, causes CARMA1 to play the role of a scaffold protein, whereas its cyclic helical domain binds to MALT1. Accordingly, MALT1 interacts with TRAF6 to induce the K63-associated polyubiquitination in Bc110 and induces IKK uptake and activation through NEMO.43,84
NF-kB secondary activation pathway
The second known pathway for NF-kB activation is the secondary pathway.85,86 In this case, a key factor that control the activation process is NF-kB inducible kinase (NIK), which activates IKK1 dimer and phosphorylation of p100 leads to IKK.
The serine residue located at the p100 C-terminus is involved in p100 phosphorylation, and shows a degree of similarity to the conserved sequence of IkBs, and inducing its interaction with SCFβTRCP and K48-associated ubiquitination. In some specific cases, p100 polyubiquitination does not completely proteolyze it, but it rather causes p52 at the N-terminus. Since in cells, p100 tends to the RelB subunit and controls its cytoplasmic position, the production of NF-kB dimer is mediated by the activation of NF-kB and p52RelB secondary pathway.3
In activating the NF-kB pathway, NIK must be stable, which is destroyed in static cells. Components that contribute to its instability include cIAP1/2, TRAF2, and TRAF3. Also, the components form the NIK ubiquitin ligase (E3) complex. cIAP1/2 are E3 ligases that induce K48 NIK-associated polyubiquitination.3,87 Moreover, these ligases are degraded by the proteasome. TRAF2 and TRAF3 are scaffold components that interact with NIK and cIAP.88,89
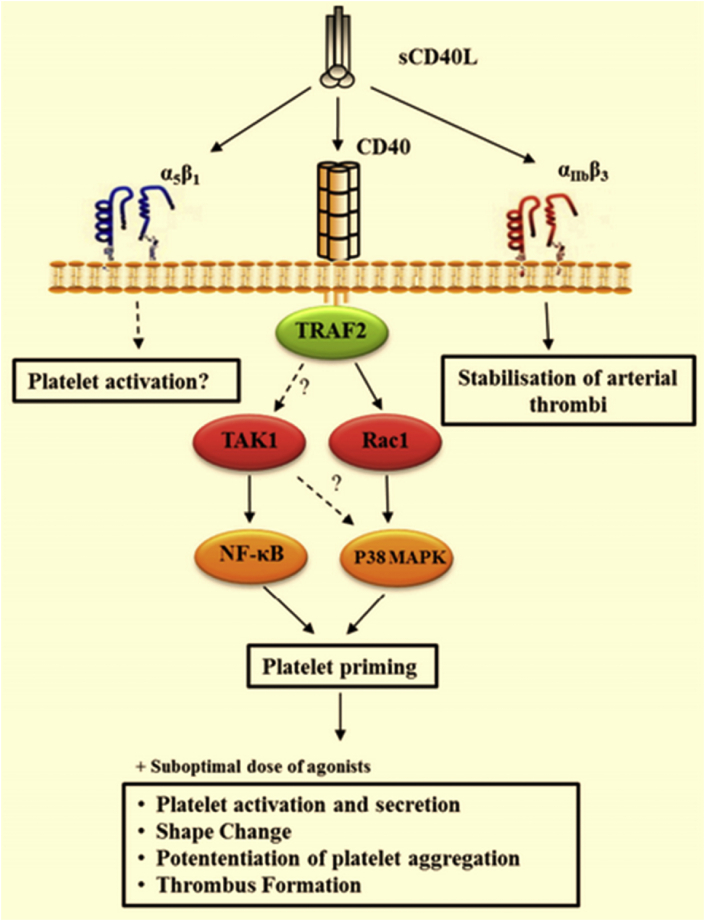
Several receptors have been reported to activate the NF-kB secondary pathway. Also, CD40 ligand (CD40L) and lymphotoxin β receptor (LTβR) are reported to be among these receptors (Fig. 6). After interaction of the receptors with their ligands, the NIK E3 complex can be used. This induces cIAP1/2 polyubiquitination by TRAF2 and targets the identification and modification of the TRAF3 poly-ubiquitin K48 chain. TRAF3 proteolysis causes NIK stability and IKK1 phosphorylation, and also induces NF-kB secondary pathway activation.90, 91, 92, 93, 94, 95, 96
Figure 6.
NF-kB secondary pathway activation. CD40 signaling pathways.107
A specific collection of receptors that activate NF-kB secondary pathway act in the development and maintenance of peripheral lymph nodes (LTβR), maturation of peripheral B cells, B cell activation and differentiation, germinal center formation and antibody isotype switching, dendritic cell maturation, and antigen formation CD40 or osteoclastogenesis. The primary and secondary NF-kB activation methods do not independently operate; however, are often considered to have separate operation. In many cases, interactions between them have been observed, indicating the integration of these two methods.97 For example, receptors that activate the secondary can simultaneously activate the main pathway. As a consequence, the expression or activity of several combinations of one path is controlled by the other one. It has been shown that, NF-kB main dimers regulate the RelB transcription, which its product associates with p52.98 On the other hand, RelB can form dimers with p50 and can be controlled by IκBs.99 In addition, as observed in tumor suppressor WW domain containing oxidoreductase (WWOX), genes regulated by the secondary pathway may control the main pathway.100 Eventually, IkBδ is derived from the p100 fragment containing ankyrin, which generates negative feedback on the main NF-kB signaling.101,102
Conclusion
Although the secondary pathway has more limited functions compared to the primary NF-kB activation pathway, it plays an important role in controlling immune-related events such as B cell maturation, peripheral lymphoid development, and thymic development. In humans, mutations affect three major components of this pathway (NIK kinase initiator and its effector, p100/p52 subunits, and NF-kB RelB subunits). In each one of the cases, immunodeficiency is mainly discovered by hypogammaglobulinemia with re-infection resulting from B-cell dysfunction and specific abnormalities. Accordingly, this affects the activation of the secondary pathway in an organism and confirms previous reports on mice with defects.
Inherited diseases caused by NF-kB failure signaling lead to a wide variety of abnormalities in the immune system, vascular, skin, bone, and CNS. On the one hand, it allows the comparison of these abnormalities with those that were observed in similar components in mice, and on the other hand, assigns specific defects observed in humans to molecular abnormalities. All of this information should help in designing and approving the treatment.
It is also clear that, the identification of NF-kB-related genetic diseases can be considered as an appropriate strategy for identifying the essential signaling pathways. By completing studies on mice and validating them on humans, the concepts that arise in this or different cellular systems allow the design of NF-kB function in humans. This will not only enable the development of treatment for rare diseases associated with NF-kB, but will also be used as a source of very useful information to address widespread consequences such as cancer or inflammatory/immune diseases.
Conflict of Interests
The authors declared no conflict of interests.
Footnotes
Peer review under responsibility of Chongqing Medical University.
Contributor Information
Mohammad Reza Zinatizadeh, Email: zinati3333@gmail.com.
Seyed Rouhollah Miri, Email: srmiri@sina.tums.ac.ir.
References
- 1.Karin M., Ben-Neriah Y. Phosphorylation meets ubiquitination: the control of NF-κB activity. Annu Rev Immunol. 2000;18(1):621–663. doi: 10.1146/annurev.immunol.18.1.621. [DOI] [PubMed] [Google Scholar]
- 2.Hayden M.S., Ghosh S. Shared principles in NF-κB signaling. Cell. 2008;132(3):344–362. doi: 10.1016/j.cell.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 3.Courtois G., Pescatore A., Gautheron J., Fusco F., Ursini M.V., Senegas A. Springer; 2015. NF-κB-Related Genetic Diseases. [Google Scholar]
- 4.Walker W.H., Stein B., Ganchi P.A. The v-rel oncogene: insights into the mechanism of transcriptional activation, repression, and transformation. J Virol. 1992;66(8):5018–5029. doi: 10.1128/jvi.66.8.5018-5029.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frederiksen A.L., Larsen M.J., Brusgaard K. Neonatal high bone mass with first mutation of the NF-κB complex: heterozygous de novo missense (p.Asp512Ser) RELA (Rela/p65) J Bone Miner Res. 2016;31(1):163–172. doi: 10.1002/jbmr.2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffmann A., Leung T.H., Baltimore D. Genetic analysis of NF-κB/Rel transcription factors defines functional specificities. EMBO J. 2003;22(20):5530–5539. doi: 10.1093/emboj/cdg534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsui R., Kearns J.D., Lynch C. IκBβ enhances the generation of the low-affinity NFκB/RelA homodimer. Nat Commun. 2015;6(1):1–10. doi: 10.1038/ncomms8068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fliegauf M., Bryant V.L., Frede N. Haploinsufficiency of the NF-κB1 subunit p50 in common variable immunodeficiency. Am J Hum Genet. 2015;97(3):389–403. doi: 10.1016/j.ajhg.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finck A., Van der Meer J.W., Schäffer A.A. Linkage of autosomal-dominant common variable immunodeficiency to chromosome 4q. Eur J Hum Genet. 2006;14(7):867–875. doi: 10.1038/sj.ejhg.5201634. [DOI] [PubMed] [Google Scholar]
- 10.Oberle E.J., Verbsky J.W., Routes J. A172: metaphyseal chondrodysplasia, ectodermal dysplasia, short stature, hypergammaglobulinemia, and spontaneous inflammation without infections in an extended family due to mutation in NFKB1A. Arthritis Rheumatol. 2014;66(S3):S224–S225. [Google Scholar]
- 11.Giuliani C., Bucci I., Napolitano G. The role of the transcription factor Nuclear Factor-kappa B in thyroid autoimmunity and cancer. Front Endocrinol. 2018;9:e471. doi: 10.3389/fendo.2018.00471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seok J., Warren H.S., Cuenca A.G. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci USA. 2013;110(9):3507–3512. doi: 10.1073/pnas.1222878110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takao K., Miyakawa T. Genomic responses in mouse models greatly mimic human inflammatory diseases. Proc Natl Acad Sci USA. 2015;112(4):1167–1172. doi: 10.1073/pnas.1401965111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warren H.S., Tompkins R.G., Moldawer L.L. Mice are not men. Proc Natl Acad Sci USA. 2015;112(4):e345. doi: 10.1073/pnas.1414857111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nathan C. Points of control in inflammation. Nature. 2002;420(6917):846–852. doi: 10.1038/nature01320. [DOI] [PubMed] [Google Scholar]
- 16.Shay T., Lederer J.A., Benoist C. Genomic responses to inflammation in mouse models mimic humans: we concur, apples to oranges comparisons won't do. Proc Natl Acad Sci USA. 2015;112(4):e346. doi: 10.1073/pnas.1416629111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lawrence T., Fong C. The resolution of inflammation: anti-inflammatory roles for NF-κB. Int J Biochem Cell Biol. 2010;42(4):519–523. doi: 10.1016/j.biocel.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 18.Takao K., Hagihara H., Miyakawa T. Reply to Warren et al. and Shay et al.: commonalities across species do exist and are potentially important. Proc Natl Acad Sci USA. 2015;112(4):E347–E348. doi: 10.1073/pnas.1417369111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janeway C.A., Jr., Medzhitov R. Innate immune recognition. Annu Rev Immunol. 2002;20(1):197–216. doi: 10.1146/annurev.immunol.20.083001.084359. [DOI] [PubMed] [Google Scholar]
- 20.Mak T.W., Saunders M.E. Elsevier; 2006. The Immune Response: Basic and Clinical Principles. [Google Scholar]
- 21.Iwasaki A., Medzhitov R. Regulation of adaptive immunity by the innate immune system. Science. 2010;327(5963):291–295. doi: 10.1126/science.1183021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ledoux A.C., Perkins N.D. NF-κB and the cell cycle. Biochem Soc Trans. 2014;42(1):76–81. doi: 10.1042/BST20130156. [DOI] [PubMed] [Google Scholar]
- 23.Zinatizadeh M.R., Momeni S.A., Zarandi P.K. The role and function of Ras-association domain family in cancer: a review. Genes Dis. 2019;6(4):378–384. doi: 10.1016/j.gendis.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karin M. Nuclear factor-κB in cancer development and progression. Nature. 2006;441(7092):431–436. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 25.Mattson M.P., Meffert M.K. Roles for NF-κB in nerve cell survival, plasticity, and disease. Cell Death Differ. 2006;13(5):852–860. doi: 10.1038/sj.cdd.4401837. [DOI] [PubMed] [Google Scholar]
- 26.Dresselhaus E.C., Meffert M.K. Cellular specificity of NF-κB function in the nervous system. Front Immunol. 2019;10:1043. doi: 10.3389/fimmu.2019.01043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beg A.A., Sha W.C., Bronson R.T., Baltimore D. Constitutive NF-κB activation, enhanced granulopoiesis, and neonatal lethality in IκBα-deficient mice. Genes Dev. 1995;9(22):2736–2746. doi: 10.1101/gad.9.22.2736. [DOI] [PubMed] [Google Scholar]
- 28.Klement J.F., Rice N.R., Car B.D. IκBα deficiency results in a sustained NF-κB response and severe widespread dermatitis in mice. Mol Cell Biol. 1996;16(5):2341–2349. doi: 10.1128/mcb.16.5.2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Page A., Navarro M., Garín M. IKKβ leads to an inflammatory skin disease resembling interface dermatitis. J Investig Dermatol. 2010;130(6):1598–1610. doi: 10.1038/jid.2010.28. [DOI] [PubMed] [Google Scholar]
- 30.Hinz M., Scheidereit C. The IκB kinase complex in NF-κB regulation and beyond. EMBO Rep. 2014;15(1):46–61. doi: 10.1002/embr.201337983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lahtela J., Nousiainen H.O., Stefanovic V. Mutant CHUK and severe fetal encasement malformation. N Engl J Med. 2010;363(17):1631–1637. doi: 10.1056/NEJMoa0911698. [DOI] [PubMed] [Google Scholar]
- 32.Zhu Mingzhao, Chin Robert K., Christiansen Peter A. NF-κB2 is required for the establishment of central tolerance through an Aire-dependent pathway. J Clin Investig. 2006;116(11):2964–2971. doi: 10.1172/JCI28326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leslie E.J., O'Sullivan J., Cunningham M.L. Expanding the genetic and phenotypic spectrum of popliteal pterygium disorders. Am J Med Genet A. 2015;167A(3):545–552. doi: 10.1002/ajmg.a.36896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sakurai H. Targeting of TAK1 in inflammatory disorders and cancer. Trends Pharmacol Sci. 2012;33(10):522–530. doi: 10.1016/j.tips.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 35.Sil A.K., Maeda S., Sano Y., Roop D.R., Karin M. IκB kinase-α acts in the epidermis to control skeletal and craniofacial morphogenesis. Nature. 2004;428(6983):660–664. doi: 10.1038/nature02421. [DOI] [PubMed] [Google Scholar]
- 36.Hu Y., Baud V., Oga T., Kim K.I., Yoshida K., Karin M. IKKα controls formation of the epidermis independently of NF-κB. Nature. 2001;410(6829):710–714. doi: 10.1038/35070605. [DOI] [PubMed] [Google Scholar]
- 37.Bartsocas C.S., Papas C.V. Popliteal pterygium syndrome. Evidence for a severe autosomal recessive form. J Med Genet. 1972;9(2):222–226. doi: 10.1136/jmg.9.2.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang C., Deng L., Hong M., Akkaraju G.R., Inoue J., Chen Z.J. TAK1 is a ubiquitin-dependent kinase of MKK and IKK. Nature. 2001;412(6844):346–351. doi: 10.1038/35085597. [DOI] [PubMed] [Google Scholar]
- 39.Pannicke U., Baumann B., Fuchs S. Deficiency of innate and acquired immunity caused by an IKBKB mutation. N Engl J Med. 2013;369(26):2504–2514. doi: 10.1056/NEJMoa1309199. [DOI] [PubMed] [Google Scholar]
- 40.Burns S.O., Plagnol V., Gutierrez B.M. Immunodeficiency and disseminated mycobacterial infection associated with homozygous nonsense mutation of IKKβ. J Allergy Clin Immunol. 2014;134(1):215–218. doi: 10.1016/j.jaci.2013.12.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mousallem T., Yang J., Urban T.J. A nonsense mutation in IKBKB causes combined immunodeficiency. Blood. 2014;124(13):2046–2050. doi: 10.1182/blood-2014-04-571265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nielsen C., Jakobsen M.A., Larsen M.J. Immunodeficiency associated with a nonsense mutation of IKBKB. J Clin Immunol. 2014;34(8):916–921. doi: 10.1007/s10875-014-0097-1. [DOI] [PubMed] [Google Scholar]
- 43.Zinatizadeh M.R., Masoumalinejad Z., Nejatizadeh A., Shekari M., Parnak F., Zaree F. A review of NEMO protein and its relationship with genetic diseases. J Genet Genome Res. 2018;5(1):33. [Google Scholar]
- 44.Laplantine E., Fontan E., Chiaravalli J. NEMO specifically recognizes K63-linked poly-ubiquitin chains through a new bipartite ubiquitin-binding domain. EMBO J. 2009;28(19):2885–2895. doi: 10.1038/emboj.2009.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Courtois G., Fauvarque M.O. The many roles of ubiquitin in NF-κB signaling. Biomedicines. 2018;6(2):e43. doi: 10.3390/biomedicines6020043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pickart C.M., Eddins M.J. Ubiquitin: structures, functions, mechanisms. Biochim Biophys Acta. 2004;1695(1–3):55–72. doi: 10.1016/j.bbamcr.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 47.Hurley J.H., Lee S., Prag G. Ubiquitin-binding domains. Biochem J. 2006;399(3):361–372. doi: 10.1042/BJ20061138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kirisako T., Kamei K., Murata S. A ubiquitin ligase complex assembles linear polyubiquitin chains. EMBO J. 2006;25(20):4877–4887. doi: 10.1038/sj.emboj.7601360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sasaki K., Iwai K. Roles of linear ubiquitinylation, a crucial regulator of NF-κB and cell death, in the immune system. Immunol Rev. 2015;266(1):175–189. doi: 10.1111/imr.12308. [DOI] [PubMed] [Google Scholar]
- 50.Shimizu Y., Taraborrelli L., Walczak H. Linear ubiquitination in immunity. Immunol Rev. 2015;266(1):190–207. doi: 10.1111/imr.12309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boisson B., Laplantine E., Prando C. Immunodeficiency, autoinflammation and amylopectinosis in humans with inherited HOIL-1 and LUBAC deficiency. Nat Immunol. 2012;13(12):1178–1186. doi: 10.1038/ni.2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Douglas T., Champagne C., Morizot A., Lapointe J.M., Saleh M. The inflammatory caspases-1 and -11 mediate the pathogenesis of dermatitis in sharpin-deficient mice. J Immunol. 2015;195(5):2365–2373. doi: 10.4049/jimmunol.1500542. [DOI] [PubMed] [Google Scholar]
- 53.Nilsson J., Schoser B., Laforet P. Polyglucosan body myopathy caused by defective ubiquitin ligase RBCK1. Ann Neurol. 2013;74(6):914–919. doi: 10.1002/ana.23963. [DOI] [PubMed] [Google Scholar]
- 54.Wang K., Kim C., Bradfield J. Whole-genome DNA/RNA sequencing identifies truncating mutations in RBCK1 in a novel Mendelian disease with neuromuscular and cardiac involvement. Genome Med. 2013;5(7):e67. doi: 10.1186/gm471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Boisson B., Laplantine E., Dobbs K. Human HOIP and LUBAC deficiency underlies autoinflammation, immunodeficiency, amylopectinosis, and lymphangiectasia. J Exp Med. 2015;212(6):939–951. doi: 10.1084/jem.20141130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hadian K., Griesbach R.A., Dornauer S. NF-κB essential modulator (NEMO) interaction with linear and lys-63 ubiquitin chains contributes to NF-κB activation. J Biol Chem. 2011;286(29):26107–26117. doi: 10.1074/jbc.M111.233163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sato Y., Yoshikawa A., Yamashita M., Yamagata A., Fukai S. Structural basis for specific recognition of Lys 63-linked polyubiquitin chains by NZF domains of TAB2 and TAB3. EMBO J. 2009;28(24):3903–3909. doi: 10.1038/emboj.2009.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kulathu Y., Akutsu M., Bremm A., Hofmann K., Komander D. Two-sided ubiquitin binding explains specificity of the TAB2 NZF domain. Nat Struct Mol Biol. 2009;16(12):1328–1330. doi: 10.1038/nsmb.1731. [DOI] [PubMed] [Google Scholar]
- 59.Silke J. The regulation of TNF signalling: what a tangled web we weave. Curr Opin Immunol. 2011;23(5):620–626. doi: 10.1016/j.coi.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 60.Walczak H. TNF and ubiquitin at the crossroads of gene activation, cell death, inflammation, and cancer. Immunol Rev. 2011;244(1):9–28. doi: 10.1111/j.1600-065X.2011.01066.x. [DOI] [PubMed] [Google Scholar]
- 61.Das T., Chen Z., Hendriks R.W., Kool M. A20/Tumor necrosis factor α-induced protein 3 in immune cells controls development of autoinflammation and autoimmunity: lessons from mouse models. Front Immunol. 2018;(9):e104. doi: 10.3389/fimmu.2018.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Trompouki E., Hatzivassiliou E., Tsichritzis T., Farmer H., Ashworth A., Mosialos G. CYLD is a deubiquitinating enzyme that negatively regulates NF-κB activation by TNFR family members. Nature. 2003;424(6950):793–796. doi: 10.1038/nature01803. [DOI] [PubMed] [Google Scholar]
- 63.Brummelkamp T.R., Nijman S.M., Dirac A.M., Bernards R. Loss of the cylindromatosis tumour suppressor inhibits apoptosis by activating NF-κB. Nature. 2003;424(6950):797–801. doi: 10.1038/nature01811. [DOI] [PubMed] [Google Scholar]
- 64.Kovalenko A., Chable-Bessia C., Cantarella G., Israël A., Wallach D., Courtois G. The tumour suppressor CYLD negatively regulates NF-κB signalling by deubiquitination. Nature. 2003;424(6950):801–805. doi: 10.1038/nature01802. [DOI] [PubMed] [Google Scholar]
- 65.Mahul-Mellier A.L., Pazarentzos E., Datler C. De-ubiquitinating protease USP2a targets RIP1 and TRAF2 to mediate cell death by TNF. Cell Death Differ. 2012;19(5):891–899. doi: 10.1038/cdd.2011.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Keusekotten K., Elliott P.R., Glockner L. OTULIN antagonizes LUBAC signaling by specifically hydrolyzing Met1-linked polyubiquitin. Cell. 2013;153(6):1312–1326. doi: 10.1016/j.cell.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fiil B.K., Damgaard R.B., Wagner S.A. OTULIN restricts Met1-linked ubiquitination to control innate immune signaling. Mol Cell. 2013;50(6):818–830. doi: 10.1016/j.molcel.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Micheau O., Tschopp J. Induction of TNF receptor I-mediated apoptosis via two sequential signaling complexes. Cell. 2003;114(2):181–190. doi: 10.1016/s0092-8674(03)00521-x. [DOI] [PubMed] [Google Scholar]
- 69.De Almagro M.C., Vucic D. Necroptosis: pathway diversity and characteristics. Semin Cell Dev Biol. 2015;39:56–62. doi: 10.1016/j.semcdb.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 70.Cai Z., Jitkaew S., Zhao J. Plasma membrane translocation of trimerized MLKL protein is required for TNF-induced necroptosis. Nat Cell Biol. 2014;16(1):55–65. doi: 10.1038/ncb2883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen X., Li W., Ren J. Translocation of mixed lineage kinase domain-like protein to plasma membrane leads to necrotic cell death. Cell Res. 2014;24(1):105–121. doi: 10.1038/cr.2013.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Narayanan K.B., Park H.H. Toll/interleukin-1 receptor (TIR) domain-mediated cellular signaling pathways. Apoptosis. 2015;20(2):196–209. doi: 10.1007/s10495-014-1073-1. [DOI] [PubMed] [Google Scholar]
- 73.Wisniewski S.A., Trzeciak W.H. A rare heterozygous TRAF6 variant is associated with hypohidrotic ectodermal dysplasia. Br J Dermatol. 2012;166(6):1353–1356. doi: 10.1111/j.1365-2133.2012.10871.x. [DOI] [PubMed] [Google Scholar]
- 74.Fujikawa H., Farooq M., Fujimoto A., Ito M., Shimomura Y. Functional studies for the TRAF6 mutation associated with hypohidrotic ectodermal dysplasia. Br J Dermatol. 2013;168(3):629–633. doi: 10.1111/bjd.12018. [DOI] [PubMed] [Google Scholar]
- 75.Ye H., Arron J.R., Lamothe B. Distinct molecular mechanism for initiating TRAF6 signalling. Nature. 2002;418(6896):443–447. doi: 10.1038/nature00888. [DOI] [PubMed] [Google Scholar]
- 76.Xu M., Skaug B., Zeng W., Chen Z.J. A ubiquitin replacement strategy in human cells reveals distinct mechanisms of IKK activation by TNFα and IL-1β. Mol Cell. 2009;36(2):302–314. doi: 10.1016/j.molcel.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tokunaga F., Sakata S., Saeki Y. Involvement of linear polyubiquitylation of NEMO in NF-κB activation. Nat Cell Biol. 2009;11(2):123–132. doi: 10.1038/ncb1821. [DOI] [PubMed] [Google Scholar]
- 78.Tarantino N., Tinevez J.Y., Crowell E.F. TNF and IL-1 exhibit distinct ubiquitin requirements for inducing NEMO-IKK supramolecular structures. J Cell Biol. 2014;204(2):231–245. doi: 10.1083/jcb.201307172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Paul S., Schaefer B.C. A new look at T cell receptor signaling to nuclear factor-κB. Trends Immunol. 2013;34(6):269–281. doi: 10.1016/j.it.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Niemann C.U., Wiestner A. B-cell receptor signaling as a driver of lymphoma development and evolution. Semin Cancer Biol. 2013;23(6):410–421. doi: 10.1016/j.semcancer.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Coudronniere N., Villalba M., Englund N., Altman A. NF-κB activation induced by T cell receptor/CD28 costimulation is mediated by protein kinase C-theta. Proc Natl Acad Sci USA. 2000;97(7):3394–3399. doi: 10.1073/pnas.060028097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Saijo K., Mecklenbräuker I., Santana A., Leitger M., Schmedt C., Tarakhovsky A. Protein kinase C beta controls nuclear factor κB activation in B cells through selective regulation of the IκB kinase α. J Exp Med. 2002;195(12):1647–1652. doi: 10.1084/jem.20020408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Thome M., Charton J.E., Pelzer C., Hailfinger S. Antigen receptor signaling to NF-κB via CARMA1, BCL10, and MALT1. Cold Spring Harb Perspect Biol. 2010;2(9) doi: 10.1101/cshperspect.a003004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Naito A., Yoshida H., Nishioka E. TRAF6-deficient mice display hypohidrotic ectodermal dysplasia. Proc Natl Acad Sci USA. 2002;99(13):8766–8771. doi: 10.1073/pnas.132636999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sun S.C. Non-canonical NF-κB signaling pathway. Cell Res. 2011;21(1):71–85. doi: 10.1038/cr.2010.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Razani B., Reichardt A.D., Cheng G. Non-canonical NF-κB signaling activation and regulation: principles and perspectives. Immunol Rev. 2011;244(1):44–54. doi: 10.1111/j.1600-065X.2011.01059.x. [DOI] [PubMed] [Google Scholar]
- 87.Willmann K.L., Klaver S., Doğu F. Biallelic loss-of-function mutation in NIK causes a primary immunodeficiency with multifaceted aberrant lymphoid immunity. Nat Commun. 2014;5(1):1–13. doi: 10.1038/ncomms6360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zarnegar B.J., Wang Y., Mahoney D.J. Noncanonical NF-κB activation requires coordinated assembly of a regulatory complex of the adaptors cIAP1, cIAP2, TRAF2 and TRAF3 and the kinase NIK. Nat Immunol. 2008;9(12):1371–1378. doi: 10.1038/ni.1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sharfe N., Merico D., Karanxha A. The effects of RelB deficiency on lymphocyte development and function. J Autoimmun. 2015;65:90–100. doi: 10.1016/j.jaut.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 90.Vallabhapurapu S., Matsuzawa A., Zhang W. Nonredundant and complementary functions of TRAF2 and TRAF3 in a ubiquitination cascade that activates NIK-dependent alternative NF-κB signaling. Nat Immunol. 2008;9(12):1364–1370. doi: 10.1038/ni.1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mitchell K., O'Sullivan J., Missero C. Exome sequence identifies RIPK4 as the Bartsocas-Papas syndrome locus. Am J Hum Genet. 2012;90(1):69–75. doi: 10.1016/j.ajhg.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kalay E., Sezgin O., Chellappa V. Mutations in RIPK4 cause the autosomal-recessive form of popliteal pterygium syndrome. Am J Hum Genet. 2012;90(1):76–85. doi: 10.1016/j.ajhg.2011.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Meylan E., Martinon F., Thome M., Gschwendt M., Tschopp J. RIP4 (DIK/PKK), a novel member of the RIP kinase family, activates NF-κB and is processed during apoptosis. EMBO Rep. 2002;3(12):1201–1208. doi: 10.1093/embo-reports/kvf236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kondo S., Schutte B.C., Richardson R.J. Mutations in IRF6 cause Van der Woude and popliteal pterygium syndromes. Nat Genet. 2002;32(2):285–289. doi: 10.1038/ng985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.De Groote P., Tran H.T., Fransen M. A novel RIPK4-IRF6 connection is required to prevent epithelial fusions characteristic for popliteal pterygium syndromes. Cell Death Differ. 2015;22(6):1012–1024. doi: 10.1038/cdd.2014.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Richardson R.J., Hammond N.L., Coulombe P.A. Periderm prevents pathological epithelial adhesions during embryogenesis. J Clin Investig. 2014;124(9):3891–3900. doi: 10.1172/JCI71946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shih V.F., Tsui R., Caldwell A., Hoffmann A. A single NFκB system for both canonical and non-canonical signaling. Cell Res. 2011;21(1):86–102. doi: 10.1038/cr.2010.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bren G.D., Solan N.J., Miyoshi H., Pennington K.N., Pobst L.J., Paya C.V. Transcription of the RelB gene is regulated by NF-κB. Oncogene. 2001;20(53):7722–7733. doi: 10.1038/sj.onc.1204868. [DOI] [PubMed] [Google Scholar]
- 99.Shih V.F., Davis-Turak J., Macal M. Control of RelB during dendritic cell activation integrates canonical and noncanonical NF-κB pathways. Nat Immunol. 2012;13(12):1162–1170. doi: 10.1038/ni.2446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fu J., Qu Z., Yan P. The tumor suppressor gene WWOX links the canonical and noncanonical NF-κB pathways in HTLV-I Tax-mediated tumorigenesis. Blood. 2011;117(5):1652–1661. doi: 10.1182/blood-2010-08-303073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tao Z., Fusco A., Huang D.B. p100/IκBδ sequesters and inhibits NF-κB through κBsome formation. Proc Natl Acad Sci USA. 2014;111(45):15946–15951. doi: 10.1073/pnas.1408552111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zinatizadeh M.R., Miri S.R., Zarandi P.K. The Hippo Tumor Suppressor Pathway (YAP/TAZ/TEAD/MST/LATS) and EGFR-RAS-RAF-MEK in cancer metastasis. Genes Dis. 2019;8(1):48–60. doi: 10.1016/j.gendis.2019.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Schmukle A.C., Walczak H. No one can whistle a symphony alone – how different ubiquitin linkages cooperate to orchestrate NF-κB activity. J Cell Sci. 2012;125(3):549–559. doi: 10.1242/jcs.091793. [DOI] [PubMed] [Google Scholar]
- 104.Chen Z., Lu W. Roles of ubiquitination and SUMOylation on prostate cancer: mechanisms and clinical implications. Int J Mol Sci. 2015;16(3):4560–4580. doi: 10.3390/ijms16034560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ramadan A., Paczesny S. Various forms of tissue damage and danger signals following hematopoietic stem-cell transplantation. Front Immunol. 2015;6:e14. doi: 10.3389/fimmu.2015.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lu H.Y., Bauman B.M., Arjunaraja S. The CBM-opathies—a rapidly expanding spectrum of human inborn errors of immunity caused by mutations in the CARD11-BCL10-MALT1 complex. Front Immunol. 2018;9:e2078. doi: 10.3389/fimmu.2018.02078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kojok K., El-Kadiry A.E., Merhi Y. Role of NF-κB in platelet function. Int J Mol Sci. 2019;20(17):e4185. doi: 10.3390/ijms20174185. [DOI] [PMC free article] [PubMed] [Google Scholar]