Abstract
Objective
Mayors have considerable and often direct influence over health policy in their cities, yet little is known about mayors’ general perceptions of current public health challenges. The objective of this study was to assess perceptions, attitudes, and priorities related to public health among US mayors.
Methods
We collected survey data from a nationally representative sample of US mayors (N = 110) in 2018 and matched survey responses with city-level health surveillance data. We conducted descriptive analyses and multivariable regression modeling to estimate associations of interest.
Results
Mayors in our sample most frequently cited obesity/chronic diseases (23.6%; 26 of 110), opioid abuse/drug addiction (22.7%; 25 of 110), and health care access (13.6%; 15 of 110) as the top health challenges facing their cities. However, mayors identified a different set of health issues for which they believed constituents hold them accountable. With the exception of opioid-related deaths, prevalence of a health concern was not associated with perceived accountability for that particular issue, whereas partisanship and sex predicted patterns in perceived accountability.
Conclusions
Mayors recognized critical health challenges at the city level but varied widely in their perceived accountability for such challenges. Findings can inform strategies to engage local policy makers in cross-sector collaborations to improve the health and overall well-being of people in cities across the United States.
Keywords: policy makers, perceptions, public health, accountability, mayors
Many health policy decisions occur at the local level.1 Scientific articles routinely call for policy makers to use evidence to inform legislative action to address public health issues,2 but little is known about how local elected officials perceive and prioritize public health concerns. Multiple issues influence policy decisions, such as budget, compatibility with existing policies, stakeholder interests, and other competing priorities (eg, education, housing).3,4 Given that local elected officials, including mayors, routinely implement and influence health policy,5-8 understanding their priorities and stances on public health issues is critical to translating science into policies that promote well-being and maximize impact.9,10
Mayors are the executives of local municipalities in the United States. Despite heterogeneity in roles, resources, and level of authority, mayors and local governments can influence a wide range of local policy outcomes.6,11-15 Mayors often have direct control over policies that affect public health (eg, transportation, safety, police-related issues, city infrastructure), even if they are not always in charge of the local health structures themselves.
A considerable proportion of mayors in the United States have prioritized public health challenges in the National League of Cities’ annual State of the City reports, elevating issues such as mental health (20% of mayors make this challenge a priority), the opioid crisis (11% of mayors), or pedestrian safety (34% of mayors) to the forefront of their platform.16-19 The annual US Conference of Mayors consistently addresses health policy, including setting annual health policy–related resolutions.20 Still, little is known about mayors’ general perceptions of current public health challenges. No studies, to our knowledge, have examined mayoral attitudes toward public health concerns in the context of city-level health metrics. Addressing these gaps may help public health researchers and practitioners communicate public health research and recommendations to local policy makers for broad community impact.
This study aimed to assess mayors’ perceptions of the top health challenges facing their cities, examine mayors’ perceptions of their own accountability for a set of public health challenges, and explore characteristics associated with perceived accountability. Because previous studies demonstrated that Republican and Democratic officials and constituents tend to hold distinct public health policy views,21-26 we hypothesized that mayoral political affiliation and city-level prevalence of a health concern would predict patterns in perceptions of accountability for public health issues.
Methods
Data from this study are from the 2018 administration of the annual Menino Survey of Mayors and city-level health surveillance data extracted from publicly available data repositories.27-30 All study procedures were approved by the institutional review board for the Charles River Campus at Boston University.
Study Sample and Recruitment
The target population consisted of mayors from US cities with ≥75 000 residents (based on the US Census Bureau’s 2016 American Community Survey) across all 50 US states and Washington, DC.31 We used municipality websites to identify all mayors from eligible cities (N = 472). We targeted midsized and large cities to enhance comparability in our units of analysis and to be consistent in our aim of surveying mayors who yield a fair amount of control over local policymaking (mayors from smaller cities have less control than mayors from larger cities). Each mayor received an email, including a description of the survey purpose and disclosure of funders. We conducted all interviews in person or via telephone from June through August 2018. The sample of 110 cities was representative of mayoral demographic characteristics and the demographic characteristics and region of the pool of cities from which the sample was drawn, and comparable with the 500 largest US cities in various health indicators.27,32
Survey Development and Administration
We designed survey modules to explore timely and understudied topics, including local policy issues and national trends. Members of the research team and public policy experts developed the 2018 modules, which included open-ended and closed-ended questions. Trained interviewers used a standardized survey administration protocol. The email assured participants of confidentiality and provided them with contact information. Nonrespondents received at least 2 email reminders. To mitigate response bias, mayors did not receive survey questions or themes before the interview (ie, mayors were not able to prepare responses in advance).
Measures
Menino Survey of Mayors
To assess mayors’ perception of community health, the survey asked participants the following open-ended question: “What is the greatest health challenge facing your city?” Some mayors mentioned more than 1 health challenge, so responses included all mentions of health challenges.
To assess mayors’ perceived expectations among voters on how mayors could and should act, independent of the varying resources or governance authority of mayors, the survey also asked, “How much do you think constituents hold you accountable for each of the following health challenges in your city?” Response categories were 0, not at all; 1, a little; 2, somewhat; or 3, very accountable. We identified the following 9 health challenges during survey development: traffic accidents, gun violence, lead and other toxins, hunger/malnourishment, opioid abuse, other substance abuse, mental health, asthma, and obesity. Public health expert opinion validated this list of challenges; it includes challenges prioritized by prominent mayors and mayoral networks in recent years and/or are considered leading threats to urban health.16-20 We assessed each health challenge individually.
City-level data
We derived city-level data on items (eg, prevalence of obesity, presence of air pollution) that mapped onto the 9 public health issues identified in the perceived accountability item from 3 sources: the City Health Dashboard 500 Cities data set,28 the Supplementary Homicide Reports,29 and the US Department of Transportation’s National Highway Traffic Safety data set (Table 1).30
Table 1.
City-level health indicators used to provide context for the public health challenges itemized in the 2018 Menino Survey of Mayorsa on perceptions of public health priorities and accountability among US mayors
| Outcome | Health indicator used and data sources |
|---|---|
| Lead exposure risk index | Index of poverty-adjusted risk
of housing-based lead exposure with a 5-year estimate
from 2017. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Limited access to healthy foods | Percentage of population
living more than ½ mile from the nearest supermarket,
supercenter, or large grocery. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Binge drinking | 1-year modeled estimate of the
percentage of adults aged ≥18 who engaged in binge
drinking in 2016. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Smoking | 1-year modeled estimate of the
percentage of adults aged ≥18 who smoked in
2016. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Opioid overdose deaths | Deaths due to opioid overdose
per 100 000 population as an average of
2014-2016. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Frequent mental distress | 1-year modeled estimate of the
percentage of adults aged >18 who rated their mental
health as “not good” for >14 days during the past 30
days in 2016. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Air pollution (particulate matter) | Average daily concentration of
fine particulate matter (PM2.5) per cubic
meter in 2015. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Obesity | 1-year modeled estimate of the
percentage of obesity among adults aged ≥18 in
2016. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Diabetes | 1-year modeled estimate of the
percentage of adults aged ≥18 with diabetes in
2016. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Cardiovascular disease deaths | Deaths attributed to
cardiovascular disease (per 100 000 population) in
2015-2017. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Walkability | 1-year modeled estimated
percentage of no leisure-time physical activity in past
month among adults aged ≥18 in 2016. Data source: City Health Dashboard 500 Cities data set from NYU Langone Health.28 |
| Traffic fatality rate per 100 000 residents | Counts of fatal traffic crashes in 2017 per municipality were obtained from the US Department of Transportation, National Highway Traffic Safety Administration Fatality and Injury Reporting System Tool.30 Using the 2016 US Census Bureau’s population estimates and geographic locator codes (GLCs),31 traffic fatality rates per 100 000 residents were calculated for each city in the database. Missing cities from the GLC list were manually matched by looking at geographic location of fatalities.30 |
| Gun violence | Data were obtained from Multiple-Imputed Supplementary Homicide Reports File, 1976-2016 by Fox.29 Because data for 13 cities were missing, additional data had to be imputed by using gun-related local news reports compiled by the Gun Violence Archive.33 Gun-related homicide rates per 100 000 population were then calculated by using the 2016 US Census Bureau’s population estimates.31 |
Abbreviation: NYU, New York University.
aData source: Einstein et al.27
Predictors of accountability
We obtained data on 3 mayoral characteristics through an online search of city websites: sex (male or female), political affiliation (Republican, Democratic, or other), and race/ethnicity (White, Black, Latino, Asian, or “other”). For each city, we obtained data on population size and median housing value (using logged values to avoid skewness) from the 2016 American Community Survey 5-year estimates.31 From each city website, we collected data on type of health authority in the city by identifying the geographic areas served by each health authority (a city, a county, or a regional area encompassing several cities or counties); we coded type of health authority into 3 categories: municipal, county, or regional. We matched and appended to the survey data set all city-level data.
Statistical Analysis
We first conducted descriptive analyses of mayors’ responses and characteristics. We identified, coded, and organized major health challenges from transcripts of responses to the open-ended health challenge question, which were then reviewed by 2 additional team members. We examined the frequencies of health challenges cited by participants by focusing on all health challenges reported by mayors, regardless of order indicated in the survey response. To graphically depict the frequency of the most pressing health challenge mayors perceived as affecting their cities, we created a word cloud. Constructed using Wordart software (Wordart.com), the word cloud depicts the frequency of health-related words or phrases mayors used in their open-ended responses to the survey question, “What is the greatest health challenge facing your city?” The size of each word correlates directly with the frequency of usage. We first removed “stop-words” (eg, “for,” “the,” “to”) using Wordart software specifications. Next, we manually sorted and removed words unrelated to health challenges (eg, “those”). We examined levels of accountability for each of the 9 public health issues by using frequencies. To compare city-level metrics of the most frequently reported major health challenge grouping (obesity, diabetes, and heart disease) with perceived accountability of these issues, we obtained data on the prevalence of the 3 conditions for cities with mayors who ranked these issues as their community’s greatest health challenge (n = 31). We divided cities into tertiles (lower third, middle third, and upper third) based on the prevalence of these chronic conditions relative to all 110 cities in our sample.
We conducted ordinary least squares multivariable regressions to examine associations between mayoral and city-level characteristics (predictors) and level of perceived accountability (outcome) for each of the prespecified 9 public health issues. Predictors included the individual characteristics of mayors (sex, political affiliation, and race/ethnicity), city-level characteristics (population size, median housing value, and type of health authority), and city-level prevalence of each corresponding health indicator. For example, for obesity, we included walkability and the prevalence of adult obesity and diabetes as predictors. We considered P ≤ .05 to be significant. We conducted all analyses using R 1.1.453 (RStudio, PBC).
Results
Study Sample
A total of 110 mayors participated in the survey (23.3% response rate), representing 110 cities on the West Coast and in the South, Northeast, and Midwest. Most participants were male (71.8%; n = 79) and White (82.7%; n = 91); 9.1% (n = 10) were Black, 5.5% (n = 6) were Latino, 1.8% (n = 2) were Asian, and 0.9% (n = 1) identified as “other.” More than half (60.0%; n = 66) identified as Democratic, 23.6% (n = 26) as Republican, and 16.4% (n = 18) as other.
Mayors’ Perceptions and Attitudes
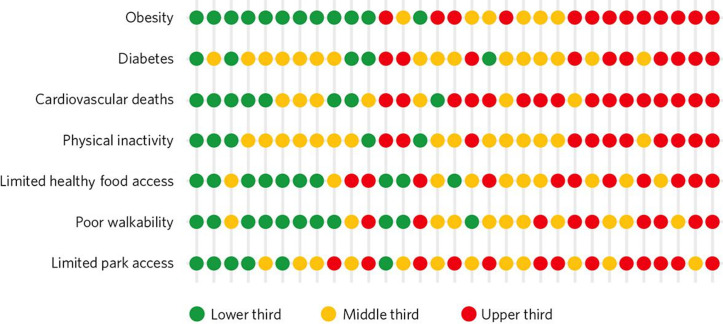
When asked the open-ended question on the greatest health challenge facing their city, mayors most frequently cited the following 5 challenges: (1) obesity, diabetes, and heart disease (23.6%; n = 26); (2) opioid abuse and other forms of addiction (22.7%; n = 25); (3) lack of access to or cost of health care (13.6%; n = 15); (4) environmental challenges (10.9%; n = 12); and (5) mental health (7.3%; n = 8) (Figure 1). Overall, 14.0% of mayors noted mental health as their community’s key challenge or in the context of other health concerns.
Figure 1.
A word cloud of perceptions of the greatest health challenge facing their cities among 110 US mayors participating in the 2018 Menino Survey of Mayors. Constructed using Wordart software, the word cloud depicts the frequency of specific health-related words or phrases mayors used in their open-ended responses to the survey question, “What is the greatest health challenge facing your city?” The size of each word correlates directly with frequency of usage. Data source: 2018 Menino Survey of Mayors by Einstein et al.27
A different set of health issues emerged in response to the closed-ended question about mayors’ perceived accountability (Figure 2). Most mayors perceived their constituents to hold them very or somewhat accountable for traffic accidents (69% of mayors), gun violence (57%), and lead and other toxins (52%), whereas obesity ranked last (9%). Other health concerns, such as opioid abuse and mental health, were also ranked low in perceived accountability.
Figure 2.
Survey results for 110 US mayors participating in the 2018 Menino Survey of Mayors. Closed-ended survey question asked the following: “How much do you think constituents hold you accountable for each of the following health challenges in your city?” All items were measured on the following scale: 0 = not at all accountable, 1 = a little accountable, 2 = somewhat accountable, 3 = very accountable. Data source: 2018 Menino Survey of Mayors by Einstein et al.27
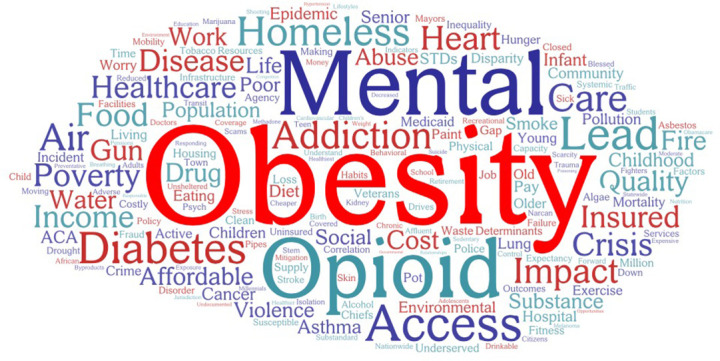
Mayors of cities with prevalence rates in the lowest tertile (Figure 3) identified obesity and related risk factors as the top health concern, even though the rates of these health outcomes were not as high in their communities as they were in other cities. Only 6 mayors in the 20 cities with the highest rates of obesity identified obesity and related chronic diseases as the most pressing health problem in their city.
Figure 3.
Seven health care challenges named by 31 US mayors by tertile (lower third, middle third, and upper third) of prevalence of obesity, diabetes, and heart disease. Each row represents the 31 mayors who mentioned obesity, diabetes, or heart disease as a key community health challenge, and each column represents an individual city. The tertiles represent all 110 cities that participated in the 2018 Menino Survey. The variables for walkability and park access were reversed for the purposes of this figure so that the upper third (in red) indicates the poorest environment. Data sources: 2018 Menino Survey of Mayors by Einstein et al27 and the City Health Dashboard 500 Cities data set from New York University Langone Health.28
Predictors of Accountability
In the multivariable regression models (Table 2), we found several significant associations. For individual-level characteristics, partisanship and sex were significantly associated with patterns in perceptions of accountability; mayors who identified as Democrat reported higher levels of perceived accountability than mayors who identified as Republican for gun violence (β = 0.785; SD, 0.259; P = .003), hunger/malnourishment (β = 0.747; SD, 0.247; P = .003), asthma (β = 0.401; SD, 0.183; P = .03), and obesity (β = 0.462; SD, 0.181; P = .02). Male mayors reported lower levels of perceived accountability than female mayors for mental health (β = −0.033; SD, 0.232; P = .03).
Table 2.
Results of multivariate regression models examining factors associated with accountability for health challenges among 110 US mayors participating in the 2018 Menino Survey of Mayorsa
| Perceived accountability for . . .b | Effect estimate (SD) [95% CI] | P valuec |
|---|---|---|
| Traffic accidents | ||
| Sex (male vs female) | −0.008 (0.018) [−0.044 to 0.028] | .67 |
| Race/ethnicity (non-White vs White) | 0.078 (0.102) [−0.124 to 0.281] | .44 |
| Political affiliation (Republican vs Democratic) | 0.328 (0.255) [−0.179 to 0.835] | .20 |
| Type of health authority present in city (municipal vs county/regional) | 0.214 (0.213) [−0.210 to 0.638] | .32 |
| Population size (logarithm of continuous variable for population) | 0.020 (0.162) [−0.301 to 0.342] | .90 |
| Median housing value (logarithm of continuous variable for median housing value) | 0.563 (0.214) [0.137 to 0.989] | .01 |
| Incidence of traffic fatalities (rate per 100 000 population) | −0.006 (0.027) [−0.060 to 0.048] | .83 |
| Gun violence | ||
| Sex (male vs female) | 0.029 (0.021) [−0.014 to 0.072] | .18 |
| Race/ethnicity (non-White vs White) | −0.037 (0.101) [−0.238 to 0.164] | .72 |
| Political affiliation (Republican vs Democratic) | 0.785 (0.259) [0.270 to 1.299] | .003 |
| Type of health authority present in city (municipal vs county/regional) | 0.038 (0.208) [−0.378 to 0.454] | .86 |
| Population size (logarithm of continuous variable for population) | −0.028 (0.202) [−0.431 to 0.375] | .89 |
| Median housing value (logarithm of continuous variable for median housing value) | −0.309 (0.208) [−0.722 to 0.105] | .14 |
| Incidence of gun-related homicides (rate per 100 000 population) | 0.001 (0.005) [−0.008 to 0.010] | .86 |
| Lead and other toxins | ||
| Sex (male vs female) | 0.228 (0.018) [−0.041 to 0.030] | .47 |
| Race/ethnicity (non-White vs White) | 0.181 (0.105) [−0.029 to 0.390] | .09 |
| Political affiliation (Republican vs Democratic) | −0.006 (0.316) [−0.400 to 0.857] | .75 |
| Type of health authority present in city (municipal vs county/regional) | 0.229 (0.225) [−0.219 to 0.678] | .32 |
| Population size (logarithm of continuous variable for population) | 0.051 (0.165) [−0.278 to 0.379] | .76 |
| Median housing value (logarithm of continuous variable for median housing value) | −0.029 (0.241) [−0.509 to 0.449] | .90 |
| Incidence of lead exposure (1-10 index) | 0.064 (0.054) [−0.044 to 0.172] | .24 |
| Hunger/malnourishment | ||
| Sex (male vs female) | −0.029 (0.016) [−0.061 to 0.002] | .07 |
| Race/ethnicity (non-White vs White) | 0.038 (0.093) [−0.147 to 0.223] | .68 |
| Political affiliation (Republican vs Democratic) | 0.747 (0.247) [0.255 to 1.239] | .003 |
| Type of health authority present in city (municipal vs county/regional) | −0.055 (0.208) [−0.469 to 0.359] | .80 |
| Population size (logarithm of continuous variable for population) | 0.110 (0.150) [−0.188 to 0.409] | .47 |
| Median housing value (logarithm of continuous variable for median housing value) | −0.312 (0.218) [−0.745 to 0.121] | .16 |
| Prevalence of limited access to healthy foods (percentage) | 0.009 (0.008) [−0.008 to 0.025] | .31 |
| Substance abuse other than opioid abuse | ||
| Sex (male vs female) | −0.026 (0.015) [−0.056 to 0.003] | .08 |
| Race/ethnicity (non-White vs White) | −0.067 (0.086) [−0.239 to 0.104] | .44 |
| Political affiliation (Republican vs Democratic) | 0.083 (0.244) [−0.402 to 0.568] | .73 |
| Type of health authority present in city (municipal vs county/regional) | 0.021 (0.176) [−0.329 to 0.370] | .91 |
| Population size (logarithm of continuous variable for population) | 0.153 (0.133) [−0.112 to 0.419] | .25 |
| Median housing value (logarithm of continuous variable for median housing value) | −0.077 (0.294) [−0.662 to 0.508] | .80 |
| Prevalence of smoking (percentage) | 0.028 (0.043) [−0.059 to 0.114] | .53 |
| Prevalence of binge drinking (percentage) | 0.043 (0.035) [−0.027 to 0.113] | .23 |
| Opioid abuse | ||
| Sex (male vs female) | −0.008 (0.016) [−0.039 to 0.024] | .63 |
| Race/ethnicity (non-White vs White) | −0.011 (0.093) [−0.204 to 0.164] | .83 |
| Political affiliation (Republican vs Democratic) | 0.210 (0.230) [−0.248 to 0.668] | .36 |
| Type of health authority present in city (municipal vs county/regional) | 0.048 (0.189) [−0.328 to 0.424] | .80 |
| Population size (logarithm of continuous variable for population) | 0.106 (0.141) [−0.174 to 0.386] | .45 |
| Median housing value (logarithm of continuous variable for median housing value) | −0.110 (0.194) [−0.495 to 0.276] | .57 |
| Incidence of opioid-related overdose deaths (per 100 000 population) | 0.019 (0.010) [0.001 to 0.037] | .05 |
| Mental health | ||
| Sex (male vs female) | −0.033 (0.232) [−0.062 to −0.003] | .03 |
| Race/ethnicity (non-White vs White) | 0.005 (0.085) [−0.165 to 0.174] | .95 |
| Political affiliation (Republican vs Democratic) | 0.274 (0.232) [−0.186 to 0.735] | .24 |
| Type of health authority present in city (municipal vs county/regional) | 0.057 (0.184) [−0.310 to 0.425] | .76 |
| Population size (logarithm of continuous variable for population) | 0.113 (0.134) [−0.155 to 0.380] | .40 |
| Median housing value (logarithm of continuous variable for median housing value) | 0.326 (0.258) [−0.187 to 0.839] | .21 |
| Prevalence of frequent mental distress (percentage) | 0.095 (0.075) [−0.054 to 0.244] | .21 |
| Asthma | ||
| Sex (male vs female) | 0.003 (0.013) [−0.023 to 0.029] | .82 |
| Race/ethnicity (non-White vs White) | 0.057 (0.074) [−0.089 to 0.204] | .44 |
| Political affiliation (Republican vs Democratic) | 0.401 (0.183) [0.037 to 0.765] | .03 |
| Type of health authority present in city (municipal vs county/regional) | 0.001 (0.170) [−0.338 to 0.340] | .10 |
| Population size (logarithm of continuous variable for population) | 0.144 (0.116) [−0.085 to 0.375] | .22 |
| Median housing value (logarithm of continuous variable for median housing value) | 0.322 (0.157) [0.009 to 0.635] | .04 |
| Presence of air pollution (fine particulate matter during a year) | 0.016 (0.046) [−0.075 to 0.107] | .73 |
| Obesity | ||
| Sex (male vs female) | −0.022 (0.014) [−0.050 to 0.005] | .12 |
| Race/ethnicity (non-White vs White) | 0.036 (0.071) [−0.106 to 0.179] | .61 |
| Political affiliation (Republican vs Democratic) | 0.462 (0.181) [0.101 to 0.823] | .02 |
| Type of health authority present in city (municipal vs county/regional) | −0.161 (0.158) [−0.477 to 0.154] | .31 |
| Population size (logarithm of continuous variable for population) | 0.260 (0.112) [0.037 to 0.482] | .02 |
| Median housing value (logarithm of continuous variable for median housing value) | −0.088 (0.315) [−0.715 to 0.538] | .78 |
| Prevalence of adult obesity (percentage) | −0.018 (0.035) [−0.088 to 0.051] | .60 |
| Prevalence of physical inactivity (percentage) | −0.017 (0.030) [−0.078 to 0.043] | .57 |
| Prevalence of diabetes (percentage) | 0.072 (0.074) [−0.075 to 0.220] | .33 |
aData sources: 2018 Menino Survey of Mayors by Einstein et al,27 City Health Dashboard 500 Cities data set from New York University Langone Health,28 Multiple-Imputed Supplementary Homicide Reports File, 1976-2016 by Fox,29 and US Department of Transportation, National Highway Traffic Safety Administration Fatality and Injury Reporting System Tool.30
bClosed-ended survey question asked the following: “How much do you think constituents hold you accountable for each of the following health challenges in your city?” All items were measured on the following scale: 0 = not at all accountable, 1 = a little accountable, 2 = somewhat accountable, 3 = very accountable.
cDetermined by ordinary least squares multivariate regressions; P ≤ .05 considered significant.
For city-level characteristics, type of health authority was not associated with perceptions of accountability for any health outcome. City population size was positively associated with perceived accountability for obesity (β = 0.260; SD, 0.112; P = .02), with mayors in larger cities perceiving a greater level of accountability for obesity than mayors in smaller cities. Median housing value was positively associated with perceived accountability for traffic accidents (β = 0.563; SD, 0.214; P = .01) and asthma (β = 0.322; SD, 0.157; P = .04). Prevalence of opioid-related overdose deaths, but no other prevalence health indicator, was positively associated with perceived accountability (β = 0.019; SD, 0.010; P = .05).
Discussion
To our knowledge, our study is one of the first to analyze the perceptions of, and attitudes toward, major public health concerns among a representative sample of mayors in the context of city-level data. Despite representing a heterogenous group of cities, mayors in our study had commonalities in health challenges, citing obesity, opioid abuse or other forms of drug addiction, and access to health care as the top 3 challenges. These perceptions may reflect national and global trends. The United States is among the list of developed countries with high rates of obesity; 36.2% of US adults are obese (surpassing obesity rates in Mexico [28.9%] and the United Kingdom [27.8%]).34 The number of nonprescription opioid users in the United States far exceeds the number in any other country, with 11 million past-year users of nonmedical pharmaceutical opioids in 2017 (4.2% of the population aged ≥12), compared with 630 000 people in Australia and New Zealand in 2017 (3.3% of the population aged 15-64) or 85 000 people in Canada in 2017 (0.4% of the population aged 15-64).35 The high rates of opioid use and subsequent mortality may partially explain why opioid-related deaths were the sole health issue found to be associated with perceived accountability in our study.
Our results indicated a discrepancy between mayors’ perceptions of health challenges and constituents’ expectations. Although mayors most frequently cited obesity as the most pressing health challenge, they believed they were held least accountable for this challenge by constituents. Mayors’ perceptions of accountability may be formed by the information (or lack thereof) at their disposal. Mayors may perceive to be held accountable for issues that are more often reported in their local news or elevated by their constituents, such as crime, the environment, or vehicular traffic. They may also be influenced by national information and priorities of the Centers for Disease Control and Prevention or local trend reports from the National League of Cities that may or may not be relevant to their city.
Another alternative explanation for the discrepancy between mayors’ beliefs about health challenges and accountability is perceptions of control. Health behaviors (eg, diet, physical activity, drug use) may be perceived as individual risk factors outside of mayoral control or regarded as in the purview of health agencies. In our study interviews, mayors often remarked unprompted that they do not run the health agency in their district. Just one-fifth of health authorities in the United States exist at the municipal level, whereas most (nearly 70%) are county-level (single-county or multicounty) agencies, and the remainder are regional authorities.36 Our sample yielded similar proportions; thus, the limited variation in this exposure of interest is a potential explanation for our finding of no association between type of health authority and perceived accountability.
In contrast, mayors may perceive health outcomes related to structural, policy, and environmental risk factors that are traditionally or typically under a mayor’s influence (eg, vehicular traffic, gun violence, exposure to lead/toxins) as within their realm of accountability. Mayors often lead or directly work with police, municipal transportation, and inspections-related departments in monitoring and intervening on public health concerns, such as traffic crashes, speeding, gun violence, or lead paint and pipes.37,38 In the 2019 State of the City report, 55% of mayors mentioned roads, streets, and signs as concerns; 37% mentioned public safety as a concern; and 41% mentioned environment and energy concerns.19
Although mayors may recognize the importance of public health concerns, including the social determinants of health and health disparities, they may perceive little to no power over these concerns at the community or city level.21 Research suggests that changing the narrative on accountability is imperative, particularly given that many top health challenges, such as obesity and opioid abuse, are complex, multifaceted conditions that require a set of multisectoral and multilevel solutions. Mayors have a critical role in leveraging assets, resources, and initiatives to catalyze change at the local level.
Another possible explanation for the discrepancy between mayors’ beliefs and accountability is competing priorities. Obesity may have emerged as a top health priority among participants in our sample, but it may not be an overall priority compared with other issues that mayors address daily. Issues such as economic development, budgeting, affordable housing, and education may take greater precedent over long-term public health issues such as obesity and physical activity.39-41 For example, although local policy makers and officials in Kansas recognized obesity as a problem, their legislative efforts focused on budgeting, education, and jobs/economy.41 Public health practitioners, including local health authorities and researchers, should consider expanding outcomes of interest beyond health and health behaviors when engaging with policy makers in promoting health interventions. In particular, framing health-promoting policies and programs as a catalyst for urban revitalization42 and community building—rather than as a public health intervention with only public health benefits—may facilitate future efforts and engage mayors as key players in targeting common health challenges.
Mayors’ partisanship predicted perceptions of accountability for certain health outcomes, with Democratic mayors often perceiving a higher level of accountability than their Republican peers. These findings are consistent with research demonstrating differences in health policy preferences by party affiliation. Democrats are more likely than Republicans or Independents to support the implementation of policies that promote overall public health,22 to favor obesity prevention legislation,24,25 and to acknowledge the existence of social determinants of health as factors shaping communities.23,26 Even among Democratic mayors in our sample, chronic conditions such as asthma (17% of mayors cited this challenge) and obesity (13% of mayors) were still ranked low in terms of perceived accountability compared with gun violence (72% of mayors) and hunger/malnourishment (55% of mayors). To advance health policy and public health impact, public health academics, local health authorities, and professionals need to consider how to frame recommendations, particularly those that address preventable chronic diseases, in ways that appeal to both conservative and liberal audiences.
With the exception of opioid-related deaths, prevalence of a health issue at the city level did not predict levels of accountability for that issue. A possible explanation for this finding is that the public, and sometimes even mayors, may not use or be aware of city-level prevalence data to inform their health policy opinions. This lack of awareness may be partially attributed to lack of comprehensive city-level data on an established set of health metrics. Comparative, reliable city-level data on traffic accidents and gun-related violence—2 areas identified as priorities to mayors—were not readily available at the time of our research. Public health researchers and practitioners should consider the expansion or creation of additional open-access data platforms, such as the City Health Dashboard,28 which provides up-to-date, centralized metrics for the public, mayors, and policy makers on the health of their communities. Such data could support the health policy decision-making process. The public health community can also facilitate channels of communication that directly connect mayors with constituents on public health topics.
Strengths and Limitations
Our study had several strengths. First, our sample was representative of US mayors and cities, including mayoral partisan distribution.27 Robustness checks showed that our sample of cities was similar to the 500 largest US cities on various demographic and health indicators.30,31 Second, we used centralized, secondary city-level data, which provided context for interpreting findings. Third, we conducted the survey through in-person or telephone interviews and spoke directly with mayors, ensuring that responses reflected mayors’ perspectives and not those of mayoral staff members answering surveys on behalf of mayors. Finally, our response rate was comparable to other surveys of local political elites.43,44
Our study also had several limitations. First, the sampling of mayors from large and midsized cities may mean that our findings are not generalizable to mayors from smaller cities. Second, we obtained all data via self-report, which is subject to social desirability bias, and the survey questions were not extensively tested for reliability and validity. Third, although informed by experts, the list of 9 public health issues identified for the accountability item did not cover all possible public health challenges; to reduce respondent burden, we listed only 9 challenges, but we acknowledge that cities face many more important health issues. Fourth, to maintain confidentiality for participating mayors and their cities, we did not report prevalence rates of public health issues in each city; reporting these rates would have allowed readers to compare actual prevalence with mayoral perceptions.
Conclusions
Our study suggests that although mayors may understand the pressing health challenges facing cities today, perceptions of accountability could improve. The growing number of health-focused policy initiatives and reports indicates that the field of health policy may be shifting to explicitly recognize the role, responsibility, and potential of elected officials in advancing city health. This shift may represent a window of opportunity to engage with and empower local elected officials, such as mayors, to engage in public health issues such as obesity, opioid abuse, and health care access. Solutions require that leaders, agencies, and advocates work together to address priorities. Cross-sector collaborations to develop and implement city-based health programs and policies are essential to promote the overall well-being and prosperity of cities in both the short term and long term. Finally, our findings highlight the need for additional research to examine the extent to which constituents’ perceptions of health challenges and priorities may differ from mayoral views and how mayoral election platforms and health policy agendas evolve.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Luisa Godinez Puig, MA https://orcid.org/0000-0001-7533-4097
References
- 1. Brownson RC., Ballew P., Dieffenderfer B. et al. Evidence-based interventions to promote physical activity: what contributes to dissemination by state health departments. Am J Prev Med. 2007;33(1 Suppl):S66-S74. 10.1016/j.amepre.2007.03.011 [DOI] [PubMed] [Google Scholar]
- 2. Murphy K., Fafard P. Taking power, politics, and policy problems seriously: the limits of knowledge translation for urban health research. J Urban Health. 2012;89(4):723-732. 10.1007/s11524-012-9694-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Liu X., Lindquist E., Vedlitz A., Vincent K. Understanding local policymaking: policy elites’ perceptions of local agenda setting and alternative policy selection. Policy Studies J. 2010;38(1):69-91. 10.1111/j.1541-0072.2009.00345.x [DOI] [Google Scholar]
- 4. Dodson EA., Stamatakis KA., Chalifour S., Haire-Joshu D., McBride T., Brownson RC. State legislators’ work on public health–related issues: what influences priorities? J Public Health Manag Pract. 2013;19(1):25-29. 10.1097/PHH.0b013e318246475c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Freudenberg N., Atkinson S. Getting food policy on the mayoral table: a comparison of two election cycles in New York and London. Public Health. 2015;129(4):295-302. 10.1016/j.puhe.2015.02.018 [DOI] [PubMed] [Google Scholar]
- 6. Karnig AK., Welch S. Black Representation and Urban Policy. University of Chicago Press; 1980. [Google Scholar]
- 7. Pomeranz JL. The unique authority of state and local health departments to address obesity. Am J Public Health. 2011;101(7):1192-1197. 10.2105/AJPH.2010.300023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gostin LO. Bloomberg’s health legacy: urban innovator or meddling nanny? Hastings Cent Rep. 2013;43(5):19-25. 10.1002/hast.208 [DOI] [PubMed] [Google Scholar]
- 9. Bernier NF., Clavier C. Public health policy research: making the case for a political science approach. Health Promot Int. 2011;26(1):109-116. 10.1093/heapro/daq079 [DOI] [PubMed] [Google Scholar]
- 10. Rütten A., Abu-Omar K., Gelius P., Schow D. Physical inactivity as a policy problem: applying a concept from policy analysis to a public health issue. Health Res Policy Syst. 2013;11(1):9. 10.1186/1478-4505-11-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bauman JF. Wilson Goode: the Black mayor as urban entrepreneur. J Negro Hist. 1992;77(3):141-158. 10.2307/2717558 [DOI] [Google Scholar]
- 12. Browning RP. Protest Is Not Enough: The Struggle of Blacks and Hispanics for Equality in Urban Politics. University of California Press; 1984. [Google Scholar]
- 13. Hopkins DJ., Mccabe KT. After it’s too late: estimating the policy impacts of Black mayoralties in U.S. cities. Am Polit Res. 2011;40(4):665-700. [Google Scholar]
- 14. Trounstine J. Segregation and inequality in public goods. Am J Polit Sci. 2016;60(3):709-725. 10.1111/ajps.12227 [DOI] [Google Scholar]
- 15. Peterson PE. City Limits. University of Chicago Press; 1981. [Google Scholar]
- 16. National League of Cities . State of the cities 2016. Accessed August 20, 2020. https://www.nlc.org/resource/state-of-the-cities-2016
- 17. National League of Cities . State of the cities 2017. Accessed August 20, 2020. https://www.nlc.org/resource/state-of-the-cities-2017
- 18. National League of Cities . State of the cities 2018. Accessed August 20, 2020. https://www.nlc.org/resource/state-of-the-cities-2018
- 19. National League of Cities . State of the cities 2019. Accessed August 20, 2020. https://www.nlc.org/resource/state-of-the-cities-2019
- 20. The United States Conference of Mayors . Adopted resolutions—87th annual meeting; June 28–July 1, 2019; Honolulu, HI. Accessed November 6, 2019. https://www.usmayors.org/the-conference/adopted-policies/adopted-resolutions-87th-annual-meeting
- 21. Purtle J., Henson RM., Carroll-Scott A., Kolker J., Joshi R., Diez Roux AV. US mayors’ and health commissioners’ opinions about health disparities in their cities. Am J Public Health. 2018;108(5):634-641. 10.2105/AJPH.2017.304298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Oberlander J. Implementing the Affordable Care Act: the promise and limits of health care reform. J Health Polit Policy Law. 2016;41(4):803-826. 10.1215/03616878-3620953 [DOI] [PubMed] [Google Scholar]
- 23. Young R., Hinnant A., Leshner G. Individual and social determinants of obesity in strategic health messages: interaction with political ideology. Health Commun. 2016;31(7):903-910. 10.1080/10410236.2015.1018699 [DOI] [PubMed] [Google Scholar]
- 24. Gollust SE., Barry CL., Niederdeppe J. Partisan responses to public health messages: motivated reasoning and sugary drink taxes. J Health Polit Policy Law. 2017;42(6):1005-1037. 10.1215/03616878-4193606 [DOI] [PubMed] [Google Scholar]
- 25. Lee TK., Kim HK. Differential effects of message framing on obesity policy support between Democrats and Republicans. Health Commun. 2017;32(12):1481-1490. 10.1080/10410236.2016.1230810 [DOI] [PubMed] [Google Scholar]
- 26. Gollust SE., Lantz PM., Ubel PA. The polarizing effect of news media messages about the social determinants of health. Am J Public Health. 2009;99(12):2160-2167. 10.2105/AJPH.2009.161414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Einstein KL., Glick DM., Palmer M., Fox S. Menino Survey of Mayors: 2018 Results. Boston University Initiative on Cities; 2019. Accessed August 25, 2020. https://www.surveyofmayors.com/reports/Menino-Survey-of-Mayors-2018-Final-Report.pdf
- 28. New York University Langone Health . City Health Dashboard. Accessed August 25, 2020. https://www.cityhealthdashboard.com
- 29. Fox JA. Multiple-Imputed Supplementary Homicide Reports File, 1976-2016. School of Criminology and Criminal Justice, Northeastern University; 2018. [Google Scholar]
- 30. US Department of Transportation, National Highway Traffic Safety Administration . Fatality and Injury Reporting System Tool. August 25, 2020. https://cdan.dot.gov/query
- 31. US Census Bureau . 2016 American Community Survey. Accessed August 25, 2020. https://www.census.gov/programs-surveys/acs
- 32. Godinez Puig L., Lusk K., Wang ML. Mayors and the Health of Cities. Boston University Initiative on Cities; 2019. Accessed August 25, 2020. https://www.surveyofmayors.com/reports/Mayors-and-the-Health-of-Cities-Report.pdf
- 33. Fox JA. Multiple-imputed supplementary homicide reports file, 1976-2016. Gun Violence Archive. 2018. Accessed September 9, 2020. https://www.gunviolencearchive.org/query
- 34. World Health Organization . Global Health Observatory data repository: prevalence of obesity among adults, BMI ≥30, age-standardized: estimates by country. Accessed April 21, 2020. https://apps.who.int/gho/data/node.main.A900A?lang=en
- 35. United Nations Office on Drugs and Crime . World drug report 2019: depressants. June 2019. Accessed August 20, 2020. https://wdr.unodc.org/wdr2019/en/depressants.html
- 36. National Association of County and City Health Officials . 2016 National profile of local health departments. January 25, 2017. Accessed August 20, 2020. https://nacchovoice.naccho.org/2017/01/25/2016-national-profile-of-local-health-departments
- 37. National League of Cities, Institute for Youth, Education, and Families . Mayors and police chiefs working together for America’s children and youth. 2006. Accessed August 20, 2020. https://cops.usdoj.gov/RIC/Publications/cops-p126-pub.pdf
- 38. Zwald ML., Eyler AA., Goins KV., Brownson RC., Schmid TL., Lemon SC. Understanding municipal officials’ involvement in transportation policies supportive of walking and bicycling. J Public Health Manag Pract. 2017;23(4):348-355. 10.1097/PHH.0000000000000152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wang ML., Goins KV., Anatchkova M. et al. Priorities of municipal policy makers in relation to physical activity and the built environment: a latent class analysis. J Public Health Manag Pract. 2016;22(3):221-230. 10.1097/PHH.0000000000000289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Maddock JE., Reger-Nash B., Heinrich K., Leyden KM., Bias TK. Priority of activity-friendly community issues among key decision makers in Hawaii. J Phys Act Health. 2009;6(3):386-390. 10.1123/jpah.6.3.386 [DOI] [PubMed] [Google Scholar]
- 41. Heinrich KM., Stephen MO., Vaughan KB., Kellogg M. Kansas legislators prioritize obesity but overlook nutrition and physical activity issues. J Public Health Manag Pract. 2013;19(2):139-145. 10.1097/PHH.0b013e318254cc57 [DOI] [PubMed] [Google Scholar]
- 42. Policy Link . Cultivating equitable food-oriented development: lessons from West Oakland. July 3, 2017. Accessed August 20, 2020. https://www.policylink.org/equity-in-action/cultivating-food-equitable-development
- 43. Farris EM., Holman MR. Public officials and a “private” matter: attitudes and policies in the county sheriff office regarding violence against women. Soc Sci Q. 2015;96(4):1117-1135. 10.1111/ssqu.12182 [DOI] [Google Scholar]
- 44. Broockman DE., Skovron C. Bias in perceptions of public opinion among political elites. Am Polit Sci Rev. 2018;112(3):542-563. 10.1017/S0003055418000011 [DOI] [Google Scholar]