Abstract
Objectives
The types of opioids abused in the United States have changed from prescription opioids to heroin to fentanyl. However, the types of opioids abused may differ by demographic factors, especially among middle-aged adults. We examined national trends in opioid overdose mortality rates among middle-aged adults by race/ethnicity and sex.
Methods
Using 1999-2018 data from the Centers for Disease Control and Prevention Wide-ranging ONline Data for Epidemiologic Research database, we examined overdose mortality rates per 100 000 population in 2018 among adults aged 45-64 that involved natural and semisynthetic opioids, heroin, synthetic opioids (excluding methadone), and methadone. We tested for significant differences in mortality rates by race/ethnicity and sex. We plotted drug-specific trends by race/ethnicity and sex from 1999 to 2018.
Results
In 2018, non-Hispanic White adults had the highest rates per 100 000 population of natural and semisynthetic overdose mortality (men: 8.7; women: 7.9; P < .001), and non-Hispanic Black adults had the highest rates of heroin (men: 17.7; women: 5.4; P < .001) and synthetic opioid (men: 36.0; women: 11.2; P < .001) overdose mortality. Men had significantly higher overdose mortality rates than women did for deaths involving natural and semisynthetic opioids, heroin, and synthetic opioids, but not methadone. From 1999 to 2018, mortality rates increased sharply for heroin and synthetic opioids, increased modestly for natural and semisynthetic opioids, and decreased for methadone. The greatest increases were among non-Hispanic Black men for heroin overdose (3.3 in 1999 to 17.7 in 2018) and synthetic opioid overdose (0.1 in 1999 to 36.0 in 2018).
Conclusions
Policy making should consider unique subgroup risks and alternative trajectories of opioid use other than people being prescribed opioids, developing opioid use disorder, subsequently moving to heroin, and then to fentanyl.
Keywords: mortality, opioid overdose, White, Black or African American, Hispanic or Latino
The beginning of the 21st century was characterized by an increase in mortality among adults aged 45-54 in the United States, partially explained by an increase in poisonings among middle-aged non-Hispanic White people.1 As prescriptions for opioid pain medications increased through the early 2000s in the United States, increases in the number of emergency department visits, treatment entries, and overdose deaths were also observed.2-4 Recent data from the National Survey on Drug Use and Health showed that more than one-third of adults aged ≥50 reported using a prescription opioid in the last year.5 Although the morphine milligram equivalents of opioids prescribed per person were stable through the latter 2000s6 and steadily decreased into the 2010s,7 the average days’ supply of opioids increased,6 and mortality rates from prescription opioids plateaued during this period.8 At the same time, methadone prescribing and methadone overdose mortality rates began to decline and have continued to decline substantially since 2006.8,9 As efforts to stem the epidemic of nonmedical use of prescription opioids increased, the estimated number of people who use heroin increased dramatically, from 404 000 in 2002 to 620 000 in 2011.10 Furthermore, the addition of fentanyl to the supply of heroin and other street drugs resulted in a 45% increase in fentanyl mortality rates per 100 000 population in a single year (from 6.2 in 2016 to 9.0 in 2017), surpassing deaths from both prescription opioid medications and heroin.8 However, a 2019 National Vital Statistics Report suggests that certain demographic groups, including middle-aged adults, are at increased risk of opioid overdose mortality.11
The apparently sequential nature of the increasing death rates from prescription opioids, heroin, and then fentanyl fostered a narrative positing that people who had been prescribed opioids developed opioid use disorder (OUD), subsequently moved to heroin, and then to fentanyl. However, not all people who use opioids follow this pattern. Although epidemiologic analyses of hospitalizations for opioid-related overdoses preceded increases in heroin overdoses, suggesting that focusing on supply-based interventions may have led to a shift in the types of opioids used,12 this generalization oversimplifies the complexities of the opioid overdose epidemic. Specifically, prescription opioid misuse is not an essential prerequisite for heroin use.13,14 Furthermore, the mixing of fentanyl and related analogues into the supply of heroin, cocaine, methamphetamine, and counterfeit prescription opioid pills may result in people being unknowingly exposed to these substances.15,16
Although evidence exists of a sequential relationship among prescription opioids, opioid misuse, and the increase in deaths from heroin, the unfolding of this epidemic is more complicated and not universal to all subgroups. The rate of opioid prescriptions plateaued in 2010, but increases in overdose mortality rates occurred through 2017.8 This increase occurred among adults aged 45-54 and 55-64, cohorts for whom the rate of heroin use is substantially lower than for adults aged 18-25.17 Variability in opioid overdose mortality also exists by sex and race/ethnicity. For example, a 2018 examination of mortality rates by sex and race/ethnicity showed an increase in heroin overdose mortality among non-Hispanic Black men without a clear increase in mortality from opioids in the preceding years.18 These findings raise the possibility that the progression from prescription opioids to heroin to fentanyl/fentanyl-laced street drugs may not generalize to all subgroups. Alternative trajectories with different policy implications are possible.
The objective of our study was to examine rates of opioid overdose mortality as they relate to a sequential trend from prescription opioids to heroin to fentanyl among middle-aged adults. Using population data from the Centers for Disease Control and Prevention (CDC),19 we examined changes in overdose mortality rates among adults aged 45-64 from prescription opioids, including natural opioids (eg, morphine, codeine) and semisynthetic opioids (eg, oxycodone, hydrocodone, hydromorphone, oxymorphone), heroin (an illicit opioid synthesized from morphine), synthetic opioids excluding methadone (eg, prescribed and illicitly manufactured fentanyl/fentanyl analogues and tramadol), and methadone (a synthetic opioid prescribed for the treatment of pain and OUD), separately for each group of drugs and by sex and race/ethnicity, from 1999 through 2018. Given the unique risk profile of methadone compared with other opioids prescribed for pain, as well as its use in the pharmacotherapeutic treatment of OUD,20 we examined methadone separately from other synthetic opioids.
Methods
We obtained data from 1999 through 2018 from the CDC Wide-ranging ONline Data for Epidemiologic Research (WONDER) multiple causes of death database.19 Mortality data are compiled annually by the National Center for Health Statistics using death certificate data for US residents. Each death certificate lists the underlying cause of death. In addition, up to 20 potentially contributing conditions are listed as multiple causes of death and are coded using the International Classification of Diseases, Tenth Revision (ICD-10).21 Death certificates are filed in all 50 states and the District of Columbia, and an estimated >99% of all deaths are registered in the United States.22 Based on guidance from the US Department of Health and Human Services and the University at Buffalo Institutional Review Board, this secondary data analysis of publicly available deidentified data was determined not to be human subjects research.
We included causes of death in the following categories (ICD-10 codes): accidental/unintentional poisoning (X40-X44), intentional self-poisoning/suicide (X60-X64), assault/homicide (X85), and undetermined intent (Y10-Y14). We included in the analyses deaths with a contributing cause of poisoning by the following types of opioids: natural and semisynthetic opioids (T40.2), heroin (T40.1), synthetic opioids other than methadone (T40.4), and methadone (T40.3). Deaths may involve >1 drug; therefore, drug-specific categories of death are not mutually exclusive.
We obtained deidentified mortality data for each aforementioned drug category and grouped them by year, sex, race, and Hispanic origin. Race and Hispanic origin are reported separately on the death certificate. To examine for potential differences in overdose mortality rates by key demographic factors, we limited our analyses to people who were identified as “African American or Black” or “White” who were also identified as “not Hispanic or Latino,” as well as those who identified as “Hispanic or Latino.” Thus, we examined opioid overdose mortality rates among non-Hispanic Black, non-Hispanic White, and Hispanic/Latino people. Furthermore, we limited our focal analyses to adults aged 45-64. We excluded data on deaths without a known age, sex, race, or Hispanic origin from stratified analyses but included them in unstratified analyses.
To place these data in the context of the greater opioid epidemic, we first characterized opioid overdose deaths in the overall US population from 1999 through 2018 by presenting the absolute number of deaths during this 20-year period, regardless of age, sex, or race/ethnicity. We then obtained the number and rate of opioid overdose deaths in 2018 by race/ethnicity and sex among adults aged 45-64 for each of the following opioid types: (1) natural and semisynthetic opioids, (2) heroin, (3) synthetic opioids other than methadone, and (4) methadone. We examined the total number of deaths and crude mortality rates, calculated as deaths per 100 000 population. We used the Pearson χ2 test and post hoc tests with Bonferroni corrections using adjusted α levels of .001 to compare differences in mortality rates by race/ethnicity and sex. We used Stata version 15.1 (StataCorp) to conduct all analyses.
We plotted drug-specific trends in mortality rates among adults aged 45-64, by race/ethnicity and sex, from 1999 through 2018 for each of the 4 aforementioned opioid types.
Results
From 1999 through 2018 across all ages, 175 004 deaths involved natural and semisynthetic opioid overdose, 115 568 deaths involved heroin overdose, 124 486 deaths involved synthetic opioid overdose, and 70 214 deaths involved methadone overdose. Most natural and semisynthetic opioid deaths (75%), heroin deaths (84%), synthetic opioid deaths (89%), and methadone deaths (60%) occurred from 2008 through 2018. About 38% of overdose deaths involving natural and semisynthetic opioids, 23% of overdose deaths involving methadone, 60% of overdose deaths involving heroin, and 76% of overdose deaths involving synthetic opioids from 1999 through 2018 occurred from 2014 through 2018.
In 2018, overdose mortality rates among men and women aged 45-64 differed significantly by race/ethnicity for natural and semisynthetic opioids, heroin, synthetic opioids, and methadone (Table). After adjusting for multiple comparisons, non-Hispanic White men had a higher overdose mortality rate per 100 000 population from natural and semisynthetic opioids (8.7; P < .001) than non-Hispanic Black (7.0) and Hispanic/Latino (3.7) men. Heroin mortality rates among non-Hispanic White and Hispanic/Latino men aged 45-64 were the same (8.5 for both; P > .99) but were twice as high among non-Hispanic Black men (17.7: P < .001). Likewise, the mortality rate for synthetic opioid overdose was significantly higher among non-Hispanic Black men (36.0; P < .001) than among non-Hispanic White (17.0) and Hispanic/Latino (11.3) men. After adjusting for multiple comparisons, the overdose mortality rates for methadone were significantly higher among non-Hispanic Black (2.3; P < .001) and non-Hispanic White (2.0; P = .001) men than among Hispanic/Latino men (1.4).
Table.
Number and rate of overdose deaths involving opioids, by race/ethnicity and sex, for adults aged 45-64, CDC WONDER, United States, 2018a
| Characteristics | Natural and semisynthetic opioidsb | Heroine | Synthetic opioidsf | Methadoneg | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deaths, no. | Ratec | P valued | Deaths, no. | Ratec | P valued | Deaths, no. | Ratec | P valued | Deaths, no. | Ratec | P valued | |
| Male | ||||||||||||
| Non-Hispanic White | 2410 | 8.7 | <.001 | 2349 | 8.5 | <.001 | 4691 | 17.0 | <.001 | 551 | 2.0 | .001 |
| Non-Hispanic Black | 334 | 7.0 | 841 | 17.7 | 1711 | 36.0 | 109 | 2.3 | ||||
| Hispanic/Latino | 221 | 3.7 | 503 | 8.5 | 667 | 11.3 | 80 | 1.4 | ||||
| Non-Hispanic White vs non-Hispanic Black | — | — | <.001 | — | — | <.001 | — | — | <.001 | — | — | .18 |
| Non-Hispanic White vs Hispanic/Latino | — | — | <.001 | — | — | >.99 | — | — | <.001 | — | — | .001 |
| Non-Hispanic Black vs Hispanic/Latino | — | — | <.001 | — | — | <.001 | — | — | <.001 | — | — | <.001 |
| Female | ||||||||||||
| Non-Hispanic White | 2245 | 7.9 | <.001 | 798 | 2.8 | <.001 | 2162 | 7.6 | <.001 | 487 | 1.7 | <.001 |
| Non-Hispanic Black | 226 | 4.1 | 300 | 5.4 | 616 | 11.2 | 84 | 1.5 | ||||
| Hispanic/Latino | 124 | 2.1 | 101 | 1.7 | 137 | 2.3 | 57 | 1.0 | ||||
| Non-Hispanic White vs non-Hispanic Black | — | — | <.001 | — | — | <.001 | — | — | <.001 | — | — | .32 |
| Non-Hispanic White vs Hispanic/Latina | — | — | <.001 | — | — | <.001 | — | — | <.001 | — | — | <.001 |
| Non-Hispanic Black vs Hispanic/Latina | — | — | <.001 | — | — | <.001 | — | — | <.001 | — | — | .01 |
Abbreviations: CDC, Centers for Disease Control and Prevention; WONDER, Wide-ranging ONline Data for Epidemiologic Research.
aData source: CDC Wonder.19 Deaths without a known race or Hispanic origin were excluded from the stratified analyses, including the population counts used to calculate mortality rates.
bNatural opioids include drugs such as morphine and codeine, and semisynthetic opioids include drugs such as oxycodone, hydrocodone, hydromorphone, and oxymorphone.
cThe rate is per 100 000 population.
d P values are for overall Pearson χ2 tests and post hoc tests with Bonferroni corrections to compare differences by race/ethnicity. P < .05 was considered significant.
eHeroin is an illicit opioid synthesized from morphine.
fSynthetic opioids (excluding methadone) include drugs such as fentanyl, fentanyl analogues, and tramadol.
gMethadone is a synthetic opioid commonly prescribed for the treatment of opioid use disorder.
Hispanic/Latina women had significantly lower overdose mortality rates than non-Hispanic White and non-Hispanic Black women across all 4 opioid categories in 2018 (Table). Non-Hispanic White women had the highest overdose mortality rate per 100 000 population for natural and semisynthetic opioids (8.7; P < .001), but non-Hispanic Black women had the highest overdose mortality rate for heroin (5.4) and synthetic opioids (11.2; both P < .001). In 2018, non-Hispanic White women had a significantly higher methadone overdose mortality rate (1.7) than Hispanic/Latina women (1.0; P < .001), although methadone overdose mortality rates were lower than the overdose mortality rates of the other 3 opioid categories for all sex and racial/ethnic groups.
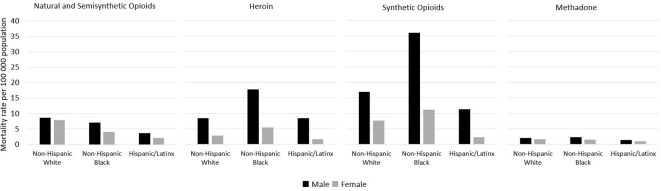
We found significant differences in the 2018 opioid overdose mortality rates between men and women of the same race/ethnicity (Figure 1). After adjusting for multiple comparisons, men had higher mortality rates per 100 000 population than women of the same race/ethnicity and age for natural and semisynthetic opioids (non-Hispanic White: 8.7 vs 7.9; non-Hispanic Black: 7.0 vs 4.1; Hispanic/Latinx: 3.7 vs 2.1), heroin (non-Hispanic White: 8.5 vs 2.8; non-Hispanic Black: 17.7 vs 5.4; Hispanic/Latinx: 8.5 vs 1.7), and synthetic opioids (excluding methadone; non-Hispanic White: 17.0 vs 7.6; non-Hispanic Black: 36.0 vs 11.2; Hispanic/Latinx: 11.3 vs 2.3; P < .001). Overdose mortality rates for methadone were low and did not differ significantly between men and women of any race/ethnicity after adjusting for multiple comparisons.
Figure 1.
Overdose mortality rates involving opioids among adults aged 45-64, by sex, United States, 2018. Natural opioids include drugs such as morphine and codeine, and semisynthetic opioids include drugs such as oxycodone, hydrocodone, hydromorphone, and oxymorphone. Heroin is an illicit opioid synthesized from morphine. Synthetic opioids (excluding methadone) include drugs such as fentanyl, fentanyl analogues, and tramadol. Methadone is a synthetic opioid commonly prescribed for the treatment of opioid use disorder. Except for overdose mortality rates involving methadone, all differences by sex were significant at P < .001 using the Pearson χ2 test with Bonferroni corrections to compare differences. Data source: Centers for Disease Control and Prevention Wide-ranging ONline Data for Epidemiologic Research.19
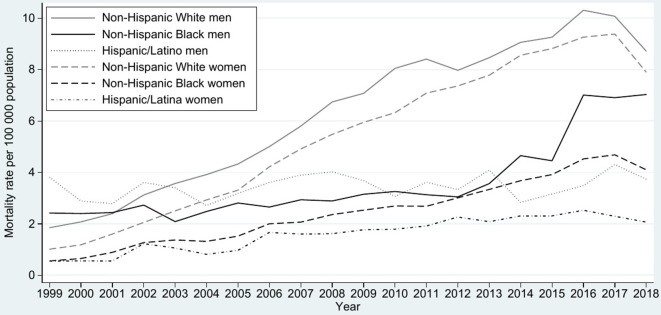
Overdose mortality rates per 100 000 population for natural and semisynthetic opioids rose steadily from 1999 to 2018; the rates increased steeply among non-Hispanic White adults (from 1.9 to 8.7 for men and from 1.0 to 7.9 for women), increased modestly among non-Hispanic Black adults (from 2.4 to 7.0 for men and from 0.6 to 4.1 for women), and were stable for Hispanic/Latinx adults (from 3.8 to 3.7 for men and from 0.6 to 2.1 for women; Figure 2). Among all 3 racial/ethnic groups, men had higher overdose mortality rates for natural and semisynthetic opioids than women of the same race/ethnicity.
Figure 2.
Overdose mortality rates involving natural and semisynthetic opioids among adults aged 45-64, United States, 1999-2018. Natural opioids include drugs such as morphine and codeine, and semisynthetic opioids include drugs such as oxycodone, hydrocodone, hydromorphone, and oxymorphone. Mortality rates may be unreliable when the death count is <20. The following subgroups had death counts <20 for the years specified: non-Hispanic Black women (1999) and Hispanic/Latina women (1999, 2000, and 2001). Data source: Centers for Disease Control and Prevention Wide-ranging ONline Data for Epidemiologic Research.19
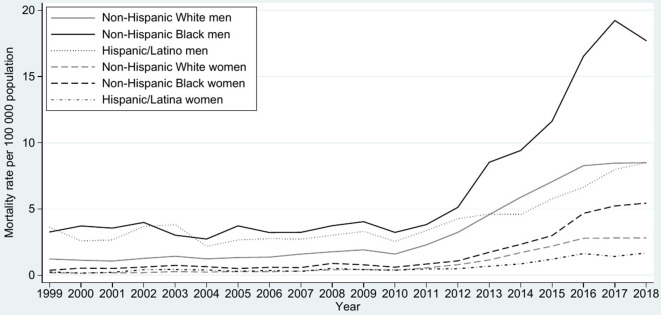
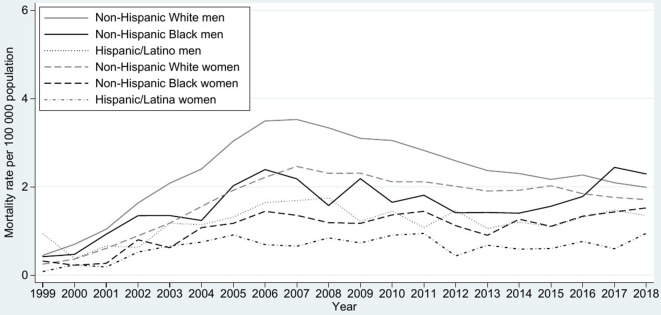
Heroin overdose mortality rates among adults aged 45-64 were relatively flat across all groups by race/ethnicity and sex until the late 2000s (Figure 3). Overdose mortality rates per 100 000 population from 1999 to 2018 increased modestly among women in each racial/ethnic group, although the increase was highest among non-Hispanic Black women (from 0.4 to 5.4), followed by non-Hispanic White women (from 0.2 to 2.8) and Hispanic/Latina women (from 0.3 to 1.8). The increase was higher among non-Hispanic Black men (from 3.3 to 17.7) than among non-Hispanic White men (from 1.2 to 8.5) and Hispanic/Latino men (from 3.6 to 8.5).
Figure 3.
Overdose mortality rates involving heroin among adults aged 45-64, United States, 1999-2018. Heroin is an illicit opioid synthesized from morphine. Mortality rates may be unreliable when the death count is <20. The following subgroups had death counts <20 for the years specified: non-Hispanic Black women (1999-2001) and Hispanic/Latina women (1999-2007 and 2009-2010). Data source: Centers for Disease Control and Prevention Wide-ranging ONline Data for Epidemiologic Research.19
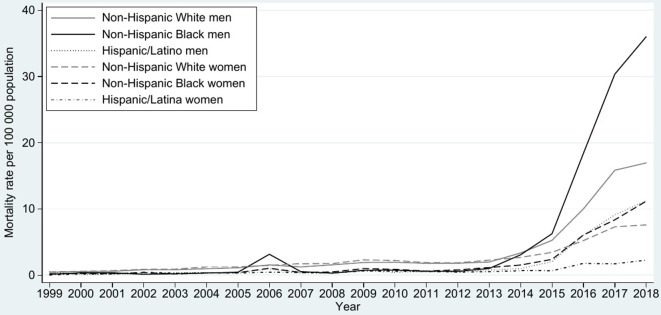
Synthetic opioid overdose mortality rates per 100 000 population were low among all adults aged 45-64 from 1999 until the early 2010s (Figure 4). In all 3 racial/ethnic groups, from 1999 to 2018, men had a greater increase in overdose mortality rates for synthetic opioids than women did. However, non-Hispanic Black women had the greatest increases in overdose mortality (from 0.2 to 11.2), followed by non-Hispanic White (from 0.3 to 7.6) and Hispanic/Latina (from 0.04 to 2.3) women. Among all adults, the largest increase in overdose mortality rates for synthetic opioids was among non-Hispanic Black men (from 0.1 to 36.0), followed by non-Hispanic White (from 0.5 to 17.0) and Hispanic/Latino (from 0.5 to 11.3) men.
Figure 4.
Overdose mortality rates involving synthetic opioids among adults aged 45-64, United States, 1999-2018. Synthetic opioids (excluding methadone) include drugs such as fentanyl, fentanyl analogues, and tramadol. Mortality rates may be unreliable when the death count is <20. The following subgroups had death counts <20 for the years specified: non-Hispanic Black men (1999-2005 and 2008), Hispanic/Latino men (1999-2005 and 2007-2008), non-Hispanic Black women (1999-2005), and Hispanic/Latina women (1999-2008). Data source: Centers for Disease Control and Prevention Wide-ranging ONline Data for Epidemiologic Research.19
Methadone overdose mortality rates were low and stable compared with mortality rates for other opioid types; they peaked in 2006 followed by a decline, especially among non-Hispanic White people (Figure 5). However, the increase in methadone overdose mortality rates per 100 000 population was higher among non-Hispanic Black (from 0.4 to 2.3) than among non-Hispanic White (from 0.5 to 2.0) and Hispanic/Latino (from 0.9 to 1.4) men. Increases were low for all women (from 0.3 to 1.7 for non-Hispanic White women; from 0.3 to 1.5 for non-Hispanic Black women; and from 0.1 to 1.0 for Hispanic/Latina women).
Figure 5.
Overdose mortality rates involving methadone among adults aged 45-64, United States, 1999-2018. Methadone is a synthetic opioid commonly prescribed for the treatment of opioid use disorder. Mortality rates may be unreliable when the death count is <20. The following subgroups had death counts <20 for the years specified: non-Hispanic Black men (1999-2000), Hispanic/Latino men (2000-2002), non-Hispanic Black women (1999-2001), and Hispanic/Latina women (1999-2002). Data source: Centers for Disease Control and Prevention Wide-ranging ONline Data for Epidemiologic Research.19
Discussion
Our findings demonstrate that overall opioid overdose mortality trends among adults aged 45-64 were high and mirror those of the opioid overdose epidemic as a whole: a wave of natural and semisynthetic opioid overdose deaths, followed by a second wave of heroin deaths, and most recently a surge in synthetic opioid overdose deaths, predominantly consisting of fentanyl and fentanyl analogue overdoses.23 Our findings suggest that the posited narrative of the opioid epidemic consisting of people who had been prescribed opioids and developed OUD, then began using heroin, and then moved to using fentanyl/fentanyl-laced heroin does not describe the trends observed among non-Hispanic Black men aged 45-64. These men are dying at high rates from heroin and synthetic opioids without having had the same increases in rates of overdose mortality from natural and semisynthetic opioids as non-Hispanic White people in the preceding years. Racial/ethnic disparities in opioid-prescribing practices may account for some of these differences; non-Hispanic Black people are less likely to be prescribed opioid analgesics for pain,24 less likely to be referred to a pain specialist,25 and more likely to be subjected to urine drug testing during chronic opioid therapy than non-Hispanic White people.25
In our study, non-Hispanic Black people aged 45-64 were at a higher risk of heroin and synthetic opioid overdose mortality than other racial/ethnic groups. One study found that non-Hispanic White people had the highest rates of fentanyl overdose mortality,11 but that study included all age groups together, which may have obscured differences in opioid overdose mortality rates among middle-aged adults by racial/ethnic group observed in the current study. Non-Hispanic Black people may hesitate to call 911 during an overdose emergency because of fear of arrest, historically negative interactions with police, and distrust of law enforcement officers.26 Non-Hispanic Black men are also disproportionately incarcerated compared with other racial/ethnic groups,27 and the risk of overdose mortality is significantly higher among people released from incarceration than among nonincarcerated people.28 Other social determinants may also affect opioid overdose mortality rates among non-Hispanic Black people. For example, poverty is associated with an elevated risk of opioid overdose, particularly in urban areas.29
Consistent with national data demonstrating a greater use of prescription opioids among non-Hispanic White adults than among adults in other racial/ethnic groups,30 our findings showed that non-Hispanic White adults aged 45-64 had the highest overdose mortality rates for natural and semisynthetic opioids. National data indicate that overdose mortality rates for heroin now exceed overdose mortality rates for natural and semisynthetic opioids.8 However, our data indicate that more non-Hispanic White men aged 45-64 are dying of natural and semisynthetic opioid overdose than of heroin overdose. These findings largely mirror the opioid overdose epidemic as a whole, showing an increase in natural and semisynthetic opioid overdose mortality among middle-aged non-Hispanic White people.31
In our study, men had higher rates of opioid overdose mortality than women did, regardless of race/ethnicity and across all opioid types, except for methadone. These findings are consistent with a recent report, which demonstrated that men had higher rates of fentanyl overdose mortality than women every year from 2011 to 2016.11 Likewise, CDC data from 2016 and 2017 showed that mortality rates from opioid overdose among men are more than twice that of women.23 Differences in opioid overdose mortality by sex in our study are consistent with known differences in opioid misuse by sex. A 2017 literature review concluded that women were more likely than men to be prescribed opioids,32 but national data show that men are more likely than women to misuse prescription opioids5 and develop OUD.33
Limitations
This study had several limitations. First, as a secondary data analysis, our selection of variables was limited to variables included in CDC WONDER. As such, we could not examine additional individual factors associated with opioid overdose mortality. Second, deaths of nonresidents (eg, nonresident aliens, nationals living abroad, and residents of Puerto Rico, Guam, the Virgin Islands, and other US territories) are not recorded in CDC WONDER and were not included in the current study. Third, death certificates without drug-specific information were excluded from this study. In these cases, toxicology tests may not have been performed or were unable to detect the opioid(s). The exclusion of nonresidents and death certificates without drug-specific information likely resulted in an underestimation of the true public health burden of opioid overdose mortality in the United States. Finally, we could not examine significant changes in mortality trends from 1999 to 2018 for some subgroups because mortality rates were considered unreliable with death counts <20.
Conclusions
Among adults aged 45-64 in the United States, non-Hispanic Black men are at the highest risk of heroin and fentanyl overdose deaths and had disproportionate increases in overdose mortality rates from heroin and fentanyl in recent years. Despite high overdose mortality rates from heroin and synthetic opioids, non-Hispanic Black people did not have the same increases in overdose mortality rates from natural and semisynthetic opioids in preceding years. Our findings illuminate alternative trajectories of opioid use and the need to consider unique subgroup risks in the development of effective public health interventions and policymaking to address the opioid overdose epidemic. Widespread criminal justice reform is needed to tackle racial/ethnic disparities in opioid overdose mortality, including decriminalization of substance use, which may help to reduce both the stigma associated with seeking treatment for OUD and the overdose risks observed among people postincarceration. Furthermore, we recommend increasing the use of medication-assisted treatment and other evidence-based treatment practices for OUD in correctional facilities, as well as broad police reform with an emphasis on improving relations in Black communities and training on the use of naloxone. In addition, policies that address fundamental determinants of health, including educational and housing reform, are likely to affect this disparity. We also recommend the use of community-based participatory research strategies to identify additional underlying factors in heroin and fentanyl overdose mortality among non-Hispanic Black men, which may inform tailored interventions and other targeted policies to curb the opioid overdose epidemic in this population.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Health Resources and Services Administration award number T32HP30035 in support of Rachel A. Hoopsick (principal investigator: Linda S. Kahn), National Center for Advancing Translational Sciences (UL1TR001412), and National Institute on Drug Abuse (R01DA034072).
ORCID iD
Rachel A. Hoopsick, PhD, MS, MPH, MCHES https://orcid.org/0000-0001-5992-9007
References
- 1. Case A., Deaton A. Rising morbidity and mortality in midlife among White non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078-15083. 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Manchikanti L., Kaye AM., Knezevic NN. et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2017;20(2 suppl):S3-S92. [PubMed] [Google Scholar]
- 3. Chen X., Wang Y., Yu X. et al. Large-scale analysis of opioid poisoning related hospital visits in New York State. AMIA Annu Symp Proc. 2018;2017:545-554. [PMC free article] [PubMed] [Google Scholar]
- 4. Hasegawa K., Espinola JA., Brown DFM., Camargo CA, Jr. Trends in U.S. emergency department visits for opioid overdose, 1993-2010. Pain Med. 2014;15(10):1765-1770. 10.1111/pme.12461 [DOI] [PubMed] [Google Scholar]
- 5. Han BH., Sherman SE., Palamar JJ. Prescription opioid misuse among middle-aged and older adults in the United States, 2015-2016. Prev Med. 2019;121:94-98. 10.1016/j.ypmed.2019.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guy GP, Jr., Zhang K., Bohm MK. et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697-704. 10.15585/mmwr.mm6626a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schieber LZ., Guy GP, Jr., Seth P. et al. Trends and patterns of geographic variation in opioid prescribing practices by state, United States, 2006-2017. JAMA Netw Open. 2019;2(3):e190665. 10.1001/jamanetworkopen.2019.0665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hedegaard H., Miniño AM., Warner M. Drug overdose deaths in the United States, 1999-2017. NCHS Data Brief. 2018;329:1-8. [PubMed] [Google Scholar]
- 9. Jones CM., Baldwin GT., Manocchio T., White JO., Mack KA. Trends in methadone distribution for pain treatment, methadone diversion, and overdose deaths—United States, 2002-2014. MMWR Morb Mortal Wkly Rep. 2016;65(26):667-671. 10.15585/mmwr.mm6526a2 [DOI] [PubMed] [Google Scholar]
- 10. Muhuri PK., Gfroerer JC., Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ Data Rev. 2013:1-17. Accessed August 8, 2020. https://www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm
- 11. Spencer MR., Warner M., Bastian BA., Trinidad JP., Hedegaard H. Drug overdose deaths involving fentanyl, 2011-2016. Natl Vital Stat Rep. 2019;68(3):1-19. [PubMed] [Google Scholar]
- 12. Unick GJ., Rosenblum D., Mars S., Ciccarone D. Intertwined epidemics: national demographic trends in hospitalizations for heroin- and opioid-related overdoses, 1993-2009. PLoS One. 2013;8(2):e54496. 10.1371/journal.pone.0054496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Compton WM., Jones CM., Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(2):154-163. 10.1056/NEJMra1508490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers—United States, 2002-2004 and 2008-2010. Drug Alcohol Depend. 2013;132(1-2):95-100. 10.1016/j.drugalcdep.2013.01.007 [DOI] [PubMed] [Google Scholar]
- 15. Macmadu A., Carroll JJ., Hadland SE., Green TC., Marshall BDL. Prevalence and correlates of fentanyl-contaminated heroin exposure among young adults who use prescription opioids non-medically. Addict Behav. 2017;68:35-38. 10.1016/j.addbeh.2017.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pichini S., Solimini R., Berretta P., Pacifici R., Busardò FP. Acute intoxications and fatalities from illicit fentanyl and analogues: an update. Ther Drug Monit. 2018;40(1):38-51. 10.1097/FTD.0000000000000465 [DOI] [PubMed] [Google Scholar]
- 17. Substance Abuse and Mental Health Services Administration . Key Substance Use and Mental Health Indicators in the United States: Results From the 2018 National Survey on Drug Use and Health. HHS Pub No PEP19-5068, NSDUH Series H-54. Center for Behavioral Health Statistics and Quality; 2019.
- 18. Shiels MS., Freedman ND., Thomas D., Berrington de Gonzalez A. Trends in U.S. drug overdose deaths in non-Hispanic Black, Hispanic, and non-Hispanic White persons, 2000-2015. Ann Intern Med. 2018;168(6):453-455. 10.7326/M17-1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Centers for Disease Control and Prevention, National Center for Health Statistics . CDC Wide-ranging ONline Data for Epidemiologic Research: multiple cause of death. Accessed February 26, 2019. https://wonder.cdc.gov/
- 20. Dowell D., Haegerich TM., Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624-1645. 10.1001/jama.2016.1464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. World Health Organization . International Statistical Classification of Diseases and Related Health Problems, 10th Revision. World Health Organization; 2016. [Google Scholar]
- 22. US Department of Health and Human Services . Technical appendix from vital statistics of United States: 1999 mortality. 2004. Accessed February 26, 2019. https://wonder-cdc-gov.gate.lib.buffalo.edu/wonder/help/CMF/TechnicalAppendix1999.pdf
- 23. Scholl L., Seth P., Kariisa M., Wilson N., Baldwin G. Drug and opioid-involved overdose deaths—United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419-1427. 10.15585/mmwr.mm675152e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pletcher MJ., Kertesz SG., Kohn MA., Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70-78. 10.1001/jama.2007.64 [DOI] [PubMed] [Google Scholar]
- 25. Hausmann LRM., Gao S., Lee ES., Kwoh CK. Racial disparities in the monitoring of patients on chronic opioid therapy. Pain. 2013;154(1):46-52. 10.1016/j.pain.2012.07.034 [DOI] [PubMed] [Google Scholar]
- 26. Latimore AD., Bergstein RS. “Caught with a body” yet protected by law? Calling 911 for opioid overdose in the context of the Good Samaritan Law. Int J Drug Policy. 2017;50:82-89. 10.1016/j.drugpo.2017.09.010 [DOI] [PubMed] [Google Scholar]
- 27. Federal Bureau of Prisons . Inmate statistics. Published 2019. Accessed April 15, 2019. https://www.bop.gov/about/statistics
- 28. Pizzicato LN., Drake R., Domer-Shank R., Johnson CC., Viner KM. Beyond the walls: risk factors for overdose mortality following release from the Philadelphia Department of Prisons. Drug Alcohol Depend. 2018;189:108-115. 10.1016/j.drugalcdep.2018.04.034 [DOI] [PubMed] [Google Scholar]
- 29. Pear VA., Ponicki WR., Gaidus A. et al. Urban–rural variation in the socioeconomic determinants of opioid overdose. Drug Alcohol Depend. 2019;195:66-73. 10.1016/j.drugalcdep.2018.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Frenk SM., Porter KS., Paulozzi LJ. Prescription opioid analgesic use among adults: United States, 1999-2012. NCHS Data Brief. 2015;189:1-8. [PubMed] [Google Scholar]
- 31. Alexander MJ., Kiang MV., Barbieri M. Trends in Black and White opioid mortality in the United States, 1979-2015. Epidemiology. 2018;29(5):707-715. 10.1097/EDE.0000000000000858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Serdarevic M., Striley CW., Cottler LB. Sex differences in prescription opioid use. Curr Opin Psychiatry. 2017;30(4):238-246. 10.1097/YCO.0000000000000337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Han B., Compton WM., Blanco C., Crane E., Lee J., Jones CM. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293-301. 10.7326/M17-0865 [DOI] [PubMed] [Google Scholar]