Abstract
Objectives
Hospitals are on the front lines of the opioid epidemic, seeing patients who overdose or have complicated infections, but the extent of services offered or whether services are evidence-based is not known. The objective of our study was to assess the extent to which nonprofit hospitals are addressing opioid abuse, a critical public health issue, through their community benefit work and to identify which evidence-based strategies they adopt.
Methods
We reviewed community benefit documents from January 1, 2015, through December 31, 2018, for a sample (N = 446) of all nonprofit hospitals in the United States. We classified hospital opioid-related strategies into 9 categories. Using logistic regression, we predicted the likelihood of hospitals adopting various strategies to address opioid abuse.
Results
Of the 446 nonprofit hospitals in our sample, 49.1% (n = 219) adopted ≥1 clinical strategy to address opioid use disorder in their community. Approximately one-quarter (26.5%; n = 118) of hospitals adopted a strategy related to treatment services for substance use disorder; 28.2% (n = 126) had ≥1 program focused on connecting patients to a primary care medical home, and 14.6% (n = 65) focused on caring for patients with opioid-related overdoses in the emergency department. We also identified factors that predicted involvement in programs that were less common than clinical strategies, but potentially effective, such as harm reduction and prescriber initiatives (both 6.3% of hospitals).
Conclusions
Evidence-based prevention and treatment require strong collaboration between health care and community institutions at all levels. Effective policy interventions may exist to encourage various types and sizes of nonprofit hospitals to adopt evidence-based interventions to address opioid abuse in their communities.
Keywords: opioids, policy, public health, hospitals, Affordable Care Act
The number of deaths caused by opioid-related overdose continues to increase. Opioid-related deaths increased nearly 6 times from 1999 to 2018; in 2018, opioids were involved in 46 802 overdose deaths, and economic experts estimate that opioid-related health care costs have reached $500 billion per year.1,2 The most recent data from the Centers for Disease Control and Prevention’s National Syndromic Surveillance Program showed that 142 557 emergency department (ED) visits from July 2016 through September 2017 were likely opioid-related overdoses.3 These data provide a strong rationale for new preventive and treatment strategies to improve health outcomes and limit unnecessary health care spending. Effective interventions to address opioid use disorder (OUD) exist, but many interventions require cross-sector collaboration and the engagement of a broad range of health care and community institutions.4-6
OUD-related services are often part of the range of community benefits provided by nonprofit hospitals as required by the Internal Revenue Service and expanded as part of the Affordable Care Act.7 In this study, we define OUD-related services as prevention, early intervention, and treatment services provided or supported by hospitals (and their systems). Nonprofit hospitals that receive tax exemption as charitable organizations must provide community benefits, including offering charity care, conducting research, and promoting community health-building activities, to improve local population health.7 Since 2012, hospitals also are required to conduct a community health needs assessment (CHNA) every 3 years to identify critical local health needs and develop a formal implementation strategy. Although many hospitals identify OUD as important in their CHNAs, the extent to which hospitals are adopting OUD-related services as part of these new community benefit requirements or which strategies they adopt is unknown.
Hospitals are on the front lines of the opioid epidemic, seeing overdose patients in the ED, treating complicated infections, and offering outpatient and inpatient treatment services for OUD.8,9 Hospitals may also serve as anchor institutions in many communities, promoting economic development and participating in community-based partnerships that may affect opioid use and local responses to the opioid epidemic.10,11 According to the National Academy of Medicine, community partnerships are critical to addressing public health challenges,12 and research suggests that hospitals are high-value participants in public health networks.13
Hospitals may participate in a spectrum of OUD-related interventions through their community benefit responsibilities, but currently we do not know the extent of their contributions or whether they are evidence-based. Hospitals may, for example, serve in public health networks to coordinate prevention of opioid misuse or engage in policy advocacy. Hospitals also participate in a range of clinical activities that may be particularly effective if they involve medication-assisted treatment (MAT) for OUD. One recent study of hospital treatment services indicated that the number of services provided by hospitals decreased as the opioid epidemic increased nationally.14 Several studies documented promising approaches that hospitals use to engage patients in the ED or inpatient services to initiate MAT before discharge.15,16 Because patients with OUD have high rates of secondary infections, such as infective endocarditis, hepatitis C virus, HIV, and skin and soft tissue infections,17,18 hospitals are ideal sites to connect with patients to begin treatment and offer harm reduction services. Focusing on the inpatient setting, researchers also documented the use of interprofessional teams to provide addiction consultation services.19 These teams can screen and initiate treatment for inpatients with substance use disorder (SUD). The existing literature on hospitals suggests that expanded OUD-related engagement in hospital settings may be particularly effective in improving health outcomes and decreasing readmissions.20 Harm reduction services may be more effective when embedded in the ED rather than as stand-alone services.21 For example, hospitals have successfully staged syringe exchange and naloxone dispensing programs.19,22,23
The aim of our study, accordingly, was to assess the approaches that nonprofit hospitals in the United States are adopting to address OUD as part of their community benefit responsibilities. Our objective was to describe the extent to which hospitals are investing in clinical strategies in which MAT can be initiated and harm reduction services provided. We also explored the hospital, community, and state policy environments in which these services are offered to determine whether environmental factors shape decisions to adopt and implement evidence-based interventions. We hypothesized that small nonteaching hospitals would be less likely than large teaching hospitals to adopt evidence-based treatment and harm reduction services and that associated state policies would encourage these efforts. Understanding the factors that shape decisions to address OUD is important to overcome barriers and develop policy interventions to encourage hospital adoption of effective services to treat OUD.
Methods
Data and Sample
We constructed a data set from several sources to explore how nonprofit hospitals in the United States are addressing OUD in their communities. Using the American Hospital Association’s (AHA’s) 2015 American Hospital Directory,24 we first took a 20% random sample of all US nonprofit hospitals (n = 2715) in each state, rounding up to the nearest whole number of hospitals, to construct our data set (n = 613). The AHA is a national advocacy organization that represents more than 80% of nonprofit, for-profit, public, and government community and specialty hospitals. They provide several databases for researchers, including annual survey data and the American Hospital Directory, which provides organizational information for nearly all hospitals in the United States. For our sample of hospitals, we collected the publicly available CHNAs and list of implementation strategies, which together comprise the entire community benefit report, from each organization’s website and coded them to classify the implementation strategies adopted. We reviewed each hospital’s most recent community benefit report, the dates for which ranged from January 1, 2015, through December 31, 2018, depending on when the hospital started its initial triennial reporting cycle. We merged this data set with several sources, including the AHA Annual Survey24 and the National Vital Statistics System,25 to include data on hospital, county, and state characteristics.
We also used a data set of state opioid policies, published by Wickramatilake and colleagues in 2017.26 These researchers disseminated a survey to state alcohol and drug agency directors and/or senior agency managers developed by the National Association of State Alcohol and Drug Abuse Directors. They collected data on programs in 7 broad categories of policy: targeted risk education, provider education, prescriber guidelines, naloxone access, prescription drug monitoring program (PDMP) reporting, MAT funding, and pain management regulations. We used these 7 categories as variables and added an eighth policy variable of whether the county was in a state that had expanded Medicaid. We created dichotomous variables for each type of policy, coding the presence of each type of policy in each state.
We reviewed each hospital implementation strategy and coded it as yes or no to indicate whether it addressed substance abuse with at least 1 program. If a hospital addressed substance abuse with at least 1 program, we read each implementation strategy and coded the number of strategies the hospital adopted to address OUD. Using the categorization scheme described by Wickramatilake and colleagues,26 we then classified each implementation strategy into 1 of 9 categories: 3 clinical approaches (SUD treatment, primary care, and ED services) and 6 other strategies (harm reduction, prescriber initiatives, targeted risk education, social determinants, policy advocacy, and community coalition building) (Table 1). If a hospital did not provide information on implementation strategies or other information publicly, we contacted the hospital and requested this information. After excluding hospitals that did not provide their implementation strategies (n = 89) and eliminating hospitals for which county data were missing, 466 hospitals remained in our sample. Given that our study focused on hospitals that adopted strategies to address OUD after first identifying this need in their CHNA, we also excluded hospitals that did not list SUD as a need in their CHNA (n = 20), bringing the analytic sample to 446 hospitals (Figure).
Table 1.
Types of implementation strategies used by a national sample of nonprofit hospitals (N = 446) to address opioid abuse, United States, 2015-2018a
| Category | Description | Examples |
|---|---|---|
| Clinical approach | ||
| Substance use disorder treatment | Programs that support hospital-based or external services to treat substance use disorders | Increasing the number of available health care providers; improving access to MAT; providing financial assistance to patients for inpatient substance abuse services |
| Primary care | Programs that support access to services in the primary care setting | Implementing substance abuse screening in primary care in general and for special populations (eg, pregnant women); helping patients connect with a primary care medical home; supporting behavioral health and primary care integration |
| ED services | Programs that are run primarily in the ED | Providing educational resources at discharge; distributing drug lockboxes; offering pain management consultations; researching needs of patients using the ED for conditions related to substance abuse; screening in the ED; hiring a full-time behavioral health provider for the ED; initiating MAT in the ED |
| Nonclinical | ||
| Harm reduction | Programs that aim to prevent overdose and secondary infections from intravenous drug use | Syringe exchange programs; naloxone distribution in the ED; supplying police with naloxone |
| Prescriber initiatives | Programs that seek to improve prescribing practices | Prescriber guidelines; prescription drug monitoring programs |
| Risk education | Programs that provide preventive education to general and special populations | Populations included schools, seniors, health care professionals, and parents; other initiatives include medication take-back events and stigma reduction workshops |
| Social determinants | Programs that explicitly address health disparities and/or the health outcomes of underserved populations | Initiatives to reduce toxic stress; substance abuse screening for underserved populations; cultural competence training for substance abuse service providers; programs for homeless patients |
| Policy advocacy | Programs that support policy change at the local, state, or federal level | Advocating for prevention funding; criminal justice reform; statewide public health prioritization of substance abuse; full implementation of behavioral health parity legislation |
| Community coalition building | Programs that facilitate collaboration with public health and behavioral health treatment providers in the community | Providing financial support for community coalitions; facilitating community-wide meetings; supporting coalitions aimed at improving health care access; establishing a health advisory council; partnering with the local health department |
Abbreviations: ED, emergency department; MAT, medication-assisted treatment.
aData were collected from community health needs assessments and implementation strategies described on hospital websites and, when necessary, by contacting the hospital directly.
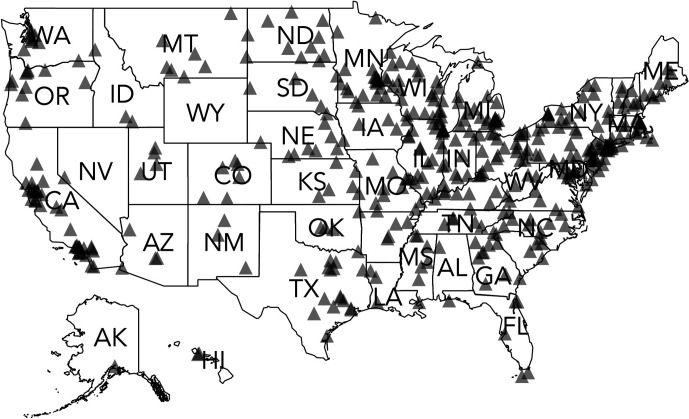
Figure.
Location of a sample of 446 nonprofit hospitals used to explore how nonprofit hospitals are addressing opioid use disorder in their communities, United States, 2015-2018. Sample was drawn from a 20% random sample of all US nonprofit hospitals (n = 2715) in each state using the American Hospital Association’s 2015 Annual Survey database.25
The first author (B.F.) and a research assistant coded the CHNAs and implementation strategies. The research assistant underwent extensive training at the beginning of the project to ensure adequate knowledge of community benefit reports and the coding strategy. At the outset, we established a codebook for the 9 strategies and used this codebook to evaluate each report. Because community benefit reports are highly structured (regulated by federal tax law), the 2 coders had a high level of consistency in coding. We assessed reliability by selecting random reports to code and comparing code applications. We did not conduct a formal interrater reliability analysis, because all coding tested was consistent. Eight reports did not identify community health needs or implementation strategies. For example, a hospital provided an overview of the CHNA process instead of describing findings. In these situations, we flagged the entries and met to code them collaboratively.
To our database of community benefit approaches, we added information on hospital characteristics from the 2015 AHA Annual Survey.24 We collected information on the total number of beds (categorized as <50, 50-199, 200-399, or ≥400 beds), whether the hospital belonged to a health system (yes or no), and whether it was a teaching hospital (ie, an academic medical center) (yes or no). To assess the extent to which our 20% random sample of US hospitals represented the entire population of hospitals, we compared our sample hospitals with the 2715 nonprofit hospitals included in the 2015 AHA Annual Survey. We compared the following hospital characteristics: system membership, teaching status, bed size, and rural or urban location. We conducted t tests to compare our sample with the entire population of nonprofit hospitals. With the exception of hospitals in the largest bed-size category (≥400 beds), our sample hospitals were not significantly different from the entire hospital population. Our sample did have a slightly higher percentage of hospitals with ≥400 beds (15% in the study sample vs 12% in the AHA population).
To describe the communities surrounding each hospital, we obtained county-level data on the percentage of residents living <138% below the federal poverty level and whether the county was urban or rural from the Health Resources & Services Administration’s Area Health Resources File.27 We obtained data on the rate of county overdose from the Centers for Disease Control and Prevention’s National Vital Statistics System 2015 mortality data.25
Analytic Strategy
We used logistic regression to evaluate the association between hospitals and community characteristics and the types of OUD initiatives implemented by hospitals. We conducted separate analyses for each hospital strategy, coding hospitals adopting the strategy as 1 and hospitals not adopting the strategy as 0. We used a 2-tailed Wald χ2 test to detect differences at a P value of < .05. Given that more than half of the hospitals in the study adopted ≥1 clinical approach, we conducted a post hoc analysis to understand how strategies may have been commonly occurring together. We conducted all statistical analyses using Stata version 15 (StataCorp LLC). Because this study used only secondary data, it was not considered humans subjects research by our institutional review board.
Results
Of the 446 nonprofit hospitals in our sample, 49.1% (n = 219) adopted ≥1 clinical strategy to address OUD in their community. Approximately one-quarter (26.5%; n = 118) of hospitals adopted a strategy related to SUD treatment services, 28.2% (n = 126) had ≥1 program focused on connecting patients to a primary care medical home, and 14.6% (n = 65) focused on caring for patients with opioid-related overdoses in the ED (Table 2). Hospitals also adopted nonclinical strategies: 32.5% (n = 141) adopted a targeted risk education program, and 25.3% (n = 113) joined a local community coalition aimed at addressing OUD in their community. Hospital participation in harm reduction programs (6.3%; n = 28), prescriber initiatives (6.3%; n = 28), strategies to address the social determinants of health (7.0%; n = 31), and engagement in policy advocacy (4.3%; n = 19) were less common.
Table 2.
Characteristics of a national sample of nonprofit hospitals (N = 446) used to explore how nonprofit hospitals are addressing opioid use disorder in their communities, United States, 2015-2018a
| Characteristics | No. (%)b |
|---|---|
| Hospital-implemented initiative | |
| Offer substance use disorder treatment services | |
| Yes | 118 (26.5) |
| No | 328 (73.5) |
| Support access to services in the primary care setting | |
| Yes | 126 (28.2) |
| No | 320 (71.8) |
| Offer harm reduction programs | |
| Yes | 28 (6.3) |
| No | 418 (93.7) |
| Adopt prescriber initiatives | |
| Yes | 28 (6.3) |
| No | 418 (93.7) |
| Offer targeted risk education programs | |
| Yes | 141 (32.6) |
| No | 305 (68.4) |
| Address the social determinants of health | |
| Yes | 31 (7.0) |
| No | 415 (93.0) |
| Care for opioid overdoses in the emergency department | |
| Yes | 65 (14.6) |
| No | 381 (85.4) |
| Engage in policy advocacy at the local, state, or federal level | |
| Yes | 19 (4.3) |
| No | 427 (95.7) |
| Join a local community coalition aimed at addressing opioid use disorder in community | |
| Yes | 113 (25.3) |
| No | 333 (74.7) |
| Hospital characteristics | |
| Hospital belongs to a health care system | |
| Yes | 322 (72.2) |
| No | 124 (27.8) |
| Hospital is a teaching hospital | |
| Yes | 37 (8.3) |
| No | 409 (91.7) |
| No. of beds at hospital | |
| <50 | 117 (26.2) |
| 50-199 | 159 (35.6) |
| 200-399 | 97 (21.8) |
| ≥400 | 65 (14.6) |
| County characteristics | |
| Rural location | |
| Yes | 162 (36.3) |
| No | 284 (63.7) |
| Mean (SD) percentage <138% federal poverty level | 22.4 (7.1) |
| State policiesc | |
| Medicaid expansion | |
| Yes | 304 (68.2) |
| No | 142 (31.8) |
| Targeted risk education | |
| Yes | 243 (54.5) |
| No | 203 (45.5) |
| Provider education | |
| Yes | 299 (67.1) |
| No | 147 (33.0) |
| MAT funding | |
| Yes | 318 (71.3) |
| No | 128 (28.7) |
| Naloxone access | |
| Yes | 296 (66.4) |
| No | 150 (33.6) |
| PDMP reporting | |
| Yes | 225 (50.5) |
| No | 221 (49.5) |
| Pain regulations | |
| Yes | 118 (26.5) |
| No | 328 (73.5) |
| Prescriber guidelines | |
| Yes | 223 (50.0) |
| No | 223 (50.0) |
Abbreviations: MAT, medication-assisted treatment; PDMP, prescription drug monitoring program; SD, standard deviation.
aSample was drawn from a 20% random sample of all US nonprofit hospitals (n = 2715) in each state using the American Hospital Association’s 2015 Annual Survey database.24
bPercentages may not add to 100% because of rounding.
cList of 7 state policies was developed by Wickramatilake and colleagues26; Medicaid expansion was added by the authors.
Several key hospital characteristics were associated with the adoption of clinical strategies to address OUD by hospitals (Tables 3 and 4). Teaching hospitals were more likely than nonteaching hospitals to adopt primary care approaches (odds ratio [OR] = 2.47; 95% CI, 1.00-6.05; P = .049), whereas system hospitals were more likely than nonsystem hospitals to adopt nonclinical strategies such as targeted risk education programs (OR = 1.67; 95% CI, 1.01-2.75; P = .04). Hospital bed size was also a significant predictor of the type of strategy adopted by hospitals: hospitals with 200-399 beds were more likely than very large (≥400 beds) hospitals to adopt primary care approaches (OR = 2.22; 95% CI, 1.00-4.93; P = .049).
Table 3.
Association of hospital, community, and state policy factors and 5 of 9 hospital-implemented substance abuse initiatives among a national sample of nonprofit hospitals (N = 446) to explore how nonprofit hospitals are addressing opioid use disorder in their communities, United States, 2015-2018a
| Characteristic | Hospital-implemented initiative | ||||
|---|---|---|---|---|---|
| Substance abuse treatment | Primary care | Harm reduction | Prescriber initiatives | Risk education | |
| Hospital characteristics | |||||
| Hospital belongs to a health care system | |||||
| Yes | 0.96 (0.57-1.60) | 1.03 (0.62-1.72) | 1.29 (0.49-3.43) | 0.60 (0.26-1.40) | 1.67 (1.01-2.75)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Hospital is a teaching hospital | |||||
| Yes | 1.03 (0.43-2.49) | 2.47 (1.00-6.05)b | 0.93 (0.17-5.05) | 1.50 (0.33-6.81) | 0.99 (0.40-2.42) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| No. of beds at hospital | |||||
| <50 | 0.69 (0.30-1.60) | 1.35 (0.54-3.38) | 1.81 (0.38-8.60) | 0.74 (0.14-4.00) | 0.77 (0.33-1.76) |
| 50-199 | 0.55 (0.26-1.15) | 1.70 (0.76-3.79) | 0.28 (0.06-1.30) | 1.11 (0.25-4.91) | 0.75 (0.36-1.57) |
| 200-399 | 0.55 (0.26-1.17) | 2.22 (1.00-4.93)b | 0.35 (0.07-1.67) | 1.06 (0.25-4.44) | 1.16 (0.56-2.44) |
| ≥400 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| County characteristics | |||||
| Rural location | |||||
| Yes | 0.81 (0.46-1.44) | 0.86 (0.48-1.53) | 0.39 (0.12-1.25) | 1.01 (0.36-2.79) | 1.95 (1.14-3.36)b |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Percentage <138% federal poverty level | 0.96 (0.93-0.99)b | 0.98 (0.95-1.01) | 0.93 (0.87-1.00) | 1.01 (0.95-1.07) | 0.96 (0.93-0.99)b |
| State policiesc | |||||
| Medicaid expansion | |||||
| Yes | 1.68 (0.88-3.20) | 0.69 (0.37-1.29) | 2.13 (0.59-7.70) | 2.16 (0.65-7.22) | 1.32 (0.74-2.37) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Targeted risk education | |||||
| Yes | 1.09 (0.65-1.81) | 1.73 (1.05-2.87)b | 4.39 (1.26-15.26)b | 2.25 (0.82-6.20) | 1.14 (0.72-1.82) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Provider education | |||||
| Yes | 0.71 (0.41-1.22) | 0.43 (0.25-0.76)d | 0.28 (0.11-0.73)b | 1.44 (0.54-3.84) | 0.93 (0.55-1.56) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| MAT funding | |||||
| Yes | 0.78 (0.41-1.49) | 1.55 (0.81-2.98) | 0.15 (0.03-0.79)b | 0.31 (0.08-1.17) | 0.72 (0.40-1.31) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Naloxone access | |||||
| Yes | 1.34 (0.71-2.54) | 1.41 (0.76-2.59) | 8.43 (1.61-44.21)b | 1.25 (0.34-4.59) | 1.57 (0.88-2.80) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| PDMP reporting | |||||
| Yes | 1.29 (0.73-2.29) | 0.87 (0.49-1.52) | 1.95 (0.47-8.16) | 3.54 (1.17-10.71)b | 1.06 (0.63-1.79) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Pain management regulations | |||||
| Yes | 1.21 (0.62-2.38) | 0.58 (0.30-1.13) | 4.51 (1.22-16.69)b | 1.03 (0.31-3.37) | 1.02 (0.55-1.90) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Prescriber guidelines | |||||
| Yes | 1.51 (0.89-2.57) | 2.34 (1.37-3.98)d | 1.01 (0.33-3.12) | 0.29 (0.11-0.81)d | 1.15 (0.71-1.88) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
Abbreviations: MAT, medication-assisted treatment; PDMP, prescription drug monitoring program.
aSample was drawn from a 20% random sample of all US nonprofit hospitals (n = 2715) in each state using the American Hospital Association’s 2015 Annual Survey database.24 All values are odds ratio (95% CI). Data on the other 4 hospital initiatives are presented in Table 4.
bSignificant at P < .05 using a 2-tailed Wald χ2 test.
cList of 7 state policies was developed by Wickramatilake and colleagues26; Medicaid expansion was added by the authors.
dSignificant at P < .01 using a 2-tailed Wald χ2 test.
Table 4.
Association of hospital, community, and state policy factors and 4 of 9 hospital-implemented substance abuse initiatives among a national sample of nonprofit hospitals (N = 446) used to explore how nonprofit hospitals are addressing opioid use disorder in their communities, United States, 2015-2018a
| Factor | Hospital-implemented initiative | |||
|---|---|---|---|---|
| Social determinants | Emergency department services | Policy advocacy | Community coalition | |
| Hospital characteristics | ||||
| Hospital belongs to a health care system | ||||
| Yes | 2.39 (0.82-6.97) | 0.69 (0.38-1.27) | 1.86 (0.50-6.95) | 1.10 (0.66-1.81) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Hospital is a teaching hospital | ||||
| Yes | 1.80 (0.29-10.97) | 0.79 (0.26-2.43) | 1.29 (0.26-6.39) | 0.75 (0.26-2.18) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| No. of beds at hospital | ||||
| <50 | 4.30 (0.60-30.58) | 0.58 (0.20-1.68) | 0.27 (0.05-1.56) | 1.51 (0.60-3.8) |
| 50-199 | 2.05 (0.33-12.71) | 0.73 (0.29-1.85) | 0.16 (0.03-0.82)b | 1.90 (0.82-4.37) |
| 200-399 | 4.52 (0.77-26.56) | 0.73 (0.28-1.89) | 0.63 (0.16-2.43) | 1.16 (0.48-2.77) |
| ≥400 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| County characteristics | ||||
| Rural location | ||||
| Yes | 1.72 (0.56-5.23) | 1.32 (0.66-2.66) | 1.95 (0.50-7.57) | 1.21 (0.70-2.09) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Percentage <138% federal poverty level | ||||
| Yes | 0.95 (0.90-1.02) | 1.00 (0.96-1.04) | 0.98 (0.91-1.06) | 0.99 (0.96-1.02) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| State policiesc | ||||
| Medicaid expansion | ||||
| Yes | 4.75 (0.88-25.67) | 1.08 (0.48-2.44) | 1.40 (0.33-5.92) | 0.94 (0.51-1.73) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Targeted risk education | ||||
| Yes | 0.86 (0.33-2.27) | 1.09 (0.58-2.05) | 0.58 (0.20-1.75) | 1.11 (0.68-1.82) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Provider education | ||||
| Yes | 0.49 (0.17-1.43) | 1.03 (0.52-2.03) | 2.53 (0.59-10.78) | 1.03 (0.60-1.76) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| MAT funding | ||||
| Yes | 2.87 (0.85-9.75) | 1.16 (0.50-2.68) | 0.79 (0.21-3.03) | 0.75 (0.40-1.42) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Naloxone access | ||||
| Yes | 1.85 (0.53-6.43) | 1.57 (0.69-3.60) | 1.41 (0.36-5.48) | 1.48 (0.79-2.76) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| PDMP reporting | ||||
| Yes | 0.37 (0.11-1.33) | 2.03 (1.00-4.12) | 1.01 (0.28-3.59) | 1.66 (0.96-2.87) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Pain management regulations | ||||
| Yes | 1.09 (0.27-4.46) | 0.34 (0.15-0.79)b | 1.69 (0.40-7.19) | 0.62 (0.32-1.18) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Prescriber guidelines | ||||
| Yes | 2.48 (0.77-7.97) | 1.76 (0.90-3.44) | 1.42 (0.42-4.79) | 0.91 (0.54-1.53) |
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
Abbreviations: MAT, medication-assisted treatment; PDMP, prescription drug monitoring program.
aSample was drawn from a 20% random sample of all US nonprofit hospitals (n = 2715) in each state using the American Hospital Association’s 2015 Annual Survey database.24 All values are odds ratio (95% CI). Data on the other 5 hospital initiatives are presented in Table 3.
bSignificant at P < .05 using a 2-tailed Wald χ2 test.
cList of 7 state policies was developed by Wickramatilake and colleagues26; Medicaid expansion was added by the authors.
Few state policy factors were associated with a willingness to adopt clinical strategies to address OUD. Hospitals in states that had implemented a policy to support risk education were more likely to adopt primary care approaches than not adopt this type of approach (OR = 1.73; 95% CI, 1.05-2.87; P = .03). In contrast, no state policies were associated with the implementation of SUD treatment services, and only pain management regulation was associated with the implementation of services in the ED (OR = 0.34; 95% CI, 0.15-0.79; P = .01).
We also found that harm reduction approaches were more common in states with support for naloxone access (OR = 8.43; 95% CI, 1.61-44.21; P = .01) than in states without this support. Hospitals in states with PDMP reporting were also more likely to adopt prescriber initiatives than hospitals in states without PDMP reporting (OR = 3.54; 95% CI, 1.17-10.71; P = .02). Hospitals in states with prescriber guidelines, however, were less likely than hospitals in states without prescriber guidelines to adopt prescriber initiatives as a community benefit strategy (OR = 0.29; 95% CI, 0.11-0.81; P = .02). The post hoc analysis showed relatively strong and significant correlations between substance abuse treatment and primary care (R = 0.17; SE, 0.08; P < .001) and between ED services and primary care (R = 0.19; SE, 0.09; P < .001), suggesting that some strategies were often bundled together by hospitals.
Discussion
Hospitals are investing in a range of strategies to address OUD, an acknowledgment of the scope of this public health challenge. Our results suggest, however, that considerable challenges remain for increasing the availability of evidence-based clinical programs, especially programs staged in hospital EDs. Hospitals in our sample adopted some strategies at higher rates than other strategies. For example, a greater percentage of hospitals adopted primary care approaches, SUD treatment services, targeted risk education, and community coalition building than other strategies. In particular, the treatment of patients with OUD in the ED was among the least common strategies, despite evidence suggesting that early initiation of MAT is associated with lower opioid abuse–related morbidity and mortality and can be used as a bridge to formal treatment services.16,28 Our data indicate that in their community benefit work, hospitals are staying closer to their traditional clinical expertise and may prefer to support opioid treatment either in primary care or in formal treatment services rather than initiate treatment in the hospital. Although treatment referrals are important, evidence suggests that they are less effective than initiation of care in the hospital because they require patients to take additional steps to access MAT.29
That fewer hospitals are engaged in harm reduction is also important to note. Harm reduction programs that increase access to naloxone and clean syringes can prevent secondary infections and overdose deaths, and some evidence suggests that harm reduction initiatives are particularly effective when embedded in EDs.29 As such, hospitals may be missing opportunities to promote harm reduction practices or engage patients to initiate treatment.
Given that only a few institutional and policy factors were associated with the provision of OUD treatment services in the ED or with harm reduction programs, how to engage hospitals effectively is unclear. Most hospitals did not adopt either strategy, despite strong evidence to support their use. At the institutional level, we found that teaching hospitals and large hospitals were more likely than small nonteaching hospitals to invest in connecting patients with OUD to a primary care medical home, which is surprising given that these institutions have more resources, including a research infrastructure, than nonteaching hospitals and small hospitals to invest in treatment initiation. Teaching hospitals and large hospitals may also be better connected than small nonteaching hospitals to primary care providers and other organizations in their communities because of their size and local connections, which may increase the likelihood that they refer patients with OUD to outpatient services.
Our findings provide strong evidence that state policies on OUD are related to hospital efforts to promote harm reduction. In particular, the odds of hospitals adopting harm reduction strategies were higher in states that had funding in place for MAT, a form of harm reduction, than in states that did not. Given that harm reduction continues to be controversial in the United States,30 state intervention and support may be especially helpful in sharing evidence and assisting hospitals interested in engaging in these types of programs. Although there is less evidence in the literature to support the effectiveness of hospital involvement in offering targeted risk education or engaging in prescriber initiatives than in offering harm reduction services, we found important differences in these programs. Rural hospitals were more likely than nonrural hospitals to adopt targeted risk education initiatives, which may reflect a lack of health care providers in rural communities available to carry out clinical strategies. Other state policies, such as issuing prescriber guidelines, significantly decreased the odds of hospitals adopting prescriber initiatives, indicating that hospitals may not feel the need to duplicate the efforts undertaken at the state level. In general, these findings provide support for state policy changes as a promising mechanism to shape hospital behavior in harm reduction, but not initiation of treatment in the ED. More specific policy support may be needed to encourage hospitals to engage patients who are in the ED or admitted for OUD-related complications.
Limitations
Several limitations of our data warrant consideration. First, our primary data source was the publicly available community benefit documents that hospitals provide to describe their OUD-related outreach activities. Hospitals choose which information to report and, therefore, may be undertaking activities that are not described in their implementation strategies. Thus, our data may not include all programs that hospitals are initiating to address OUD in their communities. Second, despite the requirement to make CHNAs publicly available, disagreement exists about whether information on implementation strategies should be shared in the same way. Some hospitals did not make their implementation strategies available or respond to requests for these documents; as a result, we excluded them from our study. Hospitals that published these reports may have been more likely to address prioritized health needs, such as OUD, than hospitals that did not publish reports. Thus, we may have missed important activities that hospitals were undertaking or overestimated the percentage of hospitals that were addressing OUD. Third, our focus on community benefit investments was, by definition, limited to nonprofit hospitals, which are about 60% of the hospitals in the United States. For-profit and other hospitals may also be addressing OUD in their surrounding communities, but currently no mechanism exists to report these activities. As such, our study was limited by our inability to account for activities to address OUD among more than one-third of hospitals in the United States. Fourth, our data on state policies were limited by the available data, which indicated only whether a policy was in place in 2015. Given the scope of the US opioid epidemic, it is likely that states have adopted additional OUD-related policies since December 31, 2018.
Conclusion
OUD is a pressing public health and health care challenge that requires the collaboration of various institutions. Hospitals are well positioned to help patients initiate and connect with evidence-based treatments such as MAT. Our findings furnish evidence that some hospitals are already doing this work and that for harm reduction in particular, some organizational, community, and state policy factors increase the odds of hospital participation. As such, our results suggest that particular policy opportunities exist to engage nonprofit hospitals to adopt or expand initiatives to address OUD. Most important, our findings indicate that current state policies are not effective at encouraging hospitals to engage patients with OUD in the ED. Policies specific to OUD interventions may be necessary to encourage hospitals to invest in interventions in their facilities. Although hospitals are not likely equipped or staffed to take part in all OUD-related efforts, state policies may be helpful to effectively communicate expectations for hospitals to serve as partners in statewide efforts to address OUD. This type of coordination would likely improve the effectiveness of efforts to treat OUD and facilitate needed cross-sector collaboration.
Acknowledgments
The authors thank the Osteopathic Heritage Foundation and the Heritage College of Osteopathic Medicine at Ohio University for their support of a mentored research fellowship, which made this research project possible.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support with respect to the research, authorship, and/or publication of this article.
ORCID iDs
Berkeley Franz, PhD https://orcid.org/0000-0003-2091-1891
Cory E. Cronin, PhD https://orcid.org/0000-0001-6381-9695
References
- 1. Centers for Disease Control and Prevention . The drug overdose epidemic: behind the numbers. 2020. Accessed February 2, 2019. https://www.cdc.gov/drugoverdose/data/index.html
- 2. The Council of Economic Advisers . The underestimated cost of the opioid crisis. 2017. Accessed February 10, 2019. https://www.whitehouse.gov/sites/whitehouse.gov/files/images/The Underestimated Cost of the Opioid Crisis.pdf
- 3. Vivolo-Kantor AM., Seth P., Gladden RM. et al. Vital signs: trends in emergency department visits for suspected opioid overdoses—United States, July 2016–September 2017. MMWR Morb Mortal Wkly Rep. 2018;67(9):279-285. 10.15585/mmwr.mm6709e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barglow P. Commentary: the opioid overdose epidemic: evidence-based interventions. Am J Addict. 2018;27(8):605-607. 10.1111/ajad.12823 [DOI] [PubMed] [Google Scholar]
- 5. Korthuis PT., McCarty D., Weimer M. et al. Primary care–based models for the treatment of opioid use disorder: a scoping review. Ann Intern Med. 2017;166(4):268-278. 10.7326/M16-2149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nosyk B., Anglin MD., Brissette S. et al. A call for evidence-based medical treatment of opioid dependence in the United States and Canada. Health Aff (Millwood). 2013;32(8):1462-1469. 10.1377/hlthaff.2012.0846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rosenbaum S., Byrnes M., Rothenberg S., Gunsalus R. Improving community health through hospital community benefit spending: charting a path to reform. December 2016. Accessed July 24, 2020. http://hsrc.himmelfarb.gwu.edu/cgi/viewcontent.cgi?article=1825&context=sphhs_policy_facpubs
- 8. Kumar J., Greenblatt L. How North Carolina hospitals, health systems, and care providers are uniting to fight the opioid epidemic. North Carolina Med J. 2015;79(3):177-179. 10.18043/ncm.79.3.177 [DOI] [PubMed] [Google Scholar]
- 9. Dadwal V., Basu L., Weston CM. et al. How co-developed are community and academic partnerships? Prog Community Health Partnersh. 2017;11(4):387-395. 10.1353/cpr.2017.0046 [DOI] [PubMed] [Google Scholar]
- 10. Austrian Z., Alexander SE., Piazza MC., Clouse C. Mission, vision, and capacity of place-based safety net hospitals: leveraging the power of anchors to strengthen local economies and communities. J Community Pract. 2015;23(3-4):348-366. 10.1080/10705422.2015.1091416 [DOI] [Google Scholar]
- 11. Franz B., Skinner D., Wynn J., Kelleher K. Urban hospitals as anchor institutions: frameworks for medical sociology. Socius Sociol Res Dyn World. 2019;5. 10.1177/2378023118817981 [DOI] [Google Scholar]
- 12. Institute of Medicine . The Future of the Public’s Health in the 21st Century. National Academies Press; 2003. 10.17226/10548 [DOI] [Google Scholar]
- 13. Mays GP., Scutchfield FD. Improving public health system performance through multiorganizational partnerships. Prev Chronic Dis. 2010;7(6):A116. [PMC free article] [PubMed] [Google Scholar]
- 14. Cronin CE., Franz B., Skinner D., Haile ZT. Hospitals and substance use disorder services in the time of the opioid epidemic. Health Serv Res. 2019;54(2):399-406. 10.1111/1475-6773.13116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fanucchi L., Lofwall MR. Putting parity into practice—integrating opioid-use disorder treatment into the hospital setting. N Engl J Med. 2016;375(9):811-813. 10.1056/NEJMp1606157 [DOI] [PubMed] [Google Scholar]
- 16. D’Onofrio G., O’Connor PG., Pantalon MV. et al. Emergency department–initiated buprenorphine/naloxone treatment for opioid dependence. JAMA. 2015;313(16):1636-1644. 10.1001/jama.2015.3474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schranz AJ., Fleischauer A., Chu VH., Rosen DL. Trends in drug use–associated infective endocarditis and heart valve surgery, 2007 to 2017. Ann Intern Med. 2019;170(1):31. 10.7326/M18-2124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zibbell JE., Asher AK., Patel RC. et al. Increases in acute hepatitis C virus infection related to a growing opioid epidemic and associated injection drug use, United States, 2004 to 2014. Am J Public Health. 2018;108(2):175-181. 10.2105/AJPH.2017.304132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Priest KC., McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. 10.1097/ADM.0000000000000496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Weinstein ZM., Wakeman SE., Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. 10.1016/j.mcna.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Masson CL., Sorensen JL., Perlman DC. et al. Hospital- versus community-based syringe exchange: a randomized controlled trial. AIDS Educ Prev. 2007;19(2):97-110. 10.1521/aeap.2007.19.2.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dwyer K., Walley AY., Langlois BK. et al. Opioid education and nasal naloxone rescue kits in the emergency department. West J Emerg Med. 2015;16(3):381-384. 10.5811/westjem.2015.2.24909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Samuels EA., Dwyer K., Mello MJ., Baird J., Kellogg AR., Bernstein E. Emergency department–based opioid harm reduction: moving physicians from willing to doing. Acad Emerg Med. 2016;23(4):455-465. 10.1111/acem.12910 [DOI] [PubMed] [Google Scholar]
- 24. American Hospital Association . AHA data & insights. Access comprehensive hospital data with AHA Annual Survey database: AHA data. Accessed February 2, 2019. https://www.ahadata.com/aha-annual-survey-database
- 25. Centers for Disease Control and Prevention, National Center for Health Statistics . National Vital Statistics System. Accessed February 10, 2019. https://www.cdc.gov/nchs/nvss/index.htm
- 26. Wickramatilake S., Zur J., Mulvaney-Day N., Selmi E., Harwood H. How states are tackling the opioid crisis. Public Health Rep. 2017;132(2):171-179. 10.1177/0033354916688206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Health Resources & Services Administration . Data downloads: area health resources files. Accessed February 10, 2019. https://data.hrsa.gov/data/download
- 28. Busch SH., Fiellin DA., Chawarski MC. et al. Cost-effectiveness of emergency department–initiated treatment for opioid dependence. Addiction. 2017;112(11):2002-2010. 10.1111/add.13900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. D’Onofrio G., Chawarski MC., O’Connor PG. et al. Emergency department–initiated buprenorphine for opioid dependence with continuation in primary care: outcomes during and after intervention. J Gen Intern Med. 2017;32(6):660-666. 10.1007/s11606-017-3993-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McGinty EE., Barry CL., Stone EM. et al. Public support for safe consumption sites and syringe services programs to combat the opioid epidemic. Prev Med. 2018;111:73-77. 10.1016/j.ypmed.2018.02.026 [DOI] [PubMed] [Google Scholar]