Key Points
Question
Does an internet-based intervention for teachers improve children’s cardiorespiratory fitness when delivered across a large number of schools?
Findings
In this cluster randomized clinical trial of 22 schools including 1188 students, use of the internet-based intervention significantly improved children’s cardiorespiratory fitness at 12 months. Follow-up assessments at 24 months showed a sustained effect.
Meaning
Results of this randomized clinical trial suggest that the intervention has potential to be scaled to benefit children’s health at a population level.
Abstract
Importance
Cardiorespiratory fitness is an important marker of childhood health and low fitness levels are a risk factor for disease later in life. Levels of children's fitness have declined in recent decades. Whether school-based physical activity interventions can increase fitness at the population level remains unclear.
Objective
To evaluate the effect of an internet-based intervention on children’s cardiorespiratory fitness across a large number of schools.
Design, Setting, and Participants
In this cluster randomized clinical trial, 22 government-funded elementary schools (from 137 providing consent) including 1188 students stratified from grades 3 and 4 in New South Wales, Australia, were randomized. The other schools received the intervention but were not included in the analysis. Eleven schools received the internet-based intervention and 11 received the control intervention. Recruitment and baseline testing began in 2016 and ended in 2017. Research assistants, blinded to treatment allocation, completed follow-up outcome assessments at 12 and 24 months. Data were analyzed from July to August 2020.
Interventions
The internet-based intervention included standardized online learning for teachers and minimal in-person support from a project mentor (9-10 months).
Main Outcomes and Measures
Multistage 20-m shuttle run test for cardiorespiratory fitness.
Results
Of 1219 participants (49% girls; mean [SD] age, 8.85 [0.71] years) from 22 schools, 1188 students provided baseline primary outcome data. At 12 months, the number of 20-m shuttle runs increased by 3.32 laps (95% CI, 2.44-4.20 laps) in the intervention schools and 2.11 laps (95% CI, 1.38-2.85 laps) in the control schools (adjusted difference = 1.20 laps; 95% CI, 0.17-2.24 laps). By 24 months, the adjusted difference was 2.22 laps (95% CI, 0.89-3.55 laps). The cost per student was AUD33 (USD26).
Conclusions and Relevance
In this study, a school-based intervention improved children's cardiorespiratory fitness when delivered in a large number of schools. The low cost and sustained effect over 24 months of the intervention suggests that it may have potential to be scaled at the population level.
Trial Registration
http://anzctr.org.au Identifier: ACTRN12616000731493
This cluster randomized clinical trial assesses whether students from schools randomized to receive an internet-based physical activity intervention would show greater improvements in cardiorespiratory fitness 12 months after baseline compared with students from control schools.
Introduction
Levels of children's cardiorespiratory fitness decreased globally in recent decades.1 Cardiorespiratory fitness is an important marker of childhood health and low levels of cardiovascular fitness are a risk factor for disease later in life.2,3 Meta-analyses of efficacy studies show that school-based physical activity interventions can improve children’s cardiorespiratory fitness.4,5,6 However, when potentially scalable versions of school-based interventions have been tested in randomized clinical trials (RCTs), the interventions have not improved children’s cardiorespiratory fitness.7,8 There is, therefore, limited evidence that school-based interventions can benefit children’s cardiorespiratory fitness at the population level.9
An intervention that may have the possibility of scaling was the elementary school–based Supporting Children’s Outcomes Using Rewards, Exercise, and Skills (SCORES) program.10 A cluster RCT efficacy study showed that SCORES significantly improved children’s cardiorespiratory fitness. The SCORES intervention, however, relied on university-based researchers to deliver training to teachers, which limited scalability. Drawing on principles from the Consolidated Framework for Implementation Research11 (eFigure 1 in Supplement 1), we adapted SCORES so that standardized intervention content could be delivered via an online platform with minimal in-person support from experienced teachers employed by the project and no direct contact between schools and the research team. The adapted intervention is known as Internet-Based Professional Learning to Help Teachers Promote Activity in Youth (iPLAY).
We tested the hypothesis that students from schools randomized to the iPLAY intervention would show greater improvements in cardiorespiratory fitness 12 months after baseline (primary end point) compared with students from control schools. Our secondary hypotheses were that positive changes in cardiorespiratory fitness would be maintained at 24 months and that iPLAY would have positive effects on secondary outcomes that are potential determinants of cardiorespiratory fitness improvement (eg, physical activity, fundamental movement skills12) and potential outcomes of this primary outcome (eg, academic achievement13), and iPLAY costs would compare favorably with costs of other school-based interventions.
We also explored potential mediating pathways that could explain intervention effects (eg, improvements in fundamental movement skills explained the effects of the SCORES intervention on physical activity and cardiorespiratory fitness12). In addition, to investigate if iPLAY was equally effective for all subpopulations, we tested if demographic (eg, age, sex) or baseline characteristics (cardiorespiratory fitness, physical activity, or fundamental movement skill competence) moderated the effects on cardiorespiratory fitness.14
Methods
Trial Design and Participants
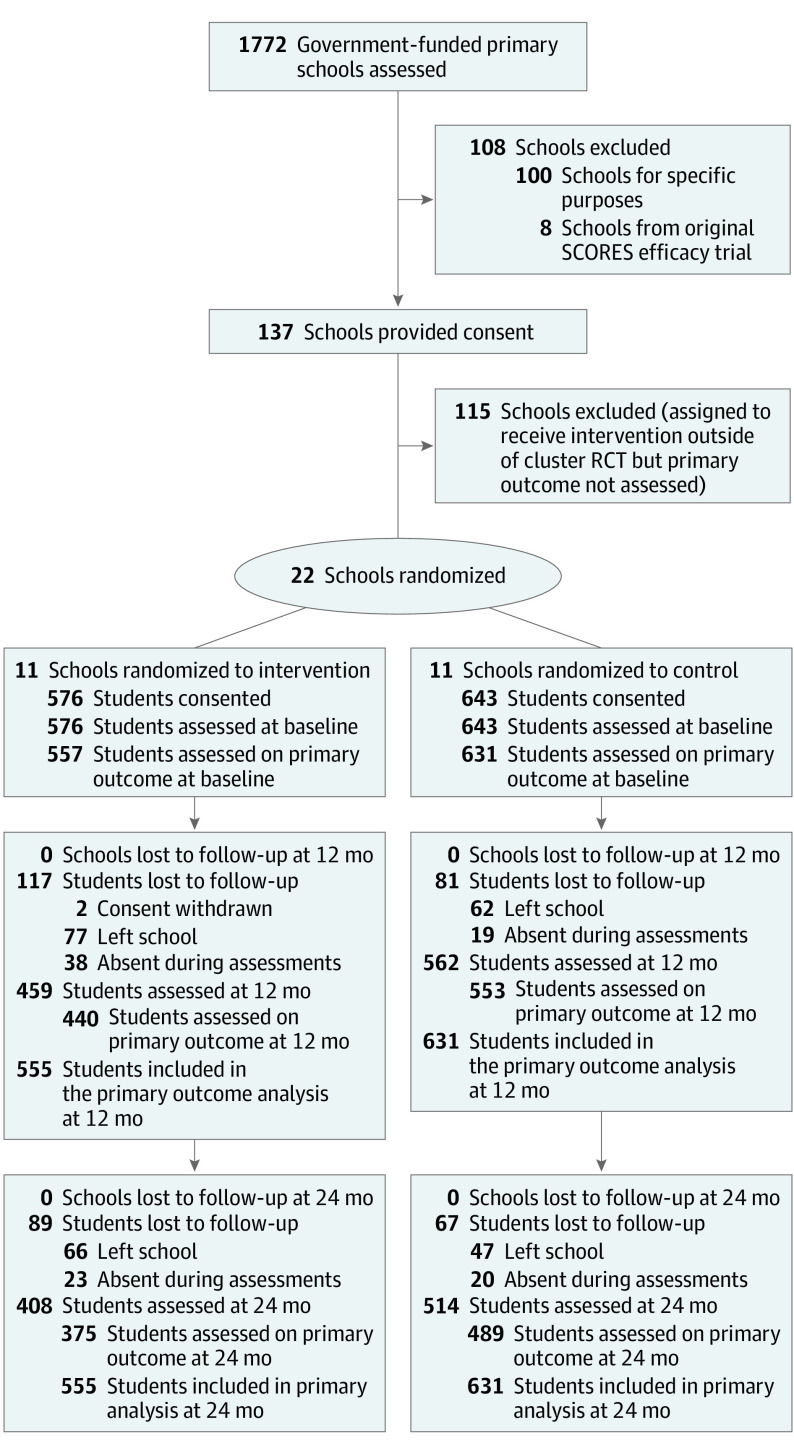
From 137 schools providing consent, we assigned 22 to a cluster RCT (Figure). We offered iPLAY to the other 115 schools (108 accepted) but did not assess the primary outcome in those schools. We did, however, assess teachers’ adoption and implementation fidelity data in all schools. In the cluster RCT, we conducted baseline assessments and then allocated schools (1:1) to the intervention or an attention control condition. We completed follow-up assessments at 12 months (postintervention) and 24 months. The protocol for this trial has been published,15 and the format used for grant application is available in Supplement 2. The New South Wales Department of Education and the university review boards provided ethical approval.
Figure. CONSORT Flow Diagram.
RCT indicates randomized clinical trials; SCORES, Supporting Children’s Outcomes Using Rewards, Exercise, and Skills.
Government-funded elementary schools (kindergarten–grade 6) in New South Wales, Australia, were eligible to participate. Schools focused on students with special needs and schools from the original SCORES efficacy study10 were not eligible. To recruit schools, we presented at principals’ meetings, sent emails to schools, and posted information on social media.
We invited all teachers in participating schools to join the study with written consent. We invited students in grades 3 and 4 (via written parental consent) to participate in outcome assessments. We collected data at the schools in which the students were enrolled.
Interventions
Based on the Centers for Disease Control and Prevention’s Comprehensive School Physical Activity Program framework,16 iPLAY included 6 components to promote physical activity participation, enhance student motivation toward physical activity, and develop fundamental movement skill competence (eFigure 2 in Supplement 1). Three components focused on curricular strategies: (1) quality physical education (delivered according to the SAAFE principles17), (2) classroom energizers (ie, brief physical activity breaks), and (3) active homework in which students completed academic tasks while being physically active. Three further components targeted noncurricular strategies: (4) active playgrounds during recess and lunch breaks (eg, providing physical activity equipment and implementing playground policies to encourage physical activity, such as “no hat, play in the shade” rather than “no hat, no play”), (5) parent engagement via newsletters (eg, ideas for active gifts at Christmas) and active school fundraising events, and (6) community physical activity links (eg, helping schools access funding for after-school physical activity programs delivered by external agencies).
An iPLAY mentor (ie, an experienced physical education teacher trained by the research team) facilitated a 2-hour group workshop for all teachers at each school using standardized multimedia content hosted on the iPLAY online platform. Mentors also visited schools to provide teachers with 1 hour of individualized implementation mentoring. The online platform provided teachers with 4 hours of additional learning modules to complete independently (eFigure 3 in Supplement 1).
Principals in each school identified up to 3 teachers as iPLAY leaders who implemented the noncurricular intervention components. Leaders completed 4 additional online modules to learn how to implement the noncurricular components. Leaders in each school then met with their school’s mentor to set implementation goals. Subsequently, leaders met with mentors once per term to review progress, set new goals, and discuss how to support teachers to implement the curricular components.
The online platform not only delivered content to mentors, leaders, and teachers but also provided adoption and implementation feedback. Mentors could oversee leaders’ and teachers’ adoption and implementation and provide support (eg, answering questions via telephone). iPLAY leaders could also monitor their teachers’ online learning module completion and offer assistance (eg, solving implementation barriers).
Mentors completed all in-person delivery within 12 months. Teachers and leaders could, however, continue to access the website after this period to complete online training or download resources.
For schools allocated to the attention control arm, we provided professional learning in curriculum unrelated to physical activity (such as science).
Outcomes
Trained research assistants assessed the primary outcome, students’ cardiorespiratory fitness, by recording laps completed in the 20-m multistage fitness test.18 This test has demonstrated strong criterion-related validity in this population and is a widely used field-based measure.2
The published protocol15 includes secondary outcome details. Briefly, we used wrist-worn accelerometers19 to measure students’ moderate to vigorous physical activity across a week: (1) within school time (per school’s schedule), (2) during lunch and recess (per schedule), (3) after school, (4) on weekends, and (5) overall. Students self-reported their well-being20 and experiences during physical education lessons.21,22,23,24,25,26 We linked student data with their standardized academic test scores27 and measured height and weight to calculate body mass index.28 Within each school, we randomly selected 1 class at baseline from which to measure students’ fundamental movement skills29 and cognitive function.30
Sample Size
Based on the SCORES efficacy trial,10 we expected intraclass correlations of 0.01 (school) and 0.09 (class), with d = 0.35 for the between-arm difference. Our power analysis31 estimated that a sample size of 1080 students from 60 classes in 20 schools would provide power of 0.91 to detect this effect size.
Recruitment, Assignment, Randomization, and Blinding
We recruited schools using procedures described in the protocol.15 We assigned 22 of the 137 schools to the cluster RCT using a blocked randomization process designed to ensure that schools in the trial were broadly representative of government schools in New South Wales and allocated to trial arms such that most school-level covariates were balanced.
We planned to assign 20 schools from 3 cohorts to the cluster RCT; however, our recruitment in the first 2 cohorts oversampled students from low socioeconomic (SES) areas–69.9% of students from low SES schools. Thus, we recruited an additional pair of high SES schools in the final cohort.
Following baseline assessments, an independent statistician randomized schools using an algorithm in the R environment, version 3 (R Foundation for Statistical Computing).
Blinded research assistants collected all student-level outcomes in the cluster RCT. We evaluated the extent to which this blinding was successful (eTable 1 in Supplement 1). Students and teachers were not blinded to allocation.
Statistical Analysis
Statisticians, blinded to schools’ allocation, tested for between-arm differences in changes in student outcomes using mixed-effects models with random effects for student, teacher, and school to account for clustering. The primary outcome was a count variable (number of 20-m shuttle run test laps) and followed a Poisson distribution; thus, we used a Poisson link function. For secondary outcomes we ran mixed-effects models with a gaussian link function. We ran all models in R version 3 using Markov Chain Monte Carlo estimation.32 We analyzed according to intention-to-treat principles. Results were considered not statistically significant if 95% CIs contained 0, and statistical tests were 2-tailed. Data were analyzed from July to August 2020.
We explored preregistered demographic moderators of intervention effects,15 including self-reported age, sex, ethnicity, weight status, and family SES (ie, a principal component of the variables wealth status and books in the home). Preregistered moderators also included baseline levels of cardiorespiratory fitness, physical activity, and fundamental movement skill competence.
In our per-protocol analyses we investigated the moderating influence of iPLAY leaders’ and teachers’ intervention adoption and implementation fidelity on the primary outcome (students’ cardiorespiratory fitness). Adoption focused on the proportion of intervention training components teachers and leaders completed (eg, online learning modules). Implementation fidelity measures focused on the proportion of strategies utilized (eTables 2-4 in Supplement 1).
To examine potential mediating processes, we used mixed-model analyses via a causal mediation approach.33 This analysis seeks to identify mechanisms by which the intervention may influence the outcome.
We assessed the cost-effectiveness of the iPLAY intervention using prospectively collected data. We determined cost resources related to iPLAY intervention delivery, including staff salaries, equipment,34 and consumables. We valued costs in 2018 Australian dollars (with US dollar equivalents). We calculated the incremental cost-effectiveness ratio as the ratio of the difference in cost and the difference in the primary outcome per student.
Results
We recruited and collected baseline data for the first cohort from July 22 to August 25, 2016, the second cohort from May 15 to June 22, 2017, and the third cohort from November 27 to December 7, 2017. From the 22 RCT schools, we recruited 1219 students (mean [SD] age, 8.85 [0.71] years; 49.38% girls) into the trial (70.0% of enrolled grade 3 and 4 students). Parents of 2 students withdrew their consent without providing reasons for their decisions. Of the 1217 participants, 1188 students completed the primary outcome assessment. Table 1 presents baseline characteristics.
Table 1. Baseline Characteristics.
| Variable | Total No. (No. in intervention) | Control, mean (SD) | Intervention, mean (SD) | Total, mean (SD) |
|---|---|---|---|---|
| Student-level variables | ||||
| Cardiorespiratory fitness (20-m shuttle laps) | 1188 (557) | 25.83 (14.95) | 22.84 (13.43) | 24.43 (14.33) |
| Girls, % | 1209 (569) | 49.06 (NA) | 49.74 (NA) | 49.38 (NA) |
| Age, y | 1190 (554) | 8.89 (0.70) | 8.81 (0.73) | 8.85 (0.71) |
| BMI | 1186 (552) | 18.14 (3.09) | 18.23 (3.58) | 18.18 (3.32) |
| BMI-z | 1174 (547) | 0.44 (1.02) | 0.42 (1.11) | 0.43 (1.06) |
| Obese/overweight status, % | 1174 (547) | 27.11 (NA) | 28.88 (NA) | 27.94 (NA) |
| Immigrant status, % | 1208 (568) | 15.62 (NA) | 26.58 (NA) | 20.78 (NA) |
| Indigenous (Aboriginal/Torres Strait Islander), % | 1206 (569) | 9.06 (NA) | 8.61 (NA) | 8.85 (NA) |
| Wealth statusa | 1196 (557) | 2.45 (0.84) | 2.45 (0.84) | 2.45 (0.84) |
| Books in homeb | 1196 (557) | 3.05 (1.14) | 2.99 (1.23) | 3.02 (1.18) |
| School-level variables | ||||
| Index of Community Socio-Educational Advantage score | 22 (11) | 986.3 (58.3) | 1006 (56) | 996.3 (56.7) |
| School size (students in kindergarten-grade 6) | 22 (11) | 294.18 (266.9) | 253.63 (190.49) | 273.91 (227.23) |
| Previous participation in the Live Life Well at School Program, %c | 22 (11) | 90.91 (NA) | 100 (NA) | 95.45 (NA) |
| NAPLAN Numeracy school mean score | 22 (11) | 445.95 (54.48) | 436.91 (49.23) | 441.42 (50.5) |
| NAPLAN Literacy school mean score | 22 (11) | 452.73 (54.62) | 447.86 (44.94) | 450.3 (49.5) |
| Urban location, % | 22 (11) | 63.64 (NA) | 72.73 (NA) | 68.18 (NA) |
| Length of school day, min | 22 (11) | 361.31 (2.24) | 358.2 (4.61) | 359.75 (3.88) |
| Time allocated to recess/lunch breaks per day, min | 22 (11) | 73.70 (5.58) | 68.72 (8.19) | 71.21 (7.21) |
| Schools with a dedicated physical education teacher, % | 20 (10) | 30.00 (NA) | 0 (NA) | 15.00 (NA) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); BMI-z, BMI z score; NAPLAN, National Assessment Program–Literacy and Numeracy; NAPLAN Literacy, combination of reading, writing, spelling and grammar scores.
Wealth status measured on scale from 1 to 5, with 1 indicating very wealthy and 5 indicating not at all wealthy.
Books in the home measured on scale from 1 to 5, with 1 indicating none or very few (0-10) books and to 5 indicating enough to fill 3 or more bookcases (more than 200 books).
Live Life Well at School was a statewide physical activity and nutrition program delivered in New South Wales from 2008 to 2015.
Our intention-to-treat analyses found that, compared with controls, students in the iPLAY intervention schools had greater increases from baseline in cardiorespiratory fitness at 12 and 24 months (Table 2). The mean (SD) number of laps in the control group at baseline on the 20-m shuttle test was 25.83 (14.95) laps, and for the intervention group was 22.84 (13.43) laps. The mean (SD) number of laps in the control group at 12 months on the 20-m shuttle test was 27.87 (16.02), and for the intervention group was 25.54 (15.27) laps. The mean adjusted difference at 12 months was 1.20 laps (95% CI, 0.17-2.24) on the 20-m shuttle test. The mean (SD) number of laps in the control group at 24 months on the 20-m shuttle test was 30.11 (17.21) laps, and for the intervention group was 30.03 (17.47) laps. At 24 months, the mean adjusted difference was 2.22 laps (95% CI, 0.89-3.55). Blinding of research assistants to schools’ allocation was largely successful. In 4 instances, research assistants became unblinded (eTable 1 in Supplement 1).
Table 2. Analysis of Cardiorespiratory Fitness Measured by Laps on Multistage 20-m Shuttle Run Test.
| Model | Follow-up, mo | Total No. (No. in intervention) | No. of laps (95% CI) | ||
|---|---|---|---|---|---|
| Change from baseline, control | Change from baseline, intervention | Adjusted difference between intervention and control in 20-m shuttle test laps | |||
| Main analysisa: controlling for schools' remoteness and Index of Community Socio-Educational Advantage score | 12 | 993 (440) | 2.11 (1.38-2.85) | 3.32 (2.44-4.2) | 1.20 (0.17-2.24) |
| 24 | 864 (375) | 4.42 (3.41-5.43) | 6.64 (5.3-7.98) | 2.22 (0.89-3.55) | |
| Sensitivity analysis 1b: model without controlling for schools' remoteness or Index of Community Socio-Educational Advantage score | 12 | 993 (440) | 1.74 (1.17-2.31) | 2.75 (2.1-3.4) | 1.01 (0.14-1.88) |
| 24 | 864 (375) | 3.63 (2.92-4.34) | 5.5 (4.61-6.4) | 1.87 (0.73-3.02) | |
| Sensitivity analysis 2a: model controlling for schools' urban status and Index of Community Socio-Educational Advantage score and imputing missing data | 12 | 1021 (459) | 2.01 (1.27-2.76) | 3.36 (2.46-4.26) | 1.35 (0.27-2.43) |
| 24 | 970 (408) | 4.56 (3.53-5.59) | 7.22 (5.8-8.65) | 2.66 (1.23-4.08) | |
Main analysis = mixed effect model with a Poisson link function. ICC student = 0.86, ICC teacher = 0.06, ICC School = 0.04.
Sensitivity analyses 2 a and b included imputation for students who were absent during a primary outcome assessment, but provided other assessment data at that time point. The median absolute deviation in shuttle runs for the control group was 8 laps (at baseline). The intervention effect size was equivalent to 15% of the median absolute deviation at 12 months and 28% of the median absolute deviation at 24 months.
Table 3 provides full moderator results. eFigure 4 in Supplement 1 depicts significant effects. At 12 and 24 months, boys showed greater benefit from the intervention compared with girls (effect estimate for boys at 12 months: 2.12 [90% CI, 0.95-3.42] vs effect estimate for girls at 12 months: 0.02 [90% CI, −1.11 to 1.14]). At 24 months, students from lower SES families, younger students, and students with better fundamental movement skills at baseline received more benefit than students from families with higher wealth status, older students, and students with worse movement skills.
Table 3. Moderator Effects on Cardiorespiratory Fitness Measured by Laps on Multistage 20-m Shuttle Run Testa.
| Moderator | Follow-up, mo | Effect estimate (90% CI) |
|---|---|---|
| Baseline cardiorespiratory fitness | 12 | 0.05 (−0.02 to 0.11) |
| 24 | −0.01 (−0.07 to 0.05) | |
| Socioeconomic status | 12 | 0.01 (−0.03 to 0.04) |
| 24 | −0.06 (−0.10 to −0.03) | |
| Age | 12 | −0.05 (−0.10 to 0.00) |
| 24 | −0.06 (−0.11 to −0.01) | |
| Immigrant status | 12 | 0.05 (−0.08 to 0.17) |
| 24 | 0.11 (−0.02 to 0.24) | |
| Indigenous status | 12 | −0.02 (−0.12 to 0.07) |
| 24 | 0.08 (−0.02 to 0.17) | |
| Sex | 12 | −0.08 (−0.14 to −0.01) |
| 24 | −0.15 (−0.22 to −0.08) | |
| Obese/overweight status | 12 | −0.01 (−0.10 to 0.07) |
| 24 | −0.09 (−0.18 to 0.00) | |
| MVPA | 12 | 0.01 (−0.03 to 0.04) |
| 24 | 0.01 (−0.03 to 0.05) | |
| Fundamental movement skills | 12 | 0.01 (−0.01 to 0.03) |
| 24 | 0.04 (0.02 to 0.06) | |
| Boys | 12 | 2.12 (0.95 to 3.42) |
| Girls | 12 | 0.02 (−1.11 to 1.14) |
| Boys | 24 | 4.29 (2.78 to 5.89) |
| Girls | 24 | −0.28 (−1.66 to 1.10) |
| Age 8 y | 24 | 3.78 (2.00 to 5.54) |
| Age 10 y | 24 | 0.15 (−1.82 to 2.10) |
| Low socioeconomic status | 24 | 4.44 (2.89-6.18) |
| High socioeconomic status | 24 | −0.10 (−1.60 to 1.45) |
| Low fundamental movement skills | 24 | −2.79 (−5.22 to −0.471) |
| High fundamental movement skills | 24 | 4.21 (1.76 to 6.71) |
Abbreviation: MVPA, moderate to vigorous physical activity.
As specified in our preregistered protocol, we explored moderation effects with significance set at P < .10. As a result, 90% CIs are provided. When significant moderator effects were found, estimates of effects at specific levels of the moderator are displayed. Low socioeconomic status = mean −1 SD. High socioeconomic status mean +1 SD. Low fundamental movement skills = first quartile. High fundamental movement skills = third quartile.
eTable 3 and eTable 4 in Supplement 1 show the proportion of teachers and leaders in the 11 RCT schools allocated to the iPLAY intervention who adopted and/or implemented each aspect of the intervention at 12 and 24 months. Briefly, adoption and implementation fidelity across the cluster RCT intervention schools and 108 non-RCT schools were similar. For example, in the RCT, 63% of teachers completed all 8 online learning modules by 24 months. In the non-RCT schools, the completion rate for these modules was 62%.
As shown in eTable 5 in Supplement 1, per-protocol analysis in the RCT suggested that students whose teachers and leaders adopted and implemented iPLAY per protocol likely received greater cardiorespiratory fitness benefit at 12 and 24 months than students whose schools did not adopt the intervention. For example, for teacher adoption at 12 months, the adjusted difference in 20-m shuttle test laps between treated vs nontreated students was 2.16 laps (95% CI, −2.14 to 6.46 laps). For leader adoption at 12 months, the adjusted difference in 20-m shuttle test laps between treated vs nontreated students was 0.88 laps (95% CI, −0.86 to 2.62 laps). Adjusted differences in the per-protocol analyses were generally larger than the main intention-to-treat analyses; however, due to the smaller effective sample sizes, the per-protocol effects were not reliably different from 0.
As shown in eTables 6 through 9 in Supplement 1, secondary outcomes analyses showed significant intervention effects on physical activity (by accelerometry) during school lunch and recess breaks at 12 and 24 months (ie, compared with intervention schools, control groups showed greater decreases in physical activity over time35). However, the intervention did not produce significant effects on physical activity at other times (during school day, after school, or weekend) or overall. There were also no significant effects on self-reported physical activity, well-being, academic achievement, or BMI. Within physical education lessons, iPLAY significantly enhanced students’ perceived support from their teachers at 24 months, but did not affect other outcomes. Data from the subsample of students who completed fundamental movement skill and cognitive function assessments showed no intervention effects on these outcomes.
Students’ moderate to vigorous physical activity during lunch/recess partially mediated the effect of the intervention on students’ cardiorespiratory fitness. At 12 months, the log odds ratio for the intervention effect was 0.06 (95% CI, 0.02-0.09) and the indirect effect was 0.02 (95% CI, 0.01-0.04). At 24 months, the log odds ratio for the intervention effect was 0.10 (95% CI, 0.06-0.13] and the indirect effect was 0.02 (95% CI, 0.01-0.03).
The cost of delivering the iPLAY intervention across 11 schools in the cluster RCT was calculated as A $88 713 (US $69 515), with an average cost of A $33 per student (US $26/student) across the 2702 from all grades in the schools. At 12 months, the incremental cost-effectiveness ratio was A $27 (US $21) for each additional lap achieved. At 24 months, this ratio was A $15 (US $12/lap) for each additional lap achieved. Bootstrapping sensitivity analyses produced similar results (eFigure 5 in Supplement 1).
No participants reported any harm. Similarly, no teachers or principals reported any harm in this trial.
Discussion
In this cluster RCT, we found that an internet-based professional learning intervention for elementary school teachers improve students’ cardiorespiratory fitness at 12 months. Effects continued to increase even after withdrawal of implementation support from mentors, with 24-month benefits nearly double the 12-month effect. Our cluster RCT appears to be the first to show that a school-based intervention can improve children’s cardiorespiratory fitness when delivered across a large number of schools (ie, 11 schools from RCT and 108 other schools).
The iPLAY intervention relies primarily on an internet-based delivery model with minimal in-person support from experienced teachers (known as iPLAY mentors). Delivery via the internet allowed us to standardize the learning content, which likely limited deviations from planned intervention protocol (known as program drift) and reductions in intervention benefits (known as voltage drop).36 Internet-based delivery also allowed teachers to learn according to a flexible schedule, which was important given their busy schedules. Internet-based delivery also allowed teachers to learn in a distributed fashion over 9 to 10 months rather than experiencing a small number of face-to-face workshops (eg, 1-1.5 days of workshops per year8).
Cardiorespiratory fitness levels are an important indicator of health in youth and a low fitness levels are associated with disease later in life.2,3 From 1981 to 2014, children’s cardiorespiratory fitness levels have decreased in many countries. In Australia, for example, children’s cardiorespiratory fitness decreased by an average of 0.17 mL/kg/min per year during this period.1 Converting our trial participants’ 20-m shuttle laps into estimated peak oxygen consumption37 showed that iPLAY improved cardiorespiratory fitness by 0.45 mL/kg/min (95% CI, 0.06-0.84 mL/kg/min) at 24 months. Thus, iPLAY could be seen to reverse approximately 3 years of the decrease observed in Australian population levels of children’s fitness in recent decades. If an intervention such as iPLAY can be implemented across the population, the effect on cardiorespiratory fitness and corresponding health benefits could be notable for society.38
With regard to cost, the iPLAY cost (A $33/student [US $26/student]) falls well below the values reported for other school-based physical activity programs (eg, Child and Adolescent Trial for Cardiovascular Health intervention39 was US $104/student [2004], equal to A $198/student [2018]). The UK Education Endowment Foundation40 considers interventions with a cost per student below £80 (US $107) per year to be very low cost.
Despite our significant overall intervention effects, iPLAY was not universally successful. For example, intervention effects on device-measured physical activity were limited to recess and lunch time breaks. This pattern of significant cardiorespiratory fitness effects alongside limited device-measured physical activity effects is, however, consistent with meta-analyses of efficacy studies.4,6,41 It is possible that iPLAY (and other school-based interventions that improved cardiorespiratory fitness but not device-measured physical activity) actually did increase students’ overall physical activity; however, the effects may not have been detectable because accelerometers did not adequately capture some physical activities. Possible sources of error include participation in organized sports (during which students often remove accelerometers), such as those promoted in the community physical activity component of the iPLAY intervention.
Relative to the controls, iPLAY increased intervention students’ cardiorespiratory fitness over the study period. However, notable differences occurred in CRF between groups at baseline. Intervention students completed nearly 3 laps fewer than control students, suggesting that iPLAY narrowed this preexisting gap. Further caution is warranted because our moderator analyses showed intervention effects were not equivalent for all students. A recent meta-analysis of school-based efficacy trials reported similar findings, with smaller intervention effects for girls and older children than for boys and younger children.6 As a result, we suggest that targeted online teacher professional learning may need to be developed and tested to ensure that all students receive benefits from this type of intervention. Further research is also warranted to assess the extent to which our results may be generalizable to populations in primary schools outside New South Wales, Australia.
Strengths and Limitations
Study strengths include stratified sampling procedures that helped ensure the results would be generalizable to the population. We recruited a high proportion of enrolled students (70%) compared with other high-quality school-based trials (eg, 60%42). We retained 84% of the baseline sample on our primary outcome assessment at 12 months, which is comparable to other high-quality school-based trials (eg, 82%-89% at 9-30 months42,43). In addition, we included a longer follow-up period (24 months) than many other school-based interventions targeting cardiorespiratory fitness (eg, mean = 13 months in a 2018 meta-analysis4).
This study also had limitations. Our trial did not have sufficient sample size at the cluster level to examine the influence of between-school moderators (eg, school size and location) on intervention effects. We were similarly underpowered to detect effects on some secondary outcomes (eg, fundamental movement skills).
Conclusions
This cluster randomized clinical trials appears to be the first to show that a school-based intervention can help increase children’s cardiorespiratory fitness levels when delivered across a large number of schools. Our internet-based intervention for teachers improved children’s cardiorespiratory fitness at 12 months. The intervention also built capacity in schools such that these benefits continued to increase for at least another year after we withdrew in-person support. This evidence, alongside the intervention’s low cost, suggests that iPLAY has potential to be scaled to benefit children’s health at a population level.
eFigure 1. Consolidated Framework for Implementation Research
eFigure 2. iPLAY Intervention Components
eFigure 3. Online Platform Screenshots
eFigure 4. Summary of Significant Moderator Effects
eFigure 5. Sensitivity Analysis for Incremental Cost-Effectiveness Ratios
eTable 1. iPLAY Data Collector Blinding Evaluation
eTable 2. iPLAY Intervention Components and Implementation Measures
eTable 3. Intervention Adoption Rates
eTable 4. Intervention Implementation Rates
eTable 5. Per Protocol Analyses of Intervention Effects on Primary Outcome
eTable 6. Main Sample Secondary Outcomes Baseline Values
eTable 7. Main Sample Secondary Outcome Analyses
eTable 8. Sub-sample Variables Baseline Values
eTable 9. Sub-sample Variables Outcome Analyses
Trial Protocol
Data Sharing Statement
References
- 1.Tomkinson GR, Lang JJ, Tremblay MS. Temporal trends in the cardiorespiratory fitness of children and adolescents representing 19 high-income and upper middle-income countries between 1981 and 2014. Br J Sports Med. 2019;53(8):478-486. doi: 10.1136/bjsports-2017-097982 [DOI] [PubMed] [Google Scholar]
- 2.Raghuveer G, Hartz J, Lubans DR, et al. ; American Heart Association Young Hearts Athero, Hypertension and Obesity in the Young Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Young . Cardiorespiratory fitness in youth: an important marker of health: a scientific statement from the American Heart Association. Circulation. 2020;142(7):e101-e118. doi: 10.1161/CIR.0000000000000866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.García-Hermoso A, Ramírez-Vélez R, García-Alonso Y, Alonso-Martínez AM, Izquierdo M. Association of cardiorespiratory fitness levels during youth with health risk later in life: a systematic review and meta-analysis. JAMA Pediatr. 2020;174(10):952-960. doi: 10.1001/jamapediatrics.2020.2400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pozuelo-Carrascosa DP, García-Hermoso A, Álvarez-Bueno C, Sánchez-López M, Martinez-Vizcaino V. Effectiveness of school-based physical activity programmes on cardiorespiratory fitness in children: a meta-analysis of randomised controlled trials. Br J Sports Med. 2018;52(19):1234-1240. doi: 10.1136/bjsports-2017-097600 [DOI] [PubMed] [Google Scholar]
- 5.García-Hermoso A, Alonso-Martínez AM, Ramírez-Vélez R, Pérez-Sousa MÁ, Ramírez-Campillo R, Izquierdo M. Association of physical education with improvement of health-related physical fitness outcomes and fundamental motor skills among youths: a systematic review and meta-analysis. JAMA Pediatr. 2020;174(6):e200223. doi: 10.1001/jamapediatrics.2020.0223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hartwig TB, Sanders T, Vasconcellos D, et al. School-based interventions modestly increase physical activity and cardiorespiratory fitness but are least effective for youth who need them most: an individual participant pooled analysis of 20 controlled trials. Br J Sports Med. 2021;bjsports-2020-102740. doi: 10.1136/bjsports-2020-102740 [DOI] [PubMed] [Google Scholar]
- 7.Stavnsbo M, Aadland E, Anderssen SA, et al. Effects of the Active Smarter Kids (ASK) physical activity intervention on cardiometabolic risk factors in children: A cluster-randomized controlled trial. Prev Med. 2020;130:105868. doi: 10.1016/j.ypmed.2019.105868 [DOI] [PubMed] [Google Scholar]
- 8.Luepker RV, Perry CL, McKinlay SM, et al. Outcomes of a field trial to improve children’s dietary patterns and physical activity: The Child and Adolescent Trial for Cardiovascular Health: CATCH collaborative group. JAMA. 1996;275(10):768-776. doi: 10.1001/jama.1996.03530340032026 [DOI] [PubMed] [Google Scholar]
- 9.Reis RS, Salvo D, Ogilvie D, Lambert EV, Goenka S, Brownson RC; Lancet Physical Activity Series 2 Executive Committee . Scaling up physical activity interventions worldwide: stepping up to larger and smarter approaches to get people moving. Lancet. 2016;388(10051):1337-1348. doi: 10.1016/S0140-6736(16)30728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen KE, Morgan PJ, Plotnikoff RC, Callister R, Lubans DR. Physical activity and skills intervention: SCORES cluster randomized controlled trial. Med Sci Sports Exerc. 2015;47(4):765-774. doi: 10.1249/MSS.0000000000000452 [DOI] [PubMed] [Google Scholar]
- 11.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen KE, Morgan PJ, Plotnikoff RC, Barnett LM, Lubans DR. Improvements in fundamental movement skill competency mediate the effect of the SCORES intervention on physical activity and cardiorespiratory fitness in children. J Sports Sci. 2015;33(18):1908-1918. doi: 10.1080/02640414.2015.1017734 [DOI] [PubMed] [Google Scholar]
- 13.Álvarez-Bueno C, Hillman CH, Cavero-Redondo I, Sánchez-López M, Pozuelo-Carrascosa DP, Martínez-Vizcaíno V. Aerobic fitness and academic achievement: A systematic review and meta-analysis. J Sports Sci. 2020;38(5):582-589. doi: 10.1080/02640414.2020.1720496 [DOI] [PubMed] [Google Scholar]
- 14.Yildirim M, van Stralen MM, Chinapaw MJ, et al. ; Energy-Consortium . For whom and under what circumstances do school-based energy balance behavior interventions work? Systematic review on moderators. Int J Pediatr Obes. 2011;6(2-2):e46-e57. doi: 10.3109/17477166.2011.566440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lonsdale C, Sanders T, Cohen KE, et al. Scaling-up an efficacious school-based physical activity intervention: Study protocol for the ‘Internet-based Professional Learning to help teachers support Activity in Youth’ (iPLAY) cluster randomized controlled trial and scale-up implementation evaluation. BMC Public Health. 2016;16(1):873. doi: 10.1186/s12889-016-3243-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC) . School health guidelines to promote healthy eating and physical activity. MMWR Recomm Rep. 2011;60(RR-5):1-76. [PubMed] [Google Scholar]
- 17.Lubans DR, Lonsdale C, Cohen K, et al. Framework for the design and delivery of organized physical activity sessions for children and adolescents: rationale and description of the ‘SAAFE’ teaching principles. Int J Behav Nutr Phys Act. 2017;14(1):24. doi: 10.1186/s12966-017-0479-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Cooper Institute . Fitnessgram and Activitygram Test Administration Manual-Updated 4th Edition. Human Kinetics; 2010. [Google Scholar]
- 19.Hildebrand M, VAN Hees VT, Hansen BH, Ekelund U. Age group comparability of raw accelerometer output from wrist- and hip-worn monitors. Med Sci Sports Exerc. 2014;46(9):1816-1824. doi: 10.1249/MSS.0000000000000289 [DOI] [PubMed] [Google Scholar]
- 20.Roberts C, Freeman J, Samdal O, et al. ; International HBSC Study Group . The Health Behaviour in School-aged Children (HBSC) study: methodological developments and current tensions. Int J Public Health. 2009;54(S2)(suppl 2):140-150. doi: 10.1007/s00038-009-5405-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vlachopoulos SP, Katartzi ES, Kontou MG. Fitting multidimensional amotivation into the self-determination theory nomological network: application in school physical education. Meas Phys Educ Exerc Sci. 2013;17(1):40-61. doi: 10.1080/1091367X.2013.741366 [DOI] [Google Scholar]
- 22.Ahn I, Patrick H, Chiu MM, Levesque-Bristol C. Measuring teacher practices that support student motivation: examining the factor structure of the teacher as social context questionnaire using multilevel factor analyses. J Psychoeduc Assess. 2019;37(6):743-756. doi: 10.1177/0734282918791655 [DOI] [Google Scholar]
- 23.Lam S-F, Jimerson S, Wong BPH, et al. Understanding and measuring student engagement in school: the results of an international study from 12 countries. Sch Psychol Q. 2014;29(2):213-232. doi: 10.1037/spq0000057 [DOI] [PubMed] [Google Scholar]
- 24.McAuley E, Duncan T, Tammen VV. Psychometric properties of the Intrinsic Motivation Inventory in a competitive sport setting: a confirmatory factor analysis. Res Q Exerc Sport. 1989;60(1):48-58. doi: 10.1080/02701367.1989.10607413 [DOI] [PubMed] [Google Scholar]
- 25.Standage M, Duda JL, Ntoumanis N. A test of self-determination theory in school physical education. Br J Educ Psychol. 2005;75(Pt 3):411-433. doi: 10.1348/000709904X22359 [DOI] [PubMed] [Google Scholar]
- 26.Solmon MA, Lee AM. Development of an instrument to assess cognitive processes in physical education classes. Res Q Exerc Sport. 1997;68(2):152-160. doi: 10.1080/02701367.1997.10607991 [DOI] [PubMed] [Google Scholar]
- 27.Australian Curriculum Assessment and Reporting Authority . NAPLAN Achievement in Reading, Persuasive Writing, Language Conventions and Numeracy: National Report for 2014. Accessed March 20, 2020. https://www.nap.edu.au/_resources /National_Assessment_Program_Literacy_and_Numeracy_national_report_for _2014.pdf
- 28.Flegal KM, Cole TJ. Construction of LMS parameters for the Centers for Disease Control and Prevention 2000 growth charts. Natl Health Stat Report. 2013;(63):1-3. [PubMed] [Google Scholar]
- 29.Ulrich DT. Test of Gross Motor Development Examiner’s Manual. 2nd ed. Pro Ed; 2000. [Google Scholar]
- 30.Paxton JL, Barch DM, Racine CA, Braver TS. Cognitive control, goal maintenance, and prefrontal function in healthy aging. Cereb Cortex. 2008;18(5):1010-1028. doi: 10.1093/cercor/bhm135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Judd CM, Westfall J, Kenny DA. Experiments with more than one random factor: designs, analytic models, and statistical power. Annu Rev Psychol. 2017;68:601-625. doi: 10.1146/annurev-psych-122414-033702 [DOI] [PubMed] [Google Scholar]
- 32.Hamra G, MacLehose R, Richardson D. Markov chain Monte Carlo: an introduction for epidemiologists. Int J Epidemiol. 2013;42(2):627-634. doi: 10.1093/ije/dyt043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Imai K, Keele L, Tingley D, Yamamoto T. Comment on Pearl: Practical implications of theoretical results for causal mediation analysis. Psychol Methods. 2014;19(4):482-487. doi: 10.1037/met0000021 [DOI] [PubMed] [Google Scholar]
- 34.Hartwig TB, Del Pozo-Cruz B, White RL, et al. A monitoring system to provide feedback on student physical activity during physical education lessons. Scand J Med Sci Sports. 2019;29(9):1305-1312. doi: 10.1111/sms.13438 [DOI] [PubMed] [Google Scholar]
- 35.Farooq MA, Parkinson KN, Adamson AJ, et al. Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. Br J Sports Med. 2018;52(15):1002-1006. doi: 10.1136/bjsports-2016-096933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117. doi: 10.1186/1748-5908-8-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Léger LA, Mercier D, Gadoury C, Lambert J. The multistage 20 metre shuttle run test for aerobic fitness. J Sports Sci. 1988;6(2):93-101. doi: 10.1080/02640418808729800 [DOI] [PubMed] [Google Scholar]
- 38.Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427-432. doi: 10.1093/ije/30.3.427 [DOI] [PubMed] [Google Scholar]
- 39.Brown HS III, Pérez A, Li Y-P, Hoelscher DM, Kelder SH, Rivera R. The cost-effectiveness of a school-based overweight program. Int J Behav Nutr Phys Act. 2007;4:47. doi: 10.1186/1479-5868-4-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sutton Trust-Education Endowment Foundation . Teaching and learning toolkit: technical appendix and process manual. Published July 2018. Accessed August 1, 2020. https://educationendowmentfoundation.org.uk/public/files/Toolkit/Toolkit_Manual_2018.pdf
- 41.Love R, Adams J, van Sluijs EMF. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes Rev. 2019;20(6):859-870. doi: 10.1111/obr.12823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adab P, Pallan MJ, Lancashire ER, et al. Effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6 and 7 year olds: cluster randomised controlled trial (WAVES study). BMJ. 2018;360:k211. doi: 10.1136/bmj.k211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kriemler S, Zahner L, Schindler C, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ. 2010;340:c785. doi: 10.1136/bmj.c785 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Consolidated Framework for Implementation Research
eFigure 2. iPLAY Intervention Components
eFigure 3. Online Platform Screenshots
eFigure 4. Summary of Significant Moderator Effects
eFigure 5. Sensitivity Analysis for Incremental Cost-Effectiveness Ratios
eTable 1. iPLAY Data Collector Blinding Evaluation
eTable 2. iPLAY Intervention Components and Implementation Measures
eTable 3. Intervention Adoption Rates
eTable 4. Intervention Implementation Rates
eTable 5. Per Protocol Analyses of Intervention Effects on Primary Outcome
eTable 6. Main Sample Secondary Outcomes Baseline Values
eTable 7. Main Sample Secondary Outcome Analyses
eTable 8. Sub-sample Variables Baseline Values
eTable 9. Sub-sample Variables Outcome Analyses
Trial Protocol
Data Sharing Statement