Abstract
This work aimed to prospectively record all primary central nervous system tumor (PCNST) cases in France, for which histological diagnosis is available. The objectives were to (i) create a national registry and a network to perform epidemiological studies; (ii) implement clinical and basic research protocols; and (iii) harmonize the health care of patients affected by PCNST. For 5 years, 25 756 cases of newly diagnosed and histologically confirmed PCNST have been recorded. Histological diagnoses included glioma (48.9%), all other neuroepithelial tumors (5%), meningioma (28.8%), nerve sheath tumors (8.4%), lymphoma (3.2%) and others (5.7%). Cryopreservation was reported for 6018 PCNST specimens. Tumor resections (R) were performed in 78% cases, while biopsies accounted for 22%. Median age (MA), sex, percentage R and number of cryopreserved tumors were detailed for each histology; for example, out of 6053 glioblastomas (MA 63 years, male 59.4%, R 62%, 1611 were cryopreserved), and out of 37 atypical teratoid/rhabdoid tumors (MA 2 years, male 56.8%, R 94%, 17 were cryopreserved). This database or databank dedicated to PCNST cases contains detailed data on clinical, histological and other characteristics, such as the inclusion of data on cryopreserved specimens that are not available in other European registries. Therefore, this is a valuable resource that can be used for planning future epidemiological and clinical research.
Keywords: brain tumor, database, epidemiology, neuro‐oncology, neuropathology, neurosurgery
INTRODUCTION
Primary central nervous system tumors (PCNSTs) represent a complex heterogeneous group of pathological entities that may be benign, malignant or of unpredictable evolution 2, 8, 24, 28, 30, 31, 42. These tumors represent a major public health problem (16), and the French epidemiological data are fragmentary 17, 20, 26, 32, 33, as a national registry for these tumor cases does not exist. The main objective of this project was to prospectively record all PCNST cases in France, for which histological diagnosis is available. The long‐term goals in creating the French Brain Tumor DataBase (FBTDB) were to: (i) create a national registry and a national network to perform epidemiological studies; (ii) implement a new database and use it for setting up both clinical and basic research protocols; (iii) allow the evaluation of the medical practices of an area or of the entire country; and (iv) harmonize the health care of patients affected by PCNST at the higher level. The French societies involved in the management of patients diagnosed with PCNST [ie, Association des Neuro‐Oncologues d'Expression Française (ANOCEF), Société Française de Neurochirurgie (SFNC), Société Française de Neuropathologie (SFNP)] were linked to initiate this work at a countrywide level through the use of a national survey on the medical practices in neuro‐oncology and a census of the protocols of fundamental research existing in France 3, 21. The methodology and initial results of the FBTDB, clinical epidemiology for childhood PCNST and a specific work concerning oncological patterns of care for patients with glioblastoma have already been published by the FBTDB 4, 5, 6, 7, 36.
Here, we report the histological results of the FBTDB on 25 756 cases of newly diagnosed and histologically confirmed PCNST, and discuss a few perspectives of such database.
MATERIALS AND METHODS
Patients with newly diagnosed and histologically confirmed PCNSTs (since 1 January 2004) were identified in the FBTDB, and initial data were prospectively collected. All neurosurgeons and neuropathologists in France who participated in creating the FBTDB were instructed to complete a data file card for each patient that underwent surgery. Histological diagnosis was always made by experienced neuropathologists; more than 90% of these neuropathologists worked in public academic centers. The methodology for the FBTDB accrual was previously described in detail (4). In summary, the data file card was placed in all operating rooms where surgery for PCNST is performed, and was systematically sent along with the sample to the pathology lab. The easy‐to‐complete card contains questions on sociodemographic, clinical, radiological, surgical and pathological data (an optional question about cryopreservation of the samples was included). The first part of the card (ie, sociodemographic, clinical, radiological and surgical data) was completed by the neurosurgeon. The second part was completed by the pathologist. All completed cards were mailed to the Tumor Registry from Herault (TRH) [Registre des Tumeurs de l'Hérault (RTH), Montpellier, France], which has extensive expertise in working with tumor data and has the required authorization for recording data with personal identifiers. The TRH compiled all cards and analyzed the data in collaboration with the University Institute of Clinical Research of Montpellier‐Nîmes (IURC, Institut Universitaire de Recherche Clinique, Montpellier‐Nîmes, France). A new data file card has been used since 2007 (Figure 1). The data presented here include age, sex, histological diagnosis according to the ICD‐0‐3 [World Health Organization (WHO) classification] and Systematized Nomenclature of Medicine (SNOMED) codes from Louis et al (28) and French nomenclature Association for the Development of Information Technology in Cytology, Anatomy and Pathology (ADICAP) (1) (a list of included codes is presented in Table 1), cryopreservation of samples and surgery (biopsy/resection).
Figure 1.
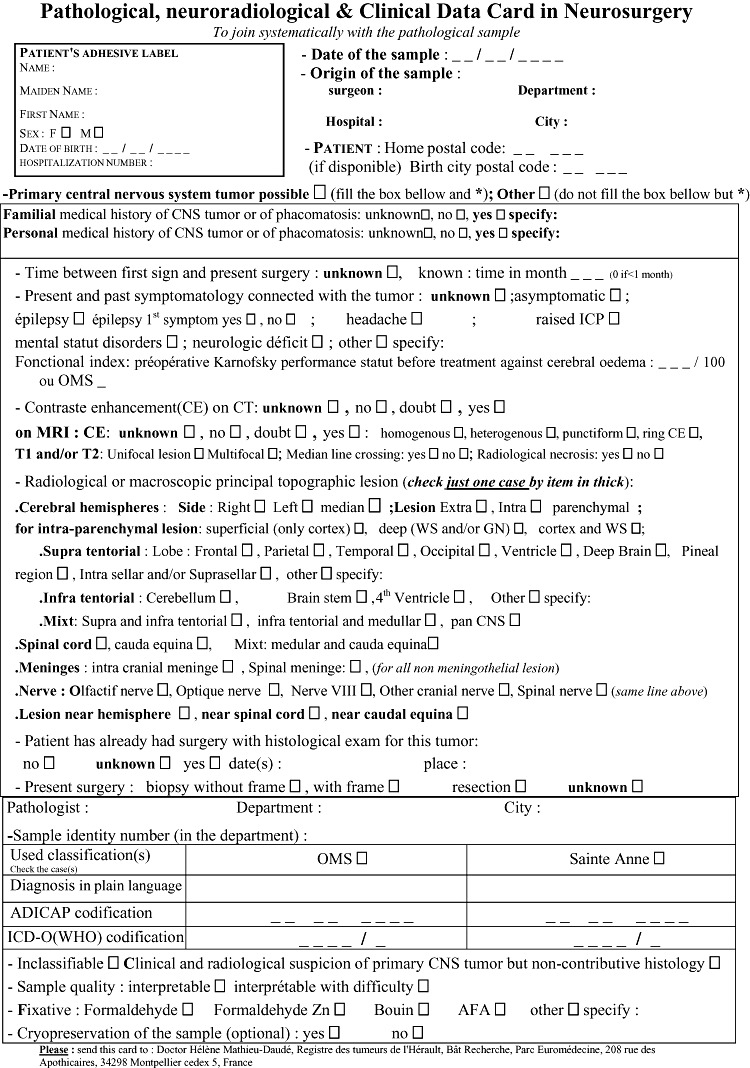
The pathological, neuroradiological and clinical card contains all the data asked for recording the primary central nervous system tumor (PCNST). It is systematically filled up for each patient by the neurosurgeon in the operating room and by the pathologist if the diagnosis of PCNST is confirmed.
Table 1.
Histological repartition of the 25 756 cases with clinical and surgical data from the French Brain Tumor Database, 2004 to 2008. Abbreviations: T = total; B = biopsy; R = resection; M = male; F = female; N = number; Med = median age at diagnosis; m = mean age at diagnosis; CRYO = cryopreservation; MPNST = malignant peripheral nerve sheath tumor.
| ICD‐O | ADICAP | N | M | F | m | Med | CRYO | Reported surgery | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| T | R (%) | B (%) | |||||||||
| Tumors of neuroepithelial tissue | |||||||||||
| Glioma NOS | 9380/3 | N7R0 | 205 | 114 | 91 | 49.96 | 56.0 | 37 | 192 | 30.7 | 69.3 |
| Astrocytic tumors | |||||||||||
| Astrocytoma NOS | 9400/3 | N7S0 | 205 | 127 | 78 | 42.82 | 46.0 | 23 | 171 | 46.2 | 53.8 |
| Pilocytic astrocytoma | 9421/1 | N0S8 | 718 | 367 | 351 | 16.26 | 12.0 | 201 | 617 | 86.7 | 13.3 |
| Pilomyxoïd astrocytoma | 9425/3 | (0001) | 4 | 1 | 3 | 10.50 | 10.0 | 2 | 2 | 50.0 | 50.0 |
| Subependymal giant cell astrocytoma | 9384/1 | N0T2/3 | 50 | 24 | 26 | 16.90 | 16.5 | 25 | 39 | 92.3 | 7.7 |
| Pleomorphic xantho‐astrocytoma | 9424/3 | N7S9 | 56 | 30 | 26 | 36.73 | 34.0 | 14 | 50 | 84.0 | 16.0 |
| Fibrillary astrocytoma | 9420/3 | N7S2 | 115 | 68 | 47 | 38.48 | 40.0 | 36 | 102 | 40.2 | 59.8 |
| Gemistocytic astrocytoma | 9411/3 | N7S4 | 41 | 26 | 15 | 45.61 | 48.0 | 11 | 35 | 45.7 | 54.3 |
| Protoplasmic astrocytoma | 9410/3 | N7S6 | 12 | 7 | 5 | 47.42 | 43.5 | 1 | 10 | 40.0 | 60.0 |
| Anaplastic astrocytoma | 9401/3 | N7T6 | 372 | 204 | 168 | 57.16 | 60.0 | 105 | 352 | 35.2 | 64.8 |
| Glioblastoma | 9440/3 | N7X0 | 6053 | 3593 | 2460 | 61.61 | 63.0 | 1611 | 5212 | 61.9 | 38.1 |
| Giant cell glioblastoma | 9441/3 | N7X2 | 115 | 63 | 52 | 55.90 | 60.0 | 43 | 109 | 67.9 | 32.1 |
| Gliosarcoma | 9442/3 | N7X4 | 62 | 40 | 22 | 55.77 | 57.0 | 17 | 54 | 92.6 | 7.4 |
| Gliomatosis cerebri | 9381/3 | N7R9 | 25 | 15 | 10 | 48.08 | 52.0 | 4 | 21 | 23.8 | 76.2 |
| 8033 | 4679 | 3354 | 55.50 | 60.0 | 2130 | 6966 | |||||
| 58.2% | 41.8% | 26.5% | 61.6 | 38.4 | |||||||
| Oligodendroglial tumors | |||||||||||
| Oligodendroglioma | 9450/3 | N7V0 | 1271 | 731 | 540 | 43.24 | 42.0 | 346 | 1064 | 61.7 | 38.3 |
| Anaplastic oligodendroglioma | 9451/3 | N7V4 | 1313 | 733 | 580 | 52.68 | 54.0 | 456 | 1202 | 69.3 | 30.7 |
| 2584 | 1464 | 1120 | 47.90 | 48.0 | 802 | 2266 | |||||
| 56.7% | 43.3% | 31.0% | 65.7 | 34.3 | |||||||
| Oligoastrocytic tumors | |||||||||||
| Oligoastrocytic tumors NOS | 9382/3 | N7R4 | 8 | 5 | 3 | 47.75 | 46.0 | 2 | 6 | 50.0 | 50.0 |
| Oligoastrocytoma | 9382/3 | N7V2 | 416 | 223 | 193 | 43.92 | 42.0 | 106 | 370 | 58.9 | 41.1 |
| Anaplastic oligoastrocytoma | 9382/3 | N7V3 | 831 | 475 | 356 | 52.24 | 55.0 | 224 | 771 | 60.7 | 39.9 |
| 1255 | 703 | 552 | 49.42 | 51.0 | 332 | 1147 | |||||
| 56.0% | 44.0% | 26.5% | 60.1 | 39.9 | |||||||
| Ependymal tumors | |||||||||||
| Subépendymoma | 9383/1 | N0W6 | 57 | 40 | 17 | 51.81 | 55.0 | 14 | 46 | 87.0 | 13.0 |
| Myxopapillary ependymoma | 9394/1 | N7W2 | 87 | 53 | 34 | 37.47 | 35.0 | 14 | 71 | 97.2 | 2.8 |
| Ependymoma, NOS | 9391/3 | N7W0 | 388 | 217 | 171 | 41.46 | 43.0 | 88 | 305 | 92.5 | 7.5 |
| Cellular ependymoma | 9391/3 | N7W1 | 30 | 16 | 14 | 33.70 | 33.0 | 9 | 28 | 92.9 | 7.1 |
| Papillary ependymoma | 9393/3 | N7W4 | 15 | 8 | 7 | 44.67 | 50.0 | 4 | 12 | 91.7 | 8.3 |
| Clear cell ependymoma | 9391/3 | N7W5 | 18 | 11 | 7 | 26.67 | 20.0 | 3 | 14 | 85.7 | 14.3 |
| Ependymoma, anaplastic | 9392/3 | N7W8 | 128 | 62 | 66 | 26.33 | 13.5 | 50 | 112 | 90.2 | 9.8 |
| Tanicytic ependymoma | 9391/3 | (0002) | 10 | 8 | 2 | 40.10 | 42.0 | 3 | 8 | 50.0 | 50.0 |
| 733 | 415 | 318 | 38.52 | 41.0 | 185 | 596 | |||||
| 56.6% | 43.4% | 25.2% | 91.4 | 8.6 | |||||||
| Total | 12 605 | 7261 | 5344 | 52.35 | 56.0 | 3449 | 10 975 | ||||
| Gliomes | 57.6% | 42.4% | 27.4% | 63.9 | 36.1 | ||||||
| Choroid plexus tumors | |||||||||||
| Choroid plexus papilloma | 9390/0 | N0Z0 | 89 | 42 | 47 | 26.70 | 22.0 | 19 | 76 | 92.1 | 7.9 |
| Atypical choroid plexus papilloma | 9390/1 | (0003) | |||||||||
| Choroid plexus carcinoma | 9390/3 | N7Z0 | 14 | 9 | 5 | 23.43 | 13.0 | 4 | 14 | 85.7 | 14.3 |
| 103 | 51 | 52 | 26.25 | 20.0 | 23 | 90 | |||||
| 49.5% | 50.5% | 22.3% | 91.1 | 8.9 | |||||||
| Other neuroepithelial tumors | |||||||||||
| Astroblastoma | 9430/3 | N7T4 | 1 | 0 | 1 | 24.00 | 24.0 | 1 | 1 | 100.0 | 0.0 |
| Chordoid glioma of the third ventricle | 9444/1 | (0004) | 3 | 2 | 1 | 41.66 | 46.0 | 1 | 2 | 50.0 | 50.0 |
| Angiocentric glioma | 9431/1 | (0005) | |||||||||
| Esthesioneuroblastoma | 9522/3 | B7F2 | 20 | 15 | 5 | 49.05 | 47.0 | 2 | 18 | 94.4 | 5.6 |
| 24 | 17 | 7 | 47.08 | 47.0 | 4 | 21 | |||||
| 70.8% | 29.2% | 16.7% | 95.0 | 5.0 | |||||||
| Neuronal and mixed neuronal–glial tumors | |||||||||||
| Dysplastic gangliocytoma of cerebellum (Lhermitte–Duclos) | 9493/0 | N0L2 | 4 | 3 | 1 | 40.75 | 42.5 | 1 | 4 | 100.0 | 0.0 |
| Desmoplastic infantile astrocytoma/ganglioma | 9412/1 | N0N0 | 5 | 1 | 4 | 16.40 | 2.0 | 0 | 5 | 100.0 | 0.0 |
| Dysembryoplastic neuroepithelial tumor | 9413/0 | N0N2 | 128 | 71 | 57 | 20.52 | 18.0 | 37 | 117 | 92.3 | 7.7 |
| Gangliocytoma | 9492/0 | N0L0 | 12 | 4 | 8 | 33.25 | 32.5 | 3 | 11 | 81.8 | 18.2 |
| Ganglioglioma | 9505/1 | N7N0 | 287 | 159 | 128 | 22.83 | 18.0 | 87 | 212 | 87.7 | 12.3 |
| Anaplastic ganglioglioma | 9505/3 | N7N1 | 34 | 19 | 15 | 45.56 | 50.0 | 10 | 28 | 89.3 | 10.7 |
| Central neurocytoma | 9506/1 | N4L0 | 74 | 37 | 37 | 35.16 | 31.0 | 23 | 62 | 90.3 | 9.7 |
| Extraventricular neurocytoma | 9506/1 | (0006) | |||||||||
| Cerebellar liponeurocytoma | 9506/1 | (0007) | |||||||||
| Papillary glioneuronal tumor | 9509/1 | (0008) | 3 | 2 | 1 | 22.00 | 16.0 | 2 | 3 | 100.0 | 0.0 |
| Rosette‐forming glioneuronal tumor of the fourth ventricle | 9509/1 | (0009) | 4 | 2 | 2 | 35.50 | 30.0 | 2 | 3 | 100.0 | 0.0 |
| Paraganglioma | 8680/1 | P0A0 | 22 | 10 | 12 | 47.77 | 44.0 | 4 | 17 | 100.0 | 0.0 |
| Paraganglioma malignant | 8680/3 | P7A0 | 3 | 1 | 2 | 52.66 | 55.0 | 0 | 2 | 50.0 | 50.0 |
| 576 | 309 | 267 | 26.72 | 23.0 | 169 | 464 | |||||
| 53.6% | 46.4% | 29.3% | 89.9 | 10.1 | |||||||
| Tumor of the pineal region | |||||||||||
| Pinealoma, NOS | 9360/1 | P7P0 | 11 | 9 | 2 | 39.73 | 44.0 | 3 | 11 | 36.4 | 63.6 |
| Pineocytoma | 9361/1 | P7P2 | 28 | 11 | 17 | 48.93 | 47.5 | 4 | 25 | 80.0 | 20.0 |
| Pineal parenchymal tumor of intermediate differentiation | 9362/3 | P7P6 | 3 | 2 | 1 | 26.33 | 28.0 | 2 | 3 | 33.3 | 66.7 |
| Pineoblastoma | 9362/3 | P7P4 | 24 | 12 | 12 | 23.08 | 18.0 | 5 | 21 | 61.9 | 38.1 |
| Papillary tumor of the pineal region | 9395/3 | (0010) | 2 | 1 | 1 | 53.00 | 53.0 | 0 | |||
| 68 | 35 | 33 | 37.44 | 39.5 | 14 | 60 | |||||
| 51.5% | 48.5% | 20.6% | 63.3 | 36.7 | |||||||
| Embryonal tumors | |||||||||||
| Medulloblastoma, NOS | 9470/3 | N7P0 | 314 | 186 | 128 | 17.90 | 11.5 | 111 | 290 | 90.0 | 10.0 |
| Desmoplastic medulloblastoma | 9471/3 | N7P2 | 53 | 35 | 18 | 12.23 | 9.0 | 22 | 45 | 93.3 | 6.7 |
| Medulloblastoma with extensive nodularity | 9471/3 | (0011) | 3 | 1 | 2 | 10.33 | 7.0 | 1 | 2 | 100.0 | 0.0 |
| Anaplastic medulloblastoma | 9474/3 | (0012) | 4 | 4 | 0 | 19.00 | 15.5 | 1 | 3 | 100.0 | 0.0 |
| Large‐cell medulloblastoma | 9474/3 | (0013) | 1 | 1 | 0 | 2.00 | 2.0 | 1 | 1 | 100.0 | 0.0 |
| CNS primitive neuroectodermal tumor | 9473/3 | N7M2 | 68 | 33 | 35 | 22.25 | 12.5 | 16 | 63 | 79.4 | 20.6 |
| CNS Neuroblastoma | 9500/3 | N7M0 | 14 | 9 | 5 | 16.36 | 5.0 | 6 | 13 | 76.9 | 23.1 |
| CNS Ganglioneuroblastoma | 9490/3 | N7M1 | 8 | 4 | 4 | 34.50 | 36.5 | 0 | 6 | 100.0 | 0.0 |
| Medulloepithélioma | 9501/3 | N7Q0 | 3 | 0 | 3 | 2.66 | 3.0 | 1 | 2 | 50.0 | 50.0 |
| Ependymoblastoma | 9392/3 | N7X8 | 1 | 0 | 1 | 25.00 | 25.0 | 0 | |||
| Atypical teratoid/rhabdoid tumor | 9508/3 | X7R8 | 37 | 21 | 16 | 9.32 | 2.0 | 17 | 32 | 93.8 | 6.3 |
| 506 | 294 | 212 | 17.33 | 10.0 | 176 | 457 | |||||
| 58.1% | 41.9% | 34.8% | 88.8 | 11.2 | |||||||
| Tumors of the cranial and paraspinal nerves | |||||||||||
| Schwannoma (neurilemnoma, neurinoma) | 9560/0 | N0A0 | 1894 | 900 | 994 | 51.75 | 53.0 | 360 | 1634 | 97.9 | 2.1 |
| Schwannoma (neurofibromatosis type1) | 9560/0 | N0B0 | 101 | 50 | 51 | 53.55 | 55.0 | 6 | 87 | 97.7 | 2.3 |
| Cellular schwannoma | 9560/0 | N4A0 | 16 | 8 | 8 | 46.62 | 52.5 | 2 | 13 | 76.9 | 23.1 |
| Plexiform schwannoma | 9560/0 | N0A6 | 8 | 2 | 6 | 47.25 | 48.5 | 0 | 7 | 100.0 | 0.0 |
| Mélanotic schwannoma | 9560/0 | N0C4 | 5 | 2 | 3 | 52.60 | 47.0 | 0 | 4 | 100.0 | 0.0 |
| Neurofibroma | 9540/0 | N0C0 | 78 | 40 | 38 | 39.89 | 39.0 | 8 | 65 | 100.0 | 0.0 |
| Plexiform neurofibroma | 9550/0 | N0C1 | 9 | 5 | 4 | 35.11 | 29.0 | 1 | 6 | 100.0 | 0.0 |
| Granular cells neurofibroma | 9540/0 | N0C8 | 3 | 0 | 3 | 57.66 | 62.0 | 1 | 2 | 100.0 | 0.0 |
| Neurofibroma (neurofibromatosis type 1) | 9540/0 | N0D0 | 13 | 7 | 6 | 34.70 | 29.0 | 2 | 10 | 100.0 | 0.0 |
| Neurofibrosarcoma (SAI) | 9540/3 | N7C0 | 6 | 3 | 3 | 43.83 | 38.5 | 2 | 6 | 83.3 | 16.7 |
| Perineurioma | 9571/0 | N0G0 | 3 | 1 | 2 | 58.33 | 59.0 | 0 | 2 | 100.0 | 0.0 |
| Intraneural perineurioma | 9571/0 | N0G4 | |||||||||
| Malignant perineurioma | 9571/3 | (0014) | |||||||||
| Malignant peripheral nerve sheath tumor | 9540/3 | N7A0 | 16 | 4 | 12 | 44.44 | 40.0 | 2 | 8 | 100.0 | 0.0 |
| Epithelioid MPNST | 9540/3 | N7A3 | |||||||||
| MPNST with mesenchymal differentiation | 9540/3 | N7H0 | |||||||||
| Melanotic MPNST | 9540/3 | N7A5 | 1 | 0 | 1 | 35.00 | 35.0 | 0 | 1 | 100.0 | 0.0 |
| MPNST with glandular differentiation | 9540/3 | N7A6 | 1 | 1 | 0 | 28.00 | 28.0 | 0 | 1 | 100.0 | 0.0 |
| 2154 | 1023 | 1131 | 51.07 | 53.0 | 384 | 1846 | |||||
| 47.5% | 52.5% | 17.8% | 97.8 | 2.2 | |||||||
| Tumors of the meninges | |||||||||||
| Tumors of meningothelial cells | |||||||||||
| Meningioma, NOS | 9530/0 | N0J0 | 1507 | 374 | 1133 | 57.19 | 57.0 | 264 | 1337 | 97.5 | 2.5 |
| Meningothelial meningioma | 9531/0 | N0K2 | 2397 | 626 | 1771 | 57.46 | 57.0 | 517 | 2029 | 97.8 | 2.2 |
| Fibrous (fibroblastic) meningioma | 9532/0 | N0J4 | 754 | 144 | 610 | 57.67 | 58.0 | 141 | 628 | 97.1 | 2.9 |
| Transitional (mixed) meningioma | 9537/0 | N0K4 | 1168 | 267 | 901 | 57.24 | 57.0 | 218 | 1013 | 97.3 | 2.7 |
| Psammomatous meningioma | 9533/0 | N0K8 | 302 | 39 | 263 | 62.29 | 63.0 | 44 | 246 | 96.7 | 3.3 |
| Angiomatous meningioma | 9534/0 | N0J2 | 151 | 61 | 90 | 58.96 | 58.5 | 29 | 136 | 96.3 | 3.7 |
| Rare variety meningioma (NOS) | 9530/0 | N0K9* | 65 | 14 | 51 | 57.71 | 57.0 | 7 | 64 | 89.1 | 10.9 |
| Microcystic meningioma | 9530/0 | N0K9 | 71 | 17 | 54 | 55.23 | 56.0 | 19 | 62 | 100.0 | 0.0 |
| Secretory meningioma | 9530/0 | N0K9 | 89 | 13 | 76 | 58.23 | 57.0 | 11 | 70 | 97.1 | 2.9 |
| Lymphoplasmacyte‐rich meningioma | 9530/0 | N0K9 | |||||||||
| Clear‐cell meningioma | 9538/1 | N0K9 | 38 | 11 | 27 | 51.39 | 50.5 | 11 | 35 | 100.0 | 0.0 |
| Chordoid meningioma | 9538/1 | N0K9 | 58 | 17 | 41 | 52.92 | 52.5 | 8 | 53 | 98.1 | 1.9 |
| Rhabdoid meningioma | 9538/3 | N0K9 | 5 | 2 | 3 | 64.40 | 66.0 | 2 | 4 | 100.0 | 0.0 |
| Metaplastic meningioma | 9530/0 | N0K3 | 40 | 10 | 30 | 56.25 | 54.0 | 3 | 33 | 93.9 | 6.1 |
| Atypical meningioma | 9539/1 | N4J0 | 624 | 299 | 325 | 59.60 | 62.5 | 128 | 482 | 97.5 | 2.5 |
| Papillary meningioma | 9538/3 | N7K6 | 8 | 5 | 3 | 47.12 | 45.0 | 3 | 7 | 100.0 | 0.0 |
| Anaplastic meningioma | 9530/3 | N7J0 | 134 | 66 | 68 | 61.23 | 62.5 | 22 | 101 | 99.0 | 1.0 |
| Meningiomatosis | 9530/1 | N4J9 | 8 | 4 | 4 | 51.00 | 53.5 | 3 | 7 | 100.0 | 0.0 |
| 7419 | 1969 | 5450 | 57.76 | 58.0 | 1430 | 6307 | |||||
| 26.5% | 73.5% | 19.3% | 97.4 | 2.6 | |||||||
| Mesenchymal tumors | |||||||||||
| Benign mesenchymal tumor (NOS) | X0H0 | ||||||||||
| Lipoma | 8850/0 | L0L0 | 19 | 14 | 5 | 31.79 | 30.0 | 1 | 16 | 93.8 | 6.3 |
| Angiolipoma | 8861/0 | L0P1 | 5 | 3 | 2 | 53.20 | 55.0 | 1 | 3 | 100.0 | 0.0 |
| Hibernoma | 8880/0 | L0M4 | |||||||||
| Liposarcoma | 8850/3 | L7L0 | 2 | 2 | 0 | 49.50 | 49.5 | 0 | 2 | 100.0 | 0.0 |
| Solitary fibrous tumor | 8815/0 | F0A1 | 33 | 14 | 19 | 54.00 | 57.0 | 11 | 30 | 93.3 | 6.7 |
| Fibrosarcoma | 8810/3 | F7A0 | |||||||||
| Histiocytome fibreux malin | 8830/3 | F7M0 | |||||||||
| Leiomyoma | 8890/0 | L0A0 | |||||||||
| Leiomyosarcoma | 8890/3 | L7A0 | 3 | 1 | 2 | 62.66 | 57.0 | 1 | 3 | 100.0 | 0.0 |
| Rhabdomyoma | 8900/0 | R0C0 | |||||||||
| Rhabdomyosarcoma | 8900/3 | R7C0 | 3 | 1 | 2 | 11.66 | 13.0 | 0 | 3 | 100.0 | 0.0 |
| Chondroma | 9220/0 | C0A0 | 4 | 3 | 1 | 20.75 | 16.0 | 0 | 2 | 100.0 | 0.0 |
| Chondrosarcoma | 9220/3 | C7A0 | 14 | 5 | 9 | 38.50 | 36.5 | 1 | 11 | 90.9 | 9.1 |
| Osteoma | 9180/3 | Q0A0 | 14 | 3 | 11 | 40.14 | 37.5 | 1 | 11 | 100.0 | 0.0 |
| Osteosarcoma | 9180/3 | Q7A0 | 6 | 5 | 1 | 32.33 | 31.5 | 2 | 5 | 100.0 | 0.0 |
| Osteochondroma | 9210/0 | C0G0 | 6 | 2 | 4 | 37.67 | 40.0 | 0 | 4 | 100.0 | 0.0 |
| Hemangioma | 9120/0 | V0A0 | 251 | 125 | 126 | 39.57 | 41.0 | 13 | 190 | 96.3 | 3.7 |
| Epithelioid hemangioendothelioma | 9133/1 | V7N0 | 3 | 1 | 2 | 68.33 | 69.0 | 0 | 3 | 100.0 | 0.0 |
| Hemangiopericytoma benign | 9150/1 | V0K0 | 30 | 16 | 14 | 53.27 | 54.5 | 8 | 26 | 100.0 | 0.0 |
| Uncertain malignancy hemangiopericytoma | V4K0 | 19 | 11 | 8 | 55.31 | 58.0 | 5 | 11 | 100.0 | 0.0 | |
| Infantile hemangiopericytoma | V0K1 | ||||||||||
| Anaplastic hemangiopericytoma | 9150/3 | V7K0 | 29 | 15 | 14 | 57.21 | 56.0 | 3 | 26 | 96.2 | 3.8 |
| Angiosarcoma | 9120/3 | V7A0 | 3 | 3 | 0 | 49.00 | 44.0 | 0 | 2 | 100.0 | 0.0 |
| Kaposi sarcoma | 9140/3 | V7R0 | |||||||||
| Ewing's sarcoma—PNET | 9364/3 | X7L0 | 8 | 5 | 3 | 23.75 | 23.5 | 2 | 8 | 100.0 | 0.0 |
| 452 | 229 | 223 | 42.49 | 45.0 | 49 | 356 | |||||
| 50.7% | 49.3% | 10.8% | 96.6 | 3.4 | |||||||
| Primary melanocytic lesions | |||||||||||
| Diffuse melanocytoma | 8728/0 | (0015) | |||||||||
| Melanocytoma | 8728/1 | (0016) | |||||||||
| Malignant melanoma | 8720/3 | M7A0 | 11 | 6 | 5 | 65.00 | 69.0 | 1 | 7 | 100.0 | 0.0 |
| Meningeal melanomatosis | 8728/3 | (0017) | |||||||||
| 11 | 6 | 5 | 65.00 | 69.0 | 1 | 7 | |||||
| 100.0 | 0.0 | ||||||||||
| Other neoplasms related to the meninges | |||||||||||
| Hemangioblastoma | 9161/1 | V0G0 | 394 | 208 | 186 | 45.91 | 45.0 | 81 | 342 | ||
| 52.8% | 47.2% | 20.6% | 98.2 | 1.8 | |||||||
| Lymphomas and hematopoietic neoplasms | |||||||||||
| Malignant lymphoma | 9590/3 | K7G0 | 321 | 172 | 149 | 62.09 | 66.0 | 57 | 178 | 25.3 | 74.7 |
| Diffuse large B cell lymphoma | 9680/3 | K7G7 | 513 | 263 | 250 | 64.67 | 67.0 | 106 | 394 | 20.3 | 79.7 |
| Plasmacytoma | 9731/3 | J7D8 | 16 | 7 | 9 | 55.87 | 56.0 | 1 | 9 | 100.0 | 0.0 |
| Granulocytic sarcoma | 9930/3 | (0018) | |||||||||
| 850 | 442 | 408 | 63.05 | 66.0 | 164 | 581 | |||||
| 52.0% | 48.0% | 19.3% | 23.1 | 76.9 | |||||||
| Germ cell tumors | |||||||||||
| Germinoma | 9064/3 | G7K0 | 54 | 46 | 8 | 20.39 | 17.5 | 9 | 48 | 37.5 | 62.5 |
| Embryonal carcinoma | 9070/3 | G7H5 | 1 | 1 | 0 | 14.00 | 14.0 | 0 | 1 | 100.0 | 0.0 |
| Yolk sac tumor | 9071/3 | G7H6 | 1 | 1 | 0 | 15.00 | 15.0 | 0 | 1 | 0.0 | 100.0 |
| Choriocarcinoma | 9100/3 | T7C0 | |||||||||
| Teratoma (NOS) | 9080/1 | D0V0 | 2 | 2 | 0 | 20.50 | 20.5 | 0 | 2 | 100.0 | 0.0 |
| Mature teratome | 9080/0 | G0G0 | 27 | 15 | 12 | 25.11 | 17.0 | 4 | 23 | 95.7 | 4.3 |
| Immature germ cell tumors (NOS) | 9080/3 | G7H0 | 4 | 2 | 2 | 19.00 | 18.0 | 0 | 4 | 75.0 | 25.0 |
| Immature teratoma | 9080/3 | G7H1 | 7 | 4 | 3 | 8.71 | 8.0 | 2 | 6 | 100.0 | 0.0 |
| Teratoma with malignant transformation | 9084/3 | G7G0 | |||||||||
| Mixed germ cell tumor | 9085/3 | T7H0 | |||||||||
| Immature teratoma and seminoma | 9080/3 | G7M6 | 1 | 0 | 1 | 8.00 | 8.0 | 0 | 1 | 100.0 | 0.0 |
| Malignant germ cell tumors (NOS) | 9064/3 | G7A0 | 9 | 8 | 1 | 15.22 | 13.0 | 3 | 9 | 55.6 | 44.4 |
| 106 | 79 | 27 | 20.10 | 17.0 | 18 | 95 | |||||
| 74.5% | 25.5% | 17.0% | 61.1 | 38.9 | |||||||
| Tumors of the sellar region | |||||||||||
| Craniopharyngioma | 9350/1 | D0N2 | 255 | 144 | 111 | 35.64 | 36.0 | 26 | 225 | 92.4 | 7.6 |
| Adamantinous craniopharyngioma | 9351/1 | (0019) | 37 | 19 | 18 | 38.46 | 35.0 | 5 | 22 | 100.0 | 0.0 |
| Papillary craniopharyngioma | 9352/1 | (0020) | 3 | 1 | 2 | 49.66 | 45.0 | 0 | 2 | 100.0 | 0.0 |
| Granular cell tumor | 9582/0 | (0021) | |||||||||
| Pituicytoma | 9432/1 | (0022) | 2 | 1 | 1 | 59.00 | 59.0 | 0 | 1 | 100.0 | 0.0 |
| Spindle cell oncocytoma (adenohypophysis) | 8291/0 | ||||||||||
| 297 | 165 | 132 | 36.29 | 36.0 | 31 | 250 | |||||
| 55.6% | 44.4% | 10.4% | 93.2 | 6.8 | |||||||
| Miscellaneous | |||||||||||
| Chordoma | 9370/3 | D4N4 | 61 | 40 | 21 | 50.88 | 56.0 | 10 | 50 | 92.0 | 8.0 |
| Uncategorized | 130 | 64 | 66 | 46.26 | 52.0 | 15 | 97 | 41.2 | 58.8 | ||
| 191 | 104 | 87 | 47.74 | 53.0 | 25 | 147 | |||||
| 54.5% | 45.5% | 13.1% | 58.5 | 41.5 | |||||||
| Total | 25 756 | 12 192 | 13 564 | 52.15 | 56.0 | 6018 | 21 997 | ||||
| 47.3% | 52.7% | 23.4% | 77.9 | 22.1 | |||||||
The italicized ICD‐O numbers are provisional codes proposed for the fourth edition of ICD‐O.
Note that from 2004 to 2006, pathologists used The WHO 2000 Classification (24). Since 2007, the new WHO classification (28) has been applied, and rare mesenchymal tumors of the meninges have been recorded only since 2007.
The study was approved by the French legislation, and by all the French societies involved in the neuro‐oncology field: ANOCEF, SFNC and SFNP.
RESULTS
From 2004 to 2008, a total of 25 756 cases of newly diagnosed histologically confirmed PCNSTs was recorded in the FBTDB. Of the 60 participating centers (coupled neurosurgical department/pathological lab) located throughout France, 50 were public centers (45 academic centers and 5 general hospitals) and 10 were private institutions. However, with regard to the number of patients, the proportions were 94% from public centers and 6% from private institutions.
Of the 25 756 PCNST cases, 12 192 were men (47.3%), 13 564 were women (52.7%), 1601 were children (age: <15 years) (6.2%) and 521 were teenagers (15 ≤ age < 20 years) (2%).
Tumor localizations were specified in 17 199 cases and included supratentorial (77.7%), infratentorial (15.7%), spinal cord or cauda equina (5.3%) and mixed (1.3%). Surgery was specified in 21 997 cases. Tumor resections represented 78% of surgical operations, while biopsies represented 22%. For each histological type and subtype, percentages of biopsy and resection are detailed in Table 1.
Histological results
The distribution by each histology, sex, mean/median age (MA) at diagnosis and surgery, for the 25 756 PCNST cases, is shown in Table 1. Gliomas accounted for about half of all PCNST cases, while meningiomas accounted for about one‐third. Gliomas were more frequent in men (57.6%), while meningiomas in women (73.5%). The MAs of gliomas/all other neuroepithelial tumors/meningiomas/nerve sheath tumors/lymphomas were 56, 18, 58, 53 and 66 years, respectively.
According to the new WHO classification 27, 28, the new entities encountered in our series were: three papillary glioneuronal tumors, four rosettes forming glioneuronal tumor of the fourth ventricle, two papillary tumors of the pineal region, two pituicytomas and no spindle cell oncocytoma of the ante hypophysis. Concerning the new variants, we counted four pilomyxoid astrocytomas, four anaplastic medulloblastomas and three medulloblastomas with extensive nodularity recorded over 2 years.
Formaldehyde was used as a fixative, alone or in association, in 68% of the case samples. Cryopreservation was reported for 6018 PCNST specimens.
DISCUSSION
This work detailed all histological types and subtypes for 25 756 cases of newly diagnosed and histologically confirmed PCNST in France from 2004 to 2008. This work was made possible, thanks to the cooperation of a large number of neurosurgeons and pathologists from all over France, and the methodological support of epidemiologists. Above all, this work shows the importance of multidisciplinary networks and databases that involve clinicians, pathologists and epidemiologists (8).
However, this discussion is mainly focused on: (i) methodology; (ii) comparison of our results (histological distribution, age, sex, surgery) with a small number of publications that detailed all types and subtypes of PCNST in a large population; and (iii) current applications and perspectives of such database for scientific and public communities.
Methodology
The primary difficulty in building a tumor registry is defining the type of tumor to be recorded. Recent publications 11, 12, 17, 30, 31, 41, the classification system of the WHO 24, 28 and the European recommendations for coding tumors of the brain and central nervous system (CNS) (18) include all primary benign and malignant tumors located in the CNS, including the envelopes of the CNS and the origin of the nerves localized in the skull and the spine. Second, a registry has to record all cases of the defined tumors. The ascertainment system could influence the selection of tumor types to be included in the registry definition. As our registration system was based on the neurosurgical French network, we decided to record tumors that are always seen in neurosurgery. At the beginning of this work in 2004, we did not include mesenchymal non‐meningothelial tumors (except hemangiopericytoma), which were not considered as primary brain tumors by the French community at that time. Except for these differences, we selected the types of tumors that are included in the WHO 2000 (24) and Central Brain Tumor Registry of the United States (CBTRUS) classification schemes. In addition, we used the French nomenclature (1) in combination with the WHO (24).
Since 2007, all the codes included in the WHO 2007 (28) have been used in the FBTDB, and we started to record pituitary tumors. However, we still had some difficulties recording some cases of pituitary tumors. So, we decided to exclude pituitary tumors in the present work.
In the future, we could adopt a complementary strategy. It has been established by the Brain Tumor Epidemiology Consortium (BTEC) that glioblastomas and meningiomas have enough general agreement over time, across regions and between individual pathologists that one can consider using existing diagnostic data without further review [ie, as long as uniform guidelines, such as those provided by the WHO, are used (15)]. This would limit the number of cases to review and would mainly concern the rare PCNSTs. Moreover, some specific studies on rare PCNSTs will soon begin in France, and in these cases, the review will be part of the projects.
Comparison of our results
To our knowledge, there is no publication that detailed the distribution of all histological types and subtypes of PCNST according to the WHO 2007 Classification, by number of cases, sex, MA, number of cryopreserved samples and surgery for all ages in a large population.
First, in most countries, brain tumor registration is restricted to malignant tumor types (13). Only a few countries (eg, USA, Canada, Scandinavian countries, Austria) report incidence rates on benign and borderline brain tumors 9, 10, 12, 38, 39, 41. These tumors constitute approximately 45.5% to 70% of all brain tumors (11). However, benign and borderline lesions may be associated with significant neurological deficits, and may show malignant biological progression over time. Therefore, increasing attempts to register all brain tumor cases have been made. In the USA, it has already become legally mandatory to report all brain tumor types (Benign Brain Tumor Cancer Registries Amendment Act; Public Law 107‐260). Second, even in publications that included primary nonmalignant tumors, the details of all histological types and subtypes are very rarely presented. Therefore, our results are mainly compared to the CBTRUS results.
The sex ratios (male/female) for the CBTRUS (11) and for the FBTDB are very similar (eg, all neuroepithelial tumors: 1.28/1.34, all gliomas: 1.29/1.36, glioblastomas: 1.37/1.46, pilocytic astrocytomas: 1.14/1.05, oligodendrogliomas: 1.21/1.35, all ependymomas: 1.13/1.30, nonmalignant and malignant neuronal/glial tumors: 1.24/1.16, embryonal/primitive/medulloblastoma: 1.46/1.39, tumors of cranial and spinal nerves: 0.94/0.91, meningiomas: 0.35/0.36, lymphomas: 1.19/1.08, etc., for CBTRUS/FBTDB, respectively).
For many tumors, the MA at diagnosis is similar in the CBTRUS (11) and in the FBTDB (eg, pilocytic astrocytoma: 13/12, oligodendroglioma: 41/42, glioblastoma: 64/63, choroid plexus tumors: 17/20, nonmalignant and malignant neuronal/glial tumors: 26/23, embryonal tumors: 9/10, tumors of cranial and spinal nerves: 53/53, craniopharyngioma: 38/36, lymphoma: 63/66 years old for CBTRUS/FBTDB, respectively). In addition, it is important to note that the MA at diagnosis is often lower in clinical trials (eg, for glioblastoma, 56 years in Stupp et al (37) and 53 years in Westphal et al (40)) and in some single‐institution studies (eg, 58 years in Filippini et al (19)). Age is an important prognostic factor for most of all PCNSTs; this underlines the importance of population studies to compare oncological management and survival between two different countries or areas.
Before comparing the percentages of each PCNST between the CBTRUS and the FBTDB, it is important to note few important points. First, CBTRUS reported more than 10% of pituitary tumors (10.7% in the 2009–2010 CBTRUS statistical report in 18 states in 2002–2006 (11), and 12.7% in CBTRUS statistical report in the USA in 2004–2006 (12)), whereas FBDTB did not include pituitary tumors in the present report. Second, unspecified neoplasm accounted for 5.1% in the CBTRUS (11), while it accounted for only 0.5% in the FBTDB. This difference could be explained by the fact that in the FBTDB, histological coding comes directly from pathologists, while the CBTRUS includes cases without histological diagnosis. Third, the percentage of meningioma is smaller in the FBTDB (28.8%) than in the CBTRUS (37.7%, when considering without pituitary tumors) (11). This difference could also be explained by the fact that in the FBTDB, only cases with histological confirmation have been recorded. In 2011, reporting of all cases of PCNST is still a challenge, specifically for nonmalignant tumors and tumors without histological confirmation. In the last report of the CBTRUS, it was stated that “the cancer registry incidence rates for the malignant tumors (cancer registry range: 4.62 to 8.69 per 100 000 person‐years) are again seen as being much less variable than the reported incidence rates for the non‐malignant tumors (cancer registry range: 6.13 to 16.74 per 100 000 person–years)”(12).
When we take into account these three points, we can consider that our results (Table 1) show a distribution by histology, MA at diagnosis and sex comparable to the recent literature 11, 12, 17, 41, even by specific histology 23, 35. The distribution of the different subtypes of PCNST is similar in France and in the USA, except for oligodendroglial tumors. Two main reasons may explain this difference: (i) the US data were collected between 2002 and 2006 (11), while the French data were collected between 2004 and 2008. Indeed, most studies (for a review, see (22)) have reported a recent increase of oligodendroglial tumors in comparison to astrocytic tumors. (ii) French neuropathologists are more influenced by the classification proposed by Daumas‐Duport et al (14) than American neuropathologists.
New entities and variants have been published by the last WHO classification in 2007 (28). As our work included the year 2008, French pathologists included few such cases. These new entities began to be described in 2008, 1 year after the new classification has been published. But, it is too early to be representative of a population study. Moreover, only few specific cases have been reported in the literature.
To our knowledge, this work is the first in Europe, and probably in the world, that specifies the surgery (biopsy or resection) for all histological types and subtypes of PCNST in a large population. Over 97% of tumors of the meninges, and cranial and paraspinal nerves are resected. Regarding gliomas, the proportion of biopsy appears to vary by country and/or studies. For example, the Glioma Outcomes Project described a biopsy rate for glioblastoma of 20% (25), and in the San Francisco Bay Area SEER registry, during the period 1991–2001, 27.3% of glioblastoma patients had a biopsy (43). In an Italian single‐institution study, biopsy was performed in 12% of all the glioblastoma cases (19), and in an Italian consortium study, the percentage of biopsies was 25% for all astrocytoma grades that were treated with RT (29). In France, the biopsy rate for glioblastoma was 44% in the year 2004 (7), and now it decreases. For the years 2004 to 2008, the biopsy rate was 38%.
Current applications and perspectives
Epidemiological data from the FBTDB already helped to build two ongoing French Hospital Clinical Research Programs (PHRCs) (one randomized multicenter phase II trial for patients with de novo unresectable glioblastoma, and one national, prospective phase II study for adult patients with medulloblastoma). The FBTDB also helped to identify and recruit patients for two other ongoing “PHRCs” (one for children with craniopharyngioma, and one for adult patients with intracranial ependymoma). Other specific projects are in progress (eg, oncological management and survival for all French glioblastoma patients newly diagnosed and histologically confirmed in 2008 in all French territory; histologically confirmed grade II glioma distribution in all French territory).
To contribute to a better completeness of reported cases, a second source for recording histologically confirmed PCNST is in progress. In agreement with the French Society of Neuropathology (SFNP), a comprehensive annual listing of all cases analyzed by each pathology lab will be sent securely to the RTH. A clinical research technician will track the missing listings, verify the registered cases, complete the database and check discordant cases with each lab. Then, the clinical research technician will complete the main clinical data for cases not registered yet, by contacting the relevant department of neurosurgery. The FBTDB recently received grants from the French cancer institute [Institut National du Cancer (INCa)] to analyze and compare oncological management and survival between the different French areas.
Apart from some specific cases, the causes of PCNST are unknown 8, 26, 34. Epidemiological studies of PCNST have examined many risk factors over the past several decades; however, there are few consistent findings. The inconclusive results may be caused by small sample sizes in individual studies and differences between studies in patients, tumor types and methods of classification. That is why the FBTDB would like to collect a huge number of cases, and study each histological type and subtype separately, and then participate in international studies with, for example, the BTEC and the International Agency for Research on Cancer (IARC).
Virtual tumor bank is one of the major interests of such database. Recording cryopreservation of samples, to our knowledge, has not been previously reported and is original in our study. More than 6000 identified PCNSTs are cryopreserved. For these cryopreserved tumors, we know the histological diagnosis, and the main clinical and radiological features. This represents the first virtual tumor bank of PCNST in Europe, and holds great potential for future biological and clinical investigations. Many specific retrospective or prospective studies will use the FBTDB to identify patients and get initial data. Collaborative studies have already been initiated.
CONCLUSION
This database or databank dedicated to PCNST contains detailed data on clinical, histological and other characteristics, such as availability of cryopreserved specimens that are not available in other European registries. Thus, it is a valuable resource that can be used for planning future epidemiological and clinical research.
ACKNOWLEDGMENTS
The authors wish to acknowledge all the doctors and professors who helped and completed the cards for the record of PCNSTs in France: Abbey Toby A. (Clichy), Adle‐Biassette H. (Paris), Adreux (Brest), Albagnac V. (Limoges), Algros M.P. (Besancon), Amat C. (Saint Pierre), Ansart F. (Besancon), Arbez‐Gindre F. (Besancon), Arbion F. (Tours), Arrivets P. (Saint Pierre), Aubriot Lorton M.H. (Dijon), Auvigne I. (Toulouse), Averous G. (Strasbourg), Badsi A. (Perpignan), Baldet P. (Montpellier), Barbey C. (Tours), Bazille C. (Paris), Bedgedjian I. (Besancon), Benabidallah S. (Bron), Benali A. (Orléans), Bergemer Fouquet A.M. (Tours), Bertocchi C. (Paris), Beuvon F. (Paris), Billotet C. (Perpignan), Blechet C. (Tours), Bondoin (Brest), Bonneau C. (Orleans), Bonyhay G. (Clichy), Bordier (Saint Pierre), Borrelly C. (Montpellier), Boudjadi S. (Reims), Bouvier C. (Marseille), Branquet D. (Clamart), Bressenot A. (Nancy), Broche C. (Nîmes), Brouchet A. (Toulouse), Brousset P. (Toulouse), Bruniau A. (Amiens), Cahn V. (Reims), Calvet P. (Toulon), Camo J. (Perpignan), Camparo P. (Paris), Carloz E. (Toulon), Cassagnau E. (Nantes), Cathelineau D. (Lille), Caulet S. (Rennes), Caveriviere P. (Toulouse), Cazals‐Hatem D. (Clichy), Charlotte F. (Paris), Chapon F. (Caen), Charpin C. (Marseille), Chatelain D. (Amiens), Chenard M.P. (Strasbourg), Chretien F. (Creteil), Clairotte A. (Besancon), Colombat M. (Clichy), Conan V. (Brest), Concha (Brest), Costa K. (Perpignan), Costes V. (Montpellier), Costes‐Charlet N. (Clermont‐Ferrand), Coulon A. (Poitiers), Couvelard A. (Clichy), Cremades (Paris), Croue A. (Angers), Cruel T. (Pringy), Danjoux M. (Toulouse), Daumas‐Duport C. (Paris), Degano‐Valmarx S. (Toulouse), Delage Corre M. (Limoges), Delattre C. (Lille), Delisle M.B. (Toulouse), Delsol M. (Toulouse), Deschamps L. (Clichy), Diebold M.D. (Reims), Donsbeck A.V. (Chambery), Dosda A. (Clichy), Duga I. (Toulouse), Dumollard J.M. (Saint Etienne), Durand L. (Montpellier), Duval H. (Rennes), Eimer S. (Bordeaux), Etchandy M.P. (Pau), Eyremandi (Pau), Fallet C. (Paris), Faraut (Nîmes), Felce Dachez M. (Clichy), Felix S. (Besancon), Fernandez C. (Marseille), Fetissof F. (Tours), Feutry C. (Pringy), Figarella‐Branger D. (Marseille), Figuccio M. (Toulon), Fornes P. (Reims), Fouet B. (Toulon), Fregeville M. (Saint Pierre), Fromont G. (Poitiers), Gaspard C. (Montpellier), Gay G. (Pau), Gontier M.F. (Amiens), Goujon J.M. (Poitiers), Gray F. (Paris), Grignon Y. (Nancy), Gros (Paris), Guillou (Reims), Guymar S. (Paris), Gyenes C. (Dijon), Hassoun J. (Marseille), Haudebourg J. (Nice), Heitzmann A. (Orleans), Henin D. (Paris), Hennequin V. (Nancy), Heymann M.F. (Nantes), Istier L. (Pringy), Jaubert F. (Paris), Jouan H. (Rennes), Jourdan F. (Tours), Jouvet A. (Bron), Justrabo E. (Dijon), Kaci R. (Paris), Kantelip B. (Besancon), Kemeny J.L. (Clermont‐Ferrand), Kerdraon O. (Lille), Kerdraon R. (Orleans), Kermanac H.P. (Pringy), Khaddage A. (Saint Etienne), Kleinclaus I. (Colmar), Kopp N. (Bron), Krzisch S. (Colmar), Kujas M. (Paris), Labrousse F. (Limoges), Lacroix C. (Le Kremlin Bicetre), Lamant L. (Toulouse), Lannes B. (Strasbourg), Laquerriere A. (Rouen), Laurent C. (Toulouse), Le Gall F. (Rennes), Le Houcq M. (Saint Pierre), Lechapt E. (Caen), Leclair F. (Nantes), Leduc (Lille), Leger F. (Bordeaux), Lerintiu F. (Colmar), Levillain P. (Poitiers), Lhermitte B. (Saint Pierre), Lhermitte B. (Strasbourg), Loussouarn D. (Nantes), Maitre F. (Orleans), Majek‐Zakine E. (Reims), Manent A.M. (Pau), Maran A. (Montpellier), Marcon N. (Nancy), Mareel A. (Pointe A Pitre), Marie B. (Nancy), Martin L. (Dijon), Maues De Paula A. (Marseille), Maurage C.A. (Lille), Mazerolles C. (Toulouse), Mergey E. (Pau), Meyronnet D. (Bron), Michalak S. (Angers), Michenet P. (Orleans), Michiels J.F. (Nice), Milin S. (Poitiers), Miquel C. (Paris), Mohr M. (Strasbourg), Mohra (Clermont‐Ferrand), Mokhtari K. (Paris), Monpon C. (Toulouse), Morand Dusserre I. (Pringy), Moreau A. (Nantes), Moreau M. (Toulouse), Moreno S. (Rouen), Musso Rigal C. (Toulouse), Neuville A. (Strasbourg), Oksman A. (Toulouse), Oukabli M. (Tours), Palasse J. (Toulouse), Parent M. (Douai), Patey M. (Reims), Pellissier J.F. (Marseille), Peoc'h M. (Saint Etienne), Philippe A. (Tours), Pialat J. (Limonest), Pluot M. (Reims), Polivka M. (Paris), Pommepuy I. (Limoges), Ponnelle T. (Dijon), Pradere Labat M. (Toulouse), Pradere M. (Toulouse), Quintana M. (Nimes), Quintin I. (Brest), Quintyn M.L. (Toulouse), Ranfaing E. (Besancon), Raynaud P. (Montpellier), Reis Borges R. (Nîmes), Renjard L. (Tours), Reyre J. (Toulouse), Richard S. (Le Kremlin Bicetre), Rigau V. (Montpellier), Ringenbach F. (Besancon), Rouquette I. (Toulouse), Rousseau A. (Nancy), Rousseau A. (Paris), Rousselet M.C. (Angers), Rousselot C. (Tours), Ruchoux M.M. (Lille), Sabourin J.C. (Rouen), Saïkali S. (Rennes), Saingra B. (Montpellier), Saint‐ Andre J.P. (Angers), Saint Blancard P. (Clamart), Saint Pierre G. (Bron), Saint‐Paul M.C. (Nice), Sarrouy J. (Pointe A Pitre), Savin C. (Nîmes), Sawan B. (Bordeaux), Schill H. (Montargis), Selves J. (Toulouse), Seurat P. (Saint Pierre), Sevestre H. (Amiens), Sorbara R. (Toulouse), Soulard P. (Paris), Soulard R. (Toulon), Souraud J.B. (Toulon), Straub P. (Colmar), Streichenberger N. (Bron), Talagas M. (Brest), Terrier P. (Toulon), Toquet C. (Nantes), Tortel M.C. (Colmar), Trouillas J. (Tours), Tubiana A. (Paris), Uro‐Coste E. (Toulouse), Valmary S. (Toulouse), Vandenbos F. (Nice), Varlet P. (Paris), Vasiljevic A. (Marseille), Vaunois B. (Saint Etienne), Verdier D. (Tours), Veresezon L. (Rouen), Vic P. (Montpellier), Viennet G. (Besancon), Vignaud J.M. (Nancy), Villa C. (Paris), Vital A. (Bordeaux), Warter A. (Fort De France), Weinbreck N. (Nancy), Yacoub M. (Poitiers), Yaziji N. (Reims), Yriarte‐Laurent M.C. (Toulouse), Yver M. (Poitiers).
Abi Lahoud G. (Paris), Achim V. (Clermont‐Ferrand), Adetchessi T. (Marseille), Aesch B. (Tours), Agha M. (Dijon), Aghakhani N. (Le Kremlin‐Bicetre), Akkhabar (Angers), Al Hallak R. (Lyon), Aldea S. (Paris), Alfieri A. (Limoges), Ali Benali M. (Limoges), Aliamus A. (Saint Pierre), Allano V. (Brest), Allaoui M. (Lille), Alliez B. (Marseille), Alliez J.R. (Marseille), Amlashi S.F.A. (Rennes), Aouad N. (Toulon), Arthuis F. (Paris), Assaker R. (Lille), Atta (Rennes), Auque J. (Nancy), Autricque A. (Pau), Ayache D. (Paris), Barat J.L. (Marseille), Baroncini M. (Lille), Barrey C. (Lyon), Bataille B. (Poitiers), Bauchet L. (Montpellier), Baussart (Le Kremlin‐Bicetre), Bayram M. (Rouen), Bazin A. (Reims), Beauchesne P. (Nancy), Beaudic Y. (Besancon), Beaurain J. (Dijon), Bedou G. (Perpignan), Belliard H. (Lyon), Bellow F. (Rouen), Beltechi R. (Strasbourg), Ben Hamouda H. (Saint Etienne), Ben Ismaïl M. (Tours), Ben Yahia M. (Rennes), Benezech J. (Montpellier), Benhima H. (Marseille), Berger C. (Saint Etienne), Bernard C. (Toulon), Bernard M.H. (Reims), Berthelot J.L. (Clichy), Besson G. (Brest), Billant (Toulon), Billon‐Grand R. (Besancon), Bitar A. (Paris), Bizette C. (Colmar), Blanc J.L. (Poitiers), Blanquet A. (Montpellier), Blond S. (Lille), Blondet (Clamart), Boch A‐L. (Paris), Boetto S. (Toulouse), Boissonnet H. (Paris), Bord E. (Nantes), Borha A. (Caen), Bouali I. (Colmar), Bouazza S. (Paris), Bougeard R. (Villeurbanne), Bouillot P. (Nimes), Bourgeois P. (Lille), Bousigue J.Y. (Cornebarrieu), Bousquet C. (Perpignan), Bousquet O. (Dijon), Bousquet P. (Toulouse), Boyer P. (Strasbourg), Brassier G. (Rennes), Bresson D. (Paris), Bret P. (Lyon), Bruneau M. (Paris), Brunon J. (Saint Etienne), Buffenoir K. (Poitiers), Cabal P. (Pau), Caille J. (M. (Bordeaux), Caire F. (Limoges), Capelle L. (Paris), Cardoso M. (Colmar), Carpentier A. (Paris), Cesari J.B. (Montpellier), Chabane A. (Clermont‐Ferrand), Champeaux K. (Bordeaux), Chaynes P. (Toulouse), Chays A. (Reims), Chazal J. (Clermont‐Ferrand), Chibbaro S. (Paris), Chinot O. (Marseille), Chobaut J.C. (Besancon), Choplain J. (Brest), Choukri M. (Le Kremlin‐Bicetre), Cioloca C. (Paris), Civit T. (Nancy), Clemenceau S. (Paris), Colnat S. (Nancy), Comoy J. (Saint Pierre), Cornelius J. (Paris), Cornu P. (Paris), Coubes P. (Montpellier), Coulbois S. (Nancy), Crampette L. (Montpellier), Cristini A. (Lyon), Cuny E. (Bordeaux), Cuttaree H. (Paris), Czorny A. (Besancon), Dagain A. (Paris), Dahman (Rennes), Dam Hieu P. (Brest), Dandine J.B. (Toulouse), Darrouzet V. (Bordeaux), Dautheribes M. (Bordeaux), David P. (Le Kremlin‐Bicetre), De Germay B. (Saint Jean), De Soultrait F. (Clamart), Debono B. (Rouen), Debono B. (Cornebarrieu), Decq P. (Creteil), Delaretti (Lille), Delhaye M. (Angers), Delion (Angers), Delmas J.M. (Paris), Delsanti C. (Marseille), Derlon J.M. (Caen), Derrey S. (Rouen), Deruty R. (Lyon), Desenclos C. (Amiens), Desgeorges M. (Paris), Desplat A. (Pau), Destandau J. (Bordeaux), Destrieux C. (Tours), Devaux B. (Paris), Dezamis E. (Paris), Dhellemmes P. (Lille), Di Rocco F. (Paris), Di Tommaso L. (Besancon), Diabira S. (Rennes), Diaz A. (Saint Pierre), Dimitriu C. (Strasbourg), Djindjian M. (Creteil), Do L. (Pointe A Pitre), Doe K. (Saint Pierre), Dorfmuller G. (Paris), Dorwling‐Carter D. (Orleans), Dran G. (Montpellier), Dubois G. (Saint Jean), Ducolombier A. (Trappes), Duffau H. (Montpellier), Dufour T. (Orleans), Duhem R. (Lille), Dulou R. (Paris), Dumas B. (Saint Etienne), Duntze (Reims), Dupard T. (Lille), Duplessis (Cornebarrieu), Durand A. (Lyon), Durandeau A. (Bordeaux), Dutertre G. (Paris), Duthel R. (Saint Etienne), El Fertit H. (Montpellier), Emery E. (Caen), Espagno C. (Cornebarrieu), Esposito P. (Strasbourg), Fabre T. (Bordeaux), Faillot T. (Clichy), Farah W. (Dijon), Farizon F. (Saint Etienne), Faure A. (Nantes), Faure P. (Limoges), Fesselet J. (Toulon), Fichten A. (Amiens), Fischer D. (Strasbourg), Fono S. (Toulouse), Fontaine D. (Nice), Fotso M.J. (Saint Etienne), Fournier D. (Angers), Francois P. (Tours), Frank B. (Argonay), Freger P. (Rouen), Freppel S. (Nancy), Froelich S. (Strasbourg), Fuentes J.M. (Montpellier), Fuentes S. (Marseille), Gadan R. (Caen), Garrel R. (Montpellier), George B. (Paris), Giacomelli R. (Colmar), Gigaud M. (Toulouse), Gil Robles S. (Montpellier), Gimbert E. (Bordeaux), Goasguen O. (Paris), Godard J. (Besancon), Gomez A. (Marseille), Gosset (Amiens), Goutagny S. (Clichy), Gras R. (Marseille), Grayeli B. (Clichy), Graziani N. (Marseille), Grellier P. (Nice), Grisoli F. (Marseille), Guarnieri J. (Caen), Guegan Y. (Rennes), Guenot M. (Lyon), Guerrier B. (Montpellier), Gueye E. (Limoges), Guinguene C. (Lyon), Guy G. (Angers), Guyotat J. (Lyon), Haddad E. (Lille), Haegelen C. (Rennes), Hallacq M. (Lyon), Hallacq P. (Limoges), Hamcha (Poitiers), Hamdi S. (Paris), Hamlat A. (Rennes), Hansen F. (Caen), Hatem O. (Saint Etienne), Hattou M. (Creteil), Hayek G. (Angers), Henry (Brest), Heyman D. (Pau), Hladky J.P. (Nimes), Huot J.C. (Pau), Iakovlev G. (Clichy), Ibrahim R. (Angers), Irthum B. (Clermont‐Ferrand), Ischac R. (Fort De France), Jacquet G. (Besancon), Jan M. (Tours), Jarraya B. (Creteil), Jouanneau E. (Lyon), Joud A. (Nancy), Joulin (Brest), Kaczmarek D. (Saint Etienne), Kaddoum H. (Pointe A Pitre), Kalamarides M. (Clichy), Karachi C. (Paris), Katrangi H. (Besancon), Kaya J.M. (Marseille), Kehrli P. (Strasbourg), Keravel Y. (Creteil), Khalil T. (Marseille), Khouri K. (Montpellier), Khouri S. (Caen), Klein O. (Nancy), Koubaïssi W. (Angers), Kuzeawu A. (Colmar), Lacerda P. (Caen), Lagarrigue J. (Toulouse), Langlois O. (Rouen), Lapierre F. (Poitiers), Lapras C. (Argonay), Le Fay (Amiens), Le Franc (Amiens), Le Guerinel C. (Creteil), Le Nen (Brest), Legars D. (Amiens), Lejeune J.P. (Lille), Lemaire J.J. (Clermont‐Ferrand), Lena G. (Marseille), Lepeintre (Le Kremlin‐Bicetre), Leriche B. (Saint Pierre), Lescure J.P. (Cornebarrieu), Leston J.M. (Creteil), Leveque (Marseille), Liguoro D. (Bordeaux), Linne M. (Lyon), Lioret E. (Tours), Lisii D. (Lille), Listrat A. (Paris), Litre F. (Reims), Litrico S. (Nice), Loiseau H. (Bordeaux), Lonjon M. (Nice), Lonjon N. (Montpellier), Lopes M. (Saint Pierre), Lot G. (Paris), Louis E. (Lille), Louveau A. (Aix Les Bains), Lubrano V. (Toulouse), Lungu G. (Colmar), Madonnet E. (Paris), Maghreu (Caen), Magro E. (Brest), Mahla K. (Villeurbanne), Maillard A. (Perpignan), Maitrot D. (Strasbourg), Malca S. (Marseille), Mandat (Creteil), Manisor M. (Limoges), Mansour (Angers), Manzo N. (Fort De France), Marchal J.C. (Nancy), Marchal T. (Creteil), Marie J.P. (Rouen), Marnet D. (Reims), Martin S. (Nantes), Mascott (Toulouse), Mazon A. (Rennes), Memia Zolo D. (Fort De France), Menegalli D. (Nantes), Menei P. (Angers), Mercier P. (Angers), Merlet Chicoine I. (Poitiers), Merlot I. (Nancy), Mertens P. (Lyon), Metellus P. (Marseille), Mineo F. (Lille), Mireau E. (Paris), Monteil P. (Bordeaux), Morandi. (Rennes), Morar S. (Le Kremlin‐Bicetre), Moreau (Caen), Moreau J.J. (Limoges), Morel C. (Villeurbanne), Mortada J. (Colmar), Mostofi K. (Fort De France), Mottolese C. (Lyon), Moubarak K. (Creteil), Mourier L. (Dijon), Muckensturm B. (Orleans), Nader E. (Angers), Nahas F. (Pointe A Pitre), Namaki H. (Perpignan), Nataf F. (Paris), Navarro S. (Paris), Nguyen J.P. (Nantes), Njee Bugha T. (Marseille), Njee T. (Pointe A Pitre), Nogues L. (Saint Pierre), Noudel R. (Reims), Nouet A. (Paris), Nseir (Nancy), Nseir R. (Creteil), Nuti C. (Saint Etienne), Orabi M. (Paris), Orenstein D. (Colmar), Page P. (Paris), Palfi S. (Creteil), Pallud J. (Paris), Pampin S. (Rennes), Paquis P. (Nice), Paradot G. (Le Kremlin‐Bicetre), Parker F. (Le Kremlin‐Bicetre), Pasqualini E. (Rennes), Pech Gourg G. (Marseille), Pejeredou (Paris), Pelissou‐Guyotat I. (Lyon), Pellet W.J. (Marseille), Peltier J. (Amiens), Pencalet P. (Paris), Penchet G. (Bordeaux), Peragut J.C. (Marseille), Perie (Paris), Pernot P (Clamart), Perrin G. (Lyon), Person H. (Brest), Peruzzi P. (Reims), Pierre‐Kahn A. (Paris), Pinaudeau M. (Perpignan), Pinelli C. (Nancy), Plas J.Y. (Cornebarrieu), Polo G. (Lyon), Poncet J.L. (Paris), Porhiel V. (Perpignan), Postelnicu A. (Caen), Pouit B. (Paris), Prades (Saint Etienne), Privat J.M. (Montpellier), Proust F. (Rouen), Puget S. (Paris), Rabehenoina C. (Rouen), Rabhi M. (Clermont‐Ferrand), Ragragui O. (Lille), Raoul S. (Nantes), Rasendrarijao D. (Nice), Redondo A. (Clichy), Regis J. (Marseille), Remond J. (Villeurbanne), Reynier Y. (Marseille), Reyns N. (Lille), Ricci Franchi A.C. (Lyon), Richet A. (Fort De France), Riem T. (Bordeaux), Riem T. (Nantes), Riffaud L. (Rennes), Rigoard P. (Poitiers), Robert G. (Paris), Roche P.H. (Marseille), Rodriguez M.A. (Montpellier), Rodriguez V. (Brest), Roualdes G. (Poitiers), Roualdes V. (Nantes), Rougier A. (Bordeaux), Roujeau (Paris), Roujeau T. (Paris), Rousseau P. (Reims), Roux F. (Toulouse), Roux F.X. (Paris), Sabatier J. (Toulouse), Sabatier P. (Montpellier), Sabbah M. (Montpellier), Sacko O. (Toulouse), Sainte‐Rose C. (Paris), Sakka L. (Clermont‐Ferrand), Salmon B. (Saint Jean), San Galli F. (Bordeaux), Sautreaux J.L. (Dijon), Scarone P. (Paris), Scavarda D. (Marseille), Scherpereel B. (Reims), Schmidt E. (Toulouse), Segnarbieux F. (Montpellier), Seguin (Saint Etienne), Seigneuret E. (Rennes), Seizeur R. (Brest), Sichez J.P. (Paris), Sid Hamed S. (Brest), Silhouette B. (Paris), Simbert (Dijon), Simon A. (Brest), Simon E. (Lyon), Sinardet D. (Clermont‐Ferrand), Sindou M. (Lyon), Sleiman M. (Lille), Sol J.C. (Toulouse), Sorin A. (Paris), Soumare O. (Marseille), Srour A. (Paris), Stecken J. (Orleans), Sterkers O. (Clichy), Stilhart B. (Colmar), Szathmari A. (Lyon), Tadie M. (Le Kremlin‐Bicetre), Taha S. (Saint Pierre), Tarek A. (Marseille), Ternier J. (Marseille), Thines L. (Lille), Thomassin J.M. (Marseille), Tobenas Dujardin A.C. (Rouen), Tonnelle Duhem V. (Lille), Tourneux (Clermont‐Ferrand), Tourneux H. (Saint Etienne), Toussaint P. (Amiens), Touta A. (Marseille), Touzet G. (Lille), Travers N. (Tours), Travers N. (Lille), Tremoulet M. (Toulouse), Turak B. (Paris), Turner F. (Marseille), Valery C. (Paris), Vallee B. (Lyon), Van Effenterre R. (Paris), Vassal F. (Saint Etienne), Velut S. (Tours), Vidal (Bordeaux), Vidal J. (Limoges), Vignes J.R. (Bordeaux), Vincentelli F. (Marseille), Vinchon M. (Lille), Voirin J. (Nancy), Voirin J. (Strasbourg), Von Langsdorf D. (Nice), Vongsouthi (Montpellier), Wager M. (Poitiers), Zaïri F. (Lille), Zanaret M. (Marseille), Zemmoura I. (Tours), Zerah M. (Paris).
This work was conducted with the financial support of grants from the Ligue Nationale Contre le Cancer (France), INCa, Schering‐Plough Laboratory, Roche Laboratory, ANOCEF, SFNC, Associations pour la Recherche sur les Tumeurs Cérébrales (ARTC and ARTC Sud) (France), Département de l'Hérault (France), Rotary Club (AGLY), Archimedes Pharma Laboratory, Sophysa Laboratory and Groupe de Neuro‐Oncologie du Languedoc Roussillon (France).
REFERENCES
- 1. ADICAP, Association pour le Développement de l'Informatique en Cytologie et en Anatomie Pathologiques (2003) Database online. Edition 2003, version 5. Available at: http://www.adicap.asso.fr/THESAURUS/Adicap_v5‐03pdf (accessed 24 May 2011).
- 2. Arora RS, Alston RD, Eden TOB, Estlin EJ, Moran A, Geraci M, Birch JM (2010) Are reported increases in incidence of primary CNS tumours real? An analysis of longitudinal trends in England, 1979–2003. Eur J Cancer 46:1607–1616. [DOI] [PubMed] [Google Scholar]
- 3. Bauchet L, Capelle L, Stilhart B, Guyotat J, Pinelli C, Roches P et al (2004) French neurosurgical practice in neuro‐oncology (national survey—part I). Neurochirurgie 50:540–547. [DOI] [PubMed] [Google Scholar]
- 4. Bauchet L, Rigau V, Mathieu‐Daudé H, Figarella‐Branger D, Hugues D, Palusseau L et al (2007) French brain tumor data bank: methodology and first results on 10,000 cases. J Neurooncol 84:189–199. [DOI] [PubMed] [Google Scholar]
- 5. Bauchet L, Rigau V, Mathieu‐Daudé H, Figarella Branger D, Fabbro P, Taillandier L, Duffau H (2008) Towards an European brain tumor data bank. Neuro-Oncol 10:1134. [abstract]. [Google Scholar]
- 6. Bauchet L, Rigau V, Mathieu‐Daudé H, Fabbro‐Peray P, Palenzuela G, Figarella‐Branger D et al (2009) Clinical epidemiology for childhood primary central nervous system tumors. J Neurooncol 92:87–98. [DOI] [PubMed] [Google Scholar]
- 7. Bauchet L, Mathieu‐Daudé H, Fabbro‐Peray P, Rigau V, Fabbro M, Chinot O et al (2010) Oncological patterns of care and outcome for 952 patients with newly diagnosed glioblastoma in 2004. Neuro-Oncol doi: 10.1093/neuonc/noq030. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bondy ML, Scheurer ME, Malmer B, Barnholtz‐Sloan JS, Davis FG, Il'yasova D et al (2008) Brain tumor epidemiology: consensus from the Brain Tumor Epidemiology Consortium. Cancer 113(Suppl. 7):1953–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Canadian Cancer Registry (2005) Cancer incidence in Canada. Available at: http/www.statcan.ca/bsolc/english/bsolc?catno=;84‐601‐X (accessed 24 May 2011).
- 10. Cancer Registry of Norway (2007) Cancer in Norway 2006—cancer incidence, mortality, survival and prevalence in Norway. Available at: http://www.kreftregisteret.no/General/Publications/Cancer‐in‐Norway/Cancer‐in‐Norway‐2006/ (accessed 20 January 2009).
- 11. CBTRUS (2009) 2009–2010 CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in eighteen states in 2002–2006. Published by the Central Brain Tumor Registry of the United States, Hinsdale, IL. Available at website: http://www.cbtrus.org (accessed 24 May 2011).
- 12. CBTRUS (2010) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2004–2006. Source: Central Brain Tumor Registry of the United States, Hinsdale, IL. Available at website: http://www.cbtrus.org (accessed 24 May 2011).
- 13. Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M et al (2007) Cancer Incidence in Five Continents, Volume IX. IARC: Lyon, France. [Google Scholar]
- 14. Daumas‐Duport C, Beuvon F, Varlet P, Fallet‐Bianco C (2000) Gliomas: WHO and Sainte‐Anne Hospital classifications. Ann Pathol 20:413–428. [PubMed] [Google Scholar]
- 15. Davis FG, Malmer BS, Aldape K, Barnholtz‐Sloan JS, Bondy ML, Brännström T et al (2008) Issues of diagnostic review in brain tumor studies: from the Brain Tumor Epidemiology Consortium. Cancer Epidemiol Biomarkers Prev 17:484–489. [DOI] [PubMed] [Google Scholar]
- 16. DeAngelis LM (2001) Brain tumors. N Engl J Med 344:114–123. [DOI] [PubMed] [Google Scholar]
- 17. Elia‐Pasquet S, Provost D, Jaffre A, Loiseau H, Vital A, Kantor G et al (2004) Incidence of central nervous system tumors in Gironde, France. Neuroepidemiology 23:110–117. [DOI] [PubMed] [Google Scholar]
- 18. ENCR, European Network of Cancer Registries (1998) Recommendations for coding Tumours of the Brain and Central Nervous System. Available at: http://www.encr.com.frDevelopment and Recommendations on Cancer Registration and Standards/Working Groups: Tumours of the Brain and Central Nervous System crossed PDF link: English. Distributed in 1998 (accessed 24 May 2011).
- 19. Filippini G, Falcone C, Boiardi A, Broggi G, Bruzzone MG, Caldiroli D et al (2008) Prognostic factors for survival in 676 consecutive patients with newly diagnosed primary glioblastoma. Neuro-Oncol 10:79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fleury A, Menegoz F, Grosclaude P, Daures JP, Henry‐Amar M, Raverdy N et al (1997) Descriptive epidemiology of cerebral gliomas in France. Cancer 79:1195–1202. [DOI] [PubMed] [Google Scholar]
- 21. Fontaine D, Bauchet L, Capelle L, Club de Neuro Oncologie de la Société Française de Neurochirurgie (2005) French neurosurgical practice in neurooncology (national survey—part II). Census of current research protocols on brain tumors in France. Neurochirurgie 51:136–141. [DOI] [PubMed] [Google Scholar]
- 22. Hartmann C, Mueller W, von Deimling A (2004) Pathology and molecular genetics of oligodendroglial tumors. J Mol Med 82:638–655. [DOI] [PubMed] [Google Scholar]
- 23. Klaeboe L, Lonn S, Scheie D, Auvinen A, Christensen HC, Feychting M et al (2005) Incidence of intracranial meningiomas in Denmark, Finland, Norway and Sweden, 1968–1997. Int J Cancer 117:996–1001. [DOI] [PubMed] [Google Scholar]
- 24. Kleihues P, Cavenee WK (2000) World Health Classification of Tumors. Tumors of the Nervous System. Pathology and Genetics. IARC Scientific Publications: Lyon, France. [Google Scholar]
- 25. Laws ER, Parney IF, Huang W, Anderson F, Morris AM, Asher A et al (2003) Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the Glioma Outcomes Project. J Neurosurg 99:467–473. [DOI] [PubMed] [Google Scholar]
- 26. Loiseau H, Huchet A, Rué M, Cowppli‐Bony A, Baldi I (2009) Epidemiology of primary brain tumor. Rev Neurol (Paris) 165:650–670. [DOI] [PubMed] [Google Scholar]
- 27. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (2007) WHO Classification of Tumours of the Central Nervous System. IARC: Lyon, France. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Magrini SM, Ricardi U, Santoni R, Krengli M, Lupattelli M, Cafaro I et al (2006) Patterns of practice and survival in a retrospective analysis of 1722 adult astrocytoma patients treated between 1985 and 2001 in 12 Italian radiation oncology centers. Int J Radiat Oncol Biol Phys 65:788–799. [DOI] [PubMed] [Google Scholar]
- 30. McCarthy BJ, Surawicz T, Bruner JM, Kruchko C, Davis F (2002) Consensus conference on brain tumor definition for registration. Neuro-Oncol 4:134–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McCarthy BJ, Kruchko C, Central Brain Tumor Registry of United States (2005) Consensus conference on cancer registration of brain and central nervous system tumors. Neuro-Oncol 7:196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ménégoz F, Martin E, Danzon A, Mathieu‐Daudé H, Guizard AV, Macé‐Lesec'h J et al (2006) Incidence and mortality of central nervous system tumors in France: trends over the period 1978–2000 and influence of registration practices on results. Rev Epidemiol Sante Publique 54:399–406. [DOI] [PubMed] [Google Scholar]
- 33. Micheli A, Ciampichini R, Oberaigner W, Ciccolallo L, de Vries E, Izarzugaza I et al (2009) EUROCARE Working Group. The advantage of women in cancer survival: an analysis of EUROCARE‐4 data. Eur J Cancer 45:1017–1027. [DOI] [PubMed] [Google Scholar]
- 34. Ohgaki H, Kleihues P (2005) Epidemiology and etiology of gliomas. Acta Neuropathol 109:93–108. [DOI] [PubMed] [Google Scholar]
- 35. Propp JM, McCarthy BJ, Davis FG, Preston‐Martin S (2006) Descriptive epidemiology of vestibular schwannomas. Neuro-Oncol l8:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rigau V, Mathieu‐Daude H, Figarella‐Branger D, Tretarre B, Bauchet F, Fabbro M et al (2010) French Brain Tumor Data Bank (FBTDB): main results on 23,648 cases. 2010 ASCO Annual Meeting, 4–8 Juin 2010. J Clin Oncol 28: (Suppl.; abstr e12536). Available at: http://www.asco.org/ASCOv2/Meetings/Abstracts?&vmview=;abst_detail_view&confID=;74&abstractID=;44003 (accessed 24 May 2011). [Google Scholar]
- 37. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. [DOI] [PubMed] [Google Scholar]
- 38. Surveillance Epidemiology and End Results (SEER) Table 31.1: a comparison of benign/borderline and malignant brain tumors counts, percents and age‐adjusted incidence ratesa by WHO histology grouping, 2004–2007. Available at: http://seer.cancer.gov/csr/1975_2007/results_merged/sect_31_benign_brain.pdf (accessed 24 May 2011).
- 39. Swedish Cancer Registry (2007) Cancer incidence in Sweden 2006. Available at: http://www.socialstyrelsen.se/Statistik/statistik_amne/Cancer (accessed 20 January 2009).
- 40. Westphal M, Hilt DC, Bortey E, Delavault P, Olivares R, Warnke PC et al (2003) A phase 3 trial of local chemotherapy with biodegradable carmustine (BCNU) wafers (Gliadel wafers) in patients with primary malignant glioma. Neuro-Oncol 5:79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wöhrer A, Waldhör T, Heinzl H, Hackl M, Feichtinger J, Gruber‐Mösenbacher U et al (2009) The Austrian Brain Tumour Registry: a cooperative way to establish a population‐based brain tumour registry. J Neurooncol 95:401–411. [DOI] [PubMed] [Google Scholar]
- 42. Wrensch M, Minn Y, Chew T, Bondy M, Berger MS (2002) Epidemiology of primary brain tumors: current concepts and review of the literature. Neuro-Oncol 4:278–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wrensch M, Rice T, Miike R, McMillan A, Lamborn KR, Aldape K, Prados MD (2006) Diagnostic, treatment, and demographic factors influencing survival in a population‐based study of adult glioma patients in the San Francisco Bay Area. Neuro-Oncol 8:12–26. [DOI] [PMC free article] [PubMed] [Google Scholar]


