HISTORY AND PHYSICAL EXAMINATION
A 58‐ year‐old man with clinical diagnosis of phacomatosis pigmentovascularis (PPV) was admitted to our neurosurgical department with a 5‐year history of tinnitus, progressive hearing loss on the right and headaches. On physical examination, multiple melanocytic and vascular nevi (more than150) together with 20 atypical nevi, extensive port‐wine stains on the first and third divisions of the trigeminal nerve, and blue spots over his right shoulder, neck, head, ear and face were identified (Figure 3). No ocular pigmentation, increased ocular pressure or seizures were observed. On neurological evaluation, only hearing loss was found.
Figure 3.

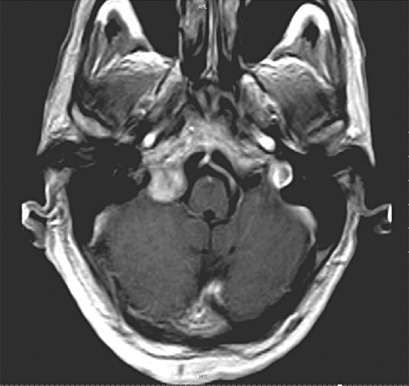
NEURORADIOLOGY
Brain MRI revealed a dumbbell‐shaped tumor located into the right jugular foramen extending towards the cerebellopontine angle (CPA) and extracranially. The lesion demonstrated a heterogeneous signal on T1 (Figure 1) and isointensity with the grey matter on T2‐weighted MR images leading to erosion and expansion of the jugular foramen. After contrast administration, homogeneous enhancement of the mass was observed (Figure 2).
Figure 1.
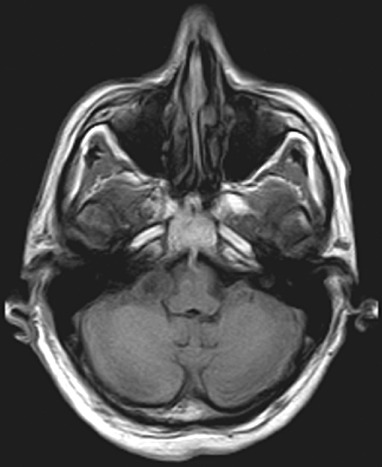
Figure 2.
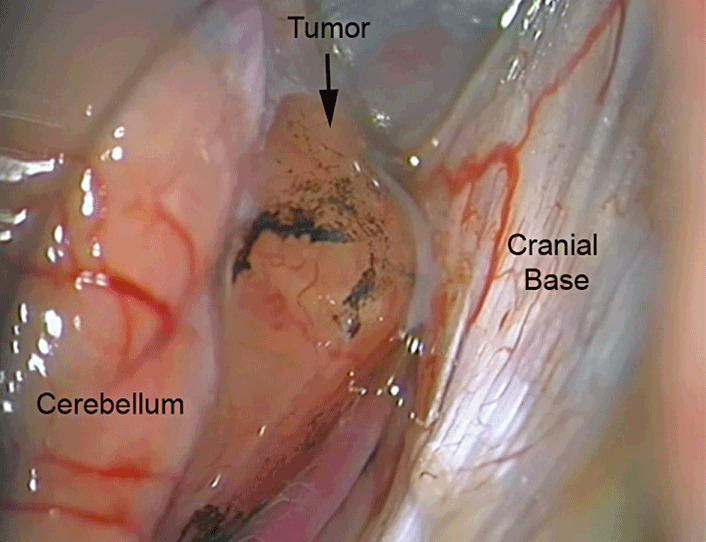
SURGICAL TREATMENT AND POSTOPERATIVE OUTCOME
A standard right retrosigmoid approach was performed while in the semi‐sitting position. After dural opening and arachnoid dissection, several pigmented spots were observed over the tumor capsule (Figure 4). The tumor was completely removed with anatomical preservation of the lower cranial nerves by using intraoperative neuromonitoring. The patient was affected by dysphonia and swallowing dysfunction due to a permanent vagus nerve neuropathy that lasted for 13 months after the surgery. There were no signs of tumor recurrence in an MRI performed 8 months postoperatively.
Figure 4.
PATHOLOGICAL FINDINGS
Multiple reddish smooth fragments measuring 1.5 cm in maximum diameter and 5 small black particles measuring 0.3 cm in maximum diameter were embedded in paraffin according to a standard protocol.
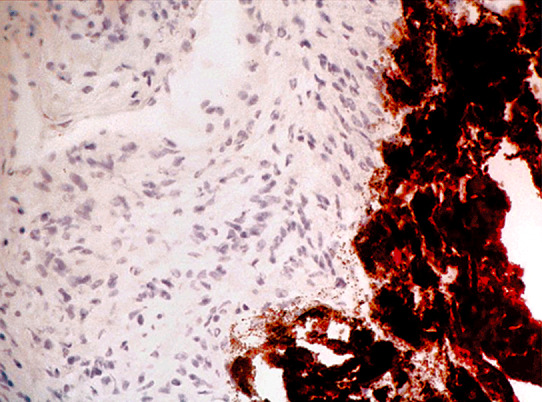
Pathological examination revealed a tumor composed by two different tissues, namely areas of compact elongated cells with nuclear palisading and less cellular areas of loose cell arrangement and lipidization. Attached to the tumor, were small fragments of a mass consisted of epithelial‐like cells of which the cytoplasm contained abundant melanin pigment granules (Figure 5). The pigmented cells were Melan‐A‐positive (Figure 6) as well as HMB45‐positive (not shown). Both tumors expressed S‐100 (not shown). The MIB‐1 labeling index was less than 1% in both tumor components.
Figure 5.
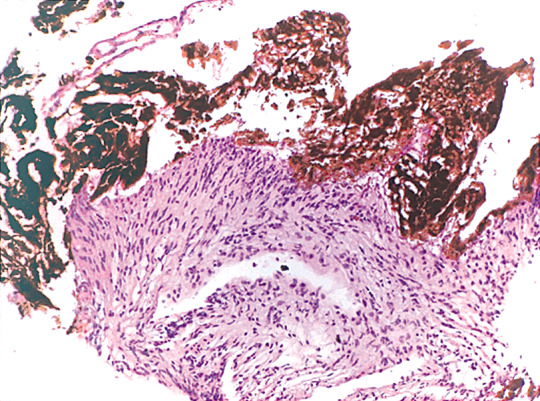
Figure 6.
What is the diagnosis?
FINAL DIAGNOSIS
Schwannoma grade I WHO of the jugular foramen associated with leptomeningeal blue nevus.
DISCUSSION
Phacomatosis pigmentovascularis (PPV) is described as a rare combination of a widespread vascular nevus (nevus flammeus—port‐wine stain) with an extensive pigmentary nevus 3, 4, 6. Happle (6) proposed a new classification of PPV into 4 types: I) cesioflammea, presenting one or more aberrant Mongolian spots and one or more port‐wine stains; II) spilorosea which is characterized by presence of rosé‐wine nevus; III) cesiomarmorata is characterized by a coexistence of aberrant Mongolian spots and cutis marmorata telangiectatica congenita and IV) includes the unclassifiable types, like the presented case.
Phacomatosis is the general term applied to describe some neurocutaneous syndromes (6). It is believed that approximately 50% of the patients affected of PPV have systemic involvement (4). Central nervous system defects, seizures, Sturge‐Weber syndrome, hydrocephalus and even plexiforme neurofibroma are some of the neurological abnormalities reported in PPV 3, 4. However, the association of PPV with an intracranial tumor, specially a pigmented tumor of the jugular foramen, has not been described to date.
The differential diagnosis of primary pigmented lesions of the leptomeninges includes primary malignant melanoma, melanotic schwannoma, meningeal melanocytoma, diffuse melanosis and cellular blue nevus. These lesions are believed to appear from the leptomeningeal melanocytes, which are originated from the neural crest elements. Melanocytes are encountered in the basal layer of the epidermis and the leptomeninges covering the surface of the basal portions of the brain and brainstem. Accordingly, these are the most common areas involved in the development of pigmented intracranial primary tumors (5). A more complete discussion can be found on the Brain Pathology website.
Interestingly, the bulk of the tumor in our case consisted of a Schwannoma WHO grade I. The pigmented cells within the small fragments of tumor corresponded to melanocytes and were attached to the schwannoma rather than part of it (Figures 7 and 8). Hence, the pigmented tumor is best described as a blue nevus‐like tumor of the leptomeninges. This is not a melanotic schwannoma since typical melanotic schwannomas consist of spindle‐shaped and epithelioid cells. In contrast, the tumor bulk in the presented case consisted of a typical schwannoma containing both Antoni A and Antoni B patterns.
Primary intracranial melanocytic tumors are occasionally associated with pigmented lesions of the skin (2). Blue nevus, nevus of Ota and neurocutaneous melanosis are skin lesions that have been described with concurrent intracranial malignant melanomas or meningeal melanocytomas 1, 2, 7, 8. This case represents an extremely rare association of a skull base schwannoma associated with a leptomeningeal blue nevus‐like tumor in a patient affected by PPV and illustrates the importance of systemic examination in PPV.
ABSTRACT
A 58‐year‐old man with clinical diagnosis of phacomatosis pigmentovascularis (PPV) experienced tinnitus and progressive hearing loss due to a jugular foramen tumor. Attached to the tumor capsule, were several pigmented spots. Pathological examination revealed a tumor composed by two different tissues, namely a Schwannoma grade I associated with a leptomeningeal blue nevus. The neuropathological aspects of this unusual association are discussed. The association of PPV with a pigmented skull base tumor has not been described to date and illustrates the importance of systemic examination in PPV.
REFERENCES
- 1. Arunkumar MJ, Ranjan A, Jacob M, Rajshekhar V (2001) Neurocutaneous melanosis: a case of primary intracranial melanoma with metastasis. Clin Oncol (R Coll Radiol) 13:52–54. [DOI] [PubMed] [Google Scholar]
- 2. Balmaceda CM, Fetell MR, O'Brien JF, Housepian CH (1993) Nevus of Ota and leptomeningeal melanocytic lesions. Neurology 43:381–386. [DOI] [PubMed] [Google Scholar]
- 3. Diociaiuti A, Guidi B, Aguilar‐Sanchez JA, Feliciani C, Capizzi R, Amerio P (2005) Phakomatosis pigmentovascularis type IIIb: A case associated with Sturge‐Weber and Klippel‐Trenaunay syndromes. J Am Acad Dermatol 53:536–539. [DOI] [PubMed] [Google Scholar]
- 4. Fernandez‐Guarino M, Boixeda P, De la Heras E, Aboin S, Garcia‐Millán C, Olasolo P (2008) Phakomatosis pigmentovascularis: Clinical findings in 15 patients and review of the literature. J Am Acad Dermatol 58:88–93. [DOI] [PubMed] [Google Scholar]
- 5. Goldgeier M, Klein LE, Klein‐Angerer S, Moellmann G, Nordlund JJ (1984)The distribution of melanocytes in the leptomeninges of the human brain. J Invest Dermatol 82:235–238. [DOI] [PubMed] [Google Scholar]
- 6. Happle R (2005) Phacomatosis pigmentovascularis: Revisited and reclassified. Arch Dermatol 141:385–388. [DOI] [PubMed] [Google Scholar]
- 7. Hartmann LC, Oliver GF, Winkelmann RK, Colby TV, Sundt TM Jr, O'Neill BP (1989) Blue nevus and nevus of Ota associated with dural melanoma. Cancer 64:182–186. [DOI] [PubMed] [Google Scholar]
- 8. Noshita N, Fujimura M, Kumabe T, Shirane R, Watanabe M, Tominaga T (2005) A Case of cellular blue naevus with Intracranial Invasion and malignant transformation. Acta Neurochir (Wien) 147:211–213. [DOI] [PubMed] [Google Scholar]


