Abstract
Background
Virtual reality (VR) computer technology creates a simulated environment, perceived as comparable to the real world, with which users can actively interact. The effectiveness of VR distraction on acute pain intensity in children is uncertain.
Objectives
To assess the effectiveness and adverse effects of virtual reality (VR) distraction interventions for children (0 to 18 years) with acute pain in any healthcare setting.
Search methods
We searched CENTRAL, MEDLINE, Embase, CINAHL, PsycINFO and four trial registries to October 2019. We also searched reference lists of eligible studies, handsearched relevant journals and contacted study authors.
Selection criteria
Randomised controlled trials (RCTs), including cross‐over and cluster‐RCTs, comparing VR distraction to no distraction, non‐VR distraction or other VR distraction.
Data collection and analysis
We used standard Cochrane methodological processes. Two reviewers assessed risk of bias and extracted data independently. The primary outcome was acute pain intensity (during procedure, and up to one hour post‐procedure). Secondary outcomes were adverse effects, child satisfaction with VR, pain‐related distress, parent anxiety, rescue analgesia and cost. We used GRADE and created 'Summary of findings' tables.
Main results
We included 17 RCTs (1008 participants aged four to 18 years) undergoing various procedures in healthcare settings. We did not pool data because the heterogeneity in population (i.e. diverse ages and developmental stages of children and their different perceptions and reactions to pain) and variations in procedural conditions (e.g. phlebotomy, burn wound dressings, physical therapy sessions), and consequent level of pain experienced, made statistical pooling of data impossible. We narratively describe results.
We judged most studies to be at unclear risk of selection bias, high risk of performance and detection bias, and high risk of bias for small sample sizes. Across all comparisons and outcomes, we downgraded the certainty of evidence to low or very low due to serious study limitations and serious or very serious indirectness. We also downgraded some of the evidence for very serious imprecision.
1: VR distraction versus no distraction
Acute pain intensity: during procedure
Self‐report: one study (42 participants) found no beneficial effect of non‐immersive VR (very low‐certainty evidence).
Observer‐report: no data.
Behavioural measurements (observer‐report): two studies, 62 participants; low‐certainty evidence. One study (n = 42) found no beneficial effect of non‐immersive VR. One study (n = 20) found a beneficial effect favouring immersive VR.
Acute pain intensity: post‐procedure
Self‐report: 10 studies, 461 participants; very low‐certainty evidence. Four studies (n = 95) found no beneficial effect of immersive and semi‐immersive or non‐immersive VR. Five studies (n = 357) found a beneficial effect favouring immersive VR. Another study (n = 9) reported less pain in the VR group.
Observer‐report: two studies (216 participants; low‐certainty evidence) found a beneficial effect of immersive VR, as reported by primary caregiver/parents or nurses. One study (n = 80) found a beneficial effect of immersive VR, as reported by researchers.
Behavioural measurements (observer‐report): one study (42 participants) found no beneficial effect of non‐immersive VR (very low‐certainty evidence).
Adverse effects: five studies, 154 participants; very low‐certainty evidence. Three studies (n = 53) reported no adverse effects. Two studies (n = 101) reported mild adverse effects (e.g. nausea) in the VR group.
2: VR distraction versus other non‐VR distraction
Acute pain intensity:during procedure
Self‐report, observer‐report and behavioural measurements (observer‐report): two studies, 106 participants:
Self‐report: one study (n = 65) found a beneficial effect favouring immersive VR and one (n = 41) found no evidence of a difference in mean pain change scores (very low‐certainty evidence).
Observer‐report: one study (n = 65) found a beneficial effect favouring immersive VR and one (n = 41) found no evidence of a difference in mean pain change scores (low‐certainty evidence).
Behavioural measurements (observer‐report): one study (n = 65) found a beneficial effect favouring immersive VR and one (n = 41) reported a difference in mean pain change scores with fewer pain behaviours in VR group (low‐certainty evidence).
Acute pain intensity: post‐procedure
Self‐report: eight studies, 575 participants; very low‐certainty evidence. Two studies (n = 146) found a beneficial effect favouring immersive VR. Two studies (n = 252) reported a between‐group difference favouring immersive VR. One study (n = 59) found no beneficial effect of immersive VR versus television and Child Life non‐VR distraction. One study (n = 18) found no beneficial effect of semi‐immersive VR. Two studies (n = 100) reported no between‐group difference.
Observer‐report: three studies, 187 participants; low‐certainty evidence. One study (n = 81) found a beneficial effect favouring immersive VR for parent, nurse and researcher reports. One study (n = 65) found a beneficial effect favouring immersive VR for caregiver reports. Another study (n = 41) reported no evidence of a difference in mean pain change scores.
Behavioural measurements (observer‐report): two studies, 106 participants; low‐certainty evidence. One study (n = 65) found a beneficial effect favouring immersive VR. Another study (n = 41) reported no evidence of a difference in mean pain change scores.
Adverse effects: six studies, 429 participants; very low‐certainty evidence. Three studies (n = 229) found no evidence of a difference between groups. Two studies (n = 141) reported no adverse effects in VR group. One study (n = 59) reported no beneficial effect in reducing estimated cyber‐sickness before and after VR immersion.
3: VR distraction versus other VR distraction
We did not identify any studies for this comparison.
Authors' conclusions
We found low‐certainty and very low‐certainty evidence of the effectiveness of VR distraction compared to no distraction or other non‐VR distraction in reducing acute pain intensity in children in any healthcare setting. This level of uncertainty makes it difficult to interpret the benefits or lack of benefits of VR distraction for acute pain in children. Most of the review primary outcomes were assessed by only two or three small studies. We found limited data for adverse effects and other secondary outcomes. Future well‐designed, large, high‐quality trials may have an important impact on our confidence in the results.
Plain language summary
What are the benefits and risks of using virtual reality in a healthcare setting to distract children from pain?
Why is this question important?
Medical procedures, such as health examinations or injections, can cause children to experience pain. In these situations, it is common practice to distract children using toys or play, in order to minimise distress and fear of pain.
One form of distraction that can be used is virtual reality. Virtual reality is an artificial environment with scenes and objects that appear to be real (for example a frozen world, or a wildlife park). Virtual reality can be:
‐ Fully‐immersive: users typically wear a headset with headphones and a screen, and interact with the virtual environment as if they were really in it.
‐ Semi‐immersive: users interact with a partially virtual environment (for example, a flight simulator where the controls are real, but the windows display virtual images).
‐ Non‐immersive: the user is connected to the virtual world by a separate monitor (for example, a computer) but can still experience the real world.
To find out whether virtual reality can distract children from pain, and whether it is associated with any adverse (unwanted) effects, we reviewed the research evidence.
How did we identify and evaluate the evidence?
We searched the medical literature for randomised controlled studies (clinical studies where people are randomly put into one of two or more treatment groups), because these provide the most robust evidence about the effects of a treatment. We compared and summarized their results. Finally, we rated our confidence in the evidence, based on factors such as study methods and sizes, and the consistency of findings across studies.
What did we find?
We found 17 studies that involved a total of 1008 children aged from four to 18 years. Medical procedures included injections, taking blood, changing wound dressings, and physical exercise. Studies compared virtual reality against no distraction, or against non‐virtual distraction. No studies compared different types of virtual reality.
During a medical procedure
We cannot tell whether virtual reality reduces self‐reported pain during a medical procedure because we have too little confidence in the evidence available (three studies).
Only two studies investigated changes in pain assessed by an observer (for example, using a rating scale that ranges from 0 (no pain) to 10 (great pain)). These reported conflicting findings: in one study fully‐immersive virtual reality was beneficial compared to non‐virtual distraction, but not in the other.
Fully‐immersive virtual reality may reduce pain assessed by an observer based on children's behaviour (for example, crying, or rubbing a body part in a way that indicates pain) more effectively than non‐virtual distraction (two studies) or no distraction (one study).
Non‐immersive virtual reality was not beneficial for pain assessed by an observer based on children's behaviour compared to no distraction (one study).
After a medical procedure
We cannot tell whether virtual reality can reduce self‐reported pain after a medical procedure, as we have too little confidence in the evidence available (16 studies).
Five studies investigated changes in pain assessed by an observer. Virtual reality was beneficial compared to no distraction in two studies, and also when compared to non‐virtual distraction in another two studies. However, it was no better than non‐virtual distraction in one study.
Two studies investigating pain assessed by an observer based on children's behaviour reported conflicting findings: immersive virtual reality was beneficial compared to non‐virtual distraction in one study, but not in the other.
We cannot tell whether there is a difference between virtual reality and no distraction for pain assessed by an observer based on children's behaviour, as we have too little confidence in the available evidence (one study).
Adverse effects
We cannot tell if virtual reality is associated with adverse effects because we have too little confidence in the evidence available (11 studies).
What does this mean?
We have little to very little confidence in the evidence we identified. It is unclear from our review whether virtual reality distraction makes a difference to pain in children. There is a need for large, well‐designed studies in this area.
How up‐to date is this review?
The evidence in this Cochrane Review is current to October 2019.
Summary of findings
Summary of findings 1. Virtual reality distraction compared to no distraction.
| Virtual reality distraction compared to no distraction | ||||||
| Patient or population: children (0 to 18 years) Setting: inpatient and outpatient paediatric healthcare setting Intervention: virtual reality distraction Comparison: no distraction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Certainty of the evidence (GRADE) | Comment | |
| Risk with no distraction | Risk with virtual reality distraction | |||||
| Acute pain intensity: self‐report (during procedure) | 42 (1 RCT) | ⊕⊝⊝⊝ VERY LOW a,b | One study found no evidence of beneficial effect of non‐immersive VR compared to no distraction. | |||
| Acute pain intensity: observer‐report (during procedure) | No study of this comparison reported this outcome. | ‐ | ‐ | ‐ | ||
| Acute pain intensity: behavioural measurement (observer‐report) (during procedure) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 62 (2 RCTs) |
⊕⊕⊝⊝ LOW a,c | One study found no evidence of beneficial effect of non‐immersive VR and another study found evidence of beneficial effect favouring immersive VR compared to no distraction. | |
| Acute pain intensity: self‐report (post‐procedure) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 461 (10 RCTs) |
⊕⊝⊝⊝ VERY LOW a,d | Four studies found no evidence of a beneficial effect of immersive, semi‐immersive or non‐immersive VR. Five other studies found evidence of beneficial effect favouring immersive VR compared to no distraction. Another study reported less pain in the VR group. |
|
| Acute pain intensity: observer‐report (post‐procedure) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 216 (2 RCTs) |
⊕⊕⊝⊝ LOW a,e | Two studies found evidence of a beneficial effect favouring immersive VR compared to no distraction for primary caregiver/parent and nurse observer‐reports. One of the studies also found evidence of a beneficial effect favouring immersive VR compared to no distraction for researcher observer‐reports. | |
| Acute pain intensity: behavioural measurement (observer‐report) (post‐procedure) | 42 (1 RCT) |
⊕⊝⊝⊝ VERY LOW a,b | One study found no evidence of beneficial effect of non‐immersive VR compared to no distraction. | |||
| Adverse effects (related to engagement with VR) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 154 (5 RCTs) |
⊕⊝⊝⊝ VERY LOW a,d | Three studies reported no adverse effects. Two studies reported mild adverse effects in the VR group. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RCT: Randomised controlled trial; VR: virtual reality | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aUnclear risk of selection bias; high risk of performance and detection bias. Downgraded one level for serious study limitations.
bSmall sample size with a wide 95% CI. Downgraded two levels for very serious imprecision.
cDifferent populations in terms of age, conditions and settings. Downgraded one level for serious indirectness.
dDifferent populations in terms of age, conditions and settings; differences in how the intervention was delivered; and differences in way outcomes measured. Downgraded two levels for very serious indirectness.
eDifferent populations in terms of conditions and settings. Downgraded one level for serious indirectness.
Summary of findings 2. Virtual reality distraction compared to non‐VR distraction.
| Virtual reality distraction compared to non‐VR distraction | ||||||
| Patient or population: children (0 to 18 years) Setting: inpatient and outpatient paediatric healthcare setting Intervention: virtual reality distraction Comparison: other non‐VR distraction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comment | |
| Risk with other non‐VR distraction | Risk with virtual reality distraction | |||||
| Acute pain intensity: self‐report (during procedure) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 106 (2 RCTs) |
⊕⊝⊝⊝ VERY LOW a,b | One study found evidence of beneficial effect favouring immersive VR and another study found no evidence of a difference in mean pain change scores between immersive VR and non‐VR distraction. | |
| Acute pain intensity: observer‐report (during procedure) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 106 (2 RCTs) | ⊕⊕⊝⊝ LOW a,c | One study found evidence of beneficial effect favouring immersive VR and another study found no evidence of a difference in mean pain change scores between immersive VR and non‐VR distraction. | |
| Acute pain intensity: behavioural measurement (observer‐report) (during procedure) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 106 (2 RCTs) | ⊕⊕⊝⊝ LOW a,c | One study found beneficial effect favouring immersive VR and another study reported evidence of a difference in mean pain change scores between immersive VR and non‐VR distraction with less pain behaviours observed for the VR group. | |
| Acute pain intensity: self‐report (post‐procedure) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 575 (8 RCTs) |
⊕⊝⊝⊝ VERY LOW a,b | Two studies found evidence of beneficial effect favouring immersive VR and another two studies reported a between group difference favouring immersive VR. Two studies found no evidence of beneficial effect for immersive and semi‐immersive VR and another two studies reported no evidence of a difference in mean pain changes scores between immersive VR and non‐VR. | |
| Acute pain intensity: observer‐report (post‐procedure) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 187 (3 RCTs) |
⊕⊕⊝⊝ LOW a,c | One study found evidence of beneficial effect favouring immersive VR for parent, nurse and researcher reports and another study also found evidence of beneficial effect favouring immersive VR for caregiver observed report. Another study reported no evidence of a difference in mean pain change scores between immersive VR and non‐VR distraction. | |
| Acute pain intensity: behavioural measurement (observer‐report) (post‐procedure) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 106 (2 RCTs) | ⊕⊕⊝⊝ LOW a,c | One study found evidence of beneficial effect favouring immersive VR and another study found no evidence of a difference in mean pain change scores between immersive VR and non‐VR distraction. | |
| Adverse effects (related to engagement with VR) | Data not pooled due to high heterogeneity in interventions, comparisons, participants, settings, and outcomes. | ‐ | 429 (6 RCTs) |
⊕⊝⊝⊝ VERY LOW a,b | Three studies found no evidence of a difference between immersive VR and non‐VR distraction for adverse effects. Another two studies reported no adverse effects in the VR group. One study reported that the change in estimated cybersickness before and after VR immersion was not significant. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RCT: Randomised controlled trial; VR: virtual reality | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aUnclear risk of selection bias; high risk of performance and detection bias. Downgraded one level for serious study limitations.
bDifferent population in terms of age, conditions and settings; differences in non‐VR distraction comparisons; and differences in way outcomes measured. Downgraded two levels for very serious indirectness.
cDifferent population in terms of age, conditions and settings; and differences in non‐VR distraction comparisons. Downgraded one level for serious indirectness.
Summary of findings 3. Virtual reality distraction compared to other VR distraction.
| Virtual reality distraction compared to other VR distraction | |||||
| Patient or population: children (0‐18 years) Setting: inpatient and outpatient paediatric healthcare setting Intervention: virtual reality distraction Comparison: other VR distraction | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | |
| Risk with other VR distraction | Risk with Virtual reality distraction | ||||
| Acute pain intensity: self‐report (during procedure) | No study of this comparison reported this outcome. | ‐ | ‐ | ‐ | |
| Acute pain intensity: observer‐report (during procedure) | No study of this comparison reported this outcome. | ‐ | ‐ | ‐ | |
| Acute pain intensity: behavioural measurement (observer‐report) (during procedure) | No study of this comparison reported this outcome. | ‐ | ‐ | ‐ | |
| Acute pain intensity: self‐report (post‐procedure) | No study of this comparison reported this outcome. | ‐ | ‐ | ‐ | |
| Acute pain intensity: observer‐report (post‐procedure) | No study of this comparison reported this outcome. | ‐ | ‐ | ‐ | |
| Acute pain intensity: behavioural measurement (observer‐report) (post‐procedure) | No study of this comparison reported this outcome. | ‐ | ‐ | ‐ | |
| Adverse effects (related to engagement with VR) | No study of this comparison reported this outcome. | ‐ | ‐ | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
Background
Description of the condition
Healthcare examinations, treatments, procedures and interventions are typical extreme stressors that can lead to pain for children (Clift 2007; Fox 2016; Horstman 2002; Melnyk 2000; Racine 2016; Rassin 2004; Wollin 2004). A recent definition describes pain as "a distressing experience associated with actual or potential tissue damage with sensory, emotional, cognitive, and social components” (Williams 2016). Similar to the International Association for the Study of Pain (IASP) original definition of pain (IASP 2011), this definition highlights that pain has both distressing sensory (i.e. pain intensity) and emotional (i.e. any negative affect secondary to pain such as distress; including anxiety, fear and/or stress) features, associated with actual or potential tissue damage. The sensory and emotional correlates of pain are ‘subjective psychological states’ (Aydede 2017) and can sometimes be difficult to distinguish between (Brown 2012; Curtis 2012; Goodenough 1999; McGrath 2008). This may be especially the case for children under eight years of age, who by virtue of their developmental abilities may be unable to differentiate pain meaningfully from other unpleasant emotions such as fear and anxiety (Blount 2006; Goodenough 1999). These two dimensions of pain (i.e. pain intensity and pain‐related distress) are important to consider in ensuring pain management strategies reduce not only pain intensity but also the distress, anxiety and/or fear associated with medical treatment‐related pain (Goodenough 1999).
Pain impacts on child and parent satisfaction with healthcare delivery and services. In an investigation of the views and experiences of children in Council of Europe member states, Kilkelly 2011 found that 60.1% of child participants rated ‘not being in pain’ as an important element of health care. Yet evidence suggests that acute pain management in children is not always optimal (Cummings 1996; Groenewald 2012; Taylor 2008). Figures estimate that 27% of children experience moderate to severe pain in hospital, with teenagers and infants experiencing higher prevalence rates of 38% and 32% respectively (Groenewald 2012). This can impact on children’s physiological, psychological and emotional well‐being, in both the short and long term.
It is inevitable that children admitted to healthcare settings will likely be exposed to potentially painful procedures on a daily basis. For instance, Stevens 2011 reported that more than three‐quarters (78.2%) of child participants (n = 3822) in their study had undergone at least one painful procedure in a 24‐hour period preceding data collection. While each child was exposed to an average of 6.3 (range 1 to 50) procedures, only a small portion (28.3%) of children had interventions specifically linked to the painful procedure. While acknowledging that certain procedures are essential for routine medical and surgical care, these procedures/treatments can cause pain for the child. Children can feel "threatened by the monster of medical care" where they fear being hurt, forced and violated by the adults delivering that care (Forsner 2009). Pain results in anxiety and stress, which, in turn, negatively impacts not only on a child’s ability to cope with the treatment/intervention but also on their recovery (Li 2009). Inadequate relief of pain during childhood treatments may have long‐term negative effects on future pain tolerance and pain responses (Young 2005).
Non‐pharmacological techniques (e.g. imagery, hypnosis, story‐telling, play, music) have long been promoted as useful adjuncts to pharmacological analgesics (Butler 2005; Klassen 2008; Landier 2010). Yet, aside from distraction and hypnosis, and more recently combined cognitive behavioural therapy and breathing, there is limited evidence to support the efficacy of many of these conventional psychological interventions (e.g. relaxation, guided imagery, music) for reducing procedure‐related pain in children (Birnie 2018; Stinson 2008). In addition, it has been documented that children may benefit more from interactive (e.g. playing a video game) as opposed to passive (e.g. watching a video game) distraction strategies (Wohlheiter 2013). One such recent ‘active’ adjunctive analgesic technique gaining momentum is virtual reality (VR) (Hoffman 2011).
With the use of technology becoming increasingly prevalent in children’s daily lives, alongside the drive towards e‐health and the empowered patient, it seems reasonable to propose that interactive technologies, if proven effective, should be considered as vital intervention vehicles for enhancing health outcomes for children. The use of VR during healthcare procedures/treatments can create a child‐friendly and developmentally sensitive environment, thereby contributing to the European campaign for a child‐friendly approach to health care (Council of Europe 2011).
Description of the intervention
VR, also referred to as virtuality, is defined as a computer technology that creates a simulated environment/world that users perceive as comparable to real world objects/events (Aguinis 2001; Chan 2007; Hoffman 2004a; Weiss 2003). The user’s attention is drawn away from real world visual, auditory and tactile stimuli, and into the virtual world by the multi‐sensory (i.e. sight, sound, touch) nature of the virtual environment (Gold 2006). VR interventions can vary considerably in terms of three core aspects: types of equipment used; content and nature of the virtual world; and levels of engagement users might have. VR draws the user’s attention to a virtual world/environment using real‐time computer graphics and various inputs (e.g. position trackers, mouse and data glove) and output (e.g. shutter glasses, head‐mounted displays, haptic and audio‐visual) devices that make the person an active participant within a computer‐generated three dimensional world. Active interaction, navigation and immersion are key characteristics of VR systems (Aguinis 2001).
The content of some VR interventions has been developed specifically for certain types of procedures (e.g. Snow World and Ice Cream Factory, devised for burn wound dressings) (Chan 2007; Hoffman 2004a), whereas other VR interventions (e.g. Virtual Gorilla) are selected for convenience to engage children at the time of invasive medical procedures (Gershon 2003; Wolitzky 2005). All VR systems are categorised according to how immersive or non‐immersive they are. With non‐immersive systems, the user is connected to the virtual world (by an external monitor) but can still communicate with the real world (e.g. the healthcare environment; Nilsson 2009). With full immersion, the user’s visual and auditory perception and haptics of stimuli in the outside world is blocked as they become fully enveloped in the computer‐generated virtual environment through the use of a head‐mounted display and a tracker position sensor (e.g. a helmet and headphones which exclude visual and auditory inputs from the healthcare environment; Gold 2006; Weiss 2003). It is this sense of presence and immersive attention (i.e. the ability to give users the sense they are somewhere else) that sets VR apart from other technological interventions such as watching television or video movies, or playing simulated or interactive video games (Chan 2007; Gorini 2011; Hoffman 2004a; Nilsson 2009; Steele 2003; Weiss 2003).
How the intervention might work
VR has been used in many contexts (e.g. treating phobias and post‐traumatic stress disorders; training military and medical personnel). For the purposes of this review, the focus is on the use of VR in the reduction of acute pain intensity and pain‐related distress associated with medical treatments/interventions in any healthcare setting. The theory of how VR works in such instances is as a form of distraction; where distraction is referred to as purposefully directing attention away from undesirable sensations (Mobily 1993). Distraction is a common coping mechanism used by school aged children and adolescents for enduring unpleasant situations (Schneider 2000). Distraction interventions function by diverting the child’s attention away from the stimulus producing the pain and refocusing the child’s attention towards a more pleasant and positive stimulus (i.e. the virtual environment; McCaul 1984; Schneider 2000). VR interventions are thought to manifest analgesic effects by altering pain perception through distracting user attention away from the painful procedure, in addition to changing the way a person interprets incoming pain signals, consequently reducing the amount of pain‐related brain activity (as seen on MRI imagery) (Morris 2009). VR exposure can target cognitive and affective pain pathways, thereby decreasing pain intensity, distress, and anxiety by altering how pain signals are processed in the central nervous system. This is achieved by a number of mechanisms including attentional distraction, conditioning of VR imagery and reduced pain.
VR distraction has been used, for example, to minimise children’s anxiety associated with chemotherapy (Ahmadi 2001; Schneider 1999), to reduce children’s pain during burn wound care (Hoffman 2000; Hoffman 2001; Hoffman 2004a), to access intravenous ports in paediatric oncology patients (Wolitzky 2005), to alleviate pain/anxiety for invasive medical procedures such as venipuncture, lumbar puncture, and bone marrow aspirates (Gershon 2003; Gold 2006; Nilsson 2009; Wint 2002), to help adolescents with cerebral palsy as they endure physiotherapy (Steele 2003), and to reduce children’s preoperative anxiety using handheld video games or films (Low 2008; Patel 2006). Together with pharmacological interventions, distraction is thought to be an effective pain management strategy by cognitively redirecting attention away from pain to a more pleasant stimulus, thereby assisting children to cope with the distress of medical treatments. Long‐term benefits include advantages for later adult life, as pain experienced during medical treatments in childhood is predictive of pain during subsequent medical procedures and avoidance of medical care during young adulthood (Blount 2006).
Why it is important to do this review
VR is a recent technological advancement with the potential to modulate children’s pain when they are undergoing healthcare treatments (e.g. intravenous cannulation, lumbar puncture, wound dressings, chemotherapy, bone marrow aspirates). For instance, Gold 2006 reported that children who underwent intravenous cannulae placement without distraction reported a fourfold increase in affective pain when compared to children immersed in a VR intervention. Additionally, children who received a VR intervention were twice as satisfied with their pain management as compared to children not exposed to a VR intervention. Schneider 2000 found 82% of children indicated that their chemotherapy treatment was better with VR as compared to previous chemotherapy treatment without VR. Parents were also satisfied with the use of VR interventions and believed such interventions did reduce children’s pain and enhance children’s cooperation during medical treatments (Gold 2006). In a review, Hoffman 2011 reported a 35% to 50% reduction in procedural pain in burn patients when in a distracting immersive VR.
Despite these positive evaluations and reports of pain reduction, there remains uncertainty over the effectiveness of VR interventions (Dahlquist 2010; Garrett 2014; Kenney 2016; Malloy 2010; Morris 2009). In addition, in comparison to other simpler forms of non‐pharmacological distraction interventions (e.g. imaginary, breathing, positive thinking), there have been some common criticisms levelled at VR such as high costs, bulky equipment, the need for specialist technological skills and the potential for cyber‐sickness, all of which may threaten the widespread implementation of VR for therapeutic healthcare interventions (Bohil 2011). It is important to conduct this systematic review to evaluate the effectiveness of VR as a pain distractor during healthcare treatments. As few psychological interventions incorporate, or evaluate the effectiveness of, modern and novel interactive technologies such as VR, this review complements other Cochrane Reviews (e.g. Birnie 2018) that evaluate the effectiveness of non‐pharmacological distraction‐based interventions for minimising pain in children when undergoing medical treatments.
Objectives
To assess the effectiveness and adverse effects of VR distraction interventions for children (0 to 18 years) with acute pain in any healthcare setting.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), including cross‐over and cluster‐RCTs.
Types of participants
We included children aged from birth up to and including 18 years, with acute pain in any healthcare setting.
Types of interventions
Any technology aimed at creating a virtual environment/world, including immersive and/or non‐immersive VR of any intensity or duration, with the purpose of reducing acute pain intensity. These interventions may be used with or without pharmacological support. We included interventions that used any combination of input and output devices (e.g. mouse and shutter glasses; position tracker and head‐mounted display). For the intervention to be VR the participant must be actively interacting with the virtual environment which responds to their actions. We excluded interventions where the user was a passive observer, such as watching a virtually‐simulated movie as opposed to actively engaging in a virtual environment through physical movement.
Interventions of interest were:
VR distraction compared to no distraction;
VR distraction compared to non‐VR distraction;
VR distraction compared to other VR distraction (grouped by level of immersion which takes account of type of technical device, VR environment and level of user interaction).
Types of outcome measures
Primary outcomes
Acute pain intensity:
-
1. during the procedure, measured using:
self‐report;
observer‐report;
behavioural measurements (observer‐report).
-
2. post‐procedure (up to one hour), measured using:
self‐report;
observer‐report;
behavioural measurements (observer‐report).
Secondary outcomes
Adverse effects related to engagement with VR. These may include motion sickness, ocular problems (e.g. eye strain, blurred vision), balance disturbances, headaches, fatigue and repetitive strain injuries.
Child satisfaction with VR.
Child pain‐related distress, for example, self‐report, observer‐report or behavioural measurements of child distress, anxiety, fear and/or stress.
Parent anxiety using parent self‐reported anxiety scales or inventories.
Administration of rescue analgesia (i.e. administration of additional analgesic medications to treat acute pain not controlled by child’s scheduled analgesic regimen).
Cost, which may include cost of the VR intervention or duration of child’s treatment (measured in original currency).
Search methods for identification of studies
Electronic searches
With assistance from the Cochrane Pain, Palliative and Supportive Care (PaPaS) Review Group, we searched the following electronic databases up to October 2019.
The Cochrane Central Register of Controlled Trials (CENTRAL) via CRSO searched on 17/10/2019
MEDLINE (OvidSP) (1989 to 17 October 2019)
Embase (OvidSP) (1989 to 17 October 2019)
CINAHL (EbscoHOST) (1989 to 17 October 2019)
PsycINFO (Proquest) (1989 to 17 October 2019)
We used a combination of controlled vocabulary under the existing databases' organisational systems (e.g. MeSH and EMTREE) and free text terms. We did not apply language restrictions. Search dates start at 1989 as the intervention did not exist before this time. Please see the appendices for the search strategies and terms used for each of the databases: CENTRAL (Appendix 1), MEDLINE (Appendix 2), Embase (Appendix 3), CINAHL (Appendix 4), and PsycINFO (Appendix 5).
Searching other resources
We searched for grey literature and ongoing trials using the following methods.
Proceedings from conferences
ProQuest Digital Dissertations and Theses
Index to Theses (Ireland and UK)
TrialsCentralTM (www.trialscentral.org)
Clinical trials register (Clinicaltrials.gov)
WHO Clinical Trial Search Portal (www.who.int/trialsearch)
Current Controlled Trials (www.controlled-trials.com)
We searched reference lists from retrieved eligible studies for other studies potentially eligible for inclusion. We handsearched relevant journals including Virtual Reality (from inception in 1995 to October 2019) and The International Journal of Virtual Reality (from inception in 1998 to October 2019). We contacted experts in the field and authors of included studies about other potentially relevant studies.
Data collection and analysis
Selection of studies
Two review authors (VL, AM) independently assessed each title and abstract retrieved from the electronic searches for relevance using Covidence 2018. We resolved any discrepancies through discussion with a third review author (PB, PH or DD) acting as arbiter as required. We sourced and assessed the full paper if no abstract was available. We obtained and read full texts of the studies that potentially met our inclusion criteria. Two review authors (VL, AM) independently assessed these full texts against the inclusion criteria before a final decision regarding inclusion/exclusion was confirmed. We resolved any discrepancies by consensus or discussion with a third review author (PB, PH or DD) acting as arbiter where necessary. We listed all potentially relevant papers excluded from the review at full‐text stage in the Characteristics of excluded studies table, noting reasons for exclusion. We listed publications in abstract form only in excluded studies. We collated and reported multiple details of the same study/duplicate publications, to ensure that each study (rather than each report) was the unit of interest in the review. We used an adapted PRISMA flow chart to report the screening and selection process.
Data extraction and management
We designed, piloted and amended as necessary a data extraction form based on the Cochrane Pain, Palliative and Supportive Care Review Group template. Two review authors (VL, AM) independently extracted and managed data from each included RCT using the tailored data extraction form. Data extracted from included studies comprised of the following items.
Methods: aim of study, study design, method of participant recruitment, funding source, declaration of interests for primary investigators, statistical methods and consumer involvement.
Risk of bias: as specified under Assessment of risk of bias in included studies.
Participants: description, participant inclusion and exclusion criteria, geographical location, setting, number, age, gender, ethnicity, principal and stage of diagnosis, type of procedure/treatment receiving.
Intervention: details of intervention (including aim, content, format, source, setting) and control/usual care, delivery of intervention (including timing, frequency, duration), providers of the intervention and intervention fidelity/integrity.
Outcomes: primary and secondary outcome measures (as detailed under Types of outcome measures), timing of assessment and methods of assessing outcome measures, follow up for non‐respondents and adverse events.
We resolved any discrepancies in data extraction between the two review authors through discussion or if required, consultation with a third review author (PB, PH or DD). The first review author (VL) entered the data into Review Manager 5 software (RevMan 2014), with the second review author (AM) checking the accuracy of data entry. We attempted to obtain any missing, unclear or incomplete data by contacting the study authors.
Assessment of risk of bias in included studies
Two authors (VL, AM) independently assessed risk of bias for each study, using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion and consensus with a third review author (DD) acting as arbiter as required. We completed a 'Risk of bias' table for each included study using the 'Risk of bias' tool in Review Manager 5.3 (RevMan 2014). We assessed the following for each study.
Random sequence generation (checking for possible selection bias)
We assessed the method used to generate the allocation sequence for each included study as having:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth, hospital or clinic record number); or
unclear risk of bias (insufficient information about the sequence generation process to permit judgement).
For cross‐over studies we also assessed for period effects (i.e. systematic differences between responses in the second period compared to the first period not due to different interventions) as having:
low risk of bias (1:1 allocation ratio where any general trends in outcomes over time will cancel; period effects included in analysis);
high risk of bias (unequal proportions of participants randomised to the different intervention sequences where a general trend in outcomes over time may lead to bias; no period effects included in analysis); or
unclear risk of bias (insufficient or no information available to permit judgement on period effects).
For random sequence generation, studies assessed as high risk of bias were excluded.
Allocation concealment (checking for possible selection bias)
The method used to conceal allocation to interventions prior to assignment determines whether intervention allocation could have been foreseen in advance of assignmet, during recruitment, or changed after assignment.
We assessed the allocation concealment methods for each included study as having:
low risk of bias (e.g. telephone or central randomisation; sequentially numbered sealed opaque envelopes);
high risk of bias (e.g. open random allocation; unsealed or non‐opaque envelopes; alternation; date of birth); or
unclear risk of bias (method of concealment not clearly described or not described in sufficient detail to allow for a definite judgement).
For allocation concealment, we excluded studies assessed as having high risk of bias.
Blinding of participants and personnel (checking for possible performance bias)
We assessed the methods used to blind study participants and personnel from knowledge of which intervention a participant received. We assessed methods as having:
low risk of bias (blinding of participants and study personnel ensured, and unlikely that the blinding could have been broken);
high risk of bias (no blinding, incomplete or attempted blinding of participants and study personnel, and possible that non‐blinding of others likely to introduce bias; or attempted blinding could have been broken; or reported as not blinded due to nature of the intervention); or
unclear risk of bias (insufficient information on blinding of participants and study personnel to permit a judgement).
Blinding of outcome assessment (checking for possible detection bias)
We assessed the methods used to blind study participants and outcome assessors from knowledge of which intervention a participant received. We assessed the methods as having:
low risk of bias (clear statement that outcome assessors were unaware of treatment allocation, and describes how this was achieved);
high risk of bias (outcome assessment not blinded or or reported as not blinded due to nature of the intervention); or
unclear risk of bias (states outcome assessors were blind to treatment allocation but lacks a clear statement on how it was achieved).
For cross‐over studies we also assessed for carry‐over effects (i.e. effects of an intervention given in one period continue into a subsequent period, thereby interfering with the effects of the second intervention) as:
low risk of bias (sufficient time for carry‐over effects to disappear before outcome assessment in second period);
high risk of bias (insufficient time for carry‐over effects to disappear before outcome assessment in second period); or
unclear risk of bias (insufficient or no information available to permit judgement on carry‐over effects).
Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We assessed the methods used to deal with incomplete data as having:
low risk of bias (no missing outcome data, less than 10% missing data, missing data balanced in numbers across intervention groups with similar reasons for missing data across groups);
high risk of bias (used 'completer' analysis, more than 10% missing data); or
unclear risk of bias (no or insufficient information provided to permit judgement).
Selective reporting (checking for reporting bias)
We assessed whether primary and secondary outcome measures were pre‐specified and whether these were consistent with those reported. We assessed the methods as having:
low risk of bias (e.g. all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (e.g. not all of the study’s pre‐specified outcomes have been reported and outcomes of interest are reported incompletely, and so cannot be used); or
unclear risk of bias (insufficient information available to permit judgement).
For cross‐over studies we also assessed for first period data on a basis of a test for carry‐over as having:
low risk of bias (results from both periods reported);
high risk of bias (results from first period only reported); or
unclear risk of bias (insufficient or no information available to permit judgement on reporting bias).
Size of study (checking for possible biases confounded by small size based on number of participants in each study arm)
We evaluated risk of bias for each included study according to the Cochrane PaPaS Review Group guidance on sample size based on the number of participants included in each study arm. We assessed studies to be at:
low risk of bias (≥ 200 participants per treatment arm);
high risk of bias (< 50 participants per treatment arm); or
unclear risk of bias (50 to 199 participants per treatment arm).
Other potential sources of bias
We assessed whether each trial was free of other problems that could put it at a risk of bias as having:
low risk of bias (appears to be free of other sources of bias);
high risk of bias (has at least one important risk of bias e.g. potential source of bias related to the specific study design used, extreme baseline imbalance etc.); or
unclear risk of bias (there may be risk of bias but there is insufficient information to assess whether an important risk of bias exists, or insufficient rationale or evidence that an identified problem will introduce bias).
We had planned to also extend the risk of bias to include specific questions for cluster trials (e.g. selective recruitment of cluster participants; baseline reporting of comparability of clusters) (Higgins 2011; Ryan 2011), but this was not necessary as we did not identify any cluster‐RCTs for inclusion in the review. We will address this in future updates if applicable.
Measures of treatment effect
We planned to analyze the data using RevMan 5.3 (RevMan 2014). For dichotomous outcomes, we planned to report risk ratios (RR) and 95% confidence intervals (CI). For continuous outcomes, we planned to report mean differences (MD) (if outcomes were measured in the same way between trials) and 95% CI. For trials that used different methods to measure the same outcome, we planned to use standardized mean differences (SMD) and 95% CI. We planned to undertake a meta‐analysis if studies were sufficiently similar in design, population, interventions and outcomes, but this was not possible. We will undertake a meta‐analysis in future updates, should more data become available.
Unit of analysis issues
We acknowledged that issues could arise from the inclusion of cross‐over designs and cluster‐RCTs. We did not identify any eligible cluster‐RCTs. In future updates of this review, if we identify any cluster‐RCTs, we will use effect size estimates and standard errors, adjusted in the analysis for clustering, and combine the studies using the generic inverse‐variance method (Higgins 2011). We will adjust sample sizes using the methods described in the Cochrane Handbook using an estimate of the intra‐cluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC.
We identified one within‐subject (cross‐over) study as eligible for inclusion in the review. We analysed the data according to recommendations in the Cochrane Handbook (Higgins 2011) for cross‐over trials. We used the effect estimate and standard deviation based on a paired t‐test. If we identify additional cross‐over studies in future updates, we will combine the studies using the generic inverse‐variance method (Higgins 2011, section 16.4) and seek statistical advice for this part of the analysis.
Dealing with missing data
We contacted study authors for missing data. We noted levels of attrition in the included studies. We were unable to perform any meta‐analysis in this review due to clinical heterogeneity in population and procedural conditions. In future updates of this review, we will conduct analysis of outcomes on an intention‐to‐treat basis (i.e. by including all randomised participants in the group to which they were randomised regardless of whether or not they received the allocated intervention). Where this is not possible (i.e. data were not provided by study authors), we will conduct an analysis based on the number of participants for whom outcome data are known. As part of our 'Risk of bias' assessment, we reported the number of participants lost to follow‐up and the levels of, and reasons for, attrition in each trial. We had intended to investigate the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis; however, there were not enough data included in the review to conduct this analysis.
Assessment of heterogeneity
We considered whether studies were sufficiently similar (based on consideration of populations, interventions, settings or methodological features) to allow pooling of data using meta‐analysis and we assessed the degree of statistical heterogeneity by visual inspection of forest plots and by examining the Tau² (tau‐squared), I², and Chi² statistics. We regarded heterogeneity as substantial if:
-
the I² value was 50% or higher; and either
there was inconsistency between trials in direction or magnitude of effects (judged visually), or a low (P < 0.10) P value in the Chi² test for heterogeneity; or
the estimate of between‐study heterogeneity (Tau²) was above zero.
We had intended to investigate the presence of substantial heterogeneity using subgroup and sensitivity analyses however there were insufficient data included in the review to conduct these analyses. We did consider whether an overall summary was meaningful, and if it had been, we would have used a random‐effects analysis to produce it.
We detected substantial clinical heterogeneity across included studies and therefore do not report pooled results from meta‐analysis but instead provide a narrative description of data.
Assessment of reporting biases
We did not identify sufficient trials (at least 10) to evaluate reporting biases graphically using funnel plots. In future updates of this review, if 10 or more studies are included, we will conduct formal tests for funnel plot asymmetry; for continuous outcomes we will use the test proposed by Egger 1997, and for dichotomous outcomes we will use the test proposed by Harbord 2006. We will perform exploratory analyses if asymmetry is detected in any of these tests or is suggested by a visual assessment to investigate it. Where we suspect reporting bias we will attempt to contact study authors asking them to provide missing outcome data. Where this is not possible, and the missing data are thought to introduce serious bias, we will explore the impact of including such studies in the overall assessment of results by a sensitivity analysis.
Data synthesis
We planned to use a random‐effects model for meta‐analysis to produce a summary of effect based on the anticipated variability in the populations and interventions of included studies. However, we did not conduct meta‐analysis due to a lack of suitable studies. We judged that the heterogeneity in interventions and comparisons, participants, settings, and outcomes in our included studies would not contribute to meaningful conclusions from a statistically‐pooled result. Therefore, we present the data in additional tables (Table 4 and Table 5), and narratively describe the results. Where possible we calculated effect estimates for each study using Review Manager 5.3 software (RevMan 2014). In future updates of this review, if we identify enough studies suitable to be combined and undergo quantitative analysis, we will conduct meta‐analysis.
1. Comparison 1: Virtual reality distraction compared to no distraction.
| Study | Measurement Tool | Data VR Intervention | Data No Distraction | P value |
| Outcome: Acute pain intensity: self‐report (during the procedure) | ||||
| Nilsson 2009 | Colour Analogue Scale (scale range 0 to 10; 0 = no pain, 10 = most pain) |
Mean (SD) During procedure (retrospective recorded after procedure) 2.20 (2.78); N = 21 |
Mean (SD) During procedure (retrospective recorded after procedure) 1.64 (2.17); N = 21 |
|
| Outcome: Acute pain intensity: behavioural measurement (observer‐report) (during the procedure) | ||||
| Nilsson 2009 | Face, Legs, Activity, Cry, Consolability Scale (total score out of maximum 10; higher score indicates pain) |
Mean (SD) During procedure (retrospective recording after procedure) 1.10 (2.00); N = 21 |
Mean (SD) During procedure (retrospective recording after procedure) 1.67 (1.59); N = 21 |
|
| Outcome: Acute pain intensity: self‐report (post‐procedure up to one hour) | ||||
| Jeffs 2014 | Adolescent Pediatric Pain Tool (scale range 0 to 100; no pain to worst pain) |
Between group difference Difference: 9.7 mm, 95% CI: ‐9.5 to 28.9 VR group reported non‐statistical significant less procedural pain compared to no distraction group |
P = 0.32 | |
| Mean (SD) 58.20 (31.7); N = 8 |
Mean (SD) 37 (31.80); N = 10 |
|||
| Nilsson 2009 | Colour Analogue Scale (scale range 0 to 10; 0 = no pain, 10 = most pain) |
Mean (SD) 1.05 (1.74); N = 21 |
Mean (SD) 0.51 (0.99); N = 21 |
|
| Schmitt 2011 | Graphic Rating Scale (scale range 0 to 100; no pain to worst pain) |
Mean (SD) After treatment condition 40.15 (30.87); N = 52 |
Mean (SD) After treatment condition 54.48 (26.68); N = 52 |
|
| Outcome: Acute pain intensity: behavioural measurement (observer‐report) (post‐procedure up to one hour) | ||||
| Nilsson 2009 | Face, Legs, Activity, Cry, Consolability Scale (total score out of maximum 10; higher score indicates pain) |
Mean (SD) 0.29 (0.56); N = 21 |
Mean (SD) 0.19 (0.51); N = 21 |
|
| Outcome: Child pain related distress (incl. anxiety, fear and distress) | ||||
| Nilsson 2009 | Facial Affective Scale (scale range 0 to 1; from least to most distressed) |
Median During procedure (retrospective recording after procedure) 0.47 (N = 21) |
Median During procedure (retrospective recording after procedure) 0.47 (N = 21) |
NS |
| Mean (SD) During procedure (retrospective recording after procedure) 0.41 (0.29) |
Mean (SD) During procedure (retrospective recording after procedure) 0.47 (0.21) |
|||
| Wolitzky 2005 | Visual Analogue Scale (scale range 0 to 100; none to maximum pain or anxiety) |
Composite score (mean of VAS anxiety and pain scores) During procedure (retrospective recorded after procedure) 12.00 (16.36) |
Composite score (mean of VAS anxiety and pain scores) During procedure (retrospective recorded after procedure) 34.45 (41.80) |
|
SD: standard deviation N: number
2. Comparison 2: Virtual reality distraction compared to non‐VR distraction.
| Study | Measurement Tool | Data VR Intervention | Data Non‐VR Distraction | P Value |
| Outcome: Acute pain intensity: self‐report (during the procedure) | ||||
| Kipping 2012 | Visual Analogue Scale (scale range 0 to 10; from no pain to pain as bad as it could possibly be) |
Mean change scores After dressing removal (taken as during procedure) 2.9 (2.3); N = 20 |
Mean change scores After Dressing removal (taken as during procedure) 4.2 (3.2); N = 21 |
P = 0.16 |
| Outcome: Acute pain intensity: observer‐report (during the procedure) | ||||
| Kipping 2012 | Visual Analogue Scale (scale range 0 to 10; from no pain to worst pain) |
Mean change scores After dressing removal (during procedure) 3.5 (2.5); N = 20 |
Mean change scores After dressing removal (during procedure) 3.8 (3.2); N = 21 |
P = 0.71 |
| Outcome: Acute pain intensity: behavioural measurements (observer‐report) (during the procedure) | ||||
| Kipping 2012 | Face, Legs, Activity, Cry, Consolability Scale (total score out of maximum 10; higher score indicates pain) |
Mean change scores After dressing removal (during procedure) 2.9 (2.4); N = 20 |
Mean change scores After dressing removal (during procedure) 4.7 (2.5); N = 21 |
P = 0.02 |
| Outcome: Acute pain intensity: self‐report (post‐procedure up to one hour) | ||||
|
Chan 2019 Emergency department |
Faces Pain Scale‐Revised (scale range 0 to 10; no pain to very much pain) |
Between group difference: ‐1.78; 95% CI, ‐3.24 to ‐0.32 | P = 0.018 | |
| Change in FPS‐R from baseline ‐1.39; 95% CI ‐2.42 to ‐0.36; N = 64 |
Change in FPS‐R from baseline 0.39; 95%CI ‐1.45 to 0.67; N = 59 |
VR intervention P = 0.009 Non‐VR distraction P = 0.47 |
||
|
Chan 2019 Outpatient pathology |
Faces Pain Scale‐Revised (scale range 0 to 10; no pain to very much pain) |
Between group difference: ‐1.39; 95% CI, ‐2.68 to ‐0.11 | P = 0.034 | |
| Change in FPS‐R from baseline 1.37; 95% CI, 0.50 to 2.23; N = 63 |
Change in FPS‐R from baseline 2.76; 95% CI, 1.79 to 3.72; N = 66 |
VR intervention P = 0.003 Non‐VR distraction P < 0.001 |
||
| Kipping 2012 | Visual Analogue Scale (scale range 0 to 10; no pain to pain as bad as it could possibly be) |
Mean change scores After dressing application (post‐procedure) 2.33 (3.4); N = 20 |
Mean change scores Dressing application (post‐procedure) 3.8 (3.6); N = 21 |
P = 0.40 |
| Jeffs 2014 | Adolescent Pediatric Pain Tool (scale range 0 to 100; higher score indicates more pain) |
Between group difference Difference: 23.7 mm, 95% CI: 2.4 to 45.0 VR group reported significant less procedural pain than PD group |
P = 0.029 | |
| Means (SD) After procedure 58.2 (31.7); N = 8 |
Means (SD) After procedure 30.2 (29.2); N = 10 |
|||
| Walther‐Larsen 2019 | Visual Analogue Scale (scale range 0 to 100; higher scores indicates more pain) |
Mean Difference 5; 95% CI, ‐3 to 13 | P = 0.23 | |
| Median (IQR) 27 (8 to 33) |
Median (IQR) 15 (5 to 30) |
|||
| Outcome: Acute pain intensity: observer‐report (post‐procedure up to one hour) | ||||
| Kipping 2012 | Visual Analogue Scale (scale range 0 to 10; no pain to worst pain) |
Mean change scores After dressing application (post‐procedure) 2.6 (3.5); N = 20 |
Mean change scores After dressing application (post‐procedure) 2.2 (4.0); N = 21 |
P = 0.75 |
| Outcome: Acute pain intensity: behavioural measurements (observer‐report) (post‐procedure up to one hour) | ||||
| Kipping 2012 | Face, Legs, Activity, Cry, Consolability Scale (total score out of maximum 10; higher score indicates pain) |
Mean change scores After dressing application (post‐procedure) 1.9 (2.8); N = 20 |
Mean change scores After dressing application (post‐procedure) 3.0 (2.8); N = 21 |
P = 0.23 |
| Outcome: Adverse effects related to engagement with VR | ||||
| Kipping 2012 | Visual Analogue Scale (scale range 0 to 10; 0 = no sick tummy (i.e., nausea), 10 = sick tummy as bad as it could possibly be) |
Mean change scores Nausea dressing removal (during procedure) ‐0.7 (1.1); N = 20 Nausea dressing application (after procedure) ‐0.3 (1.0); N = 20 |
Mean change scores Nausea dressing removal (during procedure) ‐0.3 (1.5); N = 21 Nausea dressing application (after procedure) ‐0.5 (1.3); N = 21 |
P = 0.27 P = 0.65 |
| Outcome: Administration of rescue analgesia | ||||
| Kipping 2012 | Frequency of rescue does of Entonox prescribed after commencement of procedure | Number (%) 3 (15%); N = 20 |
Number (%) 9 (43%); N = 21 |
P = 0.05 |
N: number SD: standard deviation
Certainty of the evidence
Two review authors (VL and AM) independently rated the certainty of evidence for each outcome. We used the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system to rank the certainty of the evidence using the GRADEprofiler Guideline Development Tool software (GRADEpro GDT 2015), and the guidelines provided in Chapter 12.2 of the Cochrane Handbook (Higgins 2011).
The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the certainty of the body of evidence for each outcome. The GRADE system uses the following criteria for assigning grades of evidence:
high: we are very confident that the true effect lies close to the estimate of effect;
moderate: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different;
low: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect;
very low: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.
We considered evidence from RCTs as high certainty but we downgraded the evidence by one (‐1) or two (‐2) where we identified:
serious (‐1) or very serious (‐2) limitation to study quality (risk of bias);
serious (‐1) or very serious (‐2) inconsistency across studies;
some (‐1) or major (‐ 2) uncertainty about directness of evidence;
serious (‐1) or very serious (‐2) imprecise data; and
high probability of the presence of publication bias (‐1).
We reported our judgement on the certainty of the evidence in the 'Summary of findings' tables.
'Summary of findings' table
We included three ‘Summary of findings' tables:
VR distraction compared to no distraction;
VR distraction compared to non‐VR distraction;
VR distraction compared to other VR distraction.
We used the methods described in Chapter 11 of the Cochrane Handbook (Schunemann 2011) to prepare the ‘Summary of findings’ tables. For each table, we presented the results for the primary outcomes of acute pain intensity self‐report, observer‐report and behavioural measurements (observer‐report) measured during procedure and up to one hour post‐procedure and the secondary outcome adverse effects, as outlined in the section on Types of outcome measures. As meta‐analysis was not possible in this review, we presented results in a narrative 'Summary of findings' table format. We used the GRADE system to judge the certainty of the evidence using GRADEprofiler software (GRADEpro GDT 2015).
Subgroup analysis and investigation of heterogeneity
We had planned to conduct the following subgroup analyses for the primary outcome:
(i) younger (0 to 9 years) versus older (10 to 18 years) aged children;
(ii) immersive versus non‐immersive VR interventions.
However, we did not do so because of a limited number of heterogeneous small trials for each intervention type and the fact that data were not reported separately for different ages. In future updates of this review, if sufficient data, we will conduct our planned subgroup analyses.
Sensitivity analysis
We had planned to conduct a sensitivity analysis based on trial quality but did not do so as we did not pool data statistically. In future updates of this review, if sufficient data are available, we will perform sensitivity analysis by separating high from low quality. We define ‘high quality’ as a trial having low risk of bias for sequence generation and adequate allocation concealment and low risk of bias for loss to follow up, classified as less than 10% for primary outcome data.
We will perform a sensitivity analysis for plausible variations in estimated intra‐cluster correlation coefficients (ICCs) if unit‐of‐analysis errors arise in future included cluster‐randomised trials and the ICCs had been estimated for those studies. We will limit sensitivity analyses to primary outcomes. We will conduct a sensitivity analysis to determine the influence of validated versus non‐validated scales on the effects of intervention on outcome.
Consumer participation
The editorial process of the Cochrane Pain, Palliative and Supportive Care Review Group included feedback on the review from one consumer referee in addition to health professionals. The first author of the review continues to engage in research in the field of children’s health care and services with particular emphasis on the voice and visibility of children themselves. These child perspectives were drawn upon in the review, alongside children’s perspectives of VR use in health care. We also obtained feedback from the consumer representative organisation Children in Hospital Ireland who recommended that for future trials it would be worth considering how children and young people are involved in the planning and design stage of the research as well as participants. Additionally, for future research it would be worth examining whether capacity/ability to understand/communicate or other aspects of a specific disability or condition would have an important influence on the effectiveness of the distraction stimulus.
Results
Description of studies
Results of the search
We identified 1827 citations in the database search and a further 19 citations through searching other resources. There were 1254 citations for screening after removal of duplicates. We excluded 1131 citations not meeting the review inclusion criteria on initial screening of titles and abstracts. We assessed 123 citations for eligibility at full‐text screening and excluded 70 citations (representing 65 studies) that did not meet the review selection criteria. Seventeen studies (reported in 18 citations) met the inclusion criteria and four studies (reported in five citations) are awaiting classification. Thirty studies (reported in 32 citations) are ongoing. See Figure 1.
1.
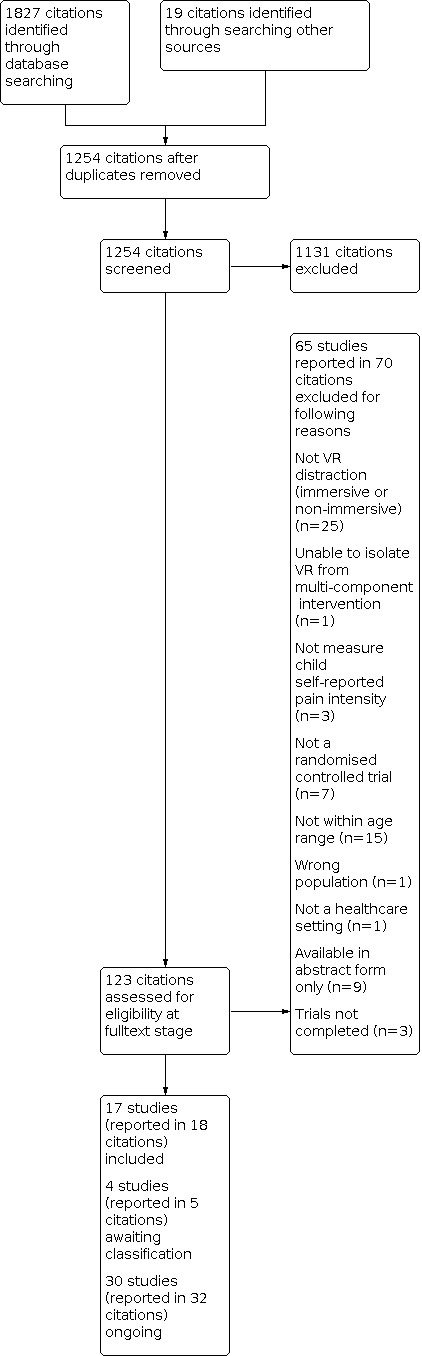
Study flow diagram.
Included studies
See Characteristics of included studies.
We identified 17 RCTs (reported in 18 citations). Thirteen of these used a parallel design (Chan 2019; reporting two RCTs); Chen 2019; Dumoulin 2019; Gerceker 2018; Gold 2006; Hua 2015; Jeffs 2014; Kipping 2012; Koushali 2017; Nilsson 2009; Walther‐Larsen 2019; Wolitzky 2005). Of these 13 studies, 10 had two groups (Chan 2019; reporting two RCTs); Chen 2019; Gold 2006; Hua 2015; Kipping 2012; Koushali 2017; Nilsson 2009; Walther‐Larsen 2019; Wolitzky 2005) and three had three groups (Dumoulin 2019; Gerceker 2018; Jeffs 2014). Four studies used a cross‐over (within‐subjects) design (Atzori 2018; Das 2005; Hoffman 2019; Schmitt 2011).
We contacted the authors of seven studies to obtain non‐reported mean and standard deviation data (Gold 2006; Jeffs 2014; Kipping 2012; Nilsson 2009; Schmitt 2011; Walther‐Larsen 2019; Wolitzky 2005). Three (Jeffs 2014; Nilsson 2009;Schmitt 2011) responded with data (recorded in Table 4 and Table 5), and one responded stating they no longer had access to the data (Wolitzky 2005).
Study population
The 17 included studies (see Table 6 for PICOs of included studies) had a total of 1008 participants undergoing needle‐related procedures for venepuncture, port access, intravenous placement or intravenous injection (Atzori 2018; Chan 2019; Chen 2019; Dumoulin 2019; Gerceker 2018; Gold 2006; Nilsson 2009; Walther‐Larsen 2019; Wolitzky 2005); wound dressing procedures for chronic wounds and burns (Das 2005; Hoffman 2019; Hua 2015; Jeffs 2014; Kipping 2012; Koushali 2017); and active‐assisted range‐of‐motion physical therapy sessions post burn injuries (Schmitt 2011). Individual study sample sizes ranged from nine (Das 2005) to 136 (Chen 2019) participants.
3. PICOs of included studies.
| STUDY | POPULATION | INTERVENTION | COMPARISON | OUTCOME | STUDY DESIGN |
|
Comparison 1: Virtual reality distraction compared to no distraction Primary Outcome: acute pain intensity |
|||||
| During the procedure: self‐report | |||||
| Nilsson 2009 | 5 to 18 years Cancer Venous puncture or venous port device access procedure |
Non‐immersive VR distraction | No distraction | Colour Analogue Scale (0 to 10; no pain to most pain) |
Parallel group design |
| During the procedure: behavioural measurement (observer‐report) | |||||
| Nilsson 2009 | 5 to 18 years Cancer Venous puncture or subcutaneous venous port device access procedure |
Non‐immersive VR distraction | No distraction | FLACC (nurse‐reported) (total score maximum of 10; higher score indicates more pain) |
Parallel group design |
| Wolitzky 2005 | 7 to 14 years Cancer Port access procedure |
Immersive VR distraction | No distraction | CHEOPS (researcher‐reported) (minimun score 4 = no pain and maximun score 13 = worst pain) | Parallel group design |
| Post‐procedure: self‐report | |||||
| Atzori 2018 | 7 to 17 years Onco‐haematological disease Venipuncture for IV placement during chemotherapy, transfusions, MRI or blood analysis |
Immersive VR distraction | No distraction | Visual Analogue Scale (scale 0 to 10; no pain to worst pain) |
Within‐subject design |
| Chen 2019 | 7 to 12 years Intravenous injections |
Immersive VR distraction | No distraction | Wong Baker faces rating scale (0 to 10; 0 no pain, 10 excruciating pain |
Parallel group design |
| Das 2005 | 5 to 16 years Acute burn injuries Wound dressing change |
Immersive VR distraction | No distraction | Modified self‐report Faces pain (scale 0 to 10; no pain to worst pain) | Within‐subject design |
| Gerceker 2018 | 7 to 12 years Phlebotomy |
Immersive VR distraction | No distraction | Wong Baker Faces pain scale (scale 0 to 10; no pain to worst pain) |
Parallel group design |
| Gold 2006 | 8 to 12 years IV placement for MRI/CT scan |
Immersive VR distraction | No distraction | Faces Pain Scale‐Revised (scale 0 to 10; no pain to very much pain) |
Parallel group design |
| Hoffman 2019 | 6 to 17 years Burn injuries Hydrotank |
Immersive VR distraction | No distraction | Graphic Rating Scale (scale 0 to 10; no pain to worst pain) |
Within‐subject design |
| Jeffs 2014 | 10 to 17 years Burn injuries Wound dressing changes |
Semi‐immersive VR distraction | No distraction | Adolescent Pediatric Pain Tool (scale range 0 to 100; no pain to worst pain) |
Parallel group design |
| Koushali 2017 | 7 to 12 years Burn injuries Wound dressing changes |
Immersive VR distraction | No distraction | Wong Baker Faces pain scale (scale 0 to 10; no pain to worst pain) |
Parallel group design |
| Nilsson 2009 | 5 to 18 years Cancer Venous punctures or subcutaneous venous port device access |
Non‐immersive VR distraction | No distraction | Colour Analogue Scale (scale 0 to 10; no pain to most pain) |
Parallel group design |
| Schmitt 2011 | 6 to 18 years Post burn injuries Active‐assistive range‐of‐motion physical therapy |
Immersive VR distraction | No distraction | Graphic Rating Scale (scale 0 to 100; no pain to worst pain) |
Within‐subject design |
| Post‐procedure: observer‐report | |||||
| Chen 2019 | 7 to 12 years Intravenous injections |
Immersive VR distraction | No distraction | Wong Baker faces rating scale (scale 0 to 10; 0 no pain, 10 excruciating pain) | Parallel group design |
| Gerceker 2018 | 7 to 12 years Phlebotomy |
Immersive VR distraction | No distraction | Visual Analogue Scale (scale 0 to 10; no pain to worst pain) |
Parallel group design |
| Post‐procedure: behavioural measurement (observer‐report) | |||||
| Nilsson 2009 | 5 to 18 years Cancer Venous punctures or subcutaneous venous port device access |
Non‐immersive VR distraction | No distraction | FLACC (nurse‐reported) (total score maximum of 10; higher score indicates more pain) |
Parallel group design |
|
Comparison 2: Virtual reality distraction compared to non‐VR distraction Primary Outcome: acute pain intensity |
|||||
| During the procedure: self‐report | |||||
| Hua 2015 | 4 to 16 years Chronic lower limb wounds Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Toys, television, books, parental comforting |
Wong‐Baker faces pain scale (scale 0 to 5; no pain to worst pain) |
Parallel group design |
| Kipping 2012 | 11 to 17 years Burn injuries Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Television, stories, music or caregivers and child preference for no distraction |
Visual Analogue Scale (scale 0 to 10; no pain to as painful as it could possibly be) |
Parallel group design |
| During the procedure: observer‐report | |||||
| Hua 2015 | 4 to 16 years Chronic lower limb wounds Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Toys, television, books, parental comforting |
Visual Analogue Scale – caregiver ratings (scale 0 to 10; no pain to worst pain) |
Parallel group design |
| Kipping 2012 | 11 to 17 years Burn injuries Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Television, stories, music or caregivers and child preference for no distraction |
Visual Analogue Scale ‐ caregiver ratings (scale 0 to 10; no pain to as painful as it could possibly be) |
Parallel group design |
| During procedure: behavioural measurements (observer‐report) | |||||
| Hua 2015 | 4 to 16 years Chronic lower limb wounds Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Toys, television, books, parental comforting |
FLACC pain rating scale (total score maximum of 10; higher score indicating more pain) |
Parallel group design |
| Kipping 2012 | 11 to 17 years Burn injuries Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Television, stories, music or caregivers and child preference for no distraction |
FLACC pain rating scale (total score maximum of 10; higher score indicating more pain) |
Parallel group design |
| Post‐procedure: self‐report | |||||
|
Chan 2019 Emergency department |
4 to 11 years Venipuncture or intravenous cannulation for any indication (ED dept.) |
Immersive VR distraction | Non‐VR distraction Age‐appropriate distraction such as child‐life therapy, toys, books, and electronic devices. Distractions allowed at discretion of clinician and standardised distractions not mandated to reflect clinical practice. Note: In the non‐VR group, distraction used in 43 patients; with electronic media (TV, video, phones, tablets) in 32 patients |
Faces Pain Scale Revised (scale 0 to 10; no pain to very much pain) |
Parallel group design |
|
Chan 2019 Outpatient pathology |
4 to 11 years Venipuncture or intravenous cannulation for any indication (Outpatients) |
Immersive VR distraction | Non‐VR distraction Age appropriate distraction such as child‐life therapy, toys, books, and electronic devices. Distractions allowed at discretion of clinician and standardised distractions not mandated to reflect clinical practice. Note: In the non‐VR group distraction used in 57 patients with electronic media in 55 patients |
Faces Pain Scale Revised (scale 0 to 10; no pain to very much pain) |
Parallel group design |
| Dumoulin 2019 | 8 to 17 years Needle‐related procedures (blood work, IV, or both) for pending or known diagnostic and visiting ED |
Immersive VR distraction | Non‐VR distraction Two groups 1. Watching TV 2. Child Life program |
Visual Analogue Scale (scale 0 to 100; higher scores indicate more pain) |
Parallel group design |
| Gerceker 2018 | 7 to 12 years Phlebotomy |
Immersive VR distraction | Non‐VR distraction External cold and vibration i.e. Buzzy |
Wong‐Baker faces rating scale (scale 0 to 10; very happy/no pain to hurts worst) |
Parallel group design |
| Hua 2015 | 4 to 16 years Chronic lower limb wounds Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Toys, television, books, parental comforting |
Wong‐Baker faces pain rating scale (scale 0 to 5; higher scores indicate more pain) |
Parallel group design |
| Jeffs 2014 | 10 to 17 years Burn injuries Wound dressing changes |
Semi‐immersive VR distraction | Non‐VR distraction Watching an age‐appropriate movie |
Adolescent Paediatric Pain Tool (scale range 0 to 100; no pain to worst pain) |
Parallel group design |
| Kipping 2012 | 11 to 17 years Burn injuries Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Television, stories, music or caregivers and child preference for no distraction |
Visual Analogue Scale (scale range 0 to 10; no pain to worst pain) |
Parallel group design |
| Walther‐Larsen 2019 | 7 to 16 years Venous cannulation before planned anaesthetic induction |
Immersive VR distraction | Non‐VR distraction Tablet or smartphone to play two‐dimensional game of own choice |
Visual Analogue Scale (scale range 0 to 100; higher score indicates more pain) |
Parallel group design |
| Post‐procedure: observer‐report | |||||
| Gerceker 2018 | 7 to 12 years Phlebotomy |
Immersive VR distraction | Non‐VR distraction External cold and vibration i.e. Buzzy |
Visual Analogue Scale (scale range 0 to 10; no pain to worst pain) |
Parallel group design |
| Hua 2015 | 4 to 16 years Chronic lower limb wounds Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Toys, television, books, parental comforting |
Visual Analogue Scale (scale range 0 to 10; no pain to worst pain) |
Parallel group design |
| Kipping 2012 | 11 to 17 years Burn injuries Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Television, stories, music or caregivers and child preference for no distraction |
Visual Analogue Scale (scale range 0 to 10; no pain to worst pain) |
Parallel group design |
| Post‐procedure: behavioural measurements (observer‐report) | |||||
| Hua 2015 | 4 to 16 years Chronic lower limb wounds Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Toys, television, books, parental comforting |
FLACC pain rating scale (total score maximum of 10; higher score indicating more pain) |
Parallel group design |
| Kipping 2012 | 11 to 17 years Burn injuries Wound dressing changes |
Immersive VR distraction | Non‐VR distraction Television, stories, music or caregivers and child preference for no distraction |
FLACC pain rating scale (total score maximum of 10; higher score indicating more pain) |
Parallel group design |
CHEOPS: Children's Hospital of Eastern Ontario Pain Scale ED: Emergency Department FLACC: Faces, Legs, Activity, Cry, Consolability VR: virtual reality
The studies varied in terms of the age of the included participants ranging from four to 18 years. Age ranges in individual studies were: seven to 17 years (Atzori 2018); four to 11 years (Chan 2019); five to 16 years (Das 2005); eight to 17 years (Dumoulin 2019); seven to 12 years (Chen 2019; Gerceker 2018; Koushali 2017); eight to 12 years (Gold 2006); six to 17 years (Hoffman 2019); four to 16 years (Hua 2015); 10 to 17 years (Jeffs 2014); 11 to 17 years (Kipping 2012); five to 18 years (Nilsson 2009); six to 18 years (Schmitt 2011; one participant was older than 18 years of age and the author shared the data set, which enabled us to extract the results for children age six to 18 years separately); seven to 16 years (Walther‐Larsen 2019); and seven to 14 years (Wolitzky 2005). Across the 17 included studies the total proportion of male participants was 61%; ranging from 40% (Hua 2015) to 88% (Walther‐Larsen 2019).
Of the six studies that included wound dressing change procedures, all studies reported the cause of the burn or wound injury (Das 2005; Hoffman 2019; Hua 2015; Jeffs 2014; Kipping 2012; Koushali 2017), five reported the total body surface area of the burn or wound size (Das 2005; Hua 2015; Jeffs 2014; Kipping 2012), four reported the wound depth (Hoffman 2019; Jeffs 2014; Kipping 2012; Koushali 2017), three reported the wound or burn site (Hoffman 2019; Hua 2015; Koushali 2017), and two reported type of dressing used (Hua 2015; Kipping 2012). Two studies reported recruiting participants who presented for their first, or first conscious, dressing change (Jeffs 2014; Kipping 2012). One study stated that to be included participants had to have had a minimum of one dressing change (Koushali 2017). One study reported that participants enrolled into the study were at either second or third dressing change (Das 2005). Whether participants were recruited for their first dressing change or multiple dressing changes was unclear in one study (Hua 2015). One study stated that pain was measured during at least one day of wound care and for up to 10 study days the patient used VR (Hoffman 2019).
For one study, eligible participants were those who required post‐burn active‐assisted range‐of‐motion physical therapy at least once during their stay in hospital (Schmitt 2011).
Of the 10 studies that included needle‐related procedures, eight reported on participant previous exposure to needle‐related procedures (Atzori 2018; Chan 2019 (reporting two RCTs); Dumoulin 2019; Gerceker 2018; Gold 2006; Nilsson 2009; Wolitzky 2005).
The main exclusion criteria for participants for the included studies were as follows.
Cognitive impairment or other condition which might impact on self‐report outcome measures (Chan 2019; Chen 2019; Das 2005; Dumoulin 2019; Gerceker 2018; Gold 2006; Hoffman 2019; Jeffs 2014; Kipping 2012; Nilsson 2009; Walther‐Larsen 2019).
Factors which might impact on the effective use of the VR intervention such as medical conditions, visual/auditory impairment, wound location/treatment and impaired range of movement (Chan 2019; Chen 2019; Das 2005; Gold 2006; Hoffman 2019; Hua 2015; Jeffs 2014; Kipping 2012; Schmitt 2011; Walther‐Larsen 2019).
Venous access already inserted or cases where topical anaesthesia not properly applied (Atzori 2018; Walther‐Larsen 2019).
No wound cleaning sessions required or burn size less than 10% TBSA (Hoffman 2019).
Receiving pain or sedative (Gold 2006; Hua 2015; Koushali 2017; Walther‐Larsen 2019).
Having a chronic, genetic, critical or secondary illness, or other conditions contributing to pain (Chan 2019; Chen 2019; Gerceker 2018; Hoffman 2019; Hua 2015).
Receiving prophylaxis for alcohol or drug withdrawal (Hoffman 2019); undergoing chemotherapy (Chen 2019); requiring blood transfusions and blood preparation (Chen 2019).
History of psychiatric disorder or demonstrating delirium, psychosis, or organic brain disorder (Hoffman 2019; Walther‐Larsen 2019).
Past history of epilepsy, seizure disorders, motion sickness, headache, dizziness or recent head injury (Atzori 2018; Chen 2019; Das 2005; Dumoulin 2019; Hoffman 2019; Jeffs 2014; Schmitt 2011; Walther‐Larsen 2019).
Unaccompanied by legal guardian (Atzori 2018) or incarcerated minors and minors in foster care (Jeffs 2014).
Communication or language deficiency (Dumoulin 2019; Gerceker 2018; Hoffman 2019; Hua 2015; Kipping 2012; Koushali 2017; Nilsson 2009; Walther‐Larsen 2019).
Child safety and protection issues (Kipping 2012).
Inability to consent/assent (Chan 2019) or refusal to participate (Gerceker 2018; Koushali 2017).
Wanting to use own distraction tool (Atzori 2018).
Medical procedure lasting more than 15 minutes (Dumoulin 2019).
One study did not report any exclusion criteria (Wolitzky 2005).
Setting
The procedures took place in the following settings.
Oncology/haematology units in Italy (Atzori 2018), Sweden (Nilsson 2009), and the US (Wolitzky 2005).
Emergency departments in Australia (Chan 2019), Taiwan (Chen 2019), and Canada (Dumoulin 2019).
Outpatient pathology in Australia (Chan 2019) and phlebotomy unit in Turkey (Gerceker 2018).
Inpatient, outpatient or intensive care burn units in the US (Hoffman 2019; Jeffs 2014; Schmitt 2011), Australia (Das 2005; Kipping 2012), and Iran (Koushali 2017).
Outpatient radiology department in the US (Gold 2006).
A paediatric centre in a tertiary hospital in China (Hua 2015).
Anaesthetic department in Denmark (Walther‐Larsen 2019).
Interventions and comparators
Types of intervention were immersive VR distraction (15 studies; Atzori 2018; Chan 2019 (reporting two RCTs); Chen 2019; Das 2005; Dumoulin 2019; Gerceker 2018; Gold 2006; Hoffman 2019; Hua 2015; Kipping 2012; Koushali 2017; Schmitt 2011; Walther‐Larsen 2019; Wolitzky 2005), semi‐immersive VR distraction (one study; Jeffs 2014), and non‐immersive VR distraction (one study; Nilsson 2009).
The following virtual environments were used.
Snow World originally designed and created at the University of Washington specifically for patients receiving burn wound procedural care (Atzori 2018; Hoffman 2019; Jeffs 2014; Schmitt 2011).
Aquatic environment developed by two of the authors (Chan 2019).
Choice of four applications i.e. roller coasters, space exploration, wildlife park, travel destinations (Chen 2019).
Game software, developed at the University of South Australia based on the game Quake (Das 2005).
Game of shooting flies flying around an apartment developed by Cyberpsychology Lab. University of Quebec Outaouais (Dumoulin 2019).
Choice of three cartoon videos (i.e. Magic English Disney Family, Princess Sofia’s Secret Library, Dinosaur Animation Cartoon) (Gerceker 2018).
Street Luge (skateboard), by Fifth Dimension Technologies (Gold 2006).
Chinese version of Ice Age 2: Meltdown game (Hua 2015)
Game Chicken LittleTM for ages 11 to 13 years and Need for SpeedTM for ages 14 to 17 years (Kipping 2012).
Smash Hit designed by Mediocre Company in musical arcade style (Koushali 2017).
The Hunt of the diamonds developed by Digital Content Creation software and Adobe Photoshop (Nilsson 2009).
Seagull Splash custom made for needle procedures in collaboration with Khora VR Denmark (Walther‐Larsen 2019).
Educational supplement for children visiting gorilla habitat at Zoo Atlanta (Wolitzky 2005).
Nine studies included no distraction as a comparison group (Atzori 2018; Chen 2019; Das 2005; Gold 2006; Hoffman 2019; Koushali 2017; Nilsson 2009; Schmitt 2011; Wolitzky 2005).
Six studies included non‐VR distractions as comparator groups (Chan 2019 (reporting two RCTs); Dumoulin 2019; Hua 2015; Kipping 2012; Walther‐Larsen 2019). Non‐VR distractions included age‐appropriate distractions such as child‐life therapy, toys, books, and electronic devices allowed at discretion of clinician (Chan 2019); toys, television, books, parental comforting (Hua 2015); television, stories, music or caregivers and child preference for no distraction (Kipping 2012); tablet or smart phone playing a two‐dimensional game of own choice (Walther‐Larsen 2019). One study included two non‐VR distraction comparison groups: one group watched TV via a portable DVD player with video of their choice and a second group received a Child Life program where three preselected activities were provided (Dumoulin 2019),
Two studies included both no distraction and non‐VR distraction as two comparison groups with non‐VR distraction defined as Buzzy a reusable bee which provides both cold compression and vibration in one study (Gerceker 2018) and as watching an age appropriate movie in one study (Jeffs 2014).
Funding sources
Of the 17 included studies, four were supported by funding from research foundations/institutes and donations (Gold 2006; Jeffs 2014; Nilsson 2009; Schmitt 2011), three received support from universities (Chen 2019; Gerceker 2018; Koushali 2017); two received funding from combined sources (i.e. research institute grants, hospital funds, donations, university and foundations) (Atzori 2018; Hoffman 2019); two were was supported by government department of industry, innovation and science (Chan 2019); one was supported by grants from Diversionary Therapy Technologies (Kipping 2012) and one was funded by Khore Virtual Reality Denmark and Kristian Bluff (Motivates) and received donations for software development (Walther‐Larsen 2019). Four studies reported no source of funding (Das 2005; Dumoulin 2019; Hua 2015; Wolitzky 2005).
Declarations of interest were not reported in seven studies (Atzori 2018; Gold 2006; Hoffman 2019; Hua 2015; Jeffs 2014; Koushali 2017; Wolitzky 2005). Ten studies reported declarations of interest statements (Chan 2019 (two RCTs); Chen 2019; Das 2005; Dumoulin 2019; Gerceker 2018; Kipping 2012; Nilsson 2009; Schmitt 2011; Walther‐Larsen 2019).
Excluded studies
See Characteristics of excluded studies.
We excluded 65 studies (reported in 70 citations) after reading full‐texts for the following reasons.
Not a randomised controlled trial (seven studies; Chan 2007; Diaz‐Hennessey 2019; Fonseca 2018; Gold 2005; LeMay 2017a; Shah 2018; Sharar 2008).
Not VR (immersive or non‐immersive) distraction according to our protocol criteria (24 studies; Altmann 2017; Babaie 2019; Blunt 1998; Brown 2014; Burns‐Nader 2013; Celikol 2019; Dosani 2019; Eijlers 2017; Feng 2018; Ferullo 2017; Inan 2019; Kumar 2017; Lozano 2018; MacLaren 2005; Miller 2010; Miller 2011; Miller 2016; Minute 2012; Mott 2008; Newell 2018; Nilsson 2013; Tschiedel 2019; vanRooijen 2017; Windlich‐Biermeier 2007; Zelmar 2015).
Not possible to isolate the effects of VR from a multi‐component intervention (one study; Wolyniez 2013).
Included participants older than 18 years; for published papers that included both children and adults we contacted the authors of these papers with requests for separate data for children 18 years or younger and in cases where we received no response from authors we excluded the paper (15 studies; Canares 2018; Gershon 2004; Gold 2018; Hoffman 2001; Hoffman 2004b; Hoffman 2008; Marteau 2018; Leibovici 2009; Mosso 2008; Parker 2016; Patterson 2010; Sharer 2007; Small 2015; vanGoor 2019; Wint 2002).
Included healthy volunteers (one study; Hoffman 2015).
Did not report pain as an outcome (three studies; Beale 2006, Goldman 2018a; Li 2011).
Focus was experimental pain not in a healthcare setting (one study; Dahlquist 2010).
Abstract form only available with insufficient study detail and results to include in the review (nine studies; Gilbert 2014; Gonzalez 2016; Hoffman 2012; Jeffs 2013; Miller 2009; Nilsson 2007; Tropez‐Arceneaux 2011; Ver Lee 2012; Yuan 2018).
Trial was not completed; confirmed through email correspondence with the authors (three studies; Faucher 2007; Jeffs 2010; LeMay 2016a).
Ongoing studies
See Characteristics of ongoing studies.
Thirty studies (reported in 32 citations) are ongoing. Twenty‐seven of the ongoing studies are registered with ClinicalTrials.gov (NCT03584776; NCT03521076; NCT03480724; NCT03985930; NCT03903510; NCT04040036; NCT03681730; NCT03681717; NCT03681743; NCT03693469; NCT03155607; NCT02986464; LeMay 2016b; NCT03680625; NCT03888690; NCT03784352; NCT03750578; NCT03913897; NCT02646787; NCT03239743; NCT03353584; NCT03464955; NCT03304769; NCT03518346; NCT03645213; NCT02929771; NCT03435367), two are registered with the Australian New Zealand Clinical Trials Registry (ACTRN12617000285358; ACTRN12618001363279) and one is registered with the Chinese Clinical Trial Registry (Wong 2019). Eleven of these studies are being conducted in the USA, eleven in Canada, three in Turkey, two in Australia, one in France, one in Hong Kong and one in Colombia. These ongoing studies are listed below.
Thirteen studies of VR for needle related procedures (i.e. intravenous cannulation, venipuncture, intramuscular medication, immunisation) (ACTRN12617000285358; NCT03985930; ACTRN12618001363279; NCT04040036; NCT03693469; NCT03681730; NCT03750578; NCT03913897; NCT03304769; NCT03518346; NCT03645213; NCT03435367; Wong 2019).
Four studies of VR for wound dressing care or physiotherapy and hydrotherapy for burns or other injuries (NCT03155607; NCT02986464; LeMay 2016b; NCT02646787).
Two studies of VR for post‐operative pain management (NCT03584776; NCT03239743).
Two studies of VR for botulinum toxin injections for spasticity management (NCT03521076; NCT03480724).
One study of VR for pain management of vaso‐occlusive crisis with sickle cell disease (NCT03353584).
One study of VR for pain management for non‐invasive surgical sub‐specialty procedures (NCT03464955).
One study of VR for procedural pain in children with cancer (NCT02929771).
One study of VR for invasive procedures in onco‐haematology unit (NCT03888690).
One study for VR for cast removal (NCT03903510)
Two studies for VR for orthopaedic outpatient procedures (NCT03680625; NCT03784352)
One study for VR for laceration repair (NCT03681717)
One study for VR for minor plastic surgery procedures (NCT03681743)
Studies awaiting classification
See Characteristics of studies awaiting classification.
We identified four studies as awaiting classification. All four studies are registered with ClinicalTrials.gov. Our initial attempts to contact authors, or to identify subsequent publications, were not successful (Festini 2016; Meyer 2014; NCH 2016; Patterson 2009). If we identify further reports from these studies, we will reassess eligibility.
Risk of bias in included studies
We have summarised ‘Risk of bias’ results in Figure 2 and Figure 3.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation
We judged thirteen studies to be at low risk of bias as methods used to generate the random sequence were adequately described (Chan 2019 (two RCTs); Chen 2019; Das 2005; Dumoulin 2019; Gerceker 2018; Hoffman 2019; Hua 2015; Jeffs 2014; Kipping 2012; Koushali 2017; Schmitt 2011; Walther‐Larsen 2019), and four to be at unclear risk of bias because insufficient information was provided on the process for random sequence generation (Atzori 2018; Gold 2006; Nilsson 2009; Wolitzky 2005).
Allocation concealment
We judged six studies to be at low risk of bias because the methods of how allocation was concealed were adequately described (Chan 2019 (two RCTs); Chen 2019; Dumoulin 2019; Gerceker 2018; Kipping 2012), and eleven to be at unclear risk of bias because insufficient information was provided about how allocation was concealed (Atzori 2018; Das 2005; Gold 2006; Hoffman 2019; Hua 2015; Jeffs 2014; Koushali 2017; Nilsson 2009; Schmitt 2011; Walther‐Larsen 2019; Wolitzky 2005).
Blinding
Performance bias
We judged sixteen studies to be at high risk of bias because there was no blinding, blinding was not described (but due to the nature of the intervention was highly unlikely), or reported as not blinded, due to the nature of the intervention (Atzori 2018; Chan 2019 (two RCTs); Chen 2019; Das 2005; Dumoulin 2019; Gerceker 2018; Gold 2006; Hoffman 2019; Hua 2015; Jeffs 2014; Kipping 2012; Nilsson 2009; Schmitt 2011; Walther‐Larsen 2019; Wolitzky 2005), and one study to be at unclear risk of bias because insufficient information was available (Koushali 2017).
Detection bias
We judged sixteen studies to be at high risk of bias because there was no blinding, blinding was not described (but due to the nature of the intervention was highly unlikely), or reported as not blinded, due to the nature of the intervention (Atzori 2018; Chan 2019 (two RCTs); Chen 2019; Das 2005; Dumoulin 2019; Gold 2006; Hoffman 2019; Hua 2015; Jeffs 2014; Kipping 2012; Koushali 2017; Nilsson 2009; Schmitt 2011; Walther‐Larsen 2019; Wolitzky 2005), and one study to be at unclear risk of bias because insufficient information was available (Gerceker 2018).
Incomplete outcome data
We judged fifteen studies to be at low risk of bias because all participant numbers were accounted for (Chan 2019 (two RCTs); Chen 2019; Dumoulin 2019; Gerceker 2018; Gold 2006; Hoffman 2019; Hua 2015; Jeffs 2014; Kipping 2012; Koushali 2017; Nilsson 2009; Schmitt 2011; Wolitzky 2005), and two to be at high risk of bias because of greater than 10% missing data (Atzori 2018; Das 2005).
Selective reporting
We judged thirteen studies to be at low risk of bias as pre‐specified outcomes were reported (Atzori 2018; Chan 2019 (two RCTs); Chen 2019; Das 2005; Dumoulin 2019; Gerceker 2018; Gold 2006; Hoffman 2019; Hua 2015; Kipping 2012; Koushali 2017; Nilsson 2009), and four to be at high risk of bias because not all outcomes were pre‐specified and data could not be used (Jeffs 2014; Schmitt 2011; Walther‐Larsen 2019; Wolitzky 2005).
Other potential sources of bias
Size of study
Following PaPaS review group guidance, we assessed the size of the trial as a potential other source of bias. We judged thirteen studies to be at high risk of bias because these studies had less than 50 participants per treatment arm (Atzori 2018; Das 2005; Dumoulin 2019; Gerceker 2018; Gold 2006; Hoffman 2019; Hua 2015; Jeffs 2014; Kipping 2012; Koushali 2017; Nilsson 2009; Walther‐Larsen 2019; Wolitzky 2005), and four to be at unclear risk of bias because these studies had 50 to 199 participants per treatment arm (Chan 2019 (two RCTs); Chen 2019; Schmitt 2011).
Other bias
We judged fourteen studies to be at low risk of other bias because no other bias was identified (Atzori 2018; Chan 2019 (two RCTs); Chen 2019; Dumoulin 2019; Gerceker 2018; Gold 2006; Hua 2015; Jeffs 2014; Kipping 2012; Koushali 2017; Schmitt 2011; Walther‐Larsen 2019; Wolitzky 2005). We judged one study to be at high risk of bias because the trial design (i.e. exposure to VR and no VR was repeatedly alternated every five minutes) made it difficult to be conclusive about the results (Hoffman 2019); and two studies to be at unclear risk of bias because there was insufficient information to assess whether a risk of bias existed due to the trial design (i.e. the order in which children had wound dressings done; some children had multiple dressings performed) (Das 2005); or differences in the procedures (i.e. insertion of subcutaneous venous port devices or venous punctures) received by participants in the control and intervention groups (Nilsson 2009).
Effects of interventions
See: Table 1; Table 2; Table 3
Comparison 1: VR distraction compared to no distraction
Primary outcome: acute pain intensity
1. During the procedure
a. Acute pain intensity: self‐report
This was reported in one study (42 participants; Nilsson 2009). The study found no evidence of a beneficial effect of non‐immersive VR compared to no distraction as measured using the Colour Analogue Scale (scale range 0 to 10; 0 = no pain, 10 = most pain) (Mean Difference (MD) 0.56, 95% Confidence Interval (CI) ‐0.95 to 2.07).
We judged this to be very low‐certainty evidence, downgraded for serious study limitations, and very serious imprecision (Table 1).
b. Acute pain intensity: observer‐report
We did not find any studies that reported this.
c. Acute pain intensity: behavioural measurement (observer‐report)
This was reported in two studies (62 participants; Nilsson 2009; Wolitzky 2005). One study used the FLACC observer‐reported pain rating scale (total score out of maximum 10; higher score indicates more pain) (Nilsson 2009). One study used the CHEOPS observer‐reported pain rating scale (minimum possible score of 4 = no pain, maximum possible score 13 = worst pain) (Wolitzky 2005).
Nilsson 2009 (n = 42) found no evidence of a beneficial effect of non‐immersive VR compared to no distraction for nurse observer‐reported pain (MD ‐0.57, 95% CI ‐1.66 to 0.52). Wolitzky 2005 (n = 20) found evidence of a beneficial effect favouring immersive VR compared to no distraction for researcher observer‐reported pain (MD ‐3.40, 95% CI ‐5.01 to ‐1.79).
We judged this to be low‐certainty evidence, downgraded for serious study limitations, and serious indirectness.
2. Post‐procedure (up to one hour)
a. Acute pain intensity: self‐report
This was reported in ten studies (461 participants; Atzori 2018; Chen 2019; Das 2005; Gerceker 2018; Gold 2006; Hoffman 2019; Jeffs 2014; Koushali 2017; Nilsson 2009; Schmitt 2011).
Atzori 2018 used a Visual Analogue Scale (scale range 0 to 10; no pain to worst pain). Chen 2019, Gerceker 2018 and Koushali 2017 used the Wong Baker Faces pain scale (scale range 0 to 10; no pain to worst/excruciating pain). Das 2005 used a modified Faces pain scale in combination with a visual analogue scale of 0 to 10 (higher score indicates more pain).Gold 2006 used both the Wong‐Baker Faces and the Faces Pain Scale‐Revised rating scales. We report the FPS‐R scale (scale range 0 to 10; no pain to very much pain) in this review because this scale is recommended for assessing self‐report pain intensity in clinical trials for children (Stinson 2006; McGrath 2008). Hoffman 2019 used a Graphic Rating Scale (scale range 0 to 10; no pain to worst pain). Jeffs 2014 used the Adolescent Pediatric Pain Tool (scale range 0 to 100; no pain to worst pain). Nilsson 2009 used the Colour Analogue Scale (scale range 0 to 10; no pain to most pain). Schmitt 2011 used a Graphic Rating Scale (scale range 0 to 100; no pain to worst pain).
Four studies (n = 95) found no evidence of a beneficial effect of immersive (MD ‐1.60, 95% CI ‐3.24 to 0.04; Atzori 2018) and (MD ‐0.60, 95% CI ‐2.47 to 1.27; Gold 2006), semi‐immersive (MD 21.20, 95% CI ‐8.31 to 50.71; Jeffs 2014) or non‐immersive VR (MD 0.54, 95% CI ‐0.32 to 1.40; Nilsson 2009) compared to no distraction.
Five studies (n = 357) found evidence of a beneficial effect favouring immersive VR compared to no distraction (MD ‐1.00, 95% CI ‐1.90 to ‐0.10; Chen 2019) and (MD ‐3.60, 95% CI ‐3.74 to ‐3.46; Gerceker 2018) and (MD ‐3.42, 95% CI ‐4.47 to ‐2.37; Hoffman 2019) and (MD ‐2.90, 95% CI ‐3.57 to ‐2.23; Koushali 2017) and (MD ‐14.33, 95% CI ‐25.42 to ‐3.24; Schmitt 2011). Another study (n = 9) reported less pain in the immersive VR group (Mean 1.3, SD 1.8) than the no distraction group (Mean 4.1, SD 2.9) (Das 2005).
We judged this to be very low‐certainty evidence, downgraded for serious study limitations, and very serious indirectness.
b. Acute pain intensity: observer‐report
This was reported in two studies (216 participants; Chen 2019; Gerceker 2018). Chen 2019 used the Wong Baker Faces pain scale (scale range 0 to 10; no pain to worst pain). Gerceker 2018 used a Visual Analogue Scale (scale range 0 to 10; no pain to worst pain).
Two studies (n = 216) found evidence of a beneficial effect of immersive VR compared to no distraction for primary caregiver/parent (MD ‐1.03, 95% CI ‐1.88 to ‐0.18; Chen 2019 and MD ‐3.20, 95% CI ‐3.34 to ‐3.06; Gerceker 2018) and nurse (MD ‐1.00, 95% CI ‐1.77 to ‐0.23; Chen 2019 and MD ‐2.70, 95% CI ‐2.81 to ‐2.59; Gerceker 2018) observer‐reports of child pain. One study (n = 80) found evidence of a beneficial effect of immersive VR compared to no distraction for researcher observer‐reports of child pain (MD ‐4.10, 95% CI ‐4.24 to ‐3.96; Gerceker 2018).
We judged this to be low‐certainty evidence, downgraded for serious study limitations, and serious indirectness.
c. Acute pain intensity: behavioural measurement (observer‐report)
This was reported in one study (42 participants; Nilsson 2009). The study found no evidence of a beneficial effect of non‐immersive VR compared to no distraction for nurse observer‐reported pain (MD 0.10, 95% CI ‐0.22 to 0.42) as measured used the FLACC observer‐reported pain rating scale (total score out of maximum 10; higher score indicates pain).
We judged this to be very low‐certainty evidence, downgraded for serious study limitations, and very serious imprecision.
Secondary outcomes
Adverse effects related to engagement with VR
Adverse effects related to VR were reported in five studies (154 participants; Atzori 2018; Gold 2006; Hoffman 2019; Jeffs 2014; Schmitt 2011).
Atzori 2018 assessed nausea in both VR and no VR conditions using a Visual Analogue Scale (scale range 0 to 10; none to worst nausea). Gold 2006 used the Child Simulator Sickness Questionnaire to determine whether the child felt sick as a result of the intervention. Hoffman 2019 assessed nausea as a result of VR using a Graphic Rating Scale (scale range 0 to 10; no nausea to vomit). Jeffs 2014 did not report what measure was used to assess adverse effects. Schmitt 2011 used a Graphic Rating Scale (scale range 0 to 100; no nausea to severe nausea) to assess nausea in the VR condition.
Two studies (n = 38) reported no adverse effects (Gold 2006; Jeffs 2014). One study (Atzori 2018; n = 15) found evidence of no evidence of a difference for nausea levels between immersive VR and non‐VR distraction conditions. Hoffman 2019 (n = 48) reported that VR nausea was less than one on a 10 point scale. Schmitt 2011 (n = 53) reported some mild nausea symptoms in the VR treatment group.
We judged this to be very low‐certainty evidence, downgraded for serious study limitations, and very serious indirectness.
Child satisfaction with VR
We did not find any studies that reported child satisfaction with VR.
Child pain‐related distress (including anxiety, fear and/or stress)
Child pain‐related distress was reported in three studies (198 participants; Chen 2019; Nilsson 2009; Wolitzky 2005). Chen 2019 used the Children Fear Scale (scale range 0 to 4; no fear to extreme fear). Nilsson 2009 used the Facial Affective Scale (FAS; scale range 0 to 1 from least to most distressed). Wolitzky 2005 used Visual Analogue Scales (scale range 0 to 100; none to maximum pain or anxiety) to report a composite distress score (i.e. mean of self‐report of anxiety and pain).
Chen 2019 found evidence of a beneficial effect of immersive VR compared to no distraction for reducing child fear (MD ‐0.46, 95% CI ‐0.90 to ‐0.02). Nilsson 2009 found no evidence of a beneficial effect for non‐immersive VR compared to no distraction for reducing pain‐related distress (MD ‐0.06, 95% CI ‐0.21 to 0.09). Wolitzky 2005 found no evidence of a difference in distress between those receiving immersive VR and no distraction (Table 4).
We judged this to be low‐certainty evidence, downgraded for serious study limitations, and serious indirectness.
Parent anxiety
We did not find any studies that reported parent anxiety.
Administration of rescue analgesia
We did not find any studies that reported administration of rescue analgesia.
Cost
We did not find any studies that reported cost.
Subgroup analyses
We did not perform meta‐analysis on any data and were not able to conduct subgroup analyses on data for this comparison.
Sensitivity analyses
We did not perform meta‐analysis on any data and were not able to conduct sensitivity analyses on data for this comparison.
Comparison 2: VR distraction compared to non‐VR distraction
Primary outcome: acute pain intensity
1. During the procedure
a. Acute pain intensity: self‐report
This was reported in two studies (106 participants; Hua 2015; Kipping 2012). Hua 2015 used the Wong‐Baker faces pain rating scale (scale range 0 to 5; no pain to worst pain). Kipping 2012 used a Visual Analogue Scale (scale range 0 to 10; from no pain to pain as bad as it could possibly be).
Hua 2015 (n = 65) found evidence of a beneficial effect favouring immersive VR compared to non‐VR distraction (MD ‐1.77, 95% CI ‐2.74 to ‐0.80). Kipping 2012 (n = 41) found no evidence of a difference in mean pain change scores between immersive VR and non‐VR distraction (Table 5).
We judged this to be very low‐certainty evidence, downgraded for serious study limitations, and very serious indirectness (Table 2).
b. Acute pain intensity: observer‐report
This was reported in two studies (106 participants; Hua 2015; Kipping 2012). The two studies used a Visual Analogue Scale to record caregiver ratings (scale ranges 0 to 10; no pain to worst pain).
Hua 2015 (n = 65) found evidence of a beneficial effect favouring immersive VR compared to non‐VR distraction (MD ‐1.90, 95% CI ‐3.23 to ‐0.57). Kipping 2012 (n = 41) found no evidence of a difference in mean pain change score between immersive VR and non‐VR distraction (Table 5).
We judged this to be low‐certainty evidence, downgraded for serious study limitations, and serious indirectness.
c. Acute pain intensity: behavioural measurements (observer‐report)
This was reported in two studies (106 participants; Hua 2015; Kipping 2012). The two studies used the FLACC pain rating scale to record nurse ratings (total score out of maximum 10; higher score indicates more pain).
Hua 2015 (n = 65) found evidence of a beneficial effect favouring immersive VR compared to non‐VR distraction (MD ‐3.18, 95% CI ‐4.75 to ‐1.61). Kipping 2012 (n = 41) found evidence of a difference in mean pain change scores between immersive VR and non‐VR distraction with fewer pain behaviours observed for the VR group (Table 5).
We judged this to be low‐certainty evidence, downgraded for serious study limitations, and serious indirectness.
2. Post‐procedure (up to one hour)
a. Acute pain intensity: self‐report
This was reported in eight studies (575 participants; Chan 2019 (two RCTs); Dumoulin 2019; Gerceker 2018; Hua 2015; Jeffs 2014; Kipping 2012; Walther‐Larsen 2019).
Chan 2019 used the Faces Pain Scale‐Revised (scale range 0 to 10; no pain to very much pain).Gerceker 2018 used the Wong‐Baker faces rating scale (scale range 0 to 10; 0 = very happy/no pain, 10 = hurts worst). Hua 2015 used the Wong‐Baker faces pain rating scale (scale range 0 to 5; higher score indicates more pain). Dumoulin 2019 and Walther‐Larsen 2019 used a Visual Analogue Scale (scale range 0 to 100; higher score indicates more pain). Kipping 2012 used a Visual Analogue Scale (scale range 0 to 10; 0 = no pain, 10 = pain as bad as it could possibly be). Jeffs 2014 used the Adolescent Pediatric Pain Tool (scale range 0 to 100; higher score indicates more pain).
Two studies (n = 146) found evidence of a beneficial effect favouring immersive VR compared to non‐VR distraction (MD ‐0.90, 95% CI ‐1.70 to ‐0.10; Hua 2015 and MD ‐0.50, 95% CI ‐0.59 to ‐0.41; Gerceker 2018). Chan 2019 (two RCTs; n = 252) reported evidence of a between group difference favouring immersive VR compared to non‐VR distraction (Table 5).
One study (n = 59) found no evidence of a beneficial effect of immersive VR compared with TV (MD ‐13.68, 95% CI ‐29.64 to 2.28) and Child Life (MD ‐3.58, 95% CI ‐19.31 to 12.15) non‐VR distraction (Dumoulin 2019). One study (n = 18) found no evidence of a beneficial effect of semi‐immersive VR compared with non‐VR distraction (MD 28.00, 95% CI ‐0.46 to 56.46; Jeffs 2014). Two studies (Kipping 2012; Walther‐Larsen 2019; n = 100) reported no evidence of a between group difference in pain scores between immersive VR and non‐VR distraction (Table 5).
We judged this to be very low‐certainty evidence, downgraded for serious study limitations, and very serious indirectness.
b. Acute pain intensity: observer‐report
This was reported in three studies (187 participants; Gerceker 2018; Hua 2015; Kipping 2012). The three studies used a Visual Analogue Scale (scale range 0 to 10; no pain to worst pain).
Gerceker 2018 (n = 81) found evidence of a beneficial effect favouring immersive VR compared to non‐VR distraction for parent (MD ‐0.50, 95% CI ‐0.59 to ‐0.41), nurse (MD ‐0.20, 95% CI ‐0.27 to ‐0.13) and researcher (MD ‐0.50, 95% CI ‐0.59 to ‐0.41) observer‐reports. Hua 2015 (n = 65) also found evidence of a beneficial effect favouring immersive VR compared with non‐VR distraction for caregiver observer‐reports (MD ‐3.27, 95% CI ‐4.12 to ‐2.42). Kipping 2012 (n = 41) reported no evidence of a difference in mean pain change scores between immersive VR and non‐VR distraction for caregiver ratings (Table 5).
We judged this to be low‐certainty evidence, downgraded for serious study limitations, and serious indirectness.
c. Acute pain intensity: behavioural measurements (observer‐report)
This was reported in two studies (106 participants; Hua 2015; Kipping 2012), as measured by the FLACC pain rating scale (total score of maximum 10; higher score indicates more pain). Hua 2015 (n = 65) found evidence of a beneficial effect favouring immersive VR compared with non‐VR distraction (MD ‐2.11, 95% CI ‐3.73 to ‐0.49). Kipping 2012 (n = 41) reported no evidence of a difference in mean pain change scores between immersive VR and non‐VR distraction (Table 5).
We judged this to be low‐certainty evidence, downgraded for serious study limitations, and serious indirectness.
Secondary outcomes
Adverse effects related to engagement with VR
Adverse effects were reported in six studies (429 participants; Chan 2019 (two RCTs); Dumoulin 2019; Jeffs 2014; Kipping 2012; Walther‐Larsen 2019). Dumoulin 2019 assessed the side effects of VR immersion using a rating scale of how much nausea was experienced in the VR distraction group. Kipping 2012 used a Visual Analogue Scale (scale range 0 to 10; no sick tummy (i.e., nausea) to sick tummy as bad as it could possibly be) to measure nausea associated with VR simulator sickness. Four studies did not report what measure was used to monitor adverse effects related with VR (Chan 2019 (two RCTs); Jeffs 2014; Walther‐Larsen 2019).
Three studies (n = 229) (Chan 2019; one RCT pathology); Kipping 2012; Walther‐Larsen 2019) found no evidence of a difference between immersive VR and non‐VR distraction groups for adverse effects (Table 5). Chan 2019 (one RCT emergency department; n = 123) reported that four participants in the non‐VR distraction group had adverse effects (i.e. dizziness, nausea, headache, vomiting) but there were no adverse effects in the VR distraction group. Dumoulin 2019 (n = 59) reported that the change in estimated cyber sickness before and after VR immersion was not significant (Table 5). Jeffs 2014 (n = 18) reported that no participants in the VR group reported seizures, nausea or adverse motion effects.
We judged this to be very low‐certainty evidence, downgraded for serious study limitations, and very serious indirectness.
Child satisfaction with VR
This was reported in two studies (118 participants; Dumoulin 2019; Walther‐Larsen 2019). The two studies assessed child satisfaction using a Visual Analogue Scale (scale range 0 to 100; higher scores indicate higher satisfaction).
Dumoulin 2019 found no evidence of a beneficial effect of immersive VR compared with Child Life non‐VR distraction (MD 0.00, 95% CI ‐11.19 to 11.19) and evidence of a beneficial effect of immersive VR compared with TV non‐VR distraction (MD 18.43, 95% CI 7.54 to 29.32). Walther‐Larsen 2019 reported no evidence of a difference between immersive VR and non‐VR groups for satisfaction with distraction measures (Table 5).
We judged this to be low‐certainty evidence, downgraded for serious study limitations, and serious indirectness.
Child pain‐related distress (including anxiety, fear and/or stress)
This was reported in three studies (311 participants; Chan 2019 (two RCTs); Dumoulin 2019). Chan 2019 measured child anxiety using a Visual Analogue Thermometer (scale range 0 to 10; no anxiety to most anxiety). Dumoulin 2019 measured child fear of pain using a Visual Analogue Scale (scale range 0‐100; from least to most fear).
Chan 2019 (for two RCTs) reported evidence of a between group difference in child self‐rated anxiety in the VR group compared to the non‐VR distraction group (Table 5). Dumoulin 2019 found no evidence of a beneficial effect for immersive VR compared to TV (MD ‐15.67, 95% CI ‐32.78 to 1.44) and Child Life (Child Life; MD ‐9.58, 95% CI ‐29.34 to 10.18) non‐VR distraction.
We judged this to be very low‐certainty evidence, downgraded for serious study limitations, and very serious indirectness.
Parent anxiety
We did not find any studies that reported parent anxiety.
Administration of rescue analgesia
Administration of rescue analgesia was reported in one study (41 participants; Kipping 2012). The study measured frequency of rescue analgesia (i.e. Entonox doses prescribed after commencement of procedure) requirement. Less frequent administration of rescue analgesia was observed in the VR intervention group (Table 5).
We judged this to be low‐certainty evidence, downgraded for serious study limitations and serious imprecision.
Cost
We did not find any studies that reported cost.
Subgroup analyses
We did not perform meta‐analysis on any data and were not able to conduct subgroup analyses on data for this comparison.
Sensitivity analyses
We did not perform meta‐analysis on any data and were not able to conduct sensitivity analyses on data for this comparison.
Comparison 3: VR distraction compared to other VR distraction
No studies reported this comparison (Table 3).
Discussion
Summary of main results
The aim of this review was to assess the effectiveness and adverse effects of VR (immersive and non‐immersive) distraction interventions for reducing acute pain intensity in children (0 to 18 years) in any healthcare setting. We identified 17 studies with 1008 participants aged between four and 18 years undergoing treatments and procedures for intravenous puncture or port access, wound dressing changes, and physical therapy sessions.
The primary outcomes of the review were acute pain intensity (self‐report, observer‐report and behavioural measurement) assessed during and up to one‐hour post‐procedure. The secondary outcomes were adverse effects related to VR, child satisfaction with VR, child pain‐related distress, parent anxiety, administration of rescue analgesia and cost.
We aimed to include studies of VR distraction compared to no distraction, other non‐VR distraction and other VR distraction.
VR distraction compared to no distraction
For acute pain intensity during the procedure we found no evidence of an effect of VR (non‐immersive) for self‐reported pain compared to no distraction. No data were reported for observer‐reported pain. For behavioural measurement (observer‐reported) of pain we found inconsistent evidence of an effect of VR (immersive and non‐immersive).
For acute pain intensity up to one‐hour post‐procedure we found inconsistent evidence of an effect of VR (immersive, semi‐immersive and non‐immersive) for self‐reported pain compared to no distraction. For observer‐reported pain we found evidence of a beneficial effect of immersive VR compared to no distraction. For behavioural measurement (observer‐reported) of pain we found no evidence of an effect of VR (non‐immersive).
For secondary outcomes, there was insufficient and inconsistent evidence to draw a conclusion on adverse effects related to VR. We found inconsistent evidence of an effect of VR for child pain related distress. No studies assessed child satisfaction with VR, parent anxiety, administration of rescue analgesia, and cost.
The GRADE rating for all outcomes for VR distraction compared to no distraction indicated low to very low certainty of evidence meaning we have little confidence in the results. We downgraded the ratings due to serious limitations of study quality, serious or very serious indirectness; and for some outcomes very serious imprecision.
VR distraction compared to other non‐VR distraction
For acute pain intensity during the procedure we found inconsistent evidence of a beneficial effect favouring VR (immersive) for self‐reported and observer‐reported pain compared to other non‐VR distraction. For behavioural measurement (observer‐reported) of pain we found evidence of a beneficial effect for immersive VR compared to other non‐VR distraction.
For acute pain intensity up to one‐hour post‐procedure we found inconsistent evidence of an effect of VR (semi‐immersive and immersive) for self‐reported pain compared to other non‐VR distraction. For observer‐reported pain and behavioural measurement (observer‐reported) of pain we also found inconsistent evidence of an effect of VR (immersive) compared to other non‐VR distraction.
For secondary outcomes, there was insufficient evidence to draw a conclusion on adverse effects related to VR. We found inconsistent evidence of an effect of VR for child satisfaction with VR and for child pain related distress. One study reported less frequent administration of rescue analgesia in the VR intervention group. No studies assessed parent anxiety or cost.
The GRADE rating for all outcomes for VR distraction compared to other non‐VR distraction indicated low to very low certainty of evidence meaning we have little confidence in the results. We downgraded ratings due to serious limitations of study quality, and serious or very serious indirectness.
VR distraction compared to other VR interventions
We found no studies that reported this comparison.
Overall completeness and applicability of evidence
The limited, low‐ to very low‐certainty evidence in this review means that the review question remains incompletely answered. We were unable to draw conclusions about the effectiveness and adverse effects of VR distraction interventions, compared to no distraction, non‐VR distraction or other VR distraction, for children with acute pain in any healthcare setting. Included studies targeted children aged between four and 18 years undergoing needle‐related procedures for venipuncture, port access or intravenous placement; wound dressing procedures for chronic wounds and burns; and active‐assisted range‐of‐motion physical therapy sessions post burn injuries in specific inpatient and outpatient paediatric healthcare settings (i.e. burn units, oncology units, emergency departments, pathology/phlebotomy units, radiology and anaesthetic departments).
The clinical heterogeneity of the child participant populations in terms of age (i.e. seven to 17 years; four to 11 years; five to 16 years; eight to 17 years; seven to 12 years; eight to 12 years; six to 17 years; four to 16 years; 10 to 17 years; 11 to 17 years; five to 18 years; six to 18 years; seven to 16 years; and seven to 14 years) and variations in procedural and treatment conditions (i.e. venipuncture, port access, intravenous placement, wound dressings, physical therapy sessions) across the included studies made statistical pooling of data impossible. Most of the review primary outcomes were assessed by only a small number of studies with small sample sizes. The following secondary outcomes were not measured in any of the included studies: parent anxiety or cost. We found limited data for the remaining secondary outcomes of adverse effects related to VR, child pain‐related distress and administration of rescue analgesia; therefore, we can draw no conclusions related to these outcomes.
Quality of the evidence
We noted that a number of studies reported insufficient information about sequence generation and allocation concealment and we judged them to be at unclear risk of bias. We judged the majority of studies to be at high risk of bias for blinding participants and study personnel, and blinding of outcome assessment, because blinding did not take place, was broken, was not described but due to the nature of the intervention blinding was highly unlikely or was reported as not blinded, due to the nature of the intervention. We also judged a number of studies to be at high risk of bias for selective reporting and the majority of studies to be at high risk of bias for small sample sizes.
We used the GRADE approach to assess the certainty of the evidence. Across all comparisons and outcomes, we downgraded the certainty of evidence to low or very low due to serious study limitations (i.e. unclear risk of selection bias and high risk of performance and detection bias) and serious or very serious indirectness (i.e. differences in populations in terms of age, conditions and settings; differences in how the intervention was delivered; differences in comparisons and differences in the way outcomes were measured). We also downgraded some of the evidence for very serious imprecision (i.e. small sample size with wide 95% CI). Overall, this level of uncertainty makes it difficult to interpret the benefits or lack of benefits of VR distraction for acute pain in children.
Potential biases in the review process
We designed the methods of the review to minimise the introduction of additional bias. Extensive searches of the literature were performed and we attempted to contact authors for additional information as required. Two review authors independently completed data screening, data extraction, risk of bias and certainty of evidence rating. We acknowledge that such assessments involve subjective judgements. For any discrepancies, we reached consensus through consultation with the other authors.
Agreements and disagreements with other studies or reviews
Our review findings largely concur with other non‐Cochrane reviews of VR distraction interventions for acute pain in children in the literature (Eijlers 2019; Garrett 2014; Kenney 2016; Iannicelli 2019; Malloy 2010; Morris 2009). These reviews mainly present limited and inconsistent evidence of the effectiveness of VR distraction for reducing pain intensity in children undergoing clinical treatments and procedures.
Morris 2009 conducted a systematic review of the effectiveness of VR distraction in conjunction with pharmacologic analgesia, compared with pharmacologic analgesia alone or other forms of distraction, on reducing pain in both children and adults with burn injuries undergoing wound dressing changes and physiotherapy management. Of nine included studies, three were specific to children; one was included in our review (Das 2005) and two were excluded (Chan 2007; Hoffman 2000).
In a narrative review of the effectiveness of VR distraction for relieving pain in children and adults according to five pain types (i.e. experimental pain; chronic pruritus; port access and venous punctures; IV placement; and burn injuries), Malloy 2010 included five studies with child participants; three of these are included in our review (Gold 2006; Nilsson 2009; Wolitzky 2005) and two were excluded (Gershon 2004; Mott 2008). In agreement with this current review, the authors conclude that there is limited conclusive evidence to support the effectiveness of immersive and non‐immersive VR distraction for reducing pain in children associated with port access, venous puncture and IV placement.
Garrett 2014 undertook a rapid evidence review of the effectiveness of VR therapy in pain management in both children and adults undergoing a variety of clinical procedures. Of the included child specific studies, Gold 2006, Kipping 2012, Schmitt 2011, and Wolitzky 2005 are included in our review and Gershon 2004, Chan 2007, and Steele 2003 were excluded because they did not meet the review eligibility criteria. The authors conclude that there is conflicting and limited evidence available and, similar to this current review's conclusions, highlight the need for further studies with greater scientific rigour to establish a better evidence base for VR distraction interventions for acute pain management.
In a meta‐analysis of the effectiveness of VR distraction for reducing pain in children and adults in experimental (e.g. cold pressor, finger pressure) and clinical (e.g. IV placement, burn wound dressings) conditions (14 controlled studies) Kenney 2016 included five studies with child populations; four of which were included in our review (Gold 2006; Jeffs 2014; Kipping 2012; Wolitzky 2005) and one was excluded (Gershon 2004). In the review, Kenney 2016 calculated a pooled effect size within each study for each indicator of pain (i.e. intensity, unpleasantness, and threshold). The results suggest that VR distraction is more effective when used with adults than with children; however, the majority of included studies with adults involved experimentally‐induced pain and it is difficult to draw comparisons here with pain experienced by children when undergoing clinical procedures and treatments.
A recent systematic review (Iannicelli 2019) of the efficacy of VR for pain reduction in children and adolescents undergoing treatments and procedures for vaso‐occlusive pain episodes, inferior alveolar nerve block, immunization, pulp therapy, phlebotomy, dressing changes, burn wound care, IV placement and venipuncture included nine studies, five of which met the inclusion criteria for this current review (Chan 2019 (two RCTs); Dumoulin 2019; Gerceker 2018; Hua 2015; Jeffs 2014). In agreement with our review, inconsistent evidence was reported with unclear overall conclusions drawn about the efficacy of VR distraction for acute pain intensity in children.
In another recent systematic review and meta‐analysis on the effectiveness of VR distraction on pain in paediatric patients undergoing medical procedures (14 studies), Eijlers 2019 conclude that VR is more effective than usual care indicating a clinical benefit however the heterogeneity of study effects was high (I² = 93.3%); as a consequence of outlying and low‐quality studies, and the different medical procedures. Eijlers 2019 further conclude that it is hard to differentiate the benefit of VR over other forms of non‐VR distraction (e.g. watching television), and no distraction, because usual care is often not well defined. Eight of these studies were included in our review (Das 2005; Gold 2006; Gerceker 2018; Hua 2015; Jeffs 2014; Kipping 2012; Schmitt 2011; Wolitzky 2005); we did not deem it appropriate to pool data statistically in this current review due to the clinical heterogeneity of the child participant populations and variations in procedural/treatment conditions across the included studies.
Collectively, these reviews, similar to the current review's conclusions, suggest that evidence is limited and of the evidence that does exist it is of low certainty and very low certainty from a small number of studies, and therefore we cannot be confident in the results. As the majority of review/meta‐analysis authors agree, more high certainty evidence with large sample sizes is needed before we can draw conclusions and consider VR distraction as a potential treatment for consistently reducing acute pain intensity in children. This supports the Birnie 2018 Cochrane systematic review of psychological interventions for needle‐related procedural pain and distress in children and adolescents. The review identified evidence supporting the efficacy of distraction, hypnosis, combined cognitive behavioural therapy and breathing interventions for reducing children’s needle related pain and distress. The quality of the trials and overall evidence remains low to very low underscoring the need for improved methodological rigour and trial reporting.
Authors' conclusions
Implications for practice.
For children with acute pain
There is very little evidence for the use of VR technology in reducing pain in children. We found low‐ to very low‐certainty evidence of the benefit of VR distraction compared to no distraction or non‐VR distraction for the reduction of acute pain intensity in children (0‐18 years) undergoing clinical treatments and procedures. We found limited data to draw any conclusions about secondary outcomes including VR side‐effects, satisfaction with VR, pain‐related distress and administration of rescue analgesia. No studies assessed parent anxiety or cost. We have very little confidence in the evidence. Future well‐designed large high‐quality trials are likely to have an important impact on our confidence in the results.
For clinicians
There is very little evidence for the use of VR technology in reducing pain in children. We found low‐ to very low‐certainty evidence of the effectiveness of VR distraction interventions in reducing acute pain intensity in children to facilitate clinicians making informed evidence based decisions regarding treatment. We found limited data for adverse effects related to VR and other secondary outcomes including child satisfaction with VR, child pain‐related distress and rescue analgesia, therefore, we can draw no conclusions. No studies assessed parent anxiety or cost. We do not have any estimates on cost for these VR distraction interventions yet. More evidence is needed before VR distraction could be considered a potential treatment for consistently reducing acute pain intensity in children.
For policy makers and funders of the intervention
There is very little evidence for the use of VR technology in reducing pain and distress. The results of this review highlight that there is low‐ to very low‐certainty evidence of the benefit of VR distraction interventions for children with acute pain undergoing clinical procedures in healthcare settings. We found limited data for adverse effects related to VR, child satisfaction with VR, child pain related‐distress and administration of rescue analgesia. Parent anxiety was not assessed in any studies and we found no evidence on the cost or cost‐effectiveness of VR distraction interventions. There is insufficient evidence to recommend or refute the use of VR distraction interventions and more funding is needed to establish the evidence base in this area. Prioritising research calls in the area of children’s pain will be critical to leveraging funding to enable large consortiums of researchers, VR developers, industry/SMEs, health care providers, and care recipients (i.e. children and their family) to conduct large high‐quality clinical trials in the future to establish an evidence base for VR distraction for acute pain in children.
Implications for research.
General implications
We conclude, based on the 17 studies included in this review, that there is low‐ to very low‐certainty evidence for the use of VR distraction interventions for children with acute pain undergoing clinical procedures. Larger high‐quality studies to confirm the effectiveness and adverse effects of VR distraction interventions for children with acute pain in any healthcare setting are needed. While the 30 ongoing studies may contribute to future updates of this review, it is important that future trials use standardized age groups, such as those recommended by the US National Institute of Child Health and Human Development, to enhance consistency in reporting age‐related data for paediatric trials (Williams 2012). This would improve the potential for data synthesis, enable exploration of age group variation and similarity regarding treatment response and safety and enable recommendations to be tailored to specific age groups (Williams 2012). This is important in identifying which actual intervention is most effective for whom recognising that age and developmental stage may influence how pain and VR is experienced (Kortesluoma 2006; Won 2017). Another avenue for future research is to see if VR is beneficial for children with chronic pain. Chronic pain is different from acute pain and consequently the function of distraction in these contexts may also differ (i.e. adaptive in acute procedural pain versus potentially maladaptive in chronic pain) (Becker 2018).
Design
Large (i.e. at least 200 participants per arm) high‐quality randomised controlled trials, with cost‐effectiveness analyses, are needed to determine the effectiveness and adverse effects of VR distraction interventions for children with acute pain. Future research should compare VR with other types of widely accessible technological distractions (i.e. smart phones, iPads, tablets, apps); other types of reality such as augmented reality (i.e. virtual experience created by superimposing a virtual image within the real environment) and other types of VR using different VR environments (e.g. off‐the‐shelf pre‐existing virtual content versus customised content created for specific clinical purposes/procedures). Future research should give greater attention to children’s preference regarding distraction and whether child characteristics such as temperament have an important influence on the effectiveness of the distraction stimulus (Koller 2012; MacLaren 2007). Future trials also need to establish the effectiveness of VR across a variety of clinical experiences with different pain intensities and distress‐levels experienced by children, including for example, pain caused by diagnosed illness and associated treatments (e.g. renal or urinary diseases and inflammatory conditions); pain caused by medical and diagnostic procedures and fundamental nursing (e.g. post‐operative treatment, bone marrow procedures and spinal cord injections, side‐effects of medications); and pain caused by accidents (e.g. resetting of fractures or dislocation, suturing and removal of stitches) (Kortesluoma 2004; Kortesluoma 2006). Also specific to future cross‐over trials, investigators should use the Consolidated Standards of Reporting Trials (CONSORT) statement extended to crossover trials to improve reporting of randomised crossover trials; thereby assisting researchers in extracting data for systematic reviews and in judging the reliability and validity of trial findings (Dwan 2019).
Measurement (endpoints)
Future large high‐quality trials using a standardized approach to measuring and reporting similar outcomes across studies are likely to have an influence on the ability to compare and pool data. A specific implication of this review is the need for future trial investigators to use core outcome domains for paediatric acute pain clinical trials such as those developed by McGrath 2008 (i.e. pain intensity, global judgement of satisfaction with treatment, symptoms and adverse effects, physical recovery, emotional response and economic factors); in addition to using recommended validated pain outcome measures (self‐report and observational) that take account of children's different developmental abilities across different age groups (Stinson 2006; von Baeyer 2007).
Also, specific to future VR trials, investigators should consider other mechanisms advanced in VR effectiveness for children with acute pain including the assessment of immersion and presence of the child in the VR environment (Won 2017). For example, the ITC‐Sense of Presence Inventory offers researchers using a range of media systems a tool to measure, post exposure, four facets of a media experience related to presence; including sense of physical space, engagement, ecological validity and negative effects (Lessister 2001).
History
Protocol first published: Issue 8, 2013 Review first published: Issue 10, 2020
Acknowledgements
We thank the Cochrane Consumers and Communication Group for their support in developing and publishing the protocol (2013) before the title was moved to the Pain, Palliative and Supportive Care Review Group (2017).
We thank the editors and staff of the Cochrane Pain, Palliative and Supportive Care Review Group for their support with the review specifically Anna Erskine, Kerry Harding, Andrew Moore and Phil Wiffen.
We would like to thank Information Specialists Joanne Abbott (Cochrane Pain, Palliative and Supportive Care Review Group) for running updated searches and John Kis‐Rigo (Cochrane Consumers and Communication Review Group) for providing assistance with our search strategy and running initial searches.
We would like to thank the peer reviewers of the full review: Walter J. Meyer, Kathryn Birnie, Tam Watson.
We would like to thank Anna Gunning, CEO, Children in Hospital Ireland for providing consumer participation feedback on the review.
Cochrane Review Group funding acknowledgement: this project was funded by the National Institute for Health Research (NIHR) via Cochrane Infrastructure funding to the Cochrane Pain, Palliative and Supportive Care Review Group (PaPaS). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Appendices
Appendix 1. CENTRAL search strategy
CENTRAL (CRSO)
#1 MESH DESCRIPTOR child EXPLODE ALL TREES
#2 MESH DESCRIPTOR infant EXPLODE ALL TREES
#3 MESH DESCRIPTOR adolescent EXPLODE ALL TREES
#4 MESH DESCRIPTOR minors
#5 MESH DESCRIPTOR pediatrics
#6 ((child* or infant* or newborn or neonat* or baby or babies or adolescen* or pediatric* or youth* or teen*)):TI,AB,KY
#7 #1 OR #2 OR #3 OR #4 OR #5 OR #6
#8 MESH DESCRIPTOR virtual reality exposure therapy
#9 ((virtual or virtuality or vr)):TI,AB,KY
#10 MESH DESCRIPTOR User‐Computer Interface
#11 MESH DESCRIPTOR Computer Simulation
#12 (computer simulation):TI,AB,KY
#13 (((simulated or augmented or mediated) adj3 (reality or world* or environment*))):TI,AB,KY
#14 MESH DESCRIPTOR video games
#15 ((videogam* or ((video or computer or electronic or online or on‐line or simulation or role playing) adj gam*))):TI,AB,KY
#16 wii:TI,AB,KY
#17 (Oculus Rift):TI,AB,KY
#18 (((head or helmet) adj mounted)):TI,AB,KY
#19 ((immersi* or spatial presence or lifelike or life‐like)):TI,AB,KY
#20 ((interactive adj3 distraction*)):TI,AB,KY
#21 #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20
#22 MESH DESCRIPTOR Pain EXPLODE ALL TREES
#23 MESH DESCRIPTOR anxiety
#24 MESH DESCRIPTOR fear EXPLODE ALL TREES
#25 ((pain* or ache* or an?esthe* or analges* or suffering or anguish*)):TI,AB,KY
#26 ((anxious* or anxiet* or fear* or panic* or dread* or worry* or agitation or agitated or apprehensi* or nervous* or distress* or catastrophiz* or discomfort*)):TI,AB,KY
#27 #22 OR #23 OR #24 OR #25 OR #26
#28 #7 AND #21 AND #27
#29 1989 TO 2017:YR
#30 #28 AND #29
Appendix 2. MEDLINE Search Strategy
MEDLINE (OVID)
1 exp child/
2 exp infant/
3 adolescent/
4 minors/
5 pediatrics/
6 (child* or infant* or newborn or neonat* or baby or babies or adolescen* or pediatric* or youth* or teen*).tw,hw.
7 or/1‐6
8 virtual reality exposure therapy/
9 (virtual or virtuality or vr).tw.
10 User‐Computer Interface/
11 Computer Simulation/
12 computer simulation.tw.
13 ((simulated or augmented or mediated) adj3 (reality or world* or environment*)).tw.
14 video games/
15 (videogam* or ((video or computer or electronic or online or on‐line or simulation or role playing) adj gam*)).tw.
16 wii.tw.
17 Oculus Rift.tw.
18 ((head or helmet) adj mounted).tw.
19 (immersi* or spatial presence or lifelike or life‐like).tw.
20 (interactive adj3 distraction*).tw.
21 or/8‐20
22 exp Pain/
23 anxiety/
24 exp fear/
25 (pain* or ache* or an?esthe* or analges* or suffering or anguish*).tw,hw.
26 (anxious* or anxiet* or fear* or panic* or dread* or worry* or agitation or agitated or apprehensi* or nervous* or distress* or catastrophiz* or discomfort*).tw,hw.
27 or/22‐26
28 7 and 21 and 27
29 randomized controlled trial.pt.
30 controlled clinical trial.pt.
31 randomized.ab.
32 placebo.ab.
33 drug therapy.fs.
34 randomly.ab.
35 trial.ab.
36 groups.ab.
37 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36
38 exp animals/ not humans.sh.
39 37 not 38
40 28 and 39
41 limit 40 to yr="1989 ‐Current"
Appendix 3. Embase search strategy
Embase (OVID)
1 exp child/
2 exp infant/
3 adolescent/
4 minors/
5 pediatrics/
6 (child* or infant* or newborn or neonat* or baby or babies or adolescen* or pediatric* or youth* or teen*).tw,hw.
7 or/1‐6
8 virtual reality exposure therapy/
9 (virtual or virtuality or vr).tw.
10 Computer Interface/
11 Computer Simulation/
12 computer simulation.tw.
13 ((simulated or augmented or mediated) adj3 (reality or world* or environment*)).tw.
14 video game/
15 (videogam* or ((video or computer or electronic or online or on‐line or simulation or role playing) adj gam*)).tw.
16 wii.tw.
17 Oculus Rift.tw.
18 ((head or helmet) adj mounted).tw.
19 (immersi* or spatial presence or lifelike or life‐like).tw.
20 (interactive adj3 distraction*).tw.
21 or/8‐20
22 exp Pain/
23 anxiety/
24 exp fear/
25 (pain* or ache* or an?esthe* or analges* or suffering or anguish*).tw,hw.
26 (anxious* or anxiet* or fear* or panic* or dread* or worry* or agitation or agitated or apprehensi* or nervous* or distress* or catastrophiz* or discomfort*).tw,hw.
27 or/22‐26
28 7 and 21 and 27
29 random$.tw.
30 factorial$.tw.
31 crossover$.tw.
32 cross over$.tw.
33 cross‐over$.tw.
34 placebo$.tw.
35 (doubl$ adj blind$).tw.
36 (singl$ adj blind$).tw.
37 assign$.tw. (=
38 allocat$.tw.
39 volunteer$.tw.
40 Crossover Procedure/
41 double‐blind procedure.tw.
42 Randomized Controlled Trial/
43 Single Blind Procedure/
44 or/29‐43
45 (animal/ or nonhuman/) not human/
46 44 not 45
47 28 and 46
48 limit 47 to yr="1989 ‐Current"
Appendix 4. CINAHL search strategy
CINAHL
S40 S30 AND S39
S39 S31 OR S32 OR S33 OR S34 OR S35 OR
S36 OR S37 OR S38
S38 (allocat* random*)
S37 (MH "Quantitative Studies")
S36 (MH "Placebos")
S35 placebo*
S34 (random* allocat*)
S33 (MH "Random Assignment")
S32 (Randomi?ed control* trial*)
S31 (singl* blind* ) or (doubl* blind* ) or (tripl* blind* ) or (trebl* blind* ) or (trebl* mask* ) or (tripl* mask* ) or (doubl* mask* ) or (singl* mask* )
S30 S7 AND S23 AND S29
S29 S24 OR S25 OR S26 OR S27 OR S28
S28 (anxious* or anxiet* or fear* or panic* or dread* or worry* or agitation or agitated or apprehensi* or nervous* or distress* or catastrophiz* or discomfort*)
S27 (pain* or ache* or an?esthe* or analges* or suffering or anguish*)
S26 (MH "Fear+")
S25 (MH "Anxiety")
S24 (MH "Pain+")
S23 S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22
S22 (interactive N3 distraction*)
S21 (immersi* or spatial presence or lifelike or life‐like)
S20 ((head or helmet) N1 mounted)
S19 Oculus Rift
S18 Oculus Rift
S17 wii
S16 (videogam* or ((video or computer
or electronic or online or on‐line or simulation or role playing) N1 gam*))
S15 (MH "Video Games")
S14 ((simulated or augmented or mediated) N3 (reality or world* or environment*))
S13 computer simulation
S12 (MH "Computer Simulation")
S11 (MH "User‐Computer Interface")
S10 (virtual or virtuality or vr)
S9 (MH "Virtual Reality Exposure Therapy")
S8 (MH "Virtual Reality Exposure Therapy")
S7 S1 OR S2 OR S3 OR S4 OR S5 OR S6
S6 (child* or infant* or newborn or neonat* or baby or babies or adolescen* or pediatric* or youth* or teen*)
S5 (MH "Pediatrics")
S4 (MH "Minors (Legal)")
S3 (MH "Adolescence")
S2 (MH "Infant+")
S1 (MH "Child+")
Appendix 5. PsycINFO search strategy
PsycINFO (OVID)
1 (child* or infant* or newborn or neonat* or baby or babies or adolescen* or pediatric* or youth* or teen*).tw,hw.
2 virtual reality/
3 (virtual or virtuality or vr).tw.
4 Computer Simulation/
5 computer simulation.tw.
6 ((simulated or augmented or mediated) adj3 (reality or world* or environment*)).tw.
7 video game/
8 (videogam* or ((video or computer or electronic or online or on‐line or simulation or role playing) adj gam*)).tw.
9 wii.tw.
10 Oculus Rift.tw.
11 ((head or helmet) adj mounted).tw.
12 (immersi* or spatial presence or lifelike or life‐like).tw.
13 (interactive adj3 distraction*).tw.
14 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13
15 exp Pain/
16 anxiety/
17 exp fear/
18 (pain* or ache* or an?esthe* or analges* or suffering or anguish*).tw,hw.
19 (anxious* or anxiet* or fear* or panic* or dread* or worry* or agitation or agitated or apprehensi* or nervous* or distress* or catastrophiz* or discomfort*).tw,hw.
20 or/15‐19
21 1 and 14 and 20
22 clinical trials/
23 (randomis* or randomiz*).tw.
24 (random$ adj3 (allocat$ or assign$)).tw.
25 ((clinic$ or control$) adj trial$).tw.
26 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
27 (crossover$ or "cross over$").tw.
28 random sampling/
29 Experiment Controls/
30 Placebo/
31 placebo$.tw.
32 exp program evaluation/
33 treatment effectiveness evaluation/
34 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw.
35 or/22‐34
36 21 and 35
37 limit 36 to yr="1989 ‐Current"
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Atzori 2018.
| Study characteristics | ||
| Methods | Randomised study: within‐subjects design | |
| Participants | 15 children aged 7 to 17 years, 10 boys and 5 girls Eligibility criteria: Onco‐haematological disease, requiring venipuncture twice in a year for intravenous placement during chemotherapy, transfusions, magnetic resonance or blood analysis, able to understand Italian language, able to complete the tests, able to wear helmet and interact with VR environment, no physical or psychological impairments. Exclusion criteria: Venous access already inserted, epilepsy diagnosis, unaccompanied by legal guardian, older than 17 years, younger than 7 years, wanting to use own distraction tool. Setting: Service of paediatric oncology and haematological diseases of an Italian children’s hospital |
|
| Interventions |
Intervention VR (immersive) distraction (n = 15) using the virtual environment SnowWorld, presented via a helmet and earphones Comparison No distraction (n = 15) All patients underwent two venipunctures on two different days; one venipuncture with no VR and one venipuncture with VR on a second visit. |
|
| Outcomes |
Timing of measurement: After procedure |
|
| Notes |
Funding source: Supported by NIH grants and Effat University Research and Consultancy Institute, Jeddah, Saudi Arabia, and the Mayday Fund. Also acknowledged support of Foundation Cassa di Risparmio di Firenze. Declarations of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information available; states treatment order was randomised but unclear how this was performed; for period effects the proportions of participants randomised to the different intervention sequences is not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely Carry‐over effects not mentioned but likely to be low risk (mean time between first and second venipuncture was 26.6 days) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Greater than 10% missing data; two children withdrew: one decided to use own distraction and one did not want to use VR during second venipuncture (reason not indicated) |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported and results for both periods reported |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Low risk | None identified |
Chan 2019.
| Study characteristics | ||
| Methods | Two randomised controlled trials: both RCTs had 2 groups | |
| Participants |
This paper reports two RCTs: one in an emergency department and one in outpatient pathology.
The eligibility and exclusion criteria were the same for both RCTs. Eligibility criteria: Aged 4 to 11 years, requiring venipuncture or intravenous cannulation for any indication, sufficient English ability to complete study instruments. Exclusion criteria: Critical medical illnesses or deteriorating clinical status, medical conditions preventing VR use or study instrument completion, inability to consent/assent. Settings:
|
|
| Interventions |
Intervention VR (immersive) distraction using VR aquatic environment developed by two authors, presented via helmet Emergency department trial (n = 64) and outpatient pathology trial (n = 63) Comparison Non‐VR distraction including age‐appropriate distraction, such as child‐life therapy, toys, books, and electronic devices. Distractions allowed at discretion of clinician and standardized distractions not mandated to reflect clinical practice. Emergency department trial (n = 59) and outpatient pathology trial (n = 66) |
|
| Outcomes |
Timing of measurement: Immediately before and after procedure |
|
| Notes |
Funding: Quote “Supported by the Australian Federal Government Department of Industry, Innovation and Science” Declarations of interest: Quote “The study funder and supporting bodies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. E.C. and P.L. hold shares in Smileyscope Pty Ltd holding intellectual property arising from this study, which includes a patent entitled “virtual reality apparatus.” The other authors declare no conflicts of interest.” |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomization sequences (stratified by site) generated in advance by computerized randomised number generator |
| Allocation concealment (selection bias) | Low risk | Concealment by opaque envelope until after baseline data collected |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Reported as not blinded, due to the nature of the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Reported as not blinded, due to the nature of the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 10% missing data. For the emergency department trial, no attrition reported. For the outpatient pathology trial, two participants withdrew assent after randomization from non‐VR distraction group. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Size | Unclear risk | 50 to 199 participants per treatment arm |
| Other bias | Low risk | None identified |
Chen 2019.
| Study characteristics | ||
| Methods | Randomised controlled trial: 2 groups | |
| Participants | 136 children aged 7 to 12 years, 77 boys and 59 girls Eligibility criteria: Aged 7 to 12 years, clearly conscious, agreed to take part, receiving intravenous injections, communicate in Mandarin or Taiwanese and read Chinese. Exclusion criteria: Developmental delay, epilepsy, or heart diseases, undergoing chemotherapy, visually or hearing impaired, near‐sighted or farsighted, head trauma in past month, confirmed obesity, required blood transfusions and blood preparation, received two or more intravenous injections and had blood drawn only one time. Setting: Emergency department of a regional teaching hospital in northern Taiwan. |
|
| Interventions |
Intervention VR (immersive) distraction (n = 68) using four virtual environments (i.e. roller coasters, space exploration, a wildlife park, and travel destinations) presented via head mounted display Comparison No distraction (n = 68) |
|
| Outcomes |
Timing of measurement: Five minutes post‐procedure |
|
| Notes |
Funding: Quote "supported by the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan (108AC‐D112)". Declarations of interest: Quote "authors declare that there is no conflict of interest". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomization method; researchers not involved in study randomly divided participants into experimental and control groups (ratio of 1:1) and assigned six combinations (No. 1–6) per group using random number generator |
| Allocation concealment (selection bias) | Low risk | Researchers placed results in opaque, sealed envelopes and numbered the envelopes, which participants opened after they and their primary caregivers signed consent forms |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 10% missing data. Four participants withdrew prior to division into the experimental and control groups |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Size | Unclear risk | 50 to 199 participants per treatment arm |
| Other bias | Low risk | None identified |
Das 2005.
| Study characteristics | ||
| Methods | Randomised trial: pilot study: within‐subject design | |
| Participants | Nine children 5 to 16 years, 6 boys and 3 girls (7 included in analysis; removed a boy and a girl; 5 boys and 2 girls) Eligibility criteria: Admitted to one specific ward, requiring dressing change for acute burn injuries (more than three percent of body surface area), aged between 5 and 18 years, Exclusion criteria: Burns to hands, face or head, past history of epilepsy, reduced intellectual capacity Setting: One ward in Women's and Children's Hospital, Adelaide, Australia |
|
| Interventions |
Intervention VR (immersive) distraction (n = 9) using game software developed based on the game Quake presented via a head‐mount display. Comparison No distraction (n = 9) |
|
| Outcomes |
Timing of measurement: First treatment half was removal of adhesive tape/bandages and under‐dressing and second half was wound debridement application of fresh dressing. Timing of measurements was the end of each phase of dressing change (i.e. removal of existing burns dressings or application of fresh burns dressing). |
|
| Notes |
Funding: None reported Declarations of interest: Quote "author(s) declare that they have no competing interests". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment to each half of the burns dressing change (removal of existing burns dressings or application of fresh dressings) following a coin toss determining the sequence; for period effects proportions of participants randomised to the different intervention sequences not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not blinded but states in text that data analyzed by a blinded assessor Subjects received VR and no VR during the same dressing change session with carry‐over effects not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Greater than 10% missing data. Two subject results withdrawn from analysis as participants were too drowsy from the effects of analgesia to participate in VR period of the session |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported (13 trials were undertaken from 9 children with 7 children included in the analysis with data reported per child and per trial) |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Unclear risk | Unclear bias depending on the order in which children had the wound dressing done i.e. first half involved removal of dressing and second half consisted of wound debridement and application of new dressing (could one half of the wound dressing be more of less painful); also some children had multiple dressings performed so the cumulative effect of pain could be different |
Dumoulin 2019.
| Study characteristics | ||
| Methods | Randomised controlled trial: 3 groups | |
| Participants | 59 children aged 8 to 17 years, 38 boys and 21 girls Eligibility criteria: Awaiting needle‐related procedures (blood work, IV placement, or both) for a pending or known diagnostic and visiting the emergency department on the occasions where the research team was available and the Child Care specialists were on duty Exclusion criteria: Cognitive impairment, not a good command of English or French, suffered from epilepsy or migraine or vomiting at time of procedure; medical procedure lasted more than 15 minutes. Setting: Emergency department of Children’s Hospital of Eastern Ontario, Canada |
|
| Interventions |
Intervention VR (immersive) distraction (n = 20) using a virtual game (i.e. shoot flies flying around an apartment) developed by Cyberpsychology Lab at Universite du Quebec en Outaouais, presented via a Head Mounted Display. Comparisons Non‐VR distraction (n = 24) including watching television i.e. portable DVD player and a video of choice (Looney Tunes or Animal Planet’s Funniest Animals) Non‐VR distraction (n = 15) including distraction provided by Child Life program i.e. three preselected activities offered (nonprocedural talk, I‐Spy books or 20 questions ball) |
|
| Outcomes |
Timing of measurement: Approximately 15 minutes before and right after the procedure |
|
| Notes |
Funding: Not reported Declarations of interest: Quote “S.B. is a consultant to and own equity in Cliniques et Developpement In Virtuo, a spin‐off company from the university that uses VR as part of its clinical services and distributes virtual environments. The terms of these arrangements have been reviewed and approved by the Universite du Quebec en Outaouais in accordance with its conflict of interest policies. The remaining authors report no financial relationships with commercial interests.” |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment by random numbers table before recruitment by researcher |
| Allocation concealment (selection bias) | Low risk | Assignment concealed until participant brought to experimenter |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Reported as not blinded, due to the nature of the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Reported as not blinded, due to the nature of the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Low risk | None identified |
Gerceker 2018.
| Study characteristics | ||
| Methods | Randomised controlled study: 3 groups | |
| Participants | 121 children aged 7 to 12 years, 61 boys and 60 girls Eligibility criteria: Children aged between 7 and 12 years who underwent (successful) phlebotomy Exclusion criteria: Refusal to participate, have a chronic or genetic disease or mental or language deficiency Setting: Paediatric phlebotomy unit in a university hospital in Izmir, Turkey |
|
| Interventions |
Intervention VR (immersive) distraction (n = 40) using choice of three cartoon videos delivered via Oculus headset. Comparison No distraction (n = 40) Non‐VR distraction (n = 41) including external cold and vibration i.e. Buzzy a reusable bee which provides both cold compression and vibration |
|
| Outcomes | Child pain self‐report, parent‐report, nurse‐report and researcher‐report assessed using the Wong‐Baker Faces Pain Rating Scale Timing of measurement: After the procedure (within 5 minutes) |
|
| Notes |
Funding: Ege University Scientific Research Projects Declaration of interest: Quote “none to report” |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomization (12 blocks) generated according to gender (two groups, boy and girl) and age (six groups, ages 7 to 12) |
| Allocation concealment (selection bias) | Low risk | Computer generated table of random numbers |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information, the authors state “The child, parent, and nurse were blinded to each other’s score, only the researcher was not blinded because she collected all the scores” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 26 children excluded because of an unsuccessful phlebotomy attempt (n = 16) and incomplete data collection (n = 10); missing outcome data balanced in numbers and in similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Size | High risk | 50 or fewer participants per treatment arm |
| Other bias | Low risk | None identified |
Gold 2006.
| Study characteristics | ||
| Methods | Randomised study: 2 groups | |
| Participants | 20 children aged 8 to 12 years, 12 boys and 8 girls, and their parents Eligibility criteria: Awaiting outpatient MRI or CT scan requiring IV placement Exclusion criteria: Cognitive disabilities, taking pain medication, failed cognitive and physical screening Setting: Outpatient radiology department |
|
| Interventions |
Intervention VR (immersive) distraction (n = 10) using Street Luge, by Fifth Dimension Technologies, presented via head‐mounted display Comparison No distraction (n = 10) |
|
| Outcomes |
Timing of measurement: Approximately 30 min before IV, immediately before IV and following IV placement |
|
| Notes |
Funding source: Quote: "generous donation and support from Mindy D.W. Weiss" Declarations of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information available |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Low risk | None identified |
Hoffman 2019.
| Study characteristics | ||
| Methods | Within‐subject within‐wound care design: pilot study | |
| Participants | 48 children aged 6 to 17 years old, 34 boys and 14 girls 44 of the 48 children were from developing Latin American countries Eligibility criteria: admitted to Shriners Hospitals for Children in Galveston Texas with greater than 10% total body surface area burn injuries and moderate or higher worst pain during no VR on Day 1; compliant and able to complete subjective evaluations; no history of previous psychiatric disorder(s); not demonstrating delirium, psychosis, or any form of organic brain disorder; and able to communicate verbally in English or Spanish Exclusion criteria: burn size less than 10% total body surface area; not capable of completing study measures; no wound cleaning sessions required; history of previous psychiatric disorder(s); demonstrating delirium, psychosis, or organic brain disorder; unable to communicate verbally in English or Spanish; history of significant cardiac, endocrine, neurologic, metabolic, respiratory, gastrointestinal, or genitourinary impairment; receiving prophylaxis for alcohol or drug withdrawal; have a developmental disability; younger than 6 years or older than 17 years; burns of eyes, eyelids, or face so severe that precluded use of VR equipment; and previous history of severe motion sickness. Setting: Intensive care unit hydro tank room in regional burn centre in United States |
|
| Interventions |
Intervention Portable water‐friendly VR (immersive) distraction (n = 48) using the virtual environment Snow World, presented via a custom robot‐like articulated arm goggle holder The technology was designed to provide a fully‐immersive experience but it was adapted for the particular cohort of patients and the full immersion could not be reached to its full potential; they maximised as much as possible immersive VR Comparison No distraction (n = 48) |
|
| Outcomes |
Timing of measurement: After procedure (i.e. wound care session) |
|
| Notes |
Funding: Shriners Hospitals for Children, Tampa Florida award to PI Walter Meyer and charitable donation from MayDay Fund. Portable water‐friendly VR system developed via NIH grant. Declaration of Interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Initial treatment order randomised using block randomization; random number sequences generated using www.random.org; for period effects the proportions of participants randomised to the different intervention sequences is not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely Carry‐over effects not mentioned and with VR and no VR repeatedly alternated every 5 minutes during wound debridement potential residual effects could be carried over |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported and all period data reported |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | High risk | Trial design makes it difficult to be conclusive about the results as during wound debridement exposure to VR and no VR was repeatedly alternated every 5 minutes with pain rated after the wound care session was finished |
Hua 2015.
| Study characteristics | ||
| Methods | Randomised study: 2 groups | |
| Participants | 65 children aged 4 to 16 years, 31 boys and 34 girls Eligibility criteria: Chronic lower limb wounds that required active dressing changes Exclusion criteria: Non‐Chinese speaking, visual or auditory disability, illness in addition to lower limb chronic wounds, on sedative medication, wounds requiring surgery Setting: Paediatric centre in tertiary hospital |
|
| Interventions |
Intervention VR (immersive) distraction (n = 33) using a Chinese version of the Ice Age 2: Meltdown game presented via head mounted display Comparison Non‐VR distraction (n = 32) including toys, television, books, parental comforting |
|
| Outcomes |
Timing of measurement: Before, during and after dressing change |
|
| Notes |
Funding source: None reported Declarations of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generated by computer |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Reported as not blinded, due to the nature of the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Reported as not blinded, due to the nature of the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Low risk | None identified |
Jeffs 2014.
| Study characteristics | ||
| Methods | Randomised controlled trial: 3 groups | |
| Participants | 28 adolescents aged 10 to 17 years, 19 boys and 9 girls Eligibility criteria: Undergoing burn wound care, first‐time visit to outpatient burn clinic or first clinic visit without conscious sedation, English speaking Exclusion criteria: Burns interfering with study procedures, motion sickness or seizure disorder history, incarcerated minors, minors in foster care, cognitive disability. Setting: Outpatient burn clinic of large academic children’s hospital |
|
| Interventions |
Intervention VR (semi‐immersive) distraction (n = 8) using Snow World, a three‐dimensional, computer‐generated, interactive VR software programme designed specifically for patients receiving burn wound care, presented via a tripod‐arm device Comparison No distraction (n = 10) Non‐VR distraction (n = 10) i.e. watching an age appropriate movie |
|
| Outcomes |
Timing of measurement: Pre‐ and post‐procedure |
|
| Notes |
Funding source: Grant from the Arkansas Children’s Hospital Research Institute/Arkansas Biosciences Institute and donation from the Arkansas Children’s Hospital Burn Center. Declarations of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated, random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether envelopes were opaque or numbered sequentially |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants broken after pre‐wound care assessments completed |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐reported outcome questionnaire (subjective data) completed by participants, administered by study team members with no knowledge of group assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 10% missing data (30 recruited and 28 included in analysis). Reason for attrition was protocol violations;one withdrew before wound care treatment and one ineligible due to requiring sedation. |
| Selective reporting (reporting bias) | High risk | Primary outcome for procedural pain not directly reported (follow up with author provided further data i.e. unadjusted means and standard deviations) |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Low risk | None identified |
Kipping 2012.
| Study characteristics | ||
| Methods | Randomised controlled trial: 2 groups | |
| Participants | 41 adolescents aged 11 to 17 years, 28 boys and 13 girls Eligibility criteria: Undergoing first conscious change of dressing for burn wound with total body surface area greater than 1% Exclusion criteria: Cognitive impairment, visual/hearing impairment, wound location impacting the ability to use VR device, non‐English speaking, child safety/protection issues Setting: Stuart Pegg Paediatric and Adult Burn Centre |
|
| Interventions |
Intervention VR (immersive) distraction (n = 20) using off the‐shelf, age appropriate software games (i.e. Chicken LittleTM for 11–13 years and Need for SpeedTM for 14–17 years presenting via a head mounted display. Comparison Non‐VR distraction (n = 21) including access to television, stories, music or caregivers and child preference for no distraction |
|
| Outcomes |
Timing of measurement: Baseline (pre‐randomisation), retrospectively after dressing removal and after dressing application |
|
| Notes |
Funding source: Grant given to the Royal Children’s Hospital, Brisbane by Diversionary Therapy Technologies Declarations of interest: Quote: "Roy Kimble part‐supervised this trial and also holds options with this company, however at the time of completion and submission of this clinical trial, will not stand to lose or gain financially or personally from the results" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence was computer generated (1:1, blocks of 20) |
| Allocation concealment (selection bias) | Low risk | Consecutively numbered sealed opaque envelopes and opened by independent administration officer |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Reported as not blinded, due to the nature of the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Reported as not blinded, due to the nature of the intervention; outcome measure responses recorded by participant, caregiver and nurse unobtrusively placing a mark on the data collection sheet |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported (reported as mean change scores for pain intensity and nausea) |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Low risk | None identified |
Koushali 2017.
| Study characteristics | ||
| Methods | Randomised controlled trial: 2 groups | |
| Participants | 40 children aged 7 to 12 years, 26 boys and 14 girls Eligibility criteria: Minimum of one dressing change, lack of severe (deep) burns, lack of underlying diseases such as disabilities or mental disorders, parental written consent and parental literacy and age above 18 years. Exclusion criteria: Required intravenous sedation during procedure, inability to communicate, unwillingness to participate Setting: Burn Center in Isfahan |
|
| Interventions |
Intervention VR (immersive) distraction (n = 20) using a multidimensional game, known as Smash Hit, designed by Mediocre company in the musical arcade style for children above 7 years, presented via a head set. Comparison No distraction (n = 20) |
|
| Outcomes |
Timing of measurement: Before and immediately after procedure |
|
| Notes |
Funding source: Quote: "the financial and material support of the study was provided by Isfahan University of Medical Science". Declarations of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly selected through convenience sampling (shuffling numbered cards) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information, the authors state "since the children were treated separately at different times, blinding was only achieved in the patient group" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Low risk | None identified |
Nilsson 2009.
| Study characteristics | ||
| Methods | Randomised study: 2 groups | |
| Participants | 42 children and adolescents aged 5 to 18 years, 25 boys and 17 girls Eligibility criteria: Children with cancer undergoing either venous punctures or subcutaneous venous port device access Exclusion criteria: Cognitive impairment, lack of good command of Swedish Setting: Paediatric Oncology Unit |
|
| Interventions |
Intervention VR (non‐immersive) distraction (n = 21) using the game/application of the hunt of the diamonds developed with Digital Content Creation software and Adobe Photoshop Comparison No distraction (n = 21) |
|
| Outcomes |
Timing of measurement: 5 minutes before, during (retrospectively recorded after procedure) and 3‐5 minute after procedure. |
|
| Notes |
Funding source: Children’s Cancer Foundation at Queen Silvia Children’s Hospital, Sigurd and Elsa Goljes Foundation, Federation of Swedish County Councils, Ebba Danelius Foundation and Wilhelm and Martina Lundgrens Foundation. Declarations of interest: Authors reported no financial or personal relationships with participants or organizations that could inappropriately influence their work |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information available |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 10% missing data. Four girls withdrew from the study; it is unclear which groups these children withdrew from and whether this was after randomization. Reason for attrition not reported. |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported (reported as medians; follow up with author provided further data i.e. means and standard deviations) |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Unclear risk | The control and intervention groups differed slightly in terms of procedure i.e. participants either underwent procedures of insertion of subcutaneous venous port devices or venous punctures; for the intervention group 7 underwent venipuncture and 14 subcutaneous venous port device and for the control group 12 underwent venipuncture and 9 subcutaneous venous port device |
Schmitt 2011.
| Study characteristics | ||
| Methods | Randomised controlled trial: within subjects (cross‐over design) | |
| Participants | 53 participants aged 6 to 18 years; 43 boys and 10 girls (this study included 54 children/young people aged 6 to 19 years; only one subject was 19 years and separate data were supplied by the author for the 53 partcipants included in this review) Eligibility criteria: Requiring post‐burn, active‐assisted range‐of‐motion physical therapy at least once during hospital stay Exclusion criteria: Extreme susceptibility to motion sickness, burns on body regions precluding VR use (e.g. ear burns), seizure activity history Setting: University of Washington Burn Center at Harborview Medical Center: Level 1 burn/trauma centre |
|
| Interventions |
Intervention VR (immersive) distraction (n = 53) using the virtual environment SnowWorld originally designed and created at the University of Washington and upgraded by Firsthand, Inc (Seattle WA), presented using one of four head‐mounted displays (helmets) Comparison No distraction (n = 53) Quote: "Both treatment conditions (i.e. virtual reality and no virtual reality) were employed within a single physical therapy session" |
|
| Outcomes |
Timing of measurement: Immediately after each treatment condition |
|
| Notes |
Funding source: National Institutes of Health and Paul G. Allen Family Foundation. Declarations of interest: Quote: "The study sponsors had no involvement in the study design, data collection, analysis and interpretation of data, writing of the manuscript, or decision to submit the manuscript for publication. The SnowWorld virtual environment was originally designed by the University of Washington Human Interface Technology Laboratory and created by Kristin Darken, Jeff Bellinghausen, and Chuck Walter (Multigen‐Paradigm, Inc.), and later upgraded by Brian Stewart (SimWright Inc.) and Howard Abrams, with 3‐dimensional modelling assistance from Duff Hendrickson (University of Washington Human Interface Technology Laboratory)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Order of conditions randomised and counterbalanced using a computer‐generated randomization schedule; for period effects proportions of participants randomised to the different intervention sequences is not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Reported as not blinded, due to the nature of the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely Subjects spent equivalent time in VR and no VR during the same treatment session with carry‐over effects not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | High risk | Data presented in figures as standard error so not extractable (follow up with author provided further data) |
| Size | Unclear risk | 53 participants exposed to both treatment conditions (i.e. VR and no VR) within the one treatment session |
| Other bias | Low risk | None identified |
Walther‐Larsen 2019.
| Study characteristics | ||
| Methods | Randomised controlled trial: 2 groups | |
| Participants | 59 children aged 7 to 16 years, 7 girls and 52 boys Eligibility criteria: Scheduled for a venous cannulation before a planned IV anaesthetic induction at the anaesthetic department, aged 7 to 16 years, Danish‐speaking Exclusion criteria: American Society of Anesthesiologists classification score greater than 2, non‐Danish speaking, receiving analgesia or sedatives, cognitive impairment, psychotic diagnosis, headache, dizziness, recent head injury, epilepsy, conditions where VR goggle application might be harmful, cases where topical anaesthesia not properly applied Setting: University Hospital Rigshospitalet, Copenhagen, Denmark |
|
| Interventions |
Intervention VR (immersive) distraction (n = 28) using VR Seagull Splash a three‐dimensional interactive game (custom made for needle procedure scenario), presented via VR goggles Comparison Non‐VR distraction (n = 31) including a Tablet or smartphone to play a two‐dimensional game of own choice |
|
| Outcomes |
Timing of measurement: 15 minutes after procedure |
|
| Notes |
Funding: Quote “Khora Virtual Reality Denmark and Kristian Bluff (Motivates) for software development. CGI/Cynergi Danmark A/S donated funds for software development.” Declarations of interest: Authors stated none to declare and also indicated they had no financial relationships relevant to the manuscript to disclose. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation (computer‐generated) was conducted for two groups |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐reported outcome subjective data collected from participants by nurse observer who was blinded to randomisation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 10% missing data. Five patients dropped out, two due to unsuccessful IV cannulation and three disliked the VR game; four from VR group and one from control group |
| Selective reporting (reporting bias) | High risk | Pre‐specified outcomes reported as medians and interquartile ranges and as mean differences and data not usable (authors contacted for data no response) |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Low risk | None identified |
Wolitzky 2005.
| Study characteristics | ||
| Methods | Randomised study: 2 groups | |
| Participants | 20 children aged 7 to 14 years, 12 boys and 8 girls Eligibility criteria: Receiving treatment for cancer and undergoing a port access procedure Exclusion criteria: None reported Setting: Children’s hospital in major metropolitan city |
|
| Interventions |
Intervention VR (immersive) distraction (n = 10) designed to be education for children visiting the gorilla habitat at Zoo Atlanta, presented via head mounted display Comparison No distraction (n = 10) |
|
| Outcomes |
Timing of measurement: Before and immediately after procedure |
|
| Notes |
Funding source: Not reported Declarations of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information available |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not described, but due to the nature of the intervention, blinding is highly unlikely |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 10% missing data. Two participants withdrew because children too ill to participate – at what point these children withdrew is unclear |
| Selective reporting (reporting bias) | High risk | Results reported as composite measure of distress (i.e. mean of child reported pain and anxiety); no data reported for parent and nurse VAS ratings |
| Size | High risk | Fewer than 50 participants per treatment arm |
| Other bias | Low risk | None identified |
CAS: Colour Analogue Scale CHEOPS: Children's Hospital of Eastern Ontario Pain Scale CT: computed tomography FAS: Facial Affective Scale FLACC: Faces, Legs, Activity, Cry, Consolability GRS: Graphic Rating Scale IV: intravenous MRI: magnetic resonance imaging VAS: Visual Analogue Scale VR: virtual reality
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Altmann 2017 | Not immersive nor non‐immersive virtual reality distraction |
| Babaie 2019 | Not immersive nor non‐immersive virtual reality distraction |
| Beale 2006 | Did not measure acute pain intensity |
| Blunt 1998 | Not immersive nor non‐immersive virtual reality distraction |
| Brown 2014 | Not immersive nor non‐immersive virtual reality distraction |
| Burns‐Nader 2013 | Not immersive nor non‐immersive virtual reality distraction |
| Canares 2018 | Not in age range |
| Celikol 2019 | Not immersive nor non‐immersive virtual reality distraction |
| Chan 2007 | Not a randomised controlled trial |
| Dahlquist 2010 | Experimental pain; not a healthcare setting |
| Diaz‐Hennessey 2019 | Not a randomised controlled trial |
| Dosani 2019 | Not immersive nor non‐immersive virtual reality distraction |
| Eijlers 2017 | Not virtual reality distraction instead it is virtual reality exposure as psychological preparation for surgery (confirmed with authors via email) |
| Faucher 2007 | Trial not completed and no plans to complete the trial (confirmed by email with author) |
| Feng 2018 | Not immersive nor non‐immersive virtual reality distraction |
| Ferullo 2017 | Not immersive nor non‐immersive virtual reality distraction |
| Fonseca 2018 | Single group assignment |
| Gershon 2004 | Not in age range |
| Gilbert 2014 | Abstract form only |
| Gold 2005 | Not a randomised controlled trial |
| Gold 2018 | Not in age range |
| Goldman 2018a | Not measure acute pain intensity as outcome |
| Gonzalez 2016 | Abstract form only |
| Hoffman 2001 | Not in age range |
| Hoffman 2004b | Not in age range |
| Hoffman 2008 | Not in age range |
| Hoffman 2012 | Abstract form only |
| Hoffman 2015 | Wrong population; included healthy volunteers |
| Inan 2019 | Not immersive nor non‐immersive virtual reality distraction |
| Jeffs 2010 | Early termination of study due to fewer subjects available than expected |
| Jeffs 2013 | Abstract form only |
| Kumar 2017 | Not immersive nor non‐immersive virtual reality distraction |
| Leibovici 2009 | Not in age range |
| LeMay 2016a | Trial withdrawn |
| LeMay 2017a | Quasi‐experimental with single group assignment |
| Li 2011 | Did not measure acute pain intensity |
| Lozano 2018 | Not immersive nor non‐immersive virtual reality distraction |
| MacLaren 2005 | Not immersive nor non‐immersive virtual reality distraction |
| Marteau 2018 | Not in age range |
| Miller 2009 | Abstract form only |
| Miller 2010 | Not immersive nor non‐immersive virtual reality distraction |
| Miller 2011 | Not immersive nor non‐immersive virtual reality distraction |
| Miller 2016 | Not immersive nor non‐immersive virtual reality distraction |
| Minute 2012 | Not immersive nor non‐immersive virtual reality distraction |
| Mosso 2008 | Not in age range |
| Mott 2008 | Not immersive nor non‐immersive virtual reality distraction |
| Newell 2018 | Not immersive nor non‐immersive virtual reality distraction |
| Nilsson 2007 | Abstract form only |
| Nilsson 2013 | Not immersive nor non‐immersive virtual reality |
| Parker 2016 | Not in age range |
| Patterson 2010 | Not in age range |
| Shah 2018 | Intervention was a combined relaxation response and virtual reality session; trial was also a single group assignment |
| Sharar 2008 | Not a randomised controlled trial |
| Sharer 2007 | Not in age range |
| Small 2015 | Not in age range |
| Tropez‐Arceneaux 2011 | Abstract form only |
| Tschiedel 2019 | Not immersive nor non‐immersive virtual reality distraction |
| vanGoor 2019 | Not in age range |
| vanRooijen 2017 | Not virtual reality distraction rather it about virtual reality as an information tool |
| Ver Lee 2012 | Abstract form only |
| Windlich‐Biermeier 2007 | Not immersive nor non‐immersive virtual reality |
| Wint 2002 | Not in age range |
| Wolyniez 2013 | Intervention was a medical clown who used cognitive and behavioural interventions including virtual reality |
| Yuan 2018 | Abstract form only |
| Zelmar 2015 | Not immersive nor non‐immersive virtual reality |
Characteristics of studies awaiting classification [ordered by study ID]
Festini 2016.
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 6 to 18 years Diagnosed with Cystic Fibrosis |
| Interventions | VR distraction compared to standard care |
| Outcomes | Pain using VAS Anxiety using VAS Distress using m‐YPAS |
| Notes | ClinicalTrials.gov Identifier: NCT02802839 Recruitment status unknown; study start date June 2016; estimated study completion date June 2017 No response to email requesting trial status update and results in August 2018. |
Meyer 2014.
| Methods | Randomised controlled trial: cross‐over assignment |
| Participants | Children aged 6 to 17 years Minimum of 10% of total burned surface area requiring wound cleansing sessions |
| Interventions | VR distraction compared to music distraction |
| Outcomes | Pain intensity, time spent thinking about pain, pain unpleasantness, fun, satisfaction with pain management using GRS |
| Notes | ClinicalTrials.gov Identifier: NCT03491657 Recruitment completed; actual enrolment 62; start date March 13, 2014; actual study completion date Jan 3, 2017 No response to email requesting update on trial status and results in August 2018 |
NCH 2016.
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children greater than 6 years and less than 19 years Diagnosed with Haemophilia A or B |
| Interventions | VR distraction compared with standard of care distraction |
| Outcomes | Feasibility using surrogate marker of duration (in minutes) of IV procedure Effectiveness of distraction technique using VAS/FACES pain scale Usability and likability of VR equipment using VAS/FACES pain scale |
| Notes | ClinicalTrials.gov Identifier: NCT03507582 Recruitment completed; enrolled 25 participants; study start date April 2016; study completion Dec 28, 2016 No response to email requesting update on trial status and results in August 2018 |
Patterson 2009.
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children greater than or equal to 8 years and up to 20 years Minimum of 3 days of physical therapy, one physical therapy session per day |
| Interventions | VR during physical therapy versus VR background pain and no VR |
| Outcomes | Pain Anxiety |
| Notes | ClinicalTrials.gov Identifier: NCT00993889 Recruitment completed; study start date May 2009; study completion date April 2017 No response to email requesting update on trial status and results in August 2018 |
VAS: Visual Analogue Scale GRS: Graphic Rating Scale IV: intravenous m‐YPAS: modified‐Yale Preoperative Anxiety Scale VR: virtual reality
Characteristics of ongoing studies [ordered by study ID]
ACTRN12617000285358.
| Study name | Investigating the management of paediatric procedural pain relief obtained through virtual reality (IMPROVR) |
| Methods | Randomised controlled trial |
| Participants | Children aged 4 to 11 years Requiring a peripheral IV cannula or venipuncture |
| Interventions | VR distraction compared with standard care |
| Outcomes | Pain using the FACES Pain Scale ‐ Revised (self‐report) and VAS (observer‐report) Anxiety using a VAS (self‐report and observer‐report) Impact on ease of performing the procedure through number of needle attempts required Safety and any adverse effects of VR using questionnaire modified from Child Simulator Sickness Questionnaire Satisfaction with management of procedure rated by child using VAS Risk of needle stick injuries and patient’s cooperation using a Likert scale (health practitioners) Time required to prepare the patient and perform the procedure |
| Starting date | First enrolment 13/07/2017; recruitment completed; target sample size 240; date of last participant enrolment 15/02/2018; date of study completion not cited No response to email requesting update on trial status and results in August 2018 |
| Contact information | Evelyn Chan, Monash Health 246 Clayton Road Clayton VIC 3168, Australia Email: Evelyn.Chan@monash.edu |
| Notes | ACTRN12617000285358 |
ACTRN12618001363279.
| Study name | The use of a virtual reality headset for 4 year old immunisations to reduce pain and distress |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 42 months to 5 years Attending general practice for immunisations |
| Interventions | VR distraction compared to standard care with usual distraction |
| Outcomes | Pain intensity using FACES pain scale and Poker Chip Tool Observer (parents and healthcare providers) ratings of pain and distress using VAS |
| Starting date | Not yet recruiting; anticipated recruitment starting date 01/02/2019; target sample size 100; anticipated recruitment end 01/02/2020 |
| Contact information | Dr Kirrily Ellerton, Wellness on Wellington, Australia Email: kirrilyellerton@gmail.com |
| Notes | ACTRN12618001363279 |
LeMay 2016b.
| Study name | Decreasing recurrent pain and anxiety in medical procedures with a pediatric population: a pilot study (DREAM‐P) |
| Methods | Randomised controlled trial: cross‐over assignment |
| Participants | Children aged 7 to 18 years Burn or another injury requiring wound dressing change or physiotherapy |
| Interventions | VR distraction compared with standard pharmacological treatment |
| Outcomes | Acceptability using pre‐tested tailored questionnaire including satisfaction and acceptability outcomes (tolerance, positive and negative aspects, secondary effects) Pain using NRS and pain experience using GRS to measure cognitive, affective and sensory components of pain Expected and experienced anxiety using Children`s Fear Scale Comfort using Behavioural Observation Scale of Comfort Level for child burn victims Pain memory using NRS Anxiety memory using Children’s Fear Scale Range of motion (only for physiotherapy sessions) using a goniometer |
| Starting date | Recruiting; estimated enrolment 20 participants; start date July 10, 2017; estimated primary completion date August 2018; estimated study completion date August 2018 |
| Contact information | Sylvie Le May, Université de Montreal; CHU Ste‐Justine Research Center, Montreal, Quebec, Canada. Email: sylvie.lemay@umontreal.ca |
| Notes | ClinicalTrials.gov Identifier: NCT02977923 |
NCT02646787.
| Study name | Virtual reality water friendly wound care (H2OWC) |
| Methods | Randomised controlled trial: factorial assignment |
| Participants | Children aged greater than or equal to 8 years Burn wound care sessions |
| Interventions | Active VR compared to passive VR and no intervention |
| Outcomes | Pain using GRS |
| Starting date | Recruiting; start date Oct 2015; estimated enrolment 200 participants; estimated primary study completion Sept 2019; estimated actual study completion Sept 2020 No response to email (davepatt@u.washington.edu) in August 2018 to confirm when results might be available including whether separate data will be reported for children < 18 years |
| Contact information | David Patterson, University of Washington Email: davepatt@u.washington.edu |
| Notes | ClinicalTrials.gov Identifier: NCT02646787 |
NCT02929771.
| Study name | Using virtual reality to reduce procedural pain in children with cancer |
| Methods | Pilot‐randomised controlled trial: cross‐over design |
| Participants | Children aged 8 to 18 years Actively undergoing cancer treatment and requiring at least two subcutaneous port needle insertions for cancer treatment over 8 weeks |
| Interventions | VR compared with usual care |
| Outcomes | Implementation outcomes including accrual and retention rates, acceptability and technical difficulties. Effectiveness outcomes including child pain intensity, distress, and fear, as well as parent distress. |
| Starting date | Recruiting; estimated enrolment 40; study start date August 1, 2017; estimated primary completion date March 2019 |
| Contact information | Jennifer Stinson, Hospital for Sick Children Toronto, Ontario, Canada. Email: jennifer.stinson@sickkids.ca |
| Notes | ClinicalTrials.gov Identifier: NCT02929771 |
NCT02986464.
| Study name | Virtual reality distraction for procedural pain management in children with burn Injuries: a randomised controlled trial |
| Methods | Pilot randomised controlled trial: within‐subject/crossover study design |
| Participants | Children aged 6 months to 7 years Burn injury requiring a hydrotherapy session |
| Interventions | VR prototype compared to standard pharmacological treatment |
| Outcomes | Pain using French version of FLACC scale Pain observational/behavioural using VAS by proxy Comfort using behavioural observation scale of comfort level for child burn victims Sedation using University of Michigan Sedation Scale Health professionals' satisfaction level using pre‐tested tailored questionnaire including tolerance, positive and negative aspects Analgesic requirement using rescue dose medication administration |
| Starting date | Recruiting; estimated enrolment 38 participants; actual study start date May 3, 2018; estimated primary completion date June 2019; estimated study completion June 2019 |
| Contact information | Sylvie Le May, Université de Montreal; CHU Ste‐Justine Research Center, Montreal, Quebec, Canada. Email: sylvie.lemay@umontreal.ca |
| Notes | ClinicalTrials.gov Identifier: NCT02986464 |
NCT03155607.
| Study name | Novel virtual reality for burn wound care in adolescents |
| Methods | Randomised trial: parallel assignment |
| Participants | Children and young people aged 10 to 21 years Undergoing burn wound care |
| Interventions | VR distraction compared to standard care |
| Outcomes | Pain perception using Adolescent Pediatric Pain Tool |
| Starting date | Recruiting; estimated enrolment 72; start date Jan 2018; estimated completion date 2020 Email correspondence with author confirmed that the trial is ongoing with no data available yet; data will be available and reported in the future for children up to 18 years |
| Contact information | Debra Jeffs, University of Arkanas, USA. Email: jeffsda@archildrens.org |
| Notes | ClinicalTrials.gov Identifier: NCT03155607 |
NCT03239743.
| Study name | Effects of virtual reality on pre‐operative anxiety and induction of anaesthesia in children and adolescents |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 5 to 11 years Undergoing tonsillectomy or tonsillectomy and adenoidectomy procedure |
| Interventions | VR compared to midazolam |
| Outcomes | Pre‐operative anxiety measured by mYPAS Induction compliance of anaesthesia measured by induction compliance checklist Post‐operative emergence delirium measured by PAED scale Post‐operative pain Post‐operative opioid use |
| Starting date | Start date July 20, 2017; currently recruiting; estimated enrolment 80 participants; estimated study completion May 2019 |
| Contact information | Vanessa Pohl, Phoenix Children’s Hospital, Arizona, United States Email: vpohl@phoenixchildrens.com |
| Notes | ClinicalTrials.gov Identifier: NCT03239743 |
NCT03304769.
| Study name | Virtual reality distraction during paediatric intravenous line placement: a prospective randomised comparison study |
| Methods | Randomised controlled trial: parallel group assignment (confirmed through email with the author as the trial registration states single group assignment) |
| Participants | Children aged 4 to 17 years Requiring IV placement |
| Interventions | VR compared to no VR |
| Outcomes | Successful IV placement with first attempt Number of attempts before successfully establishing IV Time to establishing successful IV Pain using FACES revised pain scale (children and parents) Anxiety using Likert‐Type Scale (children and parents) Age range of patients that tolerate VR |
| Starting date | Recruiting; estimated enrolment 116; actual study start date Sept 28, 2017; estimated completion Jan 2018 Email to author confirmed this trial is ongoing with 100 participants enrolled to date |
| Contact information | Anna K Schlechter, University of Texas at Austin. Email: anna.schlechter@gmail.com |
| Notes | ClinicalTrials.gov Identifier: NCT03304769 |
NCT03353584.
| Study name | Effect of virtual reality technology for pain management of vaso‐occlusive crisis in patients with sickle cell disease |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children greater or equal to 6 years and less than or equal to 25 years Have sickle cell disease (any genotype) seeking care for acute vaso‐occlusive crisis pain |
| Interventions | VR therapy compared to standard care/no intervention |
| Outcomes | Change in pain scores |
| Starting date | Recruiting; actual study start date Feb 5, 2018; estimated enrolment 76 participants; estimated study completion Feb 2021 No response to email (referralinfo@stjude.org) in September 2018 inquiring whether separate data for children 6 to 18 years would be reported. It does state that participants will be randomised by age. |
| Contact information | Latika Puri, St. Jude Children's Research Hospital USA Email: referralinfo@stjude.org |
| Notes | ClinicalTrials.gov Identifier: NCT03353584 |
NCT03435367.
| Study name | Immersive virtual reality to reduce procedural pain during IV insertion in children in the emergency department |
| Methods | Pilot randomised control trial: parallel assignment |
| Participants | Children aged 8 to 17 years Requiring IV insertion |
| Interventions | VR compared to standard care |
| Outcomes | Pain intensity using NRS (self‐report and observer‐report – parents and nurses) Child distress using NRS (self‐report and observer‐report – parents and nurses) Child fear using Child Fear Scale Parent Distress Parent distress using Parent Distress Questionnaire Child Presence Measure Implementation outcomes including accrual and retention rates, acceptability and technical difficulties |
| Starting date | Recruiting; estimated enrolment 80; study start date Feb 1, 2018; estimated primary completion date March 2019 |
| Contact information | Jennifer Stinson, Hospital for Sick Children Toronto, Ontario, Canada. Email: jennifer.stinson@sickkids.ca |
| Notes | ClinicalTrials.gov Identifier: NCT03435367 |
NCT03464955.
| Study name | VR usage in non‐invasive surgical sub‐specialty procedures |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 2 to 18 years Undergoing non‐invasive surgical subspecialty procedures |
| Interventions | Technology based distractions (VR headsets, augmented reality headset, tablets, or BERT (Bedside Entertainment Theatre) projector) compared to no intervention/standard of care |
| Outcomes | Change in Pain Score Anxiety Score Childhood Anxiety Meter Family Satisfaction Patient Cooperation Brief Behavioural Distress Scale Patient Compliance Parent Pain Catastrophizing Scale |
| Starting date | Recruiting; start date Oct 16, 2017; estimated primary completion date Oct 16, 2019 |
| Contact information | Samuel Rodriguez, Stanford University. Email: sr1@stanford.edu |
| Notes | ClinicalTrials.gov Identifier: NCT03464955 |
NCT03480724.
| Study name | Assessing the efficacy of virtual reality analgesia (VRA) in pediatric patients for pain control (PEDSPAINVR) |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 5 to 18 years Spasticity requiring Botulinum toxin injections |
| Interventions | Oculus rift VR distraction compared to goggle cardboard box VR and no VR |
| Outcomes | Severity of Pain using the FLACC scale Severity of anxiety using Short State‐Trait Anxiety Inventory Anxiety scale |
| Starting date | Recruiting; study start date July 6, 2017; estimated primary completion date Aug 2018; estimated study completion date Dec 2018. Email correspondence to author confirmed ongoing recruitment (up to 90 participants) with some promising preliminary data been presented at American Academy of Physical Medicine and Rehabilitation conference Oct 2018 |
| Contact information | Yuxi Chen, Montefiore Medical Center, New York, USA. Email: yuchen@montefiore.org |
| Notes | ClinicalTrials.gov Identifier: NCT03480724 |
NCT03518346.
| Study name | Use of virtual reality game playing during venipuncture |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 8 to 19 years Receiving a blood draw |
| Interventions | VR compared to standard care/distraction |
| Outcomes | Attempting versus refusing venipuncture (number of patients) Blood volume collected in ml Patient reports of pain using pain scale Child and parent satisfaction survey Patient reports of fear on using fear scale Time (in minutes) to achieve optimal blood volume |
| Starting date | Enrolling by invitation; estimated enrolment 120 participants; start date April 9, 2018; estimated primary completion date March 31, 2020; estimated study completion date March 31, 2021 Email correspondence to author confirmed that the trial is ongoing and no data is available yet; when available data will be looked at by age groups 8 to 12 years and 15 to 19 years so there will potentially be data available/reported for 8 to 12 years of age for inclusion in a future review. |
| Contact information | Julie Schweitzer, University of California, Davis. Email:jschweitzer@ucdavis.edu |
| Notes | ClinicalTrials.gov Identifier: NCT03518346 |
NCT03521076.
| Study name | Randomised controlled trial of virtual reality |
| Methods | Randomised controlled trial: crossover assignment |
| Participants | Children aged 4 years and older receiving botulinum toxin injections |
| Interventions | VR distraction compared with standard care |
| Outcomes | Pain intensity using Faces Pain Scale ‐ Revised Patient and parent/caregiver anxiety, proportion of the treatment time spent thinking about pain, worst pain during treatment, satisfaction with pain management and nausea assessed using series of VAS Medication use, provider description of whether VR enhanced clinical care, reduction or avoidance of medication due to VR, total amounts of medications given and notation of patient side effects from VR (from medical records) |
| Starting date | Not yet recruiting; estimated enrolment 40 participants; estimated study start July 2018; estimated study completion 2020 Email to author confirmed commencement of the trial and it is anticipated that when reporting results separate data will be reported for children < 18 years. |
| Contact information | Chantel Barney, Gillette Children's Specialty Healthcare Email: CBarney@gillettechildrens.com |
| Notes | ClinicalTrials.gov Identifier: NCT03521076 |
NCT03584776.
| Study name | Virtual reality for post‐operative pain management |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 6 to 17 years Diagnosis of adolescent idiopathic scoliosis or neuromuscular scoliosis; having spinal infusion |
| Interventions | VR distraction compared to usual standard of care |
| Outcomes | Timing of pain medication Doses of pain medication Pain‐related behavioural changes using Parent Postoperative Pain Measure Pain intensity using Faces Pain Scale‐Revised Patient and parent anxiety, patient and parent time spent thinking about pain, pain unpleasantness, average pain rating, pain rating right now, worst pain rating, least pain rating, engagement during VR (VR group only) and satisfaction with pain management using VAS Length of inpatient stay following surgery (medical records) Nursing pain assessment scores (medical records) Duration of time from surgery to patient out of bed and walking (medical records) |
| Starting date | Estimated study start Oct 2018; not yet recruiting; estimated enrolment 80 participants; estimated study completion Oct 2021 |
| Contact information | Chantel Barney, Gillette Children's Specialty Healthcare Email: CBarney@gillettechildrens.com |
| Notes | ClinicalTrials.gov Identifier: NCT03584776 |
NCT03645213.
| Study name | Two different distraction methods on pain and fear during venipuncture in children |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 7 to 12 years Undergoing venipuncture |
| Interventions | VR distraction compared to non‐VR distraction on a tablet computer and no distraction |
| Outcomes | Child pain assessed by Wong‐Baker faces rating scale Child fear assessed by Children Fear Scale Outcomes reported by children, parent and observer |
| Starting date | Actual study start date Sept 2017; enrolment of 120 participants; actual study completion date Aug 2018 |
| Contact information | Merdiye Sendir, Saglik Bilimleri University, Istanbul, Turkey Email: none provided |
| Notes | ClinicalTrial.gov Identifier: NCT03645213 |
NCT03680625.
| Study name | Virtual reality vs. passive distraction for pain management |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 7 to 21 years During common paediatric orthopaedic outpatient procedures including: cast application, cast removal, hardware removal (i.e. pins and screws), suture and staple removal and Botox injections |
| Interventions | VR distraction compared to non‐VR passive distraction (i.e. watching a video on an iPad) |
| Outcomes | Pain intensity self‐report using Numerical Rating Scale Pain experience using Graphic Rating Scale Anxiety level using Children's Fear Scale Parents' and children's satisfaction levels using numerical scale Healthcare professionals' satisfaction level using a tailored questionnaire Need for rescue medication Use of other non‐pharmacological interventions (parental distraction, music/singing, comforting, or other) during the procedure Occurrence of side effects related to interventions Children's memory of pain using Numerical Rating Scale Children's memory of anxiety using Children's Fear Scale |
| Starting date | Actual study start day June 2019; estimated enrolment 88 participants; estimated study completion date December 2020; potential data will be available and reported in the future for children up to 18 years |
| Contact information | Sylvie Le May St. Justine's Hospital Montreal, Quebec, Canada Email: sylvie.lemay@umontreal.ca |
| Notes | ClinicalTrials.gov Identifier: NCT03680625 |
NCT03681717.
| Study name | Virtual reality vs. standard‐of‐care for comfort during laceration repair |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 6 to 16 years Arriving to emergency department and requiring a laceration repair procedure |
| Interventions | VR distraction compared to standard of care |
| Outcomes | Self‐report pain using Faces Pain Scale ‐ Revised Self‐report anxiety using Venham Situational Anxiety Score Patient satisfaction determined qualitatively Medication dose Timing in minutes from readiness for procedure until procedure completion and until discharge from emergency department |
| Starting date | Actual study start date Feb 2018; estimated enrolment 64 participants; estimated study completion date Jan 2019 |
| Contact information | Ran Goldman, British Columbia Children's Hospital, Vancouver, Canada Email: rgoldman@cw.bc.ca |
| Notes | ClinicalTrials.gov Identifier: NCT03681717 |
NCT03681730.
| Study name | Virtual reality vs. standard‐of‐care for comfort during intravenous catheterisation |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 6 to 16 years Undergoing IV placement procedure |
| Interventions | VR distraction compared to standard of care |
| Outcomes | Self‐report pain using Faces Pain Scale ‐ Revised Self‐report anxiety using Venham Situational Anxiety Score Patient satisfaction using Global Rating Scale Medication dose used Number of IV trials until success Timing in minutes from readiness for procedure until procedure completion and until discharge from emergency department |
| Starting date | Actual study start date May 2018; estimated enrolment 64 participants; estimated study completion date May 2019 |
| Contact information | Ran Goldman, British Columbia Children's Hospital, Vancouver, Canada Email: rgoldman@cw.bc.ca |
| Notes | ClinicalTrials.gov Identifier: NCT03681730 |
NCT03681743.
| Study name | VR vs. standard‐of‐care for comfort during minor plastic surgery procedures in children |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 6 to 16 years Undergoing minor painful procedure in plastic surgery clinic |
| Interventions | VR distraction compared to standard of care |
| Outcomes | Self‐report pain using Faces Pain Scale ‐ Revised Self‐report anxiety using Venham Situational Anxiety Score Patient satisfaction determined qualitatively Medication dose Timing in minutes from readiness for procedure until procedure completion and until discharge from emergency department Patient use of VR in the future |
| Starting date | Actual study start date May 2018; estimated enrolment 64 participants; estimated study completion date May 2019 |
| Contact information | Ran Goldman, British Columbia Children's Hospital, Vancouver, Canada Email: rgoldman@cw.bc.ca |
| Notes | ClinicalTrials.gov Identifier: NCT03681743 |
NCT03693469.
| Study name | Virtual reality vs. standard‐of‐care for comfort during immunizations in children |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 6 to 16 years Arriving to immunisation clinic for immunisation |
| Interventions | VR distraction compared to standard of care |
| Outcomes | Self‐report pain using Faces Pain Scale ‐ Revised Self‐report anxiety using Venham Situational Anxiety Score Patient satisfaction using Global Rating Scale Medication dose used Length of time of procedure (in minutes) |
| Starting date | Actual study start date Oct 2018; estimated enrolment 64 participants; estimated study completion date Oct 2019 |
| Contact information | Ran Goldman, British Columbia Children's Hospital, Vancouver, Canada Email: rgoldman@cw.bc.ca |
| Notes | ClinicalTrials.gov Identifier: NCT03693469 |
NCT03750578.
| Study name | Virtual reality for needle procedures in the pediatric emergency department |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 7 to 17 years Undergoing venipuncture (IV placement or diagnostic venipuncture) |
| Interventions | VR distraction compared to standard care |
| Outcomes | Self‐reported pain using Verbal Numerical Rating Scale Patient, parent and nurse evaluation of overall pain management (i.e. pain relief, side effects, physical and emotional recovery) using numeric rating scale Procedure‐related distress using Procedure Behaviour Check List by research nurse Procedure related distress using Child Fear Scale |
| Starting date | Actual study start date Dec 2018; enrolment of 62 participants; actual study completion date June 2019 |
| Contact information | Esli Osmanlliu, Emergency Department, St Justine Hospital, Montreal, Canada Email: none provided |
| Notes | ClinicalTrials.gov Identifier: NCT03750578 |
NCT03784352.
| Study name | Virtual reality pediatric orthopaedic outpatient procedures |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 4 to 18 years During common paediatric orthopaedic outpatient procedures including: cast application, cast removal, hardware removal (i.e. pins and screws), suture and staple removal and Botox injections |
| Interventions | VR distraction compared to no distraction |
| Outcomes | Child self‐report pain using Wong‐Baker rating scale Intra‐professional state anxiety using Children's Emotional Manifestation Scale Procedural time Nausea using Baxter Retching Faces Scale State anxiety using short state anxiety inventory scale Trait anxiety using Penn State Worry Questionnaire for Children |
| Starting date | Actual study start date Feb 2019; estimated enrolment 240 participants; estimated study completion date Nov 2019 |
| Contact information | Bejann Jivraj and Emily Schaeffer, British Columbia Children's Hospital, Vancouver, Ontario, Canada Email: b.jivraj@cw.bc.ca and emily.schaeffer@cw.bc.ca |
| Notes | ClinicalTrials.gov Identifier: NCT03784352 |
NCT03888690.
| Study name | Effect of virtual reality distraction on procedural pain for children and adolescents in onco‐haematology |
| Methods | Randomised controlled trial: cross‐over assignment |
| Participants | Children aged 8 to 17 years Undergoing invasive procedures in onco‐haematology unit |
| Interventions | VR distraction compared to standardised procedures without VR |
| Outcomes | Pain scores assessed by visual analogue scale Anxiety scores assessed by Yale scale |
| Starting date | Estimated study start date Apr 2019; estimated enrolment 96 participants; estimated study completion June 2020 |
| Contact information | Isabelle Perot and Marie‐Helene Petit, Central Hospital, Nancy, France Email: isaperot@orange.fr and mh.petit@chru‐nancy.fr |
| Notes | ClinicalTrials.gov Identifier: NCT03888690 |
NCT03903510.
| Study name | Virtual reality during paediatric cast removal |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 4 to 12 years Undergoing cast removal |
| Interventions | VR distraction compared to usual standard of care |
| Outcomes | Heart rate Self‐reported pain using Wong‐Baker faces pain scale Parent‐reported pain using Wong‐Baker faces pain scale Parent anxiety using VAS Parent satisfaction using VAS Parent assessment of pleasantness using VAS |
| Starting date | Actual study start date May 2019; estimated enrolment 184 participants; estimated study completion date Sept 2020 |
| Contact information | Andrew Georgiadis, Gilette Children's Speciality Healthcare, Saint Paul, Immesota, United States Email: andrewgeordiadis@gillettechildrens.com |
| Notes | ClinicalTrials.gov Identifier: NCT03903510 |
NCT03913897.
| Study name | The effect of virtual reality and kaleidoscope on pain and anxiety levels during venipuncture in children |
| Methods | Randomised controlled trial: factorial assignment |
| Participants | Children aged 4 to 10 years Undergoing venipuncture |
| Interventions | VR distraction compared to kaleidoscope distraction and no distraction |
| Outcomes | Child fear and anxiety assessed by Children Fear Scale Child pain assessed by self‐report Visual Analogue Scale and Wong‐Baker faces pain scale |
| Starting date | Actual study start date June 2018; enrolment of 135 participants; study completion Nov 2018 |
| Contact information | Tuba Koe Oxhan, Adiyaman University Research Hospital, Turkey Email: none |
| Notes | ClinicalTrials.gov Identifier: NCT03913897 |
NCT03985930.
| Study name | Non‐immersive virtual reality for paediatric pain management |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 1 to 6 years Procedures for venipuncture, administration of intramuscular medication and vaccination |
| Interventions | VR compared to treatment as usual (for children 3 to 6 years) Video projection distraction compared to treatment as usual (for children aged under 3 years) |
| Outcomes | LLANTO pain level measured using LLANTO pain scale |
| Starting date | Estimated study start date Nov 2019; estimated enrolment 200 participants; estimated study completion date Dec 2021 |
| Contact information | Maria Palacios‐Ariza, Fundacion Universitaria Sanitas, Bogota, Colombia Email: mapalaciosar@unisanitas.edu.co |
| Notes | ClinicalTrials.gov Identifier: NCT03985930 |
NCT04040036.
| Study name | Effects of virtual reality on pain, fear and anxiety during blood draw in children aged 5‐12 years old |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 5 to 12 years Undergoing blood draw procedure |
| Interventions | VR rollercoaster distraction compared to VR ocean rift and no distraction |
| Outcomes | Pain assessed by Wong‐Baker faces rating scale Procedure related fear assessed by Child Fear Scale Procedure related anxiety assessed by Children's Anxiety Meter |
| Starting date | Actual study start date Sept 2017; 136 participants enrolled; study completion date Dec 2017 |
| Contact information | Gulcin Ozalp Gerceker, Dokuz Eylul University, Izmir, Turkey Email: none |
| Notes | ClinicalTrials.gov Identifier: NCT04040036 |
Wong 2019.
| Study name | Effects of immersive virtual reality intervention on pain and anxiety among paediatric patients undergoing venipuncture: a randomised controlled trial |
| Methods | Randomised controlled trial: parallel assignment |
| Participants | Children aged 4 to 12 years Scheduled to undergo venepuncture |
| Interventions | Immersive VR compared to standard care without VR |
| Outcomes | Child pain using Faces Pain Scale‐Revised Anxiety using VAS (for children 4 to 7 years) and state anxiety scale (for children 8‐12 years) Heart rate Stress levels using salivary cortisol assay Length of procedure Staff satisfaction using staff satisfaction scale Cost‐effectiveness |
| Starting date | Study start date Jan 2019; target sample size 200; anticipated study completion Dec 2020 |
| Contact information | Cho Lee Wong, Nethersole School of Nursing, Chinese University of Hong Kong Email: jojowong@cuhk.edu.hk |
| Notes | ChiCTR1800018817 |
BERT: Bedside EnterRtainment Theatre FLACC: Faces, Legs, Activity, Cry, Consolability GRS: Graphic Rating Scale IV: intravenous m‐YPAS: modified‐Yale Preoperative Anxiety Scale NRS: Numerical Rating Scale PAED: Paediatric Emergence Delirium VAS: Visual Analogue Scale VR: virtual reality
Differences between protocol and review
To avoid confusion and for clarity purposes we removed the word ‘simulation’ from the title and throughout the review and instead use the term ‘distraction.' We revised the review title and objective to conform to the standard format recommended by PaPaS, and to reflect changes to the scope of this review.
We moved the first two paragraphs of the section ‘why is it important to do this review’ to the ‘description of the condition’ section to highlight the high prevalence and negative consequences of poorly managed pain in children to describe the condition. Other changes to background sections included updating and changing order of references and updating the definition of pain.
We refined types of participants to children with acute pain. We removed chronic pain because it is different from acute pain and the function of distraction in these contexts may also differ. Primary and secondary outcomes in our protocol were heavily focused on acute pain.
We refined types of intervention, and comparisons, to the following: VR distraction compared to no distraction; VR distraction compared to other non‐VR distraction; and VR distraction compared to other VR distraction to more accurately reflect the focus on distraction.
We split the primary outcome of ‘child pain’ to separate pain outcomes for different reporters of pain (i.e. self‐report, observer‐report and behavioural measurement) acknowledging that different reporters can under‐ or over‐estimate pain intensity in children (Brudvik 2016; Garcia‐Munitis 2006); and also to take account of different time points of pain assessment during and post‐procedure for different reporters of pain.
We removed length of child's recovery time from the secondary outcome cost because of lack of clarity about how this might be costed for acute pain intensity in children.
Under selection of studies, we added that publications in abstract form only were not included in the review due to limited data but were listed as excluded studies.
We added extra details to assessing risk of bias by including the extra domain of size of study as recommended by PaPaS. We also added extra detail for assessing risk of bias in cross‐over studies.
We added more details on the methods for assessing certainty of the evidence and creating 'Summary of findings' tables using wording suggested by PaPaS.
The protocol stated that we would prepare a ‘Summary of findings’ table using the primary outcome child pain and the following secondary outcomes: child satisfaction with VR simulation, child pain‐related distress and parent anxiety. Due to a change in how we reported the primary outcome, we reported the following primary outcomes: acute pain intensity: self‐report (during the procedure); acute pain intensity: observer‐report (during the procedure); acute pain intensity: behavioural measurements (observer‐report) (during the procedure); acute pain intensity: self‐report (up to one hour post‐procedure); acute pain intensity: observer‐report (up to one hour post‐procedure); acute pain intensity: behavioural measurements (observer‐report) (up to one hour post‐procedure) and the secondary outcome of adverse effects instead.
Sensitivity analysis: we revised our definition of a 'high‐quality study' from less than 20% for primary outcome data to less than 10% to reflect what we stated in our methods section for risk of bias for incomplete outcome data.
Contributions of authors
Veronica Lambert (VL) contributed to the design of the protocol and the instigation of the review, screened and selected studies, appraised the quality of and extracted data from selected papers, entered data, analyzed and interpreted the data and wrote the main review.
Patrick Boylan (PB) served as technical expert in relation to VR and contributed to decisions on inclusion where further consultation was required.
Lorraine Boran (LB) served as content expert in relation to pain and pain measurement and contributed to decisions where further clarifications were required.
Paula Hicks (PH) served as technical expert in relation to VR and contributed to decisions on inclusion where further consultation was required.
Richard Kirbakaran (RK) served as an experienced meta analytical statistician and contributed to discussions, clarifications and decisions specific to cross‐over trials.
Declan Devane (DD) served as methodological expert and advised on writing all stages of the protocol and review.
Anne Matthews (AM) provided expertise in conducting systematic reviews and assisted with study screening and selection, data extraction, quality appraisal, data entry, analysis and interpretation.
Sources of support
Internal sources
None, Other
External sources
None, Other
Declarations of interest
VL: None known.
PB: None known.
LB: None known.
PH: None known.
RK: None known.
DD: None known.
AM: None known.
New
References
References to studies included in this review
Atzori 2018 {published data only}
- Atzori B, Hoffman HG, Vagnoli L, Patterson DR, Alhalabi W, Messeri A, et al. Virtual reality analgesia during venipuncture in pediatric patients with onco-hematological diseases. Frontiers in Psychology 2018;9:2508 doi:10.3389/fpsyg.2018.02508. [Google Scholar]
Chan 2019 {published data only}
- Chan E, Hovenden M, Ramage E, Ling N, Pham JH, Rahim A, et al. Virtual reality for pediatric needle procedural pain: two randomised clinical trials. Journal of Pediatrics 2019;209:160-7,e4.doi:10.1016/j.jpeds.2019.02.034. [Google Scholar]
Chen 2019 {published and unpublished data}
- *.Chen Y-J, Cheng S-F, Lee P-C, Lai C-H, Hou I-C, Chen C-W. Distraction using virtual reality for children during intravenous injections in an emergency department: a randomized trial. Journal of Clinical Nursing 2019;12 Nov:doi: 10.1111/JOCN.15088. [Google Scholar]
- Chen Y-J. Distraction using VR for children during IV in an emergency department. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 18 November 2019] 2019.
Das 2005 {published data only}
- Das D, Grimmer K, Sparnon A, McRae S, Thomas B. The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: a randomised controlled trial. BMC Pediatrics 2005;5(1):PMID:15745448. [Google Scholar]
Dumoulin 2019 {published data only}
- Dumoulin S, Bouchard S, Ellis J, Lavoie KL, Vezina M, Charbonneau P, et al. A randomised controlled trial on the use of virtual reality for needle-related procedures in children and adolescents in the emergency department. Games for Health Journal 2019;8(4):285-93. [Google Scholar]
Gerceker 2018 {published data only}
- Gerceker GO, Binay S, Bilsin E, Kahraman A, Yulmaz HB. Effects of virtual reality and external cold and vibration on pain in 7 to 12 year-old children during phlebotomy: a randomised controlled trial. Journal of PeriAnesthesia Nursing 2018;33(6):981-9. [Google Scholar]
Gold 2006 {published data only}
- Gold JI, Kim SH, Kant AJ, Joseph MH, Rizzo AS. Effectiveness of virtual reality for pediatric pain distraction during IV placement. CyberPsychology and Behavior 2006;9(2):207-12. [Google Scholar]
Hoffman 2019 {published data only}
- Hoffman HG, Rodriguez RA, Gonzalez M, Bernardy M, Pena R, Beck W, et al. Immersive virtual reality as an adjunctive non-opioid analgesic for pre-dominately Latin American children with large severe burn wounds during burn wound cleaning in the intensive care unit: a pilot study. Frontiers in Human Neuroscience 2019;13(262):doi:10.3389/fnhum.2019.00262. [Google Scholar]
Hua 2015 {published data only}
- Hua Y, Qiu R, Yao W, Zhang Q, Chen X. The effect of virtual reality distraction on pain relief during dressing changes in children with chronic wounds on lower limbs. American Society for Pain Management Nursing 2015;16(5):685-91. [Google Scholar]
Jeffs 2014 {published data only}
- Jeffs D, Dorman D, Brown S, Files A, Graves T, Kirk E, et al. Effect of virtual reality on adolescent pain during burn wound care. Journal of Burn Care and Research 2014;35:395-408. [Google Scholar]
Kipping 2012 {published data only}
- Kipping B, Rodger S, Miller K, Kimble RM. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: A prospective randomized controlled trial. Burns 2012;38:650-7. [Google Scholar]
Koushali 2017 {published data only}
- *.Koushali AN, Daryabeigi R, Alimohammadi N, Najafi M. The effect of a multi-dimensional play program on children's pain intensity during burn dressing change in burn intensive care units: a clinical trial. Critical Care Nursing 2017;10(4):e58845. [Google Scholar]
- Koushali AN. Compare the effectiveness of virtual reality games and positively communicate in reducing symptoms of stress and pain during dressing change in children hospitalized with burns. IRCT: Iranian Registry of Clinical Trials (http://www.irct.ir) [accessed 7 September 2018] 2017.
Nilsson 2009 {published data only}
- Nilsson S, Finnstrom B, Kokinsky E, Enskar K. The use of virtual reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. European Journal of Oncology Nursing 2009;13:102-9. [Google Scholar]
Schmitt 2011 {published data only}
- Schmitt YS, Hoffman HG, Blough DK, Patterson DR, Jensen MP, Soltani M, et al. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns 2011;37(1):61-8. [Google Scholar]
Walther‐Larsen 2019 {published data only}
- Walther-Larsen S, Peterson T, Friis SM, Aagaard G, Drivenes B, Opstrup P. Immersive virtual reality for pediatric procedural pain: a randomised clinical trial. Hospital Pediatrics 2019;9(7):501-7. [Google Scholar]
Wolitzky 2005 {published data only}
- Wolitzky K, Fivush R, Zimand E, Hodges L, Rothbaum BO. Effectiveness of virtual reality distraction during a painful medical procedure in pediatric oncology patients. Psychology and Health 2005;20(6):817-24. [Google Scholar]
References to studies excluded from this review
Altmann 2017 {published data only}
- Altmann U, Worrack S, Kaczmarek MC, Mühleck J, Volk GF, Guntinas-Lichius O, et al. Acceptance of emotion-sensitive training systems of individuals suffering from facial paralysis and their relatives. Laryngo-rhino-otologie 2017;96(6):380-7. [Google Scholar]
Babaie 2019 {published data only}
- *.Babaie M, Farahani AS, Nourian M, Pourhoseingholt A, Masoumpour A. The effect of audio-visual distraction on catheterization pain among school-age children. Evidence Based Care Journal 2019;9(1):35-42. [Google Scholar]
- Babaie M. Influence of virtual reality on catheterisation pain control in 6 - 12 year old patients. Iranian Registry of Clinical Trials (http://en.irct.ir/) [accessed 18 November 2019] 2012.
Beale 2006 {published data only}
- Beale IL, Marín-Bowling VM, Guthrie N, Kato PM. Young cancer patients’ perceptions of a video game used to promote self care. International Electronic Journal of Health Education 2006;9:202-12. [Google Scholar]
Blunt 1998 {published data only}
- Blunt D, Hastie C, Stephens P. More than nintended? Anaesthesia and Intensive Care 1998;26(3):330. [Google Scholar]
Brown 2014 {published data only}
- Brown NJ, David M, Cuttle L, Kimble RM, Rodger S, Higashi H. Cost-effectiveness of a nonpharmacological intervention in pediatric burn care. Value in Health 2015;18:631-7. [Google Scholar]
- *.Brown NJ, Kimble RM, Rodger S, Ware RS, Cuttle L. Play and heal: randomized controlled trial of DittoTM intervention efficacy on improving re-epithelialization in pediatric burns. Burns 2014;40:204-13. [Google Scholar]
- Brown NJ, Rodger S, Ware RS, Kimble RM, Cuttle L. Efficacy of a children’s procedural preparation and distraction device on healing in acute burn wound care procedures: study protocol for a randomized controlled trial. Trials 2012;13:238. [Google Scholar]
Burns‐Nader 2013 {published data only}
- Burns-Nader S, Hernandez-Reif M, Thoma SJ. Play and video effects on mood and procedure behaviors in school-aged children visiting the pediatrician. Clinical Pediatrics 2013;52(10):929–35. [Google Scholar]
Canares 2018 {published data only}
- Canares T. Virtual reality during procedures in pediatric patients. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 18 November 2019] 2018.
Celikol 2019 {published data only}
- Celikol S, Buyuk TE, Yildizlar O. Children's pain, fear and anxiety during invasive procedures. Nursing Science Quarterly 2019;32(3):226-32. [Google Scholar]
Chan 2007 {published data only}
- Chan EA, Chung JW, Wong TK, Lien AS, Yung Yang J. Application of a virtual reality prototype for pain relief of pediatric burn in Taiwan. Journal of Clinical Nursing 2007;16:786-93. [Google Scholar]
Dahlquist 2010 {published data only}
- Dahlquist LM, Weiss KE, Law EF, Sil S, Herbert LJ, Horn SB, et al. Effects of videogame distraction and a virtual reality type head-mounted display helmet on cold pressor pain in young elementary school-aged children. Journal of Pediatric Psychology 2010;35(6):617-25. [Google Scholar]
Diaz‐Hennessey 2019 {published data only}
- Diaz-Hennessey S, O'Shea ER, King K. Virtual reality: augmenting the acute pain experience in children. Pediatric Nursing 2019;45(3):122-127. [Google Scholar]
Dosani 2019 {published data only}
- Dosani S, Kyriakopoulos M. Clinical research updates. Child and Adolescent Mental Health 2019;24(3):291-2. [Google Scholar]
Eijlers 2017 {published data only}
- Eijers R. Virtual reality exposure before elective pediatric day-care surgery: effects on pre- and postoperative anxiety and pain. NTR: Netherlands Trial Register (http://www.trialregister.nl) [accessed 7 September 2018] 2017.
- *.Eijlers R, Legerstee JS, Dierckx B, Staals LM, Berghmans J, Schroeff MP, et al. Development of a virtual reality exposure tool as psychological preparation for elective pediatric day care surgery: methodological approach for a randomized controlled trial. JMIR Research Protocols 2017;6(9):e174. [Google Scholar]
Faucher 2007 {unpublished data only}
- Faucher L. Study in the use of virtual reality as an adjunct to pain control in burn patients. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2007.
Feng 2018 {published data only}
- Feng Z, Tang Q, Lin J, He Q, Peng C. Application of animated cartoons in reducing the pain of dressing changes in children with burn injuries. International Journal of Burns and Trauma 2018;8(5):106-13. [Google Scholar]
Ferullo 2017 {unpublished data only}
- Ferullo J. At their fingertips: The effects of child-led distraction using a tablet computer on children’s distress and pain during painful medical procedures; a randomised controlled trial. ANZCTR: Australian New Zealand Clinical Trials Registry (http://wwwanzctr.org.au/) [accessed 25 October 2019] 2017.
Fonseca 2018 {unpublished data only}
- Fonseca A. Technology-based distractions during minor procedures. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2018.
Gershon 2004 {published data only}
- Gershon J, Zimand E, Pickering M, Rothbaum BO, Hodges L. A pilot and feasibility study of virtual reality as a distraction for children with cancer. Journal of the American Academy of Child and Adolescent Psychiatry 2004;43(10):1243-9. [Google Scholar]
Gilbert 2014 {published data only}
- Gilbert K, Parker R, Ciorciari J, Beswick M, Carbis C. The use of guided imagery to alleviate pain in paediatric patients (4 - 12 year olds) undergoing treatment in the emergency department. Australasian College for Emergency Medicine 30th Annual Scientific Meeting. Emergency Medicine Australasia 2014;26:1-21. [Google Scholar]
Gold 2005 {published data only}
- Gold JI, Kant AJ, Kim SH, Rizzo AS. Virtual anesthesia: The use of virtual reality for pain distraction during acute medical interventions. Seminars in Anesthesia, Perioperative Medicine and Pain 2005;24:203-10. [Google Scholar]
Gold 2018 {published data only}
- Gold JI, Mahrer NE. Is virtual reality really for prime time in the medical space? A randomised controlled trial of pediatric virtual reality for acute procedural pain management. Journal of Pediatric Psychology 2018;43(3):266-75. [Google Scholar]
Goldman 2018a {unpublished data only}
- Goldman R. Virtual reality vs. standard of care for comfort before and after sedation in the emergency department. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 25 October 2019] 2018.
Gonzalez 2016 {published data only}
- Gonzalez M, Hoffman HG, Pena R, Bernardy M, Beck W, Bermea S, et al. Water-friendly adjunctive virtual reality pain distraction for pediatric burn patients during wound debridement in the ICU tubroom. 48th Annual Meeting of the American Burn Association - Journal of Burn Care and Research 2016;37:S97. [Google Scholar]
Hoffman 2001 {published data only}
- Hoffman HG, Patterson DR, Carrougher GJ, Sharar S. The effectiveness of virtual reality based pain control with multiple treatments. Clinical Journal of Pain 2001;17:229-35. [Google Scholar]
Hoffman 2004b {published data only}
- Hoffman HG, Richards TL, Coda B, Bills AR, Blough D, Richards AL, et al. Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. NeuroReport 2004;15(8):1245-8. [Google Scholar]
Hoffman 2008 {published data only}
- Hoffman HG, Patterson DR, Seibel E, Soltani M, Jewett-Leahy L, Sharar SR. Virtual reality pain control during burn wound debridement in the hydrotank. Clinical Journal of Pain 2008;24(4):299-304. [Google Scholar]
Hoffman 2012 {published data only}
- Hoffman HG, Meyer IW, Russell WJ, Fuchs H, Cowen A, Wiechman SA, et al. A randomized multisite study on virtual reality pain distraction in pediatric burn patients during physical therapy. 44th Annual Meeting of the American Burn Association. Journal of Burn Care and Research 2012;33(Suppl1):S156. [Google Scholar]
Hoffman 2015 {published data only}
- Hoffman HG, Meyer WJ, Gonzalez M, Ramirez M, Herrero R, Navarro M, et al. Auditory interactivity task increases effectiveness of virtual reality pain distraction (with and without oculus rift VR goggles). 47th Annual Meeting of the American Burn Association - Journal of Burn Care and Research 2015;36:S114. [Google Scholar]
Inan 2019 {published data only}
- Inan G, Inal S. The impact of 3 different distraction techniques on the pain and anxiety levels of children during venipuncture. Clinical Journal of Pain 2019;35(2):140-7. [Google Scholar]
Jeffs 2010 {unpublished data only}
- Jeffs D. Comparison of virtual reality and passive distraction on burn wound care pain in adolescents. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2010.
Jeffs 2013 {published data only}
- Jeffs D, Dorman D, Brown S, Files A, Graves T, Kirk E, et al. Effect of virtual reality on adolescent pain during burn wound care. 45th Annual Meeting of the American Burn Association - Journal of Burn Care and Research 2013;34((2 Suppl1)):S75. [Google Scholar]
Kumar 2017 {unpublished data only}
- Kumar KA, Das S. Perioperative anxiety and stress in children and parents undergoing congenital cardiac surgery: Effect of brief intervention. WHO International Clinical Trials Registry (http://www.who.int/trialsearch) [accessed 25 October 2019] 2017.
Leibovici 2009 {published data only}
- Leibovici V, Magora F, Cohen S, Ingber A. Effects of virtual reality immersion and audiovisual distraction techniques for patients with pruritus. Pain Research and Management 2009;14(4):283-6. [Google Scholar]
LeMay 2016a {unpublished data only}
- LeMay S. Decreasing recurrent pain and anxiety in medical procedures with a pediatric population: trial (DREAM-T). ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2016.
LeMay 2017a {unpublished data only}
- *.Khadra C, Ballard A, Déry J, Paquin D, Fortin J-S, Perreault I, et al. Projector-based virtual reality dome environment for procedural pain and anxiety in young children with burn injuries: a pilot study. Journal of Pain Research 2018;11:343-53. [Google Scholar]
- LeMay S. Virtual reality distraction for procedural pain management and anxiety in children with burn injuries: a pilot study. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2017.
Li 2011 {published data only}
- Li WHC, Chung JO, Ho EK. The effectiveness of therapeutic play, using virtual reality computer games, in promoting the psychological well-being of children hospitalised with cancer. Journal of Clinical Nursing 2011;20:2135-43. [Google Scholar]
Lozano 2018 {published data only}
- Lozano EI, Potterton JL. The use of Xbox Kinect™ in a Paediatric Burns Unit. South African Journal of Physiotherapy 2018;74(1):a429. [Google Scholar]
MacLaren 2005 {published data only}
- MacLaren JE, Cohen LL. A comparison of distraction strategies for venipuncture distress in children. Journal of Pediatric Psychology 2005;30(5):387-96. [Google Scholar]
Marteau 2018 {unpublished data only}
- Marteau S. Evaluation of pain and anxiety in patients with an invasive procedure in emergencies. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 25 October 2019] 2018.
Miller 2009 {published data only}
- Miller K, Rodger S, Bucolo S, Wang XQ, Kimble RM. Study on the pain of relieving children's wound healing with multi-sensory distraction device. Chinese Journal of Burns 2009;25:352-6. [Google Scholar]
Miller 2010 {published data only}
- Miller K, Rodger S, Bucolo S, Greer R, Kimble RM. Multi-modal distraction: using technology to combat pain in young children with burn injuries. Burns 2010;36:647-58. [Google Scholar]
Miller 2011 {published data only}
- Miller K, Rodger S, Kipping B, Kimble RM. A novel technology approach to pain management in children with burns: a prospective randomized controlled trial. Burns 2011;37:395-405. [Google Scholar]
Miller 2016 {published data only}
- Miller K, Tan X, Hobson AD, Khan A, Ziviani J, O’Brien E, et al. A prospective randomized controlled trial of nonpharmacological pain management during intravenous cannulation in a pediatric emergency department. Pediatric Emergency Care 2016;32:444-51. [Google Scholar]
Minute 2012 {published data only}
- Minute M, Badina L, Cont G, Montico M, Ronfani L, Barbi E, et al. Videogame playing as distraction technique in course of venipuncture [La Pediatria medicae chirurgica]. Medical and Surgical Pediatrics 2012;34:77-83. [Google Scholar]
Mosso 2008 {published data only}
- Mosso JL, Gorini A, Senties S, la Cerda G, López G, Vaca VL, et al. Virtual reality on mobile phones to reduce anxiety in outpatient surgery. Annual Review of Cybertherapy and Telemedicine 2008;6:140-5. [Google Scholar]
Mott 2008 {published data only}
- Mott J, Bucolo S, Cuttle L, Mill J, Hilder M, Miller K, et al. The efficacy of an augmented virtual reality system to alleviate pain in children undergoing burns dressing changes: a randomised controlled trial. Burns 2008;34:803-8. [Google Scholar]
Newell 2018 {published data only}
- Newell A, Keane J, McGuire BE, Heary C, McDarby V, Dudley B, et al. Interactive versus passive distraction and parent psychoeducation as pain management techniques during pediatric venepuncture: a randomised controlled trial. Clinical Journal of Pain 2018;34(11):1008-16. [Google Scholar]
Nilsson 2007 {published data only}
- Nilsson S, Enskär K, Finnström B, Brunsson I. Virtual reality in a child oncology unit. Pediatric Blood and Cancer 2007;49(4(supplement, 39th Annual Conference of the International Society of Paediatric Oncology, SIOP 2007, Mumbai, India):412, Abstract 0.049. [Google Scholar]
Nilsson 2013 {published data only}
- Nilsson S, Enskär K, Hallqvist C, Kokinsky E. Active and passive distraction in children undergoing wound dressings. Journal of Pediatric Nursing 2013;28:158-66. [Google Scholar]
Parker 2016 {published data only}
- Parker M, Delahunty B, Heberlein N, Devenish N, Wood FM, Jackson T, et al. Interactive gaming consoles reduced pain during acute minor burn rehabilitation: A randomized, pilot trial. Burns 2016;42:91-6. [Google Scholar]
Patterson 2010 {published data only}
- Patterson DR, Jensen MP, Wiechman SA, Sharar SR. Virtual reality hypnosis for pain associated with recovery from physical trauma. International Journal of Clinical and Experimental Hypnosis 2010;58(3):288-300. [Google Scholar]
Shah 2018 {unpublished data only}
- Shah N. Role of virtual reality (VR) in patients with sickle cell disease (SCD). ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2018.
Sharar 2008 {published data only}
- Sharar SR, Miller W, Teeley A, Soltan M, Hoffman HG, Jensen MP, et al. Applications of virtual reality for pain management in burn-injured patients. Expert Review of Neurotherapeutics 2008;8(11):1667-74. [Google Scholar]
Sharer 2007 {published data only}
- Sharar SR, Carrougher GJ, Nakamura D, Hoffman HG, Blough DK, Patterson DR. Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: preliminary results from 3 ongoing studies. Archives of Physical Medicine & Rehabilitation 2007;88(Suppl 2):S43-9. [Google Scholar]
Small 2015 {published data only}
- Small C, Stone R, Pilsbury J, Bowden M, Bion J. Virtual restorative environment therapy as an adjunct to pain control during burn dressing changes: study protocol for a randomised controlled trial. Trials 2015;16:329. [Google Scholar]
Tropez‐Arceneaux 2011 {published data only}
- Tropez-Arceneaux LL, Meyer WJ, Hoffman HG, Fuchs HL, Kampschmidt J, Suman OE. Pain and perceived exertion in pediatric burn patients during exercise with virtual reality. 43rd Annual Meeting of the American Burn Association - Journal of Burn Care and Research 2011;32:S66. [Google Scholar]
Tschiedel 2019 {published data only}
- Tschiedel E, Beckers K, GroBe-Lordemann A, Basu O, Felderhoff-Muser U, Dohna-Schwake C. Visual distraction during sleep induction with propofol in pediatric patients - can cartoon watching influence the sedative dose? Klinische Padiatric 2019;231(1):35-40. [Google Scholar]
vanGoor 2019 {published data only}
- vanGoor H. The effect of virtual reality on post-surgery pain and recovery. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 18 November 2019] 2019.
vanRooijen 2017 {unpublished data only}
- vanRooijen SJ. The effect of virtual reality as an information tool on anxiety, pain and patient satisfaction in children undergoing intravenous infusion. NTR: Netherlands Trial Register (http://www.trialregister.nl/) [accessed 7 September 2018] 2017.
Ver Lee 2012 {published data only}
- VerLee S, Butz C, Ackerman C, Burger J, Fabia R, Besner G. The utility of virtual reality in minimising procedural distress with pediatric burn patients. 44th Annual Meeting of the American Burn Association - Journal of Burn Care and Research 2012;1:S178. [Google Scholar]
Windlich‐Biermeier 2007 {published data only}
- Windlich-Biermeirer A, Sjoberg I, Dale JC, Eshelman D, Guzzetta CE. Effects of distraction on pain, fear and distress during venous post access and venipuncture in children and adolescents with cancer. Journal of Pediatric Oncology Nursing 2007;24(1):8-19. [Google Scholar]
Wint 2002 {published data only}
- Wint SS, Eshelman D, Steele J, Guzzetta CE. Effects of distraction using virtual reality glasses during lumbar punctures in adolescents with cancer. Oncology Nursing Forum 2002;9(1):e8-15. [Google Scholar]
Wolyniez 2013 {published data only}
- Wolyniez I, Rimon A, Scolnik D, Gruber A, Tavor O, Haviv E, et al. The effect of a medical clown on pain during intravenous access in the pediatric emergency department: a randomized prospective pilot study. Clinical Pediatrics 2013;52(12):1168-72. [Google Scholar]
Yuan 2018 {published data only}
- Yuan JC, Joseph A, Rodriguez S, Caruso TJ. Active virtual reality improves vascular access compliance in anxious children. Anesthesia and Analgesia 2018;127(1):114-5. [Google Scholar]
Zelmar 2015 {unpublished data only}
- Zelmar A. Augmented reality to reduce pain during botulinum toxin injections in cerebral-palsied children (MINIDOCS). ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2015.
References to studies awaiting assessment
Festini 2016 {unpublished data only}
- Festini F. Virtual reality for the reduction of pain during venipuncture in children with CF (VRAP). ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2016.
Meyer 2014 {unpublished data only}
- Meyer W. Virtual reality analgesia for pediatric burn survivors. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2014.
NCH 2016 {unpublished data only}
- Dunn AL, Patterson J, Biega C. A feasibility and usability study of a nursing orchestrated, customized 3 dimensional virtual reality environment in children with hemophilia undergoing routine intravenous procedures. In: Blood. Vol. 130. 2017:3691.
- *.Nationwide Children’s Hospital. Virtual reality for hemophilia. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2016.
Patterson 2009 {unpublished data only}
- Patterson DR. Virtual reality analgesia during pediatric physical therapy (VRD/Peds). ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2009.
References to ongoing studies
ACTRN12617000285358 {unpublished data only}
- ACTRN12617000285358. Investigating the management of paediatric procedural pain relief obtained through virtual reality (IMPROVR) [To investigate the effect of using Virtual reality distraction (using a computer simulation of an environment) on pain and distress in children aged 4 – 11 year olds during needle based procedures compared to standard care]. anzctr.org.au/Trial/Registration/TrialReview.aspx?id=372399 (first received 23 Feburary 2017).
ACTRN12618001363279 {unpublished data only}
- ACTRN12618001363279. The use of a virtual reality headset for 4 year old immunisations to reduce pain and distress [Virtual reality for immunisation pain: a randomised controlled clinical trial in general practice]. anzctr.org.au/Trial/Registration/TrialReview.aspx?id=375746 (first received 6 August 2018).
LeMay 2016b {unpublished data only}
- *.LeMay S, Paquin D, Bouchard S, Fortin J-S, Khadra C. DREAM Project: Decreasing recurrent pain and anxiety in medical procedures on a pediatric population. International Journal of Virtual Reality 2016;16(1):49-57. [Google Scholar]
- LeMay S. Decreasing recurrent pain and anxiety in medical procedures with a pediatric population: a pilot study (DREAM-P). ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 7 September 2018] 2017.
NCT02646787 {unpublished data only}
- NCT02646787. Virtual reality water friendly wound care (H2OWC) [Water friendly virtual reality for burns]. clinicaltrials.gov/ct2/show/NCT02646787 (first received 6 Janurary 2016).
NCT02929771 {unpublished data only}
- NCT02929771. Using virtual reality to reduce procedural pain in children with cancer [Using virtual reality to reduce procedural pain in children with cancer: a pilot randomized controlled trial]. clinicaltrials.gov/ct2/show/NCT02929771 (first received 11 October 2016).
NCT02986464 {unpublished data only}
- NCT02986464. Virtual reality distraction for procedural pain management in children with burn injuries: a randomized controlled trial. clinicaltrials.gov/ct2/show/NCT02986464 (first received 8 December 2016).
NCT03155607 {unpublished data only}
- NCT03155607. Novel virtual reality for burn wound care pain in adolescents. clinicaltrials.gov/ct2/show/study/NCT03155607 (first received 16 May 2017).
NCT03239743 {unpublished data only}
- NCT03239743. Effects of virtual reality on pre-operative anxiety and induction of anesthesia in children and adolescents [A pilot study to evaluate the efficacy of virtual reality on pre-operative anxiety and Induction of anesthesia in a children's hospital]. clinicaltrials.gov/ct2/show/NCT03239743 (first received 4 August 2017).
NCT03304769 {unpublished data only}
- NCT03304769. Virtual reality distraction during pediatric intravenous line placement [Virtual reality distraction during pediatric intravenous line placement: a prospective randomized comparison study]. clinicaltrials.gov/ct2/show/NCT03304769 (first received 9 October 2017).
NCT03353584 {unpublished data only}
- NCT03353584. Effect of virtual reality technology for pain management of vaso-occlusive crisis in patients with sickle cell disease [Pain management of vaso-occlusive crisis in children and young adults with sickle cell disease-effect of virtual reality technology]. clinicaltrials.gov/ct2/show/NCT03353584 (first received 27 November 2017).
NCT03435367 {unpublished data only}
- NCT03435367. Immersive virtual reality to reduce procedural pain during IV insertion in children in the emergency department [Immersive virtual reality to reduce procedural pain during IV insertion in children in the emergency department: a feasibility pilot study]. clinicaltrials.gov/ct2/show/NCT03435367 (first received 19 February 2018).
NCT03464955 {unpublished data only}
- NCT03464955. VR usage in non-invasive surgical sub-specialty procedures [Virtual reality usage in non-invasive surgical sub-specialty procedures]. clinicaltrials.gov/ct2/show/NCT03464955 (first received 14 March 2018).
NCT03480724 {unpublished data only}
- NCT03480724. Assessing the efficacy of virtual reality analgesia (VRA) in pediatric patients for pain control (PEDSPAINVR) [Assessing the efficacy of virtual reality analgesia (VRA) in pediatric patients for pain control during botox injections for spasticity management: a randomized control trial]. clinicaltrials.gov/ct2/show/NCT03480724 (first received 29 March 2018).
NCT03518346 {unpublished data only}
- NCT03518346. Use of virtual reality game playing during venipuncture. clinicaltrials.gov/ct2/show/NCT03518346 (first received 8 May 2018).
NCT03521076 {unpublished data only}
- NCT03521076. Randomized controlled trial of virtual reality [Randomized controlled trial of virtual reality for pain management in a specialty rehabilitation context]. clinicaltrials.gov/ct2/show/NCT03521076 (first received 11 May 2018).
NCT03584776 {unpublished data only}
- NCT03584776. Virtual reality for post-operative pain management [A randomized controlled trial of virtual reality for pain management in the post-operative period following orthopedic surgery]. clinicaltrials.gov/ct2/show/NCT03584776 (first received 12 July 2018).
NCT03645213 {published data only}
- NCT03645213. Two different distraction methods on pain and fear duingvenipuncture in children [Comparision of two different distraction methods on pain and fear during venipuncture in school-age children: a randomized controlled trial]. clinicaltrials.gov/ct2/show/NCT03645213 (first retrieved 24 August 2018).
NCT03680625 {unpublished data only}
- NCT03680625. Virtual reality vs passive distraction for pain management [Virtual reality compared to passive distraction for pain management during orthopedic procedures in children: a randomized controlled trial.]. clinicaltrials.gov/ct2/show/NCT03680625 (first received 21 September 2018).
NCT03681717 {unpublished data only}
- NCT03681717. Virtual reality vs. standard-of-care for comfort during laceration repair [A pragmatic randomized controlled trial of virtual reality vs. standard-of-care for comfort during laceration repair]. clinicaltrials.gov/ct2/show/NCT03681717 (first received 24 September 2018).
NCT03681730 {unpublished data only}
- NCT03681730. Virtual reality vs. standard-of-care for comfort during intravenous catherterization [A pragmatic randomized controlled trial of virtual reality vs standard-of-care for comfort during intravenous catheterization]. clinicaltrials.gov/ct2/show/NCT03681730 (first received 24 September 2018).
NCT03681743 {unpublished data only}
- NCT03681743. Virtual reality vs. standard-of-care for comfort during minor plastic surgery procedures in children [A pragmatic randomized controlled trial of virtual reality vs. standard-of-care for comfort during minor plastic surgery procedures in children]. clinicaltrials.gov/ct2/show/NCT03681743 (first received 24 September 2018).
NCT03693469 {published data only}
- NCT03693469. Virtual reality vs. standard-of-care for comfort during immunizations in children [A pragmatic randomized controlled trial of virtual reality vs. standard-of-care for comfort during immunizations in children]. clinicaltrials.gov/ct2/show/NCT03693469 (first received 3 October 2018).
NCT03750578 {published data only}
- NCT03750578. Virtual reality for needle procedures in pediatric emergency department [Distraction in the emergency using virtual reality for intravenous needs in children to improve comfort (DEVINCI): a pilot randomized controlled trial]. clinicaltrials.gov/ct2/show/NCT03750578 (first received 23 November 2018).
NCT03784352 {published data only}
- NCT03784352. Virtual reality pediatric orthopaedic outpatient procedures [Virtual reality in reducing pain and anxiety in pediatric orthopaedics, a pilot randomized controlled trial]. clinicaltrials.gov/ct2/show/NCT03784352 (first received 21 December 2018).
NCT03888690 {unpublished data only}
- NCT03888690. Effect of virtual reality distraction on procedural pain for children and adolescents in onco-haematology unit [Randomized controlled trial evaluating the effectiveness of the virtual reality distraction compared to current practice on reducing procedural pain in children and adolescents supported in pediatric onco-hematology unit]. clinicaltrials.gov/ct2/show/NCT03888690 (first received 25 March 2019).
NCT03903510 {published data only}
- NCT03903510. Virtual reality during paediatric cast removal [A randomized control trial of virtual reality to reduce anxiety during pediatric cast removal]. clinicaltrials.gov/ct2/show/NCT03903510 (first received 4 April 2019).
NCT03913897 {published data only}
- NCT03913897. The effect of virtual reality and kaleidoscope on pain and anxiety levels during venepuncture in children. clinicaltrials.gov/ct2/show/NCT03913897 (first received 12 April 2019).
NCT03985930 {unpublished data only}
- NCT03985930. Non-immersive virtual reality for paediatric pain management. clinicaltrials.gov/ct2/show/NCT03985930 (first received 14 June 2019).
NCT04040036 {published data only}
- NCT04040036. Effects of virtual reality on pain, fear and anxiety during blood draw in children aged 5-12 years old [Effects of virtual reality on pain, fear and anxiety during blood draw in children aged 5-12 years old: a randomized controlled study]. clinicaltrials.gov/ct2/show/NCT04040036 (first received 31 July 2019).
Wong 2019 {unpublished data only}
- ChiCTR1800016589. Effects of immersive virtual reality intervention on pain and anxiety among paediatric patients undergoing venipuncture: a randomized controlled trial. chictr.org.cn/showprojen.aspx?proj=28246 (first received 11 June 2018).
- *.Wong CL, Wa Lui MM, Choi KC. Effects of immersive virtual reality intervention on pain and anxiety among pediatric patients undergoing venipuncture: a study protocol for a randomized controlled trial. Trials 2019;20(369):doi.org/10.1186/s13063-019-3443-z. [Google Scholar]
Additional references
Aguinis 2001
- Aguinis H, Henle CA, Beaty JC. Virtual reality technology: a new tool for personnel selection. International Journal of Selection and Assessment 2001;9(1/2):70-83. [Google Scholar]
Ahmadi 2001
- Ahmadi M. Virtual reality may help children undergoing chemotherapy. Journal of the National Cancer Institute 2001;93:675-6. [Google Scholar]
Aydede 2017
- Aydede M. Defending the IASP definition of pain. The Monist 2017;100(4):439-64. [Google Scholar]
Becker 2018
- Becker S, Navratilova E, Nees F, Van Danme S. Emotional and motivational pain processing: current state of knowledge and perspectives in translational research. Pain, Research and Management 2018;Jul 18:doi.org/10.1155/2018/5457870. [Google Scholar]
Birnie 2018
- Birnie KA, Noel M, Chambers CT, Uman LS, Parker JA. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database of Systematic Reviews 2018, Issue 10. Art. No: CD005179. [DOI: 10.1002/14651858.CD005179.pub4] [DOI] [Google Scholar]
Blount 2006
- Blount RL, Piira T, Cohen LL, Cheng PS. Pediatric procedural pain. Behavior Modification 2006;30(1):24-49. [Google Scholar]
Bohil 2011
- Bohil CJ, Alicea B, Biocca FA. Virtual reality in neuroscience research and therapy. Nature Reviews Neuroscience 2011;12:752-62. [Google Scholar]
Brown 2012
- Brown NJ, Rodger S, Ware RS, Kimble RM, Cuttle L. Efficacy of a children’s procedural preparation and distraction device on healing in acute burn wound care procedures: study protocol for a randomized controlled trial. Trials 2012;13:238. [Google Scholar]
Brudvik 2016
- Brudvik C, Moutte S-D, Baste V, Morken T. A comparison of pain assessment by physicians, parents and children in an outpatient setting. Emergency Medicine 2017;32:138-144. [Google Scholar]
Butler 2005
- Butler LD, Symons BK, Henderson SL, Shortliffe LD, Spiegel D. Hypnosis reduces distress and duration of an invasive medical procedure for children. Pediatrics 2005;115(1):e77-85. [Google Scholar]
Clift 2007
- Clift L, Dampier S, Timmons S. Adolescents’ experiences of emergency admission to children’s wards. Journal of Child Health Care 2007;11(3):195-207. [Google Scholar]
Council of Europe 2011
- Council of Europe. Guidelines on child-friendly health care. Available from https://wcd.coe.int/ViewDoc.jsp?id=1836421&Site=COE [accessed 10th June 2012] 2011.
Covidence 2018 [Computer program]
- Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org, 2018.
Cummings 1996
- Cummings EA, Reid GJ, Finley AC, McGrath PJ, Ritchie JA. Prevalence and source of pain in pediatric patients. Pain 1996;68:25-31. [Google Scholar]
Curtis 2012
- Curtis S, Wingert A, Ali S. The Cochrane Library and procedural pain in children: an overview of reviews. Evidence-Based Child Health: A Cochrane Review Journal 2012;7:1363-99. [Google Scholar]
Dwan 2019
- Dwan K, Li T, Altman DG, Elbourne D. CONSORT 2010 statement: extension to randomised crossover trials. British Medical Journal 2019;366(14378):doi: 10.1136/bmj.l4378. [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. British Medical Journal 1997;315:629-34. [Google Scholar]
Eijlers 2019
- Eijlers R, Utens EM, Staals LM, Nijs PF, Berghmans JM, Wijnen RM, et al. Systematic review and meta-analysis of virtual reality in pediatrics: effects on pain and anxiety. Anesthesia and Analgesia 2019;129(5):1344-53. [Google Scholar]
Forsner 2009
- Forsner M. Afraid of medical care: school-aged children’s narratives about medical fear. Journal of Pediatric Nursing 2009;24(6):519-28. [Google Scholar]
Fox 2016
- Fox JK, Halpern LF, Dangman BC, Giramonti KM, Kogan BA. Children’s anxious reactions to an invasive medical procedure: The role of medical and non-medical fears. Journal of Health Psychology 2016;21(8):1587-96. [Google Scholar]
Garcia‐Munitis 2006
- Garcia-Munitis P, Bandeira M, Pistorio A, Magni-Manzoni S, Ruperto N, Schivo A, et al. Level of agreement between children, parents and physicians in rating pain intensity in juvenile idiopathic arthritis. Arthritis and Rheumatism 2006;55(2):177-183. [Google Scholar]
Garrett 2014
- Garrett B, Taverner T, Masinde W, Gromala D, Shaw C, Negraeff M. A rapid evidence assessment of immersive virtual reality as an adjunct therapy in pain management. Clinical Journal of Pain 2014;30(12):1089-98. [Google Scholar]
Gershon 2003
- Gershon J, Zimand E, Lemos R, Rothbaum BO, Hodges L. Use of virtual reality as a distractor for painful procedures in a patient with pediatric cancer: a case study. CyberPsychology and Behavior 2003;6(6):657-61. [Google Scholar]
Goodenough 1999
- Goodenough B, Thomas W, Champion GD, Perrott D, Taplin JE, vonBaeyer CL, et al. Unravelling age effects and sex differences in needle pain: ratings of sensory intensity and unpleasantness of venepuncture pain by children and their parents. Pain 1999;80:179-90. [Google Scholar]
Gorini 2011
- Gorini A, Capideville CS, DeLeo G, Mantovani F, Riva G. The role of immersion and narrative in mediated presence: the virtual hospital experience. Cyberpsychology, Behavior and Social Networking 2011;14(3):99-105. [Google Scholar]
Groenewald 2012
- Groenewald CB, Rabbitts JA, Schroeder DR, Harrison TE. Prevalence of moderate–severe pain in hospitalized children. Pediatric Anesthesia 2012;22(7):661-8. [Google Scholar]
Harbord 2006
- Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Statistics in Medicine 2006;25:3443-57. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration 2011, Available from www.cochrane-handbook.org.
Hoffman 2000
- Hoffman HG, Doctor JN, Patterson DR, Carrougher GJ, Furness TA. Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain 2000;85:305-9. [Google Scholar]
Hoffman 2004a
- Hoffman HG. Virtual-reality therapy. Scientific American 2004;291(1):58-65. [Google Scholar]
Hoffman 2011
- Hoffman HG, Chambers G, Meyer W, Arceneaux LL, Russell W, Seibel E, et al. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Annals of Behavioral Medicine 2011;41(2):183-91. [Google Scholar]
Horstman 2002
- Horstman M, Bradding A. Helping children to speak up in the health service. European Journal of Oncology Nursing 2002;6(2):75-84. [Google Scholar]
Iannicelli 2019
- Iannicelli AM, Vito D, Dodaro CA, De Matteo P, Nocerino R, Sepe A, et al. Does virtual reality reduce pain in pediatric patients? A systematic review. Italian Journal of Pediatrics 2019;45(171):doi.org/10.1186/s13052-019-0757-0. [Google Scholar]
IASP 2011
- International Association for the Study of Pain (IASP). Pain terms: a current list with definitions and notes on usage: recommended by the IASP Subcommittee on Taxonomy. Available at: https://www.iasp-pain.org/terminology?navItemNumber=576 2011.
Kenney 2016
- Kenney MP, Milling LS. The effectiveness of virtual reality distraction for reducing pain: a meta-analysis. Psychology of Consciousness: Theory, Research and Practice 2016;3(3):199-210. [Google Scholar]
Kilkelly 2011
- Kilkelly U. Child-friendly health care: the views and experiences of children and young people in Council of Europe member states. Available at: http://www.coe.int/t/dg3/health/Child_Friendly_Healthcare_Final_Report__English_version_.pdf [accessed 10th June 2012] 2011.
Klassen 2008
- Klassen JA, Liang Y, Tjosvold L, Klassen TP, Hartling L. Music for pain and anxiety in children undergoing medical procedures: a systematic review of randomized controlled trials. Ambulatory Pediatrics 2008;8:117-28. [Google Scholar]
Koller 2012
- Koller D, Goldman RD. Distraction techniques for children undergoing procedures: a critical review of pediatric research. Journal of Pediatric Nursing 2012;27(6):652-81. [Google Scholar]
Kortesluoma 2004
- Kortesluoma R-L, Nikkonen M. ‘I had this horrible pain’: the sources and causes of pain experiences in 4- to 11-year-old hospitalized children. Journal of Child Health Care 2004;8(3):210-31. [Google Scholar]
Kortesluoma 2006
- Kortesluoma R, Nikkonen M. “The most disgusting ever”: children’s pain descriptions and views of the purpose of pain. Journal of Child Health Care 2006;10(3):213-26. [Google Scholar]
Landier 2010
- Landier W, Tse AM. Use of complementary and alternative medical interventions for the management of procedure-related pain, anxiety, and distress in pediatric oncology: an integrative review. Journal of Pediatric Nursing 2010;25:566-79. [Google Scholar]
Lessister 2001
- Lessister J, Freeman J, Keogh E, Davidoff J. A cross-media presence Questionnaire: the ITC-sense of presence Inventory. Presence: Teleoperators and Virtual Environments 2001;10(3):282-297. [Google Scholar]
Li 2009
- Li WHC, Chung OKJ. Enhancing the efficacy of psychoeducational interventions for paediatric patients in a randomized controlled trial: methodological considerations. Journal of Clinical Nursing 2009;18:3013-21. [Google Scholar]
Low 2008
- Low DK, Pittaway AP. The ‘iPhone’ induction – a novel use for Apple iphone. Pediatric Anesthesia 2008;18:559-77. [Google Scholar]
MacLaren 2007
- MacLaren JE, Cohen LL. Interventions for paediatric procedure-related pain in primary care. Paediatric Child Health 2007;12(2):111-6. [Google Scholar]
Malloy 2010
- Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clinical Psychology Review 2010;30:1011-8. [Google Scholar]
McCaul 1984
- McCaul KD, Malott JM. Distraction and coping with pain. Psychological Bulletin 1984;95:516-33. [Google Scholar]
McGrath 2008
- McGrath PJ, Walco GA, Turk DC, Dworkin RH, Brown MT, Davidson K, et al. Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. Journal of Pain 2008;9(9):771-83. [Google Scholar]
Melnyk 2000
- Melnyk BM. Intervention studies involving parents of hospitalized young children: an analysis of the past and future recommendations. Journal of Pediatric Nursing 2000;15(1):4-13. [Google Scholar]
Mobily 1993
- Mobily PR, Herr KA, Kelly LS. Cognitive-behavioural techniques to reduce pain: a validation study. International Journal of Nursing Studies 1993;30(6):537-48. [Google Scholar]
Morris 2009
- Morris LD, Louw QA, Grimmer-Somers K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: a systematic review. Clinical Journal of Pain 2009;25(9):815-26. [Google Scholar]
Patel 2006
- Patel A, Schieble T, Davidson M, Tran MC, Schoenberg C, Delphin E, et al. Distraction with a hand-held video game reduces pediatric preoperative anxiety. Pediatric Anesthesia 2006;6:1019-27. [Google Scholar]
Racine 2016
- Racine NM, Pillai Riddell RR, Khan M, Calic M, Taddio A, Tablon P. Systematic review: predisposing, precipitating, perpetuating, and pesent factors predicting anticipatory distress to painful medical procedures in children. Journal of Pediatric Psychology 2016;41(2):159-181. [Google Scholar]
Rassin 2004
- Rassin M, Gutman Y, Silner D. Developing a computer game to prepare children for surgery. Association of periOperative Registered Nurses (AORN) Journal 2004;80(6):1095-102. [Google Scholar]
RevMan 2014
- Review Manager (RevMan) [Computer program]. Version 5.3.. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration 2014.
Ryan 2011
- Ryan R, Hill S, Prictor M, McKenzie J, Cochrane Consumers and Communication Review Group. Study Quality Guide. Available from http://www.latrobe.edu.au/chcp/cochrane/resources.html 2011.
Schneider 1999
- Schneider SM, Workman ML. Effects of virtual reality on symptom distress in children receiving chemotherapy. CyberPsychology and Behavior 1999;2:125-34. [Google Scholar]
Schneider 2000
- Schneider SM, Workman ML. Virtual reality as a distraction intervention for older children receiving chemotherapy. Pediatric Nursing 2000;26(6):593-7. [Google Scholar]
Schunemann 2011
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and ‘Summary of findings' tables. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration. Available from www.cochrane-handbook.org, 2011. [Google Scholar]
Steele 2003
- Steele E, Grimmer K, Thomas B, Mulley B, Fulton I, Hoffman H. Virtual reality as a pediatric pain modulation technique: a case study. CyberPsychology and Behavior 2003;6(6):633-8. [Google Scholar]
Stevens 2011
- Stevens JB, Abbott LK, Yamada J, Harrison D, Stinson J, Taddio A, et al. Epidemiology and management of painful procedures in children in Canadian hospitals. Canadian Medical Association Journal 2011;183(7):e403-10. [Google Scholar]
Stinson 2006
- Stinson JN, Kavanagh T, Yamada J, Gill N, Stevens B. Systematic review of the psychometric properties, interpretability and feasibility of self-report pain intensity measures for use in clinical trials in children and adolescents. Pain 2006;125:143-57. [Google Scholar]
Stinson 2008
- Stinson J, Yamada J, Dickson A, Lamba J, Stevens B. Review of systematic reviews on acute procedural pain in children in the hospital setting. Pain Research and Management 2008;13(1):51-7. [Google Scholar]
Taylor 2008
- Taylor EM, Boyer K, Campbell FA. Pain in hospitalized children: a prospective cross-sectional survey of pain prevalence, intensity, assessment and management in a Canadian pediatric teaching hospital. Pain Research and Management 2008;13(1):25-32. [Google Scholar]
von Baeyer 2007
- Baeyer CL, Spagrud LJ. Systematic review of observational (behavioral) measures of pain for children and adolescents aged 3 to 18 years. Pain 2007;127(1):140-50. [Google Scholar]
Weiss 2003
- Weiss PL, Naveh Y, Katz N. Design and testing of a virtual environment to train stroke patients with unilateral spatial neglect to cross a street safely. Occupational Therapy International 2003;10(1):39-55. [Google Scholar]
Williams 2012
- Williams K, Thomson D, Seto I, Contopoulos-Ioannidis DG, Ioannidis JP, Curtis S, et al. Standard 6: age groups for pediatric trials. Pediatrics 2012;129(Suppl 3):S153-60. [Google Scholar]
Williams 2016
- Williams AC, Craig KD. Updating the definition of pain. Pain 2016;157:2420-3. [Google Scholar]
Wohlheiter 2013
- Wohlheiter KA, Dahlquist LM. Interactive versus passive distraction for acute pain management in young children: the role of selective attention and development. Journal of Pediatric Psychology 2013;38(2):202-12. [Google Scholar]
Wollin 2004
- Wollin SR, Plummer JL, Owen H, Hawkins RM, Materazzo F, Morrison V. Anxiety in children having elective surgery. Paediatric Nursing 2004;19(2):128-32. [Google Scholar]
Won 2017
- Won AS, Bailey J, Bailenson J, Tataru C, Yoon IA, Golianu B. Immersive virtual reality for pediatric pain. Children 2017;4(52):doi: 10.3390/children4070052. [Google Scholar]
Young 2005
- Young KD. Pediatric procedural pain. Annals of Emergency Medicine 2005;45(2):160-71. [Google Scholar]
References to other published versions of this review
Lambert 2013
- Lambert V, Matthews A, Hicks P, Boran L, Devane D. Virtual reality simulation for reducing pain in children. Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No: CD010686. [DOI: 10.1002/14651858.CD010686] [DOI] [Google Scholar]


