Abstract
Background
Antisocial personality disorder (AsPD) is associated with poor mental health, criminality, substance use and relationship difficulties. This review updates Gibbon 2010 (previous version of the review).
Objectives
To evaluate the potential benefits and adverse effects of psychological interventions for adults with AsPD.
Search methods
We searched CENTRAL, MEDLINE, Embase, 13 other databases and two trials registers up to 5 September 2019. We also searched reference lists and contacted study authors to identify studies.
Selection criteria
Randomised controlled trials of adults, where participants with an AsPD or dissocial personality disorder diagnosis comprised at least 75% of the sample randomly allocated to receive a psychological intervention, treatment‐as‐usual (TAU), waiting list or no treatment. The primary outcomes were aggression, reconviction, global state/functioning, social functioning and adverse events.
Data collection and analysis
We used standard methodological procedures expected by Cochrane.
Main results
This review includes 19 studies (eight new to this update), comparing a psychological intervention against TAU (also called 'standard Maintenance'(SM) in some studies). Eight of the 18 psychological interventions reported data on our primary outcomes.
Four studies focussed exclusively on participants with AsPD, and 15 on subgroups of participants with AsPD. Data were available from only 10 studies involving 605 participants.
Eight studies were conducted in the UK and North America, and one each in Iran, Denmark and the Netherlands. Study duration ranged from 4 to 156 weeks (median = 26 weeks). Most participants (75%) were male; the mean age was 35.5 years. Eleven studies (58%) were funded by research councils. Risk of bias was high for 13% of criteria, unclear for 54% and low for 33%.
Cognitive behaviour therapy (CBT) + TAUversus TAU
One study (52 participants) found no evidence of a difference between CBT + TAU and TAU for physical aggression (odds ratio (OR) 0.92, 95% CI 0.28 to 3.07; low‐certainty evidence) for outpatients at 12 months post‐intervention.
One study (39 participants) found no evidence of a difference between CBT + TAU and TAU for social functioning (mean difference (MD) −1.60 points, 95% CI −5.21 to 2.01; very low‐certainty evidence), measured by the Social Functioning Questionnaire (SFQ; range = 0‐24), for outpatients at 12 months post‐intervention.
Impulsive lifestyle counselling (ILC) + TAU versus TAU
One study (118 participants) found no evidence of a difference between ILC + TAU and TAU for trait aggression (assessed with Buss‐Perry Aggression Questionnaire‐Short Form) for outpatients at nine months (MD 0.07, CI −0.35 to 0.49; very low‐certainty evidence).
One study (142 participants) found no evidence of a difference between ILC + TAU and TAU alone for the adverse event of death (OR 0.40, 95% CI 0.04 to 4.54; very low‐certainty evidence) or incarceration (OR 0.70, 95% CI 0.27 to 1.86; very low‐certainty evidence) for outpatients between three and nine months follow‐up.
Contingency management (CM) + SM versus SM
One study (83 participants) found evidence that, compared to SM alone, CM + SM may improve social functioning measured by family/social scores on the Addiction Severity Index (ASI; range = 0 (no problems) to 1 (severe problems); MD −0.08, 95% CI −0.14 to −0.02; low‐certainty evidence) for outpatients at six months.
‘Driving whilst intoxicated' programme (DWI) + incarcerationversus incarceration
One study (52 participants) found no evidence of a difference between DWI + incarceration and incarceration alone on reconviction rates (hazard ratio 0.56, CI −0.19 to 1.31; very low‐certainty evidence) for prisoner participants at 24 months.
Schema therapy (ST) versus TAU
One study (30 participants in a secure psychiatric hospital, 87% had AsPD diagnosis) found no evidence of a difference between ST and TAU for the number of participants who were reconvicted (OR 2.81, 95% CI 0.11 to 74.56, P = 0.54) at three years. The same study found that ST may be more likely to improve social functioning (assessed by the mean number of days until patients gain unsupervised leave (MD −137.33, 95% CI −271.31 to −3.35) compared to TAU, and no evidence of a difference between the groups for overall adverse events, classified as the number of people experiencing a global negative outcome over a three‐year period (OR 0.42, 95% CI 0.08 to 2.19). The certainty of the evidence for all outcomes was very low.
Social problem‐solving (SPS) + psychoeducation (PE) versus TAU
One study (17 participants) found no evidence of a difference between SPS + PE and TAU for participants’ level of social functioning (MD −1.60 points, 95% CI −5.43 to 2.23; very low‐certainty evidence) assessed with the SFQ at six months post‐intervention.
Dialectical behaviour therapy versus TAU
One study (skewed data, 14 participants) provided very low‐certainty, narrative evidence that DBT may reduce the number of self‐harm days for outpatients at two months post‐intervention compared to TAU.
Psychosocial risk management (PSRM; 'Resettle') versus TAU
One study (skewed data, 35 participants) found no evidence of a difference between PSRM and TAU for a number of officially recorded offences at one year after release from prison. It also found no evidence of difference between the PSRM and TAU for the adverse event of death during the study period (OR 0.89, 95% CI 0.05 to 14.83, P = 0.94, 72 participants (90% had AsPD), 1 study, very low‐certainty evidence).
Authors' conclusions
There is very limited evidence available on psychological interventions for adults with AsPD. Few interventions addressed the primary outcomes of this review and, of the eight that did, only three (CM + SM, ST and DBT) showed evidence that the intervention may be more effective than the control condition. No intervention reported compelling evidence of change in antisocial behaviour. Overall, the certainty of the evidence was low or very low, meaning that we have little confidence in the effect estimates reported.
The conclusions of this update have not changed from those of the original review, despite the addition of eight new studies. This highlights the ongoing need for further methodologically rigorous studies to yield further data to guide the development and application of psychological interventions for AsPD and may suggest that a new approach is required.
Plain language summary
Psychological treatments for people with antisocial personality disorder
Background
People with antisocial personality disorder (AsPD) may behave in a way that is harmful to themselves or others and is against the law. They can be dishonest and act aggressively without thinking. Many also misuse drugs and alcohol. Certain types of psychological treatment, such as talking or thinking therapies, may help people with AsPD. Such treatments aim to change the person’s behaviour, to change the person’s thinking, or to help the person manage feelings of anger, self‐harm, drug and alcohol abuse or negative behaviour.
This review updates one published in 2010.
Review question
What are the effects of talking or thinking therapies for adults (aged 18 years and older) with AsPD, compared to treatment‐as‐usual (TAU), waiting list or no treatment?
Study characteristics
We searched for relevant studies up to 5 September 2019. We found 19 relevant studies for 18 different psychological interventions. Data were reported for 10 studies involving 605 adults (aged 18 years and older) with a diagnosis of AsPD, living in the community, hospital or prison. Eight interventions reported on the main outcomes of the review (aggression, reconviction, general/social functioning and adverse events), but few had data for participants with AsPD. The studies compared a psychological intervention against TAU, which is sometimes referred to as 'standard maintenance' (SM).
Most studies were conducted in the UK or North America and were financed by grants from major research councils. They included more male (75%) participants than females (25%), the average age of which was 35.5 years. The length of the studies ranged from 4 weeks to 156 weeks. Most of the studies (10 of the 19) used methods that were flawed, which means we cannot be certain of their findings and, as a result, are unable to draw any firm conclusions.
Main results
Below, we report the findings for each comparison, where data were available for a primary outcome.
Cognitive behaviour therapy (CBT) + TAUversus TAU. There was no difference between CBT + TAU and TAU for physical aggression or social functioning but the evidence is uncertain.
Impulsive lifestyle counselling (ILC) + TAU versus TAU. There was no difference between ILC + TAU and TAU for aggression or the adverse events of death or incarceration but the evidence is very uncertain.
Contingency management (CM) + SM versus SM. CM + SM, compared to SM, may improve social functioning slightly.
‘Driving whilst intoxicated' programme (DWI) + incarcerationversus incarceration. There was no difference between DWI + incarceration and incarceration on reconviction (re‐arrest) rates but the evidence is very uncertain.
Schema therapy (ST) versus TAU. The evidence is very uncertain about the effect of ST compared to TAU on reconviction. There is some evidence that, compared to TAU, ST may improve one aspect of social functioning: time to unescorted leave. There was no difference between ST and TAU for overall adverse events classified globally as negative outcomes but the evidence is very uncertain.
Social problem‐solving therapy (SPS) + psychoeducation (PE) versus TAU. There was no difference between SPS + PE and TAU for participants’ level of social functioning but the evidence is very uncertain.
Dialectical behaviour therapy (DBT) versus TAU. There was a suggestion that, compared to TAU, DBT may reduce for the number of self‐harm days but the evidence is very uncertain.
Psychosocial risk management (PSRM 'Resettle' programme) versus TAU. There was no difference between PSRM and TAU for the number of offences reported one year after release from prison, or for the risk of dying during the study, although the evidence is very uncertain.
Conclusions
The review shows that there is not enough good quality evidence to recommend or reject any psychological treatment for people with a diagnosis of AsPD.
Summary of findings
Summary of findings 1. Cognitive behaviour therapy + treatment‐as‐usual versus treatment‐as‐usual alone for antisocial personality disorder.
| Cognitive behaviour therapy + treatment‐as‐usual versus treatment‐as‐usual alone for antisocial personality disorder | ||||||
| Patient or population: adults with antisocial personality disorder Setting: outpatient Intervention: cognitive behaviour therapy + treatment‐as‐usual Comparison: treatment‐as‐usual alone | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with treatment‐as‐usual alone | Risk with cognitive behaviour therapy + treatment‐as‐usual | |||||
|
Aggression (any act of physical aggression) Assessed by: number reporting any act of physical aggression measured with the MacArthur Community Violence Screening Instrument (MCVSI) (9 behavioural items, rated yes/no; higher score = greater number of violent behaviour reported) Timing of assessment: 12 months |
Study population | OR 0.92 (0.28 to 3.07) | 52 (1 RCT) | ⊕⊕⊝⊝ Lowa | ‐ | |
| 296 per 1000 | 279 per 1000 (17 fewer per 1000; from 191 fewer to 268 more) | |||||
| Reconviction | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Global state/functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
|
Social functioning Assessed by: Social Functioning Questionnaire (range of possible scores = 0‐24; higher score = poorer outcome) Timing of assessment: 12 months |
The mean social functioning score in the control group was 11.6 points | The mean social functioning score in the intervention group was 1.6 points lower (5.21 lower to 2.01 higher) | ‐ | 39 (1 RCT) | ⊕⊝⊝⊝ Very lowb | ‐ |
| Adverse events | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: Randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence (Schünemann 2013) High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aEvidence downgraded two levels overall. We downgraded one level due to limitations in the design/implementation suggested possible risk of bias ('blinding of participants' bias and possible risk of 'blinding of personnel' bias), and one level for imprecision due to optimal information size criterion not being met. bEvidence downgraded three levels overall. We downgraded one level due to limitations in the design/implementation suggested possible risk of bias ('blinding of participants' bias and possible risk of 'blinding of personnel' bias), one level for imprecision due to optimal information size criterion not being met, and one level for indirectness as the outcome was measured by a questionnaire.
Summary of findings 2. Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone for antisocial personality disorder.
| Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone for antisocial personality disorder | ||||||
| Patient or population: adults with antisocial personality disorder Setting: outpatient Intervention: Impulsive lifestyle counselling + treatment‐as‐usual Comparison: treatment‐as‐usual alone | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with treatment‐as‐usual alone | Risk with impulsive lifestyle counselling + treatment‐as‐usual | |||||
|
Aggression: trait Assessed by: Buss‐Perry Aggression Questionnaire ‐ Short Form (12 items rated on 5‐point Likert scale ranging from extremely uncharacteristic (1) to extremely characteristic (5); range = 12‐60; high score = poor outcome) Timing of assessment: 9 months |
The mean trait aggression score in the control group was 3.52 points | The mean trait aggression score in the intervention group was 0.07 points higher (0.35 lower to 0.49 higher) | ‐ | 118 (1 RCT) | ⊕⊝⊝⊝ Very lowa | ‐ |
| Reconviction | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Global state/functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Social functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
|
Adverse events: death Assessed by: number of participant deaths between a 3‐ and 9‐month follow‐up period Timing of assessment: between 3 and 9 months |
Study population | OR 0.40 (0.04 to 4.54) | 142 (1 RCT) | ⊕⊝⊝⊝ Very lowa | ‐ | |
| 31 per 1000 | 13 per 1000 (19 fewer per 1000; from 30 fewer to 96 more) | |||||
|
Adverse events:incarceration Assessed by: incarceration between a 3‐ and 9‐month follow‐up period Timing of assessment: 9 months |
Study population | OR 0.70 (0.27 to 1.86) | 142 (1 RCT) | ⊕⊝⊝⊝ Very lowa | ‐ | |
| 156 per 1000 | 115 per 1000 (41 fewer per 1000; from 109 fewer to 100 more) | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: Randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence (Schünemann 2013) High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aEvidence downgraded three levels overall. We downgraded two levels for limitations in the design/implementation suggested high risk of bias (‘incomplete outcome data/attrition’ bias; possible risk of ‘allocation concealment’ bias, ‘blinding of participants’ bias, ‘blinding of personnel’ bias, ‘blinding of outcome assessors’ bias, ‘selective reporting’ bias and ‘other’ bias), and one level for imprecision due to optimal information size criterion not being met .
Summary of findings 3. Contingency management + standard maintenance versus standard maintenance alone for antisocial personality disorder.
| Contingency management + standard maintenance versus standard maintenance alone for antisocial personality disorder | ||||||
| Patient or population: adults with antisocial personality disorder Setting: outpatient Intervention: contingency management + standard maintenance Comparison: standard maintenance alone | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with standard maintenance alone | Risk with contingency management + standard maintenance | |||||
| Aggression | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Reconviction | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Global state/functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
|
Social functioning Assessed by: adjusted composite scores on the Family/Social domain of the Addiction Severity Index (composite scores range from no problems (0) to severe problems (1); higher score = worse outcome) Timing of assessment: 6 months |
The mean social functioning score in the control group was 0.16 points | The mean social functioning score in the intervention group was 0.08 points lower (0.14 lower to 0.02 lower) | ‐ | 83 (1 RCT) | ⊕⊕⊝⊝ Lowa | Analysis based on summary data of completers supplied by the trial investigators and derived from a mixed regression model that included time‐specific random effects and an interaction term (see Table 4). |
| Adverse events | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: Randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence (Schünemann 2013) High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aEvidence downgraded two levels overall. We downgraded one level due to possible risk of bias ('blinding of participants' bias, possible risk of 'blinding of personnel' and possible risk of 'incomplete outcome data/attrition' bias), and one level due to likely imprecision due to optimal information size criterion not met.
13. Comparison 3. Contingency management (CM) + standard maintenance (SM) versus SM: Addiction Severity Index scores.
| Study | Outcome | Experimental group: CM + SM | Control group: SM | Difference of least square means over months 1 to 6 | df | P value | Comments | ||
| Adjusted mean | SE | Adjusted mean | SE | ||||||
| Neufeld 2008 | Family/social domain scores | 0.08 | 0.02 | 0.16 | 0.02 | −0.09 | 81 | 0.005 | Favours experimental group: CM + SM |
| Neufeld 2008 | Employment domain scores | 0.72 | 0.04 | 0.72 | 0.04 | 0.006 | 81 | 0.91 | Favours neither group |
| Neufeld 2008 | Alcohol domain scores | 0.02 | 0.01 | 0.04 | 0.01 | −0.02 | 81 | 0.17 | Favours neither group |
| Neufeld 2008 | Drug domain scores | 0.16 | 0.01 | 0.19 | 0.01 | −0.03 | 81 | 0.09 | Favours neither group |
| CM: contingency management; df: degrees of freedom SE: standard error; SM: standard maintenance. | |||||||||
Summary data supplied by the trial investigators. Adjusted means obtained from mixed regression model, which included time‐specific random effects and an interaction term.
Summary of findings 4. 'Driving whilst intoxicated' programme + incarceration versus incarceration alone for antisocial personality disorder.
| 'Driving whilst intoxicated programme' + incarceration versus incarceration alone for antisocial personality disorder | ||||||
| Patient or population: adults with antisocial personality disorder Setting: prison Intervention: 'driving whilst intoxicated' programme + incarceration Comparison: incarceration alone | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with incarceration alone | Risk with 'driving whilst intoxicated' programme + incarceration | |||||
| Aggression | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
|
Reconviction (for drink‐driving) Assessed by: Cox regression of re‐arrest rates over 24 months Timing of assessment: 24 months |
‐ | ‐ | HR 0.56 (−0.19 to 1.31) | 52 (1 RCT) | ⊕⊝⊝⊝ Very lowa | ‐ |
| Global state/functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Social functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Adverse events | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; HR: hazard ratio; RCT: Randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence (Schünemann 2013) High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aEvidence downgraded three levels overall. We downgraded two levels for limitations in the design/implementation suggested possible risk of bias (‘random sequence generation’ bias, ‘allocation concealment’ bias, ‘blinding of participants’ bias, ‘blinding of personnel’ bias, ‘blinding of outcome assessors’ bias, ‘incomplete outcome data/attrition’ bias and ‘other’ bias), and one level for likely imprecision due to optimal information size criterion not being met.
Summary of findings 5. Schema therapy versus treatment‐as‐usual for antisocial personality disorder.
| Schema therapy versus treatment‐as‐usual for antisocial personality disorder | ||||||
| Patient or population: adults with antisocial personality disorder Setting: forensic psychiatric clinic Intervention: schema therapy Comparison: treatment‐as‐usual | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with treatment‐as‐usual | Risk with schema therapy | |||||
| Aggression | ‐ | ‐ | ‐ | ‐ | No data available | |
|
Reconviction Assessed by: number of participants documented to have recidivated (documented as a global negative outcome) Timing of assessment: over the 3 years |
Study population | OR 2.81 (0.11 to 74.56) | 30 (1 RCT) | ⊕⊝⊝⊝ Very lowa | ‐ | |
| 0 per 1000 | 63 per 1000 (0 fewer to 0 more) | |||||
| Global state/functioning | ‐ | ‐ | ‐ | ‐ | No data available | |
|
Social functioning Assessed by: mean number of days until unsupervised leave grantedb Timing of assessment: over the 3 years |
The mean number of days to unsupervised leave in the control group was817.13 days | The mean number of days to unsupervised leave in the intervention group was137.33 fewerdays (271.31 fewer to 3.35 fewer) | ‐ | 30 (1 RCT) | ⊕⊝⊝⊝ Very lowa | ‐ |
|
Adverse events Assessed by: number of participants with a global negative outcome (e.g. dropping out of therapy, recidivism or being transferred to another facility due to poor treatment response) overall Timing of assessment: over the 3 years |
Study population | ‐ | ||||
| 357 per 1000 | 189 per 1000 (168 fewer per 1000; 315 fewer to 192 more) | OR 0.42 (0.08 to 2.19) | 30 (1 RCT) | ⊕⊝⊝⊝ Very lowa | ||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). AsPD: antisocial personality disorder; CI: confidence interval; df: degrees of freedom OR: odds ratio; RCT: Randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence (Schünemann 2013) High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aEvidence was downgraded three levels overall. We downgraded one level due to limitations in the design/implementation suggested high risk of bias (‘selective reporting’ bias; possible risk of ‘blinding of participants’ bias, ‘blinding of personnel’ bias, ‘blinding of outcome assessors’ bias and ‘other’ bias), one level for indirectness (only 87% of the population had a diagnosis of AsPD and subgroup data for AsPD only were not available), and one level for imprecision due to optimal information size criterion not being met. bWe chose to report 'days to unescorted leave' (rather than 'days to escorted leave'), as the measure of social functioning, as this reflects the person gaining a higher level of independence and progress. The results for 'days to escorted leave' (at both two and three years) are reported in the Effects of interventions section.
Summary of findings 6. Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual for antisocial personality disorder.
| Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual for antisocial personality disorder | ||||||
| Patient or population: adults with antisocial personality disorder Setting: outpatient Intervention: social problem‐solving therapy + psychoeducation Comparison: treatment‐as‐usual | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with treatment‐as‐usual | Risk with social problem‐solving therapy + psychoeducation | |||||
| Aggression | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Reconviction | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Global state/functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
|
Social functioning
Assessed by: Social Functioning Questionnaire (8 items rated on 4‐point scale; anchors vary across items; high score = poor outcome) Timing of assessment: 6 months |
The mean social functioning score in the control group was 11.78 points | The mean social functioning score in the intervention group was 1.60 points lower (5.43 lower to 2.23 higher) | ‐ | 17 (1 RCT) | ⊕⊝⊝⊝ Very lowa | ‐ |
| Adverse events | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RCT: Randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence (Schünemann 2013) High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aEvidence downgraded three levels overall. We downgraded one level for limitations in the design/implementation suggested possible risk of bias, one level for indirectness (the outcome was measured by questionnaire), and one level for imprecision due to optimal information size criterion not being met.
Summary of findings 7. Dialectical behaviour therapy versus treatment‐as‐usual for antisocial personality disorder.
| Dialectical behaviour therapy versus treatment‐as‐usual for antisocial personality disorder | ||||||
| Patient or population: adults with antisocial personality disorder Setting: outpatient Intervention: dialectical behaviour therapy Comparison: treatment‐as‐usual | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with treatment‐as‐usual | Risk with dialectical behaviour therapy | |||||
| Aggression | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Reconviction | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Global state/functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Social functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
|
Adverse events (self‐harm) Assessed by: mean number of self‐harm days in past 2 months Timing of assessment: 2 months |
The mean number of self‐harm days for participants in the DBT group was 3.6 (SD = 6.95, range = 0 to 160), compared to 12.22 (SD = 19.58, range = 0 to 57) for participants in the TAU group | ‐ | 14 (1 RCT) | ⊕⊝⊝⊝ Very lowa | Narrative data only (skewed data; see Table 9) | |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DBT: dialectical behaviour therapy; RCT: Randomised controlled trial; SD: standard deviation; TAU: treatment‐as‐usual. | ||||||
| GRADE Working Group grades of evidence (Schünemann 2013) High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aEvidence downgraded three levels overall, due to possible risk of bias (‘blinding of participants’ bias, ‘blinding of personnel’ bias, ‘blinding of outcome assessors’ bias, ‘incomplete outcome data/attrition’ bias and ‘selective reporting’ bias; downgraded one level), and likely imprecision (downgraded two levels) due to optimal information size criterion not being met as well as skewed data.
20. Comparison 7. Dialectical behavior therapy (DBT) versus treatment‐as‐usual (TAU): number of self‐harm days (skewed data).
| Study | Outcome | Experimental group: DBT | Control group: TAU | Statistic | Comments | ||||
| n | Mean | SD | n | Mean | SD | ||||
| Priebe 2012 | Adverse events: number of self‐harm days in past 2 months (averaged), at baseline | 5 | 17.27 | 25.34 | 9 | 10.7 | 6.31 | None reporteda | DBT range = 0.83 to 60.83; TAU range = 1.0 to 18.67 |
| Priebe 2012 | Adverse events: number of self‐harm days in past 2 months (averaged), at 2 months | 5 | 3.6 | 6.95 | 9 | 12.22 | 19.58 | None reporteda | DBT range = 0 to 16; TAU range = 0 to 57 |
| AsPD: antisocial personality disorder; DBT: Dialectical Behavior Therapy; n: numbers of participants; SD: standard deviation; TAU: treatment as usual. | |||||||||
aSummary data for AsPD subgroup (n = 14) provided by K Barnicot on 2 March 2017; no statistics provided.
Summary of findings 8. Psychosocial risk management ('Resettle' programme) versus treatment‐as‐usual for antisocial personality disorder.
| Psychosocial risk management ('Resettle' programme) compared with treatment‐as‐usual (standard probation supervision) for antisocial personality disorder | ||||||
|
Patient or population: adults with antisocial personality disorder Settings: prison and community Intervention: psychosocial risk management (PSRM 'Resettle' programme) Comparison: treatment‐as‐usual (standard probation supervision) | ||||||
| Outcomes | Anticipated absolute effects (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with treatment‐as‐usual alone | Risk with psychosocial risk management 'Resettle' | |||||
| Aggression | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
|
Reconviction: total number of official offences recorded (higher number = worse outcome) Timing of the assessment: 1 year after release from prison |
The mean number of official offences recorded for 16 participants in the PSRM group one year after release from prison was 4.13 (SD = 5.78, range = 0 to 22), compared to 5.21 (SD = 3.28, range = 0 to 11) for 19 participants in the TAU group | ‐ | 35 (1 study) | ⊕⊝⊝⊝ Very lowa | Narrative data only (skewed data), see Table 11 | |
| Global state/functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
| Social functioning | ‐ | ‐ | ‐ | ‐ | ‐ | No data available |
|
Adverse events: death during the study period Timing of assessment: 2 years after release from prison |
29 per 1000 |
26 per 1000 3 fewer per 1000 (28 fewer to 281 more) |
OR 0.89 (0.05 to 14.83) | 35 (1 study) | ⊕⊝⊝⊝ Very lowa | ‐ |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; PSRM: Psychosocial risk management; RCT: Randomised controlled trial; SD: Standard deviation; TAU: Treatment‐as‐usual. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aEvidence downgraded three levels overall due to high risk of bias (‘blinding of personnel’ bias, ‘blinding of outcome assessors’ bias, ‘incomplete outcome data/attrition’ bias, ‘selective reporting’ bias and 'other' bias; downgraded two levels), and likely imprecision (downgraded one level) due to optimal information size criterion not being met as well as skewed data.
23. Comparison 11 Psychosocial Risk Management 'Resettle' programme (PSRM) versus treatment‐as‐usual (probation supervision): recidivism (skewed data).
| Study | Outcome | Experimental group: PSRM | Control group: TAU | Statistic | Commentsa | ||||
| n | Mean | SD | n | Mean | SD | ||||
| Nathan 2019 | Recidivism: total number of official criminal offences recorded in year 1 (higher = worse outcome) | 16 | 4.13 | 5.78 | 19 | 5.21 | 3.28 | None reported | Experimental group median = 2, range = 0 to 22; control group median = 4, range = 0 to 11 |
| Nathan 2019 | Recidivism: total number of official criminal offences recorded in year 2 (higher = worse outcome) | 8 | 3.63 | 4.10 | 8 | 3.25 | 3.77 | None reported | Experimental group median = 2, range = 0 to 11; control group median = 1.5, range = 0 to 9 |
| Nathan 2019 | Recidivism: total number of self‐report antisocial acts as reported by SRD in year 1 (higher = worse outcome) | 16 | 9.69 | 19.34 | 19 | 7.37 | 5.17 | None reported | Experimental group median = 4, range = 0 to 78; control group median = 7, range = 0 to 17 |
| Nathan 2019 | Recidivism: total number of self‐report antisocial acts as reported by SRD in year 2 (non‐cumulative) (higher = worse outcome) | 8 | 8.75 | 14.05 | 9 | 7.33 | 9.51 | None reported | Experimental group median = 2, range = 0 to 38 ; control group median = 4, range = 0 to 27 |
| AsPD: antisocial personality disorder; PSRM: Psychosocial risk management 'resettle' programme n: numbers of participants; SD: standard deviation; SRD: Self‐Report Delinquency scale; TAU: treatment as usual. | |||||||||
aRaw data provided by study authors; all descriptive statistics extracted by review authors for participants with a definite or probable diagnosis of AsPD.
Background
Description of the condition
Antisocial personality disorder (AsPD) is one of the 10 specific personality disorder categories in the current edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM‐5). The DSM‐5 defines personality disorder as "an enduring pattern of inner experience and behaviour that deviates markedly from the expectations of the individual's culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time, and leads to distress or impairment" (p 645). The general criteria for personality disorder according to DSM‐5 are given in Table 12.
1. DSM‐5 general criteria for personality disorder.
| Criteria | Description (DSM‐5, p 646‐7) |
| A. | An enduring pattern of inner experience and behaviour that deviates markedly from the expectations of the individual’s culture. This pattern is manifested in two (or more) of the following areas.
|
| B. | The enduring pattern is inflexible and pervasive across a broad range of personal and social situations. |
| C. | The enduring pattern leads to clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| D. | The pattern is stable and of long duration, and its onset can be traced back at least to adolescence or early adulthood. |
| E. | The enduring pattern is not better explained as a manifestation or consequence of another mental disorder. |
| F. | The enduring pattern is not attributable to the physiological effects of a substance (e.g. a drug of abuse, a medication) or a another medical condition (e.g. head trauma). |
DSM‐5: Diagnostic and Statistical Manual of Mental Disorders‐Fifth Edition
AsPD is described in the DSM‐5 as “a pattern of disregard for, and violation of, the rights of others” (p 645). In order to be diagnosed with AsPD (301.7) according to the DSM‐5, a person must fulfil both the general criteria for personality disorder outlined above and also the specific criteria for AsPD (criteria A, B, C and D, as shown in Table 13). DSM‐5 also states, in reference to the traits of AsPD, that “this pattern has also been referred to as psychopathy, sociopathy or dyssocial personality disorder” (p 659). There continues, however, to be debate about the status of psychopathy compared to AsPD (for example, see Ogloff 2006), how it is measured and the degree to which it is subject to change, which is beyond the scope of this review.
2. DSM‐5 diagnostic criteria for antisocial personality disorder (301.7).
| Criteria | Description (DSM‐5, p 659) |
| A. | A pervasive pattern of disregard for and violation of the rights of others, occurring since age 15 years, as indicated by three (or more) of the following.
|
| B. | The individual is at least 18 years. |
| C. | There is evidence of conduct disorder with onset before age of 15 years. |
| D. | The occurrence of antisocial behavior is not exclusively during the course of schizophrenia or bipolar disorder. |
DSM‐5: Diagnostic and Statistical Manual of Mental Disorders‐Fifth Edition
The focus of this review is AsPD, although this condition is often classified as dissocial personality disorder (F60.2) also, using the International Classification of Diseases ‐ 10 Edition (ICD‐10). AsPD and dissocial personality disorder are often used interchangeably by clinicians and they describe a very similar presentation. While there is considerable overlap between these two diagnostic systems, they differ in two respects. First, the DSM‐5 requires that those meeting the diagnostic criteria also show evidence of conduct disorder with onset before the age of 15 years, whereas there is no such requirement when making the diagnosis of dissocial personality disorder using ICD‐10 criteria. However, a study comparing participants meeting the full criteria for AsPD (which the DSM‐5 has retained) with those who otherwise fulfilled criteria for AsPD but who did not demonstrate evidence of childhood conduct disorder, did not find any clinically important differences (Perdikouri 2007). Second, dissocial personality disorder focuses more on interpersonal deficits (for example, incapacity to experience guilt, a very low tolerance of frustration, proneness to blame others) and less on antisocial behaviour. Table 14 shows the ICD‐10 diagnostic criteria to diagnose dissocial personality disorder (F60.2).
3. ICD‐10 diagnostic criteria for dissocial personality disorder (F60.2).
| Description (ICD‐10) |
Personality disorder, usually coming to attention because of gross disparity between behaviour and the prevailing social norms, and characterised by:
There may also be persistent irritability as an associated feature. Conduct disorder during childhood and adolescents, though not invariably present, may further support the diagnosis. |
ICD‐10: International Classification of Diseases‐Tenth Revision
It is acknowledged that the classification and diagnosis of personality disorder is an area of controversy and complexity with ongoing debate about the usefulness of multiple categories of personality disorder versus a dimensional approach (Tyrer 2015; Skodol 2018), and others who feel the very label of personality disorder to be pejorative and unhelpful (Johnstone 2018, p 221). Indeed, a major paradigm shift in the conceptualisation of personality disorder is being suggested in the latest iteration of the International Classification of Diseases (ICD‐11). The proposed ICD‐11 model takes a dimensional approach and is made up of three components; a general severity rating; five maladaptive personality trait domains; and a borderline pattern qualifier (Oltmanns 2019). The proposed classification changes to personality disorder, however, are outside the scope of this review, which is focussed on interventions for AsPD, as defined in the current, predominant classification systems of DSM‐5 and ICD‐10.
Most studies report the prevalence of AsPD to be between 2% and 3% in the general population (Moran 1999; Coid 2006; NICE 2015). A systematic review and meta‐analysis of the prevalence of personality disorders in the general adult population in Western countries found a prevalence rate for AsPD of 3% (Volkert 2018). Prevalence rates are considerably higher in men compared with women (Dolan 2009; NICE 2015) and a 3:1 ratio of men to women has been described (Compton 2005). It has also been suggested that there are sex differences in how this condition may present, with women with AsPD being less likely than men with AsPD to present with violent antisocial behaviour (Alegria 2013). AsPD (and other personality disorder diagnoses) may be less likely to be diagnosed in non‐white populations (McGilloway 2010).
As would be expected, AsPD is especially common in prison settings. In the UK prison population, the prevalence of people with AsPD has been identified as 63% in male remand prisoners, 49% in male sentenced prisoners and 31% in female prisoners (Singleton 1998). A systematic review of mental disorders in prisoners examined 62 studies from 12 countries and reported the prevalence of AsPD in male prisoners to be 47%, with prisoners approximately 10 times more likely to have AsPD than the general population (Fazel 2002).
The condition is associated with a wide range of disturbance, including greatly increased rates of criminality, substance use, unemployment, homelessness and relationship difficulties (Martens 2000), as well as negative long‐term outcomes. Many adults with AsPD are imprisoned at some point in their life. Although follow‐up studies have demonstrated some improvement over the longer term, particularly in rates of re‐offending (Weissman 1993; Grilo 1998; Martens 2000), men with AsPD who reduce their offending behaviour over time may nonetheless continue to have major problems in their interpersonal relationships (Paris 2003). Black 1996 found that men with AsPD who were younger than 40 years of age had a strikingly high rate of premature death, and obtained a value of 33 for the standardised mortality rate (the age‐adjusted ratio of observed deaths to expected deaths), meaning that they were 33 times more likely to die than males of the same age without this condition. This increased mortality was linked not only to an increased rate of suicide but also to reckless behaviours such as drug misuse and aggression. A 27‐year follow‐up study also found AsPD to be a strong predictor of all‐cause mortality (Krasnova 2019). Black 2015 noted that earlier age of onset has been linked to poorer long‐term outcomes, although marriage, employment, early incarceration and degree of socialisation may act as moderating factors. Follow‐up studies in forensic psychiatric settings suggest a similarly concerning picture. For example, Davies 2007 reported that 20 years after discharge from a medium‐secure unit almost half of the patients were reconvicted, with reconviction rates higher in those with personality disorder compared to those with mental illness (such as schizophrenia and bipolar affective disorder). Similarly, Coid 2015 examined reconviction after discharge from seven medium‐secure units in England and Wales and found that patients with personality disorder were more than two and a half times more likely than those with schizophrenia/schizoaffective disorder to violently offend after discharge.
Significant comorbidity exists between AsPD and many mental health conditions; mood and anxiety disorders are common (Goodwin 2003; Black 2010; Galbraith 2014). The presence of personality disorder co‐occurring with another mental health condition may have a negative impact on the outcome of the latter (Skodol 2005; Newton‐Howes 2006). There is a particularly strong association between AsPD and substance use disorders (Robins 1998). Compared to those without AsPD, those with AsPD are 15 times more likely to meet the criteria for drug dependence and seven times more likely to meet the criteria for alcohol dependence (Trull 2010). Guy 2018 reported that 77% of people with AsPD met the lifetime criteria for alcohol use disorder.
Description of the intervention
Psychological interventions have traditionally been the mainstay of treatment for AsPD, but the evidence upon which this is based is weak (Duggan 2007; Gibbon 2010; NICE 2010). Psychological therapies encompass a wide range of interventions (Bateman 2004a), and those that may be used in AsPD are drawn from all the main areas of psychological treatment. These interventions may be delivered on an individual basis, in a group, or in a mixture of group and individual sessions. By their nature, such interventions tend to be delivered over many weeks and typically last between three months and 12 months. Due to the heterogeneity of possible psychological interventions, it is beyond the scope of this review to summarise them in detail.
Table 15 gives a summary of examples of psychological interventions that may be used for this condition. Those wishing to learn more about the theoretical basis and delivery of specific therapies are directed to the references provided in Table 15.
4. Examples of types of psychological interventions and how they might work.
| Psychological intervention | How the intervention may work |
| Cognitive behaviour therapy (CBT) | CBT‐based treatments place emphasis on encouraging the patient to challenge their core beliefs and thoughts in order to gain insight into how these influence their feelings and behaviour (Bateman 2004a; Henwood 2015). |
| Cognitive analytic therapy (CAT) | CAT utilises ideas from psychodynamic psychotherapy and cognitive therapy (Denman 2001). CAT encourages patients to identify and change learned attitudes and beliefs about themselves and how these impact on their patterns of relating to others. |
| Dialectical behavioural therapy (DBT) | DBT is a complex psychological intervention developed using some of the principles of CBT (Linehan 1993). DBT provides individuals with skills training in four modules (i.e. mindfulness, distress tolerance, emotion regulation, interpersonal effectiveness). |
| Psychoanalytic therapy or dynamic psychotherapy |
The British Psychoanalytic Council defines psychoanalytic therapies as "a range of therapeutic treatments derived from psychoanalytic ideas and methods and a critical appreciation of the effect of childhood experiences on adult personality development" (British Psychoanalytical Council 2018; quote, p 2). (see also Piper 1993, Winston 1994, Bateman 2001 and Leichsenring 2003). |
| Mentalisation‐based therapy (MBT) | MBT has developed from attachment theory and aims to help patients identify and reflect on what they, and others are feeling and why, in order to better regulate their behaviour and emotions (Bateman 2004b). |
| Schema therapy (ST) | In ST, the therapist helps the patient identify long‐standing, self‐defeating patterns of thinking, feeling and behaving (‘schemas’) and develop healthier alternatives to replace them (Young 2003). |
| Nidotherapy | Nidotherapy is a formalised, planned method for achieving environmental change to minimise the effect of the participant’s difficulties upon themselves and others. Unlike most other therapies, it aims to fit the immediate environment to the patient, rather than change the patient to cope in the existing environment (Tyrer 2007). In order to achieve this, a detailed psychological formulation is developed for the individual participant (Tyrer 2005a). |
| Therapeutic community (TC) treatment | TC treatments involve participants engaging in group psychotherapy whilst being involved in a shared, therapeutic environment. This provides them with an opportunity to “explore intrapsychic and interpersonal problems and find more constructive ways of dealing with distress” (Campling 2001, quote, p 365). (see also Lees 1999). |
| Contingency management | Contingency management is based on the psychological principles of behaviour modification and aims to incentivise and reinforce changes in behaviour through the use of financial (or other rewards) that are of value to the patient. (Petry 2011). |
CAT = Cognitive analytic therapy CBT = Cognitive behaviour therapy DBT = Dialectical behavioural therapy MBT = Mentalisation‐based therapy ST = Schema therapy TC = Therapeutic community
It is important to note that this review considers all relevant studies without restriction on the type of psychological therapy, and also considers psychological interventions where drugs are given as an adjunctive intervention.
How the intervention might work
The exact mechanism of action of psychological interventions is unclear and different psychological treatments place different emphasis upon particular putative mechanisms of action. For example, cognitive behaviour therapy (CBT)‐based techniques place emphasis on changing thinking patterns and behaviours, whilst more psychoanalytic‐based approaches place greater emphasis on aiding the person to develop a better understanding of their current self and how this relates to their past experiences, and how unconscious processes and conflict influence interpersonal relationships. Common aspects of psychological therapies are the use of direct (usually verbal) communication between the therapist and the person, to develop a shared understanding of difficulties, and linking this to changes in thinking and behaviour (Muran 2018). These therapies may also involve changing behaviours and the environment as a way to change thinking and encourage more positive actions.
When treating AsPD, it is hoped that psychological interventions will allow the person to develop a better understanding of themselves, others and their difficulties, and that from this they will develop new skills in order to better manage themselves and life difficulties, leading to a decrease in impulsivity, anger, self‐harm, rule‐breaking, substance abuse and negative behaviour.
Those wishing to learn more about the theoretical basis of specific therapies are directed to the additional references provided in Table 15.
Why it is important to do this review
AsPD is an important condition that has a considerable impact on individuals, families and society. Even by the most conservative estimate, AsPD appears to have the same prevalence in men as schizophrenia, the condition that receives the greatest attention from mental health professionals. Furthermore, AsPD is associated with significant costs (Sampson 2013), arising from emotional and physical damage to people, damage to property, use of police time and involvement of the criminal justice system and prison services. Related costs include increased use of healthcare facilities, lost employment opportunities, family disruption, gambling and problems related to alcohol and substance misuse (Myers 1998; Kershaw 1999). In one study, Scott 2001, the lifetime public services costs for a group of adults with a history of conduct disorder (of which 50% will go on to develop adult AsPD) were found to be 10 times those for a similar group without the disorder.
AsPD is closely associated with criminal offending and any intervention that seeks to improve the outcome of AsPD is also likely to impact upon this offending. Aos 1999 reported that for some crimes (especially those involving violence), the cost benefits in favour of intervention are often considerable, as the costs of these types of crimes are often very high.
Despite this, there is currently a dearth of evidence on how best to treat people diagnosed with AsPD, and to date, the few reviews that have been carried out have been inconclusive and hampered by poor methodology. These issues were highlighted in Dolan and Coid’s extensive review of the treatment of psychopathy and AsPD (Dolan 1993). In our previous review of psychological interventions for this condition, Gibbon 2010, we found a lack of high‐quality evidence. The current NICE clinical practice guidelines on the treatment of AsPD rely heavily upon expert opinion and comment that "(a)lthough the evidence base is expanding, there are a number of major gaps..." (NICE 2010, p 9)
It had been hoped that since the last publication of this review, good‐quality studies had been conducted that addressed the methodological issues highlighted in Gibbon 2010, to address this important topic.
Objectives
To evaluate the potential benefits and adverse effects of psychological interventions for people with AsPD.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) in which participants were randomly allocated to an experimental group and a control group, where the control condition was either treatment‐as‐usual (TAU), waiting list or no treatment. We included all relevant RCTs, with or without blinding of the assessors, that were published in any language.
Types of participants
We included studies involving adult (18 years or over) men or women with a diagnosis of AsPD or dissocial personality disorder defined by the DSM (DSM‐IV; DSM‐IV‐TR; DSM‐5) and ICD‐10 diagnostic classification systems. We excluded studies of people with major functional mental illnesses (i.e. schizophrenia, schizoaffective disorder or bipolar disorder), organic brain disease, and intellectual disability. The decision to exclude persons with these conditions is based on the rationale that the presence of such disorders (and the possible confounding effects of any associated management or treatment) might obscure whatever other psychopathology (including personality disorder) might be present. However, we included studies of people diagnosed with AsPD who also had other comorbid personality disorders or other mental health problems. We placed no restrictions on setting and included studies with participants living in the community as well as those incarcerated in prison or detained in hospital settings. We included studies with subsamples of patients with AsPD provided that the data for this group were available separately. We also included studies where participants with a AsPD diagnosis comprised at least 75% of the sample. Lastly, we required studies where participants with antisocial or dissocial personality disorder formed a small subgroup to have randomised at least five people with AsPD.
Types of interventions
We included studies of psychological interventions, both group and individual‐based. This included, but was not limited to, interventions such as:
behaviour therapy;
cognitive analytic therapy (CAT);
cognitive behavioural therapy (CBT);
dialectical behaviour therapy (DBT);
psychodynamic psychotherapy;
transference‐focussed psychotherapy;
group psychotherapy;
mentalisation‐based therapy (MBT);
nidotherapy;
schema therapy;
social problem‐solving therapy;
therapeutic community (TC) treatment; and
contingency management.
We included studies of psychological interventions where medication was given as an adjunctive intervention to all groups but reported separately any studies where the comparison was directly between a psychological and a pharmacological intervention.
We only included studies where an intervention was compared to TAU, waiting list or no treatment. We did not include head‐to‐head trials that compared two or more psychological interventions directly with one another without an adequate control condition.
Types of outcome measures
The primary and secondary outcomes are listed below in terms of single constructs. Given the relatively stable nature of traits of AsPD (by definition), we chose outcomes that could be subject to change and that were potentially measurable by a variety of means (including self‐report and observation). Some traits, such as risk‐taking, are difficult to measure directly. Given the large negative impact of aggression and reconviction, we thought these particularly important; such outcomes could represent a final common pathway encompassing a variety of traits, including failure to confirm to social norms, deceitfulness, impulsivity, recklessness, irresponsibility and lack of remorse. These outcomes are also measurable by self‐report, psychometrics, observed behaviour, informant information and official records. We were also mindful of the issues described in DSM‐5 (p 659): “Because deceit and manipulation are central features of antisocial personality disorder, it may be especially helpful to integrate information acquired from systematic clinical assessments with information collected from collateral sources”. We anticipated that the studies included in this review would have used a range of outcome measures (for example, aggression could have been measured by a self‐report instrument or by an external observer). We provide examples of potential measures of each outcome; however, we also accepted other, similar ways of recording each outcome.
Primary outcomes
Aggression (trait aggression or state/dynamic/current aggression; reduction in aggressive behaviour or aggressive feelings; continuous or dichotomous outcome dependent upon how this was reported), measured through changes in scores on the Aggression Questionnaire (AQ; Buss 1992) for trait aggression, the Modified Overt Aggression Scale (MOAS; Malone 1994) for state aggression, or a similar, validated instrument; or as number of observed incidents.
Reconviction (continuous, dichotomous, or time‐to‐event outcome dependent upon how these data were reported), measured as reconviction in terms of the overall reconviction rate or numbers reconvicted for the sample (continuous), recidivism yes/no (dichotomous), or time to reconviction/reoffending (time‐to‐event data).
Global state/functioning (continuous outcome), measured through improvement on the Global Assessment of Functioning (GAF) numeric scale (DSM‐IV‐TR).
Social functioning (continuous or dichotomous outcome dependent upon how this was reported), measured through improvement in scores on the Social Adjustment Scale‐Self‐Report (SAS‐SR; Weissman 1976), the Social Functioning Questionnaire (SFQ; Tyrer 2005b), a similar, validated instrument, or a proxy measure of social functioning (e.g. decreased level of support required/time taken to achieve leave from hospital).
Adverse events (the incidence of overall adverse events and of the three most common adverse events; dichotomous outcome), measured as numbers reported.
Secondary outcomes
Quality of life (self‐reported improvement in overall quality of life; continuous outcome), measured through improvement in scores on the European Quality of Life (EuroQol) instrument (EuroQoL Group 1990), or a similar, validated instrument.
Engagement with services (health‐seeking engagement with services; continuous outcome), measured though improvement in scores on the Service Engagement Scale (SES; Tait 2002), or a similar, validated instrument.
Satisfaction with treatment (continuous outcome), measured through improvement in scores on the Client Satisfaction Questionnaire‐8 (CSQ‐8; Attkisson 1982), or a similar, validated instrument.
Leaving the study early (dichotomous outcome), measured as proportion of participants discontinuing treatment.
Substance misuse (dichotomous outcome), measured as an improvement on the Substance Use Rating Scale Patient version (SURSp; Duke 1994), or a similar, validated instrument; or biological measurements of substance use (such as urine illicit drug testing). Where possible, we differentiated between drug misuse outcomes and alcohol misuse outcomes.
Employment status (continuous outcome), measured as number of days in employment over the assessment period or similar.
Housing/accommodation status (continuous outcome), measured as number of days living in independent housing/accommodation over the assessment period.
Economic outcomes (any economic outcome such as cost‐effectiveness; continuous outcome), measured using cost‐benefit ratios or incremental cost‐effectiveness ratios (ICERs).
Impulsivity (state or trait impulsivity, self‐reported improvement in impulsivity; continuous outcome), measured through reduction in scores on the Barratt Impulsivity Scale (BIS; Patton 1995), or a similar, validated instrument.
Anger (self‐reported improvement in anger expression and control; continuous outcome), measured through reduction in scores on the State‐Trait Anger Expression Inventory‐2 (STAXI‐II; Spielberger 1999), or a similar, validated instrument.
Mental state (continuous outcome): general mental state, such as ratings of general mental health symptoms, measured by the Brief Psychiatric Rating Scale (BPRS; Overall 1962) or the Symptom Check List‐90 (SCL‐90; Derogatis 1973); or specific symptoms, such as dissociative experiences measured by the Dissociative Experiences Scale (DES; Carlson 1993), mood/anxiety measured by the Hospital Anxiety and Depression Scale (HADS; Zigmond 1983), or the Beck Anxiety and Depression Scale (BADS; Beck 1988); or global mental health, measured by the Clinical Outcomes in Routine Evaluation–Outcome Measure (CORE‐OM; Barkham 2001).
Prison and service outcomes (for example, retention in community or prison programmes or use of resources such as hospital admission; continuous outcome), measured by trial authors.
Other outcomes measured in the included studies that did not fall into one of the above categories (continuous or dichotomous outcomes dependent upon how the outcomes were reported).
Whilst acknowledging that the nature of the disorder can lead to difficulty in long‐term follow‐up of individuals with AsPD, we reported relevant outcomes with no restriction on period of follow‐up. We divided outcomes into immediate (within six months), short‐term (> six months to 24 months), medium term (> 24 months to five years) and long‐term (> five years) follow‐up, where there were sufficient studies to warrant this.
Search methods for identification of studies
The searches for the previous version of this review were designed to find studies for a suite of reviews on a range of personality disorders. For this update, we revised the population section of the strategy by including only the search terms relevant to antisocial personality disorder. We also made changes to the databases we searched (see Differences between protocol and review).
Electronic searches
We ran searches in the following electronic databases and trial registers in September 2016, followed by top‐up searches in October 2017, October 2018 and September 2019.
Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 9) in the Cochrane Library, which includes the Cochrane Developmental, Psychosocial and Learning Problems Specialised Register (searched 5 September 2019).
MEDLINE Ovid (1946 to August Week 5 2019).
MEDLINE In‐Process & Other Non‐Indexed Citations Ovid (searched 5 September 2019).
MEDLINE Epub Ahead of Print Ovid (searched 5 September 2019).
Embase OVID (1974 to 4 September 2019).
CINAHL Plus EBSCOhost (Cumulative Index to Nursing and Allied Health Literature; 1937 to 5 September 2019).
PsycINFO OVID (1967 to September Week 1 2019).
Science Citation Index Web of Science (1970 to 5 September 2019).
Social Sciences Citation Index Web of Science (1970 to 5 September 2019).
Conference Proceedings Citation Index ‐ Science Web of Science (1990 to 5 September 2019).
Conference Proceedings Citation Index ‐ Social Science & Humanities Web of Science (1990 to 5 September 2019).
Sociological Abstracts Proquest (1952 to 5 September 2019).
Criminal Justice Abstracts EBSCOhost (1910 to 5 September 2019).
Cochrane Database of Systematic Reviews (CDSR; 2019, Issue 9), part of the Cochrane Library (searched 5 September 2019).
Database of Abstracts of Reviews of Effects (DARE; 2015, Issue 2. Final Issue), part of the Cochrane Library (searched 5 September 2019).
ClinicalTrials.gov (www.clinicaltrials.gov; searched 5 September 2019).
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP; apps.who.int/trialsearch/AdvSearch.aspx; searched 5 September 2019).
WorldCat (limited to theses; www.worldcat.org; searched 5 September 2019).
Detailed search strategies for each of these sources are provided in Appendix 1. The searches were designed to find records for two separate reviews of interventions for AsPD or dissocial personality disorder; a) psychological interventions and b) pharmacological interventions (Khalifa 2010). For this review, we selected only those studies that were relevant to psychological interventions.
Searching other resources
We searched the reference lists of included and excluded studies for additional trials. We also examined bibliographies of systematic reviews identified in the search to identify relevant studies. We contacted the authors of relevant studies to enquire about other sources of information, and the first author or corresponding author of each included study for information regarding unpublished data.
Data collection and analysis
In the following sections, we report only the methods that we were able to use in this review. We direct the reader to our protocol, Gibbon 2009, and Table 16, for information on additional methods that we intend to use in future updates of this review, should data permit.
5. Additional methods for future updates.
| Issue | Method |
| Types of interventions | We will consider widening the range of interventions examined in future reviews to include concepts such as 'Motivation to Change'. |
| Measures of treatment effect |
Continuous data We will summarise change‐from‐baseline ('change score') data alongside endpoint data where these are available. Change‐from‐baseline data may be preferred to endpoint data if their distribution is less skewed, but both types may be included together in meta‐analysis when using the MD (Higgins 2011a, p 270). Where the data are insufficient for meta‐analysis, we will report the results of the trial investigators' own statistical analyses comparing treatment and control conditions, using change scores. |
| Unit of analysis issues |
Cluster‐randomised trials Where trials use clustered randomisation, study investigators may present their results after appropriately controlling for clustering effects (robust standard errors or hierarchical linear models). If, however, it is unclear whether a cluster‐randomised trial has used appropriate controls for clustering, we will contact the study investigators for further information. If appropriate controls were not used, we will request individual participant data and re‐analyse these using multilevel models that control for clustering. Following this, we will conduct a meta‐analysis of effect sizes and standard errors in RevMan 5 (Review Manager 2014), using the generic inverse method (Higgins 2011a). If appropriate controls were not used and individual participant data are not available, we will seek statistical guidance from the Cochrane Methods Group and external experts as to which method to apply to the published results in attempt to control for clustering. If there is insufficient information to control for clustering, we will enter the outcome data into RevMan5 (Review Manager 2014), using the individual as the unit of analysis, and then conduct a sensitivity analysis to assess the potential biasing effects of inadequately controlled clustered trials (Donner 2001). |
| Dealing with missing data | The standard deviations of the outcome measures should be reported for each group in each trial. If these are not given, we will calculate these, where possible, from standard errors, confidence intervals, t‐values, F values or P values using the method described in the Cochrane Handbook for Systematic Reviews of Interventions, section 7.7.3.3 (Higgins 2011a). If these data are not available, we will impute standard deviations using relevant data (for example, standard deviations or correlation coefficients) from other, similar studies (Follman 1992), but only if, after seeking statistical advice, to do so is deemed practical and appropriate. Assessment will be made of the extent to which the results of the review could be altered by the missing data by, for example, a sensitivity analysis based on consideration of 'best‐case' and 'worst‐case' scenarios (Gamble 2005). Here, the 'best‐case' scenario is where all participants with missing outcomes in the experimental condition had good outcomes, and all those with missing outcomes in the control condition had poor outcomes; the 'worst‐case' scenario is the converse (Higgins 2011a, section 16.2.2). We will report data separately from studies where more than 50% of participants in any group were lost to follow‐up. Where meta‐analysis is undertaken, we will assess the impact of including studies with attrition rates greater than 50% through a sensitivity analysis. If inclusion of data from this group results in a substantive change in the estimate of effect of the primary outcomes, we will not add the data from these studies to trials with less attrition and will present them separately. Any imputation of data will be informed, where possible, by the reasons for attrition where these are available. We will interpret the results of any analysis based in part on imputed data with recognition that the effects of that imputation (and the assumptions on which it is based) can have considerable influence when samples are small. |
| Assessment of reporting biases | We will draw funnel plots (effect size versus standard error) to assess small study effects, when there are greater than 10 studies. Asymmetry of the plots may indicate publication bias, although they may also represent a true relationship between trial size and effect size. If such a relationship is identified, we will further examine the clinical diversity of the studies as a possible explanation (Egger 1997; Jakobsen 2014; Lieb 2016). |
| Data synthesis | For homogeneous interventions, we will group outcome measures by length of follow‐up, and use the weighted average of the results of all the available studies to provide an estimate of the effect of specific psychological interventions for people with antisocial personality disorder. We will use regression techniques to investigate the effects of differences in study characteristics on the estimate of the treatment effects. We will seek statistical advice before attempting meta‐regression. If meta‐regression is performed, it will be executed using a random‐effects model as per protocol. Where studies provide both endpoint or change data, or both, for continuous outcomes, we will perform meta‐analysis that combines both data types using the methods described by Da Costa 2013. We will consider pooling outcomes reported at different time points where this does not obscure the clinical significance of the outcome being assessed. To address the issue of multiplicity, future reviews should consider the following:
|
| Subgroup analysis and investigation of heterogeneity | We will undertake subgroup analysis to examine the effect on primary outcomes of:
|
| Sensitivity analysis | We will undertake sensitivity analyses to investigate the robustness of the overall findings in relation to certain study characteristics. A priori sensitivity analyses are planned for:
|
MD= Mean difference
Selection of studies
Working independently, two review authors read the titles and abstracts generated by the searches and discarded those that were clearly irrelevant. They next obtained the full‐text reports of those deemed potentially relevant or for which more information was need to determine relevance, and assessed them against the inclusion criteria (Criteria for considering studies for this review). The reviewers resolved uncertainties concerning the appropriateness of studies for inclusion in the review through consultation with a third review author who had not been involved in the initial screening. We recorded the selection process in a PRISMA diagram (Moher 2009).
For studies reported in a language other than English, we initially examined the English version of the title and abstract, before obtaining a translation of the full paper in order to reach a decision on its eligibility.
Data extraction and management
Four review authors extracted data independently for all studies using a data extraction form (which had previously been piloted) (see Appendix 2). Where data were not available in the published trial reports, we contacted the study authors and asked them to supply the missing information. Two review authors entered the data into Review Manager 5 (Review Manager 2014), which one review author checked for accuracy. Disagreements were resolved by consultation with a third review author; less than 5% of papers required such discussion.
Assessment of risk of bias in included studies
For each included study, two review authors independently completed Cochrane’s tool for assessing risk of bias (Higgins 2011b), resolving any disagreements through consultation with a third review author (from the same subgroup). We assessed the papers against the following domains:
random sequence generation (selection bias);
allocation concealment (selection bias);
blinding of participants and personnel to intervention received (performance bias);
blinding of outcome assessment (detection bias);
incomplete outcome data (attrition bias);
selective outcome reporting (reporting bias); and
other sources of bias, including allegiance bias and treatment adherence.
For each domain, we allocated ratings of ‘high’, ‘low’ or ‘unclear’ risk of bias, where we considered the risk of bias to be high, low or uncertain or unknown, respectively.
Overall risk of bias
We assessed the overall risk of bias within studies using the method recommended by Higgins 2011b. We assessed a study at low risk of bias overall if we rated it at low risk of bias on all key domains; at unclear risk of bias overall where we assessed the study at unclear risk of bias on one or more key domains; and at high risk of bias overall where we rated the study at high risk of bias on one or more key domains. If a single domain was rated a high risk but other domains were unclear, we rated the study at high risk of bias overall. We used the results of this assessment to inform our GRADE ratings (see section on 'Summary of findings' below).
Measures of treatment effect
Dichotomous data
For dichotomous (binary) data, we used the odds ratio (OR) presented with 95% confidence intervals (CI), to summarise results within each study. We chose the OR because it has statistical advantages relating to its sampling distribution and its suitability for modelling, and because it is a relative measure and so can be used to combine studies.
Continuous data
For continuous data, such as the measurement of impulsiveness on a scale, we compared the mean score for each outcome, as determined by a standardised tool between the two groups, to give a mean difference (MD) and presented this with 95% CI. We used the mean difference (MD) where the same outcome measure was reported in more than one study, and the standardised mean difference (SMD) if studies used different outcome measures of the same construct.
We reported continuous data that were skewed in a separate table, and did not calculate treatment effect sizes, to minimise the risk of applying parametric statistics to data that departed significantly from a normal distribution. However, if the trial investigators provided results of their own statistical analysis on such data (e.g. hazard ratios), we reported their results descriptively within the section on Effects of interventions. We defined skewness as occurring when, for a scale or measure with positive values and a minimum value of zero, the mean was less than twice the standard deviation (SD) (Altman 1996).
Time‐to‐event data
For time‐to‐event data, we used the hazard ratio (HR) with 95% CI. Reconviction (dichotomous or time‐to‐event outcome dependent upon how this was reported), was measured as the overall reconviction rate for the sample or as an analysis of time to reconviction (please see Differences between protocol and review).
Other
Where possible, we made these comparisons at specific follow‐up periods: immediate (within six months), short‐term (> six months to 24 months), medium term (> 24 months to five years) and long‐term (> five years) follow‐up. Where possible, we presented endpoint data.
Unit of analysis issues
We did not identify any cluster‐randomised trials or multi‐arm trials or issues with multiplicity. For information on how we will handle these issues should they arise in future updates of this review, please see our protocol, Gibbon 2009, and Table 16.
Dealing with missing data
We attempted to contact the original investigators to request any missing data and information on whether or not the data could be assumed to be ‘missing at random’. If these data were made available to us, we included the data in the review. If data were not forthcoming, we attempted to contact at least one of the co‐investigators. We permitted a reasonable length of time (at least 12 weeks) for the investigator(s) to supply the missing data before we proceeded with the analysis.
For dichotomous data, we reported missing data and dropouts for each included study, and the number of participants who were included in the final analysis as a proportion of all participants in each study. We provided reasons for the missing data in the narrative summary, where these were available.
For missing continuous data, we provided a qualitative summary. We reported missing data information in the 'incomplete outcome data' section of the 'Risk of Bias' tables.
Assessment of heterogeneity
We assessed the clinical homogeneity of studies with regard to the type of therapeutic intervention reported, the setting, and the population from which AsPD participants were drawn. We assessed the methodological heterogeneity of studies with regard to the study design. We assessed the extent of between‐trial differences and the consistency of results of any meta‐analysis in three ways: first, by visual inspection of the forest plots; second, by performing the Chi2 test of heterogeneity (where a significance level less than 0.10 was interpreted as evidence of heterogeneity); and finally by examining the I2 statistic (Higgins 2011a, section 9.5.2). The I2 statistic describes approximately the proportion of variation in point estimates due to heterogeneity rather than sampling error. We considered I2 values less than 30% as indicating low heterogeneity, values in the range 30% to 70% as indicating moderate heterogeneity, and values greater than 70% as indicating high heterogeneity. We attempted to identify any significant determinants of heterogeneity categorised as moderate or high.
Assessment of reporting biases
Due to insufficient data, we were unable to conduct our preplanned funnel plots (see Gibbon 2009; Table 16), to assess reporting biases.
Data synthesis
We combined comparable outcome measures across studies of clinically homogeneous interventions (where the interventions and populations did not differ substantially) in a meta‐analysis using a fixed‐effect model. For single studies, or where studies were too clinically diverse to be combined, we provided a narrative description of the results. Although we considered multiplicity (the concern that performing multiple comparisons increases the risk of falsely rejecting the null hypothesis), this was not an issue in this review, as the available data did not allow the making of multiple comparisons. We have outlined how we will address multiplicity in future reviews in Table 16.
Subgroup analysis and investigation of heterogeneity
Due to insufficient data we were unable to conduct any of our preplanned subgroup analyses (see Gibbon 2009; Table 16).
Sensitivity analysis
Due to insufficient data we were unable to conduct any of our preplanned sensitivity analyses (see Gibbon 2009; Table 16).
Summary of findings and assessment of the certainty of the evidence
Following the guidelines set out in Schünemann 2013, we used GRADEpro GDT software (GRADEpro) to prepare 'Summary of findings' tables for the following comparisons.
Cognitive behaviour therapy + treatment‐as‐usual versus treatment‐as‐usual alone
Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone
Contingency management + standard maintenance versus standard maintenance alone
'Driving whilst intoxicated' programme + incarceration versus treatment‐as‐usual alone
Schema therapy versus treatment‐as‐usual
Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual
Dialectical behaviour therapy versus treatment‐as‐usual
We presented all primary outcomes (aggression, reconviction, global/state functioning, social functioning and adverse events), assessed at any time point, in the 'Summary of findings' tables, presenting pooled data where possible.
Two review authors independently assessed the overall certainty of the evidence for all primary outcomes using the GRADE approach (Schünemann 2013), which considers the risk of bias in the study, level of inconsistency, indirectness, imprecision and publication bias. We rated the certainty of the evidence for each outcome as being high, moderate, low or very low certainty, and where relevant, provided reasons for downgrading the certainty of the evidence in the footnotes. We resolved any disagreements by discussion, or in consultation with a third review author.
Results
Description of studies
Results of the search
For the original version of this review (Gibbon 2010), we searched for studies from the inception of each database to September 2009. These searches identified in excess of 16,398 records, of which 48 appeared to merit closer inspection. From these, we identified 11 studies (from 17 reports) that met the inclusion criteria.
We ran the searches for this update from September 2009 to September 2019. and found a total of 35,562 records. Once duplicate records were removed, we were left with 24,801 unique records which we screened by title and abstract. We excluded 24,561 irrelevant records, and retrieved the full text of the remaining 240 records for closer inspection. From these, we identified two additional reports of previously included studies and eight new studies (from 18 reports) that fully met the inclusion criteria. We calculated the inter‐rater agreement for the selection of studies by the reviewer, which was kappa = 0.72; the strength of this agreement is classified as good by Altman 1996 (< 0.20 = poor, 0.21 to 0.40 = fair, 0.41 to 0.60 = moderate, 0.61 to 0.80 = good, 0.81 to 1.00 = very good).
In total, this review now has 19 included studies (from 37 reports) and 89 excluded studies (from 117 reports). We also identified seven studies which are awaiting classification, and six ongoing studies. The flow of studies for this updated review is shown in Figure 1, as recommended by Stovold 2014.
1.
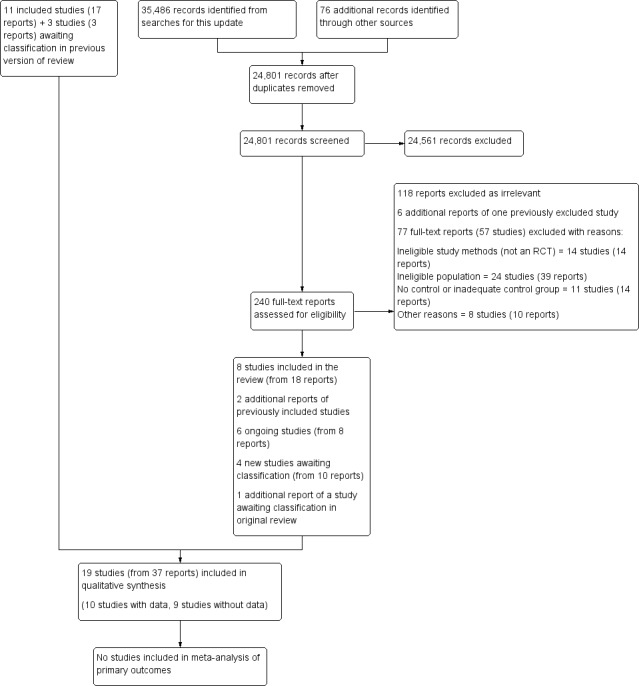
Study flow diagram showing the results of an updated literature search (5 September 2019).
Included studies
In the original version of this review (Gibbon 2010), we performed electronic searches over two consecutive time periods to minimise the difficulty in managing large numbers of citations. Searches to December 2006 produced in excess of 10,000 records. Searches from December 2006 to September 2009 produced 6398 records. These original searches identified 48 records where all or part of the sample appeared to meet diagnostic criteria for antisocial or dissocial personality disorders, and resulted in 11 studies being included in the review. The searches in 2019 identified eight additional included studies. Further details are provided in the 'Characteristics of included studies' tables.
Design
Seventeen of the 19 included studies were parallel trials with allocation by individual participant. The two remaining studies were cluster‐RCTs: Havens 2007 was a cluster‐RCT where the unit of allocation was treatment site; Feigenbaum 2012 was a cluster‐RCT where allocation was balanced for geographic, gender and diagnostic criteria (i.e. presence of borderline personality disorder). The 17 parallel trials included two three‐armed trials (Woody 1985; Asmand 2015) and one four‐armed trial (Messina 2003).
Sample sizes
There was some variation in sample size between studies. Overall, 848 participants with antisocial or dissocial personality disorder were randomised in the 17 trials where this allocation was reported unambiguously, with the size of sample ranging from 11 (Feigenbaum 2012) to 176 (Thylstrup 2015) participants (mean = 49.8, SD = 38.1). Data were available for eight trials where 100% of the sample/subsample of participants had AsPD (Woody 1985; Messina 2003; Huband 2007; Woodall 2007; Neufeld 2008; Davidson 2009; Asmand 2015; Thylstrup 2015); in these eight studies, 514 participants with antisocial or dissocial personality disorder were randomised, and the sample size ranged from 14 (Priebe 2012) to 176 (Thylstrup 2015) participants (mean = 64.3, SD = 48.4). We included, and reported separately, data from one study with an 87% subsample of participants with AsPD (AsPD n = 26) (Bernstein 2012), and data from one study with a 90% subsample of participants with AsPD (AsPD n = 65) (Nathan 2019). The number of participants completing was reported unambiguously in 11 studies (Messina 2003; Havens 2007; Woodall 2007; Neufeld 2008; Davidson 2009; Tarrier 2010; Bernstein 2012; Feigenbaum 2012; Priebe 2012; Asmand 2015; Nathan 2019), in which the proportion ranged from 55.5% (Tarrier 2010) to 100% (Woodall 2007; Asmand 2015) (mean = 83.1%).
Only four of the 19 studies focussed exclusively on participants with a diagnosis of AsPD (Neufeld 2008; Davidson 2009; Asmand 2015; Thylstrup 2015). For the remaining 15 studies, participants with antisocial or dissocial personality formed a subgroup. The size of this antisocial subgroup ranged from 11 to 65 participants, representing 3.1% to 90.3% respectively of the total sample (mean = 37.8%). Data on the entire antisocial subgroup were available to us for only four of these 15 studies (Messina 2003; Huband 2007; Woodall 2007; Priebe 2012). In line with our plan to include data where the subgroup of a sample with AsPD comprised over 75% of the total sample but where the data were not presented by subgroup, we also examined the data from Bernstein 2012 and Nathan 2019, where the AsPD subgroups consisted of 87% and 90.3% of the total sample respectively.
Setting
Eight studies were carried out in the UK (Tyrer 2004; Huband 2007; Davidson 2009; Tarrier 2010; Feigenbaum 2012; Priebe 2012; McMurran 2016; Nathan 2019), eight took place in North America (Woody 1985; McKay 2000; Messina 2003; Ball 2005; Havens 2007; Marlowe 2007; Woodall 2007; Neufeld 2008), with a single study each from Denmark (Thylstrup 2015), Iran (Asmand 2015) and the Netherlands (Bernstein 2012). Nine were multicentre trials: Messina 2003 and Davidson 2009 with two sites; Tyrer 2004 and Huband 2007 with five sites; Bernstein 2012 with seven sites; Havens 2007 with 10 sites; Thylstrup 2015 with 13 sites; Nathan 2019 with 21 sites; and McMurran 2016 with an unspecified number of sites. Two studies took place in a hospital inpatient setting (Tarrier 2010; Bernstein 2012). Thirteen studies took place in an outpatient or community setting, and three studies took place in a prison or custodial environment (Marlowe 2007; Woodall 2007; Asmand 2015). Two studies took place in a community or custodial environment, or both (Thylstrup 2015; Nathan 2019).
Participants
Seven studies restricted participants to males (Woody 1985; McKay 2000; Davidson 2009; Tarrier 2010; Bernstein 2012; Asmand 2015; Nathan 2019). The remaining 12 studies had a mix of male and female participants, with all but four of these studies randomising more men than women (Tyrer 2004; Feigenbaum 2012; Priebe 2012; McMurran 2016). The overall mix was 75% men compared to 25% women. All 19 studies involved adult participants, with the mean age per study ranging between 25.1 and 43.5 years (mean = 35.5 years, SD = 5.2).
Nine studies focussed on participants with substance misuse difficulties. For these, inclusion criteria included: opioid substance dependence disorder (Woody 1985; Neufeld 2008); cocaine dependence disorder (McKay 2000; Messina 2003); recent alcohol or drug use whilst homeless (Ball 2005); being an intravenous drug user (Havens 2007); being sentenced for a drug‐related offence (Marlowe 2007); being sentenced for driving whilst intoxicated (Woodall 2007); and receiving outpatient treatment for substance (drug or alcohol) use disorder (Thylstrup 2015). The remaining 10 studies did not recruit participants on the basis of substance misuse. For these studies, the focus was on recurrent self‐harm (Tyrer 2004), violence (Davidson 2009), meeting DSM‐IV criteria for any personality disorder (Huband 2007; Tarrier 2010; Feigenbaum 2012; Priebe 2012; McMurran 2016), meeting DSM‐IV criteria for AsPD (Asmand 2015), meeting criteria for any cluster B personality disorder (Bernstein 2012), or high‐risk personality disordered offenders (Nathan 2019).
The precise definition of AsPD and the method by which it was assessed varied between the studies. Eighteen studies included participants with AsPD (under DSM criteria).
Fourteen studies used DSM‐IV criteria. Six of these studies made assessments using the Structured Clinical Interview for DSM‐IV Axis II Personality Disorders (SCID‐II) (Messina 2003; Havens 2007; Davidson 2009; Tarrier 2010; Feigenbaum 2012; Priebe 2012). For the remaining eight studies, one used an antisocial PD interview developed by the investigators from the SCID‐II (Marlowe 2007); one study used the Personality Disorder Questionnaire (Ball 2005); three studies used the International Personality Disorder Examination (Huband 2007; McMurran 2016; Nathan 2019); one study used the Structured Interview for DSM‐IV Personality Disorders (Bernstein 2012); one study used the Millon Clinical Multiaxial Inventory (Asmand 2015); and one study used the Mini International Neuropsychiatric Interview (Thylstrup 2015).
Three studies used DSM‐III‐R criteria and made assessments using the SCID‐II (McKay 2000; Neufeld 2008), or the Diagnostic Interview Schedule (Woodall 2007).
One earlier study used DSM‐III criteria and made assessments using the Schedule for Affective Disorders & Schizophrenia and the Maudsley Personality Inventory (Woody 1985).
One study used ICD‐10 criteria and made assessments using the PAS‐Q Quick Personality Assessment Schedule (Tyrer 2004).
Five studies did not report the ethnicity of participants (Tyrer 2004; Huband 2007; Bernstein 2012; Feigenbaum 2012; Thylstrup 2015). Where ethnicity was reported, the proportion of the sample described by the investigators as either 'white' or 'Caucasian' ranged from 7% (McKay 2000) to 94.5% (Nathan 2019). The total proportion of white participants randomised (expressed as a percentage of the total number randomised) was 53.5% for those studies where this information was available (Woody 1985; McKay 2000; Messina 2003; Ball 2005; Marlowe 2007; Woodall 2007; Neufeld 2008; Davidson 2009; Tarrier 2010; Priebe 2012; McMurran 2016; Nathan 2019).
Interventions
The following types of interventions were represented: case‐management (Havens 2007); cognitive behaviour therapy (Tyrer 2004; Davidson 2009); cognitive behaviour therapy + standard maintenance (Messina 2003); cognitive behaviour therapy + contingency management + standard maintenance (Messina 2003); contingency management (Messina 2003; Neufeld 2008); dialectical behaviour therapy (Feigenbaum 2012; Priebe 2012; Asmand 2015); 'driving whilst intoxicated' programme (Woodall 2007); dual focus schema therapy (Ball 2005); impulsive lifestyle counselling (Thylstrup 2015); optimal judicial supervision (Marlowe 2007); psychoeducation and social problem‐solving therapy (Huband 2007); psychoeducation + social problem‐solving therapy + treatment‐as‐usual (TAU) (McMurran 2016); psychosocial risk management (Nathan 2019); rational emotive behaviour therapy (Asmand 2015); relapse prevention (McKay 2000); schema modal therapy (Tarrier 2010); schema therapy (Bernstein 2012); and supportive expressive psychotherapy (Woody 1985). Interventions that were group‐based may have included elements of group psychotherapy, depending on how group psychotherapy was defined. None of the 19 included studies evaluated therapeutic community treatment, cognitive analytic therapy, mentalisation‐based therapy or nidotherapy.
The duration of the interventions ranged between four (Ball 2005) and 156 weeks (Tarrier 2010; Bernstein 2012) (mean = 55.8 weeks, median = 26 weeks). Thirteen studies followed up participants beyond the end of the intervention period by, on average, 52 weeks (range = 4 to 104 weeks) (McKay 2000; Messina 2003; Tyrer 2004; Ball 2005; Havens 2007; Marlowe 2007; Woodall 2007; Tarrier 2010; Feigenbaum 2012; Priebe 2012; Thylstrup 2015; McMurran 2016; Nathan 2019). One study, Bernstein 2012, had not yet completed the follow‐up stage of the study at the time of this review.
Full details of the psychological interventions are provided in the 'Characteristics of included studies' tables and summarised in Table 17.
6. Details of the psychological interventions examined in the 19 included studies.
| Study | Intervention | Description |
| Woody 1985 | Supportive‐expressive psychotherapy + standard maintenance | Supportive‐expressive psychotherapy is an analytically‐oriented, focal psychotherapy. Standard maintenance is an individual counselling intervention focused on providing external services rather than dealing with intrapsychic processes, plus methadone maintenance. |
| McKay 2000 | Individualised relapse prevention aftercare | Individualised relapse prevention is a manualised, modular intervention for substance users in the maintenance phase of recovery. Risky situations are identified and improved coping responses encouraged. Clients receive 1 individual relapse prevention session and 1 group session per week for up to 20 weeks. |
| Messina 2003 | Cognitive behaviour therapy (CBT) + standard maintenance | CBT is a structured intervention based on behavioural principles with positive verbal reinforcement of decreased or no use of illicit drugs, or for prosocial behaviour. Comprises 48 group sessions of 90 minutes (3 per week for 16 weeks) with typically 4 to 8 participants in each group. Participants continue on standard maintenance treatment (including methadone, mean = 72 mg/day). |
| Contingency management + standard maintenance | Contingency management + standard maintenance comprises a brief meeting (2 to 5 minutes) with a contingency management technician. Clean urine specimens are rewarded with vouchers of escalating value (to a maximum of USD 1277.50 if drug‐free for the 16 weeks of the trial) and with praise/encouragement. Positive samples result in the vouchers being withheld but the participant is not rebuked or punished. Participants continue on standard maintenance treatment (including methadone, mean = 62 mg/day). | |
| Cognitive behavioural therapy (CBT) + contingency management + standard maintenance | CBT + contingency management + standard maintenance is a structured intervention based on behavioural principles with positive verbal reinforcement of decreased or no use of illicit drugs, or for prosocial behaviour. Comprises 48 group sessions of 90 minutes (3 per week for 16 weeks) with typically 4 to 8 participants in each group. Participants continue on standard maintenance treatment (including methadone, mean = 68 mg/day) and meet with a contingency management technician (2 to 5 minutes). Clean urine specimens are rewarded with vouchers of escalating value (to a maximum of USD 1277.50 if drug‐free for the 16 weeks of the trial) and with praise or encouragement. Positive samples result in the vouchers being withheld but the participant is not rebuked or punished. | |
| Tyrer 2004 | Cognitive behavioural therapy (CBT) + treatment as usual | Manual‐assisted CBT (MACT) is a treatment for self‐harming behaviour where participants are provided with a booklet based on CBT principles plus an offer of 5 plus 2 booster sessions of CBT in the first 3 months. |
| Ball 2005 | Dual‐focus schema therapy | Dual focus schema therapy is a 24‐week, manual‐guided individual therapy that integrates symptom‐focused relapse prevention coping skills techniques with schema‐focused techniques for early maladaptive schemas and coping styles. |
| Neufeld 2008 | Contingency management + standard maintenance | Contingency‐based behavioural programme is a highly structured contingency‐based, adaptive treatment protocol comprising counselling sessions and behavioural interventions. Drug abstinence and counselling attendance are rewarded by greater control over methadone management with negative reinforcers being a reduction in methadone dosage and control of the dosage. Standard maintenance comprises standard methadone substitution treatment with 2 individual counselling sessions per week with bi‐weekly reviews; negative drug screens are rewarded with methadone take‐home doses. |
| Havens 2007 | Strengths‐based case management | Strengths‐based case management of 5 to 24 minutes duration; includes engagement, strengths assessment, personal case planning, and resource acquisition. Services provided by case managers include advice on referrals to health and social services, and on transportation and employment. |
| Huband 2007 | Social problem‐solving therapy with psychoeducation | A brief, individual psychoeducation programme followed by 16 weekly, group‐based problem‐solving sessions (lasting approximately 2 hours) based on the 'Stop and Think!' method. Groups start with no more than 8 participants in each and are single gender. |
| Marlowe 2007 | Optimal judicial supervision | Optimal (‘matched’) schedule of court hearings in which frequency of court attendance is matched with risk, so that high‐risk offenders (those with antisocial personality disorder and a history of drug treatment) attend with greater frequency. Group sessions are psychoeducational and cover a range of topics including relapse prevention strategies. |
| Woodall 2007 | 'Driving whilst intoxicated program' + incarceration | The ‘Driving whilst intoxicated program' is nonconfrontational and utilises a psychoeducational approach on the harmful effects of alcohol, stress management, and a work‐release programme for those in employment. It also incorporates culturally appropriate elements (71% of participants were native American). The programme was delivered whilst participants were subject to 28 days incarceration. |
| Davidson 2009 | Cognitive behavioural therapy (CBT) + treatment as usual | CBT involves a cognitive formulation of the individual’s problems (to promote engagement) and therapy focusing on beliefs about self and others that impair social functioning. Individuals were offered 15 or 30 sessions of CBT (to determine the optimal ‘dose’) and therapist adherence/competence was assessed for a random selection (30%) of sessions by audio recording and found to be “within the 'competent range'” (quote, p 517) |
| Bernstein 2012 | Schema therapy (ST) | ST is an integrative therapy for personality disorders combining cognitive, behavioural, psychodynamic object relations, and humanistic/experiential approaches; individual therapy delivered twice a week according to adapted procedures for forensic patients set out in a practitioner’s guide; treatment lasts from 2 to 3 years, with frequency reduced to 1 session per week in the third year of treatment. |
| Feigenbaum 2012 | Dialectical behavioural therapy (DBT) | DBT pretreatment phase of 3‐6 weeks of goal‐setting and commitment‐building followed by offer of 1 year DBT treatment contract; DBT treatment consists of 1 hour of individual therapy and 2.5 hours of group skills training per week plus out‐of‐hours telephone consultation, as required. |
| Priebe 2012 | Dialectical behavioural therapy (DBT) | 12 months of DBT delivered according to Linehan’s treatment and skills training manuals (Linehan 1993); 1 × 1‐hour individual therapy session per week; 1 × 2‐hour skills training group per week; out‐of‐hours skills coaching by telephone, as required. |
| Asmand 2015) | Dialectical behavioural therapy (DBT) | DBT condition and mode of delivery was very poorly described by the study authors; possibly delivered through 16 × 1‐hour sessions. |
| Rational emotional behaviour Therapy (REBT) | REBT, based on cognitive behaviour therapy principles, was very poorly described by the study authors; possibly delivered through 16 × 1‐hour sessions. | |
| McMurran 2016 | Psychoeducation with problem‐solving (PEPS) + treatment as usual | PEPS therapy is a cognitive–behavioural intervention that integrates individual and group therapies with optional individual support sessions; up to four individual psychoeducation sessions; 12 × 2‐hour group sessions of problem‐solving therapy; individual support sessions offered every 2 weeks through the 12‐week problem‐solving group (optional). Patients also received treatment as usual. |
| Tarrier 2010 | Schema modal therapy (SMT) + treatment as usual | SMT followed Young’s SMT protocol (Young 2003); 1 60‐minute individual session each week for a minimum of 18 months. Participants also received treatment as usual. |
| Thylstrup 2015 | Impulsive lifestyle counselling (ILC) + treatment as usual | ILC is a manualised, psychoeducational intervention; 6 sessions cover specific topics and include mandatory questions, printed handouts and worksheets for the patient. |
| Nathan 2019 | Psychosocial risk management (PSRM) | 'Resettle' PSRM is a non‐manualised, integrative sociotherapy underpinned by case formulation, risk management, probation supervision and intervention planning. The programme consists of 3 levels: 1) therapeutic milieu generated by appropriate and prosocial relationships; 2) group work to enhance participants' capacity for self‐reflection and understanding of others; and 3) individual psychosocial interventions focused on risk management, well‐being and social integration. PSRM treatment consists of a 6‐month preparatory phase (before individual is released from prison), followed by community‐based treatment (time frame = 1‐2 years). |
CBT = Cognitive behaviour therapy DBT = Dialectical behavioural therapy ILC = Impulsive lifestyle counselling MACT = Manual‐assisted CBT PEPS = Psychoeducationwith problem‐solving PSRM = Psychosocial risk management REBT = Rational emotional behaviour therapy SMT = Schema modal therapy ST = Schema therapy
Control conditions
The 19 included studies compared the 18 psychological interventions to a relevant control condition (i.e. TAU, waiting list or no treatment), as required by the inclusion criteria for this review (see Types of studies). Full details are provided in the 'Characteristics of included studies' tables and summarised in Table 18. It is important to note that participants allocated to the experimental condition in these studies commonly received some degree of TAU in addition to the intervention under evaluation. We considered that all 19 studies had a control condition that could be described as TAU. This decision was straightforward for 13 of the 19 studies, as follows. For seven studies, it was clear that TAU simply comprised whatever treatment the participants would have received had the trial not taken place (Tyrer 2004; Davidson 2009; Tarrier 2010; Bernstein 2012; Feigenbaum 2012; Priebe 2012; McMurran 2016). For one study, Huband 2007, TAU was the treatment they had whilst on the waiting list for the intervention. In the five remaining studies, TAU was passive referral in Havens 2007, standard (‘unmatched’) scheduled court hearings in Marlowe 2007, incarceration in Woodall 2007 and Asmand 2015, and standard probation supervision following release from prison custody in Nathan 2019.
7. Details of the comparator interventions examined in the 19 included studies.
| Study | Comparator |
| Woody 1985 | SM: an individual counselling intervention focused on providing external services rather than dealing with intrapsychic processes, plus methadone maintenance |
| McKay 2000 | TAU: standard continuing care comprising 2 group therapy sessions per week where the orientation was a mix of addictions counselling and 12‐step recovery practices |
| Messina 2003 | SM: methadone maintenance; treatment, with daily clinic visits for methadone, twice‐monthly counselling sessions, plus medical care and case management visits, as required |
| Tyrer 2004 | TAU: participants were seen by another designated therapist and offered the standard treatment in the area concerned or the continuation of current therapy. |
| Ball 2005 | TAU: standard group substance abuse counselling as normally provided at the drop‐in centre where clients are typically offered a total of 3 opportunities per week to attend group psychoeducation and counselling sessions |
| Havens 2007 | Passive referral: strengths‐based case management (SBCM) of 0 to 4 minutes duration |
| Huband 2007 | TAU: placed on waiting list for active intervention |
| Marlowe 2007 | Standard (‘unmatched’) schedule court hearings requiring attendance every 4 to 6 weeks |
| Neufeld 2008 | SM: standard methadone substitution treatment and participants attended 2 individual counselling sessions per week |
| Woodall 2007 | Incarceration |
| Davidson 2009 | TAU: “all participants received whatever treatment they would have received had the trial not taken place” (quote; p 570, column 2) |
| Tarrier 2010 | TAU: “Group‐based enhanced thinking skills and sex offender treatment were the most frequently provided therapies recorded on the TAU logs." (quote; p 14); other noted TAU therapies included: social therapy and resettlement work; review of clinical or psychology reports; discussion of therapy; neurorehabilitation; review of previous assessments; end of therapy meeting support work; and "talking sessions” (quote; p 14) |
| Bernstein 2012 | TAU: standard treatment that patients receive at each clinic usually another (non‐ST) form of individual psychotherapy such as cognitive‐behaviour therapy, psychodynamic therapy, or client‐centred therapy |
| Feigenbaum 2012 | TAU: range of individualised service provision, including outpatient psychiatric review, case management, psychoanalytic psychotherapy, cognitive behaviour therapy, supportive structured counselling, inpatient admission, drug and alcohol treatment and crisis management |
| Priebe 2012 | TAU: participants allocated to the TAU condition were referred back to the referrer and encouraged to engage in any kind of treatment other than DBT; "this may have included treatment from psychotherapists, psychiatrists, community mental health teams, counsellors, general practitioners or user‐run support groups, all of which were offered free of charge under the NHS." (quote; p 358) |
| Asmand 2015 | TAU: unclear but TAU control group may have received individual work, but no details were provided |
| Thylstrup 2015 | TAU: access to opioid substitution treatment (if required); psychosocial support such as casework, counselling, or referral to residential rehabilitation; referral to 'off‐site' psychiatrist for treatment of other psychiatric conditions |
| McMurran 2016 | TAU: provided by participants’ usual‐care teams; TAU includes assessment, care planning, risk assessment and psychological interventions; participants excluded at baseline if accessing/likely to access psychological treatment programme specifically designed for personality disorder. |
| Nathan 2019 | TAU: standard probation supervision following release from prison; TAU comprises regular meetings (weekly initially) with the offender manager and engagement with other services where specified in the licence conditions. |
SBCM = Strengths‐based case management SM = Standard maintenance TAU = Treatment as usual
For the remaining six studies, all of which focussed on participants with substance misuse difficulties, we considered carefully whether the control condition was TAU or an intervention in its own right. In each case, we concluded that the control condition could properly be described as TAU because it represented what a treatment‐seeking participant with similar substance misuse problems would normally experience had the trial not taken place. The control conditions for these six studies are summarised below.
Woody 1985: standard drug counselling, which the investigators described as "a standard individual counselling intervention focussed on providing external services rather than dealing with intra‐psychic processes", plus standard methadone maintenance.
McKay 2000: two group therapy sessions per week based on addictions counselling and 12‐step recovery practices, which the trial investigators described as "standard continuing care treatment".
Messina 2003: one counselling session per fortnight, standard methadone maintenance, case management visits and medical care, which the trial investigators described as "methadone maintenance".
Ball 2005: up to three sessions per week of group counselling and psychoeducation sessions plus standard methadone maintenance, where appropriate, which the trial investigators described as "standard group substance abuse counselling".
Neufeld 2008: two individual counselling sessions per week with standard methadone maintenance treatment, which the trial investigators described as "standard methadone treatment".
Thylstrup 2015: access to opioid substitution treatment (if required); psychosocial support such as casework, counselling, or referral to residential rehabilitation; or referral to 'off‐site' psychiatrist for treatment of other psychiatric conditions (if required).
None of the active interventions were used as the control condition in any of the studies.
Outcomes
Primary outcomes
There were five studies that did not report on any of the primary outcomes defined in the protocol for this review (Gibbon 2009): Woody 1985; McKay 2000; Messina 2003; Havens 2007 and Asmand 2015. For the 14 studies that did report on one or more of our primary outcomes, we provide a summary below of which studies assessed which primary outcomes.
Five studies included aggression as an outcome: Davidson 2009, Tarrier 2010, Bernstein 2012, Feigenbaum 2012 and Thylstrup 2015.
Four studies included reconviction as an outcome: Marlowe 2007, Woodall 2007, Bernstein 2012 and Nathan 2019.
Three studies reported global state/functioning as an outcome: Tyrer 2004 and McMurran 2016, both of whom used the Global Assessment of Functioning (GAF) scale; and Bernstein 2012 who reported a dichotomous global outcome for participants.
Eight studies included self‐reported social functioning as an outcome: Tyrer 2004, Huband 2007, Davidson 2009 and McMurran 2016, all of whom used the Social Functioning Questionnaire; and Ball 2005, Neufeld 2008, Tarrier 2010 and Bernstein 2012 who used other methods.
Seven studies reported data on adverse events: Tyrer 2004, Marlowe 2007, Feigenbaum 2012, Priebe 2012, Thylstrup 2015, McMurran 2016, and Nathan 2019.
Please see Appendix 3 for full details of all the primary outcomes and measures used.
Secondary outcomes
Fourteen of the included studies addressed one or more of the secondary outcomes defined in this review. Below, we provide a summary of which studies assessed which secondary outcomes. Please see Appendix 3 for full details of all the secondary outcomes.
Three studies reported on quality of life: Tyrer 2004, Priebe 2012 and McMurran 2016.
Four studies reported on engagement with services: Havens 2007, Neufeld 2008, Bernstein 2012 and McMurran 2016.
Only a single study examined satisfaction with treatment: Davidson 2009.
Thirteen studies reported data on leaving the study early: Woody 1985, McKay 2000, Messina 2003, Ball 2005, Marlowe 2007, Neufeld 2008, Davidson 2009, Tarrier 2010, Bernstein 2012, Priebe 2012, Thylstrup 2015, McMurran 2016 and Nathan 2019. Of these 13 studies, four had data available for participants with AsPD: Messina 2003, Neufeld 2008, Davidson 2009 and Thylstrup 2015.
Eight studies reported on substance misuse. To aid interpretation, we considered substance misuse as two separate outcomes: substance misuse ‐ drugs; and substance misuse ‐ alcohol. Six studies examined substance misuse ‐ drugs: Woody 1985, McKay 2000, Messina 2003, Marlowe 2007, Neufeld 2008 and Thylstrup 2015. Six studies examined substance misuse ‐ alcohol: McKay 2000, Marlowe 2007, Woodall 2007, Neufeld 2008, Davidson 2009 and Thylstrup 2015.
Two studies considered employment status: Neufeld 2008 and McMurran 2016.
Four studies considered economic outcomes: Tyrer 2004, Davidson 2009, Priebe 2012 and McMurran 2016 examined direct economic outcomes; and Feigenbaum 2012 and McMurran 2016 examined indirect economic outcomes.
Two studies measured self‐reported impulsivity: Huband 2007 and Tarrier 2010.
Four studies included a self‐reported measure of anger: Huband 2007, Davidson 2009, Tarrier 2010 and Feigenbaum 2012.
Eight studies assessed mental state: Woody 1985, Davidson 2009, Tarrier 2010, Bernstein 2012, Feigenbaum 2012, Priebe 2012, Asmand 2015 and McMurran 2016.
Six studies assessed other outcomes. Four of these six studies assessed early maladaptive schemas and schema modes (Ball 2005; Davidson 2009; Tarrier 2010; Bernstein 2012), and two studies assessed dissociation using the Dissociative Experiences Scale (DES) (Huband 2007; Feigenbaum 2012).
No study assessed housing/accommodation status or prison/service outcomes.
Appendix 3 provides details of other relevant outcomes reported by the included studies; this includes details of psychometric assessments of mental state, measurements of change on risk assessment tools, and measures of therapy adherence.
Study funding sources
The 19 included studies were funded by a variety of sources, including research councils, government departments, charities and commercial organisations. Of the 19 studies, 13 were funded by grants from a single organisation; five studies received financial support from two or more organisations (Huband 2007; Bernstein 2012; Feigenbaum 2012; Thylstrup 2015; Nathan 2019); and one study was not directly funded (Asmand 2015). Eleven studies were funded through grants from major research councils such as: Medical Research Council (UK) (Tyrer 2004; Davidson 2009); National Institute for Health Research (UK) (Priebe 2012; McMurran 2016); National Institute on Alcohol Abuse and Alcoholism (USA) (Woodall 2007); National Institute on Drug Abuse (USA) (Woody 1985; McKay 2000; Messina 2003; Havens 2007; Marlowe 2007; Neufeld 2008). Four studies were fully or partially funded by government departments (Huband 2007; Tarrier 2010; Bernstein 2012; Nathan 2019) and two studies were funded by not‐for‐profit or charitable organisations (Ball 2005; Thylstrup 2015); Thylstrup 2015 was also partially funded by a commercial organisation. Full details of study funding is provided in the 'Notes' section in each of the Characteristics of included studies tables.
Excluded studies
We excluded a total of 201 full‐text reports from the updated searches; 118 reports were irrelevant and are not reported in any more detail. The remaining 57 studies (from 77 reports) initially appeared to meet the inclusion criteria, but on closer inspection did not. The reasons for excluding these studies are reported in the Characteristics of excluded studies table following guidance in Chapter Four of the Cochrane Handbook of Systematic Reviews of Interventions (Lefebvre 2019), together with details of 32 studies excluded from the original review (Gibbon 2010). Two additional studies excluded from the previous review are actually additional reports of Vinnars 2005 and treated as such in this update. Readers are advised that studies may be excluded for multiple reasons and not all reasons may be noted.
In summary, we excluded 89 studies (from 117 reports) for the following reasons: 19 studies were not RCTs; 38 studies had an ineligible population (e.g. AsPD was a diagnosis of exclusion, no AsPD participants, comorbid diagnosis of a major mental illness); 21 studies used a control condition that was not considered to be TAU, waiting list, or a 'no treatment' control; 11 studies for other reasons (e.g. insufficient number of AsPD participants to allow the mean or SD to be calculated for group data, non‐psychological intervention).
Studies awaiting classification
In the original review (Gibbon 2010), we categorised three studies as awaiting classification (Evans 1999; Linehan 2006; Berget 2008). We identified a new citation for Berget 2008 in the updated searches and sought clarification from the trial investigators; however, no further information was available at the time this review was prepared.
The updated searches identified a further four studies categorised as awaiting classification. Of these, there were three studies of psychological treatments for samples of participants with a mixture of personality disorders, where it remains unclear whether or not a subgroup of participants with a diagnosis of antisocial or dissocial personality disorder have been included (Clarke 2013; Jochems 2015; Black 2016). We sought clarification from the trial investigators; however, no further information was available at the time this review was prepared. We also identified one study where the study authors provided a manuscript that was 'under review' with a journal, but not yet published (Buric 2019).
We summarise these seven studies below. Further details on these studies are provided in the Characteristics of studies awaiting classification tables.
Evans 1999 compared manual assisted cognitive behavioural therapy (MACT) with TAU for individuals with a recent self‐harm episode and personality disturbance. The study may have a subgroup of participants with a diagnosis of AsPD.
Linehan 2006 compared dialectical behaviour therapy with community treatment by experts for women with recent suicidal and self‐injurious behaviours meeting the criteria for borderline personality disorder (BPD). The study may have recruited a subgroup with AsPD since 11 of 101 participants (10.9%) had a cluster B personality disorder other than BPD.
Berget 2008 compared animal‐assisted therapy with a control condition in individuals with psychiatric disorders, and may have recruited a subgroup with dissocial personality disorder, since 22 of the 90 participants had a disorder diagnosed under sections F60 to 69 (disorders of adult personality and behaviour) in the ICD‐10.
Clarke 2013 compared cognitive analytic therapy + TAU with TAU alone in individuals with personality disorder referred to a specialist outpatient service. Of the 99 randomised participants, at least 18 had a cluster B personality disorder. We contacted the trial author with a request to identify the potential number of participants with AsPD.
Jochems 2015 compared motivational feedback with TAU for patients receiving individual outpatient treatment for a mental disorder. Ordinarily, this study would meet the exclusion criteria for this review as it included patients with psychotic disorders. However, it reported an interaction effect of personality disorder on outcomes. Correspondence with the study author confirmed 25/294 (8%) participants with AsPD at baseline and 12/254 (5%) participants with AsPD at follow‐up; however, further clarification is required regarding the presence or absence of comorbid psychotic disorder.
Black 2016 reported a secondary analysis of previously unpublished data from two studies of Systems Training for Emotional Predictability and Problem Solving (STEPPS) + TAU compared with TAU. Published data are provided for AsPD participants in the intervention group (n = 16) and the reviewers contacted the study author to request information on any AsPD participants in the control group.
Buric 2019 reported unpublished data comparing mindfulness meditation, yoga, and waiting‐list control for inmates in a clinical prison unit for individuals with severe personality disorder.
Ongoing studies
Six ongoing studies were identified in the updated searches (NCT03883646; NCT02524171; ISRCTN32309003; ISRCTN14994755; Van Dijk 2019; NCT04033835). A brief summary of these studies is provided below; comprehensive details of the studies can be found in the Characteristics of ongoing studies tables.
NCT03883646 is comparing mindfulness, relapse prevention, waiting‐list control and TAU (intervention duration is not stated) for female prisoners with alcohol use disorders. The study investigators have confirmed that they are assessing antisocial personality disorder and psychopathy (NCT03883646). The primary outcomes of the study include alcohol craving, alcohol consumption, temptation to drink alcohol and criminal behaviour.
NCT02524171 is comparing a 12‐week, group‐based, cognitive‐behavioural intervention (moral reconation therapy plus usual care) with usual care for veterans with AsPD or substance use disorder (or both). The primary outcome of the trial is risk for criminal recidivism. Secondary outcomes include substance use, mental health and housing/employment problems.
ISRCTN32309003 is comparing a group or individual intervention (one‐hour session of individual MBT plus 75 minutes, group‐based mentalisation, once a month for 12 months) with probation‐as‐usual for male offenders who have a history of violent behaviour. The primary outcome is frequency of aggressive acts. Secondary outcomes include changes in psychometric assessment of clinical outcomes, anger, social functioning, impulsiveness, alcohol and drug use, service engagement, client satisfaction and suicidal/self‐harm behaviour.
ISRCTN14994755 compared a flexible intervention (six to 10 sessions of psychological support for personality delivered over three to six months) with TAU for adults using secondary care mental health services. The primary outcomes of the trial were social functioning, mental well‐being, suicidal thoughts, health‐related quality of life, satisfaction with care, resources use/costs, and change in mental health. The secondary outcome was participant confidence in their ability to 'get yourself through difficult times and situations'.
Van Dijk 2019 compared 18‐week, group schema‐focussed therapy enriched with psychomotor therapy with TAU for older adults (60 years or older) with personality disorder. The primary outcomes of the study were psychological distress, quality of life and cost‐effectiveness. The secondary outcomes were life satisfaction, mental well‐being, personality functioning, interoceptive body awareness, substance use and mental state.
NCT04033835 is comparing 18 months of introductory mentalisation‐based treatment with TAU for male sentenced prisoners with borderline or antisocial personality disorder (or both). The primary outcome of the study is successful completion of the study. The secondary outcomes of the study are change in interpersonal functioning, impulsivity, mental state, depressive symptoms, anxiety symptoms, social functioning, global functioning, challenging behaviour and satisfaction with treatment.
Risk of bias in included studies
There was considerable variation in how the included studies were reported. We attempted to contact the investigators wherever the available trial reports provided insufficient information for decisions to be made about the likely risk of bias.
We summarise below the risk of bias for the 19 included studies. Studies with data that could be extracted for the antisocial or dissocial personality disorder subgroup (10 studies: made up of 100% AsPD subgroup (eight studies: Messina 2003; Huband 2007; Woodall 2007; Neufeld 2008; Davidson 2009; Priebe 2012; Asmand 2015; Thylstrup 2015); or > 75% AsPD in sample (2 studies: Bernstein 2012 and Nathan 2019)) are summarised separately from those for which data were unavailable (nine studies: Woody 1985; McKay 2000; Tyrer 2004; Ball 2005; Havens 2007; Marlowe 2007; Tarrier 2010; Feigenbaum 2012; McMurran 2016). This allows the reader to make a separate judgement about possible bias associated with the quantitative data from which conclusions are drawn in this review. Full details of our assessment of the risk of bias in each included study are tabulated within the 'Risk of bias' tables in the 'Characteristics of included studies' section. Graphical summaries of the risk of bias in each included study are presented in Figure 2 and Figure 3.
2.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
Sequence generation
With data (10 studies)
We considered the generation of allocation sequence to be adequate in eight studies where allocation was by random numbers that were: computer‐generated (Huband 2007; Davidson 2009; Bernstein 2012; Priebe 2012; Thylstrup 2015; Nathan 2019); derived from a table (Messina 2003); or used the toss of coin (Neufeld 2008). We classified the adequacy of the sequence generation as unclear in the remaining two studies: Woodall 2007, where the investigators reported that participants had been allocated at random but provided no further information on how this had been achieved; and Asmand 2015 where use of a random number table was indicated in the study protocol, but not reported in the paper.
Without data (nine studies)
We classified sequence generation as adequate for four studies: Tyrer 2004 and McMurran 2016 (computer‐generated random numbers); and Tarrier 2010 and Feigenbaum 2012 (telephone randomisation process). We rated the sequence generation as unclear for the remaining five studies (Woody 1985; McKay 2000; Ball 2005; Havens 2007; Marlowe 2007). In each case, the investigators reported that participants had been allocated at random, but provided no further information on how this had been achieved.
Allocation concealment
With data (10 studies)
We considered concealment of the allocation sequence adequate for seven studies (Messina 2003; Huband 2007; Neufeld 2008; Davidson 2009; Bernstein 2012; Priebe 2012; Nathan 2019), where we considered that there was sufficient evidence that the person enrolling participants could not have foreseen assignment. We classified the adequacy of sequence concealment as unclear in three studies (Woodall 2007; Asmand 2015; Thylstrup 2015), because the information available was insufficient to allow a judgment to be made.
Without data (nine studies)
We considered concealment of the allocation sequence adequate for four studies due to stated methodology: Tyrer 2004; Tarrier 2010; Feigenbaum 2012; and McMurran 2016. We classified the adequacy of sequence concealment as unclear in the remaining five studies (Woody 1985; McKay 2000; Ball 2005; Havens 2007; Marlowe 2007), again because the information available was insufficient to allow a judgement to be made.
Blinding
Performance bias
We judged 17 studies to be an unclear risk of performance bias for participants because it was not clear whether or not participants could have foreseen treatment allocation. We considered two studies, Feigenbaum 2012 and McMurran 2016, to be at high risk of bias because participants were not blinded to treatment allocation.
We judged that blinding of personnel involved in the delivery of the intervention was not practical in the design of trials of psychological interventions summarised in this review. For this reason, we judged 16 studies to be at an unclear risk of performance bias for personnel. We considered two studies, McMurran 2016 and Nathan 2019, to be at high risk of bias because personnel were not blinded to treatment allocation. We judged only one study, Tarrier 2010, to be at low risk of bias for blinding of personnel because the evaluation was conducted by an independent team.
Detection bias
With data (10 studies)
We considered the adequacy of blinding of outcome assessors to be adequate in two studies and that it was unlikely that this blinding could have been broken (Neufeld 2008; Davidson 2009). Two studies did not blind the outcome assessors and so we rated these at high risk of detection bias (Messina 2003; Nathan 2019). We classified the six remaining studies at unclear risk of detection bias because the information available was insufficient to allow a judgment to be made (Huband 2007; Woodall 2007; Bernstein 2012; Priebe 2012; Asmand 2015; Thylstrup 2015).
Without data (nine studies)
We judged the adequacy of blinding of outcome assessors to be adequate for two studies due to stated methodology (Woody 1985; Tarrier 2010), and not adequate for two studies as assessors were informed of the treatment condition (McKay 2000), or could mostly identify the treatment group of the patient (Feigenbaum 2012). In the remaining five studies (Tyrer 2004; Ball 2005; Havens 2007; Marlowe 2007; McMurran 2016), there was insufficient information to allow a judgement to be made.
Incomplete outcome data
With data (10 studies)
We judged a single study to have adequately addressed attrition bias (Bernstein 2012). We classified three studies as inadequately addressing attrition bias (Asmand 2015; Thylstrup 2015; Nathan 2019) and the remaining six studies at unclear risk of attrition bias because, although numbers were balanced approximately between treatment conditions, the reasons for attrition were not available (Messina 2003; Huband 2007; Woodall 2007; Neufeld 2008; Davidson 2009; Priebe 2012). This generally arose because participants failed to complete endpoint measures without providing a reason. Three of these six studies reported undertaking an intention‐to‐treat analysis for at least one primary or secondary outcome (Huband 2007; Davidson 2009; Priebe 2012), and four provided analysis for those participants classed by the investigators as 'completers' (Messina 2003; Woodall 2007; Neufeld 2008; Priebe 2012).
Without data (nine studies)
We judged a single study, Tarrier 2010, to have adequately addressed attrition bias. We classed seven studies at unclear risk of attrition bias because it was not possible, in the absence of data from the subgroup with antisocial or dissocial personality disorder, to judge the extent and nature of any missing data and whether the reasons for such missing data were balanced across intervention groups. We judged a single study, McMurran 2016, at high risk of attrition bias. This study was terminated early due to safety concerns and reported the use of multiple data imputation.
Selective reporting
With data (10 studies)
We judged five studies at low risk of reporting bias as they appeared to have reported on all the measures they set out to use, and at all time scales, in as far as could be discerned from the published reports without access to the original protocols (Messina 2003; Huband 2007; Woodall 2007; Neufeld 2008; Davidson 2009). We classified two studies at unclear risk of reporting bias as there was insufficient information on which to make a judgement (Priebe 2012; Thylstrup 2015). We assessed three studies as having a high risk of reporting bias due to non‐reporting of stated outcomes (Bernstein 2012; Asmand 2015; Nathan 2019) . Bernstein 2012 acknowledged selective reporting as a consequence of the publication of preliminary and incomplete trial data.
Without data (nine studies)
We judged five studies at low risk of reporting bias as they appeared to have reported on all the measures they set out to use, and at all time scales, in as far as could be discerned from the published reports without access to the original protocols (Woody 1985; McKay 2000; Tyrer 2004; Havens 2007; Marlowe 2007). We classified three studies at unclear risk of reporting bias as there was insufficient information on which to make a judgement (Tarrier 2010; Feigenbaum 2012; McMurran 2016). We assessed one study as having a high risk of reporting bias due to the non‐reporting of endpoint or follow‐up data for three stated outcomes (Ball 2005).
Other potential sources of bias
With data (10 studies)
We considered two studies to be at high risk of other potential sources of bias (Asmand 2015; Nathan 2019). Asmand 2015 was judged to be at high risk of language or comprehension bias due to the poor quality of the English‐language translation and the numerous typographical errors in the report. Nathan 2019 was considered to be at high risk of allegiance bias and 'vested interest' bias due to funding and commissioning issues, and also to have an unclear risk of publication bias due to the long period of time between the study's completion and publication of results.
We assessed five studies to have an unclear risk of other sources of bias (Messina 2003; Huband 2007; Woodall 2007; Bernstein 2012; Thylstrup 2015). Messina 2003 reported providing a reduction of US$40 per month (representing a discount of between 22% and 29%) in the cost of methadone maintenance treatment as an incentive for participation in the study; we classed this study at an unclear risk of bias because of uncertainty about whether or not this could have introduced bias. Huband 2007 reported measurements at two time points (baseline and endpoint) and may be subject to bias from those participants in either a very optimistic or pessimistic state of mind; this study may also have potential bias arising from a baseline imbalance as those in the intervention group were significantly more likely to have had psychiatric hospitalisation at some time in their life in comparison with the controls. Woodall 2007 reported a baseline imbalance where the intervention group was significantly more likely to have histories of drinking and driving in comparison with the controls, although it was unclear if this applied to the AsPD subgroup. We assessed Bernstein 2012 as potentially having 'vested interests' in the development of the intervention under investigation and the development of tools/instruments used in the study. Lastly, Thylstrup 2015 was partially funded by manufacturers of an opioid replacement drug and participants may have received an opioid replacement as part of their treatment‐as‐usual regimen; however, it is uncertain whether or not this could have introduced bias.
We judged the remaining three studies to be free of other potential sources of bias (Neufeld 2008; Davidson 2009; Priebe 2012).
Without data (nine studies)
We classed one study, Tarrier 2010, at high risk of allegiance bias as funding had been secured to develop a service delivering the experimental intervention and there was a long delay in the publication of the study results in a peer‐reviewed journal. We also had concerns regarding adherence to the treatment protocol, as participants in the control condition reportedly received more therapy than the intervention group.
We assessed four studies as having an unclear risk of other sources of bias (Havens 2007; Marlowe 2007; Feigenbaum 2012; McMurran 2016). We classed Havens 2007 as unclear risk of bias because, as the trial investigators acknowledged, bias may have been present because only those completing the one‐month follow‐up were eligible for psychiatric assessment and participants in the case management arm were significantly less likely to have been followed up. We classed Marlowe 2007 at unclear risk of bias because of uncertainty about possible risk of bias arising from a diagnosis of AsPD using an 'antisocial personality disorder interview' derived from SCID‐II by the trial investigators, but with no information on its validation. We classed Feigenbaum 2012 at unclear risk of bias for both attention and allegiance bias, as treatments offered in the TAU condition were not examined as carefully as the experimental condition; the investigators provided most, but not all, of the components of the experimental intervention; the intervention was provided through a newly‐established clinical service; and there was a significant time lapse between the study completion and publication in a peer‐reviewed journal. We classed McMurran 2016 at unclear risk of bias as there was potential allegiance bias from the intervention, and warnings provided about the study may have impacted on the study management and ongoing treatment delivery, though it is unclear whether this could have introduced bias.
We judged the remaining four studies to be free of other potential sources of bias (Woody 1985; McKay 2000; Tyrer 2004; Ball 2005).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 5; Table 6; Table 7; Table 8; Table 10
Data on participants with AsPD were available, either in the study report or directly from the study authors, for 10 of the 19 included studies (Messina 2003; Huband 2007; Woodall 2007; Neufeld 2008; Davidson 2009; Bernstein 2012; Priebe 2012; Asmand 2015; Thylstrup 2015; and Nathan 2019). Data on the subgroup of participants with antisocial or dissocial personality disorder from the other nine studies were not available at the time this review was prepared and thus these studies are not discussed any further in this section (Woody 1985; McKay 2000; Tyrer 2004; Ball 2005; Havens 2007; Marlowe 2007; Tarrier 2010; Feigenbaum 2012McMurran 2016).
A significant proportion of the quantitative data available from the studies included in this review met our criteria for skewed data, as described in the section on 'Measures of treatment effect'. Consequently, in the absence of raw data from the trial investigators, we presented all skewed data in 'Additional tables' and reported statistics on comparisons between conditions as calculated by the trial investigators, rather than performing our own analyses.
We did not carry out any syntheses of primary or secondary outcome data using meta‐analyses (other than for the outcome of 'leaving the study early') because (a) data for an outcome were available from only one study, or (b) we wanted to minimise the risk of applying parametric statistics to skewed data that was not normally distributed.
Comparison 1: cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone
We included one study in this comparison: Davidson 2009 (male outpatients with AsPD and recent verbal/physical violence; six and 12 months treatment; n = 52). See Table 1.
Primary outcomes
Aggression
Davidson 2009 found no difference between the treatment and control conditions at 12 months post‐intervention in numbers reporting any act of verbal aggression (OR 1.25, 95% CI 0.40 to 3.94, P = 0.70, 52 participants, 1 study, low‐certainty evidence Analysis 1.1) or physical aggression (OR 0.92, 95% CI 0.28 to 3.07, P = 0.90, 52 participants, 1 study, low‐certainty evidence, Analysis 1.2), assessed with the MacArthur Community Violence Screening Instrument. Davidson 2009 also found no significant difference between the treatment and control conditions from baseline to endpoint (at 12 months) in the change (reduction) in number reporting any act of verbal aggression (OR 0.94, 95% CI 0.29 to 3.00, P = 0.92, 52 participants, 1 study, low‐certainty evidence, Analysis 1.3) or of physical aggression (OR 1.20, 95% CI 0.40 to 3.62, P = 0.75, 52 participants, 1 study, low‐certainty evidence, Analysis 1.4). The trial investigators observed, however, that "incidents of any acts of verbal or physical aggression decreased in both groups over the year of the study" (p 574).
1.1. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 1: Aggression: number reporting any act of verbal aggression; MCVSI interview; at 12 months
1.2. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 2: Aggression: number reporting any act of physical aggression; MCVSI interview; at 12 months
1.3. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 3: Aggression: change in number reporting any act of verbal aggression (high = good); MCVSI interview; baseline to endpoint at 12 months
1.4. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 4: Aggression: change in number reporting any act of physical aggression (high = good); baseline to endpoint at 12 months
Social functioning
Davidson 2009 found no clear difference between the treatment and control conditions in mean scores on the Social Functioning Questionnaire (SFQ; eight items, rated on four‐point scale (anchors vary across items) by responders who indicate the extent to which they experienced problems over past two weeks; scores range from 0 to 24; higher scores indicate greater social dysfunction) at 12 months/last recorded assessment (MD −1.60 points, 95% CI −5.21 to 2.01, P = 0.39, 39 participants, 1 study, very low‐certainty evidence, Analysis 1.5). Davidson 2009 also found no clear difference between the treatment and control conditions in the 'difference between baseline and last value' of total scores on the SFQ (MD 1.70, 95% CI −1.80 to 5.10, P = 0.33; analysis by trial investigators; analysis not shown).
1.5. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 5: Social functioning: mean SFQ scores (high = poor); at 12 months
The study did not report data on any of our other primary outcomes: reconviction; global state/functioning; or adverse events.
Secondary outcomes
Satisfaction with treatment
Davidson 2009 found no significant difference between the treatment and control conditions in mean scores for 'satisfaction with taking part in the study' (rated on a six‐point Likert scale ranging from one (not at all) to seven (very much); higher scores indicate greater satisfaction) (MD 0.70, 95% CI −0.22 to 1.62, P = 0.14, 25 participants, Analysis 1.6).
1.6. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 6: Satisfaction with treatment: satisfaction with taking part in the study (high = good); at 12 months
Leaving the study early
Davidson 2009 found no significant difference between the treatment and control conditions for number of participants leaving the study early by three months (OR 0.63, 95% CI 0.19 to 2.13, P = 0.46, 52 participants, 1 study, low‐certainty evidence, Analysis 1.7), six months (OR 0.96, 95% CI 0.31 to 2.96, P = 0.94, 52 participants, 1 study, low‐certainty evidence, Analysis 1.8), nine months (OR 1.84, 95% CI 0.61 to 5.57, P = 0.28, 52 participants, 1 study, low‐certainty evidence, Analysis 1.9), or by 12 months (OR 0.88, 95% CI 0.23 to 3.33, P = 0.84, 52 participants, 1 study, low‐certainty evidence, Analysis 1.10).
1.7. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 7: Leaving the study early; by 3 months
1.8. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 8: Leaving the study early; by 6 months
1.9. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 9: Leaving the study early; by 9 months
1.10. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 10: Leaving the study early; by 12 months
Substance misuse ‐ alcohol
Davidson 2009 reported skewed summary data (see Table 19) that indicated no significant difference between the treatment and control conditions at 12 months for mean overall scores (MD (change from baseline) 4.1, 95% CI −0.6 to 8.9, P = 0.08; last‐observation‐carried‐forward by the trial investigators) and total unit scores (MD (change from baseline) 0.6, 95% CI −7.6 to 8.8, P = 0.88; intention‐to treat‐analysis by the trial investigators in each case) on the AUDIT (Alcohol Use Disorders Identification Test; 10‐items, rated on five‐point scale (ranging from zero to four; response anchors vary across item content); a score of eight or more indicates harmful alcohol use).
8. Comparison 1. Cognitive behavioural therapy (CBT) + treatment‐as‐usual (TAU) versus TAU: alcohol abuse scores (skewed data).
| Study | Outcome | Experimental group: CBT + TAU | Control group: TAU | Comparison of difference (95% CI) | Notes | ||||
| Baseline mean (SD), [n] | Last value mean (SD) [n] | Difference (95% CI) | Baseline mean (SD) [n] | Last value Mean (SD) [n] | Difference (95% CI) | ||||
| Davidson 2009 | AUDIT scores (high = poor); at 12 months | 8.2 (6.8), [25] | 5.9 (7.6), [19] | 4.1 (0.5 to 7.7), P = 0.03 | 11.1 (5.9), [27] | 11.0 (9.4), [20] | 0.3 (−3.1 to 3.7), P = 0.85 | 4.1 (−0.6 to 8.9), P = 0.08 | Favours neither group LOCF analysisa |
| Davidson 2009 | AUDIT total units scores (high = poor); at 12 months | 8.4 (9.1), [24] | 7.9 (10.0), [18] | 2.7 (−2.8 to 8.2), P = 0.31 | 15.7 (12.4), [26] | 10.7 (14.7), [20] | 5.5 (−1.7 to 12.8), P = 0.12 | 0.6 (−7.6 to 8.8), P = 0.88 | Favours neither group LOCF analysisa |
| AUDIT: Alcohol Use Identification Test;CBT: cognitive behavioural therapy; CI: confidence interval; LOCF: last‐observation‐carried‐forward; n: number of participants;SD: standard deviation; TAU: treatment as usual. | |||||||||
aTrial investigators have used a last‐observation‐carried‐forward procedure (i.e. endpoint scores based on last available value).
Economic outcomes
Davidson 2009 provided data on the total cost of health, social work and criminal justice services received over 12 months, and the average cost per participant for NHS services alone over 12 months (see Table 20), but with no statistics.
9. Comparison 1. Cognitive behavioural therapy (CBT) + treatment‐as‐usual (TAU) versus TAU: costs of services received.
| Study | Outcome | Experimental group: CBT + TAU (n = 25) | Control group: TAU (n = 27) | Statistic |
| Davidson 2009 | Total cost of health, social work and criminal justice services received; over 12 months | GBP 38,004 | GBP 31,097 | No statistic available |
| Davidson 2009 | Average cost per participant for NHS services alone; over 12 months | GBP 1295 | GBP 1133 | No statistic available |
| CBT: cognitive behavioural therapy; GBP: British pound sterling; n: number of participants; TAU: treatment as usual. | ||||
Anger
Davidson 2009 found no significant difference between the treatment and control conditions at 12 months in mean scores on the Novaco Anger Scale (25‐item scale, rated on four‐point scale ranging from zero (little to no annoyance) to three (very angry), total score range = 0 to 100; higher scores indicate greater problems with anger) (MD −1.30 points, 95% CI −13.97 to 11.37, P = 0.84, 39 participants, Analysis 1.11), or in mean scores on the Novaco Provocation Inventory (80 items, rated on four‐point scale, ranging from one (very little) to five (very much), total score range = 80 to 400; higher scores indicate greater problems with anger) (MD −2.60 points, 95% CI −11.51 to 6.31, P = 0.57, 39 participants, Analysis 1.12).
1.11. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 11: Anger: mean Novaco Anger Scale scores (high = poor); at 12 months
1.12. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 12: Anger: mean Novaco Provocation Inventory scores (high = poor); at 12 months
Mental state
Davidson 2009 found no significant difference between the treatment and control conditions at 12 months in mean anxiety scores (MD −0.30 points, 95% CI −2.70 to 2.10, P = 0.81, 43 participants, 1 study, low‐certainty evidence, Analysis 1.13) and depression scores (MD −1.30 points, 95% CI −4.38 to 1.78, P = 0.41, 43 participants, 1 study, low‐certainty evidence, Analysis 1.14), assessed with the Hospital Anxiety and Depression Rating Scale (14‐item, self‐rating scale comprising two comprising two subscales (anxiety (seven items) and depression (seven items)), rated on a four‐point severity scale (ranging from zero (not at all) to three (all of the time); total score range = 0 to 21, with scores equal to 11 or above on either scale indicate a definite case).
1.13. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 13: Other: anxiety; mean HADS score (high = poor); at 12 months
1.14. Analysis.

Comparison 1: Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 14: Other: depression; mean HADS score (high = poor); at 12 months
Other outcomes
Davidson 2009 reported skewed summary data (see Table 21; intention‐to treat‐analysis by the trial investigators in each case), which indicated no significant difference between the treatment and control conditions at 12 months for mean scores on the following subscales of the Brief Core Schema Scales (24‐item, self‐report questionnaire comprising four scales measuring positive and negative beliefs about self and others; each scale comprises six statements with which the participant rates agreement (yes/no); if agree, they rate the strength of their belief from one (slightly) to four (totally); total item scores range from zero to four and total subscale scores from zero to 24).
10. Comparison 1: Cognitive behavioural therapy (CBT) + treatment‐as‐usual (TAU) versus TAU: schema scores; at 12 months (skewed data).
| Study | Outcome | Experimental group: CBT + TAU | Control group: TAU | Comparison of difference (95% CI) | Comments | ||||
| Baseline mean (SD), [n] | Last value mean (SD), [n] | Difference (95% CI) | Baseline mean (SD), [n] | Last value mean (SD), [n] | Difference (95% CI) | ||||
| Davidson 2009 | BCSS self‐as‐positive belief scores; at 12 months | 8.6 (5.7), [25] | 8.8 (6.3), [19] | 0.2 (−1.9 to 2.4), P = 0.84 | 7.8 (6.1) [27] | 7.2 (6.8), [20] | −0.1 (−3.0 to 2.7), P = 0.92 | −0.2 (−3.6 to 3.1), P = 0.89 | Favours neither group LOCF analysisa |
| Davidson 2009 | BCSS self‐as‐negative belief scores; at 12 months | 8.6 (5.5), [25] | 7.7 (6.7), [19] | 2.2 (−0.4 to 4.8), P = 0.09 | 10.1 (6.6) [27] | 8.6 (6.1), [20] | 0.5 (−2.1 to 3.1), P = 0.68 | −0.8 (−4.3 to 2.7), P = 0.64 | Favours neither group LOCF analysisa |
| Davidson 2009 | BCSS others‐as‐positive belief scores; at 12 months | 9.3 (6.1), [25] | 9.6 (6.4), [19] | −0.4 (−3.0 to 2.2), P = 0.74 | 6.6 (4.4) [27] | 5.6 (4.4), [20] | 1.2 (−1.0 to 3.4), P = 0.28 | −2.6 (−5.8 to 0.5), P = 0.10 | Favours neither group LOCF analysisa |
| Davidson 2009 | BCSS others‐as‐negative belief scores; at 12 months | 12.9 (7.4), [25] | 11.9 (8.2), [19] | 0.2 (−1.7 to 2.1), P = 0.82 | 11.8 (7.1) [27] | 9.1 (5.3), [20] | 2.4 (−0.7 to 5.6), P = 0.12 | −2.4 (−5.8 to 0.9), P = 0.15 | Favours neither group LOCF analysisa |
| BCSS: Brief Core Schema Scales; CBT: cognitive behavioural therapy; CI: confidence interval; LOCF: last‐observation‐carried‐forward; n: number of participants; SD: standard deviation; TAU: treatment as usual. | |||||||||
aTrial investigators have used a last‐observation‐carried‐forward procedure (i.e. endpoint scores based on last available value).
'self‐as‐positive' belief scores (MD (change from baseline) −0.2, 95% CI −3.6 to 3.1, P = 0.89).
'self‐as‐negative' belief scores (MD (change from baseline) −0.8, 95% CI −4.3 to 2.7, P = 0.64).
'others‐as‐positive' belief scores (MD (change from baseline) −2.6, 95% CI −5.8 to 0.5, P = 0.10).
'others‐as‐negative' belief scores (MD (change from baseline) −2.4, 95% CI −5.8 to 0.9, P = 0.15).
Neither study reported data on any of our other secondary outcomes: quality of life; engagement with services; employment status; housing/accommodation status; impulsivity; mental state; or prison and service outcomes.
Comparison 2: impulsive lifestyle counselling (ILC) + treatment‐as‐usual versus treatment‐as‐usual alone
We included one study in this comparison: Thylstrup 2015 (male and female adults with AsPD receiving outpatient treatment for drug and alcohol problems; intervention delivered over six sessions; n = 176). See Table 2.
Primary outcomes
Aggression
Thylstrup 2015 reported scores on the 12‐item short‐form of the Buss‐Perry Aggression Questionnaire (scored on a five‐point Likert scale ranging from one (extremely uncharacteristic) to five (extremely characteristics), at baseline, and three and nine months post‐intervention (Table 22). There was no difference between ILC + treatment‐as‐usual (TAU) and TAU alone for trait aggression at three months (MD 0.18, 95% CI −0.22 to 0.58; 131 participants, 1 study, very low‐certainty evidence; Analysis 2.1) or at nine months (MD 0.07, CI −0.35 to 0.49, 118 participants, 1 study, very low‐certainty evidence; Analysis 2.2).The study authors also reported scores − skewed data (Table 23) − on the Self‐Report of Aggression and Social Behavior Measure (SRASBM) at baseline, and three and nine months post‐intervention. Although aggression decreased from baseline to both three and nine months, the study authors reported that "No differences were found between ILC and TAU at any point, but across both groups considerable reductions in interpersonal aggression were observed at both follow‐up waves" (p 8, column 1).
11. Comparison 2. Impulsive lifestyle counselling (ILC) + treatment‐as‐usual (TAU) versus TAU; additional SMD data for aggression outcomes.
| Study | Outcome | Experimental group: ILC + TAU | Control group: TAU | Statistic | Comments | ||
| SMD | n | SMD | n | ||||
| Thylstrup 2015 | Aggression: change in BPAQ‐SF from baseline to 3 months | 0.34 | 70 | 0.50 | 61 | None reported | ‐ |
| Thylstrup 2015 | Aggression: change in BPAQ‐SF from baseline to 9 months | 0.72 | 63 | 0.76 | 55 | None reported | ‐ |
| Thylstrup 2015 | Aggression: change in SRASBM from baseline to 3 months | 0.47 | 70 | 0.57 | 61 | None reported | ‐ |
| Thylstrup 2015 | Aggression: change in SRASBM from baseline to months | 0.75 | 63 | 0.31 | 55 | None reported | ‐ |
| BPAQ‐SF: Buss‐Perry Aggression Questionnaire ‐ Short Form; ILC: impulsive lifestyle counselling; n: number of participants; SMD: standardised mean difference; SRASBM: Self‐Report of Aggression and Social Behavior Measure; TAU: treatment as usual. | |||||||
2.1. Analysis.

Comparison 2: Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 1: Aggression: scores on Buss‐Perry Aggression Questionnaire (BPAQ) at 3 months
2.2. Analysis.

Comparison 2: Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 2: Aggression: scores on Buss‐Perry Aggression Questionnaire (BPAQ) at 9 months
12. Comparison 2. Impulsive lifestyle counselling (ILC) + treatment‐as‐usual (TAU) versus TAU (skewed data).
| Study | Outcome | Experimental group: ILC + TAU | Control group: TAU | Statistic | Comments | ||||
| n | Mean | SD | n | Mean | SD | ||||
| Thylstrup 2015 | Aggression: Self‐Report of Aggression and Social Behavior Measure (SRASBM) at 3 months | 70 | 0.64 | 0.49 | 61 | 0.64 | 0.46 | Regression coefficienta = 0.083 (95% CI −0.092 to 0.260), P > 0.05 | Favours neither group |
| Thylstrup 2015 | Aggression: Self‐Report of Aggression and Social Behavior Measure (SRASBM) at 9 months | 63 | 0.47 | 0.39 | 55 | 0.61 | 0.52 | Regression coefficientb = 0.026 (95% CI −0.158 to 0.210), P > 0.05 | Favours neither group |
| Thylstrup 2015 | Substance misuse: Addiction Severity Index (ASI), drug composite score at 3 months | 70 | 0.17 | 0.12 | 61 | 0.21 | 0.12 | Regression coefficientc = −0.052 (95% CI −0.096 to −0.009), P = 0.018. | Favours experimental group: ILC + TAU |
| Thylstrup 2015 | Substance misuse: Addiction Severity Index (ASI), drug composite score at 9 months | 63 | 0.15 | 0.12 | 55 | 0.16 | 0.13 | Regression coefficientd = −0.0040 (95% CI −0.049 to 0.042), P > 0.05 | Favours neither group |
| Thylstrup 2015 | Substance misuse: Addiction Severity Index (ASI), alcohol composite score at 3 months | 72 | 0.12 | 0.22 | 61 | 0.12 | 0.22 | Regression coefficiente = 0.008 (95% CI −0.061 to 0.077), P > 0.05 | Favours neither group |
| Thylstrup 2015 | Substance misuse: Addiction Severity Index (ASI), alcohol composite score at 9 months | 63 | 0.12 | 0.21 | 55 | 0.1 | 0.18 | Regression coefficientf = 0.049 (95% CI −0.023 to 0.121), P > 0.05 | Favours neither group |
| Thylstrup 2015 | Substance misuse: Days abstinent (in previous 30 days) at 3 months | 72 | 13.2 | 12.7 | 61 | 10.8 | 11.2 | Regression coefficientg = 4.319 (95% CI 0.183 to 8.456), P < 0.05 | Favours experimental group: ILC + TAU |
| Thylstrup 2015 | Substance misuse: Days abstinent (in previous 30 days) at 9 months | 63 | 15.3 | 13.3 | 55 | 13.7 | 12.7 | Regression coefficienth = 3.584 (95% CI −0.751 to 7.919), P > 0.05 | Favours neither group |
| ASI: Addiction Severity Index; CI: confidence interval; ILC: impulsive lifestyle counselling; n: number of participants; SD: standard deviation; SRASBM: Self‐Report of Aggression and Social Behaviour Measure; TAU: treatment as usual. | |||||||||
aResult of mixed effects regression on aggression outcomes (SRASBM as dependent variable), ILC × 3 months. bResult of mixed effects regression on aggression outcomes (SRASBM as dependent variable), ILC × 9 months. cResult of mixed effects regression on substance abuse outcomes (ASI Drugs composite score as dependent variable), ILC × 3 months. dResult of mixed effects regression on substance abuse outcomes (ASI Drugs composite score as dependent variable), ILC × 9 months. eResult of mixed effects regression on substance abuse outcomes (ASI Alcohol composite score as dependent variable), ILC × 3 months. fResult of mixed effects regression on substance abuse outcomes (ASI Alcohol composite score as dependent variable), ILC × 9 months. gResult of mixed effects regression on substance abuse outcomes (Days abstinent in previous 30 days as dependent variable), ILC × 3 months. hResult of mixed effects regression on substance abuse outcomes (Days abstinent in previous 30 days as dependent variable), ILC × 9 months.
Adverse events
Thylstrup 2015 reported the number of participant deaths between the three‐ and nine‐month follow‐up period. There was no significant difference between the ILC intervention and control group (OR 0.40, 95% CI 0.04 to 4.54, P = 0.46, 142 participants, 1 study, very low‐certainty evidence, Analysis 2.3). Thylstrup 2015 also reported on the number of participants incarcerated during the follow‐up period. Again, there was no significant difference between the ILC intervention and control group (OR 0.70, 95% CI 0.27 to 1.86, P = 0.48, 142 participants, 1 study, very low‐certainty evidence, Analysis 2.4).
2.3. Analysis.

Comparison 2: Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 3: Adverse events: death between 3‐month and 9‐month follow‐up
2.4. Analysis.

Comparison 2: Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 4: Adverse events: incarceration during follow‐up period
The study did not report data on our other primary outcomes: reconviction; global state/functioning; and social functioning.
Secondary outcomes
Leaving the study early
Thylstrup 2015 reported the number of participants leaving the study early at three months and at nine months post‐intervention. There was no significant difference between the ILC +TAU intervention group and the TAU control group at both three months (OR 1.54, 95% CI 0.72 to 3.30, P = 0.27, 167 participants, 1 study, very low‐certainty evidence, Analysis 2.5) and nine months (OR 1.38, 95% CI 0.70 to 2.72, P = 0.35, 167 participants, 1 study, very low‐certainty evidence, Analysis 2.6) post‐intervention.
2.5. Analysis.

Comparison 2: Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 5: Leaving the study early: number at 3 months
2.6. Analysis.

Comparison 2: Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone, Outcome 6: Leaving the study early: number at 9 months
Substance misuse
Thylstrup 2015 reported on the percentage of participants using drugs or alcohol daily at three months post‐intervention (ILC intervention + TAU group = 37%; TAU control group = 36%) and at nine months post‐intervention (ILC intervention + TAU group = 31%; TAU control group = 33%). Thylstrup 2015 also reported skewed data (from a mixed‐effects regression analysis) for the drug composite score and alcohol composite score of the ASI (comprising 1) severity ratings (10‐point assessment of lifetime and current problem severity) in seven problem areas affected by substance use disorder by interviewer, and 2) composite scores (range from zero = no problems to one = severe problems) for each domain based on client responses to items measuring behaviour in the 30 days prior to interview. The results for the drug composite score favoured the experimental ILC + TAU condition at three months post‐intervention but not at nine months post‐intervention (Table 23). There was no difference between the groups in terms of alcohol composite scores at three and nine months post‐intervention (Table 23).
Thylstrup 2015 reported the percentage of participants abstinent of drugs or alcohol at three months post‐intervention (ILC intervention + TAU group = 17%; TAU control group = 13%) and at nine months post‐intervention (ILC intervention + TAU group = 21%; TAU control group = 13%). Thylstrup 2015 also reported skewed data (from a mixed‐effects regression analysis) for the number of days abstinent in the previous 30 days, which favoured the experimental ILC + TAU condition at three months post‐intervention, and favoured neither condition at nine months post‐intervention (Table 23).
The trial investigators concluded that "(m)oderate short‐term improvements in substance use were associated with randomization to Impulsive Lifestyle Counselling. The findings support the usefulness of providing psycho‐education to outpatients with antisocial personality disorder" (quote from Abstract, p 1, Thylstrup 2015).
The study did not report data on our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; employment status; housing/accommodation status; economic outcomes; impulsivity; anger; mental state; prison and service outcomes; or other outcomes.
Comparison 3: contingency management + standard maintenance versus standard maintenance alone
We included two studies in this comparison: Neufeld 2008 (outpatients with AsPD and opioid dependence; six months treatment; n = 100); and Messina 2003 (outpatients with cocaine dependence; AsPD subgroup; 16 weeks treatment; n = 26). See Table 3.
Primary outcomes: social functioning
Neufeld 2008 found a significant difference between the groups at six months post‐intervention in (adjusted) composite family/social domain scores, assessed with the Addiction Severity Index (ASI; severity ratings (10‐point assessment of lifetime and current problem severity) in seven problem areas affected by substance use disorder by interviewer; and composite scores (range from zero = no problems to one = severe problems) for each domain (based on client responses to items measuring behaviour in the 30 days prior to interview)), which favoured the treatment condition (MD −0.08 points, 95% CI −0.14 to −0.02, P = 0.005, 83 participants, 1 study, low‐certainty evidence, Analysis 3.1). This analysis is based on summary data of completers supplied by the trial investigators and derived from a mixed regression model that included time‐specific random effects and an interaction term (see Table 4).
3.1. Analysis.

Comparison 3: Contingency management + standard maintenance versus standard maintenance alone, Outcome 1: Social functioning: mean family/social domain scores (high = poor); ASI; at 6 months
The study did not report data on our other primary outcomes: aggression; reconviction; global state/functioning; or adverse events.
Secondary outcomes
Leaving the study early
Both Neufeld 2008 and Messina 2003 reported data on leaving the study early. A meta‐analysis of data from these two studies indicated no significant difference between the treatment and control conditions (OR 0.59, 95% CI 0.28 to 1.24, P = 0.16, I2 = 0%, P value for heterogeneity = 0.69, 127 participants, 2 studies, low‐certainty evidence, Analysis 3.2).
3.2. Analysis.

Comparison 3: Contingency management + standard maintenance versus standard maintenance alone, Outcome 2: Leaving the study early
Substance misuse
Drugs
Messina 2003 found significant differences between the groups in numbers of patients with cocaine‐negative specimens by week 17 (OR 8.56, 95% CI 1.33 to 54.95, P = 0.02, 24 participants, 1 study, low‐certainty evidence, Analysis 3.3), week 26 (OR 11.67, 95% CI 1.53 to 89.12, P = 0.02, 22 participants, 1 study, low‐certainty evidence, Analysis 3.4), and week 52 (OR 10.00, 95% CI 1.44 to 69.26, P = 0.02, 24 participants, 1 study, low‐certainty evidence, Analysis 3.5), in favour of the treatment condition in each case. Messina 2003 also reported skewed summary data (see Table 24), which indicated a significant, greater mean number of cocaine‐negative specimens for the treatment condition compared to the control condition, by 16 weeks (P < 0.05; two‐way analysis of variance (ANOVA) with Tukey‐Kramer post hoc test; analysis of completers by the trial investigators).
3.3. Analysis.

Comparison 3: Contingency management + standard maintenance versus standard maintenance alone, Outcome 3: Substance misuse (drugs): numbers with cocaine‐negative specimens; at 17 weeks
3.4. Analysis.

Comparison 3: Contingency management + standard maintenance versus standard maintenance alone, Outcome 4: Substance misuse (drugs): numbers with cocaine‐negative specimens; at 26 weeks
3.5. Analysis.

Comparison 3: Contingency management + standard maintenance versus standard maintenance alone, Outcome 5: Substance misuse (drugs): numbers with cocaine‐negative specimens; at 52 weeks
14. Comparison 3. Contingency management (CM) + standard maintenance (SM) versus SM alone: cocaine abstinence (skewed data).
| Study | Outcome | Experimental group: CM + SM | Control group: SM | Statistic | Comments | ||||
| n | Mean | SD | n | Mean | SD | ||||
| Messina 2003 | Number cocaine‐negative specimens; by 16 weeksa | 15 | 39.4 | 11.4 | 12 | 9.3 | 11.3 | P < 0.05 (Two‐way ANOVA; Tukey‐Kramer post hoc test; no further details) | Favours experimental group: CM + SM |
| ANOVA: analysis of variance; CM: contingency management; n: participant numbers reported as randomised to each condition; SD: standard deviation; SM: standard maintenance. | |||||||||
aOutcome is mean number of cocaine‐negative specimens per participant.
Neufeld 2008 found no significant difference between the groups in (adjusted) mean composite drug domain scores, assessed with the ASI (10‐point assessment of lifetime and current problem severity) in seven problem areas affected by substance use disorder by the interviewer; and composite scores (range from zero = no problems to one = severe problems) for each domain (based on client responses to items measuring behaviour in the 30 days prior to interview), at six months post‐intervention (data presented graphically; hierarchical regression model with variables at one, two, three and six months, including condition, time, time‐by‐condition interaction and polydrug use at baseline; analysis of completers by the trial investigators, see Table 4). Neufeld 2008 also reported summary data (see Table 25; each being an analysis of completers carried out by the trial investigators), which indicated no significant difference between the treatment and control conditions at six months post‐intervention for overall percentage of: opioid‐negative urine specimens (OR 1.31, 95% CI 0.71 to 2.42, P = 0.39); cocaine‐negative urine specimens (OR 1.59, 95% CI 0.86 to 2.96, P = 0.14); sedative‐negative urine specimens (OR 1.82, 95% CI 0.72 to 4.42, P = 0.18); and negative urine specimens for any drug (OR 1.70, 95% CI 0.94 to 3.07, P = 0.08).
15. Comparison 3. Contingency management (CM) + standard maintenance (SM) versus SM alone: percentage drug‐negative specimens.
| Study | Outcome | Experimental group: CM + SM | Control group: SM | Statistic | Comments |
| Neufeld 2008 | Percentage opioid‐negative specimens; at 6 months | 80.5% | 73.7% | OR 1.31 (95% CI 0.71 to 2.42, P = 0.393) | Favours neither group |
| Neufeld 2008 | Percentage cocaine‐negative specimens; at 6 months | 77.3% | 66.7% | OR 1.59 (95% CI 0.86 to 2.96, P = 0.139) | Favours neither group |
| Neufeld 2008 | Percentage sedative‐negative specimens; at 6 months | 96.2% | 90.8% | OR 1.82 (95% CI 0.715 to 4.42, P = 0.184) | Favours neither group |
| Neufeld 2008 | Percentage (any) drug‐negative specimens; at 6 months | 68.7% | 54.2% | OR 1.70 (95% CI 0.94 to 3.07, P = 0.081) | Favours neither group |
| CI: confidence interval;CM: contingency management; OR: odds ratio; SM: standard maintenance. | |||||
Statistics provided by trial investigators; data relate to proportion of specimens that were negative, rather than proportion of participants who provided negative specimens.
Alcohol
Neufeld 2008 found no significant difference between the treatment and control conditions in (adjusted) mean composite alcohol domain scores, assessed with the ASI (10‐point assessment of lifetime and current problem severity) in seven problem areas affected by substance use disorder by the interviewer; and composite scores (range from zero = no problems to one = severe problems) for each domain (based on client responses to items measuring behaviour in the 30 days prior to interview), at six months post‐intervention (data presented graphically; hierarchical regression model with variables at one, two, three and six months, including condition, time, time‐by‐condition interaction and polydrug use at baseline; analysis of completers by the trial investigators, see Table 4).
Employment status
Neufeld 2008 found no significant difference between the treatment and control conditions in (adjusted) mean composite employment domain scores, assessed with the ASI (10‐point assessment of lifetime and current problem severity) in seven problem areas affected by substance use disorder by the interviewer; and composite scores (range from zero = no problems to one = severe problems) for each domain (based on client responses to items measuring behaviour in the 30 days prior to interview), at six months post‐intervention (data presented graphically; hierarchical regression model with variables at one, two, three and six months, including condition, time, time‐by‐condition interaction and polydrug use at baseline; analysis of completers by the trial investigators, see Table 4).
Other outcomes
Neufeld 2008 reported summary data (see Table 26) that indicated a significant difference in the overall number of counselling sessions attended (in relation to the total number of sessions offered) for the active treatment condition compared to the control condition, by six months post‐intervention (OR 4.00, 95% CI 2.39 to 6.70, P < 0.0001, analysis of completers by the trial investigators). The trial investigators concluded that "subjects in the experimental group had significantly better counselling attendance. . . compared to the control group. The experimental intervention increased attendance in subjects with low and high levels of psychopathy and with and without other psychiatric co‐morbidity." (Neufeld 2008, quote from Abstract, p 101).
16. Comparison 3. Contingency management (CM) + standard maintenance (SM) versus SM alone: attendance at counselling sessions.
| Study | Outcome | Experimental group: CM + SM (sessions attended/sessions available) | Control group: SM (sessions attended/sessions available) | Statistic | Comments |
| Neufeld 2008 | Number of counselling sessions attended in proportion to total number of sessions offered by 6 months | 83.2%a (1285/1545) | 53.4%a (897/1679) | OR 4.00, 95% CI 2.39 to 6.70, P < 0.0001; statistics provided by trial investigators | Favours experimental group: CM + SM |
| CI: confidence intervals; CM: contingency management; OR: odds ratio; SM: standard maintenance. | |||||
aThe percentage data relate to the counselling sessions attended, and not to the numbers of participants who attended.
Neufeld 2008 found no significant difference between the treatment and control conditions in the proportion of participants transferred to routine care due to poor or partial treatment response by six months post‐intervention (OR 0.42, 95% CI 0.17 to 1.04, P = 0.06; 100 participants, 1 study, low‐certainty evidence, Analysis 3.6).
3.6. Analysis.

Comparison 3: Contingency management + standard maintenance versus standard maintenance alone, Outcome 6: Other: proportion transferred to routine care due to poor treatment response (high = poor); by 6 months
Neither study reported data on our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; housing/accommodation status; economic outcomes; impulsivity; anger; mental state; or prison and service outcomes.
Comparison 4: 'driving whilst intoxicated' programme + incarceration versus incarceration
We included one study in this comparison: Woodall 2007 (incarcerated drink‐driving offenders with AsPD; 28 days treatment; n = 52). See Table 5.
Primary outcomes: reconviction
Woodall 2007 found no evidence of a difference between treatment and control conditions in reconviction for drink‐driving (Cox regression of re‐arrest rates) over 24 months (hazard ratio 0.56, 95% CI −0.19 to 1.31, P = 0.15, 52 participants, 1 study, very low‐certainty evidence, Analysis 4.1).
4.1. Analysis.

Comparison 4: 'Driving whilst intoxicated' program + incarceration versus incarceration alone, Outcome 1: Reconviction: reconviction for drink‐driving; Cox regression of rearrest rates; at 24 months
The study did not report data on our other primary outcomes: aggression; global state/functioning; social functioning; or adverse events.
Secondary outcomes
Substance misuse ‐ alcohol
Woodall 2007 provided descriptive and graphical summaries (p 983, column 1) of analyses of self‐reported alcohol use assessed using the Form 90 measure (a time‐line follow‐back method to assess drinking over the previous 90 days). These showed a significant difference between the groups (group x AsPD x time interaction) over the 24‐month period for both total standard ethyl‐alcohol consumption units and number of drinking days, in favour of the treatment condition in each case (P < 0.05; omnibus test; repeated measures ANOVA, mixed‐factorial design with Geisser‐Greenhouse adjustment; analysis of completers by the trial investigators). A similar analysis for average blood alcohol content did not indicate significant differences (P = 0.05). Woodall 2007 concluded that "participants randomized to receive the first offender incarceration and treatment [DWI] programme reported greater reductions in alcohol consumption from baseline levels when compared with participants who were only incarcerated. AsPD participants reported heavier and more frequent drinking but showed significantly greater decline in drinking from intake to post‐treatment assessments." (quote from Abstract, p 974).
Other outcomes
Woodall 2007 reported skewed summary data that indicated no significant difference between treatment and control conditions for mean number of days driving after drinking in past 30 days (see Table 27) and for mean number of days driving after five or more drinks in past 30 days (see Table 28) at six, 12 and 24 months post‐incarceration (P values not provided, but not significant for the group‐by‐time interaction; ANOVA mixed‐factorial design; completer analysis by the trial investigators). However, the trial investigators reported a significant overall main effect of time for the whole sample (P < 0.001), "indicating a decline in self‐reported drinking and driving from intake to post‐incarceration assessments" (p 982, column 2), and a "significant AsPD‐by‐time interaction (P < 0.001) resulting from the fact that, contrary to expectations, the AsPD participants showed a greater improvement over time than the non‐AsPD participants on both these self‐reports of drinking and driving." (p 982, column 2).
17. Comparison 4. 'Driving whilst intoxicated program' (DWI) + incarceration versus incarceration alone: days drink driving, self‐reported (skewed data).
| Study | Outcome | Experimental group: DWI + incarceration | Control group: incarceration | Statistic | Comments | ||||
| n | Mean | SD | n | Mean | SD | ||||
| Woodall 2007 | Days driving after drinking in past 30 days; self‐reported; at 6 months | 30 | 0.83 | 3.70 | 13 | 0.69 | 2.50 | None provided | Favours neither group Completer analysisa |
| Woodall 2007 | Days driving after drinking in past 30 days; self‐reported; at 12 months | 30 | 0.63 | 1.69 | 13 | 0.46 | 0.88 | None provided | Favours neither group Completer analysisa |
| Woodall 2007 | Days driving after drinking in past 30 days; self‐reported; at 24 months | 30 | 0.67 | 1.75 | 13 | 0.38 | 0.38 | None provided | Favours neither group Completer analysisa |
| Woodall 2007 | Days driving after drinking in past 30 days; self‐reported; mean improvement over baseline; at 24 months | 30 | 4.26 | 6.32 | 13 | 3.03 | 4.08 | None provided | Favours neither group Completer analysisa |
| ANOVA: analysis of variance; AsPD: antisocial personality disorder; DWI: 'Driving whilst intoxicated program'; n: numbers of participants; SD: standard deviation. | |||||||||
aTrial investigators reported a significant, overall main effect of time (P < 0.001), "indicating a decline in self‐reported drinking and driving from intake to post‐incarceration assessments" (column 2, p 982) and a significant AsPD‐by‐time interaction (P < 0.001) "resulting from the fact that the AsPD participants showed a greater improvement over time than the non‐AsPD participants" (column 2, p 982), but that the group‐by‐time interaction was not significant (ANOVA, mixed factorial design).
18. Comparison 4. 'Driving whilst intoxicated program' (DWI) + incarceration versus incarceration alone: days driving after five or more drinks, self‐reported (skewed data).
| Study | Outcome | Experimental group: DWI + incarceration | Incarceration | Statistic | Comments | ||||
| n | Mean | SD | n | Mean | SD | ||||
| Woodall 2007 | Days driving after 5 or more drinks in past 30 days; self‐reported; at 6 months | 30 | 0.87 | 3.73 | 13 | 0.08 | 0.28 | None provided | Favours neither group Completer analysisa |
| Woodall 2007 | Days driving after 5 or more drinks in past 30 days; self‐reported; at 12 months | 30 | 0.57 | 1.63 | 13 | 0.38 | 0.77 | None provided | Favours neither group Completer analysisa |
| Woodall 2007 | Days driving after 5 or more drinks in past 30 days; self‐reported; at 24 months | 30 | 0.50 | 1.25 | 13 | 0.31 | 0.63 | None provided | Favours neither group Completer analysisa |
| Woodall 2007 | Days driving after 5 or more drinks in past 30 days; self‐reported; mean improvement over baseline; at 24 months | 30 | 3.02 | 4.93 | 13 | 2.28 | 4.22 | None provided | Favours neither group Completer analysisa |
| ANOVA: analysis of variance; AsPD: antisocial personality disorder; DWI: 'Driving whilst intoxicated program';n: numbers of participants; SD: standard deviation. | |||||||||
aTrial investigators reported a significant overall main effect of time (P < 0.001), "indicating a decline in self‐reported drinking and driving from intake to post‐incarceration assessments" (column 2, p 982) and a significant AsPD‐by‐time interaction (P < 0.001) "resulting from the fact that the AsPD participants showed a greater improvement over time than the non‐AsPD participants" (column 2, p 982), but that the group‐by‐time interaction was not significant (ANOVA, mixed factorial design).
The study did not report data on our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; leaving the study early; employment status; housing/accommodation status; economic outcomes; impulsivity; anger; mental state; or prison and service outcomes.
Comparison 5: schema therapy versus treatment‐as‐usual
We included one study in this comparison: Bernstein 2012 (male forensic patients with personality disorder; 26 of the 30 completers (87%) had a diagnosis of AsPD; we included the total sample data in the analyses as the proportion of AsPD was greater than 75%). See Table 6.
Bernstein 2012 reported preliminary results only and outcome data for the following 'mental state' variables were not provided: personality disorder symptoms (assessed with Structured Interview for DSM‐IV Personality Disorders (SIDP‐IV)); scores on patient version of the Schedule for Nonadaptive and Adaptive Personality (SNAP); scores on the informant version of the Schedule for Nonadaptive and Adaptive Personality (SNAP‐I): early maladaptive schemas and schema modes (assessed with the Young Schema Questionnaire‐Short Version (YSQ) and Schema Mode Inventory (SMI)); and general psychopathology (assessed with the Symptom‐Checklist 90 (SCL‐90)) .
Primary outcomes
Reconviction
Bernstein 2012 reported data on the number of participants reconvicted at three years. They found no difference between the groups for this outcome (OR 2.81, 95% CI 0.11 to 74.56, P = 0.54, 30 participants (87% AsPD diagnosis), 1 study, very low‐certainty evidence, Analysis 5.1).
5.1. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 1: Recidivism: number of participants to recidivate, documented as a global negative outcome
Social functioning
Bernstein 2012 reported data on the number of patients obtaining supervised and unsupervised leave at two and three years follow‐up, and found no differences between the groups:
supervised leave at two years (OR 3.00, 95% CI 0.68 to 13.31, P = 0.15, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence; Analysis 5.2);
unsupervised leave at two years (OR 5.91, 95% CI 0.60 to 58.48, P = 0.13, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence; Analysis 5.3);
supervised leave at three years follow‐up (OR 1.18, 95% CI 0.20 to 7.08, P = 0.85, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence; Analysis 5.4); and
unsupervised leave at three years follow‐up (OR 1.25, 95% CI 0.29 to 5.41, P = 0.77, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence; Analysis 5.5).
5.2. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 2: Social functioning: number of patients with supervised leave at 2 years
5.3. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 3: Social functioning: number of patients with unsupervised leave at 2 years
5.4. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 4: Social functioning: number of patients with supervised leave at 3 years
5.5. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 5: Social functioning: number of patients with unsupervised leave at 3 years
Bernstein 2012 reported skewed data for the mean number of days for patients to gain supervised leave and found no difference between the groups (Table 29; study investigators reported t‐test (degrees of freedom (df) = 22) = 1.07, P > 0.05). Bernstein 2012 also reported the mean number of days for patients to gain unsupervised leave and found a difference between the groups in favour of the treatment condition (OR −137.33, 95% CI −271.31 to −3.35, P = 0.04, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence, Analysis 5.6). We chose to report this last result as the measure of social functioning in Table 6, as 'days to unescorted leave' reflects the person gaining a higher level of independence and progress than 'days to escorted leave'.
19. Comparison 5. Schema therapy (ST) versus treatment‐as‐usual (TAU): continuous data; number of days to supervised leave (skewed data).
| Study | Outcome | Experimental group: ST | Control group: TAU | Statistic | Comments | ||||
| n | Mean | SD | n | Mean | SD | ||||
| Bernstein 2012 | Social functioning: mean number of days to supervised leave | 16 | 424.38 | 309.65 | 14 | 564.91 | 317.55 | Study author‐reported t‐test (df = 22), 1.07, P > 0.05 | Favours neither group |
| df: degrees of freedom; n: numbers of participants; SD: standard deviation; ST: Schema Therapy; TAU: treatment as usual. | |||||||||
5.6. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 6: Social functioning: mean number of days to unsupervised leave
Bernstein 2012 concluded that "(t)he observation that ST patients moved through the resocialization process more rapidly than the TAU patients, receiving leave on average about 4.5 months faster for both unsupervised and supervised leave, raises the possibility that it may be a cost‐effective form of treatment" (quote from Discussion, p 321, column 1).
Adverse events
Bernstein 2012 classified adverse events, such as dropping out of therapy, recidivism or being transferred to another facility due to poor treatment response as global negative outcomes. They reported data on the number of participants with global negative outcomes overall and found no difference between the groups (OR 0.42, 95% CI 0.08 to 2.19, P = 0.30, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence Analysis 5.7).
5.7. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 7: Adverse events: global negative outcomes overall
The study did not report data on our other primary outcomes: aggression; or global state/functioning.
Secondary outcomes: other outcomes
Bernstein 2012 reported the recidivism risk score on the Historical Clinical Risk Management‐20. There was no difference between the groups in a repeated‐measures ANOVA (interaction of treatment by time (linear effect): F (1, 20) = 0.12, P = 0.73; interaction of treatment by time (curvilinear effect): F (1, 20) = 3.24, P = 0.09).
In addition to the number of patients who recidivated (Analysis 5.1), Bernstein 2012 provided four additional reasons that would lead to a patient receiving a global negative outcome. They found no difference between the groups for any of these four reasons:
number of patients transferred to other clinics due to lack of treatment response (OR 0.40, 95% CI 0.03 to 4.96, P = 0.48, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence, Analysis 5.8);
number of patients terminating therapy due to worsening of psychiatric condition (OR 0.27, 95% CI 0.01 to 7.25, P = 0.44, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence, Analysis 5.9);
number of patients that terminated therapy due to lack of treatment response (OR 0.27, 95% CI 0.01 to 7.25, P = 0.44, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence, Analysis 5.10); and
number of patients terminated due to lack of co‐operation with the research (OR 0.87, 95% CI 0.05 to 15.28, P = 0.92, 30 participants (87% ASPD diagnosis), 1 study, very low‐certainty evidence, Analysis 5.11).
5.8. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 8: Adverse events: number of patients transferred to other clinics due to lack of treatment response
5.9. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 9: Adverse events: number of patients terminating therapy due to worsening of psychiatric condition
5.10. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 10: Adverse events: number of patients that terminate therapy due to lack of treatment response
5.11. Analysis.

Comparison 5: Schema therapy versus treatment‐as‐usual, Outcome 11: Adverse events: number of patients terminated due to lack of co‐operation with the research
The study did not report data on our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; leaving the study early; substance misuse; employment status; housing/accommodation status; economic outcomes; impulsivity; anger; mental state; or prison and service outcomes.
Comparison 6: social problem‐solving therapy + psychoeducation versus treatment‐as‐usual alone
We included one study in this comparison: Huband 2007 (community‐living adults with personality disorder; AsPD subgroup; 24 weeks treatment; n = 24). The authors of Huband 2007 were able to provide data on the AsPD subgroup, however the investigators noted that their trial was not designed to have sufficient power to detect significant changes in subgroups of this size, and also that 20 of the 24 had at least one other Axis II diagnosis. See Table 7.
Primary outcomes: social functioning
Huband 2007 found no clear difference between the treatment and control conditions in mean scores on the SFQ (eight items, rated on a four‐point scale (anchors vary across items) by responders who indicated the extent to which they experienced problems over the past two weeks, scores range from 0 to 24; higher scores indicate greater social dysfunction) at six months post‐intervention (MD −1.60 points, 95% CI −5.43 to 2.23, P = 0.41, 17 participants, 1 study, very low‐certainty evidence, Analysis 6.1).
6.1. Analysis.

Comparison 6: Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual alone, Outcome 1: Social functioning: mean social functioning scores (high = poor); SFQ; at 6 months
The study did not report data on our other primary outcomes: aggression; reconviction; global state/functioning; or adverse events.
Secondary outcomes
Leaving the study early
Huband 2007 found no significant difference between treatment and control conditions for the outcome 'leaving the study early' (OR 1.19, 95% CI 0.20 to 6.99, P = 0.85, 24 participants, 1 study, very low‐certainty evidence, Analysis 6.2).
6.2. Analysis.

Comparison 6: Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual alone, Outcome 2: Leaving the study early
Impulsivity
Huband 2007 found no significant difference between treatment and control conditions in mean scores on the Barrett Impulsiveness Scale (BIS; 30 items scored on a four‐point Likert scale ranging from one (rarely or never) to four (almost always/always); higher scores indicate greater impulsivity) at six months post‐intervention (MD 6.58 points, 95% CI −4.81 to 17.97, P = 0.26, 14 participants, 1 study, very low‐certainty evidence, Analysis 6.3).
6.3. Analysis.

Comparison 6: Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual alone, Outcome 3: Impulsivity: mean impulsiveness scores (high = poor); BIS; at 6 months
Anger
Huband 2007 found no significant difference between treatment and control conditions in mean scores on the Anger Expression Index (overall measure of total anger expression, calculated by subtracting the summed scores on the 16‐item anger control scale from the summed scores on the 16‐item anger expression scale (both scales rated on four‐point Likert scale from one (not at all/almost never) to four (very much so/almost always)) and adding 48 to eliminate the possible of negative numbers; higher scores indicate greater levels of overall anger expression) of the State‐Trait Anger Expression Inventory‐2 (STAXI‐2) at six months follow‐up (MD −1.74 points, 95% CI −12.64 to 9.16, P = 0.75, 14 participants, 1 study, very low‐certainty evidence, Analysis 6.4).
6.4. Analysis.

Comparison 6: Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual alone, Outcome 4: Anger: mean Anger Expression Index scores (high = poor); STAXI‐2; at 6 months
Other outcomes
Huband 2007 found no significant differences between the treatment and control conditions at six months follow‐up in mean social problem‐solving ability scores on the Social Problem Solving Inventory‐Revised (SPSI‐R; 5 subscales; total scores range 0 to 20 with higher scores indicating greater problem‐solving ability) (MD 0.18 points, 95% CI −2.57 to 2.93, P = 0.90, 16 participants, 1 study, very low‐certainty evidence, Analysis 6.5), mean shame scores on the Experience of Shame Scale (25‐item questionnaire assessing characterological shame and behavioural shame over the past year, each item scored on a four‐point scale ranging from one (not at all) to four (very much), yielding a total score between 25 and 100; higher scores indicate greater shame) (MD 14.64 points, 95% CI −12.70 to 41.98, P = 0.29, 14 participants, 1 study, very low‐certainty evidence, Analysis 6.6), and mean dissociation scores on the Dissociative Experiences Scale (28‐item questionnaire asking about percentage of time (range = 0% to 100%) that a particular symptom is experienced, overall score = average of all individual scores; scores of 20 or more consistent with post‐traumatic or dissociative disorders) (MD 4.30 %, 95% CI −21.19 to 29.79, P = 0.74, 13 participants, 1 study, very low‐certainty evidence, Analysis 6.7).
6.5. Analysis.

Comparison 6: Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual alone, Outcome 5: Other: social problem‐solving ability; mean overall scores (high = good); SPSI; at 6 months
6.6. Analysis.

Comparison 6: Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual alone, Outcome 6: Other: shame; mean overall shame scores (high = poor); ESS; at 6 months
6.7. Analysis.

Comparison 6: Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual alone, Outcome 7: Other: dissociation; mean dissociation scores (high = poor); DES: at 6 months
The study did not report data on any of our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; substance misuse; employment status; housing/accommodation status; economic outcomes; mental state; or prison and service outcomes.
Comparison 7: dialectical behaviour therapy versus treatment‐as‐usual
We included two studies in this comparison: Asmand 2015 (adult male prisoners in Iran with AsPD; n = 32); and Priebe 2012 (mixed gender community outpatients with personality disorder; n = 14; AsPD subgroup data available). The description of the DBT intervention provided by Asmand 2015 was very poor, and for participants in the control condition of this study, TAU was standard incarceration rather than the psychiatric outpatient treatment offered in Priebe 2012. See Table 8.
Primary outcomes: adverse events
Priebe 2012 reported skewed data for the mean number of self‐harm days in the past two months for five AsPD participants in the intervention group and nine AsPD participants in the control condition (Table 9; data provided by the study authors; baseline data, data at month two and change between these is shown in the table; no statistics were provided by the study authors for this extracted data). Priebe 2012 concluded that "DBT can be effective in reducing self‐harm in patients with personality disorder, possibly incurring higher total treatment costs. The effect is stronger in those who complete treatment" (quote from Abstract, p 356).
The study did not report data for any of the other primary outcomes: aggression; reconviction; global state/functioning; or social functioning.
Secondary outcomes
Mental state
Priebe 2012 reported total scores on the Brief Psychiatric Rating Scale (BPRS; 24 items rated by an observer, total scores ranging from 24 to 168) at two months follow‐up. There was a difference between the groups in mean BPRS total scores, in favour of the treatment condition (MD −15.32 points, 95% CI −27.55 to −3.09, P = 0.01, 11 participants, 1 study, very low‐certainty evidence, Analysis 7.1).
7.1. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 1: Mental state: score on Brief Psychiatric Rating Scale (BPRS) (total sum), at month 2
Asmand 2015 reported data on changes in anxiety, measured by the Beck Anxiety and Depression Scale (BADS; 21 items rated on four‐point scale, ranging from zero (never) to three (I can't stand it), overall score range = 0 to 63; higher scores indicate more severe anxiety symptoms). There was no difference between the groups in mean BADS total scores at follow‐up (MD −0.50 points, 95% CI −10.35 to 9.35, P = 0.92, 32 participants, 1 study, very low‐certainty evidence, Analysis 7.2).
7.2. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 2: Mental state: anxiety on Beck Anxiety and Depression Scale (BADS)
Other outcomes
Asmand 2015 (32 participants, 1 study, very low‐certainty evidence) reported the results of comparisons between the treatment and control conditions on 10 subscales of the Jones' Illogical Beliefs Questionnaire [(sic), query Irrational Beliefs Test (Jones 1969)]. This is a 100‐item questionnaire, comprising 10 subscales, each with 10 questions rated on a five‐point Likert scale ranging from one (quite disagree) to five (quite agree); subscale scores are summed to give a total score, and the higher the score the more severe the illogical belief. Using the 10 subscale names reported by Asmand 2015, the results favoured neither condition and were as follows:
need for high degree of confirmation (MD −0.22 points, 95% CI −6.06 to 3.62, P = 0.62, 32 participants, 1 study, very low‐certainty evidence Analysis 7.3);
high expectations of self (MD −1.31 points, 95% CI −5.16 to 2.54, P = 0.50, 32 participants, 1 study, very low‐certainty evidence, Analysis 7.4);
tend to blame (MD 0.25 points, 95% CI −4.20 to 4.70, P = 0.91, 32 participants, 1 study, very low‐certainty evidence, Analysis 7.5);
reaction to failure (MD 0.44 points, 95% CI −3.04 to 3.92, P = 0.80, 32 participants, 1 study, very low‐certainty evidence, Analysis 7.6);
emotional irresponsibility (MD −3.44 points, 95% CI −7.04 to 0.16, P = 0.06, 32 participants, 1 study, very low‐certainty evidence, Analysis 7.7);
anxiety and stress (MD −1.44 points, 95% CI −3.75 to 0.87, P = 0.22, 32 participants, 1 study, very low‐certainty evidence, Analysis 7.8);
avoidance of exposition to the pitfalls (MD −3.31 points, 95% CI −7.15 to 0.53, P = 0.09, 32 participants, 1 study, very low‐certainty evidence, Analysis 7.9);
dependence (MD 0.31 points, 95% CI −2.79 to 3.41, P = 0.84, 32 participants, 1 study, very low‐certainty evidence, Analysis 7.10);
helplessness to changes (MD −1.87 points, 95% CI −5.21 to 1.47, P = 0.27, 32 participants, 1 study, very low‐certainty evidence, Analysis 7.11); and
perfectionism (MD −0.25 points, 95% CI −4.10 to 3.60, P = 0.90, 32 participants, 1 study, very low‐certainty evidence Analysis 7.12).
7.3. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 3: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test] 'High degree of confirmation' subscale
7.4. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 4: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'High expectations of self' subscale
7.5. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 5: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Tend to blame' subscale
7.6. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 6: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Reaction to failure' subscale
7.7. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 7: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Emotional irresponsibility' subscale
7.8. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 8: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Anxiety and stress' subscale
7.9. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 9: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Avoidance of exposition to the pitfalls' subscale
7.10. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 10: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Dependence' subscale
7.11. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 11: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; ' Helplessness to changes ' subscale
7.12. Analysis.

Comparison 7: Dialectical behaviour therapy versus treatment‐as‐usual, Outcome 12: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Perfectionism' subscale
None of the studies provided data on our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; leaving the study early; substance misuse; employment status; housing/accommodation status; economic outcomes; impulsivity; anger; or prison and service outcomes.
Comparison 8: cognitive behavioural therapy + standard maintenance versus standard maintenance alone
We included one study in this comparison: Messina 2003 (outpatients with cocaine dependence; AsPD subgroup; 16 weeks treatment; n = 27).
Primary outcomes
Messina 2003 did not report data on our primary outcomes: aggression; reconviction; global state/functioning; social functioning; or adverse events.
Secondary outcomes
Leaving the study early
Messina 2003 found no difference between treatment and control conditions for the outcome of 'leaving the study early' (OR 0.38, 95% CI 0.03 to 4.87, P = 0.46, 26 participants, 1 study, very low‐certainty evidence, Analysis 8.1).
8.1. Analysis.

Comparison 8: Cognitive behavioural therapy + standard maintenance versus standard maintenance alone, Outcome 1: Leaving the study early
Substance misuse ‐ drugs
Messina 2003 found no significant difference between treatment and control conditions in numbers of participants with cocaine‐negative specimens by week 17 (OR 2.72, 95% CI 0.48 to 15.47, P = 0.26; 23 participants, 1 study, very low‐certainty evidence; Analysis 8.2), or by week 26 (OR 5.60, 95% CI 0.81 to 38.51, P = 0.08, 22 participants, 1 study, very low‐certainty evidence, Analysis 8.3). However, Messina 2003 did find a significant difference between treatment and control conditions in numbers of participants with cocaine‐negative specimens by week 52, in favour of the treatment condition (OR 8.00, 95% CI 1.13 to 56.79, P = 0.04, 22 participants, 1 study, very low‐certainty evidence, Analysis 8.4). Messina 2003 also reported skewed summary data (see Table 30) that indicated a significant difference in mean number of cocaine‐negative specimens in the groups by 16 weeks (P < 0.05, two‐way ANOVA with Tukey‐Kramer post hoc test, analysis of completers by the trial investigators), again in favour of the treatment condition.
8.2. Analysis.

Comparison 8: Cognitive behavioural therapy + standard maintenance versus standard maintenance alone, Outcome 2: Substance misuse (drugs): numbers with cocaine‐negative specimens; at 17 weeks
8.3. Analysis.

Comparison 8: Cognitive behavioural therapy + standard maintenance versus standard maintenance alone, Outcome 3: Substance misuse (drugs): numbers with cocaine‐negative specimens; at 26 weeks
8.4. Analysis.

Comparison 8: Cognitive behavioural therapy + standard maintenance versus standard maintenance alone, Outcome 4: Substance misuse (drugs): numbers with cocaine‐negative specimens; at 52 weeks
21. Comparison 8. Cognitive behavioural therapy (CBT) + standard maintenance (SM) versus SM: cocaine abstinence (skewed data).
| Study | Outcome | Experimental group: CBT + SM | Control group: SM | Statistic | Comments | ||||
| n | Mean | SD | n | Mean | SD | ||||
| Messina 2003 | Number cocaine‐negative specimens; by 16 weeksa | 14 | 24.8 | 15.6 | 12 | 9.3 | 11.3 | P < 0.05 (Two‐way ANOVA; Tukey‐Kramer post‐hoc test) | Favours experimental group: CBT + SM |
| ANOVA: analysis of variance; CBT: cognitive behavioural therapy; n: numbers reported as randomised to each condition; SD: standard deviation; SM: standard maintenance. | |||||||||
aOutcome is mean number of cocaine‐negative specimens per participant.
Messina 2003 did not report data on any of our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; employment status; housing/accommodation status; economic outcomes; impulsivity; anger; mental state; or prison and service outcomes.
Comparison 9: contingency management + cognitive behavioural therapy + standard maintenance versus standard maintenance alone
We included one study in this comparison: Messina 2003 (outpatients with cocaine dependence; AsPD subgroup; 16 weeks treatment; n = 19).
Primary outcomes
The study did not report data on any of our primary outcomes: aggression; reconviction; global state/functioning; social functioning; or adverse events.
Secondary outcomes
Leaving the study early
Messina 2003 found no significant difference between the treatment and control conditions for the outcome 'leaving the study early' (OR 0.28, 95% CI 0.01 to 6.72, P = 0.43, 19 participants, 1 study, very low‐certainty evidence, Analysis 9.1).
9.1. Analysis.

Comparison 9: Contingency management + cognitive behavioural therapy + standard maintenance versus standard maintenance alone, Outcome 1: Leaving the study early
Substance misuse ‐ drugs
Messina 2003 found no significant difference between the treatment and control conditions in numbers with cocaine‐negative specimens by week 17 (OR 3.11, 95% CI 0.41 to 23.39, P = 0.27, 17 participants, 1 study, very low‐certainty evidence, Analysis 9.2) or by week 26 (OR 7.00, 95% CI 0.69 to 70.74, P = 0.10, 15 participants, 1 study, very low‐certainty evidence, Analysis 9.3). However, Messina 2003 did find a significant difference between the groups in numbers with cocaine‐negative specimens by week 52, in favour of the treatment condition (OR 16.00, 95% CI 1.09 to 234.25, P = 0.04, 15 participants, 1 study, very low‐certainty evidence, Analysis 9.4). Messina 2003 also reported skewed summary data (see Table 31) that indicated a difference in mean number of cocaine‐negative specimens between the groups by 16 weeks, again in favour of the treatment condition (P < 0.05, two‐way ANOVA with Tukey‐Kramer post hoc test, completer analysis by the trial investigators).
9.2. Analysis.

Comparison 9: Contingency management + cognitive behavioural therapy + standard maintenance versus standard maintenance alone, Outcome 2: Substance misuse (drugs): numbers with cocaine‐negative specimens; at 17 weeks
9.3. Analysis.

Comparison 9: Contingency management + cognitive behavioural therapy + standard maintenance versus standard maintenance alone, Outcome 3: Substance misuse (drugs): numbers with cocaine‐negative specimens; at 26 weeks
9.4. Analysis.

Comparison 9: Contingency management + cognitive behavioural therapy + standard maintenance versus standard maintenance alone, Outcome 4: Substance misuse (drugs): numbers with cocaine‐negative specimens; at 52 weeks
22. Comparison 9. Contingency management (CM) + cognitive behavioural therapy (CBT) + standard maintenance (SM) versus SM: cocaine abstinence (skewed data).
| Study | Outcome | Experimental group: CM + CBT + SM | Control group: SM | Statistic | Comments | ||||
| n | Mean | SD | n | Mean | SD | ||||
| Messina 2003 | Number cocaine‐negative specimens; by 16 weeksa | 7 | 37.7 | 13.3 | 12 | 9.3 | 11.3 | P < 0.05 (Two‐way ANOVA; Tukey‐Kramer post‐hoc test) | Favours experimental group: CM + CBT + SM |
| ANOVA: analysis of variance; CBT: cognitive behavioural therapy; CM: contingency management; n: numbers reported as randomised to each condition; SD: standard deviation; SM: standard maintenance. | |||||||||
aOutcome is mean number of cocaine‐negative specimens per participant.
The study did not report data on any of our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; employment status; housing/accommodation status; economic outcomes; impulsivity; anger; mental state; or prison and service outcomes; or other outcomes.
Comparison 10: rational emotive behaviour therapy (REBT) versus treatment‐as‐usual
We included one study in this comparison: Asmand 2015 (adult male prisoners in Iran with AsPD; n = 32). The description of the REBT intervention provided by Asmand 2015 was very poor.
Primary outcomes
The study did not report data on any of our primary outcomes: aggression; reconviction; global state/functioning; social functioning; or adverse events.
Secondary outcomes
Mental state
Asmand 2015 reported data on changes in anxiety, measured by the Beck Anxiety Depression Scale (BADS; 21 questions, rated on a four‐point scale, ranging from zero (never) to three (I can't stand it); overall score range = 0 to 63; higher scores indicate more severe anxiety symptoms). There was no difference between REBT treatment and control conditions at follow‐up in mean BADS total scores (MD −4.00 points, 95% CI −12.34 to 4.34, P = 0.35, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.1).
10.1. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 1: Mental state: anxiety score on Beck Anxiety and Depression Scale
Other outcomes
Asmand 2015 reported differences between the groups in four of the 10 subscales of the Jones' Illogical Beliefs Questionnaire [(sic), query Irrational Beliefs Test (Jones 1969)]. This is a 100‐item questionnaire, comprising 10 subscales, each with 10 questions rated on a five‐point Likert scale ranging from one (quite disagree) to five (quite agree); subscale scores are summed to give a total score and the higher the score, the more severe the illogical belief. Using the subscale names reported by Asmand 2015, the results were as follows:
high degree of confirmation (MD −4.47 points, 95% CI −10.06 to 1.12, P = 0.12, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.2, favours neither condition);
high expectations of self (MD −5.31 points, 95% CI −9.86 to −0.76, P = 0.02, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.3, favours intervention condition);
tend to blame (MD −2.12 points, 95% CI −7.17 to 2.93, P = 0.41, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.4, favours neither condition);
reaction to failure (MD −4.13 points, 95% CI −8.78 to −0.52, P = 0.08, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.5, favours neither condition);
emotional irresponsibility (MD −6.25 points, 95% CI −10.35 to −2.15, P = 0.003, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.6, favours the intervention condition);
anxiety and stress (MD −2.69 points, 95% CI −6.03 to 0.65, P = 0.11, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.7, favours neither condition);
avoidance of exposition to the pitfalls (MD −4.31 points, 95% CI −8.85 to 0.23, P = 0.06, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.8, favours neither condition);
dependence (MD −1.94 points, 95% CI −5.94 to 2.06, P = 0.34, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.9, favours neither condition).
helplessness to changes (MD −5.62 points, 95% CI −9.78 to −1.46, P = 0.008, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.10, favours the intervention condition); and
perfectionism (MD −5.07 points, 95% CI −9.51 to −0.63, P = 0.03, 32 participants, 1 study, very low‐certainty evidence, Analysis 10.11 , favours the intervention condition).
10.2. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 2: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'High degree of confirmation' subscale
10.3. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 3: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'High expectations of self' subscale
10.4. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 4: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Tend to blame' subscale
10.5. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 5: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Reaction to failure' subscale
10.6. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 6: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Emotional irresponsibility' subscale
10.7. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 7: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Anxiety and stress' subscale
10.8. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 8: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Avoidance of exposition to the pitfalls' subscale
10.9. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 9: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Dependence' subscale
10.10. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 10: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; ' Helplessness to changes ' subscale
10.11. Analysis.

Comparison 10: Rational emotive behaviour therapy versus treatment‐as‐usual, Outcome 11: Other: Jones' Illogical Beliefs Questionnaire (sic), [Irrational Beliefs Test]; 'Perfectionism' subscale
The study did not provide data on any of our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; employment status; housing/accommodation status; economic outcomes; impulsivity; anger; or prison and service outcomes.
Comparison 11: psychosocial risk management ('Resettle programme') versus treatment‐as‐usual
We included one study in this comparison: Nathan 2019 (adult male prisoners in UK; AsPD; n = 65; whole sample data included (n = 72) as over 90% of participants had AsPD diagnosis).
Primary outcomes
Recidivism
Nathan 2019 provided raw study data that allowed us to extract summary statistics (skewed data) for the total number of official offences recorded after release from prison (Table 11). These showed there were no differences between total number of offences recorded in the first year (35 participants) and second year (non‐cumulative; 16 participants) after release from prison (Table 11).
Nathan 2019 reported the results of an intention‐to‐treat regression analysis to predict the total offences committed in the two years following release, which favoured the control condition (OR 1.188, 95% CI −0.042 to 2.334, P = 0.042, 72 participants (90% AsPD), 1 study, very low‐certainty evidence; Analysis 11.1); however, this effect disappeared when the analysis was corrected for time in the community (OR 1.204, 95% CI −0.014 to 2.423, P 0 = 0.053, 72 participants (90% AsPD), 1 study, very low‐certainty evidence; Analysis 11.2). The study authors noted that "one offender in the intent‐to‐treat group had nine offences and that was the maximum score in the entire cohort" (p 6, column 2). Nathan 2019 also reported the results of an intention‐to‐treat analysis (72 participants, 90% AsPD) to predict the binary outcome (no offences versus 1 or more offences) for official offences at two years post‐release, which favoured the PSRM Resettle intervention (OR 2.371, 95% CI 0.464 to 4.278, P = 0.015, 72 participants (90% AsPD), 1 study, very low‐certainty evidence, Analysis 11.3); however, this effect disappeared when the analysis was corrected for time in the community (OR 2.077, 95% CI −0.188 to 4.201, P = 0.073, 72 participants (90% AsPD), 1 study, very low‐certainty evidence, Analysis 11.4). The study authors noted that "there was about a 2 times higher odds that offenders (including the intent‐to‐treat offenders) in the Resettle programme had no offending (rather than any level of offending) in the two year follow‐up period than offenders in the control group" (p 6, column 2).
11.1. Analysis.
Comparison 11: Psychosocial risk management ('Resettle programme') versus treatment‐as‐usual, Outcome 1: Recidivism: total official offences at 2 years post‐release
| Recidivism: total official offences at 2 years post‐release | |||||
| Study | Estimate | SE | 95% CI | p | Comments |
| Nathan 2019 | 1.188 | 0.585 | ‐0.042 to 2.334 | 0.042 | Statistical prediction of the number of Poisson‐distributed official offences by the ITT Resettle group versus the control group, provided by study investigators (n = 72, 90% AsPD). |
11.2. Analysis.
Comparison 11: Psychosocial risk management ('Resettle programme') versus treatment‐as‐usual, Outcome 2: Recidivism: total official offences at 2 years, corrected for time in the community
| Recidivism: total official offences at 2 years, corrected for time in the community | |||||
| Study | Estimate | SE | 95% CI | p | Comments |
| Nathan 2019 | 1.204 | 0.621 | ‐0.014 to 2.423 | 0.053 | Statistical prediction of the number of Poisson‐distributed official offences by the ITT Resettle group versus the control group, provided by study investigators (n = 72, 90% AsPD) |
11.3. Analysis.
Comparison 11: Psychosocial risk management ('Resettle programme') versus treatment‐as‐usual, Outcome 3: Recidivism: binary outcome (no offences vs 1 or more offences) for official offences at 2 years post release
| Recidivism: binary outcome (no offences vs 1 or more offences) for official offences at 2 years post release | |||||
| Study | Estimate | SE | 95% CI | p | Comments |
| Nathan 2019 | 2.371 | 0.973 | 0.464 to 4.278 | 0.015 | Statistical prediction of the zero‐inflation binary factor (no offence vs. 1 or more offences) reported by ITT Resettle group versus the control, reported by the study investigators (n = 72, 90% AsPD). The study authors stated ( p 5, col 1) "When conducting zero‐inflated regression models, Mplus creates a continuous outcome measure as well as a latent binary outcome measure, since zero‐inflated measures benefit from examining whether participants who score zero versus any other value other than zero might differ in relation to the independent variables. Positive values on the binary outcome are interpreted to mean that lower values are related to greater chance of the dependent variable assuming zero values. Negative values on the binary outcome are interpreted to mean that higher values (using categorical contrast coding) on the independent variable are related to more non‐zero values on the dependent variable." |
11.4. Analysis.
Comparison 11: Psychosocial risk management ('Resettle programme') versus treatment‐as‐usual, Outcome 4: Recidivism: binary outcome (no offences vs 1 or more offences) for official offences at 2 years post release, corrected for time in the community
| Recidivism: binary outcome (no offences vs 1 or more offences) for official offences at 2 years post release, corrected for time in the community | |||||
| Study | Estimate | SE | 95% CI | p | Comments |
| Nathan 2019 | 2.077 | 1.12 | ‐0.188 to 4.201 | 0.073 | Statistical prediction of the zero‐inflation binary factor (no offence vs. 1 or more offences) reported by ITT Resettle group versus the control, reported by the study investigators (n = 72, 90% AsPD). The study authors stated (p 5, col 1) "When conducting zero‐inflated regression models, Mplus creates a continuous outcome measure as well as a latent binary outcome measure, since zero‐inflated measures benefit from examining whether participants who score zero versus any other value other than zero might differ in relation to the independent variables. Positive values on the binary outcome are interpreted to mean that lower values are related to greater chance of the dependent variable assuming zero values. Negative values on the binary outcome are interpreted to mean that higher values (using categorical contrast coding) on the independent variable are related to more non‐zero values on the dependent variable." |
Nathan 2019 provided raw study data that allowed us to extract summary statistics (skewed data) for the total number of self‐reported antisocial acts, reported using an adapted Self‐reported Delinquency Scale (SRD; 32‐item, self‐report measure), to record the frequency (ranging from 0 (low delinquency) to 32 (high delinquency)) in the first year (35 participants) and second year (non‐cumulative; 17 participants) after release from prison (Table 11).
Nathan 2019 reported the results of an intention‐to‐treat regression analysis (20 participants, 90% AsPD), to predict the total number of self‐reported antisocial acts reported by the SRD, which favoured neither condition (OR 1.534, 95% CI −0.210 to 3.277, P = 0.085, 20 participants (90% AsPD), 1 study, very low‐certainty evidence, Analysis 11.5).
11.5. Analysis.
Comparison 11: Psychosocial risk management ('Resettle programme') versus treatment‐as‐usual, Outcome 5: Recidivism: total antisocial behaviour assessed with the Self‐report Delinquency Scale
| Recidivism: total antisocial behaviour assessed with the Self‐report Delinquency Scale | |||||
| Study | Estimate | SE | 95% CI | p | Comments |
| Nathan 2019 | 1.534 | 0.889 | ‐0.210 to 3.277 | 0.085 | Statistical prediction of number Poisson‐distributed self‐report of antisocial behaviours (SRS total) by ITT Resettle group versus the control group (20 participants, 90% AsPD) |
Adverse events
Nathan 2019 reported the number of participants that died during the study period, with results favouring neither condition (OR 0.89, 95% CI 0.05 to 14.83, P = 0.94, 72 participants (90% AsPD), 1 study, very low‐certainty evidence, Analysis 11.6).
11.6. Analysis.

Comparison 11: Psychosocial risk management ('Resettle programme') versus treatment‐as‐usual, Outcome 6: Adverse event: death during study period
The study did not report data on any of our other primary outcomes: aggression; global state/functioning; or social functioning.
Secondary outcomes
Leaving the study early
Nathan 2019 incidentally reported the number of participants who did not contribute data to the ITT analysis of the primary outcome (number of official offences recorded at two years after release from prison), with results favouring neither condition (OR 2.07, 95% CI 0.63 to 6.83, P = 0.23, 72 participants (90% AsPD), 1 study, very low‐certainty evidence, Analysis 11.7).
11.7. Analysis.

Comparison 11: Psychosocial risk management ('Resettle programme') versus treatment‐as‐usual, Outcome 7: Leaving the study early: participants not included in ITT analysis of primary outcome
The study did not provide data on any of our other secondary outcomes: quality of life; engagement with services; satisfaction with treatment; employment status; housing/accommodation status; economic outcomes; impulsivity; anger; or prison and service outcomes.
Discussion
Antisocial personality disorder (AsPD) is a prevalent condition associated with considerable negative consequences for both the person with AsPD (including poor mental health, substance abuse, relationship difficulties, premature death) and society (including criminality and unemployment). Given the combination of its prevalence and widespread negative impact, it might be expected that the identification of effective interventions for this condition would be a research priority. Unfortunately, the conclusion of this review is similar to previous reviews (Gibbon 2010; NICE 2010), and it remains the case that there is little evidence as to what might (or might not) be effective for this condition.
The first point to make is how few studies there were to consider. The second concerns the design and methodological quality of the 19 included studies. The participant populations, attrition statistics, wide range of interventions investigated, choice of assessment tools (e.g. using measures designed for static 'trait' outcomes) and low quality of data, hinder the ability of this review to make meaningful comparisons between groups and draw conclusions from the evidence.
Disappointingly, few of the included studies addressed the primary outcomes defined in this review. While the underlying personality structure of AsPD comprises disparate traits, such as impulsivity, lack of remorse and irritability, its most common behavioural manifestation is persistent rule‐breaking (NICE 2015). Although the focus on behaviour, rather than on the underlying personality structure, has been frowned upon by some commentators (e.g. Livesley 2007), we argue that persistent rule‐breaking is akin to a final, common pathway manifestation of the underlying personality structure. If one accepts this argument, it is surprising that only four of the 19 included studies had reconviction as an outcome (Marlowe 2007; Woodall 2007; Bernstein 2012; Nathan 2019). Additionally, only five studies used self‐reported or institutional reports of aggression (Davidson 2009; Tarrier 2010; Bernstein 2012; Feigenbaum 2012; Thylstrup 2015). In the light of the important, adverse cost consequences of the condition, and likely need for complex and expensive interventions, it was also disappointing that only six studies considered the economic impact of their intervention directly or indirectly (Tyrer 2004; Davidson 2009; Bernstein 2012; Feigenbaum 2012; Priebe 2012; McMurran 2016).
Of the 19 included studies, nearly half (n = 9) were focussed on reducing substance misuse (Woody 1985; McKay 2000; Messina 2003; Ball 2005, Havens 2007; Marlowe 2007; Woodall 2007; Neufeld 2008; Thylstrup 2015). As many within the sample of substance misusers also satisfied the criteria for AsPD, there was an opportunity to report on these separately. Hence, strictly speaking, these were not interventions for AsPD; rather, they were interventions to reduce substance misuse in a sample, some of whom also satisfied criteria for AsPD. While these studies were not without their limitations, there is evidence that contingency management is effective in reducing substance misuse in people with AsPD. This finding is in keeping with NICE guidance on opioid detoxification (NICE 2007), and it suggests that this principle of intervention is also effective in those with AsPD.
Summary of main results
The focus of this review was relatively broad, since it sought evidence on the effectiveness of any psychological intervention in the treatment of AsPD or dissocial PD. We found considerable differences between the studies in terms of participants, sample sizes, interventions and outcome measures.
There were significant limitations in the certainty of the evidence (which was generally low), which limits the certainty of any conclusions we can draw from this review. The conclusions that we can draw may be subject to change with the addition of future research. Whist we did not find clear evidence of benefit from psychological interventions for this condition, we cannot tell if this is due to an absence of effective interventions or an absence of trials of a sufficient quality to detect this benefit (i.e. the absence of evidence is not evidence of absence of effect).
We identified eight interventions (primarily developed for people with substance abuse) that reported evidence for our primary outcomes.
Cognitive behaviour therapy (CBT) + treatment‐as‐usual (TAU)versus TAU
One study (52 participants, low‐certainty evidence) found no evidence of a difference between CBT + TAU and TAU alone for physical aggression for outpatients at 12 months post‐intervention.
One study (39 participants, very low‐certainty evidence) found no evidence of a difference between CBT + TAU and TAU alone for social functioning measured by the Social Functioning Questionnaire (SFQ) for outpatients at 12 months post‐intervention.
Impulsive lifestyle counselling (ILC) + TAU versus TAU
One study (118 participants, very low‐certainty evidence) found no evidence of a difference between ILC + TAU and TAU alone for trait aggression (assessed with Buss‐Perry Aggression Questionnaire‐Short Form) for outpatients at nine months.
One study (142 participants, very low‐certainty evidence) found no evidence of a difference between ILC + TAU and TAU alone for the adverse event of death or incarceration for outpatients between three and nine months follow‐up.
Contingency management (CM) + standard maintenance (SM) versus SM
One study (83 participants, low‐certainty evidence) found evidence that, compared to SM alone, CM + SM may improve social functioning, measured by family/social scores on the Addiction Severity Index for outpatients at six months.
‘Driving whilst intoxicated' programme (DWI) + incarcerationversus incarceration
One study (52 participants, very low‐certainty evidence) found no evidence of a difference between DWI + incarceration and incarceration alone on reconviction (re‐arrest) rates for prisoner participants at 24 months.
Schema therapy (ST) versus TAU
One study (30 participants, of whom 87% had AsPD diagnosis, very low‐certainty evidence) found no evidence of a difference between ST and TAU for the number of participants reconvicted as patients in a secure psychiatric hospital at three years. This study also found evidence that ST, compared to TAU, may improve for social functioning (assessed by the number of days for patients to gain unsupervised leave at three years) and that there was no evidence of a difference between ST and TAU for overall adverse events classified globally as negative outcomes at three years, but the evidence is very uncertain.
Social problem‐solving therapy (SPS) + psychoeducation (PE) versus TAU.
One study (17 participants, very low‐certainty evidence) found no evidence of a difference between SPS + PE and TAU for participants’ level of social functioning assessed with the SFQ at six months post‐intervention.
Dialectical behaviour therapy versus TAU
One study (skewed data, 14 participants, very low‐certainty evidence) provided narrative evidence that DBT, compared to TAU, may reduce adverse events (number of self‐harm days) for outpatients at two months post‐intervention
Psychosocial risk management (PSRM; 'Resettle' programme) versus TAU
One study (skewed data, 35 participants, very low‐certainty evidence) found no evidence of a difference between PSRM and TAU for participants' number of officially recorded offences at one year after release from prison. The same study also found no evidence of difference between the PSRM and TAU for the adverse event of death at two years after release from prison, but the evidence is very uncertain.
Of these eight interventions, five (CBT + TAU; ILC + TAU; DWI programme + incarceration; SPS; and PSRM ('Resettle' programme)) demonstrated little or no difference compared to control for the primary outcomes considered in this review. Two interventions (CM + SM; and ST) showed some benefit over the control condition in terms of social functioning, although these findings were based only on single study data with small numbers of participants (83 and 30 participants, respectively). For the remaining intervention (DBT), narrative evidence suggested that DBT may be more effective than control at reducing the adverse event of self‐harm, although this was also based on findings from a single study with skewed data.
For the CM intervention, two studies produced contrasting results in terms of the secondary outcome 'substance misuse' (Messina 2003; Neufeld 2008). The Addiction Severity Index results for substance misuse (drugs and alcohol) favoured the intervention over the control in the Messina 2003 study but not in the Neufeld 2008 study. However, CM was superior in terms of social functioning and attendance at counselling sessions in the Neufeld 2008 study. These differences may have arisen because of differences in the nature of the behavioural intervention. Both studies described CM but the positive reinforcements available in the Messina 2003 study for participants who stayed drug‐free seem considerably more attractive. For example, a participant in the Messina 2003 study who managed to stay drug‐free for the whole 16 weeks of the trial could earn redeemable vouchers worth a total of US$1277. In contrast, the positive reinforcement in the Neufeld 2008 trial comprised greater control over methadone clinic attendance and dosage in reward for drug abstinence and attendance at counselling sessions.
Overall completeness and applicability of evidence
The evidence obtained from the included studies is relevant and applicable to the review question, but is incomplete for the following reasons.
Although 18 different psychological interventions were compared, none of the studies evaluated therapeutic community treatment, cognitive analytic therapy, mentalisation‐based therapy or nidotherapy.
The majority of studies did not focus primarily on the treatment of AsPD; only four recruited samples where all participants had this diagnosis.
Nine studies focussed on participants with difficulties with substance misuse. Although drug or alcohol misuse (or both) is often relevant to people with AsPD, having a substance misuse problem is not part of the diagnostic criteria for AsPD.
The findings in two studies may not fully generalise to the population of interest: the sample in Woodall 2007 was drawn mainly from a Native American community; and Marlowe 2007 found that women were significantly over‐represented in their sample, and that individuals with more severe drug problems and less severe criminal histories were significantly more likely to have participated.
Many of the included studies did not address the primary outcomes specified in this review. Of the 19 included studies, only five reported on aggression and only four reported on reconviction. Five of the included studies did not report any of the primary outcomes.
The review only considered effectiveness trials, where interventions were compared with either TAU, waiting‐list, or a 'no treatment' control group, rather than head‐to‐head trials comparing two or more psychological interventions without an adequate control condition.
The review identified three ongoing RCTs of psychological interventions for individuals with a diagnosis of AsPD that may represent different interventional approaches to the treatment of AsPD in future updates of this review. One RCT is examining the effectiveness of moral reconation therapy (NCT02524171) and two other trials are assessing the effectiveness of mentalisation‐based therapy (ISRCTN32309003; NCT04033835). Three further ongoing studies have samples that may include participants with AsPD: one examining the impact of low‐intensity psychological support for people with personality disorder (ISRCTN14994755); one examining group schema‐focussed therapy enriched with psychomotor therapy for older adults with personality disorder (Van Dijk 2019); and one examining mindfulness for alcohol‐abusing female offenders (NCT03883646).
Quality of the evidence
The 19 studies that met the criteria for inclusion in this review involved a total of 848 participants with AsPD. Of these 19 studies, only 10 provided suitable data, involving 605 participants with AsPD.
All of the included studies were RCTs; however, as Guyatt 2011 acknowledges, even RCTs can be limited by problems such as failure to conceal allocation, failure to blind, loss to follow‐up, failure to use the intention‐to‐treat principle, stopping early for apparent benefit, and selective reporting of outcomes. Such issues increase the risk of bias, which, in turn, can overestimate the benefits and underestimate the harms identified (Moher 1998; Moher 2010). We used the GRADE approach to assess the certainty of the reported evidence (Schünemann 2013), and considered the risk of bias, inconsistency, indirectness, imprecision of the evidence and publication bias. We assessed the certainty of the evidence from all included studies with data for AsPD participants separately for individual outcomes. In every case, the evidence was downgraded due to a combination of issues with risk of bias (high or possible risk of bias), indirectness (e.g. due to use of self‐reported questionnaire), or imprecision (due to small sample size/optimal information size criteria not being met or non‐reporting of outcome data).The largest risk of bias in the included studies came from inadequate blinding of outcome assessors, incomplete outcome data (attrition bias) and selective reporting bias. We rated the certainty of the evidence for all primary outcomes as low or very low (i.e. we have very little confidence in the effect estimate, and the true effect is likely to be substantially difference from the estimate of effect). None of the outcome effect estimates assessed using the GRADE approach received a rating of moderate certainty (i.e. the true effect is likely to close to the estimate of the effect, but there is a possibility that it is substantially different), or a rating of high certainty (i.e. that we could be confident that the true effect lies close to that of the estimate of the effect).
We judged the overall certainty of the evidence from the included trials to be poor for the following reasons.
The review relied on data from only 10 of the 19 included studies despite attempts to contact the trial investigators for information on the AsPD subgroups.
The study samples were heterogeneous; they encompassed, for example, both prisoners, inpatients and outpatients. In addition, AsPD (or dissocial personality disorder) was diagnosed under four similar but not identical rubrics (DSM‐III, DSM‐III‐R, DSM‐IV and ICD‐10).
Where the completion rate was reported, it was high (mean = 83.5%). This may be misleading because of the custodial element of some interventions. For example, Woodall 2007 had a 100% completion rate, which might be expected given that one component of the intervention was incarceration.
There was inconsistency in the way studies measured and reported the primary and secondary outcomes.
Although Guyatt 2011 suggests that a single, very large, rigorously planned and conducted multicentre RCT may provide high‐certainty evidence, others suggest that there should be at least two independent, well‐conducted RCTs or single‐case experiments for a treatment to be considered effective (Chambless 1998). The majority of studies reported small sample sizes and provided evidence for individual comparisons; it was not possible to pool data given the heterogeneity of the interventions and participants. In light of this, we considered that the body of evidence summarised in this review is insufficient to allow any conclusion to be drawn about the use of psychological interventions in the treatment of AsPD.
A further limitation with the certainty of the evidence arises from an acknowledgement that personality disorder, in general, is a complex condition and clinical outcomes are best measured across multiple domains (see Gibbon 2010). A broad approach to outcome evaluation in personality disorder has been recognised by international experts in the field (e.g. Crawford 2007).
Potential biases in the review process
As Lieb 2016 discuss, we were aware of a potential for bias that might be seen as arising because two of the authors in the original review (CD and NH) were investigators in one of the studies included in this review (Huband 2007). We minimised this risk by ensuring that neither author took part in the extraction of data, summarising the risk of bias for this trial or assessing the certainty of the evidence using GRADE. When it became necessary to request additional data from this study's lead investigator, correspondence was handled via Cochrane Developmental, Psychosocial and Learning Problems (DPLP). These requests were referred by NH to the trial's research committee who responded via Cochrane DPLP. There were no such conflicts of interest in this update.
We acknowledge that a small number of decisions taken during the review process may have introduced 'selective reporting bias' to the review. First, the decision to include studies with two treatment conditions where the trial investigators randomised ‘at least five people with AsPD’ may have resulted in the exclusion of a small number of studies. In this case, we considered that the potential for bias was minimal, as any excluded studies with very small numbers were usually not RCTs. Second, the 12‐week cut‐off period for receiving missing data from study authors could have resulted in relevant data being omitted from the review. In this way, it could be interpreted that we selectively reported the missing data and that the review is open to reporting bias. However, this is not the case, as no missing data were excluded. Third, we decided to include only studies where at least 75% of participants were diagnosed with AsPD. Although this appeared clinically and scientifically appropriate, this decision may have introduced reporting bias to the review.
Agreements and disagreements with other studies or reviews
It remains the case that the most recent and widest ranging relevant review with which to compare our findings is that carried out in the development of the NICE clinical guideline on antisocial personality disorder (NICE 2010). In reporting their systematic review, the NICE guideline authors observed that there had been little formal development of psychological interventions specifically for the treatment of AsPD, whereas there had been "considerable development of interventions aimed at reducing offending behaviour" (p 171, section 7.2.1, NICE 2010). In recognition of this, they chose to consider not only interventions that targeted AsPD itself, but also those that targeted the symptoms or behaviours associated with the diagnosis (such as anger, impulsivity and aggression), as well as interventions specifically for offenders regardless of diagnosis. Thus, the review described by NICE 2010 is broader than our current review, which focuses solely on studies of participants with a diagnosis of antisocial or dissocial personality disorder.
Although our original review (Gibbon 2010) and the NICE 2010 review identified four of the same studies (Woody 1985; McKay 2000; Messina 2003 and Davidson 2009), there were several differences between them.
Gibbon 2010, identified one study, Neufeld 2008, which was a later and more complete summary of the trial initially reported by Brooner 1998, which was included in the NICE 2010 review.
Gibbon 2010, identified two additional studies with data that were not included in the NICE 2010 review: Huband 2007 and Woodall 2007.
NICE 2010 considered three additional studies that we excluded from our original review (Gibbon 2010): Hesselbrock 1991 on hospitalisation for alcohol dependence, which we excluded because it was not an RCT and had no control condition; Wölwer 2001 on CBT versus coping skills training versus TAU in alcohol dependence, which we excluded because too few participants had AsPD; and Vannoy 2004 on anger management versus waiting‐list TAU in offenders, which we excluded because no participants had AsPD.
NICE 2010 additionally considered a further 21 studies of treatments for offending behaviour in young people (n = 11), in adults (n = 5) and in offenders with substance misuse problems (n = 5). These studies were not eligible for inclusion in this review (neither in the original review (Gibbon 2010) nor this update), because the participants had no formal diagnosis of antisocial or dissocial personality disorder.
In their conclusions, NICE 2010 considered that the evidence for the psychological treatment of antisocial personality disorder was limited to one community trial (Davidson 2009), that the quality of the evidence varied between low and moderate, and that the limited economic evidence from that trial suggested that CBT may not be cost saving in the short term. They considered, however, that there was modest evidence for the effectiveness of cognitive and behavioural interventions, primarily delivered in groups, in reducing offending for adults with substance misuse problems and that this effect has been found in variety of settings, including institutional, outpatient and probation settings.
The current review concludes that good‐quality evidence in favour of any psychological intervention for AsPD continues to be virtually non‐existent.
Authors' conclusions
Implications for practice.
This review concludes that there is insufficient evidence to support or refute the effectiveness of any psychological intervention for AsPD. There are particular difficulties with conducting trials in this area and the limited number of studies limits the extent to which useful conclusions can be drawn. In the absence of good‐quality trial data, the use of psychological interventions to treat people with AsPD in clinical practice remains a matter for the clinician, who will wish to weigh the limited evidence of effectiveness against any risk of possible harm; it should ideally be based on consultation with the patient, their family and carers (subject to their consent) and the multidisciplinary team involved in the individual's care.
Implications for research.
Given the very few studies that could be considered in this review, there is clearly an imperative to conduct further well‐designed trials. These trials should be of an active psychological treatment against treatment‐as‐usual (effectiveness trials) rather than head‐to‐head trials. It would be helpful if future studies could provide more detail about the interventions that were delivered.
Future trials should use assessment tools that are designed to identify clinical change rather than static traits. We are also mindful of the issues described in the DSM‐5 (p 659): “Because deceit and manipulation are central features of antisocial personality disorder, it may be especially helpful to integrate information acquired from systematic clinical assessments with information collected from collateral sources”. In deciding outcomes for future trials, consideration should also be given to those that are measurable by a number of means such as self‐report, psychometrics, observed behaviour, informant information and official records. It is also notable that there have not been any studies focussing on women with AsPD.
A major problem in carrying out trials involving AsPD participants is that this is a challenging group to retain in treatment, as people with AsPD are often treatment‐rejecting rather than treatment‐seeking (NICE 2010). However, this caveat does not apply to those in prison, where there are a large number of individuals incarcerated with AsPD. This may also help to address the difficulties that previous studies have encountered regarding small sample size. If a prison population was chosen, then reconviction on release ought to be the outcome of choice, as this is, unfortunately, a relatively common outcome in many with AsPD, with approximately two‐thirds of those being released from prison reoffending within two years (Kershaw 1999; ONS 2004). The major negative impact of aggression and reconviction (which could represent a final common pathway encompassing a variety of traits, including failure to confirm to social norms, deceitfulness, impulsivity, recklessness, irresponsibility and lack of remorse) makes this outcome particularly important. Hence, we suggest that reconviction is chosen as the primary outcome in such a trial, preferably in conjunction with an economic evaluation.
If there was a consensus on a single outcome measured across studies, then it would be possible to make cross‐study comparisons, a task that is difficult to perform at present because of the wide range of outcomes and measures that are used.
What's new
| Date | Event | Description |
|---|---|---|
| 29 June 2020 | New citation required but conclusions have not changed | We added eight new studies to the review. The conclusions of the review have not changed. |
| 5 September 2019 | New search has been performed | The review was updated following a new search on 29 September 2016, and top‐up searches on 31 October 2017, 3 October 2018 and 5 September 2019. |
History
Protocol first published: Issue 1, 2009 Review first published: Issue 6, 2010
| Date | Event | Description |
|---|---|---|
| 25 August 2020 | Amended | Minor changes in response to copy editing |
| 2 November 2017 | Amended | Searches updated and full revision of data and analyses |
Acknowledgements
We gratefully acknowledge: Margaret Anderson (Cochrane Developmental, Psychosocial and Learning Problems Group) for running the electronic searches and Joanne Duffield (Cochrane Developmental, Psychosocial and Learning Problems Group) for her ongoing advice and support during the preparation of this review. We would like to acknowledge Nottinghamshire Healthcare NHS Foundation Trust for supporting this work. We would like to thank the previous authors of this review (Jutta M Stoffers‐Winterling, Nick Huband, Michael Ferriter, Klaus Lieb and Conor Duggan) and all of the primary study authors who responded to our requests and provided further information. Finally, we would like to thank the following reviewers for their comments on an earlier version of this update: Dr Gemma L Clayton, Department of Population Health Sciences, Bristol Medical School, University of Bristol, UK; Professor Jane L Ireland, University of Central Lancashire and Mersey Care NHS Trust, UK; Dr Ely M Marceau, Illawarra Health and Medical Research Institute and School of Psychology, University of Wollongong, Wollongong, New South Wales, Australia; Dr Anna Motz, Family Assessment and Safeguarding Service, Oxford Health NHS Foundation Trust, Oxford, UK; and Dr Odie Geiger, Community Engagement Advisory Network, Vancouver, Canada.
Appendices
Appendix 1. Search strategy
CENTRAL, part of the Cochrane Library
Searched 3 October 2016 [1371 records] Searched 31 October 2017 [66 records] Searched 3 October 2018 [359 records] Searched 5 September 2019 [296 records]
#1[mh "Antisocial Personality Disorder"] #2[mh ^"personality disorder"] #3(asocial* or antisocial* or anti next social* or dissocial* or dis next social* or dyssocial* or dys next social*) #4(self next defeating or masochistic) #5multi next impulsiv* #6((moral* or amoral or "a‐moral") near/5 (character* or personalit*)) #7[mh ^"Multiple Personality Disorder"] #8[mh Narcissism] #9narciss* #10(sociopath* or socio next path*) #11(psychopath or psychopaths or psychopathic*) #12(psycho next path or psycho next paths or psycho next pathic*) #13[mh sadism] #14sadis* #15(self next defeating or masochist*) #16[mh "Disruptive, Impulse Control, and Conduct Disorders"] #17[mh Aggression] #18[mh "Impulsive behavior"] #19((aggress* or deceitful* or impulsiv* or irritab* or reckless*) near/5 (person* or disorder*)) #20"Cluster B" #21"F60.2" #22"301.7" #23{or #1‐#22} Publication Year from 2009 to 2016, in Trials #24{or #1‐#22} Publication Year from 2016 to 2017, in Trials #25{or #1‐#22} Publication Year from 2017 to 2018, in Trials #26{or #1‐#22} Publication Year from 2018 to 2019, in Trials
MEDLINE Ovid
Searched 29 September 2016 [3988 records] Searched 31 October 2017 [635 records] Searched 3 October 2018 [614 records] Searched 5 September 2019 [525 records]
1 Antisocial Personality Disorder/ 2 personality disorders/ 3 (asocial$ or antisocial$ or anti‐social$ or dissocial$ or dis‐social$ or dyssocial$ or dys‐social$).tw,kf. 4 (self‐defeating or masochistic).tw,kf. 5 multi‐impulsiv$.tw,kf. 6 ((moral$ or amoral or "a‐moral") adj5 (character$ or personalit$)).tw,kf. 7 Multiple Personality Disorder/ 8 Narcissism/ 9 narciss$.tw,kf. 10 (sociopath$ or socio‐path$).tw,kf. 11 (psychopath$2 or psycho‐path$2).tw,kf. 12 sadism/ 13 sadis$.tw,kf. 14 (self‐defeating or masochist$).tw,kf. 15 "Disruptive, Impulse Control, and Conduct Disorders"/ 16 Aggression/ 17 Impulsive behavior/ 18 ((aggress$ or deceitful$ or impulsiv$ or irritab$ or reckless$) adj5 (person$ or disorder$)).tw,kf. 19 Cluster B.tw,kf. 20 "F60.2".tw,kf. 21 "301.7".tw,kf. 22 or/1‐21 23 randomized controlled trial.pt. 24 controlled clinical trial.pt. 25 randomi#ed.ab. 26 placebo$.ab. 27 drug therapy.fs. 28 randomly.ab. 29 trial.ab. 30 groups.ab. 31 or/23‐30 32 exp animals/ not humans.sh. 33 31 not 32 34 22 and 33 35 limit 34 to yr="2009 ‐Current" 36 limit 34 to ed=20160901‐20171019 37 limit 34 to ed=20171020‐20180920 38 limit 34 to ed=20180921‐20190829
MEDLINE In‐Process & Other Non‐Indexed Citations Ovid
Searched 30 September 2016 [840 records] Searched 31 October 2017 [471 records] Searched 3 October 2018 [474 records] Searched 5 September 2019 [514 records]
1 (asocial$ or antisocial$ or anti‐social$ or dissocial$ or dis‐social$ or dyssocial$ or dys‐social$).tw,kf. 2 (self‐defeating or masochistic).tw,kf. 3 multi‐impulsiv$.tw,kf. 4 ((moral$ or amoral or "a‐moral") adj5 (character$ or personalit$)).tw,kf. 5 narciss$.tw,kf. 6 (sociopath$ or socio‐path$).tw,kf. 7 (psychopath$2 or psycho‐path$2).tw,kf. 8 sadis$.tw,kf. 9 (self‐defeating or masochist$).tw,kf. 10 Cluster B.tw,kf. 11 "F60.2".tw,kf. 12 "301.7".tw,kf. 13 ((aggress$ or deceitful$ or impulsiv$ or irritab$ or reckless$) adj5 (disorder$ or person$)).tw,kf. 14 or/1‐13 15 (random$ or trial$ or control$ or group$ or placebo$ or blind$ or prospectiv$ or longitudinal$ or meta‐analys$ or systematic review$).tw,kf. 16 14 and 15
MEDLINE Epub Ahead of Print Ovid
Searched 30 September 2016 [381 records] Searched 31 October 2017 [175 records] Searched 3 October 2018 [171records] Searched 5 September 2019 [187 records]
1 (asocial$ or antisocial$ or anti‐social$ or dissocial$ or dis‐social$ or dyssocial$ or dys‐social$).tw,kf. 2 (self‐defeating or masochistic).tw,kf. 3 multi‐impulsiv$.tw,kf. 4 ((moral$ or amoral or "a‐moral") adj5 (character$ or personalit$)).tw,kf. 5 narciss$.tw,kf. 6 (sociopath$ or socio‐path$).tw,kf. 7 (psychopath$2 or psycho‐path$2).tw,kf. 8 sadis$.tw,kf. 9 (self‐defeating or masochist$).tw,kf. 10 Cluster B.tw,kf. 11 "F60.2".tw,kf. 12 "301.7".tw,kf. 13 ((aggress$ or deceitful$ or impulsiv$ or irritab$ or reckless$) adj5 (disorder$ or person$)).tw,kf. 14 or/1‐13 15 (random$ or trial$ or control$ or group$ or placebo$ or blind$ or prospectiv$ or longitudinal$ or meta‐analys$ or systematic review$).tw,kf. 16 14 and 15
Embase OVID
Searched 2009 to 30 September 2016 (3060 records) Searched 2016 to November 2017 (219 records) Searched 2017 to 3 October 2018 (344 records) Searched 2018 to 5 September 2019 (382 records)
1 Antisocial Personality Disorder/ 2 *Personality disorder/ 3 ((asocial$ or antisocial$ or anti‐social$ or dissocial$ or dis‐social$ or dyssocial$ or dys‐social$) adj5 (person$ or disorder$)).tw,kw. 4 (self‐defeating or masochistic).tw,kw. 5 ((moral$ or amoral or "a‐moral") adj5 (character$ or personalit$)).tw,kw. 6 multiple personality/ 7 narcissism/ 8 narciss$.tw,kw. 9 (sociopath$ or socio‐path$).tw,kw. 10 psychopathy/ 11 (psychopath$2 or psycho‐path$2).tw,kw. 12 sadism/ 13 sadis$.tw,kw. 14 masochism/ 15 (self‐defeating or masochist$).tw,kw. 16 impulse control disorder/ 17 *impulsiveness/ 18 *Aggression/ 19 ((aggress$ or deceitful$ or impulsiv$ or irritab$ or reckless$) adj5 (person$ or disorder$)).tw,kw. 20 Cluster B.tw,kw. 21 "F60.2".tw,kw. 22 "301.7".tw,kw. 23 or/1‐22 24 Randomized controlled trial/ 25 controlled clinical trial/ 26 Single blind procedure/ 27 Double blind procedure/ 28 triple blind procedure/ 29 Crossover procedure/ 30 (crossover or cross‐over).tw. 31 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 32 Placebo/ 33 placebo.tw. 34 prospective.tw. 35 factorial$.tw. 36 random$.tw. 37 assign$.ab. 38 allocat$.tw. 39 volunteer$.ab. 40 or/24‐39 41 23 and 40 42 limit 41 to yr="2009 ‐Current" 43 remove duplicates from 42 44 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/ 45 human/ or normal human/ or human cell/ 46 44 and 45 47 44 not 46 48 43 not 47
CINAHL Plus EBSCOhost
Searched 2009 to 3 October 2016 (2426 records) Searched 2016 to 2 November 2017 (199 records) Searched 2017 to3 October 2018 (714 records) Searched 2018 to 5 September 2019 (422 records)
S1(MH "Antisocial Personality Disorder") S2(MH "Personality Disorders") S3(asocial* or antisocial* or anti‐social* or dissocial* or dis‐social* or dyssocial* or dys‐social*) S4multi‐impulsiv* S5((moral* or amoral or "a‐moral") N5 (character* or personalit*)) S6(MH "Multiple‐Personality Disorder") S7(MH "Narcissism") S8narciss* S9(sociopath* or socio‐path*) S10(psychopath or psychopaths or psychopathic or psycho‐path*) S11sadis* S12(MH "Disruptive Behavior") S13(MH "Aggression") S14MH social behavior disorders S15(MH "Deception") S16((aggress* or deceitful* or impulsiv* or irritab* or reckless*) N5 (person* or disorder*)) S17"Cluster B" S18"F60.2" S19"301.7" S20S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 S21(MH "Clinical Trials+") S22MH random assignment S23(MH "Meta Analysis") S24(MH "Crossover Design") S25(MH "Quantitative Studies") S26PT randomized controlled trial S27PT Clinical trial S28(clinical trial*) or (control* N2 trial*) S29("follow‐up study" or "follow‐up research") S30(prospectiv* study or prospectiv* research) S31(evaluat* N2 study or evaluat* N2 research) S32(MH "Program Evaluation") S33(MH "Treatment Outcomes") S34TI(single N2 mask* or single N2 blind*) OR AB(single N2 mask* or single N2 blind*) S35TI((doubl* N2 mask*) or (doubl* N2 blind*)) OR AB((doubl* N2 mask*) or (doubl* N2 blind*)) S36TI ((tripl* N2 mask*) or (tripl* N2 blind*)) or ((trebl* N2 mask*) or (trebl* N2 blind*)) OR AB((tripl* N2 mask*) or (tripl* N2 blind*)) or ((trebl* N2 mask*) or (trebl* N2 blind*) S37random* S38S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 S39S20 AND S38
PsycINFO OVID
Searched 2009 to 30 September 2016 (6366 records) Searched 2016 to 2 November 2017.(1072 records) Searched 2017 to 3 October 2018 (704 records) Searched 2018 to 5 September 2019 (684 records)
1 Antisocial Personality Disorder/ 2 *Personality Disorders/ 3 ((asocial$ or antisocial$ or anti‐social$ or dissocial$ or dis‐social$ or dyssocial$ or dys‐social$) adj5 (person$ or disorder$)).tw,id. 4 (self‐defeating or masochistic).tw,id. 5 ((moral$ or amoral or "a‐moral") adj5 (character$ or personalit$)).tw,id. 6 Dissociative Identity Disorder/ 7 NARCISSISM/ 8 narciss$.tw,id. 9 (sociopath$ or socio‐path$).tw,id. 10 psychopathy/ 11 (psychopath$2 or psycho‐path$2).tw,id. 12 Sadism/ 13 sadis$.tw,id. 14 MASOCHISM/ ) 15 Self‐Defeating Behavior/ 16 (self‐defeating or masochist$).tw,id. 17 exp Impulse Control Disorders/ 18 Impulsiveness/ 19 Aggressiveness/ 20 *Aggressive behavior/ 21 ((aggress$ or deceitful$ or impulsiv$ or irritab$ or reckless$) adj5 (person$ or disorder$)).tw,id. 22 Cluster B.tw,id. 23 "F60.2".tw,id. 24 "301.7".tw,id. 25 or/1‐24 26 clinical trials/ 27 longitudinal studies/ 28 exp program evaluation/ 29 exp Treatment Effectiveness Evaluation/ 30 random$.tw. 31 ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$)).tw. 32 (crossover$ or "cross over$").tw. 33 trial$.tw. 34 group$.ab. 35 treatment effectiveness evaluation/ 36 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 37 prospective.tw. 38 factorial$.tw. 39 (assign$ or allocat$).ab. 40 control.ab. 41 placebo.ab. 42 (crossover or cross‐over).tw. 43 or/26‐42 44 25 and 43
Science Citation Index Web of Science
Searched 2019 to 3 October 2016 (1233 records) Searched 2016 to 2 November 2017 (198 records) Searched 2017 to 3 October 2018 (181 records) Searched 2018 to 5 September 2019 (170 records)
#14 #13 AND #12 DocType=All document types; Language=All languages; #13 TS=(random* or trial* or control* or group* or placebo* or blind* or prospectiv* or longitudinal* or meta‐analys* or systematic review*) DocType=All document types; Language=All languages; #12 #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #2 OR #1 DocType=All document types; Language=All languages; #11 TS="301.7" DocType=All document types; Language=All languages; #10 TS="F60.2" DocType=All document types; Language=All languages; #9 TS=("Cluster B" and (person* or trait* or character*)) DocType=All document types; Language=All languages; #8 TS=sadis* DocType=All document types; Language=All languages; #7 TS=(psychopath or psychopaths or psychopathic ) DocType=All document types; Language=All languages; #6 TS=(sociopath* or socio‐path*) DocType=All document types; Language=All languages; #5 TS=narciss* DocType=All document types; Language=All languages; #4 TS=((moral* or amoral or "a‐moral") near/5 (character* or personalit*)) DocType=All document types; Language=All languages; #3 TS=multi‐impulsiv* DocType=All document types; Language=All languages; #2 TS=(self‐defeating or masochistic) DocType=All document types; Language=All languages; #1 TS= ((asocial* or antisocial* or anti‐social* or dissocial* or dis‐social* or dyssocial* or dys‐social*) NEAR/5 (person* )) DocType=All document types; Language=All languages;
Social Science Citation Index Web of Science
Searched 2019 to 3 October 2016 (2119 records) Searched 2016 to 2 November 2017 (386 records) Searched 2017 to 3 October 2018 (378 records) Searched 2018 to 5 September 2019 (363 records)
#14 #13 AND #12 DocType=All document types; Language=All languages; #13 TS=(random* or trial* or control* or group* or placebo* or blind* or prospectiv* or longitudinal* or meta‐analys* or systematic review*) DocType=All document types; Language=All languages; #12 #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #2 OR #1 DocType=All document types; Language=All languages; #11 TS="301.7" DocType=All document types; Language=All languages; #10 TS="F60.2" DocType=All document types; Language=All languages; #9 TS=("Cluster B" and (person* or trait* or character*)) DocType=All document types; Language=All languages; #8 TS=sadis* DocType=All document types; Language=All languages; #7 TS=(psychopath or psychopaths or psychopathic ) DocType=All document types; Language=All languages; #6 TS=(sociopath* or socio‐path*) DocType=All document types; Language=All languages; #5 TS=narciss* DocType=All document types; Language=All languages; #4 TS=((moral* or amoral or "a‐moral") near/5 (character* or personalit*)) DocType=All document types; Language=All languages; #3 TS=multi‐impulsiv* DocType=All document types; Language=All languages; #2 TS=(self‐defeating or masochistic) DocType=All document types; Language=All languages; #1 TS= ((asocial* or antisocial* or anti‐social* or dissocial* or dis‐social* or dyssocial* or dys‐social*) NEAR/5 (person* )) DocType=All document types; Language=All languages;
Conference Proceedings Citation Indexes ‐ Science, and ‐ Social Science & Humanities Wed of Science
Searched 2019 to 3 October 2016 (19 records) Searched 2016 to 2 November 2017 (17 records) Searched 2017 to 3 October 2018 (18 records) Searched 2018 to 5 September 2019 (18 records)
#14 #13 AND #12 DocType=All document types; Language=All languages; #13 TS=(random* or trial* or control* or group* or placebo* or blind* or prospectiv* or longitudinal* or meta‐analys* or systematic review*) DocType=All document types; Language=All languages; #12 #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #2 OR #1 DocType=All document types; Language=All languages; #11 TS="301.7" DocType=All document types; Language=All languages; #10 TS="F60.2" DocType=All document types; Language=All languages; #9 TS=("Cluster B" and (person* or trait* or character*)) DocType=All document types; Language=All languages; #8 TS=sadis* DocType=All document types; Language=All languages; #7 TS=(psychopath or psychopaths or psychopathic ) DocType=All document types; Language=All languages; #6 TS=(sociopath* or socio‐path*) DocType=All document types; Language=All languages; #5 TS=narciss* DocType=All document types; Language=All languages; #4 TS=((moral* or amoral or "a‐moral") near/5 (character* or personalit*)) DocType=All document types; Language=All languages; #3 TS=multi‐impulsiv* DocType=All document types; Language=All languages; #2 TS=(self‐defeating or masochistic) DocType=All document types; Language=All languages; #1 TS= ((asocial* or antisocial* or anti‐social* or dissocial* or dis‐social* or dyssocial* or dys‐social*) NEAR/5 (person* )) DocType=All document types; Language=All languages;
Sociological Abstracts Proquest
Searched 2009 to 3 October 2016 (878 records) Searched 2016 to 2 November 2017 (87 records) Searched 2017 to 3 October 2018 (89 records) Searched 2018 to 5 September 2019. (86 records)
(SU.EXACT("Personality Disorders") OR SU.EXACT("Sociopathic Personality") OR TI,AB(asocial* or antisocial* or anti‐social* or dissocial* or dis‐social* or dyssocial* or dys‐social*) OR TI,AB(self‐defeating or masochistic*) OR TI,AB( narciss* or sociopath* or socio‐path* or psychopath* or sadis*) OR TI,AB((aggress* or deceitful* or impulsiv* or irritab* or reckless*) NEAR/5 (person* or disorder*)) OR TI,AB("Cluster B" or "F60.2" or "301.7")) AND (SU.EXACT("Random Samples") OR SU.EXACT("Effectiveness") OR SU.EXACT("Intervention") OR SU.EXACT("Treatment Outcomes") OR SU.EXACT("Evaluation Research") OR SU.EXACT("Program Evaluation") OR SU.EXACT("Comparative Analysis") OR TI,AB(random* OR trial* OR control* OR placebo OR intervention* OR treat* OR evaluat* ))
Criminal Justice Abstracts EBSCOhost
Searched 2009 to 3 October 2016 (1104 records) Searched 2016 to 2 November 2017(144 records) Searched 2017 to 3 October 2018 (164 records) Searched 2018 to 5 September 2019 (123 records)
S10 S6 AND S9 S9 S7 OR S8 S8 TI(random* OR control* OR placebo OR intervention* OR treat* OR therap* ) OR AB(random* OR control* OR placebo OR intervention* OR treat* OR therap*) S7 (ZU "randomized controlled trials") or (ZU "randomized controlled trials ‐‐ research") S6 S1 OR S2 OR S3 OR S4 OR S5 S5 ("Cluster B" or "F60.2" or "301.7") S4 (narciss* or sociopath* or "socio‐path*" or psychopath* or sadis*) N5 (person* or disorder*) S3 (self‐defeating or masochistic*) S2 antisocial or anti‐social or dissocial OR "dis‐social" OR dys‐social OR dyssocial S1 (ZU "antisocial personality disorders")
Cochrane Database of Systematic Reviews, part of the Cochrane Library
Searched 3 October 2016 (9 records) Searched 31 October 2017 (1 record) Searched 3 October 2018 (8 records) Searched 5 September 2019 (0 records)
#1[mh "Antisocial Personality Disorder"] #2((asocial* or antisocial* or anti next social* or dissocial* or dis next social* or dyssocial* or dys next social*) next/5 (person* or disorder*)):ti,ab,kw #3(self next defeating or masochistic):ti,ab,kw #4multi next impulsiv*:ti,ab,kw #5((moral* or amoral or "a‐moral") near/5 (character* or personalit*)):ti,ab,kw #6[mh ^"Multiple Personality Disorder"] #7[mh Narcissism] #8narciss*:ti,ab,kw #9(sociopath* or socio next path*):ti,ab,kw #10(psychopath or psychopaths or psychopathic*):ti,ab,kw #11(psycho next path or psycho next paths or psycho next pathic*):ti,ab,kw #12[mh sadism] #13sadis*:ti,ab,kw #14(self next defeating or masochist*):ti,ab,kw #15"Cluster B":ti,ab,kw #16"F60.2":ti,ab,kw #17"301.7":ti,ab,kw #18{or #1‐#17} #19[mh "Disruptive, Impulse Control, and Conduct Disorders"] #20[mh Aggression] #21[mh "Impulsive behavior"] #22((aggress* or conduct* or deceitful* or disruptiv* or impulsiv* or irritab* or reckless*) next/5 (person* or disorder*)):ti,ab,kw in Cochrane Reviews (Reviews and Protocols) #23{or #19‐#22} #24[mh ^"personality disorders"] #25(personalit* near/3 disorder*):ti,ab,kw #26#24 or #25#27#23 and #26 #28#18 or #27 Publication Year from 2009 to 2016, in Cochrane Reviews (Reviews and Protocols) #29#18 or #27 Publication Year from 2016 to 2017, in Cochrane Reviews (Reviews and Protocols) #30#18 or #27 Publication Year from 2017 to 2018, in Cochrane Reviews (Reviews and Protocols) #31#18 or #27 Publication Year from 2018 to 2019, in Cochrane Reviews (Reviews and Protocols)
Database of Abstracts of Reviews of Effects, part of the Cochrane Library
Searched 2009 to 2016 [5 records]. Final issue. No new content added.
#1[mh "Antisocial Personality Disorder"] #2((asocial* or antisocial* or anti next social* or dissocial* or dis next social* or dyssocial* or dys next social*) next/5 (person* or disorder*)):ti,ab,kw #3(self next defeating or masochistic):ti,ab,kw #4multi next impulsiv*:ti,ab,kw #5((moral* or amoral or "a‐moral") near/5 (character* or personalit*)):ti,ab,kw #6[mh ^"Multiple Personality Disorder"] #7[mh Narcissism] #8narciss*:ti,ab,kw #9(sociopath* or socio next path*):ti,ab,kw #10(psychopath or psychopaths or psychopathic*):ti,ab,kw #11(psycho next path or psycho next paths or psycho next pathic*):ti,ab,kw #12[mh sadism] #13sadis*:ti,ab,kw #14(self next defeating or masochist*):ti,ab,kw #15"Cluster B":ti,ab,kw #16"F60.2":ti,ab,kw #17"301.7":ti,ab,kw #18{or #1‐#17} #19[mh "Disruptive, Impulse Control, and Conduct Disorders"] #20[mh Aggression] #21[mh "Impulsive behavior"] #22((aggress* or conduct* or deceitful* or disruptiv* or impulsiv* or irritab* or reckless*) next/5 (person* or disorder*)):ti,ab,kw in Cochrane Reviews (Reviews and Protocols) #23{or #19‐#22} #24[mh ^"personality disorders"] #25(personalit* near/3 disorder*):ti,ab,kw #26#24 or #25 #27#23 and #26 #28#18 or #27 Publication Year from 2009 to 2016, in Other Reviews
ClinicalTrials.gov (www.clinicaltrials.gov/ct2/home)
Searched 3 October 2016 (14 records) Searched 3 November 2017 for trials registered between 1 October 2016 and 3 November 2017 (1 record) Searched 4 October 2018 for trials registered between 3 November 2017 and 4 October 2018(3 records) Searched 5 September 2019 for trials registered between 4 October 2018 and 5 September 2019 (3 records)
antisocial personality disorder | Interventional Studies
ICTRP (apps.who.int/trialsearch/AdvSearch.aspx)
Searched all years 3 October 2016 (41 records) Searched 3 November 2017 for trials registered between 1 October 2016 and 3 November 2017 (5 records) Searched 4 October 2018 for trials registered between 3 November 2017 and 4 October 2018 (10 records) Searched 5 September 2019 for trials registered between 4 October 2018 and 5 September 2019 (3 records)
antisocial personality OR antisocial AND disorder OR antisocial AND behaviour
WorldCat (theses only; www.worldcat.org)
Searched 3 October 2016 (6 records) Searched 2016 to 31 October 2017 (3 records) Searched 2017 to 4 October 2018 (1 record) Searched 2018 to 5 September 2019 (3 records)
KW: ("ANTISOCIAL PERSONALITY DISORDER" OR "ANTI‐SOCIAL PERSONALITY DISORDER ") AND KW:(TREAT* OR RANDOM* OR THERAP* OR INTERVENTION*)
Appendix 2. Data extraction form
Psychological interventions for antisocial personality disorder
Source
| Corresponding number on journal article: | Trial ID (e.g. Plizska 2000): |
| Trial registry with ID (search www.clinicaltrials.gov from 2008 and apps.who.int/trialsearch/Default.aspx from 2004): | |
| Full citation: | |
| Form filled by (date, name): | |
| Author contact information: | |
| Other publications on same study: | |
| Publication type: | |
| Country of origin: | |
| ID: Identifier | |
Eligibility
| Confirm eligibility: yes/no/awaiting |
| At least 5 or more AsPD participants: yes/no |
| AsPD: Antisocial personality disorder |
Correspondence
| Correspondence required: yes/no |
Method
| Corresponding number on journal article: | How randomised (individual/cluster)?: | Participants receiving:
|
| Location (e.g. hospital, outpatient clinic): | ||
| Summary (method): | An X‐week trial with X arms: |
| Methods | Allocation: Blinding: Duration of trial: Duration of participation: Setting: Phases: Intended follow‐up period: Validated instruments used: Unvalidated instruments used: |
| Participants | Number of participants screened: |
|
Control group Method of recruitment of participants: Number of participants included (male, female): Number of participants followed up: Number of withdrawals (reason): Diagnosis of AsPD (DSM/ICD): Means of assessment: Mean age (range): in years IQ: Ethnicity: Pre‐existing substance misuse (specify if drugs/alcohol): Other comorbid diagnoses: | |
|
Experimental group Method of recruitment of participants: Number of participants included (male, female): Number of participants followed up: Number of withdrawals (reason): Diagnosis of AsPD (DSM/ICD): Means of assessment: Mean age (range): in years IQ: Ethnicity: Pre‐existing substance misuse (specify if drugs/alcohol): Other comorbid diagnoses: | |
| Inclusion criteria met | |
| Exclusion criteria met | |
| Interventions |
Experimental group Treatment name: Delivery (small/large group vs Individual): Number randomised to experimental condition: Duration (days/weeks/months): Concomitant psychotherapy: Concomitant pharmacotherapy: Adherence to treatment regimen: |
|
Control/comparison group Comparison name: Number randomised to group: Duration (days/weeks/months): Concomitant psychotherapy: Concomitant pharmacotherapy: Adherence to treatment regimen: | |
| Outcomes (if possible, identify if outcomes are immediate (within 6 months), short‐term (> 6 months to 24 months), medium‐term (> 24 months to 5 years) and long‐term (beyond 5 years)) |
Primary
|
Secondary
| |
|
Statistical results Reported means, standard deviation, standard errors, confidence intervals, F values or P values and range for key variables: |
| Notes | Sample size calculation: |
| Power (under/adequately powered): | |
| Ethics approval: | |
| Comments from study authors | |
| Limitations of study | |
| Strengths of study | |
| Key conclusion of study authors | |
| Supplemental information regarding/data received through personal email correspondence with the authors in month/year |
| Any additional comments you would like to make about this study: |
Risk of bias
| Item | Quote to support decision | Risk of bias (low, unclear, high) |
| Random sequence generation/generation of allocation sequence (selection bias) | ||
| Allocation concealment (selection bias) | ||
| Blinding of personnel to intervention received (performance bias) | ||
| Blinding of participants to intervention received (performance bias) | ||
| Blinding of outcome assessment (detection bias) | ||
| Incomplete outcome data (ITT, imputation method) (attrition bias) | ||
| Selective outcome reporting (according to protocol?) (selection bias) | ||
| Treatment adherence | ||
| Allegiance bias | ||
| Attention bias | ||
| Vested interest (funding or author affiliations or both) | ||
| Publication bias | ||
| Language bias | ||
| Other sources of bias | ||
| ITT: intention‐to‐treat | ||
Appendix 3. Detailed outcomes
Primary outcomes
There were five studies that did not report on any of the primary outcomes defined in the protocol for this review (Gibbon 2009): Woody 1985; McKay 2000; Messina 2003; Havens 2007; and Asmand 2015. Of these, only Asmand 2015 and Messina 2003 had data available for participants with antisocial personality disorder (AsPD).
Aggression
Five studies included aggression as an outcome, and used self‐report or psychometric questionnaires (or both) to assess levels of state or trait aggression. Two studies included self‐reported aggression as an outcome: Davidson 2009 summarised the number of participants reporting any incident of physical or verbal aggression , measured with the MacArthur Community Violence Screening Instrument interview, plus additional questions on four other behaviours (shouting angrily at others; threatening harm to others; causing damage to property; self‐harm); while Thylstrup 2015 used scores on the Self‐Report of Aggression and Social Behaviour Measure and the 12‐item, short‐form, Buss‐Perry Aggression Questionnaire. Two studies, Tarrier 2010 and Feigenbaum 2012, used the Overt Aggression Scale (OAS) and modified version of the OAS, respectively. One study, Bernstein 2012, assessed levels of institutional violence via aggression and other incident records but did not report aggression data.
Reconviction
Four studies included reconviction as an outcome. Marlowe 2007 assessed re‐arrests and convictions using state criminal justice databases (but had no data available for the subgroup of participants with AsPD); Nathan 2019 assessed the number and type of officially recorded offending according to the Police National Computer (PNC) (data were obtained for every offence recorded on the PNC between the point of initial release until the completion of the study; and Woodall 2007 reported drink‐driving reconviction using data from the New Mexico State Citation Tracking System. Two studies included recidivism, non‐convicted offences or incarceration as an outcome: Bernstein 2012 reported recidivism as a component of an overall 'negative outcome'; and Nathan 2019 assessed non‐convicted offences and incident reporting of antisocial behaviour using the Self‐Reported Delinquency scale.
Global state functioning
Three studies included global state functioning as an outcome: Bernstein 2012 reported a global outcome for participants as positive, negative or neutral, whereas McMurran 2016 and Tyrer 2004 used the Global Assessment of Functioning scale.
Social functioning
Eight studies included self‐reported social functioning as an outcome. Tyrer 2004; Huband 2007; Davidson 2009; and McMurran 2016 reported mean scores on the Social Functioning Questionnaire. Bernstein 2012 reported the number of days to participants gaining supervised and unsupervised leave, while Tarrier 2010 assessed participants' interpersonal style via the Chart of Interpersonal Reactions in Close Living Environments. Neufeld 2008 reported composite scores on the family/social domain of the Addiction Severity Index (ASI), and Ball 2005 reported scores using the same measure but with no data available for the subgroup with antisocial personality disorder. The ASI is a semi‐structured interview designed to assess problem severity in seven areas commonly affected by substance misuse difficulties, one of which is termed the family/social domain. Investigators obtained composite scores for this domain, ranging from zero to one, based on problems reported in the last 30 days. Other domains relevant to this review are those concerning alcohol use, drug use and employment problems (see 'Substance misuse' below under 'Secondary outcomes').
Adverse events
Seven studies reported on adverse events: Feigenbaum 2012 reported self‐harm and suicide attempts; Marlowe 2007 noted the absence of any study‐related adverse events; McMurran 2016 reported incidents of death, self‐harm and hospitalisation; Nathan 2019 reported incidents of death ; Priebe 2012 reported the number of days and type of self‐harm; Thylstrup 2015 reported number of deaths and incarceration; and Tyrer 2004 reported number of completed suicides and frequency of self‐harm episodes via the Parasuicide History Interview.
Secondary outcomes
Studies varied widely in their use of the secondary outcomes considered in this review.
Quality of life
Three studies reported quality of life as an outcome measure: McMurran 2016 used the European Quality of Life‐5 Dimensions to calculate quality‐adjusted life‐years; Priebe 2012 reported scores on the Manchester Short Assessment of Quality of Life; and Tyrer 2004 reported scores on the Euro Quality of Life.
Engagement with services
Four studies reported on engagement with services as an outcome. Bernstein 2012 reported use of the Treatment Engagement Rating Scale for Forensic Outpatient Treatment; Havens 2007 reported numbers entering into drug addiction treatment services; McMurran 2016 reported the number of completers and non‐completers, and the mean number of weeks in the trial; and Neufeld 2008 reported adherence to counselling sessions.
Satisfaction with treatment
Only one study, Davidson 2009, examined satisfaction with treatment as an outcome: the investigators used a semi‐structured interview to enquire about 'satisfaction with taking part in study' and rated responses on a Likert scale from 1 to 7.
Leaving the study early
Thirteen studies reported on leaving the study early, measuring this as the number/proportion of participants discontinuing treatment before endpoint. Of these 13, only four studies had data available for participants with AsPD (Messina 2003; Neufeld 2008; Davidson 2009; Thylstrup 2015).
Substance misuse
To aid interpretation, we considered 'substance misuse' as two separate outcomes: 'substance misuse ‐ drugs' and 'substance misuse ‐ alcohol' (see section on Differences between protocol and review). Five studies examined 'substance misuse ‐ drugs' using the drug use domain of the ASI (Woody 1985; McKay 2000; Marlowe 2007; Neufeld 2008; Thylstrup 2015), the Cocaine Relapse Interview (McKay 2000), and urinalysis (McKay 2000; Messina 2003; Marlowe 2007; Neufeld 2008). Five studies examined 'substance misuse ‐ alcohol' using the alcohol use domain of the ASI (McKay 2000; Neufeld 2008; Thylstrup 2015), the Alcohol Use Disorders Identification Test (Davidson 2009) , the Form 90 (a time‐line follow‐back self‐report method to assess drinking over the previous 90 days), and the Drinker Inventory of Consequences (Woodall 2007). In addition, Woodall 2007 reported the frequency of drink‐driving in 30 days prior to arrest, or in previous 30 days, measured via questionnaire.
Employment status
Two studies considered employment status: McMurran 2016 reported number of days in employment over the assessment period and the number of days lost from work as a result of health problems (absenteeism); while Neufeld 2008 reported mean composite scores on the employment domain of the Addiction Severity Index.
Housing/accommodation status
None of the 19 included studies considered housing/accommodation status as an outcome.
Economic outcomes
Four studies considered direct economic outcomes: Davidson 2009 examined the total cost per participant of healthcare, social care and criminal justice services, measured using case records and the Client Service Receipt Inventory (CSRI); McMurran 2016 and Priebe 2012 reported the cost of services (direct and indirect) for health and social care service utilisation using CSRI, although neither study presented data for the subset with AsPD; McMurran 2016 also examined the cost impact of absence from work ; and Tyrer 2004 calculated total costs per participant, including costs incurred by all service‐providing sectors and productivity losses resulting from time off work due to illness, although with no data available for the subgroup with dissocial personality disorder. One additional study, Feigenbaum 2012, provided indirect economic outcomes in the form of service use (e.g. inpatient bed days, accident and emergency department visits) but did not attribute costs to these data, while another study, Bernstein 2012, mentioned economic outcomes in the discussion section of their study only but did not provide any data.
Impulsivity
Two studies measured self‐reported trait impulsivity using mean scores on the Barratt Impulsiveness Scale (BIS) (Huband 2007) and BIS‐II (Tarrier 2010).
Anger
Four studies included a self‐reported measure of anger: Davidson 2009 provided mean scores on the Novaco Anger Scale and Provocation Inventory (NAS‐PI); Feigenbaum 2012 and Huband 2007 provided mean anger expression index scores using the State‐Trait Anger Expression Inventory (STAXI) (STAXI for Feigenbaum 2012 and STAXI‐2 for Huband 2007); and Tarrier 2010 reported scores on the NAS.
Mental state
Nine studies measured general mental state. Two studies reported depression scores using the Beck Depression Inventory (BDI) (Woody 1985) or BDI‐II (Feigenbaum 2012). Eight studies measured both anxiety and depression symptoms using the 'Beck Anxiety Questionnaire' (sic) (Beck Anxiety and Depression Scale) (Asmand 2015) or the Hospital Anxiety and Depression Rating Scale (Davidson 2009; McMurran 2016); or generally using the Brief Symptom Inventory (Ball 2005; Priebe 2012), the Symptoms Checklist (Woody 1985; Bernstein 2012), or the Brief Psychiatric Rating Scale (Tarrier 2010; Priebe 2012). One study, Feigenbaum 2012, reported total scores on the Clinical Outcomes in Routine Evaluation‐Outcome Measure and post‐traumatic stress disorder symptoms.
Nine studies measured psychiatric symptoms. Four studies assessed early maladaptive schemas and schema modes using the Early Maladaptive Schema Questionnaire‐Research (Ball 2005), Young Schema Questionnaire‐Short version (Tarrier 2010; Bernstein 2012), Schema Mode Inventory (Bernstein 2012), or the Brief Core Schema Scales (Davidson 2009). Ball 2005 also reported on interpersonal problems via the Inventory of Interpersonal Problems and on the severity of personality disorder via the Personality Diagnostic Questionnaire. Bernstein 2012 additionally reported personality disorder symptoms on the Structured Interview for DSM‐IV Personality Disorders, and patient and informant versions of Schedule for Nonadaptive and Adaptive Personality. Feigenbaum 2012 and Huband 2007 assessed dissociation using the Dissociative Experiences Scale. Huband 2007 also reported on shame using the Experience of Shame Scale, and both Huband 2007 and McMurran 2016 reported on social problem‐solving ability via Social Problem Solving Inventory‐Revised. Priebe 2012 reported borderline personality disorder symptoms using Zanarini Rating Scale for Borderline Personality Disorder and Tarrier 2010 reported antisocial personality traits using the Antisocial Personality Questionnaire.
Other relevant outcomes
Asmand 2015 reported illogical/irrational beliefs using the 'Jones Illogical Beliefs Questionnaire' (sic) (Jones Irrational Belief Questionnaire). Therapy retention was measured as total weeks in treatment (Ball 2005), as adherence to counselling sessions (Neufeld 2008) or as the proportion therapeutically transferred over to routine care due to poor/partial treatment response in response to ongoing drug use or poor attendance to scheduled services (Neufeld 2008). The mean number of continuing care sessions attended was additionally reported by McKay 2000 , and McMurran 2016 also examined the strength of the therapeutic alliance using the Working Alliance Inventory . Risk of violence was assessed by Bernstein 2012 and Tarrier 2010 using the Historical Clinical Risk Management ‐ 20 and the Violence Risk Scale; Bernstein 2012 also used the Short‐term Assessment of Risk and Treatability, and Tarrier 2010 also used the Institutional Behaviour Rating Scale.
Data and analyses
Comparison 1. Cognitive behavioural therapy + treatment‐as‐usual versus treatment‐as‐usual alone.
Comparison 2. Impulsive lifestyle counselling + treatment‐as‐usual versus treatment‐as‐usual alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Aggression: scores on Buss‐Perry Aggression Questionnaire (BPAQ) at 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.2 Aggression: scores on Buss‐Perry Aggression Questionnaire (BPAQ) at 9 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.3 Adverse events: death between 3‐month and 9‐month follow‐up | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.4 Adverse events: incarceration during follow‐up period | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.5 Leaving the study early: number at 3 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.6 Leaving the study early: number at 9 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3. Contingency management + standard maintenance versus standard maintenance alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Social functioning: mean family/social domain scores (high = poor); ASI; at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.2 Leaving the study early | 2 | 127 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.28, 1.24] |
| 3.3 Substance misuse (drugs): numbers with cocaine‐negative specimens; at 17 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.4 Substance misuse (drugs): numbers with cocaine‐negative specimens; at 26 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.5 Substance misuse (drugs): numbers with cocaine‐negative specimens; at 52 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.6 Other: proportion transferred to routine care due to poor treatment response (high = poor); by 6 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 4. 'Driving whilst intoxicated' program + incarceration versus incarceration alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Reconviction: reconviction for drink‐driving; Cox regression of rearrest rates; at 24 months | 1 | Hazard Ratio (IV, Fixed, 95% CI) | Totals not selected |
Comparison 5. Schema therapy versus treatment‐as‐usual.
Comparison 6. Social problem‐solving therapy + psychoeducation versus treatment‐as‐usual alone.
Comparison 7. Dialectical behaviour therapy versus treatment‐as‐usual.
Comparison 8. Cognitive behavioural therapy + standard maintenance versus standard maintenance alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Leaving the study early | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.2 Substance misuse (drugs): numbers with cocaine‐negative specimens; at 17 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.3 Substance misuse (drugs): numbers with cocaine‐negative specimens; at 26 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.4 Substance misuse (drugs): numbers with cocaine‐negative specimens; at 52 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 9. Contingency management + cognitive behavioural therapy + standard maintenance versus standard maintenance alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Leaving the study early | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.2 Substance misuse (drugs): numbers with cocaine‐negative specimens; at 17 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.3 Substance misuse (drugs): numbers with cocaine‐negative specimens; at 26 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.4 Substance misuse (drugs): numbers with cocaine‐negative specimens; at 52 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 10. Rational emotive behaviour therapy versus treatment‐as‐usual.
Comparison 11. Psychosocial risk management ('Resettle programme') versus treatment‐as‐usual.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 11.1 Recidivism: total official offences at 2 years post‐release | 1 | Other data | No numeric data | |
| 11.2 Recidivism: total official offences at 2 years, corrected for time in the community | 1 | Other data | No numeric data | |
| 11.3 Recidivism: binary outcome (no offences vs 1 or more offences) for official offences at 2 years post release | 1 | Other data | No numeric data | |
| 11.4 Recidivism: binary outcome (no offences vs 1 or more offences) for official offences at 2 years post release, corrected for time in the community | 1 | Other data | No numeric data | |
| 11.5 Recidivism: total antisocial behaviour assessed with the Self‐report Delinquency Scale | 1 | Other data | No numeric data | |
| 11.6 Adverse event: death during study period | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 11.7 Leaving the study early: participants not included in ITT analysis of primary outcome | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by year]
Woody 1985.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: methadone‐maintained male outpatients with AsPD and opioid dependencea Sex: all males Age: (for whole samplea) mean = 29 years (SD = 6) Unit of allocation: individual participant Number randomised: 50 with AsPD (breakdown by treatment group not availablea) Number completing: not availablea Setting: outpatient; single site; urban; USA (Philadelphia) Inclusion criteria: male; aged 18 to 55 years; meeting Food and Drug Administration requirements for methadone maintenance treatment; had been receiving methadone for at least 2 weeks but not more than 6 months during their current treatment episode; subgroup met DSM‐III criteria for AsPD (obtained via MPI and SADS) Exclusion criteria: psychosis; persistent or clinically significant organic brain syndrome; serious medical, legal or personal problems that would require movement from local area within 1 year Ethnicity: (for whole samplea) black (62%); white (38%) Baseline characteristics: (for whole samplea) lifetime major depressive disorder (35%); lifetime anxiety disorder, any (20%); lifetime alcoholism (19%); antisocial personality disorder (45%) |
|
| Interventions | Three conditions: supportive‐expressive psychotherapy (SE) + standard maintenance (SM); cognitive behavioural therapy (CBT) + SM; or SM only
Details of conditions:
Duration of intervention: 24 weeks Duration of trial: 28 weeks Length of follow‐up: participants were not followed up after the end of treatment. |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
aAlthough the study recruited a subgroup with antisocial personality disorder (50/110 had DSM‐III AsPD), investigators did not provide pre/post data nor effect sizes for AsPD participants in the control condition. They reported “(t)he DC group was not included in the present analysis as our major interest was in comparing response to psychotherapy among the various diagnostic subgroups” (p 1083, column 2). Thus, no data extractable on any AsPD subgroup Study funding: National Institute of Drug Abuse and the National Institute of Mental Health Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk |
Quote: "Patients were randomly assigned to three treatment conditions. . ." (p 1082, column 1). Comment: No further information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Comment: No information provided. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Low risk |
Quote: "Addiction Severity Interviews were done by independent technicians who were not part of the treatment staff and were not aware of patients group assignments" (p 1082, column 2). Comment: Review authors judged that blinding of outcome assessors was adequate for this outcome and that it was unlikely that this blinding could have been broken. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Unclear whether there were missing outcome data for the AsPD control condition and, if so, whether the numbers of and reasons for such missing data were balanced across intervention groups. Review authors unable to make a judgement unless data from AsPD control condition become available |
| Selective reporting (reporting bias) | Low risk | Comment: Review authors judged that the published report included all expected outcomes, including those that were prespecified. |
| Other bias | Low risk | Comment: The study appeared to be free of other sources of bias. Review authors noted that, although participants were not paid for attending sessions, they could receive up to USD 55 for completing all the measures required over the course of the project. The case for this was argued in the paper. Review authors considered that this is unlikely to have introduced a source of bias. |
McKay 2000.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: male outpatients with cocaine dependence Sex: all males Age: (for AsPD subgroupa) mean = 41.2 years (SD = 6.8) Unit of allocation: individual participant Number randomised: (for AsPD subgroup) 46 (no details on numbers randomised to each conditiona) Number completing: no details for AsPD subgroupa Setting: outpatient; single sites; urban; USA (Philadelphia) Inclusion criteria: male; diagnosis of cocaine dependence (DSM‐III‐R; SCID); cocaine use in the 6 months before entrance into the IOPb; willingness to participate in research; literacy at approximately the fourth‐grade level; not homeless Exclusion criteria: history of psychotic disorder requiring antipsychotic medication; current severe dementia Ethnicity: (for AsPD subgroup) African‐American (89.1%); white (6.5%); other (4.3%) Baseline characteristics: (for AsPD subgroupa) veterans = 100%; in education for a mean of 12.6 (SD = 1.5) years; lifetime alcohol dependence = 84.8%; lifetime major depression = 46.7%; mean duration regular cocaine use = 7.9 (SD = 5.6) years; mean duration of regular drinking = 17.6 (SD = 9.1) years |
|
| Interventions | Two conditions: individualised relapse prevention (IRP); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: mean = 20 weeks Duration of trial: 17 months Length of follow‐up: follow‐up at 3, 6 and 12 months following treatment |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
a46 participants out of 127 (36.2%) who were randomised had AsPD under DSM‐III‐R. Details on characteristics of, and outcomes for, this subgroup have been requested from trial investigators. bBefore entering aftercare, trial investigators reported that most patients participated in a 4‐week Intensive Outpatient Program (IOP; 5 days/week, 3 hours/day) at the Philadelphia Veterans Administration Medical Center. Treatment was focussed on overcoming denial, fostering participation in self‐help groups, and providing information about the process of addiction and cues to relapse. Study funding: National Institute on Drug Abuse Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk |
Quote: "An urn randomization procedure was used. . . which balanced the groups on five potential prognostic factors (marital status, employment status, race, site of initial treatment, and completion of the IOP within the standard 4‐week period)" (p 289). Comment: Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | High risk |
Comment: Outcome assessors not blinded Quote: “Baseline and follow‐up interviews were conducted by research personnel who had received extensive training in the use of the assessment instruments. . . these interviewers had not been informed of the study hypotheses but they had been informed of treatment condition” (McKay 1997, p 781, column 1). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Unclear whether there were missing outcome data for the AsPD subgroup and, if so, whether the numbers of and reasons for such missing data were balanced across intervention groups. Review authors unable to make a judgement unless data from AsPD subgroup were available |
| Selective reporting (reporting bias) | Low risk | Comment: Review authors judged that the published report included all expected outcomes, including those that were prespecified. |
| Other bias | Low risk | Comment: The study appeared to be free of other sources of bias. In terms of baseline imbalance, a significantly lower percentage of those in the intervention group were married compared to the controls, but as the groups were equivalent on percentages of those living with a romantic partner for 2 years or more, the risk of bias from this source was judged not to be significant. |
Messina 2003.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: cocaine‐dependent outpatients (with AsPD subgroup) receiving methadone maintenance treatment Sex: (for AsPD subgroup) 34/48 (71%) males; 14/48 (29%) females Age: (for AsPD subgroup) mean = 43.5 years (SD = 8.1) Unit of allocation: individual participant Number randomised: 48 (n = 14 CBT; n = 15 CM; n = 7 CM + CBT; n = 12 MM only) Number completing: 44 at 17 weeks; 41 at 26 weeks; 41 at 52 weeks Setting: outpatient, multisite (2 sites), urban, USA (Los Angeles) Inclusion criteria: cocaine dependence (DSM‐IV); receiving methadone maintenance treatment at 1 of 2 clinics for at least 90 daysa; urine sample testing positive for cocaine use during month prior to study enrolment; antisocial personality disorder (DSM‐IV, SCID‐II) for AsPD subgroup Exclusion criteria: alcohol or benzodiazepine dependence requiring withdrawal medication; received specific treatment for cocaine dependency in past 30 days; court mandated to treatment Ethnicity: (for AsPD subgroup) 31% white; 21% black; 48% Hispanic/other Baseline characteristics: described by investigators as having "relatively low motivation" (quote; p 322, column 2); 60% had completed at least 12 years of schooling; 13% had been in steady employment over last 3 years; self‐reported drug/alcohol use in the 30 days prior to admission to the study was: 60% alcohol use, 35% alcohol use to intoxication, 27% marijuana use, 79% heroin use, 31% other opiate use, 96% cocaine use and 8% amphetamine use |
|
| Interventions | Four conditions: cognitive behavioural therapy (CBT); contingency management (CM); CBT + CM; and standard maintenance (SM)
Details of conditions:
Duration of intervention: 16 weeks Duration of trial: 52 weeks (16‐week intervention + 36 weeks of follow‐up) Length of follow‐up: participants were followed up at weeks 17, 26 and 52 (i.e. weeks 1, 10 and 36 following end of intervention) Dose adjustment: none |
|
| Outcomes |
Primary outcomes
Secondary outcomes
|
|
| Notes |
aAll participants were paying for their methadone maintenance treatment (either USD140 or USD180/month depending upon centre) but received a discount of USD40/month for participating in the study. Prior to the introduction of this incentive, only 4 participants had volunteered for the study after 60 days of recruitment. Study funding: National Institute on Drug Abuse Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: Information received from trial investigators (email received 19 October 2009 confirmed that a random numbers table was used to prepare numbered sealed envelopes. Review authors judged this adequate to minimise bias. |
| Allocation concealment (selection bias) | Low risk | Comment: Information received from trial investigators (email received 19 October 2009) confirmed that allocation codes were sealed within envelopes that were opened in turn at each site at time of allocation. Only the principal investigator and project co‐ordinator had access to these envelopes. Review authors considered it unlikely that participants or any investigator enrolling participants could foresee assignment. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | High risk | Comment: Information received from trial investigators (email received 19 October 2009) confirmed that outcome assessors were not blinded to participant allocation. This may have introduced bias. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: The actual number of participants with AsPD failing to complete treatment (at 17 weeks) and to provide data relating to the key outcome (substance misuse ‐ cocaine, by urinalysis) was broadly balanced between the treatment conditions (1/14 for CBT condition; 1/15 for the CM condition, 0/7 for the CBT + CM condition, and 2/12 for the control (SM) condition). |
| Selective reporting (reporting bias) | Low risk | Comment: Study protocol was not available but it seemed clear that the published report included all expected outcomes. No evidence of selective reporting. All prospectively stated outcomes were reported. |
| Other bias | Unclear risk | Comment: Trial investigators acknowledged the presence of other psychiatric disorders in the sample; review authors did not judge this to introduce a significant risk of bias. However, whilst all participants were paying for their methadone maintenance treatment (either USD 140 or USD 180/month depending upon centre), they received a discount of USD 40/month for participating in the study. Prior to the introduction of this incentive, only 4 subjects had volunteered for the study after 60 days of recruitment. Review authors were unclear whether this payment would introduce bias. |
Tyrer 2004.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: patients with recurrent self‐harm presenting at hospital emergency departments Sex: (for whole sample) 154 males; 326 females Age: (for whole sample) mean = 31.0 years (SD = 11.0) Unit of allocation: individual participant Number randomised: 480 (for whole sample); no details for dissocial PD subgroupa Number completing: no details for dissocial PD subgroupa Setting: outpatient; 5 sites; urban; UK (Glasgow, Edinburgh, Nottingham, West London, South London) Inclusion criteria: recent episode of self‐harm and presenting at hospital emergency department; at least 1 previous episode of self‐harm; willing to provide written consent Exclusion criteria: requiring inpatient psychiatric treatment after self‐harm episode; primary diagnosis of substance dependence; psychotic or bipolar disorder Ethnicity: no information provided Baseline characteristics: (for whole samplea) any personality disorder (ICD‐10; PAS‐Q) (42.1%); paranoid PD (7.5%); schizoid PD (1.0%); dissocial PD (3.1%); impulsive PD (12.9%); borderline PD (14.0%); histrionic PD (6.7%); anankastic PD (4.0%); anxious PD (14.2%); dependent PD 11.3%) |
|
| Interventions | Two conditions: manual‐assisted cognitive behaviour therapy (MACT); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: up to 7 treatment sessions (total duration not specified) Duration of trial: one year Length of follow‐up: 6 months and 12 months post‐treatment |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
a15 participants out of 480 (3.1%) who were randomised had dissocial PD. Details of characteristics of, and outcomes for, this subgroup have been requested from trial investigators. Study funding: Medical Research Council Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk |
Quote: "The Stata software was used to generate allocation using randomly permuted blocks. . ." (Tyrer 2003, p 60) Comment: Review authors judged that an appropriate computer‐generated randomisation method was used for random sequence generation. |
| Allocation concealment (selection bias) | Low risk | Comment: Participants were randomly allocated by telephone or fax from the trial's co‐ordinating centre. Review authors judged that concealment was achieved by use of central allocation so that neither participants nor any investigator enrolling participants could foresee assignment. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Comment: Insufficient information to allow a judgement to be made. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Unclear whether there were missing outcome data for the dissocial PD subgroup and, if so, whether the numbers of and reasons for such missing data were balanced across intervention groups. Review authors unable to make a judgement unless data from dissocial PD subgroup become available |
| Selective reporting (reporting bias) | Low risk | Comment: Review authors judged that the published report included all expected outcomes, including those that were prespecified. |
| Other bias | Low risk | Comment: The study appeared to be free of other sources of bias. |
Ball 2005.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: homeless adults with substance abuse difficulties and personality disorder Sex: (for whole samplea) 49/52 (94%) males; 3/52 (6%) females Age: (for whole samplea) mean 38.3 = years (SD = 10.4, range = 19 to 57) Unit of allocation: individual participant Number randomised: 52 (for whole sample; no details for AsPD subgroupa) Number completing: no details for AsPD subgroupa Setting: outpatient; single site; urban; USA (Manhattan) Inclusion criteria: at least 18 years old; alcohol or drug use in past 30 days; diagnosis of PD (DSM‐IV; PDQb); able to read and comprehend consents and assessments; willingness to be a research participant Exclusion criteria: acute schizophrenia; bipolar disorder; organic syndrome; acute violence or suicidality; incarceration pending; actively participating in counselling at another substance abuse or mental health clinic whilst in active treatment phase Ethnicity: (for whole samplea) white (23%); Hispanic (26%); African American (49%) Baseline characteristics: (for whole samplea) never married (58%); currently married (4%); separated/divorced (33%); high school education (67%); essentially unemployed for prior 3 years (26%); some full‐time or part‐time work in prior 3 years (49%); alcohol as primary misuse substance (50%); illicit drugs as primary misuse substance (50%); average age of diagnosis onset for alcohol abuse 23.5 (SD = 7.8, median = 22) years; average age of diagnosis onset for drug abuse 21.0 (SD = 5.8, median = 19) years; cluster A PD diagnosis (88%); cluster B PD diagnosis (74%); cluster C PD diagnosis (85%); no period of stable living arrangements over last 3 years (27%) |
|
| Interventions | Two conditions: dual focus schema therapy (DFST); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: 24 weeks Duration of trial: 9 months Length of follow‐up: 3 months following end of treatment (although investigators reported "successful follow up in the sample proved to be extraordinarily difficult to achieve"; quote, p 374, column 1) |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
a24 participants out of 52 (47%) who were randomised had AsPD. Details of characteristics of, and outcomes for, this subgroup have been requested from trial investigators. bTrial investigators noted significant missing data for PDQ scores: “because of a major computer malfunction, the personality disorder profiles of 16 of the participants could not be recovered” (quote; p 373, column 1) Study funding: Jacob and Valeria Langeloth Foundation Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk |
Quote: "after completion of baseline assessments, subjects were randomly allocated to 1 of 2 study treatments" (p 374, column 1). Comment: no further details reported. Clarification about method of sequence generation has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Insufficient information to allow a judgement to be made. Clarification about method of allocation concealment has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not that they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Comment: Insufficient information to allow a judgement to be made. Clarification about blinding of outcome assessors has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: The trial investigators noted significant missing data for PDQ scores "because of a major computer malfunction, the personality disorder profiles of 16 of the participants could not be recovered" (quote; p 373, column 1). Although review authors considered this could have introduced bias for one outcome (severity of PD), this was not one of the primary or secondary outcomes addressed in this review. Unclear whether there were missing outcome data for the AsPD subgroup and, if so, whether the numbers of and reasons for such missing data were balanced across intervention groups. Review authors unable to make a judgement unless data from AsPD subgroup become available |
| Selective reporting (reporting bias) | High risk | Comment: Investigators did not report endpoint or follow‐up data for 3 outcomes, measured with the Early Maladaptive Schema Questionnaire, the Inventory of Interpersonal Problems and the Addiction Severity Index. |
| Other bias | Low risk | Comment: The study appeared to be free of other sources of bias. |
Havens 2007.
| Study characteristics | ||
| Methods | Design: cluster‐randomised controlled trial | |
| Participants |
Participants: intravenous drug users (subgroup with AsPD) attending an outpatient needle exchange programme Sex: 68% males (for whole sample, including non‐AsPD) Age: median = 38 years (for whole sample, including non‐AsPD) Unit of allocation: sitea Number randomised: 10 sites, 254 participants (for whole sample, including non‐AsPD) (breakdown by treatment condition not supplied) Number completing: 162 (n = 74 intervention group; n = 88 control group) (for whole sample, including non‐AsPDb) Setting: outpatient; multisite (10 sites); urban; USA (Baltimore) Inclusion criteria: diagnosis of AsPD (DSM‐IV, SCID‐II); intravenous drug user participating in the Baltimore needle exchange programme Exclusion criteria: none reported Ethnicity: (for whole sample, including non‐AsPD) 76% black Baseline characteristics: 19% current major depressive disorder; 14% current generalised anxiety disorder; Addiction Severity Index mean score 0.23; 28% HIV positive; 31% had entered opiate agonist treatment |
|
| Interventions | Two conditions: strengths‐based case management (SBCM‐subsequently split in to SBCM of 5 to 24 minutes duration, or SBCM of at least 25 minutes duration); or control
Details of conditions:
Duration of intervention: median treatment duration of SBCM was 25 minutes Duration of trial: 1 month Length of follow‐up: 1 month Dose adjustment: n/a |
|
| Outcomes |
Primary outcomes
Secondary outcomes
|
|
| Notes |
aRandom allocation was by site. Havens 2007 did not clarify this, but an earlier report of the same study (Strathdee 2006) stated “To limit contamination participants were randomised by NEP site. Specifically, at the beginning of the study NEP site was randomised to receive the intervention (case management) or control condition (passive referral). Approximately halfway through the recruitment period, a 1 month washout period was scheduled during which time no participants were recruited. After washout, sites originally randomised to case management received the control intervention and vice versa until the end of enrolment.” (quote; p 226, column 1) bFigures given for AsPD subgroup not provided, except that 37 of those completing 1‐month follow up had AsPD. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. cWhole sample only, no AsPD subgroup Study funding: National Institute on Drug Abuse Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: No information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Comment: No information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Comment: Insufficient information to allow a judgement to be made. Clarification about blinding of outcome assessors has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Unclear whether there were missing outcome data for the AsPD subgroup and, if so, whether the numbers of and reasons for such missing data were balanced across intervention groups. Review authors unable to make a judgement unless data from AsPD subgroup become available. |
| Selective reporting (reporting bias) | Low risk | Comment: Review authors judged that the published report included all expected outcomes, including those that were prespecified. |
| Other bias | Unclear risk | Comment: There is the possibility of bias arising from baseline imbalance in that the median age of first injection (of drugs) was greater in the control group than in the intervention group. |
Neufeld 2008.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: outpatients with AsPD and opioid dependency Sex: 77/100 (77%) males; 33/100 (33%) females Age: mean = 39 years (SD = 7.1) Unit of allocation: individual participant Number randomised: 100 (n = 51 experimental group; n = 49 control group) Number completing: 86 (n = 42 experimental group; n = 44 control group) Setting: outpatient, single site, urban, USA (Baltimore) Inclusion criteria: antisocial personality disorder (DSM‐III‐R; SCID‐II); opioid dependence (DSM‐III‐R; SCID‐I) Exclusion criteria: pregnancy; bipolar disorder; schizophrenia Ethnicity: 40/100 (40%) Caucasian Baseline characteristics: all participants recruited from local addiction treatment programme; 75/100 (75%) were new admissions to the programme and 25/100 (25%) were already in treatment and responding poorly; 12/100 (12%) married; 34/100 (34%) employed; mean = 10.7 years (SD = 2.1) in education; 72/100 (72%) income less than USD 500 per month; all participants met criteria for both lifetime and current opioid use disorder (includes both dependence and abuse); 95/100 (95%) met criteria for lifetime cocaine use disorder and 49/100 (49%) current cocaine use disorder; 82/100 (82%) met criteria for lifetime alcohol use disorder and 18/100 (18%) current alcohol use disorder; 58/100 (58%) met criteria for lifetime sedative use disorder and 11/100 (11%) current sedative use disorder; 74/100 (74%) met criteria for lifetime cannabis use disorder and 12/100 (12%) current cannabis use disorder; 41/100 (41%) met criteria for lifetime other stimulants use disorder and 0/100 (0%) current other stimulants use disorder; 38/100 (38%) met criteria for lifetime hallucinogen use disorder and 1/100 (1%) current hallucinogen use disorder; 35/100 (35%) met criteria for lifetime axis I diagnosis and 25/100 (25%) current axis I diagnosis; 28/100 (28%) met criteria for axis II diagnosis (presumably other than AsPD); 46/100 (46%) met criteria for any axis I or II diagnosis |
|
| Interventions | Two conditions: contingency‐based behavioural programme; or standard maintenance
Details of conditions:
Duration of intervention: 6 months Duration of trial: 7 months (initial 4‐week baseline evaluation period followed by 6 months of randomised treatment) Length of follow‐up: none Dose adjustment: dose of methadone was adjusted according to protocol as determined by group membership (see above) |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
Study funding: National Institute on Drug Abuse Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: Information received from trial investigators (email to NH received 17 November 2009) confirmed that sequence generation was by coin toss. |
| Allocation concealment (selection bias) | Low risk | Comment: Information received from trial investigators (email to NH, received 17 November 2009) indicated that the nature of the allocation process was such that allocation status could not have been predicted or foreseen by the participants or any investigator enrolling participants. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Low risk | Comment: Information received from trial investigators (email to NH, received 17 November 2009) confirmed that the laboratory technicians who tested the urines were not privy to the study design or group assignment, that the data entry people who collated attendance did not know the assignment of the patient, and that the research staff who collected the ASI questionnaire data over the course of the study did not know to which arm of the study the patient was assigned. Review authors judged that blinding of outcome assessors was adequate and that it was unlikely that this blinding could have been broken. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: For urinalysis results, 31% of data missing from experimental group and 33% of data missing from control group. Investigators reported that missing data were equally distributed across study conditions, but reasons were not given. For ASI results, 9/51 (18%) data missing from experimental group and 5/49 (10%) missing from control group. Review authors unable to judge whether reasons for missing data differed substantially across the groups or if reasons for missing outcome data were likely to be related to true outcome. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Comment: Review authors judged that the published report included all expected outcomes, including those that were prespecified. |
| Other bias | Low risk | Comment: The study appeared to be free of other sources of bias. Investigators commented that the presence of a therapeutic transfer procedure may have reduced drug abuse in order to avoid transfer to a more intensive routine treatment allocation, although investigators reported that this dropout rate is comparable to other studies of opioid‐dependent subjects. |
Woodall 2007.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: incarcerated drink‐driving offenders with AsPD sentenced to a Driving While Intoxicated (DWI) treatment programme Sex: (for AsPD subgroup) 45/52 (87%) males; 7/52 (13%) females Age: (for AsPD subgroup) mean = 26.5 years (SD = 7.9) Unit of allocation: individual participant Number randomised: 52 (n = 36 intervention group; n = 16 control group) Number completing: 52 (n = 36 intervention group; n = 16 control group) Setting: prison, single site, USA (New Mexico) Inclusion criteria: court‐defined first offenders sentenced to the Driving While Intoxicated (DWI) treatment programme whilst in prison; diagnosis of AsPD (DSM‐III‐R, Diagnostic Interview Schedule) Exclusion criteria: none reported Ethnicity: (for AsPD subgroup) 37/52 (71%) Native American; 12/52 (23%) Non‐Hispanic white; 3/52 (6%) Hispanic or other Baseline characteristics: 42/52 (89%) met DSM‐III‐R criteria for alcohol dependency using the Diagnostic Interview Schedule; mean DrinC score = 23.8 (SD 9.9); mean number of days drinking in past 30 days = 9.2 (SD 8.4) days; mean number of days in last 30 days when had drank and then driven = 3.9 (SD 5.3) days; mean number of drinks per drinking day = 5.9 (SD 5.1); mean number of days with 5 or more drinks = 5.9 (SD 6.9); mean number of days driving after 5 or more drinks = 2.9 (SD 4.3); Form 90 measures of drinking over past 90 days: total standard ethyl‐alcohol consumption (SEC) = 328.0 (SD 431.3), drinking days = 25.7 (SD 26.3), mean blood alcohol content (BAC) = 0.043 (SD 0.058) |
|
| Interventions | Two conditions: 'driving whilst intoxicated' programme (DWI) + incarceration; or incarceration only
Details of conditions:
Duration of intervention: 28 days Duration of trial: 25 months (1 month of intervention and 24 months of follow‐up) Length of follow‐up: 6, 12 and 24 months Dose adjustment: n/a |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
Study funding: National Institute on Alcohol Abuse and Alcoholism Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: No information provided. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Comment: No information provided. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Comment: Insufficient information to allow a judgement to be made. Clarification about blinding of outcome assessors has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: For the outcome of self‐reported drink‐driving behaviour, data missing for 6/36 (17%) of the intervention group and for 3/16 (19%) of control group. Although these numbers appear similar, reasons for this missing data were not provided. For the outcome of alcohol use, the amount of missing self‐report data was not reported but review authors judged it reasonable to assume that the above figures also applied to this as it was measured similarly. For the outcome of drink‐driving recidivism, it was unclear what numbers of missing data occurred in the AsPD subgroup, although for the entire sample missing data on this item was reported as 31/305 (10%). Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Comment: Study protocol was not available but it seemed clear that the published report included all expected outcomes. No evidence of selective reporting. All prospectively stated outcomes were reported. |
| Other bias | Unclear risk | Comment: In terms of baseline imbalance, the intervention group was significantly more likely to have histories of drinking and driving in comparison with the controls, although it was unclear if this applied to the AsPD subgroup. |
Huband 2007.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: community living adults with personality disorder Sex: (for AsPD subgroupa) 18 males; 6 females Age: (for AsPD subgroupa) mean = 34.4 years (SD = 8.4) Unit of allocation: individual participant Number randomised: (for AsPD subgroup) 24 (13 = intervention, 11 = control) Number completing: not reported; used last‐observation‐carried‐forward Setting: outpatient; 5 sites; urban and rural; UK (East Midlands) Inclusion criteria: presence of at least one personality disorder (DSM‐IV; IPDE); age 18 to 65 years; literacy and cognitive functioning sufficient to allow engagement with the intervention; able to provide written informed consent Exclusion criteria: major functional psychosis Ethnicity: no information on ethnicity reported for AsPD subgroup Baseline characteristics: for whole sample, including non‐AsPD participants: 49/176 (27.8%) visited Accident and Emergency (A + E) for any reason in the previous 6 months; 25/176 (14.2%) visited A + E due to self‐harm in the previous 6 months; 21/176 (11.9%) psychiatric hospital admission in the previous 6 months; mean number of contacts with a psychiatrist/month in the last 6 months 0.21 (intervention) and 0.27 (control group); mean number of contacts with other mental health staff/month in the last 6 months 0.63 (intervention) and 0.83 (control group). For the AsPD subgroupa: 4/24 (16.7%) AsPD as the only personality disorder; 20/24 (83.3%) AsPD comorbid with at least one other personality disorder |
|
| Interventions | Two conditions: brief individual psychoeducation plus problem‐solving group sessions; or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: mean = 24 weeks (range = 21 to 28) Duration of trial: mean = 24 weeks (range = 21 to 28) Length of follow‐up: none |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
a24 (13.6%) of all 176 participants in the sample had AsPD. Of these, 13 were allocated to intervention and 11 to control conditions. Data from this AsPD subgroup supplied by trial investigators Study funding: National Programme for Forensic Mental Health R&D and the Home Office Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: Research investigators described a block randomisation procedure using computer‐generated random numbers provided by an independent statistician. Review authors judged this adequate to minimise bias. |
| Allocation concealment (selection bias) | Low risk | Comment: Allocation codes pre‐sealed into identical, sequentially numbered, opaque envelopes that were opened in sequence by research staff with trial coordinator masked to allocations. Review authors considered it unlikely that participants or any investigator enrolling participants could foresee assignment. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Outcome measures were self‐report questionnaires completed by participants who were not blind to their own allocation status and were scored by research assistants who could have been aware of this allocation status in some cases. In view of this uncertainty, review authors considered a judgement of 'unclear' to be appropriate as some possibility of bias remains. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Data from the AsPD subgroup supplied by trial investigators indicated that at the end of the trial 4 of 13 (30.8%) were missing from the intervention condition and 3 of 11 (27.3%) were missing from the TAU condition (all outcomes). Reasons for missing data (and any differences in the reasons between conditions) were not available. Feedback from trial investigators confirmed that missing data occurred where clients declined to complete endpoint questionnaires. Although no further information was available on why these clients declined to participate in this task, review authors considered the reasons for missing data were reasonably likely to be balanced across the treatment conditions. |
| Selective reporting (reporting bias) | Low risk | Comment: Review authors judged that the published report included all expected outcomes, including those that were prespecified. |
| Other bias | Unclear risk | Comment: Trial investigators noted that outcomes were based on measurements at just two time points (baseline and endpoint) so may be open to bias from those participants in either a very optimistic or pessimistic state of mind. They also noted that 20 of 24 (83.3%) participants had at least one other personality disorder. There was also the possibility of bias arising from baseline imbalance in that those in the intervention group were significantly more likely to have had psychiatric hospitalisation at some time in their life in comparison with the controls (although they were not significantly more likely to have been hospitalised in the previous 6 months). |
Marlowe 2007.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: adults charged with a drug‐related offence and admitted to a pre‐adjudication court Sex: (for whole samplea) 75% males; 25% females Age: (for whole samplea) mean = 25.1 years (SD = 8.4) Unit of allocation: individual participant Number randomised: 279 (for sample as a whole; no details for AsPD subgroupa) Number completing: no details for AsPD subgroupa Setting: outpatient; single site; urban; USA (Wilmington, Delaware) Inclusion criteria: at least 18 years old; admitted to a misdemeanour (pre‐adjudication) drug court located in Wilmington, Delaware, USA; having pleaded guilty to the initial charge (the plea of guilty was held in abeyance pending graduation or termination from the programme); charged with possession or consumption of cannabis, possession of drug paraphernalia, possession of hypodermic syringes, or driving under the influence; resident in New Castle County, Delaware or committed his/her offence there Exclusion criteria: having a history of a violent offence involving serious injury to a victim or use of a deadly weapon Ethnicity: (for whole samplea) white (60%); African American (35%) Baseline characteristics: (for whole samplea) unmarried (94%); employed (66%); currently abusing cannabis (68%); currently abusing alcohol to intoxication (47%); currently abusing stimulants or cocaine (14%), opiates (13%) or hallucinogens (3%) |
|
| Interventions | Two conditions: optimal (‘matched’) schedule of court hearings; or standard (‘unmatched’) schedule court hearings
Details of conditions:
Duration of intervention: minimum 14 weeks, although clients required on average approximately 9 months to satisfy all the conditions for graduation Duration of trial: 15 months (9 months to graduation plus 6 months post‐discharge) Length of follow‐up: 6 months post‐discharge |
|
| Outcomes |
Primary outcomes
Secondary outcomes
|
|
| Notes |
aInvestigators used diagnosis of AsPD as one criterion in the assessment of risk. Diagnosis of AsPD was via an antisocial personality disorder interview derived from SCID‐II. Characteristics of, and outcomes for, this subgroup have been requested from trial investigators. Study funding: National Institute on Drug Abuse Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: No information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Comment: No information given. Insufficient reporting to permit judgement of Yes or No. Clarification has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Comment: Insufficient information to allow a judgement to be made. Clarification about blinding of outcome assessors has been requested from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Unclear whether there were missing outcome data for the AsPD subgroup and, if so, whether the numbers of and reasons for such missing data were balanced across intervention groups. Review authors unable to make a judgement unless data from AsPD subgroup were available |
| Selective reporting (reporting bias) | Low risk | Comment: Review authors judged that the published report included all expected outcomes, including those that were prespecified. |
| Other bias | Unclear risk | Comment: Review authors unable to judge unless data from the AsPD subgroup become available. It is important to note, however, that the diagnosis of AsPD was via an 'antisocial personality disorder interview' derived from SCID‐II by the trial investigators, but with no evidence that this has been validated. This may have introduced bias. |
Davidson 2009.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: male outpatients with AsPD and recent verbal/physical violence Sex: all males Age: mean = 37.9 years (SD = 10.4) Unit of allocation: individual participant Number randomised: 52 (n = 25 CBT + TAU; n = 27 TAU only) Number completing: 41 (n = 20 CBT + TAU; n = 21 TAU only) at 12 months Setting: outpatient; multisite (2 sites); urban; UK (Glasgow and London) Inclusion criteria: male; aged 18 to 65 years; diagnosis of AsPD (DSM‐IV; SCID); living in community; endorsement of at least one item on MacArthur Community Violence Screening Instrument (MCVSI); interviewed in 6 months prior to baseline; able to provide written informed consent Exclusion criteria: currently receiving a systematic psychological therapy; insufficient knowledge of English to participate/understand; diagnosis of psychosis (schizophrenia or bipolar‐affective disorder); currently receiving inpatient treatmenta Ethnicity: 35/52 (67%) white Baseline characteristics: 51/52 (98%) reported verbal aggression in previous six months; 45/52 (87%) reported physical aggression against others in previous 6 months; mean = 4.9 (SD = 20.4) days in psychiatric hospital in previous 12 months; mean age at first contact with psychiatric services = 19.8 (SD = 12.5) years; mean age at first trouble with law = 14.3 (SD = 7.6) years; mean total Drug and Alcohol Screening Test score = 5.7 (SD = 4.4); mean age at leaving school = 15.6 (SD = 1.4) years; mean number of months in work during last 5 years = 16.5 (SD = 22.9) months; 38/52 (73%) unemployed at entry into study; 37/52 (71%) assessed as at least below average literacy on Test of Word Reading Efficacy |
|
| Interventions | Two conditions: cognitive behavioural therapy plus treatment‐as‐usual (CBT + TAU); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: 6 months or 12 months (see note 2). Participants who were randomised to CBT + TAU were further randomly allocated to treatment over either 6 months as 15 x 1‐hour sessions (n = 12) or 12 months as 30 x 1‐hour sessions (n = 13) Duration of trial: 12 monthsb Length of follow‐up: Participants were not followed up beyond end of trial at 12 months. |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
aInvestigators did not list substance dependency as an exclusion criterion. Trial investigators have, however, confirmed (telephone conversation between SG and Prof Davidson on 14 August 2009) that 3 participants who were obviously physically dependent on drugs or alcohol (or both) to such an extent that they were unable to co‐operate with the trial were excluded and referred on to appropriate substance abuse services. bFeedback from trial investigators (telephone conversation between SG and Prof Davidson on 14 August 2009) confirmed that one aim in this feasibility study was to determine whether clients would comply best with a 6‐ or 12‐month intervention. Investigators reported no difference at baseline between those who received the 6‐month and those who received the 12‐month intervention, and that the two groups were not analysed separately. Study funding: Medical Research Council Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk |
Comment: Web‐based system used to generate the allocation sequence with stratification by centre Quote: "randomisation schedule was constructed using the method of randomised permuted blocks of size four. Randomisation was conducted using a web‐based system" (p 570). After contacting the investigators (telephone conversation between SG and Prof Davidson on 14 August 2009), review authors judged that an appropriate computer‐generated randomisation method was used for random sequence generation. |
| Allocation concealment (selection bias) | Low risk |
Quote: "the randomisation schedules were generated by the study data centre. . . and kept securely and confidentially by the trial coordinator at the study coordinating centre in Glasgow. The trial coordinator informed the referring agent of the result of the randomisation immediately and in writing, and then contacted the CBT therapists in each area with the participants details so that CBT could be initiated" (p 570). Comment: Review authors judged that concealment achieved by use of central allocation so that participants and any investigator enrolling participants could not foresee assignment. |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Low risk |
Quote: "the research assistants on each site carried out all the assessments at 3‐monthly intervals until the participant exited the trial (after 12 months) and were blind to allocation" (p 571). Comment: Review authors judged that blinding of outcome assessors was adequate and that it was unlikely that this blinding could have been broken. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Number missing varied across the 4 time points for all outcomes, although at each time point the numbers missing were approximately balanced across the groups. At the final time point (i.e. endpoint at 12 months), there were 5/25 (20%) missing from the CBT group and 6/27 (22%) missing from the TAU group. Reasons for missing data (and any differences in the reasons between groups) were not reported. Feedback from trial investigators (telephone conversation between SG and Prof Davidson on 14 August 2009) confirmed that missing data occurred where clients declined to participate and did not attend. Although no further information was available on why these clients declined to participate, review authors considered the reasons for non‐participation were reasonably likely to be balanced across the treatment conditions. |
| Selective reporting (reporting bias) | Low risk | Comment: Investigators noted that three additional behaviours were assessed ('shouting angrily at others'; 'threatening to harm others'; 'causing damage to property'), but the published report did not appear to fully report the results of these besides noting that "overall, no differences were found between those randomised to CBT or TAU on any of the measures at 12‐month follow‐up" (quote; p 574). However, feedback from trial investigators (telephone conversation between SG and Prof Davidson on 14 August 2009) confirmed that 'shouting angrily at others' and 'threatening to harm others' were reported together as 'verbal aggression', and that 'causing damage to property' was included in outcome 'number reporting any act of physical aggression'. |
| Other bias | Low risk | Comment: Review authors judged study to be free of other forms of bias despite the analysis being partial rather than true intention‐to‐treat. |
Tarrier 2010.
| Study characteristics | ||
| Methods | Design: parallel randomised control trial | |
| Participants |
Participants: male patients aged 18‐70 from the personality disorder service of a UK high secure hospital Sex: 100% male Age: (for whole samplea) schema modal therapy (SMT) + treatment‐as‐usual (TAU) (mean = 41.8 years, SD = 9.92); treatment‐as‐usual (TAU) (mean = 42.74 years, SD = 12.44) Unit of Allocation: individual Number randomised: 63 for whole sample (AsPD subsample = 43)a; schema modal therapy + TAU group (n = 29; AsPD subgroup = 18); TAU group (n = 34; AsPD subgroup = 25) Number completing: 35a; Schema modal therapy + TAU group (n = 15, 51.7%); TAU group (n = 20, 58.8%) Setting: high secure psychiatric hospital; Ashworth Hospital, National Health Service, England, UK Inclusion criteria: at least one diagnosis on Structured Clinical Interview for DSM‐IV Axis II personality disorder (SCID‐II); consent from clinical team; consent from patient Exclusion criteria: current symptoms of psychotic illness or an organic brain syndrome; IQ of less than 80; patient due to be transferred; patient in seclusion Ethnicity:a white Caucasian: schema modal therapy + TAU n = 26/29 (89.7%); TAU n = 29/34 (85.3%) Baseline characteristics:a)
|
|
| Interventions | Two conditions: schema modal therapy (SMT); or treatment‐as‐usual (TAU)
Details of conditions:b
Duration of intervention: 24 months Duration of trial: 36 months Length of follow‐up: 6, 12, 24 and 36 months after baseline |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
a18/29 (62%) patients randomised to SMT, and 25/34 (74%) of patients randomised to TAU had a diagnosis of AsPD; no data for AsPD subsample bParticipants in both groups also received social, occupational and recreational activities that were not classed as formal therapy. Study funding: Ministry of Justice Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was conducted independently via a remote telephone randomisation service based at Christie’s Hospital, Manchester, with the purpose of avoiding any potential bias in treatment group allocation." (p 6) |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomisation was conducted independently via a remote telephone randomisation service based at Christie’s Hospital, Manchester, with the purpose of avoiding any potential bias in treatment group allocation." (p 7) |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not that they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Low risk | Quote:"A number of safeguards were put in place to try and ensure that independent researchers were blinded to treatment allocation. These included: anonymised data sets; using separate offices and administrative procedures; instructing patients not to reveal details of their care; data entry being carried out independent of the assessors; sanitising clinical notes to remove any reference to psychological treatment received before being used in assessments; and using coding systems for treatment groups." (p 7) |
| Blinding (performance bias and detection bias) of outcome assessors | Low risk | Quote: "The Evaluation Team were independent of the Treatment Team who provided the SMT intervention." (p 6) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote:"All statistical analyses of treatment effects were carried out using the Intention‐To‐Treat principle. That is, outcomes were compared for participants as they were randomised and not according to the treatment or interventions that they actually received. Outcomes at the four different follow‐up times (6, 12, 24 and 36 months) were analysed simultaneously in a repeated measures analysis, using all available data." (p 9) |
| Selective reporting (reporting bias) | Unclear risk | Comment: Review authors judged that the published reports did not include data on all expected outcomes; e.g. data for the Institutional Behaviour Rating Scale was not reported. |
| Other bias | High risk | Comment: Review authors identified a number of additional sources of potential bias. Allegiance bias: funding had been secured to develop an SMT service within the personality disorder service. Publication bias; the trial was conducted in 2004‐08, reported initially in a Ministry of Justice paper in 2010 and then in a peer review publication in 2016; the delay in publication of this trial could be a result of the null findings of the impact of SMT. Treatment bias: treatment adherence in terms of competence of therapists in the SMT condition was reported as poor; additionally, participants in the TAU group received more therapy than the intervention group: "When the numbers of therapies received by the SMT + TAU and TAU groups were compared, the TAU group received a significantly higher number of therapies than the SMT + TAU group (10 v 6.76: t = 2.21, p = 0.03) and a significantly higher mean number of therapies than the SMT + TAU group (mean .91 v.61: t = 2.21, p = 0.03) across the 11 quarters of the study period." (quote; p 14) |
Bernstein 2012.
| Study characteristics | ||
| Methods | Design: parallel randomised controlled trial | |
| Participants |
Participants: male forensic patients with personality disorder Sex: male Age: (for sample as a wholea) mean = 41.3 years (SD = 8.5) Unit of Allocation: individual Number randomised: 33 (for sample as a wholea); schema therapy = 16; control group = 14; unknown = 3 Number completing: 30; schema therapy = 16; control = 14 Setting: seven government‐run forensic psychiatric clinics (terbeschikkingstelling (TBS)) in Netherlands Inclusion criteria: male patients with antisocial, borderline, narcissistic or paranoid personality disorder; personality disorder‐not otherwise specified, if patient had at least five cluster B symptoms and no other Axis II PD diagnosis Exclusion criteria: other personality disorders (e.g. histrionic personality disorder); presence of current psychotic symptoms, schizophrenia or bipolar disorder; current drug or alcohol dependence; low intelligence (full scale IQ < 80); serious neurological impairment (e.g. dementia); autistic spectrum disorder; paedophilia Ethnicity: not reported Baseline characteristics: (for sample as a wholea)
|
|
| Interventions | Two conditions: schema therapy (ST); or treatment‐as‐usual (TAU)
Details of conditions:
Both groups also received concomitant therapy such as: individual or group psychotherapy, art therapy, relapse prevention programmes for addiction and aggression, pharmacological interventions, vocational training, milieu therapy Duration of intervention: 3 years Duration of trial: 6 yearsb Two phases: 3‐year treatment phase (3‐year follow‐up phase = not reported) Length of follow‐up: noneb |
|
| Outcomes |
Primary outcomesb
Secondary outcomes
Other outcomes
|
|
| Notes |
a26/30 (87%) of trial completing participants had AsPD; no data for AsPD sub‐sample bThe authors only reported preliminary results as follow‐up phase is ongoing. Study funding: Netherlands Ministry of Justice, the Expertise Center for Forensic Psychiatry, Maastricht University’s Faculty of Psychology and Neuroscience, and the participating forensic hospitals Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random assignment is accomplished using an “adapted biased urn procedure”(Schouten, 1995), which randomly assigns patients to treatment conditions at each site using an algorithm that assures that the overall proportion of patients in the experimental and control condition will be in equal balance." (p 317, column 2) |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients are assigned by a central research assistant who is blind to any information about the patient." (p 317, column 2) |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study.We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Quote: "Raters were not kept blind to treatment condition, as this was not feasible in a three‐year study in clinical settings." (p 319, column 1) |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Quote: "...that research assistants were not blind to the patients’ treatment conditions." (p 322, col.1). Inter‐rater agreement between blind and non‐blind ratings were provided for risk assessment scores for a subsample: "In a sub‐sample of 16 patients, the interrater reliability (intra‐class correlation (ICC) for the average of two raters) for the HCR‐20 overall judgment of the risk level within the hospital was.81; there was perfect agreement for ratings of risk level outside of the hospital (ICC = 1.0). The interrater reliability for the PCL‐R total score was ICC = .88; ratings were also internally consistent (Cronbach’s alpha = .80)." (p 319, column 1) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "We did not use intention‐to‐treat analysis, as there were no missing data for these analyses." (p 319, column 2) |
| Selective reporting (reporting bias) | High risk | Comment: Stated outcome measures including aggression (institutional violence) and engagement with treatment (TER) were not reported, however the trial investigators reported "Finally, as this report is preliminary in nature, we did not provide full information about all aspects of the research design (e.g., number of sessions of ST versus TAU) or the results; we will provide further details when we publish our complete findings." (quote; p 322, column 2). |
| Other bias | Unclear risk | Comment: The review authors considered that there was a potential risk of allegiance bias in this study as ST for forensic patients was developed by D. Bernstein and T. Kersten (unclear risk). Vested interest bias: unvalidated instruments developed by DB were used in the study (unclear risk). |
Feigenbaum 2012.
| Study characteristics | ||
| Methods | Design: randomised control trial | |
| Participants |
Participants: referrals to a new specialist personality disorder service Sex: (for sample as a wholea) female (n = 30/41, 73%); male (n = 11/41, 27%) Age: (for sample as a wholea).
Unit of Allocation: cluster (balancing for geographic, demographic (gender) and diagnostic criteria (presence of borderline personality disorder)); for every 3 patients randomised, 2 assigned to DBT and 1 to TAU Number randomised: 41 (for sample as a wholea). DBT group n = 25; TAU group n = 16 Number completing: 31 (for sample as a wholea). DBT group n = 17; TAU group n = 14 Setting: National Health Service (NHS) specialist personality disorder service; London, UK Inclusion criteria: diagnosis of cluster B personality disorder; aged 18‐65 years old; provide written consent Exclusion criteria: currently in long‐term psychotherapeutic treatment; meet DSM‐IV criteria for comorbid psychotic disorder or bipolar disorder; opiate dependence requiring specialist treatment; mental impairment; evidence of organic brain disorder Ethnicity: not stated Baseline characteristics (for sample as a wholea)
|
|
| Interventions | Two conditions: dialectical behaviour therapy (DBT); or treatment‐as‐usual (TAU) (2:1 allocation)
Details of conditions:
Duration of intervention: 55‐58 weeks Duration of trial: 20 months Length of follow‐up: 12 months after baseline |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
a11/41 of randomised participants (27%) had a diagnosis of AsPD; no data for AsPD subsample bDue to comorbidity of personality disorders, percentages summed to more than 100%. Study funding: Camden and Islington Health Authority and North Thames Regional Health Authority Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Treatment allocation was made offsite via telephone randomization using a stochastic minimization programme (MINIM) balancing for sector within the regions to avoid differences in terms of differential referral practices, gender, and presence of BPD." (p 124) |
| Allocation concealment (selection bias) | Low risk | Quote: "Treatment allocation was made offsite via telephone randomization using a stochastic minimization programme (MINIM) balancing for sector within the regions to avoid differences in terms of differential referral practices, gender, and presence of BPD. Clients were randomized so that two of three entered DBT and one of three TAU in order to build the caseloads for staff, as this was a new service with no existing clients." (p 124) |
| Blinding (performance bias and detection bias) of participants | High risk |
Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not that they were participating in a psychological intervention and may also be aware of the nature of this intervention. Quote: "Patients in the TAU group were informed that they would receive DBT in 1 year, if they still wished for this therapy." (p 125) Comment:The review authors considered that this statement increased the risk of bias that might result from differential behaviours by participants in the TAU and DBT groups. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | High risk | Quote:"...while we attempted blinding of assessments, as is often the case with psychosocial treatment trials, those carrying out the research assessments could mostly identify the treatment group of the patient." (p 137) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment:The trial investigators reported DBT data withdrawal (n = 1) and conducted an ITT analysis. The paper did not provide adequate information on statistical processes to make a judgement of Yes or No. |
| Selective reporting (reporting bias) | Unclear risk | Comment: It was unclear if the study was subject to selective reporting as no protocol was available. It should be noted however that there was considerable time between the study completion and publication of the results in a peer‐reviewed journal. |
| Other bias | Unclear risk |
Comment:
|
Priebe 2012.
| Study characteristics | ||
| Methods | Design: parallel randomised control trial | |
| Participants |
Participants: individuals who self‐harm and have a diagnosis of at least one personality disorder referred from primary, secondary and tertiary health services to dialectical behaviour therapy (DBT) service Sex: (for whole samplea) female (n = 70/80, 87.5%); male (n = 10/80, 12.5%) Age: (for whole samplea) Intervention group, dialectical behaviour therapy (DBT) (mean age = 33.0 years, SD = 10.7); control group, treatment‐as‐usual (TAU) (mean age = 31.3 years, SD = 11.0) Unit of Allocation: individual Number randomised: 80 (for whole samplea) DBT group (n = 40; AsPD subgroup n = 6); TAU group (n = 40; AsPD subgroup n = 9) Number completing: 74 (for whole sample) (AsPD subgroup n = 14) DBT group (n = 38; AsPD subgroup n = 5); TAU group (n = 36; AsPD subgroup n = 9) Setting: outpatient; National Health Service DBT service; London Borough of Newham, England, UK Inclusion criteria: five days or more with self‐harm in the year prior to treatment; age 16 years or over; diagnosis of at least one personality disorder (DSM‐IV criteria using SCID‐II) Exclusion criteria: severe learning difficulties; inability to read or write English Ethnicity: (for whole samplea) DBT group: white (n = 26, 65%); black (n = 4, 10%); Asian (n = 8, 20%), mixed/other (n = 2, 5%). TAU group: white (n = 20, 50%): black (n = 8, 20%); Asian (n = 9, 22.5%); mixed/other (n = 3, 7.5%) Baseline characteristics: (for whole samplea) Employment: unemployed (n = 43/80, 56%); voluntary/protected/sheltered work (n = 8/80, 10%); regular employment (n = 29/80, 37%). Accommodation: homeless or 24‐hour supervised accommodation (n = 6/80, 8%); sheltered/supported accommodation (n = 6/80, 8%), independent accommodation (n = 68/80, 84%). Psychiatric diagnoses: number of patients with Axis I disorder (n = 63/80); number of Axis 1 disorders (mean 8.0, SD 3.1); number of patients with Axis II disorders (n = 80/80, 100%); number of Axis II disorders (mean 3.5, SD 1.6). Self‐harm and suicide: number of patients with suicide attempts in past 12 months (n = 79/80, 98.8%); number of suicide attempts in past 12 months (mean 2.2, SD 6.0); number of patients with self‐harm days in past 2 months (n = 78/80, 97.5%); number of self‐harm days in past 2 months (mean 13.9, SD 18.4). |
|
| Interventions | Two conditions: dialectical behaviour therapy (DBT) or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: 12 months Duration of trial: 26 months (March 2008 to May 2010) Length of follow‐up: follow‐up every 2 months until 12 months after baseline |
|
| Outcomes |
Primary outcomes
Secondary outcomes
|
|
| Notes |
aEmail correspondence with Kirsten Barnicot on 24 January 2017 established that 15/80 participants (18.75%) who were randomised had a diagnosis of AsPD; limited data for AsPD sub‐sample at baseline and 2‐month follow‐up (number of days self‐harm; BPRS total score; BSI total score) provided by KB on 02 March 2017. Study funding: National Institute for Health Research Declaration of interests: None |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was computer generated with a 1: 1 allocation by an independent statistician, using 6 blocks of 12 randomly permuted treatment allocation sequences, with a final block of 8." (p 358) |
| Allocation concealment (selection bias) | Low risk | Quote:"Randomisation was computer generated with a 1: 1 allocation by an independent statistician, using 6 blocks of 12 randomly permuted treatment allocation sequences, with a final block of 8." (p 358) |
| Blinding (performance bias and detection bias) of participants | Unclear risk |
Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not that they were participating in a psychological intervention and may also be aware of the nature of this intervention. Quote: "Participants allocated to the TAU condition were referred back to the referrer and encouraged to engage in any kind of treatment other than DBT..." (p 358). "...referring those allocated to TAU back to their original referral sources following randomisation may have had a negative impact on participants, which may have augmented any negative outcomes observed in this group..." (p 362). Comment: The review authors found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Quote: "Due to the nature of the questions researchers asked regarding service use, coupled with the frequency of contact between researchers and participants (every 2 months) it was impractical to blind researchers to allocation; this may have biased the way in which the interviews were conducted." (p 362) |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Quote:"The cost assessment included questions on service use which revealed the patients’ allocation to the DBT or TAU group. Interviewers were therefore not masked to treatment allocation. However, the data analyst remained masked throughout the study period." (p 358) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: The trial investigators reported using an ITT analysis based on 38/40 DBT and 36/40 TAU participants; baseline data is missing for 2 TAU, follow‐up data is missing for 2/40 DBT and 2/40 TAU, however the investigators reported that they "...conducted a sensitivity analysis with last observation carried forward." (quote; p 358). The investigators anticipated a high treatment dropout and planned a priori subgroup analyses of completers vs. dropouts; they note an effect of treatment completion on their primary outcome of self‐harm: ."..only 48% of patients allocated to the DBT group completed the envisaged 1‐year treatment period, and the reduction of self‐harm was substantially greater for those who completed the intervention than for those who did not." (quote; p 362). |
| Selective reporting (reporting bias) | Unclear risk | Comment: The review authors were unable to locate a published protocol for this study and therefore there was insufficient information to allow a judgement to be made. All outcomes measures described in the method section were reported by the trial investigators. |
| Other bias | Low risk | Comment: The study appeared to be free of other sources of bias. |
Thylstrup 2015.
| Study characteristics | ||
| Methods | Design: parallel, randomised control trial | |
| Participants |
Participants: new and existing patients with AsPD receiving outpatient treatment for drug or alcohol problems Sex: male (n = 124/142, 87%); female (n = 18/142, 13%); data only for the participants who completed the study; no data provided for the 176 randomised patientsa Age: (for sample as a wholea) mean age = 32.2 years (SD = 8.9) Unit of Allocation: cluster; stratified by clinic; randomised permuted blocks or randomly varying size with ratio 1:1 (4 or 6 per block) Number randomised: 176; impulsive lifestyle counselling (ILC) + treatment‐as‐usual (TAU) = 96; TAU = 80 Number completing: 142 patients completed at least 1 follow‐up; ILC + TAU = 78; TAU = 64 Setting: community‐based substance abuse treatment centres across 13 municipalities of Denmark Inclusion criteria: outpatients aged 18 to 65; meet AsPD criteria using Mini International Neuropsychiatric Interview (MINI); able to provide written informed consent; seeking/already in treatment for a substance use disorder Exclusion criteria: patient has plans that would interfere with participation in psychoeducation in next 3 months (e.g. moving away, prison, residential rehab); participating in group treatment with another subject in trial; known to suffer from acute psychosis; severe brain damage; does not speak Danish Ethnicity: no information given Baseline characteristics:
|
|
| Interventions | Two conditionsb: impulsive lifestyle counselling (ILC); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: 6 sessions, time period not reported Duration of trial: 31 months; January 2012 to July 2014. Length of follow‐up: follow‐up at 3 months and 9 months |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
aData analysed for the 142 participants who completed at least one follow‐up (79% of whole group). b36.5% of whole group received opioid substitution treatment at the point of randomisation. Study funding: Trygfonden, and Reckitt‐Benckiser Declaration of interests: None |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization schedules were generated by the trial coordinator and kept secure and confidential at the study coordinating center in Copenhagen. The randomization schedule was constructed using the method of randomized permuted blocks of randomly varying size with a ratio of 1:1 (4 or 6 per block)." (p 3) |
| Allocation concealment (selection bias) | Unclear risk | Quote:"The trial coordinator informed the referring clinician of the result of randomization immediately after being notified that the patient had been assessed and was found to be eligible for study participation. After this, the clinician informed the patient of the result. In the cases in which patients were randomized to the ILC treatment, the clinician then contacted one of the ILC counsellors at the uptake unit with the participants’ details so that the sessions could be initiated as quickly as possible. Because the randomization had to take place immediately after the assessment interview, the trial coordinator was unable to check whether the baseline assessment was complete before randomizing, and patients with incomplete data at baseline had to be excluded after randomization." (p 3). |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: Participants were not blind. The trial investigators reported that patients were informed of the result of the randomisation by the clinician undertaking the baseline eligibility assessments. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Quote:"The trial coordinator informed the referring clinician of the result of randomization immediately after being notified that the patient had been assessed and was found to be eligible for study participation... ... In the cases in which patients were randomized to the ILC treatment, the clinician then contacted one of the ILC counsellors at the uptake unit with the participants’ details so that the sessions could be initiated as quickly as possible." (p 3) |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk |
Quote: "Research technicians not affiliated with the clinics carried out all assessments at the 3 and 9‐month follow‐up interviews and were blind to treatment group allocation." (p 5). Comment: The review authors noted that there was no reference to the blinding of the data analysts and therefore insufficient information to allow a judgement to be made. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Authors reported it was an ITT analysis but it was not clear that this was the case as 176 were randomised but they only analysed data for subjects who completed baseline data (167) and then completed at least one follow‐up (142). |
| Selective reporting (reporting bias) | Unclear risk | Comment: Trial information on the ISRCTN register indicated additional secondary outcome measures that are not reported in the 2015 paper: perceived help for antisocial personality disorder (reported in 2017 post hoc secondary analysis only); readiness to change antisocial behaviour measured using the adapted readiness ruler; and staff‐rated improvement in in‐clinic antisocial behaviour, general antisocial behaviour and substance use. |
| Other bias | Unclear risk | Comment: Vested interest bias (funding and/or author affiliations): although not a pharmacological trial, the study was partially funded by grant from Reckitt‐Benckiser who manufacture an opioid replacement drug. Some subjects in the trial were administered opioid substitution treatment. |
Asmand 2015.
| Study characteristics | ||
| Methods | Design: parallel randomised control trial | |
| Participants |
Participants: adult prisoners with antisocial personality disorder Sex: all male Age: in the DBT group 37.5% were aged 20‐25 years; REBT group 50% were aged 20‐25 years; control group range 18‐40 years Unit of Allocation: individual Number randomised: 48 (DBT = 16, REBT = 16, control = 16) Setting: Ilam Prison, Irana Inclusion criteria: AsPD diagnosis; aged 18‐40 years; conviction length > 1 year Exclusion criteria: two episodes of non‐compliance Ethnicity: not stated Baseline characteristics:
|
|
| Interventions | Three conditions: dialectical behavioural therapy (DBT); rational emotive behavioural therapy (REBT); or control
Details of conditions:
Duration of intervention: 16 sessions over 20 daysc Duration of trial: 20 weeks Length of follow‐up: 20 days after initial therapy sessionc |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
aThe review authors have concerns about possible ethical issues, given the particular setting and circumstances of the prisoners in this study. bThe authors provided a very poor description of the two interventions offered and their mode of delivery; the TAU control group may have received individual work but no details were provided. cThe intervention duration was unclearly reported, possibly 16 sessions of 1 hour, possibly over 20 days (1 day per week over a 20‐week period) Study funding: none Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Investigators reported use of random number table in the study protocol, however the randomisation process was not reported in the paper. Insufficient reporting to permit judgement of Yes or No |
| Allocation concealment (selection bias) | Unclear risk | Comment: We found no indication of any specific measures taken to address allocation concealment. Insufficient reporting to permit judgement of Yes or No |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not that they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind participants in this type of study. We found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) of personnel | Unclear risk | Comment: In a study such as this, full blinding is difficult to achieve because personnel would be aware whether or not they were participating in a psychological intervention and may also be aware of the nature of this intervention. The review authors judged that it would thus not be possible to fully blind personnel in this type of study. |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Comment: The review authors found no evidence of any measures taken to address blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Attrition from dropouts/other reasons was not reported in the paper, however there was reference to noncompliance and "...lack of cooperation of some samples and absent prison and more than two sessions..." (quote; p 2, column 2). |
| Selective reporting (reporting bias) | High risk | Comment: The trial authors reported four primary outcomes in the study protocol; irrational belief ('irrational beliefs questionnaire'), anxiety ('beke Anxiety questionnaire' [sic]), depression ('Beck Depression questionnaire') and aggression ('agrretion questionnaire' [sic]). Outcomes for depression and aggression were not reported in the paper. |
| Other bias | High risk | Comment: The review authors considered there was a high risk for language/comprehension bias as the quality of the translation into English was exceptionally poor. The review authors also had concerns regarding the recruitment and coercion of participants as all were incarcerated in prison and no ethics approvals were reported; "The specimens were randomly assigned to treatment groups of 16 persons consisted [sic] of DBT and REBT group and one control group." (quote; p 2, column 2) |
McMurran 2016.
| Study characteristics | ||
| Methods | Design: multisite, parallel randomised control trial | |
| Participants |
Participants: community‐living adults with a diagnosis of one (or more) personality disorder Sex:aIntervention group, psychoeducation and problem‐solving (PEPS): male (n = 39/154, 25%); female (n = 115/154, 75%). Control group, treatment‐as‐usual (TAU): male (n = 37/152, 24%); female (n = 115/152, 76%) Age:a intervention group (PEPS) mean age 38.6 years (SD 10.9); control group (TAU) mean 37.8 years (SD 11.0) Unit of allocation: block stratified by recruiting centre and sex; intervention to control allocation ratio was 1:1 Number randomised: 306; PEPS (n =154); TAU (n = 152) Number completing: 306 (for sample as a whole) (see notes 1 and 2) PEPS (n = 154); TAU (n = 152) Setting: multisite; community National Health Service (NHS) mental health services; United Kingdom Inclusion criteria: one or more personality disorders (this could include Personality Disorder Not Otherwise Specified, PD‐NOS); aged 18 years or over; living in the community; proficient in spoken English; capacity to provide informed consent Exclusion criteria: insufficient degree of literacy, comprehension or attention to allow engagement in therapy and assessments; currently undertaking psychological treatment for personality disorder or likely to start such treatment during the trial period; participation in any other trial Ethnicity: PEPS group: white (n = 129, 84%); mixed (n = 6, 4%); black Caribbean (n = 5, 3%); black African (n = 2, 1%); other (n = 12, 8%). TAU group: white (n = 127, 83%); mixed (n = 9, 6%); black Caribbean (n = 6, 4%); black other (n = 2, 1%); Asian Indian (n = 1, 2%); Asian other (n = 1, 1%); other (n = 6, 4%) Baseline characteristics: (for sample as a whole) (see note a) PEPS group: age left full‐time education (mean 17·2 years, SD 3·7); highest educational attainment, none (n = 24, 16%), GCSE (n = 22,14%), A‐level (n = 35, 23%), vocational (n = 10, 7%), degree (n = 36, 23%), other (n = 25, 16%), missing (n = 2, 1%); socioeconomic status, never worked and long‐term unemployed (n = 105, 68%), routine and manual occupations (n = 20, 13%), intermediate occupations (n = 9, 6%), managerial and professional occupations (n = 20, 13%); personality disorder diagnosis using International Personality Disorder Examination (IPDE), [participants may have more than one type] paranoid PD (n = 13, 8%), schizoid PD (n = 4, 3%), antisocial PD (n = 23, 15%), borderline PD (n = 93, 60%), histrionic PD (n = 2, 1%), narcissistic PD (n = 1, 1%), avoidant PD (n = 57, 37%), dependent PD (n = 4, 3%), obsessive‐compulsive PD (n = 14, 9%), personality disorder not otherwise specified (n = 14, 9%); personality disorder classification, simple PD (n = 61, 40%); complex PD (n = 93, 60%) TAU group: age left full‐time education (mean 16·9 years, SD 3·3); highest educational attainment, none (n = 29, 19%), GCSE (n = 16, 10%), A‐level (n = 45, 30%), vocational (n = 10, 7%), degree (n = 32, 21%), other (n = 20, 13%); socioeconomic status, never worked and long‐term unemployed (n = 96, 63%), routine and manual occupations (n = 28, 18%), intermediate occupations (n = 13, 9%), managerial and professional occupations (n = 15, 10%); personality disorder diagnosis using International Personality Disorder Examination (IPDE), [participants may have more than one type] paranoid PD (n = 16, 11%), schizoid PD (n = 1, 1%), antisocial PD (n = 31, 20%), borderline PD (n = 90, 59%), histrionic PD (n = 6, 4%), narcissistic PD (n = 3, 2%), avoidant PD (n = 56, 37%), dependent PD (n = 7, 5%), obsessive‐compulsive PD (n = 20, 13%), personality disorder not otherwise specified (n = 10, 7%); personality disorder classification, simple PD (n = 77, 51%), complex PD (n = 75, 49%) |
|
| Interventions | Two conditions: psychoeducation and problem solving (PEPS); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: ~16 weeks (4 weeks of psychoeducation + 12 weeks of social problem‐solving) Duration of trial: 28 monthsb (August 2010 to November 2012) Length of follow‐up:intended follow‐up period of 72 weeksb |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
aThe intervention group (PEPS) had 23/154 (15%) participants with a diagnosis of AsPD; the control group (TAU) had 31/152 (20%) of participants with an AsPD diagnosis; no data for the AsPD subsample bTrial stopped in month 30 of the recruitment phase due to safety concerns (recruitment due to be 32 months duration); no more patients were randomised after this point; patients receiving PEPS had treatment stopped and were informed of possibility of harm; all patients followed up as per trial protocol Study funding: National Institute for Health Research Health Technology Assessment Programme Declaration of interests: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was based on a computer generated pseudo‐random code using random permuted blocks of randomly varying size created by the Nottingham Clinical Trials Unit (NCTU) in accordance with their standard operating procedure and held on a secure server. The randomisation was stratified by recruiting centre and sex. The sequence of treatment allocations was concealed until recruitment, data collection, and all other trial‐related assessments were complete. The investigator, or an authorised designee, accessed the treatment allocation for each participant by means of a remote, internet‐based randomisation system developed and maintained by the NCTU. Allocation was therefore fully concealed from recruiting staff." (HTA report, p xxiv) |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomisation was based on a computer‐generated pseudo‐random code using random permuted blocks of randomly varying size, created by the Nottingham Clinical Trials Unit in accordance with their standard operating procedure and held on a secure server. Allocation was stratified by recruiting centre and sex." (quote from HTA report, p xxiv) |
| Blinding (performance bias and detection bias) of participants | High risk |
Comment: In a study such as this, full blinding is difficult to achieve because participants would be aware whether or not that they were participating in a psychological intervention and may also be aware of the nature of this intervention. Quote: "Participants, mental health workers delivering the interventions, and participants’ usual care teams were aware of the treatment allocation." (HTA report, p 16) Comment: The review authors noted that most of the outcome data were obtained from self‐report questionnaires from participants who were not blind to treatment allocation. |
| Blinding (performance bias and detection bias) of personnel | High risk | Comment: The trial investigators reported that both the mental health workers who delivered the interventions, and the usual‐care teams of participants, were aware of the participant's treatment allocation. |
| Blinding (performance bias and detection bias) of outcome assessors | Unclear risk | Quote: "...outcome measures were administered by research assistants blinded to treatment allocation in order to reduce assessment bias as far as possible. Data analysts remained blinded to allocation during the study by having access to only aggregate data and no access to data that could reveal treatment arm, such as course attendance. Final analyses were conducted using treatment labels A/B, with allocation decodes released only after completion of analyses. Data that could reveal allocation were analysed following release of allocation decodes." (p 16) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "The pattern of missing data was investigated by examining variables recorded at baseline that were associated with ‘missingness’ of SFQ score at the 72‐week follow‐up. Multiple imputation and analysis of multiple imputed data sets were conducted using ‘mi’ procedures in Stata. The imputation model contained site, age, sex, ethnicity, social status, PD category (simple or complex), SFQ at baseline and 24 weeks, baseline EQ‐5D health state score, baseline HADS score, baseline SPSI‐R score and baseline three main problems score, and 20 data sets were imputed." (p 12) |
| Selective reporting (reporting bias) | Unclear risk | Comment: The trial investigators reported 'a priori' minimum completion rates for a valid analysis ("...80% completion rate at baseline and 50% completion at follow‐up..." (quote; p 36)). Two proposed outcomes were not reported as data completion rates did not reach the prespecified level required for a valid analysis; Global Assessment of Functioning (GAF) and Working Alliance Inventory – Short Revised (WAI). |
| Other bias | Unclear risk |
Comment:
|
Nathan 2019.
| Study characteristics | ||
| Methods | Design: multisite, parallel, randomised control trial | |
| Participants |
Participants: male prisoners with personality disorder (whole sample, see notea) Sex: all male Age: (see notea) intervention group ('Resettle') mean age = 35.8 years (SD = 11.3); control group (treatment‐as‐usual; TAU) mean age = 32.6 years (SD = 11.6); total sample mean age = 34.3 years (SD = 11.5) Unit of allocation: individual participant Number randomised: (see notea) intervention (n = 38); control (n = 34) Number completing: (see note a) intervention group (Resettle: primary outcome ‐ intention‐to‐treat (ITT), n = 28; secondary outcome at y1, n = 25; secondary outcome at y2, n = 12); control group (TAU: primary outcome ITT, n = 29; secondary outcome at y1, n = 24; secondary outcome at y2, n = 11) Setting: prison and community in the North West of England Inclusion criteria: male prisoners over 18 years of age, likely to have personality disorder and identified as 'high risk' and in need of multi‐agency risk management arrangements (MAPPA) Exclusion criteria: severe intellectual impairment or psychotic mental illness identified from a review of the records or from the initial baseline assessment Ethnicity: (see note a) intervention (Resettle) group (white British ‐ 34 (89.5%); white Irish ‐ 1 (2.6%); white & black Caribbean ‐ 0; African ‐ 1 (2.6%); other mixed backgrounds ‐ 2 (5.3)); control (TAU) group (white British ‐ 33 (97.1%); white Irish ‐ 0; white & black Caribbean ‐ 1 (2.9%); African ‐ 0; other mixed backgrounds ‐ 0) Baseline characteristics: (see note a) Intervention (Resettle) group Age at first conviction: 'before age 15': n = 13 (34.2%); 'age 15‐17': n = 11 (28.9%); 'age 18 +': n = 14 (36.8%) Number of previous convictions: 13.3 (SD = 9.6) Number of previously convicted offences: 32.5 (SD = 25.4) Index offence: violent (n = 25, 65.8%), sexual (n = 10, 26.3%), burglary (n = 1, 2.6%), robbery (n = 7, 18.4%), other (n = 7, 18.4%) Psychopathy Checklist‐Screening Version (PCL‐SV): total mean score = 16.2 (SD = 4.6), facet 1 mean = 7.1 (SD = 3.0), facet 2 mean = 9.0 (SD = 3.3) Number of days from release to follow‐up: mean = 882.5 (SD = 187.1) SCL‐90 Global Severity Index: mean score = 0.85 (SD = 0.66) DSM‐IV personality disorders definite diagnosis: paranoid (n = 5, 12.2%); schizoid (n = 0); schizotypal (n = 0); antisocial (n = 34, 89.5%); borderline (n = 9, 23.7%); narcissistic (n = 1, 2.6%); avoidant (n = 1, 2.6%); obsessive compulsive (n = 0); not otherwise specified (n = 3, 7.9%) DSM‐IV personality disorders probable diagnosis: paranoid (n = 3, 7.9%); schizoid (n = 3, 7.9%); schizotypal (n = 0); antisocial (n = 2, 5.3%); borderline (n = 7, 18.4%); narcissistic (n = 0); avoidant (n = 3, 7.9%); obsessive compulsive (n = 1, 2.6%); not otherwise specified (n = 0) Control (TAU) group Age at first conviction: 'before age 15': n = 13 (38.2%); 'age 15‐17': n = 12 (35.5%); 'age 18 +': n = 9 (26.5%) Number of previous convictions: n = 14.2 (SD = 10.9) Number of previously convicted offences: n = 30.2 (SD = 27.2) Index offence: violent (n = 25, 73.5%), sexual (n = 5, 14.7%), burglary (n = 3, 8.8%), robbery (n = 7, 20.6%), other (n = 5, 14.7%) Psychopathy Checklist‐Screening Version (PCL‐SV): total mean score = 15.7 (SD = 4.5), facet 1 mean = 6.5 (SD = 3.5), facet 2 mean = 9.2 (SD = 2.4) Number of days from release to follow‐up: mean = 832.6 (SD = 144.1) SCL‐90 Global Severity Index: mean score = 0.82 (SD = 0.78) DSM‐IV personality disorders definite diagnosis: paranoid (n = 1, 2.9%); schizoid (n = 0); schizotypal (n = 1, 2.9%); antisocial (n = 31, 91.2%); borderline (n = 4, 11.8%); narcissistic (n = 2, 5.9%); avoidant (n = 1, 2.9%); obsessive compulsive (n = 2, 5.9%); not otherwise specified (n = 3, 8.8%) DSM‐IV personality disorders probable diagnosis: paranoid (n = 1, 2.9%); schizoid (n = 2, 5.9%); schizotypal (n = 0); antisocial (n = 2, 5.9%); borderline (n = 5, 14.7%); narcissistic (n = 0); avoidant (n = 1, 2.9%); obsessive compulsive (n = 1, 2.9%); not otherwise specified (n = 3, 8.8%) |
|
| Interventions | Two conditions: Resettle programme; TAU
Details of conditions:
Duration of intervention: at least 2 years 6 months (6 months prior to release, then 2 years after release) Duration of trial: variable but approximately 30‐36 months Length of follow‐up: 2 years following discharge from prison; outcomes measured at 1 year and 2 years after release |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
|
| Notes |
aIn the intervention group (n = 38), 34 participants had a definite AsPD diagnosis and 2 had a probable AsPD diagnosis. In the control group (n = 34), 31 participants had a definite AsPD diagnosis and 2 had a probable AsPD diagnosis. Reported participant demographic data are for the whole intervention group (n = 38) and control group (n = 34) bThe SRD scale is a 32‐item self‐report measure that asks respondents to indicate the frequency with which they have engaged in a wide range of antisocial behaviours (from theft to sexual or violent offending) over the previous year (Huizinga 1986), amended for use in an adult group (Palmer 2000). cRaw study data was provided by the study authors, allowing data extraction for the primary outcome to be undertaken for a 100% AsPD subsample |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was carried out by an administrator unconnected to the study using random numbers generated by the study statistician. The Minim stratified randomisation programme was utilized to minimise the imbalance between the two groups for the type of index offence (violent versus sexual offence), SCID I diagnosis of drug and alcohol abuse (presence versus absence), and the designated probation office." (p 3, column 1) |
| Allocation concealment (selection bias) | Low risk | Quote: "The administrator informed the researcher, who had undertaken the baseline assessment, of the group allocation. In turn, the researcher informed the offender manager of allocation." (p 3, column 1) |
| Blinding (performance bias and detection bias) of participants | Unclear risk | Comment: Due to the nature of the intervention, it is not possible to blind participants to their allocation; the impact of this on risk of bias is unclear. In the intervention arm: "Participants initially attended Resettle for 6 days each week. In this phase, there were two key‐worker sessions a week...." (quote, p 3, column 1) In the control arm: "Usual care involved standard probation supervision following release from prison custody. This entailed regular meetings (weekly initially) with the offender manager and engagement with other services where specified in the licence conditions. Although the offender manager may have visited the participant in prison prior to release and if he was returned, this was very limited contact in comparison to the contact between the Resettle practitioners and the participants randomised to the intervention group." (quote, p 3, column 1) |
| Blinding (performance bias and detection bias) of personnel | High risk | Comment: This is an open‐label study: the offender manager was aware of group allocation. Resettle practitioners only worked with the participants randomised to the intervention. Quote: "The administrator informed the researcher, who had undertaken the baseline assessment, of the group allocation. In turn, the researcher informed the offender manager of allocation. For control group allocation, the offender manager made usual arrangements. In the event of allocation to the intervention group, there was liaison between the offender manager and the Resettle service." (p 3, column 1) |
| Blinding (performance bias and detection bias) of outcome assessors | High risk | Quote: "Follow‐up was not conducted blindly because assignment to the treatment and control groups was evident from the contact process." (p 4) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: The attrition rate was high for the intervention and control groups. ITT was utilised in the analysis but numbers were still smaller than would be expected in the ITT and reasons for the missing numbers were unclear. E.g. Resettle: n = 38 randomised, ITT primary outcome reported as n = 28; TAU: n = 34 randomised, ITT primary outcome reported as n = 29 |
| Selective reporting (reporting bias) | High risk | Comment: primary outcome measures reported in protocol as of 13 June 2013 were significantly different from those reported in the paper. The trial register indicated that several outcome measures were administered (e.g. Inventory of Interpersonal Problems (IIP); Barratt Impulsivity Scale (BIS)) but the study only reported data for reoffending and self‐reported antisocial behaviour. Protocol primary outcomes of 13 June 2013: 1. Reoffending data (Records from Police National Computer (PNC); Probation records) Nathan 2019 primary outcome: "The primary outcome was number and type of officially recorded offending according to the Police National Computer (PNC)." (quote, p 3‐4). Secondary outcomes reported in the protocol as of 13 June 2013: 1. Antisocial behaviour (Self‐Report Delinquency (SRD) scale). 2. Personality functioning (Inventory of Interpersonal Problems (IIP); Barratt Impulsivity Scale (BIS)). 3. Psychiatric illness/symptom and substance abuse/dependency (Structured Clinical Interview for DSM‐IV (SCID I); Symptom Check List‐90‐Revised (SCL‐90‐R)) Nathan (2019) secondary outcome: "The secondary outcome measure was self‐reported antisocial behaviour. This was recorded at 1 and 2 year follow‐up assessments using the Self‐reported Delinquency Scale (SRD) (Huizinga & Elliott, 1986) amended for use in an adult group (Palmer & Hollin, 2000)." (quote, p 4 column 1) |
| Other bias | High risk |
Comment:
|
A + E = accident and emergency AIDS = acquired immune deficiency syndrome APQ = Antisocial Personality Questionnaire ASI = Addiction Severity Index AsPD = antisocial personality disorder AUDIT = Alcohol Use Disorders Identification Test BCSS = Brief Core Schema Scales BDI = Beck Depression Inventory BIS = Barratt Impulsivity Scale BPAQ‐SF = Buss‐Perry Aggression Questionnaire‐12‐Item Short‐Form BPD = borderline personality disorder BPRS = Brief Psychiatric Rating Scale BSI = Brief Symptom Inventory CBT = cognitive behavioural therapy CIRCLE = Chart of Interpersonal Reactions in Close Living Environments CM = contingency management CORE‐OM = Clinical Outcomes in Routine Evaluation‐Outcome Measure CRACMS = community risk assessment and case management service CSRI = Client Service Receipt Inventory DAST = Drug and Alcohol Screening Test DBT = dialectical behaviour therapy DC = drug counseling DES = Dissociative Experiences Scale DFST = dual‐focus schema therapy DoH = Department of Health (England and Wales) DSM (III, IV) = Diagnostic and Statistical Manual of Mental Disorders (Third Edition, Fourth Edition) DrinC = Drinker Inventory of Consequences DSPD = dangerous and severe personality disorder DWI = driving while intoxicated EQ‐5D = European Quality of Life‐5 dimensions ESS = Experience of Shame Scale EUROQOL = EuroQol Research Foundation GAF = Global Assessment of Functioning GCSE = General Certificate of Secondary Education HADS = Hospital Anxiety and Depression Scale HCR‐20 = Historical Clinical Risk Management‐20 HIV = human immunodeficiency virus HTA = Health Technology Assessment IBRS = Institutional Behaviour Rating Scale ICC = intra‐class correlations ICD‐10 = International Classification of Diseases‐Tenth Revision IIP = Inventory of Interpersonal Problems ILC = impulsive lifestyle counselling IOP = intensive outpatient programme IPDE = International Personality Disorder Examination IQ = intelligence quotient IRP = individualised relapse prevention ITT = intention‐to‐treat analysis MACT= manual‐assisted cognitive behaviour therapy MANSA = Manchester Short Assessment of Quality of Life MAPPA = multi‐agency public protection arrangements MCVSI = MacArthur Community Violence Screening Instrument MINI = Mini International Neuropsychiatric Interview MINIM = randomisation program for running minimisation in clinical trials MOAS = Modified Overt Aggression Scale n/a = not applicable NAS = Novaco Anger Scale NCTU = Nottingham Clinical Trials Unit NEP = needle exchange programme NHS = National Health Service OAS = Overt Aggression Scale PAS‐Q = Quick Personality Assessment Schedule PCL‐R = Psychopathy Checklist‐Revised PCL‐SV = Psychopathy Checklist‐Screening Version PD = personality disorder PD‐NOS = personality disorder‐not otherwise specified PDQ = Personality Diagnostic Questionnaire PEPS = psychoeducation and problem‐solving PNC = Police National Computer PTSD = post‐traumatic stress disorder QALY = quality‐adjusted life year QOL = quality of life REBT = rational emotional behaviour therapy Resettle = programme of psychosocial interventions for high risk personality disordered offenders SASII = Suicide Attempt Self‐Injury Interview SBCM = strengths‐based case management SCID = Structured Clinical Interview for DSM [Diagnostic and Statistical Manual of Mental Disorders] SCL‐90‐R = Symptom Checklist 90 SD = standard deviation SE = standard error SFQ = Social Functioning Questionnaire SIDP = Structured Interview for DSM‐IV Personality Disorders SM = standard maintenance SMI = schema mode inventory SMT = schema modal therapy SNAP = Schedule for Nonadaptive and Adaptive Personality SPSI‐R = Social Problem Solving Inventory‐Revised SRASBM = Self‐Report of Aggression and Social Behaviour Measure SRD = Self‐Reported Delinquency Scale ST = schema therapy START = Short‐Term Assessment of Risk and Treatability STAXI = State‐Trait Anger Expression Inventory SVR‐20 = Sexual Violence Risk‐20 TAU = treatment‐as‐usual TBS = Terbeschikkingstelling TER = Treatment Engagement Rating Scale for Forensic Outpatient Treatment USD = United States Dollar VRS = Violence Risk Scale WAI = Working Alliance Inventory YSQ = Young Schema Questionnaire‐Short Version ZAN‐BPD = Zanarini Rating Scale for Borderline Personality Disorder
Characteristics of excluded studies [ordered by year]
| Study | Reason for exclusion |
|---|---|
| Sloane 1976 | Randomised trial comparing psychoanalytically‐oriented psychotherapy, behaviour therapy and waiting‐list controls in outpatients. Excluded because diagnosis of AsPD not attempted |
| Liberman 1981 | Randomised trial comparing BT with insight‐oriented therapy for repeated suicide attempters. Excluded because no participants had a diagnosis of AsPD and there was no control condition that could be classified as TAU, waiting list or no treatment |
| Hesselbrock 1991 | Outcome study of inpatients with alcohol dependency. Excluded because participants were not randomised |
| Longabaugh 1994 | Randomised trial comparing CBT and relationship‐enhancement therapy for alcohol abusers. Investigators reported that 48 of 229 participants recruited had AsPD. Excluded because there was no control condition that could be classified as TAU, waiting list or no treatment |
| Winston 1994 | Randomised trial comparing brief adaptive psychotherapy with short‐term dynamic psychotherapy and with waiting‐list controls in outpatients. Excluded because there was no AsPD subgroup (trial excluded participants with history of violent behaviour or destructive impulse control problems) |
| Springer 1996 | Randomised trial comparing DBT‐derived CBT group therapy with discussion control group for inpatients with PD, assessed using MCMI‐II. Excluded because no indication that any participant had a diagnosis of AsPD |
| Wölwer 2001 | Randomised trial comparing CBT and coping skills training against treatment as usual in outpatients with alcohol dependency. Excluded because only 10 participants had a diagnosis of AsPD. Review authors judged the numbers of participants randomised to each of the 3 conditions to be too small for extraction of means and SDs for each condition. |
| Messina 2002 | Study comparing 2 therapeutic community treatments. PD assessed using MCMI‐II. Excluded because the participants were not randomised and there was no control condition that could be classified as TAU, waiting list or no treatment |
| Kool 2003 | Randomised trial comparing psychodynamic supportive therapy plus pharmacotherapy with pharmacotherapy for depressive disorder in depressed patients with and without AsPD. Excluded because only 4 participants had a diagnosis of AsPD (confirmed by study investigators via email to J Dennis on 29 May 2009, Kool 2003) |
| Chiesa 2003 | Prospective study comparing 2 specialist psychosocial interventions (therapeutic community‐based inpatient treatment and step‐down). Excluded because participants were not randomised |
| Colom 2004 | Randomised trial comparing a group psychoeducation intervention with a non‐structured control intervention in patients with PD and bipolar disorder. Only 2 participants had a diagnosis of AsPD. Excluded because participants had bipolar disorder in addition to AsPD |
| Vannoy 2004 | Randomised trial comparing anger management with a waiting‐list control condition. Excluded because there was no AsPD subgroup |
| Vinnars 2005 | Randomised trial comparing manualised supportive‐expressive psychotherapy with non‐manualised community‐delivered psychotherapy. Excluded because there was no control condition that could be classified as TAU, waiting list or no treatment |
| Mörtberg 2007 | Randomised trial comparing group cognitive therapy, individual cognitive therapy and TAU in outpatients with social phobia. Investigators used the SCID‐II screener but made no formal diagnostic assessment of PD. Excluded because no indication that any participant had a diagnosis of AsPD |
| Weertman 2007 | Randomised trial comparing present‐focused and past‐focused cognitive therapy in outpatients. Excluded because no participant had a diagnosis of AsPD, and there was no control condition that could be classified as TAU, waiting list or no treatment |
| Zorn 2007 | Randomised trial comparing schema‐focused emotional behaviour therapy and classical social skills training. Excluded because no participant had a diagnosis of AsPD |
| Lynch 2007 | Randomised trial comparing medication plus a DBT‐based intervention with medication only in older adults with comorbid PD and depression. Excluded because only 1 participant had a diagnosis of AsPD |
| Milrod 2007 | Randomised trial comparing psychodynamic psychotherapy with relaxation for individuals with panic disorder. Excluded because no participant had a diagnosis of AsPD, and there was no control condition that could be classified as TAU, waiting list or no treatment |
| Kallert 2007 | Randomised trial comparing acute day hospital care with inpatient care. Excluded because no participant had a diagnosis of AsPD (confirmed by study authors via email on 2 June 2009, see Kallert 2007) |
| Kool 2007 | Randomised trial comparing psychodynamic supportive therapy plus pharmacotherapy with pharmacotherapy alone for depressive disorder in depressed patients with and without AsPD (article in Dutch). Excluded because only 3 participants had a diagnosis of AsPD |
| Ball 2007 | Randomised trial comparing dual‐focus schema therapy with 12‐step facilitation therapy in opioid‐dependent outpatients. Excluded because there was no control condition that could be classified as TAU, waiting list or no treatment |
| Easton 2007 | Study aggregating results from two RCTs (Carroll 1998; Carroll 2004) to compare CBT, interpersonal psychotherapy, 12‐step facilitation therapy, supportive psychotherapy and disulfiram in outpatients with alcohol and cocaine dependence. Both trials had a subgroup with AsPD. Excluded because neither trial had a control condition that could be classified as TAU, waiting list or no treatment |
| Fournier 2008 | Randomised trial comparing antidepressants with cognitive therapy in patients with and without PD. Excluded because no participant had a diagnosis of AsPD (confirmed by investigators via email on 3 June 2009, see Fournier 2008). Placebo control condition only in the follow‐up of treatment responders |
| Petersen 2008 | Randomised trial comparing a specialised, psychotherapeutic day treatment programme with a waiting‐list control condition for adults with personality disorder. Excluded because a diagnosis of AsPD was an exclusion criterion |
| Bagby 2008 | Analyses the aggregated results of two randomised trials comparing CBT and pharmacotherapy for adults with major depression. Excluded because a diagnosis of AsPD was an exclusion criterion, and because there was no control condition that could be classified as TAU, waiting list or no treatment |
| Daughters 2008 | Study examining the interactive effects of court‐mandated treatment and AsPD on treatment dropout in a sample of male substance users who were receiving residential substance‐abuse treatment. Excluded because participants were not randomised, and there was no control condition that could be classified as TAU, waiting list or no treatment |
| Abbass 2008 | Randomised trial comparing intensive short‐term dynamic psychotherapy with TAU in outpatients. Excluded as insufficient number of observations; only one participant had a diagnosis of AsPD |
| Vera 2008 | Study describing a cognitive behavioural group treatment for adults with OCD symptoms plus comorbid personality disorder. Excluded because there was no random allocation and no control condition that could be classified as TAU, waiting list or no treatment |
| Bowen 2009 | Randomised trial comparing mindfulness‐based relapse prevention for substance disorders with TAU. Excluded as participants were not assessed for PD |
| Frisman 2009 | Secondary analysis of data from a randomised trial of assertive community treatment and clinical case management in participants with substance disorders (Essock 2006). Excluded as participants also had axis I disorders such as schizophrenia |
| Tyrer 2009 | Randomised trial of early versus late assessment of dangerous and severe PD in a sample of prisoners. Excluded because there was no psychological treatment in either allocated condition |
| Bateman 2009 | Randomised superiority trial of mentalisation‐based treatment and structured clinical management for patients with AsPD and comorbid borderline PD. Excluded as the trial did not have a control condition that could be classified as TAU, waiting list or no treatment |
| Kelly 2009 | Randomised trial comparing individual problem‐solving, group depression prevention and TAU with a European sample of adults with depressive disorder (the ODIN [Outcome of Depression International Network] study). Investigators reported that 93 of the 301 participants who were fully assessed met criteria for at least 1 PD. Excluded because no AsPD subgroup was identified and because a proportion of the sample had a diagnosis of bipolar disorder |
| Muran 2009 | Randomised trial comparing CBT, brief relational therapy and short‐term dynamic psychotherapy in fee‐paying outpatients. Excluded because the primary inclusion criterion was a diagnosis of cluster C PD or PD‐NOS, with no indication of any AsPD subgroup. In addition, there was no control condition that could be classified as TAU, waiting list or no treatment |
| Arnevik 2009 | Randomised trial comparing short‐term, day hospital psychotherapy and outpatient individual psychotherapy for adults with PD. Excluded because a diagnosis of AsPD was an exclusion criterion, and because there was no control condition that could be classified as TAU, waiting list or no treatment |
| Holmqvist 2009 | Superiority trial comparing aggression replacement training and a relationally‐orientated treatment for young offenders. Excluded as the trial was not randomised and used juvenile participants |
| Hesse 2010 | Randomised trial of psychoeducation as an addition to substance abuse treatment vs attention placebo. Excluded as only participants in the treatment arm were formally assessed for PD |
| Bartak 2010 | Superiority trial comparing 3 treatments (outpatient, day hospital and inpatient) for patients with cluster B personality disorders. Excluded as participants were not randomised to treatment conditions, and there was no control condition that could be classified as TAU, waiting list or no treatment |
| McGauley 2011 | Pilot study of mentalisation‐based treatment for men with AsPD delivered in 1 site of a multisite trial. Excluded as the participants were not randomised and there was no control condition that could be classified as TAU, waiting list or no treatment |
| Høglend 2011 | Randomised superiority trial of dynamic psychotherapy with or without transference interpretation in patients with predominately cluster C personality disorders (1 patient with AsPD was reported in the transference treatment group). Excluded as there was no control condition that could be classified as TAU, waiting list or no treatment |
| Korrelboom 2011 | Randomised trial comparing memory training therapy and TAU in patient participants with low self‐esteem. Excluded as borderline PD was the predominant diagnosis and patients with AsPD were treated in another clinical department to where the study was conducted |
| Ball 2011 | Randomised study comparing manual‐guided individual dual‐focus schema therapy or individual drug counselling as an addition to standard residential therapeutic community treatment. Excluded as there was no control condition that could be classified as TAU, waiting list or no treatment |
| Easton 2012 | Randomised superiority trial comparing 4 cognitive‐behavioural interventions for substance‐dependent participants with or without AsPD. Excluded as there was no control condition that could be classified as TAU, waiting list or no treatment |
| Rees‐Jones 2012 | Trial of a cognitive‐behavioural programme (reasoning and rehabilitation mental health programme) for mentally disordered offenders treated in forensic mental health setting. Excluded as participants were not randomised |
| Young 2013 | Controlled trial of a cognitive skills programme for personality‐disordered offenders (Reasoning and Rehabilitation ADHD program). Excluded as participants were not randomised to the experimental treatment or waiting‐list control groups |
| McMurran 2013 | Randomised trial comparing a specialist treatment for PD with or without a goal‐based motivational interview. Excluded as the specialist nature of the intervention meant that no condition could be classified as TAU, waiting list or no treatment |
| Rademacher 2013 | Controlled trial of individual systemic therapy (voluntary participation vs participation mandated by conditions of probation, vs waiting‐list control), to reduce aggressiveness. Excluded as participants were not randomised |
| Johnson 2013 | Double‐blind RCT comparing topiramate + CBT with placebo + CBT in cocaine‐dependent adults. Excluded because no diagnosis of PD was made |
| Lorentzen 2013 | Randomised trial of short‐ and long‐term group analytic psychotherapy for patients with mood, anxiety or PD. Excluded as insufficient number of observations; only 2 patients with AsPD were reported in the study (none in the short‐term group, 2 in the long‐term group) |
| De Jong 2013 | Randomised trial comparing group and individual treatment in participants with personality problems. Excluded as the trial did not have a control condition that could be classified as TAU, waiting list or no treatment |
| Doyle 2013 | Controlled trial to assess the effectiveness of enhanced thinking skills in offenders with AsPD traits. Excluded as participants were not randomised |
| Dean 2013 | Randomised trial of a cognitive skills programme (Reasoning and Rehabilitation) for mentally disordered offenders. Excluded as participants were described as having a "psychotic disorder" |
| Davidson 2014 | Randomised trial of manual‐assisted cognitive therapy to promote engagement in services and address self‐harm in patients admitted to hospital following an episode of self‐harm. Excluded as no AsPD reported in paper; author (Kate Davidson) was contacted by email (28 February 2017, see Davidson 2014) and confirmed she is unable to access and check the original study data. |
| Witkiewitz 2014 | Randomised superiority trial of mindfulness‐based relapse prevention and standard relapse prevention for substance‐addicted women offenders. Excluded as there was no control condition that could be classified as TAU, waiting list or no treatment |
| Chen 2014 | Randomised study comparing a CBT training programme plus routine intervention (TAU) vs TAU in young male violent offenders. Excluded because some participants were juveniles and no reported diagnosis of PD |
| Hakvoort 2015 | Randomised trial of 'cognitive‐behavioral music therapy' vs TAU for anger management and coping skills in a forensic psychiatric setting. Email correspondence with the author on 21 November 2017 confirmed all participants had a diagnosis of AsPD (Hakvoort 2015). Excluded as intervention was not a specific psychological therapy as defined in this review |
| Suszek 2015 | Protocol for a randomised trial of 2 group interventions (intensive psychodynamic therapy and CBT) vs waiting‐list control for patients with anxiety disorders and comorbid depressive or PD. Excluded as this was a study protocol |
| Brazão 2015 | Randomised controlled study of a CBT group intervention (Growing Pro‐Social) for male offenders. Excluded as no diagnosis of PD reported |
| Crane 2015 | Randomised study comparing a brief motivational interview with a control intervention on treatment compliance in violent offenders. Excluded as no diagnosis of PD was reported |
| Urban 2015 | Randomised cross‐over trial of animal‐assisted (dog) therapy for patients undergoing drug withdrawal. Excluded after email from author on 14 February 2017 confirmed that there were no participants with AsPD comorbidity in the sample (Urban 2015) |
| Wupperman 2015 | Trial of individual mindfulness and modification therapy vs TAU for women with substance use and aggression difficulties. Excluded as the participants were not randomised and PD was not reported |
| Swogger 2016 | RCT comparing a brief motivational intervention for substance‐using offenders. Psychopathic traits were assessed; however, the study was excluded as there was no formal assessment of PD |
| Keefe 2016 | Secondary analysis of randomised trial of cognitive therapy, antidepressants and placebo for major depressive disorder (DeRubeis 2005). Excluded as AsPD was an exclusion criteria in the original trial |
| Leichsenring 2016 | Controlled trial of manualised psychoanalytical and psychodynamic therapy for cluster B PD. Excluded as the study was not a RCT as participants were randomised to the 2 treatment conditions but not the control condition |
| Elsner 2016 | Controlled parallel trial of schema‐orientated psychotherapy vs TAU with personality‐disordered forensic patients. Excluded as the study was not a randomised trial |
| Gysin‐Maillart 2016 | Randomised trial of a suicide prevention intervention vs TAU. Excluded as author confirmed by email that no participants had a diagnosis of AsPD (22 March 2017, Gysin‐Maillart 2016) |
| Blattman 2017 | Randomised study of CBT (designed to foster self‐regulation, patience, and a noncriminal identity and lifestyle), with or without cash grants of USD 200, for criminally engaged men in Liberia. Excluded as no diagnosis of AsPD/dissocial PD |
| Välimäki 2017 | Protocol for a cluster‐randomised trial comparing the impact of an educational programme for staff or standard care on the outcomes of inpatients with a diagnosis of schizophrenia. Excluded as participants had a diagnosis of major mental illness, and it was the staff members who were randomised in the study, not the patients |
| Shaw 2017 | Randomised trial comparing the completion of collaborative case formulations (CFs) and usual practice, on the relationships between offender managers and high‐risk offenders with PD. Excluded as it was the offender managers, rather than the offenders, who were randomised into the intervention and control groups |
| Tomlinson 2017 | Randomised, waiting‐list controlled trial of DBT for forensic psychiatric patients. Excluded after correspondence with the study author (email from MT on 9 November 2018, Tomlinson 2017), which confirmed that of the 4 participants with a diagnosis of AsPD, 3 also had a serious mental illness (schizophrenia; delusional disorder; schizoaffective disorder) |
| NCT03382808 | Ongoing, parallel randomised trial of emotional recognition training (behavioural SEE training versus behavioural GAZE training) for antisocial violent offenders with psychopathic traits. Excluded as this study did not have a true control condition; GAZE training was described as an "active comparator" |
| Pearce 2017 | Randomised trial comparing democratic therapeutic community treatment with crisis planning plus TAU for adults with PD. 7 participants diagnosed with AsPD (5 in intervention group; 2 in control group). Excluded as the addition of 'crisis planning' to the control group intervention was not TAU |
| Conrad 2017 | Pre/post‐treatment evaluation of the effectiveness of a 10‐week group psychological intervention based on DBT skills with patients diagnosed with either cluster B PD or a mood disorder. Excluded as the study was not an RCT |
| DRKS0001326 | Trial registry citation of a pre‐post study of schema therapy for adult inpatients with PD randomised to different baseline lengths. Excluded from classification as an 'on‐going' study in this review as it was not an RCT and AsPD was an exclusion criterion |
| Nitschke 2018 | Study documented a violence‐prevention treatment based on psychoeducation, group training, and individual treatment on violence risk co‐management for forensic psychiatry outpatients. Excluded as the study was not an RCT |
| Lay 2018 | Randomised trial of a psychoeducation intervention (focusing on behaviours prior to and during illness‐related crises) and TAU in a sample of psychiatric inpatients with compulsory admission to hospital. Excluded after email correspondence with the study author (B Lay) on 21 November 2018 confirmed that no participants had a diagnosis of AsPD (Lay 2018) |
| NCT03677037 | Randomised trial of mentalisation‐based therapy (20 weeks/short‐term compared with 14 months/long‐term) for outpatients with subthreshold or diagnosed borderline PD. Excluded as AsPD was an exclusion criterion and there was no control condition that could be classified as TAU, waiting list or no treatment |
| Davis 2018 | Randomised trial of multi‐systemic therapy (MST‐EA) for young adults (17‐20 years) with serious mental health conditions referred for state vocational rehabilitation services. Excluded as the study included juveniles and AsPD was not assessed/recorded |
| Kool 2018 | Randomised trial of therapy dosage (25 compared to 50 sessions in a year) and type of therapy (schema therapy compared to short‐term psychodynamic supportive psychotherapy) for patients with comorbid depressive disorder and PD. Excluded as there was no control condition that could be classified as TAU, waiting list or no treatment |
| Larden 2018 | Nonrandomised comparison of a cognitive‐behavioural intervention (aggression‐replacement training) in adult offenders within the Swedish prison and probation service. Excluded as the study was not an RCT |
| Kingston 2018 | Randomised trial comparing a cognitive skills programme (Reasoning and Rehabilitation 2: Short version for Adults) and TAU in a sample of offenders with mental illness. Excluded as participants were diagnosed with serious mental illnesses such as bipolar disorder and psychosis. We contacted the study authors to confirm if any participants had comorbid AsPD and anxiety/trauma‐related diagnoses but received no response (Kingston 2018) |
| Klein Tuente 2018 | Protocol for an ongoing, waiting‐list controlled trial of a virtual reality intervention for aggressive forensic psychiatric inpatients with any DSM‐5 diagnosis (virtual reality aggression‐prevention training). Excluded because the intervention could not be described as a purely psychological intervention, as the training was delivered using virtual reality technology headsets |
| Haeyen 2018 | Randomised, waiting‐list control trial of a group‐based, art therapy intervention for adult participants diagnosed with a cluster B/C PD. The intervention used theoretical elements of DBT, schema‐focused therapy, gestalt art therapy and creative problem‐solving. Excluded as there were no reported participants with a diagnosis of AsPD |
| Keefe 2018 | Secondary analysis of a randomised trial of 3 psychotherapies for people with panic disorder (with or without agoraphobia) comparing CBT, panic‐focused psychodynamic psychotherapy and applied relaxation training (ART). Excluded as there was no control condition that could be classified as TAU, waiting list or no treatment, and ART data were not presented |
| De Jong 2018 | Randomised trial of outcome‐monitoring feedback (to therapist or patients and therapists or no feedback) with day treatment patients and inpatients with PD. Excluded as there were no patients with AsPD reported |
| Grenyer 2018 | Cluster‐RCT of a stepped‐care model of psychological therapy compared with TAU for inpatients with PD. Excluded as the study recruited people aged 12 years or over |
| Deng 2019 | RCT of a five‐week intervention for male violent prisoners comparing 3 conditions: gratitude‐sharing, blessing‐counting, and control. Excluded as AsPD was not assessed |
| Sewall 2019 | Long‐term, community follow‐up of men completing sexual offender treatment in a Canadian prison. Excluded as the study was not an RCT |
| Bianchini 2019 | Randomised trial of 12 months DBT plus standard REMS treatment (TAU) versus TAU for male forensic psychiatric patients with borderline PD. Pre and post‐assessments included BIS‐11, DERS and TAS‐20. Excluded as there was no information regarding AsPD or other diagnoses such as psychosis and bipolar disorder |
ADHD = attention deficit hyperactivity disorder ART = applied relaxation training AsPD = antisocial personality disorder BIS‐11 = Barratt Impulsiveness Scale Version 11 BT = behaviour therapy CBT = cognitive behavioural therapy CF = case formulation DBT = dialectical behaviour therapy DERS = Difficulties in Emotion Regulation Scale DSM‐5 = Diagnostic and Statistical Manual of Mental Disorders‐Fifth Edition GAZE = GAZE training sequence comprises four weekly sessions using a modified dote‐probe paradigm (averted vs directed gaze) MCMI‐II = Millon Clinical Multiaxial Inventory II MST‐EA = multi‐systemic therapy for emerging adults OCD = obsessive‐compulsive disorder ODIN = Outcome of Depression International Network PD = personality disorder PD‐NOS = personality disorder not otherwise specified RCT = randomised controlled trial REMS = 'Residenze per l'Esecuzione delle Misure di Sicurezza' Italian high intensity therapeutic facility treatment SCID‐II = Structured clinical Interview for DSM‐IV [Diagnostic and Statistical Manual of Mental Disorders‐Fourth Edition] SD = standard deviation SEE = SEE training sequence comprises four weekly sessions using a modified dote‐probe paradigm (fearful vs neutral expression) TAS‐20 = Toronto Alexithymia Scale 20 TAU = treatment as usual USD = United States Dollars vs = versus
Characteristics of studies awaiting classification [ordered by year]
Evans 1999.
| Methods | Design: parallel randomised controlled trial |
| Participants |
Participants: individuals with recent self‐harm episode and personality disturbance within ICD‐10 'flamboyant' clustera Sex: mixed (breakdown not provided, although treatment groups similar in terms of male:female ratio) Age: range = 16 to 50 years Unit of allocation: individual participant Number randomised: for whole sample n = 34 (n = 18 intervention group; n = 16 control group; data not extractable for any AsPD subgroup)a Number completing: data not extractable for any AsPD subgroupa Setting: outpatient; 2 sites; urban; United Kingdom (London) Inclusion criteria: aged 16 to 50 years; recent episode of self‐harm; at least one other episode of self‐harm in past 12 months; minimum score of personality disturbance (i.e. one level below personality disorder) within the ICD‐10 flamboyant cluster (antisocial, histrionic or emotionally unstable) on the Personality Assessment Schedule (PAS) Exclusion criteria: primary ICD‐10 diagnosis within the organic (F0), alcohol or drug dependence (F1) or schizophrenia (F2) groups Ethnicity: no details given Baseline characteristics: (for whole samplea) groups very similar in age, sex ratio, marital status and employment with no important differences in baseline assessments apart from scores on the Social Functioning Questionnare (manual assisted cognitive behavioural therapy (MACT) mean = 11.9; TAU mean = 15.6) |
| Interventions | Two conditions: brief manual assisted cognitive behavioural therapy (MACT); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: between 2 and 6 sessions Duration of trial: to 6 months post‐treatment Length of follow‐up: Participants were followed up for 6 months after end of treatment. |
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
| Notes | aStudy may have recruited a subgroup with AsPD since all participants had scores at least to the level of personality disturbance within the flamboyant cluster of ICD‐10 (which includes dissocial personality disorder). However, numbers of formal axis II diagnoses were not described in the paper. No data extractable on any AsPD subgroup. Awaiting clarification from investigators |
Linehan 2006.
| Methods | Design: parallel randomised controlled trial |
| Participants |
Participants: women with recent suicidal and self‐injurious behaviours meeting criteria for BPDa Sex: all female Age: mean = 29.3 years (SD = 7.5) Unit of allocation: individual participant Number randomised: for whole sample n = 101 (n = 52 intervention group; n = 49 control group); data not extractable for any AsPD subgroupa Number completing: data not extractable for any AsPD subgroupa Setting: outpatient; single site; urban; USA (Washington) Inclusion criteria: aged 18 to 45 years; meeting criteria for BPD (DSM‐IV, IPDE); current or past suicidal behaviour (2 suicide attempts or self‐injuries in past 5 years, with at least 1 in past 8 weeks) Exclusion criteria: lifetime diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder, psychotic disorder, psychotic disorder not otherwise specified, mental retardation; seizure disorder requiring medication; a mandate to treatment; needing primary treatment for another debilitating condition Ethnicity: (for whole samplea) white (87%), African American (4%), Asian American (2%), native American (1%), other (5%) Baseline characteristics: (for whole samplea) single, divorced or separated (87.2%); median number suicide attempts in past 5 years 1.0 (IQR 0.5 to 4.0); median number self‐injuries in past 5 years 10.0 (interquartile range = 2.0 to 47.0); college graduate (23.8%); current major depressive disorder (72.3%); current anxiety disorder (78.2%); current substance use disorder (29.7%); current eating disorder (23.8%); current panic disorder (40.6%); comorbid cluster A personality disorder (3.0%); comorbid cluster B personality disorder other than BPD (10.9%), cluster C PD (25.7%) |
| Interventions | Two conditions: dialectical behaviour therapy (DBT); or community treatment by experts (CTBE)
Details of conditions:
Duration of intervention: 12 months Duration of trial: 12 months Length of follow‐up: Participants were followed up for 12 months after end of treatment. |
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
| Notes | aStudy may have recruited a subgroup with AsPD since 11 of 101 participants (10.9%) had a cluster B personality disorder other than BPD. No data extractable on any AsPD subgroup. Awaiting clarification from investigators (Linehan 2006) |
Berget 2008.
| Methods | Design: parallel randomised controlled trial |
| Participants |
Participants: adult psychiatric inpatients and outpatients with various diagnosesa Sex: (for whole sample) 59 women; 31 men Age: (for whole sample) mean = 34.7 years (SD = 10.7, range = 18 to 58) Unit of allocation: individual participant Number randomised: for whole sample n = 90 (n = 60 intervention group; n = 30 control group; data not extractable for any AsPD subgroupa) Number completing: data not extractable for any AsPD subgroupa Setting: community; 15 sites (farms); rural; Oslo (Norway) Inclusion criteria: adults currently receiving psychiatric care (both inpatients and outpatients) Exclusion criteria: aged less than 18 years; acute psychotic disorder; mental retardation; serious drug addiction; being in a job during the 6 months prior to start of intervention Ethnicity: no information Baseline characteristics: (for whole samplea) current inpatients = 14/90 (15.5%); current outpatients = 76/90 (84.5%); ill for more than 5 years (> 50%); treated in psychiatric institutions for > 3 years (72%); receiving daily medication (83%) |
| Interventions | Two conditions: animal‐assisted therapy with farm animals plus treatment‐as‐usual (AAT + TAU); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: 12 weeks Duration of trial: 9 months Length of follow‐up: Participants were followed up for 6 months after end of treatment. |
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
| Notes | aStudy may have recruited a subgroup with AsPD since 22 of 90 participants had an ICD‐10 F60‐69 disorder (disorder of adult personality and behaviour). No data extractable on any AsPD subgroup. Awaiting clarification from investigators (Berget 2008) |
Clarke 2013.
| Methods | Design: randomised control trial |
| Participants |
Participants: individuals with personality disorder referred to a specialist outpatient service Sex:a 28 men, 71 women Age:a mean age = 36.0 years (SD = 9.5, range = 19‐59) Unit of allocation: individual, stratified by cluster Number randomised: experimental group (n = 50); control/TAU group (n = 49) Number completing: experimental group (n = 38), control/TAU group (n = 40) Setting: specialist outpatient clinic of public health service (NHS, UK) Inclusion criteria: participants met diagnostic criteria for a personality disorder; participants had completed at least one previous episode of therapy (see note 2) Exclusion criteria: diagnosis of psychotic illness, substance dependence or intellectual disability based on DSM‐IV criteria; participant reports self‐harming behaviour on at least a monthly basis Ethnicity: not stated Baseline characteristics:a 88% of the sample had a diagnosis of two or more personality disorders; 53% displayed diagnoses across two clusters; 28% across all three clusters; 68% of participants had a diagnosis of borderline personality disorder |
| Interventions | Two conditions: cognitive analytic therapy (CAT); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: 24 sessions Duration of trial: 10 months Length of follow‐up: 12 months |
| Outcomes |
Secondary outcomes
Other outcomes
|
| Notes | aFor all of those randomised (n = 99) at least 18 participants had a cluster B personality disorder. Author (Susan Clarke) contacted by email on 19 January 2017 with request to identify the number of participants with AsPD; no data for AsPD subset. No response received (Clarke 2013) |
Jochems 2015.
| Methods | Design: cluster‐randomised control trial |
| Participants |
Participants: patients receiving individual outpatient treatment for a mental disorder Sex: (for sample as a wholea,b) Intervention group: motivation feedback (MF) + treatment‐as‐usual (TAU): male (n = 98/148, 66%); female (n = 50/148, 34%). Control group: treatment‐as‐usual group (TAU): male (n = 81/146, 55%); female (n = 65/146, 45%) Age: (for sample as a wholea,b) MF + TAU group: mean age = 45.47 years (SD = 10.4, range = 18‐65). TAU group: mean age = 42.5 years (SD = 10.0, range = 18‐65) Unit of allocation: cluster Number randomised: 294 for sample as a wholea,b; MF + TAU group (n) = 148; TAU group (n) = 146 Number completing: 254 for sample as a wholea,b; MF+ TAU group (n) = 127; TAU group (n) = 127 Setting: 12 community mental health care teams affiliated with two mental health institutions in the Netherlands Inclusion criteria: patients with a primary diagnosis of psychotic disorder or personality disorder (DSM‐TR VI); aged between 18‐65 years old; receiving outpatient treatment for their mental disorder Exclusion criteria: insufficient command of the Dutch language; documented diagnosis of dementia or chronic toxic encephalopathy Ethnicity: (for sample as a wholea,b) MF + TAU group: Dutch ethnicity (n = 116, 78.4%); other ethnicity (n = 32, 21.6%). TAU group: Dutch ethnicity (n = 92, 63%); other ethnicity (n = 54, 37%) Baseline characteristics: (for sample as a wholea,b) Education level: MF + TAU group: no education/elementary (n = 57, 38.5%); secondary school (n = 57, 38.5%); upper high school (n = 32, 21.6%). TAU group: no education/elementary (n = 51, 34.9%); secondary school (n = 67, 45.9%); upper high school (n = 27, 18.5%) Living situation: MF + TAU group: living alone (n = 88, 59.5%); with partner or children or both (n = 49, 33.1%); mental health centre facility (n = 10, 6.8%); homeless (n = 1, 0.7%). TAU group: living alone (n = 59, 40.4%); with partner or children or both (n = 70, 47.9%); mental health centre facility (n = 16, 11%); homeless (n = 1, 0.7%) Primary diagnosis: MF + TAU group: psychotic disorder (n = 104, 70.2%); personality disorder (n = 44, 29.7%); comorbid substance use problems (n = 42, 28.4%). TAU group: psychotic disorder (n = 95, 65.1%); personality disorder (n = 51, 34.9%); comorbid substance use problems (n = 32, 21.9%) Prescribed medication: MF + TAU group: classical antipsychotics (n = 37, 25%); atypical antipsychotics (n = 63, 42.6%); combination of typical and atypical antipsychotics (n = 12, 8.1%); benzodiazepines (n = 42, 28.4%); antidepressants (n = 40, 27%). TAU group: classical antipsychotics (n = 26, 17.8%); atypical antipsychotics (n = 67, 45.9%); combination of typical and atypical antipsychotics (n = 15, 10.3%); benzodiazepines (n = 39, 26.7%); antidepressants (n = 53, 36.3%) Age of first contact with mental health: MF + TAU group: mean age = 27.16 years (SD = 10.34); TAU group: mean age = 24.95 years (SD = 10.24). Number of patient participants with one or more previous hospitalizations: MF + TAU group: n = 113 (76.4%); TAU group: n = 114 (78.1%) Number of patient participants with a legal mandate: MF + TAU group: n = 11 (7.4%); TAU group: n = 13 (8.9%). |
| Interventions | Two conditions: motivational feedback (MF); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: 12 months Duration of trial: May 2011 and September 2012 (16 months) Length of follow‐up: 12 months |
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
| Notes |
aWhole sample: number of patients with a diagnosis of personality disorder at baseline: intervention group (n = 44, 29.7%); control group (n = 51, 34.9%) bNumber of patients with a diagnosis of AsPD: at baseline (n = 25/294, 8%); at follow‐up (n = 12/254, 5%), data on group allocation was not provided; no data are currently available for the AsPD subsample cThis study would meet the review exclusion criteria of including patients with psychotic disorders; however, an interaction effect of personality disorder on outcomes was reported. Email correspondence with Eline Jochems (EJ) confirmed n = 25 AsPD at baseline and n = 12 AsPD at follow‐up. Email contact on 7 February 2017 from EJ "In the meanwhile, I will ask my project members for their approval to share data" (quote from email correspondence; Jochems 2015) |
Black 2016.
| Methods | Design: secondary analysis of randomised control triala |
| Participants |
Participants: patients with borderline PD and comorbid AsPD recruited to previous RCT of systems training + TAU vs TAU (Blum 2008) Sex:b 7 males and 9 females Age: over age 18 years Unit of Allocation: not stated Number randomised: unclear; 16 participants with AsPD randomised to the intervention group; no data available for the control group in the original RCT Number completing: not stated Setting: inpatient and outpatient settings of University of Iowa and local Iowa psychiatric services Inclusion criteria: original RCT; DSM‐IV borderline personality disorder diagnosis, with other DSM‐IV diagnoses assessed Exclusion criteria: not English speaker; psychotic or primary neurological disorder; cognitive impairment; current (past month) substance abuse or dependence; previously participated in Systems Training for Emotional Predictability and Problem Solving (STEPPS) programme Ethnicityb: Caucasian (n = 15); other (n = 1) Baseline characteristicsb Marital status: never married (n = 10), married/living together (n = 4), divorced/separated (n = 2) Education: < high school (n = 1), high school (n = 2), some college (n = 11), college degree (n = 1), graduate degree (n = 1) Employment: employed (n = 8), disabled (n = 4), other (e.g. student) (n = 4) Mental health: 9 (69%) participants had a prior psychiatric hospitalisation; 14 (88%) had prior suicide attempts; 12 (75%) had prior self‐harm; 7 (44%) had current major depressive disorder; mean number of lifetime Structured Clinical Interview for DSM‐IV (SCID) disorders = 10.3 (SD = 5.0); mean number of Structured Interview for DSM‐IV Personality (SIDP‐IV) disorders = 4.5 (SD = 1.4); mean number of SIDP‐IV BPD criteria = 7.6 (SD = 1.1) |
| Interventions | Two conditions: Systems Training for Emotional Predictability and Problem Solving (STEPPS) + treatment‐as‐usual (TAU); or TAU
Details of conditions
Duration of intervention: 20 weeks Duration of trial: 72 weeks Length of follow‐up: 1 year (assessments at month 1, 3, 6, 9 and 12) |
| Outcomes |
Primary outcomesa,c:
Secondary outcomesa,c:
Other outcomes
|
| Notes |
aPaper reported a secondary analysis of previously unpublished data from two studies, one of which was an RCT (Blum 2008). Review authors contacted the study author (Donald Black) to request data for the AsPD participants in the intervention and control groups from the original RCT study described (Blum 2008). An email was received from DB on 16 February 2017 indicating that these data are potentially available but subject to contact with the original project statistician (Black 2016). bDemographic data available only for the 16 AsPD participants randomised to the intervention (STEPPS + TAU); data requested for the participants with AsPD in the control group (TAU) cPublished data were provided only for AsPD participants in the intervention group. |
Buric 2019.
| Methods | Design: randomised controlled study (see notesab) |
| Participants |
Participants: prisoners with personality disorder (see notec) Sex: all male Age: whole sample (see notec): 41 years (SD = 8.00) Unit of allocation: individual (stratified random sampling) Number randomised: 30 (see notea) Number completing: 21 (see note c) (7/10 mindfulness group; 5/10 yoga group; 9/10 control group) (intention‐to‐treat analysis) Setting: prison; clinical unit in high‐security prison, for prisoners with severe personality disorder Inclusion criteria: aged 18‐65 years; willing to participate and able to provide informed consent Exclusion criteria: major neurological disorders (not specified) that compromise completion of the interventions or assessments; difficulty understanding English Ethnicity: not stated Baseline characteristics:(see notec) Age: mindfulness group mean = 37.60 (SD = 3.24); yoga group mean = 41.60 (SD = 7.15); control group mean = 42.60 (SD = 6.79) Psychopathy Checklist‐Revised score: mindfulness group mean = 31.75 (SD = 4.12); yoga group mean = 29.32 (SD = 4.99); control group mean = 33.16 (SD = 6.98) Diagnosis (definite or probable) of personality disorder: paranoid PD (mindfulness group = 60%; yoga group = 65%; control group = 60%); schizoid PD: (mindfulness group = 5%; yoga group = 10%; control group = 10%); schizotypal PD: (mindfulness group = 0%; yoga group = 25%; control group = 10%); AsPD (mindfulness group = 100%; yoga group = 85%; control group = 90%); borderline PD (mindfulness group = 85%; yoga group = 75%; control group = 85%); histrionic PD (mindfulness group = 25%; yoga group = 10%; control group = 25%); narcissistic PD (mindfulness group = 40%; yoga group = 45%; control group = 40%); avoidant PD (mindfulness group = 20%; yoga group = 40%; control group = 20%); dependent PD (mindfulness group = 0%; yoga group = 0%; control group = 5%); obsessive‐compulsive PD (mindfulness group = 15%; yoga group = 10%; control group = 10%) Number of psychotherapy sessions: mindfulness group mean = 392.10 (SD = 366.90); yoga group mean = 403.20 (SD = 344.55); control group mean = 380.40 (SD = 293.68) |
| Interventions | Three conditions: mindfulness meditation programme; yoga programme; or waiting‐list control
Details of conditions
Duration of intervention: 10 sessions (15 hours) over 5 days Duration of trial: 4‐5 weeks but unclear (pre‐intervention assessments = 2 weeks; intervention = 1 week; post‐intervention = 10 days) Length of follow‐up: up to 2 weeks but unclear (follow‐up commenced 3 days after intervention was complete and lasted for 10 days) |
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
|
| Notes |
aEmail correspondence sent to I Buric on 12 September 2019 requesting full text of study. Further email sent to both I Buric and M Farias on 3 December 2019 and 17 December 2019 requesting confirmation of whether the study was an RCT. Response received on 17 December 2019 confirming randomisation procedure and that the paper is currently under review with the International Journal of Offender Therapy and Comparative Criminology (Buric 2019). Given that the study has not been though a peer‐review process (and data may be subject to amendment), the review authors considered that this study should remain in the 'awaiting assessment' until the peer‐review process has taken place. bParticipants were stratified by the amount of therapy received (from 0 to 5 years), dominant cluster of personality disorders (A, B, C or equally dominant A and B, and B and C), comorbid psychiatric disorder (7 had ADHD, 2 had major depressive disorder, and 21 had no other psychiatric diagnosis), and previous experience in meditation or yoga (5 had experience in meditation, 2 had experience in yoga). cWhole sample data only. 90% of recruited participants had a diagnosis of AsPD (mindfulness group: 100% definite diagnosis of AsPD; yoga group: 85% definite AsPD; control group: 90% definite AsPD). No data for AsPD subgroup. No details of assessment method for AsPD diagnosis provided, though all participants were recruited from a specialist clinical service for personality disordered offenders dThe trial authors noted that "all prisoners attend a 5‐year trauma‐informed treatment programme that consists of group and individual therapy, and aims to improve mental well‐being, emotional self‐regulation, and consequently reduce risk of reoffending" (p 9, pre‐publication manuscript; Buric 2019). |
AAT = animal‐assisted therapy ACAT = Association of Cognitive Analytic Therapy ADHD = attention deficit hyperactivity disorder AsPD = antisocial personality disorder BPD = borderline personality disorder CAT = cognitive analytic therapy CTBE = community treatment by experts DBT = dialectical behaviour therapy DSM‐IV (‐TR) = Diagnostic and Statistical Manual of Mental Disorders‐Fourth Edition (‐Text Revision) ERP = event‐related potentials F0 = diagnoses F00‐F09 in the International Classification of Diseases‐Tenth Edition F1 = diagnoses F10‐F19 in the International Classification of Diseases‐Tenth Edition F2 = diagnoses F20‐F29 in the International Classification of Diseases‐Tenth Edition ICD‐10 = International Classification of Diseases‐Eleventh Edition IPDE = International Personality Disorder Examination IQR = inter‐quartile range MACT= manual‐assisted cognitive behaviour therapy MF = motivation feedback NHS = National Health Service PAS = Personality Assessment Schedule PD = personality disorder RCT = randomised controlled trial SCID = Structured Clinical Interview for DSM‐IV [Diagnostic and Statistical Manual of Mental Disorders‐Fourth Edition] SD = standard deviation SFQ = Social Functioning Questionnaire SIDP‐IV = Structured Interview for DSM‐IV Personality STEPPS = systems training for emotional predictability and problem solving TAU = treatment as usual USA = United States of America
Characteristics of ongoing studies [ordered by year]
NCT03883646.
| Study name | Mindfulness for Alcohol Abusing Offenders |
| Methods | Design: single‐blind, parallel assignment, randomised control study |
| Participants |
Participants: female prisoners with alcohol use disorders (see notea ) Sex: female Age:18 years to 65 years Unit of allocation: not stated Target sample size: 480 Blinding: outcomes assessor blinding only Inclusion criteria: 18‐65 years of age; alcohol use disorder; female (biological sex at birth); time to release from incarceration > 3 months to < 24 months; 5th grade or higher reading level; able to speak and understand English Exclusion criteria: uncorrectable auditory or visual deficits; intelligence quotient score below 70; history of serious head injury with loss of consciousness and ongoing soft signs, or positive radiology magnetic resonance imaging (MRI) reading for significant brain damage; history of dementia or other cognitive disability; current psychotic disorder; currently taking antipsychotic medication; major medical illness or central nervous system disease; MRI incompatibility (e.g. metal in body) |
| Interventions | 4 conditions: mindfulness; relapse prevention; waiting‐list control; or treatment as usual (TAU)
Details of conditions:
Duration of intervention: not stated (see noteb) Duration trial: not stated (see noteb) Length of follow‐up: one year after release from prison |
| Outcomes |
Primary outcomes of trial
Secondary outcomes of trial
Other outcomes of trial
|
| Starting date | 1 July 2018 (estimated completion date is 30 April 2023) |
| Contact information | Kent Kiehl, Professor of Psychology, Neuroscience and Law, Executive Science Officer, The Mind Research Network, Albuquerque, New Mexico, United States, 87106 Carla Harenski (charenski@mrn.org) |
| Notes |
aEmail correspondence from Carla Harenski: 'We assess personality disorders using the SCID‐5‐PD. We also assess psychopathic personality using the Psychopathy Checklist‐Revised (PCL‐R), given the important differences between psychopathy and ASPD' (quote from email correspondence; NCT03883646). bAssessments reported to be at 4 weeks, 8 weeks, and up to one year after release from prison |
NCT02524171.
| Study name | Improving treatment engagement and outcomes among justice‐involved veterans |
| Methods | Design: parallel randomised trial |
| Participants |
Participants: veterans with antisocial personality disorder and/or substance use disorder Sex: all Age: not clear ‐ child, adult, senior all included on clinical trial register (CTR) protocol Unit of allocation: not stated Target sample size: 365 Blinding: single‐blind (research assistants conducting the 6‐ and 12‐month outcome assessments are blinded to condition assignment) Inclusion criteria: veterans who (a) are entering a mental health residential rehabilitation treatment programme (MH RRTP) at one of three study sites (Palo Alto, Little Rock, or Bedford, Veterans Affairs), and (b) had been arrested and charged and/or released from incarceration in the past 5 years prior to MH RRTP admission will be eligible for participation. Exclusion criteria: only exclusion criterion is being too cognitively impaired to understand the informed consent process and other study procedures. |
| Interventions | Two conditions: moral reconation therapy (MRT); or usual care (UC)
Details of conditions:
Duration of intervention: 12 weeks Duration trial: April 4, 2016 to estimated finish date of 31st December 2019 Length of follow‐up: 12 months |
| Outcomes |
Primary outcomes of triala
Secondary outcomes of trial
|
| Starting date | 4 April 2016 |
| Contact information | Daniel M Blonigen (email: Daniel.Blonigen@va.gov) Christine Timko (email: Christine.Timko@va.gov) |
| Notes |
aTime frame: 12 months for all outcome measures Clinical trial registry: clinicaltrials.gov/ct2/show/record/NCT02524171 ClinicalTrials.gov identifier: NCT02524171 Sponsor: Veterans Affairs Office of Research and Development |
ISRCTN32309003.
| Study name | A national randomised controlled trial to evaluate mentalisation based therapy for antisocial personality disorder |
| Methods | Design: parallel randomised controlled trial |
| Participants |
Participants: male offenders who have a history of violent behaviour, are subject to statutory provision by the National Probation Service and have at least 6 months remaining on their licence Age: 21 years or above Unit of allocation: multicentre trial; 1:1 allocation Target sample size: 302 Inclusion criteria: participants subject to statutory provision by the National Probation Service; aged 21 or over; at least 6 months remaining of their license or community sentence; adequate level of English; evidence of a history of violent behaviour, that may include verbal assault, assaults against objects and/or assault against others; DSM‐IV‐R diagnosis of AsPD (using SCID‐II); and evidence of recent aggressive acts (using OAS‐M) Exclusion criteria: conviction for child sexual offences (including child pornography); current diagnosis for schizophrenia or bipolar disorder; neurodevelopmental disorder or significant cognitive impairment; severe substance or alcohol dependency |
| Interventions | Two conditions: mentalisation‐based therapy for anti‐social personality disorder (MBT‐ASPD); or probation as usual (PAU)
Details of conditions:
Duration of intervention: 2 months, after which patients will be reassessed by a member of the trial clinical team and referred for further management if required, for up to 12 months Duration of trial: 24 months (assessment at baseline, month 6 and 12 (in‐treatment), month 18 and 24 (post‐treatment) Length of follow‐up: 12 months |
| Outcomes |
Primary outcomes of trial
Secondary outcomes of trial
Other outcomes of trial
|
| Starting date | 01 January 2016 |
| Contact information | Ms Elizabeth Simes (email: MOAM@ucl.ac.uk) Address: Research Department of Clinical Educational & Health Psychology, University College London, 1‐19 Torrington Place, London, United Kingdom, WC1E 7HB |
| Notes | Sponsor: project funded by the National Institute for Health Research HTA (14/186/01) |
ISRCTN14994755.
| Study name | Low intensity psychological support for people with personality disorder: randomised controlled trial |
| Methods | Design: parallel randomised controlled trial |
| Participants |
Participants: adults using secondary care mental health services in London, UKa Age: 18 years or over Unit of allocation: 1:1, stratified by referring team and gender Target sample size: 60 Inclusion criteria: clinical diagnosis of personality disorder; positive screening result using the International Personality Disorder Examination self‐administered questionnaire; competent and willing to provide written, informed consent Exclusion criteria:current clinical diagnosis of a coexisting organic or psychotic mental disorder (dementia, bipolar affective disorder (type I and II), delusional disorder, schizophrenia, schizoaffective disorder or schizotypal disorder; cognitive or language difficulties that would preclude subjects providing informed consent or compromise participation in study procedures; currently receiving psychological treatment for personality disorder |
| Interventions | Two conditions: psychological support for personality (PSP); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: flexible (6 to 10 sessions, delivered over 3 to 6 months) Duration of trial: six months Length of follow‐up: 24 weeks after baseline |
| Outcomes |
Primary outcomes of trial
Secondary outcomes of trial
Other outcomes of trial
|
| Starting date | 13 July 2017 |
| Contact information | Ms Amy Claringbold (email a.claringbold@imperial.ac.uk) Address: Personality Disorder Research Unit, Centre for Psychiatry, Imperial College London, London, UK Tel: +44 20 8383 4134 Sponsor: Central and North West London NHS Foundation Trust Funder: National Institute for Health Research |
| Notes | aRecruitment from community mental health teams, home treatment teams, and other community‐based mental health services |
Van Dijk 2019.
| Study name | Group schema‐focussed therapy enriched with psychomotor therapy for older adults with personality disorders in specialised mental health care: a (cost‐)effectiveness study |
| Methods | Design: multicentre randomised trial |
| Participants |
Participants: older persons, with a cluster B or C personality disorder or meeting the general criteria for a personality disorder, treated in specialised mental health care settings Age: 60 years or older Unit of allocation: stratified block randomisation to assign participants evenly (1:1) over the two conditions (stratified by presence of a full versus subthreshold cluster B or C personality disorder) Target sample size: 140 Inclusion criteria: age of 60 years or above; cluster B or C personality disorder (or falling one content criterion short) as confirmed by the Structured Clinical Interview for DSM‐5 for personality disorders (SCID‐5‐PD); mentally able to adhere to the group SFT treatment schedule and to fill out the schema questionnaires; able to give informed consent after having received oral and written information Exclusion criteria: severe current mental illness, including bipolar I disorder, psychosis, or substance abuse disorders needing clinical detoxification; an established neurodegenerative disorder; cognitive impairment defined as a sum score below 23 points on the Montreal Cognitive Assessment (MoCA) battery; having received schema‐focussed therapy in the previous year or during the current illness episode; suicide risk interfering with adequate treatment delivery |
| Interventions | Two conditions: group schema‐focussed therapy enriched with psychomotor therapy (group SFT + PMT); or treatment‐as‐usual (TAU)
Details of conditions:
Duration of intervention: 18 weeks (plus 2 individual pre‐treatment sessions without PMT, to make a personal treatment plan and explain the concept of group SFT + PMT in more detail) Duration of trial: 26 weeks Length of follow‐up: unclear: the protocol reports follow‐up at 6 months and 12 months; the clinical trials register reports there are two follow‐up sessions, 1 at week 22 and 1 at week 26, i.e. 8 weeks post‐intervention |
| Outcomes |
Primary outcomes of trial:
Secondary outcomes of trial:
Other outcomes of trial:
|
| Starting date | 2017‐08‐01 |
| Contact information | Name: M.S.Veenstra Email: m.s.veenstra@umcg.nl Phone: +31 50 3612079 University Medical Center Groningen, Department of Psychiatry, P.O. Box 30.001, 9700 RB, Groningen, The Netherlands |
| Notes | Current trial ID: NL6443 Old trial ID: NTR6621 |
NCT04033835.
| Study name | Mentalisation Based Treatment ‐ Introductory group for male prisoners with borderline and/or antisocial personality disorder in Her Majesty's Prison Barlinnie |
| Methods | Design:Open label, cross‐over, randomised clinical trial |
| Participants |
Participants: Male sentenced prisoners with primary diagnosis of borderline PD and/or anti‐social PD Age:18 years and older Unit of allocation: individual Target sample size: 30 participants Inclusion criteria: primary diagnosis of BPD and/or AsPD; comorbidity with other personality disorder is accepted; sentenced prisoners with estimated date of liberation > six months Exclusion criteria: comorbid severe and enduring mental illness (schizophrenia, delusional disorder, bipolar affective disorder, major depressive disorder); comorbid organic brain disorder (acquired brain injury, alcohol‐related brain damage); remand prisoners; uncontrolled substance dependence; index offence of sexual offending; repeatedly chaotic, antisocial or violent behaviour in prison; care in segregation and reintegration unit in past 3 months; current individual specialist psychological therapy in prison; English as not first language |
| Interventions | Two conditions: Mentalisation‐Based Treatment‐Introductory (MBT‐I); or waiting‐list control/treatment‐as‐usual
Details of conditions:
Duration of intervention: 18 months Duration of trial: 21 months Length of follow‐up: 3 months post‐intervention |
| Outcomes |
Primary outcomes of trial
Secondary outcomes of trial (time frame for all secondary outcomes is 21 months; measures administered one week pre‐, one week post‐ and three months post‐intervention)
Other outcomes of trial
|
| Starting date | 1 August 2019a; estimated completion date 1 August 2021 |
| Contact information | Stephen Davidson (s.davidson7@nhs.net) Erica Packard (erica.packard@ggc.scot.nhs.uk) NHS Greater Glasgow and Clyde, Glasgow, United Kingdom |
| Notes | aThe last update on the clinical trials site [26 July 2019] stated that the study is not yet recruiting. |
AsPD = antisocial personality disorder ASUS = Adult Service Use Schedule AUDIT = Alcohol Use Disorders Identification Test BAI = Beck Anxiety Inventory BDI = Beck Depression Inventory BIS = Barratt Impulsiveness Scale BPD = borderline personality disorder BSI (‐53) = Brief Symptom Inventory CGI = Clinical Global Impression CORE‐OM = Clinical Outcomes in Routine Evaluation–Outcome Measure CSQ = Client Satisfaction Questionnaire CTR = Clinical Trial Register DSM‐IV‐R = Diagnostic and Statistical Manual of Mental Disorders‐Fourth Edition‐Revised DUDIT = Drug Use Disorders Identification Test EQ‐5D (‐5L) = EuroQol 5 dimensions, 5 levels instrument HTA = Health Technology Assessment IEP = incentives and enhanced privileges MAIA = Multidimensional Assessment of Interoceptive Awareness MASC = Movie for the Assessment of Social Cognition MBT (‐I) = mentalization based treatment‐introductory MCVSI = MacArthur Community Violence Screening Instrument MIH RRTP = mental health residential rehabilitation treatment programme MoCA = Montreal Cognitive Assessment MRI = magnetic resonance imaging MRT = moral reconation therapy NHSPM = National Household Survey of Psychiatric Morbidity OAS‐M = Overt Aggression Scale‐Modified PAU = probation as usual PCL‐R = Psychopathy Checklist‐Revised PD = personality disorder PMT = psychomotor therapy PPI‐R = Psychopathic Personality Inventory‐Revised PSP = psychological support for personality RFQ(54) = Reflective Functioning Questionnaire‐54 SAS‐SR = Social Adjustment Scale‐Self‐Report SBQ‐R = Suicidal Behaviours Questionnaire–Revised SCID‐5‐PD (‐11) = Structured Clinical Interview for DSM‐5 [DSM‐5 = Diagnostic and Statistical Manual of Mental Disorders‐Fifth Edition] for Personality Disorders SES = Service Engagement Scale SFQ = Social Functioning Questionnaire SFSUS = Secure Facilities Service Use Schedule SFT = schema‐focussed therapy SHI = Self Harm Inventory SIPP‐SF = Severity Indices of Personality Problems–Short Form STAXI 2 = State Trait Anger Expression Inventory 2 TAU = treatment as usual UC = usual care vs = versus WEMWBS = Warwick‐Edinburgh Mental Wellbeing Scale WSAS = Work and Social Adjustment Scale
Differences between protocol and review
This review differs from the original protocol (Gibbon 2009) and previous review (Gibbon 2010) in the following ways.
Authorship
For this update, the following review authors stepped down: Conor Duggan, Jutta Stoffers, Nick Huband, Michael Ferriter, and Klaus Lieb. They were replaced by Najat R Khalifa, Natalie H‐Y Cheung, and Lucy McCarthy.
Types of participants
For this update, we added an additional restriction to this section to apply to studies where participants with antisocial or dissocial personality disorder formed a small subgroup. This required that studies included in the review should have randomised at least five people with antisocial or dissocial personality disorder. The rationale was that variance and standard deviation cannot be calculated in samples of two or less, and so a two‐condition study randomising fewer than five (relevant) participants would have at least one arm for which the standard deviation could not be calculated (Newman 1939).
We included in this update, studies where the AsPD group or subgroup data were not available, but where at least 75% of participants had a diagnosis of AsPD. We chose a threshold of 75% as this appeared pragmatic and reflects that the overwhelming majority of participants have AsPD; these data were analysed separately.
Types of outcome measures
-
For this update, we:
modified the social functioning criteria to include also proxy measures of social functioning to reflect clinically relevant changes (e.g. decreased level of support required/time taken to achieve leave from hospital);
modified the outcome of 'substance misuse', so that a reader would find it easier to differentiate drug misuse outcomes from alcohol misuse outcomes (specifically, we replaced it with two separate categories: 'substance misuse ‐ drugs' and 'substance misuse ‐ alcohol');
added two additional secondary outcomes 'mental state' and 'prison and service outcomes' to collect data on outcomes relevant to participants' general mental health symptoms (i.e. specific symptoms such as dissociative experiences, mood/anxiety, or global mental health) and use of prison/probation services (e.g. treatment of people in the community, duration of treatment programme, changes in services provided by or through care/probation teams), respectively;
reported other outcomes measured in the included studies that did not fall into one of the above categories (continuous or dichotomous outcomes dependent upon how the outcomes were reported); and
took the decision to exclude any study that did not report any of our primary or secondary outcomes, as any additional outcomes would be considered to be clinically irrelevant, trivial or potentially confusing, and the review is already looking at a large number of clinically‐relevant outcomes (five primary outcomes and 12 secondary outcomes).
We acknowledge that there was an oversight in the original protocol regarding the possible use of dichotomous or time‐to‐event data for certain outcomes (e.g. reconviction, leaving the study early and adverse events); these outcomes are more likely to be dichotomous (or time‐to‐event), rather than continuous, data.
Search methods for identification of studies
In the previous version of the review (Gibbon 2010), we added the National Criminal Justice Reference Service Abstracts Database, to capture relevant studies in the justice and drug‐related literature.
-
For this update, we revised:
the list of electronic databases because we either no longer had access (ASSIA, BIOSIS, Dissertation Abstracts which we replaced with WorldCat, National Criminal Justice Reference Service Abstracts which we replaced with Criminal Justice Abstracts), or because previous searches were unproductive (OpenSIGLE, now OpenGrey, COPAC, which has since been replaced by Library Hub Discover.and Zetoc);
added two daily updated segments of MEDLINE (MEDLINE Epub Ahead of Print and MEDLINE In‐Process & Other Non‐Indexed Citations), which were unavailable last time;
used the Cochrane Database of Systematic Reviews and DARE, to identify other relevant systematic reviews, in order to search their reference lists;
did not search the specialised register of the Cochrane Schizophenia group because people with comorbid major functional mental illnesses (including schizophrenia) were excluded from this review; and
searched trials registers using WHO ICTRP as metaRegister of Controlled Trials was no longer available.
Data collection and analysis
This update omits six analyses specified in the original protocol because of insufficient data (see Table 16).
-
In this update, we added the following new methods, which we may use in future updates of this review (see Table 16).
We may consider widening the range of interventions examined in future reviews to include concepts such as 'motivation to change', in order to assess the impact, if any, this would have on producing a behaviour change.
Contrary to the protocol (Gibbon 2009), we have specified that we will summarise change‐from‐baseline ('change score') data alongside endpoint data where these are available in future updates of this review, and combine both data types in a meta‐analysis using the methods described by Da Costa 2013 since both types may be included together in meta‐analysis when using the MD (Higgins 2011a, p 270). However, we have specified that we would prefer change‐from‐baseline data to endpoint data if their distribution is less skewed, and that where the data are insufficient for meta‐analysis, we will report the results of the trial investigators' own statistical analyses comparing treatment and control conditions using change scores. We prefer change scores because they are more efficient and powerful than end scores.
To reduce ambiguity, we clarified that we would only draw funnel plots when there are more than 10 studies included in a meta‐analysis.
Where a meta‐analysis is undertaken, we will assess the impact of including studies with attrition rates greater than 50% through a sensitivity analysis. If inclusion of data from this group results in a substantive change in the estimate of effect of the primary outcomes, we will not add the data from these studies to trials with less attrition and will present them separately. Any imputation of data will be informed, where possible, by the reasons for attrition where these are available. We will interpret the results of any analysis based in part on imputed data with recognition that the effects of that imputation (and the assumptions on which it is based) can have considerable influence when samples are small. In studies with less than a 50% dropout rate, we will consider people leaving early to have had the negative outcome, except for adverse effects such as death.
We will consider pooling outcomes reported at different time points where this does not obscure the clinical significance of the outcome being assessed.
We explained how we would manage issues of multiplicity should they arise in future updates of the review, as this was missing from the protocol.
We have specified that we will conduct a sensitivity analysis of studies with data where at least 75% of participants have a diagnosis of antisocial personality disorder in order to test its impact on the results.
Summary of findings and assessment of the certainty of the evidence
In keeping with current recommendations, we included a new section on 'Summary of findings and assessment of the certainty of the evidence' in this update, in which we explain how we assessed the certainty of the evidence for clinically relevant outcomes and summarised these in a 'Summary of findings' table.
Contributions of authors
Simon Gibbon selected studies for inclusion, extracted data, assessed risk of bias, rated the certainty of the evidence, provided a clinical perspective, and helped to write and revise the final review. Simon Gibbon is the guarantor for the review.
Lucy McCarthy coordinated the review, selected studies for inclusion, obtained papers, extracted data, corresponded with study authors for additional information, entered data into Review Manager (Review Manager 2014), assessed risk of bias, rated the certainty of the evidence, interpreted the data, and wrote and revised the final review.
Natalie Cheung selected studies for inclusion, extracted data, assessed risk of bias, rated the certainty of the evidence, and contacted authors of papers for additional information.
Najat Khalifa selected studies for inclusion, extracted data, assessed risk of bias and rated the certainty of the evidence.
Birgit Vollm obtained and reviewed reports of studies published in the German language and provided resources for the review.
Sources of support
Internal sources
-
Nottinghamshire Healthcare NHS Foundation Trust, UK
Provided financial support for the time of LM, SG, NC and NK to facilitate review.
External sources
None, Other
Declarations of interest
Simon Gibbon ‐ none known.
Lucy McCarthy is a former colleague of the authors of Huband 2007 and is acknowledged in that study. She was not involved in the assessment of eligibility, extraction of data, or assessment of 'Risk of bias' for that study. However, she was involved in the GRADE assessment, but this was independently reviewed by Simon Gibbon.
Natalie H‐Y Cheung ‐ none known.
Najat Khalifa ‐ none known.
Birgit A Völlm ‐ none known.
Disclaimer: The results of a Cochrane Review can be interpreted differently depending on people's perspectives and circumstances. Please consider the conclusions presented carefully. They are the opinions of review authors, and are not necessarily those of the NHS or the Department of Health.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Asmand 2015 {published data only}
- Asmand P, Mami S, Valizade R. The effectiveness of dialectical behavior therapy and rational emotive behavior therapy in irrational believes treatment, anxiety among young male prisoners who have antisocial personality disorder in Ilam prison. International Journal of Health System & Disaster Management 2015;3(1):1-7. [DOI: 10.4103/2347-9019.147135] [DOI] [Google Scholar]
Ball 2005 {published data only}
- Ball SA, Cobb-Richardson P, Connolly AJ, Bujosa CT, O'Neall TW. Substance abuse and personality disorders in homeless drop-in center clients: symptom severity and psychotherapy retention in a randomized clinical trial. Comprehensive Psychiatry 2005;46(5):371-9. [DOI: 10.1016/j.comppsych.2004.11.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bernstein 2012 {published data only}
- Bernstein D, Arntz A. S18-04 Schema focused therapy for forensic patients with personality disorders: new research findings. European Psychiatry 2009;24(Suppl 1):S94. [DOI: 10.1016/S0924-9338(09)70327-X] [S18-04] [DOI] [Google Scholar]
- *.Bernstein DP, Nijman HL, Karos K, Keulen-de Vos M, De Vogel V, Lucker TP. Schema therapy for forensic patients with personality disorders: design and preliminary findings of a multicenter randomized clinical trial in the Netherlands. International Journal of Forensic Mental Health 2012;11(4):312-24. [DOI: 10.1080/14999013.2012.746757] [psycnet.apa.org/record/2012-33431-009] [DOI] [Google Scholar]
- Nentjes L, Bernstein D. S26-02 The effectiveness of schema-focused therapy; indirect, experimental measures of emotional change in forensic patients. European Psychiatry 2011;26(Suppl 1):2105. [DOI: 10.1016/S0924-9338(11)73808-1] [S26-02 ] [DOI] [Google Scholar]
- Van Den Broek E, Keulen-de Vos M, Bernstein DP. Arts therapies and schema focused therapy: a pilot study. Arts in Psychotherapy 2011;38(5):325-32. [DOI: 10.1016/j.aip.2011.09.005] [DOI] [Google Scholar]
Davidson 2009 {published data only}
- Davidson K, Halford J, Kirkwood L, Newton-Howes G, Sharp M, Tata P. CBT for violent men with antisocial personality disorder. Reflections on the experience of carrying out therapy in MASCOT, a pilot randomized controlled trial. Personality and Mental Health 2010;4:86-95. [DOI: 10.1002/pmh.94] [DOI] [Google Scholar]
- Davidson K (University of Glasgow, Faculty of Medicine, Gartnavel Royal Hospital, Glasgow, UK). [personal communication]. Conversation with Dr S Gibbon (Arnold Lodge, Nottinghamshire Healthcare NHS Foundation Trust, Leicester, UK) 14 August 2009.
- *.Davidson KM, Tyrer P, Tata P, Cooke D, Gumley A, Ford I, et al. Cognitive behaviour therapy for violent men with antisocial personality disorder in the community: an exploratory randomized controlled trial. Psychological Medicine 2009;39(4):569-77. [DOI: 10.1017/S0033291708004066] [PMID: ] [DOI] [PubMed] [Google Scholar]
Feigenbaum 2012 {published data only}
- Feigenbaum JD, Fonagy P, Pilling S, Jones A, Wildgoose A, Bebbington PE. A real-world study of the effectiveness of DBT in the UK National Health Service. British Journal of Clinical Psychology 2012;51(2):121-41. [DOI: 10.1111/j.2044-8260.2011.02017.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Havens 2007 {published data only}
- *.Havens JR, Cornelius LJ, Ricketts EP, Latkin CA, Bishai D, Lloyd JJ, et al. The effect of a case management intervention on drug treatment entry among treatment-seeking injection drug users with and without comorbid antisocial personality disorder. Journal of Urban Health 2007;84(2):267-71. [DOI: 10.1007/s11524-006-9144-4] [PMC2231639] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Ricketts EP, Huettner S, Cornelius L, Bishai D, Havens JR, et al. Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: results from a community-based behavioral intervention trial. Drug and Alcohol Dependence 2006;83(3):225-32. [DOI: 10.1016/j.drugalcdep.2005.11.015] [PMC2196224] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Huband 2007 {published data only}
- Huband N, McMurran M, Evans C, Duggan C. Social problem-solving plus psychoeducation for adults with personality disorder: pragmatic randomised controlled trial. British Journal of Psychiatry 2007;190:307-13. [DOI: 10.1192/bjp.bp.106.023341] [PMID: ] [DOI] [PubMed] [Google Scholar]
Marlowe 2007 {published data only}
- Marlowe DB, Festinger DS, Dugosh KL, Lee PA, Benasutti KM. Adapting judicial supervision to the risk level of drug offenders: discharge and 6-month outcomes from a prospective matching study. Drug and Alcohol Dependence 2007;88(Suppl 2):S4-S13. [DOI: 10.1016/j.drugalcdep.2006.10.001] [PMC1885231] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
McKay 2000 {published data only}
- *.McKay JR, Alterman AI, Cacciola JS, Mulvaney FD, O'Brien CH. Prognostic significance of antisocial personality disorders in cocaine-dependent patients entering continuing care. Journal of Nervous and Mental Disease 2000;188(5):287-96. [PMID: ] [DOI] [PubMed] [Google Scholar]
- McKay JR, Alterman AI, Cacciola JS, Rutherford MJ, O'Brian CP, Koppenhaver J. Group counselling versus individualized relapse prevention aftercare following intensive outpatient treatment for cocaine dependence: initial results. Journal of Consulting and Clinical Psychology 1997;65(5):778-88. [PMID: ] [DOI] [PubMed] [Google Scholar]
McMurran 2016 {published data only}
- *.McMurran M, Crawford MJ, Reilly J, Delport J, McCrone P, Whitham D, et al. Psychoeducation with problem-solving (PEPS) therapy for adults with personality disorder: a pragmatic randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of a manualised intervention to improve social functioning. Health Technology Assessment 2016;20(52):1-250. [DOI: 10.3310/hta20520] [PMC4967813] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMurran M, Crawford MJ, Reilly JG, McCrone P, Moran P, Williams H, et al. Psycho-education with problem solving (PEPS) therapy for adults with personality disorder: a pragmatic multi-site community-based randomised clinical trial. Trials 2011;12:198. [DOI: 10.1186/1745-6215-12-198] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMurran M, Day F, Reilly J, Delport J, McCrone P, Whitham D, et al. Psychoeducation and problem solving (PEPS) therapy for adults with personality disorder: a pragmatic randomized-controlled trial. Journal of Personality Disorders 2017;31(6):810-26. [DOI: 10.1521/pedi_2017_31_286] [PMID: ] [DOI] [PubMed] [Google Scholar]
Messina 2003 {published data only}
- *.Messina N, Farabee D, Rawson R. Treatment responsivity of cocaine-dependent patients with antisocial personality disorder to cognitive-behavioral and contingency management interventions. Journal of Consulting and Clinical Psychology 2003;71(2):320-9. [psycnet.apa.org/record/2003-02091-011] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Messina N. Cochrane Review [personal communication]. Email to: Unknown review author 19 October 2009.
Nathan 2019 {published and unpublished data}
- Miller K, Baker V, Oluonye S. From design to reality: the challenges of developing and delivering treatment and intervention services for offenders with personality disorders. Mental Health Review Journal 2010;15(4):46-50. [DOI: 10.5042/mhrj.2010.0739] [DOI] [Google Scholar]
- *.Nathan R, Centifanti L, Baker V, Hill J. A pilot randomised controlled trial of a programme of psychosocial interventions (Resettle) for high risk personality disordered offenders. International Journal of Law and Psychiatry 2019;66:101463. [DOI: 10.1016/j.ijlp.2019.101463] [PMID: ] [DOI] [PubMed] [Google Scholar]
Neufeld 2008 {published data only}
- Brooner RK, Kidorf M, King VL, Stoller K. Preliminary evidence of good treatment response in antisocial drug abusers. Drug and Alcohol Dependence 1998;49(3):249-60. [DOI: 10.1016/s0376-8716(98)00018-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
- *.Neufeld KJ, Kidorf MS, Kolodner K, King VL, Clark M, Brooner RK. A behavioral treatment for opioid-dependent patients with antisocial personality. Journal of Substance Abuse Treatment 2008;34(1):101-11. [10.1016/j.jsat.2007.02.009] [17574801] [PMC2193670] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neufeld KJ. Cochrane Review [personal communication]. Email to: N Huband 17 November 2009.
Priebe 2012 {published data only}
- Barnicott K. Effectiveness and cost-effectiveness of dialectical behaviour therapy for self-harming patients with personality disorder: a pragmatic randomised controlled trial (2012) [personal communication]. Email to: N Cheung 2 March 2017. [DOI] [PubMed]
- Barnicott K. Effectiveness and cost-effectiveness of dialectical behaviour therapy for self-harming patients with personality disorder: a pragmatic randomised controlled trial (2012) [personal communication]. Email to: N Cheung 24 February 2017. [DOI] [PubMed]
- *.Priebe S, Bhatti N, Barnicot K, Bremner S, Gaglia A, Katsakou C, et al. Effectiveness and cost-effectiveness of dialectical behaviour therapy for self-harming patients with personality disorder: a pragmatic randomised controlled trial. Psychotherapy and Psychosomatics 2012;81(6):356-65. [DOI: 10.1159/000338897] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tarrier 2010 {published data only}
- Doyle M, Tarrier N, Shaw J, Dunn G, Dolan M. Exploratory trial of schema-focussed therapy in a forensic personality disordered population. Journal of Forensic Psychiatry & Psychology 2016;27(2):232-47. [DOI: 10.1080/14789949.2015.1107119] [DOI] [Google Scholar]
- *.Tarrier N, Dolan M, Doyle M, Dunn G, Shaw J, Blackburn R. Exploratory randomised control trial of schema modal therapy in the personality disorder service at Ashworth Hospital; March 2010. www.ohrn.nhs.uk/resource/policy/RCTSchema.pdf.
Thylstrup 2015 {published data only}67266318
- Thylstrup B, Hesse M. Why run the risk? Motivation for offences by patients with substance use and antisocial personality disorders which they rated as most risky to their own well-being. Criminal Behaviour and Mental Health 2018;28(2):187-201. [DOI: 10.1002/cbm.2059] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Thylstrup B, Schrøder S, Fridell M, Hesse M. Did you get any help? A post-hoc secondary analysis of a randomized controlled trial of psychoeducation for patients with antisocial personality disorder in outpatient substance abuse treatment programs. BMC Psychiatry 2017;17(1):7. [DOI: 10.1186/s12888-016-1165-2] [PMC5223491] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Thylstrup B, Schrøder S, Hesse M. Psycho-education for substance use and antisocial personality disorder: a randomized trial. BMC Psychiatry 2015;15:283. [DOI: 10.1186/s12888-015-0661-0] [PMC4647713] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tyrer 2004 {published data only}
- Tyrer P, Tom B, Byford S, Schmidt U, Jones V, Davidson K, et al. Differential effects of manual assisted cognitive behavior therapy in the treatment of recurrent deliberate self-harm and personality disturbance: the POPMACT study. Journal of Personality Disorders 2004;18(1):102-16. [PMID: ] [DOI] [PubMed] [Google Scholar]
Woodall 2007 {published data only}
- Woodall WG, Delaney HD, Kunitz SJ, Westerberg VS, Zhao H. A randomized trial of a DWI intervention program for first offenders: intervention outcomes and interactions with antisocial personality disorder among a primarily American-Indian sample. Alcoholism, Clinical and Experimental Research 2007;31(6):974-87. [DOI: 10.1111/j.1530-0277.2007.00380.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Woody 1985 {published data only}
- Luborsky L, McLellan AT, Woody GE, O'Brien CP, Auerbach A. Therapist success and its determinants. Archives of General Psychiatry 1985;42(6):602-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Woody GE, Luborsky L, McLellan AT, O'Brien CP, Beck AT, Blaine J, et al. Psychotherapy for opiate addicts. Does it help? Archives of General Psychiatry 1983;40(6):639-45. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Woody GE, McLellan AT, Luborsky L, O'Brien CP, Blaine J, Fox S, et al. Severity of psychiatric symptoms as a predictor of benefits from psychotherapy: the Veterans Administration-Penn study. American Journal of Psychiatry 1984;141(10):1172-7. [DOI: 10.1176/ajp.141.10.1172] [PMID: ] [DOI] [PubMed] [Google Scholar]
- *.Woody GE, McLellan AT, Luborsky L, O'Brien CP. Sociopathy and psychotherapy outcome. Archives of General Psychiatry 1985;42(11):1081-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abbass 2008 {published data only}
- Abbass A, Sheldon A, Gyra J, Kalpin A. Intensive short-term dynamic psychotherapy for DSM-IV personality disorders: a randomized controlled trial. Journal of Nervous and Mental Disease 2008;196(3):211-6. [DOI: 10.1097/NMD.0b013e3181662ff0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Arnevik 2009 {published data only}
- Antonsen BT, Johansen MS, Rø FG, Kvarstein EH, Wilberg T. Is reflective functioning associated with clinical symptoms and long-term course in patients with personality disorders? Comprehensive Psychiatry 2016;64:46-58. [DOI: 10.1016/j.comppsych.2015.05.016] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Arnevik E, Wilberg T, Urnes Ø, Johansen M, Monsen JT, Karterud S. Psychotherapy for personality disorders: 18 months' follow-up of the Ullevål personality project. Journal of Personality Disorders 2010;24(2):188-203. [DOI: 10.1521/pedi.2010.24.2.188] [PMID: ] [DOI] [PubMed] [Google Scholar]
- *.Arnevik E, Wilberg T, Urnes O, Johansen M, Monsen JT, Karterud S. Psychotherapy for personality disorders: short-term day hospital psychotherapy versus outpatient individual therapy - a randomized controlled study. European Psychiatry 2009;24(2):71-8. [DOI: 10.1016/j.eurpsy.2008.09.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gullestad FS, Johansen MS, Høglend P, Karterud S, Wilberg T. Mentalization as a moderator of treatment effects: findings from a randomized clinical trial for personality disorders. Psychotherapy Research 2013;23(6):674-89. [DOI: 10.1080/10503307.2012.684103] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gullestad FS, Wilberg T, Klungsøyr O, Johansen MS, Urnes Ø, Karterud S. Is treatment in a day hospital step-down program superior to outpatient individual psychotherapy for patients with personality disorders? 36 months follow-up of a randomized clinical trial comparing different treatment modalities. Psychotherapy Research 2012;22(4):426-41. [DOI: 10.1080/10503307.2012.662608] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Klungsøyr O, Antonsen B, Wilberg T. Contours of a causal feedback mechanism between adaptive personality and psychosocial function in patients with personality disorders: a secondary analysis from a randomized clinical trial. BMC Psychiatry 2017;17(1):210. [DOI: 10.1186/s12888-017-1365-4] [PMC5460464] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvarstein EH, Arnevik E, Halsteinli V, Rø FG, Karterud FS, Wilberg T. Health service costs and clinical gains of psychotherapy for personality disorders: a randomized controlled trial of day-hospital-based step-down treatment versus outpatient treatment at a specialist practice. BMC Psychiatry 2013;13:315. [DOI: 10.1186/1471-244X-13-315] [PMC4222503] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bagby 2008 {published data only}
- Bagby RM, Quilty LC, Segal ZV, McBride CC, Kennedy SH, Costa PT. Personality and differential treatment response in major depression: a randomized controlled trial comparing cognitive-behavioural therapy and pharmacotherapy. Canadian Journal of Psychiatry 2008;53(6):361-70. [DOI: 10.1177/070674370805300605] [PMC2543930] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ball 2007 {published data only}
- Ball SA. Comparing individual therapies for personality disordered opioid dependent patients. Journal of Personality Disorders 2007;21(3):305-21. [DOI: 10.1521/pedi.2007.21.3.305] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ball 2011 {published data only}
- Ball SA, Maccarelli LM, LaPaglia DM, Ostrowski MJ. Randomized trial of dual-focused vs single-focused individual therapy for personality disorders and substance dependence. Journal of Nervous and Mental Disease 2011;199(5):319-28. [DOI: 10.1097/NMD.0b013e3182174e6f] [PMC3100211] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bartak 2010 {published data only}
- Bartak A. On the Effectiveness of Psychotherapy in Personality Disorders [PhD Thesis]. Amsterdam (NL): University of Amsterdam, 2010. [Google Scholar]
Bateman 2009 {published data only}
- *.Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. American Journal of Psychiatry 2009;166(12):1355-64. [DOI: 10.1176/appi.ajp.2009.09040539] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Bateman A, O’Connell J, Lorenzini N, Gardner T, Fonagy P. A randomised controlled trial of mentalization-based treatment versus structured clinical management for patients with comorbid borderline personality disorder and antisocial personality disorder. BMC Psychiatry 2016;16(1):304. [DOI: 10.1186/s12888-016-1000-9] [PMC5006360] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bianchini 2019 {published data only}
- Bianchini V, Cofini V, Curto M, Lagrotteria B, Manzi A, Navari S, et al. Dialectical behaviour therapy (DBT) for forensic psychiatric patients: an Italian pilot study. Criminal Behaviour and Mental Health 2019;29(2):122-30. [DOI: 10.1002/cbm.2102] [PMID: ] [DOI] [PubMed] [Google Scholar]
Blattman 2017 {published data only}
- Blattman C, Jamison JC, Sheridan M. Reducing crime and violence: experimental evidence from cognitive behavioral therapy in Liberia. American Economic Review 2017;104(4):1165-206. [DOI: 10.3386/w21204] [DOI] [PubMed] [Google Scholar]
Bowen 2009 {published data only}
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, et al. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Substance Abuse 2009;30(4):295-305. [DOI: 10.1080/08897070903250084] [NIHMS353693] [PMC3280682] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brazão 2015 {published data only}
- Brazão N, Da Motta C, Rijo D, Do Céu Salvador M, Pinto-Gouveia J, Ramos J. Clinical change in anger, shame, and paranoia after a structured cognitive-behavioral group program: early findings from a randomized trial with male prison inmates. Journal of Experimental Criminology 2015;11(2):217-37. [DOI: 10.1007/s11292-014-9224-5] [psycnet.apa.org/record/2015-04499-001] [DOI] [Google Scholar]
- *.Brazão N, Da Motta C, Rijo D, Do Céu Salvador M, Pinto-Gouveia J, Ramos J. Clinical change in cognitive distortions and core schemas after a cognitive–behavioral group intervention: preliminary findings from a randomized trial with male prison inmates. Cognitive Therapy and Research 2015;39(5):578–89. [DOI: 10.1007/s10608-015-9693-5] [psycnet.apa.org/record/2015-42214-001] [DOI] [Google Scholar]
- Brazão N, Rijo D, Da Silva DR, Do Céu Salvador M, Pinto-Gouveia J. Personality pathology profiles as moderators of the growing pro-social program: outcomes on cognitive, emotion, and behavior regulation in male prison inmates. Journal of Personality Disorders 2019 April 15 [Epub ahead of print]. [DOI: 10.1521/pedi_2019_33_424] [PMID: ] [DOI] [PubMed]
- Brazão N, Rijo D, Do Céu Salvador M, Pinto-Gouveia J. The effects of the growing pro-social program on cognitive distortions and early maladaptive schemas over time in male prison inmates: a randomized controlled trial. Journal of Consulting and Clinical Psychology 2017;85(11):1064-79. [DOI: 10.1037/ccp0000247] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Brazão N, Rijo D, Do Céu Salvador M, Pinto-Gouveia J. The efficacy of the growing pro-social program in reducing anger, shame, and paranoia over time in male prison inmates: a randomized controlled trial. Journal of Research in Crime and Delinquency 2018;55(5):649-86. [DOI: 10.1177/0022427818782733] [DOI] [Google Scholar]
Chen 2014 {published data only}
- Chen C, Li C, Wang H, Ou JJ, Zhou JS, Wang XP. Cognitive behavioral therapy to reduce overt aggression behavior in Chinese young male violent offenders. Aggressive Behavior 2014;40(4):329-36. [DOI: 10.1002/ab.21521] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chiesa 2003 {published data only}
- Chiesa M, Fonagy P. Psychosocial treatment for severe personality disorder: 36 month follow-up. British Journal of Psychiatry 2003;183:356-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Colom 2004 {published data only}
- Colom F, Vieta E, Sánchez-Moreno J, Martiíez-Arán A, Torrent C, Reinares M, et al. Psychoeducation in bipolar patients with comorbid personality disorders. Bipolar Disorders 2004;6(4):294-8. [DOI: 10.1111/j.1399-5618.2004.00127.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Conrad 2017 {published data only}
- Conrad AM, Sankaranarayanan A, Lewin TJ, Dunbar A. Effectiveness of a 10-week group program based on dialectical behaviour therapy skills among patients with personality and mood disorders: findings from a pilot study. Australasian Psychiatry 2017;25(5):466-70. [DOI: 10.1177/1039856217707393] [PMID: ] [DOI] [PubMed] [Google Scholar]
Crane 2015 {published data only}
- Crane CA, Eckhardt CI, Schlauch RC. Motivational enhancement mitigates the effects of problematic alcohol use on treatment compliance among partner violent offenders: results of a randomized clinical trial. Journal of Consulting and Clinical Psychology 2015;83(4):689-95. [DOI: 10.1037/a0039345] [PMC4881299] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Daughters 2008 {published data only}
- Daughters SB, Stipelman BA, Sargeant MN, Schuster R, Bornovalova MA, Lejuez CW. The interactive effects of antisocial personality disorder and court-mandated status on substance abuse treatment dropout. Journal of Substance Abuse Treatment 2008;34(2):157-64. [DOI: 10.1016/j.jsat.2007.02.007] [PMC3586262] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davidson 2014 {published data only}
- Davidson K. Re: manual-assisted cognitive therapy for self-harm in PD and substance misuse (2014) [personal communication]. Email to: N Cheung 28 February 2017.
- *.Davidson KM, Brown TM, James V, Kirk J, Richardson J. Manual-assisted cognitive therapy for self-harm in personality disorder and substance misuse: a feasibility trial. Psychiatric Bulletin 2014;38(3):108-11. [DOI: 10.1192/pb.bp.113.043109] [PMC4115373] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 2018 {published data only}
- Davis M, Sheidow AJ, McCart MR, Perrault RT. Vocational coaches for justice-involved emerging adults. Psychiatric Rehabilitation Journal 2018;41(4):266-76. [DOI: 10.1037/prj0000323] [PMC6776998 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dean 2013 {published data only}
- Dean K. A multi-centre RCT of a group psychological intervention to reduce antisocial behaviour in a medium secure setting. Australian and New Zealand Journal of Psychiatry 2013;47(Suppl 1):18-9. [DOI: 10.1177/0004867412486854] [DOI] [Google Scholar]
De Jong 2013 {published data only}
- De Jong A, Van der Heiden C, Deen M. Treatment of patients with personality problems: group versus individual treatment [Behandeling van patiënten met persoonlijkheidsproblematiek: groep versus individuele behandeling]. Gedragstherapie 2013;46(2):77-88. [www.tijdschriftgedragstherapie.nl/scripts/shared/artikel_pdf.php?id=TG-2013-2-3] [Google Scholar]
De Jong 2018 {published data only}
- De Jong K, Segaar J, Ingenhoven T, Van Busschbach J, Timman R. Adverse effects of outcome monitoring feedback in patients with personality disorders: a randomized controlled trial in day treatment and inpatient settings. Journal of Personality Disorders 2018;32(3):393-413. [DOI: 10.1521/pedi_2017_31_297] [PMID: ] [DOI] [PubMed] [Google Scholar]
Deng 2019 {published data only}
- Deng Y, Xiang R, Zhu Y, Li Y, Yu S, Liu X. Counting blessings and sharing gratitude in a Chinese prisoner sample: effects of gratitude-based interventions on subjective well-being and aggression. Journal of Positive Psychology 2019;14(3):303-11. [DOI: 10.1080/17439760.2018.1460687] [DOI] [Google Scholar]
Doyle 2013 {published data only}
- Doyle M, Khanna T, Lennox C, Shaw J, Hayes A, Taylor J, et al. The effectiveness of an enhanced thinking skills programme in offenders with antisocial personality traits. Journal of Forensic Psychiatry & Psychology 2013;24(1):1-15. [DOI: 10.1080/14789949.2012.752519] [DOI] [Google Scholar]
DRKS0001326 {published data only}
- DRKS00013266. Schema therapy for inpatients with personality disorders. www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00013266 (first received 03 November 2017).
Easton 2007 {published data only}
- Easton CJ, Babuscio T, Carroll KM. Treatment retention and outcome among cocaine-dependent patients with and without active criminal justice involvement. Journal of the American Academy of Psychiatry and the Law 2007;35(1):83-91. [PMID: ] [PubMed] [Google Scholar]
Easton 2012 {published data only}
- Easton CJ, Oberleitner LM, Scott MC, Crowley MJ, Babuscio TA, Carroll KM. Differences in treatment outcome among marijuana-dependent young adults with and without antisocial personality disorder. American Journal of Drug and Alcohol Abuse 2012;38(4):305-13. [DOI: 10.3109/00952990.2011.643989] [PMC3633215] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Elsner 2016 {published data only}
- Elsner K, König A. Schema-oriented psychotherapy with forensic patients [Schemaorientierte psychotherapie mit forensischen patienten]. Forensische Psychiatrie Psychologie Kriminologie 2016;10(1):4-13. [DOI: 10.1007/s11757-015-0354-z] [DOI] [Google Scholar]
Fournier 2008 {published data only}
- *.Fournier JC, DeRubeis RJ, Shelton RC, Gallop R, Amsterdam JD, Hollon SD. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. British Journal of Psychiatry 2008;192(2):124-9. [DOI: 10.1192/bjp.bp.107.037234] [PMC2682552] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier JC. Cochrane enquiry [personal communication]. Email to: Unknown review author 3 June 2009.
Frisman 2009 {published data only}
- *.Essock SM, Mueser KT, Drake RE, Covell NH, McHuga GJ, Frisman LK, et al. Comparison of ACT and standard case management for delivering integrated treatment for co-occurring disorders. Psychiatric Services 2006;57(2):185-96. [DOI: 10.1176/appi.ps.57.2.185] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Frisman LK, Mueser KT, Covell NH, Lin HJ, Crocker A, Drake RE, et al. Use of integrated dual disorder treatment via assertive community treatment versus clinical case management for persons with co-occurring disorders and antisocial personality disorder. Journal of Nervous and Mental Disease 2009;197(11):822-8. [DOI: 10.1097/NMD.0b013e3181beac52] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Mueser KT, Crocker AG, Frisman LB, Drake RE, Covell NH, Essock SM. Conduct disorder and antisocial personality disorder in persons with severe psychiatric and substance use disorders. Schizophrenia Bulletin 2006;32(4):626-36. [DOI: 10.1093/schbul/sbj068] [PMC2632266] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grenyer 2018 {published data only}
- *.Grenyer BFS, Lewis KL, Fanaian M, Kotze B. Treatment of personality disorder using a whole of service stepped care approach: a cluster randomized controlled trial. PLOS One 2018;13(11):e0206472. [DOI: 10.1371/journal.pone.0206472] [PMC6219775] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grenyer BFS. An integrative relational step-down model of care: the Project Air Strategy for personality disorders. ACPARIAN 2014;9:8-13. [projectairstrategy.org/content/groups/public/@web/@ihmri/documents/doc/uow177533.pdf] [Google Scholar]
- McCarthy L. Cochrane review query [personal communication]. Email to: BFS Grenyer 12 September 2019.
Gysin‐Maillart 2016 {published data only}
- *.Gysin-Maillart A, Schwab S, Soravia L, Megert M, Michel K. A novel brief therapy for patients who attempt suicide: a 24-months follow-up randomized controlled study of the Attempted Suicide Short Intervention Program (ASSIP). PLOS Medicine 2016;13(3):e1001968. [DOI: 10.1371/journal.pmed.1001968] [PMC4773217] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michel K. 24-months follow-up randomized controlled dtudy of the ASSIP [personal communication]. Email to: N Cheung 22 March 2017.
Haeyen 2018 {published data only}
- Haeyen S, Kleijberg M, Hinz L. Art therapy for patients diagnosed with personality disorders cluster B/C: a thematic analysis of emotion regulation from patient and art therapist perspectives. International Journal of Art Therapy: Inscape 2018;23(4):156-68. [DOI: 10.1080/17454832.2017.1406966] [DOI] [Google Scholar]
- Haeyen S, Van Hooren S, Dehue F, Hutschemaekers G. Development of an art-therapy intervention for patients with personality disorders: an intervention mapping study. International Journal of Art Therapy 2018;23(3):125-35. [DOI: 10.1080/17454832.2017.1403458] [DOI] [Google Scholar]
- *.Haeyen S, Van Hooren S, Van Der Veld W, Hutschemaekers G. Efficacy of art therapy in individuals with personality disorders cluster B/C: a randomized controlled trial. Journal of Personality Disorders 2018;32(4):527-42. [DOI: 10.1521/pedi_2017_31_312] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hakvoort 2015 {published data only}
- *.Hakvoort L, Bogaerts S, Thaut MH, Spreen M. Influence of music therapy on coping skills and anger management in forensic psychiatric patients: an exploratory study. International Journal of Offender Therapy and Comparative Criminology 2015;59(8):810-36. [DOI: 10.1177/0306624X13516787] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Hakvoort L. Cochrane Review update-request for information [personal communication]. Email to: L McCarthy 21 November 2017.
Hesse 2010 {published data only}
- Hesse M. Psychoeducation for personality disorders as an add-on to substance abuse treatment versus attention placebo: a controlled trial. Drugs and Alcohol Today 2010;10(1):25-32. [DOI: 10.5042/daat.2010.0125] [DOI] [Google Scholar]
Hesselbrock 1991 {published data only}
- Hesselbrock MN. Gender comparison of antisocial personality disorder and depression in alcoholism. Journal of Substance Abuse 1991;3(2):205-19. [PMID: ] [DOI] [PubMed] [Google Scholar]
Holmqvist 2009 {published data only}
- Holmqvist R, Hill T, Lang A. Effects of aggression replacement training in young offender institutions. International Journal of Offender Therapy and Comparative Criminology 2009;53(1):74-92. [DOI: 10.1177/0306624X07310452] [PMID: ] [DOI] [PubMed] [Google Scholar]
Høglend 2011 {published data only}
- Høglend P, Dahl HS, Hersoug AG, Lorentzen S, Perry JC. Long-term effects of transference interpretation in dynamic psychotherapy of personality disorders. European Psychiatry 2011;26(7):419-24. [DOI: 10.1016/j.eurpsy.2010.05.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Johnson 2013 {published data only}
- Blevins D, Wang XQ, Sharma S, Ait-Daoud N. Impulsiveness as a predictor of topiramate response for cocaine use disorder. American Journal on Addictions 2019;28(2):71-6. [DOI: 10.1111/ajad.12858] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Johnson BA, Ait-Daoud N, Wang XQ, Penberthy JK, Javors MA, Seneviratne C, et al. Topiramate for the treatment of cocaine addiction: a randomized clinical trial. JAMA Psychiatry 2013;70(12):1338-46. [DOI: 10.1001/jamapsychiatry.2013.2295] [DOI] [PubMed] [Google Scholar]
Kallert 2007 {published data only}
- *.Kallert TW, Priebe S, McCabe R, Kiejna A, Rymaszewska J, Nawka P, et al. Are day hospitals effective for acutely ill psychiatric patients? A European multicenter randomized controlled trial. Journal of Clinical Psychiatry 2007;68(2):278-97. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kallert TW. Cochrane enquiry [personal communication]. Email to: Unknown review author 2 June 2009.
Keefe 2016 {published data only}
- DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Archives of General Psychiatry 2005;62(4):409-16. [DOI: 10.1001/archpsyc.62.4.409] [PMID: ] [DOI] [PubMed] [Google Scholar]
- *.Keefe JR, Webb CA, DeRubeis RJ. In cognitive therapy for depression, early focus on maladaptive beliefs may be especially efficacious for patients with personality disorders. Journal of Consulting and Clinical Psychology 2016;84(4):353–64. [DOI: 10.1037/ccp0000071] [PMC4936187] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Keefe 2018 {published data only}
- *.Keefe JR, Milrod BL, Gallop R, Barber JP, Chambless DL. What is the effect on comorbid personality disorder of brief panic-focused psychotherapy in patients with panic disorder? Depression and Anxiety 2018;35(3):239-47. [DOI: 10.1002/da.22708] [PMC5842115 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milrod B, Chambless DL, Gallop R, Busch FN, Schwalberg M, McCarthy KS, et al. Psychotherapies for panic disorder: a tale of two sites. Journal of Clinical Psychiatry 2016;77(7):927-35. [DOI: 10.4088/JCP.14m09507] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kelly 2009 {published data only}
- Kelly BD, Nur UA, Tyrer P, Casey P. Impact of severity of personality disorder on the outcome of depression. European Psychiatry 2009;24(5):322-6. [DOI: 10.1016/j.eurpsy.2008.12.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kingston 2018 {published data only}
- *.Kingston DA, Olver ME, McDonald J, Cameron C. A randomised controlled trial of a cognitive skills programme for offenders with mental illness. Criminal Behaviour and Mental Health 2018;28(4):369-82. [DOI: 10.1002/cbm.2077] [PMID: ] [DOI] [PubMed] [Google Scholar]
- McCarthy L. Cochrane Review query [personal communication]. Email to: D Kingston 27 November 2018.
Klein Tuente 2018 {published data only}
- Klein Tuente S, Bogaerts S, Van Ijzendoorn S, Veling W. Effect of virtual reality aggression prevention training for forensic psychiatric patients (VRAPT): study protocol of a multi-center RCT. BMC Psychiatry 2018;18(1):251. [DOI: 10.1186/s12888-018-1830-8] [PMC6091200] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kool 2003 {published data only}
- *.Kool S, Dekker J, Duijsens IJ, De Jonghe F, Puite B. Efficacy of combined therapy and pharmacotherapy for depressed patients with and without personality disorders. Harvard Review of Psychiatry 2003;11(3):133-41. [DOI: 10.1080/10673220303950] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kool S. Cochrane enquiry [personal communication]. Email to: J Dennis 29 May 2009.
Kool 2007 {published data only}
- Kool S, Schoevers R, Duijsens IJ, Peen J, Van AAlst G, De Jonghe F, et al. Treatment of depressive disorder and comorbid personality pathology: combined therapy versus pharmacotherapy [Behandeling van de depressieve stoornis en comorbide persoonlijkheidspathologie: gecombineerde therapie versus farmacotherapie]. Tijdschrift voor Psychiatrie 2007;49(6):361-72. [www.tijdschriftvoorpsychiatrie.nl/assets/articles/articles_1635pdf.pdf] [PMID: ] [PubMed] [Google Scholar]
Kool 2018 {published data only}
- Kool M, Van HL, Bartak A, De Maat SCM, Arntz A, Van Den Eshof JW, et al. Optimizing psychotherapy dosage for comorbid depression and personality disorders (PsyDos): a pragmatic randomized factorial trial using schema therapy and short-term psychodynamic psychotherapy. BMC Psychiatry 2018;18(1):252. [DOI: 10.1186/s12888-018-1829-1] [PMC6081852 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Korrelboom 2011 {published data only}
- Korrelboom K, Marissen M, Van Assendelft T. Competitive memory training (COMET) for low self-esteem in patients with personality disorders: a randomized effectiveness study. Behavioural and Cognitive Psychotherapy 2011;39(1):1-19. [DOI: 10.1017/S1352465810000469] [PMID: ] [DOI] [PubMed] [Google Scholar]
Larden 2018 {published data only}
- Larden M, Norden E, Forsman M, Langstrom N. Effectiveness of aggression replacement training in reducing criminal recidivism among convicted adult offenders. Criminal Behaviour and Mental Health 2018;28(6):476-91. [DOI: 10.1002/cbm.2092] [DOI] [PubMed] [Google Scholar]
Lay 2018 {published data only}
- *.Lay B, Kawohl W, Rössler W. Outcomes of a psycho-education and monitoring programme to prevent compulsory admission to psychiatric inpatient care: a randomised controlled trial. Psychological Medicine 2018;48(5):849-60. [DOI: 10.1017/s0033291717002239] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Lay B. Cochrane enquiry [personal communication]. Email to: L McCarthy 21 November 2018.
Leichsenring 2016 {published data only}
- Leichsenring F, Masuhr O, Jaeger U, Rabung S, Dally A, Dümpelmann M, et al. Psychoanalytic-interactional therapy versus psychodynamic therapy by experts for personality disorders: a randomized controlled efficacy-effectiveness study in cluster B personality disorders. Psychotherapy and Psychosomatics 2016;85(2):71-80. [DOI: 10.1159/000441731] [PMID: ] [DOI] [PubMed] [Google Scholar]
Liberman 1981 {published data only}
- Liberman RP, Eckman T. Behavior therapy vs insight-oriented therapy for repeated suicide attempters. Archives of General Psychiatry 1981;38(10):1126-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
Longabaugh 1994 {published data only}
- Longabaugh R, Rubin A, Malloy P, Beattie M, Clifford PR, Noel N. Drinking outcomes of alcohol abusers diagnosed as antisocial personality disorder. Alcoholism, Clinical and Experimental Research 1994;18(4):778-85. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lorentzen 2013 {published data only}
- Fjeldstad A, Høglend P, Lorentzen S. Presence of personality disorder moderates the long-term effects of short-term and long-term psychodynamic group therapy: a 7-year follow-up of a randomized clinical trial. Group Dynamics: Theory, Research, and Practice 2016;20(4):294-309. [DOI: 10.1037/gdn0000055] [psycnet.apa.org/record/2016-51692-001] [DOI] [Google Scholar]
- Lorentzen S, Fjeldstad A, Ruud T, Marble A, Klungsøyr O, Ulberg R, et al. The effectiveness of short- and long-term psychodynamic group psychotherapy on self-concept: three years follow-up of a randomized clinical trial. International Journal of Group Psychotherapy 2015;65(3):362-85. [DOI: 10.1521/ijgp.2015.65.3.362] [DOI] [PubMed] [Google Scholar]
- *.Lorentzen S, Ruud T, Fjeldstad A, Høglend P. Comparison of short- and long-term dynamic group psychotherapy: randomised clinical trial. British Journal of Psychiatry 2013;203(3):280-7. [DOI: 10.1192/bjp.bp.112.113688] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Lorentzen S, Ruud T, Fjeldstad A, Høglend PA. Personality disorder moderates outcome in short- and long-term group analytic psychotherapy: a randomized clinical trial. British Journal of Clinical Psychology 2015;54(2):129-46. [DOI: 10.1111/bjc.12065] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lynch 2007 {published data only}
- Lynch TR, Cheavens JS, Cukrowicz KC, Thorp SR, Bronner L, Beyer J. Treatment of older adults with co-morbid personality disorder and depression: a dialectical behavior therapy approach. International Journal of Geriatric Psychiatry 2007;22(2):131-43. [DOI: 10.1002/gps.1703] [PMID: ] [DOI] [PubMed] [Google Scholar]
McGauley 2011 {published data only}
- McGauley G, Yakeley J, Williams A, Bateman A. Attachment, mentalization and antisocial personality disorder: the possible contribution of mentalization-based treatment. European Journal of Psychotherapy & Counselling 2011;13(4):371-93. [DOI: 10.1080/13642537.2011.629118] [DOI] [Google Scholar]
McMurran 2013 {published data only}
- McMurran M, Cox WM, Coupe S, Whitham D, Hedges L. The addition of a goal-based motivational interview to standardised treatment as usual to reduce dropouts in a service for patients with personality disorder: a feasibility study. Trials 2010;11:98. [DOI: 10.1186/1745-6215-11-98] [PMC2964698] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.McMurran M, Cox WM, Whitham D, Hedges L. The addition of a goal-based motivational interview to treatment as usual to enhance engagement and reduce dropouts in a personality disorder treatment service: results of a feasibility study for a randomized controlled trial. Trials 2013;14:50. [DOI: 10.1186/1745-6215-14-50] [PMC3598789] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Messina 2002 {published data only}
- Messina NP, Wish ED, Hoffman JA, Nemes S. Antisocial personality disorder and TC treatment outcomes. American Journal of Drug and Alcohol Abuse 2002;28(2):197-212. [PMID: ] [DOI] [PubMed] [Google Scholar]
Milrod 2007 {published data only}
- Milrod BI, Leon AC, Barber JP, Markowitz JC, Graf E. Do comorbid personality disorders moderate panic-focused psychotherapy? An exploratory examination of the American Psychiatric Association practice guideline. Journal of Clinical Psychiatry 2007;68(6):885-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mörtberg 2007 {published data only}
- Mörtberg E, Bejerot S, Aberg Wistedt A. Temperament and character dimensions in patients with social phobia: patterns of change following treatments? Psychiatry Research 2007;152(1):81-90. [DOI: 10.1016/j.psychres.2006.10.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Muran 2009 {published data only}
- Muran JC, Safran JD, Gorman BS, Samstag LW, Eubanks-Carter C, Winston A. The relationship of early alliance ruptures and their resolution to process and outcome in three time-limited psychotherapies for personality disorders. Psychotherapy 2009;46(2):233-48. [DOI: 10.1037/a0016085] [PMID: ] [DOI] [PubMed] [Google Scholar]
NCT03382808 {published data only}
- *.NCT03382808. Emotion recognition training in antisocial violent offenders with psychopathic traits. clinicaltrials.gov/show/nct03382808 (first received 12 December 2017).
- Schönenberg M, Christian S, Gaußer AK, Mayer SV, Hautzinger M, Jusyte A. Addressing perceptual insensitivity to facial affect in violent offenders: first evidence for the efficacy of a novel implicit training approach. Psychological Medicine 2014;44(5):1043-52. [DOI: 10.1017/S0033291713001517] [PMID: ] [DOI] [PubMed] [Google Scholar]
NCT03677037 {published data only}
- NCT03677037. The short-term MBT project (MBT-RCT) [Short-term versus long-term mentalization-based therapy for outpatients with subthreshold or diagnosed borderline personality disorder: a randomized clinical trial]. clinicaltrials.gov/ct2/show/NCT03677037 (first received 14 September 2018).
Nitschke 2018 {published data only}
- Nitschke J, Sünkel Z, Mokros A. Forensic preventive assertive community treatment: pilot project to prevent violent crimes in the context of psychiatric disorders [Die forensische praventionsambulanz: modellprojekt zur vermeidung von gewalttaten im rahmen psychischer erkrankungen]. Der Nervenarzt 2018;89(9):1054-62. [DOI: 10.1007/s00115-018-0573-6] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pearce 2017 {published data only}
- Pearce S, Scott L, Attwood G, Saunders K, Dean M, De Ridder R, et al. Democratic therapeutic community treatment for personality disorder: randomised controlled trial. British Journal of Psychiatry 2017;210(2):149-56. [DOI: 10.1192/bjp.bp.116.184366] [PMID: ] [DOI] [PubMed] [Google Scholar]
Petersen 2008 {published data only}
- Petersen B, Toft J, Christensen NB, Foldager L, Munk-Jörgensen P, Lien K, et al. Outcome of a psychotherapeutic programme for patients with severe personality disorders. Nordic Journal of Psychiatry 2008;62(6):450-6. [DOI: 10.1080/08039480801984271] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rademacher 2013 {published data only}
- Rademacher J, Lehmann W, Menzel D, Lampe R. Taming the wrath - effects of systemic individual therapy in violent behavior [Zähmung des zorns –effekte dystemischer einzeltherapie bei gewalttätigem verhalten]. Familiendynamik 2013;38(04):308-21. [www.familiendynamik.de/article/fd_2013_04_0308-0321_0308_01] [Google Scholar]
Rees‐Jones 2012 {published data only}
- Rees-Jones A, Gudjonsson G, Young S. A multi-site controlled trial of a cognitive skills program for mentally disordered offenders. BMC Psychiatry 2012;12:44. [DOI: 10.1186/1471-244X-12-44] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sewall 2019 {published data only}
- Sewall LA, Olver ME. Psychopathy and treatment outcome: results from a sexual violence reduction program. Personality Disorders: Theory, Research, and Treatment 2019;10(1):59-69. [DOI: 10.1037/per0000297] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shaw 2017 {published data only}
- Shaw J, Higgins C, Quartey C. The impact of collaborative case formulation with high risk offenders with personality disorder. Journal of Forensic Psychiatry & Psychology 2017;28(6):777-89. [DOI: 10.1080/14789949.2017.1324579] [DOI] [Google Scholar]
Sloane 1976 {published data only}
- Sloane RB, Staples FR, Cristol AH, Yorkston NJ, Whipple K. Patient characteristics and outcome in psychotherapy and behavior therapy. Journal of Consulting and Clinical Psychology 1976;44(3):330-9. [932262] [DOI] [PubMed] [Google Scholar]
Springer 1996 {published data only}
- Springer T, Lohr NE, Buchtel HA, Silk KR. A preliminary report of short-term cognitive-behavioral group therapy for inpatients with personality disorders. Journal of Psychotherapy Practice and Research 1996;5(1):57-71. [PMC3330405] [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Suszek 2015 {published data only}
- Suszek H, Holas P, Wyrzykowski T, Lorentzen S, Kokoszka A. Short-term intensive psychodynamic group therapy versus cognitive-behavioral group therapy in day treatment of anxiety disorders and comorbid depressive or personality disorders: study protocol for a randomized controlled trial. Trials 2015;16:319. [DOI: 10.1186/s13063-015-0827-6] [PMC4517633] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Swogger 2016 {published data only}
- Swogger MT, Conner KR, Caine ED, Trabold N, Parkhurst MN, Prothero LM, et al. A test of core psychopathic traits as a moderator of the efficacy of a brief motivational intervention for substance-using offenders. Journal of Consulting and Clinical Psychology 2016;84(3):248-58. [DOI: 10.1037/ccp0000065] [PMC4760863] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tomlinson 2017 {published and unpublished data}
- Tomlinson M. Cochrane review enquiry [personal communication]. Email to: L McCarthy 9 November 2018.
- *.Tomlinson MF, Hoaken PNS. The potential for a skills-based dialectical behavior therapy program to reduce aggression, anger, and hostility in a Canadian forensic psychiatric sample: a pilot study. International Journal of Forensic Mental Health 2017;16(3):215-26. [DOI: 10.1080/14999013.2017.1315469] [DOI] [Google Scholar]
Tyrer 2009 {published data only}
- Tyrer P, Cooper S, Rutter D, Seivewright H, Duggan C, Maden T, et al. The assessment of dangerous and severe personality disorder: lessons from a randomised controlled trial linked to qualitative analysis. Journal of Forensic Psychiatry & Psychology 2009;20(1):132-46. [10.1080/14789940802236872] [Google Scholar]
Urban 2015 {published data only}
- *.Urban S, Dehn LB, Zillmer B, Driessen M, Beblo T. Effects of dog-assisted therapy on patients during their stationary drug withdrawal in an acute psychiatry hospital [Effekte eines therapiebegleit-hundes auf patienten im stationären drogenentzug]. SUCHT 2015;61(3):139-46. [DOI: 10.1024/0939-5911.a000366] [DOI] [Google Scholar]
- Urban S. Effects of a dog-assisted therapy on patients during their stationary drug withdrawal in an acute psychiatry hospital (2015) [personal communication]. Email to: N Cheung 14 February 2017.
Välimäki 2017 {published data only}
- Välimäki M, Yang M, Normand SL, Lorig KR, Anttila M, Lantta T, et al. Study protocol for a cluster randomised controlled trial to assess the effectiveness of user-driven intervention to prevent aggressive events in psychiatric services. BMC Psychiatry 2017;17(1):123. [DOI: 10.1186/s12888-017-1266-6] [PMC5379524] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vannoy 2004 {published data only}
- Vannoy SD, Hoyt WT. Evaluation of an anger therapy intervention for incarcerated adult males. Journal of Offender Rehabilitation 2004;39(2):39-57. [DOI: 10.1300/J076v39n02_03] [DOI] [Google Scholar]
Vera 2008 {published data only}
- Vera L, Mirabel-Sarron C, Ba K. Cognitive and behavioral therapy of obsessive and compulsive troubles with associated personality troubles: group therapy [Thérapie comportementale et cognitive du trouble obsessionnel et compulsif et des troubles de la personnalité comorbides: thérapie de groupe]. Annales Medico-Psychologiques 2008;166(8):673-6. [DOI: 10.1016/j.amp.2008.07.008] [DOI] [Google Scholar]
Vinnars 2005 {published data only}
- *.Vinnars B, Barber JP, Norén K, Gallop R, Weinryb RM. Manualized supportive-expressive psychotherapy versus nonmanualized community-delivered psychodynamic therapy for patients with personality disorders: bridging efficacy and effectiveness. American Journal of Psychiatry 2005;162(10):1933-40. [DOI: 10.1176/appi.ajp.162.10.1933] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Vinnars B, Barber JP, Norén K, Thormählen B, Gallop R, Lindgren A, et al. Who can benefit from time-limited dynamic psychotherapy? A study of psychiatric outpatients with personality disorders. Clinical Psychology & Psychotherapy 2007;14(3):198-210. [DOI: 10.1002/cpp.530] [DOI] [Google Scholar]
- Vinnars B, Thormählen B, Gallop R, Norén K, Barber JP. Do personality problems improve during psychodynamic supportive-expressive psychotherapy? Secondary outcome results from a randomized controlled trial for psychiatric outpatients with personality disorders. Psychotherapy 2009;46(3):362-75. [DOI: 10.1037/a0017002] [NIHMS164112] [PMC2808137] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Weertman 2007 {published data only}
- Weertman A, Arntz A. Effectiveness of treatment of childhood memories in cognitive therapy for personality disorders: a controlled study contrasting methods focusing on the present and methods focusing on childhood memories. Behaviour Research and Therapy 2007;45(9):2133-43. [DOI: 10.1016/j.brat.2007.02.013] [PMID: ] [DOI] [PubMed] [Google Scholar]
Winston 1994 {published data only}
- Winston A, Laikin M, Pollack J, Samstag LW, McCullough L, Muran JC. Short-term psychotherapy of personality disorders. American Journal of Psychiatry 1994;151(2):190-4. [DOI: 10.1176/ajp.151.2.190] [PMID: ] [DOI] [PubMed] [Google Scholar]
Witkiewitz 2014 {published data only}
- Witkiewitz K, Warner K, Sully B, Barricks A, Stauffer C, Thompson BL, et al. Randomized trial comparing mindfulness-based relapse prevention with relapse prevention for women offenders at a residential addiction treatment center. Substance Use & Misuse 2014;49(5):536-46. [DOI: 10.3109/10826084.2013.856922] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wölwer 2001 {published data only}
- Wölwer W, Burtscheidt W, Redner C, Schwarz R, Gaebel W. Out-patient behaviour therapy in alcoholism: impact of personality disorders and cognitive impairments. Acta Psychiatrica Scandinavica 2001;103(1):30-7. [DOI: 10.1111/j.1600-0447.2001.00149.x ] [DOI] [PubMed] [Google Scholar]
Wupperman 2015 {published data only}
- Wupperman P, Cohen MG, Haller DL, Flom P, Litt LC, Rounsaville BJ. Mindfulness and modification therapy for behavioral dysregulation: a comparison trial focused on substance use and aggression. Journal of Clinical Psychology 2015;71(10):964-78. [DOI: 10.1002/jclp.22213] [PMID: ] [DOI] [PubMed] [Google Scholar]
Young 2013 {published data only}
- Young S, Hopkin G, Perkins D, Farr C, Doidge A, Gudjonsson G. A controlled trial of a cognitive skills program for personality-disordered offenders. Journal of Attention Disorders 2013;17(7):598-607. [DOI: 10.1177/1087054711430333] [PMID: ] [DOI] [PubMed] [Google Scholar]
Zorn 2007 {published data only}
- Zorn P, Roder V, Muller DR, Tschacher W, Thommen M. Schema focused emotive behavioural therapy ('SET'): a randomised controlled trial on patients with cluster B and C personality disorders [Schemazentrierte emotiv-behaviorale therapie (SET): eine randomisierte evaluationsstudie an patienten mit persönlichkeitsstörungen aus den clustern B und C]. Verhaltenstherapie 2007;17(4):233-41. [DOI: 10.1159/000110129] [DOI] [Google Scholar]
References to studies awaiting assessment
Berget 2008 {published data only}
- *.Berget B, Ekeberg Ø, Braastad BO. Animal-assisted therapy with farm animals for persons with psychiatric disorders: effects on self-efficacy, coping ability and quality of life, a randomized controlled trial. Clinical Practice & Epidemiology in Mental Health 2008;4:9. [DOI: 10.1186/1745-0179-4-9] [PMC2323374] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berget B, Ekeberg Ø, Pedersen I, Braastad BO. Animal-assisted therapy with farm animals for persons with psychiatric disorders: effects on anxiety and depression, a randomized controlled trial. Occupational Therapy in Mental Health 2011;27(1):50-64. [DOI: 10.1080/0164212X.2011.543641] [DOI] [Google Scholar]
- Cheung N. Animal-assisted therapy with farm animals, RCTs [personal communication]. Email to: B Berget 03 February 2017.
Black 2016 {published data only (unpublished sought but not used)}
- Black D. Predictors of response to STEPPS for BPD (2009) and Do people with BPD complicated by AsPD benefit from the STEPPS program? (2016) [personal communication]. Email to: N Cheung 16 February 2017.
- Black DW, Allen J, St John D, Pfohl B, McCormick B, Blum N. Predictors of response to systems training for emotional predictability and problem solving (STEPPS) for borderline personality disorder: an exploratory study. Acta Psychiatrica Scandinavica 2009;120(1):53-61. [DOI: 10.1111/j.1600-0447.2008.01340.x] [PMC3665337] [PMID: 19183126 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black DW, Blum N, Allen J. STEPPS treatment programme for borderline personality disorder: which scale items improve? An item-level analysis. Personality and Mental Health 2018;12(4):345-54. [DOI: 10.1002/pmh.1431] [PMID: ] [DOI] [PubMed] [Google Scholar]
- *.Black DW, Simsek-Duran F, Blum N, McCormick B, Allen J. Do people with borderline personality disorder complicated by antisocial personality disorder benefit from the STEPPS treatment program? Personality and Mental Health 2016;10(3):205-15. [DOI: 10.1002/pmh.1326] [PMC4911327] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blum N, St John D, Pfohl B, Stuart S, McCormick B, Allen J, et al. Systems training for emotional predictability and problem solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. American Journal of Psychiatry 2008;165(4):468-78. [DOI: 10.1176/appi.ajp.2007.07071079] [PMC3608469] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Buric 2019 {published data only}
- Buric I, Farias M, Kurtev S, Van Mulukom V, Mee C, Gould L, et al. The genomic, neural, and behavioral effects of intensive mindfulness meditation and yoga on prisoners with personality disorders: a randomized controlled pilot study. International Journal of Offender Therapy and Comparative Criminology (under review).
- *.Buric I, Farias M, Van Mulukom V, Jong J, Kurtev S, Mee C, et al. The neural, genetic and behavioural effects of intensive meditation and yoga on prisoners with personality disorders. Brain, Behavior, and Immunity 2019;76 Suppl:e17. [DOI: 10.1016/j.bbi.2018.11.224] [Abstract #30999] [DOI] [Google Scholar]
- Buric I. Cochrane review request [personal communication]. Email to: L McCarthy 17 December 2019.
- McCarthy L. Cochrane review request [personal communication]. Email to: I Buric 12 September 2019.
- McCarthy L. Cochrane review request [personal communication]. Email to: I Buric, M Farias 3 December 2019.
Clarke 2013 {published data only}
- Cheung N. Cognitive analytic therapy for personality disorder: a randomised control trial [personal communication]. Email to: S Clarke 19.01.2017.
- *.Clarke S, Thomas P, James K. Cognitive analytic therapy for personality disorder: randomised controlled trial. British Journal of Psychiatry 2013;202(2):129-34. [DOI: 10.1192/bjp.bp.112.108670] [PMID: ] [DOI] [PubMed] [Google Scholar]
Evans 1999 {published data only}
- Evans K, Tyrer P, Catalan J, Schmidt U, Davidson K, Dent J, et al. Manual-assisted cognitive-behaviour therapy (MACT): a randomized controlled trial of a brief intervention with bibliotherapy in the treatment of recurrent deliberate self-harm. Psychological Medicine 1999;29(1):19-25. [PMID: ] [DOI] [PubMed] [Google Scholar]
Jochems 2015 {published data only}
- Jochems E. Motivation and treatment engagement intervention trial [personal communication]. Email to: Cheung N 7 February 2017.
- Jochems EC, Mulder CL, Van Dam A, Duivenvoorden HJ, Scheffer SC, Van Der Spek W, et al. Motivation and Treatment engagement Intervention Trial (MotivaTe-IT): the effects of motivation feedback to clinicians on treatment engagement in patients with severe mental illness. BMC Psychiatry 2012;12:209. [DOI: 10.1186/1471-244X-12-209] [PMC3536707] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jochems EC, Van Dam A, Duivenvoorden HJ, Scheffer SC, Van Der Feltz-Cornelis CM, Mulder CL. Different perspectives of clinicians and patients with severe mental illness on motivation for treatment. Clinical Psychology & Psychotherapy 2016;23(5):438-51. [DOI: 10.1002/cpp.1971] [PMID: ] [DOI] [PubMed]
- *.Jochems EC, Van Der Feltz-Cornelis CM, Van Dam A, Duivenvoorden HJ, Mulder CL. The effects of motivation feedback in patients with severe mental illness: a cluster randomized controlled trial. Neuropsychiatric Disease and Treatment 2015;11:3049-64. [DOI: 10.2147/NDT.S95190] [PMC4686323] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Linehan 2006 {published data only}
- *.Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomised controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry 2006;63(7):757-66. [DOI: 10.1001/archpsyc.63.7.757] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Unknown review author. Cochrane review enquiry [personal communication]. Email to: M Linehan 2010.
References to ongoing studies
ISRCTN14994755 {published data only}
- Crawford MJ, Thana L, Parker J, Turner O, Xing KP, McMurran M, et al. Psychological support for personality (PSP) versus treatment as usual: study protocol for a feasibility randomized controlled trial of a low intensity intervention for people with personality disorder. Trials 2018;19(1):547. [DOI: 10.1186/s13063-018-2920-0] [PMC6180621] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.ISRCTN14994755. Low intensity psychological support for people with personality disorder: randomised controlled trial [Assessing a low intensity treatment for enduring personality-related problems]. www.isrctn.com/ISRCTN14994755 (first received 31 May 2017).
ISRCTN32309003 {published data only}
- ISRCTN32309003. Mentalization-based therapy (MBT) for individuals with antisocial personality disorder [Mentalization for offending adult males: a national randomised controlled trial (MOAM)]. www.isrctn.com/ISRCTN32309003 (first received 18 February 2015).
NCT02524171 {published data only}
- Blonigen DM, Cucciare MA, Timko C, Smith JS, Harnish A, Kemp L, et al. Study protocol: a hybrid effectiveness-implementation trial of moral reconation therapy in the US Veterans Health Administration. BMC Health Services Research 2018;18(1):164. [DOI: 10.1186/s12913-018-2967-3] [PMC5842602] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.NCT02524171. Justice-involved veterans and moral reconation therapy (MRT) [Improving treatment engagement and outcomes among justice-involved veterans]. clinicaltrials.gov/ct2/show/NCT02524171 (first received 5 August 2015).
NCT03883646 {published data only}
- Harenski C. NCT03883646, 18114, Mindfulness for alcohol abusing offenders [personal communication]. Email to: McCarthy L 13 December 2019.
- *.NCT03883646. Mindfulness for alcohol abusing offenders (MIT). clinicaltrials.gov/ct2/show/NCT03883646 (first received 18 March 2019).
NCT04033835 {published data only}
- NCT04033835. Mentalization based treatment - introductory (MBT-I) group for male prisoners with borderline and/or antisocial personality disorder [Mentalization based treatment - introductory group for male prisoners with borderline and/or antisocial personality disorder in Her Majesty's Prison Barlinnie]. clinicaltrials.gov/ct2/show/NCT04033835 (first received 10 July 2019).
Van Dijk 2019 {published data only}
- Van Dijk S, Veenstra M, Bouman R, Peekel J, Veenstra D, Van Dalen P, et al. Group schema-focused therapy enriched with psychomotor therapy versus treatment as usual for older adults with cluster B and/or C personality disorders: a randomized trial. BMC Psychiatry 2019;19(1):26. [DOI: 10.1186/s12888-018-2004-4] [PMC6334382 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Alegria 2013
- Alegria AA, Blanco C, Petry NM, Skodol AE, Liu SM, Grant B, et al. Sex differences in antisocial personality disorder: results from the National Epidemiological Survey on Alcohol and Related Conditions. Personality Disorders 2013;4(3):214–22. [DOI: 10.1037/a0031681] [PMC3767421] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313(7066):1200. [PMC2352469] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Aos 1999
- Aos S, Phipps P, Barnoski R, Leib R. The comparative costs and benefits of programs to reduce crime: a review of national research findings with implications for Washington State; May 1999. bit.ly/3ezYYVz (accessed prior to 18 August 2020).
Attkisson 1982
- Attkisson CC, Zwick R. The Client Satisfaction Questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning 1982;5(3):233-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Barkham 2001
- Barkham M, Margison F, Leach C, Lucock M, Mellor-Clark J, Evans C, et al. Service profiling and outcomes benchmarking using the CORE-OM: toward practice-based evidence in the psychological therapies. Clinical outcomes in routine evaluation-outcome measures. Journal of Consulting and Clinical Psychology 2001;69(2):184-96. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bateman 2001
- Bateman A, Fonagy P. Treatment of borderline personality disorder with psychoanalytically orientated partial hospitalisation: an 18 month follow-up. American Journal of Psychiatry 2001;158(1):36-42. [DOI: 10.1176/appi.ajp.158.1.36] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bateman 2004a
- Bateman AW, Tyrer P. Psychological treatment for personality disorders. Advances in Psychiatric Treatment 2004;10(5):378-88. [DOI: 10.1192/apt.10.5.378] [DOI] [Google Scholar]
Bateman 2004b
- Bateman AW, Fonagy P. Mentalization-based treatment of BPD. Journal of Personality Disorders 2004;18(1):36-51. [DOI: 10.1521/pedi.18.1.36.32772] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beck 1988
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology 1988;56(6):893-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Black 1996
- Black DW, Baumgard CH, Bell SE, Kao C. Death rates in 71 men with antisocial personality disorder. A comparison with general population mortality. Psychosomatics 1996;37(2):131-6. [DOI: 10.1016/S0033-3182(96)71579-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
Black 2010
- Black DW, Gunter T, Loveless P, Allen J, Sieleni B. Antisocial personality disorder in incarcerated offenders: psychiatric comorbidity and quality of life. Annals of Clinical Psychiatry 2010;22(2):113-20. [PMID: ] [PubMed] [Google Scholar]
Black 2015
- Black DW. The natural history of antisocial personality disorder. Canadian Journal of Psychiatry 2015;60(7):309-14. [DOI: 10.1177/070674371506000703] [PMC4500180] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blum 2008
- Blum N, St John D, Pfohl B, Stuart S, McCormick B, Allen J, et al. Systems training for emotional predictability and problem solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. American Journal of Psychiatry 2008;165(4):468-78. [DOI: 10.1176/appi.ajp.2007.07071079] [PMC3608469] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
British Psychoanalytical Council 2018
- British Psychoanalytic Council. Psychoanalytic psychotherapy: what’s the evidence? www.bpc.org.uk/sites/psychoanalytic-council.org/files/FINAL%20Overview_Evidence_Base_Briefing%20June2015.pdf (accessed 1 February 2018).
Brooner 1998
- Brooner RK, Kidorf M, King VL, Stoller K. Preliminary evidence of good treatment response in antisocial drug abusers. Drug and Alcohol Dependence 1998;49(3):249-60. [PMID: ] [DOI] [PubMed] [Google Scholar]
Buss 1992
- Buss AH, Perry M. The Aggression Questionnaire. Journal of Personality and Social Psychology 1992;63(3):452-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Campling 2001
- Campling P. Therapeutic communities. Advances in Psychiatric Treatment 2001;7(5):365-72. [DOI: 10.1192/apt.7.5.365] [DOI] [Google Scholar]
Carlson 1993
- Carlson EB, Putnam FW. An update on the Dissociative Experiences Scale. Dissociation: Progress in the Dissociative Disorders 1993;6(1):16-27. [psycnet.apa.org/record/1994-27927-001] [Google Scholar]
Carroll 2004
- Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, Shi J, et al. Efficacy of disulfiram and cognitive behavior therapy in cocaine-dependent outpatients: a randomized placebo-controlled trial. Archives of General Psychiatry 2004;61(3):264-72. [DOI: 10.1001/archpsyc.61.3.264] [NIHMS466084] [PMC3675448] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carroll 1998
- Carroll KM, Nich C, Ball SA, McCance E, Rounsavile BJ. Treatment of cocaine and alcohol dependence with psychotherapy and disulfiram. Addiction 1998;93(5):713-27. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chambless 1998
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology 1998;66(1):7-18. [DOI: 10.1037/0022-006X.66.1.7] [PMID: ] [DOI] [PubMed] [Google Scholar]
Coid 2006
- Coid J, Yang M, Tyrer P, Roberts A, Ullrich S. Prevalence and correlates of personality disorder in Great Britain. British Journal of Psychiatry 2006;188:423-31. [DOI: 10.1192/bjp.188.5.423] [PMID: ] [DOI] [PubMed] [Google Scholar]
Coid 2015
- Coid JW, Yang M, Ullrich S, Hickey N, Kahtan N, Freestone M. Psychiatric diagnosis and differential risks of offending following discharge. International Journal of Law and Psychiatry 2015;38:68-74. [DOI: 10.1016/j.ijlp.2015.01.009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Compton 2005
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry 2005;66(6):677–85. [DOI: 10.4088/JCP.v66n0602] [PMID: ] [DOI] [PubMed] [Google Scholar]
Crawford 2007
- Crawford M, Rutter D, Price K, Weaver T, Josson M, Tyrer P, et al. Learning the lessons: a multi-method evaluation of dedicated community-based services for people with personality disorder; November 2007. www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1404-083_V01.pdf (accessed prior to 18 August 2020).
Da Costa 2013
- Da Costa BR, Nüesch E, Rutjes AW, Johnston BC, Reichenbach S, Trelle S, et al. Combining follow-up and change data is valid in meta-analyses of continuous outcomes: meta-epidemiological study. Journal of Clinical Epidemiology 2013;66(8):847-55. [DOI: 10.1016/j.jclinepi.2013.03.009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Davies 2007
- Davies S, Clarke M, Hollin C, Duggan C. Long-term outcomes after discharge from medium secure care: a cause for concern. British Journal of Psychiatry 2007;191:70-4. [DOI: 10.1192/bjp.bp.106.029215] [PMID: ] [DOI] [PubMed] [Google Scholar]
Denman 2001
- Denman C. Cognitive-analytic therapy. Advances in Psychiatric Treatment 2001;7(4):243-52. [DOI: 10.1192/apt.7.4.243] [DOI] [Google Scholar]
Derogatis 1973
- Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale - preliminary report. Psychopharmacology Bulletin 1973;9(1):13-28. [PMID: ] [PubMed] [Google Scholar]
DeRubeis 2005
- DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Archives of General Psychiatry 2005;62(4):409-16. [DOI: 10.1001/archpsyc.62.4.409] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dolan 1993
- Dolan B, Coid J. Psychopathic and Antisocial Personality Disorders: Treatment and Research Issues. London (UK): Gaskell, 1993. [Google Scholar]
Dolan 2009
- Dolan M, Völlm B. Antisocial personality disorder and psychopathy in women: a literature review on the reliability and validity of assessment instruments. International Journal of Law and Psychiatry 2009;32(1):2-9. [DOI: 10.1016/j.ijlp.2008.11.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Donner 2001
- Donner A, Piaggio G, Villar J. Statistical methods for the meta-analysis of cluster randomization trials. Statistical Methods in Medical Research 2001;10(5):325-38. [DOI: 10.1177/096228020101000502] [PMID: ] [DOI] [PubMed] [Google Scholar]
DSM‐5
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM–5). 5th edition. Arlington (VA): American Psychiatric Association, 2013. [Google Scholar]
DSM‐IV
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). 4th edition. Washington (DC): American Psychiatric Association, 1994. [Google Scholar]
DSM‐IV‐TR
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). 4th edition. Arlington (VA): American Psychiatric Association, 2000. [Google Scholar]
Duggan 2007
- Duggan C, Huband N, Smailagic N, Ferriter M, Adams C. The use of psychological treatments for people with personality disorder: a systematic review of randomized controlled trials. Personality and Mental Health 2007;1(2):95-125. [DOI: 10.1002/pmh.22] [DOI] [Google Scholar]
Duke 1994
- Duke PJ, Pantelis C, Barnes TR. South Westminster Schizophrenia Survey. Alcohol use and its relationship to symptoms, tardive dyskinesia and illness onset. British Journal of Psychiatry 1994;164(5):630-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey-Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI: 10.1136/bmj.315.7109.629] [PMC2127453] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Essock 2006
- Essock SM, Mueser KT, Drake RE, Covell NH, McHuga GJ, Frisman LK, et al. Comparison of ACT and standard case management for delivering integrated treatment for co-occurring disorders. Psychiatric Services 2006;57(2):185-96. [DOI: 10.1176/appi.ps.57.2.185] [PMID: ] [DOI] [PubMed] [Google Scholar]
EuroQoL Group 1990
- EuroQoL Group. EuroQoL: a new facility for measurement of health-related quality of life. Health Policy 1990;16(3):199-208. [PMID: ] [DOI] [PubMed] [Google Scholar]
Fazel 2002
- Fazel S, Danesh J. Serious mental disorder in 23000 prisoners: a systematic review of 62 surveys. Lancet 2002;359(9306):545-50. [DOI: 10.1016/S0140-6736(02)07740-1] [PMID: 11867106 ] [DOI] [PubMed] [Google Scholar]
Follman 1992
- Follmann D, Elliot P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. Journal of Clinical Epidemiology 1992;45(7):769-73. [DOI: 10.1016/0895-4356(92)90054-Q] [PMID: ] [DOI] [PubMed] [Google Scholar]
Galbraith 2014
- Galbraith T, Heimberg RG, Wang S, Schneier FR, Blanco C. Comorbidity of social anxiety disorder and antisocial personality disorder in the National Epidemiological Survey on Alcohol and Related Conditions (NESARC). Journal of Anxiety Disorders 2014;28(1):57-66. [DOI: 10.1016/j.janxdis.2013.11.009] [NIHMS549496] [PMC3951602] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gamble 2005
- Gamble C, Hollis S. Uncertainty method on best-worst case analysis in a binary meta-analysis. Journal of Clinical Epidemiology 2005;58(6):579-88. [DOI: 10.1016/j.jclinepi.2004.09.013] [PMID: ] [DOI] [PubMed] [Google Scholar]
Goodwin 2003
- Goodwin RD, Hamilton SP. Lifetime comorbidity of antisocial personality disorder and anxiety disorders among adults in the community. Psychiatry Research 2003;117(2):159-66. [DOI: 10.1016/S0165-1781(02)00320-7] [DOI] [PubMed] [Google Scholar]
GRADEpro [Computer program]
- GRADEpro GDT. Version accessed 3 January 2017. Hamilton (ON): McMaster University (developed by Evidence Prime), 2017. Available at gradepro.org.
Grilo 1998
- Grilo CM, McGlashan TH, Oldham JM. Course and stability of personality disorders. Journal of Practical Psychiatry and Behavioral Health 1998;4(2):61-75. [DOI: 10.1097/00131746-199803000-00001] [DOI] [Google Scholar]
Guy 2018
- Guy N, Newton-Howes G, Ford H, Williman J, Foulds J. The prevalence of comorbid alcohol use disorder in the presence of personality disorder: systematic review and explanatory modelling. Personality and Mental Health 2018;12(3):216-28. [DOI: 10.1002/pmh.1415] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence - study limitations (risk of bias). Journal of Clinical Epidemiology 2011;64(4):407-15. [DOI: 10.1016/j.jclinepi.2010.07.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Henwood 2015
- Henwood KS, Chou S, Browne KD. A systematic review and meta-analysis on the effectiveness of CBT informed anger management. Aggression and Violent Behavior 2015;25(Part B):280-92. [DOI: 10.1016/j.avb.2015.09.011] [psycnet.apa.org/record/2015-47235-001] [DOI] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JPT, Altman DG, Sterne JAC, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2019
- Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). Cochrane 2019. www.training.cochrane.org/handbook.. [WEBSITE: www.training.cochrane.org/handbook.]
Huizinga 1986
- Huizinga D, Elliott D. Reassessing the reliability and validity of self-report delinquency measures. Journal of Quantitative Criminology 1986;2(4):293–327. [DOI: 10.1007/BF01064258] [DOI] [Google Scholar]
ICD‐10
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva (CH): World Health Organization, 1992. [Google Scholar]
ICD‐11
- World Health Organization. ICD-11: International Classification of Diseases for Mortality and Morbidity Statistics. www.who.int/classifications/icd/en (accessed 3 July 2020);(11th revision).
Jakobsen 2014
- Jakobsen JC, Wetterslev J, Winkel P, Lange T, Gluud C. Thresholds for statistical and clinical significance in systematic reviews with meta-analytic methods. BMC Medical Research Methodology 2014;14:120. [DOI: 10.1186/1471-2288-14-120] [PMC4251848] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnstone 2018
- Johnstone L, Boyle M, Cromby J, Dillon J, Harper D, Kinderman P, et al. The Power Threat Meaning Framework: Towards the Identification of Patterns in Emotional Distress, Unusual Experiences and Troubled or Troubling Behaviour, as an Alternative to Functional Psychiatric Diagnosis. Leicester (UK): British Psychological Society, 2018. [Google Scholar]
Jones 1969
- Jones RG. A Factored Measure of Ellis' Irrational Belief System with Personality and Maladjustment Correlates [PhD thesis]. Lubbock (TX): Texas Technological College, 1969. [Google Scholar]
Kershaw 1999
- Kershaw C. Reconviction of Offenders Sentenced or Discharged from Prison in 1994, England and Wales: Home Office Statistical Bulletin 5/99. London (UK): Home Office, 1999. [Google Scholar]
Khalifa 2010
- Khalifa N, Duggan C, Stoffers J, Huband N, Völlm BA, Ferriter M, et al. Pharmacological interventions for antisocial personality disorder. Cochrane Database of Systematic Reviews 2010, Issue 8. Art. No: CD007667. [DOI: 10.1002/14651858.CD007667.pub2] [PMC4160654] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krasnova 2019
- Krasnova A, Eaton WW, Samuels JF. Antisocial personality and risks of cause-specific mortality: results from the Epidemiologic Catchment Area study with 27 years of follow-up. Social Psychiatry and Psychiatric Epidemiology 2019;54(5):617-25. [DOI: 10.1007/s00127-018-1628-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lees 1999
- Lees J, Manning N, Rawlings B. Therapeutic community effectiveness: a systematic international review of therapeutic community treatment for people with personality disorders and mentally disordered Offenders. www.york.ac.uk/media/crd/crdreport17.pdf (accessed prior to 18 August 2020);(CRD report 17).
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Chapter 4: Searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Leichsenring 2003
- Leichsenring F, Leibing E. The effectiveness of psychodynamic therapy and cognitive behavior therapy in the treatment of personality disorders: a meta-analysis. American Journal of Psychiatry 2003;160(7):1223-32. [DOI: 10.1176/appi.ajp.160.7.1223] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lieb 2016
- Lieb K, Von der Osten-Sacken J, Stoffers-Winterling J, Reiss N, Barth J. Conflicts of interest and spin in reviews of psychological therapies: a systematic review. BMJ Open 2016;6:e010606. [DOI: 10.1136/bmjopen-2015-010606] [DOI] [PMC free article] [PubMed] [Google Scholar]
Linehan 1993
- Linehan MM. Skills Training Manual for Treating Borderline Personality Disorder. 1st edition. New York (NY): Guilford Press, 1993. [Google Scholar]
Livesley 2007
- Livesley WJ. A framework for integrating dimensional and categorical classifications of personality disorder. Journal of Personality Disorders 2007;21(2):199-224. [DOI: 10.1521/pedi.2007.21.2.199] [PMID: ] [DOI] [PubMed] [Google Scholar]
Malone 1994
- Malone RP, Luebbert RP, Pena-Ariet M, Biesecker K, Delaney MA. The Overt Aggression Scale in a study of lithium in aggressive conduct disorder. Psychopharmacology Bulletin 1994;30(2):215-8. [PMID: ] [PubMed] [Google Scholar]
Martens 2000
- Martens WHJ. Antisocial and psychopathic personality disorders: causes, course, and remission - a review article. International Journal of Offender Therapy and Comparative Criminology 2000;44(4):406-30. [DOI: 10.1177/0306624X00444002] [psycnet.apa.org/record/2001-00934-001] [DOI] [Google Scholar]
McGilloway 2010
- McGilloway A, Hall RE, Lee T, Bhui KS. A systematic review of personality disorder, race and ethnicity: prevalence, aetiology and treatment. BMC Psychiatry 2010;10:33. [DOI: 10.1186/1471-244X-10-33] [PMC2882360] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
McKay 1997
- McKay JR, Alterman AI, Cacciola JS, Rutherford MJ, O'Brian CP, Koppenhaver J. Group counselling versus individualized relapse prevention aftercare following intensive outpatient treatment for cocaine dependence: initial results. Journal of Consulting and Clinical Psychology 1997;65(5):778-88. [PMID: ] [DOI] [PubMed] [Google Scholar]
Moher 1998
- Moher D. CONSORT: an evolving tool to help improve the quality of reports of randomized controlled trials. Consolidated Standards of Reporting Trials. JAMA 1998;279(18):1489-91. [10.1001/jama.279.18.1489] [PMID: ] [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [PMC2707599] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2010
- Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c869. [DOI: 10.1136/bmj.c869] [PMC2844943] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moran 1999
- Moran P. The epidemiology of antisocial personality disorder. Social Psychiatry and Psychiatric Epidemiology 1999;34(5):231-42. [PMID: ] [DOI] [PubMed] [Google Scholar]
Muran 2018
- Muran JC, Safran JD, Eubanks CF, Gorman BS. The effect of alliance-focused training on a cognitive-behavioral therapy for personality disorders. Journal of Consulting & Clinical Psychology 2018;86(4):384-97. [DOI: 10.1037/ccp0000284] [PMC5901896 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Myers 1998
- Myers MG, Stewart DG, Brown SA. Progression from conduct disorder to antisocial personality disorder following treatment for adolescent substance abuse. American Journal of Psychiatry 1998;155(4):479-85. [DOI: 10.1176/ajp.155.4.479] [PMID: ] [DOI] [PubMed] [Google Scholar]
Newman 1939
- Newman D. The distribution of range in samples from a normal population, expressed in terms of an independent estimate of standard deviation. Biometrika 1939;31:20-30. [DOI: 10.1093/biomet/31.1-2.20] [psycnet.apa.org/record/1940-00666-001] [DOI] [Google Scholar]
Newton‐Howes 2006
- Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. British Journal of Psychiatry 2006;188:13-20. [DOI: 10.1192/bjp.188.1.13] [PMID: ] [DOI] [PubMed] [Google Scholar]
NICE 2007
- National Institute for Health and Clinical Excellence. Drug misuse in over 16s: opioid detoxification. www.nice.org.uk/CG52 (accessed 29 October 2009). [PubMed]
NICE 2010
- National Institute for Health and Care Excellence. Antisocial personality disorder: prevention and management. www.nice.org.uk/guidance/cg77/evidence/full-guideline-242104429 (accessed 29 April 2019). [PubMed]
NICE 2015
- National Institute for Health and Care Excellence. Personality disorders: borderline and antisocial. www.nice.org.uk/guidance/qs88 (accessed prior to 18 August 2020). [ISBN: 978-1-4731-1247-6]
Ogloff 2006
- Ogloff JRP. Psychopathy/antisocial personality disorder conundrum. Australian & New Zealand Journal of Psychiatry 2006;40(6-7):519-28. [DOI: 10.1080/j.1440-1614.2006.01834.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Oltmanns 2019
- Oltmanns JR, Widiger TA. Evaluating the assessment of the ICD-11 personality disorder diagnostic system. Psychological Assessment 2019;31(5):674-84. [DOI: 10.1037/pas0000693] [PMC6488396 [Available on 2020-05-01] ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
ONS 2004
- Office for National Statistics. Social Trends 34. London (UK): Office of National Statistics, 2004. [Google Scholar]
Overall 1962
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports 1962;10:799-812. [DOI: 10.2466/pr0.1962.10.3.799] [psycnet.apa.org/record/1963-05043-001] [DOI] [Google Scholar]
Palmer 2000
- Palmer E, Hollin C. The interrelations of socio-moral reasoning, perceptions of own parenting and attributions of intent with self-reported delinquency. Legal and Criminal Psychology 2000;15:201–18. [DOI: 10.1348/135532500168092] [DOI] [Google Scholar]
Paris 2003
- Paris J. Personality Disorders Over Time: Precursors, Course, and Outcome. Arlington (VA): American Psychiatric Association, 2003. [DOI] [PubMed] [Google Scholar]
Patton 1995
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. Journal of Clinical Psychology 1995;51(6):768-74. [PMID: ] [DOI] [PubMed] [Google Scholar]
Perdikouri 2007
- Perdikouri M, Rathbone G, Huband N, Duggan C. A comparison of adults with antisocial personality traits with and without childhood conduct disorder. Annals of Clinical Psychiatry 2007;19(1):17-23. [DOI: 10.1080/10401230601163501] [PMID: ] [DOI] [PubMed] [Google Scholar]
Petry 2011
- Petry NM. Contingency management: what it is and why psychiatrists should want to use it. Psychiatrist 2011;35(5):161-3. [DOI: 10.1192/pb.bp.110.031831] [PMC3083448] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Piper 1993
- Piper WE, Rosie JS, Azim HF, Joyce AS. A randomised trial of psychiatric day treatment for patients with affective and personality disorders. Hospital & Community Psychiatry 1993;44(8):757-63. [PMID: ] [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Robins 1998
- Robins LN. The intimate connection between antisocial personality and substance abuse. Social Psychiatry and Psychiatric Epidemiology 1998;33(8):393-9. [DOI: 10.1007/s001270050071] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ryle 2002
- Ryle A, Kerr IB. Introducing Cognitive Analytic Therapy: Principles and Practice. Chichester (UK): John Wiley & Sons Ltd, 2002. [Google Scholar]
Sampson 2013
- Sampson CJ, James M, Huband N, Geelan S, McMurran M. Cost implications of treatment non-completion in a forensic personality disorder service. Criminal Behaviour and Mental Health 2013;23(5):321-35. [DOI: 10.1002/cbm.1866] [PMC3920639] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
Scott 2001
- Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ 2001;323(7306):191-4. [DOI: 10.1136/bmj.323.7306.191 ] [PMC35269] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Singleton 1998
- Singleton N, Melzer H, Gatward R. Psychiatric Morbidity Among Prisoners in England and Wales. London (UK): HM Stationery Office, 1998. [Google Scholar]
Skodol 2005
- Skodol AE, Oldham JM, Bender DS, Dyck IR, Stout RL, Morey LC, et al. Dimensional representations of DSM-IV personality disorders: relationships to functional impairment. American Journal of Psychiatry 2005;162(10):1919-25. [DOI: 10.1176/appi.ajp.162.10.1919] [PMID: ] [DOI] [PubMed] [Google Scholar]
Skodol 2018
- Skodol AE. Can personality disorders be redefined in personality trait terms? American Journal of Psychiatry 2018;175(7):590-2. [DOI] [PubMed] [Google Scholar]
Spielberger 1999
- Spielberger CD. STAXI-2: State-Trait Anger Expression Inventory-2: Professional Manual. Odessa (FL): Psychological Assessment Resources, 1999. [Google Scholar]
Stovold 2014
- Stovold E, Beecher D, Foxlee R, Noel-Storr A. Study flow diagrams in Cochrane systematic review updates: an adapted PRISMA flow diagram. Systematic Reviews 2014;3:54. [DOI: 10.1186/2046-4053-3-54] [PMC4046496] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Strathdee 2006
- Strathdee SA, Ricketts EP, Huettner S, Cornelius L, Bishai D, Havens JR, et al. Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: results from a community-based behavioral intervention trial. Drug and Alcohol Dependence 2006;83(3):225-32. [DOI: 10.1016/j.drugalcdep.2005.11.015] [NIHMS36559] [PMC2196224] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tait 2002
- Tait L, Birchwood M, Trower P. A new scale (SES) to measure engagement with community mental health services. Journal of Mental Health 2002;11(2):191-8. [DOI: 10.1080/09638230020023570-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Trull 2010
- Trull TJ, Jahng S, Tomko RL, Wood PK, Sher KJ. Revised NESARC personality disorder diagnoses: gender, prevalence, and comorbidity with substance dependence disorders. Journal of Personality Disorders 2010;24(4):412-26. [DOI: 10.1521/pedi.2010.24.4.412] [PMC3771514] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tyrer 2003
- Tyrer P, Jones V, Thompson S, Catalan J, Schmidt U, Davidson K, et al. Service variation in baseline variables and prediction of risk in a randomised controlled trial of psychological treatment in repeated parasuicide: the POPMACT Study. International Journal of Social Psychiatry 2003;49(1):58-69. [DOI: 10.1177/0020764003049001148] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tyrer 2005a
- Tyrer P, Bajaj P. Nidotherapy: making the environment do the therapeutic work. Advances in Psychiatric Treatment 2005;11(3):232-8. [DOI: 10.1192/apt.11.3.232] [DOI] [Google Scholar]
Tyrer 2005b
- Tyrer P, Nur U, Crawford M, Karlsen S, McLean C, Rao B, et al. The Social Functioning Questionnaire: a rapid and robust measure of perceived functioning. International Journal of Social Psychiatry 2005;51(3):265-75. [PMID: ] [PubMed] [Google Scholar]
Tyrer 2007
- Tyrer P, Kramo K, Miloŝeka K, Seivewright H. The place for nidotherapy in psychiatric practice. Psychiatric Bulletin 2007;31(1):1-3. [DOI: 10.1192/pb.31.1.1] [DOI] [Google Scholar]
Tyrer 2015
- Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet 2015;383(9969):717-26. [DOI: 10.1016/S0140-6736(14)61995-4] [DOI] [PubMed] [Google Scholar]
Volkert 2018
- Volkert J, Gablonski TC, Rabung S. Prevalence of personality disorders in the general adult population in Western countries: systematic review and meta-analysis. British Journal of Psychiatry 2018;213(6):709-15. [DOI: 10.1192/bjp.2018.202] [PMID: ] [DOI] [PubMed] [Google Scholar]
Weissman 1976
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry 1976;33(9):1111-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Weissman 1993
- Weissman MM. The epidemiology of personality disorders: a 1990 update. Journal of Personality Disorders 1993;Suppl 1:44-62. [psycnet.apa.org/record/1993-33722-001] [Google Scholar]
Young 2003
- Young JE, Klosko JS, Weishaar ME. Schema Therapy: A Practitioner’s Guide. New York (NY): Guildford Press, 2003. [Google Scholar]
Zigmond 1983
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica 1983;67(6):361-70. [DOI: 10.1111/j.1600-0447.1983.tb09716.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Gibbon 2009
- Gibbon S, Duggan C, Stoffers JM, Huband N, Völlm BA, Ferriter M, et al. Psychological interventions for antisocial personality disorder. Cochrane Database of Systematic Reviews 2009, Issue 1. Art. No: CD007668. [DOI: 10.1002/14651858.CD007668] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gibbon 2010
- Gibbon S, Duggan C, Stoffers J, Huband N, Völlm BA, Ferriter M, et al. Psychological interventions for antisocial personality disorder. Cochrane Database of Systematic Reviews 2010, Issue 6. Art. No: CD007668. [DOI: 10.1002/14651858.CD007668.pub2] [PMC4167848 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]


