Abstract
Background
Skeletal muscle cramps are common and often occur in association with pregnancy, advanced age, exercise or motor neuron disorders (such as amyotrophic lateral sclerosis). Typically, such cramps have no obvious underlying pathology, and so are termed idiopathic. Magnesium supplements are marketed for the prophylaxis of cramps but the efficacy of magnesium for this purpose remains unclear.
This is an update of a Cochrane Review first published in 2012, and performed to identify and incorporate more recent studies.
Objectives
To assess the effects of magnesium supplementation compared to no treatment, placebo control or other cramp therapies in people with skeletal muscle cramps.
Search methods
On 9 September 2019, we searched the Cochrane Neuromuscular Specialised Register, CENTRAL, MEDLINE, Embase, LILACS, CINAHL Plus, AMED, and SPORTDiscus. We also searched WHO‐ICTRP and ClinicalTrials.gov for registered trials that might be ongoing or unpublished, and ISI Web of Science for studies citing the studies included in this review.
Selection criteria
Randomized controlled trials (RCTs) of magnesium supplementation (in any form) to prevent skeletal muscle cramps in any patient group (i.e. all clinical presentations of cramp). We considered comparisons of magnesium with no treatment, placebo control, or other therapy.
Data collection and analysis
Two review authors independently selected trials for inclusion and extracted data. Two review authors assessed risk of bias. We attempted to contact all study authors when questions arose and obtained participant‐level data for four of the included trials, one of which was unpublished. We collected all data on adverse effects from the included RCTs.
Main results
We identified 11 trials (nine parallel‐group, two cross‐over) enrolling a total of 735 individuals, amongst whom 118 cross‐over participants additionally served as their own controls. Five trials enrolled women with pregnancy‐associated leg cramps (408 participants) and five trials enrolled people with idiopathic cramps (271 participants, with 118 additionally crossed over to control). Another study enrolled 29 people with liver cirrhosis, only some of whom suffered muscle cramps. All trials provided magnesium as an oral supplement, except for one trial which provided magnesium as a series of slow intravenous infusions. Nine trials compared magnesium to placebo, one trial compared magnesium to no treatment, calcium carbonate or vitamin B, and another trial compared magnesium to vitamin E or calcium. We judged the single trial in people with liver cirrhosis and all five trials in participants with pregnancy‐associated leg cramps to be at high risk of bias. In contrast, we rated the risk of bias high in only one of five trials in participants with idiopathic rest cramps.
For idiopathic cramps, largely in older adults (mean age 61.6 to 69.3 years) presumed to have nocturnal leg cramps (the commonest presentation), differences in measures of cramp frequency when comparing magnesium to placebo were small, not statistically significant, and showed minimal heterogeneity (I² = 0% to 12%). This includes the primary endpoint, percentage change from baseline in the number of cramps per week at four weeks (mean difference (MD) −9.59%, 95% confidence interval (CI) −23.14% to 3.97%; 3 studies, 177 participants; moderate‐certainty evidence); and the difference in the number of cramps per week at four weeks (MD −0.18 cramps/week, 95% CI −0.84 to 0.49; 5 studies, 307 participants; moderate‐certainty evidence). The percentage of individuals experiencing a 25% or better reduction in cramp rate from baseline was also no different (RR 1.04, 95% CI 0.84 to 1.29; 3 studies, 177 participants; high‐certainty evidence). Similarly, no statistically significant difference was found at four weeks in measures of cramp intensity or cramp duration. This includes the number of participants rating their cramps as moderate or severe at four weeks (RR 1.33, 95% CI 0.81 to 2.21; 2 studies, 91 participants; moderate‐certainty evidence); and the percentage of participants with the majority of cramp durations of one minute or more at four weeks (RR 1.83, 95% CI 0.74 to 4.53, 1 study, 46 participants; low‐certainty evidence).
We were unable to perform meta‐analysis for trials of pregnancy‐associated leg cramps. The single study comparing magnesium to no treatment failed to find statistically significant benefit on a three‐point ordinal scale of overall treatment efficacy. Of the three trials comparing magnesium to placebo, one found no benefit on frequency or intensity measures, another found benefit for both, and a third reported inconsistent results for frequency that could not be reconciled. The single study in people with liver cirrhosis was small and had limited reporting of cramps, but found no difference in terms of cramp frequency or cramp intensity.
Our analysis of adverse events pooled all studies, regardless of the setting in which cramps occurred. Major adverse events (occurring in 2 out of 72 magnesium recipients and 3 out of 68 placebo recipients), and withdrawals due to adverse events, were not significantly different from placebo. However, in the four studies for which it could be determined, more participants experienced minor adverse events in the magnesium group than in the placebo group (RR 1.51, 95% CI 0.98 to 2.33; 4 studies, 254 participants; low‐certainty evidence). Overall, oral magnesium was associated with mostly gastrointestinal adverse events (e.g. diarrhoea), experienced by 11% (10% in control) to 37% (14% in control) of participants.
Authors' conclusions
It is unlikely that magnesium supplementation provides clinically meaningful cramp prophylaxis to older adults experiencing skeletal muscle cramps. In contrast, for those experiencing pregnancy‐associated rest cramps the literature is conflicting and further research in this population is needed. We found no RCTs evaluating magnesium for exercise‐associated muscle cramps or disease‐state‐associated muscle cramps (for example amyotrophic lateral sclerosis/motor neuron disease) other than a single small (inconclusive) study in people with liver cirrhosis, only some of whom suffered cramps.
Plain language summary
Magnesium for muscle cramps
Review question
We reviewed the evidence about the effect of magnesium supplements on muscle cramps, and included the widest possible range of studies. This meant including studies on anyone suffering muscle cramps, regardless of why they suffered them. It also meant including studies where magnesium was given in any of the ways available. This includes being swallowed as a pill or liquid, being injected slowly over a number of hours directly into the blood ('intravenous infusion'), and being injected into muscle ('intramuscular injection'). We included studies comparing magnesium to placebo, comparing magnesium to no treatment, and comparing magnesium to other existing cramp treatments. We found a total of 11 studies. To assess benefit, we examined the effect of magnesium on cramp frequency, cramp pain, and cramp duration, and we examined the number of participants whose cramp rate reduced by 25% or more. To assess for potential harm, we examined how often major and minor adverse health events occurred.
Background
Muscle cramps are common and occur in a wide range of settings. Older adults and pregnant women commonly complain of leg cramps while they are resting, athletes can cramp when they are pushing the limits of their endurance, and some people develop muscle cramps as a symptom of other medical conditions. One potential treatment that is already being marketed to prevent muscle cramps is magnesium supplementation. Magnesium is a common mineral in our diets and extra oral supplements of this mineral are available either over the Internet or in health food stores and pharmacies (usually in the form of tablets or powders to be dissolved in water). We wanted to combine studies to get the best estimate of magnesium's effect on cramping. We also wanted to examine the effect of magnesium in different categories of cramp sufferers, in case it might work in one setting, and not another.
Study characteristics
We searched for all high‐quality published studies evaluating the effectiveness of magnesium to prevent muscle cramps and found five studies in older adults, five studies in pregnant women, and one study in people with liver cirrhosis. The studies in older adults included 271 participants (61.6 to 69.3 years of age) and the studies in pregnant women included 408 participants. The single study in people with liver cirrhosis enrolled only 29 people, not all of whom experienced cramping. There were no studies of people who cramp while exercising. Magnesium was compared to placebo in nine of 11 studies, and compared to calcium, vitamin E, vitamins B₁ and B₆, and no treatment, in two studies of pregnant women. The included studies ranged from 14 to 56 days of treatment. Magnesium was given orally in 10 of 11 studies, and by four‐hour intravenous infusion on five consecutive days in one study. Funding for included studies came from a manufacturer of magnesium tablets in two studies, independent sources in three studies, and was not reported in six studies.
Key results and certainty of the evidence
The combined results of five seemingly reliable studies suggest, with moderate‐certainty, that magnesium is unlikely to reduce the frequency or severity of muscle cramps in older adults. In contrast, the five studies in pregnant women had important limitations to their reliability (both in study design and reporting of results), did not consistently show benefit, and could not be combined. As a result we are very uncertain as to whether pregnant women experiencing muscle cramps would benefit from magnesium. The single study in people with liver cirrhosis reported no difference in cramp frequency or intensity but was too small for conclusions to be drawn.
More research on magnesium in pregnant women is needed. The same is true for those who suffer cramps associated with medical conditions, or while exercising. However older adult cramp sufferers appear unlikely to benefit from this therapy. Major side effects were infrequent and participants withdrew from the study at similar rates when given magnesium or placebo. However minor side effects, mostly diarrhoea (as would be expected from magnesium salts) and nausea, were common and affected roughly 11% (10% in control) to 37% (14% in control) of participants.
The review is up to date to September 2019.
Summary of findings
Background
Description of the condition
Skeletal muscle cramps are sudden, involuntary, painful, and palpable muscle contractions lasting seconds to minutes. Skeletal muscle cramps can be disease‐associated but are more commonly idiopathic, that is they occur in the absence of obvious pathology. An understanding of the mechanism behind muscle cramps is lacking but a variety of evidence points either to the lower motor neuron or its distal axonal extensions as the site of origin (Miller 2005). In support of this, neuromuscular diseases associated with cramps are those that involve the lower motor neuron (e.g. amyotrophic lateral sclerosis, which is also known as motor neuron disease (ALS/MND), recovered poliomyelitis, nerve root compression, and polyneuropathies), while diseases of the muscle or central nervous system are not usually associated with cramps. Other conditions associated with cramps include some metabolic diseases (for example liver failure), medications (for example diuretics and inhaled beta‐agonists), and haemodialysis (especially if large volumes of fluid are being removed) (Garrison 2012a; McGee 1990). Cramping is commonly seen in the absence of serious disease, however, and is more frequent in individuals who are either elderly, pregnant, continuing to contract a muscle already at its shortest length, or exercising vigorously.
Exercise‐associated muscle cramps occur either during or immediately following intense exercise, usually in the exercising muscle groups (Schwellnus 2008). In contrast, cramps associated with pregnancy or advanced age occur in the legs or feet during periods of prolonged inactivity, such as while lying in bed at night, when they are termed rest cramps or nocturnal leg cramps. Rest cramps associated with aging are very common in general practice. Within a UK general practice population, roughly one‐third of men and women over the age of 50 reported experiencing a rest cramp during the preceding two months and of those who experienced such cramps, 40% cramped three or more times per week and six per cent cramped nightly (Naylor 1994). Although they can occasionally occur in the same people and share a similar name, rest cramps and restless leg syndrome should not be confused. Restless leg syndrome is not painful and has no palpable muscle tightening, rather it is an unpleasant sensation of 'needing to move' one's legs that prevents relaxation.
Description of the intervention
Magnesium (chemical symbol: Mg) is the fourth most abundant mineral in the human body and a normal component of a typical diet. Foods which are generally high in magnesium include dark green leafy vegetables, legumes, nuts, seeds, and unrefined grains. Oral magnesium supplements are also widely available without prescription and many of these are actively marketed for cramp prophylaxis. Such supplements are salts of magnesium and typically combine magnesium with citrate, lactate, gluconate, malate, orotate, chloride, oxide, carbonate, hydroxide, sulphate, or combinations of these anions. Most are in tablet form but some are available as liquid suspensions or as powders or crystals to be dissolved in water. Magnesium is absorbed largely in the small bowel by both passive diffusion and by a saturable active transport mechanism that results in a smaller percentage of the ingested oral magnesium being absorbed as dosage increases (Graham 1960; Quamme 2008). As a result, higher doses of oral magnesium salts can potentially lead to diarrhoea because of osmotic retention of fluid within the colon. Some magnesium salts, such as magnesium sulphate and magnesium hydroxide, are commonly employed as laxatives for that reason. Other than the diarrhoea occurring with high doses, oral magnesium supplements are generally considered to be safe and relatively free of adverse effects. Injectable magnesium salts (e.g. magnesium sulphate) are also available and are indicated intravenously (IV) in some countries for the acute management of seizures, especially in pregnancy (eclampsia). Excessively rapid IV magnesium infusion can lead to cardiorespiratory suppression and flaccid paralysis of skeletal muscle (AHFS 2010). Although the IV preparation can be given intramuscularly (IM), it is associated with discomfort at the injection site.
How the intervention might work
The demonstrated efficacy of IV magnesium to prevent eclamptic seizures (Eclampsia Trialists 1995; MAGPIE 2002), and the neuromuscular suppression (loss of strength, diminished reflexes) which can manifest when high parenteral doses of magnesium are used (Somjen 1966), both suggest that magnesium could potentially play a role in reducing neuromuscular excitability. Although the mechanism behind skeletal muscle cramps is unclear, if a threshold for depolarization needs to be reached within motor neurons to initiate cramping, anything which conceivably reduces excitability might provide cramp prophylaxis. Hence, if magnesium supplementation were to truly suppress excitable tissue, it might also suppress muscle cramps. This would be consistent with the description of symptoms said to arise from severe magnesium deficiency, which include muscle cramping, though probably as a manifestation of tetany (Bilbey 1996; Hall 1973; Shils 1969).
Why it is important to do this review
The only intervention for cramp prophylaxis whose (modest) efficacy is supported by systematic review is the antimalarial drug quinine. Compared to placebo, over a two‐week interval quinine significantly reduced cramp number by 28%, cramp intensity by 10% and number of cramp days by 20% (El‐Tawil 2015). Cramp duration remained unchanged. Unfortunately, quinine has also been associated with significant haematologic and cardiac toxicity and its use as an off‐label cramp prophylactic has been actively discouraged by multiple drug regulatory agencies such as the US Food and Drug Administration (FDA) and its counterparts in Australia and New Zealand (ADRAC 2002; FDA 2006; Medsafe 2007). The commonest non‐prescription alternative to quinine for the prophylaxis of cramps, widely marketed over the Internet and readily available in both pharmacies and health food stores, is oral magnesium supplementation. We are aware of several studies employing oral magnesium for rest cramp prophylaxis in both pregnant and elderly populations. We are also aware that these data conflict to some degree. Given how common skeletal muscle cramps are, especially in older adults, an effective and safe alternative to quinine is needed. With this review we hope to determine whether, in any setting in which skeletal muscle cramps occur, magnesium supplementation provides effective cramp prophylaxis. The current version of this review is an update, with the original protocol published in 2011 (Garrison 2011b), and the original full review published in 2012 (Garrison 2012b).
Objectives
To assess the effects of magnesium supplementation compared to no treatment, placebo control, or other cramp therapies in people with skeletal muscle cramps.
Methods
Criteria for considering studies for this review
Types of studies
Open‐label, single‐blind, or double‐blind randomized controlled trials (RCTs) (including parallel‐group and cross‐over trials). We did not exclude studies based on language or publication status.
Types of participants
People in any age group with any form of skeletal muscle cramp, whether idiopathic or disease‐associated, and in any body part.
Participants potentially included (but were not limited to) those with nocturnal leg cramps, pregnancy‐associated leg cramps, exercise‐associated cramps, and disease‐state‐associated cramps such as those associated with ALS/MND, haemodialysis or liver failure.
Types of interventions
Magnesium salts and combinations of salts (e.g. magnesium citrate, lactate, gluconate, malate, orotate, chloride, oxide, carbonate, hydroxide, or sulphate) administered orally or parenterally (IM or IV) at any dose. We excluded trials if the intervention combined magnesium salts with other active ingredients unless the same intervention was given to both groups.
Valid comparators included placebo, no treatment, or other cramp therapies (e.g. prophylactic stretching, quinine, calcium channel blockers, sodium channel blockers, electrolyte supplements, or supplemental hydration).
Types of outcome measures
The outcomes gathered for meta‐analysis are listed below, but we used none as criteria for study inclusion.
Primary outcomes
Cramp frequency (percentage change from baseline at 4 weeks), measured as the per cent change from baseline in the number of muscle cramps per week at four weeks
We chose per cent change from baseline in the number of muscle cramps per week as the primary outcome because we believe it to be the most clinically relevant outcome measure and because the effect of cramp treatments in general is more likely to be proportional to baseline cramp rate than to be additive (i.e. a person with 20 cramps per week and a person with two cramps per week who receive benefit from a therapy are more likely to see a similar percentage reduction in cramps than to share a similar absolute reduction in the number of cramps per week).
Secondary outcomes
Cramp frequency (percentage change from baseline at 12 weeks)
Cramp frequency (responder analysis), measured as the percentage of participants with at least a 25% reduction from baseline in the number of muscle cramps per week at four weeks and 12 weeks
We performed a responder analysis as a secondary outcome since most therapies only work in a subset of individuals. Hence, it is useful to know how many people experience what we believe to be the minimum clinically important difference (a 25% reduction in cramp rate).
Cramp frequency (cramps per week on treatment), measured as the number of cramps per week at four weeks and 12 weeks
We chose this as a secondary outcome to improve the ability to pool results if studies did not report baseline cramp rates. We also chose this measure because percentage change in cramp rate (the primary outcome) can have low power when the correlation between baseline and post‐treatment measures is low (i.e. Pearson correlation coefficient less than 0.5) and in this low range of correlation the difference between treatment groups at the end of treatment offers better power than either percentage change or absolute change from baseline (Vickers 2001). In a recent RCT that we conducted (five consecutive days of IV magnesium versus IV placebo infusions in nocturnal leg cramp sufferers with comparison of change in cramp rate from baseline at days 30 and 90), we found the correlation coefficient between baseline and post‐treatment cramps to be approximately 0.5 (Garrison 2011a). We believe the minimum clinically important difference for this measure to be one cramp per week.
Cramp intensity (pain scale), as measured on a three‐point scale at four weeks and 12 weeks
We chose to work with a three‐point intensity scale believing that some studies would record intensity as mild, moderate, or severe. If discretely recorded in this way, we would consider that mild equals 1, moderate equals 2, and severe equals 3 on our three‐point scale. We translated the mean of all cramp intensities (if cramps were individually rated) or the global assessment of cramp pain while on treatment into a three‐point scale representing cramp intensity if the study used a scale with a different range. If cramp intensity was rated on a scale from 0 to 10, for instance, we converted to a three‐point scale by multiplying mean and SD by 3/10. We analyzed intensity this way because it allowed us to combine the largest possible number of studies, and have the greatest power to demonstrate a difference between groups. However, our conversion of ordinal data to continuous data impairs the clinical interpretation of the resulting mean difference. Like the common use of standard mean difference to pool disparate scales, this measure sacrifices clinical meaning to have the greatest chance of determining whether a difference exists. To provide clinical meaning for cramp intensity, we have also included the following dichotomous measure.
Cramp intensity (moderate or worse), as measured by the number of individuals rating their cramps as moderate or severe (i.e. a score of at least 2 on a 3‐point intensity scale)
Counting the number of people with at least moderately painful cramps allowed us to report any change in cramp intensity in a more relatable way than a pain scale can provide.
Cramp duration of 1 minute or more, as measured by the number of individuals with the majority of their cramps lasting one minute or more
Knowing that duration was often being recorded categorically, and with different scales, we chose to analyse it as a dichotomous outcome in order to maximize the chance of being able to combine participant‐level data.
Treatment withdrawals due to adverse events
Minor adverse events, measured as the number of participants reporting minor adverse events (minor adverse events being symptoms not requiring medical treatment).
Major adverse events, measured as the number of participants reporting major adverse events (major adverse events being death, hospitalizations, or symptoms requiring medical treatment)
Search methods for identification of studies
Electronic searches
We searched the following databases.
Cochrane Neuromuscular Specialised Register via the Cochrane Register of Studies (CRS Web; searched 9 September 2019; Appendix 1)
Cochrane Central Register of Controlled Trials (CENTRAL) via the CRS Web; searched 9 September 2019; Appendix 2)
MEDLINE (1946 to 6 September 2019; Appendix 3)
Embase (1974 to 6 September 2019; Appendix 4)
AMED (1985 to August 2019; Appendix 5)
LILACS (1982 to 6 September 2019; Appendix 6)
CINAHL (1937 6 September 2019; Appendix 7)
SPORTDiscus (1985 to 6 September 2019; Appendix 8)
US National Institutes of Health Ongoing Trials Register (www.ClinicalTrials.gov; searched 6 September 2019; Appendix 9)
World Health Organization International Clinical Trials Registry Platform (WHO‐ICTRP; apps.who.int/trialsearch; searched 6 September 2019; Appendix 10)
Searching other resources
We searched ISI Web of Science for articles citing the studies included in this review (2 December 2019). To do this, we manually used their "cited reference browser" to separately locate each included study and then reviewed all titles listed as citing that work. We also checked all references in the identified trials and, when needed, contacted the trial authors for clarification and to obtain additional published or unpublished data. In our original review (2012), hoping to capture any trials that predated trial registration, we also contacted the American Food and Drug Administration (FDA), Health Canada, and relevant pharmaceutical manufacturers to request any unpublished trials that might be in their possession.
Data collection and analysis
Selection of studies
Two review authors (from SG, RS, ND) independently examined the titles and abstracts of all articles identified by the searches, obtained the full text of all potentially relevant studies and determined which studies met the inclusion criteria. A third review author (either SG or ND) was available to adjudicate any disagreements regarding study inclusion.
We created a PRISMA flow chart to outline the study selection process.
Data extraction and management
We collected information on study design and setting, participant characteristics (including cramp‐associated conditions and age), study eligibility criteria, details of the intervention(s) given, the outcomes assessed, the source of study funding and any conflicts of interest stated by the investigators. Two review authors (from SG, ND, MK, TK, GMA) independently extracted data onto specially designed forms. SG (original review) and ND (2019 update) entered data into Review Manager 5 (RevMan 5) and a second author (from VM, GMA, RS) independently checked data entry (Review Manager 2014).
Assessment of risk of bias in included studies
Two review authors (from SG, VM, GMA, TK, MK, ND) assessed the risk of bias in the included studies using the Cochrane 'Risk of bias' tool (Higgins 2011). We resolved differences in assessment of bias by consensus with a third author (SG), available in cases of disagreement. We documented the risk of bias within each study according to eight domains: sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective outcome reporting; use of a cramp diary; and 'other sources of bias'. We rated the included studies at high, low, or unclear risk of bias in each domain. Use of a cramp diary was included as a dimension for bias in this review since participant recollection at the time of an exit interview is open to more bias, especially if blinding is poor. Two review authors, SG and Karim Khan (author of previous version), were also co‐authors of one of the included trials. Neither of these authors participated in the bias rating of their own trial.
Measures of treatment effect
Diary recording of individual cramps, along with their intensity and duration, was the preferred measure of cramps, but we accepted any means of recording cramp data (e.g. participant recollection at the time of reassessment) from which the number of cramps per week could be calculated. In order to combine results, the number of cramps per week needed to be reported and calculable on a continuous scale. We did not use cramp frequency data for meta‐analysis if it was reported in category ranges such as 'less than two cramps per week' or 'more than seven cramps per week'.
For duration and intensity of cramps, either an average of the duration and intensity of each cramp over the treatment period or a global assessment by each participant regarding duration and intensity was acceptable, so long as we could meaningfully convert intensity into our three‐point intensity scale, and so long as we could meaningfully apply our '1 minute or more' duration cut‐off.
We reported the mean difference (MD) and 95% confidence interval (CI) for cramp frequency, cramp intensity and cramp duration. For responder analyses and adverse events we reported the risk ratio (RR) with 95% CI.
Unit of analysis issues
For each included study, the unit of analysis and the unit of randomization (expected to be the participant) needed to match to prevent the introduction of bias. We combined continuous outcomes using the generic inverse variance method (GIV) which allowed paired data from cross‐over trials (in which participants serve as their own controls) to be combined with two‐group parallel studies. We obtained standard error estimates for included studies from intervention and control group means and standard deviations when unpaired t‐tests were applied (parallel‐group trials), and from the MD between groups and P value for the difference when paired t‐tests were used (cross‐over trials).
Dealing with missing data
We requested any missing data from the study authors. Where studies measured cramp rate, intensity, or duration in categories that did not allow us to meaningfully convert cramp rate into a continuous number of cramps per week (or intensity and duration into our three‐point scales), we described and discussed these studies but did not include them in the meta‐analysis.
Assessment of heterogeneity
We assessed heterogeneity by using a Chi² test on n minus 1 degree of freedom and by calculating the I² statistic. If I² exceeded 25% we conducted a sensitivity analysis. We considered heterogeneity to have potential clinical importance when I² exceeded 40% and also the Chi² test was significant at P less than 0.1.
Assessment of reporting biases
We planned to use a funnel plot to assess publication bias but there were too few studies for this to be meaningful. We considered outcome reporting bias in 'Risk of bias' assessments.
Data synthesis
Our inclusion criteria encompassed a wide range of diagnoses (e.g. cramps associated with exercise, pregnancy, aging or disease states such as ALS/MND) for which a variation in treatment effect was certainly possible. However, combining such disparate patient populations using a random‐effects model and producing an overall treatment effect for magnesium across all populations could have been misleading and not properly address the clinical question, which should clearly account for the clinical setting. Accordingly, we undertook a fixed‐effect analysis within each of the clearly defined clinical settings for which data were available (these being pregnancy and idiopathic leg cramps) and did not provide meta‐analysis across all participant groups. The exception to this was adverse events, which we needed to pool across patient groups in order to obtain sufficient data to report, and which we believed would be more similar across populations. Any across‐group comparison was descriptive (qualitative) in nature. For meta‐analysis within each clinical setting we calculated the I² statistic and, if it exceeded 25%, we conducted a sensitivity analysis (see Sensitivity analysis). We combined trial data identified for inclusion in this review using the Cochrane statistical package, RevMan 5 (Review Manager 2014).
Subgroup analysis and investigation of heterogeneity
An insufficient number of studies was available to permit meaningful subgroup analysis at this time.
We planned, if a sufficient number of studies had been found, to use subgroup analysis to search for variation in treatment effect and to explore possible sources of heterogeneity. Subgroups related to clinical presentation were to include gender and cramp frequency with a 'high frequency' versus 'low frequency' subgroup defined as averaging one or more cramps per day at baseline. Subgroups related to method of treatment were to include route of administration (oral versus parenteral), formulation (grouped by the specific magnesium salt used), and duration of therapy (four weeks or less, more than four to eight weeks, more than eight weeks). We intended to view results from these subgroup analyses merely as hypothesis generating. To conduct a predefined subgroup analysis we required two or more subgroups within the analysis to have a minimum of 75 participants in each treatment arm.
Sensitivity analysis
We planned in our protocol to present results both with and without the outlying trial(s), where heterogeneity exists. While 'outlying' trials potentially include trials with extreme results, we also mean it to encompass any trial with a meaningful difference in study design ‒ such as high risk of bias, differing approaches to recruitment or resulting study populations, differing intervention (e.g. dose, formulation, duration of treatment), and differing sources of funding.
Heterogeneity existed only in the trials of magnesium versus placebo for the prophylaxis of pregnancy‐associated leg cramps (three studies). None of these trials reported outcomes in a way that permitted data pooling. We discussed differences in study design that could have led to their discrepant results qualitatively.
Summarizing findings and assessing certainty of the evidence
We included 'Summary of findings' tables for magnesium versus placebo in people with idiopathic cramps and in people with pregnancy‐associated cramps. We included adverse events' data for all causes of cramp. The 'Summary of findings' table presented our assessments of the certainty of the evidence for the following outcomes.
-
Cramp frequency
Percentage change from baseline at four weeks
Responder analysis
Cramps per week on treatment
Cramp intensity (moderate or worse))
Cramp duration ≥ one minute at four weeks
Minor adverse events (all causes)
Major adverse events (all causes)
We used the GRADE approach to assess the overall certainty of the evidence for each outcome and each comparison, and used GRADEpro GDT to calculate natural frequencies (GRADEpro GDT). Starting from ’high certainty’ (because we only included RCTs), we downgraded the certainty for serious study limitations including high risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates, or potential publication bias. We downgraded once if a consideration was present to a serious degree and twice if very serious. We included footnotes to explain reasons for downgrading (Schünemann 2011a; Schünemann 2011b).
Results
Description of studies
Results of the search
In total (current update and original search) our search returned the following number of citations: Medline 110, Embase 93, CENTRAL 35, CINAHL Plus 21, SPORTDiscus 16, Cochrane Neuromuscular Specialized Register 7, AMED 1, LILACS 1, WHO‐ICTRP 76, ClinicalTrials.gov 3, ISI Web of Science 79.
The authors reviewed full texts of 21 studies. We excluded 10 (see Characteristics of excluded studies), leaving 10 published studies that met our inclusion criteria. Additionally, one completed but unpublished study was identified through the WHO‐ICTRP registry (NCT00963638), bringing the total of included studies to 11.
Searching CinicalTrials.gov and WHO‐ICTRP revealed one ongoing study (NCT03082625). We contacted the author and no preliminary results were available. Examining reference lists of all included studies and relevant reviews revealed two studies whose full papers we obtained but which we excluded. Contacting the FDA, Health Canada, and relevant manufacturers (for our original 2012 review) revealed no additional studies.
See Table 3 for a tabulated summary of the included trials, and Figure 1 and Figure 2 for the study flow diagrams of the original and updated searches. All included trials are in English but we made no exclusions based on language. Of the 11 included studies, seven were available for our original (2012) review and four are newly identified (Cohen‐Hagai 2018; Roguin Maor 2017; Shahraki 2006; Supakatisant 2015). Study design and participant characteristics are summarized in Table 3.
1. Study design of the eleven included trials.
| Study | Number/design/clinical Setting | Mean age (years) | % Female | Magnesium dose and route of administration | Frequency of administration | Treatment and assessment periods (days) | Washout period (days) | Comparator |
| Cohen‐Hagai 2018 | N = 29 Parallel Liver cirrhosis |
62.0 | 41.4% | 520 mg magnesium oxide tablets (315 mg elemental Mg) | Once daily | Treatment 56 Assessment 56 |
Not applicable | Matched placebo tablet |
| Dahle 1995 | N = 73 Parallel Pregnancy |
Not given (child‐ bearing years) |
100% | 5 mmol combination Mg lactate + Mg citrate (122 mg elemental Mg) taken orally | Once each morning and twice each evening | Treatment 21 Assessment 21 |
Not applicable | Matched placebo tablet |
| Frusso 1999 | N = 45 Cross‐over Idiopathic |
61.6 | 73.3% | Mg citrate 900 mg tablet (100 mg elemental Mg) taken orally | Twice daily | Treatment 28 Assessment 28 |
28 | Matched placebo tablet |
| Garrison 2011a | N = 46 Parallel Idiopathic |
69.3 | 69.6% | 20 mmol Mg sulphate (486 mg elemental Mg) given intravenously | Once daily over 4 hrs on 5 consecutive days | Treatment 5 Assessment 90 |
Not applicable | Matched placebo solution |
| Nygaard 2008 | N = 45 Parallel Pregnancy |
30.9 | 100% | Mg lactate and Mg citrate chewable tablets containing 122 mg elemental Mg taken orally | Once each morning and twice each evening | Treatment 14 Assessment 14 |
Not applicable | Matched placebo tablet |
| Roffe 2002 | N = 73 Cross‐over Idiopathic |
62.9 | 54.3% | 1830 mg of tri‐magnesium dicitrate powder (300 mg elemental Mg) poured from a sachet into a glass of water taken orally | Once each evening | Treatment 42 Assessment during last 28 days of treatment |
First 14 days of second treatment period considered as washout |
Matched placebo powder |
| NCT00963638 | N = 40 Parallel Idiopathic |
66.6 | 57.5% | Slow release tablet of Mg lactate containing 84 mg of elemental Mg taken orally |
2 tablets twice daily | Treatment 30 Assessment 30 |
Not applicable | Matched placebo tablet |
| Sohrabvand 2006 | N = 84 Parallel Pregnancy |
Not given (child‐ bearing years) |
100% | 7.5 mmol magnesium aspartate (182 mg elemental Mg) taken orally. Unclear if tablet or powder / solution |
Twice daily | Treatment 14 Assessment 28 |
Not applicable | 3 different comparators 1) No treatment 2) 500 mg calcium carbonate tablet once daily 3)100 mg of thiamine (vit B₁) plus 40 mg of pyridoxine (vit B₆) once daily |
| Shahraki 2006 | N = 120 Parallel Pregnancy |
29.2 | 100% | 8 cc of an 8% milk of magnesium suspension (267.2 mg of elemental magnesium) | 3 times a day | Treatment 45 Assessment 90 |
Not applicable | 2 different comparators 1) 100 mg of vitamin E once daily 2) 500 mg of calcium carbonate once daily |
| Supakatisant 2015 | N = 86 Parallel Pregnancy |
28.7 | 100% | Mg bisglycinate tablets containing 100 mg of elemental mg taken orally | 3 times a day | Treatment 28 Assessment 28 |
Not applicable | Matched placebo tablets |
| Roguin Maor 2017 | N = 94 Parallel Idiopathic |
64.9 | 63% | 865 mg magnesium oxide capsules (520 mg elemental Mg) | Once daily at bedtime | Treatment 28 Assessment 28 |
Not applicable | Matched placebo capsules |
vit B₁: vitamin B₁
1.
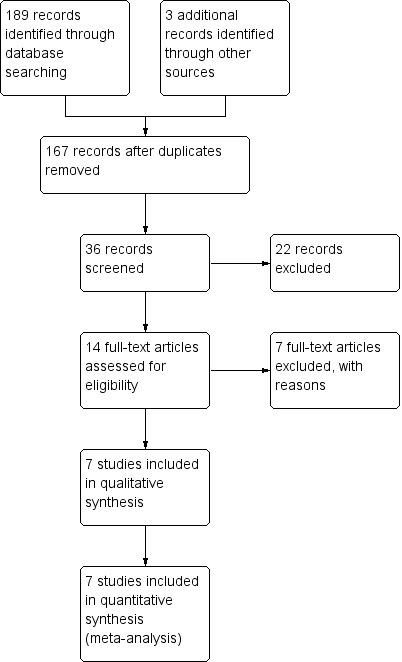
Study flow diagram for the original (2012) systematic review.
2.
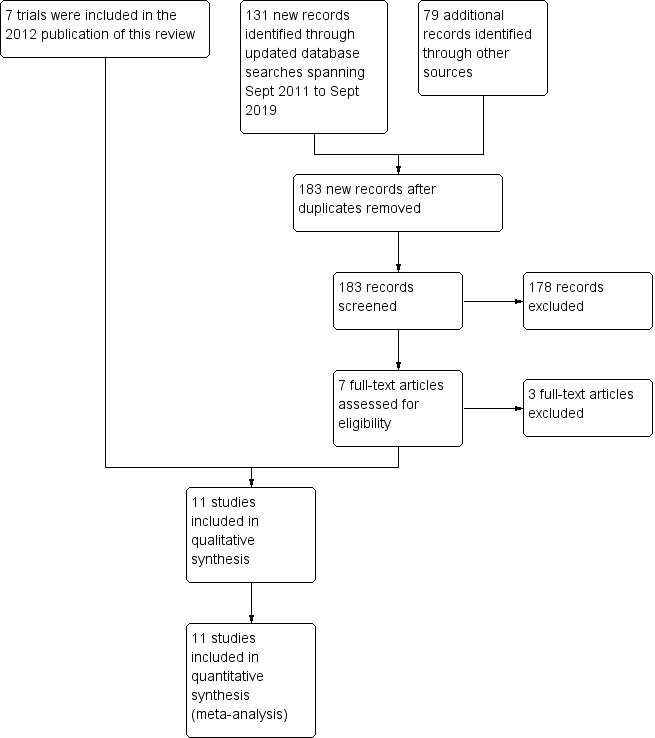
Study flow diagram for the September 2019 update.
Included studies
Study design
Nine of the studies were parallel in design (Cohen‐Hagai 2018; Dahle 1995; Garrison 2011a; NCT00963638; Nygaard 2008; Roguin Maor 2017; Shahraki 2006; Sohrabvand 2006; Supakatisant 2015); and two idiopathic cramp studies were cross‐over (Frusso 1999; Roffe 2002). One of the cross‐over trials included a 28‐day washout period (Frusso 1999). The other did not have a formal washout period but evaluated outcomes only in the last four weeks of each of two sequential six‐week treatment periods (Roffe 2002). This effectively gave a two‐week washout to those who started on magnesium and an extra two weeks of magnesium therapy (while on magnesium) prior to each evaluation period. A total of 735 participants were enrolled in these trials. Of these, 118 were participants in cross‐over trials and additionally formed their own controls. All trials were small, varying from 29 to 120 participants.
Interventions and comparators
Magnesium was generally compared to placebo (eight trials). One trial, however, with four parallel treatment arms compared no treatment to magnesium, calcium carbonate, and a combined supplement of vitamins B₁ and B₆ (Sohrabvand 2006), and one trial compared magnesium to either a calcium or a vitamin E supplement (Shahraki 2006).
Magnesium was given orally in all but one trial, where it was administered as a series of intravenous infusions (Garrison 2011a). Oral magnesium was given either once daily (Cohen‐Hagai 2018; Roffe 2002; Roguin Maor 2017); twice daily (Dahle 1995; Frusso 1999; NCT00963638; Nygaard 2008; Sohrabvand 2006), with larger doses at night in two studies (Dahle 1995; Nygaard 2008); or three times a day (Shahraki 2006; Supakatisant 2015).
The amount of elemental magnesium administered daily through the various oral protocols included 366 mg from "primarily magnesium lactate and magnesium citrate" tablets (Dahle 1995; Nygaard 2008), 200 mg from magnesium citrate tablets (Frusso 1999), 300 mg from tri‐magnesium dicitrate powder dissolved in water (Roffe 2002), 336 mg from magnesium lactate as slow‐release tablets (NCT00963638), 300 mg from magnesium bisglycinate tablets (Supakatisant 2015), 802 mg from 8% milk of magnesium suspension (Shahraki 2006), 520 mg from magnesium oxide tablets (Roguin Maor 2017), 315 mg from magnesium oxide tablets (Cohen‐Hagai 2018), and 364 mg from magnesium aspartate (Sohrabvand 2006) (unclear if tablet or powder).
The durations of treatment for oral magnesium ranged from 14 to 56 days, with total oral doses of elemental magnesium over the entire treatment period ranging from 5096 mg to 36,072 mg. The study providing magnesium intravenously gave 20 mmol of magnesium sulphate (486 mg of elemental magnesium) as an infusion over four hours on five consecutive days (Garrison 2011a). This provided a total treatment dose of 2430 mg of elemental magnesium, although with possibly different (higher) bioavailability. This trial recorded cramps for 90 days post infusions but all other trials recorded cramps over only two to four weeks.
Outcomes
Published and unpublished data were available for the following outcomes.
Cramp frequency
All five idiopathic cramps trials reported the number of cramps per week during the treatment period. Of these, three trials also provided data for per cent change from baseline in the number of cramps per week, and three trials provided data for a responder analysis (≥ 25% reduction from baseline frequency). In contrast, of the five pregnancy‐associated cramp trials, one reported per cent change from baseline, one reported a responder analysis (≥ 50% reduction from baseline frequency), and three reported cramp frequency on treatment but each was reported in a way that prevented results being combined. This included cramp frequency on a five‐point ordinal scale (daily, every other day, twice a week, once a week, never), mean number of days and nights with leg cramps present, and number of days and nights of cramping. The single trial in people with liver cirrhosis collected information on cramp frequency but did not report cramp frequencies in each group, instead reporting only 1) a P value for the difference in cramp frequency between groups and 2) the number of people who were experiencing cramps in each group at baseline and on treatment.
Cramp intensity
Four of the idiopathic cramp trials provided cramp intensity on a pain scale such that results could be scaled and pooled, and two trials provided data that allowed us to determine the number of cramps that were moderate or worse. Three of the pregnancy‐associated cramp trials reported pain intensity, but none in a way that permitted pooling of results. The single trial in people with liver cirrhosis provided only a P value for the difference in cramp intensity between groups.
Cramp duration
Four idiopathic cramp trials reported cramp duration, but only one reported it in a way that allowed us to determine the number of cramps that lasted one minute or more. None of the pregnancy‐associated trials reported cramp duration, nor did the trial in people with liver cirrhosis.
Withdrawals due to adverse effects
Most studies had omissions or inconsistencies which prevented the determination of the number of withdrawals due to adverse effects but the total number of withdrawals was available for three of five idiopathic cramp trials, all five pregnancy‐associated cramp trials, and the single trial in people with liver cirrhosis.
Minor adverse events
Most trials reported minor adverse events, but only one idiopathic cramp trial, two pregnancy‐associated cramp trials, and the single trial in people with liver‐cirrhosis‐associated muscle cramps did so in a way that allowed us to determine the number of people experiencing any minor adverse event.
Major adverse events
Major adverse events were reported in two idiopathic cramp trials and one pregnancy‐associated cramp trial.
Participants
Five studies involved treatment of pregnancy‐associated leg cramps (Dahle 1995; Nygaard 2008; Shahraki 2006; Sohrabvand 2006; Supakatisant 2015), one study involved treatment of people with liver cirrhosis (only some of whom experienced cramps) (Cohen‐Hagai 2018), and the remaining five studies involved the treatment of idiopathic cramps in older adults (most of whom are presumed to have been suffering nocturnal leg cramps) (Frusso 1999; Garrison 2011a; NCT00963638; Roffe 2002; Roguin Maor 2017). We found no studies investigating exercise‐associated cramps. All participants were community dwelling. Most participants were outpatients recruited from primary care or maternity clinics, although some were recruited by newspaper or radio advertisement. In the five trials reporting participants' age and sex, idiopathic cramp trial participants were 64.9 years of age on average and 62.1% were female. In the single study of people with liver cirrhosis, participants were 62.0 years of age and 41.4% were female. Only three of the five pregnancy‐associated cramp trials provided data on mean age (29.3 years).
Unpublished data
One of the trials was unpublished (NCT00963638), but some participant‐level data were made available to us. Three other studies also made participant‐level data available (Garrison 2011a; Roffe 2002; Roguin Maor 2017), although the data from Roffe 2002 did not include noncompleters.
See Characteristics of included studies and Additional tables.
Excluded studies
We excluded 10 studies. Excluded trials were either uncontrolled, not randomized, did not have a magnesium treatment arm, did not measure outcomes relevant to cramping, or had differences in how groups were treated other than receipt of magnesium or control. See Characteristics of excluded studies.
Ongoing studies
We identified one ongoing study (NCT03082625). See Characteristics of ongoing studies.
Risk of bias in included studies
We carried out the 'Risk of bias' assessment as outlined in the methods and summarized our assessments in Figure 3. There was considerable variability in the quality of included trials. There was also an issue with one of the cross‐over studies whose author kindly provided us participant‐level data (Roffe 2002). It is our opinion that this cross‐over trial demonstrated a large difference in treatment effect depending on the sequence of treatments. Of 17 participants receiving the sequence magnesium followed by placebo, eight favoured magnesium, seven favoured placebo, and two were unchanged. In contrast, of 29 participants receiving the sequence placebo followed by magnesium, 21 favoured magnesium, five favoured placebo, and three were unchanged. It is unclear how much of this difference was due to the period effect and how much was due either to the high rate of noncompleters (27 of 73 participants did not complete the trial), the potential for carry‐over, or the potential for unblinding. As a result of this sequence order effect we chose to minimize these potential sources of bias by using only data from the first period of the study.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study. Red (+) = high risk of bias; yellow (?) = unclear risk of bias; green (+) = low risk of bias.
Allocation
The risk of selection bias (randomization or allocation) was unclear (though likely adequate) in six of 11 trials, largely because of inadequate description of methods in the manuscripts and our inability to obtain responses from some authors (Cohen‐Hagai 2018; Dahle 1995; Frusso 1999; NCT00963638; Nygaard 2008; Sohrabvand 2006). In one cross‐over trial, the manufacturer provided randomization in large blocks that were either unbalanced initially or became unbalanced because of noncompleters (17 participants were randomized to placebo followed by magnesium and 29 to magnesium followed by placebo) (Roffe 2002). Since the treatment effect in this trial varied depending on the sequence order of treatment, this imbalance in sequence allocation was an important potential source of bias and thus we pooled data only for the first treatment period, effectively considering this as a parallel‐group study. Once this limitation to the first treatment period was made, we considered Roffe 2002 to be at low risk of allocation bias. We considered one trial at high risk of bias because it was unclear how randomization was done and no information was available regarding allocation concealment (mentioning only that a written prescription was given to each participant) (Shahraki 2006). We considered the three remaining trials at low risk of selection bias (Garrison 2011a; Roguin Maor 2017; Supakatisant 2015).
Blinding
Blinding was at low risk of bias for both performance and detection bias in six of 11 trials (Cohen‐Hagai 2018; Frusso 1999; NCT00963638; Nygaard 2008; Roguin Maor 2017; Supakatisant 2015). In one trial the risk of bias was unclear because of a greater likelihood of magnesium recipients experiencing a burning sensation at the IV site during intravenous infusion (Garrison 2011a). In one cross‐over trial the risk of bias was unclear because no description was given as to whether magnesium and placebo solutions could be distinguished by taste (Roffe 2002). In one trial, the risk of performance bias was low, but the risk of detection bias was unclear because the investigators obtained data through interview of participants, but provided no information regarding the blinding of interviewers (Dahle 1995). The risk of bias was high in two trials because they were unblinded (open label) (Sohrabvand 2006; Shahraki 2006).
Incomplete outcome data
Six of the 11 trials were at low risk of attrition bias (Dahle 1995; Frusso 1999; Garrison 2011a; NCT00963638; Roguin Maor 2017; Sohrabvand 2006). The risk of attrition bias was unclear in one trial with a 15.6% dropout rate (Nygaard 2008); and unclear in one trial that dealt with missing data by treating all participants with missing data as treatment failures ‒ as more data were missing in the control group, this favoured the intervention (Supakatisant 2015). We considered three trials at high risk of bias: the first because of a 37% dropout rate (Roffe 2002); the second because 30 out of 120 participants were not included in the analysis, and the report provided no information concerning at least 10 of them (Shahraki 2006); and the third because of a per‐protocol analysis and a large imbalance in dropout rates, with six of 14 magnesium recipients dropping out (42.8%) compared to only one of 15 (6.7%) placebo recipients (Cohen‐Hagai 2018).
Selective reporting
In six of the 11 trials, we considered the risk of reporting bias to be low (Frusso 1999; Garrison 2011a; Nygaard 2008; Roffe 2002; Roguin Maor 2017; Shahraki 2006). This included two studies whose manuscripts did report selectively (that is, both reported that some secondary outcomes were not statistically significant without providing actual numbers), but whose authors made the participant‐level data available to the authors of this review to allow for the calculation of these outcomes (Garrison 2011a; Roffe 2002). One study had an unclear risk of bias because of inconsistencies in reporting (Sohrabvand 2006). Four studies were at high risk of bias: one study because of inconsistency and possible mislabelling of results (Supakatisant 2015); one unpublished study, whose risk was high because only a subset of outcomes was available (NCT00963638); one study because it was unclear how well the outcomes were predefined (there was no description of outcomes by primary and secondary and the outcomes were incompletely described in the methods) (Dahle 1995); and one study which stated that cramp frequency and intensity were collected, but reported only P values for differences (Cohen‐Hagai 2018).
Other potential sources of bias
Cramp diary (recall bias)
We viewed two of the five trials in pregnant women as having a high risk of bias because they did not use cramp diaries (instead recalling cramp frequency at the time of exit interviews) (Dahle 1995; Sohrabvand 2006); and we considered three at unclear risk of bias because how they recorded cramps was not clear (Cohen‐Hagai 2018; Shahraki 2006; Supakatisant 2015).
Other bias
We identified no other potential sources of bias.
Effects of interventions
Summary of findings 1. Magnesium for idiopathic rest cramps (largely older adults).
| Magnesium compared with placebo for skeletal muscle cramps | ||||||
|
Patient or population: for effects on cramps, people (other than pregnant women) with muscle cramps (largely older adults); for adverse events, all populations Settings: outpatients recruited through primary care clinics or community advertising Intervention: magnesium supplements (oral or intravenous) Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Magnesium | |||||
| People (other than pregnant women) with muscle cramps, largely older adults | ||||||
| Cramp frequency (percentage change from baseline at 4 weeks) | The mean percentage change in cramp frequency in the control groups was −28.7% | The mean percentage change in cramp frequency in the magnesium groups was an additional 9.59% lower (23.14% lower to 3.97% higher) |
MD −9.59% (−23.14 to 3.97) |
177 (3 studies) | ⊕⊕⊕⊝
Moderatea due to imprecision |
Magnesium probably results in little to no difference in cramp frequency (based on percentage change from baseline at 4 weeks). The 95% CI excludes a 25% reduction beyond placebo |
|
Cramp frequency (responder analysis: 25% or better reduction at 4 weeks) |
644 per 1000 | 669 per 1000 (541 to 830) | RR 1.04 (0.84 to 1.29) | 177 (3 studies) | ⊕⊕⊕⊕ High | Magnesium results in little to no difference in cramp frequency (based on the proportion of people responding at 4 weeks) |
|
Cramp frequency (mean number of cramps per week on treatment at 4 weeks) |
The mean number of cramps per week in the placebo groups while on treatment was 4.68 |
The mean number of cramps per week in the magnesium groups was 0.18 cramps per week lower (0.84 lower to 0.49 higher) |
MD −0.18 cramps per week (−0.84 to 0.49) |
307 (5 studies) | ⊕⊕⊕⊝
Moderateb due to inconsistency |
Magnesium probably results in little to no difference in cramp frequency (based on number of cramps per week at 4 weeks). The 95% CI excludes a 1 cramp per week reduction |
|
Cramp intensity (moderate or worse at 4 weeks) |
300 per 1000 | 399 per 1000 (243 to 663) |
RR 1.33 (0.81 to 2.21) |
91 (2 studies) |
⊕⊕⊕⊝
Moderatec due to imprecision |
Magnesium is unlikely to reduce the number of people with cramp intensity of moderate or worse at 4 weeks |
|
Cramp duration (≥ 1 minute at 4 weeks) |
227 per 1000 | 416 per 1000 (168 to 1000) | RR 1.83 (0.74 to 4.53) | 46 (1 study) | ⊕⊕⊝⊝
Lowd due to very serious imprecision |
Magnesium may not reduce the number of people with a cramp duration ≥ 1 minute at 4 weeks |
| Adverse events: all populations | ||||||
| Major adverse events | 33 per 1000 |
23 per 1000 (5 to 110) |
RR 0.68 (0.14 to 3.31) |
185 (3 RCTs) | ⊕⊝⊝⊝
Very Lowe due to very serious imprecision and indirectness |
It is uncertain as to whether magnesium differs from placebo in terms of major adverse events |
| Minor adverse events | 198 per 1000 | 305 per 1000 |
RR 1.51 (0.98 to 2.33) |
254 (4 studies) |
⊕⊕⊝⊝
Lowf due to imprecision and indirectness |
Although this difference was borderline for statistical significance, the number of people dropping out of the included studies was no different in the magnesium group than it was in the placebo group. |
| CI: confidence interval; IV: intravenous; MD: mean difference; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderatecertainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aDowngraded once for imprecision since our investigator‐defined 25% minimum clinically important difference (MCID) is not derived from feedback from people with cramps. A smaller MD (e.g. 20%) might still be important to some people and is not yet ruled out. An additional consideration was that 1 unpublished study combined in this analysis was rated at high risk of bias for selective (incomplete) reporting. However this study was combined with 2 studies at low risk of bias with which its findings were consistent, and our initial downgrade for imprecision due to investigator‐defined MCID was considered a soft indication for a downgrade. Hence we chose not to add a second downgrade. bDowngraded once for inconsistency: although statistical heterogeneity was low and the CI excluded a '1 cramp per week' reduction, 3 of the 5 trials had point estimates exceeding a '1 cramp per week' reduction, with the overall estimate being pulled towards less benefit by 1 trial with 70% of the weighting in the analysis. Hence there is some inconsistency in the results. cDowngraded once for imprecision because the number of people with moderate to severe cramps was low (28). Although 1 of the 2 trials combined in analysis was at high risk of bias due to attrition (Roffe 2002), our high bias rating described the entire trial. We obtained and utilized patient level data for only the first period of this cross‐over study, which substantially mitigated the risk. Hence we did not carry out a second downgrade. dDowngraded twice for very serious imprecision as this estimate is based on a single trial with only 15 participants having cramps that lasted over a minute. eDowngraded 3 times ‒ twice for very serious imprecision, as this estimate is derived from only 5 events, and once for indirectness because we combined individuals with a variety of cramp syndromes (idiopathic rest cramps, pregnancy‐associated cramps, and liver‐cirrhosis‐associated cramps) fDowngraded once for imprecision because the number of people with minor adverse events was low (64), and downgraded once for indirectness because we combined individuals with a variety of cramp syndromes (idiopathic rest cramps, pregnancy‐associated cramps, and liver‐cirrhosis‐associated cramps)
Summary of findings 2. Magnesium for pregnancy‐associated leg cramps.
| Magnesium compared with placebo for skeletal muscle cramps | ||||||
|
Patient or population: pregnant women with leg cramps Settings: outpatients recruited through obstetrical care providers Intervention: magnesium supplements (oral) Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Magnesium | |||||
|
Cramp frequency (percentage change from baseline at 4 weeks) |
None of the 3 relevant studies measured cramp frequency in a way that permitted pooling of data. 1 study found benefit, 1 study was uninterpretable, and 1 study (the only 1 of the 3 that was not rated high risk of bias) trended in favor of placebo. Taken collectively, no conclusions can be drawn. | 204 (3 studies) |
⊕⊝⊝⊝
very lowa due to very serious risk of bias, inconsistency, and imprecision |
Whether or not magnesium supplementation reduces cramp frequency in pregnant women is uncertain | ||
|
Cramp frequency (responder analysis: 25% or better reduction at 4 weeks) | ||||||
|
Cramp frequency (mean number of cramps per week on treatment at 4 weeks) | ||||||
|
Cramp intensity (moderate or worse at 4 weeks) |
None of the studies reported cramp intensity in a way that permitted this to be determined. |
No studies | No evidence | |||
|
Cramp duration (≥ 1 minute at 4 weeks) |
None of the studies reported cramp duration | No studies | No evidence | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aDowngraded twice for very serious risk of bias given 2 of the 3 studies were considered at high risk of bias; downgraded once for inconsistency given 1 study reported benefit and another trended towards harm; and downgraded once for imprecision given all studies were relatively small (largest had 86 participants) and none could be pooled.
Magnesium versus placebo
Primary outcome: cramp frequency (percentage change from baseline at four weeks)
While all studies attempted to measure the cramp frequency, or change in cramp frequency, three trials in pregnant women used frequency measures that prevented data pooling and only one clearly used a cramp diary (Nygaard 2008). Cramp frequency measures that could not be pooled included cramp frequency on a five‐point ordinal scale (Dahle 1995), change in cramp frequency on a three‐point ordinal scale (Sohrabvand 2006), and number of days and nights in which cramps occurred (Nygaard 2008). In contrast, all five idiopathic rest cramp trials used cramp diaries and recorded the occurrence of each cramp, permitting analysis of cramp frequency as a continuous variable. The resulting pooled estimates of cramp frequency measures include data from two trials rated as having a high risk of bias, either due to a high dropout rate (Roffe 2002), which we mitigated by using only the first cross‐over period, or selective reporting (NCT00963638).
Pregnancy‐associated cramps
Only one pregnancy‐associated cramp trial reported a mean percentage reduction in the number of muscle cramps per week at four weeks (Supakatisant 2015). In this trial, 86 pregnant women received 100 mg of elemental magnesium three times daily or a matching placebo for four weeks. Participants in the magnesium group noted a 79% (95% CI 70.2% to 87.8%) mean reduction at four weeks compared to a 32.4% (95% CI 3.4% to 61.5%) reduction in the placebo group (P = 0.003). However, reporting in this trial appeared inconsistent (possibly due to a language barrier) with the authors stating and confirming by e‐mail that the median cramp rate actually increased during the trial. The other two trials did not appear to determine the baseline cramp rate needed to calculate a percentage change (Dahle 1995; Nygaard 2008).
Idiopathic rest cramps
At four weeks
Three of the five idiopathic rest cramp trials measured the baseline cramp rate over a pre‐treatment period of 30 days (Garrison 2011a), 14 days (Roguin Maor 2017), or seven days (NCT00963638). Pooling these three studies produced a small difference in the percentage change in cramp rate, magnesium versus placebo (MD −9.59%, 95% CI −23.14% to 3.97%; I² = 0%; 3 trials, 177 participants; moderate‐certainty evidence; Figure 4; Analysis 1.1). There was no evidence of heterogeneity and the resulting 95% CI excludes a 25% reduction in cramp rate over placebo.
4.

Forest plot of comparison: 1 Idiopathic rest cramps, magnesium versus placebo, outcome: 1.1 % Change in cramp frequency from baseline at 4 weeks.
1.1. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 1: Cramp frequency (percentage change from baseline at four weeks)
Secondary outcome: cramp frequency (percentage change from baseline at 12 weeks)
Pregnancy‐associated cramps
This outcome was not measured in the pregnancy‐associated cramp trials.
Idiopathic rest cramps
Only one study had data to 12 weeks (Garrison 2011a). The trial found a small difference in the percentage reduction in cramps for magnesium versus placebo (MD −12.09%, 95% CI −40.22% to 16.04%: 43 participants; Analysis 1.2).
1.2. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 2: Cramp frequency (percentage change from baseline at 12 weeks)
Secondary outcome: cramp frequency (responder analysis)
Pregnancy‐associated cramps
None of the pregnancy‐associated cramp trials reported percentage of participants with 25% or more reduction in cramp frequency or provided sufficient data to calculate such an effect. One trial did report percentage of participants with 50% or more reduction in cramp frequency (Supakatisant 2015). In this four‐week trial, 86% of women in the magnesium group noted a 50% or more reduction compared to 60.5% of women in the placebo group (P = 0.007).
Idiopathic rest cramps
At four weeks
Pooling results from the three trials with sufficient available data to calculate this outcome showed 64.4% of participants (56 of 87) in the placebo group to have achieved a 25% or better reduction in cramp frequency (Garrison 2011a; NCT00963638; Roguin Maor 2017), compared to 60 of 90 participants (66.6%) in the magnesium group, which is essentially equivalent (RR 1.04, 95% CI 0.84 to 1.29; I² = 12%; 3 studies, 177 participants; high‐certainty evidence; Figure 5; Analysis 1.3). There was only minor heterogeneity for which we did not downgrade the certainty of the evidence.
5.

Forest plot of comparison: 1 Magnesium versus placebo (idiopathic cramps ‐ efficacy), outcome: 1.3 Cramp frequency (responder analysis at four weeks).
1.3. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 3: Cramp frequency (responder analysis at four weeks)
At 12 weeks
The single study to 12 weeks found the percentage of participants achieving a 25% or better reduction in the frequency of cramps to be 10 of 20 participants in the placebo group (50%) and 14 of 23 participants (61%) in the magnesium group (Garrison 2011a), which is 22% higher in favour of magnesium (RR 1.22, 95% CI 0.70 to 2.10; 1 study, 43 participants; Analysis 1.4). The result was very imprecise.
1.4. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 4: Cramp frequency (responder analysis at 12 weeks)
Secondary outcome: cramp frequency (number of cramps on treatment)
Pregnancy‐associated cramps
At four weeks
Three trials evaluating the frequency of leg cramps compared magnesium to placebo in pregnant women (Dahle 1995; Nygaard 2008; Supakatisant 2015).
The earliest was the first published RCT of magnesium for cramping in any setting (Dahle 1995). It measured cramp frequency on a five‐point ordinal scale (daily, every other day, twice a week, once a week, never) and also measured participant evaluation of treatment effect on a five‐point ordinal scale (entirely free of symptoms, considerably improved, unchanged, worsened, considerably worsened). This study reported a reduction in the frequency of symptoms "from the initial average of every other day, to every three days in the placebo group and one to two times a week in the magnesium group (P < 0.05)". The way in which this result is reported is problematic in that "every 3 days" and "one to two times a week" do not belong to the five‐point ordinal scale used to measure this outcome. Dahle 1995 also reported benefit in participant evaluation of treatment effect, in that "the magnesium group indicated that they had to a significantly greater extent "improved considerably" or "become asymptomatic" compared with the placebo group (P = 0.0002)" (17/34 magnesium and 11/35 placebo recipients improving considerably, and 10/34 magnesium and 3/35 placebo recipients becoming asymptomatic). In contrast, the subsequent trial measured the mean number of days and nights with leg cramps present and found no significant benefit with 7.7 ± 4.7 (SD) days and nights of cramping over two weeks in the placebo group and 9.5 ± 5.1 in the magnesium group (P = 0.27) (Nygaard 2008). The most recent trial in pregnancy‐associated cramps reported an increase in the median number of cramps per week in both the magnesium (1 cramp per week increase) and placebo groups (3 cramps per week increase) (Supakatisant 2015). These increases, which we confirmed with the trial authors, are hard to reconcile with the substantial mean percentage reduction in cramp rate for both groups that the trial authors simultaneously report.
At 12 weeks
There were no trials of more than four weeks' duration that compared magnesium to placebo in pregnant women.
Idiopathic rest cramps
At four weeks
Cramps per week on treatment was available as an outcome for all five of the idiopathic rest cramp trials. The pooled estimate for the number of cramps per week was MD −0.18 cramps per week for magnesium versus placebo (95% CI −0.84 to 0.49; I² = 0; 5 studies, 307 participants; moderate‐certainty evidence due to inconsistency; Figure 6; Analysis 1.5). There was no evidence of heterogeneity and the CI excluded a 'one cramp per week' reduction. However the overall estimate is pulled towards less benefit by one trial with 70% of the weighting in the analysis. If this heavily weighted trial were removed the (non‐significant) pooled estimate would be for a 'one cramp per week' reduction. Hence there is some inconsistency in the results. As mentioned under Included studies, we used data from only the first period of Roffe 2002 because of an unbalanced randomization and a difference in benefit depending on treatment order.
6.

Forest plot of comparison: 1 Idiopathic rest cramps, magnesium versus placebo, outcome: 1.6 Number of cramps per week at 4 weeks.
1.5. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 5: Cramp frequency (number of cramps per week at four weeks)
At 12 weeks
The single study to 12 weeks found a nonsignificant MD in the number of cramps per week of −0.84 (95% CI −3.23 to 1.55; 1 study, 43 participants; Analysis 1.6) (Garrison 2011a). The result was very imprecise and consistent with a difference of more than a one cramp per week reduction in favour of either magnesium or placebo.
1.6. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 6: Cramp frequency (number of cramps on treatment at 12 weeks)
Liver‐cirrhosis‐associated cramps
Although the single trial in people with liver cirrhosis collected data on cramp frequency, the trialists reported only that at eight weeks: "Improvement in the severity and frequency of muscle cramps was not significant (P = 0.438 and 0.483 respectively)" (Cohen‐Hagai 2018). They additionally reported that in the intervention group, the percentage of people experiencing cramps fell from 80% at baseline to 22.2% at eight weeks, compared to the percentage of people in the control group experiencing cramps falling from 84% at baseline to 58.33% at eight weeks (with the P value stated to not be significant, but with no actual numeric P value provided). These numbers are somewhat problematic, in that it is not clear how a percentage of 22.2% could be obtained given there were only eight people analysed in the intervention group (i.e. no integer divided by eight equals 0.222). We were unable to reach the trial authors by e‐mail to obtain more information.
Secondary outcome: cramp intensity (pain scale)
Pregnancy‐associated cramps
Although all three trials comparing magnesium to placebo in pregnant women recorded cramp severity on scales which could potentially have been transformed into our three‐point scale, none reported results in a manner that allowed us to do so. In Dahle 1995, cramp intensity was recorded on a 0 mm to 100 mm visual analogue scale (VAS) but mean scores were reported without SD along with P value thresholds for the difference in change from baseline within and between groups. These results were reported as follows: "Subjectively experienced distress according to the VAS was reduced from 68.2 mm before to 47.8 mm after treatment (P < 0.05) in the placebo group and from 70.4 mm to 30.3 mm (P < 0.05) in the magnesium group. The reduction of distress in the magnesium group was significantly greater (P < 0.05) than in the placebo group." In Nygaard 2008, the intensity of cramping during each nighttime and each daytime were recorded on a 0 to 4 intensity scale (0 = no pain, 1 = light pain, 2 = medium pain, 3 = strong pain, 4 = severe pain) and added together over the two‐week assessment period. The mean of each participant's summed intensity scores was 11.4 ± 8.5 (SD) for placebo and 13.2 ± 6.5 for magnesium, with a nonsignificant P value for the difference (P = 0.46). In Supakatisant 2015, cramp intensity was recorded on a 0 mm to 100 mm VAS and results were reported as median absolute change of pain score at four weeks, being 34 mm and 53 mm with magnesium and placebo, respectively. This is difficult to interpret, as greater change is suggested in the placebo group. By contacting the authors we learned that mean cramp intensity score on the 0 mm to 100 mm VAS at four weeks was 20.3 mm with magnesium versus 32.1 mm with placebo. It seems likely that there is some mislabelling of what the reported numbers in the manuscript represent.
Idiopathic rest cramps
At four weeks
Pooling results from the four trials with available data (Frusso 1999; Garrison 2011a; Roguin Maor 2017; first period of Roffe 2002) shows, on a three‐point intensity scale, no important difference between magnesium and placebo (MD −0.02, 95% CI −0.16 to 0.12; I² = 0; 4 studies, 269 participants; Analysis 1.7).
1.7. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 7: Cramp intensity (pain scale) at four weeks
At 12 weeks
The single study with 12‐week data showed no important difference, on a three‐point intensity scale, between magnesium and placebo (MD −0.18, 95% CI −0.55 to 0.19; 1 study, 43 participants; Analysis 1.8) (Garrison 2011a).
1.8. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 8: Cramp intensity (pain scale) at 12 weeks
Liver‐cirrhosis‐associated cramps
Although the single trial in people with liver cirrhosis collected data on cramp intensity, the trialists reported only that at eight weeks: "Improvement in the severity and frequency of muscle cramps was not significant (P = 0.438 and 0.483 respectively)" (Cohen‐Hagai 2018). We were unable to reach the authors by e‐mail to obtain more information.
Secondary outcome: cramp intensity (moderate or worse)
Pregnancy‐associated cramps
None of the studies in pregnant women reported results in this way and participant‐level data were unavailable.
Idiopathic rest cramps
At four weeks
Results were not reported in this manner but participant‐level data were available from two studies (Garrison 2011a; first period of Roffe 2002) to allow us to calculate this statistic. Pooled results showed the mean percentage of placebo recipients rating their cramps as moderate or severe (i.e. 2 or 3 on the 3‐point scale) to be 30% (15 of 50 participants), with the mean percentage of magnesium recipients rating their cramps as moderate or severe being somewhat higher than in the placebo group (RR 1.33, 95% CI 0.81 to 2.21; 2 studies, 91 participants; I² = 6%; moderate‐certainty evidence; Analysis 1.9). Study populations were very different on this measure. Only three of 46 participants (6.5%) in Garrison 2011a rated their cramps as moderate to severe, compared to 25 of 45 participants (56%) in Roffe 2002. Differences in recruitment methods might account for the difference in participant populations, since Roffe 2002 recruited 100% of participants from community advertising, while Garrison 2011a recruited half from advertising and half from GP referral. Alternatively, the conversion of different scales to our three‐point scale (one integer, and one ordinal) might explain the difference. The higher dropout rate in Roffe 2002 (37% versus 0%) might also have contributed if participants who would have rated their cramps as less severe were more likely to drop out of the trial.
1.9. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 9: Cramp intensity (moderate or worse) at four weeks
At 12 weeks
The single study with 12‐week data found that 10% of placebo recipients (2 of 20) and 4% (1 of 23) magnesium recipients rated their cramps as moderate or severe (RR 0.43, 95% CI 0.04 to 4.44; 1 study, 43 participants; Analysis 1.10) (Garrison 2011a).
1.10. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 10: Cramp intensity (moderate or worse) at 12 weeks
Secondary outcome: cramp duration
Pregnancy‐associated cramps
None of the studies comparing magnesium to placebo in pregnant women recorded the duration of cramps.
Idiopathic rest cramps
At four weeks
Four idiopathic cramp trials measured cramp duration. Frusso 1999 used a four‐point ordinal scale divided into less than five minutes, 5 to 10 minutes, 10 to 30 minutes and over 30 minutes. Garrison 2011a used a three‐point ordinal scale divided into less than 1 minute, one to five minutes and over five minutes. Roffe 2002 used a three‐point ordinal scale divided into short, medium and long. Roguin Maor 2017 reported mean cramp duration in minutes. All four studies reported no statistically significant difference in duration. The single study that recorded duration using a one‐minute cut‐off found the mean percentage of placebo recipients with a majority of cramp durations of one minute or more to be 22.7% (Garrison 2011a). Five of 22 participants who received placebo and 10 of 24 participants who received magnesium experienced cramps lasting one minute or more. This favoured placebo (RR 1.83, 95% CI 0.74 to 4.53; 1 study, 46 participants; low‐certainty evidence due to imprecision; Analysis 1.11).
1.11. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 11: Cramp duration ≥ 1 minute at four weeks
At 12 weeks
The single study with 12‐week data found the placebo group to have 25% (5 of 20) of participants reporting the majority of their cramps as lasting one minute or more, compared to 39% (9 of 23 participants) in the magnesium group, which also favoured placebo (RR 1.57, 95% CI 0.63 to 3.91; 1 study, 43 participants; Analysis 1.12) (Garrison 2011a). The data were very imprecise.
1.12. Analysis.

Comparison 1: Magnesium versus placebo (idiopathic cramps): efficacy, Outcome 12: Cramp duration ≥ 1 minute at 12 weeks
Secondary outcome: treatment withdrawals due to adverse events
Most studies had omissions or inconsistencies which made the determination of the number of withdrawals due to adverse effects difficult. Because we believed that the difference in withdrawals due to adverse events and the difference in total withdrawals between groups would be estimating the same parameter, we used total withdrawals for each group whenever it was unclear how many participants withdrew due to adverse effects. Neither of the cross‐over studies could be used to estimate withdrawals due to adverse effects (Frusso 1999; Roffe 2002), since information on participant experience in each period was not available (i.e. would participants withdrawing in one period have also withdrawn in the other?). Although we had participant‐level data for Roffe 2002, we could not use data from the first period to estimate withdrawals, since the data provided to us only included participants completing both study periods. Determined in this way, and using only parallel studies, 13 of 206 magnesium‐treated participants and 11 of 204 placebo group participants withdrew. The percentage difference in withdrawals across all studies (which we presume to be due to adverse events) was slightly higher in the magnesium group compared to the placebo group (RR 1.17, 95% CI 0.56 to 2.47; 7 studies, 410 participants; Analysis 2.1).
2.1. Analysis.

Comparison 2: Magnesium versus placebo (pregnancy‐associated, idiopathic, and liver‐cirrhosis‐associated cramps): adverse effects, Outcome 1: Treatment withdrawals due to adverse events
Secondary outcome: minor adverse events
Adverse events were reported in most studies but usually not in a way that allowed us to determine the number of participants reporting minor adverse events. Some studies reported any adverse events, others reported only gastrointestinal adverse events.
Pregnancy‐associated cramps
In Nygaard 2008, six of 23 participants (26.1%) in the magnesium arm and six of 22 participants (27.3%) in the placebo arm reported adverse events which were lumped together as gastrointestinal in nature (nausea, flatulence, diarrhoea, intestinal air). Dahle 1995 only noted adverse events as being infrequent (without specifying placebo versus magnesium) and consisting of "primarily slight or initial nausea". In Supakatisant 2015, 16 of 43 participants (37.2%) in the magnesium arm and six of 43 participants (14.0%) in the placebo arm reported diarrhoea, nausea, or both.
Idiopathic rest cramps
Frusso 1999 reported diarrhoea, nausea or vomiting as occurring in 10.7% of magnesium recipients and 10.1% of placebo recipients. Roguin Maor 2017 reported minor adverse events (mostly gastrointestinal) in 14 of 48 participants (29.2%) receiving magnesium and 13 of 46 participants (28.3%) receiving placebo. Roffe 2002 and Garrison 2011a reported the number of participants with different specific side effects but not the number of participants with any side effect (i.e. the same participants may be counted more than once). In Roffe 2002, diarrhoea occurred in 30% on magnesium and 17% on placebo. Constipation occurred in 13% on magnesium and 24% on placebo. Nausea, indigestion or flatulence occurred in two magnesium and four placebo participants. Other side effects included skin peeling (one on magnesium), bruising (one on placebo) and headaches (one on placebo). Garrison 2011a was different, in that it was a study of magnesium given intravenously. Side effects included asymptomatic hypotension (reported by the study nurse) in three of 24 magnesium versus none of 22 placebo participants and facial flushing being noted in nine of 24 magnesium and seven of 22 placebo recipients but not generally complained of by participants. Two magnesium recipients noted transient light‐headedness several hours after the infusions on day three and day four and more magnesium recipients noted burning of the IV site (12 of 24 versus 0 of 22) with five of 24 magnesium participants receiving some piggybacked extra dilution of the IV solution to improve tolerability.
Liver‐cirrhosis‐associated cramps
In Cohen‐Hagai 2018, three of 14 (21.4%) magnesium recipients experienced diarrhoea bad enough to stop treatment, compared to none of 15 placebo recipients. No other specific adverse effects were described.
Pregnancy‐associated, idiopathic, and liver‐cirrhosis‐associated cramps combined
Overall, when we combined data from the four trials of oral magnesium reporting the number of participants with minor adverse events (Cohen‐Hagai 2018; Nygaard 2008; Roguin Maor 2017; Supakatisant 2015), 39 of 128 magnesium‐treated participants and 25 of 126 participants in the placebo group experienced minor adverse events, which was higher in the magnesium group (RR 1.51, 95% CI 0.98 to 2.33; I² = 28.9%; 4 studies, 254 participants; low‐certainty evidence due to imprecision and indirectness; Analysis 2.2).
2.2. Analysis.

Comparison 2: Magnesium versus placebo (pregnancy‐associated, idiopathic, and liver‐cirrhosis‐associated cramps): adverse effects, Outcome 2: Minor adverse events
Secondary outcome: major adverse effects
Pregnancy‐associated cramps
Nygaard 2008 reported no major adverse events during the study. The other studies do not state this outcome explicitly.
Idiopathic rest cramps
Garrison 2011a and Roffe 2002 both reported one stroke that occurred in the placebo arms but reported no other major adverse events. Roguin Maor 2017 reported four major adverse events (hospitalizations) during the treatment phase, two in each group. These data were not available from NCT00963638; and Frusso 1999 did not explicitly state whether major adverse events occurred. When we combined data from Garrison 2011a and Roguin Maor 2017, two of 95 magnesium‐treated participants and three of 90 placebo group participants experienced major adverse events, which was similar in both groups (RR 0.68, 95% CI 0.14 to 3.31; 2 studies, 140 participants; I² = 0%; very low certainty evidence; Analysis 2.3). Being a cross‐over trial without data on all participants for both periods, Roffe 2002 could not be combined in this analysis.
2.3. Analysis.

Comparison 2: Magnesium versus placebo (pregnancy‐associated, idiopathic, and liver‐cirrhosis‐associated cramps): adverse effects, Outcome 3: Major adverse events
Magnesium versus other treatments
Two trials in pregnant women compared magnesium with other treatments for pregnancy‐associated cramps. Sohrabvand 2006 compared no treatment to magnesium, calcium carbonate and a combined supplement of vitamins B₁ and B₆, and Shahraki 2006 compared magnesium to either a calcium or a vitamin E supplement.
Primary outcome: cramp frequency (percentage change from baseline at 4 weeks)
Pregnancy‐associated cramps
The two trials comparing magnesium to other treatments in pregnant women did not report the percentage reduction in the number of cramps (Shahraki 2006; Sohrabvand 2006).
Secondary outcome: cramp frequency (responder analysis)
Pregnancy‐associated cramps
The two trials comparing magnesium to other treatments in pregnant women did not provide the necessary data to calculate the percentage of participants with a 25% or more reduction in cramp frequency (Shahraki 2006; Sohrabvand 2006).
Secondary outcome: cramp frequency (number of cramps on treatment)
Pregnancy‐associated cramps
At four weeks
One study used four parallel treatment arms to compare no treatment with either 182 mg elemental magnesium twice daily (from magnesium aspartate), 500 mg of calcium carbonate once daily, or 100 mg of thiamine (vitamin B₁) combined with 40 mg of pyridoxine (vitamin B₆) once daily in a group of pregnant Iranian women (Sohrabvand 2006). This trial had an unusual design, with the intervention being given over two weeks but outcomes assessed over four weeks. The outcome for this study was "change in muscle spasms" on a three‐point ordinal scale of "no change", "relative improvement", and "absolute improvement." We clarified with the authors that this meant no improvement, partial resolution and complete resolution of cramping. A multinomial regression test was applied to each of the three possible response categories to see if any of the active treatment arms differed from no treatment. Significantly more women reported absolute improvement in both the B vitamin and calcium arms, but not in the magnesium arm. Neither was there a difference in relative improvement between no treatment and the magnesium arm. Comparisons between the active intervention arms were not made.
One 3‐arm study compared 8 mL of an 8% milk of magnesium suspension three times daily to either 100 mg of vitamin E once daily or 500 mg of calcium carbonate once daily in 120 pregnant women for 45 days (Shahraki 2006). This trial was considered at high risk of bias as a lot of information was unclear and data were not available for 30 of the 120 enrolled participants. Twenty of these participants were described as being excluded due to side effects, while another 10 appear unaccounted for. We sought more information by contacting the author but we got no response. They reported number of cramps per day at 45 days and not number of cramps per week at four or 12 weeks. The mean number of cramps per day in the milk of magnesium group went from 4.7 at baseline to 3.6 at 45 days. It is unclear if the difference was statistically significant. In participants using vitamin E and calcium carbonate, similar reductions in daily cramps were observed, with the mean number of cramps per day falling from 5.5 to 2.8 and from 4.9 to 3.6, respectively.
Secondary outcome: cramp intensity (pain scale)
Pregnancy‐associated cramps
None of the studies comparing magnesium to other treatments in pregnant women reported results that permitted cramp intensity to be determined as a continuous variable.
Secondary outcome: cramp intensity (moderate or worse)
Pregnancy‐associated cramps
In Shahraki 2006, cramp intensity was classified as low pain (1 to 5 on a 1 to 10 VAS) or high pain (6 to 10). The number of magnesium recipients with high pain went from 25 of 30 at baseline to 20 of 30 at day 45, as compared to vitamin E recipients (29 of 30 at baseline, 17 of 30 at day 45), and calcium carbonate recipients (29 of 30 at baseline, 23 of 30 day 45). Again, we considered this trial at high risk of bias and data are missing for 30 of the 120 enrolled participants. Patient‐level data was not available to convert to our three‐point intensity scale. Sohrabvand 2006 did not report cramp intensity.
Secondary outcome: cramp duration
Pregnancy‐associated cramps
Shahraki 2006 reported cramp duration in seconds. At 45 days, participants receiving magnesium recorded a mean reduction in cramp duration of 6.8 seconds. It was not clear if this result was statistically significant but it is likely not clinically important. Sohrabvand 2006 did not report cramp duration.
Secondary outcome: treatment withdrawals due to adverse events
Pregnancy‐associated cramps
Treatment withdrawals due to adverse events could be calculated from the two trials comparing magnesium to different treatments in pregnant women. Of these, one trial did not report any treatment withdrawal or adverse event (Sohrabvand 2006), and the other reported some withdrawals and some adverse events, but there is no information regarding at least 10 participants who were not included in the analysis (Shahraki 2006).
Secondary outcome: minor adverse events
Pregnancy‐associated cramps
Adverse events were not reported in the two trials comparing magnesium to other treatments in pregnant women.
Secondary outcome: major adverse effects
Pregnancy‐associated cramps
Adverse events were not reported in the two trials comparing magnesium to other treatments in pregnant women.
Discussion
Summary of main results
We identified 11 trials (9 parallel‐group, 2 cross‐over) enrolling a total of 735 individuals, amongst whom 118 cross‐over participants additionally served as their own controls. Our main findings are as follows.
Magnesium versus placebo
Idiopathic rest cramps
There is moderate‐certainty evidence that magnesium supplementation does not offer a clinically important benefit over placebo in the prophylaxis of idiopathic cramps in older adults (most of whom are presumed to have been experiencing nocturnal leg cramps). The difference in percentage change in cramps per week from baseline at four weeks was small and the CI excluded a 25% reduction (the difference we predefined as being clinically important). In addition, while medications are often only effective in a subset of participants, the percentage of participants obtaining a 25% or greater reduction from baseline in the number of cramps per week at four weeks was similar in both groups. This makes it less likely that a meaningful subset of participants receiving a greater than 25% benefit is being missed by averaging their results in with non‐responders. Cramp frequency was also measured looking at the number of cramps per week on treatment at four weeks. This measure allowed pooling of the largest number of studies (five studies, 307 participants) and similarly found no evidence of a difference in the change in cramps per week on treatment with a CI that excluded a 'one cramp per week' reduction.
Similarly, there is moderate‐certainty evidence that cramp intensity is no different in magnesium recipients than in placebo participants, whether measured on a three‐point pain scale at four weeks, or by examining the number of participants rating their cramps as moderate or severe. Only one study reported cramp duration in a format that allowed us to determine the number of participants with the majority of cramp durations longer than one minute. In this study, the mean percentage of participants having the majority of their cramp durations lasting one minute or longer was slightly higher in the magnesium group than the placebo group (low‐certainty evidence). Three other studies reported cramp duration in different formats and in none was there a significant difference. We also sought all the above outcomes at 12 weeks but only one study had 12‐week data. The results of this single study at 12 weeks were not materially different from the four‐week results above.
Pregnancy‐associated cramps
According to three discordant studies that we could not pool (very low certainty evidence), it is unclear whether magnesium supplementation can provide an advantage over placebo in the prophylaxis of pregnancy‐associated cramps. Dahle 1995 reported a reduction in cramp frequency on a five‐point ordinal scale, a reduction in cramp intensity on a VAS, and a more favourable global assessment of treatment effect also on a five‐point ordinal scale. In contrast, the subsequent trial measured the mean number of days and nights with leg cramps present and found no benefit (7.7 ± 4.7 (SD) days and nights of cramping over two weeks in the placebo group and 9.5 ± 5.1 in the magnesium group; P = 0.27) (Nygaard 2008). Nor was there evidence of a difference in cramp intensity (on a 5‐point ordinal scale). The most recent study reported benefit, but the results provided appear contradictory (Supakatisant 2015). Specifically, this study reported 1) a higher percentage reduction in the number of cramps per week at four weeks among magnesium recipients compared to placebo (79.0% versus 32.4%; P = 0.003); and 2) a higher proportion of participants reporting at least a 50% reduction in cramp frequency (86.0% versus 60.5%; P = 0.007), but simultaneously reported (confirmed with the trial author) that the median number of cramps per week increased in both the magnesium and placebo groups (which is not compatible with the large reported percentage reductions).
Two of these trials were parallel double‐blind RCTs in women attending Scandinavian maternity clinics and used the same intervention, a chewable tablet containing 122 mg elemental magnesium "primarily as Mg lactate or Mg citrate" taken once each morning and twice each evening (366 mg daily). Despite these similarities, they were discrepant (Dahle 1995; Nygaard 2008). Factors which might have prevented Nygaard 2008 from showing benefit include less power (although there was not even a trend to benefit) due to fewer participants (45 versus 73), a shorter period of therapy (two weeks versus three) and the lack of baseline measures of cramp frequency. The lack of baseline measures is particularly important, since the outcome was the number of cramps during the treatment period and it is not known if the mean baseline cramp rates were equal. Conversely, the trial design of Dahle 1995 might have biased towards benefit in that outcomes were not well defined (in particular no primary outcome was identified), randomization and allocation concealment were not described and no cramp diary was used. Of these, the only trial not judged to be at high risk of bias is Nygaard 2008, which found not even a trend to benefit for magnesium.
Liver‐cirrhosis‐associated cramps
The single study of magnesium in people with liver cirrhosis reported results on only 22 participants, and only about 82% of those participants were experiencing muscle cramps at baseline. Although the trial reported that no statistically significant difference in cramp frequency or cramp intensity was observed, the focus of this study was on other issues (primarily cognitive changes), it was at high risk of bias because of a per protocol analysis and a large imbalance in dropouts (42.8% dropping out of the magnesium group compared to 6.7% dropping out from the placebo group), and it was likely underpowered for this outcome. As a result, we could draw no conclusions regarding the utility of magnesium to reduce the burden of muscle cramps in people with liver cirrhosis.
Adverse events
Adverse events and withdrawals due to adverse events were poorly reported in most trials. When combining data from all trials comparing magnesium to placebo and supplementing the number of withdrawals due to adverse events with total withdrawals, we found no difference for the number of withdrawals due to adverse events. Three major adverse events (strokes or hospitalizations) were reported in the placebo groups (90 participants) and two in the magnesium group (95 participants). However, in the four of eight trials comparing oral magnesium to placebo that had relevant data, minor adverse effects were more common in the magnesium group. Qualitatively it appears that side effects while on oral magnesium are mostly gastrointestinal (e.g. diarrhoea), and common, ranging from 11% (10% in control) to 37% (14% in control) of participants. Intravenous magnesium appeared to cause a burning sensation at the IV site in half of participants (compared to none in the placebo group) and a small subset of participants had either asymptomatic hypotension or light‐headedness.
Magnesium versus other treatments
Pregnancy‐associated cramps
Two trials used a comparator other than placebo. Sohrabvand 2006 used four parallel treatment arms to compare no treatment with either oral magnesium, calcium carbonate or a combined vitamin B₁ and B₆ supplement. The outcome for this study was the participants' reporting of either no improvement, partial resolution or complete resolution of cramping. A multinomial regression test was applied to each of the three possible response categories to see if any of the active treatment arms differed from no treatment. Significantly more women reported absolute improvement in the B vitamin and calcium arms, but not in the magnesium arm. Neither was there a significant difference in relative improvement between the no treatment and the magnesium arm. Comparisons between the active intervention arms were not made. It would not be unusual for placebo to show benefit from baseline in cramp trials. One might speculate that the same 'placebo effect' benefit might be seen for any active intervention over no treatment, which makes the benefit seen for B vitamins and calcium over no treatment in this trial unreliable. Magnesium was certainly no better than calcium or vitamin B supplements, however, and was alone in not reaching significance for benefit against no treatment. Collectively, these results do not support a clinically important benefit for magnesium over no treatment. Shahraki 2006 compared magnesium to vitamin E or calcium carbonate in pregnant women for 45 days. This trial was at high risk of bias because of lack of blinding and what appeared to be a per protocol analysis. An improvement in the number of cramps per day over time was reported for the magnesium group but was not larger than the improvement seen in vitamin E or calcium carbonate recipients. Neither did the magnesium group outperform vitamin E or calcium carbonate at lowering cramp intensity or reducing cramp duration. The results of this study are hard to interpret but they do not suggest a clinically important benefit.
Effect of dose, duration and route of administration
Serum magnesium levels are known to correlate poorly with tissue magnesium, making it difficult to detect participants with magnesium deficiency in the clinic. In theory, if magnesium deficiency played a role in skeletal muscle cramping, either the duration of therapy or the total dose provided over the course of the trial might be an important variable (since a deficit might be better replaced in longer duration, higher total dose trials). The differences in dosing and duration for the oral magnesium trials is modest, with the idiopathic rest cramp trials using 200 mg to 520 mg of elemental magnesium daily over four to six weeks and the pregnancy‐associated cramp trials using 300 to 802 mg per day over 14 to 45 days. Overall, no obvious dose response is present, although the oral trials may be too few and too close in dose and duration to be able to detect any meaningful pattern. However, one trial used a series of slow IV infusions of magnesium to improve delivery and simultaneously measured 24‐hour urinary magnesium excretion to determine the extent to which participants were retaining magnesium (Garrison 2011a). Measuring the percentage retention of the infused magnesium was felt to be important because it had been used as a tool to predict total body magnesium deficiency (retention of magnesium suggesting the presence of deficiency) (al‐Ghamdi 1994; Cohen 1990; Lim 1972; Quamme 1993; Ryzen 1985), and because there is a strong positive correlation between the total amount of IV magnesium retained during replacement therapy and the rise in intracellular magnesium on skeletal muscle biopsy (Lim 1972). In this trial of IV magnesium, no correlation was found between per cent retention of magnesium on day one of infusions and the reduction in the number of cramps per week from baseline. On its own, this finding argues against a therapeutic benefit from magnesium in providing cramp prophylaxis.
Overall completeness and applicability of evidence
Idiopathic cramp sufferers are often older adults with rest cramps ‒ individuals who typically wake from sleep with cramps in the lower limbs. In our experience, this is the commonest presentation of muscle cramping in a primary care population. For this large subgroup of cramp sufferers we can say with moderate certainty that magnesium is unlikely to provide a meaningful clinical benefit. In contrast, the evidence for those with pregnancy‐associated cramps and liver‐cirrhosis‐associated cramps is far from clear, and there is no evidence for the role of magnesium in treating cramps associated with exercise or other medical conditions (e.g. motor neuron disease or renal failure).
Quality of the evidence
Idiopathic rest cramps
We identified five trials of idiopathic rest cramps (313 participants including useable cross‐over controls). The largest amount of poolable data (all five trials) was available to estimate the number of cramps per week at four weeks. In this analysis, the mean difference compared to placebo was clinically unimportant (−0.02 cramps per week), the CI excluded a 'one cramp per week' reduction, and there was no heterogeneity (I² = 0). Risk of bias was low overall for three of the five studies we combined for this analysis, and risk was mitigated for one of the two studies at high risk by using only the first study period. Concordant results were obtained for other measures of cramp frequency, including our primary outcome (per cent change from baseline in the number of cramps per week) whose 95% CI excluded the 25% reduction we had predefined as clinically important. We did not downgrade the responder analysis but did downgrade the number of cramps per week on treatment (due to inconsistency) and the percentage change from baseline (due to imprecision), providing moderate‐certainty evidence for each. We similarly found no difference in cramp intensity when examining the number of participants with moderate or worse cramps (2 studies, 91 participants, downgraded to moderate‐certainty evidence due to imprecision). And we found no difference in cramp duration when measured as cramps lasting one minute or more (1 study, 43 participants, downgraded to low‐certainty evidence due to very serious imprecision).
Pregnancy‐associated cramps
We considered all but one of the five pregnancy‐associated cramp trials to be at high risk of bias; and none measured frequency, intensity, or duration in a way that permitted us to pool data. Trial results were discrepant. Of the three trials comparing magnesium to placebo, two trials reported benefit (Supakatisant 2015; Dahle 1995), but each had inconsistency in how cramp frequency was being reported. The one trial at low overall risk of bias reported not even a trend to benefit for its frequency measure (Nygaard 2008), and the two trials comparing magnesium to other treatments (which included calcium, B vitamins, vitamin E, and no treatment), found magnesium to be no better than any of the other treatment arms (Shahraki 2006; Sohrabvand 2006). Given results were discrepant, and given the studies did not report results in a way that permitted pooling of data, we were unable to produce a meaningful estimate of effect.
Liver‐cirrhosis‐associated cramps
The single study in people with liver cirrhosis was underpowered, at high risk of bias, and did not report results in a way that allowed us to calculate any of our pre‐defined outcomes. Hence we were unable to provide a meaningful estimate of effect.
Adverse events
Only two studies (140 participants) reported major adverse events, for which we downgraded the evidence to low certainty because of very serious imprecision. Four studies (254 participants) reported the number of participants with minor adverse effects but we downgraded the evidence to low because of imprecision and indirectness (due to combining trials with multiple clinical presentations).
Potential biases in the review process
Data were available from all relevant RCTs identified for inclusion in this trial. This includes participant‐level data for three of the five trials of magnesium for idiopathic cramps in older adults, including one cross‐over trial from which we used participant‐level data (by looking at the first period only) to reduce potential bias from an unbalanced randomization and a strong treatment‐order effect (Roffe 2002). Although we were able to identify one relatively recent (2011) unpublished trial using a clinical trial registry (NCT00963638), we could be missing other unpublished RCTs that predate trial registration. However, we would expect such missing trials to be less likely to have demonstrated a significant benefit because of publication bias. All of the included trials were fairly small, ranging from 29 to 120 participants, and all had some degree of methodological limitations (Figure 3). However, heterogeneity was low whenever studies could be pooled.
Agreements and disagreements with other studies or reviews
We have found that magnesium is unlikely to provide meaningful cramp prevention to older adults (the majority of cramp sufferers), but that its role in the prophylaxis of pregnancy‐associated cramps is unclear. These are effectively the same conclusions reached in other systematic reviews, including one systematic review examining magnesium for the prevention of muscle cramps in any clinical setting (Sebo 2014), and one systematic review examining any treatments for pregnancy‐associated cramps (Zhou 2015). Although we did not attempt a systematic review of non‐randomized studies, we also know our results to be consistent with a survey in which cramp sufferers were asked to rate the effectiveness of any treatments they had tried. In that survey quinine, an agent with modest established benefit, was found to be "quite helpful", "very helpful", or "100% effective" by 16 of 18 respondents (89%), and found to be "a little help" or "useless" by 2 of 18 (11%). In comparison, magnesium was found to be "quite helpful", "very helpful", or "100% effective" by only 16 of 44 respondents (36%), and found to be "a little help" or "useless" by 28 of 44 (64%) (Blyton 2012).
Authors' conclusions
Implications for practice.
It is unlikely that magnesium supplementation provides clinically meaningful cramp prophylaxis for idiopathic skeletal muscle cramps, largely in older adults, at any of the dosages used. This is supported by evidence of moderate certainty. In contrast, for women suffering pregnancy‐associated rest cramps the literature is of lower certainty, conflicting, and unclear. No RCTs evaluating magnesium for exercise‐associated muscle cramps or disease‐state‐associated muscle cramps have been conducted other than a single trial in people with liver cirrhosis, whose small size and method of reporting prevent us drawing conclusions.
Implications for research.
Given the low probability of benefit for idiopathic skeletal muscle cramps in older adult cramp sufferers, investigators may be less inclined to pursue the evaluation of magnesium for other cramp indications. There is, however, conflicting evidence surrounding the benefit of magnesium for pregnancy‐associated leg cramps and it is conceivable that magnesium could have differing efficacies in metabolically distinct populations. To resolve the uncertainty surrounding the role of magnesium in pregnant women, parallel‐group, blinded, placebo‐controlled RCTs of magnesium in that population are needed. The same is true for those with exercise or disease‐state‐associated cramps. Trialists should measure cramp rates as a continuous variable (for example number of cramps on treatment or change from baseline) to permit pooling of data. If not using change from baseline, they should also consider stratifying the study randomization by baseline cramp rate to help prevent an unequal distribution of cramp frequencies invalidating their findings.
What's new
| Date | Event | Description |
|---|---|---|
| 2 December 2019 | New search has been performed | We added 4 new studies (1 idiopathic cramp trial, 1 liver‐cirrhosis‐associated cramp trial, and 2 pregnancy‐associated cramp trials). We also made a correction to the data entered into the meta‐analysis of cramp intensity and number of cramps per week at 4 weeks for 1 study (specifically, for Frusso 1999, our calculation of MD and SED for these outcomes in the original review was in error). The description of how cramp intensity was analysed in the Methods section was altered to be more explicit, but no changes were made to how data were analysed other than the conversion of risk differences (used in the original review for dichotomous outcomes) to risk ratios. We made this change recognizing risk ratios to be more generalizable. |
| 2 December 2019 | New citation required and conclusions have changed | We upgraded the certainty of evidence for two outcomes as a result of more data. The review includes new inconclusive data on cramps in people with liver cirrhosis. Christina S Korowny, Michael R Kolber and Nicolas Dugré joined the review team, Karim M Khan withdrew. |
History
Protocol first published: Issue 11, 2011 Review first published: Issue 9, 2012
Acknowledgements
This project was supported by the National Institute for Health Research (NIHR) via Cochrane Infrastructure funding to Cochrane Neuromuscular. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, UK National Health Service or the UK Department of Health. Cochrane Neuromuscular is also supported by the MRC Centre for Neuromuscular Disease and the Motor Neuron Disease Association.
Appendices
Appendix 1. Cochrane Neuromuscular Specialised Register via the Cochrane Register of Studies (CRS‐Web)
Search date 9 September 2019
#1 (muscle NEAR cramp*) or (muscle NEAR spasm*) or (muscle NEAR contraction*) or (leg NEAR cramp*) AND INREGISTER #2 (charley NEXT horse) or (charlie NEXT horse) or eamc AND INREGISTER #3 #1 or #2 AND INREGISTER #4 magnesium or mg2 AND INREGISTER #5 #3 and #4 AND INREGISTER
Appendix 2. Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Register of Studies (CRS‐Web)
Search date 9 September 2019
#1 (muscle NEAR cramp*) or (muscle NEAR spasm*) or (muscle NEAR contraction*) or (leg NEAR cramp*) AND CENTRAL:TARGET #2 (charley NEXT horse) or (charlie NEXT horse) or eamc AND CENTRAL:TARGET #3 #1 or #2 AND CENTRAL:TARGET #4 magnesium or mg2 AND CENTRAL:TARGET #5 #3 and #4 AND CENTRAL:TARGET
Appendix 3. MEDLINE (OvidSP) search strategy
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations and Daily <1946 to September 06, 2019> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 randomized controlled trial.pt. (488816) 2 controlled clinical trial.pt. (93272) 3 randomi#ed.tw. (584203) 4 placebo.ab. (200564) 5 drug therapy.fs. (2137026) 6 randomly.ab. (317666) 7 trial.ab. (475671) 8 groups.ab. (1951309) 9 or/1‐8 (4543002) 10 exp animals/ not humans.sh. (4615941) 11 9 not 10 (3935351) 12 (muscle cramp$ or muscle spasm$).mp. (4794) 13 leg cramp$.mp. (436) 14 Muscle Contraction$.mp. (104761) 15 (charley horse$ or charlie horse$).mp. (8) 16 eamc.mp. (30) 17 exercise associated muscle cramp$.mp. (55) 18 or/12‐17 (109586) 19 (magnesium or mg2).mp. (123224) 20 11 and 18 and 19 (122) 21 remove duplicates from 20 (122)
Appendix 4. Embase (OvidSP) search strategy
Database: Embase <1974 to 2019 September 06> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 crossover‐procedure/ (60604) 2 double‐blind procedure/ (165321) 3 randomized controlled trial/ (569054) 4 single‐blind procedure/ (36509) 5 (random$ or factorial$ or crossover$ or cross over$ or cross‐over$ or placebo$ or (doubl$ adj blind$) or (singl$ adj blind$) or assign$ or allocat$ or volunteer$).tw. (2117260) 6 or/1‐5 (2214070) 7 exp animals/ (24642639) 8 exp humans/ (20126777) 9 7 not (7 and 8) (4515862) 10 6 not 9 (2004984) 11 limit 10 to (conference abstracts or embase) (1680085) 12 (muscle cramp$ or muscle spasm$ or muscle contraction$ or leg cramp$).mp. (112258) 13 (charley horse$ or charlie horse$).mp. (12) 14 eamc.mp. (50) 15 exercise associated muscle cramp$.mp. (63) 16 or/12‐15 (112282) 17 (magnesium or mg2).mp. (167959) 18 11 and 16 and 17 (112) 19 remove duplicates from 18 (111)
Appendix 5. AMED (OvidSP) search strategy
Database: AMED (Allied and Complementary Medicine) <1985 to August 2019> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 Randomized controlled trials/ (2251) 2 Random allocation/ (323) 3 Double blind method/ (732) 4 Single‐Blind Method/ (137) 5 exp Clinical Trials/ (4110) 6 (clin$ adj25 trial$).tw. (7582) 7 ((singl$ or doubl$ or treb$ or trip$) adj25 (blind$ or mask$ or dummy)).tw. (3187) 8 placebos/ (626) 9 placebo$.tw. (3396) 10 random$.tw. (19575) 11 research design/ (2003) 12 Prospective Studies/ (1320) 13 meta analysis/ (299) 14 (meta?analys$ or systematic review$).tw. (4280) 15 control$.tw. (38515) 16 (multicenter or multicentre).tw. (1127) 17 ((study or studies or design$) adj25 (factorial or prospective or intervention or crossover or cross‐over or quasi‐experiment$)).tw. (14048) 18 or/1‐17 (59676) 19 (cramp$ or spasm$ or contraction$).mp. (7207) 20 leg cramp$.mp. (6) 21 (charley horse$ or charlie horse$).mp. (0) 22 eamc.mp. (1) 23 exercise associated muscle cramp$.mp. (3) 24 or/19‐23 (7207) 25 (magnesium or mg2).mp. (300) 26 18 and 24 and 25 (1)
Appendix 6. LILACS (IAHx) search strategy
("muscle cramp" or "muscle cramps" or "Calambre Muscular" or "caibra muscular" or "muscle spasm" or espasmo or "muscle contraction" or "muscle contractions" or "Contraccion Muscular" or "Contracao Muscular" or "charley horse" or "charlie horses" or eamc) and (magnesium or mg2 or magnesio) and ((PT:"Randomized Controlled Trial" or "Randomized Controlled trial" or "Ensayo Clínico Controlado Aleatorio" or "Ensaio Clínico Controlado Aleatório" or PT:"Controlled Clinical Trial" or "Ensayo Clínico Controlado" or "Ensaio Clínico Controlado" or "Random allocation" or "Distribución Aleatoria" or "Distribuição Aleatória" or randon$ or Randomized or randomly or "double blind" or "duplo‐cego" or "duplo‐cego" or "single blind" or "simples‐cego" or "simples cego" or placebo$ or trial or groups) AND NOT (B01.050$ AND NOT (humans or humanos or humanos)))
Appendix 7. CINAHL Plus (EBSCOhost) search strategy
Monday, September 09, 2019 6:14:05 AM S25 S24 Limiters ‐ Exclude MEDLINE records 2 S24 S18 AND S22 AND S23 27 S23 magnesium or mg2 7,122 S22 S19 OR S20 OR S21 12,659 S21 eamc or exercise associated muscle cramp* 45 S20 charley horse* or charlie horse* 9 S19 muscle cramp* or muscle spasm* or muscle contraction* or leg cramp* 12,654 S18 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 1,265,664 S17 ABAB design* 121 S16 TI random* or AB random* 299,975 S15 ( TI (cross?over or placebo* or control* or factorial or sham? or dummy) ) or ( AB (cross?over or placebo* or control* or factorial or sham? or dummy) ) 598,165 S14 ( TI (clin* or intervention* or compar* or experiment* or preventive or therapeutic) or AB (clin* or intervention* or compar* or experiment* or preventive or therapeutic) ) and ( TI (trial*) or AB (trial*) ) 232,078 S13 ( TI (meta?analys* or systematic review*) ) or ( AB (meta?analys* or systematic review*) ) 85,305 S12 ( TI (single* or doubl* or tripl* or trebl*) or AB (single* or doubl* or tripl* or trebl*) ) and ( TI (blind* or mask*) or AB (blind* or mask*) ) 45,661 S11 PT ("clinical trial" or "systematic review") 166,177 S10 (MH "Factorial Design") 1,140 S9 (MH "Concurrent Prospective Studies") or (MH "Prospective Studies") 393,630 S8 (MH "Meta Analysis") 39,743 S7 (MH "Solomon Four‐Group Design") or (MH "Static Group Comparison") 98 S6 (MH "Quasi‐Experimental Studies") 11,191 S5 (MH "Placebos") 11,446 S4 (MH "Double‐Blind Studies") or (MH "Triple‐Blind Studies") 42,475 S3 (MH "Clinical Trials+") 266,257 S2 (MH "Crossover Design") 17,918 S1 (MH "Random Assignment") or (MH "Random Sample") or (MH "Simple Random Sample") or (MH "Stratified Random Sample") or (MH "Systematic Random Sample") 93,653
Appendix 8. SPORTDiscus (EBSCOHost) search strategy
Monday, September 09, 2019 7:04:08 AM Database – SPORTDiscus with Full Text S11 S5 and S9 and S10 Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 15 S10 magnesium or mg2 Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 1,465 S9 S6 or S7 or S8 Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 24,131 S8 eamc Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 45 S7 charley horse* or charlie horse* Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 40 S6 cramp* or spasm* or contraction* Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 24,097 S5 S1 or S2 or S3 or S4 Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 166,499 S4 cross?over or placebo* or control* or factorial or sham? or dummy Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 153,549 S3 (single* or doubl* or tripl* or trebl*) and (blind* or mask*) Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 8,274 S2 clinical trial* Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 16,100 S1 randomi* Expanders ‐ Apply equivalent subjects Search modes ‐ Boolean/Phrase 30,845
Appendix 9. ClinicalTrials.gov search strategy
Advanced search
Condition: cramp
Study type: interventional
Intervention: magnesium
Appendix 10. WHO trials registry (ICTRP) search strategy
Advanced search
Condition: cramp
Intervention: magnesium
Recruitment status: all
Data and analyses
Comparison 1. Magnesium versus placebo (idiopathic cramps): efficacy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Cramp frequency (percentage change from baseline at four weeks) | 3 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐9.59 [‐23.14, 3.97] |
| 1.2 Cramp frequency (percentage change from baseline at 12 weeks) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐12.09 [‐40.22, 16.04] |
| 1.3 Cramp frequency (responder analysis at four weeks) | 3 | 177 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.84, 1.29] |
| 1.4 Cramp frequency (responder analysis at 12 weeks) | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.70, 2.10] |
| 1.5 Cramp frequency (number of cramps per week at four weeks) | 5 | 307 | Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.84, 0.49] |
| 1.6 Cramp frequency (number of cramps on treatment at 12 weeks) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐0.84 [‐3.23, 1.55] |
| 1.7 Cramp intensity (pain scale) at four weeks | 4 | 269 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.16, 0.12] |
| 1.8 Cramp intensity (pain scale) at 12 weeks | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.55, 0.19] |
| 1.9 Cramp intensity (moderate or worse) at four weeks | 2 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.81, 2.21] |
| 1.10 Cramp intensity (moderate or worse) at 12 weeks | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.04, 4.44] |
| 1.11 Cramp duration ≥ 1 minute at four weeks | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.74, 4.53] |
| 1.12 Cramp duration ≥ 1 minute at 12 weeks | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [0.63, 3.91] |
Comparison 2. Magnesium versus placebo (pregnancy‐associated, idiopathic, and liver‐cirrhosis‐associated cramps): adverse effects.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Treatment withdrawals due to adverse events | 7 | 410 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.56, 2.47] |
| 2.1.1 Idiopathic cramps (largely older adults) | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.34, 4.32] |
| 2.1.2 Pregnancy‐associated leg cramps | 3 | 201 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.09, 1.50] |
| 2.1.3 Liver‐cirrhosis‐associated cramps | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.43 [0.88, 46.92] |
| 2.2 Minor adverse events | 4 | 254 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.98, 2.33] |
| 2.2.1 Idiopathic cramps (largely older adults) | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.55, 1.95] |
| 2.2.2 Pregnancy‐associated leg cramps | 2 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.80 [0.97, 3.34] |
| 2.2.3 Liver‐cirrhosis‐associated cramps | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.47 [0.42, 132.78] |
| 2.3 Major adverse events | 3 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.14, 3.31] |
| 2.3.1 Idiopathic cramps (largely older adults) | 2 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.14, 3.31] |
| 2.3.2 Pregnancy‐associated leg cramps | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cohen‐Hagai 2018.
| Study characteristics | ||
| Methods | Double‐blind, parallel‐group RCT | |
| Participants | 29 adults (mean age 62.0 years) attending Israeli outpatient clinics with liver cirrhosis (mainly from viral hepatitis and non‐alcoholic fatty liver disease) and no hepatic encephalopathy | |
| Interventions | Either 520 mg magnesium oxide daily versus identical‐appearing placebo tablets. Presumably given for the full 8‐week observation period, although this is not explicitly stated | |
| Outcomes | Primary outcome not explicitly stated but study appears focused on measures of cognition Secondary outcomes are drawn from a "quality of life questionnaire that included eight parameters including fatigue level, concentration ability, frequency of muscle cramps, and daily physical performance" |
|
| Conflicts of interest | Conflicts of interest not reported | |
| Funding | Funding not reported. However, does say investigator‐initiated, so possibly independent funding | |
| Notes | Published. Participants recruited between November 2013 and January 2014 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Process not described but says randomized |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Matched placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not described. Probably adequate |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of the 29 participants enrolled, only 22 completed the trial, 8 in the intervention group and 14 in the placebo group. This imbalance resulted from 6 participants dropping out of the magnesium group (42.8%), while only 1 participant dropped out of the placebo group (6.7%). Only a per protocol analysis is carried out |
| Selective reporting (reporting bias) | High risk | Regarding cramps: the authors state that they are collecting cramp frequency and cramp pain ‒ but report only that "Improvement in the severity and frequency of muscle cramps was not significant (P = 0.438 and 0.483, respectively)." The only numbers which are reported pertain to whether muscle cramps are occurring ‒ with percentages given for each group and a nonsignificant statistical test being indicated. An e‐mail request was sent to the authors asking for more information but no response was obtained |
| Cramp diary (recall bias) | Unclear risk | It is not stated whether or not a cramp diary was used ‒ but this seems unlikely as cramping was not the focus of the study |
| Other bias | Low risk | No obvious other bias |
Dahle 1995.
| Study characteristics | ||
| Methods | Double‐blind, parallel‐group RCT | |
| Participants | 73 pregnant women (mean 29 wk gestation) with rest cramps and no previous cramp treatment. Recruitment from Swedish prenatal care clinics | |
| Interventions | Either a chewable tablet containing 122 mg elemental magnesium ("primarily as Mg lactate or Mg citrate") (n = 34), or matched placebo tablet (n = 35), taken once each morning and twice each evening for 3 weeks | |
| Outcomes | Primary outcome unclear Change in cramp frequency on a 5‐point ordinal scale Time of day cramps occurred on a 4‐point nominal scale Presence of symptoms the day after a night of cramping on a 3‐point ordinal scale Global participant assessment of treatment effect on a 5‐point ordinal scale Cramp intensity on a VAS Serum magnesium and calcium and 24‐hour urinary magnesium and calcium excretion |
|
| Conflicts of interest | No mention of conflicts of interest | |
| Funding | Manufacturer sponsored | |
| Notes | Published. Laboratory tests performed at only 1 of the 2 centres. The period during which the trial was conducted is not stated (first received by publisher 2 August 1994). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were then randomly allocated to either magnesium or placebo". No further description |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “A magnesium‐placebo tablet batch of 90 numbered bottles was prepared by ACO Lakemedel...” Comment: probably satisfactory, although pills were not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcomes measured via an interview. No information available regarding blinding of interviewers but study mentions double‐blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4/73 participants dropped out of the study and were excluded from the analysis. Reasons for dropout were well described but treatment group was not identified. 1 placebo participant withdrew from treatment but appears (unclear) to have been included in the analysis. Comment: probably adequate as total number of dropouts was small |
| Selective reporting (reporting bias) | High risk | No description of outcomes by primary and secondary, and outcomes were incompletely described in methods, i.e. only in the results is it evident that before and after comparisons, mean differences and numbers attaining specific cut‐offs are used. Unclear how well outcomes were predefined. Inadequate reporting: no actual numbers for many P values. This study also reported a reduction in cramp frequency "from the initial average of every other day, to every 3 days in the placebo group and one to two times a week in the magnesium group (P < 0.05)". However, "every 3 days" and "one to two times a week" do not belong to the 5‐point ordinal scale used to measure this outcome (daily, every other day, twice a week, once a week, never) |
| Cramp diary (recall bias) | High risk | No diary used |
| Other bias | Low risk | Participants treated differently at each site (1 used laboratory testing, the other did not). Likely not an important difference |
Frusso 1999.
| Study characteristics | ||
| Methods | Double‐blind RCT of cross‐over design | |
| Participants | 45 non‐pregnant rest cramp sufferers > 18 years (mean age 61.6 years) having a normal neurologic exam and at least 6 leg cramps in a 4‐week placebo run‐in. Recruitment from a single large university‐based Argentinean family practice clinic | |
| Interventions | Magnesium citrate 900 mg pill (approximately 100 mg elemental magnesium) (n = 45) twice daily or similar‐tasting and appearing placebo (n = 45), each for 4 weeks. 4‐week placebo run‐in and 4‐week washout between treatments | |
| Outcomes | Primary: number of cramps in treatment period Secondary:
|
|
| Conflicts of interest | No mention of conflicts of interest | |
| Funding | Independent funding | |
| Notes | Published. The 4‐week placebo run‐in was pre‐randomization. Unclear what the range for the analog scale of intensity is (assumed 0 to 10). Cramp duration was recorded by ordinal category but reported with a mean and standard deviation in minutes. Conducted from March 1996 to March 1997 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Patients randomly received magnesium or placebo...” Comment: unclear how randomization was performed |
| Allocation concealment (selection bias) | Unclear risk | Quote: “The codes were inside a sealed envelope opened at the end of the analysis.” Comment: unclear who allocated participants and maintained the blinding |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Each pill contained 900 mg of magnesium citrate or matched placebo (same appearance and taste).” Comment: satisfactory blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes measured via diaries completed by participants blind to the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3/45 participants withdrew with reasons given. Report does not state which intervention participants were receiving at the time or how their data were dealt with. Comment: probably satisfactory as the number of dropouts was small |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting for clinical endpoints (although urine for magnesium was collected and not reported). Duration of cramps was measured on a 4‐point ordinal scale but results were reported with the mean duration and standard deviation measured in minutes as though they were a continuous variable |
| Cramp diary (recall bias) | Low risk | Diary used |
| Other bias | Low risk | No obvious other bias |
Garrison 2011a.
| Study characteristics | ||
| Methods | Double‐blind, parallel‐group RCT | |
| Participants | 46 non‐pregnant rest cramp sufferers (mean age 69.3 yrs) with at least 8 cramps in a 30 day baseline diary. Recruitment from posters and pamphlets in 21 Canadian (Richmond, British Columbia) family practitioner offices and also by newspaper advertisement | |
| Interventions | 5 days consecutive 4‐hour IV infusions of 250 ml 5% dextrose in water either with 20 mmol of magnesium sulphate (treatment group) (n = 24) or without magnesium sulphate (control group) (n = 22) (20 mmol magnesium sulphate = 486 mg elemental magnesium) |
|
| Outcomes | Primary: Change in the number of cramps per week from baseline at 30 days Secondary:
|
|
| Conflicts of interest | No mention of conflict of interest | |
| Funding | Independent funding | |
| Notes | Published. Conducted from January 2007 to October 2008 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization, using a computer generated random allocation sequence without any blocking or stratification was carried out by the hospital pharmacist dispensing the study drugs according to a series of opaque allocation envelopes kept in the pharmacy." Comment: satisfactory randomization |
| Allocation concealment (selection bias) | Low risk | Quote: "All investigators, study nurses and subjects were blinded as to treatment allocation." Comment: satisfactory allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: 1) "Active and Placebo solutions were indistinguishably clear and colorless." 2) "Subjects had been told that IV site discomfort was possible with both placebo and Mg infusions. While generally it was considered that blinding was reasonable, the sensation of burning at the IV site, coupled with the additional saline dilution in some Mg participants, could have compromised the blind to some extent (presumably favouring the intervention)." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Diary completed by participants blinded to the intervention but blinding to the intervention was at an unclear risk of bias. To avoid compromising the blind, all participants underwent urine collection identically, and results of urine testing (along with baseline serum Mg) were sequestered from investigators until trial completion. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts or losses to follow‐up. ITT analysis |
| Selective reporting (reporting bias) | Low risk | Did not process urine samples for magnesium of those getting placebo (although did a reasonable job collecting urine samples from all participants to make sure the blinding was not broken). Report described severity and duration of cramps only as not being different (i.e. no numbers given); however, trial authors made these data available. |
| Cramp diary (recall bias) | Low risk | Diary used |
| Other bias | Low risk | No obvious other bias |
NCT00963638.
| Study characteristics | ||
| Methods | Double‐blind, parallel‐group RCT | |
| Participants | 40 non‐pregnant rest cramp sufferers (mean age 66.6, 42.5% male) with normal renal function having at least 2 cramps per week that were rated 5 or more on a 0 to 10 pain scale. Recruitment by radio advertisement in a US state (Michigan) population | |
| Interventions | Either 168 mg elemental magnesium from slow release magnesium lactate tablets (MagTabSR) (n = 18) or matching placebo tablets (n = 19) taken orally twice daily for 30 days | |
| Outcomes | Frequency, duration and severity of leg cramps captured daily × 1 week pre‐intervention and daily during the 30 days of intervention (via diary recording of cramps and sleep disturbance) Pittsburgh Sleep Quality questionnaire also administered pre‐ and post‐intervention |
|
| Conflicts of interest | Sponsorship and conflicts of interest not provided | |
| Funding | Sponsorship and conflicts of interest not provided | |
| Notes | Unpublished. Participant‐level data for cramp frequency were kindly provided by study statistician. Conducted between April and November of 2009 according to trial registry | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated as randomized but details not provided |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Masking: Double Blind (Subject, Investigator, Outcomes Assessor)". No details provided. Probably adequate |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes measured from diaries completed by blinded participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Small number of dropouts, 2 from magnesium and 1 from placebo. Reasons not provided |
| Selective reporting (reporting bias) | High risk | Participant‐level data were provided to us but were only available for a subset of the outcomes |
| Cramp diary (recall bias) | Low risk | Diary used |
| Other bias | Low risk | No obvious other bias |
Nygaard 2008.
| Study characteristics | ||
| Methods | Double‐blind, parallel‐group RCT | |
| Participants | 45 pregnant women with rest cramps and no previous cramp treatment. Recruitment by pamphlets provided to pregnant Norwegian women undergoing 18‐week ultrasound | |
| Interventions | Either a chewable tablet containing 122 mg elemental magnesium ("primarily as Mg lactate and Mg citrate") (n = 23), or a matched placebo tablet (n = 22), taken once each morning and twice each evening for 2 weeks | |
| Outcomes | Number of days or nights in which cramps occurred over 2 weeks Degree of cramp pain on a 5‐point ordinal scale Side effects Serum magnesium and calcium and 24‐hour urinary magnesium on days 1 and 15 |
|
| Conflicts of interest | 1 author contributed in developing the magnesium tablet in 1985, and he received a compensation from Nycomed for this effort. The rest of the authors have no conflict of interest. | |
| Funding | Source of funding not provided | |
| Notes | Published. Conducted from August 2000 to January 2003 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “The randomization program was provided by Medstat Research AS.” Comment: probably adequate; however, the frequency of cramping at baseline was not assessed, making it impossible to tell if the group was imbalanced in this important baseline characteristic |
| Allocation concealment (selection bias) | Unclear risk | No description of any method of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Both groups received a plastic container with the trial medication, 42 chewable tablets...”, containing either magnesium or placebo, both provided by the manufacturer Comment: probably adequate |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes measured from forms completed by blinded participants |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 7/45 women (15.6%) dropped out (2 from the treatment arm and 5 from control). Reasons were given and most were unrelated to potential drug effects. None of the 7 dropouts were included in the analysis, because of a lack of data |
| Selective reporting (reporting bias) | Low risk | Primary outcome assumed to be the number of days and nights with cramping, but not explicitly stated. All outcomes reported |
| Cramp diary (recall bias) | Low risk | Diary used |
| Other bias | Low risk | No other obvious bias |
Roffe 2002.
| Study characteristics | ||
| Methods | Double‐blind RCT of cross‐over design | |
| Participants | 73 non‐pregnant rest cramp sufferers (mean age 63 years), having at least 2 cramps per week. Recruitment by community advertisement in a UK population. Patient‐level data available only for those who completed the study (n = 46) | |
| Interventions | Either 1830 mg of tri‐magnesium dicitrate powder (300 mg elemental magnesium) poured from a sachet into a glass of water (n = 17), or matched placebo powder (n = 29), taken orally each night for 6 weeks before switching to the alternate therapy. 2‐week magnesium‐free run‐in and effectively a 2‐week washout between treatments, since only the last 4 weeks of each 6 weeks on treatment were used for outcome assessment | |
| Outcomes | Number of cramps during the last 4 weeks of each treatment period Severity of cramps (mild, moderate, severe) Duration of cramps (short, medium, long) Self‐reported assessment of treatment effectiveness (yes or no) |
|
| Conflicts of interest | No mention of conflict of interest | |
| Funding | Manufacturer sponsored | |
| Notes | Published. We only used data from the first period in this review because large differences in treatment effect are seen depending on the sequence in which treatment is given. Patient‐level data provided by the principal investigator. The period during which the trial was conducted is not stated (first received by publisher 14 December 2001). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The manufacturer provided centralized randomization for the trial in large blocks of 10. Specifics regarding the sequence generation were not given. The resulting allocation was unequal, with more participants included in the analysis receiving magnesium second (29 versus 17) |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomisation code was not known to the investigators who gave out the sachets. The code remained concealed from everyone except the pharmacist who prepared the sachets..." Comment: satisfactory concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No description of whether the magnesium and placebo suspensions tasted different |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcomes measured from diaries completed by blind participants but blinding of participants unclear |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Reasons for dropout documented, but 27 of 73 participants (37%) did not complete the study |
| Selective reporting (reporting bias) | Low risk | Severity and duration of cramps were described only as not being different (i.e. no numbers given); however, the trial authors provided us with these data |
| Cramp diary (recall bias) | Low risk | Diary used |
| Other bias | Low risk | Manufacturer played an active role in the trial. There was a large difference in treatment effect depending on the sequence of treatments (much greater benefit if treatment was received in the order placebo→magnesium). Unclear if this difference was due entirely to period effect or if noncompleters, the potential for carry‐over or unblinding contributed. This difference in benefit resulting from treatment order was important, since the randomization was unbalanced (many more participants received the placebo→magnesium sequence). However, we used only data from the first treatment period of this study, which mitigates this risk |
Roguin Maor 2017.
| Study characteristics | ||
| Methods | Parallel, double‐blind, randomized, placebo‐controlled trial | |
| Participants | 94 non‐pregnant nocturnal leg cramps sufferers at least 21 years of age (mean age 64.9 years, 39% male) with normal renal function and having at least 4 nocturnal leg cramps during the 2‐week screening phase. Recruitment via advertisements in clinics, pharmacies and local media in northern Israel | |
| Interventions | Either 1 capsule of 865 mg magnesium oxide (n = 48) (520 mg elemental Mg) once daily at bedtime or a matching placebo (n = 46) for 4 weeks. All participants received daily text reminders and twice weekly phone calls to ensure adherence to allocation and completion of diaries. | |
| Outcomes | Primary: change in the frequency of nocturnal leg cramps per week between the 4‐week treatment phase and the 2‐week screening phase, as recorded in a sleep diary Secondary:
|
|
| Conflicts of interest | Authors reported no conflict of interest | |
| Funding | The study was funded entirely by the manufacturer (Naveh‐Pharma Ltd) | |
| Notes | Published. Stopped early for futility at an interim analysis. Trial conducted from February to October 2013 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A randomization schedule was computer generated using blocks of 10 and participants received sequential numbers. Number of cramps per week at baseline was somewhat imbalanced (7.84 cramps per week in the Mg group, 8.51 cramps per week in the placebo group). This is likely to bias our outcome of difference between groups in cramps per week on treatment in favour of the Mg group, whose baseline rate was lower |
| Allocation concealment (selection bias) | Low risk | Identical pills and bottles were prepared in advance. These bottles were identified with sequential numbers that were assigned to each participant in order of recruitment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Identical capsules and bottles. "Both patients and researchers were blind to treatment allocation" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes reported (in diaries) by blinded participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All analyses were ITT with multiple imputations of missing data (assumed to be the baseline value). 3/46 (6.5%) placebo and 3/48 (6.3%) magnesium recipients discontinued the intervention |
| Selective reporting (reporting bias) | Low risk | Results are reported for all outcomes described under methods and these match the trial protocol |
| Cramp diary (recall bias) | Low risk | Diary used |
| Other bias | Low risk | No obvious other bias |
Shahraki 2006.
| Study characteristics | ||
| Methods | Open‐label, parallel‐group RCT | |
| Participants | 120 pregnant, multiparous women aged 25 to 35 years (mean age 29.2 years old) who suffered from muscular cramps and were in the 25th to 28th week of pregnancy when referred to a gynaecology clinic in Shahrekord, Iran | |
| Interventions | Randomized to 3 groups: Group 1: 100 mg Vitamin E oral pill once a day (n = 40) Group 2: 8 cc of a 8% milk of magnesium suspension (267.2 mg elemental magnesium) 3 times a day, before meals (n = 40) Group 3: 500 mg calcium carbonate oral pill once a day (n = 40) All treatments administered for 45 days |
|
| Outcomes | Number of cramps over the last 24 hours Duration of cramps in seconds Cramp intensity (measured on a 1 to 10 points VAS) Frequency of low and high pain (1 to 5 = low pain rate and 6 to 10 = high pain) Each outcome measured on day 0, 45, and 90 |
|
| Conflicts of interest | Funding and conflicts of interest not reported | |
| Funding | Funding and conflicts of interest not reported | |
| Notes | Published in English but likely translated from a different language, with the result that some information is incomprehensible. Conducted from September 2004 to July 2005 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No information available on the method of randomization. Quote: “Each group was included 40 persons which were divided randomizly and turn of coming.” No table with baseline characteristics |
| Allocation concealment (selection bias) | High risk | No information available |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open label |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open label |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 120 initially included but results only presented for 90 participants. Paper only describes 20 participants quitting the study. Type of analysis unclear, likely to be per protocol |
| Selective reporting (reporting bias) | Low risk | All planned outcomes are addressed in the results |
| Cramp diary (recall bias) | Unclear risk | Unclear but given reporting was recall of the last 24 hours; unlikely that a diary was used |
| Other bias | Low risk | No obvious other bias |
Sohrabvand 2006.
| Study characteristics | ||
| Methods | Open‐label RCT with 4 parallel treatment groups | |
| Participants | 84 pregnant women. Recruitment method (Iranian women) not provided | |
| Interventions | Group 1: 500 mg calcium carbonate tablet once daily (n = 21) Group 2: 7.5 mmol magnesium aspartate (182 mg elemental magnesium) twice daily (n = 21) Group 3: 100 mg of thiamine (vitamin B₁) plus 40 mg of pyridoxine (vitamin B₆) once daily (n = 21) Group 4: no treatment (n = 21) |
|
| Outcomes | "Change in muscle spasms" on a 3‐point ordinal scale (no change, "relative improvement", or "absolute improvement") | |
| Conflicts of interest | Funding source and conflicts of interest not provided | |
| Funding | Funding source and conflicts of interest not provided | |
| Notes | Unusual design. Each treatment was given over 2 weeks but efficacy was assessed at 4 weeks. Published as a "brief communication" (letter) only. No definition of relative and absolute improvement was given in the manuscript but this was confirmed with the author to mean partial and complete resolution of the overall cramp burden (which presumably takes into account both intensity and frequency). The period during which the trial was conducted is not stated (first received by publisher 6 March 2006) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description. Baseline characteristics were said to be not significantly different but they were not provided |
| Allocation concealment (selection bias) | Unclear risk | No description. Baseline characteristics were said to be not significantly different but they were not provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label trial. Unclear who rated the degree of improvement (participant or physician) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label trial. Unclear who rated the degree of improvement (participant or physician) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No details in the manuscript regarding flow of participants but author communication suggests no dropouts |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not identified (though only 1 outcome reported) Table 2 showed statistical significance in total improvement for groups 2 and 3 compared to group 4 but in the text it stated groups 1 and 3 (which is supported by the CI results). Trial was very under‐reported. Outcomes were grouped in an impractical way |
| Cramp diary (recall bias) | High risk | Specifics were not given but there appeared to have only been a qualitative assessment of the change in cramps upon study completion |
| Other bias | Low risk | No obvious other bias |
Supakatisant 2015.
| Study characteristics | ||
| Methods | Double‐blind, parallel‐group RCT | |
| Participants | 86 women with pregnancy induced rest cramps (mean 28.0 weeks' gestation) having at least 2 cramps per week and beng free of both medical disease and obstetrical complications. Recruitment was from a university‐affiliated antenatal specialty clinic in Thailand | |
| Interventions | Either magnesium bisglycinate chelate (100 mg elemental magnesium per tablet) (n = 43) or matched placebo tablet (n = 43), taken as 1 tablet 3 times daily with meals for 4 weeks. | |
| Outcomes | 50% reduction in cramp frequency (cramps per week) 50% reduction in cramp intensity VAS Side effects |
|
| Conflicts of interest | Authors declare they have no conflict of interest. | |
| Funding | Independent funding | |
| Notes | Published. Conducted from June 2010 to August 2011 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number sequence with fixed blocks of 4 was generated from a random number table and used to number bottles of study medication, which were provided to participants in sequence as they were enrolled |
| Allocation concealment (selection bias) | Low risk | Nurses who were unaware of the contents of each bottle selected the next bottle in sequence and provided it to participants |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The opaque plastic container contained 84 tablets of magnesium or placebo (identical in size, shape and colour)." "Both health care providers and women were masked to treatment assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes measured from diaries and forms completed by participants blind to treatment group |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 6/86 women did not complete the study (7%). In an ITT analysis, the authors treated these participants as "worst‐case scenario" but we confirmed this to mean that the trialists considered all participants with incomplete data as treatment failures. As 4 control group participants did not complete the study, and 2 intervention group participants did not complete the study, handling missing data in this way attributed 4 treatment failures to the control group and 2 to the intervention group. This approach biases the results in favour of the intervention (as compared to a more typical worst‐case scenario approach, which would conservatively categorize missing data in the intervention group as treatment failure but missing data in the control group as treatment success). |
| Selective reporting (reporting bias) | High risk | Primary outcome not clearly stated until the discussion (although the authors describe powering for what was eventually described as the primary outcome) and methods do not describe how each outcome was intended to be analysed. The reported results also appear incongruous despite requests for clarification from trial authors. In particular, the trial authors confirm that the median number of cramps per week increased from baseline in both groups (a median increase of 1 cramp per week in treatment and 3 cramps per week in control) while simultaneously reporting a large per cent reduction in cramp rates (a 79% reduction in the magnesium group and 32.4% reduction in the placebo group). A language barrier, mislabelling of results, or both, might explain some of these discrepancies. The reported median absolute change in pain score was also higher in the placebo group than in the treatment group. As the trial authors describe pain scores decreasing in both groups, this does not make sense and the trial authors probably mean this to be median pain on treatment rather than median absolute change. |
| Cramp diary (recall bias) | Unclear risk | Although the trial authors use the phrase "diary chart" in the text, it does not appear that individual cramps were recorded. Rather the "case record forms" that participants filled out appear to be based on recall of cramps at baseline and again upon conclusion of the study. |
| Other bias | Low risk | No obvious other bias |
CI: confidence interval ITT: intention‐to‐treat IV: intravenous Mg: magnesium RCT: randomized controlled trial VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aagaard 2005 | This RCT looked at muscle strength, muscle mass and muscle magnesium content. It did not look at measures of muscle cramping |
| Bachem 1986 | No control group. Article in German with English abstract. Methods translated |
| Bartl 1982 | Did not appear to be randomized. Evaluated serum magnesium levels in pregnant cramp sufferers before and after magnesium supplementation. Did not evaluate changes in muscle cramping. Article in German with English abstract. Methods translated |
| Hammar 1987 | No magnesium treatment arm |
| Häringer 1981 | No control group. Article in German. Abstract and Methods translated |
| Riss 1983 | Uncontrolled. Article in German with English abstract |
| Siegmund‐Schultze 2017 | Not a trial. Article in German reviewing and commenting on Roguin Maor 2017 |
| Weiss 2018 | Not randomized |
| Weller 1998 | This RCT looked at exercise performance and magnesium concentration in various tissues. It did not look at measures of muscle cramping |
| Zarean 2017 | This RCT of pregnant women with hypomagnaesemia (only some of whom experienced muscle cramps) gave magnesium to the intervention group and not to the control group. However these 2 groups also appeared to take differing multimineral supplements (we attempted to confirm this with the trial authors but obtained no response). Our inclusion/exclusion criteria require treatment to be the same in each group, other than the provision of magnesium, and it is for this reason we chose to exclude the trial. This trial also looked at pregnancy outcomes more broadly, and did not focus on cramps. None of our specified outcomes were reported, only the number of unblinded participants self‐reporting "cramps" (yes/no) in each group |
RCT: randomized controlled trial
Characteristics of ongoing studies [ordered by study ID]
NCT03082625.
| Study name | Topical magnesium and muscle cramps in dialysis patients |
| Methods | Randomized, placebo‐controlled, cross‐over trial |
| Participants | People on haemodialysis |
| Interventions | Transdermal spray of magnesium versus transdermal spray containing vehicle only (5 sprays each on the 2 most affected muscle groups twice daily). 8‐week treatment periods and 4‐week washout in between |
| Outcomes | Primary: difference between groups in the number of cramps per week on treatment during the final 3 weeks on treatment. Secondary: difference in cramp duration and difference in cramp severity (final 3 weeks); percentage change in serum magnesium from baseline at the end of treatment; difference in restless leg symptoms |
| Starting date | 1 May 2017 |
| Contact information | Neil Boudville (Head of Dept of Renal Medicine, Sir Charles Gairdener Hospital)) e‐mail: neil.boudville@uwa.edu.au |
| Notes | ClinicalTrials.gov registration: NCT03082625 |
Differences between protocol and review
Authors
With this update, authorship has changed according to ongoing contribution. Specifically, MRK, CSK and ND joined the review team and became authors while K Khan (with thanks for his prior contribution) was removed.
Searching other resources
For the original review, we carried out three additional approaches to obtaining studies for our review that we had not pre‐identified in our study protocol. This included searching the International Clinical Trials Registry Platform (WHO‐ICTRP) in an attempt to uncover unpublished trials, searching ISI Web of Science for papers citing the studies included in this review, and contacting the FDA to ask if they had any related clinical trial information in their possession.
For this update, in addition to the WHO‐ICTRP trial registry we additionally searched ClinicalTrials.gov. We did not newly contact the FDA or Health Canada looking for trials, as we anticipated any new trials would be registered.
We included details of Web of Science searches.
Data collection and analysis
We expanded the methods as follows.
-
Selection of studies: we
declared that we did not exclude studies based on language or publication status;
declared that we did not use outcome reporting to select studies;
included an additional PRISMA flow chart to document the study selection process for the 2019 update.
We also:
listed extracted data;
reported methods for resolving disagreements in 'Risk of bias' assessment;
separated blinding of participants and personnel from blinding of outcome assessors;
added interpretation of the I² statistic;
reported that we pooled adverse events data across participant groups;
specified a minimum number of participants for subgroup analysis;
switched several outcomes from risk difference to risk ratio to allow better external generalization of our finding.
'Summary of findings' table addition
Under the heading 'Secondary outcomes' in the original study protocol we had pre‐identified our plans for a 'Summary of findings' table with several elements. Since considerably more poolable data were available for the outcome "Number of cramps per week at four weeks" we chose to add this outcome to the 'Summary of findings' table.
Contributions of authors
Protocol stage: SRG drafted the protocol and the other authors commented and approved the final text.
Initial review: SG and RKS selected studies for inclusion. SRG and GMA extracted data. SRG, GMA and VMM rated studies for bias (SRG did not participate in the rating of his own trial). SRG performed all data analysis and wrote the draft manuscript. All authors commented on and approved the final text.
Update: SRG, ND, MRK and CSK selected studies for inclusion, extracted data and rated new studies for risk of bias. ND updated the results and the analysis including the new studies. All authors commented on and approved the final text.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Canadian Institutes of Health Research ‐ Doctoral Research Award in the Area of Research on Aging, Canada
Trainee Stipend (Dr. Garrison)
Declarations of interest
SRG: He is the author of an included study. Other conflicts: none known.
CSK: none known
MRK: none known
GMA: none known
VMM: none known
RKS: none known
ND: none known
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Cohen‐Hagai 2018 {published data only (unpublished sought but not used)}
- Cohen-Hagai K, Feldman D, Turani-Feldman T, Hadary R, Lotan S, Kitay-Cohen Y. Magnesium Deficiency and Minimal Hepatic Encephalopathy among Patients with Compensated Liver Cirrhosis. Israel Medical Association Journal 2018;20(9):533-8. [PubMed] [Google Scholar]
Dahle 1995 {published data only (unpublished sought but not used)}
- Dahle LO, Berg G, Hammar M, Hurtig M, Larsson L. The effect of oral magnesium substitution on pregnancy-induced leg cramps. American Journal of Obstetrics and Gynecology 1995;173(1):175-80. [PMID: ] [DOI] [PubMed] [Google Scholar]
Frusso 1999 {published data only (unpublished sought but not used)}
- Frusso R, Zárate M, Augustovski F, Rubinstein A. Magnesium for the treatment of nocturnal leg cramps: a crossover randomized trial. Journal of Family Practice 1999;48(11):868-71. [PMID: ] [PubMed] [Google Scholar]
Garrison 2011a {published and unpublished data}
- Garrison SR, Birmingham CL, Koehler BE, McCollom RA, Khan KM. The effect of magnesium infusion on rest cramps: randomized controlled trial. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2011;66(6):661-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
NCT00963638 {unpublished data only}
- NCT00963638. Beneficial effects of magnesium supplementation on idiopathic muscle cramps. clinicaltrials.gov/show/NCT00963638 (first received 21 August 2009).
Nygaard 2008 {published data only (unpublished sought but not used)}
- Nygaard IH, Valbø A, Pethick SV, Bøhmer T. Does oral magnesium substitution relieve pregnancy-induced leg cramps? European Journal of Obstetrics, Gynecology, and Reproductive Biology 2008;141(1):23-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Roffe 2002 {published and unpublished data}
- Roffe C, Sills S, Crome P, Jones P. Randomised, cross-over, placebo controlled trial of magnesium citrate in the treatment of chronic persistent leg cramps. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research 2002;8(5):CR326-30. [PMID: ] [PubMed] [Google Scholar]
Roguin Maor 2017 {published data only (unpublished sought but not used)}
- Roguin Maor N, Alperin M, Shturman E, Khairaldeen H, Friedman M, Karkabi K, et al. Effect of magnesium oxide supplementation on nocturnal leg cramps: a randomized clinical trial. JAMA Internal Medicine 2017;177(5):617-23. [DOI: 10.1001/jamainternmed.2016.9261] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shahraki 2006 {published data only (unpublished sought but not used)}
- Shahraki AD. Effects of vitamin E, calcium carbonate and milk of magnesium on muscular cramps in pregnant women. Journal of Medical Sciences 2006;6(6):979-83. [DOI: 10.3923/jms.2006.979.983 ] [EMBASE: 44811339] [Google Scholar]
Sohrabvand 2006 {published data only (unpublished sought but not used)}
- Sohrabvand F, Shariat M, Haghollahi F. Vitamin B supplementation for leg cramps during pregnancy. International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics 2006;95(1):48-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Supakatisant 2015 {published data only}
- Supakatisant C, Phupong V. Oral magnesium for relief in pregnancy-induced leg cramps: a randomised controlled trial. Maternal & Child Nutrition 2015;11(2):139-45. [PMID: ] [DOI] [PMC free article] [PubMed]
References to studies excluded from this review
Aagaard 2005 {published data only}
- Aagaard NK, Andersen H, Vilstrup H, Clausen T, Jakobsen J, Dorup I. Magnesium supplementation and muscle function in patients with alcoholic liver disease: a randomized, placebo-controlled trial. Scandinavian Journal of Gastroenterology 2005;40(8):972-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bachem 1986 {published data only}
- Bachem MG, Scheffler K, Jastram U, Pfeiffer EF. Effectiveness of oral magnesium substitution in type I diabetic patients with nocturnal leg cramps [Effektivität einer peroralen Magnesiumsubstitution bei Typ-I-Diabetikern mit nächtlichen Wadenkrämpfen]. Magnesium-Bulletin 1986;8(3):280-3. [Google Scholar]
Bartl 1982 {published data only}
- Bartl W, Riss P. Pathophysiology and therapy of magnesium deficiency in pregnancy [Zur Pathophysiologie und Therapie des Magnesiummangels in der Schwangerschaft]. Zeitschrift für Geburtshilfe und Perinatologie 1982;186(6):335-7. [PubMed] [Google Scholar]
Hammar 1987 {published data only}
- Hammar M, Berg G, Solheim F, Larsson L. Calcium and magnesium status in pregnant women. A comparison between treatment with calcium and vitamin C in pregnant women with leg cramps. International Journal for Vitamin and Nutritional Research 1987;57(2):179-83. [PMID: ] [PubMed] [Google Scholar]
Häringer 1981 {published data only}
- Häringer E. Calf cramps at night: A deficiency of magnesium? [Wadenkrämpfe in der Nacht: Fehlt Magnesium?]. Ärtzliche Praxis 1981;33:2653-4. [Google Scholar]
Riss 1983 {published data only}
- Riss P, Bartl W, Jelincic D. Clinical aspects and treatment of calf muscle cramps during pregnancy [Zur Klinik und Therapie von Wadenkrämpfen in der Schwangerschaft]. Geburtshilfe und Frauenheilkunde 1983;43(5):329-31. [PMID: ] [DOI] [PubMed] [Google Scholar]
Siegmund‐Schultze 2017 {published data only}
- Siegmund-Schultze N. Prevention of nocturnal muscle cramps: magnesium for 1 month is not more effective than placebo [Magnesium für 1 Monat nicht wirksamer als Placebo]. Deutsches Arzteblatt International 2017;114(22-3):1123. [Google Scholar]
Weiss 2018 {published data only}
- Weiss D, Brunk DK, Goodman DA. Scottsdale Magnesium Study: absorption, cellular uptake, and clinical effectiveness of a timed-release magnesium supplement in a standard adult clinical population. Journal of the American College of Nutrition 2018;37(4):316-27. [DOI] [PubMed] [Google Scholar]
Weller 1998 {published data only}
Zarean 2017 {published data only (unpublished sought but not used)}
- Zarean E, Tarjan A. Effect of Magnesium Supplement on Pregnancy Outcomes: A Randomized Control Trial. Advanced Biomedical Research 2017 Aug 31;6:109. [DOI: 10.4103/2277-9175.213879] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
NCT03082625 {unpublished data only}
- Topical magnesium and muscle cramps in dialysis patients. Ongoing study. 1 May 2017. Contact author for more information.
Additional references
ADRAC 2002
- Adverse Drug Reactions Advisory Committee. Quinine and profound thrombocytopenia. Australian Adverse Drug Reactions Bulletin 2002;21(3):10. [Google Scholar]
AHFS 2010
- Magnesium sulfate. McEvoy GK, editors(s). American Hospital Formulary Service (AHFS) Drug Information. 2010 edition. Bethesda, MD: American Society of Health-System Pharmacists, 2010:2282-5. [Google Scholar]
al‐Ghamdi 1994
- al-Ghamdi SM, Cameron EC, Sutton RA. Magnesium deficiency: pathophysiologic and clinical overview. American Journal of Kidney Diseases 1994;24(5):737-52. [DOI] [PubMed] [Google Scholar]
Bilbey 1996
- Bilbey DL, Prabhakaran VM. Muscle cramps and magnesium deficiency: case reports. Canadian Family Physician 1996;42:1348-51. [PMC free article] [PubMed] [Google Scholar]
Blyton 2012
- Blyton F, Chuter V, Burns J. Unknotting night-time muscle cramp: a survey of patient experience, help-seeking behaviour and perceived treatment effectiveness. Journal of Foot and Ankle Research 2012;5:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 1990
- Cohen L, Laor A. Correlation between bone magnesium concentration and magnesium retention in the intravenous magnesium load test. Magnesium Research 1990;3(4):271-4. [PubMed] [Google Scholar]
Eclampsia Trialists 1995
- The Eclampsia Trial Collaborative Group. Which anticonvulsant for women with eclampsia? Evidence from the Collaborative Eclampsia Trial. Lancet 1995;345(8963):1455-63. [PubMed] [Google Scholar]
El‐Tawil 2015
- El-Tawil S, Al Musa T, Valli H, Lunn MPT, Brassington R, El-Tawil T, Weber M. Quinine for muscle cramps. Cochrane Database of Systematic Reviews 2015, Issue 4. Art. No: CD005044. [DOI: 10.1002/14651858.CD005044.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
FDA 2006
- Drug products containing quinine; enforcement action dates. Federal Register 2006;71(241):75557–60.
Garrison 2012a
- Garrison SR, Dormuth CR, Morrow RL, Carney GA, Khan KM. Nocturnal leg cramps and prescription use that precedes them: a sequence symmetry analysis. Archives of Internal Medicine 2012;172(2):120-6. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime, Inc.) GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime, Inc.). Available from gradepro.org.
Graham 1960
- Graham LA, Caesar JJ, Burgen AS. Gastrointestinal absorption and excretion of Mg 28 in man. Metabolism 1960;9:646-59. [PubMed] [Google Scholar]
Hall 1973
- Hall RC, Joffe JR. Hypomagnesemia. Physical and psychiatric symptoms. JAMA 1973;224(13):1749-51. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Lim 1972
- Lim P, Jacob E. Magnesium status of alcoholic patients. Metabolism 1972;21(11):1045-51. [DOI] [PubMed] [Google Scholar]
MAGPIE 2002
- Altman D, Carroli G, Duley L, Farrell B, Moodley J, Neilson J, et al, Magpie Trial Collaboration Group. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: a randomised placebo-controlled trial. Lancet 2002;359(9321):1877-90. [DOI: ] [DOI] [PubMed] [Google Scholar]
McGee 1990
- McGee SR. Muscle cramps. Archives of Internal Medicine 1990;150(3):511-8. [PubMed] [Google Scholar]
Medsafe 2007
- Medsafe Pharmacovigilance Team, New Zealand Medicines and Medical Devices Safety Authority. Quinine - not for leg cramps anymore. Prescriber Update 2007;28(1):2-6. [Google Scholar]
Miller 2005
- Miller TM, Layzer RB. Muscle cramps. Muscle and Nerve 2005;32(4):431-42. [DOI] [PubMed] [Google Scholar]
Naylor 1994
- Naylor JR, Young JB. A general population survey of rest cramps. Age and Ageing 1994;23(5):418-20. [DOI] [PubMed] [Google Scholar]
Quamme 1993
- Quamme GA. Laboratory evaluation of magnesium status. Renal function and free intracellular magnesium concentration. Clinics in Laboratory Medicine 1993;13(1):209-23. [PubMed] [Google Scholar]
Quamme 2008
- Quamme GA. Recent developments in intestinal magnesium absorption. Current Opinion in Gastroenterology 2008;24(2):230-5. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ryzen 1985
- Ryzen E, Elbaum N, Singer FR, Rude RK. Parenteral magnesium tolerance testing in the evaluation of magnesium deficiency. Magnesium 1985;4(2-3):137-47. [PubMed] [Google Scholar]
Schwellnus 2008
- Schwellnus MP, Drew N, Collins M. Muscle cramping in athletes--risk factors, clinical assessment, and management. Clinics in Sports Medicine 2008;27(1):183-94, ix-x. [DOI] [PubMed] [Google Scholar]
Schünemann 2011a
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and ‘Summary of findings' tables. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Schünemann 2011b
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al, on behalf of the Cochrane GRADEing Methods Group and the Cochrane Statistical Methods Group. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011.. Available from www.cochrane-handbook.org.
Sebo 2014
- Sebo P, Cerutti B, Haller DM. Effect of magnesium therapy on nocturnal leg cramps: a systematic review of randomized controlled trials with meta-analysis using simulations. Family Practice 2014;31(1):7-19. [DOI] [PubMed] [Google Scholar]
Shils 1969
- Shils ME. Experimental human magnesium depletion. Medicine (Baltimore) 1969;48(1):61-85. [DOI] [PubMed] [Google Scholar]
Somjen 1966
- Somjen G, Hilmy M, Stephen CR. Failure to anesthetize human subjects by intravenous administration of magnesium sulfate. Journal of Pharmacology and Experimental Therapeutics 1966;154(3):652-9. [PubMed] [Google Scholar]
Vickers 2001
- Vickers AJ. The use of percentage change from baseline as an outcome in a controlled trial is statistically inefficient: a simulation study. BMC Medical Research Methodology 2001;1:6. [DOI: 10.1186/1471-2288-1-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhou 2015
- Zhou K, West HM, Zhang J, Xu L, Li W. Interventions for leg cramps in pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 8. Art. No: CD010655. [DOI: 10.1002/14651858.CD010655.pub2] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Garrison 2011b
- Garrison SR, Allan GM, Sekhon RK, Musini VM, Khan KM. Magnesium for skeletal muscle cramps. Cochrane Database of Systematic Reviews 2011, Issue 11. Art. No: CD009402. [DOI: 10.1002/14651858.CD009402] [DOI] [PMC free article] [PubMed] [Google Scholar]
Garrison 2012b
- Garrison SR, Allan GM, Sekhon RK, Musini VM, Khan KM. Magnesium for skeletal muscle cramps. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No: CD009402. [DOI: 10.1002/14651858.CD009402.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


