Abstract
Background
The prevalence of opiate use among pregnant women can range from 1% to 2% to as high as 21%. Just in the United States alone, among pregnant women with hospital delivery, a fourfold increase in opioid use is reported from 1999 to 2014 (Haight 2018). Heroin crosses the placenta, and pregnant, opiate‐dependent women experience a six‐fold increase in maternal obstetric complications such as low birth weight, toxaemia, third trimester bleeding, malpresentation, puerperal morbidity, fetal distress and meconium aspiration. Neonatal complications include narcotic withdrawal, postnatal growth deficiency, microcephaly, neuro‐behavioural problems, increased neonatal mortality and a 74‐fold increase in sudden infant death syndrome. This is an updated version of the original Cochrane Review first published in 2008 and last updated in 2013.
Objectives
To assess the effectiveness of any maintenance treatment alone or in combination with a psychosocial intervention compared to no intervention, other pharmacological intervention or psychosocial interventions alone for child health status, neonatal mortality, retaining pregnant women in treatment, and reducing the use of substances.
Search methods
We updated our searches of the following databases to February 2020: the Cochrane Drugs and Alcohol Group Specialised Register, CENTRAL, MEDLINE, Embase, PsycINFO, CINAHL, and Web of Science. We also searched two trials registers and checked the reference lists of included studies for further references to relevant randomised controlled trials (RCTs).
Selection criteria
Randomised controlled trials which assessed the efficacy of any pharmacological maintenance treatment for opiate‐dependent pregnant women.
Data collection and analysis
We used the standard methodological procedures expected by Cochrane.
Main results
We found four trials with 271 pregnant women. Three compared methadone with buprenorphine and one methadone with oral slow‐release morphine. Three out of four studies had adequate allocation concealment and were double‐blind. The major flaw in the included studies was attrition bias: three out of four had a high dropout rate (30% to 40%), and this was unbalanced between groups.
Methadone versus buprenorphine:
There was probably no evidence of a difference in the dropout rate from treatment (risk ratio (RR) 0.66, 95% confidence interval (CI) 0.37 to 1.20, three studies, 223 participants, moderate‐quality evidence). There may be no evidence of a difference in the use of primary substances between methadone and buprenorphine (RR 1.81, 95% CI 0.70 to 4.68, two studies, 151 participants, low‐quality evidence). Birth weight may be higher in the buprenorphine group in the two trials that reported data MD;‐530.00 g, 95%CI ‐662.78 to ‐397.22 (one study, 19 particpants) and MD: ‐215.00 g, 95%CI ‐238.93 to ‐191.07 (one study, 131 participants) although the results could not be pooled due to very high heterogeneity (very low‐quality of evidence). The third study reported that there was no evidence of a difference. We found there may be no evidence of a difference in the APGAR score (MD: 0.00, 95% CI ‐0.03 to 0.03, two studies,163 participants, low‐quality evidence). Many measures were used in the studies to assess neonatal abstinence syndrome. The number of newborns treated for neonatal abstinence syndrome, which is the most critical outcome, may not differ between groups (RR 1.19, 95% CI 0.87 to1.63, three studies, 166 participants, low‐quality evidence).
Only one study which compared methadone with buprenorphine reported side effects. We found there may be no evidence of a difference in the number of mothers with serious adverse events (AEs) (RR 1.69, 95% CI 0.75 to 3.83, 175 participants, low‐quality evidence) and we found there may be no difference in the numbers of newborns with serious AEs (RR 4.77, 95% CI 0.59, 38.49,131 participants, low‐quality evidence).
Methadone versus slow‐release morphine:
There were no dropouts in either treatment group. Oral slow‐release morphine may be superior to methadone for abstinence from heroin use during pregnancy (RR 2.40, 95% CI 1.00 to 5.77, one study, 48 participants, low‐quality evidence).
In the comparison between methadone and slow‐release morphine, no side effects were reported for the mother. In contrast, one child in the methadone group had central apnoea, and one child in the morphine group had obstructive apnoea (low‐quality evidence).
Authors' conclusions
Methadone and buprenorphine may be similar in efficacy and safety for the treatment of opioid‐dependent pregnant women and their babies. There is not enough evidence to make conclusions for the comparison between methadone and slow‐release morphine. Overall, the body of evidence is too small to make firm conclusions about the equivalence of the treatments compared. There is still a need for randomised controlled trials of adequate sample size comparing different maintenance treatments.
Plain language summary
Maintenance treatments for opiate‐dependent pregnant women
Review question
This review summarised research studies comparing different types of pharmacologic maintenance treatments for pregnant women with opioid dependence
Key messages:
Methadone and buprenorphine may be substantially similar in efficacy and safety for the treatment of opioid‐dependent pregnant women and their babies. There is not enough evidence to make conclusions for the comparison between methadone and slow‐release morphine. Overall, the body of evidence is too small to make firm conclusions.
Background
Some women continue to use opiates when they are pregnant, yet heroin readily crosses the placenta. Opiate‐dependent women experience a sixfold increase in maternal obstetric complications and may give birth to low‐weight babies. The newborn may experience narcotic withdrawal (neonatal abstinence syndrome) and have development problems. There is also increased neonatal mortality and a 74‐fold increase in the risk of sudden infant death syndrome. Maintenance treatment with methadone provides a steady concentration of opiate in the pregnant woman's blood, and so prevents the adverse effects on the fetus of repeated withdrawals. Buprenorphine is also used.
Search date
The evidence is current to 18 February 2020.
Study characteristics
Only four randomised controlled trials with 271 participants satisfied the inclusion criteria for the review: two from Austria (outpatients), one from the USA (inpatients) and the fourth a multicentre, international study conducted in Austria, Canada and the USA. The trials continued for 15 to 18 weeks. Three compared methadone with buprenorphine (223 participants) and one compared methadone with oral slow‐release morphine (48 participants).
Study funding sources
The National Institute on Drug Abuse funded two studies, one received a grant from the Mayor of Vienna, and in the fourth study Schering Plough provided an educational grant to the first author to employ personnel required to conduct this study.
Key results
This review found few differences in newborn or maternal outcomes for pregnant, opiate‐addicted women who were maintained on methadone, buprenorphine or oral slow‐release morphine from a mean gestational age of 23 weeks to delivery.
Comparing methadone with buprenorphine, there is probably little or no difference in the number of women who dropped out of treatment. There may be little or no difference in the use of a primary substance and the number of newborns treated for neonatal abstinence syndrome between the methadone and buprenorphine groups. We are very uncertain whether newborns with mothers receiving buprenorphine could have a heavier birth weight.
Comparing methadone with oral slow‐release morphine, there were no dropouts in the only study included. The use of heroin in the third trimester may be lower with slow‐release morphine. However, there may be little or no difference in infant birth weight or duration of neonatal abstinence syndrome.
The number of participants in the trials was small and may not be sufficient to draw firm conclusions. All the included studies ended immediately after the baby was born. No severe complications were noted.
Quality of evidence
In the comparison of methadone with buprenorphine, the quality of the evidence ranged from moderate to very low because of inconsistency in the results of the studies for some outcomes, high rates of participants who dropped out from the studies, and small sample sizes of the included studies. In the comparison of methadone with slow‐release morphine, the quality of the evidence was low because of the small sample size of the study.
Summary of findings
Summary of findings 1. Methadone compared to buprenorphine for opiate‐dependent pregnant women.
| Methadone compared to buprenorphine for opiate‐dependent pregnant women | ||||||
| Patient or population: opiate‐dependent pregnant women Setting: outpatients Intervention: methadone Comparison: buprenorphine | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with buprenorphine | Risk with methadone | |||||
| Dropout rate follow‐up: range 15 weeks to 18 weeks | Study population | RR 0.66 (0.37 to 1.20) | 223 (3 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | ||
| 318 per 1000 | 210 per 1000 (118 to 382) | |||||
| Use of primary substance follow‐up: range 15 weeks to 18 weeks | Study population | RR 1.81 (0.70 to 4.68) | 151 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | ||
| 75 per 1000 | 135 per 1000 (52 to 349) | |||||
| Birth weight follow‐up: mean 18 weeks | The mean birth weight ranged from 3.093 g to 3530 gr | MD ranged from ‐530.00 gr (662.78,lower to 397.22 lower) to ‐215.00 gr (238.93, lower to 191.07 lower) | ‐ | 19 and 131 participants (2 RCTs) | ⊕⊝⊝⊝ VERY LOW 2 3 4 | |
| APGAR score Scale from: 0 to 10 follow‐up: mean 18 weeks | The mean APGAR score was 8.95 | MD 0 (0.03 lower to 0.03 higher) | ‐ | 163 (2 RCTs) | ⊕⊕⊝⊝ LOW 2 4 | |
| Number treated for NAS follow‐up: range 15 weeks to 18 weeks | Study population | RR 1.19 (0.87 to 1.63) | 166 (3 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | ||
| 447 per 1000 | 532 per 1000 (389 to 729) | |||||
| Serious adverse events for the mother | Study population | RR 1.69 (0.75 to 3.83) | 175 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | ||
| 93 per 1000 | 157 per 1000 (70 to 356) | |||||
| Serious adverse events for the child | Study population | RR 4.77 (0.59 to 38.49) | 131 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | ||
| 17 per 1000 | 82 per 1000 (10 to 664) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 downgraded one level due to imprecision: optimal information size not met
2 downgraded one level due to study limitations: high risk of attrition bias
3 downgraded one level due to inconsistency: high heterogeneity: I2 95%
4 downgraded one level due to imprecision: fewer than 400 participants
Summary of findings 2. Methadone compared to oral slow‐release morphine for opiate‐dependent pregnant women.
| Methadone compared to oral slow‐release morphine for opiate‐dependent pregnant women | ||||||
| Patient or population: opiate‐dependent pregnant women Setting: Intervention: methadone Comparison: oral slow‐release morphine | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with oral slow‐release morphine | Risk with methadone | |||||
| Dropout rate from treatment follow‐up: mean 15 weeks | No dropouts from either group | 48 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | |||
| Use of substance follow‐up: mean 15 weeks | Study population | RR 2.40 (1.00 to 5.77) | 48 (1 RCT) | ⊕⊕⊝⊝ LOW 1 3 | ||
| 208 per 1000 | 500 per 1000 (208 to 1000) | |||||
| Birth weight follow‐up: mean 15 weeks | The mean birth weight was 2912 g | MD 124 higher (186.94 lower to 434.94 higher) | ‐ | 48 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | |
| APGAR score (APGAR score ) follow‐up: mean 15 weeks | The study did not assess this outcome | ‐ | ||||
| Adverse events for the mother follow‐up: mean 15 weeks |
No side effects for the mother were reported | 48 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | |||
| Serious adverse events for the child follow‐up: mean 15 weeks |
No severe complications were noted in any of the neonates as monitored by polysomnography, although one child in the methadone group had central apnoea and one child in the morphine group had obstructive apnoea. | 48 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 not applicable
2 downgraded two levels: fewer than 100 participants
3 downgraded two level: optimal information size not met
Background
Description of the condition
Prenatal opioid use has increased dramatically since 2000. In the United States, the trend of current illegal drug use among pregnant women remained relatively stable from 2007 to 2008 (5.1%) up to 2009 to 2010 (4.4%) (Behnke 2013). However, the nationwide use of opioids during pregnancy has increased and more than quadrupled between 1999 and 2014 (Haight 2018).
The prevalence of opioid abuse is also increasing in other countries. In Australia, the National Drug Strategy Household Survey in 2013 found that among pregnant women, a small minority had used illicit substances; 2.4% before knowledge of their pregnancy and 1.6% after they knew they were pregnant (AIHW 2014). In the older version of the same survey conducted in 2010, it was reported that less than one in 20 women (4.2%) who were pregnant and breastfeeding in the past 12 months used any illicit drug while they were pregnant. This included those who used illicit drugs in the time before they knew they were pregnant (AIHW 2011).
The Canadian Maternity Experiences Survey found that 7% of women reported street drug use in the three months before pregnancy, which was then reduced to 1% once aware of pregnancy (Ordean 2018). The European Monitoring Centre for Drug & Drug Addiction (EMCDDA 2014) report indicates that the actual prevalence of drug use among pregnant women in Europe is difficult to ascertain. In many European countries, the data are simply not available due to a lack of scheduled antenatal visits among drug users. An isolated study conducted in a maternity hospital in Dublin, Ireland, found that 4% of prenatal and 6% of postnatal women tested positive for drug metabolites. Prevalence data of opioid use among pregnant women in other important data resources are limited (sources searched: World Health Organization (WHO 2014), United Nations Office on Drug and Crime ‐ World Drug Report (UNODC 2018), Office of National Drug Control Policy, USA (ONDCP 2020), Monitoring the Future 2019 Survey (Monitoring the future 2017).
Heroin readily crosses the placenta, and untreated opiate dependence in pregnant women is associated with many environmental and medical factors that contribute to poor maternal and child outcomes. It causes a six‐fold increase in obstetric complications, such as low birth weight, toxaemia, third trimester bleeding, malpresentation, puerperal morbidity, fetal distress and meconium aspiration. Neonatal complications include neonatal abstinence syndrome (NAS), postnatal growth deficiency, microcephaly, neurobehavioural problems, increased neonatal mortality and a 74‐fold increase in sudden infant death syndrome (Dattel 1990; Fajemirokun 2006; Ludlow 2004; Reddy 2017).
All of the commonly used opioids, including heroin and methadone, can produce neonatal abstinence syndrome in infants born to opiate‐dependent mothers. Neonatal abstinence syndrome combines all the symptoms of an adult withdrawal syndrome with irritability, poorly co‐ordinated sucking and, in the most severe cases, seizures and death (Kaltenbach 1998).
Description of the intervention
Since the early 1970s, treatment with methadone has been the standard of care for pregnant women addicted to opiates. Despite its ability to induce fetal dependence and withdrawal, maintenance treatment provides a steady concentration in the maternal blood plasma. It thus prevents the adverse effects of repeated withdrawal on the fetus (Jarvis 1994).
Buprenorphine has also been administered to opioid‐dependent pregnant women as a maintenance treatment. Placental transfer of buprenorphine may be less than with methadone, reducing fetal exposure and development of neonatal abstinence syndrome (Rayburn 2004).
How the intervention might work
Methadone maintenance treatment given during pregnancy reduces maternal illicit opiate use and fetal exposure, enhances compliance with obstetric care, and is associated with improved neonatal outcomes such as heavier birth weight (Fajemirokun 2006; Kaltenbach 1998). Additional benefits include a potential reduction in drug‐seeking behaviours, including commercial sex, to gain money for drugs. This reduction may decrease a woman's chance of acquiring sexually transmitted diseases such as human immunodeficiency virus (HIV) and hepatitis. For all these reasons, methadone treatment has become the 'gold standard' for the management of pregnant heroin users (NIH 1998) and many guidelines, in the UK (UK Guidelines 2007), USA (CSAT 2005) and Australia (Dunlop 2003), support the use of methadone during pregnancy.
Previous studies have been performed in centres that offered methadone and comprehensive services, including obstetric, health, psychiatric care, individual, group and family therapy. Consequently, it is difficult to evaluate the results of these studies and to distinguish the benefits of methadone itself from other measures of psychosocial and obstetric care (Wang 1999).
The available clinical literature suggests that buprenorphine maintenance is also associated with reduced maternal illicit opiate use and fetal exposure, enhanced compliance with obstetric care, and improved neonatal outcomes such as heavier birth weight (Johnson 2003; Lejuene 2006).
Why it is important to do this review
The Cochrane Drugs and Alcohol Group has conducted several systematic reviews on maintenance treatment: methadone (Faggiano 2003; Mattick 2009), heroin (Ferri 2011), levomethadyl acetate hydrochloride (LAAM) (Clark 2002), buprenorphine (Mattick 2008), naltrexone (Minozzi 2011), psychosocial treatment alone (Mayet 2004) and psychosocial treatment combined with maintenance treatment (Amato 2011). However, none of these reviews include studies on pregnant, opiate‐dependent women.
Two narrative reviews have discussed the risks and benefits of maintenance treatment in opiate‐dependent women (Rayburn 2004; Wang 1999); however, neither specified the inclusion criteria for the studies. They also described the studies and the results in a very generic way and did not draw firm conclusions about the superiority of one drug treatment over another. Two other out‐of‐date reviews also included observational studies and assessed the relationship between maternal opiate use and infant birth weight (Hulse 1997) and neonatal mortality (Hulse 1998). They found better results in patients taking methadone in terms of birth weight but no reduction in mortality. A more recent observational systematic review was conducted on the efficacy and safety of detoxification from opioids compared to maintenance with methadone or buprenorphine to treat opioid‐dependent pregnant women (Wang 2018). They included 235 pregnant women from three cohort studies in the meta‐analysis. Maternal maintenance therapy was associated with increased risk of relapse (RR 1.91, 95% confidence interval (CI) 1.14 to 3.21) but no treatment differences were observed for rates of NAS (RR 0.99, 95% CI 0.38 to 2.53) or preterm birth (RR 0.39, 95% CI 0.10 to 1.60). Another narrative review was conducted (including 75 articles from 1975 to 2015) and concluded that women with opioid use addiction during pregnancy could be treated with methadone or buprenorphine (Klaman 2017).
Objectives
To assess the effectiveness of any opioid agonist maintenance treatment alone or in combination with a psychosocial intervention compared to no intervention, other pharmacological intervention or psychosocial interventions for child health status, neonatal mortality, retaining pregnant women in treatment, and reducing the use of substances.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials which enrolled pregnant women were eligible. Studies starting after the delivery were excluded.
Types of participants
Opiate‐addicted according to the "Diagnostic and Statistical Manual of mental disorders" (DSM‐IV or DSM‐V) criteria pregnant women of any age irrespective of the duration of pregnancy. There was no restriction concerning the physical or psychological illness.
Types of interventions
Experimental intervention
Any pharmacological intervention (methadone, buprenorphine, LAAM, heroin, morphine, codeine) alone or combined with psychosocial intervention(s) for maintenance treatment
Control intervention
No intervention
Other pharmacological interventions
Psychosocial intervention alone
Types of outcome measures
For the woman
1. Dropout from treatment, as measured by the number of women who had dropped out at the end of the intervention
2. Use of primary substance of abuse
2.1 Use of primary substance as measured by the number of women using heroin during or at the end of treatment (self‐report or urine analysis results)
2.2. Use of primary substance at follow‐up as measured by the number of women using heroin at the end of follow‐up (after childbirth)
3. Obstetric outcomes
3.1 Third trimester bleeding
3.2 Fetal distress and meconium aspiration
3.3 Caesarean section
3.4 Abnormal presentation
3.5 Medical complications at delivery
3.6 Breastfeeding following delivery
3.7 Puerperal morbidity
For the child
4. Health status measured as:
4.1 Birth weight
4.2 APGAR score (Activity, Pulse, Grimace, Appearance and Respiration score)
4.3 Neonatal abstinence syndrome
4.4 Prenatal and neonatal mortality
Secondary outcomes
5. Nicotine consumption 6. Use of other substances 7. Side effects for the mother 8. Side effects for the child
Search methods for identification of studies
Electronic searches
For this update, we revised all our search strategies in line with current Cochrane Drugs and Alcohol Group practices. We searched the following databases up to 18 February 2020:
Cochrane Drugs and Alcohol Group (CDAG) Specialised Register (searched 18 February 2020) Appendix 1;
Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Register of Studies (CRS‐Web); (searched 18 February 2020) Appendix 2;
MEDLINE (OVID) (2013 to 18 February 2020) Appendix 3;
Embase (OVID) (2013 to 18 February 2020) Appendix 4;
PsycINFO (Ovid) (2013 to 18 February 2020) Appendix 5;
CINAHL (EBSCO Host) (2013 to 18 February 2020) Appendix 6;
Web of Science (2013 to 18 February 2020) Appendix 7.
We searched the following trials registries on 18 February 2020:
ClinicalTrials.gov (clinicaltrials.gov);
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/).
Details of the previous search strategies are available in Minozzi 2013.
Searching other resources
We checked the bibliographies of included studies and relevant reviews for further references to relevant trials.
We contacted the authors of included studies and experts in the field in various countries to find out if they knew any other published or unpublished controlled trials.
We did not apply any language restrictions.
Data collection and analysis
Selection of studies
Two authors (Minozzi, Bellisario) independently inspected the search hits by reading titles and abstracts. We obtained each potentially relevant study located by the search in full text and the two authors assessed each for inclusion independently. Doubts were resolved by discussion between the authors.
Data extraction and management
Two authors (Minozzi, Bellisario) independently extracted data from studies using a standardised checklist. Any disagreement was resolved by discussion.
Assessment of risk of bias in included studies
Two authors (Minozzi, Bellisario) independently performed the 'Risk of bias' assessment for RCTs and "Controlled Clinical Trials"(CCTs) using the criteria recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The recommended approach for assessing the risk of bias in studies included in Cochrane Reviews is a two‐part tool, addressing six specific domains, namely: sequence generation and allocation concealment (selection bias), blinding of participants and providers (performance bias), blinding of outcome assessor (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias). The first part of the tool involves describing what was reported to have happened in the study. The second part of the tool consists of assigning a judgement relating to the risk of bias for that entry in terms of low, high or unclear risk. To make these judgements, we used the criteria indicated in the Cochrane Handbook for Systematic Reviews of Interventions adapted to the addiction field. See Appendix 8 for details.
We considered blinding of participants, personnel and outcome assessors (avoidance of performance bias and detection bias) separately for objective outcomes (e.g. dropouts, use of the substance of abuse measured by urine analysis, participants relapsed at the end of follow‐up, participants engaged in further treatment) and subjective outcomes (e.g. duration and severity of signs and symptoms of withdrawal, patient self‐reported use of the substance, side effects).
We considered incomplete outcome data (avoidance of attrition bias) for all outcomes except for dropout from the treatment, which is very often the primary outcome measure in trials on addiction.
Grading of evidence
We assessed the overall quality of the evidence for the primary outcomes and the secondary outcome "side effects" using the GRADE system. The Grading of Recommendation, Assessment, Development and Evaluation Working Group (GRADE) developed a method for grading the quality of evidence (Schunemann 2013), which takes into account issues not only related to internal validity but also external validity, such as directness of results. The 'Summary of findings' tables presents the main findings of a review in a transparent and straightforward tabular format. In particular, they provide crucial information concerning the quality of evidence, the magnitude of the effect of the interventions examined and the sum of available data on the primary outcomes.
The GRADE system uses the following criteria for assigning grades of evidence:
High: further research is very unlikely to change our confidence in the estimate of effect.
Moderate: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low: any estimate of effect is very uncertain.
Grading is decreased for the following reasons:
Serious (‐1) or very serious (‐2) limitation to study quality.
Important inconsistency (‐1).
Some (‐1) or major (‐2) uncertainty about directness.
Imprecise or sparse data (‐1).
High probability of reporting bias (‐1).
Measures of treatment effect
We analysed dichotomous outcomes by calculating the risk ratio (RR) for each trial with the uncertainty in each result being expressed by its confidence interval. We analysed continuous outcomes by calculating the mean difference (MD) or the standardised mean difference (SMD) with 95% CI. For nicotine use, we compared the contrast of the mean number of cigarettes smoked from baseline to end of treatment in the experimental and control groups. In the case of missing standard deviations (SDs) for the difference from baseline to the end of treatment, we imputed the SD using the SD of the mean at the end of treatment for each group.
We did not use data presented as the number of positive urine tests over the total number of tests in the experimental and control group as a measure of substance abuse. This is because using tests instead of participants as the unit of analysis violates the hypothesis of independence among observations. In fact, the results of tests done in each participant are not independent.
Unit of analysis issues
If multi‐arm studies were included in the meta‐analyses and one arm was considered more than once in the same comparisons (e.g. two different dosages of drugs compared with the same control group), we combined all the relevant experimental groups into a single group and we compared it with the control to avoid double counting of participants in the control groups. No cross‐over or cluster‐randomised trials were expected to be found because these study desings are not adequate with these types of participants and of interventions .
Dealing with missing data
For the analysis of binary outcome data (number of women using heroin), all randomised patients were included in the statistical analysis, with those who dropped out or were lost to follow‐up assigned to the 'using drug' category. For continuous outcomes, only the available data were considered.
Assessment of heterogeneity
We analysed heterogeneity by means of the I2 statistic and the Chi2 test for heterogeneity. The cut points were an I2 value > 50% and a P‐value of the Chi2 test of < 0.1.
Assessment of reporting biases
We intended to use funnel plots (plots of the effect estimate from each study against the standard error) to assess the potential for bias related to the size of the trials, which could indicate possible publication bias, if a sufficient number of studies (i.e. at least ten studies) were included. If asymmetry had been found, we would have conducted the Egger test (Egger 1997).
Data synthesis
We combined the outcome measures from the individual trials through meta‐analysis where possible (good comparability of intervention and outcomes between trials). We used the random‐effect model because we expected a certain degree of heterogeneity among trials
Subgroup analysis and investigation of heterogeneity
No subgroup analyses were planned. In case of substantial heterogeneity (i.e. I2 value > 90%) and inconsistency in the direction of effect, meta‐analysis was not done.
Sensitivity analysis
To incorporate the assessment of risk of bias into the review process, we first plotted the intervention effect estimates against the evaluation of risk of bias. We inspected the results stratified for risk of bias. If we found significant associations between the measure of effect and risk of bias, we excluded studies with a high risk of bias from the analysis. The items considered in the sensitivity analysis were: random sequence generation, allocation concealment and blinding of personnel and outcome assessors.
Results
Description of studies
Results of the search
In the previous version of our review (Minozzi 2013), we retrieved a total of 1385 records. Once duplicates had been removed, we had a total of 968 records. We excluded 933 records based on titles and abstracts. We obtained the full text of the remaining 35 records. We excluded 20 studies. We included four studies reported in 15 references (see Characteristics of included studies). For a further description of our screening process, see the study flow diagram (Figure 1).
1.
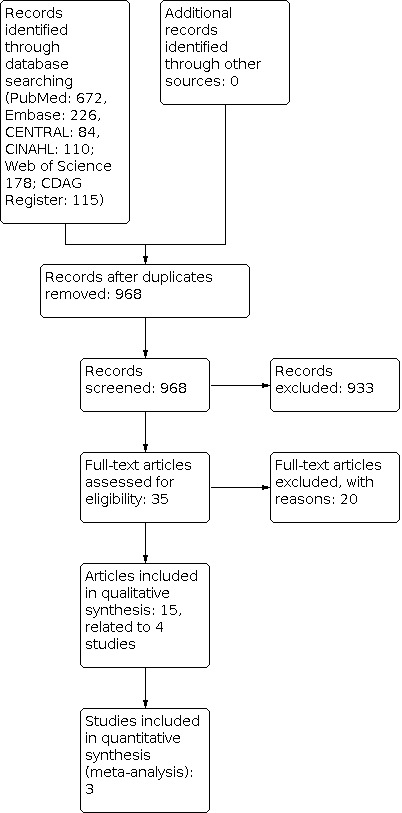
Study flow diagram September 2013.
As shown in Figure 2, our update searches identified 633 records. Once duplicates had been removed, we had a total of 467 records. We screened out 462 references based on titles and abstracts. We examined the remaining five records in full text and excluded one (see Characteristics of excluded studies). We did not include new studies; the remaining four records are new reposts of a previously included study (MOTHER Study). We identified one ongoing study (NCT 03098407).
2.
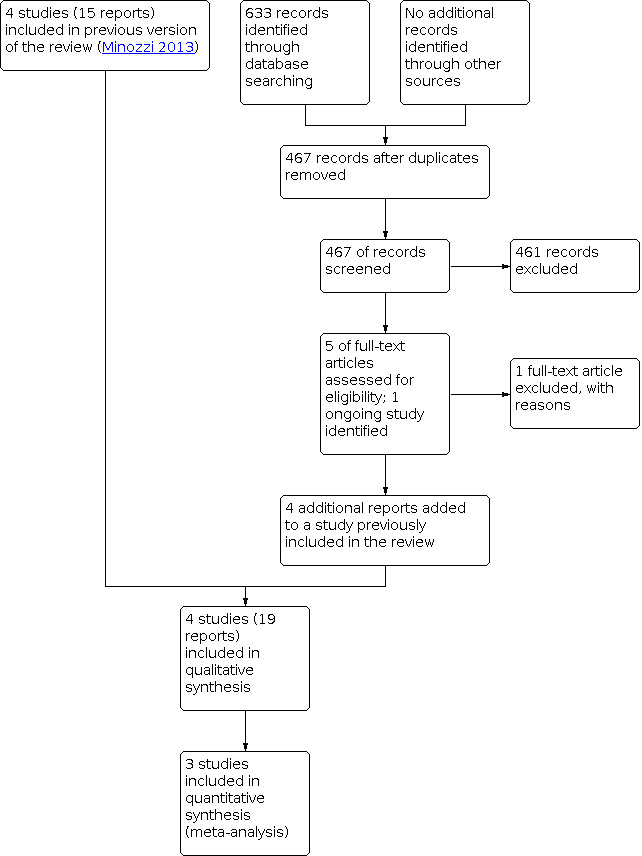
Study flow diagram February 2020.
Included studies
Four studies with 271 participants met the inclusion criteria for this review.
Duration of trials
The mean duration of the trials was 16.3 weeks (range 15 to 18 weeks).
Treatment regimens and settings
Two trials were conducted in Austria (Fischer 1999; Fischer 2006) and one in the USA (Jones 2005). The MOTHER study is a multicentre, international study conducted in Austria, Canada and the USA.
Three trials compared a methadone dose of between 20 and 140 mg/day with a buprenorphine dose of between 2 and 32 mg/day (Fischer 2006; Jones 2005; MOTHER Study). One trial compared methadone (mean dose at delivery 53.48 mg) with oral slow‐release morphine (mean dose at delivery 300.43 mg) (Fischer 1999).
Three studies were conducted in an outpatient setting (Fischer 1999; Fischer 2006; MOTHER Study) and one in an inpatient setting (Jones 2005).
Participants
Two hundred seventy‐one opiate‐dependent pregnant women meeting the DSM‐IV criteria were included in the studies. The mean age of participants was 27.3 years. The mean gestational age was 22 weeks. Nicotine use during pregnancy was reported only in one trial (Fischer 1999) as a mean number of cigarettes per day: it was 27.56 (SD 26.28) for the methadone group and 31.30 (SD 22.56) for the morphine group.
Rating instruments utilised in the studies
All the included studies measured neonatal abstinence syndrome using the Finnegan scale (Finnegan 1992), but the MOTHER Study used a modified Finnegan scale (called the MOTHER neonatal abstinence syndrome scale), which includes 28 items with 19 items used for scoring and medication decisions. Scores on the modified scale range from 0 to 42, with higher scores indicating more severe withdrawal. Original neonatal abstinence syndrome item definitions, as well as the morphine medication protocol, were refined before data collection.
Comparisons
Comparison 1
Methadone versus buprenorphine was compared in three trials with 223 participants (Fischer 2006; Jones 2005; MOTHER Study).
Comparison 2
Methadone versus slow‐release morphine was compared in one trial with 48 participants (Fischer 1999).
Excluded studies
Twenty‐one studies did not meet the criteria for inclusion in this review. The grounds for exclusion were: study design (13 studies) (Bandstra 2012; Binder 2008; Ebner 2007; Fisher 1998; Gordon 2004; Hulse 2004; Keyser‐Marcus 2002; Jones 2008; Lacroix 2011; Laken 1997; Martin 2011; Newman 2009; Stine 2009), type of participants (four studies) (Bell 2007; Dawe 2007; Jackson 2004; Suchman 2007), type of experimental intervention (two studies) (Carroll 1995; Cochran 2019) and type of control intervention (two studies) (Jones 2011; Tuten 2012).
Risk of bias in included studies
See Figure 3 and Figure 4. All of the studies were randomised controlled trials.
3.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
4.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation
Only one study (Jones 2005) used a random sequence generation method and was at low risk of selection bias. We judged all the other studies to be at unclear risk of bias.
Allocation concealment
There was a low risk of bias for allocation concealment in three studies (Fischer 2006; Jones 2005; MOTHER Study) and an unclear risk in the fourth study (Fischer 1999).
Blinding
Subjective outcomes
We judged one study (Fischer 1999) to be at a high risk of performance and detection bias because it was an open‐label study. All the other studies were double‐blind, and we judged them to be at a low risk of bias.
Objective outcomes
We judged all four studies to be at a low risk of performance and detection bias.
Incomplete outcome data
Only one study had no attrition (Fischer 1999). We judged the other three to be at high risk of attrition bias because the attrition rate was high and unbalanced between groups.
Selective reporting
Only one study (MOTHER Study) had a protocol published before the completion of the study; it was judged at low risk of selective reporting because the results of all the predefined outcomes were reported. The other studies were judged to be at unclear risk because no protocol was available
Effects of interventions
Comparison 1: Methadone versus buprenorphine
See Table 1.
Primary outcomes: for the woman
1. Dropouts from treatment
We analysed the number of participants who did not complete the treatment (Fischer 2006; Jones 2005; MOTHER Study): There was no evidence of a difference between treatments (RR 0.66, 95% confidence interval (CI) 0.37 to 1.20, 223 participants, three studies, moderate quality evidence). (Analysis 1.1).
1.1. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 1: Dropout rate
2. Use of primary substance of abuse
2.1 During or at the end of treatment
We pooled two trials (Jones 2005, MOTHER Study) with 151 participants. There was no evidence of a difference between treatments (RR 1.81, 95% CI 0.70 to 4.68, low quality evidence) (Analysis 1.2).
1.2. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 2: Use of primary substance
2.2 At follow‐up
None of the studies considered this outcome.
3. Obstetric outcomes
3.1 Third trimester bleeding
Data for this outcome were not reported in any of the included studies.
3.2 Preterm delivery
In Fischer 2006, three children were delivered prematurely in the methadone group and two in the buprenorphine group (one at week 34, one at week 35 and three at week 36). In Jones 2005, there was one preterm birth in the methadone group (week not reported). In the MOTHER Study, there were 19% preterm deliveries in the methadone group and 7% in the buprenorphine group. There was no evidence of a difference between treatments.
3.3 Fetal distress and meconium aspiration
Data for this outcome were not reported in Jones 2005 and Fischer 2006. In the MOTHER Study, there was one case of meconium aspiration in the buprenorphine group.
3.4 Caesarean section
In Jones 2005, all but one birth in each group were vaginal. In Fischer 2006, two women maintained on buprenorphine were delivered by planned caesarean section at week 40. In the MOTHER Study, there were 37% of caesarean sections in the methadone group and 29% in the buprenorphine group. There was no evidence of a difference between treatments.
3.5 Abnormal presentation
In Jones 2005, all births were normal presentation. Data were not reported in Fischer 2006. In the MOTHER Study, there were 14% abnormal fetal presentations in the methadone group and 5% in the buprenorphine group. There was no evidence of a difference between treatments.
3.6 Medical complications at delivery
In Fischer 2006, one woman in the methadone group required vacuum extraction due to a prolonged delivery. No medical complications occurred in Jones 2005. In the MOTHER Study, there were 51% medical complications at delivery in the methadone group and 31% in the buprenorphine group (P = 0.03).
3.7 Breastfeeding following delivery
Data were not reported in any of the included studies.
3.8 Puerperal morbidity
No cases of puerperal morbidity were observed in Jones 2005 or in the MOTHER Study. Data were not reported in Fischer 2006.
Primary outcomes: for the child
4. Health status
4.1 Birth weight
Two studies (Jones 2005; MOTHER Study) with 150 participants reported data for this outcome (one mother in the buprenorphine group delivered twins; twin data were not considered for this outcome because it could be altered by twin status). The results were in favour of buprenorhine in both studies: MD; ‐530.00 g (95%CI ‐662.78 to ‐397.22) in Jones 2005 and MD: ‐215.00 g (95%CI ‐238.93 to ‐191.07) in the MOTHER Study; data were not pooled due to high heterogeneity ( P < 0.00001, I2 = 95%). Quality of evidence was judged as very low.The third study (Fischer 2006) did not report data but stated that there was no evidence of a difference between treatments in birth weight (mean 2820 g).
4.2 APGAR score (Activity, Pulse, Grimace, Appearance and Respiration score) at five minutes
We pooled two studies (Jones 2005; MOTHER Study) with 163 participants. There was no evidence of a difference between treatments (MD 0.00, 95% CI ‐0.03 to 0.03, low quality evidence) (Analysis 1.4;). The third study (Fischer 2006) did not report data but stated that there was no evidence of a difference between treatments in the APGAR score between groups.
1.4. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 4: APGAR score
4.3 Neonatal abstinence syndrome
We pooled the number of newborns treated for neonatal abstinence syndrome from three studies with 166 participants (Fischer 2006; Jones 2005; MOTHER Study). There was no evidence of a difference between treatments (RR 1.19; 95% CI 0.87 to 1.66, low quality evidence) (Analysis 1.5).
1.5. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 5: Number treated for NAS
Neonatal abstinence syndrome peak score during the overall observation days were measured in two studies (Jones 2005; MOTHER Study). In Jones 2005 (21 participants), the results were methadone: 4.9, buprenorphine: 6.8 (SDs not provided); There was no evidence of a difference between treatments. In the MOTHER Study (131 participants), the results were methadone: 12.8 ± 0.6, buprenorphine: 11.0 ± 0.6 (P = 0.04), which is in favour of buprenorphine.
We pooled the mean duration of treatment for neonatal abstinence syndrome results from two studies (Fischer 2006; MOTHER Study) (145 participants). There was no evidence of a difference between treatments (MD 0.00; 95% CI ‐0.03 to 0.03) (Analysis 1.6).
1.6. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 6: Mean duration of NAS treatment
The total number of morphine drops administered was measured in one study with 21 participants (Jones 2005). The results were methadone: 93.1, buprenorphine: 23.6; There was no evidence of a difference between treatments.
Length of hospital stay was reported by two studies (Jones 2005; MOTHER Study) (152 participants). One study (Jones 2005) did not found signficant difference (MD 1.30,days, 95%CI 0.60, to 2.00), while the MOTHER Study repoted shorter hospital stay in the buprenorphin group: MD 6.70 days, 95%CI 6.24 to 7.16). Data were not pooled to very high heterogeneity (P < 0.00001, I2 = 99%) (Analysis 1.7).
1.7. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 7: Length of hospital stay
Total amount of morphine required to manage neonatal abstinence syndrome was reported in two studies (Fischer 2006; MOTHER Study) (145 participants). One study (Fischer 2006) did not found signficant diference (MD: 0.71mg, 95%CI ‐1.22,to 2.64), while the MOTHER Study reported significant less morphine required in the buprenorphine group (MD:9.30 mg, 95%CI 8.68 to 9.92) Data were not pooled to very high heterogeneity (P < 0.00001, I2 = 99%) (Analysis 1.8).
1.8. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 8: Total amount of morphine for NAS
4.4 Prenatal and neonatal mortality
In one study (Fischer 2006), there was one sudden intrauterine death at 38 weeks of pregnancy and one late abortion at 28 weeks of pregnancy, both in the methadone group. In the first woman, urine toxicology revealed 66% opioid‐positive results, 48% cocaine‐positive results and 16% benzodiazepine‐positive results over the study period. Cigarette consumption was a mean of 35 per day. In the second woman, all urine toxicology results were negative.
Secondary outcomes
5. Nicotine consumption
Smoking data were available from 124 (methadone n = 67 and buprenorphine n = 57) of the patients enrolled in the MOTHER Study. Among the sample, 95% reported cigarette smoking at treatment entry. Participants in the two medication conditions were similar for pretreatment characteristics, including smoking rates and daily cigarette amounts. Throughout the pregnancy, no meaningful changes in cigarette smoking were observed for either medication condition. The fitted difference in change in adjusted cigarettes per day between the two conditions was small and non‐significant (â = 0.08, standard error (SE) = 0.05, P = 0.132).
6. Use of other substances Jones 2005 reported the percentage of results that were urine positive for each substance during the study period for the methadone and buprenorphine group, respectively. The results were cocaine: 15.6% and 16.7%; benzodiazepines: 0.4% and 2.5%; amphetamine: 0% and 0%; and marijuana 7.5% and 0%. The Fischer 2006 study reported the median number of urine samples positive for methadone and buprenorphine, respectively: cocaine: 0.00 and 0.00; benzodiazepines: 7.82 and 5.36. No data were reported in the MOTHER Study.
7. Side effects for the mother No side effects for the mothers were reported in the Jones 2005 and Fischer 2006 studies. In the MOTHER Study, there were 14/89 (16%) serious adverse events in the methadone group and 8/86 (9%) in the buprenorphine group (RR 1.69, 95% CI 0.75 to 3.83) (Analysis 1.9). There were fewer non‐serious adverse events in the buprenorphine group (66/86; 77%) compared to methadone (83/89; 93%) (RR 1.22, 95% CI 1.07 to 1.38, low quality evidence) (Analysis 1.10).
1.9. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 9: Serious AE for the mother
1.10. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 10: Serious AE for the child
8. Side effects for the child No side effects for the child were reported in the Jones 2005 and Fischer 2006 studies. In the MOTHER Study, there were more serious adverse events (6/73; 8%) in the methadone group than in the buprenorphine group (1/58; 2%) (RR 1.22, 95% CI 1.07 to 1.38) (Analysis 1.11). There was no significant difference in the frequency of non‐serious adverse events: 34/73 (47%) in the methadone group and 29/58 (50%) in the buprenorphine group (RR 1.08, 95% CI 0.74 to 1.59, low quality evidence). There was no evidence of a difference between treatments.
1.11. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 11: Non‐serious AE for the mother
Comparison 2: Methadone versus oral slow‐release morphine
See Table 2. This comparison included one study (Fischer 1999) with 48 participants.
Primary outcomes: for the woman
1. Dropouts from treatment
No participants dropped out from either group, low quality evidence.
2. Use of primary substance of abuse
2.1 During or at the end of treatment
The result for the number of participants who used heroin in the third trimester was RR 2.40 (95% CI 1.00 to 5.77) low quality evidence, in favour of oral slow‐release morphine (Analysis 2.1).
2.1. Analysis.

Comparison 2: Methadone versus oral slow‐release morphine, Outcome 1: Use of primary substance
2.2 At follow‐up
The study did not consider this outcome.
3. Obstetric outcomes
3.1 Third trimester bleeding
Data were not reported.
3.2 Preterm delivery
One woman delivered at 31 weeks due to early amniotic rupture, but it was not reported to which group she was allocated. No other gynaecological problems occurred during the study period. The mean week of delivery was as follows: methadone: 38.92 (SD 1.74), morphine: 37.79 (SD 2.55). There was no evidence of a difference between treatments.
3.3 Fetal distress and meconium aspiration
Data were not reported.
3.4 Caesarean section
The percentage of caesarean sections was 25% in both groups.
3.5 Abnormal presentation
Data were not reported.
3.6 Medical complications at delivery
The percentage of vacuum extractions was 8.3% in both groups.
3.7 Breastfeeding following delivery
Data were not reported.
3.8 Puerperal morbidity
Data were not reported.
Primary outcomes: for the child
4. Health status
4.1 Birth weight
There was no evidence of a difference between treatments (MD 124 g, 95% CI ‐186 to 434, low quality evidence) (Analysis 2.2).
2.2. Analysis.

Comparison 2: Methadone versus oral slow‐release morphine, Outcome 2: Birth weight
4.2 APGAR score
The study did not consider this outcome.
4.3 Neonatal abstinence syndrome
There was no evidence of a difference between treatments in the mean duration of neonatal abstinence syndrome (MD ‐5.00, 95% CI ‐10.97 to 0.97, low quality evidence) (Analysis 2.3).
2.3. Analysis.

Comparison 2: Methadone versus oral slow‐release morphine, Outcome 3: NAS mean duration
4.4 Prenatal and neonatal mortality
There was no prenatal or neonatal mortality in either group.
Secondary outcomes
5. Nicotine consumption
Fischer 1999 measured the difference in the mean number of cigarettes smoked per day before and at the end of treatment. At the start of the trial, the mean number of cigarettes smoked per day was 27.56 (SD 16.28) and 31.30 (SD 22.56) for the methadone and morphine group, respectively. At delivery, it was 15.89 (SD 12.24) and 15.20 (SD 8.24), respectively (MD ‐4.43, 95% CI ‐1.47 to 10.33); There was no evidence of a difference between treatments (Analysis 2.4).
2.4. Analysis.

Comparison 2: Methadone versus oral slow‐release morphine, Outcome 4: Nicotine consumption
6. Use of other substances
The study only reported the percentage of negative urine testing during each week of treatment for methadone and slow‐release morphine in a graph: the mean percentages for the whole study period were about 95% and 90%, respectively, for cocaine and 54% and 89% for benzodiazepines.
7. Side effects for the mother
No side effects for the mother were reported;(low quality evidence) .
8. Side effects for the child
No severe complications were noted in any of the neonates as monitored by polysomnography, although one child in the methadone group had central apnoea, and one child in the morphine group had obstructive apnoea; (low quality evidence) .
Sensitivity analysis
The only difference among the trials in terms of risk of bias was in random sequence generation (we judged one as at low risk and two as at unclear risk of bias). No differences were found in the results when studies were stratified for risk of bias for random sequence generation. Therefore, we did not perform sensitivity analyses.
Assessment of reporting bias
We did not use a funnel plot to explore publication bias because only four studies were included, all with small sample sizes. In fact, the power of this method is very limited when meta‐analysis comprises only a few small studies (Higgins 2011).
Discussion
Summary of main results
Only four trials with 271 pregnant women satisfied the criteria for inclusion in the review. Three (Fischer 2006; Jones 2005; MOTHER Study) compared methadone with buprenorphine (223 participants), and one (Fischer 1999) compared methadone with oral slow‐release morphine (48 participants).
In the comparison of methadone versus buprenorphine, we found moderate‐quality evidence of little or no difference in the dropout rate of the mothers. We also found low‐quality evidence of no difference in the use of the primary substance between the methadone and buprenorphine groups. Birth weight was higher in the buprenorphine group in the two trials that repoterd data, but the quality of evidence is very low. The third study reported that there was no evidence of a difference between treatments. For the APGAR score, none of the studies found a significant difference, with low‐quality evidence. Many measures were used in the studies to assess neonatal abstinence syndrome. For the number of newborns treated for neonatal abstinence syndrome, the most critical outcome, we found low‐quality evidence of no significant difference.
In the comparison of methadone versus oral slow‐release morphine, we found no difference in the dropout rate, whereas slow‐release morphine seemed to be superior to methadone for abstinence of women from the use of heroin. The study did not find evidence of a difference between treatments in birth weight or mean duration of neonatal abstinence syndrome. The APGAR score was not considered in the study. We judged the quality of evidence to be low for all outcomes.
Only one study which compared methadone with buprenorphine reported side effects. For the mother, there was no significant difference between groups in the frequency of serious adverse events, while the non‐serious adverse events were fewer in the buprenorphine groups. There were no significant differences in the frequency of severe or non‐severe adverse events for the newborn. The quality of evidence was low.
In the comparison of methadone versus slow‐release morphine, no side effects were reported for the mother, whereas one child in the methadone group had central apnoea, and one child in the morphine group had obstructive apnoea.
The difficulty of determining whether the opioid substitution is associated with better outcomes for newborns always needs to be considered in relation to the direct effects of cigarette smoking. Only one study (Fischer 1999) reported data on cigarette consumption at the start of the study and at delivery. Women smoked a mean of 29 cigarettes per day at enrollment in the study and a mean of 14 cigarettes per day at delivery. There was no statistically significant difference between groups in the reduction of cigarettes smoked. This seems to be a relevant outcome and was not considered by the majority of the included studies. The level of nicotine exposure during pregnancy does affect birth weight and could affect neonatal abstinence syndrome.
Overall completeness and applicability of evidence
The number of included studies and participants is too small to allow definite conclusions. Although, from a clinical point of view, it is well recognised that, for both women opiate addicts and their infants, agonist treatment during pregnancy is protective, but many questions remain unanswered. Which is the most effective drug treatment and at what dosage? What is the most appropriate type of setting? In particular, is it useful or not to associate any type of psychosocial intervention with pharmacological treatment?
Furthermore, it would be useful to know, both for maternal and child health, whether the mothers continued to use maintenance treatments after their delivery.
Quality of the evidence
Three out of four studies had adequate allocation concealment and were double‐blind. The major flaw of the studies was attrition bias: three out of four had a high dropout rate (30% to 40%), and this was unbalanced between groups. In the comparison of methadone versus buprenorphine, quality of the evidence ranged from moderate to very low and was downgraded for risk of attrition bias, inconsistency and imprecision of the estimate. In the comparison of methadone versus slow‐release morphine, quality of the evidence was low and was downgraded for imprecision in the estimate due to a very small sample size.
Potential biases in the review process
To lower the risk of bias in the review process, two review authors independently screened abstracts, assessed full texts, rated risk of bias for included studies and extracted data from primary studies. None of the review authors has any personal, scientific or financial conflicts of interest or expected advantages from significant results in terms of reviewer decisions or raising funds, We could not inspect funnel plots for risk of possible publication bias due to the small number of studies included in the meta‐analyses; however, we did not find any unpublished studies, despite contacting all of the first authors of the included studies and searching conference proceedings.so the likelihood of publication bias can be considered low" .
Agreements and disagreements with other studies or reviews
We did not find any other systematic reviews on this topic. One narrative review published in 2008 (Winklbaur 2008) considered all types of treatment for pregnant opioid‐dependent women and included both randomised and non‐randomised studies. This review cited the three randomised controlled trials (RCTs) published before 2006 and concluded that buprenorphine and methadone are substantially equivalent but may attenuate neonatal abstinence syndrome. A mixed‐method systematic review of interventional and observational systematic reviews identified 3 RCTs (n = 223), and 15 cohort observational (OBS) (n = 1923) studies to assess the safety of buprenorphine compared with methadone to treat pregnant women with opioid use disorder (Zedler 2016). Considering methadone as comparator, buprenorphine was found to be associated with lower risk of preterm birth (RCT risk ratio (RR) 0.40, 95% CI 0.18 to 0.91; OBS RR 0.67, 95% CI 0.50 to 0.90), and greater birth weight (RCT weighted mean difference (MD) 277 g, 95% CI 104 to 450; OBS MD 265 g, 95% CI 196 to 335). Authors concluded that methadone presents with a lower risk of preterm birth, and greater birth weight compared with buprenorphine treatment of maternal opioid use disorder during pregnancy.
An older published narrative review (Jones 2012) compared buprenorphine with methadone and included the same three RCTs together with observational studies but did not pool the data in a meta‐analysis. This review reached the same conclusions, reporting that there was no significant difference between methadone and buprenorphine for maternal outcomes, whereas buprenorphine "...results in a clinically significant less severe neonatal abstinence syndrome (NAS) than treatment with methadone". They also stated, "...concluding that buprenorphine is an effective treatment for opioid dependence during pregnancy does not mean that methadone should no longer be considered a useful and effective medication for opioid dependence, nor does it mean that all opioid‐dependent pregnant women should be treated with buprenorphine without regard to their preferences and life circumstances."
Authors' conclusions
Implications for practice.
Methadone and buprenorphine may be substantially similar in efficacy and safety for the treatment of opioid‐dependent pregnant women and their babies. There is not enough evidence to make conclusions for the comparison between methadone and slow‐release morphine. Overall, the body of evidence is too small to draw firm conclusions. about the equivalence of the treatments compared. Many questions remain unanswered. Which is the most effective drug treatment and at what dosage? What is the most appropriate type of setting? In particular, is it useful or not to associate any type of psychosocial intervention with pharmacological treatment?
Implications for research.
Large randomised controlled trials which compare different pharmacological maintenance treatments are still needed, with longer follow‐up periods (ideally up to one year) and which also consider as relevant outcomes the level of nicotine exposure, concomitant use during pregnancy of other prescribed medications (such as selective serotonin reuptake inhibitors and benzodiazepines) and use of non‐prescribed drugs such as cocaine, alcohol and marijuana. Moreover, studies assessing the effectiveness of psychosocial treatments in addition to pharmacological treatments versus pharmacological treatments alone should be conducted.
What's new
| Date | Event | Description |
|---|---|---|
| 10 March 2020 | New citation required but conclusions have not changed | No new studies included |
| 10 March 2020 | New search has been performed | New search |
History
Protocol first published: Issue 1, 2007 Review first published: Issue 2, 2008
| Date | Event | Description |
|---|---|---|
| 10 December 2013 | New citation required and conclusions have changed | Conclusions changed |
| 10 December 2013 | New search has been performed | New search, new trials |
| 20 October 2008 | Amended | Contact details updated |
| 26 March 2008 | Amended | Converted to new review format |
| 8 January 2008 | New citation required and conclusions have changed | Substantive amendment. |
Acknowledgements
We would like to thank Zuzana Mitrova for developing and running the search strategies and for her help in the editorial process.
Appendices
Appendix 1. Cochrane Drugs and Alcohol Group Specialised Register search strategy
February 18, 20120 (5 hits)
#1 MESH DESCRIPTOR Opiate Substitution Treatment EXPLODE ALL AND INREGISTER #2 (maintenance near2 (therapy OR treatment)) AND INREGISTER #3 (MMT or BMT or OST) AND INREGISTER #4 #1 OR #2 OR #3 #5 MESH DESCRIPTOR Pregnancy EXPLODE ALL AND INREGISTER #6 (pregnan* or prenatal* or perinatal* or antenatal* or mother or matern*) AND INREGISTER #7 #5 OR #6 #8 #7 AND #4 #9 >2012:YR AND INREGISTER
Appendix 2. CENTRAL search strategy
CENTRAL (via crsweb.cochrane.org)
February 18, 20120 (87 hits)
#1 MESH DESCRIPTOR Opioid‐Related Disorders EXPLODE ALL AND CENTRAL:TARGET
#2 ((drug or substance) near (abuse* or addict* or dependen* or disorder*)):ti,ab,kw AND CENTRAL:TARGET
#3 ((opioid* or opiate*) near (abuse* or addict* or dependen* or mainten*)):ti,ab,kw AND CENTRAL:TARGET
#4 #1 OR #2 OR #3
#5 MESH DESCRIPTOR Opiate Substitution Treatment EXPLODE ALL AND CENTRAL:TARGET
#6 (maintenance near2 (therapy OR treatment)) AND CENTRAL:TARGET
#7 (MMT or BMT or OST):ti,ab AND CENTRAL:TARGET
#8 heroin or methadone or buprenorphine or codeine or morphine or LAAM AND CENTRAL:TARGET
#9 #5 OR #6 OR #7 OR #8
#10 #4 AND #9
#11 MESH DESCRIPTOR Pregnancy EXPLODE ALL AND CENTRAL:TARGET
#12 (pregnan* or prenatal* or perinatal* or antenatal* or mother or matern*):ti,ab,kw AND CENTRAL:TARGET
#13 MESH DESCRIPTOR Pregnant Women EXPLODE ALL AND CENTRAL:TARGET
#14 #11 OR #12 OR #13
#17 #4 AND #10 AND #14
Appendix 3. MEDLINE search strategy
February 18, 20120 (74 hits)
exp Opioid‐Related Disorders/
((drug or substance) and (abuse* or addict* or dependen* or disorder*)).mp.
((opioid* or opiate*) and (abuse* or addict* or dependen* or mainten*)).mp.
1 or 2 or 3
Opiate Substitution Treatment/
(maintenance adj2 (therapy or treatment)).mp.
(MMT or BMT or OST).ti,ab.
(heroin or methadone or buprenorphine or codeine or morphine or LAAM).mp.
5 or 6 or 7 or 8
exp Pregnancy/
Pregnant Women/
exp Pregnancy Complications/
(pregnan* or prenatal* or perinatal* or antenatal* or mother or matern*).ti,ab.
10 or 11 or 12 or 13
4 and 9 and 14
randomized controlled trial.pt.
controlled clinical trial.pt.
random*.ab.
placebo.ab.
clinical trials as topic.sh.
random allocation.sh.
trial.ti.
16 or 17 or 18 or 19 or 20 or 21 or 22
exp animals/ not humans.sh.
23 not 24
15 and 25
limit 26 to yr="2013 ‐Current
Appendix 4. Embase search strategy
February 18, 20120 (97 hits)
opiate addiction/
addiction/
((drug or substance or opioid* or opiat*) adj5 (abuse* or addict* or depend* or disorder*)).mp.
1 or 2 or 3
opiate substitution treatment/
(heroin or methadone or buprenorphine or codeine or morphine or LAAM).mp.
(maintenance adj2 (therapy or treatment)).mp.
(MMT or BMT or OST).ti,ab.
9 5 or 6 or 7 or 8
pregnancy/
pregnant woman/
pregnancy complication/
(pregnan* or prenatal* or perinatal* or antenatal* or mother or matern*).ti,ab.
10 or 11 or 12 or 13
4 and 9 and 14
crossover‐procedure/ or double‐blind procedure/ or randomized controlled trial/ or single‐blind procedure/ or (random* or factorial* or crossover* or cross over* or placebo* or (doubl* adj blind*) or (singl* adj blind*) or assign* or allocat* or volunteer*).tw.
15 and 16
limit 17 to yr="2013 ‐Current
Appendix 5. CINAHL search strategy
February 18, 20120 (248 hits)
(MH "Substance Use Disorders+")
TX(drug N3 addict*) or TX(drug N3 dependen*) or TX(drug N3 abuse*)
TX(substance N3 addict*) or TX(substance N3 dependen*) or TX(substance N3 abuse*) or TX(substance N3 misus*)
TX(opioid* N3 addict*) or TX(opioid* N3 dependen*) or TX(opioid* N3 abuse*) orTX(opiate* N3 addict*) or TX(opiate* N3 dependen*) or TX(opiate* N3 abuse*)
S1 OR S2 OR S3 OR S4
MH "Heroin"
TX heroin
TX "Opioid substitution therapy" or TX(maintenance N3 therapy) or TX(maintenance N3 treatment)
TI(MMT or BMT or OST) or AB(MMT or BMT or OST)
(MH "Methadone")
TX (heroin or methadone or buprenorphine or codeine or morphine or LAAM)
S6 OR S7 OR S8 OR S9 OR S10 OR S11
(MH "Pregnancy+")
TX(pregnan* or prenatal* or perinatal* or antenatal* or mother or matern*)
S13 OR S14
S5 AND S12 AND S15
MH "Clinical Trials+"
PT Clinical trial
TI clinic* N1 trial* or AB clinic* N1 trial*
TI ( singl* or doubl* or trebl* or tripl* ) and TI ( blind* or mask* )
AB ( singl* or doubl* or trebl* or tripl* ) and AB ( blind* or mask* )
TI randomi?ed control* trial* or AB randomi?ed control* trial*
MH "Random Assignment"
TI random* allocat* or AB random* allocat*
MH "Placebos"
TI placebo* or AB placebo*
MH "Quantitative Studies"
S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27
S16 AND S28
Appendix 6. PsycINFO search strategy
February 18, 20120 (34 hits)
exp Drug Addiction/ or intravenous drug usage/
((drug or substance) adj5 (abuse* or addict* or dependen* or disorder*)).mp.
((opioid* or opiate*) adj5 (abuse* or addict* or dependen* or mainten*)).mp.
1 or 2 or 3
(maintenance adj2 (therapy or treatment)).mp.
(MMT or BMT or OST).ti,ab.
(heroin or methadone or buprenorphine or codeine or morphine or LAAM).mp.
5 or 6 or 7
4 and 8
exp Pregnancy/
(pregnan* or prenatal* or perinatal* or antenatal* or mother or matern*).mp.
10 or 11
9 and 12
exp Clinical Trials/
(random* or (clinical adj3 trial*) or (reserch adj3 design*) or (evaluat adj3 stud*) or (prospective* adj3 stud*)).tw.
((singl* or doubl* or trebl* or tripl*) adj3 (blind* or mask*)).tw.
14 or 15 or 16
13 and 17
limit 18 to yr="2013 ‐Current"
Appendix 7. Web of Science search strategy
February 18, 20120 (88 hits)
TS=((opioid* OR opiate* OR opium OR heroin OR methadone) same (abuse* or addict* or dependen* or disorder*))
TS=(heroin or methadone or buprenorphine or codeine or morphine or LAAM or BMT or MMT or OST)
TS="Opioid substitution therapy"
#3 OR #2
#4 AND #1
TS=(pregnan* or prenatal* or perinatal* or antenatal* or mother or matern*)
#6 AND #5
TS=(randomi* OR randomly OR placebo* OR trial*)
#8 AND #7
Appendix 8. 'Risk of bias' assessment criteria
| Item | Judgement | Description |
| 1. Random sequence generation (selection bias) | Low risk | The investigators describe a random component in the sequence generation process such as: random number table; computer random number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing of lots; minimisation |
| High risk | The investigators describe a non‐random component in the sequence generation process such as: odd or even date of birth; date (or day) of admission; hospital or clinic record number; alternation; judgement of the clinician; results of a laboratory test or a series of tests; availability of the intervention | |
| Unclear risk | Insufficient information about the sequence generation process to permit judgement of low or high risk | |
| 2. Allocation concealment (selection bias) | Low risk | Investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based and pharmacy‐controlled randomisation); sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes |
| High risk | Investigators enrolling participants could possibly foresee assignments because one of the following methods was used: open random allocation schedule (e.g. a list of random numbers); assignment envelopes without appropriate safeguards (e.g. if envelopes were unsealed or nonopaque or not sequentially numbered); alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure | |
| Unclear risk | Insufficient information to permit judgement of low or high risk. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement | |
| 3. Blinding of participants and providers (performance bias) Objective outcomes |
Low risk |
No blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding
Blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken |
| High risk | No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding Blinding of key study participants and personnel attempted, but likely that the blinding could have been broken, and the outcome is likely to be influenced by lack of blinding | |
| Unclear risk | Insufficient information to permit judgement of low or high risk | |
| 4. Blinding of participants and providers (performance bias) Subjective outcomes |
Low risk |
Blinding of participants and providers and unlikely that the blinding could have been broken |
| High risk | No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding Blinding of key study participants and personnel attempted, but likely that the blinding could have been broken, and the outcome is likely to be influenced by lack of blinding | |
| Unclear risk | Insufficient information to permit judgement of low or high risk | |
| 5. Blinding of outcome assessor (detection bias) Objective outcomes |
Low risk |
No blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding Blinding of outcome assessment ensured, and unlikely that the blinding could have been broken |
| High risk | No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding Blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement is likely to be influenced by lack of blinding |
|
| Unclear risk | Insufficient information to permit judgement of low or high risk | |
| 6. Blinding of outcome assessor (detection bias) Subjective outcomes |
Low risk |
No blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding Blinding of outcome assessment ensured, and unlikely that the blinding could have been broken |
| High risk | No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding Blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement is likely to be influenced by lack of blinding |
|
| Unclear risk | Insufficient information to permit judgement of low or high risk | |
| 7. Incomplete outcome data (attrition bias) For all outcomes except retention in treatment or dropouts |
Low risk |
No missing outcome data Reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias) Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size Missing data have been imputed using appropriate methods All randomised patients are reported/analysed in the group they were allocated to by randomisation irrespective of non‐compliance and co‐interventions (intention‐to‐treat) |
| High risk | Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size 'As‐treated' analysis done with substantial departure of the intervention received from that assigned at randomisation |
|
| Unclear risk | Insufficient information to permit judgement of low or high risk (e.g. number randomised not stated, no reasons for missing data provided; number of dropouts not reported for each group) | |
| 8. Selective reporting (reporting bias) | Low risk | The study protocol is available and all of the study’s prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were prespecified (convincing text of this nature may be uncommon) |
| High risk | Not all of the study’s prespecified primary outcomes have been reported One or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not prespecified One or more reported primary outcomes were not prespecified (unless clear justification for their reporting is provided, such as an unexpected adverse effect) One or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis. The study report fails to include results for a key outcome that would be expected to have been reported for such a study |
|
| Unclear risk | Insufficient information to permit judgement of low or high risk |
Data and analyses
Comparison 1. Methadone versus buprenorphine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Dropout rate | 3 | 223 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.37, 1.20] |
| 1.2 Use of primary substance | 2 | 151 | Risk Ratio (M‐H, Random, 95% CI) | 1.81 [0.70, 4.68] |
| 1.3 Birth weight | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.4 APGAR score | 2 | 163 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.03, 0.03] |
| 1.5 Number treated for NAS | 3 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.87, 1.63] |
| 1.6 Mean duration of NAS treatment | 2 | 145 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.03, 0.03] |
| 1.7 Length of hospital stay | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.8 Total amount of morphine for NAS | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.9 Serious AE for the mother | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.75, 3.83] |
| 1.10 Serious AE for the child | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.77 [0.59, 38.49] |
| 1.11 Non‐serious AE for the mother | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [1.07, 1.38] |
| 1.12 Non‐serious AE for the child | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.74, 1.59] |
1.3. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 3: Birth weight
1.12. Analysis.

Comparison 1: Methadone versus buprenorphine, Outcome 12: Non‐serious AE for the child
Comparison 2. Methadone versus oral slow‐release morphine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Use of primary substance | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.40 [1.00, 5.77] |
| 2.2 Birth weight | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 124.00 [‐186.94, 434.94] |
| 2.3 NAS mean duration | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐5.00 [‐10.97, 0.97] |
| 2.4 Nicotine consumption | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 4.43 [‐1.47, 10.33] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Fischer 1999.
| Study characteristics | ||
| Methods | Randomised controlled trial Open‐label | |
| Participants | Participants: 48 pregnant adults; mean age 26 years; 39.6% unmarried; duration of opioid dependence: mean 57.2 months Mean gestational age at entry: 22 weeks Inclusion criteria: opioid‐dependent and polysubstance abusing pregnant females meeting DSM‐IV criteria | |
| Interventions | (1) oral methadone (24 participants) versus (2) oral slow‐release morphine (24 participants) after an induction period of 10 days. At delivery, mean methadone dose was 53.48 mg; mean morphine dose was 300.43 mg Outpatients Follow‐up mean: 15 weeks | |
| Outcomes | Neonatal outcomes: fetal distress; birth weight; NAS (Finnegan scale) Maternal outcomes: retention; cocaine and benzodiazepine consumption (urinalysis); opioid use (identification of injection sites for morphine‐maintained group and urinalysis for methadone‐maintained group) |
|
| Notes |
Country: Austria Funding: grant from the Mayor of Vienna Conflict of interest : not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The women were randomly assigned to receive either oral methadone or oral slow‐release morphine, and induction occurred over a period of 10 days". |
| Allocation concealment (selection bias) | Unclear risk | No information provided concerning allocation concealment |
| Blinding of participants and personnel (performance bias) subjective outcomes | High risk | Open‐label |
| Blinding of participants and personnel (performance bias) objective outcomes | Low risk | COMMENT: open‐label trial but objective outcomes were unlikely to be biased by lack of blinding |
| Blinding of outcome assessment (detection bias) subjective outcomes | High risk | Open‐label |
| Blinding of outcome assessment (detection bias) objective outcomes | Low risk | COMMENT: open‐label trial but objective outcomes were unlikely to be biased by lack of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
Fischer 2006.
| Study characteristics | ||
| Methods | Randomised controlled trial Double‐blind | |
| Participants | Participants: 18 pregnant adults; mean age 25.9 years; 66.6% single; 61.1% completed 9 years of education; duration of heroin consumption: mean 20.6 months Mean gestational age at entry: 24 weeks Inclusion criteria: opioid‐dependent pregnant females meeting DSM‐IV criteria Exclusion criteria: severe somatic or other severe psychiatric diseases, high‐risk pregnancy | |
| Interventions | (1) oral methadone (9 participants) versus (2) oral buprenorphine (9 participants). Dose of methadone between 40 and 100 mg/day; dose of buprenorphine between 8 and 24 mg/day Outpatients Follow‐up: mean 16 weeks | |
| Outcomes | Neonatal outcomes: birth weight; NAS (Finnegan scale); child health status APGAR score Maternal outcomes: retention; maternal withdrawal symptoms (Wang Withdrawal Questionnaire); illicit drugs use: opioid, cocaine, benzodiazepine (urinalysis) |
|
| Notes |
Country: Austria Funding: Schering Plough provided an educational grant to Gabriele Fischer to employ personnel required to conduct this study. Conflict of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information concerning method of random sequence generation not provided |
| Allocation concealment (selection bias) | Low risk | Quote: "Subjects were randomised externally by the hospital pharmacy using a double‐blind, double‐dummy design and received supervised medication daily from the study pharmacist at the addiction clinic". |
| Blinding of participants and personnel (performance bias) subjective outcomes | Low risk | Quote: "To maintain study blinding, placebo treatment matched the active treatment. Methadone (EBEWE Arzneimittel GesmbH and Gatt/Koller GesmbH KG, Austria) was prepared at the hospital pharmacy as an oral solution at the required concentration. Placebo for the methadone arm consisted of 30 mg dextromethorphan oral solution (Nowak GmbH, Germany) to simulate the taste of methadone, as used previously in double‐dummy trials". |
| Blinding of participants and personnel (performance bias) objective outcomes | Low risk | Quote: "To maintain study blinding, placebo treatment matched the active treatment. Methadone (EBEWE Arzneimittel GesmbH and Gatt/Koller GesmbH KG, Austria) was prepared at the hospital pharmacy as an oral solution at the required concentration. Placebo for the methadone arm consisted of 30 mg dextromethorphan oral solution (Nowak GmbH, Germany) to simulate the taste of methadone, as used previously in double‐dummy trials". |
| Blinding of outcome assessment (detection bias) subjective outcomes | Low risk | Quote: "Neonates were observed for a minimum of 10 days on an in‐patient basis under blinded conditions for the mothers’ treatment condition and scored every 4 hours using the Finnegan scale (range 0–45)". Quote: "The double‐blind, double‐dummy code remained blinded until 30 days after delivery". |
| Blinding of outcome assessment (detection bias) objective outcomes | Low risk | Quote: "Neonates were observed for a minimum of 10 days on an in‐patient basis under blinded conditions for the mothers’ treatment condition and scored every 4 hours using the Finnegan scale (range 0–45)". Quote: "The double‐blind, double‐dummy code remained blinded until 30 days after delivery". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4 dropouts occurred during the study period. One participant maintained on methadone (70 mg/day) experienced a stillbirth caused by a sudden intrauterine death during week 38 of pregnancy. A second woman maintained on methadone had a late abortion during week 28. 2 other participants were withdrawn from the study due to lack of compliance with the scheduled visits. 1 patient was taking buprenorphine and the other methadone. This attrition left 14 participants who completed the study, 6 in the methadone group and 8 in the buprenorphine group. The 4 women who failed to complete the study were older and had a longer duration of opioid dependency than those who completed the study, whereas no significant differences in sociodemographic characteristics were seen at enrollment (see Table 1). COMMENT: high dropout (33.3%) in the methadone group and unbalanced (11.1% in the buprenorphine group) Reason for dropouts given and likely to be linked to treatments received |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
Jones 2005.
| Study characteristics | ||
| Methods | Randomised controlled trial Double‐blind | |
| Participants | Participants: 30 pregnant adults; mean age 30.1 years; 75% African‐American, 20% white, 5% other; 55% unemployed but seeking work, 40% unemployed and not seeking work, 5% homemakers; mean years of education 10.2; use of cocaine in past 30 days: 75%; opioid use: > 4 x day: 55%
Mean gestational age at entry: 23 weeks
Inclusion criteria: estimated gestational age of 16 to 30 weeks; opioid‐dependent pregnant females meeting DSM‐IV criteria Exclusion criteria: current diagnosis of alcohol abuse or dependence; self‐reported use of benzodiazepines; serious medical illness; diagnosis of preterm labour; evidence of fetal malformation; positive HIV test |
|
| Interventions | (1) Oral methadone (15 participants) versus (2) oral buprenorphine (15 participants). Dose of methadone: mean 60 mg/day; dose of buprenorphine: mean 12 mg /day Setting: inpatients Follow‐up mean: 18 weeks | |
| Outcomes | Neonatal outcomes: number of neonates treated for NAS; peaks of NAS score; length of neonatal hospitalisation; birth weight; child health status; APGAR score Maternal outcomes: retention; illicit drug use (urinalysis) |
|
| Notes |
Country: USA Funding: grants DA R01 12220 from the National Institute on Drug Abuse and M01RR‐02719 from the General Clinical Research Centers Program of the National Center of Research Resources, National Institutes of Health Conflict of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "They were assigned to one of the two treatment groups using a computerized dynamic balanced randomisation". |
| Allocation concealment (selection bias) | Low risk | Quote: "Research staff, with no other study involvement, generated the randomised allocation sequence". |
| Blinding of participants and personnel (performance bias) subjective outcomes | Low risk | Once medically cleared and randomised, participants were switched from their individualised dose of immediate‐release morphine onto an equivalent dose of double‐blind study medication. To maintain the double‐blind, the actual dose changes were known only to pharmacy staff. |
| Blinding of participants and personnel (performance bias) objective outcomes | Low risk | Once medically cleared and randomised, participants were switched from their individualised dose of immediate‐release morphine onto an equivalent dose of double‐blind study medication. To maintain the double‐blind, the actual dose changes were known only to pharmacy staff. |
| Blinding of outcome assessment (detection bias) subjective outcomes | Low risk | Once medically cleared and randomised, participants were switched from their individualised dose of immediate‐release morphine onto an equivalent dose of double‐blind study medication. To maintain the double‐blind, the actual dose changes were known only to pharmacy staff. |
| Blinding of outcome assessment (detection bias) objective outcomes | Low risk | Once medically cleared and randomised, participants were switched from their individualised dose of immediate‐release morphine onto an equivalent dose of double‐blind study medication. To maintain the double‐blind, the actual dose changes were known only to pharmacy staff. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of the 30 randomised patients, 20 delivered while enrolled in the study; the remaining 10 dropped out during the study. Of those randomised to buprenorphine, reasons for dropouts included: discharged for medical condition (n = 1), missed consecutive dosing days (n = 4) and elected to withdraw (n = 1). Of those randomised to methadone, reasons for discharge included: missed consecutive dosing days (n = 3) and elected to withdraw (n = 1). COMMENT: high dropouts (40%) in the methadone group and unbalanced (26% in the buprenorphine group) |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
MOTHER Study.
| Study characteristics | ||
| Methods | Multicentre, randomised controlled trial Double‐blind, double‐dummy |
|
| Participants | 175 pregnant adults; mean age 27.3 years; 83.2% white; employed 13.3%; mean years of education 11.3; mean n.of days of substance use in the previous 30 days: heroin 10.2, cocaine 4.8, any alcohol: 0.4, benzodiazepines: 0.8
Mean estimated gestational age of fetus: 18.6 weeks Inclusion criteria: opioid‐dependent women meeting DSM‐IV criteria between the ages of 18 and 41 years with a singleton pregnancy between 6 and 30 weeks of gestation Exclusion criteria: no medical or other conditions contraindicating participation; pending legal action; disorders related to the use of benzodiazepines or alcohol; planning to give birth outside the hospital at the study site |
|
| Interventions | (1) Sublingual tablets of buprenorphine (58 participants) versus (2) oral methadone (73 participants). Flexible dose range of 2 to 32 mg of buprenorphine; dose range of 20 to 140 mg of methadone Setting: outpatients Follow‐up: up to 10 days after delivery | |
| Outcomes | Neonatal outcome measures: neonates requiring treatment for NAS, peak NAS score, total amount of morphine needed for treatment of NAS, length of hospital stay and head circumference, number of days during which medication was given for NAS, weight and length at birth, preterm birth, gestational age at delivery, and 1‐minute and 5‐minute APGAR scores Maternal outcomes measures: caesarean section, weight gain, abnormal fetal presentation during delivery, anaesthesia during delivery, the results of drug screening at delivery, medical complications at delivery, study discontinuation, amount of voucher money earned for drug‐negative tests and number of prenatal obstetric visits Adverse events for children and mothers |
|
| Notes |
Country: United States, Austria, Canada Funding: Funded by the National Institute on Drug Abuse Conflict of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised within three stratification factors: (i) site; (ii) EGA (6 weeks and 0/7 days–18 weeks and 6/7 days; 19 weeks and 0/7–30 weeks and 6/7 days) to control for differences in duration of medication exposure; and (iii) cocaine use in the past 30 days (yes/no)" COMMENT: no further detail provided on the randomisation procedure |
| Allocation concealment (selection bias) | Low risk | Quote: "The Center for Substance Abuse Research (CESAR) at the University of Maryland, College Park, was the coordinating center responsible for across‐site randomisation, data collection, coordination and protocol adherence monitoring. Randomization assignment was communicated from CESAR directly to the site’s pharmacy." |
| Blinding of participants and personnel (performance bias) subjective outcomes | Low risk | Quote: "A blinded, individualized dosing schedule was used for the study medications, and a double‐blind method was used to implement dose‐unit increases or decreases (with dose adjustments of 2 mg for buprenorphine and 5 or 10 mg for methadone). Patients received seven tablets (three in the size of an 8‐mg tablet and four in the size of a 2‐mg tablet) to place under the tongue for 5 minutes, or until the tablets dissolved. Each tablet contained buprenorphine or placebo. After receiving these tablets, participants received liquid containing methadone or placebo. Oral methadone and flavour‐masking concentrates were diluted to provide the dose in a fixed volume (e.g. 40 mL at US sites and 50 mL in Vienna). Methadone placebo was given in the same fixed volume and included the same flavour‐masking concentrates as the active drug concentrate." |
| Blinding of participants and personnel (performance bias) objective outcomes | Low risk | Quote: "A blinded, individualized dosing schedule was used for the study medications, and a double‐blind method was used to implement dose‐unit increases or decreases (with dose adjustments of 2 mg for buprenorphine and 5 or 10 mg for methadone). Patients received seven tablets (three in the size of an 8‐mg tablet and four in the size of a 2‐mg tablet) to place under the tongue for 5 minutes, or until the tablets dissolved. Each tablet contained buprenorphine or placebo. After receiving these tablets, participants received liquid containing methadone or placebo. Oral methadone and flavour‐masking concentrates were diluted to provide the dose in a fixed volume (e.g. 40 mL at US sites and 50 mL in Vienna). Methadone placebo was given in the same fixed volume and included the same flavour‐masking concentrates as the active drug concentrate." |
| Blinding of outcome assessment (detection bias) subjective outcomes | Low risk | Quote: "With limited exceptions, data were submitted to CESAR using a paper document capture and processing methodology. The Center for Substance Abuse Research (CESAR) at the University of Maryland, College Park, was the coordinating centre responsible for data collection". COMMENT: not specified whether the trained personnel who collected data were blinded, but given the double‐blind condition for personnel who provided dugs and participants, we judged that they were. |
| Blinding of outcome assessment (detection bias) objective outcomes | Low risk | The outcomes were not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "A total of 16 of the 89 women in the methadone group (18%) and 28 of the 86 women in the buprenorphine group (33%) discontinued treatment before delivery (P = 0.02). Dissatisfaction with the study medication was reported as the reason for discontinuation by 71% of participants in the buprenorphine group, as compared with only 13% of those in the methadone group". COMMENT: high dropout (33.%) in the buprenorphine group and unbalanced (18% in the methadone group). Reasons for dropouts given and likely to be linked to treatments received |
| Selective reporting (reporting bias) | Low risk | The results of all the outcomes described in the protocol have been reported. |
APGAR score: Activity, Pulse, Grimace, Appearance and Respiration score DSM: Diagnostic and Statistical Manual of Mental Disorders NAS: neonatal abstinence syndrome VAS: visual analogue scale HAD: Hamilton Depression Scale WWQ: Wang Withdrawal Questionnaire
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bandstra 2012 | Editorial |
| Bell 2007 | Commentary on a randomised controlled trial where pregnant women were not included |
| Binder 2008 | Study defined as randomised but not clear from the text if women were randomised to different maintenance treatments; it seems that they were not |
| Carroll 1995 | Excluded as the type of control intervention was not among our inclusion criteria: both groups received methadone at the same dose |
| Cochran 2019 | Protocol of a study comparing two different psychosocial approaches combined with pharmacotherapy |
| Dawe 2007 | Participants did not meet the inclusion criteria: not pregnant women |
| Ebner 2007 | Excluded as the study design did not meet the inclusion criteria: not a randomised controlled trial |
| Fisher 1998 | Excluded as the study design did not meet the inclusion criteria: not a randomised controlled trial |
| Gordon 2004 | Excluded as the study design did not meet the inclusion criteria: not a randomised controlled trial |
| Hulse 2004 | Excluded as the study design did not meet the inclusion criteria: not a randomised controlled trial |
| Jackson 2004 | Excluded as the type of participants did not meet the inclusion criteria: newborns randomised to receive different treatments after the delivery |
| Jones 2008 | Narrative review |
| Jones 2011 | Intervention did not meet the inclusion criteria: psychosocial intervention |
| Keyser‐Marcus 2002 | Excluded as the study design did not meet the inclusion criteria: not a randomised controlled trial |
| Lacroix 2011 | Study design did not meet the inclusion criteria: not a randomised study |
| Laken 1997 | Excluded as the study design did not meet the inclusion criteria: not a randomised controlled trial |
| Martin 2011 | Narrative review |
| Newman 2009 | Comment, letter |
| Stine 2009 | Study design did not meet the inclusion criteria: comparison of women who did and did not give consent to participate in the MOTHER study |
| Suchman 2007 | Participants did not meet the inclusion criteria: non‐pregnant women |
| Tuten 2012 | Intervention did not meet the inclusion criteria: psychosocial treatment |
Characteristics of ongoing studies [ordered by study ID]
NCT 03098407.
| Study name | A pilot randomized comparative effectiveness clinical trial of buprenorphine vs. methadone for the treatment of opioid dependence in pregnancy |
| Methods | Randomised controlled parallel‐group trial; open‐label |
| Participants | Pregnant women 18+ years old, with a singleton pregnancy ≤ 28 weeks gestation confirmed by ultrasound, who meet the Diagnostic and Statistical Manual‐IV criteria for opioid dependence confirmed by urine drug screen |
| Interventions | Buprenorphine maintenance treatment; methadone maintenance treatment |
| Outcomes | Number of participants who are recruited, enrolled, retained, and who complete the study |
| Starting date | April 2017 |
| Contact information | |
| Notes |
Differences between protocol and review
We reassessed the risk of bias of the included studies in the updated version of the review according to the new recommendations of Cochrane.
Contributions of authors
Minozzi and Bellisario inspected the search hits by reading titles and abstracts; Minozzi and Bellisario independently assessed for inclusion each potentially relevant study located in the search; Minozzi and Bellisario extracted data independently. Minozzi performed a meta‐analysis and wrote the text of the review. Amato commented on the draft and contributed with Ferri to the discussion and the conclusions of the review, and Davoli supervised. Shayesteh Jahanfar updated the introduction, discussion and conclusion, and edited the review.
Sources of support
Internal sources
Department of Epidemiology, Lazio Regional Health Service, Italy
External sources
No sources of support supplied
Declarations of interest
None.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Fischer 1999 {published data only}
- Fischer G, Jagsch R, Eder H, Gombas W, Etzerdorfer P, Schmidl-Mohl K, et al. Comparison of methadone and slow-release morphine maintenance in pregnant addicts. Addiction 1999;94(2):231-9. [DOI] [PubMed] [Google Scholar]
Fischer 2006 {published data only}
- Fischer G, Ortner R, Rohrmeister K, Jagsch R, Baewert A, Langer M, et al. Methadone versus buprenorphine in pregnant addicts: a double-blind, double dummy comparison study. Addiction 2006;101(2):275-81. [DOI] [PubMed] [Google Scholar]
Jones 2005 {published data only}
- Jones HE, Johnson RE, Jasinski DR, O'Grady KE, Chisholm CA, Choo RE, et al. Buprenorphine versus methadone in the treatment of pregnant opioid-dependent patients: effects on the neonatal abstinence syndrome. Drug and Alcohol Dependence 2005;79(1):1-10. [DOI] [PubMed] [Google Scholar]
MOTHER Study {published data only}
- Chisolm MS, Fitzsimons H, Leoutsakos JM, Acquavita SP, Heil SH, Wilson-Murphy M, et al. A comparison of cigarette smoking profiles in opioid-dependent pregnant patients receiving methadone or buprenorphine. Nicotine Tobacco Research 2013;15(7):1297-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle MG, Salisbury AL, Lester BM, Jones HE, Lin H, Graf-Rohrmeister K, et al. Neonatal neurobehavior effects following buprenorphine versus methadone exposure. Addiction 2012;107(Suppl 1):63-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaalema DE, Scott TL, Heil SH, Coyle MG, Kaltenbach K, Badger GJ, et al. Differences in the profile of neonatal abstinence syndrome signs in methadone- versus buprenorphine-exposed neonates. Addiction 2012;107(Suppl 1):53-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbrook AM, Baxter JK, Jones HE, Heil SH, Coyle MG, Martin PR, et al. Infections and obstetric outcomes in opioid-dependent pregnant women maintained on methadone or buprenorphine. Addiction 2012;107(Suppl 1):83-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbrook AM, Jones HE, Heil SH, Martin PR, Stine SM, Fischer G, et al. Induction of pregnant women onto opioid-agonist maintenance medication: an analysis of withdrawal symptoms and study retention. Drug and Alcohol Dependence 2013;132(0):329-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansson LM, Dipietro JA, Velez M, Elko A, Williams E, Milio L, et al. Fetal neurobehavioral effects of exposure to methadone or buprenorphine. Neurotoxicology and Teratology 2011;33(2):240-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Dengler E, Garrisond A, O'Gradye KE, Seashore C, Horton E, et al. Neonatal outcomes and their relationship to maternal buprenorphine dose during pregnancy. Drug and Alcohol Dependence 2014;134:414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Fischer G, Heil SH, Kaltenbach K, Martin PR, Coyle MG, et al. Maternal Opioid Treatment: Human Experimental Research (MOTHER) - approach, issues and lessons learned. Addiction 2012;107(Suppl 1):28-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Jansson LM, O’Gradyc KE, Kaltenbach K. The relationship between maternal methadone dose at delivery and neonatal outcome: methodological and design considerations. Neurotoxicology and Teratology 2013:110-5. [DOI: 10.1016/j.ntt.2013.05.003] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, Johnson RE, Jasinski DR, Tuten M, Milio L. Dosing pre to postpartum with either buprenorphine or methadone. In: 69th Annual Scientific Meeting of the College on Problems of Drug Dependence. Quebec City, Canada, 2007:16-21.
- Jones HE, Johnson RE, O'Grady KE, Jasinski DR, Tuten M, Milio L. Dosing adjustments in postpartum patients maintained on buprenorphine or methadone. Journal of Addiction Medicine 2008;2(2):103-7. [DOI] [PubMed] [Google Scholar]
- Jones HE, Kaltenbach K, Heil SH, Stine SM, Coyle MG, Arria AM, et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. New England Journal of Medicine 2010;363:2320-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaltenbach K, O’Grady KE, Heil SH, Salisbury AL, Coyle MG, Fischer G, et al. Prenatal exposure to methadone or buprenorphine: early childhood developmental outcomes. Drug and Alcohol Dependence 2018;185:40-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger A, Jagsch R, Bäwert A, Winklbaur B, Rohrmeister K, Martin PR, et al. Are male neonates more vulnerable to neonatal abstinence syndrome than female neonates? Gender Medicine 2011;8(6):355-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson-Murphy MM, Chisolm MS, Leoutsakos JS, Kaltenbach K, Heil SH, Martin PR. Treatment completion in opioid-dependent pregnant patients randomised to agonist treatment: the role of intravenous drug use. In: 73rd Annual Scientific Meeting of the College on Problems of Drug Dependence. 2011:195, Abstract no: 778.
- Winklbaur-Hausknost B, Jagsch R, Graf-Rohrmeister K, Unger A, Baewert A, Langer M, et al. Lessons learned from a comparison of evidence-based research in pregnant opioid-dependent women. Human Psychopharmacology 2013;28(1):15-24. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bandstra 2012 {published data only}
- Bandstra, Emmalee S. Maternal Opioid Treatment: Human Experimental Research (MOTHER) study: maternal, fetal and neonatal outcomes from secondary analyses. Addiction 2012;107(Suppl 1):1-4. [DOI] [PubMed] [Google Scholar]
Bell 2007 {published data only}
- Bell J, Zador D. Dihydrocodeine as effective as methadone for maintenance of treatment for opiate dependence? Evidence Based Mental Health 2007;10(3):88. [DOI] [PubMed] [Google Scholar]
Binder 2008 {published data only}
- Binder T, Vavrinkova B. Prospective randomised comparative study of the effect of buprenorphine, methadone and heroin on the course of pregnancy, birthweight of newborns, early postpartum adaptation and course of the neonatal abstinence syndrome (NAS) in women followed up in the outpatient department. Neuro Endocrinology Letters 2008;29(1):80-6. [PubMed] [Google Scholar]
Carroll 1995 {published data only}
- Carroll KM, Chang G, Behr H, Clinton B, Kosten TR. Improving treatment outcome in pregnant, methadone-maintained women. American Journal on Addictions 1995;4(1):56-9. [Google Scholar]
Cochran 2019 {published data only}
- Cochran G, Smid MC, Krans EE, Bryan MA, Gordon AJ, Lundahl B, et al. A pilot multisite study of patient navigation for pregnant women with opioid use disorder. Contemporary Clinical Trials 2019;87:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dawe 2007 {published data only}
- Dawe S, Harnett P. Reducing potential for child abuse among methadone-maintained parents: results from a randomized controlled trial. Journal of Substance Abuse Treatment 2007;32(4):381-90. [DOI] [PubMed] [Google Scholar]
Ebner 2007 {published data only}
- Ebner N, Rohrmeister K, Winklbaur B, Baewert A, Jagsch R, Peternell A, et al. Management of neonatal abstinence syndrome in neonates born to opioid maintained women. Drug and Alcohol Dependence 2007;87:131-8. [DOI] [PubMed] [Google Scholar]
Fisher 1998 {published data only}
- Fisher G, Etzersdorfer P, Eder H, Jagsch R, Langer M, Weninger M. Buprenorphine maintenance in pregnant opiate addicts. European Addiction Research 1998;1:32-6. [DOI] [PubMed] [Google Scholar]
Gordon 2004 {published data only}
- Gordon AL, Stacey H, Pearson V, Haslam RR, Lopatko OV, White JM. Buprenorphine and methadone in pregnancy: effects on the mother and fetus/neonate. In: Sixty-Sixth Annual Scientific Meeting of the College on Problems of Drug Dependence. 2004.
Hulse 2004 {published data only}
- Hulse GK, O'Neil G, Arnold-Reed DE. Methadone maintenance vs. implantable naltrexone treatment in the pregnant heroin user. International Journal of Gynaecology & Obstetrics 2004;85(2):170-1. [DOI] [PubMed] [Google Scholar]
Jackson 2004 {published data only}
- Jackson L, Ting A, Mckay S, Galea P, Skeoch C. A randomised controlled trial of morphine versus phenobarbitone for neonatal abstinence syndrome. Archives of Disease in Childhood. Fetal and Neonatal Edition 2004;89:300-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2008 {published data only}
- Jones HE, Martin PR, Heil SH, Kaltenbach K, Selby P, Coyle MG, et al. Treatment of opioid-dependent pregnant women: clinical and research issues. Journal of Substance Abuse Treatment 2008;35(3):245-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2011 {published data only}
- Jones HE, O'Grady KE, Tuten M. Reinforcement-based treatment improves the maternal treatment and neonatal outcomes of pregnant patients enrolled in comprehensive care treatment. American Journal on Addictions 2011;20(3):196-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keyser‐Marcus 2002 {published data only}
- Keyser-Marcus L, Miles D, Jansson L, Jones H, Svikis D. Perinatal opiate dependence: methadone and birth outcomes. In: Drug and Alcohol Dependence. Vol. 66 Suppl 1. 2002.
Lacroix 2011 {published data only}
- Lacroix I, Berrebi A, Garipuy D, Schmitt L, Hammou Y, Chaumerliac C, et al. Buprenorphine versus methadone in pregnant opioid-dependent women: a prospective multicenter study. European Journal of Clinical Pharmacology 2011;67(10):1053-9. [DOI] [PubMed] [Google Scholar]
Laken 1997 {published data only}
- Laken MP, McComish JF, Ager J. Predictors of prenatal substance use and birth weight during outpatient treatment. Journal of Substance Abuse Treatment 1997;14(4):359-66. [DOI] [PubMed] [Google Scholar]
Martin 2011 {published data only}
- Martin PR. Opioid dependence during pregnancy: balancing risk versus benefit. Klinik Psikofarmakoloji Bülteni 2011;21:S35. [Google Scholar]
Newman 2009 {published data only}
- Newman R. Response to "Methadone maintenance vs. methadone taper during pregnancy" paper. American Journal on Addictions 2009;18(3):250; author reply 251. [DOI] [PubMed] [Google Scholar]
Stine 2009 {published data only}
- Stine SM, Heil SH, Kaltenbach K, Martin PR, Coyle MG, Fischer G, et al. Characteristics of opioid-using pregnant women who accept or refuse participation in a clinical trial: screening results from the MOTHER study. American Journal of Drug and Alcohol Abuse 2009;35(6):429-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Suchman 2007 {published data only}
- Suchman NE, Rounsaville B, DeCoste C, Luthar S. Parental control, parental warmth, and psychosocial adjustment in a sample of substance-abusing mothers and their school-aged and adolescent children. 2007 Journal of Substance Abuse Treatment;32(1):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tuten 2012 {published data only}
- Tuten M, Svikis DS, Keyser-Marcus L, O'Grady KE, Jones HE. Lessons learned from a randomized trial of fixed and escalating contingency management schedules in opioid-dependent pregnant women. American Journal of Drug and Alcohol Abuse 2012;38(4):286-92. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT 03098407 {published data only}
- NCT03098407. Opioid dependence treatment therapies in pregnancy [A pilot randomized comparative effectiveness clinical trial of buprenorphine vs. methadone for the treatment of opioid dependence in pregnancy]. clinicaltrials.gov/show/NCT03098407 (first received 31 March 2017).
Additional references
AIHW 2011
- Australian Institute of Health and Welfare. National Drug Strategy Household Survey detailed report 2010. Canberra: Australian Institute of Health and Welfare. www.aihw.gov.au/reports/illicit-use-of-drugs/2010-ndshs/contents/table-of-contents (accessed 23 March 2020).
AIHW 2014
- Australian Institute of Health and Welfare. National Drug Strategy Household Survey detailed report 2013. www.aihw.gov.au/reports/illicit-use-of-drugs/2013-ndshs-detailed/contents/table-of-contents (accessed 23 March 2020).
Amato 2011
- Amato L, Minozzi S, Davoli M, Vecchi S, Ferri M, Mayet S. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database of Systematic Reviews 2011, Issue 10. Art. No: CD004147. [DOI: 10.1002/14651858.CD004147.pub4] [DOI] [PubMed] [Google Scholar]
Behnke 2013
- Behnke M, Smith VC. Prenatal substance abuse: short- and long-term effects on the exposed fetus. Pediatrics 2013;131:e1009-24. [DOI: 10.1542/peds.2012-3931] [DOI] [PMC free article] [PubMed] [Google Scholar]
Clark 2002
- Clark NC, Lintzeris N, Gijsbers A, Whelan G, Dunlop A, Ritter A, et al. LAAM maintenance vs methadone maintenance for heroin dependence. Cochrane Database of Systematic Reviews 2002, Issue 2. Art. No: CD002210. [DOI: 10.1002/14651858.CD002210] [DOI] [PubMed] [Google Scholar]
CSAT 2005
- Center for Substance Abuse Treatment. Medication-assisted treatment for opioid addiction in opioid treatment programs. (Treatment Improvement Protocol Series 43). www.ncbi. nlm.nih.gov 2005. [PubMed]
Dattel 1990
- Dattel B. Substance abuse in pregnancy. Seminars in Perinatology 1990;14(2):179-87. [PubMed] [Google Scholar]
Dunlop 2003
- Dunlop AJ, Panjari M, O'Sullivan H, Henschke P, Love V et al. Clinical guidelines for the use of buprenorphine in pregnancy. Turning Point Alcohol and Drug Centre, Fitzroy, Australia 2003.
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
EMCDDA 2014
- European Monitoring Centre for Drugs and Drug Addiction. Pregnancy and opioid use: strategies for treatment. In: EMCDDA Papers. Luxembourg: Publications Office of the European Union, 2014. [Google Scholar]
Faggiano 2003
- Faggiano F, Vigna-Taglianti F, Versino E, Lemma P. Methadone maintenance at different dosages for opioid dependence. Cochrane Database of Systematic Reviews 2003, Issue 3. Art. No: CD002208. [DOI: 10.1002/14651858.CD002208] [DOI] [PubMed] [Google Scholar]
Fajemirokun 2006
- Fajemirokun-Odudeyi O, Sinha C, Tutty S, Pairaudeau P, Armstrong D, Phillips T, et al. Pregnancy outcome in women who use opiates. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2006;126(2):170-5. [DOI] [PubMed] [Google Scholar]
Ferri 2011
- Ferri M, Davoli M, Perucci CA. Heroin maintenance for chronic heroin-dependent individuals. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD003410. [DOI: 10.1002/14651858.CD003410.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Finnegan 1992
- Finnegan LP, Kaltenbach K. Neonatal abstinence syndrome. In: Primary Pediatric Care. 2nd edition. St Louis: CV Mosby, 1992. [Google Scholar]
Haight 2018
- Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization - United States, 1999-2014. Morbidity and Mortality Weekly Report 2018;67(31):845-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hulse 1997
- Hulse GK, Milne E, English DR, Holman CD. The relationship between maternal use of heroin and methadone and infant birth weight. Addiction 1997;92(11):1571-9. [PubMed] [Google Scholar]
Hulse 1998
- Hulse GK, Milne E, English DR, Holman CD. The relationship between maternal opiate use and neonatal mortality. Addiction 1998;93(7):1033-42. [DOI] [PubMed] [Google Scholar]
Jarvis 1994
- Jarvis MA, Schnoll SH. Methadone treatment during pregnancy. Journal of Psychoactive Drugs 1994;26(2):155-61. [DOI] [PubMed] [Google Scholar]
Johnson 2003
- Johnson RE, Jones HE, Fisher G. Use of buprenorphine in pregnancy: patient management and effects on the neonate. Drug and Alcohol Dependence 2003;70:S87-101. [DOI] [PubMed] [Google Scholar]
Jones 2012
- Jones HE, Heil SH, Baewert A, Arria AM, Kaltenbach K, Martin PR, et al. Buprenorphine treatment of opioid-dependent pregnant women: a comprehensive review. Addiction 2012;107(Suppl 1):5-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaltenbach 1998
- Kaltenbach K, Berghella V, Finnegan L. Opioid dependence during pregnancy: effects and management. Obstetrics and Gynecology Clinics of North America 1998;25:139-51. [DOI] [PubMed] [Google Scholar]
Klaman 2017
- Klaman SL, Isaacs K, Leopold A, Perpich J, Hayashi S, Vender J, et al. Treating women who are pregnant and parenting for opioid use disorder and the concurrent care of their infants and children: literature review to support national guidance. Journal of Addiction Medicine 2017;11:178-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lejuene 2006
- Lejuene C, Simmat-Durand L, Gourarier L, Aubisson S for the Groupe d'Etudes Grossesses et Addictions (GEGA). Prospective multicenter observational study of 260 infants born to 259 opiate-dependent mothers on methadone or high-dose buprenorphine substitution. Drug and Alcohol Dependence 2006;82(3):250-7. [DOI] [PubMed] [Google Scholar]
Ludlow 2004
- Ludlow JP, Evans SF, Hulse G. Obstetric and perinatal outcomes in pregnancies associated with illicit substance abuse. Australian and New Zealand Journal of Obstetrics and Gynaecology 2004;44(4):301-6. [DOI] [PubMed] [Google Scholar]
Mattick 2008
- Mattick RP, Kimber J, Breen C, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database of Systematic Reviews 2008, Issue 2. Art. No: CD002207. [DOI: 10.1002/14651858.CD002207.pub3] [DOI] [PubMed] [Google Scholar]
Mattick 2009
- Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No: CD002209. [DOI: 10.1002/14651858.CD002209.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mayet 2004
- Mayet S, Farrell M, Ferri M, Amato L, Davoli M. Psychosocial treatment for opiate abuse and dependence. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No: CD004330. [DOI: 10.1002/14651858.CD004330.pub2] [DOI] [PubMed] [Google Scholar]
Minozzi 2011
- Minozzi S, Amato L, Vecchi S, Davoli M, Kirchmayer U, Verster A. Oral naltrexone maintenance treatment for opioid dependence. Cochrane Database of Systematic Reviews 2011, Issue 4. Art. No: CD001333. [DOI: 10.1002/14651858.CD001333.pub4] [DOI] [PubMed] [Google Scholar]
Monitoring the future 2017
- National Institute of Drug Abuse. Monitoring the future: treating opioid use disorder during pregnancy. www.drugabuse.gov/publications/treating-opioid-use-disorder-during-pregnancy (accessed prior to 8 October 2020).
NIH 1998
- National Institutes of Health Consensus Development Panel. Effective medical treatment of opiate addiction. JAMA 1998;280(22):1936-43. [PubMed] [Google Scholar]
ONDCP 2020
- Office of National Drug Control Policy. National Drug Control Strategy. Washington, D.C: Office of National Drug Control Policy, Executive Office of the President, 2020. [Google Scholar]
Ordean 2018
- Ordean A. Opioid agonist treatment during pregnancy: review of methadone and buprenorphine. In: Best Start Resource Centre Annual Conference; 2018 February 7. en.beststart.org/2018-bsrc-conference-handouts, 2018.
Rayburn 2004
- Rayburn W, Bogenschutz MP. Pharmacotherapy for pregnant women with addiction. American Journal of Obstetrics and Gynecology 2004;191:1885-97. [DOI] [PubMed] [Google Scholar]
Reddy 2017
- Reddy UM, Davis JM, Ren Z, Greene MF, Opioid Use in Pregnancy, Neonatal Abstinence Syndrome, and Childhood Outcomes Workshop invited speakers. Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes: executive summary of a joint workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, American Congress of Obstetricians and Gynecologists, American Academy of Pediatrics, Society for Maternal-Fetal Medicine, Centers for Disease Control and Prevention, and the March of Dimes Foundation. Obstetrics and Gynecology 2017;130(1):10-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schunemann 2013
- Schunemann H, Brozek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
UK Guidelines 2007
- Department of Health (England), The Scottish Government, Welsh Assembly Government and Northern Ireland Executive. Drug Misuse and Dependence: UK Guidelines on Clinical Management. www.smmgp.org.uk 2007.
UNODC 2018
- UNODC/WHO. World Drug Report 2018. www.unodc.org/wdr2018/ (accessed prior to 8 October 2020).
Wang 1999
- Wang EC. Methadone treatment during pregnancy. Journal of Obstetric, Gynecologic, and Neonatal Nursing 1999;28:615-22. [DOI] [PubMed] [Google Scholar]
Wang 2018
- Wang M. Opioid detoxification during pregnancy: systematic review and meta-analysis of maternal and neonatal outcomes. Obstetrics & Gynecology 2018;131:197s. [Google Scholar]
WHO 2014
- World Health Organization. Guidelines for the Identification and Management of Substance Use and Substance Use Disorders in Pregnancy. Geneva, Switzerland: World Health Organization, 2014. [PubMed] [Google Scholar]
Winklbaur 2008
- Winklbaur B, Kopf N, Ebner N, Jung E, Thau K, Fischer G. Treating pregnant women dependent on opioids is not the same as treating pregnancy and opioid dependence: a knowledge synthesis for better treatment for women and neonates. Addiction 2008;103(9):1429-40. [DOI] [PubMed] [Google Scholar]
Zedler 2016
- Zedler BK, Mann AL, Kim MM, Amick HR, Joyce AR, Murrelle EL, et al. Buprenorphine compared with methadone to treat pregnant women with opioid use disorder: a systematic review and meta-analysis of safety in the mother, fetus and child. Addiction 2016;11:2115-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Minozzi 2013
- Minozzi S, Amato L, Bellisario C, Ferri M, Davoli M. Maintenance agonist treatments for opiate-dependent pregnant women. Cochrane Database of Systematic Reviews 2013, Issue 12. Art. No: CD006318. [DOI: 10.1002/14651858.CD006318.pub3] [DOI] [PubMed] [Google Scholar]


