Abstract
Background
Annually, infections contribute to approximately 25% of the 2.8 million neonatal deaths worldwide. Over 95% of sepsis‐related neonatal deaths occur in low‐ and middle‐income countries. Hand hygiene is an inexpensive and cost‐effective method of preventing infection in neonates, making it an affordable and practicable intervention in low‐ and middle‐income settings. Therefore, hand hygiene practices may hold strong prospects for reducing the occurrence of infection and infection‐related neonatal death.
Objectives
To determine the effectiveness of different hand hygiene agents for preventing neonatal infection in community and health facility settings.
Search methods
We used the standard search strategy of Cochrane Neonatal to search the Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 5), in the Cochrane Library; MEDLINE via PubMed (1966 to 10 May 2019); Embase (1980 to 10 May 2019); and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (1982 to 10 May 2019). We also searched clinical trials databases and the reference lists of retrieved articles for randomised controlled trials (RCTs) and quasi‐randomised trials. Searches were updated 1 June 2020.
Selection criteria
We included RCTs, cross‐over trials, and quasi‐RCTs that included pregnant women, mothers, other caregivers, and healthcare workers who received interventions within the community or in health facility settings
Data collection and analysis
We used standard methodological procedures expected by Cochrane and the GRADE approach to assess the certainty of evidence. Primary outcomes were incidence of (study author‐defined) suspected infection within the first 28 days of life, bacteriologically confirmed infection within the first 28 days of life, all‐cause mortality within the first seven days of life (early neonatal death), and all‐cause mortality from the 8th to the 28th day of life (late neonatal death).
Main results
Our review included five studies: one RCT, one quasi‐RCT, and three cross‐over trials with a total of more than 5450 neonates (two studies included all neonates but did not report the actual number of neonates involved). Four studies involved 279 nurses working in neonatal intensive care units and all neonates on admission. The fifth study did not clearly state how many nurses were included in the study. Studies examined the effectiveness of different hand hygiene practices for the incidence of (study author‐defined) suspected infection within the first 28 days of life. Two studies were rated as low risk for selection bias, another two were rated as high risk, and one study was rated as unclear risk. One study was rated as low risk for allocation bias, and four were rated as high risk. Only one of the five studies was rated as low risk for performance bias.
4% chlorhexidine gluconate (CHG) compared to plain liquid soap
We are uncertain whether plain soap is better than 4% chlorhexidine gluconate (CHG) for nurses’ skin based on very low‐certainty evidence (mean difference (MD) ‐1.75, 95% confidence interval (CI) ‐3.31 to ‐0.19; 16 participants, 1 study; very low‐certainty evidence). We identified no studies that reported on other outcomes for this comparison.
4% chlorhexidine gluconate compared to triclosan 1%
One study compared 1% w/v triclosan with 4% chlorhexidine gluconate and suggests that 1% w/v triclosan may reduce the incidence of suspected infection (risk ratio (RR) 1.04, 95% CI 0.19 to 5.60; 1916 participants, 1 study; very low‐certainty evidence). There may be fewer cases of infection in the 1% w/v triclosan group compared to the 4% chlorhexidine gluconate group (RR 6.01, 95% CI 3.56 to 10.14; 1916 participants, 1 study; very low‐certainty evidence); however, we are uncertain of the available evidence.
We identified no study that reported on all‐cause mortality, duration of hospital stay, and adverse events for this comparison.
2% CHG compared to alcohol hand sanitiser (61% alcohol and emollients)
We are uncertain whether 2% chlorhexidine gluconate reduces the risk of all infection in neonates compared to 61% alcohol hand sanitiser with regards to the incidence of all bacteriologically confirmed infection within the first 28 days of life (RR 2.19, 95% CI 1.79 to 2.69; 2932 participants, 1 study; very low‐certainty evidence) in the 2% chlorhexidine gluconate group, but the evidence is very uncertain.
The adverse outcome was reported as mean visual scoring on the skin. There may be little to no difference between the effects of 2% CHG on nurses’ skin compared to alcohol hand sanitiser based on very low‐certainty evidence (MD ‐0.80, 95% CI 0.01 to 1.59; 118 participants, 1 study; very low‐certainty evidence).
We identified no study that reported on all‐cause mortality and other outcomes for this comparison.
None of the included studies assessed all‐cause mortality within the first seven days of life nor duration of hospital stay.
Authors' conclusions
We are uncertain as to the superiority of one hand hygiene agent over another because this review included very few studies with very serious study limitations.
Plain language summary
Can hand hygiene prevent infection in newborn babies?
Review question
Can hand hygiene prevent infection in newborn babies?
Background
Every year, about 500,000 newborn babies die as a result of infection caused by bacteria. Most of these deaths occur in poor countries. These infections can be prevented when caregivers of these babies practice good hand hygiene.
Search date
The search is up‐to‐date as of 1 June 2020.
Study characteristics
We included five studies that involved nurses working in intensive care units of hospitals and all neonates on admission. Four of the studies involved 279 nurses, and the fifth study did not clearly report how many nurses were recruited into the study. Studies compared 'antiseptic detergent' versus alcohol hand rub (sanitiser); 'antiseptic detergent' versus plain soap; 1% triclosan versus 'antiseptic detergent'; and antiseptic that contained iodine versus another (Prepodyne versus betadine).
Study funding sources
Sources of funding were unclear in four of the included studies, and one reported that the study was not funded.
Key results
Our review provides no evidence to support the effectiveness of one hand hygiene intervention compared to another for preventing infection in newborns. None of the five included studies examined other important issues such as death and duration of hospital stay. There was not much difference in the undesirable effects of various hand hygiene interventions on the skin of caregivers.
In conclusion, we are not sure of the hand hygiene intervention that is better for preventing infection in newborn babies. We assessed only a few studies that involved small numbers of nurses and babies. In addition, most of the studies assessed had high risk of bias. Larger studies with low risk of bias are needed so reliable conclusions can be reached.
Certainty of evidence
We have no confidence in the available evidence to draw conclusions about the effectiveness of these hand hygiene interventions for preventing infection in newborns.
Summary of findings
Background
Annually, infection contributes to approximately 25% of the 2.8 million neonatal deaths worldwide. Over 95% of sepsis‐related neonatal deaths occur in low‐ and middle‐income countries (Liu 2015). Neonatal infection may be acquired through exposure to contaminated secretions of the birth canal, or through contact with the contaminated environment (Chan 2013; Gebremedhin 2016; Schuchat 2000). Important environmental sources of infection for the neonate include the hands of individuals who care for the many needs of the baby, including healthcare workers (HCWs) (Ram 2017; Rhee 2008). Contaminated hands play a major role in community‐acquired and hospital‐acquired neonatal infection, particularly among preterm infants, who are most susceptible. Community‐based and health facility‐based studies have suggested that handwashing may play a preventive role in neonatal infection in low‐, middle‐, and high‐income countries (Herruzo‐Cabrera 2001; Janota 2014; Rhee 2008).
Hand hygiene is an inexpensive and cost‐effective way of preventing neonatal infection, making it a practicable intervention in low‐ and middle‐income settings (WHO 2009). Therefore, hand hygiene practices may hold strong prospects for reducing the occurrence of infection and infection‐related neonatal death.
Description of the condition
The International Paediatric Sepsis Consensus Conference of 2005 defined neonatal sepsis as systemic inflammatory response syndrome in the presence of, or as a result of, suspected or proven infection in a neonate (Goldstein 2005). Neonatal sepsis is caused by a variety of micro‐organisms of bacterial, viral, fungal, or rickettsial origin. Neonatal sepsis can be classified as an early‐onset (mainly acquired before or during delivery, or both) or late‐onset condition (often acquired from exposure to a contaminated environment). However, the age cut‐off distinguishing early‐ from late‐onset neonatal sepsis ranges from 48 hours to seven days (Haque 2007). Neonates are particularly susceptible to infection because of poor cutaneous and mucosal barrier mechanisms, poor macrophage function, poor opsonisation, and low levels of serum immunoglobulins and complement (Cortese 2016; Wynn 2010). Susceptibility to neonatal infection is inversely related to gestational age, with preterm neonates at higher risk of infection compared to term neonates (Afonso 2017).
Neonatal infection may lead to life‐threatening multi‐systemic morbidities such as shock, disseminated intravascular coagulopathies, cardiac failure, adrenal insufficiency, renal insufficiency, and metabolic derangements (Cortese 2016; Goldstein 2005). Therefore, in spite of the availability of antibiotics and other adjunctive treatments, neonatal infection still leads to mortality and accounts for about a quarter of global neonatal deaths (Liu 2015), prolonged hospital stay, early complications (Chu 2014), late complications (Adams‐Chapman 2006), and huge economic burden (Ranjeva 2018).
The hands of mothers, other caregivers, and HCWs harbour significant microbial pathogens acquired during contact with patients or environmental surfaces (Aiello 2003). Contact of caregivers' and HCWs' hands with respiratory secretions, diaper changes, and direct skin contacts are often associated with transmission of infection to the newborn (Pessoa‐Silva 2004). Average bacterial loads on the hands of caregivers (usually mothers) and neonatal intensive care unit (NICU) nurses may consist of up to hundreds of thousands of bacteria (Aiello 2003). This pattern of bacterial loads may vary among patients, but it is relatively constant for any individual (Aiello 2003; Larson 1998).
The World Health Organization (WHO) has described five steps of transmission of infection from person to person through the hands of HCWs. These steps include the following.
Organisms present in the skin of HCWs or on objects close to the patient.
Organisms transferred to the hands of HCWs.
Organisms surviving on the hands of HCWs for several minutes.
Handwashing or hand antisepsis by HCWs inadequate or completely omitted, or use of inappropriate agents by HCWs for hand hygiene.
Contaminated hands of HCWs coming in contact with baby or with an object that will come in contact with baby (WHO 2009).
Organisms often found to contaminate the hands of caregivers include Staphylococcus aureus, Klebsiella spp., Proteus mirabilis, and Actinobacter spp. These organisms are capable of causing infection in newborns (Cortese 2016; Herruzo‐Cabrera 2001).
Description of the intervention
Hand hygiene refers to any form of hand cleansing. It is often used interchangeably with handwashing, which implies washing hands with plain or antimicrobial soap and water (WHO 2009). Hand hygiene also includes the use of various alcohol‐based hand rubs, wipes, scrubs, and antiseptic agents such as 0.5% chlorhexidine gluconate (CHG) (CADTH 2014), chlorine derivatives, chloroxylenol (PCMX), quaternary ammonium compounds, and triclosan (WHO 2009). It is recommended that caregivers should perform hand hygiene before touching hospital equipment and instruments, before touching neonates, and between cleaning and caring for neonates (Loveday 2014; WHO 2009).
How the intervention might work
Frequent and adequate hand hygiene by caregivers and HCWs may reduce neonatal infection by reducing dirt, organic materials, and microbial contamination on the hands of these personnel, thereby reducing the risk of contamination of babies and objects that come in contact with babies (Herruzo‐Cabrera 2001; Janota 2014; Won 2004).
Handwashing with water alone washes away dirt but may not remove fat and oil on contaminated hands. This necessitates the use of soaps and detergents that have the capacity to dissolve fatty and hydrophobic materials, to facilitate their subsequent removal with water (WHO 2009). Rotter 1999 reported that washing hands for 30 seconds reduced bacterial count to a greater extent than washing hands for 15 seconds.
Alcohol‐based hand antiseptics and rubs have the ability to denature protein (Ali 2001). Alcohol‐based preparations containing 60% to 80% alcohol have been reported to be most effective and safe (Ali 2001). Alcohol has been found to have excellent in vitro germicidal activity against both drug‐susceptible and drug‐resistant bacteria, Mycobacterium tuberculosis, some viruses, and fungi (Ali 2001; Herruzo‐Cabrera 2001). Frequent use of appropriate alcohol‐based hand rubs limits the spread of infection from the hands of HCWs to neonates (Herruzo‐Cabrera 2001; Janota 2014).
Chlorhexidine solution attaches to and disrupts cytoplasmic membranes of pathogenic bacteria on the hands of HCWs, thereby precipitating their cellular contents and resulting in cellular death (Rotter 1999). This action is similar to that of other hand antiseptic agents. Mortimer 1962 demonstrated that frequent hand hygiene with hexachlorophene antiseptic agents significantly reduced the risk of transmission of Staphylococcus aureus pathogens from nurses to babies admitted to the NICU compared to the risk of transmission from nurses who did no handwashing or hand rubbing with the antiseptic agent. Hand hygiene has also been reported by several study investigators to reduce the rate and cross‐transmission of pathogenic microbial agents, including methicillin‐resistant Staphylococcus aureus strain (MRSA), in neonatal care units (Webster 1994; Zafar 1995).
As effective as hand hygiene may be, compliance on the part of HCWs may present a challenge to the overall benefits to be accrued from the practice. A study of healthcare providers in neonatal and paediatric intensive care units shows overall hand hygiene compliance of 37%, with differential compliance of 41.4% for nurses and 31.9% for doctors, and for both cadres, compliance was best immediately after patients or patients' environments were touched (Karaaslan 2014). Lack of motivation and a heavy workload were proffered as reasons for poor compliance, but it is plausible that the type of hand hygiene agent available may also influence the frequency of hand hygiene practices. Preference for specific hand hygiene agents may be determined by the types of adverse events related to the use of such agents.
Adverse events in the form of skin irritation and allergic skin reaction may occur following the use of hand hygiene agents. Some liquid soaps, hand lotions, creams, and ointments contain ingredients such as iodine, iodophors, triclosan, chlorhexidine, and chloroxylenol, which may act as irritants or allergens. Frequent exposure of the skin to some of these allergens leads to progressive depletion of surface lipids in the superficial layers of the skin, thereby exposing deeper layers of the skin to the effects of allergens (WHO 2009). Adverse events that may follow hand hygiene procedures include skin dryness, burning, erythematic scaling, fissuring, a sensation of roughness, and irritation such as eczema, as described in Abd El‐AAl 2013. In this study, dryness, burning/irritation, and eczema were reported by 61%, 30%, and 1% of nurses. Indeed, healthcare providers have been reported to have a higher prevalence of skin irritation than is observed in the general population; this was ascribed to frequent hand hygiene during patient care (Larson 2006).
Why it is important to do this review
Stringent hand hygiene practices in communities and health facilities may reduce the risk and incidence of neonatal infection and ultimately may contribute to the desired reduction in infection‐related neonatal death and the economic burden of associated morbidities (Adams‐Chapman 2006; Chu 2014; Ranjeva 2018). A conservative estimate of the economic impact of neonatal sepsis in sub‐Saharan Africa (SSA) revealed that 5.29 to 8.73 million disability‐adjusted life‐years (DALYs) are lost annually in the region to neonatal sepsis. This corresponds to an annual economic burden ranging from USD 10 billion to USD 469 billion in SSA alone (Ranjeva 2018). This huge economic cost may be reduced substantially through meticulous hand hygiene practices.
Effective handwashing practices may be a more efficient and cost‐effective intervention aimed at reducing neonatal death for developing economies, as the cost of procuring the required materials (soap and water and/or alcohol rubs) may be negligible compared to direct and indirect costs of taking care of morbidities associated with neonatal infection (WHO 2009). Hand hygiene may also be more psychologically satisfying and thus more acceptable for families compared to more technologically advanced preventive measures (Greenland 2013; WHO 2009). A priority‐setting exercise that involved stakeholders from Anglophone West African countries identified this review question as very important (Effa 2017). However, no systematic reviews have examined the effectiveness of different hand hygiene agents for prevention of neonatal infection and associated morbidities and death.
The United Nations, through global goals termed “Sustainable Development Goals” (SDGs), aims to end preventable death of newborns and children under five years of age by 2030, among other lofty goals (UN 2017). The third goal of the 17 SDGs cannot be achieved without reduced neonatal mortality. One way this goal might be achieved is to substantially reduce infection‐related neonatal mortality in low‐ and middle‐income countries (UN 2017). Meticulous hand hygiene practices are potential interventions for reducing these preventable deaths of newborns.
Objectives
To determine the effectiveness of different hand hygiene agents for preventing neonatal infection in community and health facility settings.
Methods
Criteria for considering studies for this review
Types of studies
We included a randomised controlled trial (RCT), cross‐over trials, and a quasi‐RCT.
Types of participants
We included participants who received the interventions (pregnant women, mothers, other caregivers, and HCWs) within the community or in health facility settings. For the purpose of this Cochrane Review, we define the community setting as any setting other than a healthcare facility.
Source of outcome data: neonates (from birth to 28 days of life).
Types of interventions
Our criteria allowed comparison of any hand hygiene agent versus another type. We included studies that compared any of the following interventions given singly or in combination with any of the comparisons.
Intervention
Handwashing with soap and water
Alcohol‐based hand sanitiser (e.g. rubs, wipes, scrubs)
Antiseptics (e.g. chlorhexidine gluconate (CHG), chlorine derivatives, parachlorometaxylenol (PCMX), quaternary ammonium compounds, triclosan)
Comparison
Handwashing with soap and water
Alcohol‐based hand rub/hand sanitiser
Antiseptics
Standard practice
Combination of any of these
Types of outcome measures
Primary outcomes
Incidence of (study author‐defined) suspected infection within the first 28 days of life
Incidence of bacteriologically confirmed infection (types of infection as specified by study authors) within the first 28 days of life
All‐cause mortality within the first seven days of life (early neonatal death)
All‐cause mortality from the 8th to the 28th day of life (late neonatal death)
Secondary outcomes
Duration of hospital stay
Any hospitalisation for neonates managed in the community setting
Incidence of community‐acquired and hospital‐acquired infection
Study author‐reported adverse events such as skin changes and reactions to handwashing and rubs
Search methods for identification of studies
We used the criteria and standard methods of Cochrane and Cochrane Neonatal (see the Cochrane Neonatal search strategy for specialised register neonatal.cochrane.org/resources-authors/author-resources-new-reviews). We searched for errata or retractions from included studies published in full text on PubMed (www.ncbi.nlm.nih.gov/pubmed), and we reported in the review the date this was done.
Electronic searches
We conducted a comprehensive search that included the Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 5), in the Cochrane Library; MEDLINE via PubMed (1966 to 10 May 2019); Embase (1980 to 10 May 2019); and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (1982 to 10 May 2019) (see Appendix 1 for the full search strategies for each database). We did not apply language restrictions.
We searched clinical trials registries for ongoing and recently completed trials (clinicaltrials.gov, www.isrctn.com). Records from WHO ICTRP databases are now contained in Cochrane CENTRAL, so this database was not searched separately.
We updated the search on 1 June 2020 as follows (see Differences between protocol and review).
We conducted a comprehensive search of CENTRAL, in the Cochrane Library; Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Daily and Versions(R) (1 January 2019 to 1 June 2020); and CINAHL (1 January 2019 to 1 June 2020). We have included the search strategies for each database in Appendix 1. We did not apply language restrictions.
We searched clinical trial registries for ongoing and recently completed trials. We searched the WHO ICTRP database (www.who.int/ictrp/search/en/), along with the US National Library of Medicine’s ClinicalTrials.gov via Cochrane CENTRAL (clinicaltrials.gov). Additionally, we searched http://www.isrctn.com/ for any unique trials not found through the Cochrane CENTRAL search.
Searching other resources
We searched the reference lists of any articles selected for inclusion in this review to identify additional relevant articles.
Data collection and analysis
Selection of studies
We applied machine learning using the Cochrane Classifier tool in the Cochrane Register of Studies (CRS) to remove reports with the least (0% to 2%) probability of being RCTs, and with the least (0% to 2%) probability of including infants in the population.
Two review authors (BPK and EEU) independently assessed the eligibility of results of the literature search for potentially relevant trials. These two review authors assessed the full reports of potentially relevant trials and independently determined whether they met the inclusion criteria, using a pre‐tested eligibility form. When there were disagreements on study eligibility, a third review author (TAO) resolved these. We listed all studies excluded after full‐text assessment, along with reasons for excluding them, in the Characteristics of excluded studies table. We ensured that trials with multiple publications were included only once, and when multiple publications included different but relevant outcomes, we included all publications on the same trial as one study in the review.
We recorded the selection process in sufficient detail to complete a PRISMA flow diagram (Moher 2009).
Data extraction and management
Two review authors (BPK and OO) independently extracted data from the included studies using a pre‐tested data extraction form. One review author (OO) entered the extracted data into Review Manager 5 (RevMan 5) (Review Manager 2014), as well as into Cochrane's review writing software, and another review author (TAO) cross‐checked the data for completeness and accuracy. We extracted data on the number of participants randomised and the number analysed in each group for each reported outcome.
For continuous outcomes, we extracted the number of participants for each treatment arm, using arithmetic means (mean differenced (MDs)) and calculated standard errors (SEs). When data were presented as rates, we extracted rates in person‐time of follow‐up for person‐time outcomes and calculated the incidence rate ratio. Also for events presented as counts, we calculated the risk ratio using the formula described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We obtained the standard error of the natural log of the rate ratio by using the formula described in Bello 2020. We used generic inverse variance to calculate the risk ratio for the person‐time outcome, and we calculated the standard error. We extracted data on reported adverse events as dichotomous outcomes (Higgins 2011). For cross‐over studies, when a sufficient washout period before switching interventions for participants was reported, we extracted the final post‐intervention data for our analysis using generic inverse variance (Larson 2005).
We attempted to contact the trial authors to request additional information on missing or unclear data.
Assessment of risk of bias in included studies
Two review authors (CO and OO) independently assessed the risk of bias (low, high, or unclear) of all included trials using the Cochrane ‘Risk of bias’ tool for the following domains (Higgins 2011).
Sequence generation (selection bias).
Allocation concealment (selection bias).
Blinding of participants and personnel (performance bias).
Blinding of outcome assessment (detection bias).
Incomplete outcome data (attrition bias).
Selective reporting (reporting bias).
Any other bias.
We resolved disagreements by discussion or by consultation with a third assessor. See Appendix 2 for a more detailed description of the risk of bias for each domain.
Measures of treatment effect
The type of treatment effect used in describing each of the listed outcomes was dependent on the type of data extracted for the specific outcome. For continuous data, we reported the mean difference (MD) for continuous outcomes. We presented all measures of effect along with their corresponding 95% confidence intervaIs (CIs). We extracted post‐intervention values and utilised mean and SD values for the analysis. For binary data, we analysed binary outcomes by calculating risk ratio (RR) and risk difference (RD) with 95% CIs.
Unit of analysis issues
If we had identified cluster‐RCTs, we would have extracted results that had been adjusted for clustering. When adjustment was not made for clustering, we would have adjusted the results for clustering by multiplying the standard errors of the treatment effect by the square root of the design effect. We planned to calculate the design effect as 1+(m‐1)*ICC, where ‘m' is the average cluster size and ICC is the intracluster correlation coefficient (Higgins 2011). When the ICC was not reported, we planned to estimate the ICC by examining other trials included in the review or by contacting trial investigators. If we could not adjust results for clustering, we would not have combined the results in meta‐analyses with individual RCTs or cluster‐adjusted RCTs but would have presented the results in an additional table. To avoid unit of analysis errors due to meta‐analysis of results from several time points, we selected a maximum of three most clinically important time points (as reported by the authors of included studies) for each outcome.
For cross‐over trials without carry‐over effects (studies that allowed time for the intervention to wash out before crossing over) that met our inclusion criteria, we presented trial results as for a parallel‐group trial (Larson 2005), and we used generic inverse variance to analyse continuous data. We used data collected at the end of the intervention and downgraded the quality of evidence as for non‐randomised studies. We did not combine the included cross‐over trials in meta‐analyses because they were too heterogeneous. The effect of chlorhexidine against micro‐organisms lasts for 48 hours on the skin, Larson 2005 reported a washout period of one month.
One included cross‐over trial did not report a 'washout' period but prepared appropriate data analyses (i.e. paired analyses) for 'umbilical cord positivity' ‐ an important outcome that was not one of the outcomes listed in this review (Amortegui 1978). We extracted data from the first phase of the cross‐over trial and analysed them using generic inverse variance for data analysis as if the trial had followed a parallel‐group design (Deeks 2011); we presented the results as 'other outcomes not pre‐specified'. The study compared betadine (povidone‐iodine) and Prepodyne ‐ two iodophor hand hygiene agents. One study reported that povidone‐iodine (betadine) can last for up to two days on the skin (Bigliardi 2017); however another study indicated that the residual effect ranged between 30 minutes and 1 hour (Gottardi 2001). We are not sure what the carryover effect of the intervention was on the outcomes reported. We rated the study as high risk for other bias and downgraded the quality of evidence to very low certainty.
Dealing with missing data
We analysed according to the intention‐to‐treat principle (all randomised participants were analysed in the groups to which they were originally assigned) when the authors of included studies accounted for all included participants. We would have assumed that data were missing at random when there was no difference in the proportion of missing data between intervention and control groups. If there were too much missing data for one treatment group compared to another group, we would have performed an ‘as‐treated analysis’, using data for those participants who completed the study and an ‘intention‐to‐treat analysis’ by analysing participants in the group to which they were randomised, and we would have assumed that the missing data had a poor outcome, irrespective of whether or not participants completed the study. We would have compared the two results and used the result that is most representative of the true effect.
We planned to contact trial authors for missing or incomplete data. When this was not feasible, we employed a complete‐case analysis, such that participants for whom no outcome was reported were excluded from the analysis, if we judged the study to be at low risk of bias regarding allocation sequence generation and allocation concealment. This analysis assumes that patients for whom an outcome is available are representative of the original randomised patients (Higgins 2011).
Assessment of heterogeneity
We would have assessed statistical heterogeneity between subgroups by visually inspecting the forest plots for overlapping CIs, by applying the Chi² test (when P < 0.10 was considered statistically significant), and by using the I² statistic (statistic with values < 25% representing no heterogeneity; 25% to 49% low; 50% to 74% moderate; and ≥ 75% substantially high heterogeneity) if there were sufficient studies for meta‐analysis.
Assessment of reporting biases
We did not explore publication biases by constructing a funnel plot due to an insufficient number of included trials.
Data synthesis
Our analysis compared the effect of each hand hygiene product versus another in a head‐to‐head comparison. We analysed data using Review Manager 5 (RevMan 5) (Review Manager 2014). We used generic inverse variance to calculate risk ratio for the person‐time outcome and mean difference for adverse events reported as a mean visual score. We extracted data as numbers of events and participants for each group for adverse events reported as dichotomous outcomes obtained at their relative risk. We also calculated risk ratio and SE for count data using the formula described in the Cochrane Handbook for Systematic Reviews of Interventions and applied generic inverse variance for the analysis. We planned to meta‐analyse the data using RevMan when it was feasible to do so. We identified insufficient studies for a meta‐analysis for each of the pre‐specified comparisons. We presented the results in narrative form and downgraded the quality of evidence for imprecision and serious risk of bias and displayed results in ‘Summary of findings' tables and in additional tables.
We presented the main results of the review alongside a GRADE appraisal of the quality of evidence in ‘Summary of findings' tables and in additional tables.
Subgroup analysis and investigation of heterogeneity
We could not investigate heterogeneity. It was not feasible to do so because we did not meta‐analyse our included studies.
We would have performed a subgroup analysis of community‐based study versus hospital‐based study if we had included a community‐based study.
Sensitivity analysis
We did not conduct a sensitivity analysis to investigate the robustness of study results. Few studies are included in our review.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach, as outlined in the GRADE Handbook (Schünemann 2013), to assess the quality of evidence of the following (clinically relevant) outcomes: incidence of (author‐defined) suspected infections within the first 28 days of life, Incidence of bacteriologically confirmed infections (types of infection as specified by authors) within the first 28 days of life, all‐cause mortality within the first seven days of life (early neonatal death), all‐cause mortality from the 8th to 28th day of life (late neonatal death).
Two review authors (OO and TAO ) independently assessed the quality of the evidence for each of the outcomes above. We considered evidence from RCTs as high certainty but downgraded the evidence one level for serious (or two levels for very serious) limitations based upon the following: design (risk of bias), consistency across studies, directness of the evidence, precision of estimates, and presence of publication bias. We considered evidence from non‐RCTs as very low certainty evidence because of very serious risk of bias
We used the GRADEpro GDT Guideline Development Tool to create three ‘Summary of findings’ tables to report the quality of the evidence (GRADEpro GDT ). The GRADE approach results in an assessment of the quality of a body of evidence as one of four grades.
High certainty: further research is very unlikely to change our confidence in the estimate of effect.
Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low certainty: we are very uncertain about the estimate.
Results
Description of studies
Results of the search
Our 2019 search yielded 1264 records. Our 2020 search yielded 108 records. After removing duplicates and applying machine learning tasks, we screened 511 records by title and abstract and excluded 496 records. We assessed 14 full‐text records and excluded seven records that did not meet our inclusion criteria (Excluded studies). This review included five studies in the qualitative analysis (Amortegui 1978; Larson 2000; Larson 2005; Sharma 2013; Webster 1991), but none in a meta‐analysis (Figure 1). We also identified one ongoing study (NCT03755635). Webster 1991 was published in triplicate and was referenced as one study; however all three publications provided data for this review.
1.
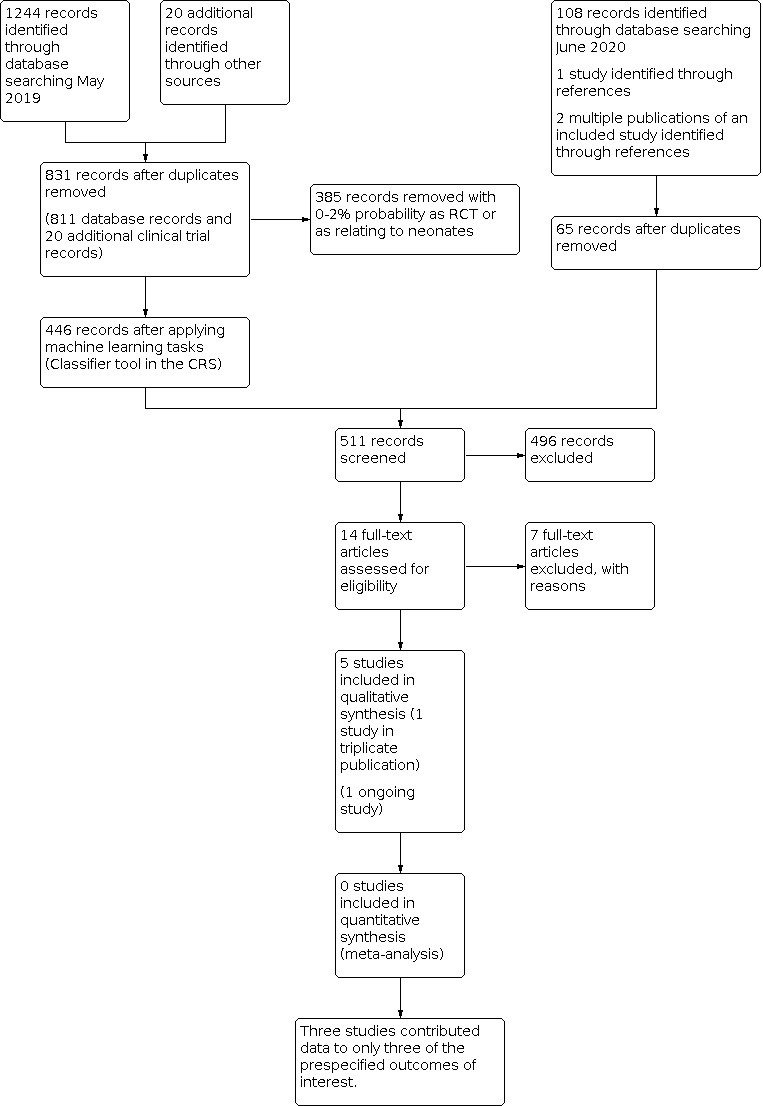
Study flow diagram.
Included studies
Our review included one RCT (Larson 2000), one quasi‐RCT (Webster 1991), and three cross‐over clinical trials (Amortegui 1978; Larson 2005; Sharma 2013). Four studies involved 279 nurses working in NICUs (Larson 2000; Larson 2005; Sharma 2013; Webster 1991). The number of nurses included in one study was not clearly stated (Amortegui 1978), and data were presented for samples obtained from nurses and neonates in each intervention group as count.
Study populations
Amortegui 1978 was conducted between October 1974 and March 1975 in two well‐baby nurseries at Magee Women's Hospital, in Pittsburgh, Pennsylvania, USA. The study included all nurses working in the nursery and all neonates on admission. The actual number of participants recruited was unclear; however, 602 samples of nurses and neonates, respectively, were cultured and data were reported as count.
Larson 2000 selected 16 nurses for this study because this design provided sufficient statistical power for researchers to determine moderate to large effect sizes for the two primary outcome variables: changes in numbers of colony‐forming units (CFUs) on hands, and clinical changes in skin condition.
Larson 2005 included 119 nurses and all neonates hospitalised for longer than 24 hours on the study units. Study authors reported that bloodstream infections, pneumonia, conjunctivitis, skin and soft tissue infections, and central nervous system infections were monitored because these represent more than 80% of all healthcare‐associated infections (HIs) in neonates. Surveillance was conducted prospectively by a study nurse epidemiologist who visited the units at least three times weekly. Sources of data included laboratory, radiology, and pharmacy records; patient records; information from physician and nursing staff; and direct observation of neonates. All microbiological testing was performed by the clinical Microbiology Service of the Columbia University Medical Center, in New York, New York. Standardised definitions from the National Nosocomial Infections Surveillance system (NNIS) adapted for use in neonates were used. The definition of conjunctivitis was broadened from the NNIS definition to include eye drainage with empirical antibiotic treatment. Interrater reliability was first established in pilot work and was confirmed during year 1 by infection data collected simultaneously and independently by the study nurse epidemiologist and by each hospital’s nurse epidemiologist. Reliability was monitored throughout the study during meetings between the nurse epidemiologist and the physician co‐investigators (a paediatric infectious disease specialist and a neonatologist). Cases with equivocal data and those that did not fulfil NNIS criteria were reviewed, and discrepancies were resolved by consensus.
Sharma 2013 was a randomised cross‐over trial involving 35 female nurses aged 25 to 48 years working in a NICU. This study did not provide any data for this review because it did not measure any of our outcomes of interest.
Webster 1991 was a 'control before and after' study with concurrent and historical control arms. This study was carried out between "the beginning of October 1989 to the end of October 1991". it included 109 nursing staff and all of the 1916 neonates in the intensive care unit of a major metropolitan Australian hospital. Study duration was 12 months, and results were published in triplicate as three different studies. Weekly nasal and umbilical swabs were taken from all babies. Those colonised with methicillin‐resistant Staphylococcus aureus (MRSA) were considered positive MRSA for the remainder of their hospital stay and were included in the estimates of weekly MRSA colonisation rates. Swabs were plated onto methicillin (10 mg/mL) mannitol salt agar (BBL11407) and were incubated at 35°C for 48 hours.
Study settings
Amortegui 1978 was conducted in two well‐baby nurseries at Magee Women's Hospital, in Pittsburgh, Pennsylvania, USA.
Larson 2000 was conducted in a 47‐bed NICU at Babies’ and Children’s Hospital of the New York Presbyterian Medical Center, in New York, New York, USA.
Larson 2005 was conducted in two NICUs in Manhattan, New York, USA.
Sharma 2013 was conducted at a level III NICU of a tertiary care institute in Northern India.
Webster 1991 was conducted in the neonatal unit at the Royal Women's Hospital, in Australia.
All studies recruited participants from NICUs. In most cases, the number of neonates included was not clearly specified.
For our primary outcomes, only one study provided data for Incidence of suspected infection (study author‐defined) within the first 28 days of life (Webster 1991). Two studies provided data on the incidence of bacteriologically confirmed infection (types of infection as specified by study authors) within the first 28 days of life (Larson 2005; Webster 1991). None of our included studies provided data on the following outcomes: 'all‐cause mortality within the first seven days of life (early neonatal death)'.and 'all‐cause mortality from the 8th to the 28th day of life (late neonatal death)'. For our secondary outcomes, none of the included studies provided data on the following: 'duration of hospital stay' and 'any hospitalisation for neonates managed at the community setting'. For the 'incidence of community‐acquired and hospital‐acquired infection' outcome, only Larson 2005 provided data. Last, Larson 2000, Larson 2005, and Webster 1991 provided data on 'study author‐reported adverse events such as skin changes and reactions to handwashing and rubs.' Two studies did not provide data for any of the listed primary and secondary outcomes (Amortegui 1978; Sharma 2013). However we presented data on umbilical cord colonisation of neonates as reported by Amortegui 1978 under 'other important outcomes not pre‐specified' because we agreed that this was an important outcome.
Interventions versus comparators
Efficacy of two iodophor products, betadine and Prepodyne (Amortegui 1978)
Head‐to‐head comparison of 2% chlorhexidine gluconate (CHG) (Scrub‐Care) versus non‐antimicrobial liquid detergent soap plus 10 second application of a 60% isopropanol preparation containing emollients (Larson 2000)
Head‐to‐head comparison of 2% CHG versus hand sanitiser containing 61% ethanol and emollients (Larson 2005)
Head‐to‐head comparison of plain soap versus alcohol hand rub and povidone‐iodine hand scrub (Sharma 2013)
4% CHG versus triclosan 1% w/v (Webster 1991)
Study funding sources
All included studies declared no conflicts of interests.
Larson 2005 was funded by grant 5 RO1 NR05197 from the National Institutes of Health, National Institute for Nursing Research, in Bethesda, Maryland, USA. "The funding organization had no influence on the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the article".
The four other studies did not declare their funding sources (Amortegui 1978; Larson 2000; Sharma 2013; Webster 1991).
Excluded studies
We excluded seven studies because they did not meet our inclusion criteria (Asare 2009; Azor‐Martinez 2018; Ditai 2019; Janota 2014; Kaufman 2014; Ng 2004; Webster 1989).
Risk of bias in included studies
Two review authors independently assessed the methodological quality of all included studies according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Figure 2; Figure 3) (Higgins 2011).
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We rated two studies as having low risk of bias for sequence generation (Larson 2000; Sharma 2013), two studies as having high risk of bias (Amortegui 1978; Webster 1991), and one study as having unclear risk of bias (Larson 2005). One study was rated as low risk of bias for allocation concealment (Sharma 2013), and the remaining four studies were rated as high risk of bias for allocation concealment (Amortegui 1978; Larson 2000; Larson 2005; Webster 1991).
Blinding
We rated one study as low risk (Sharma 2013), three studies as high risk (Larson 2000; Larson 2005; Webster 1991), and one study as unclear risk (Amortegui 1978), respectively, for performance bias.
We rated Sharma 2013 as low risk for detection bias, Webster 1991 as high risk for detection bias, and three studies as unclear risk for this domain (Amortegui 1978; Larson 2000; Larson 2005).
Incomplete outcome data
Four studies were rated as low risk of attrition bias (Amortegui 1978; Larson 2000; Larson 2005; Sharma 2013). One study was assessed as unclear risk of attrition bias because the information required to make a decision was not available (Webster 1991).
Selective reporting
We rated one study as low risk of bias (Larson 2000), three studies as unclear risk of bias (Amortegui 1978; Larson 2005; Webster 1991), and one study as high risk of bias (Sharma 2013), respectively, for selective reporting.
Other potential sources of bias
Larson 2000 was rated as low risk of bias and four studies as high risk of bias for suspected publication bias (Amortegui 1978; Larson 2005; Sharma 2013Webster 1991). Data obtained from Webster 1991 were reported in three different publications. Amortegui 1978 did not report whether there was a washout period before participants crossed to a new intervention group. Larson 2005 allowed a four week washout period before switching interventions; however rates of gloving used and rates of patient contact differ significantly between the two groups, and this is likely to affect outcomes. Sharma 2013 did not report any usable data.
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings 1. 2% chlorhexidine gluconate (CHG) compared to alcohol hand sanitiser (61% alcohol and emollients) for prevention of infection in neonates.
| 2% CHG compared to alcohol hand sanitiser (61% alcohol and emollients) for prevention of infection in neonates | ||||||
| Patient or population: prevention of infection in neonates Setting: neonatal intensive care unit Intervention: 2% CHG Comparison: alcohol hand sanitiser (61% alcohol and emollients) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with alcohol hand sanitiser (61% alcohol and emollients) | Risk with 2% CHG | |||||
| Incidence of (study author‐defined) suspected infection within the first 28 days of life | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Incidence of bacteriologically confirmed infection (types of infection as specified by study authors) within the first 28 days of life ‐ all infections | Study population | RR 2.19 (1.79 to 2.69) | 2932 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | Rates of patient contact differ significantly in the 2 groups and this is likely to affect outcomes | |
| 134 per 1000 | 294 per 1000 (240 to 361) | |||||
| All‐course mortality within the first 7 days of life (early neonatal death) | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| All‐cause mortality from the 8th to the 28th day of life (late neonatal death) | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Duration of hospital stay | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Incidence of community‐acquired infection and hospital‐acquired infection | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Adverse events (higher score is better) ‐ mean observers reported skin changes in nurses (mean score) | Mean adverse events (higher score is better) ‐ mean observers reported skin changes in nurses (mean score was 0) | MD 0.19 higher (0.03 higher to 0.35 higher) | ‐ | 120 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWe downgraded by two levels for very serious risk of bias due to study limitations.
bWe downgraded by one level for serious imprecision.
Summary of findings 2. 4% chlorhexidine gluconate (CHG) compared to plain liquid soap for prevention of infection in neonates.
| 4% CHG compared to plain liquid soap for prevention of infection in neonates | ||||||
| Patient or population: nurses and neonates Setting: neonatal intensive care unit Intervention: 4% CHG Comparison: plain liquid soap | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with plain liquid soap | Risk with 4% CHG | |||||
| Adverse outcome (higher score is better) ‐ mean visual scoring of skin (mean score) | Mean adverse outcome (higher score is better) ‐ mean visual scoring of skin (mean score) was 0 | MD 1.75 lower (3.31 lower to 0.19 lower) | ‐ | 16 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | Very small study. It was not reported if allocation was concealed, probably not done. Also it was not stated whether participants and assessors were blinded. Probably not done |
| Adverse outcome (higher score is better) ‐ mean hand self‐assessment (mean score) | Mean adverse outcome (higher score is better) ‐ mean hand self‐assessment (mean score) was 0 | MD 9.25 lower (12.29 lower to 6.21 lower) | ‐ | 16 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | |
| Incidence of bacteriologically confirmed infection within the first 28 days of life | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Incidence of (study author‐defined) suspected infection within the first 28 days of life | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| All‐cause mortality within the first 7 days of life (early neonatal death) | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| All‐cause mortality from the 8th to the 28th day of life (late neonatal death) | ‐ | Not reported | ||||
| Duration of hospital stay | ‐ | Not measured | ||||
| Any hospitalisation for neonates managed in the community setting | ‐ | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWe downgraded by two levels for very serious to high risk of bias due to study limitations.
bWe downgraded by two levels for very serious imprecision due to very wide confidence intervals.
Summary of findings 3. Chlorhexidine gluconate 4% compared to triclosan 1% for prevention of infection in neonates.
| Chlorhexidine gluconate 4% compared to triclosan 1% for prevention of infection in neonates | ||||||
| Patient or population: prevention of infection in neonates Setting: neonatal Intensive care unit Intervention: chlorhexidine gluconate 4% Comparison: triclosan 1% | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with triclosan 1% | Risk with chlorhexidine gluconate 4% | |||||
| Incidence of suspected new infection | Study population | RR 1.04 (0.19 to 5.60) | 1916 (1 RCT) | ⊕⊝⊝⊝ Very lowa‐c | ||
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Total incidence of new infection (bacteriologically confirmed) | Study population | RR 6.01 (3.56 to 10.14) | 1916 (1 RCT) | ⊕⊝⊝⊝ Very lowa‐c | ||
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| All‐cause mortality within the first 7 days of life (early neonatal death) | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| All‐cause mortality from the 8th to the 28th day of life (late neonatal death) | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Duration of hospital stay ‐ not measured | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Incidence of community‐acquired and hospital‐acquired infection | ‐ | ‐ | ‐ | ‐ | ‐ | Not measured |
| Study author‐reported adverse events assessed with: Visual scoring of skin condition scale follow‐up: mean 7 weeks |
Mean study author‐reported adverse events score was 1.9 | MD 1.04 score higher (0.5 higher to 1.58 higher) | ‐ | 1916 (1 RCT) | ⊕⊝⊝⊝ Very lowa‐c | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWe downgraded by two levels for very serious risk of bias due to study limitations.
bWe downgraded by two levels for very serious imprecision.
cWe downgraded by one level for publication bias because the data were published in multiple studies.
Primary outcomes
1. Incidence of (study author‐defined) suspected infection within the first 28 days of life
Webster 1991 compared the effects of 1% w/v triclosan (Novaderm) versus 4% w/v chlorhexidine gluconate (Hibiciens) for prevention of infection. Study authors reported fewer new cases of suspected infection in the 1% w/v triclosan group. One study compared 1% w/v triclosan versus 4% chlorhexidine gluconate and reported a lower incidence of suspected infection in the 1% w/v triclosan group (risk ratio (RR) 1.04, 95% confidence interval (CI) 0.19 to 5.60; 1916 participants, 1 study; very low‐certainty evidence) compared to the 4% chlorhexidine gluconate (CHG) group (Analysis 3.1).
3.1. Analysis.

Comparison 3: Chlorhexidine gluconate 4% versus triclosan 1%, Outcome 1: incidence of new infection
2. Incidence of bacteriologically confirmed infection (types of infection as specified by study authors) within the first 28 days of life
Larson 2005 assessed the effects of antiseptic detergent hand wash (2% chlorhexidine gluconate) versus alcohol hand sanitiser (61% alcohol and emollients) on the infection rate in neonates. We are uncertain whether 2% chlorhexidine gluconate reduces the risk of all infection among neonates compared to 61% alcohol hand sanitiser with regards to the following types of infection: pneumonia (RR 2.17, 95% CI 0.79 to 5.96; 2932 participants, 1 study; very low‐certainty evidence), central nervous system (CNS) infection (RR 2.57, 95% CI 0.84 to 7.85; 2932 participants, 1 study; very low‐certainty evidence), and skin sepsis (RR 1.76, 95% CI 0.94 to 3.29; 2932 participants, 1 study; very low‐certainty evidence). This analysis shows that neonates tend to have lower risk of conjunctivitis (RR 3.18, 95% CI 2.32 to 4.37; 2932 participants, 1 study; very low‐certainty evidence) and bloodstream infection (RR 2.26, 95% CI 1.73 to 2.93; 2932 participants, 1 study; very low‐certainty evidence), and lower overall risk of infection (RR 2.19, 95% CI 1.79 to 2.69; 2932 participants, 1 study; very low‐certainty evidence) with alcohol hand sanitiser (61% ethanol and emollients) (Analysis 1.2). Larson 2005 used standardised definitions from the NNIS for diagnosis of neonatal infection adapted for use in neonates.
Overall, Webster 1991 reported fewer cases of methicillin‐resistant Staphylococcus aureus (MRSA) infection in the 1% w/v triclosan group compared to the CHG group, respectively (RR 1.04, 95% CI 0.19 to 5.60; 1916 participants, 1 study; very low‐certainty evidence). The incidence of nosocomial septicaemia was lower in the 1% w/v triclosan group compared to the CHG group (RR 10.97, 95% CI 5.35 to 22.51; 1916 participants, 1 study; very low‐certainty evidence), and new cases of necrotising enterocolitis were fewer (RR 6.61, 95% CI 2.55 to 17.12; 1919 participants, 1 study), as were new cases of total infection (RR 6.01, 95% CI 3.56 to 10.14; 1916 participants, 1 study). However, there was no difference in the rate of new cases of nosocomial meningitis (RR 3.14, 95% CI 0.20 to 50.27; 1916 participants, 1 study; very low‐certainty evidence) and new cases of nosocomial viral infection (RR 3.14, 95% CI 0.63 to 15.58; 1916 participants, 1 study; very low‐certainty evidence) (Analysis 3.1).
3. All‐cause mortality within the first seven days of life (early neonatal death)
None of the included studies reported on this outcome.
4. All‐cause mortality from the 8th to the 28th day of life (late neonatal death)
None of the included studies reported on this outcome.
Sharma 2013 did not report any usable data, and study authors did not respond to our request for additional data.
Secondary outcomes
5. Duration of hospital stay
None of the included studies reported on this outcome.
6. Any hospitalisation for neonates managed in the community setting
None of the included studies reported on this outcome.
7. Incidence of community‐acquired and hospital‐acquired infection
None of our included studies reported this outcome; our intention was to disaggregate this outcome into community‐acquired infection and hospital‐acquired infection. However, Larson 2005 reported seven clusters of bacterial infection during this study. Four clusters were in the 2% CHG group, and three were in the alcohol hand sanitiser group. Study authors indicated that they were not sure if the outbreaks were related to the interventions and stated that "because of these uncertainties, we could not control for these clusters in the analysis".
8. Study author‐reported adverse events such as skin changes and reactions to hand wash and rubs/sanitisers
Three of the included studies pre‐specified the skin condition of nurses' hands as one of their outcomes and reported effects of the intervention (Larson 2000; Larson 2005; Webster 1991). All three used previously validated scales; with these scales, a higher score means the intervention has greater benefit and a lower score means the intervention causes greater harm. Skin conditions were reported as "extensive cracking of skin surface, widespread reddening, or occasional bleeding, damaged or undamaged hand".
Larson 2005 assessed the comparative effects of detergent soap versus alcohol hand rinse (61% alcohol and emollients) versus antiseptic detergent hand wash (2% CHG alone) on skin conditions. We are uncertain whether antiseptic detergent has better effects on skin than 'alcohol hand sanitiser' (mean difference (MD) ‐0.80, 95% CI 0.01 to 1.59; 274 participants, 1 study; very low‐certainty evidence). We are not certain whether antiseptic detergent is better for the skin than alcohol hand sanitiser (MD ‐0.19, 95% CI 0.03 to 0.35; 274 participants, 1 study; very low‐certainty evidence) (Analysis 1.2).
1.2. Analysis.

Comparison 1: 2% chlorhexidine gluconate (CHG) versus alcohol hand sanitiser (61% alcohol and emollients), Outcome 2: Adverse events (higher score is better)
Webster 1991 reported that the proportion of nurses with different skin conditions was higher in the CHG group than in the triclosan group (reported as 'mean hand damage score') (MD 1.04, 95% CI 0.50 to 1.58; 1916 participants, 1 study; very low‐certainty evidence). In addition, Larson 2000 reported that the skin condition in the plain soap group was rated as better than in the 4% CHG for mean 'visual score of skin condition' (MD ‐1.75, 95% CI ‐3.31 to ‐0.19; 16 participants, 1 study; very low‐certainty evidence) and mean 'hand self‐assessment score' (MD ‐9.25, 95% CI ‐12.29 to ‐6.21; 16 participants, 1 study; very low‐certainty evidence) (Analysis 2.1).
2.1. Analysis.

Comparison 2: 2% chlorhexidine gluconate (CHG) versus plain liquid soap, Outcome 1: Adverse outcome (higher score is better)
We are uncertain whether plain soap has a better effect on the skin compared to 4% CHG.
Other important outcomes were not pre‐specified.
Amortegui 1978 assessed the effects of two iodophor products (betadine versus Prepodyne) on umbilical cord swab culture positivity. We are uncertain whether betadine prevents umbilical cord positivity compared to Prepodyne (RR 2.97, 95% CI 2.49 to 3.53; very low‐certainty evidence) (Analysis 4.2).
4.2. Analysis.

Comparison 4: Iodophor products (betadine vs Prepodyne), Outcome 2: Infant umbilical positivity
Discussion
Summary of main results
The main objective of this review was to ascertain the effectiveness of different hand hygiene agents for prevention of neonatal infection in community and health facility settings. Infections including sepsis in newborns are major causes of death (Liu 2015), prolonged hospital stay, and early and long‐term complications, as well as huge economic burdens, particularly in low‐ and middle‐income countries (LMICs) (Ranjeva 2018). Contaminated hands of mothers, other caregivers, and healthcare workers (HCWs) are major sources of these infections; therefore, it is plausible that good hand hygiene interventions, which are relatively cheap and easy to implement, may reduce the incidence and burden of infection among newborns. We conducted this review with the aim of generating evidence‐based statements with regards to the effectiveness of different hand hygiene agents for preventing infection in the newborn.
In summary, we found five studies, four of which had usable data; unfortunately, all provided evidence of very low certainty. Pertaining to the primary outcomes, none of the studies retrieved compared any form of hand hygiene practice versus no intervention, possibly because hand hygiene is a universally recommended aspect of hospital care (WHO 2009); hence, it would be unlikely to have studies with the outright exclusion of some forms of hand hygiene for ethical reasons. Three studies assessed the superiority or otherwise of the use of one form of antiseptic agent for hand hygiene over another as regards prevention of non‐invasive infection ‐ Amortegui 1978; Webster 1991 ‐ and invasive infection ‐ Larson 2005 ‐ in the newborn. Another study reported significantly fewer new cases of methicillin‐resistant Staphylococcus aureus (MRSA) infection among neonates in the 1% w/v triclosan group compared to the 4% chlorhexidine gluconate group (Webster 1991). Similarly, neonates in the 2% chlorhexidine gluconate antiseptic detergent wash group recorded reduced risks of conjunctivitis, skin infection, central nervous system infection, pneumonia, and bloodstream infection compared to neonates in the 61% alcohol hand sanitiser group (Larson 2005), but the evidence is very uncertain. Unfortunately, the heterogeneity of assessed hand hygiene agents and the high risk of bias of most of the included studies did not permit any meaningful conclusions.
None of the included studies reported on the effectiveness of hand hygiene practice for all‐cause early or late neonatal death, duration of hospital stay, or the need for in‐hospital care for neonates studied in the community. Nevertheless, three studies assessed the adverse effects of one form of hand hygiene agent over another as regards skin changes and skin reactions in the hands of HCWs, although these studies were all rated as providing very low‐certainty evidence (Larson 2000, Larson 2005, Webster 1991). Triclosan (Webster 1991), detergent soap with 61% alcohol hand rinse (Larson 2005), and plain soap with alcohol‐based hand rinse ‐ Larson 2000 ‐ were all rated better by HCWs than various strengths and formulations of 4% chlorhexidine gluconate (CHG) in terms of objective or self‐assessment reports of skin changes and reactions following use. However, the ease of application of the former, being faster to carry out, may reduce the duration of contact with the skin with less irritation and better quality of hand wash (Larson 2005).
One study compared the effects of two iodophors (betadine and Prepodyne) on umbilical cord colonisation; however we are uncertain whether Prepodyne was more effective for preventing neonatal skin colonisation (Amortegui 1978). According to the study authors, the difference observed "was probably due to nursery variation rather than product variation". Although colonisation was not a pre‐specified outcome in this review, a possible reduction in colonisation rates may be clinically useful as it may be a pointer to the potential of these agents in reducing neonatal infection.
Overall completeness and applicability of evidence
The identified studies fell short in addressing all objectives set out in the protocol for this study. Community‐based trials assessing effects of hand hygiene practice on important outcomes such as all‐cause mortality, prolonged hospitalisation, and need for in‐hospital care were not available. The trials included in this review assessed different hand antiseptic agents, making meta‐analysis not feasible. Additionally, only one of the included studies was conducted in a low‐ and middle‐income country (LMIC), but this study was not usable as it did not provide data on any of the pre‐specified outcomes of interest (Sharma 2013). It is also important to note that all trials included in this study were conducted in the hospital setting, specifically in neonatal intensive care units. Participants in all trials were nurses, as none of the studies reported parental involvement. This limits our consideration of input from the community and parental perspective.
In view of the paucity of reliable clinical trials on this problem, no conclusive statement can be made for now on the effectiveness of any hand hygiene agent for preventing infection in the newborn. The challenge is the diverse nature of agents deployed for the various trials. It probably would have been a lot better if most of the studies had used the same or similar hand hygiene agents. It is important to note that only one study measured a clinically important infection rate in terms of hospital‐acquired infection, but this finding is of limited value as the study authors could not confidently ascribe the observed clustering of infection outbreaks to the interventions (Larson 2005). Chlorhexidine, in varying concentrations, and alcohol hand sanitisers.are currently recommended for hand hygiene practice in patient care. Only three studies provided data on the adverse effects of these interventions, and fewer adverse events were reported for 1% w/v triclosan (Webster 1991), plain soap (Larson 2000), and disinfectant detergents only (Larson 2005). However, patterns and grading of severity of these adverse events with respect to each type of intervention were not described in detail.
Therefore, we summarise here that the applicability of findings in this review is limited by the fact that all assessed trials were conducted in high‐income countries (HICs), within hospital settings, among nurses without non‐healthcare worker involvement, and some of the interventions reported on are no longer recommended for use in patient care. However, antiseptic soaps, chlorhexidine, and alcohol hand sanitisers continue to be recommended for use during patient care.
Quality of the evidence
This review included data from one randomised controlled trial (RCT), three cross‐over trials, and one randomised cross‐over trial with low to high risk of bias across all domains (Figure 2). Two studies were rated low risk, two studies were rated high risk, and one study was rated unclear risk for selection bias. One study was rated low risk and four studies were rated high risk for allocation bias. Only one of the studies was rated low risk for performance bias. Using the GRADE approach (Schünemann 2013), we rated the quality of evidence for the primary outcomes of incidence of study author‐defined infection as low, as reported in the 'Summary of findings' tables (Table 1; Table 2), and evidence of adverse skin reactions or skin changes following the use of various hand hygiene agents was rated as very low certainty (Table 3). We downgraded the quality of this evidence for very serious study limitations and imprecision.
Potential biases in the review process
This review clearly highlights the paucity of high‐quality clinical trials on the effectiveness of hand hygiene for prevention of infection among newborns. This is regarded as a limitation of this review. Similarly, some of the studies included in this review were quasi‐randomised clinical trials with potentially high risk of bias. We contacted one of the study authors by email to ask for additional information (Sharma 2013); however, this author could not provide the requested data because the outcomes were not assessed.
One of the trials we assessed reported on umbilical cord colonisation rather than suspected or confirmed neonatal infection as pre‐specified outcomes (Amortegui 1978). Although we agree that colonisation is not the same as infection, we reported this outcome as other outcomes not pre‐specified because we believe strongly that it is an important outcome and could be useful for decision‐making. Extensive search of standard databases was conducted, and this search has been lately updated with no additional significantly useful findings. We are not oblivious to the likelihood of a few relevant publications in some hard‐to‐reach databases currently not being accessed. If there were studies in the databases comparing interventions with no form of hand hygiene, such studies would have been found due to their associated ethical importance. Inclusion of the study with a suspected non‐validated scale for measuring skin conditions complicating the use of hand hygiene agents was considered helpful, as this study provided insight into the spectrum of skin conditions that may occur following the use of hand hygiene agents. The pre‐specified outcome was author‐reported skin changes rather than grades of severity of skin conditions. To resolve the problem of missing data in the included study with unusable data (Sharma 2013), we contacted one of the study authors but received no response.
Agreements and disagreements with other studies or reviews
Our review finding is consistent with the conclusion of another Cochrane systematic review (Tanner 2016), which found no conclusive evidence 'that one type of hand antisepsis was better than another in reducing surgical site infections'. However, a non‐Cochrane systematic review concluded that hand rub appeared more effective when compared to hand wash in intensive care units based on low‐quality evidence (Bello 2020).
Authors' conclusions
Implications for practice.
RCTs have provided insufficient data for review authors to determine the most effective agent for hand hygiene for prevention of neonatal infection.
In addition, we found a paucity of data that would allow us to reach meaningful conclusions pertaining to the superiority of one form of antiseptic hand hygiene agent over another for prevention of neonatal infection. Also, the sparse available data were of very low certainty.
Other critical aspects of hand hygiene such as the actual technique of hand hygiene, particularly the seven steps and five moments of handwashing, as well as the duration of the hand hygiene procedure, were not measured in the included trials. These are also critical in influencing the effectiveness of hand hygiene for preventing neonatal infection or the superiority of one antiseptic agent over another. We received insufficient data from the included trials to determine the best hand hygiene agents, resulting in no confidence in the effect estimate due to very serious study limitations and imprecision.
Implications for research.
The findings of this review derived from trials conducted in high‐income countries (HICs) clearly call for more carefully designed randomised controlled trials (RCTs) that will be conducted in both HICs and low‐ and middle‐income countries (LMICs) to assess the effects of hand hygiene practices on prevention of non‐invasive and invasive infection among newborns and infection‐related mortality and morbidity, including length of hospital stay, and will provide information of more widespread applicability. Future studies should measure outcomes of invasive and non‐invasive infection, as well as associated mortality. This implies that subsequent trials should specify accepted definitions of suspected and confirmed infection as measurable outcomes. These future studies should adopt validated scales by which to grade the severity of skin conditions occurring as adverse effects of hand hygiene agents. This, along with the ease and duration of application, may be used to assess the acceptability of hand hygiene agents. In addition, such trials should specifically adopt a universally recommended technique for hand hygiene such as the seven steps and five moments of hand hygiene. It is also important for researchers to assess compliance with hand hygiene needs.
The use or otherwise of these hand hygiene agents depends on their acceptability by caregivers and healthcare workers (HCWs), which, in turn, depends on whether or not the agent is skin friendly. Conducting additional clinical trials on effects of these hand hygiene agents on skin reactions and skin changes among caregivers and HCWs will be worthwhile.
What's new
| Date | Event | Description |
|---|---|---|
| 27 May 2021 | Amended | Minor edits to forest plots. |
History
Protocol first published: Issue 5, 2019 Review first published: Issue 1, 2021
Acknowledgements
We would like to thank Cochrane Neonatal ‐ Colleen Ovelman, Managing Editor; Jane Cracknell, Assistant Managing Editor; Roger Soll, Co‐coordinating Editor; and Bill McGuire, Co‐coordinating Editor ‐ who provided editorial and administrative support. Carol Friesen, Information Specialist, designed and ran the literature searches. Jeffrey Horbar and Jacqueline Ho peer‐reviewed and offered feedback on this review.
This Cochrane Review is a product of the priority setting exercise conducted by Cochrane Nigeria for the Cochrane African Network Project. We acknowledge the contributions of the staff and associates of Cochrane Nigeria and all stakeholders including consumer representatives who participated in the priority setting exercise. We thank Yemisi Pius, a member of the Cochrane Consumer Network, for her comments and suggestions.
The Methods section of this protocol is based on a standard template used by Cochrane Neonatal.
Appendices
Appendix 1. Search strategies
The RCT filters have been created using Cochrane's highly sensitive search strategies for identifying randomised trials (Higgins 2011). The neonatal filters were created and tested by the Cochrane Neonatal Information Specialist. Ovid MEDLINE Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily, and Ovid MEDLINE(R) 1946 to Present: Terms: 1. exp Hand Hygiene/ 2. exp Hand Disinfection/ 3. (handwash* or handrub*).mp. 4. (hand* adj2 (clean* or decontaminat* or disinfect* or hygiene or hygienic* or saniti* or sterili* or wash* or scrub* or alcohol* or antisep* or disinfect* or rub* or aseps* or aseptic* or wipe* or chlorhexidine or triclosan or soap* or propanol* or ethanol* or antiinfective* or anti‐infective*)).mp. 5. (hand* adj2 chlorine adj2 derivative*).mp. 6. (hand* adj2 iodine chloroxylenol).mp. 7. (hand* adj2 quaternary ammonium compound*).mp. 8. (scrub* adj2 surgical).mp. 9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 10. exp HAND/ 11. hand*.tw,kf. 12. 10 or 11 13. exp Bacterial Infections/pc [Prevention & Control] 14. exp Cross Infection/pc [Prevention & Control] 15. exp HYGIENE/ 16. exp Infection Control/ 17. exp DISINFECTANTS/ 18. exp SOLUTIONS/ 19. exp ALCOHOLS/ 20. exp Anti‐Infective Agents, Local/ 21. exp SOAPS/ 22. exp ANTISEPSIS/ 23. exp DISINFECTION/ 24. exp STERILIZATION/ 25. exp CHLORHEXIDINE/ 26. exp TRICLOSAN/ 27. exp Quaternary Ammonium Compounds/ 28. 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 29. 12 and 28 30. 9 or 29 31. exp infant, newborn/ 32. (newborn* or new born or new borns or newly born or baby* or babies or premature or prematurity or preterm or pre term or low birth weight or low birthweight or VLBW or LBW or infant or infants or infantile or infancy or neonat*).ti,ab. 33. 31 or 32 34. randomized controlled trial.pt. 35. controlled clinical trial.pt. 36. randomized.ab. 37. placebo.ab. 38. drug therapy.fs. 39. randomly.ab. 40. trial.ab. 41. groups.ab. 42. or/34‐41 43. exp animals/ not humans.sh. 44. 42 not 43 45. 33 and 44 46. 30 and 45 MEDLINE via PubMed: Terms: ((("Hand Hygiene"[Mesh] OR "Hand Disinfection"[Mesh]) OR (handwash* OR handrub*) OR (hand* AND (clean* OR decontaminat* OR disinfect* OR hygiene OR hygienic* OR saniti* OR sterili* OR wash* OR scrub* OR alcohol* OR antisep* OR disinfect* OR rub* OR aseps* OR aseptic* OR wipe* OR chlorhexidine OR triclosan OR soap* OR propanol* OR ethanol* OR antiinfective* OR anti‐infective*)) OR (hand* AND chlorine AND derivative*) OR (hand* AND iodine chloroxylenol) OR (hand* AND quaternary ammonium compound*) OR (scrub* AND surgical)) OR (("Hand"[Mesh] OR hand*) AND ((((((((((((((("Bacterial Infections/prevention and control"[Mesh]) OR "Cross Infection/prevention and control"[Mesh]) OR "Hygiene"[Mesh]) OR "Infection Control"[Mesh]) OR "Disinfectants"[Mesh]) OR "Solutions"[Mesh]) OR "Alcohols"[Mesh]) OR "Anti‐Infective Agents, Local"[Mesh]) OR "Soaps"[Mesh]) OR "Antisepsis"[Mesh]) OR "Disinfection"[Mesh]) OR "Sterilization"[Mesh]) OR "Chlorhexidine"[Mesh]) OR "Triclosan"[Mesh]) OR "Quaternary Ammonium Compounds"[Mesh]))) AND (((infant, newborn[MeSH] OR newborn*[TIAB] OR "new born"[TIAB] OR "new borns"[TIAB] OR "newly born"[TIAB] OR baby*[TIAB] OR babies[TIAB] OR premature[TIAB] OR prematurity[TIAB] OR preterm[TIAB] OR "pre term"[TIAB] OR "low birth weight"[TIAB] OR "low birthweight"[TIAB] OR VLBW[TIAB] OR LBW[TIAB] OR infant[TIAB] OR infants[TIAB] OR infantile[TIAB] OR infancy[TIAB] OR neonat*[TIAB]) AND (randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized[tiab] OR placebo[tiab] OR drug therapy[sh] OR randomly[tiab] OR trial[tiab] OR groups[tiab]) NOT (animals[mh] NOT humans[mh]))) Publication date from 2018/04/01 CINAHL via EBSCOhost: Terms: (hand* AND (clean* OR decontaminat* OR disinfect* OR hygiene OR hygienic* OR saniti* OR sterili* OR wash* OR scrub* OR alcohol* OR antisep* OR disinfect* OR rub* OR aseps* OR aseptic* OR wipe* OR chlorhexidine OR triclosan OR soap* OR propanol* OR ethanol* OR antiinfective* OR anti‐infective*)) OR (hand* AND chlorine AND derivative*) OR (hand* AND iodine chloroxylenol) OR (hand* AND quaternary ammonium compound*) OR (scrub* AND surgical)) AND (infant or infants or infantile or infancy or newborn* or "new born" or "new borns" or "newly born" or neonat* or baby* or babies or premature or prematures or prematurity or preterm or preterms or "pre term" or premies or "low birth weight" or "low birthweight" or VLBW or LBW) AND (randomized controlled trial OR controlled clinical trial OR randomized OR placebo OR clinical trials as topic OR randomly OR trial OR PT clinical trial) Embase via Ovid: Terms: 1. exp hand washing/ 2. exp hand disinfection/ 3. (handwash* or handrub*).mp. 4. (hand* adj2 (clean* or decontaminat* or disinfect* or hygiene or hygienic* or saniti* or sterili* or wash* or scrub* or alcohol* or antisep* or disinfect* or rub* or aseps* or aseptic* or wipe* or chlorhexidine or triclosan or soap* or propanol* or ethanol* or antiinfective* or anti‐infective*)).mp. 5. (hand* adj2 chlorine adj2 derivative*).mp. 6. (hand* adj2 iodine chloroxylenol).mp. 7. (hand* adj2 quaternary ammonium compound*).mp. 8. (scrub* adj2 surgical).mp. 9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 10. exp hand/ 11. hand*.mp. 12. 10 or 11 13. exp bacterial infection/pc [Prevention] 14. exp cross infection/pc [Prevention] 15. exp hygiene/ 16. exp infection control/ 17. exp disinfectant agent/ 18. exp "solution and solubility"/ 19. exp alcohol derivative/ 20. exp alcohol/ 21. exp topical antiinfective agent/ 22. exp soap/ 23. exp antisepsis/ 24. exp disinfection/ 25. exp instrument sterilization/ 26. exp chlorhexidine/ 27. exp triclosan/ 28. exp quaternary ammonium derivative/ 29. 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 30. 12 and 29 31. 9 or 30 32. exp prematurity/ 33. exp infant/ 34. (newborn* or new born or new borns or newly born or baby* or babies or premature or prematurity or preterm or pre term or low birth weight or low birthweight or VLBW or LBW or infant or infants or infantile or infancy or neonat*).ti,ab. 35. 32 or 33 or 34 36. (human not animal).mp. 37. (randomized controlled trial or controlled clinical trial or randomized or placebo or clinical trials as topic or randomly or trial or clinical trial).mp. 38. 35 and 36 and 37 39. 31 and 38 Cochrane CENTRAL via CRS Web: Terms: 1. MESH DESCRIPTOR Hand Hygiene EXPLODE ALL AND CENTRAL:TARGET 2. MESH DESCRIPTOR Hand Disinfection EXPLODE ALL AND CENTRAL:TARGET 3. handwash* or handrub* AND CENTRAL:TARGET 4. hand* ADJ2 (clean* or decontaminat* or disinfect* or hygiene or hygienic* or saniti* or sterili* or wash* or scrub* or alcohol* or antisep* or disinfect* or rub* or aseps* or aseptic* or wipe* or chlorhexidine or triclosan or soap* or propanol* or ethanol* or antiinfective* or anti‐infective*) AND CENTRAL:TARGET 5. hand* ADJ2 chlorine ADJ2 derivative* AND CENTRAL:TARGET 6. hand* ADJ2 iodine chloroxylenol AND CENTRAL:TARGET 7. hand* ADJ2 quaternary ammonium compound* AND CENTRAL:TARGET 8. scrub* ADJ2 surgical AND CENTRAL:TARGET 9. #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 10. MESH DESCRIPTOR Bacterial Infections EXPLODE ALL WITH QUALIFIER PC AND CENTRAL:TARGET 11. MESH DESCRIPTOR Cross Infection EXPLODE ALL WITH QUALIFIER PC AND CENTRAL:TARGET 12. MESH DESCRIPTOR Hygiene EXPLODE ALL AND CENTRAL:TARGET 13. MESH DESCRIPTOR Infection Control EXPLODE ALL AND CENTRAL:TARGET 14. MESH DESCRIPTOR Disinfectants EXPLODE ALL AND CENTRAL:TARGET 15. MESH DESCRIPTOR Solutions EXPLODE ALL AND CENTRAL:TARGET 16. MESH DESCRIPTOR Alcohols EXPLODE ALL AND CENTRAL:TARGET 17. MESH DESCRIPTOR Anti‐Infective Agents, Local EXPLODE ALL AND CENTRAL:TARGET 18. MESH DESCRIPTOR SOAPS EXPLODE ALL AND CENTRAL:TARGET 19. MESH DESCRIPTOR Antisepsis EXPLODE ALL AND CENTRAL:TARGET 20. MESH DESCRIPTOR Disinfection EXPLODE ALL AND CENTRAL:TARGET 21. MESH DESCRIPTOR Sterilization EXPLODE ALL AND CENTRAL:TARGET 22. MESH DESCRIPTOR Chlorhexidine EXPLODE ALL AND CENTRAL:TARGET 23. MESH DESCRIPTOR Triclosan EXPLODE ALL AND CENTRAL:TARGET 24. MESH DESCRIPTOR Quaternary Ammonium Compounds EXPLODE ALL AND CENTRAL:TARGET 25. #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 26. MESH DESCRIPTOR Hand EXPLODE ALL AND CENTRAL:TARGET 27. (hand*):TI AND CENTRAL:TARGET 28. (hand*):AB AND CENTRAL:TARGET 29. (hand*):KW AND CENTRAL:TARGET 30. (hand*):KY AND CENTRAL:TARGET 31. #30 OR #29 OR #28 OR #27 OR #26 32. #31 AND #25 33. #9 OR #32 34. MESH DESCRIPTOR Infant, Newborn EXPLODE ALL AND CENTRAL:TARGET 35. infant or infants or infantile or infancy or newborn* or "new born" or "new borns" or "newly born" or neonat* or baby* or babies or premature or prematures or prematurity or preterm or preterms or "pre term" or premies or "low birth weight" or "low birthweight" or VLBW or LBW or ELBW or NICU AND CENTRAL:TARGET 36. #35 OR #34 AND CENTRAL:TARGET 37. #36 AND #33 Clinical Trial Registries: Clinicaltrials.gov: Search terms: handwash* OR hand hygiene OR hand washing OR hand rub OR handrub OR hand sanitizer OR hand sanitiser OR hand disinfection OR hand cleaning OR hand scrub | infant OR newborn OR neonate OR neonatal OR neonates OR preterm OR low birth weight OR low birthweight OR LBW | Child Date searched: May 10, 2019 Retrieved: 23 (20 after duplicates removed) ISRCTN.com: Search terms: newborn AND infection AND hand hygiene infant AND infection AND hand hygiene Neonate AND infection AND hand hygiene
Appendix 2. Risk of bias tool
1. Sequence generation (checking for possible selection bias). Was the allocation sequence adequately generated?
For each included study, we categorised the method used to generate the allocation sequence as:
low risk (any truly random process, e.g. random number table; computer random number generator);
high risk (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number); or
unclear risk.
2. Allocation concealment (checking for possible selection bias). Was allocation adequately concealed?
For each included study, we categorised the method used to conceal the allocation sequence as:
low risk (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk (open random allocation; unsealed or non‐opaque envelopes; alternation; date of birth); or
unclear risk.
3. Blinding of participants and personnel (checking for possible performance bias). Was knowledge of the allocated intervention adequately prevented during the study?
For each included study, we categorised the methods used to blind study participants and personnel from knowledge of which intervention a participant received. Blinding was assessed separately for different outcomes or classes of outcomes. We categorised the methods as:
low risk, high risk, or unclear risk for participants; and
low risk, high risk, or unclear risk for personnel.
4. Blinding of outcome assessment (checking for possible detection bias). Was knowledge of the allocated intervention adequately prevented at the time of outcome assessment?
For each included study, we categorised the methods used to blind outcome assessment. Blinding was assessed separately for different outcomes or classes of outcomes. We categorised the methods as:
low risk for outcome assessors;
high risk for outcome assessors; or
unclear risk for outcome assessors.
5. Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations). Were incomplete outcome data adequately addressed?
For each included study and for each outcome, we described the completeness of data including attrition and exclusions from the analysis. We noted whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion when reported, and whether missing data were balanced across groups or were related to outcomes. When sufficient information was reported or supplied by the trial authors, we re‐included missing data in the analyses. We categorised the methods as:
low risk (< 20% missing data);
high risk (≥ 20% missing data); or
unclear risk.
6. Selective reporting bias. Are reports of the study free of the suggestion of selective outcome reporting?
For each included study, we described how we investigated the possibility of selective outcome reporting bias and what we found. For studies in which study protocols were published in advance, we compared pre‐specified outcomes versus outcomes eventually reported in the published results. If the study protocol was not published in advance, we contacted study authors to gain access to the study protocol. We assessed the methods as:
low risk (when it is clear that all of the study's pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk (when not all of the study's pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified outcomes of interest and are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported); or
unclear risk.
7. Other sources of bias. Was the study apparently free of other problems that could put it at high risk of bias?
For each included study, we described any important concerns we had about other possible sources of bias (e.g. whether there was a potential source of bias related to the specific study design, whether the trial was stopped early due to some data‐dependent process). We assessed whether each study was free of other problems that could put it at risk of bias as:
low risk;
high risk; or
unclear risk.
If needed, we explored the impact of the level of bias through undertaking sensitivity analyses.
Data and analyses
Comparison 1. 2% chlorhexidine gluconate (CHG) versus alcohol hand sanitiser (61% alcohol and emollients).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Changes in the numbers of colony‐forming units (CFUs) on nurses’ hands | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.12, 0.32] | |
| 1.2 Adverse events (higher score is better) | 1 | Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.37, ‐0.06] | |
| 1.2.1 Mean self‐reported skin change of nurses (mean score) | 1 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐1.59, ‐0.01] | |
| 1.2.2 Mean observer‐reported skin changes of nurses (mean score) | 1 | Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.35, ‐0.03] | |
| 1.3 Incidence rate of infection | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.3.1 Pneumonia | 1 | 2932 | Risk Ratio (IV, Fixed, 95% CI) | 2.17 [0.79, 5.96] |
| 1.3.2 CNS | 1 | 2932 | Risk Ratio (IV, Fixed, 95% CI) | 2.57 [0.84, 7.85] |
| 1.3.3 Skin | 1 | 2932 | Risk Ratio (IV, Fixed, 95% CI) | 1.76 [0.94, 3.29] |
| 1.3.4 Conjunctivitis | 1 | 2932 | Risk Ratio (IV, Fixed, 95% CI) | 3.18 [2.32, 4.37] |
| 1.3.5 Bloodstream | 1 | 2932 | Risk Ratio (IV, Fixed, 95% CI) | 2.26 [1.73, 2.93] |
| 1.3.6 All infections | 1 | 2932 | Risk Ratio (IV, Fixed, 95% CI) | 2.19 [1.79, 2.69] |
1.1. Analysis.

Comparison 1: 2% chlorhexidine gluconate (CHG) versus alcohol hand sanitiser (61% alcohol and emollients), Outcome 1: Changes in the numbers of colony‐forming units (CFUs) on nurses’ hands
1.3. Analysis.

Comparison 1: 2% chlorhexidine gluconate (CHG) versus alcohol hand sanitiser (61% alcohol and emollients), Outcome 3: Incidence rate of infection
Comparison 2. 2% chlorhexidine gluconate (CHG) versus plain liquid soap.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Adverse outcome (higher score is better) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1.1 Mean visual scoring of skin (mean score) | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | ‐1.75 [‐3.31, ‐0.19] |
| 2.1.2 Mean hand self‐assessment (mean score) | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | ‐9.25 [‐12.29, ‐6.21] |
Comparison 3. Chlorhexidine gluconate 4% versus triclosan 1%.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 incidence of new infection | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1.1 Nosocomial septicaemia | 1 | 1916 | Risk Ratio (IV, Fixed, 95% CI) | 10.97 [5.35, 22.51] |
| 3.1.2 Nosocomial meningitis | 1 | 1916 | Risk Ratio (IV, Fixed, 95% CI) | 3.14 [0.20, 50.27] |
| 3.1.3 Nosocomial viral infection | 1 | 1916 | Risk Ratio (IV, Fixed, 95% CI) | 3.14 [0.63, 15.58] |
| 3.1.4 Necrotising enterocolitis | 1 | 1916 | Risk Ratio (IV, Fixed, 95% CI) | 6.61 [2.55, 17.12] |
| 3.1.5 Total infection | 1 | 1916 | Risk Ratio (IV, Fixed, 95% CI) | 6.01 [3.56, 10.14] |
| 3.1.6 Incidence of suspected new infection | 1 | 1916 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [0.19, 5.60] |
| 3.2 Adverse events (mean hand damage score) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.2.1 Mean hand damage score | 1 | 1916 | Mean Difference (IV, Fixed, 95% CI) | 1.04 [0.50, 1.58] |
3.2. Analysis.

Comparison 3: Chlorhexidine gluconate 4% versus triclosan 1%, Outcome 2: Adverse events (mean hand damage score)
Comparison 4. Iodophor products (betadine vs Prepodyne).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Personnel hand colonisation | 1 | Risk Ratio (IV, Fixed, 95% CI) | 2.76 [2.35, 3.24] | |
| 4.1.1 Right hand | 1 | Risk Ratio (IV, Fixed, 95% CI) | 2.92 [2.43, 3.51] | |
| 4.1.2 Left hand | 1 | Risk Ratio (IV, Fixed, 95% CI) | 2.32 [1.68, 3.21] | |
| 4.2 Infant umbilical positivity | 1 | Risk Ratio (IV, Fixed, 95% CI) | 2.97 [2.49, 3.53] |
4.1. Analysis.

Comparison 4: Iodophor products (betadine vs Prepodyne), Outcome 1: Personnel hand colonisation
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Amortegui 1978.
| Study characteristics | ||
| Methods | Cross‐over clinical trial | |
| Participants | Numbers of nurses and neonates were unclear ( "A total of 1,806 cultures were evaluated. The study was single‐blind to nurses. Nurses involved fluctuated between four and six in
each nursery, according to the baby census" Inclusion criteria
Exclusion criteria Not reported |
|
| Interventions |
Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes | A total of 1806 cultures were evaluated. The study was single‐blind to the nurses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No randomisation is applied Quote: "both products were used alternatively for hand wash in each of the two study nurseries in an effort to minimise nursery variation" |
| Allocation concealment (selection bias) | High risk | Not reported, probably not done |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | It is unclear what study authors meant by (quote) "The study was single blinded to the nurses" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "the cultures were interpreted by one of the technologists in the microbiology laboratory. This person was also involved in culture collection" It was not stated whether this person was blinded to the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no report of attrition |
| Selective reporting (reporting bias) | Unclear risk | We did not have access to the study protocol; it is unclear |
| Other bias | High risk | The numbers of nurses and neonates involved in the study were not clearly stated. Also the study did not report if there was a washout period before participants crossed to a new intervention group |
Larson 2000.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | 16 full‐time neonatal intensive care unit (NICU) nurses Inclusion criteria: nurses were selected for inclusion in the study because they represent a stable and consistent staff and because approximately 70% of direct patient contacts on that unit were provided by nurses
Exclusion criteria "Nurses were eligible to participate if they worked full time on day or night shift in the NICU, had no dermatologic conditions such as psoriasis or latex hypersensitivity were not receiving topical or systemic steroids or antibiotics, were willing to be randomly assigned to one of 2 treatment groups and follow all study regimens, and had no vacation scheduled during the 4‐week study period" |
|
| Interventions |
Treatment group
Control group
|
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 16 nurses (8 per group) were randomly assigned by coin toss to 1 of 2 hand care regimens |
| Allocation concealment (selection bias) | High risk | it was not reported if allocation was concealed, probably not done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding, and 1 of the outcomes (self‐rating hand skin assessment) is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated whether outcome assessors were blinded to the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for |
| Selective reporting (reporting bias) | Low risk | All important outcomes were reported |
| Other bias | Low risk | None is suspected |
Larson 2005.
| Study characteristics | ||
| Methods | Controlled cross‐over trial | |
| Participants | 119 nurses plus all neonates (2932) hospitalised longer than 24 hours on the study units were eligible for inclusion in the study Inclusion criteria
Exclusion criteria "Part‐time and agency nurses and nurses from other units who occasionally worked in the NICU were not eligible" |
|
| Interventions | [Antiseptic detergent hand wash (2% chlorhexidine gluconate) vs alcohol hand sanitiser (61% alcohol and emollients) (3M Avagard D Instant Antiseptic Hand Sanitizer with Moisturizers; 3M HealthCare, St Paul, MN, USA)] "During the alcohol phase, a non‐antimicrobial liquid soap (Kindest Kare Body Wash and Shampoo; Steris Corporation) was also provided for use when hands were physically soiled. Hand lotion (Soft Skin Conditioner; Steris Corporation) was provided throughout the study in both NICUs. Other hand hygiene policies and products were standardized across both study units" |
|
| Outcomes |
|
|
| Notes | Data collection periods were 1 March 2001 to 31 January 2002 (year 1) and 1 March 2002 to 31 January 2003 (year 2) with a month hiatus (February 2002), during which the product
cross‐over occurred and the staff became accustomed to the change. During year 1, NICU 1 used CHG and NICU 2 used ALC, and products were reversed in year 2. All staff and visitors
to each NICU used the designated product. "Prior to the study, a CHG product was used in both study units for traditional hand hygiene, and alcohol hand products were not in use"
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "the clinical trial used a sequential crossover design in which each hand hygiene product was used by each study NICU in random order for 11 consecutive months" |
| Allocation concealment (selection bias) | High risk | Allocation to intervention arms was not concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding, and 1 of the outcomes (self‐rating hand skin assessment) is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated whether outcome assessors were blinded to the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for |
| Selective reporting (reporting bias) | Unclear risk | It is unclear, as we did not have access to the study protocol |
| Other bias | High risk | Rates of gloving used and rates of patient contact differ significantly in the 2 groups; this is likely to affect outcomes |
Sharma 2013.
| Study characteristics | ||
| Methods | Randomised cross‐over study | |
| Participants | 35 nursing staff and all babies in NICU Inclusion criteria
Exclusion criteria: nurses with a history of iodine sensitivity were excluded |
|
| Interventions | Alcohol hand rub (45% 2‐propanol, 30% 1‐propanol, and 0.2% ethyl‐hexadecyl‐dimethyl‐ammonium‐ethylsulphate) vs povidone‐iodine hand scrub with 0.5% w/v available iodine vs plain (non‐antimicrobial) soap (head‐to‐head comparison) Treatment group
Control group
2‐propanol, 30% 1‐propanol, and 0.2% ethyl‐hexadecyl‐dimethyl‐ammonium‐ethylsulphate (Sterilium, Raman and Weil Pvt Ltd., Mumbai, India). 2 mL of solution was dispensed, smeared on the hands, and allowed to dry
|
|
| Outcomes |
|
|
| Notes |
"The scores range from 6 (normal, no observable scale or irritation) to 1 (extensive cracking of skin surface, widespread reddening or occasional bleeding)" "In previous studies, including validation with dermatologist ratings, an interrater agreement of > 95% within a score ± 1 was consistently obtained over a large spectrum of damaged and undamaged hands of various skin types"
"Subjects gave themselves a score from 1 to 7 in 4 dimensions: appearance, intactness, moisture content, and sensation. The possible range of scores is 4 to 28, with 28 indicating totally healthy skin. In previous studies, scores correlated significantly with other physiologic measures of skin damage"
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The random sequences were generated online" Randomisation was done at the end of the first neutral period |
| Allocation concealment (selection bias) | Low risk | Serially numbered opaque and sealed envelopes were opened as nurses were enrolled |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were not blinded but outcomes are likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "the microbiologist was blinded to the hand hygiene method used and the identity of the subjects" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no attrition |
| Selective reporting (reporting bias) | High risk | Neonatal infection at baseline was reported; however, the result post intervention was not available for this important outcome |
| Other bias | High risk | No usable data were provided post intervention compared to pre‐intervention |
Webster 1991.
| Study characteristics | ||
| Methods | Controlled before and after trial | |
| Participants | 109 nursing staff and all 1916 neonates in intensive care and special care nurseries Inclusion criteria
Exclusion criteria: not reported |
|
| Interventions |
Treatment group: 4% w/v chlorhexidine gluconate (Hibiciens) Control group: 1% w/v triclosan (Novaderm) (head‐to‐head comparison) |
|
| Outcomes |
|
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This is a controlled before and after clinical trial (Quote: ‘Hibiclens’ was replaced by ‘Novaderm’ at each liquid soap dispenser in ICN whilst the use of ‘Hibiclens’ continued in SCN" |
| Allocation concealment (selection bias) | High risk | Not described. Probably not done "Hand‐washing with ‘Novaderm’ was the only change to routine practice" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not described. Probably not done |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not described. Probably not done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | High risk | We suspect for publication bias. The study author published data from the study in 3 publications |
ALC: alcohol.
CFU: colony‐forming unit.
CFU‐C: colony‐forming unit count.
CHG: chlorhexidine gluconate.
MRSA: methicillin‐resistant Staphylococcus aureus.
NICU: neonatal intensive care unit.
RCT: randomised controlled trial.
SCBU: special baby care unit.
SD: standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Asare 2009 | Not a randomised controlled trial (observational study) |
| Azor‐Martinez 2018 | Age of participants included in the study was outside the range for the newborn. Average age of participants was about 20 months |
| Ditai 2019 | This study was a pilot and feasibility study |
| Janota 2014 | Not an RCT (was a prospective observational study) |
| Kaufman 2014 | Not the intervention of interest; study authors assessed hand hygiene and non‐sterile hand gloves vs hand hygiene alone |
| Ng 2004 | Not an RCT |
| Webster 1989 | Wrong study design |
RCT: randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
NCT03755635.
| Study name | Neonatal Sepsis at Neonatal Intensive Care Units in Ghana |
| Methods | Non‐randomised intervention model: parallel assignment, open‐label |
| Participants | |
| Interventions | WHO multimodal hand hygiene strategy Age: up to 48 hours (child) |
| Outcomes | Prevention |
| Starting date | 1 October 2018 |
| Contact information | Korle Bu Teaching Hospital, Accra, Ghana |
| Notes | Completed 1 May 2020 |
WHO: World Health Organization.
Differences between protocol and review
We presented a narrative synthesis of neonatal skin colonisation, which was not pre‐specified in the published protocol (Kuti 2019). We presented the outcome under 'other outcomes not pre‐specified'.
Searching
As of July 2019, Cochrane Neonatal no longer searches Embase for its reviews. RCTs and controlled clinical trials (CCTs) from Embase are added to the Cochrane Central Register of Controlled Trials (CENTRAL) via a robust process (see How CENTRAL is created). Cochrane Neonatal has validated its searches to ensure that relevant Embase records are found while searching CENTRAL.
Also starting in July 2019, Cochrane Neonatal no longer searches for RCTs and CCTs on the following platforms: ClinicalTrials.gov or the World Health Organization’s International Clinical Trials Registry Platform (ICTRP), as records from both platforms are added to CENTRAL on a monthly basis (see How CENTRAL is created). Comprehensive search strategies are executed in CENTRAL to retrieve relevant records. The ISRCTN Registry (at www.isrctn.com/, formerly Controlled‐trials.com) is searched separately.
For the 2020 updated search, we ran searches in the following databases: CENTRAL via CRS Web, MEDLINE via Ovid, and CINAHL via EBSCOhost.
Contributions of authors
All review authors contributed to the concept and the design of the review protocol (Kuti 2019). We prepared and developed this protocol under the guidance of Martin Meremikwu (MM). All review authors critically appraised and approved the final review draft.
Sources of support
Internal sources
None, Other
External sources
-
Vermont Oxford Network, USA
Cochrane Neonatal Reviews are produced with support from Vermont Oxford Network, a worldwide collaboration of health professionals dedicated to providing evidence‐based care of the highest quality for newborn infants and their families.
Declarations of interest
BPK has no conflicts to declare. TAO has no conflicts to declare. OO has no conflicts to declare. CO has no conflicts to declare. EU has no conflicts to declare. MM has no conflicts to declare.
Edited (no change to conclusions)
References
References to studies included in this review
Amortegui 1978 {published data only}
- Amortegui AJ, Buffenmeyer C. Comparison of the antiseptic effect of two Iodophor preparations on hand washing in a well-baby nursery. Journal of Obstetric, Gynecologic, and Neonatal Nursing 1978;7(6):35-8. [PMID: 252552 ] [DOI] [PubMed] [Google Scholar]
Larson 2000 {published data only}
- Larson E, Silberger M, Jakob K, Whittier S, Lai L, Latta PD, et al. Assessment of alternative hand hygiene regimens to improve skin health among neonatal intensive care unit nurses. Heart and Lung: Journal of Critical Care 2000;29(2):136-42. [PMID: ] [PubMed] [Google Scholar]
Larson 2005 {published data only}
- Larson EL, Cimiotti J, Haas J, Parides M, Nesin M, Della-Latta P, et al. Effect of antiseptic handwashing vs alcohol sanitizer on health care-associated Infections in neonatal intensive care units. Archives of Pediatrics and Adolescent Medicine 2005;159(4):377-83. [PMID: 15809394 ] [DOI] [PubMed] [Google Scholar]
Sharma 2013 {published data only}
- Sharma VS, Dutta S, Taneja N, Narang A. Comparing hand hygiene measures in a neonatal ICU: a randomized crossover trial. Indian Pediatrics 2013;50(10):917-21. [PMID: 23585422 ] [DOI] [PubMed] [Google Scholar]
Webster 1991 {published data only}
- Webster J, Faoagali JL, Cartwright D. Elimination of methicillin-resistant Siaphylococcus aureus from a neonatal intensive care unit after hand washing with triclosan. Journal of Paediatric Child Health 1994;30:59-64. [DOI] [PubMed] [Google Scholar]
- Webster J. Handwashing in a neonatal intensive care nursery: product acceptability and effectiveness of chlorhexidine gluconate 4% and triclosan 1%. Journal of Hospital Infection 1992;21:137-41. [DOI] [PubMed] [Google Scholar]
- Webster J. Hand-washing in a neonatal Intensive care unit: comparative effectiveness of chlorhexidine gluconate 4% w/v and triclosan 1% w/v. Australian College of Midwives Incorporated Journal 1991;4(2):25-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Asare 2009 {published data only}
- Asare A, Enweronu-Laryea CC, Newman MJ. Hand hygiene practices in a neonatal intensive care unit in Ghana. Journal of Infection in Developing Countries 2009;3(5):352-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Azor‐Martinez 2018 {published data only}
- Azor-Martinez E, Yui-Hifume R, Muñoz-Vico FJ, Jimenez-Noguera E, Strizzi JM, Martinez-Martinez I, et al. Effectiveness of a hand hygiene program at child care centers: a cluster randomized trial. Pediatrics 2018;142(5):e20181245. [PMID: 30297500 ] [DOI] [PubMed] [Google Scholar]
Ditai 2019 {published data only}
- Ditai J, Abeso J, Odeke NM, Mobbs N, Dusabe-Richards J, Mudoola M, et al. BabyGel pilot: a pilot cluster randomised trial of the provision of alcohol handgel to postpartum mothers to prevent neonatal and young infant infection-related morbidity in the community. Pilot and Feasibility Studies 2019;5(49):eCollection 2019. [DOI: 10.1186/s40814-019-0432-7] [PMID: 30962946 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Janota 2014 {published data only}
- Janota J, Šebková S, Višňovská M, Kudláčková J, Hamplová D, Zach J. Hand hygiene with alcohol hand rub and gloves reduces the incidence of late onset sepsis in preterm neonates. Acta Paediatrica 2014;103(10):1053-6. [DOI: 10.1111/apa.12731] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kaufman 2014 {published data only}
- Kaufman DA, Blackman A, Conaway MR, Sinkin RA. Nonsterile glove use in addition to hand hygiene to prevent late-onset infection in preterm infants: randomized clinical trial. JAMA Pediatrics 2014;168(10):909-16. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ng 2004 {published data only}
- Ng PC, Wong HL, Lyon DJ, So KW, Liu F, Lam RK, et al. Combined use of alcohol hand rub and gloves reduces the incidence of late onset infection in very low birthweight infants. Archives of Disease in Childhood. Fetal and Neonatal Edition 2004;89:F336-40. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Webster 1989 {published data only}
- Webster J, Faoagali JL. An in-use comparison of chlorhexidine gluconate 4% w/v, glycol-poly-siloxane plus methylcellulose and a liquid soap in a special care baby unit. Journal of Hospital Infection 1989;14:141-51. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT03755635 {published data only}
- NCT03755635. Neonatal sepsis at neonatal intensive care units in Ghana. https://clinicalTrials.gov/show/NCT03755635. [DOI: ]
Additional references
Adams‐Chapman 2006
- Adams-Chapman I, Stoll BJ. Neonatal infection and long-term neurodevelopmental outcome in the preterm infant. Current Opinion in Infectious Diseases 2006;19(3):290-7. [DOI: 10.1097/01.qco.0000224825.57976.87] [PMID: ] [DOI] [PubMed] [Google Scholar]
Afonso 2017
- Afonso ED, Blot S. Effect of gestational age on the epidemiology of late-onset sepsis in neonatal intensive care units - a review. Expert Review of Anti-infective Therapy 2017;15(10):917-24. [DOI: 10.1080/14787210.2017.1379394] [PMID: ] [DOI] [PubMed] [Google Scholar]
Aiello 2003
- Aiello AE, Cimiotti J, Della-Latta P, Larson EL. A comparison of the bacteria found on the hands of ‘homemakers' and neonatal intensive care unit nurses. Journal of Hospital Infection 2003;54(4):310-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ali 2001
- Ali Y, Dolan MJ, Fendler EJ, Larson EL. Alcohols. In: Block SS, editors(s). Disinfection, Sterilization, and Preservation. 5th edition. Philadelphia (PA): Lippincott Williams & Wilkins, 2001:229-54. [Google Scholar]
Bello 2020
- Bello S, Bamgboye EA, Ajayi DT, Ossai EN, Aniwada EC, Salawu MM, et al. Handwash versus hand-rub practices for preventing nosocomial infection in hospital intensive care units: a systematic review and meta-analysis. Canadian Journal of Infection Control 2020;35(2):82-90. [Google Scholar]
Bigliardi 2017
- Bigliardi PL, Alsagoff SA, El-Kafrawi HY, Pyon JK, Wa CT, Villa MA. Povidone iodine in wound healing: a review of current concepts and practices. International Journal of Surgery 2017;1(44):260-8. [DOI] [PubMed] [Google Scholar]
CADTH 2014
- Canadian Agency for Drugs and Technologies in Health. Alcohol with chlorhexidine hand sanitizers: clinical effectiveness and guidelines. https://cadth.ca/alcohol-chlorhexidine-hand-sanitizers-clinical-effectiveness-and-guidelines (accessed 19 March 2019).
Chan 2013
- Chan GJ, Lee AC, Baqui AH, Tan J, Black RE. Risk of early-onset neonatal infection with maternal infection or colonization: a global systematic review and meta-analysis. PLoS Medicine 2013;10(8):e1001502. [DOI: 10.1371/journal.pmed.1001502] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chu 2014
- Chu SM, Hsu JF, Lee CW, Lien R, Huang HR, Chiang MC, et al. Neurological complications after neonatal bacteremia: the clinical characteristics, risk factors, and outcomes. PLOS One 2014;9(11):e105294. [DOI: 10.1371/journal.pone.0105294] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cortese 2016
- Cortese F, Scicchitano P, Gesualdo M, Filaninno A, De Giorgi E, Schettini F, et al. Early and late infections in newborns: where do we stand? A review. Pediatrics and Neonatology 2016;57(4):265-73. [DOI: 10.1016/j.pedneo.2015.09.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG, on behalf of the Cochrane Statistical Methods Group, editor(s). Analysing data and undertaking meta-analysis. In: Higgins JPT, Green S editor(s), editors(s). Cochrane Handbook for Systematic Reviews of Interventions, Chapter 9. Version 5.1.0 edition. Available from cochrane-handbook.org: Cochrane, 2011, updated March 2011. [Google Scholar]
Effa 2017
- Effa E, Durao S, Kredo T, Mbuagbaw L, Meremikwu M, Ongolo-Zogo P, et al. Process and lessons learned during priority setting in three countries in Africa. In: Abstracts of the Global Evidence Summit. Vol. 9 Suppl 1. Cape Town, South Africa: Cochrane Database of Systematic Reviews, 2017:107. [DOI: ]
Gebremedhin 2016
- Gebremedhin D, Berhe H, Gebrekirstos K. Risk factors for neonatal sepsis in public hospitals of Mekelle City, North Ethiopia, 2015: unmatched case control study. PLOS One 2016;11(5):e0154798. [DOI: 10.1371/journal.pone.0154798] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldstein 2005
- Goldstein B, Giroir B, Randolph A, International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatric Critical Care Medicine 2005;6(1):2-8. [DOI: 10.1097/01.PCC.0000149131.72248.E6] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gottardi 2001
- Gottardi W. Iodine and iodine compounds. In: Block SS, editors(s). Disinfection, sterilization, and preservation. 5th edition. Vol. 4. Gainesville, FL: Lippincott Williams & Wilkins, 2001:159-83. [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version accessed 2 April 2018. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available at gradepro.org.
Greenland 2013
- Greenland K, Iradati E, Ati A, Maskoen YY, Aunger R. The context and practice of handwashing among new mothers in Serang, Indonesia: a formative research study. BMC Public Health 2013;13:830. [DOI: 10.1186/1471-2458-13-830] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Haque 2007
- Haque KN. Defining common infections in children and neonates. Journal of Hospital Infection 2007;65(Suppl 2):110-4. [DOI: 10.1016/S0195-6701(07)60026-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
Herruzo‐Cabrera 2001
- Herruzo-Cabrera R, Garcia-Caballero J, Martin-Moreno J, Graciani-Perez-Regadera MA, Perez-Rodriguez J. Clinical assay of N-duopropenide alcohol solution on hand application in newborn and pediatric intensive care units: control of an outbreak of multiresistant Klebsiella pneumoniae in a newborn intensive care unit with this measure. American Journal of Infection Control 2001;29(3):162-7. [DOI: 10.1067/mic.2001.115582] [PMID: ] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Larson 1998
- Larson EL, Hughes CA, Pyrek JD, Sparks SM, Cagatay EU, Bartkus JM. Changes in bacterial flora associated with skin damage on hands of health care personnel. American Journal of Infection Control 1998;26(5):513-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Liu 2015
- Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 2015;385(9966):430-40; Erratum in: Lancet; 2015; 31;385(9966):420. [DOI: 10.1016/S0140-6736(14)61698-6] [PMID: ] [DOI] [PubMed] [Google Scholar]
Loveday 2014
- Loveday HP, Wilson JA, Pratt RJ, Golsorki M, Tingle A, Bak A, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. Journal of Hospital Infection 2014;86 Suppl(1):S1-70. [DOI: 10.1016/S0195-6701(13)60012-2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Journal of Clinical Epidemiology 2009;62(10):1006-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mortimer 1962
- Mortimer EA Jr, Lipsitz PJ, Wolinsky E, Gonzaga AJ, Rammelkamp CH Jr. Transmission of staphylococci between newborns. Importance of the hands to personnel. American Journal of Diseases of Children (1960) 1962;104:289-95. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pessoa‐Silva 2004
- Pessoa-Silva CL, Dharan S, Hugonnet S, Touveneau S, Posfay-Barbe K, Pfister R, et al. Dynamics of bacterial hand contamination during routine neonatal care. Infection Control and Hospital Epidemiology 2004;25(3):192-7. [10.1086/502376] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ram 2017
- Ram PK, Nasreen S, Kamm K, Allen J, Kumar S, Rahman MA, et al. Impact of an intensive perinatal handwashing promotion intervention on maternal handwashing behavior in the neonatal period: findings from a randomized controlled trial in rural Bangladesh. BioMed Research International 2017;2017:6081470. [DOI: 10.1155/2017/6081470] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ranjeva 2018
- Ranjeva SL, Warf BC, Schiff SJ. Economic burden of neonatal sepsis in sub-Saharan Africa. BMJ Global Health 2018;3(1):e000347. [DOI: 10.1136/bmjgh-2017-000347] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rhee 2008
- Rhee V, Mullany LC, Khatry SK, Katz J, LeClerq SC, Darmstadt GL, et al. Maternal and birth attendant hand washing and neonatal mortality in southern Nepal. Archives of Pediatrics & Adolescent Medicine 2008;162(7):603-8. [DOI: 10.1001/archpedi.162.7.603] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rotter 1999
- Rotter M. Hand washing and hand disinfection. In: Mayhall CG, editors(s). Hospital Epidemiology and Infection Control. 2nd edition. Philadelphia (PA): Lippincott Williams & Wilkins, 1999:1339-55. [Google Scholar]
Schuchat 2000
- Schuchat A, Zywicki SS, Dinsmoor MJ, Mercer B, Romaguera J, O'Sullivan MJ, et al. Risk factors and opportunities for prevention of early-onset neonatal sepsis: a multicenter case-control study. Pediatrics 2000;105(1 Pt 1):21-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for Grading the Quality of Evidence and the Strength of Recommendations Using the GRADE Approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
Tanner 2016
- Tanner J, Dumville JC, Norman G, Fortnam M. Surgical hand antisepsis to reduce surgical site infection. Cochrane Database of Systematic Reviews 2016, Issue 1. Art. No: CD004288. [DOI: 10.1002/14651858.CD004288.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
UN 2017
- United Nations Economic and Social Council. Progress towards the sustainable development goals: report of the Secretary-General. 2017. https://unstats.un.org/sdgs/files/report/2017/secretary-general-sdg-report-2017--EN.pdf (accessed 28 June 2018).
Webster 1994
- Webster J, Faoagali JL, Cartwright D. Elimination of methicillin-resistant Staphylococcus aureus from a neonatal intensive care unit after hand washing with triclosan. Journal of Paediatrics and Child Health 1994;30(1):59-64. [PMID: ] [DOI] [PubMed] [Google Scholar]
WHO 2009
- World Health Organization. WHO guidelines on hand hygiene in health care: a summary. http://apps.who.int/iris/bitstream/10665/70126/1/WHO_IER_PSP_2009.07_eng.pdf (accessed 2 April 2018).
Won 2004
- Won SP, Chou HC, Hsieh WS, Chen CY, Huang SM, Tsou KI, et al. Handwashing program for the prevention of nosocomial infections in a neonatal intensive care unit. Infection Control and Hospital Epidemiology 2004;25(9):742-6. [DOI: 10.1086/502470] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wynn 2010
- Wynn JL, Levy O. Role of innate host defences in susceptibility to early-onset neonatal sepsis. Clinics in Perinatology 2010;37(2):307-37. [DOI: 10.1016/j.clp.2010.04.001] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zafar 1995
- Zafar AB, Butler RC, Reese DJ, Gaydos LA, Mennonna PA. Use of 0.3% triclosan (Bacti–Stat) to eradicate an outbreak of methicillin-resistant Staphylococcus aureus in a neonatal nursery. American Journal of Infection Control 1995;23(3):200-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Kuti 2019
- Kuti BP, Ogunlesi TA, Oduwole O, Oringanje C, Udoh EE, Meremikwu MM. Hand hygiene for the prevention of infections in neonates. Cochrane Database of Systematic Reviews 2019, Issue 5. Art. No: CD013326. [DOI: 10.1002/14651858.CD013326] [DOI] [Google Scholar]


