CLINICAL HISTORY AND IMAGING STUDIES
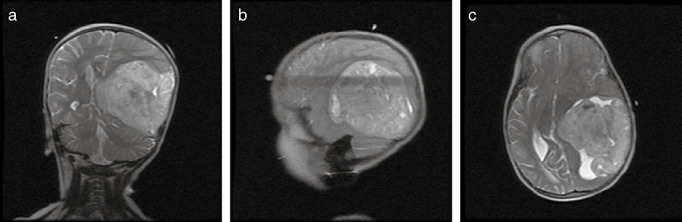
A 3‐year‐old girl with a history of mild motor delay, presented with a change in mental status, gait difficulty, nausea and vomiting. The patient was in her usual state of health until 9 months prior to presentation, when she was found to have abnormal adduction of the left eye. Over the next several months, she developed gait difficulties and behavioral changes. On the day of admission, she developed confusion, severe gait difficulties, nausea and vomiting. On physical examination, she had right homonymous hemianopsia, right hemiparesis, and increased deep tendon reflexes of her right Achilles tendon. She subsequently became unresponsive. She was intubated and given mannitol and steroids. An external ventricular drain was placed. Neuroimaging showed a minimally heterogeneous enhancing tumor measuring 8 × 8 × 9 cm involving the left parietal region and, partly filling the left lateral ventricle, with accompanying hydrocephalus, midline shift and uncal herniation (Figures 1a, 1b, 1c). Gross total resection of the tumor was confirmed by post‐operative imaging. Staging evaluation revealed no metastasis. The patient was discharged one week later.
Figure 1.
NEUROPATHOLOGIC FINDINGS
Grossly, tumor submitted for neuropathological evaluation consisted of multiple pieces of soft, tan and red tissue altogether measuring 2 × 2 × 2 cm in aggregate.
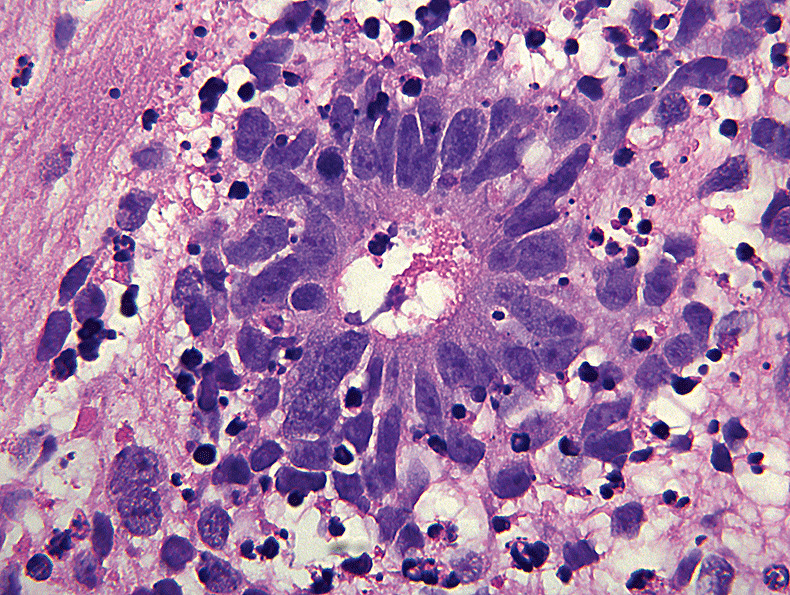
Microscopically (4, 5, 6, 7, 8), the tumor was comprised of clusters and cords of small to medium sized hyperchromatic cells with round to oval nuclei and indistinct cell borders set in a neuropil‐like matrix (figure 2). Rosettes with well‐formed central lumina, some with central granular material were seen (Figure 3). Densely cellular regions with extensive apoptosis were also present. MIB‐1 proliferation index was high, focally approaching 70%. The neuropil‐like areas were labeled with synaptophysin antibodies (figure 3). True rosettes were highlighted by vimentin immunostaining (figure 4), but were negative for GFAP and neurofilament protein immunostains.
Figure 4.
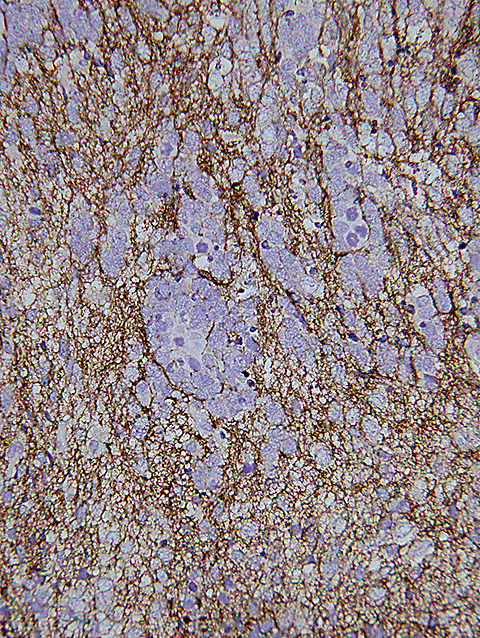
Figure 5.
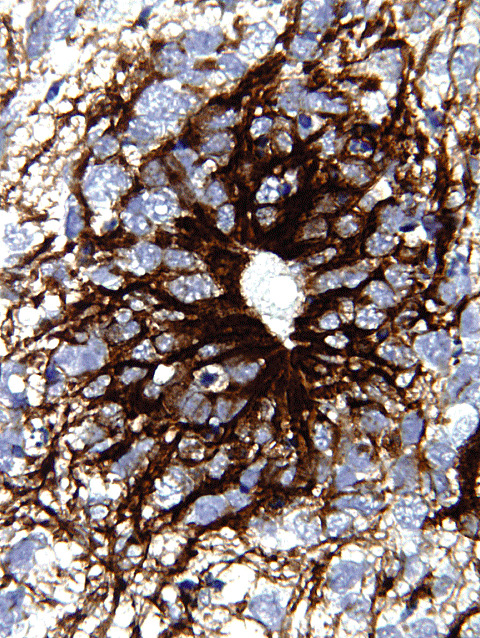
Figure 2.
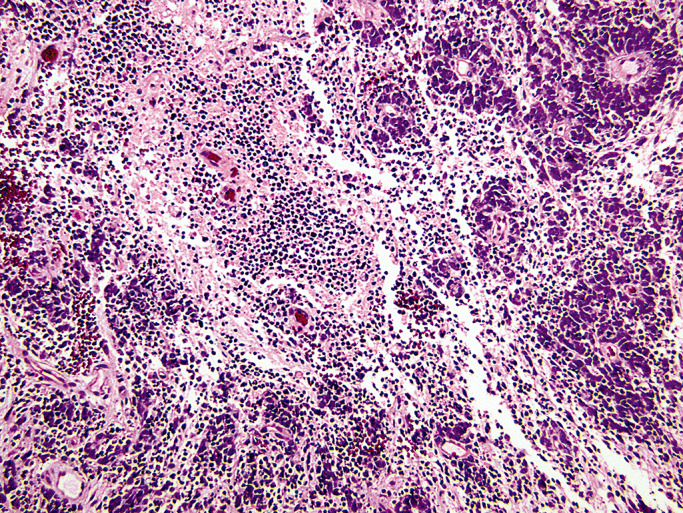
Figure 3.
DIAGNOSIS
Embryonal tumor with abundant neuropil and true rosettes (ETANTR).
DISCUSSION
The embryonal tumor with abundant neuropil and true rosettes (ETANTR), first described by Eberhart et al in 2000, combines features of both cerebral neuroblastoma and ependymoblastoma (1). A Pubmed literature search revealed a total of 35 cases; occurring in both infants and young children with a mean age of 26 months 2, 3. A more detailed discussion of this case along with additional references can be found at http://path.upmc.edu/divisions/neuropath/bpath/cases/case210.html.
In contrast to meduloblastoma, ETANTR predominantly occurs in females, with a female : male ratio of 2:1. It preferentially affects the supratentorial region, most commonly occurring in the frontal and parietal lobes, in isolation or with extension into the thalamus. Patients usually present with nausea, vomiting, visual and movement disturbance. The prognosis is extremely poor with the majority of children dying 1 to 30 months after presentation.
Histologically the lesion is unique in its biphasic composition of hypercellular regions alternating with paucicellular fibrillar neuropil with lumen containing rosettes. These rosettes characteristically contain small circular or slit‐like lumens, some filled with granular debris. The neuropil exhibits synaptophysin positivity. Unlike rosettes encountered in ependymal tumors, the rosettes in ETANTR do not react with antibodies to GFAP, although small foci of GFAP positive glial cells may be encountered elsewhere within the tumor. A single case of ETANTR with prominent neurocytic differentiation has been reported (4). The main histologic differential diagnosis includes medulloepithelioma, ependymoblastoma, neuroblastoma, and atypical teratoid/rhabdoid tumor (AT/RT).
Medulloepithelioma is an embryonal tumor composed of tall pseudostratified primitive epithelium arranged in glands, tubules, or canals with long surfaces resembling embryonic neural tube. This epithelium is delineated by well‐defined, periodic acid‐Schiff‐positive basement membrane material on its outer surface. Its inner or luminal surfaces, demonstrate ill‐defined amorphous pseudomembranes. Mitotic figures are often identified adjacent to the lumen. In contrast to ETANTR, medulloepitheliomas do not contain neuropil rich areas. The long surfaces and PAS+ outer basement membranes characteristic of medulloepithelioma are absent in ETANTR. Ependymoblastomas also lack paucicellular neuropil, so characteristic of ETANTR. Ependymoblastic rosettes tend to be elongated structures, while ETANTR rosettes tend to be round (resembling Flexner‐Wintersteiner rosettes). Neuroblastoma does not contain true rosettes, but instead may show Homer Wright rosettes. Occasionally, ETANTR may manifest mesenchymal differentiation and/or large pleomorphic cells, bringing AT/RT into the differential diagnosis. However, rhabdoid cells have not been described in ETANTR. Furthermore unlike AT/RT immunostaining for epithelial membrane antigen is negative, and INI‐1 is positive in ETANTR.
ABSTRACT
We report a case of a 3‐year‐old girl with a 9‐month history of focal neurologic finding and signs of increased intracranial pressure. Radiological imaging studies showed a minimally heterogeneous enhancing large tumor involving left parietal region and partly filling the left lateral ventricle. Microscopically, the tumor contained prominent small true rosettes set into areas of fibrillar neuropil‐like matrix. Foci of cellular tumor with extensive apoptosis were present. The neuropil‐like areas and true rosettes were positive for synaptophysin immunostain. The tumor was negative for GFAP and neurofilament protein immunostains. MIB‐1 proliferation index was high focally approaching 80%.
REFERENCES
- 1. Eberhart CG, Brat DJ, Cohen KJ, Burger PC (2000) Pediatric neuroblastic brain tumors containing abundant neuropil and true rosettes. Pediatr Dev Pathol 3(4):346–52. [DOI] [PubMed] [Google Scholar]
- 2. Gessi M, Giangaspero F, Lauriola L, Gardiman M, Scheithauer BW, Halliday W, Hawkins C, Rosenblum MK, Burger PC, Eberhart CG (2009) Embryonal tumors with abundant neuropil and true rosettes: a distinctive CNS primitive neuroectodermal tumor. Am J Surg Pathol 33(2):211–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fuller C, Fouladi M, Gajjar A, Dalton J, Sanford RA, Helton KJ (2006) Chromosome 17 abnormalities in pediatric neuroblastic tumor with abundant neuropil and true rosettes. Am J Clin Patho 126(2):277–83. [DOI] [PubMed] [Google Scholar]
- 4. Dunham C, Sugo E, Tobias V, Wills E, Perry A (2007) Embryonal tumor with abundant neuropil and true rosettes (ETANTR): report of a case with prominent neurocytic differentiation. J Neurooncol. 84(1):91–8. [DOI] [PubMed] [Google Scholar]


