Abstract
We report a term newborn who presented on day 3 of life with unilateral, tender scrotal swelling with skin discolouration, which was subsequently diagnosed as haemophilia A at about 6 months of age. He received intramuscular vitamin K and hepatitis B vaccine at birth uneventfully. The scrotal swelling was treated as an infected hydrocoele, considering the absence of a family history of bleeding disorder and other risks of bleeding tendency, as well as the ultrasonographic features. He also had congenital pneumonia requiring venepuncture, non-invasive oxygen supplementation and intravenous antibiotics, without any complication. The swelling slowly improved over 2 months. He later developed post-trial vaccine injection haematoma at 4 months of age, and multiple non-traumatic bruises when he was 6 months old, leading to the diagnosis. This case demonstrates an uncommon, but a possible, early manifestation of haemophilia A at birth with a unilateral scrotal haematoma.
Keywords: haematology (incl blood transfusion), paediatrics, paediatric surgery
Background
Scrotal swelling is a relatively common occurrence in neonates.1 Although most scrotal swellings are benign and self-limiting in nature, some conditions can lead to a potentially catastrophic outcome, such as testicular neoplasm, testicular torsion and irreducible inguinal hernias.1
The other diagnosis that should be considered in neonates with scrotal swelling is a scrotal haematoma. This condition is usually associated with risk factors like birth trauma, testicular torsion, hypoxia, sepsis and adrenal haemorrhage.2 Idiopathic neonatal scrotal haematoma, although reported, is rare.2 When no apparent risk is present, bleeding disorders such as haemophilia needs to be considered.
Haemophilia is a group of disorder of the blood coagulation pathway. It can be inherited or acquired. They are categorised as mild, moderate or severe, based on the clotting factor activity. The onset of first bleeding is earlier in severe disease, with a mean age of first bleeding reported at 1 month.3 In neonates with severe haemophilia, the common site of first bleeding is the central nervous system, extracranial sites such as cephalohematoma and sites of medical procedures such as bleeding from the circumcision site.4 However, there has been no literature on scrotal haematoma as the presenting feature of haemophilia in neonates.
We report a term neonate with severe haemophilia A who presented with a scrotal haematoma on day 3 of life but not diagnosed until 6 months of age.
Case presentation
A baby boy, born at 37 weeks of gestation via uncomplicated spontaneous vertex delivery, with a birth weight of 2.81 kg and a good Apgar score, was referred to the special care nursery at 12 hours of life for congenital pneumonia. Antenatal and perinatal histories were uneventful. On examination, he had tachypnoea with a respiratory rate of 60 breaths per minute. Subcostal muscle retractions were present. No other abnormalities were noted. Chest X-ray showed ill-defined air space consolidation in the left upper and middle zone, consistent with infective changes. Septic screen (full blood count and C reactive protein) was normal. He was given supplemental oxygen via nasal cannula as well as intravenous penicillin and gentamicin. Supplemental oxygen was weaned off at day 6 of life. There was no excessive bleeding or bruises on the venepuncture sites, heel prick sites or umbilicus.
During routine examination at 45 hours of life, he was noted to have a right scrotal swelling, about the size of a quail’s egg. The swelling was not reducible. It was tender to touch, erythematous, and transillumination test was positive. Urgent ultrasonography did not suggest testicular torsion; however, it showed a right complex scrotal collection measuring 2.0 cm×2.2 cm, with no blood flow seen on Doppler in the collection, likely to be infective (figure 1). The radiologist also suggested a differential diagnosis of a haematoma. His platelet count was 397×109/L. No coagulation profile was performed.
Figure 1.
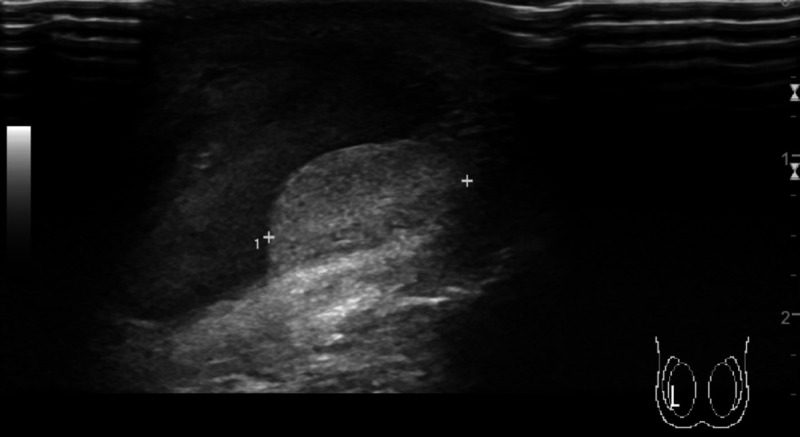
Ultrasound image showing a heterogenous fluid collection surrounding the right testicle.
There was no family history of haemophilia or bleeding disorder. He has an older brother who has been well. His mother was not on any medication. His birth was uneventful, and there was no trauma to the perineal region. Intramuscular vitamin K and hepatitis B vaccine were given at birth without any complication.
We referred him to a paediatric surgeon. The surgeon suggested to manage the scrotal swelling as an infected hydrocoele, and the newborn completed a 1-week course of intravenous cloxacillin. He was discharged home well at day 9 of life. The size of the swelling reduced slowly over 2 months.
The mother, who is a staff nurse in a neonatal intensive care unit (NICU), together with the father, consented for the boy to participate in a vaccine trial at the age of 1½ months. The vaccine trial involved the administration of three doses of an intramuscular trial vaccine in the first year of life. During the screening visit, some residual scrotal swelling was noted clinically and on repeat ultrasound. There was no suspicion of familial coagulopathy due to the absence of family history, and history of uneventful intramuscular injections and venepunctures at birth. He was thus considered eligible and received the first dose of intramuscular trial vaccine. He was observed in the clinic for 30 min after the injection without any adverse reaction.
He was seen in the study visit clinic at the age of 4 months for the second dose of the trial vaccine. During this visit, his mother reported that he was well; with no adverse event occurring at home after the first-dose injection. On physical examination, there were no bruises. The scrotal swelling had resolved completely. The second dose of the trial vaccine was thus administered. After administration of the vaccine, he was observed for 30 min in the clinic, without any adverse reaction. However, his mother noted a huge swelling at the injection site on his right thigh the day after at home. The swelling was firm, measuring 8 inches in the longest diameter with about 1 cm in thickness. The overlying skin was erythematous and was tender to touch. The parents did not seek medical attention. His mother reported that the swelling resolved spontaneously after 5 days.
When the baby returned for the third study visit at the age of 6 months, the study doctor noted multiple spontaneous bruises on his inner forearm and right iliac crest region (figure 2). According to the mother, the bruises developed the day before the third study visit spontaneously. There was no trauma to the affected region. There was no bleeding from other body parts. He was not on any medication. A provisional diagnosis of bleeding disorder was made, and blood investigations performed. The boy did not receive the third study vaccine dose.
Figure 2.

Spontaneous bruises appearing on the right iliac crest at 6 months of age.
Investigations
On admission during the neonatal period, his haemoglobin level was 194 g/L, total white cell count was 27.7×109/L and platelet count was 397×109/L. C reactive protein level was normal at 0.32 mg/dL. There was no repeat full blood count during this admission, as the baby remained clinically pink throughout his stay in the ward.
At 6 months of age, his partial thromboplastin time (PTT) was significantly prolonged at 109 s. There was no other abnormality noted in the full blood count and picture. After discussion with the haematopathologist, coagulation factor VIII and IX level were performed. Mixing test with normal pooled plasma showed correction of PTT at intermediate and 2 hours postincubation. Factor VIII activity was <1%, but he had normal factor IX activity. The finding was consistent with the diagnosis of severe haemophilia A.
The child was referred to the haemophilia clinic for family screening and counselling. Targeted mutation analysis for intron 22 and intron 1 inversions was done for the child. Although these are the common factor VIII variants causing severe haemophilia, neither of them was detected in our case. Linkage analysis for the child showed that the association of the affected allele with extragenic marker variable number of tandem repeat DXS52 (St 14) c, Hind III 469, 248, Intron 13 (CA) b haplotype and Intron 22 (CA) a haplotype. His mother had a normal coagulation profile, and her linkage analysis showed homozygous for all the four linkage markers. Therefore, the carrier status for his mother could not be determined. Whole factor VIII gene sequencing is needed to detect the exact mutation associated with haemophilia A in the child, as well as to confirm the carrier status of his mother; both of which are not available at the time of writing. His father and older brother had normal coagulation profile.
Differential diagnosis
During the neonatal period, the initial provisional diagnosis for the acute unilateral scrotal swelling was testicular torsion, which is a surgical emergency. Thus, we arranged for urgent ultrasonography of the scrotum, which showed a complex collection in the scrotum potentially infective in nature, or a haematoma. Owing to uneventful birth history, and in the absence of a family history of a bleeding disorder, although suggested by the radiologist, the haematoma was deemed as not likely, and the swelling was treated as infected hydrocoele. Indeed, the swelling seemingly resolved with the antibiotics and time. The history of swelling at the injection site which did resolve after the second study vaccine dose did not raise any concern by the mother (who is a trained staff nurse at the NICU) and the study doctor. The bleeding disorder was only suspected when the infant returned at 6 months of age with spontaneous bruises, and the retrospective history of an injection site swelling after second vaccine injection. On hindsight, the infant could have a scrotal haematoma due to haemophilia during the neonatal period. Although difficult to prove now, this was potentially possible given the neonatal history and ultrasound findings.
Treatment
The child was given on-demand factor VIII replacement therapy since he was diagnosed with haemophilia A at 6 months of age. He required factor VIII infusion almost biweekly due to minor trauma or spontaneous soft tissue and mucosal bleeding episode. Hence, he was started on prophylactic therapy with plasma-derived factor VIII at the age of 1 year 3 months. At the time of writing, the frequency of factor VIII infusion has been increased from weekly to twice weekly, with ultimate target of thrice weekly infusion.
Outcome and follow-up
After the diagnosis of haemophilia A, the child was withdrawn from the vaccine trial formally because the intramuscular injection is a contraindication, according to the trial protocol. A protocol deviation was also reported to the independent ethics committee. The Mother and Child Health Clinic, where he received his Malaysian National Immunisation Programme, was informed of the diagnosis. His subsequent vaccinations were given by subcutaneous routes uneventfully.
Both parents were given information about haemophilia, the prognosis and the complications. They were educated on the injury-prevention measures and the recognition of warning signs of significant bleeding.
He had two episodes of fall with trauma to the head after the diagnosis of haemophilia A was made. The first fall happened as he was playing on the floor, where he lost his balance, fell backwards and injured his occiput. The second incident happened when he tripped and fell forward, injuring his forehead. He had bruises at the site of impact in both incidents. For both episodes, medical attention was sought. Besides the haematoma on the site of impact, he did not have any signs and symptoms of increased intracranial pressure to suggest intracranial bleed. In both occasions, after observation, he was discharged and remained well without any investigation or treatment. Subsequently, as he started to ambulate, he required almost biweekly factor VIII infusion due to minor trauma and spontaneous mucosal bleed.
His family had since installed soft padding to the flooring at their house as a preventive measure. At the time of writing, the child was 17 months old with typical developmental milestones. He did have some bruises on his limbs from minor trauma occasionally. Otherwise, there have been no joint swelling or haemarthroses. He is being followed up regularly at the haemophilia clinic.
Discussion
Management of acute scrotal swelling in neonates focused on causes such as neonatal testicular torsion, testicular neoplasms, supernumerary testicles and hydrocoele.1
This newborn presented with unilateral scrotal swelling with discolouration at day 3 of life, but was managed as an infected hydrocoele despite no clinical and laboratory evidence of infection. Although rare in neonates, there were reports of neonates developing infected hydrocoele.5 6 However, none of the reported cases of infected hydrocoele occur within the first week of life. Infected hydrocoele was thought to be related to patent processus vaginalis with bacterial seeding from the peritoneum, or concurrent urinary tract and hydrocoele infection.5 6 In our case, the blood investigations and clinical findings of the newborn did not suggest infection. Thus, alternative diagnoses need to be considered before committing to this diagnosis.
On hindsight, the scrotal swelling could represent a haematoma. Although the ultrasound examination did suggest haematoma as a cause of the scrotal swelling, it was not considered then, because scrotal haematoma was usually associated with testicular torsion,2 adrenal haemorrhage,2 a traumatic birth or breech deliveries,7 all of which were absent in this case. Although there were case reports of a toddler with penoscrotal swelling due to haemophilia,8 and of an adult with undiagnosed haemophilia A who presented with scrotal haematoma,9 there has been no report of similar cases presenting during the neonatal period. Moreover, the absence of a family history of bleeding disorders made the diagnosis seemingly more unlikely. Thus, the differential diagnosis of scrotal haematoma due to haemophilia or bleeding disorders was not considered initially for this infant. This would be the first reported case and youngest presentation of haemophilia with a unilateral scrotal haematoma.
Haemophilia is a group of disorder of the blood coagulation pathway. It can be inherited or acquired. The most common inherited haemophilia is haemophilia A (deficiency of clotting factor VIII) and haemophilia B (deficiency of clotting factor IX). Haemophilia is an X-linked recessive disease, mainly affecting boys, although it can also rarely manifest in girls. Although most cases of haemophilia were diagnosed with a positive family history, it was reported that up to 55% of haemophilia A were sporadic.10
Looking back, when a neonate presents with scrotal swelling with discolouration, scrotal haematoma should be considered as a differential, even in the absence of risk factors and family history of bleeding disorders. A coagulation profile should be included as part of the evaluation. An abnormal coagulation profile would undoubtedly raise the suspicion of inherited bleeding disorders, especially in neonates. If the bleed was significant, a repeat full blood count could potentially demonstrate a drop in the haemoglobin level, hence raising the suspicion of a bleeding disorder; but in our case, a drop in the haemoglobin level might not have happened because the haematoma was not huge to indicate a significant bleed. Early diagnosis of haemophilia enables rapid recognition and administration of appropriate treatment in the event of significant bleed like intracranial haemorrhage, which can improve the outcome.11
Patient’s perspective.
The child’s mother, who is a registered nurse in a neonatal unit, narrated and shared her experience.
My second son was born healthy. The only different thing I noticed about him was the size of his testis. It was bigger, maroon in colour and not normal. The doctors told me that he has an infection, and he would receive antibiotics. My biggest fear then was, will he require surgery? I was relieved when the surgeon told me that he needed no surgery. He seemed to respond to antibiotics. The swelling reduced slowly, but at least it was regressing.
When he was around 1½ months old, I got to know about the vaccine study going on in the hospital from a friend. It was about the pneumococcal vaccine, so I was keen to participate because as a nurse, I know how severe and debilitating pneumococcal diseases are, particularly in young infants. My husband and I attended the first visit. After a thorough explanation on the study procedures, risks and benefits of the study, and the contraindications, we agreed for our son to participate in this trial. At that time, nobody knew that he has haemophilia. Furthermore, neither my husband nor myself have any relatives with such disease. Moreover, I knew he was given intramuscular vitamin K and hepatitis B vaccine at birth with no problems, so I thought there shouldn’t be an issue.
He received his first dose of trial vaccine uneventfully. However, after receiving the second dose 2 months later, there’s a visible swelling over the injection site. It was red. He was also quite irritable for a few days, but he was not feverish. I attributed it to the pain over the injection site, which, for me, is a known complication. I decided to observe it and true enough, the swelling gradually became smaller and disappeared by about 1 week.
I did not give much thought to it. Nevertheless, at 6 months of age, my son seemed to get bruises on his body pretty quickly. Whenever he rested his arms and forearms on the table, bruises appeared. When he laid in the prone position, bruises appeared. It seemed a very trivial touch, but it’s enough to cause a big bruise on him. My mother told me I was like that as a child, so it’s nothing to worry. My main concern at that time was, could this be an unknown side effect of the trial vaccine? Because I have not seen anything like this before. So, I decided to get the trial doctor to have a look. The doctor explained that because the bruising was quite extensive, and in the absence of significant trauma, we needed to do some blood test to look for bleeding disorders.
When they told me that his blood investigation showed that he has severe haemophilia A, I was dumbfounded. As a nurse, I remember seeing this word, I remember reading about it, but it never struck me that I am carrying it, and can pass it to my child. Although I am a nurse, I have never looked after patients with haemophilia, and I have no idea what will happen to them. My husband and I were in denial initially. How could our son get this disease? Nobody in our family has them. Has it got anything to do with the trial vaccine?
The doctor referred us to the haemophilia clinic, which was wonderful. The specialist patiently explained to us about the disease, the genetic component, the prognosis and treatment options. She advised for family screening, including for my older son. Luckily, none of us has haemophilia. As our understanding of the disease increased, we started to accept the diagnosis, but we became anxious. Do we, as a family, have what it takes to care for him? Can he live a normal life? We started to read up on the condition. There are lots of information on the internet. Some of my colleagues, who are doctors, guided me to reliable websites, where parents of kids with haemophilia share their stories and experience. With improved understanding, we are now more confident and prepared to go on this journey with our son.
Looking back, I am grateful that our son participated as a subject in the vaccine trial. If he were not a trial subject, I would not have sought medical advice for the bruising. I would have believed I was the same when I was young. I would have thought it was benign. Who knows what could have happened? He could have bleeding in his brains later, and we still would not know that he has haemophilia!
Was I upset that his scrotal swelling was misdiagnosed in the first place? To be honest, I am more confused than upset. I am sure the paediatric doctors and surgeon did what they thought was best for him. How could I say they were wrong when the scrotal swelling seemed to respond to antibiotics at that time? On the other hand, if a coagulation profile was performed then, the haemophilia might have been picked up even earlier. It is always easier to say what need or doesn’t need to be done on hindsight, so, I guess this is a learning experience for all of us. However, I couldn’t help thinking: if the diagnosis was made earlier, I would not have enrolled him in the vaccine clinical trial, which required an intramuscular injection. I would have saved him of all the pain he had to endure.
The experience wasn’t particularly pleasant, but it’s a good learning experience for us as a family. In particular, I learned that there’s no such thing as a ‘normal bruising’, especially in a young infant. As a nurse taking care of newborn infants, in the future, I would certainly be more aware of the possibility of haemophilia if I see another child who presents similarly.
Learning points.
Haemophilia may present within the first week of life as a unilateral tender scrotal haematoma.
Clinical and radiological features of scrotal haematoma in neonates are relatively non-specific; in the absence of a family history of bleeding disorders and other risk factors, diagnosis of scrotal haematoma is challenging.
Caregivers of infants who received vaccinations should be educated to recognise the complications of the vaccine they receive, such as haematoma, and a plan of action should be provided to them in case of any adverse event.
Acknowledgments
The authors thank the Director-General of Health, Malaysia for his permission to present and publish this case report. The authors also thank Dr Wong See Chiong for providing the ultrasound images, Miss Shelly binti Henry Buyu (study coordinator) and the parents of the patient for their cooperation and contributions to this write-up.
Footnotes
Contributors: JS-YL: conceptualised, designed and drafted the first draft of the manuscript and approved the final manuscript. T-HT and C-HC: conceptualised and designed the manuscript, critically revised the manuscript as submitted and approved the final manuscript. MM: critically revised the manuscript as submitted and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Basta AM, Courtier J, Phelps A, et al. Scrotal swelling in the neonate. Journal of Ultrasound Medicine 2015;34:495–505. 10.7863/ultra.34.3.495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jimoh BM, Chinwe EB, Adebisi AO, et al. Idiopathic scrotal hematoma in neonate: a case report and review of the literature. Case Rep Urol 2014;2014:1–3. 10.1155/2014/212914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kulkarni R, Soucie JM, Lusher J, et al. Sites of initial bleeding episodes, mode of delivery and age of diagnosis in babies with haemophilia diagnosed before the age of 2 years: a report from The Centers for Disease Control and Prevention’s (CDC) Universal Data Collection (UDC) project. Haemophilia 2009;15:1281–90. 10.1111/j.1365-2516.2009.02074.x [DOI] [PubMed] [Google Scholar]
- 4.Kulkarni R, Presley RJ, Lusher JM, et al. Complications of haemophilia in babies (first two years of life): a report from the centers for disease control and prevention universal data collection system. Haemophilia 2017;23:207–14. 10.1111/hae.13081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.JH K, Yim SY, Lee NK, et al. Infected hydrocoele in a neonate. Urologia Internationalis 2000;65:216–7. [DOI] [PubMed] [Google Scholar]
- 6.Jones WG, Deeths HJ. Infected hydrocele in neonate. Urology 1975;5:526–7. 10.1016/0090-4295(75)90082-5 [DOI] [PubMed] [Google Scholar]
- 7.Diamond DA, Borer JG, Peters CA, et al. Neonatal scrotal haematoma: mimicker of neonatal testicular torsion. BJU Int 2003;91:675–7. 10.1046/j.1464-410X.2003.04201.x [DOI] [PubMed] [Google Scholar]
- 8.Siddiqui SA, Tomar V. Spontaneous penoscrotal bleeding in haemophilia a. BMJ Case Rep 2016;2016:bcr2016217596 http://casereports.bmj.com/ 10.1136/bcr-2016-217596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alam SI, Rahman MM, Rayhan F, et al. 52 year Male with Haemophila-A; Presented with scrotal haematoma: Managed in resource constraint settings - A case report. Journal of Shaheed Suhrawardy Medical College 2018;10:118–21. 10.3329/jssmc.v10i2.41173 [DOI] [Google Scholar]
- 10.Kasper CK, Lin JC. Prevalence of sporadic and familial haemophilia. Haemophilia 2007;13:90–2. 10.1111/j.1365-2516.2006.01397.x [DOI] [PubMed] [Google Scholar]
- 11.Ghosh K, Nair AP, Jijina F, et al. Intracranial haemorrhage in severe haemophilia: prevalence and outcome in a developing country. Haemophilia 2005;11:459–62. 10.1111/j.1365-2516.2005.01134.x [DOI] [PubMed] [Google Scholar]


