Abstract
Objectives
This study aimed to better understand reasons why children in South Africa die at home, including caregivers’ care-seeking experiences, decision-making, choice of treatment provider and barriers to accessing care during a child’s final illness.
Design
This qualitative study included semi-structured in-depth interviews and focus group discussions with caregivers of children who died below the age of 5 years. Data were thematically analysed, and key findings compared with the Pathways to Survival Framework—a model frequently used in the study of child mortality. An adapted model was developed.
Setting
Two rural health and demographic surveillance system (HDSS) sites in South Africa—the Agincourt HDSS and the Africa Health Research Institute.
Participants
Thirty-eight caregivers of deceased children (29 participated in in-depth interviews and 9 were participants in two focus group discussions). Caregivers were purposively sampled to ensure maximum variation across place of death, child age at death, household socioeconomic status, maternal migration status and maternal HIV status.
Findings
Although caregivers faced barriers in providing care to children (including insufficient knowledge and poor transport), almost all did seek care from the formal health system. Negative experiences in health facilities did not deter care-seeking, but most respondents still received poor quality care and were not given adequate safety-netting advice. Traditional healers were only consulted as a last resort when other approaches had failed.
Conclusion
Barriers to accessing healthcare disrupt the workings of previously accepted care-seeking models. The adapted model presented in this paper more realistically reflects care-seeking experiences and decision-making during severe childhood illness in rural South Africa and helps explain both the persistence of home deaths despite seeking healthcare, and the impact of a child’s death on care-seeking in future childhood illness. This model can be used as the basis for developing interventions to reduce under-5 mortality.
Keywords: paediatrics, community child health, primary care, public health, qualitative research
Strengths and limitations of this study.
Caregivers’ accounts were used to modify the Pathways to Survival Framework to produce a care-seeking model for fatal childhood illness in rural South Africa.
This study included a diverse sample of caregivers, including fathers and traditional healers whose views are seldom included in studies of child illness and care-seeking.
Interviews and focus group discussions were conducted in participants’ first language (isiZulu or Xitsonga), enabling inclusion of caregivers who did not speak English fluently; however, subtleties of meaning and tone may have been lost in the translation process.
Interviews and focus group discussions took place at least 1 year after the child’s death, which may have resulted in recall bias.
Introduction
Under-5 mortality remains a priority in low-and middle-income countries. Despite advances in the care of mothers, newborns and children in resource-constrained settings, over 5.3 million children died in 2018 before their fifth birthday globally, 54% of those in sub-Saharan Africa (SSA).1 Moreover, in SSA, over 50% of child deaths occur at home despite many children having contact with the formal healthcare system during their final illness.2–5 Understanding the factors that contribute to home deaths is critical to designing interventions to reduce under-5 mortality in SSA, including those which occur beyond the remit of the formal healthcare sector.
A large body of research across SSA has drawn on the Pathways to Survival Framework6 in an attempt to analyse under-5 deaths.2 7–9 This approach has a number of advantages; it demonstrates the fluid interaction between healthcare provided within and beyond the home, recognising too the role of informal healthcare providers, whether alongside or in place of formal providers. The model has been used to highlight the different stages at which children were lost from formal care pathways.2 7–9 In South Africa specifically, research has highlighted that over 80% of the carers of children who died at home had sought formal healthcare during the child’s final illness, of whom about a third sought care more than once.10 11 One modifiable factor may be the low referral rate of children from primary level facilities to higher levels of care.10–13 Use of informal providers including traditional healers may also contribute to home deaths,14 although the limited quantitative data from South Africa do not support this10; and qualitative studies have highlighted that the direction of any association is unclear as informal providers are often used in conjunction with formal healthcare providers, or may be used where formal healthcare providers are difficult to access due to distance, transport or cost and so where other barriers exist that may increase the risk of home deaths, unrelated to the actual use of informal providers.15–18
There have been no previous qualitative studies in South Africa to explore reasons for children dying at home. This paper reports on one such study, using the findings to adapt the Pathways to Survival Framework, which helps to identify key sites for future interventions to tackle the problem of child death at home.
Methods
Study design and setting
We conducted a qualitative study using semi-structured in-depth interviews and focus group discussions (FGDs), from July 2018 to January 2019, with caregivers of children who died under the age of 5 years.
This research was conducted in two largely rural health and demographic surveillance system (HDSS) sites in South Africa (Agincourt in Mpumalanga province and the Africa Health Research Institute (AHRI) in KwaZulu-Natal).19 20 These sites are considered broadly representative of the dynamics found across rural South Africa. Together these sites include over 280 000 people in over 40 500 households, most of which fall into the lowest socioeconomic quintiles nationally. In Agincourt, most residents speak Xitsonga, while in AHRI isiZulu is predominant. Routine household surveys are conducted every 4 months (in AHRI) and annually (in Agincourt) to update household rosters, record births, deaths, pregnancy outcomes, migrations, education level of each household member, household assets, income sources and employment status. There are high levels of temporary labour migration (33%–36%) with household members oscillating between their place of work and rural homes. Most households rely on income from government social grants including the old age pension currently valued at R1860 per month (US$180) and child support grant (R450/per month (US$30)). Public healthcare facilities comprise primary healthcare clinics (open from 07:00 to 16:00 hours Monday to Sunday, staffed by nurses), community health centres (open 24 hours Monday to Sunday, staffed by nurses) and district hospitals (open 24 hours Monday to Sunday, staffed by doctors and nurses). Allopathic medical care is also accessible from private general practitioners in the area. Informal healthcare is provided by traditional and faith healers who operate in each village. Both sites routinely conduct verbal autopsies (VAs) on all deaths to determine probable biological cause of death.19 20
Sampling
All under-5 deaths where a VA was completed in 2017 were eligible for inclusion in this study. Participants were recruited using purposive sampling to seek maximum variation, based on relevant demographic details from the completed VA and household survey. Consideration was given to place of death (at home or in a health facility), age of the child at death, socioeconomic status of the household, whether the child or mother was known to be HIV-positive and whether the mother was a temporary migrant at the time of the child’s deaths, all of which affect child mortality, place of death and care-seeking during the final illness.10 21–23 Sample size was determined by the point at which data saturation was reached.24 25
Selected participants were directly approached at their place of residence to participate in this study. The most appropriate respondent was usually the child’s mother. However, given high levels of temporary migration in the study communities, grandmothers and aunts were sometimes more appropriate.
Data collection
In-depth interviews were conducted by three interviewers to gather personal narratives describing the time around the child’s death. FGDs (facilitated by the same interviewers) produced communal narratives around childhood illness and were used to validate findings from in-depth interviews. All interviews and FGDs were conducted between 6 and 24 months after the child’s death, in the participant’s first language (either isiZulu or Xitsonga), digitally audio-recorded and subsequently transcribed and translated into English by the interviewer. A random selection of transcripts were reviewed to ensure accurate translation. All interviewers were from the local communities, trained in qualitative research and each received additional training from JP to work through the topic guide. All were non-medical (ie, they were not doctors, nurses or community health workers) thereby minimising the effect of social desirability bias,26 which often leads to under-reporting of traditional medicine use, and may have discouraged participants from speaking freely about their experiences of the healthcare system (particularly negative experiences).
Data analysis
We undertook thematic analysis27 28 to identify and analyse the main themes emerging from the interviews and FGDs. The initial coding scheme was based on the topic guide (deductive codes) (online supplemental material 1) and updated to reflect interview and focus group content (inductive codes).29 Related codes were grouped into themes. A sample of six interview transcripts were independently coded by JP and MW to confirm and expand the coding scheme. JP and LH—an experienced social scientist—met to develop the coding frame, whereafter a team meeting was held including JP, MW, LH, AH, JS and KK to agree on a coding framework, which was then used to code all 29 interviews and the focus group discussions. JP, JS and KK have over 30 years combined experience working with these communities and were able to provide context and sensitivity to interpretation of the data. We used the One Sheet of Paper method27 to summarise each of the codes relating to a given theme, being careful to retain nuances across different accounts to represent both convergent and divergent experiences. Findings from the interviews were validated by presenting them to focus group discussions. We considered data saturation to be reached for the major themes after 10–12 interviews at each study site, and a further 3–4 interviews per site did not alter the understanding of the main themes.
bmjopen-2020-043652supp001.pdf (87.3KB, pdf)
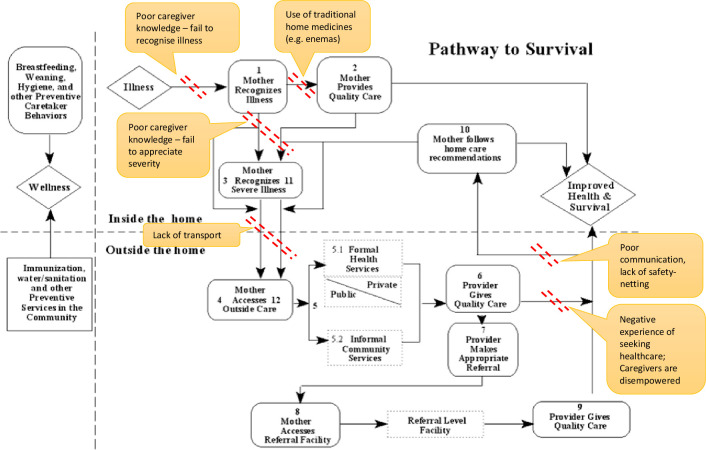
In developing the analysis, we adapted the Pathways to Survival Framework (figure 1),6 which considers care provision within the home and care-seeking outside the home when a child becomes unwell. We demonstrated the stages of the care-seeking process at which each major theme acted, and how caregivers’ accounts of the processes of seeking and receiving healthcare in rural South African communities deviated from those outlined in the original model.
Figure 1.
Adaptation of the Pathways to Survival Framework showing those modifiable factors identified by participants within and outside the home, and the stage of the pathway at which each factor acts.
We used NVivo V.11 (QSR International, Australia) to assist in data management, coding of transcripts and organisation of codes into themes.
Data sharing
To protect confidentiality of participants, anonymised transcripts will only be made available on request.
Patient and public involvement
The community advisory boards at each HDSS site provided input into the study design and assisted with the distribution of findings back to the communities.
Results
Participant characteristics
We conducted 29 in-depth interviews and 2 FDGs (including 4 participants in Agincourt and 5 participants in AHRI). Respondent demographics and key case details are presented in table 1 and online supplemental material 2. Of a total of 38 respondents, 29 were parents (27 mothers, 2 fathers), 7 grandmothers and 2 aunts. Interviews and FGDs detailed events relating to a total of 38 deaths, comprising 4 neonatal deaths (0–27 days), 16 deaths of infants 1–11 months and 18 deaths of children 1–4 years. Nineteen children had died in health facilities, 16 at home and 3 on route to a health facility. Overall, 32 caregivers had sought formal healthcare for their child during the child’s final illness. Eight caregivers used traditional or faith-based medicines and practices during the final illness, all of whom also sought formal healthcare. A further four indicated that traditional medicines and practices had been used in previous illness episodes for the child or other family members even if not used in the final illness. Three caregivers neither provided home care nor sought any formal, traditional or faith-based care outside the home—all three children died within 24 hours of caregivers recognising signs of illness.
Table 1.
Summary of characteristics of respondents and their deceased children*
| Characteristic | Total (n=38) | Agincourt (n=19) | AHRI (n=19) | |||
| N | % | N | % | N | % | |
| Age of the deceased child | ||||||
| 0–27 days (neonate) | 4 | 11 | 2 | 11 | 2 | 11 |
| 1–11 months | 16 | 42 | 9 | 47 | 7 | 37 |
| 12–59 months | 18 | 47 | 8 | 42 | 10 | 53 |
| Sex of deceased child | ||||||
| Male | 21 | 55 | 11 | 58 | 10 | 53 |
| Female | 17 | 45 | 8 | 42 | 9 | 47 |
| Relationship of respondent to the deceased | ||||||
| Mother | 27 | 71 | 10 | 53 | 17 | 89 |
| Father | 2 | 5 | 2 | 11 | 0 | 0 |
| Grandmother | 7 | 18 | 5 | 26 | 2 | 11 |
| Aunt | 2 | 5 | 2 | 11 | 0 | 0 |
| Place of death | ||||||
| Home | 16 | 42 | 6 | 32 | 10 | 53 |
| Healthcare facility | 19 | 50 | 12 | 63 | 7 | 37 |
| On route | 3 | 8 | 1 | 5 | 2 | 11 |
| Cause of death | ||||||
| Acute respiratory infection | 11 | 29 | 8 | 42 | 3 | 16 |
| Diarrhoeal disease | 4 | 11 | 0 | 0 | 4 | 21 |
| Meningitis/Encephalitis | 3 | 8 | 0 | 0 | 3 | 16 |
| Neonatal conditions | 3 | 8 | 2 | 11 | 1 | 5 |
| Burns | 2 | 5 | 2 | 11 | 0 | 0 |
| Other | 5 | 13 | 3 | 16 | 2 | 11 |
| Unknown | 10 | 26 | 4 | 21 | 6 | 32 |
| Household socioeconomic quintile within HDSS | ||||||
| 1 (poorest) | 8 | 21 | 7 | 37 | 1 | 5 |
| 2 | 9 | 24 | 5 | 26 | 4 | 21 |
| 3 | 7 | 18 | 4 | 21 | 3 | 16 |
| 4 | 7 | 18 | 1 | 5 | 6 | 32 |
| 5 (least poor) | 7 | 18 | 2 | 11 | 5 | 26 |
| Mother’s HIV status | ||||||
| Positive | 8 | 21 | 3 | 16 | 5 | 26 |
| Negative | 23 | 61 | 14 | 74 | 9 | 47 |
| Unknown/Unreported | 7 | 18 | 2 | 11 | 5 | 26 |
| Mozambican descent | Not totalled | 4 | 21 | – | – | |
| Sought formal healthcare outside the home | 32 | 84 | 16 | 84 | 16 | 84 |
| Used traditional medicine or consulted a traditional healer for child’s final illness | 6 | 16 | 1 | 5 | 5 | 26 |
| Used traditional medicine or consulted a traditional healer for previous childhood illness | 10 | 26 | 3 | 16 | 7 | 37 |
*Data for table 1 is drawn from data collected as part of the routine household survey conducted in each site, as well as data collected specifically as part of this study.
AHRI, Africa Health Research Institute.
bmjopen-2020-043652supp002.pdf (99KB, pdf)
Themes
The main themes to emerge from the analysis relate to (1) caregiver knowledge and advice-seeking, (2) the use of traditional medicines and practices, (3) transport barriers, (4) experiences of care-seeking during the final illness and (5) communication.
Caregiver knowledge and advice-seeking
Some caregivers seemed not to appreciate the severity of their child’s symptoms or comprehend why their child died. As noted by a mother whose child died at home:
I can say that if I could have taken my child to the hospital early maybe he would have been fine, because maybe they would have help him; because I never thought, but I just thought it was a normal cry for most of the babies. (Participant 21, mother, child died at home from meningitis/encephalitis)
When caregivers were uncertain about a child’s illness, they sometimes turned to family members and neighbours for advice in assessing the illness and whether to seek care outside the home. In general, mothers felt such consultations were not about seeking family members’ permission to take a given action, but rather consulting them in an exercise of joint decision-making based on a joint assessment of the child’s condition. The mother of a child who died at home explained their household’s usual processes of assessing child illness and whether further care was needed:
We normally discuss [the child’s condition] with whoever is around home (Participant 26, mother, child died at home from an unknown cause)
However, such processes of advice seeking did not necessarily improve the capacity to assess the situation accurately. One grandmother explained that both she and the mother were uncertain about the child’s illness:
We were sharing ideas on what to do. Even my daughter’s sister in-law was also here and she is the one who said that it is better to take the child to the clinic. (Participant 6, grandmother, child died in a health facility from an acute respiratory infection)
Traditional medicine and practices
Traditional medicine and practices in these settings operate within a complex set of belief systems.30 31 Most participants reported practising cultural traditions or rituals related to African ancestral belief systems which underpin their worldview. However, our participants differentiated use of traditional healers and medicine from the much more common practice of cultural rituals and traditions. For example, one mother explained:
Yes, [we practice] the burning of incense, also we do slaughtering. In most times maybe we slaughter goats when we have something we will be doing… (Participant 25, mother, child died at home from diarrhoeal disease)
But this participant also noted:
In our church we don’t go for traditional healers nor faith healers. (Participant 25, mother, child died at home from diarrhoeal disease)
The motivations participants described for using traditional medicines and traditional healers varied. Some caregivers admitted to administering traditional enemas as part of the routine care they provide within the home to promote well-being or treat common symptoms of mild illness. One grandmother frequently administered enemas to her grandchildren:
Children here at home are being given enemas when the sun is too hot to release the gall. She used to enema them, not only my child but all the kids at home. (Participant 30, mother, child died in a health facility from an acute respiratory infection)
Other caregivers used traditional enemas despite being aware of advice against this, because they did not seem to know what to do instead and did not want to do nothing:
It’s not easy. They say children should no longer be given enemas. [But] you are also trying to help. (Participant 35, mother, child died on route to a health facility from diarrhoeal disease)
Caregivers who consulted traditional healers during the child’s final illness all did so as a last resort, having experienced formal providers as unhelpful.
I thought I will go to someone [a traditional healer] to hear what is really happening for I’ve been to the clinic, there was no help, I go to the doctor I get no help. (Participant 24, mother, child died at home of an unknown cause)
In our study, caregivers who consulted traditional healers did not express a strongly held belief that their child’s illness had an underlying traditional cause. In fact, some caregivers distinguished their recourse to traditional healers in these cases, from others in which they went directly to a traditional healer in the belief that the cause of the illness was traditional and therefore traditional treatment was the most appropriate means of healthcare.
Transport barriers
A lack of affordable transport frequently caused a delay in accessing healthcare and was an important consideration in deciding when and where to access healthcare.
There are people who end up not getting to clinic because they don’t have money for transport. (Participant 26, mother, child died at home from an unknown cause)
Participants noted that ambulances were slow or unavailable. Arranging a private car was difficult and often caused delays with disastrous consequences:
I was not having a car by that time. Then we found my wife’s father’s car. While we were on our way to the hospital around [the village] the car just stopped. We waited for another car to come and assist us. The car came and when we arrived at [the hospital], we found that … I am not sure if the child died at the gate of the hospital or he died inside the hospital, I can’t remember. We never got any assistance because he was dead already. (Participant 9, father, child died on arrival at a health facility from an acute respiratory infection)
Many were ultimately able to overcome the transport barrier, borrowing money from family and neighbours to cover the costs of taxis or hire private cars, or by asking others to help with lifts to the health facilities. But a lack of transport frequently caused a delay in accessing healthcare and was an important consideration in deciding when and where to access healthcare. Participants from the FDGs added that transport barriers were exacerbated at night as:
There is no other option but to pay for someone’s car and go to [the 24-hour clinic] as it is always open. (Participant 36, grandmother, child died in a health facility from severe acute malnutrition)
Experiences of care-seeking during the final illness
For many of the caregivers, a negative experience at the hands of nurses or doctors was not unusual; yet this did not deter them from seeking care for their sick children at formal healthcare facilities. Unfortunately, many of the children who died at home were sent home on the strength of inadequate diagnoses or treatment, and/or little information as to what to look out for and when to seek further care (ie, poor safety netting advice).
Table 2 summarises the specific features of care-seeking interactions during the final illness that caregivers associated with a positive or negative experience. Of note, most caregivers had very low expectations of the healthcare system, so much so that positive experiences of care-seeking were often the result of an absence of poor care rather than the presence of good care practices. For example, participants were satisfied with a care-seeking interaction when:
Table 2.
Care-seeking experiences
| Negative care-seeking experiences | Positive care-seeking experiences |
Poor communication
|
Good communication
|
Inattentive staff
|
Tangible sense of ‘being treated’
|
Delays or waiting
|
Timings
|
The nurses didn’t blame me or say something that was out of line (participant 3, grandmother, child died at home of unknown cause), and when they didn’t shout at me. (Participant 21, mother, child died at home from meningitis/encephalitis)
However, many caregivers continued to engage with formal health services despite negative experiences of seeking care—and so these are not sufficient to explain the phenomenon of home deaths.
Communication
Communication clearly influenced caregivers’ overall experience of care and more directly linked to their subsequent care-seeking behaviour. Features of good communication included demonstrating respect for the caregiver’s knowledge of their child, explaining what procedures or treatments were being administered and not shouting at or blaming caregivers. As one mother recalled:
The nurses from [the hospital] communicate with you as the children’s parents, ask how the child is and what changes you see or that you don’t see change. (Participant 22, grandmother, child died in a health facility of unknown cause)
Unfortunately, most caregivers experienced poor communication when seeking care during the child’s final illness and reported that healthcare workers were hostile, rude and dismissive, shouted at caregivers for bringing children at the wrong time (either too late in the day or at the weekend) and blamed caregivers for the child’s illness—especially if traditional medicine was used—saying they ‘killed the child’. (Participants 30, mother, child died a health facility of an acute respiratory illness and participant 36, grandmother, child died in a health facility of severe acute malnutrition).
In some cases, healthcare workers were dismissive of caregivers’ concerns, despite caregivers being sure that something was seriously wrong with their child. The mother of a child who died at home was worried:
I woke up with him in that morning and he was not fine. (Participant 25, mother, child died at home from diarrhoeal disease)
She took her child to the clinic, but the nurses dismissed her, saying:
They don’t work on nominals [non-emergency patients] on Sunday. (Participant 25, mother, child died at home from diarrhoeal disease).
Despite waiting many hours at the clinic, the staff refused to assess the child and eventually she left the facility without receiving help. A father whose neonate was crying constantly, not eating or drinking, and was dismissed by nurses at the clinic explained:
We didn’t get any help from the clinic (participant 8, father, child died on route to heath facility from neonatal sepsis).
Safety-netting was another important part of communication: one father who had taken his child to a GP during the final illness recalled:
[The GP] told us that he is going to give us some medication that we need to go and give to the child. He also said to us as it is Monday today, if you don’t see any changes on Tuesday, please come back. (Participant 8, father, child died on route to heath facility from neonatal sepsis)
This experience was in contrast to the experiences of most other participants, for whom poor communication was the norm and who did not recall being given any advice about what danger signs to look out for and when to come back for review. This implies that many caregivers did not know what they should expect of the treatment or that the child might deteriorate despite receiving medication and need to return to the healthcare facility.
Poor communication also resulted in caregivers failing to understand why their child had died. This left caregivers feeling anxious, often doubting their own assessment of the child’s condition. They lost confidence in their ability to assess and manage future child illness (even mild cases), and internalised blame for the child’s death. Many caregivers said that, following their child’s death, they now relied fully on clinic staff to assess the severity of their other children’s illnesses and provide treatment guidance:
I don’t do anything by myself. I take the child to the clinic. Even if it can be something that I know, I do take the child to the clinic… because of what happened to me last time, I think that something like that can happen again. (Participant 13, mother, child died at home of unknown cause)
For me, I use the clinic a lot because I learnt a lesson with the one that died. When they have a little cough or diarrhoea, no-one tells me, I put one on my back and pull the other by the hand to the clinic, I no longer make a mistake. (Participant 37, mother, child died at home of diarrhoeal disease)
I encourage the clinic because I have buried other children. (Participant 36, grandmother, child died in a health facility from severe acute malnutrition)
Discussion
This study highlighted the multiple barriers faced by caregivers in providing care to children within the home, and seeking and receiving care outside the home. Caregivers’ knowledge of childhood illness varied—with some unable to identify severe illness in their child or appreciate the urgency of the need for healthcare. Traditional medicine was used by some caregivers, although rarely as a first port of call. When used as part of home care, caregivers suggested that they turned to traditional medicines as something familiar, particularly when they felt desperate, even when they did not identify a traditional cause of their child’s illness. Transport barriers remain significant: cost, limited minibus-taxi times and having to arrange to hire or borrow private cars caused delays in accessing healthcare. Finally, caregivers continued to engage formal healthcare services despite many reporting negative care-seeking experiences; poor communication both exacerbated negative experiences and contributed to failures to re-seek care appropriately. Furthermore, failure to explain the cause of death of the child led to a greater a sense of dependency on formal healthcare services in future child illness. As such, existing models of care-seeking must be adapted to reflect caregivers’ realities.
Adapting the pathways to survival framework
Figure 1 shows the Pathways to Survival Framework.6 Many of the key issues identified by participants are overlaid on this model, demonstrating the stage and manner in which they act as barriers to accessing high-quality healthcare. We found that transport delays are an important issue, in contrast to findings from standard quantitative verbal and social autopsies (VASAs) in this context (probably because the VASA questions are framed too broadly).2 In figure 2, we summarise the care-seeking process in rural South Africa, based on barriers reported by caregivers in this study.
Figure 2.
Modified model of the process of seeking and providing healthcare during fatal childhood illness in rural South Africa.
The pathway for a severely ill child is indicated by black arrows. While the initial pathway remains similar to the standard model, differences arise following negative experiences of seeking care outside the home (step 4), and so when the child deteriorates (step 5) caregivers’ responses may differ: some might re-seek care, although often going to a different provider (either to a different clinic, to a private GP or to a hospital) (step 6a). Some believe that the failure to improve having received allopathic treatment must indicate that this is a traditional problem and so seek out traditional healers (step 6b). Others are either unable to re-seek care, or believe that having seen a healthcare professional already, there is nothing more to be done (step 6c). Ultimately, the child dies (whether at home or in a health facility) (steps 6c, 7). Although depicted as a broadly linear model for ease of understanding, caregivers may simultaneously seek care from multiple providers (both formal and informal).
In addition to more accurately describing the care pathway for fatal child illness in rural South Africa as experienced by caregivers, our proposed model is the first to offer insights into the effects on care-seeking in future childhood illness in the context of poor caregiver knowledge both in identifying signs of severe illness and in understanding why the first child died (pathway indicated by orange dashed arrows). Following the death of their child, caregivers lose confidence in their ability to identify severe child illness (arrow A) and become reliant on healthcare workers to identify disease and guide treatment (arrow B). This is true even for very mild childhood illness which could be adequately managed at home. As a result, there is a growing burden on the health system, whereby mildly unwell children are also brought to the clinic (as has been described in work by Horwood et al32), exacerbating the existing supply-side barriers to high-quality care (staff shortages, resource limitations, poor management, long waiting times, etc33) (arrow C) and perpetuating negative experiences of care (arrow D).
Our model also highlights the role of traditional healers and traditional medicine use in South Africa. While participants admitted to continued use of traditional medicines (traditional enemas in particular), their motivations largely reflect a familiarity with these treatment methods and a trust in their value based on a shared world view. Traditional treatments such as enemas (which may include herbal administrations, toothpaste, water and dishwashing liquid) are common home treatments in South Africa used in both preventative and curative traditional healthcare.34 35 Traditional healers were not typically the first port of call for fatal child illnesses, although were consulted if a child was not improving after formal medical care. Work elsewhere in Africa also shows that use of traditional healers as the first treatment provider is declining.36 Caregivers did not clearly identify a specific traditional cause of disease that they were trying to treat, although other work in SSA found that many caregivers believe in traditional explanations and so preferentially seek traditional care for specific disease symptoms—such as convulsions associated with cerebral malaria.37–39
Sharkey et al18 report that repeated negative experiences of care result in care-seeking from multiple service providers and use of traditional healers (although not as the first port of call),18 but they suggest that this pattern demonstrated a distrust in the formal healthcare system. In contrast, we did not find evidence to support a loss of trust in formal healthcare providers. This may reflect differences in the degree of community and caregiver empowerment, caregiver education or between rural and urban communities (with urban caregivers seeking care more frequently and from more providers). Furthermore, their model does not describe care-seeking for future child illness.
Social exclusion
Amartya Sen’s work on social exclusion40 may help explain caregivers’ response of increasing (rather than reducing) use of the formal healthcare system despite repeated negative experiences and low expectations of the quality of care they are likely to receive. Sen argues that impoverishment extends beyond the material and includes non-material elements (‘capabilities’), which are critical to the freedom to access opportunities.40
In the South African public healthcare context, negative engagements with healthcare professionals undermine caregivers’ ability to claim a minimum standard of healthcare by reinforcing perceptions of social exclusion which feed into their lived experience of poverty. This also helps explain the persistently low expectations of the healthcare system that were implicit in many of the respondents’ comments. This behaviour is described elsewhere in the South African healthcare system in relation to maternal care-seeking and institutional delivery. Verbal and physical abuse of labouring mothers by nursing staff is well documented across South Africa,41 however mothers have come to normalise nurses’ aggressive language as a means of coping with the situation, and as a result may no longer feel that it is unacceptable or offensive.42
In our study, one caregiver exemplified this, referring to their child’s death as ‘their mistake’, rather than recognising that there were multiple failures throughout the healthcare system that contributed to the child’s death. The internalisation of self-doubt and self-blame for the child’s death may be explained by capacity deprivation and social exclusion driven by the negative experiences of care-seeking. Consequently, caregivers lose confidence in their assessment of illness severity. Instead of doubting the healthcare system, or even turning away from it, caregivers delegate more of the assessment and management of their children to healthcare professionals.
Policy implications and priorities for further research
Our adapted care-seeking model highlights the urgent need to empower caregivers, building confidence in seeking and providing appropriate healthcare for their children both within and outside the home and increasing expectations of the quality of care they receive. Policy implications therefore include improved communication strategies with specific emphasis on providing safety netting information at every consultation and encouraging caregivers to ask questions about their child’s diagnosis and treatment. Behaviour change programmes targeting staff attitudes have been successful when trialled at individual facilities.43 44 Strategies to provide such programmes at scale should be prioritised. Finally, community mobilisation programmes using women’s groups and care groups have been shown to effectively improve neonatal and child health, improving caregiver knowledge and capability.45–48 As investment in community health worker programmes is extended, consideration should be given to their role in mobilising such groups within the communities they serve.
Further research is needed to understand in which circumstances parents react to a child death by increasing their use of health services for minor illnesses in subsequent children, or by not seeking treatment from formal health services until the illness becomes severe. Validating the model in a larger sample or with mixed-methods research may also help identify differences in the pathways for children who died at home or en route to a facility compared with those who die in a facility. We would also recommend research to elucidate the care pathway for severely ill children who improve, as this may provide valuable insights into those factors which promote positive outcomes. Further qualitative research is also needed to understand why traditional enemas are so commonly used for home treatment of childhood illnesses in South Africa, while they are not so commonplace elsewhere. This could help to inform the development of interventions to improve the use of home treatments and treatment-seeking behaviour for children in South Africa.
Strengths and limitations
This study had four important strengths, and corresponding limitations. First, all interviews and FGDs were conducted in participants’ first language (isiZulu or Xitsonga). This encouraged participation of individuals who might otherwise have refused or been unable to participate in the study if all data collection had been in English or via an interpreter. However, it is possible that some of the subtleties of the meaning and tone of the conversation were lost during translation of the interviews into English. Second, interviews were conducted at least 1 year after the death of the children in question, but in some cases up to 2 years after the child’s death. Most caregivers had therefore grieved the loss of their child and the risk of the study causing significant emotional distress was lower. However, this time delay also introduced the potential for recall bias. We tried to reduce the impact of this by concentrating on caregiver’s impressions of healthcare services and how they felt about their care-seeking experiences and less on precise timings or medications prescribed. Third, our sampling strategy allowed us to capture a diverse set of opinions and included fathers and traditional healers who were the primary caregivers of the child during their final illness—both of whom are generally under-represented in research on childhood illness49 50 despite being important stakeholders, contributing to decision-making and caregiving, often holding positions of authority within the household and community and sometimes acting as gatekeepers to care. Fourth, caregivers’ accounts were used to modify the Pathways to Survival Framework to produce a care-seeking model for childhood illness in rural South Africa. This model contributes to the literature on theories of care-seeking and access to healthcare and can be used as a basis for further research on childhood illness and intervention development to reduce child mortality. However, the adapted model may be context-specific and would require further validation in other settings before it is more widely applied.
Conclusion
Understanding factors that contribute to home deaths in rural South Africa is critical in designing effective policies to reduce child mortality. Failure to recognise signs of severe illness, lack of access to transport, poor communication and a lack of safety-netting advice from healthcare providers all contribute to home deaths of children under-5. Furthermore, repeated negative experiences of care-seeking in the context of poverty and social exclusion may disempower caregivers, limiting their ability to claim a minimum standard of healthcare. This realisation is critical in refining our thinking around care-seeking. Interventions designed to empower caregivers—including improved communication and safety netting, changing staff attitudes and community mobilisation—should be prioritised as part of a wider strategy to reduce child mortality.
Supplementary Material
Footnotes
Twitter: @Price_Jess
Correction notice: Following line has been added to the funding statement "LH based in The Healthcare Improvement Studies Institute (THIS Institute), University of Cambridge. THIS Institute is supported by the Health Foundation, an independent charity committed to bringing about better health and healthcare for people in the UK."
Contributors: JP, LH, MW, KK and AH conceived and designed the study. VD, AK and PK conducted, transcribed and translated the interviews and FGDs. JP, MW and LH analysed the data with input from KK, JS, VD, AK and PK. JP and LH led the writing of the manuscript. All author contributed to, and critically revised it.
Funding: This study was funded by the Grand Challenges Research Fund (0005119). JP was funded by the Rhodes Scholarship (no grant number available), and travel costs were covered by the Africa Oxford Travel Grant (AfiOx-19), and Green Templeton College (no grant number available). MW’s salary was funded by the National Institute of Health Research (NIHR), under grant CL-2016-26-005. The Africa Health Research Institute and the MRC/Wits-Agincourt Unit are both nodes of the South African Population Research Infrastructure Network (SAPRIN), funded by the National Department of Science and Innovation and hosted by the South African Medical Research Council (no grant number available). The Africa Health Research Institute’s Population Intervention Programme is also funded by the Wellcome Trust (201433/Z/16/Z). The MRC/Wits-Agincourt Unit has also been supported by the University of the Witwatersrand, the Medical Research Council, South Africa, the Wellcome Trust, UK (grants 058893/Z/99/A; 069683/Z/02/Z; 085477/Z/08/Z; 085477/B/08/Z). LH based in The Healthcare Improvement Studies Institute (THIS Institute), University of Cambridge. THIS Institute is supported by the Health Foundation, an independent charity committed to bringing about better health and healthcare for people in the UK.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. To protect confidentiality of participants, anonymised transcripts will only be made available on request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the Oxford Tropical Research Ethics Committee (OxTREC ref: 509-18), the University of the Witwatersrand Human Research Ethics Committee (Medical) (M180102), the Mpumalanga Province Health Research Committee (MP_201804_006) and the University of KwaZulu-Natal Biomedical Ethics Research Committee (BE259/18). Participants provided written consent to participate.
References
- 1.UNICEF . Under-five mortality. UNICEF, 2019. Available: https://data.unicef.org/topic/child-survival/under-five-mortality/
- 2.Price J, Lee J, Willcox M, et al. Place of death, care-seeking and care pathway progression in the final illnesses of children under five years of age in sub-Saharan Africa: a systematic review. J Glob Health 2019;9:020422. 10.7189/jogh.09.020422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Savigny D, Mayombana C, Mwageni E, et al. Care-seeking patterns for fatal malaria in Tanzania. Malar J 2004;3:27. 10.1186/1475-2875-3-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Källander K, Hildenwall H, Waiswa P, et al. Delayed care seeking for fatal pneumonia in children aged under five years in Uganda: a case-series study. Bull World Health Organ 2008;86:332–8. 10.2471/BLT.07.049353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koffi AK, Kalter HD, Loveth EN, et al. Beyond causes of death: the social determinants of mortality among children aged 1-59 months in Nigeria from 2009 to 2013. PLoS One 2017;12:e0177025. 10.1371/journal.pone.0177025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waldman R, Campbell CC, Steketee RW. Overcoming remaining barriers: the pathway to survival. Arlington, 1996. Available: https://pdf.usaid.gov/pdf_docs/PNABZ644.pdf
- 7.Koffi AK, Libite P–R, Moluh S, et al. Social autopsy study identifies determinants of neonatal mortality in Doume, Nguelemendouka and Abong–Mbang health districts, eastern region of Cameroon. J Glob Health 2015;5. 10.7189/jogh.05.010413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koffi AK, Maina A, Yaroh AG, et al. Social determinants of child mortality in niger: results from the 2012 national verbal and social autopsy study. J Glob Health 2016;6:10603. 10.7189/jogh.06.010603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Källander K, Kadobera D, Williams TN, et al. Social autopsy: indepth network experiences of utility, process, practices, and challenges in investigating causes and contributors to mortality. Popul Health Metr 2011;9:44. 10.1186/1478-7954-9-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Price J, Willcox M, Kabudula CW. Home deaths of children under 5 years in rural South Africa: a population‐based longitudinal study. Trop Med Int Heal 2019;24:862–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Price J, Willcox M, Kabudula CW, et al. Care pathways during a child's final illness in rural South Africa: findings from a social autopsy study. PLoS One 2019;14:e0224284. 10.1371/journal.pone.0224284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tlebere P, Jackson D, Loveday M, et al. Community-Based situation analysis of maternal and neonatal care in South Africa to explore factors that impact utilization of maternal health services. J Midwifery Womens Health 2007;52:342–50. 10.1016/j.jmwh.2007.03.016 [DOI] [PubMed] [Google Scholar]
- 13.Haskins L, Grant M, Phakathi S, et al. Insights into health care seeking behaviour for children in communities in KwaZulu-Natal, South Africa. Afr J Prim Health Care Fam Med 2017;9:1–9. 10.4102/phcfm.v9i1.1378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hill Z, Kendall C, Arthur P, et al. Recognizing childhood illnesses and their traditional explanations: exploring options for care-seeking interventions in the context of the IMCI strategy in rural Ghana. Trop Med Int Health 2003;8:668–76. 10.1046/j.1365-3156.2003.01058.x [DOI] [PubMed] [Google Scholar]
- 15.Hooft A, Nabukalu D, Mwanga-Amumpaire J, et al. Factors Motivating traditional healer versus biomedical facility use for treatment of pediatric febrile illness: results from a qualitative study in southwestern Uganda. Am J Trop Med Hyg 2020;103:501–7. 10.4269/ajtmh.19-0897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.James PB, Wardle J, Steel A, et al. Traditional, complementary and alternative medicine use in sub-Saharan Africa: a systematic review. BMJ Glob Health 2018;3:e000895. 10.1136/bmjgh-2018-000895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Q. Chapter 12: traditional and complementary medicine in primary health care. : Medcalf A, Bhattacharya S, Momen H, et al., . Health for all: the journey of universal health coverage. York: Centre for Global Health Histories, 2015. [Google Scholar]
- 18.Sharkey A, Chopra M, Jackson D, et al. Influences on healthcare-seeking during final illnesses of infants in under-resourced South African settings. J Health Popul Nutr 2011;29:379–87. 10.3329/jhpn.v29i4.8455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kahn K, Collinson MA, Gómez-Olivé FX, et al. Profile: Agincourt health and socio-demographic surveillance system. Int J Epidemiol 2012;41:988–1001. 10.1093/ije/dys115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tanser F, Hosegood V, Bärnighausen T, et al. Cohort profile: Africa centre demographic information system (ACDIS) and population-based HIV survey. Int J Epidemiol 2008;37:956–62. 10.1093/ije/dym211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark SJ, Kahn K, Houle B, et al. Young children's probability of dying before and after their mother's death: a rural South African population-based surveillance study. PLoS Med 2013;10:e1001409. 10.1371/journal.pmed.1001409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sartorius B, Kahn K, Collinson MA, et al. Survived infancy but still vulnerable: spatial-temporal trends and risk factors for child mortality in the Agincourt rural sub-district, South Africa, 1992-2007. Geospat Health 2011;5:285–95. 10.4081/gh.2011.181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kabudula CW, Houle B, Collinson MA, et al. Socioeconomic differences in mortality in the antiretroviral therapy era in Agincourt, rural South Africa, 2001–13: a population surveillance analysis. Lancet Glob Health 2017;5:e924–35. 10.1016/S2214-109X(17)30297-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Braun V, Clarke V. Planning and designing qualitative research. in: successful qualitative research: a practical guide for beginners. London: SAGE Publications Ltd, 2013: 42–74. [Google Scholar]
- 25.Guest G, Bunce A, Johnson L. How many interviews are enough? an experiment with data saturation and variability. Field methods 2006;18:59–82. [Google Scholar]
- 26.Braun V, Clarke V. Interactive data collection 1: interviews. In: Successful Qualitative Research: A Practical Guide for Beginners. London: SAGE Publications Ltd, 2013: 77–106. [Google Scholar]
- 27.Ziebland S, McPherson A. Making sense of qualitative data analysis: an introduction with illustrations from DIPEx (personal experiences of health and illness). Med Educ 2006;40:405–14. 10.1111/j.1365-2929.2006.02467.x [DOI] [PubMed] [Google Scholar]
- 28.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 29.Green J, Thorogood N. Qualitative methods for health research. 4th ed. Thousand Oaks, California: SAGE Publications Ltd, 2018. [Google Scholar]
- 30.Helman CG. Culture, health and illness. London: Arnold, 2001. [Google Scholar]
- 31.Dugmore H, Van Wyk B-E. Muthi and myths from the African bush. Pretoria: Marula Books (an imprint of Briza Publications), 2008. [Google Scholar]
- 32.Horwood C, Butler LM, Vermaak K, et al. Disease profile of children under 5 years attending primary health care clinics in a high HIV prevalence setting in South Africa. Trop Med Int Heal 2011;16:42–52. 10.1111/j.1365-3156.2010.02672.x [DOI] [PubMed] [Google Scholar]
- 33.Maphumulo WT, Bhengu BR. Challenges of quality improvement in the healthcare of South Africa post-apartheid: a critical review. Curationis 2019;42:e1-e9. 10.4102/curationis.v42i1.1901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kauchali S, Rollins N, Van den Broeck J, et al. Local beliefs about childhood diarrhoea: importance for healthcare and research. J Trop Pediatr 2004;50:82–9. 10.1093/tropej/50.2.82 [DOI] [PubMed] [Google Scholar]
- 35.Pretorius E. Complimentary and alternative medicine and traditional health care in South Africa. : van Rensburg H, . Health and health care in South Africa. Pretoria: Van Schaik Publishers, 2012: 593–646. [Google Scholar]
- 36.Graz B, Willcox M, Berthé D, et al. Home treatments alone or mixed with modern treatments for malaria in Finkolo AC, South Mali: reported use, outcomes and changes over 10 years. Trans R Soc Trop Med Hyg 2015;109:209–13. 10.1093/trstmh/tru181 [DOI] [PubMed] [Google Scholar]
- 37.Muela SH, Ribera JM, Tanner M. Fake malaria and hidden parasites-the ambiguity of malaria. Anthropol Med 1998;5:43–61. 10.1080/13648470.1998.9964548 [DOI] [PubMed] [Google Scholar]
- 38.Cunnama L, Honda A. A mother's choice: a qualitative study of mothers' health seeking behaviour for their children with acute diarrhoea. BMC Health Serv Res 2016;16:669. 10.1186/s12913-016-1911-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nuwaha F, Okware J, Hanningtone T, et al. False teeth "Ebiino" and Millet disease "Oburo" in Bushenyi district of Uganda. Afr Health Sci 2007;7:25–32. 10.5555/afhs.2007.7.1.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sen A. Social exclusion: concept, application, and scrutiny., 2000. Available: https://www.adb.org/sites/default/files/publication/29778/social-exclusion.pdf
- 41.Human Rights Watch . ‘Stop making excuses’: accountability for maternal health care in South Africa, 2011. Available: http://www.hrw.org
- 42.Kruger Lou‐Marié, Schoombee C. The other side of caring: abuse in a South African maternity ward. J Reprod Infant Psychol 2010;28:84–101. 10.1080/02646830903294979 [DOI] [Google Scholar]
- 43.Fonn S, Xaba M. Health workers for change: developing the initiative. Health Policy Plan 2001;16 Suppl 1:13–18. 10.1093/heapol/16.suppl_1.13 [DOI] [PubMed] [Google Scholar]
- 44.Kim J, Motsei M. "Women enjoy punishment": attitudes and experiences of gender-based violence among PHC nurses in rural South Africa. Soc Sci Med 2002;54:1243–54. 10.1016/s0277-9536(01)00093-4 [DOI] [PubMed] [Google Scholar]
- 45.Prost A, Colbourn T, Seward N, et al. Women's groups practising participatory learning and action to improve maternal and newborn health in low-resource settings: a systematic review and meta-analysis. Lancet 2013;381:1736–46. 10.1016/S0140-6736(13)60685-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Manandhar DS, Osrin D, Shrestha BP, et al. Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet 2004;364:970–9. 10.1016/S0140-6736(04)17021-9 [DOI] [PubMed] [Google Scholar]
- 47.Women's groups to improve maternal and child health outcomes: different evidence paradigms toward impact at scale. Glob Health Sci Pract 2015;3:323–6. 10.9745/GHSP-D-15-00251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sutter E, Maphorogo S. The elim care groups: a community project for the control of trachoma. Community Eye Health 2001;14:47. [PMC free article] [PubMed] [Google Scholar]
- 49.Kauchali S, Rollins N, Bland R, et al. Maternal perceptions of acute respiratory infections in children under 5 in rural South Africa. Trop Med Int Health 2004;9:644–50. 10.1111/j.1365-3156.2004.01238.x [DOI] [PubMed] [Google Scholar]
- 50.Iyun BF, Tomson G. Acute respiratory infections-mothers' perceptions of etiology and treatment in south-western Nigeria. Soc Sci Med 1996;42:437–45. 10.1016/0277-9536(95)00103-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-043652supp001.pdf (87.3KB, pdf)
bmjopen-2020-043652supp002.pdf (99KB, pdf)
Data Availability Statement
Data are available on reasonable request. To protect confidentiality of participants, anonymised transcripts will only be made available on request.