Abstract
This is a rare presentation of scrub typhus with cerebral venous thrombosis. A 32-year-old woman presented with signs of raised intracranial tension. Examination revealed maculopapular skin rashes and an ‘eschar’ over the right thigh. Nuchal rigidity and bilateral papilloedema were found. Scrub typhus was diagnosed by the presence of IgM antibody in serum. CT scan of the brain showed cerebral oedema. MRI of the brain was normal. Magnetic resonance venography of the brain showed thrombosis of several venous sinuses. Cerebrospinal fluid analysis revealed lymphocytic pleocytosis with raised protein level. Other causes of prothrombotic states were ruled out by doing specific test results. There was no history of hormonal contraception and prolonged bed rest. A case of scrub typhus complicated with meningoencephalitis and cerebral venous thrombosis was diagnosed. She responded to treatment with doxycycline, anticoagulants, antipyrectics and intravenous saline. Early identification of such atypical neurological involvement in scrub typhus was helpful in satisfactory outcome.
Keywords: infections, neurology (drugs and medicines), infectious diseases, infection (neurology)
Background
Scrub typhus is caused by the rickettsia, Orientia tsutsugamushi, and is transmitted to humans by the bite of larval stage of trombiculid mites. It is commonly seen during the monsoon and postmonsoon season in India. It can involve multiple systems of the body.1 Systemic dissemination occurs by lymphatic and haematogenous spread. Clinical features include fever, headache, myalgias, cough, conjunctival injection, skin rash, lymphadenopathy, gastrointestinal symptoms, features of pneumonitis and myocarditis. The most characteristic skin rash is eschar—caused by the bite of the larval mite. Eschar is seen in about 04%–46% of patients with scrub typhus.2 Diagnosis of scrub typhus is confirmed by detection of IgM antibody in serum, which has high sensitivity and specificity.3 Neurological manifestations of scrub typhus are well described in literature.4 5 The most common neurological manifestation is meningoencephalitis; also seen are acute disseminated encephalomyelitis (ADEM), cerebral infarction, cranial neuropathy, Guillain-Barre syndrome, peripheral neuropathy, brachial plexopathy and transverse myelitis.6 7 Cerebral venous sinus thrombosis in scrub typhus is rare.
Neural tissue injury may occur by direct neuroinvasion or by immune-mediated mechanisms. The organism crosses the blood–brain barrier (BBB) by either breaking the integrity of BBB cells or interacts with epithelial cells of the blood–choroid barrier. The cellular entry routes could be either intercellular or transcellular or by infected macrophages through leucocytes.8 The neurological invasion occurs during the systemic phase of infection via the bloodstream.
Case history
A 32-year-old woman presented with high remittent fever (102–104°F) for last the 10 days. History of holocranial headache, vomiting, visual disturbances with photophobia and occasional confusional state was obtained. There was no history of seizure. The patient was not bed bound prior to these symptoms. She was normotensive, non-diabetic, euthyroid and was not on hormonal contraceptives. Examination revealed fever (103°F) and confusion with disorientation to place, time and person. She was irritable with poor attention span. Nuchal stiffness and bilateral papilloedema were noted. No other neurological localisation signs were found. Maculopapular rashes in different parts of the body and an ‘eschar’ over the medial side of right thigh (figure 1) were seen. Other systemic examinations were normal. Relevant investigations were sent to determine the aetiology of fever with meningeal irritation and bilateral papilloedema.
Figure 1.
Eschar over the medial aspect of the right thigh.
Investigations
Routine laboratory investigations revealed mild leucocytosis 11 000/mm3 (normal value=4000–10 000/mm3) with peripheral lymphocytosis of 50% (normal value=20%–40%); abnormal liver function tests in the form of raised alanine transaminase, 90 IU/L (normal value=7–40) and aspartate transaminase, 86 IU/L (normal value=7–50); erythrocyte sedimentation rate, 16 (normal value=<30); fasting blood sugar, 106 mg/dL (normal value=80–120 mg/dL); serum sodium+, 138 mEQ/L (normal value=130–145 mEQ/L); serum potassium+, 4.2 mEQ/L (normal value=3.4–5.5 mEQ/L); urea, 22 mg/dL (normal value=7–20 mg/dL); and creatinine, 0.7 mg/dL (normal value=0.7–1.3 mg/dL). Blood and urine culture showed no growth of micro-organisms. Investigations for malaria, dengue, typhoid, chikungunya and viral serologies for hepatitis B, C and HIV were all negative. Only IgM antibody for scrub typhus was positive. Chest X-ray and ultrasonography of the whole abdomen was normal. CT scan of the brain showed diffuse brain swelling without any focal lesion (figure 2). Cerebrospinal fluid (CSF) study revealed protein level of 120 mg% (normal value=20–40 mg%), normal glucose and adenosine deaminase and lymphocytic pleocytosis of 30 cells/cumm (normal value=0–10 cells/cumm). Herpes simplex virus (HSV) PCR was negative. MRI of the brain did not show any stroke or demyelinating lesions. Magnetic resonance (MR) venography demonstrated thrombosis of the terminal portion of the superior sagittal sinus, straight sinus, right sigmoid and transverse sinuses (figures 3–5). Other causes of cerebral venous sinus thrombosis were ruled out by negative results from serum homocysteiene, Anti-Nuclear Antibody (ANA) profile, antiphospholipid antibodies, activated partial thromboplastin time, prothrombin time and International Normalized Ratio (INR), protein C, protein S, antithrombin III, factor V Leiden and prothrombin gene mutation. A diagnosis of scrub typhus complicated with meningoencephalitis and cerebral venous thrombosis was made.
Figure 2.

CT of the brain plain showing diffuse cerebral oedema.
Figure 3.
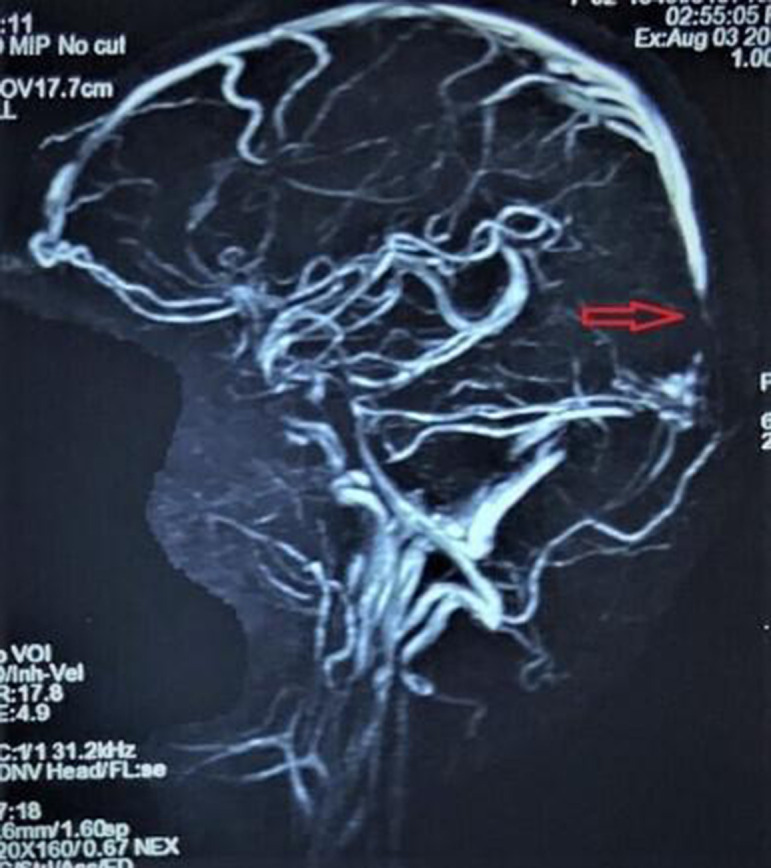
Magnetic resonance venography in volume rendering view showing thrombosis (red arrow) in the terminal part of the superior sagittal sinus.
Figure 4.
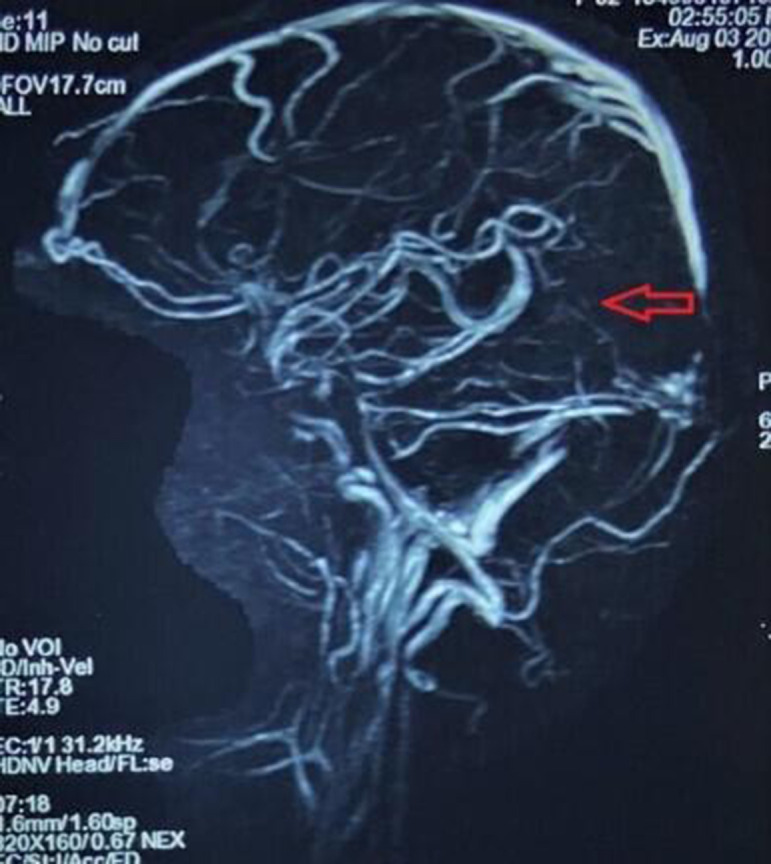
Magnetic resonance venography in volume rendering view showing thrombosis (red arrow) in the straight sinus.
Figure 5.
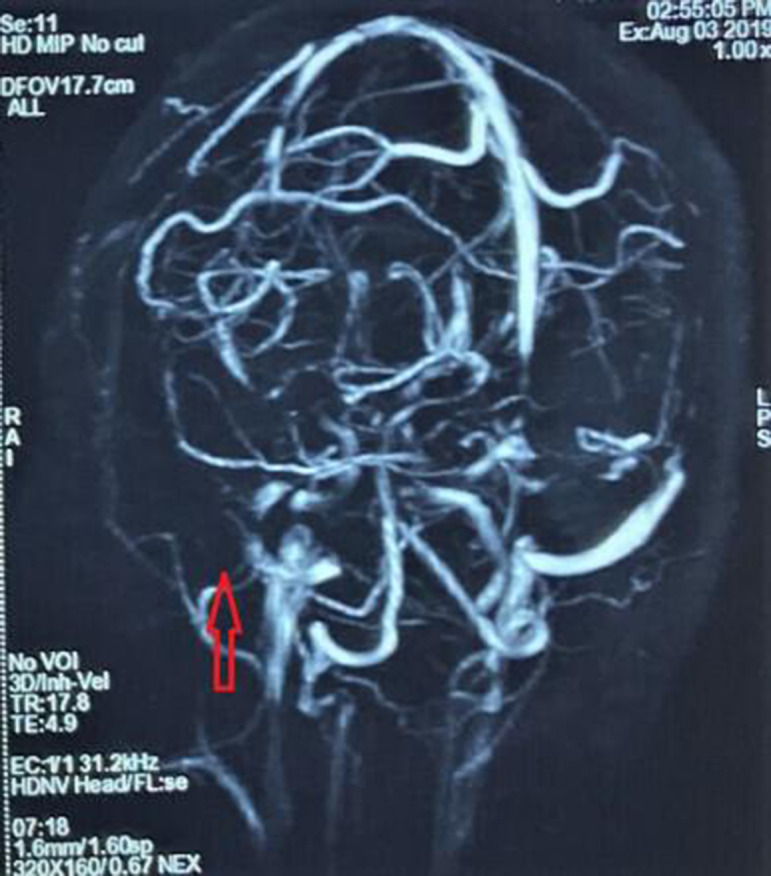
Magnetic resonance venography in volume rendering view showing thrombosis (red arrow) in the right sigmoid and transverse sinus.
Differential diagnosis
This patient with scrub typhus had features suggestive of meningoencephalitis. Other common infective causes of meningoencephalitis like fengue, chikungunya, HSV, tuberculosis, and ear and sinus infections were excluded. The other causes of cerebral venous sinus thrombosis were looked into. There was no history of use of hormonal contraception and prolonged bed rest. Thrombophilia and prothombotic states were excluded by normal results of serum homocysteiene, ANA profile, antiphospholipid antibodies, activated partial thromboplastin time, prothrombin time and INR, protein C, protein S, antithrombin III, factor V Leiden and prothrombin gene mutation. ADEM of parainfectious nature was excluded by the absence of white matter involvement in the MRI of the brain.
Therapy
The patient was treated with doxycycline, initially intravenous for 2 days and then given orally (100 mg two times per day) for another 10 days. Mannitol infusion (100 mL) three times a day for 1 day was given for raised intracranial pressure. It was stopped once venous thrombosis was detected. Adequate hydration was maintained with intravenous saline. Anticoagulants were used—initially low-molecular weight heparin (clexane 60 mg/day) for 3 days, and then changed to warfarin, keeping INR around 2.5.
Outcome
The patient started improving symptomatically after 3 days of therapy. She became afebrile and other symptoms gradually improved. She was ultimately discharged from the hospital after 10 days. At the time of discharge, she was asymptomatic. She was followed up at the outpatient department once a month with INR report. She was continued on oral anticoagulants for a total of 6 months. She was maintaining activities of daily living well until the end of follow-up. Repeat venogram was suggested but could not be done due to financial constraints.
Discussions
This patient with scrub typhus developed meningoencephalitis and cerebral venous sinus thrombosis, characterised by fever, headache, nuchal rigidity, confusion and disorientation, lymphocytic pleocytosis with raised protein and normal glucose level in CSF, diffuse brain swelling from CT scan of the brain and evidence of cerebral venous sinus thrombosis from MR venography. Meningoencephalitis in scrub typhus has been described in as high as 80% of cases. Clinical manifestations usually include fever, headache, vomiting, seizure and altered sensorium. Apart from seizure, other symptoms were seen in this patient. There were no evidence of cerebral infarction or demyelinating lesions from MRI of the brain, but MR venography showed thrombosis of the terminal part of the superior sagittal sinus, straight sinus, and right-sided transverse and sigmoid sinus. Occurrence of cerebral venous sinus thrombosis is extremely rare in scrub typhus, and only two cases have so far been reported in literature: one from Vellore, South India, in 2014, where scrub typhus was complicated with cerebral venous sinus thrombosis and cerebral infarction, and the other by V Sardana and P Shringi, in which case scrub typhus was associated with venous sinus thrombosis and bilateral high frontoparietal oedema.9 10 The cause of this venous thrombosis is likely to be vasculopathy, resulting from endothelial injury caused by cytokine release due to rickettsia infection. There is localised platelet aggregation, polymorph and monocyte proliferation, leading to focal occlusive and angiitis causing microinfarcts in various tissues.11
Patient’s perspective.
I was very ill when was admitted to hospital by my parents. I was really worried then regarding my future. But with excellent care given by the doctors and other hospital staffs, I became well soon. I am now as I was earlier before my illness. I wish my caregivers in the hospitals all the best.
Learning points.
Meningoencephalitis, along with cerebral venous sinus thrombosis, can complicate scrub typhus.
Venous sinus thrombosis is due to vasculopathy caused by endothelial injury following cytokine release.
Early diagnosis is always rewarding as definitive treatment gives satisfactory outcome.
Footnotes
Twitter: @SidharthaChat14
Contributors: SD and SC analysed clinical data and drafted the initial manuscript. KM contributed to discussions and reviewed the manuscript. SB critically reviewed the manuscript including the references and gave it the final shape. All the authors critically reviewed the manuscript for intellectual contents and approved the final version and were accountable for all aspects of the work in terms of accuracy and integrity.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Brown GW. Scrub typhus: pathogenesis and clinical syndromes. : Walker DH, . Biology of rickettsial diseases. Vol1. Broca Raton: Florida, CRC Press, 1988: 93–100. [Google Scholar]
- 2.Mathai E, Rolain JM, VERGHESE GM, et al. Outbreak of scrub typhus in southern India during the cooler months. Ann N Y Acad Sci 2003;990:359–64. 10.1111/j.1749-6632.2003.tb07391.x [DOI] [PubMed] [Google Scholar]
- 3.Prakash JAJ, Abraham OC, Mathai E. Evaluation of tests for serological diagnosis of scrub typhus. Trop Doct 2006;36:212–3. 10.1258/004947506778604715 [DOI] [PubMed] [Google Scholar]
- 4.Mishra UK, Kalita J, Mani VE. Neurological manifestations of scrub typhus. JNNP 2015;86:761–6. [DOI] [PubMed] [Google Scholar]
- 5.Rana A, Mahajan SK, Sharma A, et al. Neurological manifestations of scrub typhus in adults. Trop Doct 2017;47:22–5. 10.1177/0049475516636543 [DOI] [PubMed] [Google Scholar]
- 6.Sameer G, Anu M. Neurological manifestations of scrub typhus. Ann of Indian Academy of Neurology 2013;16:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahajan SK, Mahajan SK. Neuropsychiatric manifestations of scrub typhus. J Neurosci Rural Pract 2017;8:421–6. 10.4103/jnrp.jnrp_44_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sekeyová Z, Danchenko M, Filipčík P, Peter Filipi P, et al. Rickettsial infections of the central nervous system. PLoS Negl Trop Dis;13:e0007469 10.1371/journalpntd0007469,Aug.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jena SS, Mathew A, Sanjith A, et al. Cerebral venous sinus thrombosis presentation in severe scrub typhus infection: a rare entity. Neurol India 2014;62, ::301–10. vol. 10.4103/0028-3886.136991 [DOI] [PubMed] [Google Scholar]
- 10.Sardana V, Shringi P. Cerebral venous sinus thrombosis in scrub typhus infection: a rare presentation. Indian J of case reports 2019;5:22–3. Vol. [Google Scholar]
- 11.Cowan G. Rickettsial diseases: the typhus group of fevers--a review. Postgrad Med J 2000;76:269–72. 10.1136/pmj.76.895.269 [DOI] [PMC free article] [PubMed] [Google Scholar]


