Abstract
Pediatric nonaortic arterial aneurysms are uncommon diagnoses and can be affiliated with underlying conditions, which include neurofibromatosis I, Ehlers-Danlos type IV syndrome, Kawasaki disease, Marfan syndrome, and Loeys-Dietz, polyarteritis nodosa, as well as Klippel-Trenauny syndrome. The standard of care has been early surgical excision and arterial reconstruction when indicated. This report details a case of recurrent brachial artery aneurysm in a 2-year-old boy despite multiple attempts at excision and reconstruction. Such recurrences were seen as rapidly as 3 months postoperatively. Ultimately, a Gore-Tex conduit was used to reinforce a reversed saphenous vein graft repair. There has been no evidence of recurrent disease during the 18-month follow-up period.
Keywords: Aneurysm, Arterial reconstruction, Gore-Tex, Vein graft, Pediatrics
Pediatric nonaortic arterial aneurysms are uncommon diagnoses and isolated upper extremity arterial aneurysms account for a small percentage of the previously published reports.1, 2, 3 In the largest case series published on pediatric nonaortic arterial aneurysms, the authors present traumatic, dysplastic, and congenital idiopathic aneurysms as the three most common subtypes.3 Underlying conditions associated with the formation of these lesions include neurofibromatosis I, Ehlers-Danlos type IV syndrome, Kawasaki disease, Marfan syndrome, and Loeys-Dietz, polyarteritis nodosa, as well as Klippel-Trenauny syndrome.4, 5, 6, 7 Although patients with brachial artery aneurysms often present with a painless pulsatile mass, individuals may experience altered distal sensation and/or motor weakness from local nerve compression, pain, or less commonly signs of distal ischemia.2,8, 9, 10
Because pediatric arterial aneurysms are likely to expand over time, the standard of care has traditionally been early surgical excision and arterial reconstruction. This evolving nature increases the risk for aneurysm rupture, thrombosis, and embolization.3,11,12 Surveillance of these lesions is less commonly reported and therefore the natural history of pediatric nonaortic arterial aneurysms is poorly understood.
Before review, patient consent was obtained from the family and this case report was approved by our institutional review board as protocol H-47733 in compliance with institutional policy.
Case report
A 2-year-old boy with no past medical or contributory family history initially presented to an outside facility with a painless pulsatile mass over the medial aspect of the right upper arm. Ultrasound imaging confirmed the diagnosis of a right brachial artery aneurysm. There were no reports of prior arterial cannulation in the patient's history. A molecular genetics workup at that time showed no evidence of an underlying genetic condition and the aneurysm was thought to be idiopathic in nature. The patient underwent excision of the lesion and reconstruction with a reverse saphenous vein graft. Pathology of this lesion confirmed the presence of a true brachial artery aneurysm with intramural capillary endothelial hyperplasia and fibrosis consistent with an organized mural thrombus. Unfortunately, the aneurysm recurred at both ends of the graft less than 4 months postoperatively, even after a second attempt of excision and saphenous vein grafting. After the second recurrence, he was referred to out institution. Fig 1 depicts the patient's arm upon presentation at Texas Children's Hospital. It was hypothesized that disease recurrence was likely secondary to poor postoperative immobilization.
Fig 1.
Preoperative photograph of recurrent right brachial artery aneurysm before the first surgery at Texas Children's Hospital.
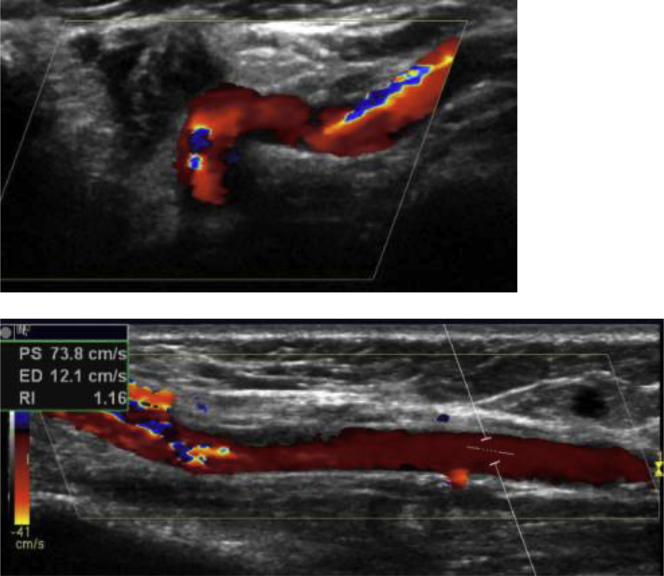
Ultrasound imaging at Texas Children's Hospital confirmed the presence of two aneurysms 7 cm apart at the margins of arterial reconstruction (Fig 2). Computed tomography angiography of the chest, abdomen, and pelvis as well as complete ultrasound imaging of both the upper and lower extremities ruled out additional disease. The distal pulses were intact and the patient had full active and passive range of motion of the right upper extremity. The patient again underwent genetic testing, which was unremarkable. The decision was made to proceed with repeat excision of the aneurysms and the intervening vein graft. Small DeBakey peripheral vascular clamps were applied proximal and distal to the aneurysm and both ends of the brachial artery were flushed with 5 mL of heparinized saline. Reconstruction was performed with a reversed saphenous vein graft with microsurgical anastomosis using interrupted 8-0 nylon sutures. Additionally, acellular dermal matrix was circumferentially wrapped around the anastomotic sites for reinforcement. The final pathology mirrored findings of the prior pathology reports, which described native arterial disease characterized as a “true vs pseudoaneurysm containing extensive myxoid lining and proliferating vascular channels,” all of which spared the interposed vein graft. Prior pathology reports suggested the possibility of native brachial artery disease we may have been incompletely resected thereby contributing to disease recurrence. Postoperatively, the patient was prescribed aspirin 81 mg/d, monitored overnight, and then discharged in a shoulder sling with axillary abduction pillow to assist with 1 month of strict upper extremity immobilization.
Fig 2.
Preoperative duplex Doppler ultrasound imaging showing two aneurysms of the brachial artery approximately 7 cm apart.
At 2 months postoperatively, the patient had returned to full activity; however, repeat ultrasound examination at 3 months showed a recurrent aneurysm vs pseudoaneurysm at the distal end of the vein graft with evidence of intraluminal thrombosis. At this time, the patient complained of occasional sharp snake bite-like pain in his right hand.
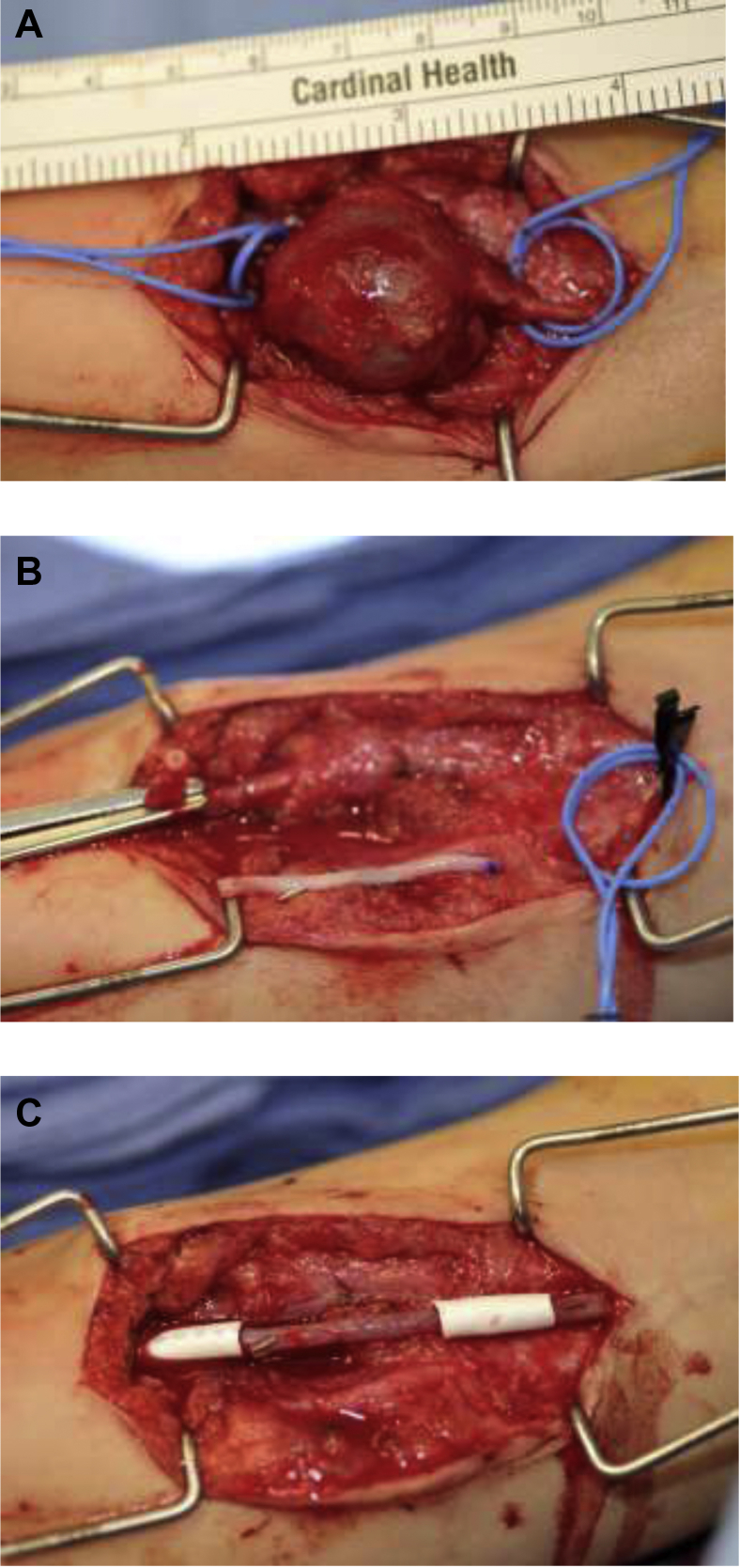
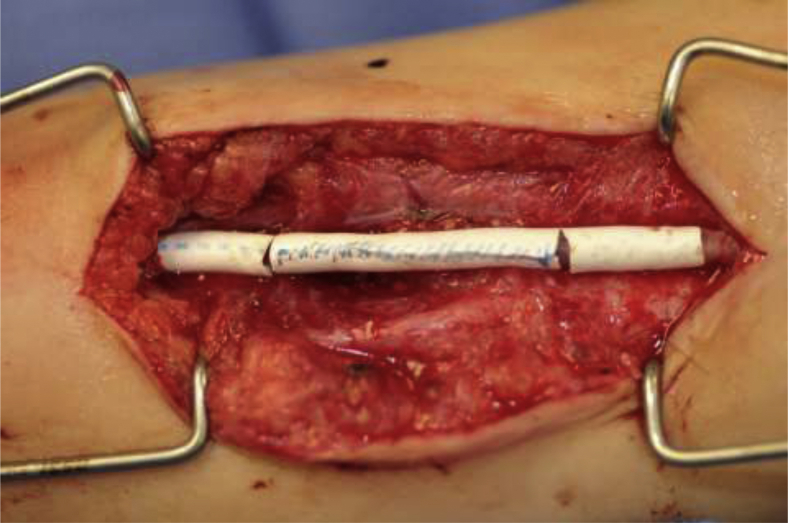
At 3 years of age, the patient was brought back to the operating room for repeat excision and reverse saphenous vein graft repair with the addition of reinforcing 8-mm Gore-Tex vascular graft wraps of both anastomotic sites and the intervening vein graft. The Gore-Tex was anchored to the two sites of anastomosis using an 8-0 nylon suture and positioned such that the wrap extended on to the native artery 7 to 8 mm proximally and distally (Fig 3). A segment of Gore-Tex not fixed in any position was placed around the vein graft approximately the length of the graft. This central segment was left without sutures fixation to allow the vessel to grow longitudinally (Fig 4). The Gore-Tex wrap was meant to counteract the internal forces that were causing aneurysmal dilation of the reconstructed artery by applying rigid external force. The acellular dermal matrix used in the previous surgery was apparently incorporated and resorbed, allowing reformation of the aneurysm. There were no further complications and the patient was discharged on postoperative day 3, again on aspirin therapy with strict right upper extremity immobilization precautions. At 7 weeks postoperatively, the patient was allowed to slowly start ranging the right upper extremity with nighttime splinting for an additional 4 weeks. At 18 months postoperatively, physical examination demonstrated a palpable Gore-Tex graft with no evidence of aneurysm recurrence and an intact palpable radial pulse. The aspirin was discontinued at this visit.
Fig 3.
Intraoperative photographs of the second attempt at aneurysm reconstruction at Texas Children's Hospital. A, In situ brachial artery aneurysm. B, Brachial artery defect after excision of aneurysm and planned reversed saphenous vein graft. C, Gore-Tex wrap reinforcing anastomoses between reversed saphenous vein graft and native brachial artery.
Fig 4.
Intraoperative view of fully reinforced saphenous vein graft with Gore-tex wrap. Note the three separate wraps, two reinforcing the anatomaoses and one spanning the reversed saphenous vein graft.
Discussion
Traditional surgical management of pediatric brachial artery aneurysms includes excision with vessel ligation vs excision with vein graft reconstruction. Vessel ligation may be appropriate when the lesion is distal to the profunda brachii artery or when chronic aneurysm thrombosis has allowed for adequate distal perfusion through neovascularization.9,12
Although it remains unclear why this aneurysm recurred after multiple attempts at excision and reconstruction, it is possible that “early” motion postoperatively (1 month) and tension on the anastomoses by an active child could have been contributing factors. The decision was, therefore, made to attempt to reinforce our initial arterial repair with acellular dermal matrix. This maneuver ultimately failed, likely owing to the incorporation and partial absorption of the material. After this recurrence, a nonabsorbing Gore-Tex wrap was applied around the anastomoses and vein graft, which to date has prevented disease recurrence. The potential downsides of this technique are the inability of the vein graft to dilate over time as the child grows and the synthetic nature of the material. Currently, there are no reports of Gore-Tex reinforced repair of arterial aneurysms in pediatric patients with recurrent peripheral arterial aneurysms.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Bahcivan M., Yuksel A. Idiopathic true brachial artery aneurysm in a nine-month infant. Interact Cardiovasc Thorac Surg. 2008;8:162–163. doi: 10.1510/icvts.2008.187187. [DOI] [PubMed] [Google Scholar]
- 2.Got C., Tan T.W., Thakur N., Marcaccio E.J., Eberson C., Madom I. Delayed presentation of a brachial artery pseudoaneurysm after a supracondylar humerus fracture in a 6-year-old boy: a case report. J Pediatr Orthop. 2010;30:57–59. doi: 10.1097/BPO.0b013e3181c80d4f. [DOI] [PubMed] [Google Scholar]
- 3.Davis F.M., Eliason J.L., Ganesh S.K., Blatt N.B., Stanley J.C., Coleman D.M. Pediatric nonaortic arterial aneurysms. J Vasc Surg. 2016;63:446–476. doi: 10.1016/j.jvs.2015.08.099. [DOI] [PubMed] [Google Scholar]
- 4.Lehrnbecher T., Gassel A.M., Rauh V., Kirchner T., Huppertz H.I. Neurofibromatosis presenting as a severe systemic vasculopathy. Eur J Pediatr. 1994;153:107–109. doi: 10.1007/BF01959219. [DOI] [PubMed] [Google Scholar]
- 5.Akagi D., Ishii S., Kitagawa T., Nagawa H., Miyata T. Popliteal arterial aneurysm associated with Klippel-Trénaunay syndrome: case report and literature review. J Vasc Surg. 2006;43:1287–1289. doi: 10.1016/j.jvs.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 6.Greene J.F., Fitzwater J.E., Burgess J. Arterial lesions associated with neurofibromatosis. Am J Clin Pathol. 1974;62:481–487. doi: 10.1093/ajcp/62.4.481. [DOI] [PubMed] [Google Scholar]
- 7.Zhao Q.M., Chu C., Wu L., Liang X.C., Sun S.N., He L. Systemic artery aneurysms and kawasaki disease. Pediatrics. 2019;144:e20192254. doi: 10.1542/peds.2019-2254. [DOI] [PubMed] [Google Scholar]
- 8.Matsubara J., Shionoya S., Ban I., Nakata Y., Shinjo K. Clinical considerations on peripheral arterial aneurysms. J Cardiovasc Surg (Torino) 1974;15:548–553. [PubMed] [Google Scholar]
- 9.Gray R.J., Stone W.M., Fowl R.J., Cherry K.J., Bower T.C. Management of true aneurysms distal to the axillary artery. J Vasc Surg. 1998;28:606–610. doi: 10.1016/s0741-5214(98)70083-7. [DOI] [PubMed] [Google Scholar]
- 10.Godwin S.C., Shawker T., Chang B., Kaler S.G. Brachial artery aneurysms in Menkes disease. J Pediatr. 2006;149:412–415. doi: 10.1016/j.jpeds.2006.05.041. [DOI] [PubMed] [Google Scholar]
- 11.Sarkar R., Coran A.G., Cilley R.E., Lindenauer S.M., Stanley J.C. Arterial aneurysms in children: clinicopathologic classification. J Vasc Surg. 1991;13:47–56. [PubMed] [Google Scholar]
- 12.Pagès O.N., Alicchio F., Keren B., Diallo S., Lefebvre F., Valla J.S. Management of brachial artery aneurisms in infants. Pediatr Surg Int. 2008;24:509–513. doi: 10.1007/s00383-007-2069-5. [DOI] [PubMed] [Google Scholar]