Abstract
Background
Hypertrophic cardiomyopathy (HCM) is a genetic disease with an autosomal‐dominant inheritance for which negative inotropes are the most widely used initial therapies. Observational studies and small randomised trials have suggested symptomatic and functional benefits using pacing and several theories have been put forward to explain why. Pacing, although not the primary treatment for HCM, could be beneficial to patients with relative or absolute contraindications to surgery or alcohol ablation. Several randomised controlled trials comparing pacing to other therapeutic modalities have been conducted but no Cochrane‐style systematic review has been done.
Objectives
To assess the effects of pacing in drug‐refractory or drug‐intolerant hypertrophic cardiomyopathy patients.
Search methods
We searched the following on the 14/4/2010: CENTRAL (The Cochrane Library 2010, Issue 1), MEDLINE OVID (from 1950 onwards ), EMBASE OVID (from1980 onwards ), Web of Science with Conference Proceedings (from 1970 onwards). No language restrictions were applied.
Selection criteria
Randomised controlled trials of either parallel or crossover design that assess the beneficial and harmful effects of pacing for hypertrophic cardiomyopathy were included. When crossover studies were identified, we considered data only from the first phase.
Data collection and analysis
Data from included studies were extracted onto a pre‐formed data extraction paper by two authors independently. Data was then entered into Review Manager 5.1 for analysis. Risk of bias was assessed using the guidance provided in the Cochrane Handbook. For dichotomous data, relative risk was calculated; and for continuous data, the mean differences were calculated. Where appropriate data were available, meta‐analysis was performed. Where meta‐analysis was not possible, a narrative synthesis was written. A QUROUM flow chart was provided to show the flow of papers.
Main results
Five studies (reported in 10 papers) were identified. However, three of the five studies provided un‐usable data. Thus the data from only two studies (reported in seven papers) with 105 participants were included for this review. There was insufficient data to compare results on all‐cause mortality, cost effectiveness, exercise capacity, Quality of life and Peak O2 consumption.
When comparing active pacing versus placebo pacing on exercise capacity, one study showed that exercise time decreased from (13.1 ± 4.4) minutes to (12.6 ± 4.3) minutes in the placebo group and increased from (12.1 ± 5.6) minutes to (12.9 ± 4.2) minutes in the treatment group (MD 0.30; 95% CI ‐1.54 to 2.14). Statistically significant data from the same study showed that left ventricular outflow tract obstruction decreased from (71 ± 32) mm Hg to (52 ± 34) mm Hg in the placebo group and from (70 ± 24) mm Hg to (33 ± 27) mm Hg in the active pacing group (MD ‐19.00; 95% CI ‐32.29 to ‐5.71). This study was also able to show that New York Heart Association (NYHA) functional class decreased from (2.5 ± 0.5) to (2.2 ± 0.6) in the inactive pacing group and decreased from (2.6 ± 0.5) to (1.7 ± 0.7) in the placebo group (MD ‐0.50; 95% CI ‐0.78 to ‐0.22).
When comparing active pacing versus trancoronary ablation of septal hypertrophy (TASH), data from one study showed that NYHA functional class decreased from (3.2 ± 0.7) to (1.5 ± 0.5) in the TASH group and decreased from (3.0 ± 0.1) to (1.9 ± 0.6) in the pacemaker group. This study also showed that LV wall thickness remained unchanged in the active pacing group compared to reduction from (22 ± 4) mm to (17 ± 3) mm in the TASH group (MD 0.60; 95% CI ‐5.65 to 6.85) and that LV outflow tract obstruction decreased from (80 ± 35.5) mm Hg in the TASH group to (49.3 ± 37.7) mm Hg in the pacemaker group.
Authors' conclusions
Trials published to date lack information on clinically relevant end‐points. Existing data is derived from small trials at high risk of bias, which concentrate on physiological measures. Their results are inconclusive. Further large and high quality trials with more appropriate outcomes are warranted.
Plain language summary
Pacing for drug‐refractory or drug‐intolerant Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is a genetic disease with an autosomal‐dominant inheritance, which can cause obstruction in the left ventricle outflow tract. This obstruction can lead to a variety of symptoms like dyspnoea, chest pain, syncope and palpitations. The prevalence of HCM in the general population, as determined from echocardiographic studies in the United States, Japan, and China, has ranged from 0.16 to 0.29 percent. Treatment options for HCM ranges from drugs to surgery with each having its own limitations. Active cardiac pacing was suggested as a treatment option in some trials. We conducted this review to assess the available evidence on the effects of active pacing in drug‐refractory or drug‐intolerant HCM patients. Five studies (reported in 10 papers) were found to be relevant. However, three of the five studies provided un‐usable data. Thus data from only two studies (reported in seven papers) with 105 participants was included for this review. There was insufficient data to compare results on all‐cause mortality, cost effectiveness, exercise capacity, Quality of life and Peak O2 consumption. There was no difference in exercise capacity when comparing active pacing versus placebo pacing. However left ventricular outflow tract obstruction decreased significantly in the active pacing group compared to placebo. New York Heart Association functional class increased in the active pacing group compared to the placebo group and this was also observed when comparing active pacing versus trancoronary ablation of septal hypertrophy. Interpretation of these data needs to be cautious because existing data is derived from small trials at high risk of bias, which concentrate on physiological measures. Their results are inconclusive. Further large and high quality trials with more appropriate outcomes are warranted.
Background
Description of the condition
Hypertrophic cardiomyopathy (HCM) is a genetic disease with an autosomal‐dominant inheritance (Maron 1987a; Richardson 1996) resulting in sarcomere dysfunction (Watkins 1995). The prevalence of HCM in the general population, as determined from echocardiographic studies in the United States, Japan, and China, has ranged from 0.16 to 0.29 percent (Maron 1995; Maron 1999c; Hada 1987; Zou 2004). These observations suggest that HCM is present in approximately one in 350 to 625 individuals. HCM has been classified into three categories, based on the presence or absence of an intracavitary pressure gradient within a hypertrophied left ventricle (Maron 1987a; Richardson 1996):
non‐obstructive HCM, with no pressure gradient and thus no symptoms;
obstructive HCM, which is characterised by resting pressure gradient; and
latent HCM, which simulates obstructive HCM but is provoked only by manoeuvres.
Obstruction occurs when the anterior displacement of the anterior mitral leaflet through systole results in apposition of the hypertrophied papillary muscle and the hypertrophied left ventricle (LV) wall at the level of the mid‐left ventricle, producing two distinct left ventricle chambers (Falicov 1977; Fighali 1987). This mitral valve‐septal contact is responsible for the subaortic pressure gradient and the mitral regurgitation ( Maron 1987b; Panza 1992a; Panza 1992b; Pollick 1982). Systolic anterior motion (SAM) of the mitral valve is the most important determinant of the severity of left ventricle outflow obstruction (LVOT).
HCM can present in infancy and childhood, but more typically develops during the pubertal growth spurt (Maron 1986), and is often diagnosed during family screening (Maron 1999 a), although late onset disease may be also seen. A small proportion of patients with HCM eventually progress to an end stage characterised by reduced systolic performance and, in severe cases, left ventricular dilation and wall thinning (Harris 2006; Kubo 2007; Spirito 1987), owing mostly to myocardial ischemias due to microvascular dysfunction (Olivotto 2006). Typical symptoms include dyspnoea, chest pain, syncope and palpitations. The presence of severe symptoms in patients with HCM (defined as New York Heart Association (NYHA) class III or IV) (Table 1) is associated with worse outcomes ( Autore 2005; Maron 1999 a; Maron 2003; Takagi 1999). The major causes of death in HCM are sudden cardiac death, heart failure, and stroke (Maron 2000; Elliotte 2006). Factors that increase the likelihood of HCM‐related death include an embolic stroke, basal outflow obstruction > 30 mmHg and marked left ventricular hypertrophy > 25 mm.
1. Table: New York Heart Association Functional Classification.
| New York Heart AssociationFunctional Class | Symptoms |
| Class I | No limitation during ordinary activity |
| Class II | Slight limitation, as evidenced by shortness of breath nor fatigue or both during moderate exertion or stress |
| Class III | Marked limitation with minimal exertion that interferes with normal daily activity |
| Class IV | Inability to carry out any physical activity; patients typically have marked neurohumoral activation and muscle wasting |
Studies conducted in England (McKenna 1981; McKenna 1984; McKenna 1988) and in Italy (Romeo 1990) on symptomatic patients demonstrated that the annual mortality rate of HCM was approximately 2% in adults and 4% to 6% in children and adolescents.
Description of the intervention
A pacemaker is an electronic surgically implanted device that maintains regular heart rate by modifying cardiac output when it senses abnormal intracardiac potentials. It consists mainly of two parts: the pulse generator and the pacing lead(s). The pulse generator controls the pacing system and interprets the signals it receives back from the beating heart, while the pacing leads are thin, specially insulated wires that carry electrical impulses to the heart and return signals back from it to the pulse generator. A pacemaker usually requires little power and runs for several years by lithium batteries (Furman 1977; Levine 2002; Mond 1983).
Two types of pacemakers are currently available: single‐chamber pacemakers sense and pace either in the atrium or the ventricle, while dual chamber pacemakers (DDD) can sense and pace in both chambers (Hauser 1983). The atrial or ventricular output can be either inhibited or triggered in response to a sensed signal. Rate responsive pacemakers have one or more sensors that detect physical activity and adjust the pacing rate accordingly, which is necessary in patients with chronotropic incompetence (Bush 1994; Clarke 1991).
In 1987, the North American Society of Pacing and Electrophysiology (NASPE) and the British Pacing and Electrophysiology Group (BPEG) set up the NASPE/BPEG Generic Pacemaker Code (NBG Code), which they developed to describe different pacing modes (Bernstein 1987). Due to recent developments in technology this code has been updated (Bernstein 2002); see Table 2 for details. See Table 3 for a Glossary of Terms.
2. Table: Revised NBG Code for Pacing Modes.
| Chamber being paced | Chamber being sensed | Response to sensing | Rate modulation | Multisite pacing |
| O = none | O = none | O = none | O = none | O = none |
| A = atrium | A = atrium | I = inhibited | R = rate modulation | A = atrium |
| V = ventricle | V = ventricle | T = triggered | V = ventricle | |
| D = dual (A + V) | D = dual (A + V) | D = dual (T + I) | D = dual (A + V) | |
| Manufacturer's designation only: S = single (A or V) | Manufacturer's designation only: S = single (A or V) | |||
3. Table: Glossary.
| A | Atrium |
| AAI | Single‐chamber atrial pacing; one lead is positioned in the atrium; pacing and sensing occurs in the atrium; atrial pacing is inhibited by sensed spontaneous atrial depolarisation; no rate modulation or multi‐site pacing |
| AAIR | Single chamber atrial pacing as above but with rate modulation |
| AV synchrony | Normal sequence of atrial depolarisation and contraction followed by ventricular depolarisation and contraction; maintenance of this sequence results in optimal ventricular filling and cardiac output |
| BPEG | British Pacing and Electrophysiology Group |
| D | Dual (atrium and ventricle) |
| DDD | Dual‐chamber pacing; use of two leads, one in the atrium and one in the ventricle; pacing and sensing occurs in both the atrium and the ventricle; in the absence of intrinsic activity, both chambers are paced at the programmed base rate; normally inhibited by atrial or ventricular sensing and with ventricular pacing triggered by atrial sensing; no rate modulation or multi‐site pacing |
| DDDR | Dual chamber as above but with rate modulation |
| HCM | Hypertrophic cardiomyopathy |
| Inhibited | A type of pacemaker response in which the output pulse is suppressed (or inhibited) when an intrinsic event is sensed |
| NASPE | North American Society of Pacing and Electrophysiology |
| NBG Code | NASPE/BPEG Generic Code |
| Rate modulation | The ability of pacemakers to increase the pacing rate in response to physical activity or metabolic demand |
| Sensing | The detection of spontaneous cardiac depolarisation |
| Tracking | A dual‐chamber pacing function in which atrial activity is sensed and results in a paced ventricular response after a predefined delay (the AV interval) |
| VDD | Ventricular pacing, triggered by atrial sensing, inhibited by ventricular sensing, with no atrial pacing |
| VVI | Single‐chamber ventricular pacing; one lead is positioned in the ventricle; pacing and sensing occurs in the ventricle; ventricular pacing is inhibited by sensed spontaneous ventricular depolarisation; no rate modulation or multi‐site pacing; loss of AV synchrony may occur with this pacing mode; may be referred to as 'non‐physiological' pacing |
Pacemakers are not without adverse events. Reported complications are paroxysmal atrial fibrillation, infection, local irritation and electrode displacement (Gao 2007; Kappenberger 1997).
How the intervention might work
Several theories have been put forward to explain how dual‐chamber pacing with short atrioventricular (AV) delay reduces systolic anterior motion and subsequent left ventricle outflow obstruction:
Pre‐excitation of the right ventricle alters the dynamics and timing of ventricular contraction, ensuring left ventricle apical activation prior to septal activation (Betocchi 2002; Pak 1998). This may help by decreasing the excursion of the septal wall into the left ventricle outflow obstruction. The paradoxical (delayed) activation of the inter‐ventricular septum during dual‐chamber pacing could limit outflow tract narrowing by decreasing the projection of the ventricular septum into the outflow tract and its dynamic obstruction (Pak 1998).
The negative inotropic effect may play a role by decreasing the ejection acceleration and decreasing early forces on the mitral valve (Sherrid 1998).
Pacing activation of the right ventricular apex could produce early activation of the papillary muscles and chordae which could limit mitral valve leaflet excursion. Premature apical tensing of the mitral apparatus ‐ thus early tensing of the chordal apparatus of the mitral valve ‐ may possibly reduce systolic anterior motion by mitigating excess slack.
Why it is important to do this review
Many treatments are now available for HCM including drug therapy, septal ablation and septal myotomy. Unfortunately the evidence on the effectiveness of these interventions is limited. Furthermore, there are no systematic reviews evaluating the beneficial and harmful effect of pacing in HCM. Also, there is data which indicates how many patients with HCM get implanted with pacemakers.
Negative inotropes, including beta blockers (Fananapazir 1992; Thompson 1980), calcium channel blockers (Bonow 1985b; Rosing 1985), and disopyramide (Sherrid 2005) are the most widely used initial therapies, although the data supporting their use come from uncontrolled studies. Unfortunately there are little randomised controlled trials on the efficacy of any of these therapies. As a result, treatment strategies are based upon observational studies and clinical experience (Fifer 2008).
Septal ablation consists of infarction and thinning of the proximal interventricular septum via an infusion of ethanol through an angioplasty catheter. This procedure, however, can be complicated by complete heart block, electrocardiogram changes, right bundle branch block and ventricular arrhythmias (Boltwood 2004).
Septal myotomy, in which an extensive part of the cardiac septal muscle has to be excised to achieve clinical progress, is in the same instance a risk factor for ventricular septal deficit (Maron 2004; Siegman 1989; ten Berg 1994).
Due to the fact that many patients will continue having symptoms or develop complications despite maximal therapy, and because only limited data is available on the efficacy of the above mentioned interventions, alternative interventions have been sought in order to improve the patient's symptoms and probably the clinical endpoint.
Observational studies and small randomised trials have suggested symptomatic and functional benefits from pacing (Gadler 1997; Kappenberger 1997). The 2008 American College of Cardiology/American Heart Association/Heart Rhythm Society (ACC/AHA/HRS) guidelines recommended use of a pacemaker in patients with HCM for sinus node dysfunction or AV block (Epstein 2008). Permanent pacing may be considered in medically refractory symptomatic patients with HCM and significant resting or provoked left ventricular outflow tract obstruction.
Pacing, although not the primary treatment for HCM, could be beneficial to patients with relative or absolute contraindications to surgery or alcohol ablation, usually because of septum/mitral valve anatomy or co‐morbidities. This review is important because it summarises the best available evidence on the benefit and harm of pacing for drug‐refractory and drug‐intolerant HCM.
Objectives
To assess the available evidence on the effects of pacing in drug‐refractory or drug‐intolerant HCM patients.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomised controlled trials (RCTs) of either parallel group or crossover design that had assessed the beneficial and harmful effects of pacing for hypertrophic cardiomyopathy. We placed no restrictions on blinding, publication status, conference proceedings, or language. We excluded quasi‐randomised and observational studies.
Types of participants
We included children (defined as <18 years old) or adults (≥18 years old) of either sex with drug‐refractory or drug‐intolerant HCM, with or without other heart co‐morbidities.
Types of interventions
Considering at least three month treatment duration and irrespective of follow‐up period, we compared dual‐chamber pacing (DDD), dual‐chamber pacing with rate modulation (DDD‐R), or VDD with appropriate programming to:
placebo (minimum rate backup pacing AAI and VVI);
myotomy;
septal ablation (non surgical septal reduction therapy with or without alcohol ablation); or
another type of pacing (DDD, DDD‐R or VDD).
Types of outcome measures
Primary outcomes
Our primary outcomes were:
all‐cause mortality;
exercise capacity;
symptoms improvement as measured by improvement of: New York Heart Association functional class and/or exercise capacity (as measured by exercise duration or walking distance or both);
quality of life, as measured according to a recognised scale.
When different scales for measuring quality of life were used in different studies, we reported the number of statistically significant differences in quality of life as improved, not improved or worsened as reported by each trialist. Where several studies had used the same scale, we summarised the results together.
Secondary outcomes
Our secondary outcomes were:
left ventricle outflow obstruction gradient;
NYHA functional classification;
left ventricular wall thickness;
peak oxygen consumption;
complications related to the device implantation; and
cost‐effectiveness.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, 2010, Issue 1), MEDLINE 1950 to April 2010, EMBASE 1980 to April 2010, and Science Citation Index Expanded (1970 to April 2010). (Royle 2003) The search strategies used can be found in Appendix 1. No language or date restrictions were applied.
Searching other resources
We checked the bibliographic references of identified randomised clinical trials and meta‐analyses to find randomised clinical trials not identified by the electronic searches. We then approached the principal authors of the identified randomised clinical trials and enquired about any other randomised clinical trials they might know of. We looked for unpublished or ongoing studies by searching the metaRegister of controlled trials (including International Standard Randomised Controlled Trial Number Register (ISRCTN) and the National Institutes of Health (NIH) ‐ randomised trial records) at http://www.controlled-trials.com/.
Data collection and analysis
We performed the review and meta‐analyses following the recommendations of The Cochrane Collaboration (Higgins 2008). We performed the analyses using Review Manager 5.1 (RevMan 2011).
Selection of studies
We listed the identified trials and two authors (HA and KC) independently assessed their fulfilment of the inclusion criteria. We listed the excluded trials with the reason for exclusion. Disagreements were resolved by discussion. We summarised the flow of papers through the search and selection process using a QUOROM flow chart.
Data extraction and management
Two authors (MQ and HA) extracted data independently and resolved disagreements by discussion. A standardised data collection form was used to extract data on methods, participants, interventions, and outcomes. If more than one publication on a single randomised clinical trial was identified, the most appropriate data was extracted.
Assessment of risk of bias in included studies
We assessed methodological quality according to the level of confidence that the design and report of a published trial restricted bias in the intervention comparison (Moher 1998). In assessing the risk of bias we used The Cochrane Collaboration’s tool for assessing risk of bias as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008).
Measures of treatment effect
Dichotomous data
We calculated the relative risks with 95% confidence intervals (CI).
Continuous data
We calculated the mean differences with 95% CI.
In case the overall results were statistically significant by the random‐effects model, we calculated relative risk reduction (RRR), the number needed to treat (NNT) and the number needed to harm (NNH) if possible.
Unit of analysis issues
When we retrieved crossover studies in the search, we took only the first arm into consideration. This should reduce the possibility of a carryover effect of pacing on left ventricular wall thickness (Fananapazir 1994).
Dealing with missing data
We performed all analyses on an intention‐to‐treat basis, using the last reported observed response ('carry forward'), and including all participants, irrespective of compliance or follow up. In addition, we performed 'a worst scenario' analysis, considering all participants with missing data as treatment failures.
Assessment of heterogeneity
We aimed to assess statistical heterogeneity using a Chi2 test and used the I2 test to quantify inconsistency across included studies (Higgins 2003, Higgins 2008) and by examining the graphical presentations ('forest plot') (Egger 1997). We would use the random‐effects model to avoid the risk that the variability between the studies may be exclusively because of a random sampling variation around a fixed effect. Using the random‐effects model is also recommended by Clinical Evidence (Clinical Evidence).
Assessment of reporting biases
We tried to locate the protocol for each included randomised controlled trial (RCT). If the protocol was available, we compared its outcomes with those in the published RCT report. If it was not available, we compared the outcomes listed in the methods section of the report with the actual reported results.We had aimed to use a funnel plot (Egger 1997) of all included trials to check the presence of publication bias.
Data synthesis
We aimed to undertake meta‐analysis where there were sufficient data of suitable type, using RevMan 5.1 (RevMan 2011). In the event that there were too few clinically homogeneous trials for us to be able to perform a meta‐analysis, we presented a narrative synthesis. When we could not find relevant RCTs, we used non‐RCT studies in the discussion section.
Subgroup analysis and investigation of heterogeneity
We aimed to perform subgroup analyses according to whether participants are:
asymptomatic or symptomatic; and
children or adults.
Sensitivity analysis
We aimed to conduct sensitivity analyses to compare:
RCTs lasting three months with those lasting for more than three months;
low‐quality and high‐quality studies.
Results
Description of studies
Results of the search
A total of 206 papers were originally retrieved by searching the databases, of which 103 papers were judged to be clearly irrelevant. The abstracts of the remaining 103 papers were retrieved and of these, 91 were excluded as they did not meet one or more of the inclusion criteria. We extracted data of the 12 remaining papers. Six of those paper were originally in English, one in French, one in Czech, one in Chinese and three in German. Both the French paper (Gras 1995b) and the Czech paper (Krejci 2006) were excluded because they were not randomised. Eventually, we had 10 papers reporting five included studies; six of the 10 papers were reported the same study (Kappenberger 1997) including two that were exactly the same but with different German‐to‐English translated titles on different databases (Medline and Embase).
In the five included studies, 184 participants were recruited. Apart from (Gao 2007) which did not specify neither the male proportion nor the mean age, the male proportion in the other four studies was 59.6% and the range of mean age is (53‐69). Three studies were conducted in the USA (Maron 1999b; Mickelsen 2004; Nishimura 1997), one in Switzerland (Kappenberger 1997) and one in China (Gao 2007). Maron 1999b was funded in part by a grant from Medtronic, Inc. No information about funding were provided in the rest. Wash‐out periods were not determined in all four cross‐over studies (Kappenberger 1997; Maron 1999b; Mickelsen 2004; Nishimura 1997).
Please refer to the QUOROM flow chart (Figure 1).
1.
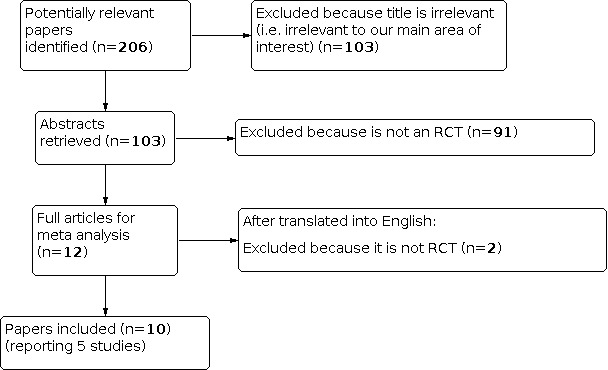
QUOROM flow chart.
See (Characteristics of included studies), and (Characteristics of excluded studies).
Included studies
Gao 2007 is a Chinese RCT (with an English abstract) of parallel design that recruited 23 participants aged > 60 years old. The Chinese full text was translated. It is the only study in this review that compared active pacing versus trancoronary ablation of septal hypertrophy.
Kappenberger 1997 is a multicenter RCT of cross‐over design done in Switzerland that recruited 82 patients. The study group classified patients into Group A when the acute study showed a peak gradient reduction of >30% after acute pacing was introduced or Group B if there was less or no gradient modification. Although it was mentioned in the study that patients were fully assessed after each phase of the study, data regarding the first phase was not provided. We contacted the authors in order to obtain the data but with no success. Luckily, the same group published another paper (Linde 1999) using the same patient group and considering only the first arm data in their analyses. Data on left ventricular outflow tract obstruction, exercise capacity and NYHA functional classification were taken from Linde 1999. Another paper (Kappenberger 1997b) was a meeting abstract for the same study published in different journal and was referenced to it. The other three papers (Meisel 1999, Miesel 2000a and Meisel 2000) referenced to Kappenberger 1997 were all in German and results in all these exactly match Kappenberger 1997. Meisel 2000 was cited twice for the same paper; one was in English and the other was the German translation and were found in different databases (Medline vs. Embase), where as Meisel 1999 was published in supplement 2 of the same journal a year before.
Maron 1999b conducted the M‐PATHY study that was a multicenter randomised, double‐blind, crossover study with 44 patients. The first six months of the study protocol used a randomised, crossover, double‐blind design where patients were randomised to either three months of DDD pacing or placebo pacing (AAI at 30bpm). Patients were crossed over to the alternative mode for the subsequent three month period. After six months, all patients were paced for six months in an uncontrolled and unblinded fashion. Clinical evaluation was performed at four intervals: baseline, after three months of either DDD pacing or AAI‐30 mode, at six months after the alternative mode, and at 12 months after six additional months of pacing. Although they evaluated their patients at the 4 aforementioned intervals, complete data was not provided in the full text. We contacted the author and the sponsoring company and they expressed that the data for the first arm is not obtainable at the time. This is unfortunate as this is one of the most important studies in this area and yet we can not analyse its data.
Mickelsen 2004 conducted a study of 11 patients that was different than the other included studies we have in our review in that they analysed the aortic flow in the descending aorta using Doppler, after they implanted the pacemaker in patients with medical refractory symptoms thought to be secondary to hypertrophic obstructive cardiomyopathy. Patients in this cross‐over RCT underwent three different types of pacing: placebo pacing (AAI set to 30 bpm), active DDD pacing with an AVinterval at 30 ms (DDD30), and active DDD pacing with the AV interval “optimised” using aortic Doppler echocardiography (DDDop). The optimisation means to select the AV interval that generated the maximal R‐N interval (QRS to notch) interval, where the notch is a sign of any sudden change in velocities which denotes obstruction. As per our protocol and in the case of a cross‐over design we considered only the first arm of the study. This study, however, did not present data separately, although they had done separate analysis after the first phase was completed. We contacted the author and unfortunately we have not heard from him yet.
Nishimura 1997 conducted an RCT with cross‐over design that recruited 21 patients and evaluated active pacing versus inactive pacing for patients with hypertrophic cardiomyopathy with severe symptoms unresponsive to medical therapy. After the cross‐over design was done there was no long follow up reported. Data about the first arm of this cross over study was not given, and even after contacting the author we have not received any response. .
Excluded studies
Out of 206 papers identified in the search, 103 papers were excluded early in the selection process because the title was irrelevant to our main area of interest. Ninety‐three papers of the remaining 103 were not randomised controlled trials. See (Characteristics of excluded studies).
Risk of bias in included studies
After assessing each of the five included studies individually by two of the authors, it was found that the methodological quality of the included studies in this review is inconsistent. Please see the characteristics of included studies tables (Characteristics of included studies). We used the ‘Risk of bias graph’ figure, which illustrates the proportion of studies with each of the judgements (‘Low risk’, ‘High risk’, ‘Unclear risk’ of bias) for each entry in the tool. Please refer to (Figure 2).
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All the five included studies were conducted using a random sequence generation, however, the methods for this aim were unclear in four of them (Gao 2007; Maron 1999b; Mickelsen 2004; Nishimura 1997) and therefore the risk of selection bias was unable to be determined. Kappenberger 1997 did mention using central randomisation to define the sequence generation and that allocation was concealed.
Blinding
Three of the included studies (Kappenberger 1997, Maron 1999b, Nishimura 1997) conducted a double‐blinded study and therefore they were classified as low risk for having performance or detection bias. One of the studies, Mickelsen 2004, conducted a single blinded study and Gao 2007, did not give any information regarding whether blinding was considered or not.
Incomplete outcome data
Fortunately, incomplete outcome data were completely reported in four of the five included studies, and therefore would be considered as low‐risk studies for attrition bias:
In Gao 2007: it was noted that two patients dropped out from the treatment group and that was clearly reported.
In Kappenberger 1997: Of the 83 participants, 81 completed the first phase of the cross over and two dropped out; three of the placebo group patients were shifted to the second arm earlier than the first 12‐week period. Data from all drop‐outs were clearly reported.
In Maron 1999b: Of the 44 participants, 12 failed to complete the protocol design; three in the second phase which is beyond the inclusion criteria of our review (taking only the first arm) and nine in the first phase (one after randomisation and eight reprogrammed early from placebo to treatment group). These incomplete data were clearly reported.
In Nishimura 1997: Of the 21 participants, One patient was excluded from the study in the first phase (from the treatment group) due to his severe symptoms and underwent myotomy. Another did not show for follow up. All these data were reported clearly.
Only in one study, Mickelsen 2004, there were no information regarding the incomplete outcome data and therefore its bias risk will be considered unclear.
Selective reporting
There was no selective reporting of outcomes, time‐points or subgroup analyses in three of the five included studies (Gao 2007; Kappenberger 1997; Maron 1999b).
Other potential sources of bias
In Kappenberger 1997 the p value of most of the parameters in the inactive pacing group were not specified making it hard to know if the effect was statically significant or not.
In Gao 2007 we noticed that the numbers about the outcomes from the table provided in the study differs significantly from the numbers provided in the English abstract.
Effects of interventions
All‐cause mortality
The description of all‐cause mortality was insufficient in all trials. None of the trials included has reported mortality among participants.
Exercise capacity
Only Kappenberger 1997 reported on exercise capacity; no data could be extracted from the other included trials on this outcome as the data from the two cross‐over phases was combined and we could not take the data regarding the first phase only. The authors were contacted to retrieve the data on the first phase only, but no additional data was provided.
Kappenberger 1997 reported on exercise capacity; exercise time has decreased from (13.1 ± 4.4) minutes to (12.6 ± 4.3) minutes. It was increased significantly from (12.1 ± 5.6) minutes to (12.9 ± 4.2) minutes at the end of the first phase in the treatment group (MD 0.30; 95% CI ‐1.55 to 2.15).
Symptoms improvement:
As measured by improvement of the NYHA functional class and/or exercise capacity (as measured by exercise duration or walking distance or both); both Gao 2007 and Kappenberger 1997 reported on symptoms improvements per protocol; no data could be extracted from the other included trials on this outcome as the data from the two cross‐over phases was combined and we could not take the data regarding the first phase only. The authors were contacted to retrieve the data on the first phase only, but no additional data was provided.
Gao 2007 reported that NYHA functional class improved from (3.2 ± 0.7) to (1.5 ± 0.5) and from (3.0 ± 0.1) to (1.9 ± 0.6) post transcoronary ablation of septal hypertrophy (TASH) and dual‐chamber cardiac pacing (PM), respectively versus baseline.
Of note, this study also used a general symptomatic score which was decreased from (5.9 ± 1.6) to (1.8 ± 0.7) and from (4.5 ± 1.3) to (2.3 ± 1.6) post TASH and PM, respectively versus baseline.
Kappenberger 1997 reported that NYHA functional class has dropped from (2.5 ± 0.5) at the baseline to (2.2 ± 0.6) and from (2.6 ± 0.5) at the baseline to (1.7 ± 0.7) at the end of the first phase in the placebo versus the treatment group, respectively.
Quality of life
Only one trial (Kappenberger 1997) reported on quality of life; no data could be extracted from the other included trials on this outcome as the data from the two cross‐over phases was combined and we could not take the data regarding the first phase only. The authors were contacted to retrieve the data on the first phase only, but no additional data was provided.
Kappenberger 1997 evaluated quality of life using the Karolinska questionnaire as per‐protocol. General quality‐of‐life questions concerned physical functioning, such as the ability to be self autonomous, that is, walking a few hundred meters on level ground, and the capacity for more strenuous physical activity, such as lifting heavy objects; social, sexual, and cognitive functioning; alertness; sleep; self‐perceived health; and emotional state. There were 16 questions on symptoms, and two questions regarding self‐perceived health status. The results were added into averages. A percentage assessment for quality‐of‐life parameters was chosen in the presentation of results, because the scales differ for the various dimensions.
In the placebo group, there was a statistically significant improvement from the baseline in the following measures: Alertness, Chest pain, Dyspnea, Dizziness, Palpitations, Cognitive functioning, Quality of sleep, Self‐autonomy, Strenuous activity, Social functioning, Self‐perceived restriction in health, Self‐perceived health, Depression score. There were no significant percentage differences (6, 29, 20, 27, 35, 27, 28, 7, 3, 8, 16, 7, 19, respectively). However there was a statistically significant worsening from the base line in sexual functioning with a percentage difference of (‐3).
In the treatment group, there was a statistically significant improvement from the baseline in the following measures: Alertness, Chest pain, Dyspnea, Dizziness, Palpitations, Quality of sleep, Self‐autonomy, Strenuous activity, Sexual functioning, Social functioning, Self‐perceived restriction in health, Self‐perceived health, Depression score. There were no significant percentage differences (19, 43, 30, 35, 40, 15, 29, 17, 7, 18, 32, 18, 17, respectively). However there was a statistically significant worsening from the base line only in cognitive functioning with a percentage difference of (‐7).
Left ventricle outflow obstruction gradient
Only two trials (Gao 2007 and Kappenberger 1997) reported on left ventricle outflow obstruction gradient per‐protocol. None of the other included trials reported outcome on the first cross‐over phase as per‐protocol as the data from the two cross‐over phases was combined. The author were contacted to retrieve the data on the first phase only, but no additional data was provided.
Gao 2007 reported that the decrease of left ventricular out flow pressure gradient was (80.0 ± 35.5) mmHg (1 mmHg =0.1333 kPa) and (49.3 ± 37.7) mmHg post transcoronary ablation of septal hypertrophy (TASH) and dual‐chamber cardiac pacing (PM) treatments respectively versus baseline (MD ‐30.70; 95% CI ‐62.41 to 1.01).
Kappenberger 1997 reported that left ventricular outflow obstruction dropped from (71 ± 32) mmHg at the baseline to (52 ± 34) mmHg, and from (70 ± 24) mmHg at the baseline to (33 ± 27) mmHg at the end of the first phase in the placebo versus the treatment group, respectively; this difference was not significant (MD ‐19.00; 95% CI ‐32.39 to ‐5.61).
New York Heart Association Functional Classification
Only two trials (Gao 2007 and Kappenberger 1997) reported on NYHA functional classification per‐protocol. None of the other included trials reported outcome on the first cross‐over phase as per‐protocol as the data from the two cross‐over phases was combined. The authors were contacted to retrieve the data on the first phase only, but no additional data was provided.
Gao 2007, and as mentioned above in symptoms Improvement, reported that NYHA class was improved from (3.2 ± 0.7) to (1.5 ± 0.5) and from (3.0 ± 0.1) to (1.9 ± 0.6) post transcoronary ablation of septal hypertrophy (TASH) and dual‐chamber cardiac pacing (PM), respectively versus baseline. Effect difference among the two treatment arms was not significant (MD ‐0.50; 95% CI ‐1.05 to 0.05).
Kappenberger 1997, and as mentioned above in symptoms Improvement, reported that NYHA functional class was dropped from (2.5 ± 0.5) at the baseline to (2.2 ± 0.6), and from (2.6 ± 0.5) at the baseline to (1.7 ± 0.7) at the end of the first phase in the placebo versus the treatment group, respectively. Active pacing significantly improved NYHA functional classification significantly compared with placebo pacing (MD ‐0.50; 95% CI ‐0.78 to ‐0.22).
Left ventricular wall thickness
Only one trial (Gao 2007) reported on left ventricular wall thickness per‐protocol. Gao 2007 reported that interventricular wall thickness was significantly reduced post transcoronary ablation of septal hypertrophy (TASH) [(22 ± 4) mm versus (17 ± 3) mm] and remained unchanged in dual‐chamber cardiac pacing (PM) group. Effect difference among the two treatment arms was not significant (MD 0.60; 95% CI ‐5.65 to 6.85).
Peak oxygen consumption
Only one trial (Kappenberger 1997) reported on Peak oxygen consumption per‐protocol. None of the other included trials reported outcome on the first cross‐over phase as per‐protocol as the data from the two cross‐over phases was combined. The authors were contacted to retrieve the data on the first phase only, but no additional data was provided.
Kappenberger 1997 reported that peak oxygen uptake, measured by ml/kg/min, decreased from (19.9 ± 5.7) to (18.2 ± 5.0) in the placebo group where increased from (17.1 ± 5.6) to (18.7 ± 5.5) in the treatment group, both at the end of the first phase .
Complications related to the device implantation
Only two trials (Gao 2007 and Kappenberger 1997) reported on complications related to the device implantation per‐protocol. Gao 2007 reported three patients with paroxysmal atrial fibrillation (two patients in TASH group and one patient in PM group) developed chronic atrial fibrillation during the follow‐up. Kappenberger 1997 mentioned that 30 reported adverse events were related to the pacemaker treatment: infection and local irritation (no=8) or electrode displacement (seven atrial and three ventricular). Despite these problems, correct pacemaker function was finally achieved in all patients. No other minor event was related to pacing; one patient was operated on during cross over phase for failure of therapy.
Cost effectiveness
None of the included trials considered cost effectiveness as one of the outcome measures.
Discussion
Summary of main results
There was no significant difference between the five studies in terms of pacing mode and patient population. All studies enrolled adult patients (>18) who were diagnosed with HOCM that was refractory to medical treatment or were not tolerating the medical treatment. Four of the studies used the cross‐over design (Kappenberger 1997; Maron 1999b; Mickelsen 2004; Nishimura 1997) and only Gao 2007 used the parallel design. The pacing mode used in the treatment group in all studies was DDD pacing and the inactive pacing was AAI pacing. Gao 2007 was the only study that compared DDD pacing to TASH. In general (except Gao 2007), all studies reported on exercise capacity and quality of life. All studies reported on NYHA functional class. We were unable to use data from 3 studies because the authors had not provided data in the first arm of the study (Maron 1999b; Mickelsen 2004; Nishimura 1997). Moreover, there was insufficient data to compare results on all‐cause mortality, cost effectiveness, quality of life and Peak O2 consumption. Thus, the data for this systematic review based on two small studies, one of which had high risk of bias.
The only study whose data can be used on the exercise capacity time was Kappenberger 1997 who reported that the exercise time has decreased from (13.1 ± 4.4) min to (12.6 ± 4.3) min in the placebo group and has increased from (12.1 ± 5.6) min to (12.9 ± 4.2) min in the treatment group (MD 0.30; 95% CI ‐1.55 to 2.15). Similarily, there was only one study (Gao 2007) whose data could be used on Left ventricular thickness which reported that the Left ventricular thickness remained unchanged in the active pacing group (MD 0.60; 95% CI ‐5.65 to 6.85). Kappenberger 1997 was able to identify worsening scores of sexual and cognitive functioning in the intervention groups compared with the placebo groups.
Overall completeness and applicability of evidence
The main limitation was the unavailability of the first phase data in three of the five included studies (Maron 1999b; Mickelsen 2004; Nishimura 1997). We attempted to obtain the data by writing to the authors, but none was forthcoming.Thus, we await these data in order to have more complete evidence. Meanwhile we cannot comment on the applicability of any evidence.
Quality of the evidence
Of the five included studies we used data from two studies (Gao 2007; Kappenberger 1997) one of which was a high‐quality studies Kappenberger 1997. Between these two studies we have 105 patients.
Potential biases in the review process
The quantity and quality of available evidence limited our findings and interpretations. Only five trials total were included in this review, three of which provided unusable data due to restrictions in our protocol regarding the cross‐over trials where we only took the first arm into consideration.
Only one of the five included studies reported on the method used in randomization and concealment (Kappenberger 1997), while all the other four only reported that the study was randomized with out specifying the method used; this can increase the selection bias in the included studies.
Moreover, none of the trials included in this review reported on patients mortality. One might argue that RCTs with longer follow‐up periods are required to confirm a beneficial effect of active pacing in hypertrophic cardiomyopathy.
Agreements and disagreements with other studies or reviews
Guidelines regarding the management of HCM have been issued by the American College of Cardiology and the European Society of Cardiology (Clinical Practice Guideline 2003; Clinical Practice Guidline 2003b). It is recommended that pharmacologic therapy is the first‐line approach to relief the symptoms of HOCM. Beta‐blockers are generally the initial choice. In case of refractory symptoms despite maximal medical treatment or in case of drug‐intolerant, other invasive therapies might be considered. These interventions consist of surgical septal myectomy, dual‐chamber pacing, and catheter‐based alcohol septal ablation. Surgical septal myotomy is usually considered to be the gold standard for treatment of HOCM. Dual‐chamber pacing is limited to patients who have coexisting illnesses that are contraindications to other therapies or those who require pacing for bradycardia (Nishimura 2004b).The evidence collected in this review shows no convincing evidence to support or refute the use of active pacing in patients with hypertrophic cardiomyopathy.
Authors' conclusions
Implications for practice.
The evidence collected in this review shows no convincing evidence to support or refute the use of active pacing in patients with HCM. Though, active pacing may decrease both the left ventricular wall thickness and the left ventricular outflow obstruction the evidence is based on small trial numbers and is thus incomplete.
Implications for research.
Adequately powered and long‐term conducted RCTs with low risk of bias are needed to support or change the current results and knowledge of the effects active pacing in HCM. We advise authors who are conducting an RCT with a cross‐over design to report the data after each phase so that data can be meaningfully interpreted. We feel that much data is missing in this area because only combined data from both phases were reported.
What's new
| Date | Event | Description |
|---|---|---|
| 26 March 2021 | Review declared as stable | This review was assessed in March 2021 as being not a clinical priority question and not an active area of research. |
History
Protocol first published: Issue 5, 2010 Review first published: Issue 5, 2012
Acknowledgements
We would like to thank Dr Joey Kwong, Managing Editor of the Cochrane Heart Group and Claire Williams, Assistant Managing Editor, for their great support during the whole process. We would also like to thank Nicole Ackermann, Trials Search Co‐ordinator, for her help in developing the search strategy.
For their great help in translating the non‐English studies included in this review, we thank Sarah Haley (helped with the German and French studies), Dr Joey Kwong (helped with the Chinese study) and Josef Pleticha (helped with the Czech study).
Appendices
Appendix 1. Search strategies
Database searched: CENTRAL (The Cochrane Library 2010, Issue 1)
Date of search: 14/4/2010
#1 MeSH descriptor Cardiomyopathy, Hypertrophic explode all trees
#2 (cardiomyopath* in All Text near/3 hypertroph* in All Text)
#3 HCM in All Text
#4 HOCM in All Text
#5 (#1 or #2 or #3 or #4)
#6 MeSH descriptor Pacemaker, Artificial this term only
#7 MeSH descriptor Cardiac Pacing, Artificial this term only
#8 pacemaker* in All Text
#9 pacing in All Text
#10 pacer* in All Text
#11 (#6 or #7 or #8 or #9 or #10)
#12 (#5 and #11)
Database searched: MEDLINE OVID (1950 onwards)
Date of search: 14/4/2010
1. exp Cardiomyopathy, Hypertrophic/
2. (hypertrophic adj3 cardiomyopath*).tw.
3. hcm.tw.
4. hocm.tw.
5. 1 or 2 or 3 or 4
6. Cardiac Pacing, Artificial/
7. Pacemaker, Artificial/
8. pacemaker*.tw.
9. pacing.tw.
10. pacer*.tw.
11. 6 or 7 or 8 or 9 or 10
12. 5 and 11
13. randomized controlled trial.pt.
14. controlled clinical trial.pt.
15. randomized.ab.
16. placebo.ab.
17. drug therapy.fs.
18. randomly.ab.
19. trial.ab.
20. groups.ab.
21. 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20
22. exp animals/ not humans.sh.
23. 21 not 22
24. 12 and 23
Database searched: EMBASE OVID (1980 onwards)
Date of search: 14/4/2010
1. exp hypertrophic cardiomyopathy/
2. (hypertrophic adj3 cardiomyopath*).tw.
3. hcm.tw.
4. hocm.tw.
5. 1 or 2 or 3 or 4
6. exp heart pacing/
7. artificial heart pacemaker/
8. pacemaker*.tw.
9. pacing.tw.
10. pacer*.tw.
11. 6 or 7 or 8 or 9 or 10
12. 5 and 11
13. random$.tw.
14. factorial$.tw.
15. crossover$.tw.
16. cross over$.tw.
17. cross‐over$.tw.
18. placebo$.tw.
19. (doubl$ adj blind$).tw.
20. (singl$ adj blind$).tw.
21. assign$.tw.
22. allocat$.tw.
23. volunteer$.tw.
24. crossover procedure/
25. double blind procedure/
26. randomized controlled trial/
27. single blind procedure/
28. 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27
29. (animal/ or nonhuman/) not human/
30. 28 not 29
31. 12 and 30
Database searched: ISI Web of Science – with Conference Proceedings (1970 onwards)
Date of search: 14/4/2010
#9 #8 AND #7 AND #3
#8 TS=(random* OR blind* OR placebo*)
#7 #6 OR #5 OR #4
#6 TS=pacer*
#5 TS=pacing
#4 TS=pacemaker*
#3 #2 OR #1
#2 TS=(hcm OR hocm)
#1 TS=(hypertrophic SAME cardiomyopath*)
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Gao 2007.
| Study characteristics | ||
| Methods | RCT with parallel design | |
| Participants | 23 participants (15 as treatment group and 8 as a comparison group), Adults (> 18) | |
| Interventions | Intervention: Transcoronary ablation of septal hypertrophy Control: Dual Chamber cardiac pacing |
|
| Outcomes | Ssymptoms improvement (NYHA classification, CCS classification) left ventricle outflow obstruction gradient (pressure gradient) New York Heart Association Functional Classification left ventricular wall thickness. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors mentioned that the patients "were randomised." |
| Allocation concealment (selection bias) | Unclear risk | No information given |
| Blinding (performance bias and detection bias) Self‐reported outcomes | Unclear risk | No information given |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | No information given |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 drop‐outs in the treatment group, clearly reported |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | No other bias could be found |
Kappenberger 1997.
| Study characteristics | ||
| Methods | RCT with crossover design | |
| Participants | 82 participants (41 as treatment group and 41 as a comparison group), Adults (> 18) | |
| Interventions | intervention: DDD pacing Control: Placebo (AAI) |
|
| Outcomes | exercise capacity (walking) symptoms improvement (Clinical hx and quality of life questionnaire) quality of life (karolinska) left ventricle outflow obstruction gradient New York Heart Association Functional Classification complications related to the device implantation (irritation, infection, electrodes displacement) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified by central randomisation |
| Allocation concealment (selection bias) | Low risk | Central randomisation |
| Blinding (performance bias and detection bias) Self‐reported outcomes | Low risk | Double blind |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Double blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of the 83 patients, 82 completed the first phase of the cross over, however, three of the placebo patients were shifted to the second arm earlier than the first 12‐week period. They were clearly reported |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | No other bias could be found |
Maron 1999b.
| Study characteristics | ||
| Methods | RCT with crossover design | |
| Participants | 44 participants (No info available on how many patients in the treatment and the comparison group), Adults (> 18) | |
| Interventions | Intervention: DDD pacing Control: Placebo (AAI) |
|
| Outcomes | Left ventricle wall thickness exercise time (Chrono‐tropic Assessment Exercise Protocol) quality of life (Minnesota Living with Heart Failure Questionnaire) oxygen consumption left ventricle outflow obstruction gradient New York Heart Association Functional Classification complications related to the device implantation (pocket site infections, generator migration,lead dislodgement, fracture or malfunction). |
|
| Notes | Its data is unusable for this review. Author was contacted and he could not provide us with the data needed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The first 6 months of the study protocol used a randomised, crossover, double‐blind design |
| Allocation concealment (selection bias) | Unclear risk | No information given |
| Blinding (performance bias and detection bias) Self‐reported outcomes | Low risk | Double blind |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Double blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12 patient failed to complete the protocol design: 9 in the first phase ( one after randomisation and 8 reprogrammed early from placebo to treatment group). Clearly reported |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | No other bias could be found |
Mickelsen 2004.
| Study characteristics | ||
| Methods | RCT with crossover design | |
| Participants | 11 participants (No info available on how many patients in the treatment and the comparison group), Adults (> 18) | |
| Interventions | Intervention: DDDwith anAVinterval at 30 ms (DDD30), and DDD with the AV interval “optimised” using aortic Doppler echocardiography (DDDop) Control: Placebo (AAI) |
|
| Outcomes | Exercise time (treadmill) quality of life (SF‐36) left ventricle outflow obstruction gradient. |
|
| Notes | Its data is unusable for this review. Author was contacted and there was no reply. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomised single‐blinded crossover trial |
| Allocation concealment (selection bias) | Unclear risk | No information given |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Single blinded |
| Blinding (performance bias and detection bias) Objective outcomes | High risk | Single blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information given the study |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | No other bias could be found |
Nishimura 1997.
| Study characteristics | ||
| Methods | RCT with crossover design | |
| Participants | 21 participants (9 as treatment group and 11 as a comparison group), Adults (> 18) | |
| Interventions | Intervention: DDD pacing Control: Placebo (AAI) |
|
| Outcomes | Exercise capacity (treadmill) symptoms improvement (Subjective as improved, no change, deteriorate) quality of life (Minnesota) left ventricle outflow obstruction gradient New York Heart Association Functional Classification peak oxygen consumption. |
|
| Notes | Its data is unusable for this review. Author was contacted and there was no reply. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised |
| Allocation concealment (selection bias) | Unclear risk | No information given |
| Blinding (performance bias and detection bias) Self‐reported outcomes | Low risk | Double blind |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Double blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One patient was excluded from the study (from the treatment group) due to his severe symptoms and underwent myotomy Another did not show for follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | No other bias could be found |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agarwal 2010 | Irelevant title (title is not related to our main area of interest). |
| Aizawa 1993 | Irelevant title (title is not related to our main area of interest). |
| Alam 2006 | Irelevant title (title is not related to our main area of interest). |
| Alam 2009 | Irelevant title (title is not related to our main area of interest). |
| Alfonso1996 | Irelevant title (title is not related to our main area of interest). |
| Anderson 1983 | Irelevant title (title is not related to our main area of interest). |
| Badie 2009 | Irelevant title (title is not related to our main area of interest). |
| Begley 2001 | not RCT, everyone got paced |
| Bellon 1995 | Irelevant title (title is not related to our main area of interest). |
| Ben 2000 | not RCT |
| Betocchi 1988 | Irelevant title (title is not related to our main area of interest). |
| Betocchi 1996 | Irelevant title (title is not related to our main area of interest). |
| Betocchi 2002 | no randomisation |
| Bhatia 2004 | not RCT |
| Binder 2008 | not RCT |
| Birnie 2006 | Irelevant title (title is not related to our main area of interest). |
| Bonow 1985 | Irelevant title (title is not related to our main area of interest). |
| Braunschweig 2000 | not RCT |
| Braunwald 1997 | Irelevant title (title is not related to our main area of interest). |
| Brignole 1988 | Irelevant title (title is not related to our main area of interest). |
| Brill 1985 | Irelevant title (title is not related to our main area of interest). |
| Bryce 2001 | not RCT |
| Can 2009 | Irelevant title (title is not related to our main area of interest). |
| Cannon 1985 | Irelevant title (title is not related to our main area of interest). |
| Cannon 1987 a | Irelevant title (title is not related to our main area of interest). |
| Cannon 1987 b | not RCT |
| Cannon 1990 | Irelevant title (title is not related to our main area of interest). |
| Capezzuto 2000 | not RCT |
| Cesario 2006 | not RCT |
| Chen 2007 | not RCT |
| Ciaramitaro 2006 | Irelevant title (title is not related to our main area of interest). |
| Coats 2008 | not RCT |
| Cregg 1999 | Irelevant title (title is not related to our main area of interest). |
| da Fonseca 2007 | Irelevant title (title is not related to our main area of interest). |
| Daley 1987 | not RCT |
| Daubert 2004 | not RCT |
| Deharo 2000 | not RCT |
| Dimitrow 2000 | no randomization |
| Dimitrow 2002 | Irelevant title (title is not related to our main area of interest). |
| Dimitrow 2004 | not randomized |
| Duarte 1999 | not RCT |
| El 2007 | Irelevant title (title is not related to our main area of interest). |
| El 2008 | Irelevant title (title is not related to our main area of interest). |
| Faber 2007 a | Irelevant title (title is not related to our main area of interest). |
| Faber 2007 b | Irelevant title (title is not related to our main area of interest). |
| Fananapazir 1991 | not randomised |
| Fananapazir 1998 | not RCT |
| Fei 2001 | not RCT |
| Ferguson 1997 | not RCT |
| Fernandes 2005 | Irelevant title (title is not related to our main area of interest). |
| Finsterer 2010 | Irelevant title (title is not related to our main area of interest). |
| Frank 1978 | not randomised |
| Frank 1983 | Irelevant title (title is not related to our main area of interest). |
| Freedman 2001 | not RCT |
| Gadler 1997 | a follow up study, not RCT |
| Gadler 1999 | not randomized |
| Gadler 1999b | not controlled |
| Gadler 2001 | not RCT |
| Gietzen 2004 | review |
| Gietzen 2005 | review |
| Gilligan 2000 | review |
| Goethals 1999 | review |
| Gold 1999 | Irelevant title (title is not related to our main area of interest). |
| Gold 2001 | not RCT |
| Goodwin 1989 | not RCT |
| Gras 1995 | not RCT |
| Gras 1995b | cohort study |
| Gras 1995c | not RCT |
| Gregoratos 1999 | not RCT |
| Hagege 2009 | not RCT |
| Harrison 1976 | Irelevant title (title is not related to our main area of interest). |
| Haruki 2010 | a case report |
| Hauer 2001 | not RCT |
| Hauer 2001b | not RCT |
| Hayes 1999 | not RCT |
| Hayes 2004a | not RCT |
| Hayes 2004b | not RCT |
| Herold 1991 | Irelevant title (title is not related to our main area of interest). |
| Hess 1982 | Irelevant title (title is not related to our main area of interest). |
| Hilleman 2001 | Irelevant title (title is not related to our main area of interest). |
| Honda 2005 | not RCT |
| Itoh 1988 | Irelevant title (title is not related to our main area of interest). |
| Izawa 1996 | Irelevant title (title is not related to our main area of interest). |
| Izawa 1997 | Irelevant title (title is not related to our main area of interest). |
| Jandik 1990 | Irelevant title (title is not related to our main area of interest). |
| Jansson 1990 | Irelevant title (title is not related to our main area of interest). |
| Jeserich 2001 a | Irelevant title (title is not related to our main area of interest). |
| Jeserich 2001 b | Irelevant title (title is not related to our main area of interest). |
| Juliard 1987 | Irelevant title (title is not related to our main area of interest). |
| Kaik 1992 | Irelevant title (title is not related to our main area of interest). |
| Kappenberger 1997c | not an RCT |
| Kappenberger 1999 | f/u and not RCT |
| Kass 1999 | Irelevant title (title is not related to our main area of interest). |
| Kido 2006 | Irelevant title (title is not related to our main area of interest). |
| Kim 1987 | Irelevant title (title is not related to our main area of interest). |
| Kovacic 2003 | Irelevant title (title is not related to our main area of interest). |
| Krejci 2006 | not randomised |
| Kuck 1987 a | not RCT |
| Kuck 1987 b | Irelevant title (title is not related to our main area of interest). |
| Kuck 1988 | not RCT |
| Kuhn 1999 | Irelevant title (title is not related to our main area of interest). |
| Kuhn 2000 | Irelevant title (title is not related to our main area of interest). |
| Kuhn 2001 | not RCT |
| Kukar 2006 | not RCT |
| Kusumoto 2002 | Irelevant title (title is not related to our main area of interest). |
| Kusumoto 2006 | Irelevant title (title is not related to our main area of interest). |
| Lakkis 1998 | not RCT |
| Lakkis 2000 | not RCT |
| Lakkis 2001 | not RCT |
| Landmark 1982 | not RCT |
| Lerakis 1997 | Irelevant title (title is not related to our main area of interest). |
| Lerakis 2001 | not RCT |
| Lo 1987 | Irelevant title (title is not related to our main area of interest). |
| Lopez 2002 | not RCT |
| Losi 1998 | not controlled |
| Maron 1995 | not RCT |
| Maron 1998 | not an RCT |
| Martin 1996 | not RCT |
| McKenna 2009 | not RCT |
| McNamara 1983 | Irelevant title (title is not related to our main area of interest). |
| Megevand 2005 | not RCT |
| Meisel 2001 | not RCT |
| Merrill 2000 | Irelevant title (title is not related to our main area of interest). |
| Milic 2005 | Irelevant title (title is not related to our main area of interest). |
| Millaire 1995 a | Irelevant title (title is not related to our main area of interest). |
| Millaire 1995 b | Irelevant title (title is not related to our main area of interest). |
| Millaire 1998 | Irelevant title (title is not related to our main area of interest). |
| Miyajima 1988 | Irelevant title (title is not related to our main area of interest). |
| Mohiddin 2002 | not an RCT |
| Mohiddin 2010 | not RCT |
| Monakier 2004 | Irelevant title (title is not related to our main area of interest). |
| Montijano Cabrera 2001 | not RCT |
| Naccarelli 1982 | Irelevant title (title is not related to our main area of interest). |
| Nagueh 2001 | Irelevant title (title is not related to our main area of interest). |
| Nakatani 1996 | Irelevant title (title is not related to our main area of interest). |
| Nandhakumar 2008 | Irelevant title (title is not related to our main area of interest). |
| Nessler 1999 | Irelevant title (title is not related to our main area of interest). |
| Niki 1999 | Irelevant title (title is not related to our main area of interest). |
| Nishimura 1993 | not RCT |
| Nishimura 1996 | not RCT |
| Nishimura 1996b | not RCT |
| Nishimura 2004 | not RCT |
| Nowinski 2005 | no randomization |
| Ohtani 2003 | case report |
| Oka 2007 | Irelevant title (title is not related to our main area of interest). |
| Ommen 1999 | not randomised, based on patient preference |
| Ovsyshcher 2004 | Irelevant title (title is not related to our main area of interest). |
| Pace 1994 | Irelevant title (title is not related to our main area of interest). |
| Pak 1998 | not RCT |
| Park 1999 | not RCT |
| Pasternac 1982 | Irelevant title (title is not related to our main area of interest). |
| Paulus 1988 | Irelevant title (title is not related to our main area of interest). |
| Posma 1996 | not RCT |
| Ralph‐Edwards 2005 | Irelevant title (title is not related to our main area of interest). |
| Reith 2003 | not RCT |
| Rousseau 1980 | Irelevant title (title is not related to our main area of interest). |
| Ryden 2001 | Irelevant title (title is not related to our main area of interest). |
| Saumarez 1992 | not randomised |
| Saumarez 1995 | Irelevant title (title is not related to our main area of interest). |
| Saumarez 2003 | Irelevant title (title is not related to our main area of interest). |
| Saumarez 2008 | not randomised |
| Schulte 1999 | not RCT |
| Seggewiss 1998 | Irelevant title (title is not related to our main area of interest). |
| Seggewiss 2003 | not RCT |
| Seggewiss 2007 | Irelevant title (title is not related to our main area of interest). |
| Shamim 2002 | not RCT |
| Shefer 1987 | Irelevant title (title is not related to our main area of interest). |
| Sherrid 2005 | Irelevant title (title is not related to our main area of interest). |
| Silva 2008 | no comparison group. |
| Slade 1996 | not RCT |
| Slade 1996b | not RCT |
| Solomon 1999 | not RCT |
| Somura 2001 | Irelevant title (title is not related to our main area of interest). |
| Sorajja 2000 | not RCT |
| Spirito 1997 | not RCT |
| Spirito 1999 | not RCT |
| Sud 2007 | Irelevant title (title is not related to our main area of interest). |
| Syed 2004 | Irelevant title (title is not related to our main area of interest). |
| Takechi 2003 | Irelevant title (title is not related to our main area of interest). |
| Talreja 2004 | Irelevant title (title is not related to our main area of interest). |
| Tascon 1995 | Irelevant title (title is not related to our main area of interest). |
| Thompson 1980 | Irelevant title (title is not related to our main area of interest). |
| Thompson 1983 | Irelevant title (title is not related to our main area of interest). |
| Topaz 1989 | Irelevant title (title is not related to our main area of interest). |
| Topilski 2006 | not RCT |
| Trohman 2004 | not RCT |
| Unno 2009 | Irelevant title (title is not related to our main area of interest). |
| van der 2005 | not a pacing study |
| Vazquez 2001 | Irelevant title (title is not related to our main area of interest). |
| Venugopa 2007 | Irelevant title (title is not related to our main area of interest). |
| Watson 1987 | Irelevant title (title is not related to our main area of interest). |
| Weiner 1999 | not RCT |
| Weiss 1976 | Irelevant title (title is not related to our main area of interest). |
| Wexler 2009 | Irelevant title (title is not related to our main area of interest). |
| Yamakado 1990 | Irelevant title (title is not related to our main area of interest). |
| Zeng 2006 | Irelevant title (title is not related to our main area of interest). |
Differences between protocol and review
No subgroup or sensitivity analyses were performed.
Contributions of authors
Mohammed Qintar: protocol development, trial identification, data extraction, data analysis, and drafting the review.
Abdulrahman Morad: protocol development and drafting the review.
Hazem Alhawasli: protocol development, trial identification, data extraction, data analysis, and drafting the review.
Khaled Shorbaji: protocol development, trial identification, data analysis, and drafting the review.
Belal M Firwana: data analysis, and drafting the review.
Adib Essali: protocol and review revision and providing consultation
Waleed Kadro: protocol and review revision and providing consultation.
All authors have contributed and approved to the final version of the review.
Sources of support
Internal sources
The Psychiatry Centre, Teshreen Hospital, Damascus, Syrian Arab Republic
External sources
No sources of support supplied
Declarations of interest
None known.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Gao 2007 {published data only}
- Gao, Y C, Li, Y, Han, Z H, Zhang, X L, Zhao, H, & Jiang, T Y. Transcoronary ablation of septal hypertrophy versus dual-chamber cardiac pacing for the treatment of aged patients with hypertrophic obstructive cardiomyopathy. Chung-Hua Hsin Hsueh Kuan Ping Tsa Chih [Chinese Journal of Cardiology] 2007;35(4):333-336. [PubMed] [Google Scholar]
Kappenberger 1997 {published data only}
- Kappenberger, L, Linde, C, Daubert, C, McKenna, W, Meisel, E, Aliot, E, Chajnovska, L, Guize, M, Jeanrenaud, X, & Gras, D. Pacing in hypertrophic obstructive cardiomyopathy (PIC). A randomised crossover study. Journal of the American College of Cardiology 1997;29(2):7961. [Google Scholar]
- Kappenberger, L, Linde, C, Daubert, C, McKenna, W, Meisel, E, Sadoul, N, Chojnowska, L, Guize, L, Gras, D, Jeanrenaud, X, & Ryden, L. Pacing in hypertrophic obstructive cardiomyopathy. A randomized crossover study. PIC Study Group. European Heart Journal 1997;18:1249-1256. [DOI] [PubMed] [Google Scholar]
- Linde, C, Gadler, F, Kappenberger, L, & Ryden, L. Placebo effect of pacemaker implantation in obstructive hypertrophic cardiomyopathy. PIC Study Group. Pacing In Cardiomyopathy. American Journal of Cardiology 1999;83(6):903-907. [DOI] [PubMed] [Google Scholar]
- Meisel, E, Rauwolf, T, Burghardt, M, & Kappenberger, L. Pacemaker therapy for hypertrophic-obstructive cardiomyopathy. Herzschrittmachertherapie und Elektrophysiologie 1999;2:58-68. [Google Scholar]
- Meisel E, Rauwolf T, Burghardt M, & Kappenberger L. DDD pacemakers in hypertrophic obstructive cardiomyopathy. Herz 2000;25(4):461-466. [PubMed] [Google Scholar]
Maron 1999b {published data only}
- Maron, B J, Nishimura, R A, McKenna, W J, Rakowski, H, Josephson, M E, & Kieval, R S. Assessment of permanent dual-chamber pacing as a treatment for drug-refractory symptomatic patients with obstructive hypertrophic cardiomyopathy. A randomized, double-blind, crossover study (M-PATHY). Circulation 1999;99:2927-2933. [DOI] [PubMed] [Google Scholar]
Mickelsen 2004 {published data only}
- Mickelsen, S, Bathina, M, Hsu, P, Holmes, J, & Kusumoto, F M. Doppler evaluation of the descending aorta in patients with hypertrophic cardiomyopathy: potential for assessing the functional significance of outflow tract gradients and for optimizing pacemaker function. Journal of Interventional Cardiac Electrophysiology 2004;11(1):47-53. [DOI] [PubMed] [Google Scholar]
Nishimura 1997 {published data only}
- Nishimura, R A, Trusty, J M, Hayes, D L, Ilstrup, D M, Larson, D R, Hayes, S N, Allison, T G, & Tajik, A J. Dual-chamber pacing for hypertrophic cardiomyopathy: a randomized, double-blind, crossover trial. Journal of the American College of Cardiology 1997;29(2):435-441. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Agarwal 2010 {published data only}
- Agarwal, S, Tuzcu, E M, Desai, M Y, Smedira, N, Lever, H M, Lytle, B W, & Kapadia, S R. Updated meta-analysis of septal alcohol ablation versus myectomy for hypertrophic cardiomyopathy. Journal of the American College of Cardiology 2010;55(8):823-834. [DOI] [PubMed] [Google Scholar]
Aizawa 1993 {published data only}
- Aizawa, Y, Naitoh, N, Kitazawa, H, Kusano, Y, Uchiyama, H, Washizuka, T, & Shibata, A. Frequency of presumed reentry with an excitable gap in sustained ventricular tachycardia unassociated with coronary artery disease. American Journal of Cardiology 1993;72(12):916-921. [DOI] [PubMed] [Google Scholar]
Alam 2006 {published data only}
- Alam, M, Dokainish, H, & Lakkis, N. Alcohol septal ablation for hypertrophic obstructive cardiomyopathy: a systematic review of published studies. Journal of Interventional Cardiology 2006;19(4):319-327. [DOI] [PubMed] [Google Scholar]
Alam 2009 {published data only}
- Alam, M, Dokainish, H, & Lakkis. Hypertrophic obstructive cardiomyopathy-alcohol septal ablation vs. myectomy: a meta-analysis. European Heart Journal 2009;30(9):1080-1087. [DOI] [PubMed] [Google Scholar]
Alfonso1996 {published data only}
- Alfonso, F. Cardiomyopathies. VIII. Sudden death in hypertrophic cardiomyopathy. Revista Espanola de Cardiologia 1996;49(4):288-304. [PubMed] [Google Scholar]
Anderson 1983 {published data only}
- Anderson, K P, Stinson, E B, Derby, G C, Oyer, P E, & Mason, J W. Vulnerability of patients with obstructive hypertrophic cardiomyopathy to ventricular arrhythmia induction in the operating room. Analysis of 17 patients. American Journal of Cardiology 1983;51(5):811-816. [DOI] [PubMed] [Google Scholar]
Badie 2009 {published data only}
- Badie, N & Bursac, N. Novel Micropatterned Cardiac Cell Cultures with Realistic Ventricular Microstructure. Biophysical Journal 2009;96(9):3873-3885. [DOI] [PMC free article] [PubMed] [Google Scholar]
Begley 2001 {published data only}
- Begley, D, Mohiddin, S, & Fananapazir, L. Dual chamber pacemaker therapy for mid-cavity obstructive hypertrophic cardiomyopathy. Pace-Pacing and Clinical Electrophysiology 2001;24(11):1639-1644. [DOI] [PubMed] [Google Scholar]
Bellon 1995 {published data only}
- Bellon, C, Kirkorian, G, Bourret, N, Richalet, C, Bonnefoy, E, & Touboul, P. Sustained ventricular tachycardia: an evaluation of long-term prognosis. Archives des Maladies du Coeur et des Vaisseaux 1995;88(7):1014-1019. [PubMed] [Google Scholar]
Ben 2000 {published data only}
- Ben, A Y, Sfaxi, A, Terras, M, Kraiem, S, Chehaibi, N, Essafi, N, Fennira, S, & Slimane, M L. Place of definitive cardiac stimulation in cardiomyopathies and atrial arrhythmia. Tunisie Medicale 2000;78(1):1-7. [PubMed] [Google Scholar]
Betocchi 1988 {published data only}
- Betocchi, S, Bonow, R O, Cannon, R O, III, Lesko, L J, Ostrow, H G, Watson, R M, & Rosing, D R. Relation between serum nifedipine concentration and hemodynamic effects in nonobstructive hypertrophic cardiomyopathy. American Journal of Cardiology 1988;61(10):830-835. [DOI] [PubMed] [Google Scholar]
Betocchi 1996 {published data only}
- Betocchi, S, Piscione, F, Losi, M A, Pace, L, Boccalatte, M, Perrone-Filardi, P, Cappelli, B, Briguori, C, Manganelli, F, Ciampi, Q, Salvatore, M, & Chiariello, M. Effects of diltiazem on left ventricular systolic and diastolic function in hypertrophic cardiomyopathy. American Journal of Cardiology 1996;78(4):451-457. [DOI] [PubMed] [Google Scholar]
Betocchi 2002 {published data only}
- Betocchi, S, Elliott, P M, Briguori, C, Virdee, M, Losi, M A, Matsumura, Y, Miranda, M, McKenna, W J, & Chiariello, M. Dual chamber pacing in hypertrophic cardiomyopathy: long-term effects on diastolic function. Pacing & Clinical Electrophysiology 2002;25(10):1433-1440. [DOI] [PubMed] [Google Scholar]
Bhatia 2004 {published data only}
- Bhatia, A, Cooley, R, Berger, M, Blanck, Z, Dhala, A, Sra, J, xtell-McBride, K, VanderVort, C, & Akhtar, M. The implantable cardioverter defibrillator: Technology, indications, and impact on cardiovascular survival. Current Problems in Cardiology 2004;29(6):303-356. [DOI] [PubMed] [Google Scholar]
Binder 2008 {published data only}
- Binder, J, Ommen, S R, Sorajja, P, Nishimura, R A, & Tajik, A J. Clinical and echocardiographic variables fail to predict response to dual-chamber pacing for hypertrophic cardiomyopathy. Journal of the American Society of Echocardiography 2008;21(7):796-800. [DOI] [PubMed] [Google Scholar]
Birnie 2006 {published data only}
- Birnie, D H & Tang, A S L. The problem of non-response to cardiac resynchronization therapy. Current Opinion in Cardiology Jan 2006;21(1):20-26. [DOI] [PubMed] [Google Scholar]
Bonow 1985 {published data only}
- Bonow, R O. Effects of calcium-channel blocking agents on left ventricular diastolic function in hypertrophic cardiomyopathy and in coronary artery disease. American Journal of Cardiology 1985;55(3):172B-178B. [DOI] [PubMed] [Google Scholar]
Braunschweig 2000 {published data only}
- Braunschweig, F, Linde, C, Gadler, F, & Ryden, L. Reduction of hospital days by biventricular pacing. European Journal of Heart Failure 2000;2(4):399-406. [DOI] [PubMed] [Google Scholar]
Braunwald 1997 {published data only}
- Braunwald, E. Induced septal infarction: a new therapeutic strategy for hypertrophic obstructive cardiomyopathy. Circulation 1997;95(8):1981-1982. [DOI] [PubMed] [Google Scholar]
Brignole 1988 {published data only}
- Brignole, M, Menozzi, C, Lolli, G, Sartore, B, & Barra, M. Natural and unnatural history of patients with severe carotid sinus hypersensitivity: a preliminary study. Pacing and clinical electrophysiology 1988;11(11):1628-1635. [DOI] [PubMed] [Google Scholar]
Brill 1985 {published data only}
- Brill, D M & Fozzard, H A. Calcium channel blocking drugs. Part II: Clinical applications. Comprehensive Therapy 1985;11(10):67-71. [PubMed] [Google Scholar]
Bryce 2001 {published data only}
- Bryce, M, Spielman, S R, Greenspan, A M, & Kotler, M N. Evolving indications for permanent pacemakers. Annals of Internal Medicine 2001;134(12):1130-1141. [DOI] [PubMed] [Google Scholar]
Can 2009 {published data only}
- Can, I & Tholakanahalli, V N. Current status of implantable cardioverter-defibrillator therapy in heart failure. Current Heart Failure Reports 2009;6(3):199-209. [DOI] [PubMed] [Google Scholar]
Cannon 1985 {published data only}
- Cannon, R O, III, Rosing, D R, Maron, B J, Leon, M B, Bonow, R O, Watson, R M, & Epstein, S E. Myocardial ischemia in patients with hypertrophic cardiomyopathy: contribution of inadequate vasodilator reserve and elevated left ventricular filling pressures. Circulation 1985;71(2):234-243. [DOI] [PubMed] [Google Scholar]
Cannon 1987 a {published data only}
- Cannon, R O. Myocardial ischemia in hypertrophic cardiomyopathy. Zeitschrift fur Kardiologie 1987;76:Suppl-4. [PubMed] [Google Scholar]
Cannon 1987 b {published data only}
- Cannon, R O, III, Schenke, W H, Maron, B J, Tracy, C M, Leon, M B, Brush, J E Jr, Rosing, D R, & Epstein, S E. Differences in coronary flow and myocardial metabolism at rest and during pacing between patients with obstructive and patients with nonobstructive hypertrophic cardiomyopathy. Journal of the American College of Cardiology 1987;10(1):53-62. [DOI] [PubMed] [Google Scholar]
Cannon 1990 {published data only}
- Cannon, R O, III, Quyyumi, A A, Schenke, W H, Fananapazir, L, Tucker, E E, Gaughan, A M, Gracely, R H, Cattau, E L Jr, & Epstein, S E. Abnormal cardiac sensitivity in patients with chest pain and normal coronary arteries. Journal of the American College of Cardiology 1990;16(6):1359-1366. [DOI] [PubMed] [Google Scholar]
Capezzuto 2000 {published data only}
- Capezzuto, A, Guerra, R, Pontillo, D, Sassara, M, Savelli, M S, Castellani, R, & Scabbia, E V. "[The long-term effects of dual-chamber stimulation in 8 patients with hypertrophic obstructive cardiomyopathy and symptoms refractory to medical therapy. Italian Heart Journal Supplement 2000;1(2):250-255. [PubMed] [Google Scholar]
Cesario 2006 {published data only}
- Cesario, D A & Dec, G W. Implantable Cardioverter- Defibrillator Therapy in Clinical Practice. Journal of the American College of Cardiology 2006;47(8):1507-1517. [DOI] [PubMed] [Google Scholar]
Chen 2007 {published data only}
- Chen, S L, Dai, Z L, Li, Z Q, Hu, Z Y, Ye, F, Zhang, J J, Zhang, F F, Luo, J, Zhu, Z S, Lin, S, Wu, C Q, & Tian, N L. Left ventricular endocardial pacing predicts the reduction of left ventricular outflow tract pressure gradient immediately after percutaneous transseptal myocardial ablation in patients with hypertrophic obstructive cardiomyopathy refractory to medication. Chinese Medical Journal 2007;120(7):562-568. [PubMed] [Google Scholar]
Ciaramitaro 2006 {published data only}
- Ciaramitaro, G, Sgarito, G, Solimene, F, Maglia, G, Vicentini, A, Di, D G, Raciti, G, Parrinello, G, & Del Giudice, G B. Role of rate control and regularization through pacing in patients with chronic atrial fibrillation and preserved ventricular function: The VRR study. Pacing and Clinical Electrophysiology 2006;29(8):866-874. [DOI] [PubMed] [Google Scholar]
Coats 2008 {published data only}
- Coats, C J & Elliott, P M. Current management of hypertrophic cardiomyopathy. Current Treatment Options in Cardiovascular Medicine 2008;10(6):496-504. [DOI] [PubMed] [Google Scholar]
Cregg 1999 {published data only}
- Cregg, N, Cheng, D C, Karski, J M, Williams, W G, Webb, G, & Wigle, E D. Morbidity outcome in patients with hypertrophic obstructive cardiomyopathy undergoing cardiac septal myectomy: early-extubation anesthesia versus high-dose opioid anesthesia technique. Journal of Cardiothoracic & Vascular Anesthesia 1999;13(1):47-52. [DOI] [PubMed] [Google Scholar]
da Fonseca 2007 {published data only}
- da Fonseca, S M, Belo, L G, Carvalho, H, Araujo, N, Munhoz, C, Siqueira, L, Maciel, W, Andrea, E, & Atie, J. Clinical follow-up of patients with implantable cardioverter-defibrillator. Arquivos Brasileiros de Cardiologia 2007;88(1):8-16. [DOI] [PubMed] [Google Scholar]
Daley 1987 {published data only}
- Daley, P J, Chapman, P D, & Troup, P J. Catheter ablation of the atrioventricular junction and activity responsive pacing. Effect on refractory atrial fibrillation with hypertrophic cardiomyopathy. Chest 1987;91(3):461-462. [DOI] [PubMed] [Google Scholar]
Daubert 2004 {published data only}
- Daubert, J C, Pavin, D, Jauvert, G, & Mabo, P. Intra- and interatrial conduction delay: Implications for cardiac pacing. Pace-Pacing and Clinical Electrophysiology 2004;27(4):507-525. [DOI] [PubMed] [Google Scholar]
Deharo 2000 {published data only}
- Deharo, J-C. The best of cardiac pacing in 1999. Archives des Maladies du Coeur et des Vaisseaux 2000;93(1):43-49. [PubMed] [Google Scholar]
Dimitrow 2000 {published data only}
- Dimitrow, P P, Grodecki, J, Bacior, B, Dudek, D, Legutko, J, Jaszcz, K K, & Dubiel, J S. The importance of ventricular septal morphology in the effectiveness of dual chamber pacing in hypertrophic obstructive cardiomyopathy. Pacing & Clinical Electrophysiology 2000;23(9):1324-1329. [DOI] [PubMed] [Google Scholar]
Dimitrow 2002 {published data only}
- Dimitrow, P P, Krzanowski, M, Grodecki, J, Malecka, B, Lelakowski, J, Kawecka-Jaszcz, K, Szczeklik, A, & Dubiel, J S. Verapamil improves the pacing-induced vasodilatation in symptomatic patients with hypertrophic cardiomyopathy. International Journal of Cardiology 2002;83(3):239-247. [DOI] [PubMed] [Google Scholar]
Dimitrow 2004 {published data only}
- Dimitrow, P P, Podolec, P, Grodecki, J, Plazak, W, Dudek, D, Pieniazek, P, Bacior, B, Legutko, J, Olszowska, M, Kostkiewicz, M, Kawecka-Jaszcz, K, Tracz, W, & Dubiel, J S. Comparison of dual-chamber pacing with nonsurgical septal reduction effect in patients with hypertrophic obstructive cardiomyopathy. International Journal of Cardiology 2004;94(1):31-34. [DOI] [PubMed] [Google Scholar]
Duarte 1999 {published data only}
- Duarte, J A & Carrageta, M. The new indications for permanent cardiac pacing. Revista Portuguesa de Cardiologia 1999;18(3):281-288. [PubMed] [Google Scholar]
El 2007 {published data only}
- El, a S, Amine, B, Saoud, B, Guedira, N, Allali, F, & Hajjaj-Hassouni, N. Complete auriculoventricular block during chloroquine treatment. Revue de Medecine Interne 2007;28(2):134-136. [DOI] [PubMed] [Google Scholar]
El 2008 {published data only}
- El, M H & Breall, J A. Alcohol septal ablation for hypertrophic obstructive cardiomyopathy. Current Cardiology Reviews 2008;4(3):193-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faber 2007 a {published data only}
- Faber, L, Welge, D, Fassbender, D, Schmidt, H K, Horstkotte, D, & Seggewiss, H. One-year follow-up of percutaneous septal ablation for symptomatic hypertrophic obstructive cardiomyopathy in 312 patients: predictors of hemodynamic and clinical response. Clinical Research in Cardiology 2007;96(12):864-873. [DOI] [PubMed] [Google Scholar]
Faber 2007 b {published data only}
- Faber, L, Welge, D, Fassbender, D, Schmidt, H K, Horstkotte, D, & Seggewiss. Percutaneous septal ablation for symptomatic hypertrophic obstructive cardiomyopathy: managing the risk of procedure-related AV conduction disturbances. International Journal of Cardiology, 2007;119(2):163-167. [DOI] [PubMed] [Google Scholar]
Fananapazir 1991 {published data only}
- Fananapazir, L & Epstein, S E. Value of electrophysiologic studies in hypertrophic cardiomyopathy treated with amiodarone. American Journal of Cardiology 1991;67(2):175-182. [DOI] [PubMed] [Google Scholar]
Fananapazir 1998 {published data only}
- Fananapazir, L & McAreavey, D. Therapeutic options in patients with obstructive hypertrophic cardiomyopathy and severe drug-refractory symptoms. Journal of the American College of Cardiology 1998;31(2):259-264. [DOI] [PubMed] [Google Scholar]
Fei 2001 {published data only}
- Fei, L & Trohman, R G. in cardiac electrophysiology and pacing. Critical Care Clinics 2001;17(2):337-364. [DOI] [PubMed] [Google Scholar]
Ferguson 1997 {published data only}
- Ferguson, T B. Pacemakers. Current Problems in Surgery 1997;34(1):6-108. [DOI] [PubMed] [Google Scholar]
Fernandes 2005 {published data only}
- Fernandes, V L, Nagueh, S F, Franklin, J, Wang, W, Roberts, R, & Spencer, W H. A prospective follow-up of alcohol septal ablation for symptomatic hypertrophic obstructive cardiomyopathy - The Baylor experience. Clinical Cardiology 2005;28(3):124-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Finsterer 2010 {published data only}
- Finsterer, J. Treatment of mitochondrial disorders. European Journal of Paediatric Neurology 2010;14(1):29-44. [DOI] [PubMed] [Google Scholar]
Frank 1978 {published data only}
- Frank, M J, Abdulla, A M, Canedo, M I, & Saylors, R E. Long-term medical management of hypertrophic obstructive cardiomyopathy. American Journal of Cardiology 1978;42(6):993-1001. [DOI] [PubMed] [Google Scholar]
Frank 1983 {published data only}
- Frank, M J, Stefadouros, M A, Watkins, L O, Prisant, L M, & Abdulla, A M. Rhythm disturbances in hypertrophic cardiomyopathies: relationship to symptoms and the effect of 'complete' beta blockade. European Heart Journal 1983;4:Suppl-43. [DOI] [PubMed] [Google Scholar]
Freedman 2001 {published data only}
- Freedman, R A. Use of implantable pacemakers and implantable defibrillators in hypertrophic cardiomyopathy. Current Opinion in Cardiology 2001;16(1):58-65. [DOI] [PubMed] [Google Scholar]
Gadler 1997 {published data only}
- Gadler, F, Linde, C, Juhlin-Dannfelt, A, Ribeiro, A, & Ryden, L. Long-term effects of dual chamber pacing in patients with hypertrophic cardiomyopathy without outflow tract obstruction at rest. European Heart Journal 1997;18(4):636-642. [DOI] [PubMed] [Google Scholar]
Gadler 1999 {published data only}
- Gadler, F, Linde, C, & Ryden, L. Rapid return of left ventricular outflow tract obstruction and symptoms following cessation of long-term atrioventricular synchronous pacing for obstructive hypertrophic cardiomyopathy. American Journal of Cardiology 1999;83(4):553-557. [DOI] [PubMed] [Google Scholar]
Gadler 1999b {published data only}
- Gadler, F, Linde, C, Daubert, C, McKenna, W, Meisel, E, Aliot, E, Chojnowska, L, Guize, L, Gras, D, Jeanrenaud, X, & Kappenberger, L. Significant improvement of quality of life following atrioventricular synchronous pacing in patients with hypertrophic obstructive cardiomyopathy. Data from 1 year of follow-up. PIC study group. Pacing In Cardiomyopathy. European Heart Journal 1999;20(14):1044-1050. [DOI] [PubMed] [Google Scholar]
Gadler 2001 {published data only}
- Gadler, F. Pacing in obstructive hypertrophic cardiomyopathy. European Heart Journal Supplements 2001;3(L):L32-L37. [Google Scholar]
Gietzen 2004 {published data only}
- Gietzen, F H, Brunn, J, Schummelfeder, J, Neuser, H, Schumacher, B, & Kerber, S. Pacing in hypertrophic obstructive cardiomyopathy. Herzschrittmachertherapie und Elektrophysiologie. 2004;15(2):137-146. [Google Scholar]
Gietzen 2005 {published data only}
- Gietzen, F H, Schummelfeder, J, Neuser, H, Brunn, J, Schumacher, B, & Kerber, S. "[Interventional treatment in hypertrophic cardiomyopathy". Herz 2005;30(2):102-110. [DOI] [PubMed] [Google Scholar]
Gilligan 2000 {published data only}
- Gilligan, D M. Dual-chamber pacing in hypertrophic cardiomyopathy. Current Cardiology Reports 2000;2(2):154-159. [DOI] [PubMed] [Google Scholar]
Goethals 1999 {published data only}
- Goethals, M A & Vanderheyden, M. Pacing in cardiomyopathy. Acta Cardiologica 1999;54(5):245-252. [PubMed] [Google Scholar]
Gold 1999 {published data only}
- Gold, M R. Optimization of ventricular pacing: Where should we implant the leads. Journal of the American College of Cardiology 1999;33(2):324-326. [DOI] [PubMed] [Google Scholar]
Gold 2001 {published data only}
- Gold, M R. Permanent pacing: new indications. Heart 2001;86(3):355-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodwin 1989 {published data only}
- Goodwin, J F. Clinical decisions in the management of the cardiomyopathies. Drugs 1989;38(6):988-999. [DOI] [PubMed] [Google Scholar]
Gras 1995 {published data only}
- Gras, D, Daubert, C, & Mabo, P. Value of cardiac pacing in hypertrophic obstructive cardiomyopathy refractory to medical treatment. Archives des Maladies du Coeur et des Vaisseaux 1995;88(4):Suppl-83.. [PubMed] [Google Scholar]
Gras 1995b {published data only}
- Gras, D, de, P C, Le, B H, Leclercq, C, Paillard, F, Mabo, P, & Daubert, C. Importance of atrioventricular synchrony in hypertrophic obstructive cardiomyopathy treated by cardiac pacing. Archives des Maladies du Coeur et des Vaisseaux 1995;88(2):215-223. [PubMed] [Google Scholar]
Gras 1995c {published data only}
- Gras, D, Leclercq, C, de, P C, Pavin, D, Le, B H, Mabo, P, & Daubert, C. The potential role of dual-chamber pacing in the management of elderly patients with hypertrophic cardiomyopathy. Cardiology in the Elderly 1995;3(6):430-438. [Google Scholar]
Gregoratos 1999 {published data only}
- Gregoratos, G. Permanent pacemakers in older persons. Journal of the American Geriatrics Society 1999;47(9):1125-1135. [DOI] [PubMed] [Google Scholar]
Hagege 2009 {published data only}
- Hagege, A A & Desnos, M. New trends in treatment of hypertrophic cardiomyopathy. Archives of Cardiovascular Diseases 2009;102(5):441-447. [DOI] [PubMed] [Google Scholar]
Harrison 1976 {published data only}
- Harrison, D C, Fitzgerald, J W, & Winkle, R A. Ambulatory electrocardiography for diagnosis and treatment of cardiac arrhythmias. New England Journal of Medicine 1976;294(7):373-380. [DOI] [PubMed] [Google Scholar]
Haruki 2010 {published data only}
- Haruki, S, Minami, Y, Kajimoto, K, Yashiro, B, Suzuki, T, Kawana, M, & Hagiwara, N. Possible acute and chronic synergistic effect of dual chamber pacing and disopyramide in obstructive hypertrophic cardiomyopathy: a case report. European Journal of Heart Failure 2010;12(1):94-97. [DOI] [PubMed] [Google Scholar]
Hauer 2001 {published data only}
- Hauer, R N W, Aliot, E, Block, M, Capucci, A, Luderitz, B, Santini, M, & Vardas, P E. Indications for implantable cardioverter defibrillator (ICD) therapy. Europace 2001;3(3):169-176. [DOI] [PubMed] [Google Scholar]
Hauer 2001b {published data only}
- Hauer, R N W, Aliot, E, Block, M, Capucci, A, Luderitz, B, Santini, M, & Vardas, P E. Indications for implantable cardioverter defibrillator (ICD) therapy - Study group on guidelines on ICDs of the Working Group on Arrhythmias and the Working Group on Cardiac Pacing of the European Society of Cardiology. European Heart Journal 2001;22(13):1074-1081. [DOI] [PubMed] [Google Scholar]
Hayes 1999 {published data only}
- Hayes, D L. Evolving indications for permanent pacing. American Journal of Cardiology 1999;85(5):161D-165D. [DOI] [PubMed] [Google Scholar]
Hayes 2004a {published data only}
- Hayes, D L & Furman, S. Cardiac pacing: How it started, where we are, where we are going. Pace-Pacing and Clinical Electrophysiology 2004;27(5):693-704. [DOI] [PubMed] [Google Scholar]
Hayes 2004b {published data only}
- Hayes, D L & Furman, S. Cardiac pacing: How it started, where we are, where we are going. Journal of Cardiovascular Electrophysiology 2004;15(5):619-627. [DOI] [PubMed] [Google Scholar]
Herold 1991 {published data only}
- Herold, M, Hrdlicka, S, Osmera, P, & Gregor, P. Determination of anti-arrhythmia therapy of ventricular arrhythmias based on programmed ventricular stimulation. Vnitrni Lekarstvi 1991;37(11-12):833-840. [PubMed] [Google Scholar]
Hess 1982 {published data only}
- Hess, O M, Hirzel, H O, & Krayenbuhl, H P. Calcium antagonists in the treatment of heart diseases. Schweizerische Medizinische Wochenschrift 1982;19:689-692. [PubMed] [Google Scholar]
Hilleman 2001 {published data only}
- Hilleman, D E & Bauman, J L. Role of antiarrhythmic therapy in patients at risk for sudden cardiac death: An evidence-based review. Pharmacotherapy 2001;21(5):556-575. [DOI] [PubMed] [Google Scholar]
Honda 2005 {published data only}
- Honda, T, Shono, H, Koyama, J, Tsuchiya, T, Hayashi, M, Hirayama, T, Uesugi, H, & Honda, T. Impact of right atrial-left ventricular dual-chamber permanent pacing in patients with severely symptomatic hypertrophic obstructive cardiomyopathy. Circulation Journal 2005;69(5):536-542. [DOI] [PubMed] [Google Scholar]
Itoh 1988 {published data only}
- Itoh, S, Kobayashi, K, Yoneda, N, Kaneda, S, Inoue, T, Ishida, K, & Fukuzaki, H. Clinical study of late potentials--comparison of late potentials in myocardial infarction, cardiomyopathy and idiopathic ventricular tachycardia. Japanese Circulation Journal 1988;52(1):21-29. [DOI] [PubMed] [Google Scholar]
Izawa 1996 {published data only}
- Izawa, H, Yokota, M, Nagata, K, Iwase, M, & Sobue, T. Impaired response of left ventricular relaxation to exercise-induced adrenergic stimulation in patients with hypertrophic cardiomyopathy. Journal of the American College of Cardiology 1996;28(7):1738-1745. [DOI] [PubMed] [Google Scholar]
Izawa 1997 {published data only}
- Izawa, H, Yokota, M, Takeichi, Y, Inagaki, M, Nagata, K, Iwase, M, & Sobue, T. "Adrenergic control of the force-frequency and relaxation-frequency relations in patients with hypertrophic cardiomyopathy. Circulation 1997;96(9):2959-2968. [DOI] [PubMed] [Google Scholar]
Jandik 1990 {published data only}
- Jandik, J, Kvasnicka, J, & Vokrouhlicky, L. Systolic and diastolic intervals in patients with hypertrophic obstructive cardiomyopathy before and after withdrawal of verapamil. Bratislavske Lekarske Listy 1990;91(9):701-704. [PubMed] [Google Scholar]
Jansson 1990 {published data only}
- Jansson, K, Dahlstrom, U, Karlsson, E, Nylander, E, Walfridsson, H, & Sonnhag, C. The value of exercise test, Holter monitoring, and programmed electrical stimulation in detection of ventricular arrhythmias in patients with hypertrophic cardiomyopathy. Pacing & Clinical Electrophysiology 1990;13(10):1261-1267. [DOI] [PubMed] [Google Scholar]
Jeserich 2001 a {published data only}
- Jeserich, M & Just, H. Current status of endocarditis prevention. Zeitschrift fur Kardiologie 2001;90(6):385-393. [DOI] [PubMed] [Google Scholar]
Jeserich 2001 b {published data only}
- Jeserich, M & Just, H. Practice guidelines and current recommendations for antibiotic endocarditis prophylaxis. Zeitschrift fur Kardiologie. 2001;90(6):385-393. [DOI] [PubMed] [Google Scholar]
Juliard 1987 {published data only}
- Juliard, J M, Charlier, P, Nitenberg, A, Merillon, J P, Masquet, C, & Gourgon, R. Non-obstructive hypertrophic cardiomyopathy and systolic compression of 3 coronary arteries. Long-term improvement with verapamil. Annales de Medecine Interne 1987;138(7):512-516. [PubMed] [Google Scholar]
Kaik 1992 {published data only}
- Kaik, J, Kaik, V, & Kiitam, M. Antiarrhythmic efficacy of ethacizine assessed by programmed electrical stimulation in patients with ventricular tachycardia. Pacing & Clinical Electrophysiology 1992;15(11):t-7. [DOI] [PubMed] [Google Scholar]
Kappenberger 1997c {published data only}
- Kappenberger, L, Linde, C, Daubert, C, McKenna, W, Meisel, E, Sadoul, N, Chojnowska, L, Guize, L, Gras, D, Jeanrenaud, X, & Ryden, L. Pacing in hypertrophic obstructive cardiomyopathy. A randomized crossover study. PIC Study Group. European Heart Journal 1997;18(8):1249-1256. [DOI] [PubMed] [Google Scholar]
Kappenberger 1999 {published data only}
- Kappenberger, L J, Linde, C, Jeanrenaud, X, Daubert, C, McKenna, W, Meisel, E, Sadoul, N, Chojnowska, L, Guize, L, Gras, D, Aebischer, N, Gadler, F, & Ryden, L. Clinical progress after randomized on/off pacemaker treatment for hypertrophic obstructive cardiomyopathy. Pacing in Cardiomyopathy (PIC) Study Group. Europace 1999;1(2):77-84. [DOI] [PubMed] [Google Scholar]
Kass 1999 {published data only}
- Kass, D A, Chen, C-H, Talbot, M W, Rochitte, C E, Lima, J A C, Berger, R D, & Calkins, H. Ventricular pacing with premature excitation for treatment of hypertensive-cardiac hypertrophy with cavity-obliteration. Circulation 1999;8:807-812. [DOI] [PubMed] [Google Scholar]
Kido 2006 {published data only}
- Kido, S, Hasebe, N, Ishii, Y, & Kikuchi, K. Tachycardia-induced myocardial ischemia and diastolic dysfunction potentiate secretion of ANP, not BNP, in hypertrophic cardiomyopathy. American Journal of Physiology - Heart & Circulatory Physiology 2006;290(3):H1064-H1070. [DOI] [PubMed] [Google Scholar]
Kim 1987 {published data only}
- Kim, S G, Felder, S D, Figura, I, Johnston, D R, Waspe, L E, & Fisher, J D. Comparison of programmed stimulation and Holter monitoring for predicting long-term efficacy and inefficacy of amiodarone used alone or in combination with a class 1A antiarrhythmic agent in patients with ventricular tachyarrhythmia. Journal of the American College of Cardiology 1987;9(2):398-404. [DOI] [PubMed] [Google Scholar]
Kovacic 2003 {published data only}
- Kovacic, J C & Muller, D. Hypertrophic cardiomyopathy: state-of-the-art review, with focus on the management of outflow obstruction. Internal Medicine Journal 2003;33(11):521-529. [DOI] [PubMed] [Google Scholar]
Krejci 2006 {published data only}
- Krejci, J, Groch, L, Meluzin, J, Vykypel, T, Halamek, J, & Vitovec, J. Non-pharmacologic therapy of hypertrophic obstructive cardiomyopathy--results of therapy based on percutaneous transluminal septal myocardial ablation compared with results of dual-chamber cardiac pacing. Vnitrni Lekarstvi 2006;52(4):313-320. [PubMed] [Google Scholar]
Kuck 1987 a {published data only}
- Kuck, K H, Kunze, K P, Geiger, M, Costard, A, & Schluter, M. "Programmed electrical stimulation in patients with hypertrophic cardiomyopathy". Zeitschrift fur Kardiologie 1987;76:6. [PubMed] [Google Scholar]
Kuck 1987 b {published data only}
- Kuck, K H. Cardiac arrhythmia in hypertrophic cardiomyopathy. Diagnosis and therapy]. Internist 1987;28(3):168-174. [PubMed] [Google Scholar]
Kuck 1988 {published data only}
- Kuck, K H, Kunze, K P, Schluter, M, Nienaber, C A, & Costard, A. Programmed electrical stimulation in hypertrophic cardiomyopathy. Results in patients with and without cardiac arrest or syncope. European Heart Journal 1988;9(2):177-185. [DOI] [PubMed] [Google Scholar]
Kuhn 1999 {published data only}
- Kuhn, H & Gietzen, F. Transcoronary ablation of septal hypertrophy (TASH): supersedes it the surgery (myectomy)? Herz 1999;24(8):647-651. [DOI] [PubMed] [Google Scholar]
Kuhn 2000 {published data only}
- Kuhn, H, Gietzen, F H, Leuner, C, Schafers, M, Schober, O, Strunk-Muller, C, Obergassel, L, Freick, M, Gockel, B, Lieder, F, & Raute-Kreinsen, U. Transcoronary ablation of septal hypertrophy (TASH): a new treatment option for hypertrophic obstructive cardiomyopathy. Zeitschrift fur Kardiologie 2000;89:41-54. [DOI] [PubMed] [Google Scholar]
Kuhn 2001 {published data only}
- Kuhn, H, Gietzen, F H, Breithardt, G, Rohrig, F R, Lieder, F, Gotsch, U, Schulte, H D, & Freick, M. Pacemaker therapy and alcohol ablation for HOCM: a randomized study. European Heart Journal 2001;22:20. [Google Scholar]
Kukar 2006 {published data only}
- Kukar, A, Sherrid, M V, & Ehlert, F A. Pacing in obstructive hypertrophic cardiomyopathy: A therapeutic option? Anadolu Kardiyoloji Dergisi 2006;6(2):49-54. [PubMed] [Google Scholar]
Kusumoto 2002 {published data only}
- Kusumoto, F M & Goldschlager, N. Device therapy for cardiac arrhythmias. Jama-Journal of the American Medical Association 2002;287(14):1848-1852. [DOI] [PubMed] [Google Scholar]
Kusumoto 2006 {published data only}
- Kusumoto, F & Goldschlager, N. Implantable cardiac arrhythmia devices - Part II: Implantable cardioverter defibrillators and implantable loop recorders. Clinical Cardiology 2006;29(6):237-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lakkis 1998 {published data only}
- Lakkis, N M, Nagueh, S F, Kleiman, N S, Killip, D, He, Z X, Verani, M S, Roberts, R, & Spencer, W H, III. Echocardiography-guided ethanol septal reduction for hypertrophic obstructive cardiomyopathy. Circulation 1998;98(17):1750-1755. [DOI] [PubMed] [Google Scholar]
Lakkis 2000 {published data only}
- Lakkis, N. New treatment methods for patients with hypertrophic obstructive cardiomyopathy. Current Opinion in Cardiology 2000;15(3):172-177. [DOI] [PubMed] [Google Scholar]
Lakkis 2001 {published data only}
- Lakkis, N, Plana, J C, Nagueh, S, Killip, D, Roberts, R, & Spencer, W H. Efficacy of nonsurgical septal reduction therapy in symptomatic patients with obstructive hypertrophic cardiomyopathy and provocable gradients. American Journal of Cardiology 2001;88(5):583-+. [DOI] [PubMed] [Google Scholar]
Landmark 1982 {published data only}
- Landmark, K, Sire, S, Thaulow, E, Amlie, J P, & Nitter-Hauge, S. Haemodynamic effects of nifedipine and propranolol in patients with hypertrophic obstructive cardiomyopathy. British Heart Journal 1982;48(1):19-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lerakis 1997 {published data only}
- Lerakis, S, Sheahan, R G, & Stouffer, G A. Hypertrophic cardiomyopathy: presentation and pathophysiology. American Journal of the Medical Sciences 1997;314(5):324-329. [DOI] [PubMed] [Google Scholar]
Lerakis 2001 {published data only}
- Lerakis, S, Cohen, D, Schwartz, R A, & Sheahan, R G. Pacing and hypertrophic cardiomyopathy. American Journal of the Medical Sciences 2001;322(3):156. [DOI] [PubMed] [Google Scholar]
Lo 1987 {published data only}
- Lo, Y S & Nguyen, K P. Electrophysiologic study in the management of cardiac arrest survivors: a critical review. American Heart Journal 1987;114(3):596-606. [DOI] [PubMed] [Google Scholar]
Lopez 2002 {published data only}
- Lopez, M M & Olvera, C S. Pacemaker stimulation in dilated and hypertrophic myocardiopathies: should its use be stratified? Archivos de Cardiologia de Mexico 2002;72:Suppl-21. [PubMed] [Google Scholar]
Losi 1998 {published data only}
- Losi, M A, Betocchi, S, Briguori, C, Piscione, F, Manganelli, F, Ciampi, Q, Stabile, G, & Chiariello, M. Dual chamber pacing in hypertrophic cardiomyopathy: influence of atrioventricular delay on left ventricular outflow tract obstruction. Cardiology 1998;89(1):8-13. [DOI] [PubMed] [Google Scholar]
Maron 1995 {published data only}
- Maron, B J. Therapeutic strategies in hypertrophic cardiomyopathy: Considerations and critique of new treatment modalities. Heart Failure 1995;11(1):27-32. [Google Scholar]
Maron 1998 {published data only}
- Maron, B J, Nishimura, R A, McKenna, W J, Rakowski, H, Josephson, M E, & Kieval, R S. Assessment of dual-chamber pacing as a treatment for drug-refractory symptomatic patients with obstructive hypertrophic cardiomyopathy: A randomized, double-blind, crossover study (M-PATHY). Circulation 1998;98(17):2658. [DOI] [PubMed] [Google Scholar]
Martin 1996 {published data only}
- Martin, L C, Arribas, J A, Pabon, O P, Saez, J A, Santos, R, I, Nieto, B F, & Rodriguez, C J. Cardiomyopathy (X). Clinical approach to the patient with hypertrophic cardiomyopathy. Revista Espanola de Cardiologia 1996;49(6):457-469. [PubMed] [Google Scholar]
McKenna 2009 {published data only}
- McKenna, W J & Kaski, J P. Pacemaker Therapy in Hypertrophic Obstructive Cardiomyopathy: Still Awaiting the Evidence. Revista Espanola de Cardiologia 2009;62(11):1217-1220. [DOI] [PubMed] [Google Scholar]
McNamara 1983 {published data only}
- McNamara, D G. Twenty-five years of progress in the medical treatment of pediatric and congenital heart disease. Journal of the American College of Cardiology 1983;1(1):264-273. [DOI] [PubMed] [Google Scholar]
Megevand 2005 {published data only}
- Megevand, A, Ingles, J, Richmond, D R, & Semsarian, C. Long-term follow-up of patients with obstructive hypertrophic cardiomyopathy treated with dual-chamber pacing. American Journal of Cardiology 2005;95(8):991-993. [DOI] [PubMed] [Google Scholar]
Meisel 2001 {published data only}
- Meisel, E, Rauwolf, T, Burghardt, M, & Kappenberger, L. Hypertrophic obstructive cardiomyopathy - Differentiated benefit of cardiac pacing. [German]. Herzschrittmachertherapie und Elektrophysiologie 2001;SUPPL:37-38. [Google Scholar]
Merrill 2000 {published data only}
- Merrill, W H, Friesinger, G C, Graham, T P, Byrd, B F, Drinkwater, D C, Christian, K G, & Bender, H W. Long-lasting improvement after septal myectomy for hypertrophic obstructive cardiomyopathy. Annals of Thoracic Surgery 2000;69(6):1732-1735. [DOI] [PubMed] [Google Scholar]
Milic 2005 {published data only}
- Milic, D J, Perisic, Z D, Zivic, S S, Stanojkovic, Z A, Stojkovic, A M, Karanovic, N D, Krstic, N H, & Salinger, S S. Prevention of pocket related complications with fibrin sealant in patients undergoing pacemaker implantation who are receiving anticoagulant treatment. Europace 2005;7(4):374-379. [DOI] [PubMed] [Google Scholar]
Millaire 1995 a {published data only}
- Millaire, A. Surgical treatment of hypertrophic cardiomyopathy; techniques, indications and results. Archives des Maladies du Coeur et des Vaisseaux 1995;88(4):Suppl-8. [PubMed] [Google Scholar]
Millaire 1995 b {published data only}
- Millaire, A, de, G P, Decoulx, E, & Ducloux, G. Current respective role of surgery and permanent endocavitary stimulation in the treatment of hypertrophic cardiomyopathies. Annales de Cardiologie et d Angeiologie 1995;44(5):226-233. [PubMed] [Google Scholar]
Millaire 1998 {published data only}
- Millaire, A. Diastolic cardiac failure: therapeutic modalities. Archives des Maladies du Coeur et des Vaisseaux 1998;91(11):1365-1369. [PubMed] [Google Scholar]
Miyajima 1988 {published data only}
- Miyajima, S, Aizawa, Y, Matsuoka, A, Okabe, M, & Shibata, A. Danger of use of disopyramide in patients with hypertrophic obstructive cardiomyopathy. An electrophysiologic study. Japanese Heart Journal 1988;29(1):115-119. [DOI] [PubMed] [Google Scholar]
Mohiddin 2002 {published data only}
- Mohiddin, S A, Kent, K, Begley, D A, Leifer, E, Shawl, F, Goldstein, S, Sachdev, V, Ageyman, K, Arai, A, & Fananapazir, L. A Randomized prospective comparison of alcohol septal ablation and dual chamber pacemaker therapy in obstructive hypertrophic cardiomyopathy associated with drug-refractory symptoms. Circulation 2002;106(19):3228. [Google Scholar]
Mohiddin 2010 {published data only}
- Mohiddin, S A & Page, S P. Long-term benefits of pacing in obstructive hypertrophic cardiomyopathy. Heart 2010;96(5):328-330. [DOI] [PubMed] [Google Scholar]
Monakier 2004 {published data only}
- Monakier, D, Woo, A, Puri, T, Schwartz, L, Ross, J, Jamorski, M, Yang, H, Liu, Z, Vannan, M, Wigle, E D, & Rakowski, H. Usefulness of myocardial contrast echocardiographic quantification of risk area for predicting postprocedural complications in patients undergoing septal ethanol ablation for obstructive hypertrophic cardiomyopathy. American Journal of Cardiology 2004;94(12):1515-1522. [DOI] [PubMed] [Google Scholar]
Montijano Cabrera 2001 {published data only}
- Montijano Cabrera, A M, Bouzas, Z B, Penas, L M, & McKenna, W J. "[Therapeutic approaches in symptomatic hypertrophic obstructive cardiomyopathy].. Revista Espanola de Cardiologia 2001;54(11):1311-1326. [DOI] [PubMed] [Google Scholar]
Naccarelli 1982 {published data only}
- Naccarelli, G V, Prystowsky, E N, Jackman, W M, Heger, J J, Rahilly, G T, & Zipes, D P. Role of electrophysiologic testing in managing patients who have ventricular tachycardia unrelated to coronary artery disease. American Journal of Cardiology 1982;50(1):165-171. [DOI] [PubMed] [Google Scholar]
Nagueh 2001 {published data only}
- Nagueh, S F, Ommen, S R, Lakkis, N M, Killip, D, Zoghbi, W A, Schaff, H V, Danielson, G K, Quinones, M A, Tajik, A J, & Spencer, W H. Comparison of ethanol septal reduction therapy with surgical myectomy for the treatment of hypertrophic obstructive cardiomyopathy. Journal of the American College of Cardiology 2001;38(6):1701-1706. [DOI] [PubMed] [Google Scholar]
Nakatani 1996 {published data only}
- Nakatani, M, Yokota, Y, & Yokoyama, M. Acute hemodynamic deterioration during rapid atrial pacing in patients wit hypertrophic cardiomyopathy. Clinical Cardiology 1996;19(5):385-392. [DOI] [PubMed] [Google Scholar]
Nandhakumar 2008 {published data only}
- Nandhakumar, B, Menon, T, Ravishankar, G, & Shanmugasundaram, S. Pacemaker pocket infection associated with septicemia caused by Pseudomonas aeruginosa. International Journal of Infectious Diseases 2008;12(1):107-108. [DOI] [PubMed] [Google Scholar]
Nessler 1999 {published data only}
- Nessler, J, Piwowarska, W, Broda, K, Nessler, B, Matysek, J, Czubek, U, Garlicki, M, & Dziatkowiak, A. The clinical course of end stage heart disease in 152 patients qualified for heart transplantation in a four year observation. Przeglad Lekarski 1999;56(9):557-561. [PubMed] [Google Scholar]
Niki 1999 {published data only}
- Niki, K, Sugawara, M, Tanino, S, Iwade, K, Hosoda, S, & Kasanuki, H. An equation to predict the changes in peak left ventricular pressure in hypertrophic obstructive cardiomyopathy after treatment: application to the administration of disopyramide. Heart & Vessels 1999;14(2):72-81. [DOI] [PubMed] [Google Scholar]
Nishimura 1993 {published data only}
- Nishimura, R A & Danielson, G K. Dual chamber pacing for hypertrophic obstructive cardiomyopathy: has its time come? British Heart Journal 1993;70(4):301-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nishimura 1996 {published data only}
- Nishimura, R A, Hayes, D L, Ilstrup, D M, Holmes, D R Jr, & Tajik, A J. Effect of dual-chamber pacing on systolic and diastolic function in patients with hypertrophic cardiomyopathy. Acute Doppler echocardiographic and catheterization hemodynamic study. Journal of the American College of Cardiology 1996;27(2):421-430. [DOI] [PubMed] [Google Scholar]
Nishimura 1996b {published data only}
- Nishimura, R A, Symanski, J D, Hurrell, D G, Trusty, J M, Hayes, D L, & Tajik, A J. Dual-chamber pacing for cardiomyopathies: A 1996 clinical perspective. Mayo Clinic Proceedings 1996;71(11):1077-1087. [DOI] [PubMed] [Google Scholar]
Nishimura 2004 {published data only}
- Nishimura, R A & Holmes, D R Jr. Clinical practice. Hypertrophic obstructive cardiomyopathy. New England Journal of Medicine 2004;350(13):1320-1327. [DOI] [PubMed] [Google Scholar]
Nowinski 2005 {published data only}
- Nowinski, K, Wecke, L, Gadler, F, Linde, C, & Bergfeldt, L. Pacing-induced electrophysiological remodeling in hypertrophic obstructive cardiomyopathy--observations on cardiac memory. Pacing & Clinical Electrophysiology 2005;28(6):561-567. [DOI] [PubMed] [Google Scholar]
Ohtani 2003 {published data only}
- Ohtani, K, Satoh, A, Eto, S, Satoh, T, Ichinose, K, Satoh, S, Takahashi, T, Koda, M, Kinjo, M, & Yonesaka, S. Dual-chamber pacing in hypertrophic obstructive cardiomyopathy with biventricular outflow tract obstruction and severe drug-refractory symptoms in a 9-year-old girl. Pediatrics International 2003;45(6):743-746. [DOI] [PubMed] [Google Scholar]
Oka 2007 {published data only}
- Oka, N, Ohmura, H, & Ueda, T. Heart failure associated with hypertrophic cardiomyopathy. Nippon Rinsho - Japanese Journal of Clinical Medicine 2007;65:Suppl-9. [PubMed] [Google Scholar]
Ommen 1999 {published data only}
- Ommen, S R, Nishimura, R A, Squires, R W, Schaff, H V, Danielson, G K, & Tajik, A J. Comparison of dual-chamber pacing versus septal myectomy for the treatment of patients with hypertrophic obstructive cardiomyopathy: a comparison of objective hemodynamic and exercise end points. Journal of the American College of Cardiology 1999;34(1):191-196. [DOI] [PubMed] [Google Scholar]
Ovsyshcher 2004 {published data only}
- Ovsyshcher, I E & Barold, S S. Drug induced bradycardia: to pace or not to pace? Pacing & Clinical Electrophysiology 2004;27(8):1144-1147. [DOI] [PubMed] [Google Scholar]
Pace 1994 {published data only}
- Pace, L, Betocchi, S, Franculli, F, Piscione, F, Ciarmiello, A, Sullo, P, Chiariello, M, & Salvatore, M. Evaluation of left ventricular asynchrony by radionuclide angiography: comparison of phase and sector analysis. Journal of Nuclear Medicine 1994;35(11):1766-1770. [PubMed] [Google Scholar]
Pak 1998 {published data only}
- , P H, Maughan, W L, Baughman, K L, Kieval, R S, & Kass, D A. Mechanism of acute mechanical benefit from VDD pacing in hypertrophied heart: similarity of responses in hypertrophic cardiomyopathy and hypertensive heart disease. Circulation 1998;98(3):242-248. [DOI] [PubMed] [Google Scholar]
Park 1999 {published data only}
- Park, M H, Gilligan, D M, Bernardo, N L, & Topaz, O. Symptomatic hypertrophic obstructive cardiomyopathy: the role of dual-chamber pacing. Angiology 1999;50(2):87-94. [DOI] [PubMed] [Google Scholar]
Pasternac 1982 {published data only}
- Pasternac, A, Noble, J, Streulens, Y, Elie, R, Henschke, C, & Bourassa, M G. Pathophysiology of chest pain in patients with cardiomyopathies and normal coronary arteries. Circulation 1982;65(4):778-789. [DOI] [PubMed] [Google Scholar]
Paulus 1988 {published data only}
- Paulus, W J, Sys, S U, Nellens, P, Heyndrickx, G R, & Andries, E. Postextrasystolic potentiation worsens fast filling of the hypertrophied left ventricle in aortic stenosis and hypertrophic cardiomyopathy. Circulation 1988;78(4):928-940. [DOI] [PubMed] [Google Scholar]
Posma 1996 {published data only}
- Posma, J L, Blanksma, P K, Van Der Wall, E E, Vaalburg, W, Crijns, H J G M, & Lie, K I. Effects of permanent dual chamber pacing on myocardial perfusion in symptomatic hypetrophic cardiomyopathy. Heart 1996;76(4):358-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ralph‐Edwards 2005 {published data only}
- Ralph-Edwards, A, Woo, A, McCrindle, B W, Shapero, J L, Schwartz, L, Rakowski, H, Wigle, E D, & Williams, W G. Hypertrophic obstructive cardiomyopathy: comparison of outcomes after myectomy or alcohol ablation adjusted by propensity score. Journal of Thoracic & Cardiovascular Surgery 2005;129(2):351-358. [DOI] [PubMed] [Google Scholar]
Reith 2003 {published data only}
- Reith, S & Klues, H G. "[Therapy and risk-stratification in hypertrophic cardiomyopathy--a current survey].. Zeitschrift fur Kardiologie 2003;92(4):283-293. [DOI] [PubMed] [Google Scholar]
Rousseau 1980 {published data only}
- Rousseau, M F, Pouleur, H, Detry, J M, & Brasseur, L A. Increased sensitivity of left ventricular relaxation to inotropic interventions in patients with coronary artery disease: comparison with normal subjects, mitral stenosis and asymmetric septal hypertrophy. European Heart Journal 1980;1:B-41. [DOI] [PubMed] [Google Scholar]
Ryden 2001 {published data only}
- Ryden, L & Gadler, F. Pharmacological therapy for hypertrophic cardiomyopathy: What is the evidence for success? European Heart Journal 2001;3:L21-L25. [Google Scholar]
Saumarez 1992 {published data only}
- Saumarez, R C, Camm, A J, Panagos, A, Gill, J S, Stewart, J T, de Belder, M A, Simpson, I A, & McKenna, W J. Ventricular fibrillation in hypertrophic cardiomyopathy is associated with increased fractionation of paced right ventricular electrograms. Circulation 1992;86(2):467-474. [DOI] [PubMed] [Google Scholar]
Saumarez 1995 {published data only}
- Saumarez, R C, Slade, A K, Grace, A A, Sadoul, N, Camm, A J, & McKenna, W J. The significance of paced electrogram fractionation in hypertrophic cardiomyopathy. A prospective study. Circulation 1995;91(11):2762-2768. [DOI] [PubMed] [Google Scholar]
Saumarez 2003 {published data only}
- Saumarez, R C, Chojnowska, L, Derksen, R, Pytkowski, M, Sterlinski, M, Huang, C L, Sadoul, N, Hauer, R N, Ruzyllo, W, & Grace, A A. Sudden death in noncoronary heart disease is associated with delayed paced ventricular activation. Circulation 2003;107(20):2595-2600. [DOI] [PubMed] [Google Scholar]
Saumarez 2008 {published data only}
- Saumarez, R C, Pytkowski, M, Sterlinski, M, Bourke, J P, Clague, J R, Cobbe, S M, Connelly, D T, Griffith, M J, McKeown, P P, McLeod, K, Morgan, J M, Sadoul, N, Chojnowska, L, Huang, C L, & Grace, A A. Paced ventricular electrogram fractionation predicts sudden cardiac death in hypertrophic cardiomyopathy. European Heart Journal 2008;29(13):1653-1661. [DOI] [PubMed] [Google Scholar]
Schulte 1999 {published data only}
- Schulte, H D, Gramsch-Zabel, H, Schwartzkopff, B, & Gams, E. [Hypertrophic cardiomyopathy (HCM). Surgical versus drug therapy].. Zeitschrift fur Kardiologie 1999;88(3):163-172. [DOI] [PubMed] [Google Scholar]
Seggewiss 1998 {published data only}
- Seggewiss, H, Gleichmann, U, Faber, L, Fassbender, D, Schmidt, H K, & Strick, S. Percutaneous transluminal septal myocardial ablation in hypertrophic obstructive cardiomyopathy: acute results and 3-month follow-up in 25 patients. Journal of the American College of Cardiology 1998;31(2):252-258. [DOI] [PubMed] [Google Scholar]
Seggewiss 2003 {published data only}
- Seggewiss, H & Rigopoulos, A. Management of hypertrophic cardiomyopathy in children. Paediatric Drugs 2003;5(10):663-672. [DOI] [PubMed] [Google Scholar]
Seggewiss 2007 {published data only}
- Seggewiss, H, Rigopoulos, A, Welge, D, Ziemssen, P, & Faber, L. Long-term follow-up after percutaneous septal ablation in hypertrophic obstructive cardiomyopathy. Clinical Research in Cardiology 2007;96(12):856-863. [DOI] [PubMed] [Google Scholar]
Shamim 2002 {published data only}
- Shamim, W, Yousufuddin, M, Wang, D, Henein, M, Seggewiss, H, Flather, M, Coats, A J S, & Sigwart, U. Nonsurgical reduction of the interventricular septum in patients with hypertrophic cardiomyopathy. New England Journal of Medicine 2002;347(17):1326-1333. [DOI] [PubMed] [Google Scholar]
Shefer 1987 {published data only}
- Shefer, A, Rozenman, Y, Ben, D Y, Flugelman, M Y, Gotsman, M S, & Lewis, B S. Left ventricular function during physiological cardiac pacing: relation to rate, pacing mode, and underlying myocardial disease. Pacing & Clinical Electrophysiology 1987;10(2):315-325. [DOI] [PubMed] [Google Scholar]
Sherrid 2005 {published data only}
- Sherrid, M V, Barac, I, McKenna, W J, Elliott, P M, Dickie, S, Chojnowska, L, Casey, S, & Maron, B J. Multicenter study of the efficacy and safety of disopyramide in obstructive hypertrophic cardiomyopathy. Journal of the American College of Cardiology 2005;45(8):1251-1258. [DOI] [PubMed] [Google Scholar]
Silva 2008 {published data only}
- Silva, L A A, Fernandez, E A, Martinelli, M, Costa, R, Siqueira, S, Ianni, R M, & Mady, C. Cardiac Pacing in Hypertrophic Cardiomyopathy. A Cohort with 24 Years of Follow-Up. Arquivos Brasileiros de Cardiologia 2008;91(4):250-256. [PubMed] [Google Scholar]
Slade 1996 {published data only}
- Slade, A K, Sadoul, N, Shapiro, L, Chojnowska, L, Simon, J P, Saumarez, R C, Dodinot, B, Camm, A J, McKenna, W J, & Aliot, E. DDD pacing in hypertrophic cardiomyopathy: a multicentre clinical experience. Heart 1996;75(1):44-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Slade 1996b {published data only}
- Slade, A K B & McKenna, W J. Pitfalls of pacemaker treatment for hypertrophic cardiomyopathy. Journal of Interventional Cardiology 1996;9(5):405-411. [Google Scholar]
Solomon 1999 {published data only}
- Solomon, A J & Gersh, B J. Effect of recent randomized trials on current pacing practice.. Cardiology in Review 1999;7(1):9-16. [DOI] [PubMed] [Google Scholar]
Somura 2001 {published data only}
- Somura, F, Izawa, H, Iwase, M, Takeichi, Y, Ishiki, R, Nishizawa, T, Noda, A, Nagata, K, Yamada, Y, & Yokota, M. Reduced myocardial sarcoplasmic reticulum Ca(2+)-ATPase mRNA expression and biphasic force-frequency relations in patients with hypertrophic cardiomyopathy. Circulation 2001;104(6):658-663. [DOI] [PubMed] [Google Scholar]
Sorajja 2000 {published data only}
- Sorajja, P, Elliott, P M, & McKenna, W J. Pacing in hypertrophic cardiomyopathy. Cardiology Clinics 2000;18(1):67-79. [DOI] [PubMed] [Google Scholar]
Spirito 1997 {published data only}
- Spirito, P, Seidman, C E, McKenna, W J, & Maron, B J. The management of hypertrophic cardiomyopathy. New England Journal of Medicine 1997;336(11):775-785. [DOI] [PubMed] [Google Scholar]
Spirito 1999 {published data only}
- Spirito, P & Maron, B J. Perspectives on the role of new treatment strategies in hypertrophic obstructive cardiomyopathy. Journal of the American College of Cardiology 1999;33(4):1071-1075. [DOI] [PubMed] [Google Scholar]
Sud 2007 {published data only}
- Sud, S, Massel, D, Klein, G J, Leong-Sit, P, Yee, R, Skanes, A C, Gula, L J, & Krahn, A D. The expectation effect and cardiac pacing for refractory vasovagal syncope. American Journal of Medicine 2007;120(1):54-62. [DOI] [PubMed] [Google Scholar]
Syed 2004 {published data only}
- Syed, J & Myers, R. Sarcoid heart disease. Canadian Journal of Cardiology 2004;20(1):89-93. [PubMed] [Google Scholar]
Takechi 2003 {published data only}
- Takechi, S, Nomura, A, Machida, M, Fujimoto, T, Kakinoki, S, Komuro, K, & Kitabatake, A. Different coronary blood flow increase in left ventricular hypertrophy due to hypertension compared to hypertrophic cardiomyopathy at elevated heart rate. Hypertension Research - Clinical & Experimental 2003;26(10):789-793. [DOI] [PubMed] [Google Scholar]
Talreja 2004 {published data only}
- Talreja, D R, Nishimura, R A, Edwards, W D, Valeti, U S, Ommen, S R, Tajik, A J, Dearani, J A, Schaff, H V, & Holmes, D R. Alcohol septal ablation versus surgical septal myectomy: comparison of effects on atrioventricular conduction tissue. Journal of the American College of Cardiology 2004;44(12):2329-2332. [DOI] [PubMed] [Google Scholar]
Tascon 1995 {published data only}
- Tascon, J C, Albarran, A, Andreu, J, & Alonso, M. Early surgical treatment of symptomatic hypertrophic obstructive myocardiopathy. Arguments against. Revista Espanola de Cardiologia 1995;48(4):229-234. [PubMed] [Google Scholar]
Thompson 1980 {published data only}
- Thompson, D S, Naqvi, N, Juul, S M, Swanton, R H, Coltart, D J, Jenkins, B S, & Webb-Peploe, M M. Effects of propranolol on myocardial oxygen consumption, substrate extraction, and haemodynamics in hypertrophic obstructive cardiomyopathy. British Heart Journal 1980;44(5):488-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thompson 1983 {published data only}
- Thompson, D S, Wilmshurst, P, Juul, S M, Waldron, C B, Jenkins, B S, Coltart, D J, & Webb-Peploe, M M. Pressure-derived indices of left ventricular isovolumic relaxation in patients with hypertrophic cardiomyopathy. British Heart Journal 1983;49(3):259-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Topaz 1989 {published data only}
- Topaz, O, Perin, E, Cox, M, Mallon, S M, Castellanos, A, & Myerburg, R J. Young adult survivors of sudden cardiac arrest: analysis of invasive evaluation of 22 subjects. American Heart Journal 1989;118(2):281-287. [DOI] [PubMed] [Google Scholar]
Topilski 2006 {published data only}
- Topilski, I, Sherez, J, Keren, G, & Copperman, I. Long-term effects of dual-chamber pacing with periodic echocardiographic evaluation of optimal atrioventricular delay in patients with hypertrophic cardiomyopathy > 50 years of age. American Journal of Cardiology 2006;97(12):1769-1775. [DOI] [PubMed] [Google Scholar]
Trohman 2004 {published data only}
- Trohman, R G, Kim, M H, & Pinski, S L. Cardiac pacing: the state of the art. Lancet 2004;364(9446):1701-1719. [DOI] [PubMed] [Google Scholar]
Unno 2009 {published data only}
- Unno, K, Isobe, S, Izawa, H, Cheng, X W, Kobayashi, M, Hirashiki, A, Yamada, T, Harada, K, Ohshima, S, Noda, A, Nagata, K, Kato, K, Yokota, M, & Murohara, T. Relation of functional and morphological changes in mitochondria to myocardial contractile and relaxation reserves in asymptomatic to mildly symptomatic patients with hypertrophic cardiomyopathy. European Heart Journal 2009;30(15):1853-1862. [DOI] [PubMed] [Google Scholar]
van der 2005 {published data only}
- van der, L C, ten Cate, F J, Geleijnse, M L, Kofflard, M J, Pedone, C, van Herwerden, L A, Biagini, E, Vletter, W B, & Serruys, P W. Percutaneous versus surgical treatment for patients with hypertrophic obstructive cardiomyopathy and enlarged anterior mitral valve leaflets. Circulation 2005;112(4):482-488. [DOI] [PubMed] [Google Scholar]
Vazquez 2001 {published data only}
- Vazquez, P M, Pichardo, R B, Gamero, J V, Saiz, A A, Lozano, V M, Gomez, J M F, & Carranza, M H. Permanent pacing of the His bundle after radiofrequency atrioventricular node ablation in patients with suprahisian conduction disturbances. Revista Espanola de Cardiologia 2001;54(12):1385-1393. [DOI] [PubMed] [Google Scholar]
Venugopa 2007 {published data only}
- Venugopal, D, Jhanjee, R, & Benditt, D G. Current management of syncope: Focus on drug therapy. American Journal of Cardiovascular Drugs 2007;7(6):399-411. [DOI] [PubMed] [Google Scholar]
Watson 1987 {published data only}
- Watson, R M, Schwartz, J L, Maron, B J, Tucker, E, Rosing, D R, & Josephson, M E. Inducible polymorphic ventricular tachycardia and ventricular fibrillation in a subgroup of patients with hypertrophic cardiomyopathy at high risk for sudden death. Journal of the American College of Cardiology 1987;10(4):761-774. [DOI] [PubMed] [Google Scholar]
Weiner 1999 {published data only}
- Weiner, S, Zweibel, S L, & Gross, J N. Current perspectives on pacing therapy in cardiomyopathies. Cardiology in Review 1999;7(2):71-76. [DOI] [PubMed] [Google Scholar]
Weiss 1976 {published data only}
- Weiss, M B, Ellis, K, Sciacca, R R, Johnson, L L, Schmidt, D H, & Cannon, P J. Myocardial blood flow in congestive and hypertrophic cardiomyopathy: relationship to peak wall stress and mean velocity of circumferential fiber shortening. Circulation 1976;54(3):484-494. [DOI] [PubMed] [Google Scholar]
Wexler 2009 {published data only}
- Wexler, R, Elton, T, Pleister, A, & Feldman, D. Cardiomyopathy: An overview. American Family Physician 2009;79(9):778-784. [PMC free article] [PubMed] [Google Scholar]
Yamakado 1990 {published data only}
- Yamakado, T, Okano, H, Higashiyama, S, Hamada, M, Nakano, T, & Takezawa, H. Effects of nifedipine on left ventricular diastolic function in patients with asymptomatic or minimally symptomatic hypertrophic cardiomyopathy. Circulation 1990;81(2):593-601. [DOI] [PubMed] [Google Scholar]
Zeng 2006 {published data only}
- Zeng, Z, Wang, F, Dou, X, Zhang, S, & Pu, J. Comparison of percutaneous transluminal septal myocardial ablation versus septal myectomy for the treatment of patients with hypertrophic obstructive cardiomyopathy--a meta analysis. International Journal of Cardiology 2006;112(1):80-84. [DOI] [PubMed] [Google Scholar]
Additional references
Autore 2005
- Autore C, Bernabò P, Barillà CS, Bruzzi P, Spirito P. The prognostic importance of left ventricular outflow obstruction in hypertrophic cardiomyopathy varies in relation to the severity of symptoms. Journal of the American College of Cardiology 2005;45:1076. [DOI] [PubMed] [Google Scholar]
Bernstein 1987
- Bernstein AD, Camm AJ, Fletcher RD. The NASPE/BPEG generic pacemaker code for antibradyarrhythmia and adaptive-rate pacing and antitachyarrhythmia devices. Pacing and Clinical Electrophysiology 1987;10(4 I):794-9. [DOI] [PubMed] [Google Scholar]
Bernstein 2002
- Bernstein AD, Daubert JC, Fletcher RD, Hayes DL, Lüderitz B, Reynolds DW, et al. revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. Pacing and Clinical Electrophysiology 2002;25(2):260-4. [DOI] [PubMed] [Google Scholar]
Boltwood 2004
- Boltwood CM Jr, Chien W, Ports, T. Ventricular tachycardia complicating alcohol septal ablation. New England Journal of Medicine 2004;351:1914-5. [DOI] [PubMed] [Google Scholar]
Bonow 1985b
- Bonow RO, Dilsizian V, Rosing DR, Maron BJ, Bacharach SL, Green MV. Verapamil-induced improvement in left ventricular diastolic filling and increased exercise tolerance in patients with hypertrophic cardiomyopathy: short- and long-term effects. Circulation 1985;72(4):853-64. [DOI] [PubMed] [Google Scholar]
Bush 1994
- Bush DE, Finucane TE. Permanent cardiac pacemakers in the elderly. Journal of the American Geriatrics Society 1994;42(3):326-34. [DOI] [PubMed] [Google Scholar]
Clarke 1991
- Clarke M, Sutton R, Ward D, Camm AJ, Rickards A, Ingram A, et al. Recommendations for pacemaker prescription for symptomatic bradycardia. British Heart Journal 1991;66:185-91. [PMC free article] [PubMed] [Google Scholar]
Clinical Evidence
- BMJ Clinical Evidence. EBM Tools: Glossary. http://clinicalevidence.bmj.com/ceweb/resources/glossary.jsp#Random_effects (accessed 16 January 2010).
Clinical Practice Guideline 2003
- Maron BJ, McKenna WJ, Danielson GK, Kappenberger LJ, Kuhn HJ, Seidman CE, Shah PM, Spencer WH 3rd, Spirito P, Ten Cate FJ, Wigle ED. ACC/ESC clinical expert consensus document on hypertrophic cardiomyopathy: a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines.. Eur Heart J 2003;24:1965-1991. [DOI] [PubMed] [Google Scholar]
Clinical Practice Guidline 2003b
- Maron BJ, McKenna WJ, Danielson GK, Kappenberger LJ, Kuhn HJ, Seidman CE, Shah PM, Spencer WH 3rd, Spirito P, Ten Cate FJ, Wigle ED. ACC/ESC expert consensus document: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines.. J Am Coll Cardiol 2003;42:1687-1713. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elliotte 2006
- Elliott PM, Gimeno JR, Thaman R, Shah J, Ward D, Dickie S, et al. Historical trends in reported survival rates in patients with hypertrophic cardiomyopathy. Heart 2006;92:785-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Epstein 2008
- Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA 3rd, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation 2008;117:2820-40. [DOI] [PubMed]
Falicov 1977
- Falicaov RE, Resnekov L. Midventricular obstruction in hypertrophic obstructive cardiomyopathy: new diagnostic and therapeutic challenge. British Heart Journal 1977;39:701-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fananapazir 1992
- Fananapazir L, Chang AC, Epstein SE, McAreavey DSO. Prognostic determinants in hypertrophic cardiomyopathy. Prospective evaluation of a therapeutic strategy based on clinical, Holter, hemodynamic, and electrophysiological findings. Circulation 1992;86(3):730-40. [DOI] [PubMed] [Google Scholar]
Fananapazir 1994
- Fananapazir L, Epstein N, Curiel R, Panza J, Tripodi D, McAreavey D. Long-term results of dual-chamber (DDD) pacing in obstructive hypertrophic cardiomyopathy. Circulation 1994;90(6):2731-42. [DOI] [PubMed] [Google Scholar]
Fifer 2008
- Fifer MA, Vlahakes GJ. Management of symptoms in hypertrophic cardiomyopathy. Circulation 2008;117(3):429-39. [DOI] [PubMed] [Google Scholar]
Fighali 1987
- Fighali S, Krajcer Z, Edelman S, Leachman RD. Progression of hypertrophic cardiomyopathy into a hypokinetic left ventricle: higher incidence in patients with mid-ventricular obstruction. Journal of the American College of Cardiology 1987;9:288-94. [DOI] [PubMed] [Google Scholar]
Furman 1977
- Furman, S. Cardiac pacing and pacemakers VI. Analysis of pacemaker malfunction. Am Heart J 1977;49:378. [DOI] [PubMed] [Google Scholar]
Hada 1987
- Hada, Y, Sakamoto, T, Amano, K. Prevalence of hypertrophic cardiomyopathy in a population of adult Japanese workers as detected by echocardiographic screening. Am J Cardiol 1987;59:183. [DOI] [PubMed] [Google Scholar]
Harris 2006
- Harris KM, Spirito P, Maron MS, Zenovich AG, Formisano F, Lesser JR, et al. Prevalence, clinical profile, and significance of left ventricular remodeling in the end-stage phase of hypertrophic cardiomyopathy. Circulation 2006;114:216-25. [DOI] [PubMed] [Google Scholar]
Hauser 1983
- Hauser RG. The electrocardiography of AV universal DDD pacemakers. Pacing Clin Electrophysiol 1983;6:399-409. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0. The Cochrane Collaboration, 2008. Available from www.cochrane-handbook.org, Updated September 2009. [Google Scholar]
Kappenberger 1997b
- Kappenberger, L, Linde, C, Daubert, C, McKenna, W, Meisel, E, Aliot, E, Chajnovska, L, Guize, M, Jeanrenaud, X, & Gras, D. Pacing in hypertrophic obstructive cardiomyopathy. American College of Cardiology (Meeting Abstract) 1997;29(2):7961.
Kubo 2007
- Kubo T, Kitaoka H, Okawa M, Matsumura Y, Hitomi N, Yamasaki N, et al. Lifelong left ventricular remodeling of hypertrophic cardiomyopathy caused by a founder frameshift deletion mutation in the cardiac Myosin-binding protein C gene among Japanese. Journal of the American College of Cardiology 2005;46:1737-43. [DOI] [PubMed] [Google Scholar]
Levine 2002
- Levine, PA. Differential diagnosis, evaluation and management of pacing system malfunction. Cardiac pacing, Ellenbogen, K, Wood, M, (Eds), Blackwell Scientific Publications, Boston 2002:345.
Linde 1999
- Linde, C, Gadler, F, Kappenberger, L, & Ryden, L. Placebo effect of pacemaker implantation in obstructive hypertrophic cardiomyopathy. PIC Study Group. Pacing In Cardiomyopathy. American Journal of Cardiology 1999;83(6):903-907. [DOI] [PubMed] [Google Scholar]
Maron 1986
- Maron BJ, Spirito P, Wesley Y, Arce J. Development and progression of left ventricular hypertrophy in children with hypertrophic cardiomyopathy: identification by two-dimensional echocardiography. New England Journal of Medicine 1986;315:610-4. [DOI] [PubMed] [Google Scholar]
Maron 1987a
- Maron BJ, Bonow RO, Cannon RO, Leon MB, Epstein SE. Hypertrophic cardiomyopathy. Interrelations of clinical manifestations, pathophysiology, and therapy (2). New England Journal of Medicine 1987;316:844-52. [DOI] [PubMed] [Google Scholar]
Maron 1987b
- Maron BJ, Bonow RO, Cannon RO, Leon MB, Epstein SE. Hypertrophic cardiomyopathy. Interrelation of clinical manifestation, pathophysiology, and therapy. New England Journal of Medicine 1987;316:780-9. [DOI] [PubMed] [Google Scholar]
Maron 1999 a
- Maron BJ, Casey SA, Poliac LC, Gohman TE, Almquist AK, Aeppli DM. Clinical course of hypertrophic cardiomyopathy in a regional United States cohort. JAMA 1999;281:650-5. [DOI] [PubMed] [Google Scholar]
Maron 1999c
- Maron BJ, Mathenge R, Casey SA, Poliac LC, Longe TF. Clinical profile of hypertrophic cardiomyopathy identified de novo in rural communities. J Am Coll Cardiol 1999;33(6):1590-5. [DOI] [PubMed] [Google Scholar]
Maron 2000
- Maron BJ, Olivotto I, Spirito P, Casey SA, Bellone P, Gohman TE, et al. Epidemiology of hypertrophic cardiomyopathy-related death: revisited in a large non-referral-based patient population. Circulation 2000;102:858. [DOI] [PubMed] [Google Scholar]
Maron 2003
- Maron BJ, Casey SA, Hauser RG, Aeppli DM. Clinical course of hypertrophic cardiomyopathy with survival to advanced age. Journal of the American College of Cardiology 2003;42:882. [DOI] [PubMed] [Google Scholar]
Maron 2004
- Maron BJ, Dearani JA, Ommen SR, Maron MS, Schaff HV, Gersh BJ, et al. The case for surgery in obstructive hypertrophic cardiomyopathy. Journal of the American College of Cardiology 2004;44(10):2044-53. [DOI] [PubMed] [Google Scholar]
McKenna 1981
- McKenna W, Deanfield J, Faruqui A, England D, Oakley C, Goodwin J. Prognosis in hypertrophic cardiomyopathy. Role of age and clinical, electrocardiographic and haemodynamic features. American Journal of Cardiology 1981;47(3):532-8. [DOI] [PubMed] [Google Scholar]
McKenna 1984
- McKenna WJ, Deanfield JE. Hypertrophic cardiomyopathy: an important cause of sudden death. Archives of Disease in Childhood 1984;59(10):971-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKenna 1988
- McKenna WJ, Franklin RC, Nihoyannopoulos P, Robinson KC, Deanfield JE. Arrhythmia and prognosis in infants, children and adolescents with hypertrophic cardiomyopathy. Journal of the American College of Cardiology 1988;11(1):147-53. [DOI] [PubMed] [Google Scholar]
Meisel 1999
- Meisel, E, Rauwolf, T, Burghardt, M, & Kappenberger, L. Pacemaker therapy for hypertrophic-obstructive cardiomyopathy. Herzschrittmachertherapie und Elektrophysiologie 1999;2:58-68. [Google Scholar]
Meisel 2000
- Meisel, E, Rauwolf, T, Burghardt, M, & Kappenberger, L Herz 2000, 25(4):461-466. DDD pacemakers in hypertrophic obstructive cardiomyopathy (EMBASE) [Schrittmacher-Therpaie der Hypertroph-Obstruktiven Kardiomyopathie]. Herz 2000;25(4):461-466. [PubMed] [Google Scholar]
Miesel 2000a
- Meisel, E, Rauwolf, T, Burghardt, M, & Kappenberger, L. Pacemaker therapy of hypertrophic obstructive cardiomyopathy. PIC (Pacing in Cardiomyopathy) Study Group (Medline) [Schrittmacher-Therapie der Hypertoph-Obstruktiven Kardiomyopathie]. Herz 2000;25(4):461-466. [PubMed] [Google Scholar]
Moher 1998
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analysis. Lancet 1998;352:609-13. [DOI] [PubMed] [Google Scholar]
Mond 1983
- Mond, HG. The cardiac pacemaker, function and malfunction. Grune & Stratton, New York 1983.
Nishimura 2004b
- Rick A Nishimura, MD, and David R Holmes Jr, MDN. Hypertrophic Obstructive Cardiomyopathy. Engl J Med 2004;350:1320-1327. [DOI] [PubMed] [Google Scholar]
Olivotto 2006
- Olivotto I, Cecchi F, Gistri R, Lorenzoni R, Chiriatti G, Girolami F, et al. Relevance of coronary microvascular flow impairment to long-term remodeling and systolic dysfunction in hypertrophic cardiomyopathy. Journal of the American College of Cardiology 2006;47:1043-8. [DOI] [PubMed] [Google Scholar]
Panza 1992a
- Panza JA, Petrone RK, Fananapazir L, Maron BJ. Utility of continuous wave Doppler echocardiography in the non-invasive assessment of left ventricular outflow tract pressure gradient in patient with hypertrophic cardiomyopathy. Journal of the American College of Cardiology 1992;19:91-9. [DOI] [PubMed] [Google Scholar]
Panza 1992b
- Panza JA, Maris TJ, Maron BJ. Development and determinants of dynamic obstruction to left ventricular outflow in young patients with hypertrophic cardiomyopathy. Circulation 1992;85:1398-405. [DOI] [PubMed] [Google Scholar]
Pollick 1982
- Pollick C, Morgan CD, Gilbert BW, Rakowski H, Wigle ED. Muscular subaortic stenosis: the temporal relation between systolic anterior motion of the anterior mitral valve leaflet and the pressure gradient. Circulation 1982;66:1087-94. [DOI] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan) [Computer program].. Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Richardson 1996
- Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O'Connell J, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation 1996;93:841-2. [DOI] [PubMed] [Google Scholar]
Romeo 1990
- Romeo F, Pelliccia F, Cristofani R, Martuscelli E, Reale A. Hypertrophic cardiomyopathy: is a left ventricular outflow tract gradient a major prognostic determinant? European Heart Journal 1990;11(3):233-40. [DOI] [PubMed] [Google Scholar]
Rosing 1985
- Rosing DR, Idanpaan-Heikkila U, Maron BJ, Bonow RO, Epstein SESO. Use of calcium-channel blocking drugs in hypertrophic cardiomyopathy. American Journal of Cardiology 1985;55(3):185B-195B. [DOI] [PubMed] [Google Scholar]
Royle 2003
- Royle P, Milne R. Literature searching for randomized controlled trials used in Cochrane reviews: rapid versus exhaustive searches. International Journal of Technology Assessment in Health Care 2003;19(4):591-603. [DOI] [PubMed] [Google Scholar]
Sherrid 1998
- Sherrid MV, Pearle G, Gunsburg DZ. Mechanism of benefit of negative inotropes in obstructive hypertrophic cardiomyopathy. Circulation 1998;97:41-7. [DOI] [PubMed] [Google Scholar]
Siegman 1989
- Siegman IL, Maron BJ, Permut LC, McIntosh CL, Clark RE. Results of operation for coexistent obstructive hypertrophic cardiomyopathy and coronary artery disease. Journal of the American College of Cardiology 1989;13(7):1527-33. [DOI] [PubMed] [Google Scholar]
Spirito 1987
- Spirito P, Maron BJ, Bonow RO, Epstein SE. Occurrence and significance of progressive left ventricular wall thinning and relative cavity dilatation in hypertrophic cardiomyopathy. American Journal of Cardiology 1987;60:123-9. [DOI] [PubMed] [Google Scholar]
Takagi 1999
- Takagi E, Yamakado T, Nakano T. Prognosis of completely asymptomatic adult patients with hypertrophic cardiomyopathy. Journal of the American College of Cardiology 1999;33:206-11. [DOI] [PubMed] [Google Scholar]
ten Berg 1994
- ten Berg JM, Suttorp MJ, Knaepen PJ, Ernst SM, Vermeulen FE, Jaarsma W. Hypertrophic obstructive cardiomyopathy. Initial results and long-term follow-up after Morrow septal myectomy. Circulation 1994;90(4):1781-5. [DOI] [PubMed] [Google Scholar]
Watkins 1995
- Watkins H, Seidman JG, Seidman CE. Familial hypertrophic cardiomyopathy: a genetic model of cardiac hypertrophy. Human Molecular Genetics 1995;4:1721-7. [DOI] [PubMed] [Google Scholar]
Zou 2004
- Zou Y, Song L, Wang Z, Ma A, Liu T, Gu H, Lu S, Wu P, Zhang dagger Y, Shen dagger L, Cai Y, Zhen double dagger Y, Liu Y, Hui R. Prevalence of idiopathic hypertrophic cardiomyopathy in China: a population-based echocardiographic analysis of 8080 adults.. Am J Med 2004;116(1):14-8. [DOI] [PubMed] [Google Scholar]


