CLINICAL HISTORY
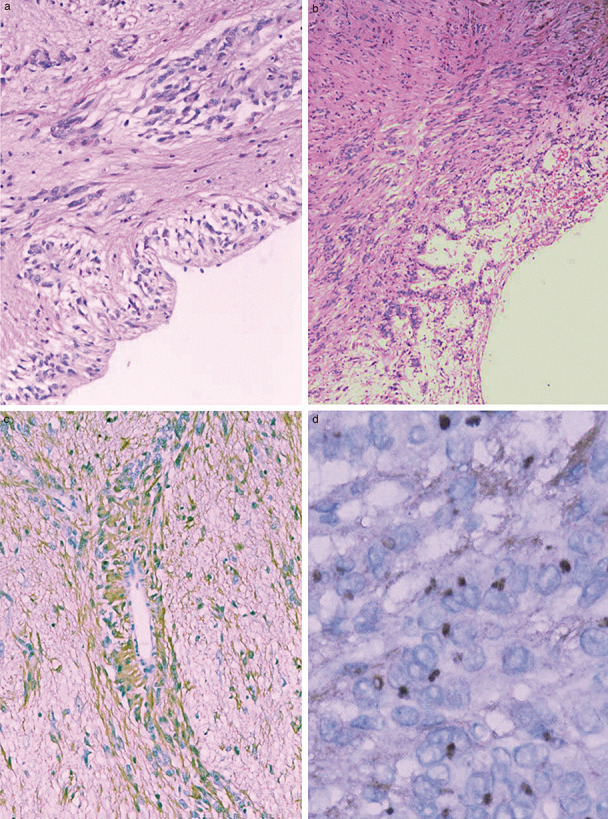
A 25‐year‐old woman had a history of 4 episodes of epilepsy over two years without treatment. MRI showed that there was a solid circumscribed, hyperintense and nonenhancing tumor (fig 1) measuring 6 × 4 × 4 cm in the hippocampus. T1‐weighted and T2‐weighted scans showed mixed signals without calcification in the tumor and no peritumoral edema. The tumor was totally resected. Macroscopically, the surgical sample was bits and pieces. Histologically, the tumor included glial, neuronal and mixed glioneuronal populations. The spindle‐shaped tumor cells showed diffuse growth and displayed characteristic angiocentric arrangements around small parenchymal vessels forming perivascular pseudorosettes. There were single or multilayered tumor cells arranged with ependymal features (fig 2). The tumor cells of the hippocampal surface formed distinctive rosettes (fig 3a) which have not been previously described. The spindle tumor cells were bipolar with elongated nuclei and inconspicuous nucleoli. In some areas, the tumor cells were schwannoma‐like (fig 3b). We could find single neurons interspersed within the tumor tissue. Necrosis and mitotic activity were absence. Immunohistochemistry was positive for GFAP (fig 3c), Vimentin and S‐100 and negative for neurofilament protein, Syn, CgA and NeuN. EMA showed “dot‐like” positive staining (fig 3d). The proliferation index was less than 1%. Epilepsy disappeared after the operation. We only follow‐up four months till now and there was no evidence of recurrence on MRI at a four month follow‐up. What is the diagnosis?
Figure 1.
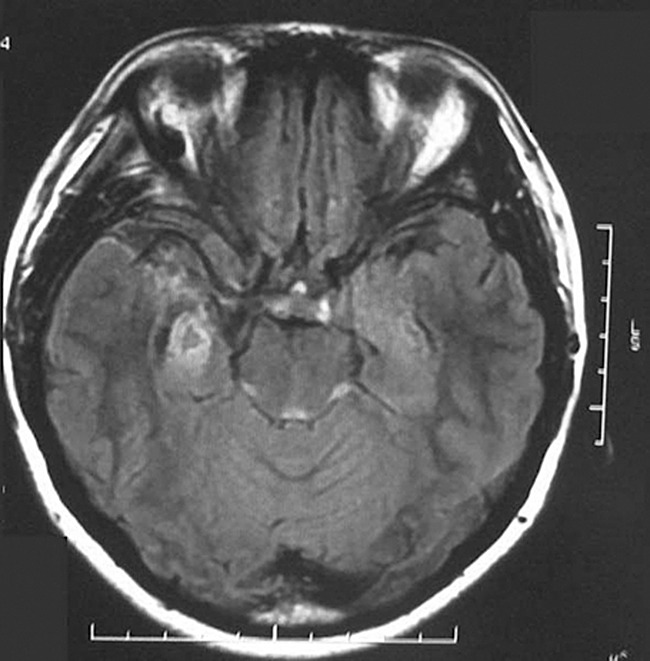
Figure 2.
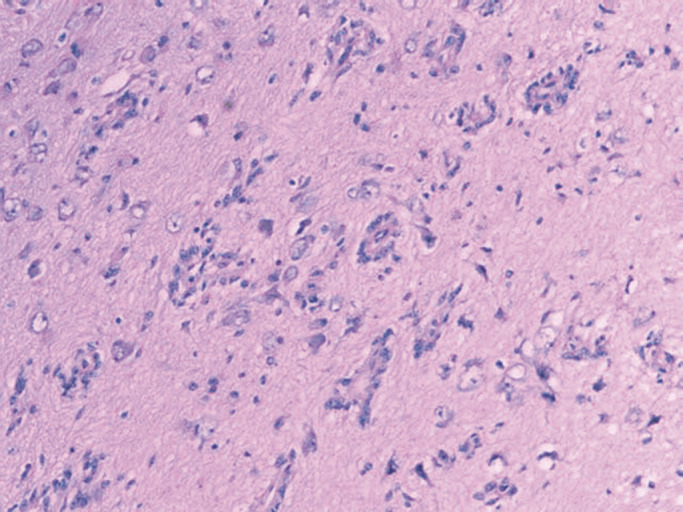
Figure 3.
DIAGNOSIS
Angiocentric glioma in the hippocampus.
DISCUSSION
Angiocentric glioma (AG) is newly described as a novel epilepsy‐associated tumor in the 2007 WHO central nervous system (CNS) tumor classification. There were only 28 cases in 4 papers that have been reported in the Pubmed literature till now 1, 2, 4, 5. Most of these patients were youngsters with drug‐resistant epilepsies in the cortex. Genetic analyses on this new tumor entity have not been performed so far because of small number of cases. Lellouch‐Tubiana et al (2) reported the presence of a neuronal cell component in all cases of their series and thus classified this tumor type as a mixed glioneuronal neoplasm. Wang et al (5) proposed the term monomorphous angiocentric glioma, whereas Lellouch‐Tubiana used the term angiocentric neuroepithelial tumor. In the new edition of the World Health Organization (WHO) classification of tumors of the nervous system, the tumor be included under the designation of “angiocentric glioma” as new distinct tumor entity (3). Given the uncertainties regarding histogenesis, angiocentric glioma was grouped with astroblastoma and chordoid glioma of the third ventricle in the category of “Other neuroepithelial tumors”, previously designated “Tumors of uncertain origin”. Due to its benign clinical behavior and the possibility of curative surgery, the neoplasm was assigned to WHO grade I (3). All patients in previous reports presented with intractable focal epilepsy in childhood. The age at surgery was later, ranged from 2.3 to 70 years (mean 17 years).
Angiocentric gliomas are located superficially. The most common sites being the fronto‐parietal cortex and the temporal lobe as well as the hippocampal region (3). MRI demonstrates a well delineated solid, hyperintense, non‐enhancing cortical lesion with extension into the subcortical or adjacent ventricle. Hyperintensities in T1‐weighted images and mixed signals in T2‐weighted are the characteristics of an AG. Necrosis and calcification are rare. Histologically, well‐developed perivascular pseudorosettes can be seen in most cases. The bipolar spindled cells arranged about cortical blood vessels in mono‐multilayered sleeves that extend lengthwise along vascular axes and as radial pseudorosettes with an ependymomatous appearance. Mitoses are rare. Complex microvascular proliferation and necrosis were not observed. Immunohistochemistry, for GFAP, S‐100, and vimentin are positive while Syn, CgA, NeuN and P53 are negative. EMA expression shows a “dot‐like” pattern in the cytoplasmic of the tumor cells forming rosettes. Immunohistochemistry and electron microscopy all suggested that AG has mixed astrocytic and ependymal differentiation. Their cortical localization argues against an origin from native ependymocyte or tanycytes.
It has been suggested that these tumors may derive from the bipolar radial glia that span the neuroepithelium during embryogenesis and that they may share ependymoglial traits of be capable of generating ependymocytes (2).
Surgical excision alone is generally curative. A possible antiepileptogenic effect of radiation therapy is described in one case without surgical resection (4). The was only one case that recurred (in anaplastic form); this tumor had exhibited typical histologic features at presentation, affected an adult and had been subtotally resected (5). Further studies are needed in order to expand the information regarding the clinical behavior and therapeutic approach of AG.
ABSTRACT
Angiocentric gliomas (AG) have only recently been described. We encountered a 25‐year‐old woman with AG who had a history of epilepsy for two years. MRI revealed that there was a solid tumor in the hippocampus. The tumor was totally removed. Histologically, the spindle tumor cells proliferated around small parenchymal vessels with perivascular pseudorosettes. The tumor cells of the hippocampus surface umbilicated forming rosettes. Immunohistochemistry demonstrated positivity for GFAP, Vimentin and S‐100, but were negative for neurofilament protein, Syn, CgA and P53. EMA had “dot‐like” positive staining. The proliferation index was less than 1%. The location of the tumor and the pathological findings confirm that the diagnose was AG. Epilepsy disappeared after the operation. When fully resected these tumors have a good prognosis.
REFERENCES
- 1. Arsene D, Ardeleanu C, Ogrezeanu I, Danaila L (2008) Angiocentric glioma: presentation of two cases with dissimilar histology. Clin Neuropahto 27:391–5. [DOI] [PubMed] [Google Scholar]
- 2. Lellouch‐Tubiana A, Boddaert N, Bourgeois M, Fohlen M, Jouvet A, Delalande O, Seidenwurm D, Brunelle F, Sainte‐Rose C (2005) Angiocentric neuroepithelial tumor (ANET): a new epilepsy‐related clinicopathological entity with distinctive MRI. Brain Patho 15:281–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (2007) The 2007 WHO Classification of Tumors of the Central Nervous System. Acta Neuropathol 114:97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Preusser M, Holschen A, Novak K, Czech T, Prayer O, Hainfellner A, Baumgartner C, Woermann FG, Tuxhorn IE, Pannek HW, Bergmann M, Radlwimmer B, Villagran R, Weber RG, Hans VH (2007) Angiocentric glioma: report of clinico‐pathologic and genetic findings in 8 cases. Am J Surg Pathol 31:1709–18. [DOI] [PubMed] [Google Scholar]
- 5. Wang M, Tihan T, Rojiani AM, Bodhireddy SR, Prayson RA, Iacuone JJ, Alles AJ, Donahue DJ, Hessler RB, Kim JH, Haas M, Rosenblum MK, Burger PC (2005) Monomorphous angiocentric glioma: a distinctive epileptogenic neoplasm with features of infiltrating astrocytoma and ependymoma. J Neuropathol Exp Neurol 64:875–881. [DOI] [PubMed] [Google Scholar]


