CLINICAL HISTORY
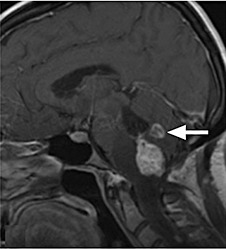
In 1995, at the age of 29, a woman presented with headache and visual disturbances. She was found to have a capillary hemangioblastoma of the brainstem, which was then resected and pathologically confirmed. The diagnosis of von Hippel‐Lindau disease was suspected at this time. One year later, she presented with worsening headache, nausea, vertigo, photophobia, and episodes of unresponsiveness. CT and MRI revealed a 4 cm mass in the right cerebellar hemisphere with effacement and displacement of the fourth ventricle. A VP shunt was placed semi‐emergently, and two days later she underwent a second craniotomy for tumor resection. The diagnosis of hemangioblastoma was once again confirmed. In 2004, follow‐up MRI of the brain and spine revealed multiple brainstem and cervical and thoracic cord lesions consistent with hemangioblastomas. An abdominal scan showed cystic kidneys with bilateral enhancing heterogeneous renal masses, suspicious for malignancy, as well as multiple pancreatic cysts and a paraaortic nodule of possible left adrenal origin; however a bone scan was normal. It is unclear whether or not the patient was treated for the presumed renal cell carcinoma at this time. In 2007, the then 41‐year‐old patient presented with a three‐day history of falls and disequilibrium, progressive quadriparesis and difficulty swallowing. An MRI of the brain was performed. Axial T2 (Figure 1) and contrast enhanced T1‐weighted (Figure 2) images showed a partially cystic (thick arrow) enhancing cerebellar mass, dorsal to the fourth ventricle. Extensive T2 hyperintensity was present in the pons, medulla (thin arrows) and middle cerebellar peduncles. Sagittal unenhanced (Figure 3) and contrast enhanced (Figure 4) T1‐weighted images showed a markedly enhancing (thick arrows) solid mass inferior to the fourth ventricle. Nodular leptomeningeal enhancement on the anterior surface of the pons was consistent with leptomeningeal involvement. The patient underwent a posterior fossa craniotomy with gross total resection of the mass in April 2007.
Figure 1.

Figure 2.
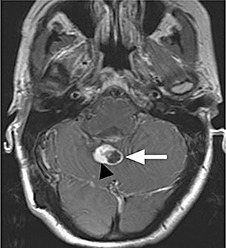
Figure 3.
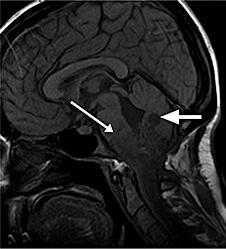
Figure 4.
PATHOLOGICAL FINDINGS
Grossly, multiple fragments of an irregular gray‐tan to red‐brown rubbery tissue with a red‐brown hemorrhagic cut surface were submitted for pathologic examination.
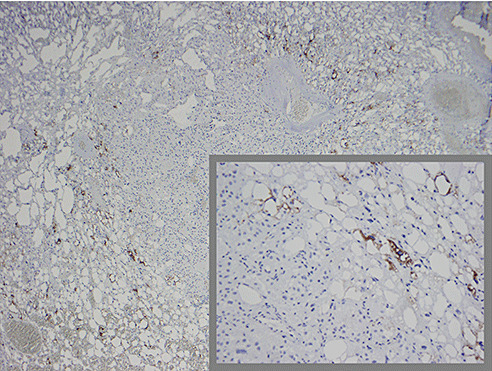
Microscopic examination revealed a well‐circumscribed, moderately cellular, highly vascular, and hemorrhagic tumor made up of polygonal vacuolated cells characterized by round hyperchromatic nuclei with mild pleomorphism (Figure 5). The tumor showed areas of cystic degeneration and was focally rimmed by gliotic brain tissue with Rosenthal fibers. Embedded within the tumor was an ill‐defined 3 mm nodule that blended in with the surrounding tissue but appeared slightly less vascular (6, 7). The epithelioid polygonal tumor cells comprising the nodule were characterized by a finely granular eosinophilic cytoplasm and larger round to oval nuclei with prominent nucleoli (Figure 8). The tumor cells within the nodule were immunoreactive for cytokeratin AE1/AE3 (Figure 9), CD10 (Figure 10), and EMA (Figure 11) and negative for inhibin‐alpha (Figure 12), while the tumor cells outside the nodule stained positive for inhibin‐alpha, but negative for cytokeratin AE1/AE3, CD10, and EMA (9, 10, 11, 12). Both tumor cell types were negative for CAM 5.2.
Figure 5.
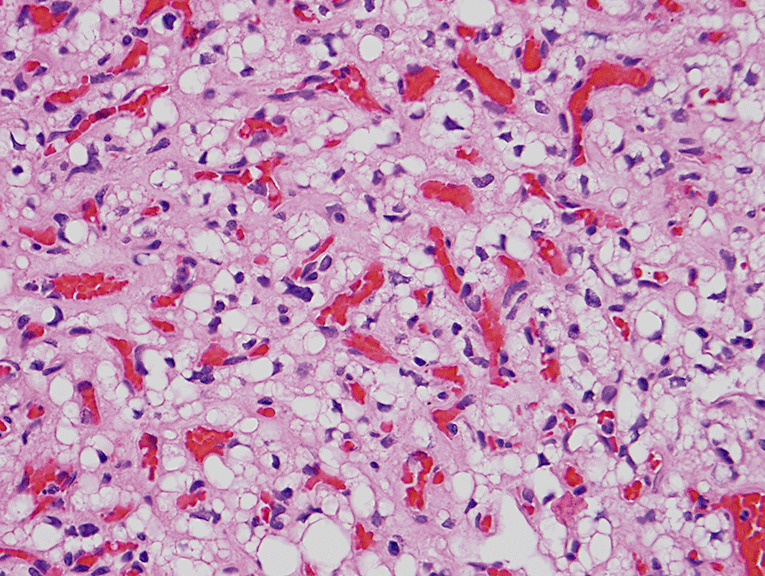
Figure 6.
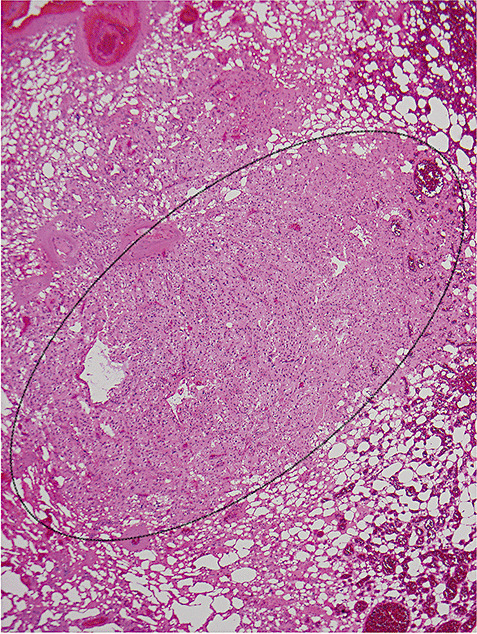
Figure 7.
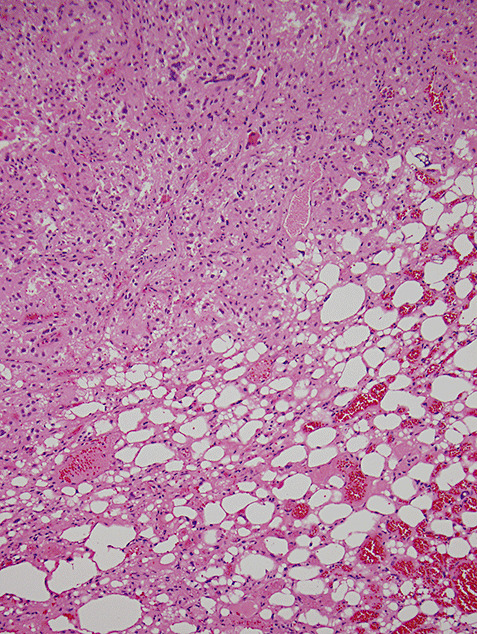
Figure 8.
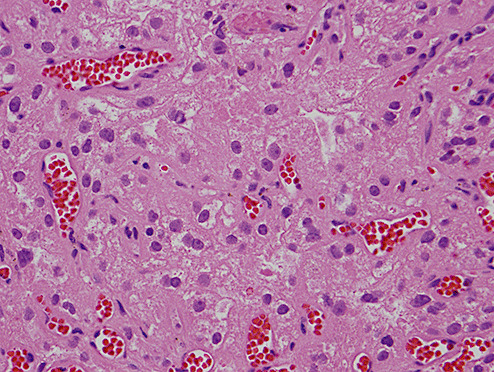
Figure 9.
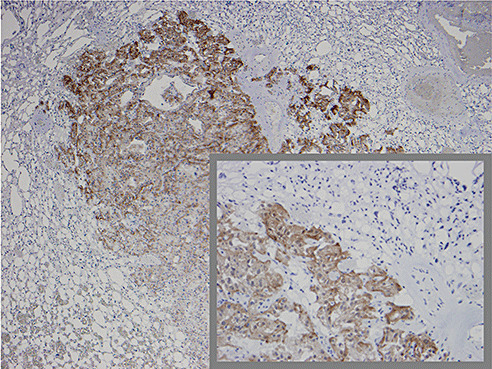
Figure 10.
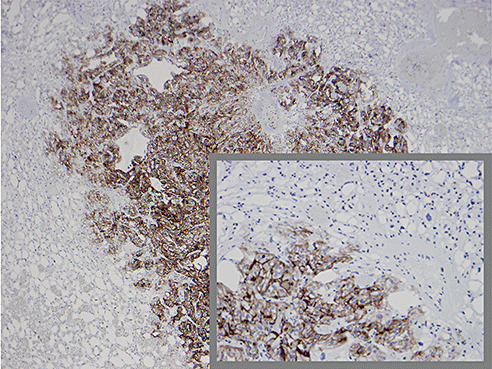
Figure 11.
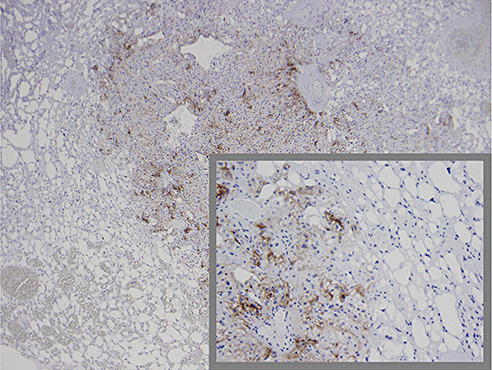
Figure 12.
What is your diagnosis?
DIAGNOSIS
Clear cell renal cell carcinoma (RCC) metastatic to capillary hemangioblastoma in the setting of von Hippel‐Lindau (VHL) disease.
DISCUSSION
VHL is an autosomal dominant disorder characterized by benign and malignant tumors and cysts (1). The most common tumors are CNS and retinal hemangioblastomas, clear cell RCC, and pheochromocytoma. RCC is found at autopsy in two‐thirds of VHL patients and accounts for one‐third of the deaths in VHL patients. Metastatic RCC is found in 40% (1, 7), and a small number of these metastatic RCCs metastasize to another tumor.
Tumor‐to‐tumor metastasis is a relatively rare phenomenon 1, 3, 5. Meningiomas are the most common recipient tumor, while RCC metastatic to a CNS hemangioblastoma is the second most common donor‐recipient tumor association (1). The precise mechanism of tumor‐to‐tumor metastasis in general is unknown but many theories have been postulated 2, 5, 8, 9. The first documented case of RCC metastatic to a CNS hemangioblastoma in a patient with VHL was described in 1992 by Jamjoom (4). Since then, thirteen other cases of RCC to hemangioblastoma have been described in the literature 1, 2, 4, 5, 7. Neither in this case nor in the previously reported cases was there radiographic evidence of a metastatic focus within the hemangioblastoma, and in only one case was the metastasis seen grossly when the tumor was sectioned (5). Hemangioblastoma consists of cells with vacuolated cytoplasm and abundant vascular stroma. The lipidized cells in clear cell RCC can have a similar appearance 2, 10. RCC are usually positive for cytokeratin AE1/AE3, EMA and CD10, while these are negative in hemangioblastomas (6). Hemangioblastomas are also positive for inhibin‐alpha and aquaphorin‐1 (10). Because of variability, the whole panel should be used to achieve the most accurate diagnosis.
We emphasize that such cases of metastatic RCC to a hemangioblastoma can be easily missed if not for careful microscopic examination. In one reported case (7), the small focus of metastatic RCC was not even seen on the hematoxylin and eosin stained section, and was only suspected because of the patient's history of RCC and discovered after immunostains were applied (7). The size of the metastatic focus was not reported in the previous cases, but was very small (3 mm) in the present case. This raises the question: are such small metastases clinically significant and do these patients behave any worse than those with a hemangioblastoma alone? This is at yet unknown, but we feel it is important that the entire resection material be submitted for pathologic examination so that a potential metastasis is not overlooked.
(For a more complete discussion, please go to: http://path.upmc.edu/divisions/neuropath/bpath/cases/case199.html.)
Presented, in part, at the 85th annual meeting of the American Association of Neuropathologists, San Antonio, Texas, June 11–13, 2009.
ABSTRACT
A 41‐year‐old woman with a 12‐year history of von Hippel‐Lindau disease presented with progressive quadriparesis and difficulty swallowing. MRI revealed a well‐circumscribed, partially cystic cerebellar neoplasm, consistent with hemangioblastoma. The tumor was resected and the diagnosis of hemangioblastoma confirmed. Embedded within the hemangioblastoma was a small focus of metastatic renal cell carcinoma (RCC). RCC metastatic to a CNS hemangioblastoma is the second most common type of tumor‐to‐tumor metastasis, which may be due to a number of factors. Proper immunostaining panels are required to clearly identify these cases since both tumor may have similar histology.
REFERENCES
- 1. Altinoz MA, Santaguida C, Guiot M‐C, Del Maestro RF (2005) Spinal hemangioblastoma containing metastatic RCC in VHL disease. Case report and review of the literature. Journal of Neurosurgery Spine 3(6):495–500. [DOI] [PubMed] [Google Scholar]
- 2. Bret P, Streichenberger N, Guyotat J (1999) Metastasis of renal carcinoma to a cerebellar hemangioblastoma in a patient with von Hippel Lindau disease: a case report. British Journal of Neurosurgery 13(4):413–6. [DOI] [PubMed] [Google Scholar]
- 3. Fried B (1930) Metastatic inoculation of a meningioma by cancer cells from a bronchogenic carcinoma. American Journal of Pathology 6:47–52. [PMC free article] [PubMed] [Google Scholar]
- 4. Jamjoom A, Kane N, Nicoll J (1992) Metastasis of a renal carcinoma to a cerebellar haemangioblastoma in a case of von Hippel‐Lindau disease. Neurosurgical Review 15(3):231–4. [DOI] [PubMed] [Google Scholar]
- 5. Jarrell ST, Vortmeyer AO, Linehan WM, Oldfield EH, Lonser RR (2006) Metastases to hemangioblastomas in von Hippel‐Lindau disease. J Neurosurg 105(2):256–63. [DOI] [PubMed] [Google Scholar]
- 6. Jung S‐M, Kuo T‐t (2005) Immunoreactivity of CD10 and inhibin alpha in differentiating hemangioblastoma of central nervous system from metastatic clear cell renal cell carcinoma. Modern Pathology 18(6):788–94. [DOI] [PubMed] [Google Scholar]
- 7. Mottolese C, Stan H, Giordano F, Frappaz D, Alexei D, Streichenberger N (2001) Metastasis of clear‐cell renal carcinoma to cerebellar hemangioblastoma in von Hippel Lindau disease: rare or not investigated? Acta Neurochirurgica 143(10):1059–63. [DOI] [PubMed] [Google Scholar]
- 8. Sonet A, Hustin J, De Coene B, Gilliard C, Gustin T, Doyen C, Vandenbossche L, Jost E, Robin V, Chatelain B, Bosly A (2001) Unusual growth within a meningioma (leukemic infiltrate). Am J Surg Pathol 25(1):127–30. [DOI] [PubMed] [Google Scholar]
- 9. Sorscher SM (2008) Metastasis in von hippel‐lindau disease [comment. J Neurosurg 109(3):568; author reply ‐9. [DOI] [PubMed] [Google Scholar]
- 10. Weinbreck N, Marie B, Bressenot A, Montagne K, Joud A, Baumann C, Klein O, Vignaud J‐M (2008) Immunohistochemical markers to distinguish between hemangioblastoma and metastatic clear‐cell renal cell carcinoma in the brain: utility of aquaporin1 combined with cytokeratin AE1/AE3 immunostaining. Am J Surg Pathol 32(7):1051–9. [DOI] [PubMed] [Google Scholar]


