Abstract
Background
Self‐harm (SH; intentional self‐poisoning or self‐injury regardless of degree of suicidal intent or other types of motivation) is a growing problem in most counties, often repeated, and associated with suicide. There has been a substantial increase in both the number of trials and therapeutic approaches of psychosocial interventions for SH in adults. This review therefore updates a previous Cochrane Review (last published in 2016) on the role of psychosocial interventions in the treatment of SH in adults.
Objectives
To assess the effects of psychosocial interventions for self‐harm (SH) compared to comparison types of care (e.g. treatment‐as‐usual, routine psychiatric care, enhanced usual care, active comparator) for adults (aged 18 years or older) who engage in SH.
Search methods
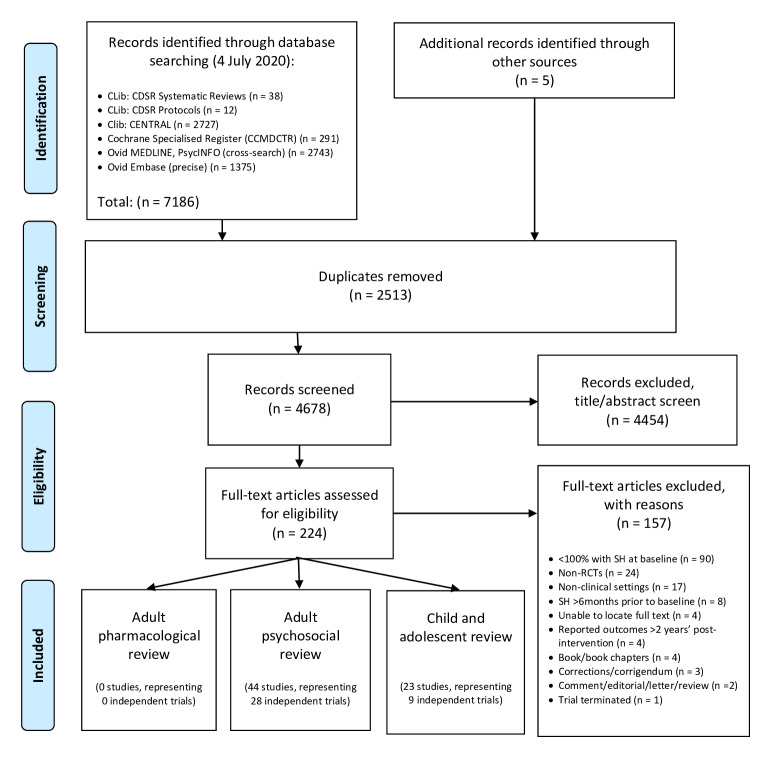
We searched the Cochrane Common Mental Disorders Specialised Register, the Cochrane Library (Central Register of Controlled Trials [CENTRAL] and Cochrane Database of Systematic reviews [CDSR]), together with MEDLINE, Ovid Embase, and PsycINFO (to 4 July 2020).
Selection criteria
We included all randomised controlled trials (RCTs) comparing interventions of specific psychosocial treatments versus treatment‐as‐usual (TAU), routine psychiatric care, enhanced usual care (EUC), active comparator, or a combination of these, in the treatment of adults with a recent (within six months of trial entry) episode of SH resulting in presentation to hospital or clinical services. The primary outcome was the occurrence of a repeated episode of SH over a maximum follow‐up period of two years. Secondary outcomes included treatment adherence, depression, hopelessness, general functioning, social functioning, suicidal ideation, and suicide.
Data collection and analysis
We independently selected trials, extracted data, and appraised trial quality. For binary outcomes, we calculated odds ratio (ORs) and their 95% confidence intervals (CIs). For continuous outcomes, we calculated mean differences (MDs) or standardised mean differences (SMDs) and 95% CIs. The overall quality of evidence for the primary outcome (i.e. repetition of SH at post‐intervention) was appraised for each intervention using the GRADE approach.
Main results
We included data from 76 trials with a total of 21,414 participants. Participants in these trials were predominately female (61.9%) with a mean age of 31.8 years (standard deviation [SD] 11.7 years). On the basis of data from four trials, individual cognitive behavioural therapy (CBT)‐based psychotherapy may reduce repetition of SH as compared to TAU or another comparator by the end of the intervention (OR 0.35, 95% CI 0.12 to 1.02; N = 238; k = 4; GRADE: low certainty evidence), although there was imprecision in the effect estimate. At longer follow‐up time points (e.g., 6‐ and 12‐months) there was some evidence that individual CBT‐based psychotherapy may reduce SH repetition. Whilst there may be a slightly lower rate of SH repetition for dialectical behaviour therapy (DBT) (66.0%) as compared to TAU or alternative psychotherapy (68.2%), the evidence remains uncertain as to whether DBT reduces absolute repetition of SH by the post‐intervention assessment. On the basis of data from a single trial, mentalisation‐based therapy (MBT) reduces repetition of SH and frequency of SH by the post‐intervention assessment (OR 0.35, 95% CI 0.17 to 0.73; N = 134; k = 1; GRADE: high‐certainty evidence). A group‐based emotion‐regulation psychotherapy may also reduce repetition of SH by the post‐intervention assessment based on evidence from two trials by the same author group (OR 0.34, 95% CI 0.13 to 0.88; N = 83; k = 2; moderate‐certainty evidence). There is probably little to no effect for different variants of DBT on absolute repetition of SH, including DBT group‐based skills training, DBT individual skills training, or an experimental form of DBT in which participants were given significantly longer cognitive exposure to stressful events. The evidence remains uncertain as to whether provision of information and support, based on the Suicide Trends in At‐Risk Territories (START) and the SUicide‐PREvention Multisite Intervention Study on Suicidal behaviors (SUPRE‐MISS) models, have any effect on repetition of SH by the post‐intervention assessment. There was no evidence of a difference for psychodynamic psychotherapy, case management, general practitioner (GP) management, remote contact interventions, and other multimodal interventions, or a variety of brief emergency department‐based interventions.
Authors' conclusions
Overall, there were significant methodological limitations across the trials included in this review. Given the moderate or very low quality of the available evidence, there is only uncertain evidence regarding a number of psychosocial interventions for adults who engage in SH. Psychosocial therapy based on CBT approaches may result in fewer individuals repeating SH at longer follow‐up time points, although no such effect was found at the post‐intervention assessment and the quality of evidence, according to the GRADE criteria, was low. Given findings in single trials, or trials by the same author group, both MBT and group‐based emotion regulation therapy should be further developed and evaluated in adults. DBT may also lead to a reduction in frequency of SH. Other interventions were mostly evaluated in single trials of moderate to very low quality such that the evidence relating to the use of these interventions is inconclusive at present.
Keywords: Adult; Female; Humans; Male; Cognitive Behavioral Therapy; Confidence Intervals; Depression; Depression/therapy; Dialectical Behavior Therapy; Mentalization; Problem Solving; Psychosocial Intervention; Psychosocial Intervention/methods; Psychotherapy, Psychodynamic; Randomized Controlled Trials as Topic; Recurrence; Secondary Prevention; Secondary Prevention/methods; Self-Injurious Behavior; Self-Injurious Behavior/psychology; Self-Injurious Behavior/therapy; Suicide Prevention
Plain language summary
Psychosocial interventions for adults who self‐harm
We have reviewed the interventional literature regarding psychosocial intervention treatment trials in the field. A total of 76 trials meeting our inclusion criteria were identified. There may be beneficial effects for psychological therapy based on cognitive behavioural therapy (CBT) approaches at longer follow‐up time points, and for mentalisation‐based therapy (MBT), and emotion‐regulation psychotherapy at the post‐intervention assessment. There may also be some evidence of effectiveness of standard dialectical behaviour therapy (DBT) on frequency of SH repetition. There was no clear evidence of effect for case management, information and support, remote contact interventions (e.g. emergency cards, postcards, telephone‐based psychotherapy), provision of information and support, and other multimodal interventions.
Why is this review important?
Self‐harm (SH), which includes intentional self‐poisoning/overdose and self‐injury, is a major problem in many countries and is strongly linked with suicide. It is therefore important that effective treatments are developed for people who engage in SH. There has been an increase in both the number of trials and the diversity of therapeutic approaches for SH in adults in recent years. It is therefore important to assess the evidence for their effectiveness.
Who will be interested in this review?
Hospital administrators (e.g. service providers), health policy officers and third party payers (e.g. health insurers), clinicians working with people who engage in SH, the people themselves, and their relatives.
What questions does this review aim to answer?
This review is an update of a previous Cochrane review from 2016 which found that CBT‐based psychological therapy can result in fewer individuals repeating SH whilst DBT may lead to a reduction in frequency of repeated SH. This updated review aims to further evaluate the evidence for effectiveness of psychosocial interventions for people engaging in SH with a broader range of outcomes.
Which studies were included in the review?
To be included in the review, studies had to be randomised controlled trials of psychosocial interventions for adults who had recently engaged in SH.
What does the evidence from the review tell us?
Overall, there were a number of methodological limitations across the trials included in this review. We found positive effects for psychological therapy based on CBT approaches at longer follow‐up assessments, and for mentalisation‐based therapy (MBT), and emotion‐regulation psychotherapy on repetition of SH at post‐intervention. There may also be some evidence of effects for standard dialectical behaviour therapy (DBT) on frequency of SH repetition. However, remote contact interventions, case management, information and support, and other multimodal interventions do not appear to have benefits in terms of reducing repetition of SH.
What should happen next?
The promising results for CBT‐based psychotherapy at longer follow‐up time points, and for MBT, group‐based emotion regulation, and DBT warrant further investigation to understand which people benefit from these types of interventions. Greater use of head‐to‐head trials (where treatments are directly compared with each other) may also assist in identifying which component(s) from these often complex interventions may be most effective.
Summary of findings
Summary of findings 1. Comparison 1.1: Individual‐based CBT‐based psychotherapy compared to TAU or another comparator for self‐harm in adults.
| Comparison 1.1: Individual‐based CBT‐based psychotherapy compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: CBT‐based psychotherapy Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with CBT‐based psychotherapy | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.35 (0.12 to 1.02) | 238 (4 RCTs) | ⊕⊕⊝⊝ LOW 1,2 | Our confidence in the effect estimate of case management on repetition of SH at post‐intervention is limited. The true effect may be substantially different from the estimate of the effect. | |
| 200 per 1000 | 80 per 1000 (29 to 203) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CBT: cognitive behavioural therapy; CI: Confidence interval; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; OR: Odds ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as we rated any of the sources of risk of bias (as described in Assessment of risk of bias in included studies) at high risk for one of the studies included in the pooled estimate.
2 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 2. Comparison 1.2: Group‐based CBT‐based psychotherapy compared to TAU or another comparator for self‐harm in adults.
| Comparison 1.2: Group‐based CBT‐based psychotherapy compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: CBT‐based psychotherapy Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with CBT‐based psychotherapy | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.66 (0.36 to 1.21) | 313 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | We are moderately confident in the effect estimate of group‐based CBT‐based psychotherapy on repetition of SH at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 190 per 1000 | 134 per 1000 (78 to 221) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CBT: cognitive behavioural therapy; CI: Confidence interval; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; OR: Odds ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 3. Comparison 2.1: DBT compared to TAU or another comparator for self‐harm in adults.
| Comparison 2.1: DBT compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: DBT Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with DBT | |||||
| Repetition of SH by post‐intervention | Study population | OR 0.71 (0.32 to 1.55) | 502 (6 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | We have very little confidence in the effect estimate of DBT on repetition of SH at post‐intervention. The true effect is likely to be substantially different from the estimate of effect. | |
| 682 per 1000 | 604 per 1000 (407 to 769) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; DBT: Dialectical behaviour therapy; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by two levels as we rated any of the sources of risk of bias (as described in Assessment of risk of bias in included studies) at high risk for two or more of the studies included in the pooled estimate.
2 We downgraded this domain by one level as the I2 value indicated substantial levels of heterogeneity.
3 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 4. Comparison 2.2: DBT group‐based skills training compared to TAU or another comparator for self‐harm in adults.
| Comparison 2.2: DBT group‐based skills training compared to TAU or alternative psychotherapy for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: DBT group‐based skills training Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with DBT group‐based skills training | |||||
| Repetition of attempted suicide at post‐intervention | Study population | OR 0.66 (0.23 to 1.86) | 66 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | We are moderately confident in the effect estimate of DBT group‐based skills training on repetition of attempted suicide at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 364 per 1000 | 274 per 1000 (116 to 515) | |||||
| Repetition of NSSI at post‐intervention | Study population | OR 0.88 (0.33 to 2.34) | 66 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | We are moderately confident in the effect estimate of DBT group‐based skills training on repetition of NSSI at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 576 per 1000 | 544 per 1000 (309 to 761) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; DBT: Dialectical behaviour therapy; NSSI: Non‐suicidal self‐injury; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 5. Comparison 2.3: DBT individual therapy compared to TAU or another comparator for self‐harm in adults.
| Comparison 2.3: DBT individual therapy compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: DBT individual therapy Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with DBT individual therapy | |||||
| Repetition of attempted suicide at post‐intervention | Study population | OR 1.46 (0.54 to 3.91) | 66 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | We are moderately confident in the effect estimate of DBT individual therapy on repetition of attempted suicide at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 364 per 1000 | 455 per 1000 (236 to 691) | |||||
| Repetition of NSSI at post‐intervention | Study population | OR 1.29 (0.48 to 3.47) | 66 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | We are moderately confident in the effect estimate of DBT individual therapy on repetition of NSSI at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 576 per 1000 | 636 per 1000 (394 to 825) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; DBT: Dialectical behaviour therapy; NSSI: Non‐suicidal self‐injury; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 6. Comparison 2.4: DBT prolonged exposure protocol compared to TAU or another comparator for self‐harm in adults.
| Comparison 2.4: DBT prolonged exposure protocol compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: DBT prolonged exposure protocol Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with DBT prolonged exposure protocol | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.67 (0.08 to 5.68) | 18 (1 RCT) | ⊕⊕⊕⊝ MODERATE1 | We are moderately confident in the effect estimate of DBT prolonged exposure protocol on repetition of SH at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 333 per 1000 | 251 per 1000 (38 to 740) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; DBT: Dialectical behaviour therapy; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 7. Comparison 3: MBT compared to TAU or another comparator for self‐harm in adults.
| Comparison 3: MBT compared TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: MBT Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with MBT | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.35 (0.17 to 0.73) | 134 (1 RCT) | ⊕⊕⊕⊕ HIGH | We are very confident that the true effect for MBT on repetition of SH at post‐intervention lies close to that of the estimate of the effect. | |
| 492 per 1000 | 253 per 1000 (141 to 414) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; MBT: Mentalisation‐based therapy; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
Summary of findings 8. Comparison 4: Emotion‐regulation psychotherapy compared to TAU or another comparator for self‐harm in adults.
| Comparison 4: Emotion‐regulation psychotherapy compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Group‐based emotion‐regulation psychotherapy Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Group‐based emotion‐regulation psychotherapy | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.34 (0.13 to 0.88) | 83 (2 RCTs) | ⊕⊕⊕⊝ MODERATE1 | We are moderately confident that the true effect of group‐based emotion‐regulation psychotherapy on repetition of SH at post‐intervention lies close to that of the estimate of the effect. | |
| 775 per 1000 | 539 per 1000 (309 to 752) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgradedthis domain by one level as one study was suggestive of benefit, whilst the second trial of this intervention was not.
Summary of findings 9. Comparison 5: Psychodynamic psychotherapy compared to TAU or another comparator for self‐harm in adults.
| Psychodynamic psychotherapy compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Psychodynamic psychotherapy Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Psychodynamic psychotherapy | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.45 (0.13 to 1.56) | 170 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | We are moderately confident in the effect estimate of psychodynamic psychotherapy on repetition of SH at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 133 per 1000 | 65 per 1000 (20 to 194) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 10. Comparison 6: Case management compared to TAU or another comparator for self‐harm in adults.
| Case management compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Case management Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Case management | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.78 (0.47 to 1.30) | 1608 (5 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | Our confidence in the effect estimate of case management on repetition of SH at post‐intervention is limited. The true effect may be substantially different from the estimate of the effect. | |
| 114 per 1000 | 91 per 1000 (57 to 143) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the I2 value indicated substantial levels of heterogeneity.
2 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 11. Comparison 7: Structured GP follow‐up compared to TAU or another comparator for self‐harm in adults.
| Structured general practitioner (GP) follow‐up compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Structured general practitioner (GP) follow‐up Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Structured general practitioner (GP) follow‐up | |||||
| Repetition of SH at post‐intervention (hospital records) | Study population | OR 1.01 (0.38 to 2.68) | 143 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | Our confidence in the effect estimate of structured general practitioner (GP) follow‐up on repetition of SH (according to hospital records) at post‐intervention is limited. The true effect may be substantially different from the estimate of the effect. | |
| 133 per 1000 | 134 per 1000 (55 to 291) | |||||
| Repetition of SH at post‐intervention (emergency records) | Study population | OR 2.56 (0.80 to 8.15) | 123 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | Our confidence in the effect estimate of structured general practitioner (GP) follow‐up on repetition of SH (according to emergency records) at post‐intervention is limited. The true effect may be substantially different from the estimate of the effect. | |
| 72 per 1000 | 167 per 1000 (59 to 389) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as we rated any of the sources of risk of bias (as described in Assessment of risk of bias in included studies) at high risk for one of the studies included in the pooled estimate.
2 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 12. Comparison 9.1: Emergency cards compared to TAU or another comparator for self‐harm in adults.
| Comparison 9.1: Emergency cards compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Emergency cards Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Remote contact interventions: Emergency cards | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.82 (0.31 to 2.14) | 1039 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | Our confidence in the effect estimate of emergency cards on repetition of SH at post‐intervention is limited. The true effect may be substantially different from the estimate of the effect. | |
| 171 per 1000 | 145 per 1000 (60 to 306) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the I2 value indicated substantial levels of heterogeneity.
2 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 13. Comparison 9.2: Coping cards compared to TAU or another comparator for self‐harm in adults.
| Comparison 9.2: Coping cards compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Coping cards Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Coping cards | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.08 (0.00 to 1.45) | 64 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | We are moderately confident in the effect estimate of coping cards on repetition of SH at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 156 per 1000 | 15 per 1000 (0 to 212) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 14. Comparison 9.4: Postcards compared to TAU or another comparator for self‐harm in adults.
| Comparison 9.4: Postcards compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Postcards Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Remote contact interventions: Postcards | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.87 (0.62 to 1.23) | 3277 (4 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | We have very little confidence in the effect estimate for postcards on repetition of SH. The true effect is likely to be substantially different from the estimate of effect. | |
| 132 per 1000 | 117 per 1000 (86 to 157) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as we rated any of the sources of risk of bias (as described in Assessment of risk of bias in included studies) at high risk for one of the studies included in the pooled estimate.
2 We downgraded this domain by one level as the I2 value indicated substantial levels of heterogeneity.
3 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 15. Comparison 9.5: Telephone contact compared to TAU or another comparator for self‐harm in adults.
| Comparison 9.5: Telephone contact compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Telephone contact Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Telephone contact | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.43 (0.04 to 5.02) | 55 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | Our confidence in the effect estimate of telephone contact on repetition of SH at post‐intervention is limited. The true effect may be substantially different from the estimate of the effect. | |
| 77 per 1000 | 35 per 1000 (3 to 295) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as we rated any of the sources of risk of bias (as described in Assessment of risk of bias in included studies) at high risk for one of the studies included in the pooled estimate.
2 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 16. Comparison 9.6: Telephone contact, emergency cards, and letters compared to TAU or another comparator for self‐harm in adults.
| Comparison 9.6: Telephone contact, emergency cards, and letters compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Telephone contact, emergency cards, and letters Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Remote contact interventions: Telephone contact, emergency cards, and letters | |||||
| Repetition of SH at post‐intervention | Study population | OR 1.05 (0.55 to 2.00) | 303 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | We are moderately confident in the effect estimate of telephone contact, emergency cards, and letters on repetition of SH at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 139 per 1000 | 145 per 1000 (82 to 244) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 17. Comparison 9.7: Telephone‐based psychotherapy compared to TAU or another comparator for self‐harm in adults.
| Comparison 9.7: Telephone‐based psychotherapy compared to TAU or alternative psychotherapy for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Telephone‐based psychotherapy Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Remote contact interventions: Telephone‐based psychotherapy | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.36 (0.01 to 8.94) | 185 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | Our confidence in the effect estimate of telephone‐based psychotherapy on repetition of SH at post‐intervention is limited. The true effect may be substantially different from the estimate of the effect. | |
| 11 per 1000 | 4 per 1000 (0 to 87) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as we rated any of the sources of risk of bias (as described in Assessment of risk of bias in included studies) at high risk for one of the studies included in the pooled estimate.
2 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 18. Comparison 10: Provision of information and support compared to TAU or another comparator for self‐harm in adults.
| Comparison 10: Provision of information and support compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Provision of information and support Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Provision of information and support | |||||
| Repetition of SH at post‐intervention | Study population | OR 1.09 (0.79 to 1.50) | 1853 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | We have very little confidence in the effect estimate for information and support on repetition of SH by the post‐intervention assessment. The true effect is likely to be substantially different from the estimate of effect. | |
| 90 per 1000 | 97 per 1000 (72 to 129) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 Publication bias is suspected as data from some centres have not been published.
2 We downgraded this domain by one level as we rated any of the sources of risk of bias (as described in Assessment of risk of bias in included studies) at high risk for one of the studies included in the pooled estimate.
3 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 19. Comparison 11: Other multimodal interventions compared to TAU or another comparator for self‐harm in adults.
| Comparison 11: Other multimodal interventions compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: Other multimodal interventions Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Other multimodal interventions | |||||
| Repetition of SH at post‐intervention | Study population | OR 0.61 (0.37 to 1.30) | 1937 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 | We have very little confidence in the effect estimate for other multimodal interventions on repetition of SH at post‐intervention. The true effect is likely to be substantially different from the estimate of effect. | |
| 252 per 1000 | 189 per 1000 (111 to 305) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by two levels as the I2 value indicated considerable levels of heterogeneity.
2 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 20. Comparison 12.5: General hospital management compared to TAU or another comparator for self‐harm in adults.
| Comparison 12.5: General hospital management compared to TAU or another comparator for self‐harm in adults | ||||||
| Patient or population: self‐harm in adults Intervention: General hospital management Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with General hospital management | |||||
| Repetition of SH at post‐intervention | Study population | OR 1.03 (0.14 to 7.69) | 77 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | We are moderately confident in the effect estimate of general hospital management on repetition of SH at post‐intervention. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. | |
| 51 per 1000 | 53 per 1000 (8 to 294) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Summary of findings 21. Comparison 12.8: Long‐term therapy compared to TAU or another comparator for self‐harm in adults.
| Comparison 12.8: Long‐term therapy compared to TAU or another comparator for self‐harm in adults | ||||||
|
Patient or population: self‐harm in adults Intervention: Long term therapy Comparison: TAU or another comparator | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with comparator | Risk with Long term therapy | |||||
| Repetition of SH at post‐intervention | Study population | OR 1.00 (0.35 to 2.86) | 80 (1 RCT) | ⊕⊕⊝⊝ LOW 1 2 | Our confidence in the effect estimate of long‐term therapy on repetition of SH at post‐intervention is limited.The true effect may be substantially different from the estimate of the effect. | |
| 225 per 1000 | 225 per 1000 (92 to 454) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; RCT: Randomised controlled trial; RR: Risk ratio; SH: Self‐harm; TAU: Treatment as usual. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded this domain by one level as we rated any of the sources of risk of bias (as described in Assessment of risk of bias in included studies) at high risk for one of the studies included in the pooled estimate.
2 We downgraded this domain by one level as the 95% CI for the pooled effect included the null value.
Background
Description of the condition
Self‐harm (SH), which includes all intentional acts of self‐poisoning (such as intentional drug overdoses) or self‐injury (such as self‐cutting), regardless of degree of suicidal intent or other types of motivation (Hawton 2003), has been a growing problem in most countries. In Australia, for example, it is estimated that there are now more than 26,000 general hospitalisations for SH each year, or a rate of 116.7 per 100,000 persons (Harrison 2014), similar to rates observed in a number of other comparable countries (Canner 2018; Griffin 2014; Morthorst 2016; Ting 2012; Wilkinson 2002). However, it is notable that rates of emergency department presentations for SH are often higher than hospitalisations (Bergen 2010; Corcoran 2015). In the UK, for example, higher rates of emergency department presentations for SH in both females (442 per 100,000) and males (362 per 100,000) have been reported (Geulayov 2016). There are also many more episodes of SH occurring in the community that do not come to the attention of clinical services. Worldwide, for example, the World Health Organization (WHO) estimates that the rate of SH may be as high as 400 per 100,000, according to self‐report data (WHO 2014).
In contrast to suicide rates, rates of hospital‐presenting SH are higher in females than in males in most countries (Canner 2018; Griffin 2014; Masiran 2017; Morthorst 2016; Ting 2012; Wilkinson 2002), with rates peaking in younger adults up to 24 years of age (Perry 2012). However, this difference decreases across the life cycle (Hawton 2008). SH is less common in older people, but tends to be associated with higher suicidal intent (Hawton 2008), with consequent greater risk of suicide (Murphy 2012).
For those who present to hospital, the most common method of SH is self‐poisoning. Overdoses of analgesics and psychotropics, especially paracetamol or acetaminophen, are common in some countries, particularly high‐income countries. Self‐cutting is the next most frequent method used by those who present to hospital. However, in the community, self‐cutting and other forms of self‐injury are far more frequent than self‐poisoning (Müller 2016).
SH is often repeated. Up to one‐quarter of those who present to hospital with SH return to the same hospital within a year (Carroll 2014; Owens 2002), although some individuals may present to another hospital. Others may not present to hospital at all given that studies identifying SH repetition via self‐report suggest as many as one in five report further SH episodes following a hospital presentation (Carroll 2014). Repetition is more common in individuals who have a history of previous episodes of SH, personality disorder, psychiatric treatment, and alcohol or drug misuse (Larkin 2014). Risks of repeat SH may also be associated with method. Rates of repetition are higher among those who present to hospital following self‐injury alone (Carroll 2014; Lilley 2008), or combined self‐injury and self‐poisoning (Perry 2012), compared to those who present for self‐poisoning alone.
SH is associated with suicide. The risk of death by suicide within one year among people who present to hospital following SH varies across studies from nearly 1% to over 3% (Liu 2020; Carroll 2014; Owens 2002). This variation reflects the characteristics of the population, and the background national suicide rate. In the UK, for example, during the first year after an episode of SH, the risk of suicide is around 50 times that of the general population, with a particularly high risk in men (Carroll 2014; Geulayov 2019). One quarter of these deaths are estimated to occur within one month after discharge, and almost 50% by three months (Forte 2019), although the risk of suicide appears to remain elevated for a number of years (Geulayov 2019). A history of SH is the strongest risk factor for suicide across a range of psychiatric disorders. Repetition of SH further increases the risk of suicide (Zahl 2004).
SH and suicide are the result of a complex interplay between genetic, biological, psychiatric, psychosocial, social, cultural, and other factors. Psychiatric disorders, particularly mood and anxiety disorders, are associated with the largest contribution to the risk of both SH (Hawton 2013), and suicide in adults (Ferrari 2014). Personality disorders, including borderline personality disorder, are also associated with SH, particularly frequent repetition. Alcohol use may also play an important role (Ferrari 2014). Both psychological and biological factors appear to further increase vulnerability to SH. Psychological factors may include difficulties in problem‐solving, low self‐esteem, impulsivity, vulnerability to having pessimistic thoughts about the future (i.e. hopelessness), and a sense of entrapment. Biological factors include disturbances in the serotonergic and stress response systems (Van Heeringen 2014).
Description of the intervention
Psychological approaches used to treat adults who engage in SH typically involve brief individual‐ or group‐based psychological therapy. Treatment may vary in terms of initial management, location of treatment, continuity, intensity, and frequency of contact with therapists. There is also considerable variation among countries in the availability of services to provide such interventions. Consequently, there is no standard psychosocial treatment of SH in adults. However, in high‐income countries, treatment generally consists of a combination of assessment, support, and individual psychological therapies. In lower and middle‐income countries, aftercare more usually involves various forms of support, both face‐to‐face and via digital means.
How the intervention might work
Psychosocial interventions may address some of the underlying psychological risk factors associated with SH. The mechanisms of action of these interventions might help people improve their coping skills and tackle specific problems, manage psychiatric disorders, improve self‐esteem, increase a sense of social connectedness, and reduce impulsivity and harmful reactions to distressing situations. What follows is a description of the psychosocial interventions that are typically available for adults who engage in SH behaviours.
Cognitive behavioural therapy‐based psychotherapy
Cognitive behavioural therapy (CBT)‐based psychotherapy helps people identify and critically evaluate the ways in which they interpret and evaluate disturbing emotional experiences and events, and aims to help them change the ways in which they deal with problems (Westbrook 2008). This is achieved in three steps: first, people are helped to change the ways in which they interpret and evaluate distressing emotions; second, they learn strategies to help them change the way in which they think about the meanings and consequences of these emotions; finally, with the benefit of modified interpretation of emotions and events, they are helped to change their behaviour and develop positive functional behaviour (Jones 2012).
Problem‐solving therapy (PST) is an integral part of CBT, although it can be delivered as a therapy in and of itself. PST assumes that ineffective and maladaptive coping behaviours that drive SH might be overcome by helping the person to learn skills to actively, constructively, and effectively solve the problems he or she faces in their daily lives (Nezu 2010). PST typically involves identification of the problem, generation of a range of solutions, implementation of chosen solutions based on appraisal, and the evaluation of these solutions (D'Zurilla 2010). Treatment goals include helping people to develop a positive problem‐solving orientation, use rational problem‐solving strategies, reduce the tendency to avoid problem‐solving, and reduce the use of impulsive problem‐solving strategies.
Dialectical behaviour therapy
In contrast to CBT and PST, which focus on changing behaviour and cognitive patterns, the focus of dialectical behavioural therapy (DBT) is to provide people with the skills to develop an awareness and acceptance of thoughts and emotions, including painful or distressing internal experiences, without judgement or attempts to alter, suppress, avoid, or otherwise change these experiences (Lynch 2006). The primary treatment goals of DBT are three‐fold: to reduce SH, reduce behaviours that interfere with the success of treatment, such as treatment non‐adherence, and reduce any other factors that may adversely affect the person's quality of life (e.g. frequency or duration of psychiatric hospitalisations) (Linehan 1993).
Mentalisation‐based therapy
Mentalisation refers to the ability to understand the behaviour of both one's self and others in terms of motivational and emotional states (Allen 2008). Maladaptive and impulsive coping behaviours, including SH, are presumed to arise from a disrupted ability to engage in these processes. In mentalisation‐based therapy (MBT), the goal is to help people understand their emotions and behaviours, and develop strategies to regulate them to minimise the risk that they will engage in SH during times of distress.
Emotion‐regulation psychotherapy
Emotion‐regulation psychotherapy is based on DBT, Acceptance and Commitment Therapy (ACT), and emotion‐focused therapy. It includes psychoeducation, identification of emotions, distress tolerance, emotional acceptance, behavioural activation, developing alternative coping strategies, impulse control, and identifying and clarifying valued directions.
Psychodynamic psychotherapy
Psychodynamic approaches focus on affective experiences, exploring and understanding the unconscious meaning and function of SH, and exploring and resolving difficulties in interpersonal relationships, and resulting emotional difficulties, within a therapeutic relational framework (Yakeley 2018).
Case management
"In its simplest form...case management is a means of coordinating services. Each...person is assigned a 'case manager' who is expected to assess that person's needs, develop a care plan, arrange for suitable care to be provided, monitor the quality of the care provided, and maintain contact with the person" (Marshall 2000a). Case management might have a significant role in the aftercare of people who engage in SH because many of them demonstrate poor treatment adherence, and because of the varied nature of the problems these individuals are often facing (Lizardi 2010).
Remote contact interventions
Remote contact interventions, which may include letters, brief text messages delivered by telephone, telephone calls, and postcards, are low‐resource and non‐intrusive interventions that seek to maintain long‐term contact with people. These interventions provide a sense of ongoing concern, and may mitigate the sense of social isolation reported by many people who engage in SH. They may also help to improve their knowledge about triggers and warning signs for SH, provide them with information on alternative coping behaviours to SH, and where they can access help (Milner 2016).
These interventions may also be combined with emergency card interventions, which encourage people to seek help when they feel distressed, and offer on‐demand emergency contact with psychiatric services or inpatient care. The aim is to reduce the risk of SH by facilitating rapid access to care.
Other multimodal interventions
Any of the above active psychosocial interventions may also be combined into a multimodal approach (Högberg 2008).
Why it is important to do this review
SH is a major social and healthcare problem. It represents significant morbidity, is often repeated, and is linked with suicide. Many countries now have suicide prevention strategies, all of which include a focus on improved management of people presenting with SH (WHO 2014). SH also leads to substantial healthcare costs (Sinclair 2011). In the UK, the overall median cost per episode of SH has been estimated to be £809, although costs are significantly higher for cases of combined self‐injury and self‐poisoning, compared to either self‐injury of self‐poisoning alone. These costs are mainly attributable to health‐service level contact (i.e. inpatient stay or admission to intensive care; Tsiachristas 2017).
In the UK, the National Collaborating Centre for Mental Health (NCCMH) produced the first guideline on the treatment of SH behaviours in 2004 (NCCMH 2004). This guideline focused on the short‐term physical and psychological management of SH. This guidance was updated in 2011, using interim data from a previous version of this review as the evidence base, and focused on the longer‐term psychological management of SH (NICE 2011). Subsequently, similar guidelines have been published by the Royal College of Psychiatrists (Royal College of Psychiatrists 2014), the Royal Australian and New Zealand College of Psychiatrists (Carter 2016), and German Professional Associations and Societies (Plener 2016), amongst others (Courtney 2019).
In 2021, the guidance contained in the 2011 NICE guidelines for the longer‐term management of SH will be due for updating. Therefore, we are updating our review (Hawton 2016), in order to provide contemporary evidence to guide clinical policy and practice.
Objectives
To assess the effects of psychosocial interventions for self‐harm (SH) compared to comparison types of care (e.g. treatment as usual, routine psychiatric care, enhanced usual care, active comparator) for adults (aged 18 years or older) who engage in SH.
Methods
Criteria for considering studies for this review
Types of studies
We considered all randomised controlled trials (RCTs) of specific psychosocial interventions versus treatment as usual, routine psychiatric care, enhanced usual care, active comparator, or a combination of these, in the treatment of adults with a recent (within six months of trial entry) presentation for self‐harm (SH). All RCTs (including cluster‐RCTs [cRCTs] and cross‐over trials) were eligible for inclusion regardless of publication type or language; however, we excluded quasi‐randomised trials.
Types of participants
While exact eligibility criteria often differ both within and between regions and countries (Witt 2020a), we included participants of both sexes and all ethnicities, who were 18 years and older, with a recent (i.e. within six months of trial entry) presentation to hospital or clinical services for SH.
We defined SH as all intentional acts of self‐poisoning (such as intentional drug overdoses) or self‐injury (such as self‐cutting), regardless of the degree of suicidal intent or other types of motivation (Hawton 2003). This definition includes acts intended to result in death ('attempted suicide'), those without suicidal intent (e.g. to communicate distress, to temporarily reduce unpleasant feelings; sometimes termed 'non‐suicidal self‐injury'), and those with mixed motivation. We did not distinguish between attempted suicide and non‐suicidal self‐injury in this review, because there is a high level of co‐occurrence between them, and the two cannot be distinguished in any reliable way, including on levels of suicidal intent (Klonsky 2011). Lastly, the motivations for SH are complex and can change, even within a single episode (De Beurs 2018).
We excluded trials in which participants presented to clinical services for suicidal ideation only (i.e. without evidence of SH).
Types of interventions
Categorisation of the interventions in this review was informed by the trials themselves, and based on consensus discussions among members of the review team, who have considerable experience in both research and clinical practice related to SH. However, based on the previous version of this review (Hawton 2016), we anticipated the following groupings:
Interventions
These included the following:
Cognitive behavioural therapy (CBT)‐based psychotherapy (e.g. CBT, problem‐solving therapy [PST]) versus TAU or another comparator;
Dialectical behaviour therapy (DBT) versus TAU or another comparator;
Mentalisation‐based therapy (MBT) versus TAU or another comparator;
Emotion‐regulation psychotherapy versus TAU or another comparator;
Psychodynamic psychotherapy versus TAU or another comparator;
Case management versus TAU or another comparator;
Structured general practitioner (GP) follow‐up versus TAU or another comparator;
Brief emergency department‐based interventions versus TAU or another comparator;
Remote contact interventions versus TAU or another comparator;
Provision of information and support versus TAU or another comparator;
Other multimodal interventions versus TAU or another comparator;
Other mixed interventions versus TAU or another comparator.
Comparators
Treatment‐as‐usual (TAU) is likely to vary widely between settings and between studies conducted over different time periods (Witt 2018). Following previous work, we defined TAU as routine clinical care that the person would receive had they not been included in the study (i.e. routine care or 'standard disposition'; Hunt 2013). Other comparators could include no specific treatment, or enhanced usual care, which refers to TAU that has, in some way, been supplemented, such as by providing psychoeducation, assertive outreach, or more regular contact with case managers, and standard assessment approaches.
Types of outcome measures
For all outcomes, we were primarily interested in quantifying the effect of treatment assignment to the intervention at baseline, regardless of whether the intervention was received as intended (i.e. the intention‐to‐treat effect).
Primary outcomes
The primary outcome measure in this review was the occurrence of repeated SH over a maximum follow‐up period of two years. Repetition of SH may be identified through self‐report, collateral report, clinical records, or research monitoring systems. As we wished to incorporate the maximum data from each trial, we included both self‐reported and hospital records of SH, where available. Preference was given to clinical records over self‐report where a trial reported both measures. We also reported proportions of participants repeating SH, frequency of repeat episodes, and time to SH repetition (where available).
Secondary outcomes
Given increasing interest in the measurement of outcomes of importance to those who engage in SH (Owens 2020b), we planned to analyse data for the following secondary outcomes (where available) over a maximum follow‐up period of two years:
Treatment adherence
This was assessed using a range of measures of adherence, including: pill counts, changes in blood measures, and the proportion of participants that both started and completed treatment.
Depression
This was assessed as either continuous data, by scores on psychometric measures of depression symptoms, for example, total scores on the Beck Depression Inventory (BDI; Beck 1961), or scores on the depression subscale of the Hospital Anxiety and Depression Scale (HADS; Zigmond 1983), or as dichotomous data as the proportion of participants who met defined diagnostic criteria for depression.
Hopelessness
This was assessed as either continuous data, by scores on psychometric measures of hopelessness, for example, total scores on the Beck Hopelessness Scale (BHS; Beck 1974), or as dichotomous data as the proportion of participants reporting hopelessness.
General functioning
This was assessed as either continuous data, by scores on psychometric measures of general functioning, for example, total scores on the Global Assessment of Functioning (GAF; APA 2000), or as dichotomous data as the proportion of participants reporting improved general functioning.
Social functioning
This was assessed as either continuous data, by scores on psychometric measures of social functioning, for example, total scores on the Social Adjustment Scale (SAS; Weissman 1999), or as dichotomous data as the proportion of participants reporting improved social functioning.
Suicidal ideation
This was assessed as either continuous data, by scores on psychometric measures of suicidal ideation, for example, total scores on the Beck Scale for Suicidal Ideation (BSSI; Beck 1988), or as dichotomous data as the proportion of participants reaching a defined cut‐off for ideation.
Suicide
This included register‐recorded deaths, or reports from collateral informants, such as family members or neighbours.
Search methods for identification of studies
Electronic searches
An information specialist searched the following databases (to 4 July 2020), using relevant subject headings (controlled vocabularies) and search syntax as appropriate for each resource: Cochrane Common Mental Disorders Specialised Register (Appendix 1), Cochrane Library (Central Register of Controlled Trials; CENTRAL), Cochrane Database of Systematic Reviews (CDSR), MEDLINE Ovid, Embase Ovid, and PsycINFO Ovid (Appendix 2).
A date restriction was applied to the search as the search was to update an earlier version of this review (Hawton 2016). However, we did not apply any further restrictions on language or publication status to the searches.
We searched for retraction statements and errata once the included studies were selected.
We also searched the World Health Organization International Clinical Trials Registry Platform, and the US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov to identify ongoing trials.
The search was based on population only, participants who self‐harm (all ages). Records were screened to identify trials which were relevant to this review and two others (Witt 2021a; Witt 2021b).
Searching other resources
Conference abstracts
In addition to conference abstracts retrieved via the main electronic search, we also screened the proceedings of recent (last five years) conferences organised by the largest scientific committees in the field:
International Association for Suicide Prevention (both global congresses and regional conferences);
Joint International Academy of Suicide Research and American Foundation for Suicide Prevention International Summits on Suicide Research.
Reference lists
We also checked the reference lists of all relevant RCTs, and the reference lists of major reviews that included a focus on psychosocial interventions for SH in adults (Bornheimer 2020; Briggs 2019; Calati 2016; D'Anci 2019; DeCou 2019; Ghanbari 2015; Gøtzsche 2017; Hawton 2016; Hanratty 2019; Hetrick 2016; Inagaki 2019; Krysinska 2017; Meerwijk 2016; Milner 2015; Milner 2016; Padmanathan 2020; Riblet 2017; Tighe 2018).
Correspondence
We consulted the corresponding authors of trials, and other experts in the field to find out if they are aware of any ongoing or unpublished RCTs on the psychosocial treatment of adults who engage in SH that were not identified by the electronic searches.
Data collection and analysis
Selection of studies
Review authors KW, KH, and one of either SH, GR, TTS, ET, or PH, independently assessed the titles of reports identified by the electronic search for eligibility. We distinguished between:
eligible or potentially eligible trials for retrieval, in which any psychosocial intervention was compared with a comparator (i.e. TAU, routine psychiatric care, standard disposition, no specific treatment, enhanced usual care);
ineligible, general treatment trials, not for retrieval (i.e. where there was no control treatment).
All trials identified as potentially eligible for inclusion then underwent a second screening. Pairs of review authors, working independently from one another, screened the full text of eligible or potentially eligible trials to identify whether the trial met our inclusion criteria. We resolved disagreements in consultation with the senior review author (KH). Where disagreements could not be resolved from the information reported in the trial, or where it was unclear whether the trial satisfied our inclusion criteria, we contacted corresponding trial authors for additional clarification.
We identified and excluded duplicate records, and collated multiple reports of the same trial, so that each trial, rather than each report, represented the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram (Liberati 2009), and completed a 'Characteristics of excluded studies' table.
Data extraction and management
Review author KW and one of either SH, or GR independently extracted data from the included trials, using a standardised extraction form. Where there were any disagreements, they were resolved in consensus discussions with KH.
Data extracted from each eligible trial included the following:
Participant information: number randomised, number lost to follow‐up or withdrawn, number analysed, mean or median age, sex composition, diagnoses, diagnostic criteria, inclusion criteria, and exclusion criteria;
Methods: trial design, total duration of the trial, details of any 'run‐in' period (if applicable), number of trial centres and their location, setting, and date;
Intervention(s): details of the intervention, including dose, duration, whether concomitant treatments were permitted and details of these treatments, and any excluded treatments;
Comparator(s): details on the comparator, including dose, duration, whether concomitant treatments were permitted and details of these treatments, and any excluded treatments;
Outcomes: raw data for each eligible outcome (see Types of outcome measures), details of other outcomes specified and reported, and time points at which outcome were reported;
Notes: source of trial funding, and any notable conflicts of interest of trial authors.
We extracted both dichotomous and continuous outcomes data from eligible trials. As the use of non‐validated psychometric scales is associated with bias, we extracted continuous data only if the psychometric scale used to measure the outcome of interest had been previously published in a peer‐reviewed journal, and was not subjected to item, scoring, or other modification by the trial authors (Marshall 2000b).
We planned the following main comparisons:
Cognitive behavioural therapy (CBT)‐based psychotherapy (e.g. CBT, problem‐solving therapy [PST]) versus TAU or another comparator;
Dialectical behaviour therapy (DBT) versus TAU or another comparator;
Mentalisation‐based therapy (MBT) versus TAU or another comparator;
Emotion‐regulation psychotherapy versus TAU or another comparator;
Case management versus TAU or another comparator;
Remote contact interventions versus TAU or another comparator;
Other multimodal interventions versus TAU or another comparator.
Assessment of risk of bias in included studies
Highly biased studies are more likely to overestimate treatment effectiveness (Moher 1998). Review author KW and one of either SH, or GR independently evaluated the risk of bias for the primary outcome (i.e. repetition of SH at post‐intervention) by using version 2 of the Cochrane Risk of Bias tool, RoB 2 (Sterne 2019). This tool encourages consideration of the following domains:
Bias in the randomisation process;
Deviations from the intended intervention (assignment to intervention);
Missing outcome data;
Bias in the measurement of the outcome;
Bias in the selection of the reported result.
For cluster‐RCTs, we also evaluated the following:
Bias arising from the timing of identification and recruitment of participants.
Signalling questions in the RoB 2 tool provided the basis for the tool’s domain‐level judgements about the risk of bias. Two review authors independently judged each source of potential bias as low risk, high risk, or some concerns. An overall 'Risk of bias' judgement was then made for each study by combining ratings across these domains. Specifically, if any of the above domains were rated at high risk, the overall 'Risk of bias' judgement was rated at high risk. We reported this overall judgement, which could be low risk, high risk, or some concerns, in the text of the review, and in the 'Risk of bias' tables.
Where inadequate details were provided in the original report, we contacted corresponding trial authors to provide clarification. We resolved disagreements through discussions with KH.
We entered and organised our RoB 2 assessments on an Excel spreadsheet (Microsoft Excel RoB2 Macro), and made them available as electronic supplements.
Measures of treatment effect
Dichotomous outcomes
We summarised dichotomous outcomes, such as the number of participants engaging in a repeat SH episode, or number of deaths by suicide, using the summary odds ratio (OR) and the accompanying 95% confidence interval (CI), as the OR is the most appropriate effect size statistic for summarising associations between two dichotomous groups (Fleiss 1994). Time to SH repetition was summarised using the hazard ratio (HR) and its accompanying 95% CI.
Continuous outcomes
For outcomes measured on a continuous scale, we used mean differences (MDs) and accompanying 95% CI where the same outcome measure was used. Where different outcome measures were used, we used the standardised mean difference (SMD) and its accompanying 95% CI.
We aggregated trials in a meta‐analysis only where treatments were sufficiently similar. For trials that could not be included in a meta‐analysis, we provided narrative descriptions of the results.
Hierarchy of outcomes
Where a trial measured the same outcome, for example, depression in two or more ways, we planned to use the most common measure across trials in any meta‐analysis. We also planned to report scores from other measures in a supplementary table.
Timing of outcome assessment
The primary end point for this review was post‐intervention (i.e. at the conclusion of the treatment period). We also reported outcomes for the following secondary end points (where data were available):
Between zero and six months after the conclusion of the treatment period;
Between six and 12 months after the conclusion of the treatment period;
Between 12 and 24 months after the conclusion of the treatment period.
Where there was more than one outcome assessment within a time period, we used data from the last assessment in the time period, unless different outcomes were assessed at different time points. For treatment adherence, we also planned to use within‐treatment results.
Unit of analysis issues
Zelen design trials
Trials in this area are increasingly using Zelen's method, in which consent is obtained subsequent to randomisation and treatment allocation (Witt 2020a). This design may lead to bias if, for example, participants allocated to one particular arm of the trial disproportionally refuse to provide consent for participation or, alternatively, if participants only provide consent if they are allowed to cross over to the other treatment arm (Torgerson 2004).
We identified five trials that used Zelen's design (Carter 2005; Gysin‐Maillart 2016; Hatcher 2011; Hatcher 2015; Hatcher 2016). Where possible, we therefore analysed data for these trials using data for all randomised participants as this is consistent with Zelen’s original intention (Zelen 1979), and preserves randomisation. This was typically possible for our primary outcome, repetition of SH, as this was generally ascertained from clinical, hospital, and/or medical records in these five trials. However, for certain self‐reported secondary outcome measures, data were only reported on the basis of those who consented to participation. We therefore planned to conduct sensitivity analyses to investigate what impact, if any, the inclusion of these trials may have on the pooled estimate of treatment effectiveness.
Cluster‐randomised trials
Cluster randomisation, for example by clinician or general practice, can lead to overestimation of the significance of a treatment effect, resulting in an inflation of the nominal type I error rate, unless appropriate adjustment is made for the effects of clustering (Donner 2002; Kerry 1998).
One trial included in this review used cluster randomisation (Bennewith 2002). We had planned to follow the guidance outlined in Higgins 2019a. Specifically, where possible, we planned to analyse data using measures that statistically accounted for the cluster design. Where this was not possible, we planned to analyse data using the effective sample size. However, the trial authors were unable to provide values for either the inter‐cluster correlation coefficient or the design effect, and further, there was no similar cluster‐RCT of this intervention approach from which these values could be approximated. We were therefore unable to statistically account for the effects of clustering in this trial.
In future updates of this review, should we be able to obtain information on either the inter‐cluster correlation coefficient or the design effect, we will follow the guidance outlined in Higgins 2019a.
Cross‐over trials
A primary concern with cross‐over trials is the carry‐over effect, in which the effect of the intervention treatment (e.g. pharmacological, physiological, psychological) influences the participant's response to the subsequent control condition (Elbourne 2002). As a consequence, on entry to the second phase of the trial, participants may differ systematically from their initial state, despite a wash‐out phase. In turn, this may result in a concomitant underestimation of the effectiveness of the treatment intervention (Curtin 2002a; Curtin 2002b).
One trial included in the current review used cross‐over methodology (Marasinghe 2012). To protect against the carry‐over effect, we only extracted data from the first phase of this trial, prior to cross‐over.
Studies with multiple treatment arms
Five trials in the current review included multiple treatment arms (Andreoli 2015; Armitage 2016; Linehan 2015; Stewart 2009; Wei 2013. For two of these trials (Andreoli 2015; Stewart 2009), it was possible to combine data from the two intervention arms given their similarity. For the remaining three, however, two different psychotherapies were compared (Armitage 2016; Linehan 2015; Wei 2013. Therefore, we included information from these trials in both categories of intervention using data from the relevant intervention arm. As we did not combine data from the intervention arms in any meta‐analysis, we used the same comparator arm data for both analyses.
Studies with adjusted effect sizes
Where trials reported both unadjusted and adjusted effect sizes, we included only observed, unadjusted effect sizes.
Dealing with missing data
We did not impute missing data, as we considered that the bias that would be introduced by doing this would outweigh any benefit of increased statistical power that may have been gained by including imputed data. However, where authors omitted standard deviations (SD) for continuous measures, we contacted corresponding authors to request missing data. Where missing data could not be provided, we calculated missing SDs using other data from the trial, such as CIs, based on methods outlined in Higgins 2019b.
Assessment of heterogeneity
Between‐study heterogeneity can be assessed using either the Chi² or I² statistics. However, in this review, we used only the I² statistic to quantify inconsistency, as this is considered to be more reliable (Deeks 2019). The I² statistic indicates the percentage of between‐study variation due to chance, and can take any value from 0% to 100% (Deeks 2019).
We used the following values to denote relative importance of heterogeneity, as per Deeks 2019:
unimportant: 0% to 40%;
moderate: 30% to 60%;
substantial: 50% to 90%;
considerable: 75% to 100%.
We also took the magnitude and direction of effects and strength of evidence for heterogeneity into account (e.g. the CI for I²).
Where substantial levels of heterogeneity were found, we explored reasons for this heterogeneity (see Subgroup analysis and investigation of heterogeneity for details).
Assessment of reporting biases
Reporting bias occurs when the decision to publish a particular trial is influenced by the direction and significance of the results (Egger 1997). Research suggests, for example, that trials with statistically significant findings are more likely to be submitted for publication and, subsequently, be accepted for publication, leading to possible overestimation of the true treatment effect (Hopewell 2009).
To assess whether trials included in any meta‐analysis were affected by reporting bias, we planned to enter data into a funnel plot when a meta‐analysis included results of at least ten trials. Should evidence of any small study effects be identified, we planned to explore reasons for funnel plot asymmetry, including the presence of possible publication bias (Egger 1997).
Data synthesis
For the purposes of this review, we calculated the pooled odds ratio (OR) and accompanying 95% CI using the random‐effects model, as this is the most appropriate model for incorporating heterogeneity between studies (Deeks 2019). We used the Mantel‐Haenszel method for dichotomous data, and the inverse variance method for continuous data. We conducted all analyses in Review Manager 5.4 (Review Manager 2020).
Subgroup analysis and investigation of heterogeneity
Subgroup analyses
We planned to undertake the following subgroup analyses where there were sufficient data to do so:
sex (males versus females);
repeater status (first SH episode versus repeat SH episode).
Given the increasing use of enhanced usual care rather than TAU in trials in this field (Witt 2020a), we also planned to undertake subgroup analyses to determine whether comparator choice influenced the pattern of results observed.
Formal tests for subgroup differences were undertaken in Review Manager 5.4 (Review Manager 2020). However, it is only possible to undertake these subgroup analyses if randomisation was stratified by these factors, otherwise, there is the risk that doing so could lead to confounding.
Randomisation was stratified by sex in five trials (Carter 2005; Hvid 2011; McAuliffe 2014; Walton 2020; Van der Sande 1997). Six trials also stratified randomisation by repeater status (Gratz 2014; Hatcher 2015; Hatcher 2016; McAuliffe 2014; Morthorst 2012; Mouaffak 2015).
Investigation of heterogeneity
Several meta‐analyses were associated with substantial levels of between‐study heterogeneity (i.e. I² ≥ 75%). For these analyses, KW and KH firstly independently triple‐checked data to ensure these were correctly entered. Next, we investigated the source of this heterogeneity using a formal statistical approach as outlined in Viechtbauer 2020.
Sensitivity analysis
We planned to undertake the following sensitivity analyses, where appropriate, to test whether key methodological factors or decisions may have influenced the main result:
Where a trial made use of Zelen's method of randomisation (see Unit of analysis issues);
Where a trial contributed to substantial between‐study heterogeneity (see Subgroup analysis and investigation of heterogeneity).
Five trials used Zelen's design (Carter 2005; Gysin‐Maillart 2016; Hatcher 2011; Hatcher 2015; Hatcher 2016). We were therefore able to undertaken sensitivity analyses, excluding these trials, to investigate what impact, if any, Zelen's design had on the pooled estimate of treatment effectiveness. We reported results of these sensitivity analyses in the text.
Additionally, several meta‐analyses were associated with substantial levels of between‐study heterogeneity. We also reported results of these sensitivity analyses in the text, alongside discussion of the likely causes of these differences.
Summary of findings and assessment of the certainty of the evidence
For each comparison, we planned to construct a 'Summary of findings' table for our primary outcome measure, repetition of SH post‐intervention, following the recommendations outlined in Schünemann 2019. These tables provide information concerning the overall quality of the evidence from all included trials that measured the outcome. We assessed the quality of evidence across the following domains:
'Risk of bias' assessment;
Indirectness of evidence;
Unexplained heterogeneity or inconsistency of results;
Imprecision of effect estimates;
Potential publication bias.
For each of these domains, we downgraded the evidence from high certainty by one level (for serious) or by two levels (for very serious). For risk of bias, we downgraded this domain by one level when we rated any of the sources of risk of bias (as described in Assessment of risk of bias in included studies) at high risk for any of the studies included in the pooled estimate, or by two levels when we rated multiple studies at high risk for any of these sources. For indirectness of evidence, we considered the extent to which trials included in any meta‐analysis used proxy measures to ascertain repetition of SH; we downgraded this domain by one level if one study used proxy measures, and by two levels if multiple studies used proxy measures. For unexplained heterogeneity or inconsistency of results, we downgraded this domain by one level where the I² value indicated substantial levels of heterogeneity, or by two levels where the I² value indicated considerable levels of heterogeneity. For imprecision, we downgraded this domain by one level where the 95% CI for the pooled effect included the null value. Finally, for the potential publication bias domain, we considered any evidence of funnel plot asymmetry (if available), as well as other evidence such as suspected selective availability of data, and downgraded by one or more levels where publication bias was suspected.
We then used these domains to rate the overall quality of evidence for the primary outcome according to the following:
High certainty: further research is very unlikely to change our confidence in the estimate of effect;
Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect, and may change the estimate;
Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect, and may change the estimate;
Very low certainty: we are very uncertain about the estimate.
We constructed 'Summary of findings' tables using GRADEpro GDT software (GRADEpro GDT 2015).
Reaching conclusions
We based our conclusions only on findings from the quantitative or narrative synthesis of the studies included in this review. Our recommendations for practice and research suggest priorities for future research, and outline remaining uncertainties in the area.
Results
Description of studies
Results of the search
For this update, a total of 7186 records were found using the search strategy as outlined in Appendix 1 and Appendix 2. Five further records were identified following correspondence and discussion with researchers in the field. After deduplication, the initial number was reduced to 4678. Of these, 4454 were excluded following title/abstract screening, whist a further 157 were excluded after reviewing the full texts (Figure 1).
1.
Study Flow Diagram
Included studies
In the previous version of this review (Hawton 2016), 55 trials of psychosocial interventions for self‐harm (SH) in adults were included. The present update located 21 new trials of psychosocial interventions for SH in adults. The present review therefore includes 76 non‐overlapping trials (see the Characteristics of included studies tables for further information on these trials).
Unpublished data were obtained from the trial authors for 42 of these trials (Bateman 2009; Beautrais 2010; Bennewith 2002; Brown 2005; Carter 2005; Cedereke 2002; Clarke 2002; Crawford 2010; Davidson 2014; Dubois 1999; Fleischmann 2008; Gratz 2006; Gratz 2014; Guthrie 2001; Gysin‐Maillart 2016; Harned 2014; Hassanian‐Moghaddam 2011; Hatcher 2011; Hatcher 2015; Hatcher 2016; Husain 2014; Hvid 2011; Kapur 2013; Kawanishi 2014; Linehan 1991; Linehan 2006; Marasinghe 2012; McAuliffe 2014; McMain 2009; Owens 2020; Patsiokas 1985; Priebe 2012; Slee 2008; Sreedaran 2020; Stewart 2009; Tapolaa 2010; Turner 2000; Tyrer 2003; Vaiva 2006; Walton 2020; Wei 2013; Weinberg 2006).
Design
Most trials (97.4%) randomised at the individual‐level employing either simple randomisation (Allard 1992; Armitage 2016; Beautrais 2010; Brown 2005; Clarke 2002; Crawford 2010; Davidson 2014; Dubois 1999; Evans 1999a; Evans 1999b; Fleischmann 2008; Gibbons 1978; Gratz 2006; Hawton 1981; Hawton 1987; Kapur 2013; Liberman 1981; McLeavey 1994; Morgan 1993; Mousavi 2015; Mousavi 2017; Naidoo 2014; O'Connor 2015; O'Connor 2020; Patsiokas 1985; Sahin 2018; Salkovskis 1990; Slee 2008; Stewart 2009; Tapolaa 2010; Torhorst 1987; Torhorst 1988; Turner 2000; Van Heeringen 1995; Wang 2016; Waterhouse 1990; Wei 2013; Weinberg 2006; Welu 1977), or a restricted randomisation scheme such as adaptive minimisation (Linehan 2015), blocked randomisation (Amadéo 2015; Andreoli 2015; Grimholt 2015; Guthrie 2001; Hassanian‐Moghaddam 2011; Husain 2014; Lin 2020; McMain 2009; McMain 2017; Priebe 2012; Sreedaran 2020; Vaiva 2018), or minimisation procedure (Bateman 2009, Harned 2014, Kawanishi 2014; Linehan 1991; Linehan 2006; O'Connor 2017; Owens 2020) procedure. One trial used a matched pair randomisation procedure (Cedereke 2002). Nine trials used stratification (Gratz 2014; Hvid 2011; McAuliffe 2014; Morthorst 2012; Mouaffak 2015; Tyrer 2003; Vaiva 2006; Van der Sande 1997; Walton 2020). Five used Zelen's design (Carter 2005; Gysin‐Maillart 2016; Hatcher 2011; Hatcher 2015; Hatcher 2016).
In one trial, cluster randomisation was used (Bennewith 2002). One trial was a cross‐over RCT (Marasinghe 2012).
Setting
Of the 76 independent RCTs included in this review, one‐quarter (25.0%) were from the UK (Bateman 2009; Bennewith 2002; Clarke 2002; Crawford 2010; Davidson 2014; Evans 1999a; Evans 1999b; Gibbons 1978; Guthrie 2001; Hawton 1981; Hawton 1987; Kapur 2013; Morgan 1993; O'Connor 2017; Owens 2020; Priebe 2012; Salkovskis 1990; Tyrer 2003; Waterhouse 1990), 14 were from the USA (Brown 2005; Gratz 2006; Gratz 2014; Harned 2014; Liberman 1981; Linehan 1991; Linehan 2006; Linehan 2015; O'Connor 2015; O'Connor 2020; Patsiokas 1985; Turner 2000; Weinberg 2006; Welu 1977), four from France (Dubois 1999; Mouaffak 2015; Vaiva 2006; Vaiva 2018), four from New Zealand (Beautrais 2010; Hatcher 2011; Hatcher 2015; Hatcher 2016), three from Australia (Carter 2005; Stewart 2009; Walton 2020), three from Canada (Allard 1992; McMain 2009; McMain 2017), three from Iran (Hassanian‐Moghaddam 2011; Mousavi 2015; Mousavi 2017), two from Denmark (Hvid 2011; Morthorst 2012), two from Germany (Torhorst 1987; Torhorst 1988), two from the Netherlands (Slee 2008; Van der Sande 1997), two from the Republic of Ireland (McAuliffe 2014; McLeavey 1994), two from Switzerland (Andreoli 2015; Gysin‐Maillart 2016), two from Sweden (Cedereke 2002; Sahin 2018), two from Taiwan (Lin 2020; Wang 2016), and one was from each of Belgium (Van Heeringen 1995), China (Wei 2013), Finland (Tapolaa 2010), French Polynesia (Amadéo 2015), India (Sreedaran 2020), Japan (Kawanishi 2014), Malaysia (Armitage 2016), Norway (Grimholt 2015), Pakistan (Husain 2014), South Africa (Naidoo 2014), and Sri Lanka (Marasinghe 2012). One was a multicentre trial conducted in a number of countries (Fleischmann 2008).
In the majority of trials, participants were identified following a clinical presentation for SH. In 16 trials (21.1%), participants were identifying following referral to outpatient mental health and/or specialist personality disorder treatment services (Bateman 2009; Gratz 2006; Gratz 2014; Harned 2014; Liberman 1981; Linehan 1991; Linehan 2006; Linehan 2015; McMain 2009; McMain 2017; Priebe 2012; Sahin 2018; Salkovskis 1990; Walton 2020; Wang 2016; Weinberg 2006). All participants in these trials had a history of SH resulting in presentation to clinical services within six months preceding trial entry.
For most trials (85.5%), treatment was delivered in an outpatient setting or in the participants' home environment. In four trials, acute‐phase treatment was delivered in an inpatient setting followed by outpatient follow‐up appointments (Amadéo 2015; Torhorst 1987; Torhorst 1988; Van der Sande 1997), whilst in two older trials, treatment was delivered in an inpatient setting (Liberman 1981; Waterhouse 1990). In the remaining five trials, the intervention was delivered while individuals were receiving treatment in hospital and/or the emergency department (Armitage 2016; Crawford 2010; O'Connor 2015; O'Connor 2017; O'Connor 2020).
Participants and participant characteristics
The included trials comprised a total of 21,414 participants. All had engaged in at least one episode of SH prior to trial entry. A history of SH prior to the index episode (i.e. a history of multiple episodes of SH) was a requirement for participation in 17 trials (Bateman 2009; Evans 1999b; Gratz 2006; Gratz 2014; Harned 2014; Liberman 1981; Linehan 1991; Linehan 2006; McMain 2009; Mousavi 2015; Mousavi 2017; Priebe 2012; Sahin 2018; Salkovskis 1990; Torhorst 1988; Tyrer 2003; Weinberg 2006). In 20 trials, around half of the sample had a history of multiple episodes of SH (Allard 1992; Brown 2005; Cedereke 2002; Evans 1999a; Guthrie 2001; Gysin‐Maillart 2016; Hatcher 2011; Hatcher 2015; Hatcher 2016; Kapur 2013; Kawanishi 2014; Lin 2020; Morthorst 2012; Mouaffak 2015; O'Connor 2017; Owens 2020; Slee 2008; Torhorst 1987; Van der Sande 1997; Welu 1977) Only one trial excluded those with a history of multiple episodes of SH prior to trial entry (Morgan 1993).
Information on the methods of SH for the index episode was not reported in half (k = 38; 50.0%) of the trials (Allard 1992; Amadéo 2015; Andreoli 2015; Armitage 2016; Bateman 2009; Cedereke 2002; Davidson 2014; Dubois 1999; Evans 1999b; Fleischmann 2008; Gratz 2006; Gratz 2014; Hvid 2011; Kapur 2013; Liberman 1981; Lin 2020; Linehan 1991; Linehan 2006; Linehan 2015; Marasinghe 2012; McMain 2009; Morthorst 2012; Mousavi 2017; Naidoo 2014; O'Connor 2020; Patsiokas 1985; Priebe 2012; Sahin 2018; Salkovskis 1990; Sreedaran 2020; Stewart 2009; Tapolaa 2010; Turner 2000; Tyrer 2003; Walton 2020; Wang 2016; Wei 2013; Weinberg 2006). Full details of the methods used at the index episode for the remaining trials is provided in Table 22. Whilst the predominance of participants engaging in self‐poisoning in the majority of these trials is reflective of the typical pattern observed in those who present to hospital, or in the community, SH more often involves self‐cutting and other forms of self‐injury (Müller 2016).
1. Methods used at the index episode of self‐harm.
| Reference | Method | |||
|
Self‐poisoning n (%) |
Self‐injury n (%) |
Combined self‐poisoning and self‐injury n (%) |
Unspecified n (%) |
|
| Allard 1992 | ‐ | ‐ | ‐ | ‐ |
| Amadéo 2015 | ‐ | ‐ | ‐ | ‐ |
| Andreoli 2015 | ‐ | ‐ | ‐ | ‐ |
| Armitage 2016 | ‐ | ‐ | ‐ | ‐ |
| Bateman 2009 | ‐ | ‐ | ‐ | ‐ |
| Beautrais 20101 | 250 (76.7) | 64 (19.6) | ‐ | 15 (4.6) |
| Bennewith 2002 | 7,733 (89.7) | 158 (8.2) | ‐ | 41 (2.1) |
| Brown 2005 | 70 (58.3) | 33 (27.5) | ‐ | 17 (14.2) |
| Carter 2005 | 772 (100) | ‐ | ‐ | ‐ |
| Cedereke 2002 | ‐ | ‐ | ‐ | ‐ |
| Clarke 20021 | 442 (94.6) | 25 (5.3) | 8 (1.70) | ‐ |
| Crawford 2010 | 74 (71.8) | 25 (24.3) | ‐ | 4 (3.9) |
| Davidson 2014 | ‐ | ‐ | ‐ | ‐ |
| Dubois 1999 | ‐ | ‐ | ‐ | ‐ |
| Evans 1999a | 808 (97.7) | ‐ | ‐ | 19 (2.3) |
| Evans 1999b | ‐ | ‐ | ‐ | ‐ |
| Fleischmann 2008 | ‐ | ‐ | ‐ | ‐ |
| Gibbons 1978 | 400 (100) | ‐ | ‐ | ‐ |
| Gratz 2006 | ‐ | ‐ | ‐ | ‐ |
| Gratz 2014 | ‐ | ‐ | ‐ | ‐ |
| Grimholt 2015 | 149 (100) | ‐ | ‐ | ‐ |
| Guthrie 2001 | 119 (100) | ‐ | ‐ | ‐ |
| Gysin‐Maillart 2016 | ‐ | ‐ | ‐ | ‐ |
| Harned 2014 | ‐ | 26 (100) | ‐ | ‐ |
| Hassanian‐Moghaddam 2011 | 2,300 (100) | ‐ | ‐ | ‐ |
| Hatcher 2011 | 471 (85.3) | 81 (14.7) | ‐ | ‐ |
| Hatcher 2015 | 532 (77.8) | 125 (18.3) | 27 (3.9) | ‐ |
| Hatcher 2016 | 115 (68.9) | 41 (24.5) | 11 (6.6) | ‐ |
| Hawton 1981 | 96 (100) | ‐ | ‐ | ‐ |
| Hawton 1987 | 80 (100) | ‐ | ‐ | ‐ |
| Husain 2014 | 217 (98.2) | 4 (1.8) | ‐ | ‐ |
| Hvid 2011 | ‐ | ‐ | ‐ | ‐ |
| Kapur 2013 | ‐ | ‐ | ‐ | ‐ |
| Kawanishi 20141 | 707 (77.3) | 332 (36.3) | ‐ | 42 (4.6) |
| Liberman 1981 | ‐ | ‐ | ‐ | ‐ |
| Lin 2020 | ‐ | ‐ | ‐ | ‐ |
| Linehan 1991 | ‐ | ‐ | ‐ | ‐ |
| Linehan 2006 | ‐ | ‐ | ‐ | ‐ |
| Linehan 2015 | ‐ | ‐ | ‐ | ‐ |
| Marasinghe 2012 | ‐ | ‐ | ‐ | ‐ |
| McAuliffe 20142 | 161 (37.2) | 57 (13.2) | ‐ | 4 (0.9) |
| McLeavey 1994 | 39 (100) | ‐ | ‐ | ‐ |
| McMain 2009 | ‐ | ‐ | ‐ | ‐ |
| McMain 2017 | ‐ | ‐ | ‐ | ‐ |
| Morgan 1993 | 207 (97.6) | ‐ | ‐ | 5 (2.4) |
| Morthorst 2012 | ‐ | ‐ | ‐ | ‐ |
| Mouaffak 20153 | ‐ | ‐ | ‐ | ‐ |
| Mousavi 2015 | 55 (100) | ‐ | ‐ | ‐ |
| Mousavi 2017 | ‐ | ‐ | ‐ | ‐ |
| Naidoo 2014 | ‐ | ‐ | ‐ | ‐ |
| O'Connor 2015 | ‐ | ‐ | ‐ | ‐ |
| O'Connor 2017 | 504 (97.3) | ‐ | ‐ | 14 (2.7) |
| O'Connor 2020 | ‐ | ‐ | ‐ | ‐ |
| Owens 2020 | 40 (64.6) | 12 (19.3) | 10 (16.1) | ‐ |
| Patsiokas 1985 | ‐ | ‐ | ‐ | ‐ |
| Priebe 2012 | ‐ | ‐ | ‐ | ‐ |
| Sahin 2018 | ‐ | ‐ | ‐ | ‐ |
| Salkovskis 1990 | ‐ | ‐ | ‐ | ‐ |
| Slee 2008 | 73 (89.0) | ‐ | ‐ | ‐ |
| Sreedaran 2020 | ‐ | ‐ | ‐ | ‐ |
| Stewart 2009 | ‐ | ‐ | ‐ | ‐ |
| Tapolaa 2010 | ‐ | ‐ | ‐ | ‐ |
| Torhorst 1987 | 141 (100) | ‐ | ‐ | ‐ |
| Torhorst 1988 | 80 (100) | ‐ | ‐ | ‐ |
| Turner 2000 | ‐ | ‐ | ‐ | ‐ |
| Tyrer 2003 | ‐ | ‐ | ‐ | ‐ |
| Vaiva 2006 | 605 (100) | ‐ | ‐ | ‐ |
| Vaiva 2018 | 926 (93.8) | ‐ | ‐ | ‐ |
| Van der Sande 1997 | 232 (84.7) | ‐ | ‐ | 42 (15.3) |
| Van Heeringen 1995 | 463 (89.7) | ‐ | ‐ | 53 (10.3) |
| Walton 2020 | ‐ | ‐ | ‐ | ‐ |
| Wang 20164 | ‐ | ‐ | ‐ | ‐ |
| Waterhouse 1990 | 77 (100) | ‐ | ‐ | ‐ |
| Wei 2013 | ‐ | ‐ | ‐ | ‐ |
| Weinberg 2006 | ‐ | ‐ | ‐ | ‐ |
| Welu 1977 | ‐ | 120 (100) | ‐ | ‐ |
1 Percentages greater than 100% as participants could have used multiple methods.
2 Methods of self‐harm for the remaining 221 (48.7%) participants were not reported.
3 The majority of participants engaged in 'non‐violent' methods (n = 258; 85.2%), followed by 'violent' methods (n = 45; 14.8%). The methods considered to be 'non‐violent' or 'violent' in this trial were not reported, however.
4 The majority of participants engaged in 'low lethality' methods (n = 57; 89.1%), followed by 'high lethality' methods, including hanging, charcoal burning, or jumping from a height (n = 7; 10.9%). The methods considered to be 'low lethality' in this trial were not reported, however.
Whilst most trials included both male and female participants, the majority of participants in the 71 trials that reported information on sex were female (61.9%), reflecting the typical pattern for SH (Hawton 2008). Of the 64 trials that reported information on age, the weighted mean age of participants at trial entry was 31.8 years (SD: 11.7 years).
In the 38 trials that reported information on psychiatric diagnoses (Allard 1992; Amadéo 2015; Andreoli 2015; Bateman 2009; Brown 2005; Carter 2005; Cedereke 2002; Clarke 2002; Crawford 2010; Davidson 2014; Dubois 1999; Evans 1999a; Evans 1999b; Gibbons 1978; Gratz 2006; Gratz 2014; Gysin‐Maillart 2016; Harned 2014; Kawanishi 2014; Lin 2020; Linehan 2006; Linehan 2015; McLeavey 1994; McMain 2009; McMain 2017; Morgan 1993; Mouaffak 2015; Priebe 2012; Sahin 2018; Slee 2008; Sreedaran 2020; Turner 2000; Tyrer 2003; Vaiva 2018; Van der Sande 1997; Van Heeringen 1995; Walton 2020; Wei 2013), participants were most commonly diagnosed with major depression (56.7%), followed by any other mood disorder (37.6%), any personality disorder (31.6%), any anxiety disorder (26.7%), and substance use disorder (26.7%). A total of 14 trials focused specifically on participants diagnosed with borderline personality disorder (Andreoli 2015; Bateman 2009; Gratz 2006; Gratz 2014; Harned 2014; Linehan 1991; Linehan 2006; Linehan 2015; McMain 2009; McMain 2017; Sahin 2018; Turner 2000; Walton 2020; Weinberg 2006), and three focused on participants diagnosed with any personality disorder (Davidson 2014; Evans 1999b; Priebe 2012). Only two trials reported information on the proportion of participants without psychiatric diagnoses at trial entry (Evans 1999a; Sreedaran 2020). In these two trials, a small proportion (15.1%) were not diagnosed with a major psychiatric disorder.
Information on comorbid diagnoses was reported in eight trials (Andreoli 2015; Bateman 2009; Davidson 2014; Gratz 2014Harned 2014; Mouaffak 2015; Sahin 2018; Turner 2000). Under one‐half (40.9%) were diagnosed with comorbid psychiatric diagnoses, typically comorbid mood or anxiety disorders and personality disorders, although the nature of these comorbidities was not always clearly reported in these trials. In three further trials (Carter 2005; McMain 2009; Slee 2008), the median number of psychiatric diagnoses was greater than two, indicating that most participants in these trials were also diagnosed with more than one psychiatric disorder; however, none of the three reported further information on specific diagnoses.
Interventions
The trials included in this review investigated the effectiveness of various forms of psychosocial interventions:
Cognitive behavioural therapy (CBT)‐based psychotherapy (e.g. CBT, problem‐solving therapy [PST]) versus TAU or another comparator;
Dialectical behaviour therapy (DBT) versus TAU or another comparator;
Mentalisation‐based therapy (MBT) versus TAU or another comparator;
Emotion‐regulation psychotherapy versus TAU or another comparator;
Psychodynamic psychotherapy versus TAU or another comparator;
Case management versus TAU or another comparator;
Structured general practitioner (GP) follow‐up versus TAU or another comparator;
Brief emergency department‐based interventions versus TAU or another comparator;
Remote contact interventions versus TAU or another comparator;
Provision of information and support versus TAU or another comparator;
Other multimodal interventions versus TAU or another comparator;
Other mixed interventions versus TAU or another comparator.
Comparators
Of the 76 RCTs included in this review, the majority (76.3%) compared the intervention to TAU (Allard 1992; Amadéo 2015; Andreoli 2015; Armitage 2016; Bateman 2009; Beautrais 2010; Bennewith 2002; Brown 2005; Carter 2005; Cedereke 2002; Clarke 2002; Crawford 2010; Davidson 2014; Dubois 1999; Evans 1999a; Evans 1999b; Fleischmann 2008; Gibbons 1978; Gratz 2006; Gratz 2014; Grimholt 2015; Guthrie 2001; Gysin‐Maillart 2016; Hassanian‐Moghaddam 2011; Hatcher 2011; Hatcher 2015; Hatcher 2016; Hawton 1987; Husain 2014; Hvid 2011; Kapur 2013; Lin 2020; Linehan 1991; McAuliffe 2014; McMain 2009; Morgan 1993; Mouaffak 2015; Mousavi 2017; O'Connor 2015; O'Connor 2017; O'Connor 2020; Owens 2020; Patsiokas 1985; Priebe 2012; Sahin 2018; Salkovskis 1990; Slee 2008; Stewart 2009; Tapolaa 2010; Tyrer 2003; Vaiva 2006; Vaiva 2018; Van der Sande 1997; Van Heeringen 1995; Wang 2016; Weinberg 2006; Welu 1977). The remaining trials compared the effectiveness of the intervention to alternative forms of psychotherapy (Harned 2014; Hawton 1981; Liberman 1981; Linehan 2006; Linehan 2015; McLeavey 1994; Mousavi 2015; Naidoo 2014; Sreedaran 2020; Torhorst 1987; Torhorst 1988; Turner 2000; Walton 2020), waiting list (Marasinghe 2012; McMain 2017), no treatment (Waterhouse 1990; Wei 2013), or enhanced usual care (EUC; Kawanishi 2014; Morthorst 2012).
Outcomes
Primary outcome
Information on the primary outcome, repetition of SH, was available for all but two (3.0%) of the included trials (Patsiokas 1985; Sreedaran 2020).
In the majority of trials, repetition of SH was ascertained either from self‐reported information alone (Amadéo 2015; Armitage 2016; Brown 2005; Davidson 2014; Fleischmann 2008; Gratz 2006; Gratz 2014; Harned 2014; Hassanian‐Moghaddam 2011; Husain 2014; Liberman 1981; Linehan 1991; Linehan 2006; Linehan 2015; McMain 2009; Mousavi 2015; Mousavi 2017; Naidoo 2014; O'Connor 2015; O'Connor 2020; Priebe 2012; Sahin 2018; Slee 2008; Tapolaa 2010; Torhorst 1987; Turner 2000; Walton 2020; Wei 2013; Weinberg 2006), followed by self‐reported information supplemented by clinical, hospital, and/or medical records (Bateman 2009; Cedereke 2002; Evans 1999b; Grimholt 2015; Guthrie 2001; Gysin‐Maillart 2016; Hvid 2011; Lin 2020; Mouaffak 2015; Tyrer 2003; Vaiva 2006; Vaiva 2018), or self‐reported information supplemented with information from a collateral informant (e.g. a general practitioner [GP]) (McLeavey 1994; McMain 2017; Van Heeringen 1995; Waterhouse 1990; Welu 1977).
For the remaining 23 trials, information on repetition of SH was obtained from clinical, hospital, and/or medical records (Andreoli 2015; Beautrais 2010; Bennewith 2002; Clarke 2002; Crawford 2010; Evans 1999a; Gibbons 1978; Hatcher 2011; Hatcher 2015; Hatcher 2016; Kapur 2013; Morgan 1993; Morthorst 2012; O'Connor 2017; Owens 2020; Salkovskis 1990; Stewart 2009; Van der Sande 1997), from monitoring systems (Carter 2005; Hawton 1981; Hawton 1987), or from clinical, hospital, and/or medical records supplemented with information from collateral informants (Allard 1992).
In one trial (McAuliffe 2014), mixed methods were used to determine repetition of SH. Specifically, self‐reported information was used at the post‐intervention and six‐month follow‐up assessments, whereas data on hospital representations were used at the 12‐month follow‐up assessment in this trial.
For five trials, information on the source of the data for repetition of SH was not clearly reported (Dubois 1999; Kawanishi 2014; Marasinghe 2012; Torhorst 1988; Wang 2016).
Secondary outcomes
Treatment adherence
Of the 28 trials that reported information on treatment adherence, this was assessed using a variety of methods. This included the proportion of participants who completed the full course of the intervention treatment (Andreoli 2015; Bateman 2009; Bennewith 2002; Brown 2005; Crawford 2010; Evans 1999b; Grimholt 2015; Harned 2014; Husain 2014; Kawanishi 2014; Lin 2020; Linehan 2015; McAuliffe 2014; McLeavey 1994; McMain 2009; McMain 2017; O'Connor 2017; Owens 2020; Priebe 2012; Slee 2008; Sreedaran 2020; Torhorst 1987; Torhorst 1988; Turner 2000; Walton 2020; Van Heeringen 1995), although for some trials, corresponding information on the proportion completing treatment in the comparator arm was not clearly reported. A smaller number of trials reported information on the total number of treatment sessions attended (Allard 1992; Brown 2005; McLeavey 1994; Torhorst 1988; Van der Sande 1997).
Depression
Depression was assessed using the BDI in just under half (47.6%) of the 42 trials that reported information on this outcome (Armitage 2016; Bateman 2009; Brown 2005; Fleischmann 2008; Gibbons 1978; Grimholt 2015; Guthrie 2001; Gysin‐Maillart 2016; Hawton 1987; Husain 2014; Liberman 1981; Linehan 1991; Marasinghe 2012; McAuliffe 2014; McMain 2009; McMain 2017; Salkovskis 1990; Slee 2008; Tapolaa 2010; Turner 2000), followed by the depression subscale of the HADS in six trials (Davidson 2014; Evans 1999b; Hatcher 2011; Hatcher 2015; Hatcher 2016; Tyrer 2003), the Hamilton Rating Scale for Depression (HRSD; Hamilton 1960) in eight trials (Andreoli 2015; Brown 2005; Harned 2014; Lin 2020; Linehan 2006; Linehan 2015; Turner 2000; Wei 2013), the Depression Anxiety Stress Scales (DASS; Lovibond 1995) in two trials (Gratz 2006; Gratz 2014), the Lorr and McNair Mood Scale (LMMS; McNair 1964) in one trial (Hawton 1981), the Montgomery‐Åsberg Depression Rating Scale (MADRS; Montgomery 1979) in one trial (Van der Sande 1997), and the Zung Self‐Rating Depression Scale (ZSRDS; Zung 1965) in one trial (Liberman 1981). In two trials, it was not clear what scale was used to assess depression (Torhorst 1987; Torhorst 1988).
Hopelessness
Hopelessness was assessed using the BHS in the majority (80.9%) of the 21 trials that reported information on this outcome (Brown 2005; Grimholt 2015; Hatcher 2011; Hatcher 2015; Hatcher 2016; Husain 2014; Kawanishi 2014; Lin 2020; Linehan 1991; McAuliffe 2014; McLeavey 1994; Patsiokas 1985; Salkovskis 1990; Stewart 2009; Van der Sande 1997; Waterhouse 1990; Wang 2016), by the future optimism subscale score on the Reasons for Living Inventory (RFL; Osman 1992), which was reverse coded in the present review to indicate a perceived lack of optimism about the future in three trials (Linehan 2015; O'Connor 2015; O'Connor 2020), and by an idiosyncratic scale in one trial (Mousavi 2017).
General functioning
General functioning was assessed using the Global Assessment Scale (GAS; Endicott 1976) in the majority (66.7%) of the six trials that reported information on this outcome (Allard 1992; Andreoli 2015; Bateman 2009; Tyrer 2003), followed by the GAF in the remaining two trials (Cedereke 2002; Sahin 2018).
Social functioning
Social functioning was assessed using the Social Adjustment Scale (SAS; Weissman 1999) in just over half (55.6%) of the nine trials that reported information on this outcome (Bateman 2009; Hawton 1981; Hawton 1987; McMain 2017; Torhorst 1988), the Social Functioning Questionnaire (SFQ; Tyrer 1990) in two trials (Evans 1999b; Tyrer 2003), and the social performance subscale of the Social Behaviour Assessment Schedule (SBAS; Platt 1983) in one trial (Waterhouse 1990). In one further trial, an idiosyncratic scale was used (Gibbons 1978).
Suicidal ideation
Eighteen trials assessed suicidal ideation using the BSSI (Brown 2005; Cedereke 2002; Davidson 2014; Grimholt 2015; Guthrie 2001; Gysin‐Maillart 2016; Hatcher 2011; Hawton 1981; Husain 2014; Lin 2020; Marasinghe 2012; McAuliffe 2014; O'Connor 2015; O'Connor 2020; Patsiokas 1985; Salkovskis 1990; Stewart 2009; Turner 2000), three trials used the Suicide Behaviors Questionnaire (SBQ; Linehan 1981) (Linehan 2006; Linehan 2015; Weinberg 2006), one trial used the Scale for Suicidal Ideators (SSI; Schotte 1982) (Linehan 1991), one the suicidal ideation subscale of the Psychiatric Status Schedule (PSS; Spitzer 1970) (Waterhouse 1990), and one the suicidal ideation subscale of the Suicide Risk Inventory (SRI; Hsu 1997) (Wang 2016). Six trials measured suicidal ideation dichotomously as the proportion with self‐reported suicidal ideation (Andreoli 2015; Hassanian‐Moghaddam 2011; Liberman 1981; Mousavi 2015; Mousavi 2017; Wei 2013).
Suicide
In over half of the 60 trials (60.0%) that recorded information on suicide, the method used to ascertain this outcome was not clearly reported (Andreoli 2015; Bateman 2009; Beautrais 2010; Brown 2005; Clarke 2002; Davidson 2014; Dubois 1999; Gratz 2006; Gratz 2014; Grimholt 2015; Guthrie 2001; Gysin‐Maillart 2016; Harned 2014; Husain 2014; Kapur 2013; Lin 2020; Linehan 1991; Linehan 2006; Linehan 2015; Marasinghe 2012; McLeavey 1994; McMain 2009; McMain 2017; Mousavi 2015; Naidoo 2014; Owens 2020; Priebe 2012; Sahin 2018; Salkovskis 1990; Slee 2008; Sreedaran 2020; Stewart 2009; Tapolaa 2010; Torhorst 1987; Walton 2020; Weinberg 2006). In the remaining trials, a variety of sources were used to ascertain suicide, including: Coroner's records (Allard 1992; Amadéo 2015; Hatcher 2011; Hatcher 2015; Hatcher 2016; Hvid 2011; Tyrer 2003), mortality registers (Carter 2005; Cedereke 2002; Hassanian‐Moghaddam 2011; Kawanishi 2014; Morthorst 2012; Mouaffak 2015; O'Connor 2017; Van Heeringen 1995), mortality statistics supplemented by Coroner’s records (Evans 1999a), hospital records (McAuliffe 2014), medical records (Van der Sande 1997), hospital and/or medical records supplemented by Coroner’s records (Vaiva 2006; Vaiva 2018), or from collateral informant report (Crawford 2010; Fleischmann 2008; Hawton 1987; Wei 2013).
Excluded studies
A total of 157 studies were excluded from this update. The most common reason for exclusion was that not all trial participants had engaged in SH within six months of trial entry (90 studies). Reasons for exclusion for the remaining studies are shown in Figure 1.
Details on the reasons for exclusion for those trials related to psychosocial interventions for SH in adults identified by this update are reported in the Characteristics of excluded studies section.
Ongoing studies
Of the 20 ongoing studies identified in the previous version of this review (Hawton 2016), seven were included in this update (Brown 2005; Lin 2020; O'Connor 2015; O'Connor 2017; O'Connor 2020; Owens 2020; Vaiva 2018). Ten were excluded: for three, trial results were unavailable, for two, trial registration subsequently lapsed, two were suspended due to feasibility difficulties, two subsequently included participants who had not engaged in SH, and one was subsequently published as a qualitative report.
A total of 25 ongoing studies were identified in this update (see Characteristics of ongoing studies section for further information).
Studies awaiting classification
Two potentially eligible trials could not be included in this review (NCT00533117; NCT00834834). Whilst results from these trials have been posted online, we were unable to confirm whether they met our inclusion criteria with the trial authors. Further information is provided in the Characteristics of studies awaiting classification section.
Risk of bias in included studies
Risk of bias was evaluated for the primary outcome repetition of SH at post‐intervention. The results of the 'Risk of bias' assessments can be seen in Figure 2 and Figure 3. Full 'Risk of bias' assessments, including the evidence we used to justify our ratings, are available here: doi.org/10.6084/m9.figshare.14159244.
2.
Summary of 'Risk of bias' assessments
3.
Results of 'Risk of bias' assessments for each study
Bias arising from randomisation process
All trials used random allocation to assign participants to the intervention and comparator arms. Most trials (98.7%) randomised at the individual level. In one trial, cluster randomisation was used (Bennewith 2002). Over half (55.3%) were rated as having a low risk of bias for this domain. Thirty (39.5%) trials were rated as having some concerns for this domain. For most of these, insufficient detail on either generation of the randomisation sequence and/or allocation concealment was reported (Allard 1992; Amadéo 2015; Brown 2005; Cedereke 2002; Dubois 1999; Gratz 2006; Gratz 2014; Kapur 2013; Liberman 1981; Linehan 2006; Marasinghe 2012; McLeavey 1994; Morgan 1993; Mousavi 2015; O'Connor 2020; Patsiokas 1985; Priebe 2012; Sahin 2018; Stewart 2009; Tapolaa 2010; Turner 2000; Van Heeringen 1995; Wang 2016; Wei 2013). For three further trials, baseline differences between the intervention and comparator arms suggested there may have been a problem with the randomisation process (Carter 2005; Guthrie 2001; Hatcher 2011), whilst for two older trials, information on characteristics of the intervention and comparator arms at baseline was not reported (Waterhouse 1990; Welu 1977). Four (5.3%) trials were rated as having high risk of bias for this domain due to insufficient detail on generation of the randomisation sequence and/or allocation concealment coupled with significant differences between the intervention and control arms at baseline on one or more factors, suggesting there may have been a problem with the randomisation process in these trials (Davidson 2014; O'Connor 2015; Torhorst 1987; Torhorst 1988).
Bias due to deviations from intended interventions
Whilst participants and clinical personnel were, typically, not blind to allocation owing to likely differences in treatment intensity between the intervention and comparator arms, most trials (69.9%) were nonetheless rated as being at low risk of bias for this domain as no deviations from the intended intervention were apparent and analyses were conducted on an intention‐to‐treat (ITT) basis, although the statistical method(s) used to undertake these analyses were not always clearly reported. Twenty‐one trials were rated as having some concerns for this domain. For the majority of these, there was insufficient information on the analyses method(s) used (Dubois 1999; Evans 1999b; Fleischmann 2008; Gibbons 1978; Gratz 2006; Hawton 1981; Liberman 1981; Linehan 1991; Linehan 2006; McAuliffe 2014; McLeavey 1994; Mousavi 2015; Mousavi 2017; O'Connor 2015; Patsiokas 1985; Sreedaran 2020; Torhorst 1987; Torhorst 1988; Waterhouse 1990; Welu 1977). For one, some minor departures from the intended intervention occurred as a result of the experimental context. Specifically, some participants moved GP practices. However, as the proportion of participants who moved practices was small and relatively balanced between the intervention and comparator arms in this trial, this was unlikely to have had a substantial impact on the results observed (Bennewith 2002). Two trials were rated as being at high risk of bias for this domain (Carter 2005; Naidoo 2014). In the first, some participants randomised to the control group mistakenly received the intervention treatment and whilst ITT analyses were undertaken, the impact was not balanced between the intervention and comparator arms in this trial (Carter 2005). In the second, the trial authors claimed the intervention was effective in preventing repeat SH even though there were major discrepancies in the data presented in the original trial report that we, as review authors, were unable to clarify through correspondence (Naidoo 2014).
Bias due to missing outcome data
The majority of trials (82.9%) were at low risk of bias for this domain as fewer than 5% of the data were missing at the post‐intervention assessment or, the proportion of missing data was balanced between the intervention and comparator arms at post‐intervention. However, there were some concerns with respect to this domain for four (5.3%) trials. For two of these, no data on repetition of SH were reported (Patsiokas 1985; Sahin 2018). For one, there was evidence of a larger proportion of missing data for the comparator arm as compared to the intervention arm (McAuliffe 2014), whilst, for one, the proportion of missing data was greater for the intervention arm (O'Connor 2015). None of these trials undertook sensitivity analyses to investigate the impact that missing data may have had on the estimate of treatment effectiveness.
Nine (11.8%) trials were rated as being at high risk of bias for this domain. For five of these, there was evidence of a difference in the proportion of missing data between the intervention and comparator arms, no information on likely causes of missingness was reported, and sensitivity analyses were not undertaken to investigate the impact of missing data (Davidson 2014; Evans 1999b; Grimholt 2015; McLeavey 1994; Wei 2013). For one trial, those with a repeat episode of SH during the follow‐up period were excluded from subsequent analyses (Sreedaran 2020); in another, data for over one‐third (38.1%) of the randomised sample were not included in follow‐up assessments (Linehan 1991). For another trial, there were major discrepancies in the data presented in the original trial report that we, as review authors, were unable to clarify through correspondence (Naidoo 2014). Finally, for one multisite and multi‐country trial there was evidence of substantial regional differences in missingness (Fleischmann 2008).
Bias in measurement of the outcome
There were some concerns regarding bias in the measurement of the outcome for just over one‐fifth (21.1%) of the trials included in this review. Typically, this was because repetition of SH was ascertained from self‐reported information alone and participants were either not blind to treatment allocation and/or participant blinding was unlikely to have been possible to achieve given the differences in therapeutic intensity between the intervention and comparator arms (Gratz 2014; Hassanian‐Moghaddam 2011; McAuliffe 2014; Mousavi 2017; O'Connor 2020; Priebe 2012; Slee 2008; Tapolaa 2010; Torhorst 1987; Torhorst 1988; Van Heeringen 1995; Walton 2020; Wei 2013; Weinberg 2006). For one trial, repetition of SH was ascertained from clinical personnel who were not blind to treatment allocation (Waterhouse 1990), whilst in another, repetition of SH was ascertained from unblinded clinical personnel for the majority of those allocated to the intervention arm (Allard 1992).
Ten (13.2%) trials were rated as being at high risk of bias for this domain. For most of these, repetition of SH was ascertained from self‐reported information alone, participant blinding was unlikely to have been possible to achieve given the differences in therapeutic intensity between the intervention and comparator arms, and assessment of the outcome could have been influenced by knowledge of the intervention received (Lin 2020; Linehan 1991; O'Connor 2015; Sahin 2018; Turner 2000; Welu 1977). For one trial, repetition of SH was obtained from self‐report. Given that participants assigned to the intervention and comparator arms in this trial received different treatment modalities (i.e. face‐to‐face versus telephone) and that previous work has shown that participants may be less willing to report sensitive information face‐to‐face than by telephone (Pridemore 2005), ascertainment of the outcome could have differed between groups in this trial (Mousavi 2015). For one further trial, there were major discrepancies for this outcome in the original trial report that we were unable to clarify through correspondence with the trial authors (Naidoo 2014). Finally, for two trials, no information on repetition of SH was reported (Patsiokas 1985; Sreedaran 2020).
Bias in selection of the reported result
Fourteen trials (18.4%) were rated as being at low risk of bias for this domain. Of these, only one clearly reported that data had been analysed in accordance with a prespecified analysis plan that had been finalised before unblinded outcome data and been made available for analysis (Tyrer 2003), whilst for 13 further trials there had been no major departures from the analysis plan as outlined in either a published trial protocol (Linehan 2015) or clinical trials register (Bateman 2009; Gysin‐Maillart 2016; Harned 2014; Hatcher 2011; Hatcher 2015; Hatcher 2016; Husain 2014; McMain 2017; O'Connor 2017; O'Connor 2020; Owens 2020; Vaiva 2018), although it should be noted that one of these trials was retrospectively registered (Bateman 2009).
Most trials (80.3%) were rated as having some concerns for this domain. In the majority of cases, this was because trials were published prior to the International Committee of Medical Journal Editors' (ICMJE) requirement in 2015 that all trials be preregistered in a publicly available clinical trials registry. It was, therefore, difficult to determine whether data had been analysed according to a prespecified plan, although there were no apparent departures from the analyses outlined in the methods section of these trials (Armitage 2016; Amadéo 2015; Andreoli 2015; Mouaffak 2015; Mousavi 2015; Mousavi 2017; Sahin 2018; Walton 2020; Wang 2016). For five trials that were preregistered, this domain was also rated as having some concerns, as the information provided within the clinical trials was not sufficiently detailed to determine whether there had been departures from the proposed analysis plan (Grimholt 2015; Kawanishi 2014; Lin 2020; McMain 2009; O'Connor 2015). For two further trials, there were some concerns for this domain as data on repetition of SH for one or more eligible time point(s) were not reported (Naidoo 2014; Salkovskis 1990); however, in both of these trials, it was unlikely results were selectively reported for favourability. Finally, for two trials, no information on repetition of SH was reported (Patsiokas 1985; Sreedaran 2020).
One trial was rated as being at high risk of bias for this domain as, although repetition of SH was a prespecified outcome, data at post‐intervention and at the 12‐month follow‐up assessment were not reported due to a high proportion of missing outcome data for these time points, although data at longer time points were reported (Sahin 2018). Additionally, we were unable to obtain unpublished data for these time points despite correspondence.
Overall bias
As a consequence, most trials (84.2%) were rated as either having some concerns or being at high risk of bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10; Table 11; Table 12; Table 13; Table 14; Table 15; Table 16; Table 17; Table 18; Table 19; Table 20; Table 21
Comparison 1: Cognitive behavioural therapy (CBT)‐based psychotherapy versus TAU or another comparator
Twenty‐one trials assessed the effectiveness of CBT‐based psychotherapy, in which participants in the intervention group were offered some form of specific psychological therapy such as CBT or problem‐solving therapy (PST), for adults (weighted mean age: 31.7 ± 12.1 years; 56.7% female) presenting to services following an episode of SH (Brown 2005, N = 120; Davidson 2014, N = 20; Dubois 1999, N = 102; Evans 1999b, N = 32; Gibbons 1978, N = 400; Guthrie 2001, N = 119; Hatcher 2011, N = 1094; Hawton 1987, N = 80; Husain 2014, N = 221; Lin 2020, N = 147; McAuliffe 2014, N = 433; Mousavi 2017, N = 60; Owens 2020, N = 62; Patsiokas 1985, N = 15; Salkovskis 1990, N = 20; Slee 2008, N = 82; Stewart 2009, N = 32; Tapolaa 2010, N = 16; Tyrer 2003, N = 480; Wei 2013, N = 162; Weinberg 2006, N = 30).
In most trials, therapy was typically very brief (i.e. ≤ 10 sessions) over a relatively brief period (i.e. median: three months; IQR: one to 3.7 months; range: one to 12 months), and was delivered on an individual basis in all but one (McAuliffe 2014).
Comparison 1.1: Individual cognitive behavioural therapy (CBT)‐based psychotherapy versus TAU or another comparator
For one trial (Stewart 2009), there were separate treatment arms for CBT and PST. We therefore combined data from these two conditions, given their similarity. For one further trial (Wei 2013), there were two intervention arms: CBT‐based psychotherapy and telephone contact. We therefore included only data for the CBT‐based psychotherapy arm.
Primary outcome
1.1.1 Repetition of SH
Four trials reported data on the proportion with a repeat episode of SH by the post‐intervention assessment (Mousavi 2017; Stewart 2009; Wei 2013; Weinberg 2006). While there was imprecision in the effect estimate, CBT‐based psychotherapy may reduce repetition of SH by post‐intervention (OR 0.35, 95% CI 0.12 to 1.02; participants = 238; studies = 4; I2 = 0%; Analysis 1.1). The overall risk of bias was high for one trial (Wei 2013) and there were some concerns for the remaining trials. According to GRADE criteria, we judged the evidence to be of low certainty.
1.1. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 1: Repetition of SH at post‐intervention
By the six‐month follow‐up assessment, on the basis of data from 12 trials, there was evidence of an effect for CBT‐based psychotherapy on repetition of SH (OR 0.52, 95% CI 0.38 to 0.70; N = 1260; k = 12; I² = 2%; Analysis 1.2). For one trial (Owens 2020), data on self‐reported SH were also reported. Using these data did not materially change this result.
1.2. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 2: Repetition of SH at six months
There was also evidence of an effect for CBT‐based psychotherapy by the 12‐month follow‐up assessment in nine trials (OR 0.81, 95% CI 0.66 to 0.99; N = 2458; k = 9; I² = 0%; Analysis 1.3). One trial also reported data for the consenting sample (i.e. including only those participants who, following treatment allocation, subsequently consented to participation), rather than all those randomised, as well as data on the proportion of participants self‐reporting an episode of SH rather than those admitted to hospital following an episode of SH, as well as data for the consenting sample (Hatcher 2011). Using either source of data for this trial, however, did not materially affect the overall result. Two trials reported data on repetition of SH by 24 months. An effect for this outcome was found (OR 0.31, 95% CI 0.14 to 0.69; N = 105; k = 2; I² = 0%; Analysis 1.4).
1.3. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 3: Repetition of SH at 12 months
1.4. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 4: Repetition of SH at 24 months
With respect to frequency of SH, data from four trials indicated no effect for CBT‐based psychotherapy on frequency of SH repetition by the post‐intervention assessment (MD ‐0.53, 95% CI ‐1.67 to 0.61; participants = 149; studies = 4; I2 = 62% ; Analysis 1.5). However, there was evidence of an effect for CBT‐based psychotherapy by the six‐month assessment (MD ‐0.71, 95% CI ‐1.32 to ‐0.11; N = 118; k = 4; I² = 0%; Analysis 1.6). One trial reported information on median, rather than mean, number of episodes of SH at six months. However, the authors found that although “[t]he rate of self‐harm episodes was lower in the [experimental] group...[it was not] significantly so” (Evans 1999b, pg.22).
1.5. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 5: Frequency of SH at post‐intervention
1.6. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 6: Frequency of SH at six months
There was evidence of an effect for CBT‐based psychotherapy by the 12‐month assessment in a single trial (mean 1.18, SD 4.22, n = 40 versus mean 4.58; SD 8.37; n = 33; MD ‐3.40, 95% CI ‐6.54 to ‐0.26; N = 73; k = 1; I² = not applicable; Slee 2008). A further trial reported information on median number of episodes of SH at 12 months’ follow‐up, finding that “[t]he median number of self‐harm episodes was two in both [the experimental and TAU] groups” (Tyrer 2003, pg.972).
Three trials reported numeric data on time to SH repetition. There was no evidence of an effect for CBT‐based psychotherapy on time to SH repetition in these three trials (Analysis 1.7). Four trials reported narrative information on time to SH repetition. In one, authors reported "[t]he time till next parasuicide act...showed trends in favour of MACT compared with TAU although [it was not] statistically significant" (Evans 1999b, pg.23), whilst in a second, trial authors reported "[i]n the experimental (treated) group, the mean time to repeat was 9.3 months, while the mean time to repeated attempt for the subjects in the control group was three months" (Salkovskis 1990, pg.874). However, trial authors in a third reported "Kaplan‐Maier survival analysis indicated that MACT effected no significant difference in time to repetition of DSH (log‐rank chi square = .88, df = 15, n.s.)" (Weinberg 2006, pg.487). Finally, in a more recent trial, "time to repetition...showed a more complex pattern, with speedier initial repetition among participants randomised to problem‐solving therapy" (Owens 2020, pg.9).
1.7. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 7: Time to SH repetition
Secondary outcomes
1.1.2 Treatment adherence
Data on treatment adherence was reported for both the intervention and comparator arms in one trial in which an effect for CBT‐based psychotherapy was found for the proportion of participants who completed all 12 sessions of therapy during the acute phase in addition to the three booster sessions (40/40 versus 33/42; OR 22.97, 95% CI 1.29 to 409.37; N = 82; k = 1; I² = not applicable; Slee 2008).
Five trials reported data on treatment adherence for the intervention arm only (Brown 2005; Evans 1999b; Husain 2014; Lin 2020; Owens 2020). Brown 2005 found that “participants in the cognitive therapy (CT) group participated in a mean (SD) of 8.92 (5.97) CT sessions (range 0‐24). Thirty participants (50%) received ten or more CT sessions” (pg.568). In Evans 1999b, five participants in the intervention group did not have specific sessions of manual‐assisted cognitive‐behaviour therapy (MACT) and received almost all input from the booklet component of CBT alone. Overall, 17 of the 18 participants in the experimental group received the booklets. Husain 2014 found that “more than half of the (intervention) group attended all six sessions (n = 56)” (pg.466). Lin 2020 found that "only around one fourth participants [sic] completed the scheduled intervention" (pg.697). Owens 2020 found that almost half (43.3%) attended all treatment sessions.
1.1.3 Depression
There was evidence of an effect for CBT‐based psychotherapy on depression scores at the post‐intervention assessment (SMD ‐0.28, 95% CI ‐0.54 to ‐0.02; N = 953; k = 4; I² = 71%; Analysis 1.8).
1.8. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 8: Depression scores at post‐intervention
There was no evidence of an effect for CBT‐based psychotherapy on depression scores at the six‐month assessment in eight trials (Analysis 1.9); however, there was evidence of an effect by the 12‐month assessment in seven trials (SMD ‐0.36, 95% CI ‐0.64 to ‐0.07; N = 1130; k = 7; I² = 76%; Analysis 1.10). One trial reported data on median (rather than mean) HDRS scores at six‐ and 12‐months follow‐up (Lin 2020); however, no effect was found for CBT‐based psychotherapy in this trial for this outcome.
1.9. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 9: Depression scores at six months
1.10. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 10: Depression scores at 12 months
Only two trials reported depression scores by the 24‐month follow‐up assessment; however, there was no evidence of an effect for CBT‐based psychotherapy by this time point (Analysis 1.11).
1.11. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 11: Depression scores at 24 months
1.1.4 Hopelessness
There was evidence of an effect for CBT‐based psychotherapy on hopelessness scores at the post‐intervention assessment in five trials (MD ‐2.99, 95% CI ‐3.91 to ‐2.07; N = 803; k = 5; I² = 0%; Analysis 1.12). One further trial also reported information on hopelessness scores at post‐intervention (Mousavi 2017); however, as an idiosyncratic scale was used in this trial, data could not be included in this review.
1.12. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 12: Hopelessness scores at post‐intervention
There was also evidence of an effect on hopelessness scores by the six‐month follow‐up assessment in two trials (MD ‐3.14, 95% CI ‐4.78 to ‐1.49; N = 315; k = 2; I² = 0%; Analysis 1.13).
1.13. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 13: Hopelessness scores at six months
Three trials reported data on hopelessness scores at 12 months, again showing a evidence of an effect for CBT‐based psychological therapy (MD ‐1.89, 95% CI ‐2.97 to ‐0.81; N = 539; k = 3; I² = 16%; Analysis 1.14). One further trial reported data on median (rather than mean) BHS scores at six‐ and 12‐months follow‐up (Lin 2020).
1.14. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 14: Hopelessness scores at 12 months
One trial reported data on hopelessness scores at 24 months (Brown 2005). However, there was no evidence of an effect for CBT‐based psychotherapy on hopelessness scores by this time point in this trial (mean 6.07, SD 5.28, n = 45 versus mean 7.24, SD 6.35, n = 40; MD ‐1.17, SD ‐3.67 to 1.33; N = 85; k = 1; I² = not applicable).
1.1.5 General functioning
One trial reported data on general functioning scores by the six‐month assessment. However, whilst there was no evidence of a difference in mean scores on this measure between the CBT‐based psychotherapy and TAU arms in this trial (i.e. 59.4 versus 59.6), insufficient information was reported to enable imputation of missing SDs (Tyrer 2003).
1.1.6 Social functioning
One trial reported data on social functioning scores at post‐intervention and, whilst there was no evidence of a difference in mean scores on this measure between the CBT‐based psychotherapy and TAU arms in this trial (i.e. 2.3 versus 2.3), insufficient information was reported to enable imputation of missing SDs (Hawton 1987).
Three trials reported data on social functioning by the six‐month follow‐up assessment (Evans 1999b; Hawton 1987; Tyrer 2003), however, for two of these trials insufficient information was reported to enable imputation of missing SDs (Hawton 1987; Tyrer 2003). For the remaining trial, there was evidence of an effect for CBT‐based psychological therapy on social functioning scores by this time point (mean 9.8, SD 4.9, n = 18 versus mean 13.1, SD 4.0, n = 12; MD ‐3.30, 95% CI ‐6.50 to ‐0.10; N = 30; k = 1; I² = not applicable; Evans 1999b).
One of these trials also reported data on social functioning scores by the 12‐month follow‐up period. However, whilst those allocated to CBT‐based psychotherapy had lower mean scores (i.e. 1.7 versus 2.1), once again insufficient information was reported to enable imputation of missing SDs (Hawton 1987).
1.1.7 Suicidal ideation
There was evidence of an effect for CBT‐based psychotherapy in five trials at the post‐intervention assessment (SMD ‐0.48, 95% CI ‐0.68 to ‐0.28; N = 718; k = 5; I² = 20%; Analysis 1.15), and by the six‐month follow‐up assessment in four trials (SMD ‐0.38, 95% CI ‐0.60 to ‐0.17; N = 353; k = 4; I² = 0%; Analysis 1.16).
1.15. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 15: Suicidal ideation scores at post‐intervention
1.16. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 16: Suicidal ideation scores at six months
One trial reported information on suicidal ideation scores by 12 months; however, CBT‐based psychotherapy was not associated with an effect by this time point in this trial (mean 3.70, SD 6.70, n = 187 versus mean 4.80, SD 7.40, n = 231; MD ‐1.10, 95% CI ‐2.45 to 0.25; N = 418; k = 1; I² = not applicable; Hatcher 2011). One trial reported data on median (rather than mean) BSSI scores at six‐ and 12‐months follow‐up (Lin 2020); however, no effect was found for CBT‐based psychotherapy in this trial for this outcome.
Two trials reported information on the proportion of participants with suicidal ideation (Mousavi 2017; Wei 2013). At post‐intervention, data from both of these trials indicated no evidence of an effect for CBT‐based psychotherapy. There was also no evidence of an effect by the six‐month or 12‐month follow‐up assessments in one of these trials (Analysis 1.17). However, it is notable that for one of these trials (Wei 2013), results were reported on the basis of those randomised despite the fact that a self‐reported measure was used, and high levels of dropout were observed by the 12‐month follow‐up assessment. As we were unable to confirm these numbers with trial authors, results much be interpreted with caution.
1.17. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 17: Proportion reporting suicidal ideation
One trial reported data on BSSI scores, however, insufficient information was available to enable imputation of missing SDs (Salkovskis 1990). One further trial reported data on the proportion scoring above zero on the BSSI at the post‐intervention, 6, 12, and 24‐month follow‐up assessments (Brown 2005), however, as this was not based on clinically established cut‐points, these data were unable to be included in this review.
1.1.8 Suicide
Sixteen trials reported data on suicide deaths during follow‐up. There was no evidence of an effect for CBT‐based psychotherapy on suicides by final follow‐up (i.e. up to 24 months) (Analysis 1.18). In one trial, there was one death in the intervention arm that medical staff considered to be a suicide, although the coroner did not record a suicide verdict in this case (Tyrer 2003). Including this death as a suicide did not materially change the overall result.
1.18. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 18: Suicide deaths by final follow‐up
Subgroup analyses
Two further trials reported data on repetition of SH by repeater status (Hatcher 2011; Lin 2020). There was no evidence of an effect for CBT‐based psychotherapy on repetition of SH by the six‐month follow‐up assessment for either those with a history of repeated SH (7/39 versus 16/49; OR 0.45, 95% CI 0.16 to 1.24; N = 88; k = 1; I² = not applicable; Lin 2020), or those without this history (3/33 versus 7/26; OR 0.27, 95% CI 0.06 to 1.18; N = 59; k = 1; I² = not applicable; Lin 2020) in one trial. However, by the 12‐month follow‐up assessment, data from these two trials indicated that whilst CBT‐based psychotherapy was not associated with an effect on repetition of SH for those without a history of SH prior to trial entry (Analysis 1.19), there was evidence of an effect on this outcome for those with a history of multiple episodes of SH (OR 0.56, 95% CI 0.36 to 0.88; N = 508; k = 1; I² = 0%; Analysis 1.19). However, the test for subgroup differences was not statistically significant for this outcome at this time point (Chi² = 1.97, df = 1, p = 0.16).
1.19. Analysis.

Comparison 1: CBT‐based psychotherapy, Outcome 19: Repetition of SH at 12 months (by repeater status)
With regards to time to SH repetition, data from one of these trials suggested that, whilst there was no evidence of an effect in those without a history of multiple episodes of SH prior to trial entry (HR 1.55, 95% CI 0.98 to 2.48; N = 135; k = 1; I² = not applicable), CBT‐based psychotherapy was associated with an effect on time to SH repetition in those with a history of multiple episodes of SH (HR 0.58, 95% CI 0.36 to 0.94; N = 194; k = 1; I² = not applicable) in this trial (Hatcher 2011).
Sensitivity analyses
One trial used Zelen's design (Hatcher 2011). Omitting this trial did not materially affect results for CBT‐based psychotherapy on repetition of SH by the 12‐month assessment, depression scores at the 12‐month assessment, hopelessness scores by the post‐intervention or 12‐month assessments, or suicidal ideation scores at post‐intervention. However, omitting this trial did cause a reduction in the SMD for CBT‐based psychotherapy on depression scores by the post‐intervention assessment and the estimate was no longer statistically significant (SMD ‐0.19, 95% CI ‐0.40 to 0.02; N = 313; k = 5; I² = 54%).
Two analyses within this comparison were associated with substantial levels of heterogeneity (Analysis 1.10, I² = 76%; Analysis 1.17.1, I² = 85%); however, analyses did not indicate any individual study was associated with excessive influence for either of these outcomes.
Comparison 1.2: Group‐based cognitive behavioural therapy (CBT)‐based psychotherapy versus TAU or another comparator
Primary outcome
1.2.1 Repetition of SH
There was no evidence of an effect for CBT‐based psychotherapy, delivered in a group‐based format, as compared to TAU by the post‐intervention assessment in a single trial (23/171 versus 27/142; OR 0.66, 95% CI 0.36 to 1.21; N = 313; k = 1; I² = not applicable). According to GRADE criteria, we judged the evidence to be of moderate certainty.
There was also no evidence of an effect for group‐based CBT‐based psychotherapy on repetition of SH by the six‐month follow‐up assessment (39/128 versus 26/106; OR 1.35, 95% CI 0.75 to 2.41; N = 234; k = 1; I² = not applicable), or by the 12‐month follow‐up assessment (54/222 versus 50/211; OR 1.03, 95% CI 0.67 to 1.61; N = 433; k = 1; I² = not applicable).
There was also no evidence of an effect for group‐based CBT‐based psychotherapy on frequency of SH repetition by the 12‐month follow‐up assessment in this trial (mean 0.43, SD 1.23, n = 222 versus mean 0.49, SD 1.53, n = 211; MD ‐0.06, 95% CI ‐0.32 to 0.20; N = 433; n = 1; I² = not applicable).
Secondary outcomes
1.2.2 Treatment adherence
Data on treatment adherence was reported for the intervention arm only. The authors found that “almost half of those assigned to [problem‐solving therapy] (103, 46.4%) attended all 6 therapy sessions” (McAuliffe 2014, pg.4).
1.2.3 Depression
There was no evidence of an effect for group‐based CBT‐based psychotherapy on depression by either the post‐intervention (mean 18.20, SD 14.80, n = 171 versus mean 20.60, SD 16.00, n = 142; MD ‐0.16, 95% CI ‐0.38 to 0.07; N = 313; k = 1; I² = not applicable) or the six‐month follow‐up assessment (mean 17.30, SD 15.90, n = 128 versus mean 19.40, SD 17.00, n = 106; MD ‐0.13, 95% CI ‐0.39 to 0.13; N = 234; k = 1; I² = not applicable).
1.2.4 Hopelessness
There was also no evidence of an effect for group‐based CBT‐based psychotherapy on hopelessness scores at the post‐intervention (mean 6.50, SD 6.10, n = 171 versus mean 7.30, SD 6.20, n = 142; MD ‐0.80, 95% CI ‐2.17 to 0.57; N = 313; k = 1; I² = not applicable) or six‐month follow‐up assessment (mean 6.80, SD 6.30, n = 128 versus mean 7.10, SD 6.10, n = 106; MD ‐0.30, 95% CI ‐1.89 to 1.29; N = 234; k = 1; I² = not applicable).
1.2.5 General functioning
No data available.
1.2.6 Social functioning
No data available.
1.2.7 Suicidal ideation
There was no evidence of an effect for group‐based CBT‐based psychotherapy on suicidal ideation by either the post‐intervention (mean 4.30, SD 8.00, n = 171 versus mean 5.80, SD 9.70, n = 142; MD ‐1.50, 95% CI ‐3.50 to 0.50; N = 313; k = 1; I² = not applicable) or the six‐month follow‐up assessment (mean 4.70, SD 8.90, n = 128 versus mean 4.90, SD 8.90, n = 106; MD ‐0.20, 95% CI ‐2.49 to 2.09; N = 234; k = 1; I² = not applicable).
1.2.8 Suicide
There was no evidence of an effect for group‐based CBT‐based psychotherapy on suicide deaths by the final follow‐up assessment (1/222 versus 2/211; OR 0.47, 95% CI 0.04 to 5.25; N = 433; k = 1; I² = not applicable).
Subgroup analyses
Randomisation was stratified by both sex and repeater status in this trial (McAuliffe 2014). However, we were unable to obtain data disaggregated by either factor from the trial authors.
Sensitivity analyses
Not applicable.
Comparison 2: Dialectical behavioural therapy (DBT) versus TAU or another comparator
Ten trials investigated the effectiveness of dialectical behaviour therapy (DBT) as compared to either TAU (Linehan 1991, N = 63; McMain 2009, N = 180; McMain 2017, N = 84; Priebe 2012, N = 80; Sahin 2018, N = 50) or other forms of alternative psychotherapy (Harned 2014, N = 26; Linehan 2006, N = 101; Linehan 2015, N = 99; Turner 2000, N = 24; Walton 2020, N = 166) in adults (weighted mean age: 27.5 ± 11.3 years; 89.7% female) diagnosed with a personality disorder, typically borderline personality disorder, and who were receiving treatment from outpatient mental health services due to recurrent SH.
For one of these trials, there were two different intervention arms: psychodynamic psychotherapy and DBT (Sahin 2018). We therefore included only data for the DBT arm. For a second of these trials, comparison was made between two different forms of DBT: DBT group‐based skills training only (DBT‐S; Linehan 2015a) and DBT individual therapy only (DBT‐I; Linehan 2015b).
Comparison 2.1: Standard DBT
Primary outcome
2.1.1 Repetition of SH
Overall, there was no evidence of an effect for standard DBT compared to either TAU or alternative psychotherapy in terms of the proportion of patients repeating SH by the post‐intervention assessment (OR 0.71, 95% CI 0.32 to 1.55; participants = 502; studies = 6; I2 = 60%; (Analysis 2.1). There was also no difference by comparator (i.e. TAU versus alternative psychotherapy). The overall risk of bias was high for two trials (Linehan 1991; Turner 2000) and there were some concerns for the remaining trials. According to GRADE criteria, we judged the evidence to be of very low certainty.
2.1. Analysis.

Comparison 2: DBT, Outcome 1: Repetition of SH by post‐intervention
There was also no evidence of an effect for DBT on repetition of SH by the 12‐month (OR 0.65, 95% CI 0.24 to 1.72; participants = 269; studies = 3; I2 = 47%; Analysis 2.2) assessment. Once again, there was no difference by comparator (i.e. TAU versus alternative psychotherapy).
2.2. Analysis.

Comparison 2: DBT, Outcome 2: Repetition of SH by 12 months
DBT was associated with an effect for frequency of repeated SH by the post‐intervention assessment when compared to either TAU or alterative psychotherapy (MD ‐5.00, 95% CI ‐8.92 to ‐1.08; N = 659; k = 7; I² = 49%; Analysis 2.3). However, this effect was no longer found by the six‐month follow‐up assessment in one trial (mean 0.32, SD 1.27, n = 42 versus mean 1.14, SD 3.94, n = 42; MD ‐0.82, 95% CI ‐2.07 to 0.43; N = 84; k = 1; I² = not applicable; McMain 2017). Following a 'naturalistic' follow‐up period, data from one further trial indicated that the effectiveness of DBT in terms of frequency of SH was maintained at 24 months in this trial; however, this outcome was only investigated for a proportion of the original participants (61.9%) who the researchers were able to contact at 24 months (Linehan 1991). Results have therefore not been reproduced in this review.
2.3. Analysis.

Comparison 2: DBT, Outcome 3: Frequency of SH by post‐intervention
One trial reported information on time to repetition of SH, finding that those "receiving DBT were half as likely to make a suicide attempt (hazard ratio, 2.66; P = .005)" (Linehan 2006, pg.757). However, insufficient information was reported to enable calculation of the accompanying CIs for this outcome for this trial.
Secondary outcomes
2.1.2 Treatment adherence
There was no evidence of an effect for DBT compared with either TAU or alternative psychotherapy for the proportion of participants who completed treatment (Analysis 2.4). There was also no evidence of a difference by comparator. Two further trials did not report information on the proportion completing treatment in the comparator arm (McMain 2017; Priebe 2012), although the comparator in the former trial was a waiting‐list control condition. We were, therefore, unable to incorporate these results in a meta‐analysis.
2.4. Analysis.

Comparison 2: DBT, Outcome 4: Treatment adherence: Proportion completing treatment
2.1.3 Depression
There was evidence of an effect for DBT compared to both TAU or alternative psychotherapy on depression scores at post‐intervention (SMD ‐0.37, 95% CI ‐0.58 to ‐0.17; N = 557; k = 6; I² = 23%; Analysis 2.5). There was no evidence of a difference by comparator. One trial also measured depression scores at post‐intervention using the HRSD; however, there was no evidence of an effect for DBT according to this measure in this trial (mean 7.50, SD 5.96, n = 12 versus mean 12.58, SD 3.90, n = 12; MD ‐5.08, 95% CI ‐9.11 to ‐1.05; N = 24; k = 1; I² = not applicable; Turner 2000).
2.5. Analysis.

Comparison 2: DBT, Outcome 5: Depression scores by post‐intervention
There was no evidence of an effect for DBT on depression scores by the six‐month follow‐up assessment in one trial (mean 27.94, SD 16.08, n = 42 versus mean 29.50, SD 15.71, n = 42; MD ‐1.56, 95% CI ‐8.36 to 5.24; N = 84; k = 1; I² = not applicable; McMain 2017) or by the 12‐month follow‐up assessment in one further trial (mean 12.60, SD 6.80, n = 46 versus mean 14.40, SD 9.10, n = 35; MD ‐1.80, 95% CI ‐5.40 to 1.80; N = 81; k = 1; I² = not applicable; Linehan 2006).
2.1.4 Hopelessness
We obtained data on hopelessness by correspondence for one trial (Linehan 1991); however, there was no evidence of an effect for DBT as compared to TAU by the 24‐month follow‐up assessment in this trial (mean 10.86, SD 6.04, n = 7 versus mean 10.69, SD 6.18, n = 11; MD 0.17, 95% CI ‐5.61 to 5.95; N = 18; k = 1; I² = not applicable).
2.1.5 General functioning
No data available.
2.1.6 Social functioning
One trial reported data on social functioning scores at post‐intervention and by the six‐month follow‐up assessment (McMain 2017). Whilst there was evidence of an effect for DBT on social functioning scores at post‐intervention in this trial (mean 2.50, SD 0.56, n = 42 versus mean 2.88, SD 0.59, n = 42; MD ‐0.38, 95% CI ‐0.63 to ‐0.13; N = 84; k = 1; I² = not applicable), this effect was no longer apparent by the six‐month follow‐up assessment (mean 2.60, SD 0.70, n = 42 versus mean 2.87, SD 0.65, n = 42; MD ‐0.27, 95% CI ‐0.56 to 0.02; N = 84; k = 1; I² = not applicable).
2.1.7 Suicidal ideation
There was no evidence of an effect for DBT when compared either to TAU or to alternative psychotherapy on suicidal ideation scores at the post‐intervention assessment in three trials (Analysis 2.6), or by the 12‐month assessment in one of these trials (mean 24.10, SD 19.80, n = 46 versus mean 31.92, SD 26.80, n = 35; MD ‐7.80, 95% CI ‐18.38 to 2.74; N = 81; k = 1; I² = not applicable; Linehan 2006). There was also no evidence of a difference by comparator.
2.6. Analysis.

Comparison 2: DBT, Outcome 6: Suicidal ideation scores by post‐intervention
2.1.8 Suicide
There was no evidence of an effect for DBT as compared to either TAU or alternative psychotherapy on suicide deaths at either post‐intervention (Analysis 2.7), the 12‐month (Analysis 2.8), or 24‐month follow‐up period (Analysis 2.9).
2.7. Analysis.

Comparison 2: DBT, Outcome 7: Suicide deaths by post‐intervention
2.8. Analysis.

Comparison 2: DBT, Outcome 8: Suicide deaths by 12 months
2.9. Analysis.

Comparison 2: DBT, Outcome 9: Suicide deaths by 24 months
Subgroup analyses
Randomisation was stratified by sex in one trial (Walton 2020). Whilst data obtained by correspondence from the trial authors indicated that, compared with alternative psychotherapy, DBT was not associated with an effect on repetition of SH by the post‐intervention assessment for females (21/38 versus 33/50; OR 0.64, 95% CI 0.27 to 1.52; N = 88; k = 1; I² = not applicable), DBT may be associated with a greater proportion of males engaging in a repeat episode of SH at this time point (12/13 versus 6/13; OR 14.00, 95% CI 1.39 to 141.49; N = 26; k = 1; I² = not applicable).
With regards to frequency of SH repetition, data obtained by correspondence for this trial indicated that, whilst DBT was associated with an effect at post‐intervention for females (mean 5.08, SD 11.13, n = 38 versus mean 17.66, SD 33.10, n = 50; MD ‐12.58, 95% CI ‐22.41 to ‐2.75; N = 88; k = 1; I² = not applicable), there was no evidence of an effect for males (mean 5.77, SD 5.34, n = 13 versus mean 4.93, SD 7.24, n = 13; MD 0.84, 95% CI ‐4.05 to 5.73; N = 26; k = 1; I² = not applicable).
There was no evidence of an effect for DBT as compared to alternative psychotherapy on the proportion of males (9/19 versus 11/18; OR 0.57, 95% CI 0.15 to 2.12; N = 37; k = 1; I² = not applicable) or females (35/62 versus 37/63; OR 0.91, 95% CI 0.45 to 1.85; N = 125; k = 1; I² = not applicable) who completed the full course of treatment on this trial.
Finally, whilst DBT was associated with an effect on depression scores as compared to alternative psychotherapy at the post‐intervention assessment for males (mean 13.54, SD 12.82, n = 13 versus mean 23.70, SD 12.30, n = 12; MD ‐10.16, 95% CI ‐20.01 to ‐0.31; N = 25; k = 1; I² = not applicable), there was no evidence of an effect on depression scores for females in this trial (mean 15.34, SD 14.01, n = 37 versus mean 21.88, SD 19.00, n = 48; MD ‐6.54, 95% CI ‐13.56 to 0.48; N = 85; I² = not applicable).
Sensitivity analyses
Not applicable.
Comparison 2.2: DBT group‐based skills training
For one trial (i.e. Linehan 2015), there were two different intervention arms: DBT group‐based skills training only (DBT‐S; Linehan 2015a) and DBT individual therapy only (DBT‐I; Linehan 2015b). For a detailed description of the therapeutic content of the two different intervention arms included in this trial, see the Characteristics of included studies section.
Here we included results for DBT group‐based skills training only as compared with standard DBT in adult women (mean age: 30.4 ± 7.5 years) diagnosed with borderline personality disorder referred for outpatient treatment for repeated SH (Linehan 2015a, N = 66).
Primary outcome
2.2.1 Repetition of SH
In this trial, data on repetition of SH were reported separately for episodes of attempted suicide and NSSI. As we were unable to obtain data on combined SH from the trial authors despite correspondence, we have reproduced the results for attempted suicide and NSSI separately.
There was no evidence of an effect for DBT group‐based skills training only as compared with standard DBT on suicide reattempts (9/33 versus 12/33; OR 0.66, 95% CI 0.23 to 1.86; N = 66; k = 1; I² = not applicable) or NSSI (18/33 versus 19/33; OR 0.88, 95% CI 0.33 to 2.34; N = 66; k = 1; I² = not applicable) at post‐intervention. According to GRADE criteria, we judged the evidence to be of moderate certainty.
There was also no evidence of an effect for DBT group‐based skills training only on suicide reattempts (6/33 versus 2/33; OR 3.44, 95% CI 0.64 to 18.51; N = 66; k = 1; I² = not applicable) or NSSI (15/33 versus 15/33; OR 1.00, 95% CI 0.38 to 2.64; N = 66; k = 1; I² = not applicable) by the 12‐month assessment in this trial.
There was no evidence of an effect for DBT group‐based skills training only on frequency of suicide reattempts (mean 2.60, SD 2.90, n = 33 versus mean 3.40, SD 4.60, n = 33; MD ‐0.80, 95% CI ‐2.66 to 1.06; N = 66; k = 1; I² = not applicable) or episodes of NSSI (mean 9.90, SD 19.70, n = 33 versus mean 10.20, SD 16.30, n = 33; MD ‐0.30, 95% CI ‐9.02 to 8.42; N = 66; k = 1; I² = not applicable) at post‐intervention. Nor was there any evidence of an effect for this intervention on frequency of suicide reattempts (mean 1.50, SD 0.60, n = 33 versus mean 2.00, SD 1.40, n = 33; MD ‐0.50, 95% CI ‐1.02 to 0.02; N = 66; k = 1; I² = not applicable) or episodes of NSSI (mean 9.40, SD 20.40, n = 33 versus mean 7.90, SD 8.50, n = 33; MD 1.50, 95% CI ‐6.04 to 9.04; N = 66; k = 1; I² = not applicable) by the 12‐month follow‐up assessment in this trial.
Finally, with regards to time to SH repetition, "[s]urvival analysis...indicated no difference between groups in the time to the first suicide attempt (χ² = 1.4 [P = .50])" (Linehan 2015, pg.4).
Secondary outcomes
2.2.2 Treatment adherence
There was no evidence of an effect for DBT group‐based skills training, as compared with standard DBT, on the proportion of participants who completed treatment by the post‐intervention assessment in this trial (20/33 versus 25/33; OR 0.49, 95% CI 0.17 to 1.42; N = 66; k = 1; I² = not applicable; Linehan 2015a).
There was also no evidence of an effect for DBT group‐based skills training, as compared with standard DBT, on the number of group therapy sessions attended (mean 4.20, SD 0.11, n = 33 versus mean 4.20, SD 0.12, n = 33; MD 0.00, 95% CI ‐0.06 to 0.06; N = 66; k = 1; I² = not applicable; Linehan 2015a). Information on the number of individual therapy sessions attended could not be estimated as individuals assigned to the group‐based skills training arm in this trial did not receive any individual therapy sessions.
2.2.3 Depression
There was no evidence of a significant treatment effect for DBT group‐based skills training, as compared with standard DBT, on depression scores at either the post‐intervention (mean 10.40, SD 6.40, n = 33 versus mean 12.30, SD 8.00, n = 33; MD ‐1.90, 95% CI ‐5.40 to 1.60; N = 66; k = 1; I² = not applicable), or 12‐month assessment (mean 11.90, SD 8.80, n = 33 versus mean 15.20, 8.60, n = 33; MD ‐3.30, 95% CI ‐7.50 to 0.90; N = 66; k = 1; I² = not applicable; Linehan 2015a).
2.2.4 Hopelessness
There was also no evidence of an effect for DBT group‐based skills training, as compared with standard DBT, on hopelessness at either the post‐intervention (mean ‐155.30, SD 41.40, n = 33 versus mean ‐168.70, SD 45.3, n = 33; MD 13.40, 95% CI ‐7.54 to 34.34; N = 66; k = 1; I² = not applicable) or 12‐month follow‐up assessment (mean ‐152.20, SD 43.20, n = 33 versus mean ‐159.90, SD 40.20, n = 33; MD 7.40, 95% CI ‐12.73 to 27.53; N = 66; k = 1; I² = not applicable; Linehan 2015a) in this trial.
2.2.5 General functioning
No data available.
2.2.6 Social functioning
No data available.
2.2.7 Suicidal ideation
There was no evidence of an effect for DBT group‐based skills training, as compared with standard DBT, on suicidal ideation scores at either the post‐intervention (mean 27.50, SD 19.10, n = 33 versus mean 32.00, SD 21.60, n = 33; MD ‐4.50, 95% CI ‐14.34 to 5.34; N = 66; k = 1; I² = not applicable) or 12‐month follow‐up assessment (mean 21.20, SD 19.20, n = 33 versus mean 28.90, SD 16.60, n = 33; MD ‐7.80, 95% CI ‐16.46 to 0.86; N = 66; k = 1; I² = not applicable).
2.2.8 Suicide
There was one suicide death in the standard DBT arm by the 24‐month follow up assessment in this trial; however, there was no evidence of an effect for DBT group‐based skills training, as compared with standard DBT, on this outcome by this time point (0/33 versus 1/33; OR 0.32, 95% CI 0.01 to 8.23; N = 66; k = 1; I² = not applicable).
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 2.3: DBT individual therapy
For one trial (i.e. Linehan 2015), there were two different intervention arms: DBT group‐based skills training only (DBT‐S; Linehan 2015a) and DBT individual therapy only (DBT‐I; Linehan 2015b). For a detailed description of the therapeutic content of the two different intervention arms included in this trial, see the Characteristics of included studies section.
Here we included results for DBT individual therapy only as compared with standard DBT in adult women (mean age: 30.6 ± 7.9 years) diagnosed with borderline personality disorder referred for outpatient treatment for repeated SH (Linehan 2015b, N = 66).
Primary outcome
2.3.1 Repetition of SH
As before, in this trial, data on repetition of SH were reported separately for episodes of attempted suicide and NSSI. As we were unable to obtain data on combined SH from the trial authors despite correspondence, we have reproduced the results for attempted suicide and NSSI separately.
There was no evidence of an effect for DBT individual therapy only as compared with standard DBT on suicide reattempts (15/33 versus 12/33; OR 1.46, 95% CI 0.54 to 3.91; N = 66; k = 1; I² = not applicable) or NSSI (21/33 versus 19/33; OR 1.29, 95% CI 0.48 to 3.47; N = 66; k = 1; I² = not applicable) at post‐intervention. According to the GRADE criteria, we judged the evidence to be of moderate certainty.
There was also no evidence of an effect for DBT individual therapy only on suicide reattempts (7/33 versus 2/33; OR 4.17, 95% CI 0.80 to 21.85; N = 66; k = 1; I² = not applicable) or NSSI (13/33 versus 15/33; OR 0.78, 95% CI 0.29 to 2.07; N = 66; k = 1; I² = not applicable) by the 12‐month assessment in this trial.
There was no evidence of an effect for DBT individual therapy only on frequency of suicide reattempts (mean 2.90, SD 3.00, n = 33 versus mean 3.40, SD 4.60, n = 33; MD ‐0.50, 95% CI ‐2.37 to 1.37; N = 66; k = 1; I² = not applicable) or episodes of NSSI (mean 20.60, SD 33.10, n = 33 versus mean 10.20, SD 16.30, n = 33; MD 10.40, 95% CI ‐2.19 to 22.99; N = 66; k = 1; I² = not applicable) at post‐intervention. Nor was there any evidence of an effect for this intervention on frequency of suicide reattempts (mean 3.60, SD 3.20, n = 33 versus mean 2.00, SD 1.40, n = 33; MD 1.60, 95% CI 0.41 to 2.79; N = 66; k = 1; I² = not applicable) or episodes of NSSI (mean 16.00, SD 32.60, n = 33 versus mean 7.90, SD 8.50, n = 33; MD 8.10, 95% CI ‐3.39 to 19.59; N = 66; k = 1; I² = not applicable) by the 12‐month follow‐up assessment in this trial.
Finally, with regards to time to SH repetition, "[s]urvival analysis...indicated no difference between groups in the time to the first suicide attempt (χ² = 1.4 [P = .50])" (Linehan 2015, pg.4).
Secondary outcomes
2.3.2 Treatment adherence
There was evidence of an effect for DBT individual therapy, as compared with standard DBT, on the proportion of participants who completed treatment by the post‐intervention assessment in this trial (17/33 versus 25/33; OR 0.34, 95% CI 0.12 to 0.97; N = 66; k = 1; I² = not applicable; Linehan 2015b).
There was no evidence of an effect for DBT individual therapy, as compared with standard DBT, on the number of individual therapy sessions attended (mean 4.16, SD 0.18, n = 33 versus mean 4.20, SD 0.18, n = 33; MD ‐0.04, 95% CI ‐0.13 to 0.05; N = 33; k = 1; I² = not applicable; Linehan 2015b). Information on the number of group therapy sessions attended could not be estimated as participants assigned to the individual therapy arm in this trial did not receive any group‐based therapy sessions.
2.3.3 Depression
There was evidence of an increase in depression scores at post‐intervention for those receiving DBT individual therapy (mean 18.20, SD 7.90, n = 33 versus mean 12.30, SD 8.00, n = 33; MD 5.90, 95% CI 2.06 to 9.74; N = 66; k = 1; I² = not applicable). By the 12‐month follow‐up assessment, however, there was no longer evidence of an effect on depression scores for DBT individual therapy, as compared with standard DBT in this trial (mean 13.90, SD 9.60, n = 33 versus mean 15.20, 8.60, n = 33; MD ‐1.30, 95% CI ‐5.70 to 3.10; N = 66; k = 1; I² = not applicable).
2.3.4 Hopelessness
There was no evidence of an effect for DBT individual therapy, as compared with standard DBT, on hopelessness at either the post‐intervention (mean ‐177.90, SD 53.10, n = 33 versus mean ‐168.70, SD 45.30, n = 33; MD ‐9.20, 95% CI ‐33.01 to 14.61; N = 66; k = 1; I² = not applicable), or 12‐month follow‐up assessment (mean ‐178.40, SD 53.70, n = 33 versus mean ‐159.90, SD 40.20, n = 33; MD ‐18.50, 95% CI ‐41.39 to 4.39; N = 66; k = 1; I² = not applicable) in this trial.
2.3.5 General functioning
No data available.
2.3.6 Social functioning
No data available.
2.3.7 Suicidal ideation
There was also no evidence of an effect for DBT individual therapy, as compared with standard DBT, on suicidal ideation scores at either the post‐intervention (mean 30.30, SD 27.50, n = 33 versus mean 32.00, SD 21.60, n = 33; MD ‐1.70, 95% CI ‐13.63 to 10.23; N = 66; k = 1; I² = not applicable) or 12‐month follow‐up assessment (mean 25.50, SD 20.80, n = 33 versus mean 28.90, SD 16.60, n = 33; MD ‐3.40, 95% CI ‐12.48 to 5.68; N = 66; k = 1; I² = not applicable).
2.3.8 Suicide
There was one suicide death in the standard DBT arm by the 24‐month follow‐up assessment in this trial; however, there was no evidence of an effect for DBT individual therapy only on this outcome by this time point (0/33 versus 1/33; OR 0.32, 95% CI 0.01 to 8.23; N = 66; k = 1; I² = not applicable).
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 2.4: DBT prolonged‐exposure protocol
The effectiveness of two forms of DBT were compared over a three‐month period in one small trial of adult (mean age: 32.6 ± 12.0 years) women diagnosed with comorbid borderline personality disorder and post‐traumatic stress disorder and who were referred to outpatient clinical services due to recurrent SH (Harned 2014, N = 26). In this trial, participants assigned to the intervention arm received, in addition to the standard DBT protocol, additional weekly therapy sessions involving in vivo and imaginal exposure to previously traumatic experiences (i.e. DBT prolonged‐exposure protocol).
Primary outcome
2.4.1 Repetition of SH
Data obtained by correspondence indicated there was no evidence of an effect for the DBT prolonged‐exposure protocol on repetition of SH by the post‐intervention assessment (3/12 versus 2/6; OR 0.67, 95% CI 0.08 to 5.68; N = 18; k = 1; I² = not applicable). According to GRADE criteria, we judged the evidence to be of moderate certainty.
There was also no evidence of an effect for the DBT prolonged‐exposure protocol on repetition of SH by the six‐month follow‐up assessment (3/12 versus 2/6; OR 0.67, 95% CI 0.08 to 5.68; N = 18; k = 1; I² = not applicable).
Data on frequency of SH, obtained following correspondence with trial authors, also suggested no effect for the DBT prolonged‐exposure protocol by either the post‐intervention (mean 0.92, SD 1.97, n = 12 versus mean 1.17, SD 2.40, n = 6; MD ‐0.25, 95% CI ‐2.47 to 1.97; N = 18; k = 1; I² = not applicable) or six‐month follow‐up assessments (mean 0.67, SD 1.50, n = 12 versus mean 0.33, SD 0.52, n = 6; MD 0.34, 95% CI ‐0.61 to 1.29; N = 18; k = 1; I² = not applicable).
Secondary outcomes
2.4.2 Treatment adherence
There was no evidence of an effect for the DBT prolonged‐exposure protocol on the proportion of participants who completed the full one‐year course of treatment (10/17 versus 5/9; OR 1.14, 95% CI 0.22 to 5.84; N = 26; k = 1; I² = not applicable). According to the trial authors, however, "...one therapist...was not adherent to DBT and had a 100% dropout rate" (Harned 2014, p.12). Excluding the four participants treated by this therapist did not, however, materially affect this result.
2.4.3 Depression
There was no evidence of an effect for the DBT prolonged‐exposure protocol for depression scores at either the post‐intervention (mean 11.80, SD 8.00, n = 12 versus mean 15.50, SD 6.50, n = 6; MD ‐3.70, 95% CI ‐10.59 to 3.19; N = 18; k = 1; I² = not applicable) or six‐month follow‐up (mean 12.50, SD 8.20, n = 12 versus mean 16.80, SD 3.40, n = 6; MD ‐4.30, 95% CI ‐9.68 to 1.08; N = 18; k = 1; I² = not applicable) assessments.
2.4.4 Hopelessness
No data available.
2.4.5 General functioning
No data available.
2.4.6 Social functioning
No data available.
2.4.7 Suicidal ideation
No data available.
2.4.8 Suicide
There was no evidence of an effect for the DBT prolonged‐exposure protocol on death by suicide by the follow‐up assessment in this trial (0/17 versus 1/9; OR 0.16, 95% CI 0.01 to 4.41, N = 26; k = 1; I² = not applicable).
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 3: Mentalisation‐based therapy (MBT) versus TAU or another comparator
A single trial investigated the effectiveness of mentalisation‐based therapy (MBT) in adults (mean age: 31.1 ± 7.7 years; 79.9% female) diagnosed with BPD referred to a specialist personality disorder treatment service following a suicide attempt or episode of life‐threatening SH (Bateman 2009, N = 134).
Primary outcome
3.1 Repetition of SH
MBT may reduce repetition of SH by the conclusion of the 18‐month treatment period based on data obtained by correspondence (18/71 versus 31/63; OR 0.35, 95% CI 0.17 to 0.73; N = 134; k = 1; I² = not applicable). According to GRADE criteria, we judged the evidence to be of high certainty.
There was also evidence of an effect for MBT on frequency of SH episodes by the post‐intervention assessment according to data obtained by correspondence (mean 0.38, SD 0.38, n = 71 versus mean 1.66, SD 2.87, n = 63; MD ‐1.28, 95% CI ‐2.01 to ‐0.55; N = 134; k = 1; I² = not applicable).
Secondary outcomes
3.2 Treatment adherence
There was no evidence of an effect for MBT on the proportion of participants who completed the full course of treatment (52/71 versus 47/63; OR 0.93, 95% CI 0.43 to 2.02; N = 134; k = 1; I² = not applicable).
3.3 Depression
MBT was associated with an effect for depression at the post‐intervention assessment (mean 14.80, SD 8.55, n = 71 versus mean 18.68, SD 8.76, n = 63, MD ‐3.88, 95% CI ‐6.82 to ‐0.94; N = 134; k = 1; I² = not applicable).
3.4 Hopelessness
No data available.
3.5 General functioning
There was evidence of an effect for MBT on general functioning at the post‐intervention assessment (mean 60.9, SD 15.8, n = 71 versus mean 53.2, SD 11.7, n = 63; MD 7.70, 95% CI 3.03 to 12.37; N = 134; k = 1; I² = not applicable).
3.6 Social functioning
There was also evidence of an effect for MBT on social functioning at the post‐intervention assessment in this trial (mean 1.76, SD 0.50, n = 71 versus mean 2.17, SD 0.64, n = 63; MD ‐0.41, 95% CI ‐0.61 to ‐0.21; N = 134; k = 1; I² = not applicable).
3.7 Suicidal ideation
No data available.
3.8 Suicide
There were no suicides in either treatment arm by the time of the post‐intervention assessment.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 4: Emotion‐regulation psychotherapy versus TAU or another comparator
Two trials investigated the effectiveness of emotion‐regulation psychotherapy, delivered in a group‐based format, in adult women (weighted mean age: 33.2 ± 11.2 years) diagnosed with BPD referred for outpatient treatment as a result of recurrent SH (Gratz 2006, N = 22; Gratz 2014, N = 61).
Primary outcome
4.1 Repetition of SH
Group‐based emotion‐regulation psychotherapy may reduce repetition of SH by the post‐intervention assessment based on evidence from two trials (OR 0.34, 95% CI 0.13 to 0.88; N = 83; k = 2; I² = 0%; Analysis 3.1). According to GRADE criteria, we judged the evidence to be of moderate certainty.
3.1. Analysis.

Comparison 3: Group‐based emotion‐regulation psychotherapy, Outcome 1: Repetition of SH at post‐intervention
There was no evidence of an effect for group‐based emotion‐regulation psychotherapy on frequency of repetition of SH by the post‐intervention assessment (Analysis 3.2).
3.2. Analysis.

Comparison 3: Group‐based emotion‐regulation psychotherapy, Outcome 2: Frequency of repetition of SH at post‐intervention
Secondary outcomes
4.2 Treatment adherence
No data available.
4.3 Depression
There was evidence of an effect for group‐based emotion‐regulation therapy on depression scores at the post‐intervention assessment (MD ‐9.59, 95% CI ‐13.43 to ‐5.75; N = 83; k = 2; I² = 0%; Analysis 3.3).
3.3. Analysis.

Comparison 3: Group‐based emotion‐regulation psychotherapy, Outcome 3: Depression scores at post‐intervention
4.4 Hopelessness
No data available.
4.5 General functioning
No data available.
4.6 Social functioning
No data available.
4.7 Suicidal ideation
No data available.
4.8 Suicide
There were no suicides in either the intervention or comparator arms in either trial by the post‐intervention assessment.
Subgroup analyses
Randomisation was stratified by repeater status in one trial (Gratz 2014). However, we were unable to obtain disaggregated data from the trial authors despite correspondence.
Sensitivity analyses
Not applicable.
Comparison 5: Psychodynamic psychotherapy versus TAU or another comparator
Two trials investigated psychodynamic psychotherapeutic approaches as compared to TAU in adults (weighted mean age: 31.7 ± 9.8 years; 88.9% female) who either presented to EDs following an episode of SH or who were receiving outpatient treatment for frequent repetition of SH (Andreoli 2015, N = 170; Sahin 2018, N = 71).
For the first trial (Andreoli 2015), there were two separate intervention arms: psychodynamic psychotherapy delivered either by certified psychotherapists or trained nurses. We therefore combined data from these two conditions given their similarity. For the second trial, however, there were two different intervention arms: psychodynamic psychotherapy and DBT (Sahin 2018). We therefore included here only data for the psychodynamic psychotherapy arm.
Primary outcome
5.1 Repetition of SH
There was no evidence of an effect for psychodynamic psychotherapy by the post‐intervention assessment in one of these trials (9/140 versus 4/30; OR 0.45, 95% CI 0.13 to 1.56; N = 170; k = 1; I² = not applicable; Andreoli 2015). According to GRADE criteria, we judged the evidence to be of moderate certainty.
This trial also reported information on time to repetition of SH, finding that "participants who received either form of AP...had increased survival to suicidal crisis relapse compared to patients assigned to TAU (AP‐P vs. TAU log‐rank test: Mantel χ² = 7.63, df = 1, p = .006; AP‐N vs. TAU log‐rank test: Mantel χ² = 9.87, df = 1, p = .002)" (Andreoli 2015, pg.11).
Secondary outcomes
5.2 Treatment adherence
There was evidence of an effect for psychodynamic psychotherapy on the proportion of participants who completed treatment by the post‐intervention assessment in one trial (131/140 versus 19/30; OR 8.43, 95% CI 3.09 to 22.99; N = 170; k = 1; I² = not applicable; Andreoli 2015).
5.3 Depression
There was evidence of an effect for psychodynamic psychotherapy on depression scores at post‐intervention in one trial (mean 9.90, SD 5.70, n = 140 versus mean 13.40, SD 6.40, n = 30; MD ‐3.50, 95% CI ‐5.98 to ‐1.02; N = 170; k = 1; I² = not applicable; Andreoli 2015).
5.4 Hopelessness
No data available.
5.5 General functioning
There was also evidence of an effect for psychodynamic psychotherapy on general functioning scores by the post‐intervention assessment in one trial (mean 62.90, SD 6.20, n = 140 versus mean 57.6, SD 7.60, n = 30; MD 5.30, 95% CI 2.39 to 8.21; N = 170; k = 1; I² = not applicable; Andreoli 2015).
5.6 Social functioning
No data available.
5.7 Suicidal ideation
One trial assessed suicidal ideation as the frequency of episodes necessitating additional intensive psychiatric care (Andreoli 2015). There was evidence of an effect for this intervention on frequency of episodes of suicidal ideation scores at post‐intervention in this trial (mean 0.30, SD 0.60, n = 140 versus mean 1.00, SD 1.10, n = 30; MD ‐0.70, 95% CI ‐1.11 to ‐0.29; N = 170; k = 1; I² = not applicable; Andreoli 2015).
5.8 Suicide
One participant died by suicide in the TAU arm in one trial by the post‐intervention assessment (0/140 versus 1/30; OR 0.07, 95% CI 0.00 to 1.76; N = 170; k = 1; I² = not applicable; Andreoli 2015).
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 6: Case management versus TAU or another comparator
Five trials investigated the provision of case management for the prevention of SH compared either to TAU (Clarke 2002, N = 467; Hvid 2011, N = 133; Van Heeringen 1995, N = 516) or enhanced usual care (EUC; Kawanishi 2014, N = 914; Morthorst 2012, N = 243) in adults (weighted mean age 37.9 ± 13.7 years; 56.2% female) admitted to hospital following an episode of SH. Although the intervention in three of these trials included aspects of PST, this was not the primary or only element of the case management strategy (Hvid 2011; Kawanishi 2014; Morthorst 2012). We therefore thought these trials were sufficiently similar to the others to justify pooling within a meta‐analysis.
Primary outcome
6.1 Repetition of SH
There was no evidence of an effect for case management on repetition of SH by the post‐intervention assessment in four of these trials, nor was there any evidence of a difference by comparator (i.e. TAU versus EUC) (OR 0.78, 95% CI 0.47 to 1.30; participants = 1608; studies = 4; I2 = 54%; Analysis 4.1). Supplementing hospital‐recorded episodes of SH with self‐reported data for Morthorst 2012 did not materially affect this result. Multiple readmissions for SH were, however, significantly more common in the case management group than in the TAU group in one trial (9/220 versus 2/247; OR 5.23, 95% CI 1.12 to 24.45; N = 467; k = 1; I² = not applicable; Clarke 2002). According to GRADE criteria, we judged the evidence to be of low certainty.
4.1. Analysis.

Comparison 4: Case management, Outcome 1: Repetition of SH at post‐intervention
There was also no evidence of an effect for case management as compared with TAU on repetition of SH by the 12‐month follow‐up assessment in one further trial (21/196 versus 34/195; OR 0.57, 95% CI 0.32 to 1.02; N = 391; k = 1; I2 = not applicable; Van Heeringen 1995).
Two trials provided information on time to SH repetition. In one, trial authors reported that "[t]he log‐rank test shows a significant difference in favour of fewer events in the intervention arm, log‐rank test 4.16 (P = 0.0414)" (Hvid 2011, pg.295). However, in the second, trial authors reported "the survival curve for the assertive case management group was not significantly different from that for the control group (log‐rank P = 0.258, Wilcoxon P = 0·103)" Kawanishi 2014, pg.197).
Secondary outcomes
6.2 Treatment adherence
The authors of one trial reported that "11 participants in the assertive case management group did not receive the intervention" (Kawanishi 2014, pg.197). However, as corresponding numbers for the EUC group were not reported, we were unable to analyse the effect of assertive case management on treatment adherence for this trial.
Case management was associated with an effect on the proportion of participants who completed treatment as compared with TAU by the 12‐month assessment in one trial (129/252 versus 102/256; OR 1.58, 95% CI 1.11 to 2.25; N = 508; k = 1; I2 = not applicable; Van Heeringen 1995).
6.3 Depression
No data available.
6.4 Hopelessness
Although the BHS was administered to participants in one trial (Kawanishi 2014), no data on this outcome was reported. Correspondence with trial authors for the previous version of this review indicated they were analysing these data to present in a future report. However, data on this outcome has not been reported in any of the secondary publications of this trial identified by this update of the review.
6.5 General functioning
No data available.
6.6 Social functioning
No data available.
6.7 Suicidal ideation
No data available.
6.8 Suicide
There was no evidence of an effect for case management on suicide by the post‐intervention assessment, nor was there any evidence of a significant difference by comparator for this outcome (Analysis 4.2). There was also no evidence of an effect for case management on suicide by the 12‐month follow‐up assessment in one further trial (6/196 versus 7/195; OR 0.85, 95% CI 0.28 to 2.57; N = 391; k = 1; I² = not applicable; Van Heeringen 1995).
4.2. Analysis.

Comparison 4: Case management, Outcome 2: Suicide deaths at post‐intervention
Subgroup analyses
One trial stratified randomisation by sex (Hvid 2011). Although there was no evidence of an effect in males in this trial (4/20 versus 4/18; OR 0.88, 95% CI 0.18 to 4.17; N = 38; k = 1; I² = not applicable), case management was associated with an effect on repetition of SH in females (2/49 versus 10/46; OR 0.15, 95% CI 0.03 to 0.74; N = 95; k = 1; I² = not applicable).
A second trial stratified randomisation by repeater status (Morthorst 2012). However, we were unable to obtain disaggregated data from the trial authors despite correspondence.
Sensitivity analyses
Not applicable.
Comparison 7: Structured general practitioner (GP) follow‐up versus TAU or another comparator
A single trial investigated the effectiveness of structured follow‐up by the participants' general practitioner (GP) compared with TAU over a six‐month period in adults (mean age: 38.2 years, SD not reported; 74.5% female) admitted to the acute ward of a general hospital following an episode of self‐poisoning (Grimholt 2015, N = 202).
Primary outcome
7.1 Repetition of SH
There was no evidence of an effect for structured GP follow‐up on the proportion repeating SH by the post‐intervention assessment according either to hospital records (8/60 versus 11/83; OR 1.01, 95% CI 0.38 to 2.68; N = 143; k = 1; I² = not applicable) or emergency medical records (9/54 versus 5/69; OR 2.56, 95% CI 0.80 to 8.15; N = 123; k = 1; I² = not applicable). According to GRADE criteria, we judged the evidence to be of low certainty.
The trial authors also reported data on self‐reported repeat episodes of self‐poisoning, self‐cutting, and other methods of SH. Whilst a greater proportion of those assigned to structured GP follow‐up reported repeat episodes of self‐poisoning by the post‐intervention assessment (15/38 versus 9/57; OR 3.48, 95% CI 1.33 to 9.12; N = 95; k = 1; I² = not applicable), there was no evidence of an effect for this intervention on self‐reported episodes of self‐cutting (10/40 versus 9/58; OR 1.81, 95% CI 0.66 to 4.98; N = 98; k = 1; I² = not applicable) or other methods of SH (5/18 versus 9/17; OR 0.34, 95% CI 0.08 to 1.39; N = 35; k = 1; I² = not applicable) by this time point.
Secondary outcomes
7.2 Treatment adherence
There was no evidence of an effect for structured GP follow‐up on the proportion of participants who completed treatment by the post‐intervention assessment in this trial (47/62 versus 64/87; OR 1.13, 95% CI 0.53 to 2.39; N = 149; k = 1; I² = not applicable).
7.3 Depression
Although those allocated to the intervention arm in this trial had slightly higher depression scores by the post‐intervention assessment, there was no evidence of an effect (mean 24.90, SD 10.10, n = 18 versus mean 18.80, SD 12.10, n = 22; MD 6.10, 95% CI ‐0.78 to 12.98; N = 40; k = 1; I² = not applicable); however, there were substantial missing data for this outcome (109/149; 73.2%).
7.4 Hopelessness
There was also no evidence of an effect for structured GP follow‐up on hopelessness scores by the post‐intervention assessment in this trial (mean 11.70; SD 5.60, n = 18 versus mean 8.70, SD 6.70, n = 26; MD 3.00, 95% CI ‐0.65 to 6.65, N = 44; k = 1; I² = not applicable). There were, however, substantial missing data for this outcome (105/149; 70.5%).
7.5 General functioning
No data available.
7.6 Social functioning
No data available.
7.7 Suicidal ideation
There was no evidence of an effect for structured GP follow‐up on suicidal ideation scores by the post‐intervention assessment (mean 19.80, SD 5.30, n = 6 versus mean 17.10, SD 7.20, n = 7; MD 2.70, 95% CI ‐4.11 to 9.51; N = 13; k = 1; I² = not applicable). Again, there were substantial missing data for this outcome (136/149; 91.3%).
7.8 Suicide
There was one suicide death in each trial arm by the post‐intervention assessment. However, there was no evidence of an effect for structured GP follow‐up by the post‐intervention assessment for this outcome (1/62 versus 1/87; OR 1.41, 95% CI 0.09 to 22.98; N = 149; k = 1; I² = not applicable).
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 8: Brief emergency department‐based interventions versus TAU or another comparator
Five trials investigated the effectiveness of a one‐off brief (i.e. between 30 to 57 minutes' duration) intervention conducted in the emergency department (ED) in adults (weighted mean age 35.4 ± 13.5 years; 61.2% female) presenting to EDs following an episode of SH (Armitage 2016, N = 226; O'Connor 2015, N = 30; O'Connor 2017, N = 518; O'Connor 2020, N = 48).
Comparison 8.1: Brief Collaborative Assessment and Management of Suicidality (CAMS)‐based intervention
Two trials investigated the effectiveness of a brief intervention informed by therapeutic principles of both the Collaborative Assessment and Management of Suicidality (CAMS) model, in which a collaborative rapport is developed together with the participant, and the functional analysis model of DBT in which validation and guided discovery is used to understand the participant's motivations for SH, in adults (weighted mean age: 42.1 ± 8.7 years; 43.6% female) presenting to the ED following an episode of SH (O'Connor 2015, N = 30; O'Connor 2020, N = 48).
Primary outcome
8.1.1 Repetition of SH
There was no evidence of an effect for brief CAMS and DBT‐based interventions on repetition of SH by the 12‐month follow‐up assessment in one of these trials (1/13 versus 2/10; OR 0.33, 95% CI 0.03 to 4.32; N = 23; k = 1; I² = not applicable; O'Connor 2020).
One trial also reported data on frequency of repeat SH by the 12‐month follow‐up assessment which could be estimated from the data reported. Once again, however, there was no evidence of an effect for a brief ED‐based intervention on frequency of repeat SH in this trial (mean 0.08, SD 0.28, n = 13 versus mean 1.30, SD 3.47, n = 10; MD ‐1.22, 95% CI ‐3.38 to 0.94; N = 23; k = 1; I² = not applicable; O'Connor 2020).
Secondary outcomes
8.1.2 Treatment adherence
No data available.
8.1.3 Depression
No data available.
8.1.4 Hopelessness
Data on hopelessness were available for both of these trials; however, the trial authors did not report information on SDs or other information to enable imputation of SDs.
By the six‐month follow‐up assessment, authors of one of these trials reported "[s]ignificant improvements across time on Reasons for Living improvements were also observed for the [intervention] group compared to the usual care group..." (O'Connor 2015, pg.431). However, data estimated from graphics presented in the trial report suggested any such difference was likely to be modest (estimated mean ‐138.00, n = 11 versus estimated mean ‐136.50, n = 13).
By the 12‐month follow‐up assessment, authors of the second of these trials reported there were "no statistically significant differences between groups on reported reasons for living...at any time point" (O'Connor 2020, pg.116).
8.1.5 General functioning
No data available.
8.1.6 Social functioning
No data available.
8.1.7 Suicidal ideation
Data on suicidal ideation scores were available for both of these trials; however, the trial authors did not report information on SDs or other information to enable imputation of SDs.
By the six‐month assessment, authors of the first trial reported "[a]lthough a trend was observed for greater improvement of suicidal ideation for the TAU group..." (O'Connor 2015, pg.431), this was not significant. Indeed, data estimated from graphics presented in the trial report suggested that suicidal ideation scores were similar between the intervention and control arms by this time point (estimated mean 7.00, n = 11 versus estimated mean 6.00, n = 13).
For the second trial (O'Connor 2020), data estimated from graphics presented in the trial report indicated there was no meaningful difference in suicidal ideation scores by the 12‐month follow‐up assessment in this trial (estimated mean 5.50, n = 13 versus estimated mean 5.30, n = 10).
8.1.8 Suicide
No data available.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 8.2: Brief guided Integrated Motivational‐Volitional‐focused intervention
Two trials investigated a guided intervention, based on the Integrated Motivational‐Volitional help‐sheet model, in which participants are encouraged to identify situations in which they may be triggered to engage in SH and link these with alternative responses that may help them to avoid SH (Armitage 2016, N = 151; O'Connor 2017, N = 518).
For one of these trials (Armitage 2016), there were two separate intervention arms: a guided implementation‐focused intervention based on the volitional help‐sheet model (Armitage 2016a), and a self‐directed implementation intention‐focused intervention (Armitage 2016b). Given that the model used in Armitage 2016a was based in a large part on O'Connor 2017, and involved authors of this latter trial in the design of the intervention, we grouped these two trials within a single analysis. For a detailed description of the therapeutic content of the two different intervention arms included in this trial, see the Characteristics of included studies section.
Primary outcome
8.2.1 Repetition of SH
There was no evidence of an effect for this intervention on repetition of SH by the six‐month follow‐up assessment in one of these trials (72/259 versus 72/259; OR 1.00, 95% CI 0.68 to 1.47; N = 518; k = 1; I² = not applicable; O'Connor 2017).
One trial reported data on frequency of repeat SH episodes by the six‐month follow‐up assessment; however, there was no evidence of an effect for this intervention in this trial (mean 0.68, SD 2.53, n = 259 versus mean 0.85, SD 2.78, n = 259; MD ‐0.17, 95% CI ‐0.63 to 0.29; N = 518; k = 1; I² = not applicable; O'Connor 2017). For the second of these trials (Armitage 2016a), data on frequency of SH could not be disaggregated from data on frequency of suicidal ideation and therefore could not be included in the review.
There was also no evidence of an effect for this intervention on time to SH repetition in one of these trials (HR 0.80, 95% CI 0.55 to 1.18, N = 518; k = 1; I² = not applicable; O'Connor 2017).
Secondary outcomes
8.2.2 Treatment adherence
Data from one trial indicated that almost all (95.7%) of those assigned to the intervention arm completed the intervention in the hospital. However, as corresponding numbers were not reported for the comparator arm in this trial, we could not calculate treatment effect sizes for this outcome (O'Connor 2017).
8.2.3 Depression
One trial reported data on depression scores by the six‐month follow‐up assessment (Armitage 2016a); however, there was no evidence of an effect for this intervention (mean 16.65, SD 5.92, n = 75 versus mean 17.78, SD 6.51, n = 73; MD ‐1.13, 95% CI ‐3.14 to 0.88; N = 148; k = 1; I² = not applicable).
8.2.4 Hopelessness
No data available.
8.2.5 General functioning
No data available.
8.2.6 Social functioning
No data available.
8.2.7 Suicidal ideation
No data available.
8.2.8 Suicide
There was no evidence of an effect for this intervention on suicide deaths by the six‐month follow‐up in one trial (1/259 versus 2/259; OR 0.50, 95% CI 0.04 to 5.53; N = 518; k = 1; I² = not applicable; O'Connor 2017).
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 8.3: Brief self‐guided Integrated Motivational‐Volitional‐focused intervention
The second intervention arm in Armitage 2016 investigated the effectiveness of a self‐guided intervention, based in the Integrated Motivational‐Volitional help‐sheet model, as compared to TAU in adults (mean age: 29.3 ± 11.9 years; 69.9% female) presenting to the emergency department following an episode of SH (Armitage 2016b, N = 151).
Primary outcome
8.3.1 Repetition of SH
For this trial, data on frequency of SH could not be disaggregated from data on frequency of suicidal ideation and therefore could not be included in the review.
Secondary outcomes
8.3.2 Treatment adherence
No data available.
8.3.3 Depression
No effect for this intervention approach was found for depression scores by the six‐month follow‐up assessment in this trial (mean 16.20, SD 6.56, n = 78 versus mean 17.78, SD 6.51, n = 73; MD ‐1.58, 95% CI ‐3.67 to 0.51; N = 151; k = 1; I² = not applicable; Armitage 2016b).
8.3.4 Hopelessness
No data available.
8.3.5 General functioning
No data available.
8.3.6 Social functioning
No data available.
8.3.7 Suicidal ideation
No data available.
8.3.8 Suicide
No data available.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 8.4: Brief alcohol‐focused intervention
One trial investigated the effectiveness of a brief ED‐based intervention for alcohol misuse on repetition of SH over a six‐month follow‐up period in adults (mean age: 37.2 ± 12.0 years; 50.0% female) who were misusing alcohol and were admitted to the ED following an episode of SH (Crawford 2010, N = 103).
Primary outcome
8.4.1 Repetition of SH
There was no evidence of an effect for brief alcohol‐focused ED‐based interventions on repetition of SH by the six‐month follow‐up assessment in this trial (7/52 versus 11/51; OR 0.57, 95% CI 0.20 to 1.60; k = 1; I² = not applicable; Crawford 2010).
Secondary outcomes
8.4.2 Treatment adherence
The trial authors reported that only around half (47.1%) of those randomised to the intervention arm attended the brief alcohol treatment session (Crawford 2010, pg.1826). However, as corresponding numbers were not available for those allocated to the control arm, who did not receive an invitation to brief alcohol treatment sessions, we could not calculate treatment effect sizes for this outcome.
8.4.3 Depression
No data available.
8.4.4 Hopelessness
No data available.
8.4.5 General functioning
No data available.
8.4.6 Social functioning
No data available.
8.4.7 Suicidal ideation
No data available.
8.4.8 Suicide
Correspondence with trial authors confirmed that no participants died by suicide in either arm over the course of the six‐month follow‐up period. However, the authors warned that, as they were unable to track participants via their National Health Service (NHS) identity numbers, they were unable to confirm numbers of suicides from national mortality data. Thus, there may have been suicide deaths amongst those participants whom the authors were unable to contact by the six‐month follow‐up assessment in this trial.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 9: Remote contact interventions versus TAU or another comparator
A number of trials investigated the effectiveness of a variety of remote contact interventions, including: emergency cards (Evans 1999a; Morgan 1993), coping cards (Wang 2016), general practitioners' (GP) letters (Bennewith 2002), postcards (Beautrais 2010; Carter 2005; Hassanian‐Moghaddam 2011; Kapur 2013), telephone contact (Cedereke 2002; Mousavi 2015; Vaiva 2006), telephone contact combined with emergency cards and letters (Mouaffak 2015; Vaiva 2018), and telephone‐based psychotherapy (Marasinghe 2012; Sreedaran 2020; Wei 2013).
Comparison 9.1: Emergency cards
Two trials investigated the effectiveness of providing an emergency contact card ('green card') providing 24‐hour access to emergency advice from a psychiatrist in addition to TAU in adults (weighted mean age: 32.6 ± 11.7 years; 55.4% female) admitted to general hospitals following an episode of SH, most commonly self‐poisoning (Evans 1999a, N = 827; Morgan 1993, N = 212). Note, repetition of SH data for Evans 1999a was reported in a secondary publication (Evans 2005).
Primary outcome
9.1.1 Repetition of SH
There was no evidence of an effect for emergency cards on repetition of SH by the post‐intervention assessment in these two trials (OR 0.82, 95% CI 0.31 to 2.14; participants = 1039; studies = 2; I2 = 68%; Analysis 5.1). According to GRADE criteria, we judged the evidence to be of low certainty.
5.1. Analysis.

Comparison 5: Remote contact interventions: Emergency cards, Outcome 1: Repetition of SH at post‐intervention
There was also no evidence of an effect for emergency cards by the 12‐month follow‐up assessment in the one trial for which data were available (Analysis 5.2).
5.2. Analysis.

Comparison 5: Remote contact interventions: Emergency cards, Outcome 2: Repetition of SH at 12 months
One trial reported data on frequency of repetition of SH as the proportion of participants who had no episodes at follow‐up, the proportion with a single episode at follow‐up, and the proportion with two or more repeat episodes of SH by the 12‐month follow‐up assessment (Evans 1999a). There was no difference between groups in the number of participants who had none (347/417 versus 351/410; OR 0.83, 95% CI 0.57 to 1.21; N = 827; k = 1; I² = not applicable), one (46/417 versus 32/410; OR 1.46, 95% CI 0.91 to 2.35; N = 827; k = 1; I² = not applicable), or two or more (24/417 versus 27/410; OR 0.87, 95% CI 0.49 to 1.53; N = 827; k = 1; I² = not applicable) further episodes of SH.
One trial also reported information on time to SH repetition. The authors found that whilst "[t]he median time to first repeat among those given a green card was 33 days (range 1‐180); in the control group it was 40 days (range 2‐156). This difference is not significant (log rank test: chi‐square 0.82, P = 0.36" (Evans 1999a, pg.25).
Secondary outcomes
9.1.2 Treatment adherence
No data available.
9.1.3 Depression
No data available.
9.1.4 Hopelessness
No data available.
9.1.5 General functioning
No data available.
9.1.6 Social functioning
No data available.
9.1.7 Suicidal ideation
No data available.
9.1.8 Suicide
Data on suicides were reported in only one trial (Evans 1999a). There was no evidence of an effect for emergency cards on suicide by the post‐intervention assessment in this trial (2/417 versus 1/410; OR 1.97, 95% CI 0.18 to 21.82; N = 827; k = 1; I² = not applicable).
Subgroup analyses
Data on repetition of SH was available by repeater status (i.e. those without a history of multiple episodes of SH versus those with a history of multiple episodes of SH) in one trial (Evans 1999a). There was no evidence of an effect for emergency cards on repetition of SH in those without a history of multiple episodes of SH; however, emergency cards were associated with an increased risk of repetition of SH in those with a history of multiple episodes of SH by the 12‐month follow‐up assessment in this trial (Analysis 5.2).
For those without a history of multiple episodes of SH, there was no difference between groups in the number of participants who had none (203/221 versus 181/206; OR 1.56, 95% CI 0.82 to 2.95; N = 427; k = 1; I² = not applicable), one (13/221 versus 16/206; OR 0.74, 95% CI 0.35 to 1.58; N = 427; k = 1; I² = not applicable), or two or more (5/221 versus 9/206; OR 0.51, 95% CI 0.17 to 1.54; N = 427; k = 1; I² = not applicable) repeat episodes of SH (Evans 1999a).
For those with a history of multiple episodes of SH, however, receipt of an emergency card was associated with a reduction in the number of participants with no further episodes of SH (142/194 versus 167/200; OR 0.54, 95%CI 0.33 to 0.88; N = 394; k = 1; I² = not applicable) coupled with an increase in the number of participants with one repeat episode of SH (33/194 versus 15/200; OR 2.53, 95% CI 1.33 to 4.82; N = 394; k = 1; I² = not applicable). There was no difference between the intervention and comparator groups with respect to the number of participants with or two or more subsequent episodes of SH for those with a history of multiple episodes of SH, however (19/194 versus 18/200; OR 1.10, 95% CI 0.56 to 2.16; N = 394; k = 1; I² = not applicable) (Evans 1999a).
Sensitivity analyses
Not applicable.
Comparison 9.2: Coping cards
A single, small trial investigated the effectiveness of coping cards, in which participants were encouraged to note down alternative activities they could engage in when feeling suicidal, resources they found helpful when seeking help, as well as the numbers of a 24‐hour crisis line and local medical services, in addition to TAU as compared to TAU alone in adults (mean age: 37.9±11.1 years; 73.4% female) referred to a specialist suicide prevention service following a suicide attempt (Wang 2016, N = 64).
Primary outcome
9.2.1 Repetition of SH
There was no evidence of an effect for coping cards on the proportion of participants re‐attempting suicide by the post‐intervention assessment (0/32 versus 5/32; OR 0.08, 95% CI 0.00 to 1.45; N = 64; k = 1; I² = not applicable; Wang 2016). According to GRADE criteria, we judged the evidence to be of moderate certainty.
Regarding time to repetition, whilst numeric data were not provided the authors report "[r]esults indicated that participants in the coping card group had a significantly longer time to re‐attempt than those in the TAU group...[at the] 3‐month" (i.e., post‐intervention) period (Wang 2016, p.112).
Secondary outcomes
9.2.2 Treatment adherence
No data available.
9.2.3 Depression
The authors indicate they measured depression; however, no data on this outcome were reported in the trial report.
9.2.4 Hopelessness
There was no evidence of an effect for coping cards on hopelessness scores at post‐intervention (mean 6.81, SD 2.98, n = 32 versus mean 8.38, SD 3.96, n = 32; MD ‐1.57, 95% CI ‐3.29 to 0.15; N = 64; k = 1; I² = not applicable; Wang 2016).
9.2.5 General functioning
No data available.
9.2.6 Social functioning
No data available.
9.2.7 Suicidal ideation
Suicidal ideation was assessed in this trial; however, an idiosyncratic six‐point scale was used. Data on this outcome were therefore unable to be included in this review.
9.2.8 Suicide
No data available.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 9.3: GP letters
A single cRCT compared the effectiveness of a letter from participants' general practitioners following discharge from hospital offering an appointment and advice compared to TAU over a 12‐month period in adults (mean age: 32.5 ± 13.2 years; 59.0% female) presenting to hospital following an episode of SH (Bennewith 2002, clusters = 98, N = 1932).
As the trial authors were unable to provide values for either the inter‐cluster correlation coefficient or the design effect, and further, there was no similar cluster RCT of this intervention approach from which these values could be approximated, we were unable to statistically account for the effects of clustering. Results presented in this section may therefore overestimate the effectiveness of this intervention.
Primary outcome
9.3.1 Repetition of SH
There was no evidence of an effect for a letter from participants' GPs on repetition of SH by the 12‐month follow‐up assessment in this trial (211/964 versus 189/968; OR 1.15, 95% CI 0.93 to 1.44; N = 1932; k = 1; I² = not applicable).
There was also no evidence of an effect for GP letters on time to SH repetition in this trial (HR, 1.15, 95% CI 0.94 to 1.42; N = 1932; k = 1; I² = not applicable).
Secondary outcomes
9.3.2 Treatment adherence
There was no effect for the number of participants with a least one contact with treatment services by the 12‐month follow‐up assessment (351/599 versus 387/681; OR 1.08, 95% CI 0.86 to 1.34; N = 1280; k = 1; I² = not applicable).
9.3.3 Depression
No data available.
9.3.4 Hopelessness
No data available.
9.3.5 General functioning
No data available.
9.3.6 Social functioning
No data available.
9.3.7 Suicidal ideation
No data available.
9.3.8 Suicide
No data available.
Subgroup analyses
Data on repetition of SH was available by sex and repeater status (i.e. those without a history of multiple episodes of SH versus those with a history of multiple episodes of SH). A post hoc analysis by sex suggested that whilst there was no effect for males (82/383 versus 84/413; OR 1.07, 95% CI 0.76 to 1.50; N = 796; k = 1; I² = not applicable), a GP letter was associated with an effect on repetition of SH for females (30/581 versus 105/555; OR 0.23, 95% CI 0.15 to 0.36; N = 1136; k = 1; I² = not applicable).
The trial authors also reported data on repetition of SH by repeater status at trial entry and concluded that "[t]he odds ratio for the effect of the intervention in patients with a history of self‐harm was 0.57 (0.33 to 0.98), indicating a beneficial effect, and in those with no history was 1.32 (1.02 to 1.70), indicating a harmful effect" (Bennewith 2002, pg.1258). However, as the raw data on which these subgroup results were based were not reported, we were unable to reproduce these results in this review.
Sensitivity analyses
Not applicable.
Comparison 9.4: Postcards
Four trials assessed the effectiveness of sending postcards on a regular basis over a 12‐month period to adults (weighted mean age: 27.1 ± 8.9 years; 63.0% female) presenting to hospital following an episode of SH (Beautrais 2010, N = 327; Hassanian‐Moghaddam 2011, N = 2113; Kapur 2013, N = 66), including one that used Zelen's design and reported data only for the randomised sample (Carter 2005, N = 772).
Primary outcome
9.4.1 Repetition of SH
Overall, there was no evidence of an effect for postcards on the proportion of patients repeating SH by the post‐intervention assessment (OR 0.87, 95% CI 0.62 to 1.23; participants = 3277; studies = 4; I2 = 51%; Analysis 6.1). According to GRADE criteria, we judged the evidence to be of very low certainty.
6.1. Analysis.

Comparison 6: Remote contact interventions: Postcards, Outcome 1: Repetition of SH at post‐intervention
There was also no evidence of an effect for postcards on repetition of SH by the 12‐month follow‐up assessment in two of these trials (Analysis 6.2).
6.2. Analysis.

Comparison 6: Remote contact interventions: Postcards, Outcome 2: Repetition of SH at 12 months
With respect to frequency of SH, we obtained data on the mean number of repeat SH episodes by correspondence for three of the four trials of postcards (Carter 2005; Hassanian‐Moghaddam 2011; Kapur 2013). Overall, there was no evidence of an effect for postcards on frequency of repeated SH by the post‐intervention assessment in these three trials (Analysis 6.3). For the one remaining trial (Beautrais 2010), the available data indicated a reduced mean number of SH episodes for the intervention group at post‐intervention (0.57 versus 0.78); however, SDs were not presented and insufficient information was reported to enable imputation of SDs. There was similarly no evidence of an effect for postcards either by the 12‐month follow‐up assessment in two trials (Analysis 6.4), or by the 24‐month follow‐up assessment in one trial (Analysis 6.5).
6.3. Analysis.

Comparison 6: Remote contact interventions: Postcards, Outcome 3: Frequency of SH at post‐intervention
6.4. Analysis.

Comparison 6: Remote contact interventions: Postcards, Outcome 4: Frequency of SH at 12 months
6.5. Analysis.

Comparison 6: Remote contact interventions: Postcards, Outcome 5: Frequency of SH at 24 months
Secondary outcomes
9.4.2 Treatment adherence
No data available.
9.4.3 Depression
No data available.
9.4.4 Hopelessness
No data available.
9.4.5 General functioning
No data available.
9.4.6 Social functioning
No data available.
9.4.7 Suicidal ideation
One trial reported information on suicidal ideation at both the post‐intervention assessment and 12‐ to 24‐months' follow‐up (Hassanian‐Moghaddam 2011). There was an effect for postcards on the proportion of participants reporting suicidal ideation at the post‐intervention assessment (302/1043 versus 446/1070; OR 0.57, 95% CI 0.48 to 0.68; N = 2113; k = 1; I² = not applicable). Data reported by the same trial authors in a subsequent follow‐up publication suggested that this effect was maintained by the 12‐ to 24‐month follow‐up assessment (465/997 versus 588/1004; OR 0.62, 95% CI 0.52 to 0.74; N = 2001; k = 1; I² = not applicable; Hassanian‐Moghaddam 2017).
9.4.8 Suicide
There was no evidence of an effect for postcards on suicide by the post‐intervention assessment in these four trials (Analysis 6.6).
6.6. Analysis.

Comparison 6: Remote contact interventions: Postcards, Outcome 6: Suicide deaths at post‐intervention
Data on suicides by the 12‐month follow‐up assessment were reported in one trial; however, no effect was found by this time point either (2/378 versus 5/394; OR 0.41, 95% CI 0.08 to 2.15; N = 772; k = 1; I² = not applicable; Carter 2005).
Subgroup analyses
Randomisation was stratified by sex in one of these trials (Carter 2005); however, there was no evidence of an effect for postcards in either sex at either the post‐intervention (Analysis 6.1) or the the 12‐month follow‐up assessment (Analysis 6.2).
Through correspondence, we were also able to obtain data on frequency of SH repetition by the post‐intervention assessment by both sex and repeater status for three trials (Carter 2005; Hassanian‐Moghaddam 2011; Kapur 2013). There was no evidence of an effect for postcards either by sex (test for subgroup differences: Chi² = 0.07, df = 1, P = 0.79; Analysis 6.3) or by repeater status (i.e. first SH episode versus repeat SH episode) (test for subgroup differences: Chi² = 0.59, df = 1, P = 0.44; Analysis 6.3) in these trials. There was also no evidence of an effect for postcards either by sex (test for subgroup differences: Chi² = 1.25, df = 1, P = 0.26; Analysis 6.4) or by repeater status (test for subgroup differences: Chi² = 0.60, df = 1, P = 0.44; Analysis 6.4) by the 12‐month follow‐up assessment in two trials, or by the 24‐month follow‐up period in one trial (sex: test for subgroup differences: Chi² = 0.57, df = 1, P = 0.45; repeater status: test for subgroup differences: Chi² = 0.35, df = 1, P = 0.55; Analysis 6.5).
Sensitivity analyses
One trial used Zelen's design (Carter 2005). Omitting this trial did not materially affect results for postcards on repetition of SH by the post‐intervention assessment. However, by the 12‐month assessment, excluding this trial caused the result for repetition of SH to become statistically significant (OR 0.67, 95% CI 0.52 to 0.86; N = 2113; k = 1; I² = not applicable). Additionally, excluding this trial suggested a potentially harmful effect of postcards on suicides by the post‐intervention assessment (OR 3.74, 95% CI 1.04 to 13.51; N = 2692; k = 3; I² = 0%).
Four analyses within this comparison were associated with substantial levels of heterogeneity (Analysis 6.4.1, I² = 84%; Analysis 6.4.1, I² = 84%; Analysis 6.4.3, I² = 76%; Analysis 6.4.4, I² = 81%); however, analyses did not indicate any individual study was associated with excessive influence for either of these outcomes.
Comparison 9.5: Telephone contact
Three trials investigated the effectiveness of telephone contact in adults (weighted mean age: 36.5 ± 13.5 years; 72.1% female) presenting to emergency departments following a suicide attempt (Cedereke 2002, N = 216; Mousavi 2015, N = 55; Vaiva 2006, N = 605).
Primary outcome
9.5.1 Repetition of SH
There was no evidence of an effect for telephone contact on repetition of SH by the post‐intervention in one trial (1/29 versus 2/26; OR 0.43, 95% CI 0.04 to 5.02; N = 55; k = 1; I² = not applicable; Mousavi 2015). According to GRADE criteria, we judged the evidence to be of low certainty.
There was also no evidence of an effect for telephone contact on repetition of SH by the 12‐month assessment in a second trial (14/83 versus 15/89; OR 1.00, 95% CI 0.45 to 2.23; N = 172; k = 1; I² = not applicable; Cedereke 2002), or by the 24‐month follow‐up assessment in a third trial (44/293 versus 59/312; OR 0.76, 95% CI 0.49 to 1.16; N = 605; k = 1; I² = not applicable; Vaiva 2006).
With respect to frequency of repetition of SH, there was no evidence of an effect for telephone contact by the post‐intervention assessment in one trial (mean 0.04, SD 0.20, n = 25 versus mean 0.18, SD 0.66, n = 22; MD ‐0.14, 95% CI ‐0.43 to 0.15; N = 47; k = 1; I² = not applicable; Mousavi 2015). The mean number of episodes of SH was similar between arms in both Cedereke 2002 by the 12‐month assessment (0.31 versus 0.30) and in Vaiva 2006 by the 24‐month assessment (0.15 versus 0.19). However, as trial authors provided insufficient information to enable imputation of SDs, we were unable to calculate the mean difference in the number of repeat episodes of SH between arms in these two trials.
Secondary outcomes
9.5.2 Treatment adherence
No data available.
9.5.3 Depression
No data available.
9.5.4 Hopelessness
No data available.
9.5.5 General functioning
Whilst data on general functioning were available for one of these trials by the 12‐month follow‐up assessment (mean 61.4, SD 20.4 versus mean 58.6, 20.2), it was unclear how many of the 163 participants with data on this outcome had been allocated to the intervention and control arms (Cedereke 2002). We were therefore unable to include these data in our review. The trial authors, however, reported that "[a]t 12 months there had been significant improvements within both the intervention and control groups in global functioning (GAF)..." (Cedereke 2002, pg.87).
9.5.6 Social functioning
No data available.
9.5.7 Suicidal ideation
Telephone contact was not associated with an effect on suicidal ideation scores by the 12‐month follow‐up assessment in one trial (mean 5.80, SD 7.80, N = 5 versus mean 4.00, SD 6.20, N = 8; MD 1.80, 95% CI ‐6.27 to 9.87; N = 13; k = 1; I² = not applicable; Cedereke 2002).
One further trial reported information on the proportion of participants reporting suicidal ideation; however, once again telephone contact was not associated with an effect by the post‐intervention assessment in this trial (2/25 versus 1/22; OR 1.83, 95% CI 0.15 to 21.64; N = 47; k = 1; I² = not applicable; Mousavi 2015).
9.5.8 Suicide
There was no evidence of an effect for telephone contact on suicides either by the post‐intervention (0/25 versus 1/22; OR 0.28, 95% CI 0.01 to 7.26; N = 47; k = 1; I² = not applicable; Mousavi 2015), 12‐month (1/107 versus 1/109; OR 1.02, 95% CI 0.06 to 16.50; N = 216; k = 1; Cedereke 2002) or 24‐month (1/293 versus 2/312; OR 0.52, 95% CI 0.05 to 5.89; N = 605; Vaiva 2006) follow‐up assessments.
Subgroup analyses
Whilst one trial stratified randomisation, this trial compared those who engaged in three or fewer suicide attempts over the three years prior to trial entry to those who had engaged in four or more episodes over this time frame, rather than those engaging in a first episode versus a repeat episode (Vaiva 2006). We were therefore unable to include these data in our review.
Sensitivity analyses
Not applicable.
Comparison 9.6: Telephone contact combined with emergency cards and letters
Two relatively large trials assessed the effectiveness of telephone contact combined with emergency cards and letters (for those unable to be contacted via telephone) compared to TAU in adults (weighted mean age: 38.4 ± 13.2 years; 64.5% female) presenting to the emergency department following a suicide attempt (Mouaffak 2015, N = 302; Vaiva 2018, N = 987).
Primary outcome
9.6.1 Repetition of SH
There was no evidence of an effect for telephone contact combined with emergency cards and letters on repetition of SH by the post‐intervention assessment in one of these trials (22/152 versus 21/151; OR 1.05, 95% CI 0.55 to 2.00; N = 303; k = 1; I² = not applicable; Mouaffak 2015). According to GRADE criteria, we judged the evidence to be of moderate certainty.
For the second of these trials, information on SH repetition was combined with that for suicide deaths (Vaiva 2018). Despite correspondence, we were unable to obtain disaggregated data for these outcomes. We were therefore unable to include these data in our analyses.
There was also no evidence of an effect for this intervention on frequency of repeated SH by the post‐intervention assessment in one of these trials (mean 0.20, SD 0.58, n = 152 versus mean 0.23, SD 0.84, n = 150; MD ‐0.03, 95% CI ‐0.19 to 0.13; N = 302; k = 1; I² = not applicable; Mouaffak 2015).
Although neither trial provided numeric data, both reported there was no effect for telephone contact combined with emergency cards and letters on time to SH repetition: "[t]he intervention had no significant impact on...the duration of the period that patients were free of attempts (Vaiva 2018, pg.5), and, there was no "significant differences between the two groups" (Mouaffak 2015, pg.916).
Secondary outcomes
9.6.2 Treatment adherence
No data available.
9.6.3 Depression
No data available.
9.6.4 Hopelessness
No data available.
9.6.5 General functioning
No data available.
9.6.6 Social functioning
No data available.
9.6.7 Suicidal ideation
No data available.
9.6.8 Suicide
There was no evidence of an effect for telephone contact combined with emergency cards and letters by the post‐intervention assessment in one trial (1/152 versus 0/150; OR 2.98, 95% CI 0.12 to 73.74; N = 302; k = 1; I² = not applicable; Mouaffak 2015), or by the 13‐month follow‐up assessment in the second trial (3/493 versus 8/494; OR 0.37, 95% CI 0.10 to 1.41; N = 987; k = 1; I² = not applicable; Vaiva 2018).
Subgroup analyses
Randomisation was stratified by history of SH prior to trial entry in one of these trials (Mouaffak 2015); however, there was no evidence of an effect for telephone contact combined with emergency cards and letters on repetition of SH by the post‐intervention assessment either in those with a history of SH (18/79 versus 17/72; OR 0.95, 95% CI 0.45 to 2.03; N = 151; k = 1; I² = not applicable) or in those without this history at trial entry (4/77 versus 4/74; OR 0.96, 95% CI 0.23 to 3.98; N = 151; k = 1; I² = not applicable).
Sensitivity analyses
Not applicable.
Comparison 9.7: Telephone‐based psychotherapy
Three trials from developing countries (i.e. China, India, and Sri Lanka) assessed the effectiveness of psychotherapy, incorporating principles from CBT‐based psychotherapy, third‐wave techniques, and social support delivered by telephone over either a one‐month (Sreedaran 2020, N = 28), three‐month (Wei 2013, N = 157), or six‐month (Marasinghe 2012, N = 68) period in adults (weighted mean age: 32.6 ± 14.0; 69.6% female) presenting to services following an episode of SH.
As this latter trial used a cross‐over design, we reported only data from the post‐intervention assessment (i.e. prior to cross‐over) in this review. Additionally, for one of these trials (i.e. Wei 2013), there were two intervention arms: CBT‐based psychotherapy and telephone‐based psychotherapy. We therefore included here only data for the telephone contact arm, and have split the comparator arm data following the advice in Higgins 2011.
Primary outcome
9.7.1 Repetition of SH
For one trial, correspondence with trial authors indicated there were "no suicide attempts in both groups in those who did not drop out [at post‐intervention]...We were unable to obtain information from those who dropped out with respect to suicide attempts. We did have one suicide attempt in the [intervention] group, but this was before all interventions were completed and so this was excluded from final analysis" (Sreedaran 2020, personal communication).
For the remaining two trials, there was no evidence of an effect for telephone‐based psychotherapy on repetition of SH by the post‐intervention in two of these trials (OR 0.36, 95% CI 0.01 to 8.94; participants = 185; studies = 2; I2 = 0%; Analysis 7.1). According to GRADE criteria, we judged the evidence to be of low certainty.
7.1. Analysis.

Comparison 7: Remote contact interventions: Telephone‐based psychotherapy, Outcome 1: Repetition of SH at post‐intervention
There was also no evidence of an effect for telephone‐based psychotherapy on repetition of SH by the six‐month (1/41 versus 4/40; OR 0.23, 95% CI 0.02 to 2.11; N = 81; k = 1; I² = not applicable; Wei 2013), or 12‐month follow‐up assessments in one of these trials (1/36 versus 5/27; OR 0.13, 95% CI 0.01 to 1.15; N = 63; k = 1; I² = not applicable; Wei 2013).
Secondary outcomes
9.7.2 Treatment adherence
There was no effect for mobile telephone‐based psychotherapy on the proportion of participants who completed treatment by the post‐intervention assessment in one of these trials (8/13 versus 7/12; OR 1.14, 95% CI 0.23 to 5.67; N = 25; k = 1; I² = not applicable; Sreedaran 2020).
9.7.3 Depression
There was also no evidence of an effect for mobile telephone‐based psychotherapy on depression scores by the post‐intervention assessment in two of these trials (Analysis 7.2), or by the six‐month (mean 6.01, SD 8.87, n = 41 versus mean 5.85, SD 8.16, n = 40; MD 0.16, 95% CI ‐3.55 to 3.87; N = 81; k = 1; I² = not applicable) or 12‐month (mean 5.73, SD 8.71, n = 36 versus mean 5.84, SD 8.23, n = 27; MD ‐0.11, 95% CI ‐4.32 to 4.10; N = 63; k = 1; I² = not applicable) follow‐up assessments in one of these trials (Wei 2013).
7.2. Analysis.

Comparison 7: Remote contact interventions: Telephone‐based psychotherapy, Outcome 2: Depression scores at post‐intervention
9.7.4 Hopelessness
No data available.
9.7.5 General functioning
No data available.
9.7.6 Social functioning
No data available.
9.7.7 Suicidal ideation
There was evidence of an effect for mobile telephone‐based psychotherapy for suicidal ideation scores at the post‐intervention assessment in one trial (mean 3.60, SD 1.60, n = 34 versus mean 7.30, SD 5.50, n = 34; MD ‐3.70, 95% CI ‐5.63 to ‐1.77; N = 68; k = 1; I² = not applicable; Marasinghe 2012).
One trial reported information on the proportion of participants reporting suicidal ideation (Wei 2013); however, there was no evidence of an effect for telephone‐based psychotherapy on the proportion reporting suicidal ideation at either the post‐intervention (37/80 versus 32/77; OR 1.21, 95% CI 0.64 to 2.27; N = 157; k = 1; I² = not applicable), six‐month (26/80 versus 24/77; OR 1.06, 95% CI 0.54 to 2.08; N = 157; k = 1; I² = not applicable), or 12‐month (24/80 versus 25/77; OR 0.89, 95% CI 0.45 to 1.75; N = 157; k = 1; I² = not applicable) follow‐up assessments in this trial. However, it is notable that, for this trial, results were reported on the basis of those randomised despite the fact that a self‐reported measure was used, and high levels of dropouts were observed by the 12‐month follow‐up assessment. As we were unable to confirm these numbers with trial authors, results much be interpreted with caution.
9.7.8 Suicide
Data obtained by correspondence indicated that there was no evidence of an effect for telephone‐based psychotherapy on suicide by the post‐intervention assessment (Analysis 7.3).
7.3. Analysis.

Comparison 7: Remote contact interventions: Telephone‐based psychotherapy, Outcome 3: Suicide deaths at post‐intervention
Subgroup analyses
Telephone‐based psychotherapy was associated with an effect for depression scores at the post‐intervention assessment in males (mean 5.90, SD 2.40, n = 17 versus mean 13.30, SD 6.10, n = 17; MD ‐7.40, 95% CI ‐10.52 to ‐4.28; N = 34; k = 1; I² = not applicable), but not in females (mean 8.10, SD 6.30, n = 17 versus mean 11.60, SD 6.50, n = 17; MD ‐3.50, 95% CI ‐7.80 to 0.80; N = 34; k = 1; I² = not applicable) in one trial (Marasinghe 2012).
However, for suicidal ideation scores, whilst there was no evidence of an effect for telephone‐based psychotherapy at the post‐intervention assessment in males in this trial (mean 3.50, SD 1.80, n = 17 versus mean 6.20, SD 5.50, n = 17; MD ‐2.70, 95% CI ‐5.45 to 0.05; N = 34; k = 1; I² = not applicable), there was, however, an effect for females (mean 3.80, SD 1.40, n = 17 versus mean 8.90, SD 6.20, n = 17; MD ‐5.10, 95% CI ‐8.12 to ‐2.08; N = 34; k = 1; I² = not applicable) (Marasinghe 2012).
Sensitivity analyses
One analysis within this comparison was associated with substantial levels of heterogeneity (Analysis 7.2, I² = 90%); however, analyses did not indicate any individual study was associated with excessive influence for this outcome.
Comparison 10: Provision of information and support versus TAU or another comparator
Two multicentre and multi‐country studies investigated the effectiveness of providing a one‐off hospital‐based information session combined with regular home visits and/or telephone contact in addition to TAU over an 18‐month period in adults (weighted mean age: 26.7 years, SD not reported; 62.6% female) presenting to the emergency department following an episode of SH: the START Study (Amadéo 2015, N = 190) and the SUPRE‐MISS Study (Fleischmann 2008, N = 1699). In one further trial, participants nominated a support person in addition to receiving information and support using the original SUPRE‐MISS model (Naidoo 2014, N = 688).
Primary outcome
10.1 Repetition of SH
There was no evidence of an effect for information and support on repetition of SH by the 18‐month post‐intervention assessment in two trials (OR 1.09, 95% CI 0.79 to 1.50; participants = 1853; studies = 2; I2 = 0%; Analysis 8.1). Whilst a third trial also reported information on repetition of SH by the post‐intervention assessment, there were major discrepancies for this outcome that we were unable to clarify with trial authors (Naidoo 2014). According to GRADE criteria, we judged the evidence to be of very low certainty.
8.1. Analysis.

Comparison 8: Provision of information and support, Outcome 1: Repetition of SH at post‐intervention
As randomisation was conducted locally for each country included in the SUPRE‐MISS study, we were also able to include results for each of the five countries separately. Although there was no difference between groups for the individual sites in Campinas, Brazil (21/71 versus 10/64; OR 2.27, 95% CI 0.97 to 5.28; N = 135; k = 1; I² = not applicable), Colombo, Sri Lanka (3/130 versus 5/121; OR 0.55, 95% CI 0.13 to 2.34; N = 251; k = 1; I² = not applicable), Karaj, Iran (33/303 versus 28/298; OR 1.18, 95% CI 0.69 to 2.00; N = 601; k = 1; I² = not applicable), and Yuncheng, China (1/58 versus 0/38; OR 2.01, 95% CI 0.08 to 50.60; N = 96; k = 1; I² = not applicable), fewer participants in the intervention group had repeated SH by the 18‐month period at the Chennai, India site (8/301 versus 17/260; OR 0.39, 95% CI 0.17 to 0.92; N = 561; k = 1; I² = not applicable).
One secondary publication for the SUPRE‐MISS study also reported data on frequency of SH for one site (i.e. Karaj, Iran) by the six‐month follow‐up assessment (Hassanzadeh 2010). At this site, there was evidence of a increase in frequency of SH repetition in the intervention and support arm relative to the TAU arm (mean 1.63, SD 1.19, n = 319 versus mean 1.17, SD 0.38, n = 310; MD 0.46, 95% CI 0.32 to 0.60; N = 629; k = 1; I² = not applicable).
Secondary outcomes
10.2 Treatment adherence
No data available.
10.3 Depression
Correspondence with trial authors revealed that information on depression was recorded at one site only: Yuncheng, China (Xu 2012). There was evidence of an effect for information and support on depression scores at this site by the post‐intervention assessment (mean 0.64, SD 0.29, n = 57 versus mean 0.52, SD 0.30, n = 54; MD 0.12, 95% CI 0.01 to 0.23; N = 111; k = 1; I² = not applicable).
10.4 Hopelessness
No data available.
10.5 General functioning
No data available.
10.6 Social functioning
No data available.
10.7 Suicidal ideation
No data available.
10.8 Suicide
There was evidence of an effect for information and support on suicide deaths by the 18‐month post‐intervention assessment (OR 0.12, 95% CI 0.03 to 0.44; N = 1889; k = 2; I² = 0%; Analysis 8.2).
8.2. Analysis.

Comparison 8: Provision of information and support, Outcome 2: Suicide deaths at post‐intervention
For the SUPRE‐MISS study, data on suicide deaths were also available for three sites in related publications (i.e. Chennai, India [Vijayakumar 2011], Karaj, Iran [Hassanzadeh 2010], and Yuncheng, China [Xu 2012]). There was evidence of an effect for information and support on suicide deaths by the 18‐month assessment at the Chennai, India site (1/302 versus 9/320; OR 0.11, 95% CI 0.01 to 0.91; N = 622; k = 1; I² = not applicable), but not at the Karaj, Iran (2/319 versus 2/310; OR 0.97, 95% CI 0.14 to 6.94; N = 629; k = 1; I² = not applicable), or the Yuncheng, China (0/57 versus 2/54; OR 0.18, 95% CI 0.01 to 3.89; N = 111; k = 1; I² = not applicable) sites. Notably, the number of completed suicides in the intervention group reported for these three subsamples was greater than the number reported for the overall SUPRE‐MISS cohort in the primary trial (i.e. Fleischmann 2008). We were unable to confirm the correct number of completed suicides in the intervention group with the authors. Including the one additional suicide for the intervention group identified from the three subsample publications with the data reported in the primary study reference, however, did not materially affect the result obtained for the overall SUPRE‐MISS cohort.
Subgroup analyses
For the SUPRE‐MISS study, data on repetition of SH were also available for males and females separately (Fleischmann 2008). Overall, across all five sites in this trial, there was no evidence of an effect on repetition of SH by the post‐intervention assessment in either males (30/349 versus 27/340; OR 1.09, 95% CI 0.63 to 1.88; N = 689; k = 1; I² = not applicable) or females (36/514 versus 33/460; OR 0.97, 95% CI 0.60 to 1.59; N = 974; k = 1; I² = not applicable). Breaking these results down by sex for the individual sites involved in the SUPRE‐MISS study revealed no effect for information and support on repetition of SH by the 18‐month assessment for either sex at any of the five study sites: Campinas, Brazil (males: 4/21 versus 3/25; OR 1.73, 95% CI 0.34 to 8.76; N = 46; k = 1; I² = not applicable; females: 17/50 versus 7/39; OR 2.35, 95% CI 0.86 to 6.44; N = 89; k = 1; I² = not applicable), Chennai, India (males: 5/148 versus 7/125; OR 0.59, 95% CI 0.18 to 1.91; N = 273; ; k = 1; I² = not applicable; females: 3/153 versus 10/153; OR 0.29, 95% CI 0.08 to 1.06; N = 306; k = 1; I² = not applicable), Colombo, Sri Lanka (males: 1/54 versus 3/53; OR 0.31, 95% CI 0.03 to 3.12; N = 107; k = 1; I² = not applicable; females: 2/76 versus 2/68; OR 0.89, 95% CI 0.12 to 6.51; N = 144; k = 1; I² = not applicable), Karaj, Iran (males 19/109 versus 14/118; OR 1.57, 95% CI 0.74 to 3.31; N = 227; k = 1; I² = not applicable; females: 14/194 versus 14/180; OR 0.92, 95% CI 0.43 to 1.99; N = 374; k = 1; I² = not applicable), Yuncheng, China (males: 1/17 versus 0/19; OR 3.55, 95% CI 0.14 to 93.01; N = 36; k = 1; I² = not applicable; females 0/41 versus 0/38; OR not estimable, 95% CI not estimable; N = 79; k = 1; I² = not applicable).
For the START study, data on repetition of SH were reported separately for those with a history of SH prior to trial entry; however, there was no evidence of an effect for information and support on repetition of SH by the post‐intervention assessment in this group (7/14 versus 9/17; OR 0.89, 95% CI 0.22 to 3.66; N = 31; k = 1; I² = not applicable; Amadéo 2015).
Sensitivity analyses
Not applicable.
Comparison 11: Other multimodal interventions versus TAU or another comparator
Three Zelen RCTs investigated the effectiveness of a package of interventions, including CBT‐based psychotherapy, remote contact interventions (e.g. telephone contact, letters, and/or postcards), and GP vouchers in adults (weighted mean age: 35.5 ± 12.5; 54.7% female) admitted to emergency departments following an episode of SH (Gysin‐Maillart 2016, N = 120; Hatcher 2015, N = 1474; Hatcher 2016, N = 365). For one of these trials, the treatment package was culturally adapted for those who identified as of Māori ethnicity (Hatcher 2016).
Primary outcome
11.1 Repetition of SH
There was no evidence of an effect for this package of interventions at post‐intervention in terms of repetition of SH (Analysis 9.1). Using data for the consenting sample (i.e. including only those participants who, following treatment allocation, subsequently consented to participation), rather than all those randomised, for Hatcher 2015 and Hatcher 2016, did not materially affect these results. According to GRADE criteria, we judged the evidence to be of very low certainty.
9.1. Analysis.

Comparison 9: Other multimodal interventions, Outcome 1: Repetition of SH at post‐intervention
One trial reported data on frequency of SH at post‐intervention. There was evidence of an effect for a multimodel package of interventions on frequency of SH in this trial (mean 0.08, SD 0.28, n = 60 versus mean 0.82, SD 1.89, n = 50; MD ‐0.74, 95% CI ‐1.27 to ‐0.21; N = 110; k = 1; I² = not applicable; Gysin‐Maillart 2016).
With regard to time to SH repetition, there was no evidence of a significant treatment effect for this package of interventions in two trials (Analysis 9.2). Information on time to first SH presentation was also reported in Hatcher 2015; however, "...there was no significant difference between the two groups in time to first re‐presentation (log‐rank test P = 0.6564)" (Hatcher 2015, pg.232). As hazard ratios (HRs) and their accompanying 95% CIs were not reported in this trial, we were unable to include this result in our review.
9.2. Analysis.

Comparison 9: Other multimodal interventions, Outcome 2: Time to SH repetition
Secondary outcomes
11.2 Treatment adherence
No data available.
11.3 Depression
There was no effect for this package of interventions on depression scores at the post‐intervention assessment (Analysis 9.3).
9.3. Analysis.

Comparison 9: Other multimodal interventions, Outcome 3: Depression scores at post‐intervention
11.4 Hopelessness
There was also no apparent effect for this package of interventions on hopelessness scores at the post‐intervention assessment (Analysis 9.4).
9.4. Analysis.

Comparison 9: Other multimodal interventions, Outcome 4: Hopelessness scores at post‐intervention
However, the trial authors for one of these trials noted that "whilst there was a greater change in hopelessness scores at...12 months [i.e. the post‐intervention assessment] in the intervention group, the control group had a significantly lower baseline score [;]...because of the significant differences in baseline scores and missing follow up data we...used a mixed linear model to estimate the differences in scores at [the post‐intervention assessment]". Using this model, the trial authors found "there was a decrease in [h]opelessness scores in the treatment group compared to the usual care group but this was statistically non‐significant" (Hatcher 2016, pg.889).
11.5 General functioning
No data available.
11.6 Social functioning
No data available.
11.7 Suicidal ideation
One trial reported information on suicidal ideation scores (Gysin‐Maillart 2016); however, there was no evidence of an effect for this package of interventions on suicidal ideation scores by the post‐intervention assessment in this trial (mean 4.80, SD 7.88, n = 35 versus mean 4.62, SD 6.48, n = 34; MD 0.18, 95% CI ‐3.22 to 3.58; N = 69; k = 1; I² = not applicable).
11.8 Suicide
There was no effect for this intervention package on suicides by the post‐intervention assessment in any trial (Analysis 9.5). For one of these trials (i.e. Hatcher 2015), one death in the intervention arm and one in the control arm were due to uncertain causes and had yet to be investigated by the Coroner. However, assuming these deaths to be attributable to suicide did not materially affect this result.
9.5. Analysis.

Comparison 9: Other multimodal interventions, Outcome 5: Suicide deaths at post‐intervention
Subgroup analyses
Randomisation was stratified by history of SH ( i.e. first SH episode versus repeat SH episode) in two of these trials (Hatcher 2015; Hatcher 2016); however, there was no difference in repetition of SH at post‐intervention in either trial for either those without a history of multiple episodes of SH prior to the index episode (i.e. first SH episode) or for those with a history of multiple episodes of SH (i.e. repeat SH episode) (Analysis 9.1).
Sensitivity analyses
As all trials included in this comparison used Zelen's design, we were unable to undertake sensitivity analyses to investigate the impact use of this design may have had on the results observed.
Two analyses within this comparison were associated with substantial levels of heterogeneity (Analysis 9.1.1, I² = 81%; Analysis 9.2, I² = 89%); however, analyses did not indicate any individual study was associated with excessive influence for any of these outcomes.
Comparison 12: Other mixed interventions versus TAU or another comparator
A number of single trials investigated the effectiveness of other mixed types of interventions compared with TAU or another comparator, including: continuity of care by the same therapist (Torhorst 1987), interpersonal problem‐solving therapy (McLeavey 1994), behaviour therapy (Liberman 1981), intensive in‐ and out‐patient treatment (Van der Sande 1997), general hospital admission (Waterhouse 1990), intensive outpatient treatment (Allard 1992; Welu 1977), home‐based psychotherapy and telephone contact (Hawton 1981), and long‐term therapy (Torhorst 1988).
Comparison 12.1: Continuity of care by the same therapist
One trial investigated the effectiveness of continuing aftercare with the same therapist (defined as continued therapeutic contact with the original hospital therapist in an outpatient setting) versus changing to a different therapist (defined as receiving therapy in a specialised suicide prevention centre which involved changing both therapist and institution) over a 12‐month follow‐up period in adults (mean ± SD age not reported; 69.5% female) admitted to hospital following an episode of self‐poisoning (Torhorst 1987, N = 141).
Primary outcome
12.1.1 Repetition of SH
There was no evidence of an effect for this intervention on repetition of SH by the 12‐month follow‐up assessment in this trial (3/70 versus 9/66; OR 0.28, 95% CI 0.07 to 1.10; N = 136; k = 1; I² = not applicable; Torhorst 1987).
Secondary outcomes
12.1.2 Treatment adherence
There was evidence of an effect for this intervention on the proportion of participants who completed treatment compared to alternative psychotherapy (49/68 versus 36/73; OR 2.65, 95% CI 1.32 to 5.34; N = 141; k = 1; I² = not applicable; Torhorst 1987).
12.1.3 Depression
Depression scores did not differ between groups at the 12‐month follow‐up assessment in this trial (mean 6.20, SD 6.90, n = 65 versus mean 7.60, SD 9.20, n = 62; MD ‐1.40, 95% CI ‐4.24 to 1.44; N = 127; k = 1; I² = not applicable; Torhorst 1987).
12.1.4 Hopelessness
No data available.
12.1.5 General functioning
No data available.
12.1.6 Social functioning
No data available.
12.1.7 Suicidal ideation
No data available.
12.1.8 Suicide
There was no evidence of an effect for this intervention on the number of participants who died by suicide by the 12‐month follow‐up period (2/70 versus 3/66; OR 0.62, 95% CI 0.10 to 3.82; N = 136; k = 1; I² = not applicable; Torhorst 1987).
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 12.2: Interpersonal problem‐solving therapy
One small trial compared the effectiveness of interpersonal problem‐solving skills training (IPSST) with alternative psychotherapy (i.e. brief problem‐oriented therapy) in adults (mean age: 23.9 ± 7.2 years; 74.3% female) admitted to accident and emergency facilities following an episode of self‐poisoning (McLeavey 1994, N = 39).
Primary outcome
12.2.1 Repetition of SH
There was no evidence of an effect for repetition of SH, defined as a 'self‐poisoning act', by the 12‐month follow‐up period (2/17 versus 4/16; OR 0.40, 95% CI 0.06 to 2.57; N = 33; k = 1; I² = not applicable) in this trial.
Secondary outcomes
12.2.2 Treatment adherence
There was no evidence of an effect on the proportion of participants who completed the full course of treatment in this trial (2/19 versus 3/20; OR = 0.67, 95% CI 0.10 to 4.51; N = 39; k = 1; I² = not applicable).
There was, however, evidence of an effect for interpersonal problem‐solving therapy in terms of the number of treatment sessions attended (mean 5.30, SD 0.48, n = 17 versus mean 4.20, SD 1.32, n = 16; MD 1.10, 95% CI 0.41 to 1.79; N = 33; k = 1; I² = not applicable).
12.2.3 Depression
No data available.
12.2.4 Hopelessness
There was no evidence of an effect for hopelessness by the six‐month follow‐up assessment in this trial (mean 6.12, SD 4.61, n = 19 versus mean 4.35, SD 4.39, n = 20; MD 1.77, 95% CI ‐1.06 to 4.60; N = 39; k = 1; I² = not applicable).
12.2.5 General functioning
No data available.
12.2.6 Social functioning
No data available.
12.2.7 Suicidal ideation
No data available.
12.2.8 Suicide
There were no suicide deaths in either the intervention or comparator arm by the 12‐month follow‐up period.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 12.3: Behaviour therapy
One small trial compared the effectiveness of behaviour therapy versus alternative psychotherapy (i.e. insight‐oriented therapy) in adults (mean age: 29.7 ± 8.8 years; 66.6% female) referred for inpatient treatment following a suicide attempt (Liberman 1981, N = 24).
Primary outcome
12.3.1 Repetition of SH
There was no evidence of an effect with regards to the proportion of participants repeating SH by the 24‐month follow‐up period (2/12 versus 3/12; OR 0.60, 95% CI 0.08 to 4.45; N = 24; k = 1; I² = not applicable).
Secondary outcomes
12.3.2 Treatment adherence
No data available.
12.3.3 Depression
Depression was measured using both the BDI and ZSRDS in one trial. There was evidence of an effect for behaviour therapy at the post‐intervention assessment according to both measures (BDI: mean 4.00, SD 4.00, n = 12 versus mean 14.00, SD 12.00, n = 12; MD ‐10.00, 95% CI ‐17.16 to ‐2.84; N = 24; k = 1; I² = not applicable; ZSRDS: mean 32.00, SD 8.00, n = 12 versus mean 43.00, SD 14.00, n = 12; MD ‐11.00, 95% CI ‐20.12 to ‐1.88; N = 24; k = 1; I² = not applicable).
By the six‐month follow‐up assessment, although there was no effect for behaviour therapy on depression according to the ZSRDS (mean 34.00, SD 8.00, n = 12 versus mean 41.00, SD 13.00, n = 12; MD ‐7.00, 95% CI ‐15.64 to 1.64; N = 24; k = 1; I² = not applicable), BDI scores did show an effect (mean 4.00, SD 6.00, n = 12 versus mean 13.00, SD 11.00, n = 12; MD ‐9.00, 95% CI ‐16.09 to ‐1.91; N = 24; k = 1; I² = not applicable).
12.3.4 Hopelessness
No data available.
12.3.5 General functioning
No data available.
12.3.6 Social functioning
No data available.
12.3.7 Suicidal ideation
There was no evidence of an effect for behaviour therapy on the proportion of participants reporting suicidal ideation by the 24‐month follow‐up assessment (5/12 versus 9/12; OR 0.24, 95% CI 0.04 to 1.36; N = 24; k = 1; I² = not applicable).
12.3.8 Suicide
No data available.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 12.4: Intensive in‐ and outpatient treatment
One trial compared the effectiveness of brief psychiatric inpatient admission followed by regular outpatient appointments and 24‐hour access to the psychiatric unit with TAU over a 12‐month follow‐up period in adults (mean age: 36.3 ± 15.1 years; 57.7% female) admitted to a general hospital following a suicide attempt (Van der Sande 1997, N = 274).
Primary outcome
12.4.1 Repetition of SH
There was no evidence of an effect for intensive in‐ and outpatient treatment on repetition of SH by the 12‐month follow‐up period (24/140 versus 20/134; OR 1.18, 95% CI 0.62 to 2.25; N = 274; k = 1; I² = not applicable).
There was no evidence of an effect for intensive in‐ and outpatient treatment on frequency of repetition of SH (mean 0.23, SD 0.57, n = 140 versus mean 0.23, SD 0.81, n = 134; MD 0.00, 95% CI ‐0.17 to 0.17, N = 274; k = 1; I² = not applicable).
There was also no evidence of an effect for intensive in‐ and outpatient treatment on time to SH repetition in this trial (HR 1.24, 95% CI 0.68 to 2.27; N = 274; k = 1; I² = not applicable).
Secondary outcomes
12.4.2 Treatment adherence
There was no effect for intensive in‐ and outpatient treatment in the total number of treatment sessions attended (mean 14.30, SD 24.20, n = 140 versus mean 11.40, SD 27.70, n = 134; MD 2.90, 95% CI ‐3.27 to 9.07; N = 274; k = 1; I² = not applicable).
12.4.3 Depression
There was also no effect for intensive in‐ and outpatient treatment on depression scores by the 12‐month follow‐up assessment (mean 30.80, SD 15.90, n = 94 versus mean 35.80, SD 16.20, n = 50; MD ‐5.00, 95% CI ‐10.52 to 0.52; N = 144; k = 1; I² = not applicable).
12.4.4 Hopelessness
There was no effect for intensive in‐ and outpatient treatment on hopelessness scores by the 12‐month follow‐up assessment in this trial (mean 6.10, SD 5.00, n = 94 versus mean 7.50, SD 5.90, n = 50; MD ‐1.40, 95% CI ‐3.32 to 0.52; N = 144; k = 1; I² = not applicable).
12.4.5 General functioning
No data available.
12.4.6 Social functioning
No data available.
12.4.7 Suicidal ideation
No data available.
12.4.8 Suicide
There was also no evidence of an effect for suicide by the 12‐month follow‐up assessment in this trial (1/140 versus 2/134; OR 0.47, 95% CI 0.04 to 5.30; N = 274; k = 1; I² = not applicable).
Subgroup analyses
Whilst randomisation was stratified, data disaggregated by sex were not reported.
Sensitivity analyses
Not applicable.
Comparison 12.5: General hospital admission
One trial investigated the effectiveness of admission to a general hospital versus non‐admission over a four‐month follow‐up period in adults (mean age: 30.0 years, SD not reported; 62.3% female) presenting to an emergency room following an episode of self‐poisoning and who had no immediate medical or psychiatric treatment needs (Waterhouse 1990, N = 77). In this trial, admission was described as consisting of little more than admission to an inpatient bed. The trial authors did not attempt to influence referral to psychiatric or other treatment services. The median length of admission for those allocated to the experimental group was 17 hours.
Primary outcome
12.5.1 Repetition of SH
There was no evidence of an effect for hospital admission on repetition of SH at the post‐intervention assessment (2/38 versus 2/39; OR 1.03, 95% CI 0.14 to 7.69; N = 77; k = 1; I² = not applicable). According to the GRADE criteria, we judged the evidence to be of moderate certainty.
There was also no evidence of an effect for general hospital management on repetition of SH by the four‐month follow‐up assessment (3/38 versus 4/39; OR 0.75, 95%CI 0.16 to 3.60; N = 77; k = 1; I² = not applicable) in this trial.
Secondary outcomes
12.5.2 Treatment adherence
No data available.
12.5.3 Depression
No data available.
12.5.4 Hopelessness
The authors reported there was no difference in hopelessness scores at the post‐intervention assessment (mean 10.29, SD 5.68 versus mean 10.21, SD 4.97); however, as they did not provide the numbers of patients in each group, we were unable to calculate the MD and its associated 95% CI. No data on hopelessness scores by the follow‐up assessment were reported.
12.5.5 General functioning
No data available.
12.5.6 Social functioning
There was no evidence of an effect for hospital admission on social functioning by the four‐month assessment in this trial (mean 0.41, SD 0.44, n = 16 versus mean 0.51, SD 0.40, n = 20; MD ‐0.10, 95% CI ‐0.38 to 0.18; N = 36; k = 1; I² = not applicable).
12.5.7 Suicidal ideation
There was no evidence of an effect for hospital admission on suicidal ideation scores by the four‐month follow‐up assessment (mean 0.22, SD 0.85, n = 27 versus mean 0.04, SD 0.20, n = 25; MD 0.18, 95% CI ‐0.15 to 0.51; N = 52; k = 1; I² = not applicable).
12.5.8 Suicide
No data available.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 12.6: Intensive outpatient treatment
Two trials compared the effectiveness of intensive outreach interventions with standard outpatient care in adults (weighted mean age: 29.0 years, SD not reported; 55.3% female) admitted to emergency departments following a suicide attempt (Allard 1992, N = 150; Welu 1977, N = 119). The first compared an intensive intervention, involving psychiatrists and a social worker, a schedule of visits including at least one home visit, therapy provided where needed, reminders (telephone or written), and home visits with treatment by regular personnel in the same hospital over a 12‐month period (Allard 1992). In the second, a specialist, intensive outreach programme in which a community mental health team contacted participants immediately after discharge and arranged home visits and weekly or bi‐weekly contact with therapists alongside routine psychiatric consultation was compared with TAU.
Primary outcome
12.6.1 Repetition of SH
There was no evidence of an effect for intensive outpatient treatment on repetition of SH by either the four‐month (3/62 versus 9/57; OR 0.27, 95% CI 0.07 to 1.06; N = 119; k = 1; I² = not applicable; Welu 1977) or 24‐month follow‐up assessment (22/63 versus 19/63; OR 1.24, 95% CI 0.59 to 2.62; N = 126; k = 1; I² = not applicable; Allard 1992).
In the one trial that included information on frequency of repeated SH by the 24‐month follow‐up assessment, the authors reported that "the experimental subjects did not make fewer attempts than the comparison subjects" (Allard 1992, pg.310).
Secondary outcomes
12.6.2 Treatment adherence
Data on treatment adherence were only available for one of these trials (Allard 1992); however, as insufficient information was reported to enable imputation of missing SDs in this trial, we were unable to calculate the mean difference in the number of treatment sessions attended. Nevertheless, the trial authors reported that "[t]he mean numbers of encounters with psychiatrists were 12.35 versus 1.54 (P < 0.001) in the first year and 2.11 versus 0.64 (P = 0.071) in the second year" (Allard 1992, pg.311).
12.6.3 Depression
No data available.
12.6.4 Hopelessness
No data available.
12.6.5 General functioning
For one of these trials, the authors found "[t]here was no difference...in scores on the...GAS" (Allard 1992, pg.311) by the 24‐month follow‐up period. However, numerical data for this outcome were not reported.
12.6.6 Social functioning
No data available.
12.6.7 Suicidal ideation
No data available.
12.6.8 Suicide
One trial reported data on suicide deaths (Allard 1992). There was no evidence of an effect for the intensive outpatient intervention on suicides by the 24‐month follow‐up assessment in this trial (3/76 versus 1/74; OR 3.00, 95% CI 0.30 to 29.52; N = 150; k = 1; I² = not applicable).
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 12.7: Home‐based psychotherapy and telephone contact
One trial investigated the effectiveness of problem‐oriented counselling delivered in two different ways, namely as a flexibly‐timed home‐based therapy, combined with open access via telephone services to the general psychiatric service, versus treatment in weekly outpatient clinics, in adults (mean age: 25.2 ± 8.2 years; 69.8% female) referred to the psychiatric department of a general hospital following admission for self‐poisoning (irrespective of suicidal intent) (Hawton 1981, N = 96).
Primary outcome
12.7.1 Repetition of SH
There was no evidence of an effect for home‐based psychotherapy and telephone contact on repetition of SH by the 12‐month follow‐up assessment in this trial (5/48 versus 7/48; OR 0.68, 95% CI 0.20 to 2.32; N = 96; k = 1; I² = not applicable).
Secondary outcomes
12.7.2 Treatment adherence
There was, however, evidence of an effect for home‐based psychotherapy and telephone contact on the proportion of participants who completed treatment over the course of the 12‐month follow‐up period (40/48 versus 20/48; OR 7.00, 95% CI 2.70 to 18.13; N = 96; k = 1; I² = not applicable).
12.7.3 Depression
Although this trial included data on depression, the trial authors modified the scale used. We were therefore unable to include data on this outcome in this review.
12.7.4 Hopelessness
No data available.
12.7.5 General functioning
No data available.
12.7.6 Social functioning
Although this trial included data on social functioning, the trial authors modified the scale used. We were therefore unable to include data on this outcome in this review.
12.7.7 Suicidal ideation
Data obtained by correspondence suggested there was no effect for suicidal ideation at either the post‐treatment assessment (Mann‐Whitney U = 984, P = 0.29) or six‐month follow‐up assessment (Mann‐Whitney U = 726, P = 0.14). As only median, rather than mean, scores were available for this outcome, we were unable to reproduce the mean difference in suicidal ideation scores between the experimental and control groups in this review.
12.7.8 Suicide
No data available.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Comparison 12.8: Long‐term therapy
One trial investigated the effectiveness of long‐term (one session per month over 12 months) versus short‐term (one session per week over 12 weeks) outpatient psychotherapy on repetition of SH over a 12‐month follow‐up period in adults (mean age: not reported, SD not reported; 100% female) admitted to hospital following repeated episodes of self‐poisoning (Torhorst 1988, N = 80). The content of therapy was not specified.
Primary outcome
12.8.1 Repetition of SH
There was no evidence of an effect for long‐term therapy on repetition of SH by the post‐intervention assessment in this trial (9/40 versus 9/40; OR 1.00, 95% CI 0.35 to 2.86; N = 80; k = 1; I² = not applicable). According to GRADE criteria, we judged the evidence to be of low certainty.
Secondary outcomes
12.8.2 Treatment adherence
The trial authors did not provide numerical data on treatment adherence, although they stated, "[a]ttendance at the first session was about equal for both groups (about 60%)" (Torhorst 1988, pg.420). However, they further stated that "participation of the 12‐month (long‐term therapy) group dropped drastically by the second session to under 40%, while the participation of the patients in the 3‐month (intensive short‐term therapy) program remained higher" (Torhorst 1988, pg.420). However, it was unclear whether this difference was statistically significant.
Overall, treatment adherence also appears to have been very low in both groups as the "average number of sessions was 3.9 (out of a possible 12 sessions) in the three‐month group and 2.6 (out of a possible 12 sessions) for the 12 month group" (Torhorst 1988, pg.420). Again, however, it was unclear whether this difference was statistically significant as insufficient information was reported to enable imputation of missing SDs in this trial.
12.8.3 Depression
Although numerical data on depression scores was not reported, means estimated by the review authors from a graph in the original report suggested there was little difference in depression scores between those allocated to long‐term therapy and those allocated to short‐term therapy by the 12‐month follow‐up assessment (estimated means 9.3 versus 6.7). However, insufficient information was reported to enable imputation of missing SDs for this outcome.
The trial authors, however, stated that "self‐evaluated depressivity...improved considerably more for the patients of the three‐month program than for those of the 12‐month program" (Torhorst 1988, pg.421). This improvement was described by the trial authors as statistically significant.
12.8.4 Hopelessness
No data provided.
12.8.5 General functioning
No data provided.
12.8.6 Social functioning
Whilst "[p]atients in the 3‐month group evaluated themselves according to the Social Adjustment Scale (SAS) significantly more positively...than did the patients of the 12‐month group" (Torhorst 1988, pg.421), numerical data for this outcome were not reported.
12.8.7 Suicidal ideation
No data provided.
12.8.8 Suicide
No data provided.
Subgroup analyses
No included trial stratified randomisation by sex or repeater status.
Sensitivity analyses
Not applicable.
Discussion
This review included 76 trials, 21 (27.6%) of which have been completed since the previous version of this review (Hawton 2016). Previously, we commented that the promising results for CBT‐based psychological therapy and DBT warranted further investigation of these approaches to understand which patients benefit from these types of interventions. There were only a few, generally small, trials of most other forms of psychosocial therapy, providing little evidence of beneficial effects; however, these could not be ruled out.
Summary of main results
The trials included in this review investigated the effectiveness of various forms of psychosocial interventions for SH in adults.
CBT‐based psychotherapy
Individual‐based CBT‐based psychotherapy
Whilst 20 trials investigated the effectiveness of individual‐based cognitive‐behavioural therapy (CBT)‐based psychotherapy, only four (20.0%) reported data on the primary outcome of this review (i.e., repetition of SH at post‐intervention). Although there was imprecision in the effect estimate, on the basis of data from four of these trials, individual‐based CBT‐based psychotherapy may reduce repetition of SH as compared to TAU or another comparator by the end of the intervention. At longer follow‐up time points, there was more robust evidence of effect for this intervention. However, there was no apparent effect for CBT‐based psychotherapy on the frequency of SH, or time to SH repetition.
Few trials reported information on secondary outcomes. CBT‐based psychotherapy was associated with a relatively consistent but small beneficial effect on depression, hopelessness, and suicidal ideation scores as compared with TAU or another comparator over time. There was no apparent effect for this intervention on suicide, however.
Group‐based CBT‐based psychotherapy
On the basis of data from a single trial in which CBT‐based psychotherapy was delivered in a group‐based format, there is probably little to no effect of group‐based CBT‐based psychotherapy on repetition of SH as compared to TAU by the end of the intervention. There was also no evidence of effect for this intervention approach at longer follow‐up assessment points.
There was also no apparent effect of this intervention approach on any of the secondary outcome measures assessed by this review.
Dialectical behaviour therapy (DBT)
Standard DBT
On the basis of data from six trials, the evidence remains uncertain as to whether standard DBT has any effect on absolute repetition of SH by the post‐intervention assessment compared to either TAU or alternative psychotherapy in terms of the proportion of participants engaging in repeat SH by the post‐intervention or 12‐month follow‐up assessments. However, standard DBT may be associated with an effect for frequency of repeated SH by the post‐intervention assessment.
Whilst there was an apparent effect for standard DBT on depression and suicidal ideation scores compared with TAU or another comparator at post‐intervention, these effects were generally no longer apparent at longer follow‐up time points; however, few trials investigated these secondary outcomes. There was no apparent effect for standard DBT on suicide.
DBT group‐based skills training
Based on one trial in which two variants of DBT were compared to standard DBT, there is probably little to no effect of DBT group‐based skills training on absolute or frequency of suicide reattempts or NSSI (Linehan 2015a). For this trial, we were unable to obtain data on combined SH from the trial authors despite correspondence. There was also no apparent effect for DBT group‐based skills training only on any of the secondary outcomes investigated in this trial.
DBT individual therapy
There is also probably little to no effect for DBT individual skills training only on absolute repetition or frequency of suicide reattempts or NSSI as compared to standard DBT, based on findings of the single trial which included this comparison (Linehan 2015b). Again, however, we were unable to obtain data on combined SH from the trial authors despite correspondence. There was also no apparent effect for DBT individual skills training only on any of the secondary outcomes investigated in this trial.
DBT prolonged‐exposure protocol
On the basis of data from a single trial, there is probably little to no effect of an experimental form of DBT in which participants were given significantly longer cognitive exposure to stressful events coupled with the standard DBT protocol on repetition of SH (Harned 2014). There was also no apparent effect for the DBT prolonged exposure intervention on frequency of SH repetition, treatment adherence, depression scores, or suicide.
Mentalisation‐based therapy (MBT)
On the basis of data from a single trial, mentalisation‐based therapy (MBT) for adults referred to a specialist personality disorder treatment service reduces both absolute repetition of SH and frequency of SH by the post‐intervention assessment as compared with TAU (Bateman 2009).
There was also an apparent effect for MBT on depression scores, general functioning scores, and social functioning scores by this time point. However, there was no apparent effect for this intervention on treatment adherence. No participants died by suicide in either trial arm by the post‐intervention assessment.
Emotion regulation psychotherapy
On the basis of data from two trials conducted by the same research group, emotion‐regulation psychotherapy for women diagnosed with borderline personality disorder provided in a group‐based setting probably reduces absolute repetition of SH by the post‐intervention assessment (Gratz 2006; Gratz 2014). There was no apparent effect for this intervention on frequency of SH repetition. However, correspondence with authors suggested that this treatment did not require participants to abstain from SH. Instead, participants were encouraged to work on resisting urges to engage in SH and, when SH occurred, to learn responses to it.
There was also evidence of an apparent effect for group‐based emotion regulation psychotherapy on depression scores by the post‐intervention assessment. No participants died by suicide in either trial arm by the post‐intervention assessment.
Psychodynamic psychotherapy
Whilst two trials investigated the effectiveness of psychodynamic psychotherapeutic approaches as compared to TAU (Andreoli 2015; Sahin 2018), we were only able to include data from the first of these trials despite attempts to obtain data for the second trial by correspondence. Therefore, based on data from one trial, there is probably little to no effect of psychodynamic psychotherapy on repetition of SH by the post‐intervention assessment. However, there was an apparent effect of this intervention on time to SH repetition.
There was also evidence of an apparent effect for this intervention on treatment adherence, depression scores, general functioning scores, and frequency of suicidal ideation episodes necessitating additional intensive psychiatric care by the post‐intervention assessment. There was no apparent effect on suicide deaths. However, these results were all based on a single trial.
Case management
Five trials investigated the effectiveness of case management as compared to either TAU (Clarke 2002; Hvid 2011; Van Heeringen 1995) or enhanced usual care (Kawanishi 2014; Morthorst 2012). On the basis of data from four of these trials, case management may have little to no effect on repetition of SH by the post‐intervention assessment. The impact of this intervention over longer term follow‐up is uncertain as only one of these trials investigated outcomes beyond the post‐intervention assessment time point. There were inconsistent findings for case management on time to SH repetition in two trials.
Findings from a single trial indicated that case management may be associated with an effect on the proportion of participants who completed treatment, which was based on attendance for outpatient clinic appointments, the patient sample having been identified before the trial as having failed to attend such appointments (Van Heeringen 1995). However, few studies reported data on other secondary outcomes. For one trial, although data on hopelessness scores at post‐intervention were collected, data on this outcome have not been reported in any secondary publications of this trial to date (Kawanishi 2014), indicating that publication bias may have been present for this outcome. There was no apparent effect for case management on suicide.
Structured general practitioner (GP) follow‐up
Based on results of a single trial of structured follow‐up by the participants' general practitioner (GP) compared with TAU in adults admitted to the acute ward of a general hospital following an episode of self‐poisoning (Grimholt 2015), this intervention may have little to no effect on repetition of SH by the post‐intervention assessment.
There was also no apparent effect for structured GP follow‐up on treatment adherence, depression scores, hopelessness scores, and suicidal ideation scores, although missing data for these secondary outcomes was substantial (i.e. 70.5% to 91.3%). Therefore, the evidence for these secondary outcomes is uncertain. There was also no apparent effect for this intervention on suicide.
Brief emergency department‐based interventions
Five trials investigated one‐off brief interventions delivered in the emergency department. Two were based, in a large part, on the Collaborative Assessment and Management of Suicidality (CAMS) approach (Jobes 2012), two were based on the Integrated Motivational‐Volitional theoretical model of suicidal behaviour (O'Connor 2011), and one focused on addressing alcohol misuse.
Brief Collaborative Assessment and Management of Suicidality (CAMS)‐based intervention
On the basis of data from a single trial, there is likely no effect of a CAMS‐based approach on repetition of SH by the 12‐month follow‐up assessment (O'Connor 2020). There was also no apparent effect for this intervention on frequency of SH repetition by this time point based on data estimated from graphics presented in the report of this trial.
Limited data were available on any of the secondary outcomes assessed in this review. Although trial authors reported that there were improvements in hopelessness and suicidal ideation scores by the six‐month assessment in the original trial of this intervention (O'Connor 2015), this effect was no longer apparent by the 12‐month follow‐up assessment in a subsequent trial of this intervention (O'Connor 2020).
Brief guided Integrated Motivational‐Volitional‐focused intervention
On the basis of data from a single trial, there is likely no effect of the Integrated Motivational‐Volitional model either on the proportion of participants who engaged in a repeat episode of SH, the frequency of SH repetition, or in the proportion dying by suicide, as compared with TAU (O'Connor 2017).
There was some evidence of an effect for this intervention on treatment adherence in this trial, however, there was also no indication that this approach led to a reduction in depression scores in a second trial (Armitage 2016a). There was also no evidence of an apparent effect for this intervention on suicide deaths.
Brief self‐guided Integrated Motivational‐Volitional‐focused intervention
The second intervention arm in Armitage 2016 investigated the effectiveness of a self‐guided version of the Integrated Motivational‐Volitional model as compared to TAU (i.e. Armitage 2016b). However, in this trial, data on repetition of non‐fatal SH could not be disaggregated from data on suicidal ideation, despite correspondence. Therefore, the evidence for these secondary outcomes is uncertain. There was no apparent effect for this intervention approach on depression scores by the post‐intervention assessment, however.
Brief alcohol‐focused intervention
Based on a single trial of a brief intervention for alcohol misuse in SH patients, there is likely no effect of this intervention on repetition of SH by the six‐month follow‐up assessment (Crawford 2010). However, only around half (47.1%) of those randomised to the brief alcohol‐focused intervention attended the treatment session.
No suicide deaths were observed amongst the group of participants for whom information was available at the six‐month follow‐up. However, the trial authors warned that, as they were unable to track participants via their National Health Service (NHS) identity numbers, they were unable to confirm numbers of suicides from national mortality data. Thus, there may have been suicide deaths amongst those participants whom the authors were unable to contact by the six‐month follow‐up assessment in this trial. The original report did, however, identify a non‐significant trend towards reduced alcohol consumption per drinking day in those allocated to the intervention arm.
Remote contact interventions
A number of trials investigated the effectiveness of a variety of remote contact interventions, including: emergency cards (Evans 1999a; Morgan 1993), coping cards (Wang 2016), general practitioners' (GP) letters (Bennewith 2002), postcards (Beautrais 2010; Carter 2005; Hassanian‐Moghaddam 2011; Kapur 2013), telephone contact (Cedereke 2002; Mousavi 2015; Vaiva 2006), telephone contact combined with emergency cards and letters (Mouaffak 2015; Vaiva 2018), and telephone‐based psychotherapy (Marasinghe 2012; Sreedaran 2020; Wei 2013).
Emergency cards
On the basis of data from two trials, emergency cards may have little to no effect on repetition of SH by the post‐intervention assessment (Evans 1999a; Morgan 1993). In the original report for one of these trials, however, a post hoc subgroup analysis indicated that receipt of the emergency card may be associated with an increased risk of repetition of SH in those with a history of multiple episodes of SH prior to the index episode (Evans 1999a).
There was also no apparent effect for this intervention on suicide deaths on the basis of data reported in one of these trials (Evans 1999a). No data on other secondary outcomes were reported in either of these two trials.
Coping cards
A single trial investigated the effectiveness of a coping card intervention, in which participants were encouraged to note down alternative activities they could engage in when feeling suicidal, resources they found helpful when seeking help, as well as the numbers of a 24‐hour crisis line and local medical services (Wang 2016). On the basis of data from this trial, there is probably little to no effect of coping cards on repetition of SH by the post‐intervention assessment. There may be an apparent effect for this intervention on time to SH repetition.
There was no apparent effect of coping cards on hopelessness scores at post‐intervention. However, whilst the authors measured depression and suicidal ideation scores at post‐intervention, we were unable to obtain data on these outcomes despite correspondence. Therefore, the evidence for these secondary outcomes is uncertain.
General practitioner (GP) letters
There is likely no effect of general practitioners (GP) letters sent to participants following their discharge from hospital after SH on repetition of SH by the six‐month follow‐up assessment in a single cluster‐RCT (Bennewith 2002). There was also no apparent effect for this intervention on time to SH repetition. These results were based on a single cluster‐RCT, which may have overestimated the effectiveness of this intervention. No data on any of the secondary outcomes were reported, however.
Postcards
Four trials investigated the effectiveness of postcards sent on a regular basis over a 12‐month period as compared to TAU (Beautrais 2010; Carter 2005; Hassanian‐Moghaddam 2011; Kapur 2013). On the basis of data from these four trials, the evidence remains uncertain as to whether postcards have any effect on repetition of SH by the post‐intervention assessment. The single largest trial of this intervention, however, did find fewer participants repeating SH in the experimental group (Hassanian‐Moghaddam 2011). This result is notable because the comparator used in this trial would have consisted of little more than discharge because of the paucity of psychiatric services in Iran as compared to Australia, New Zealand, and the UK, where these trials were conducted and which have well‐developed services. This raises the possibility that this type of intervention may be more effective in such settings. Additionally, the postcards used in this trial included religious and philosophical messages in addition to providing general support, which may also explain their apparent efficacy in reducing SH and suicidal behaviour in this setting.
There was no apparent effect of postcards on frequency of SH repetition by this time point. It should be noted that the positive effect on frequency of repetition of SH as reported in one of these trials was, according to the trial's author, largely accounted for by difference in repetition in a small subsample (fewer than 3% of the total sample) of women with a history of three or more episodes of SH prior to trial entry (Carter 2005). There was also no apparent effect of this intervention on suicide deaths.
Telephone contact
On the basis of data from one trial at each time point, telephone contact may have little to no effect on repetition of SH by either the post‐intervention (Mousavi 2015), 12‐month (Cedereke 2002), or 24‐month (Vaiva 2006) follow‐up assessments. There was also no evidence of an effect for this intervention on frequency of SH repetition. There was also no apparent effect for telephone contact on suicide, or on any of the other secondary outcomes.
Telephone contact combined with emergency cards and letters
Two trials investigated the effect of combining telephone contact with emergency cards and letters for those unable to be contacted by telephone (Mouaffak 2015; Vaiva 2006). On the basis of data from the first of these trials, telephone contact combined with emergency cards and letters probably has little to no effect on repetition of SH by the post‐intervention assessment. However, data from the second trial of this intervention approach was excluded as information on non‐fatal SH repetition was combined with that for suicide deaths and we were unable to obtain disaggregated data from the trial authors in time for publication. There was also no apparent effect for this intervention on frequency of SH repetition, time to SH repetition, or on suicide. Neither trial investigated other secondary outcomes, including depression, general or social functioning, or suicidal ideation.
Telephone‐based psychotherapy
Three trials investigated the effectiveness of psychotherapy delivered via telephone (Marasinghe 2012; Sreedaran 2020; Wei 2013). In all three, the intervention approach incorporated principles of CBT‐based psychotherapy, third‐wave techniques, and social support. On the basis of data from two of these trials, telephone‐based psychotherapy may have little to no effect on repetition of SH by the post‐intervention assessment, or by the six‐ or 12‐month follow‐up assessments based on results in one of these trials. There was no apparent effect for telephone‐based psychotherapy on treatment adherence, depression, suicidal ideation, or suicide.
Provision of information and support
On the basis of data from two multicentre and multi‐country trials, one of the START model (Amadéo 2015) and a second of the SUPRE‐MISS model (Fleischmann 2008), in which participants received a hospital‐based information service combined with regular home support, telephone support or both, the evidence remains uncertain as to whether this intervention has any effect on repetition of SH by the post‐intervention assessment. We had to exclude one further trial of this approach from our analyses as there were major discrepancies in the data reported which we were unable to clarify with the trial authors despite correspondence (Naidoo 2014).
There was an apparent effect for this intervention approach on suicide deaths. However, we have noted that there is a discrepancy between findings for the overall cohort for one of these trials (i.e. Fleischmann 2008) and those reported for the individual sites (i.e. Hassanzadeh 2010; Vijayakumar 2011; Xu 2012), in that the number of suicides reported for the overall cohort for the intervention arm was fewer than that reported in the three local site reports (i.e. two versus three respectively). Data on secondary outcomes were only reported for the individual trial sites, rather than for the overall cohort for these trials.
Other multimodal interventions
Three Zelen RCTs investigated the effectiveness of a package of interventions, including CBT‐based psychotherapy, remote contact interventions (e.g. telephone contact, letters, and/or postcards), and GP vouchers in adults admitted to emergency departments following an episode of SH (Gysin‐Maillart 2016; Hatcher 2015; Hatcher 2016). For one of these trials, the treatment package was culturally adapted for those who identified as being of Māori ethnicity (Hatcher 2016). The evidence remains uncertain as to whether this package of interventions has any effect on repetition of SH by the post‐intervention assessment, or on time to SH repetition. There was an apparent effect on frequency of SH repetition in one of these trials (Gysin‐Maillart 2016).
There was no evidence of an apparent effect for this package of interventions on depression, hopelessness, or suicidal ideation scores by the post‐intervention assessment. There was also no evidence of an apparent effect for this package of interventions on suicide by the post‐intervention assessment.
Other mixed interventions
Continuity of care by the same therapist
Based on a single trial, there is likely no effect of continuity of care by the same therapist compared to receiving therapeutic contact from a different therapist on repetition of SH by the 12‐month assessment (Torhorst 1987). There was an apparent effect for this intervention on treatment adherence, but no such effect on either depression scores or suicide.
Interpersonal problem‐solving therapy
Based on a single trial, there is likely no effect of interpersonal problem‐solving skills training (IPSST) compared to alternative psychotherapy (i.e. brief problem‐oriented psychotherapy) on repetition of SH, hopelessness scores, and suicide by the 12‐month follow‐up assessment (McLeavey 1994). There was also no overall effect for this intervention on treatment adherence, although those assigned to the IPSST group did attend a greater number of treatment sessions.
Behaviour therapy
Based on a single trial, there is likely no effect of behaviour therapy compared to alternative psychotherapy (i.e. insight‐oriented therapy) on repetition of SH by the 24‐month follow‐up assessment, although there was an apparent effect for behaviour therapy on depression scores as compared to alternative psychotherapy, at least in the short term (i.e. post‐intervention assessment) (Liberman 1981). Behaviour therapy was also associated with mixed findings with respect to suicidal ideation scores in this trial.
Intensive in‐ and outpatient treatment
Based on a single trial, there is likely no effect of brief inpatient psychiatric admission admission followed by regular outpatient appointments plus 24‐hour access to a treatment service (i.e. intensive in‐ and outpatient treatment) compared to TAU on repetition of SH, frequency of SH repetition, or on time to SH repetition by the 12‐month follow‐up assessment (Van der Sande 1997). There was also no apparent effect for this intervention on treatment adherence, depression scores, hopelessness scores, or suicide.
General hospital admission
Based on a single trial involving patients who would normally have been admitted to a general hospital following SH, there is probably little to no effect of general hospital admission compared with discharge from the hospital on repetition of SH by either the post‐intervention or the four‐month follow‐up assessment (Waterhouse 1990). There was also no apparent effect for this intervention on social functioning or suicidal ideation scores by either time point. However, as trial entry was limited to low‐risk participants, only around 15% of presenting patients were eligible for inclusion in this trial.
Intensive outpatient treatment
Based on two trials that compared a combination of intensive therapies, including psychotherapy, behaviour therapy, and family therapy versus standard outpatient care, there is likely no effect of intensive outpatient treatment on repetition of SH by either the four‐month (Welu 1977) or 24‐month (Allard 1992) follow‐up assessments. There is likely no effect of this intervention on treatment adherence, general functioning, or suicide deaths; although secondary outcomes were only investigated in one of these two trials (Allard 1992).
Home‐based psychotherapy and telephone contact
Based on a single trial, there is likely no effect of home‐based psychotherapy on repetition of SH by the 12‐month follow‐up assessment (Hawton 1981). Whilst there was an apparent effect for this intervention on treatment adherence, there was no such effect on suicidal ideation scores. As modified scales were used to assess depression and social functioning, however, we were unable to include data for these secondary outcomes in our review.
Long‐term therapy
Based on a single trial, long‐term therapy (the therapeutic content and focus of this approach was not specified) may have little to no effect on repetition of SH by the post‐intervention assessment compared with short‐term intensive therapy (Torhorst 1988). Overall treatment adherence was fairly low in both groups, however. Estimates of scores from graphs also suggests there was no apparent effect for long‐term therapy on depression scores.
Overall completeness and applicability of evidence
Completeness of evidence
Where it was unclear whether a trial satisfied our inclusion criteria, we contacted corresponding trial authors for clarification. We also contacted corresponding authors where data were either not clearly reported, or where we required data reported in a different format to allow for their inclusion in a meta‐analysis. However, despite engaging in over 200 emails with corresponding authors we were not always able to obtain all relevant data. This was due to a combination of non‐response to our enquiries and to authors being unable to access relevant data, often due to moving on to later positions or as a result of working from home due to COVID‐19 pandemic quarantine orders. This is a common problem in meta‐analyses (Selph 2014).
There are some concerns with regards to completeness of evidence for two large multicentre and multi‐country trials of information and support. For the START Study, although the trial was originally scheduled to be conducted in 13 countries (De Leo 2013), data from only one of these sites (i.e. French Polynesia; Amadéo 2015) has been published to date. Additionally, while the SUPRE‐MISS trial was scheduled to be conducted in 18 sites (Fleischmann 2002), data from only five of these were reported in Fleischmann 2008 and a related publication (Bertolote 2010). Secondary data from three sites (i.e. China [Xu 2012], Iran [Hassanzadeh 2010], and India [Vijayakumar 2011]) have also been published. However, data for the remaining sites involved in this trial have not been published to date.
Presence of publication bias could only be formally evaluated for three meta‐analyses for CBT‐based psychotherapy with respect to repetition of SH at six months (Figure 4) and 12 months (Figure 5), and for suicide deaths at final follow‐up (Figure 6). In all cases, some funnel plot asymmetry was apparent and seemed to affect the right side of the plot suggesting that there may be unpublished trials in which the intervention was found to be ineffective. However, as the remaining meta‐analyses in this review included fewer than 10 trials, we were unable to investigate publication bias for these analyses.
4.

Funnel plot: CBT‐based psychotherapy on repetition of SH at six‐months.
5.

Funnel plot: CBT‐based psychotherapy on repetition of SH at 12‐months.
6.

Funnel plot: CBT‐based psychotherapy on suicide deaths by final follow‐up.
Whilst all but two of the included trials reported information on repetition of SH, publication bias may have been more common for the secondary outcomes assessed by this review. However, formal testing of publication bias was not possible due to the small number of trials. Therefore, we cannot rule out the possibility that publication bias may have affected the results of the other analyses in this review. This is a problem that commonly affects clinical data (Easterbrook 1991).
Applicability of evidence
The majority of participants in these trials were female, reflecting the typical pattern in hospital‐presenting populations (Hawton 2008). Only four trials stratified randomisation by sex (Hvid 2011; McAuliffe 2014; Van der Sande 1997; Walton 2020) whilst data were analysed separately by sex in six further trials (Bennewith 2002; Carter 2005; Fleischmann 2008; Hassanian‐Moghaddam 2011; Kapur 2013; Marasinghe 2012). Trials where sex was reported largely indicated benefits for females, but not males, in line with a previous review (Krysinska 2016). However, as these trials generally included fewer males, it may be that subgroup results for males were underpowered. Given that there are some differences in the motives for SH in males as compared to females (Claes 2007), further work on the treatment needs and preferences of males who engage in SH, as well as their experiences of clinical services, and how these may differ from females who engage in SH, is warranted. Further, a binary approach to gender was evident in the majority of trials. There was therefore poor attention to, and reporting of, outcomes for those with a non‐binary gender identity. There is good evidence that there are higher risks of self‐harm in those who are gender diverse (Newcomb 2020).
The majority of trials included either patients who have all engaged in intentional drug overdoses or self‐poisoning, or samples where the majority had, again reflecting the typical pattern observed in patients who present to general hospitals following SH (Hawton 2007). However, there are other important patient subgroups, such as those who engage in self‐cutting, who may have different treatment needs (Hawton 2004). None of the trials included in this review specifically focused on these patients; although it should be noted that method switching is common in those who engage in repeat episodes of SH (Witt 2019). In some trials there was a lack of information relating to the method of SH. Seventeen (22.4%) trials focused on those with a history of repeated SH, which is a particular issue in this clinical population, given the association of individuals with a history of repeat episodes having a greater risk of suicide (Zahl 2004). However, only 14 investigated impacts of psychosocial interventions for those with an initial episode of SH versus those engaging in repeated SH (Amadéo 2015; Bennewith 2002; Carter 2005; Evans 1999a; Gratz 2014; Hatcher 2011; Hatcher 2015; Hatcher 2016; Hassanian‐Moghaddam 2011; Kapur 2013; Lin 2020; McAuliffe 2014; Morthorst 2012; Mouaffak 2015). Outcomes were generally not stratified by recruitment setting (e.g. emergency department, community, and/or GP‐based referrals). This could be a focus of future trials and reviews. Secondary outcomes were also infrequently assessed which limits interpretation of possible mechanisms of effect.
Compared to previous versions of this review (Hawton 2016), there is now greater representation of trials from low‐to‐middle‐income countries, including: Iran (Hassanian‐Moghaddam 2011; Mousavi 2015; Mousavi 2017), Taiwan (Lin 2020; Wang 2016), China (Wei 2013), India (Sreedaran 2020), Malaysia (Armitage 2016), Pakistan (Husain 2014), South Africa (Naidoo 2014), and Sri Lanka (Marasinghe 2012). Additionally, two multicentre and multi‐country trials were conducted in a number of countries, including several low‐to‐middle‐income countries (e.g. Brazil, China, India, and Iran (Fleischmann 2008), and French Polynesia (Amadéo 2015)).
This review focused exclusively on those who engaged in SH. As a result, we have excluded trials in which participants were diagnosed with conditions such as borderline personality disorder but where SH was not required for trial entry. We also excluded trials in which participants engaged in repetitive self‐injurious behaviour in the context of an intellectual disability or developmental disorder (e.g. an autism spectrum disorder). Readers interested in the use of psychosocial interventions for these patient groups are instead referred to the relevant reviews (Cristea 2017; Oliver 2010).
Quality of the evidence
Certainty of evidence, as assessed using the GRADE approach, was generally moderate to very low suggesting that further research is likely to have an important impact on our confidence in the estimates of treatment effectiveness, and may in fact change the estimates. This is particularly likely to affect results for those interventions that so far have only been assessed in single trials.
Additionally, using the Cochrane 'Risk of bias' tool version 2.0 (Sterne 2019), for almost all (85.5%) trials included in this review there were some concerns or a high risk of bias in relation to at least one aspect of trial design, with weaknesses most commonly observed with respect to selection of the reported result and measurement of the outcome.
For most trials, insufficient information was reported to determine whether data were analysed in accordance with a prespecified plan. In 2015, the International Committee of Medical Journal Editors (ICMJE) recommended all clinical trials should be preregistered in a public trials registry (Witt 2020a). Whilst around half (54.5%) of the 22 trials published subsequent to this recommendation were preregistered, in some cases there was insufficient detail provided within the clinical trial register to determine how key outcome(s) were defined. This made it difficult to determine whether there had been any substantive changes to the proposed analysis plan and, if so, the reasons for any such departures. Future trials should provide sufficient detail within the clinical trial register to determine how key outcome(s) are defined and measured to aid in the determination as to whether there has been any substantive changes to the proposed analysis plan, and if so, the reasons for any such departures.
There were also some concerns relating to bias in the measurement of the outcome. This was typically because repetition of SH was based on self‐reported information. Given that around two‐thirds of SH recorded in medical and clinical records are not reported by participants, prevalence estimates derived from self‐reported information alone may underestimate the true rate of SH (Mitchell 2016). By supplementing data on self‐reported SH with information from clinical or medical records, future trials could compare results based on self‐reported information with those obtained from objective sources to investigate what impact, if any, this bias may have had on the estimate of treatment effectiveness.
Additionally, participants and clinical personnel were, typically, not blind to allocation owing to likely differences in treatment intensity between the intervention and control arms (Witt 2020a). Indeed, due to safety considerations, unblinding may be unavoidable in these types of trials. However, given that repetition of SH was based on self‐report in a number of the included trials (Amadéo 2015; Armitage 2016; Brown 2005; Davidson 2014; Fleischmann 2008; Gratz 2006; Gratz 2014; Harned 2014; Hassanian‐Moghaddam 2011; Husain 2014; Liberman 1981; Linehan 1991; Linehan 2006; Linehan 2015; McMain 2009; Mousavi 2015; Mousavi 2017; Naidoo 2014; O'Connor 2015; O'Connor 2020; Priebe 2012; Sahin 2018; Slee 2008; Tapolaa 2010; Torhorst 1987; Turner 2000; Walton 2020; Wei 2013; Weinberg 2006), this may introduce potential bias.
Lastly, the trials included in this review were, in general, relatively small to detect differences in proportions of patients who engage in a repeat episode of SH, although it is acknowledged that some of the trials were feasibility studies (Davidson 2014; Evans 1999b; Gibbons 1978; Harned 2014; Kapur 2013; O'Connor 2015; O'Connor 2020; Owens 2020; Sreedaran 2020). Whilst sample sizes have increased over time, most trials in this field are still underpowered. We have previously calculated that trials in this field may need to recruit up to a minimum of 1862 participants per arm to detect an effect for repetition of SH with 80% power at the conventional alpha level (Witt 2020a). Future trials should therefore supply a priori power calculations to justify their sample size.
Potential biases in the review process
We are confident that we have identified all relevant psychosocial interventions for SH in adults. However, we cannot rule out the possibility that some relevant outcome data may be missing from this review. Although data on repetition of SH were available for all but two of the included trials, limited data were available on secondary outcomes. Nevertheless, by using the random‐effects model in all analyses, our results possess greater generalisability than if we had used the fixed‐effect model (Erez 1996).
It is worth noting that the categorisation and grouping of interventions in this review may, in some cases, obscure the nature of the discrete interventions within a particular comparison. For example, a decision was made to group brief problem solving therapy (PST) with CBT into a single comparison we have referred to as 'CBT‐based psychotherapy'. As PST is usually a component of CBT, we have included trials where PST was the key therapeutic modality. It is important that those making decisions about the interventions examined in this review attend to the particular therapeutic components used in each trial included in any particular comparison (as we have detailed in the Characteristics of included studies table).
Agreements and disagreements with other studies or reviews
This review is an update of the 2016 Cochrane Review on psychosocial interventions for SH in adults (Hawton 2016). The previous review included 55 trials of seven different approaches, finding that CBT‐based psychological therapy may result in fewer individuals repeating SH whilst DBT may lead to a reduction in frequency of repeated SH. This update concurs with its previous iteration. There appears to be a probable beneficial effect for CBT‐based psychotherapy on repetition of SH as compared to TAU or another comparator immediately after the end of therapy, and this effect appears to be maintained over time. There also appears to be limited positive findings for DBT in terms of reduced frequency of SH.
We identified 18 further reviews that included a focus on psychosocial interventions for SH in adults that have been completed since the previous version of this review was published. Six were systematic reviews (D'Anci 2019; Hanratty 2019; Inagaki 2019; Krysinska 2017; Milner 2015; Tighe 2018), 10 included meta‐analysis (Bornheimer 2020; Briggs 2019; Calati 2016; DeCou 2019; Gøtzsche 2017; Hetrick 2016; Meerwijk 2016; Milner 2015; Padmanathan 2020; Riblet 2017), and two were narrative reviews (Ghanbari 2015; Pirkis 2020). The majority of these reviews included studies where participants had mixed clinical presentations (i.e. clinically significant levels of suicidal ideation and/or SH), and not all were limited to RCTs.
Of these reviews, those that have focused on specific intervention approaches, including acceptance and commitment therapy (ACT)‐based approaches (Tighe 2018), brief contact interventions (Ghanbari 2015; Milner 2015; Milner 2016), CBT (Gøtzsche 2017), the Collaborative Assessment and Management of Suicidality (CAMS) model (Hanratty 2019), DBT (DeCou 2019), psychoanalytic and psychodynamically‐oriented therapy (Briggs 2019), and provision of information and support (Pirkis 2020), have generally reported evidence of benefit for the approach examined; although two reviews of brief contact interventions (Milner 2015; Milner 2016) and one each of the ACT (Tighe 2018) and CAMS model (Hanratty 2019) indicated there was limited evidence for these approaches on repetition of SH, in line with findings from our review.
Of these reviews that have adopted a broader focus, whilst they generally indicated that delivering some form of psychotherapy is likely to be more effective than nothing (e.g. Bornheimer 2020; Calati 2016; Hetrick 2016; Inagaki 2019; Meerwijk 2016; Riblet 2017), these reviews have tended to statistically pool results from very different interventions together and so the results are largely meaningless for clinical practice as they provide little insight into which approach may be most beneficial for particular clinically relevant subgroups of patients.
Future reviews should undertake network meta‐analysis to investigate which component(s) of these typically multi‐component intervention approaches are most effective. Individual participant data meta‐analyses would also assist with the identification of clinically relevant subgroups of patients who may benefit from certain more intensive forms of intervention.
Authors' conclusions
Implications for practice.
The number of trials and range of interventions identified in this version of the review represents a considerable increase compared with the previous version (Hawton 2016). In this update, we found 76 non‐overlapping trials of a wide range of psychosocial interventions for adults who engage in SH. Overall, there were significant methodological limitations across the trials included in this review. There may be some positive effects for cognitive behavioural therapy (CBT)‐based psychotherapy for individuals in reducing repetition of SH compared with treatment‐as‐usual (TAU), particularly over the longer term. This is perhaps unsurprising as these trials were generally much briefer in terms of the number of therapy sessions delivered (e.g., often between 3 to 5 sessions, and never more than 10 sessions) as compared with traditional CBT‐based psychotherapy for depression. Services may wish, where this is feasible, to ensure availability of clinicians to deliver these types of intervention. This is in keeping with official guidance (Carter 2016; NICE 2011).
There were also some positive effects, particularly with regards to frequency of SH repetition, for several interventions for the treatment of individuals with borderline personality disorder (in which repetitive self‐harm is often a feature), noting that the trial participants were mostly female in these trials. Arguably, where patients engage in repeated episodes of SH, reduction in the frequency of SH could be viewed as a key outcome. Variation in the method of provision of DBT does not appear to differ in effectiveness from standard DBT. The standard DBT approach is, however, lengthy (typically one year; Linehan 1991) and necessitates considerable therapist time. We also found some positive effects for both MBT and emotion‐regulation psychotherapy delivered in a group‐based format in individuals diagnosed with borderline personality disorder, although these findings were based on a single trial (MBT) or trials conducted by the same group (emotion‐regulation psychotherapy). We therefore recommend further evaluation of these approaches. Given the multi‐component nature of these intervention approaches for treatment of individuals with borderline personality disorder, greater use of head‐to‐head trials, which allow for dismantling of the effect size(s) between one or more component(s), should be considered, especially as this might help to identify effective components which could be delivered more briefly.
Remote contact interventions, such as sending regular postcards to patients, have been evaluated in several trials. Whilst positive results compared to TAU with regard to repetition of SH at both short‐ and longer‐term follow‐up have been reported, the main positive result comes from a single large trial conducted in a resource‐poor setting (Iran) where mental health services are sparse (e.g. Iran has an average of 2.0 psychiatrists and 9.5 mental health‐trained nurses per 100,000 persons; WHO 2019). Therefore this relatively low intensity intervention may represent a considerable improvement over the likelihood of receiving little to no aftercare. Remote contact interventions may therefore hold some promise in settings where there are very limited psychiatric services, and should remain an area for further development in such settings.
An argument for intervention following an episode of SH is that it may improve other outcomes even if it does not reduce SH. Secondary outcomes were examined variably in many of the included trials. There was only limited evidence that experimental interventions result in better outcomes in these other domains. CBT‐based psychotherapy, DBT, MBT, and emotion‐regulation psychotherapy may lead to better outcomes in depression severity, hopelessness, and possibly also social functioning in the short term. Case management may improve treatment adherence. However, the certainty of evidence was very low to moderate.
Indeed, few specific types of psychosocial interventions appear to perform better than TAU. However, TAU was not well described in most clinical trials we examined. TAU also varies greatly across clinical settings (Witt 2018). For example, in one trial in which the comparator was 'enhanced usual care' this consisted of little more than GP management (Kawanishi 2014). Whilst this may represent enhanced usual care in that setting, it does not compare favourably with TAU in a number of other studies of this intervention approach (e.g. Clarke 2002). A positive step forward would be the operationalisation of TAU to inform both clinical practice and research. It is possible that TAU has an advantage over some of these interventions because it offers more flexibility to tailor treatment to the specific needs of patients.
Results of this review would also suggest that, whilst case management approaches did not appear to be effective in reducing the proportion of participants who repeat SH, case management may increase engagement with subsequent treatment whilst, additionally, enabling the identification of psychosocial needs that should be addressed during treatment. A comprehensive therapeutic psychosocial assessment combined with case management may have a potential role in encouraging individuals to attend for other types of therapy and therefore might be a useful part of a clinical intervention. This is in keeping with official guidance (NICE 2011).
Implications for research.
The primary outcome of this review was repetition of SH at post‐intervention to ensure consistency between the reviews in this suite of studies and, additionally, as this was the time point for which data were reported most consistently between the trials included in this review. However, it is acknowledged that, in contrast to trials of pharmacological interventions (which is the subject of a related review) where repetition of SH by post‐intervention may be the most appropriate choice, there is no consensus presently as to what time point(s) may be most appropriate for trials of predominately psychosocial interventions. As the aim of many of these approaches is to equip patients with new skills that may take time for them to master and use in dealing with future crises, it may be unrealistic to expect benefits to be apparent immediately post‐intervention. This may be particularly so for the many brief intervention approaches we identified in this review. Longer follow‐up assessments are therefore advisable. Given that naturalistic studies of SH patients following discharge from services would suggest that the risk of SH repetition and suicide may be greatest in the 12‐months following discharge, peaking at one‐month post‐discharge (Geulayov 2019; Gunnell 2008; Gilbody 1997), assessments at these time points should be considered in future trials.
Given that SH results from a complex interplay between genetic, biological, psychiatric, psychosocial, social, cultural, and other factors, the development of psychosocial interventions for SH in adults could benefit from being based on detailed investigation of these factors, including those that might enhance resilience that thereby reduces the risk of further SH, as well as having benefits for other outcomes.
Additionally, trials of psychosocial interventions for adults who engage in SH should include a range of outcome measures, not just SH and suicide, but also acceptability, adherence, and attitudes to treatment by patients, their caregivers, and services providers as these may help to identify contributors to any apparent benefit or lack of impact. In particular, the inclusion of outcomes that matter to those who engage in SH is required to further inform intervention development (Owens 2020b). It is also important that adverse effects, both short‐ and long‐term, are carefully evaluated.
Investigation of the mechanisms through which treatments might work is also desirable to assist with the identification of clinically relevant subgroups of patients who may benefit from certain, more intensive forms of intervention. For example, whilst CBT‐based psychotherapy may have benefit in patients for whom SH is predominately driven by depressive symptomatology (Gøtzsche 2017), more intensive forms of psychosocial intervention (e.g. standard DBT, MBT, and possibly emotion‐regulation psychotherapy) may be more appropriate for those who engage in frequent and repetitive SH in the context of a personality disorder, particularly borderline personality disorder.
In trials where sex differences were examined, outcomes generally favoured females (perhaps partly because mixed‐sex trials included far more women than men, with consequent power issues for examining outcomes in men). However, given that suicide following SH is more common in men (Geulayov 2019; Carroll 2014), attention needs to be paid to the development of interventions that may address the particular needs of men who engage in SH.
There is a major need for further development and evaluation of interventions in lower‐ and middle‐income countries, particularly where psychiatric services may be limited. Such developments are likely to include remote contact and support interventions, which should be evaluated in large‐scale trials, particularly as repetition of SH appears often to be less frequent than in Western settings (Carroll 2014; Knipe 2019).
Heed should also be paid to the principles of development and evaluation of treatments, as laid out in the UK Medical Research Council guidance regarding complex interventions. Additionally, from a service planning perspective, future trials should also include economic evaluations in order to determine which interventions may be more feasible to routinely implement throughout a health service (Bustamante‐Madsen 2018).
What's new
| Date | Event | Description |
|---|---|---|
| 21 April 2021 | New citation required and conclusions have changed | A new protocol including updated methodology was applied (Witt 2020b). Twenty‐one new studies were included in this review compared to the earlier version (Hawton 2016). |
| 21 April 2021 | New search has been performed | This review updates and replaces the Cochrane Review 'Psychosocial interventions for self‐harm in adults' (Hawton 2016). |
History
Protocol first published: Issue 7, 2020 Review first published: Issue 4, 2021
| Date | Event | Description |
|---|---|---|
| 1 July 2020 | New citation required and major changes | We updated the protocol developed for Hawton 2016 |
Risk of bias
Risk of bias for analysis 1.1 Repetition of SH at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Mousavi 2017 | Some concerns | "Eligible subjects were allocated to two groups (intervention and control), with simple randomization by a third party physician using tables of random numbers" (p.2). No information on allocation concealment reported. "There is no difference between the two groups in terms of demographic and clinical characteristics" (p.3). |
Some concerns | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. There was no information as to whether intention‐to‐treat analyses had been conducted. Subsequent analyses appear to be based on those participants with available information suggesting modified intention to treat analyses were used. |
Low risk of bias | Data were available for 100% of those randomised. | Some concerns | Data on repetition of self‐harm was obtained via self‐report. However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). As both the intervention and comparator arms received face‐to‐face therapy in this trial, there was no significant difference in treatment modality. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. However, as the intervention was not found to be significant, this is unlikely. |
Some concerns | Data on repetition of self‐harm was obtained via self‐report. All eligible reported results for repetition of SH correspond to all intended analyses of the data. | Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Stewart 2009 | Some concerns | Correspondence with trial authors clarified that "[n]ames of treatment groups were drawn from a container and participants were allocated to a treatment group". However, no information on allocation concealment reported. Referring to Table 1 (p.542), only data on certain clinical characteristics (e.g., hopelessness, satisfaction with treatment, social problem solving, and suicidal ideation scores at baseline were reported. Whilst there were no significant differences between the intervention and comparator arms on these variables, there were no data reported on any demographic factors at baseline. |
Low risk of bias | Correspondence with authors clarified that the “treatment condition was offered to the client via a phone call”, suggesting that participants would have known to which arm they had been allocated. Correspondence with trial authors further clarified that the therapist running the research was aware of which treatment condition the participant was being offered. There were no apparent deviations from the intended intervention. Correspondence with authors clarified that 10 participants dropped out of the comparator arm, 12 dropped out of the CBT arm, and 11 dropped out of the PST arm. Data were analysed using the modified intention to treat principle. |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "…repeated attempt data from hospital chart audits that recorded re‐presentation to hospital for suicide attempts"(p.541). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Correspondence with authors clarified that the "therapist collected outcome data via self‐report measures and chart audits." However, neither clinical personnel were not blind to treatment allocation. Repetition of SH as determined by clinical and hospital records represents an observer‐reported outcome. |
Some concerns | "Measures were administered...directly following treatment (for the PST and CBT groups), and at two months follow‐up (for the TAU group)" (p.542). All eligible reported results for repetition of SH correspond to all intended outcome. "…repeated attempt data from hospital chart audits that recorded re‐presentation to hospital for suicide attempts" (p.541). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Wei 2013 | Some concerns | "[P]articipants...were randomly assigned...using a computerized randomization program" (p. 109). However, no information on allocation concealment reported. "The three groups did not significantly differ on age, education, minority race, marriage, sex, occupation, and mental disorder diagnosis" (p.110). |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "All analyses were conducted using the intent‐to‐treat (ITT) principle..." (p.110). |
High risk of bias | Data were available for 72.0% of those randomised. Sensitivity analyses were not undertaken. "...the cumulative dropout rate [at post‐intervention] was 32.9% (n = 27) for the cognitive therapy group, 30.0% (n = 24) for the telephone intervention group, and 20.8% (n = 16) for the control group; the proportion of participants with missed assessment of three groups was not significantly different" (p.110). No other information on causes of missingness reported. |
Some concerns | "...research assessors followed up patients by telephone using measures of a detailed structured questionnaire...[to assess] suicidal history of patients" (p.110). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If clinical personnel were acting as outcome assessors, they may have influenced assessment of the outcome. However, as the intervention was not found to be significant, this is unlikely. |
Some concerns | "At the 3 months, 6 months, and 12 months post baseline assessments, the research assessors followed up patients..." (p.110). All eligible reported results for repetition of SH correspond to all intended outcome. "...research assessors followed up patients by telephone using measures of a detailed structured questionnaire...[to assess] suicidal history of patients" (p.110). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
High risk of bias | Overall, this trial was rated as some concerns for risk of bias as missingness in the outcome could have depended on its true value and analyses did not correct for bias, nor were sensitivity analyses undertaken to investigate the potential effect of missing data. |
| Weinberg 2006 | Low risk of bias | "Subjects were randomly assigned..." (p. 485). Correspondence with trial authors clarified that "subjects were asked to choose between 2 similar envelopes..." However, detail on the randomisaton method was not reported. Additionally, it was not clear whether these envelopes were sequentially numbered. There were no significant differences between the intervention and comparator arms for any of the demographic characteristics and clinical variables measured (Table 1, p.486). |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. Although "[a]ll [intervention] participants completed 6 sessions of MACT. Two [comparator] group participants were not available for the post‐treatment assessments" (p. 485). Nevertheles, "[a]ll participants were interviewed at the 6 months follow up" (p.485), suggesting that intention‐to‐treat analyses were undertaken. |
Low risk of bias | Data were available for 100% of those randomised (by the six‐month assessment). | Some concerns | Repetition of self‐harm was ascertained from the "Parasuicide History Interview‐PHI " (p.486). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If clinical personnel were acting as outcome assessors, they may have influenced assessment of the outcome. However, as the intervention was not found to be significant, this is unlikely. |
Some concerns | "The follow‐up assessments by [sic] performed after completion of the [intervention] (e.g, 6‐8 weeks after baseline assessments) and at a similar time point in the control group" (p.486). All eligible reported results for repetition of SH correspond to all intended outcome. Repetition of self‐harm was ascertained from the "Parasuicide History Interview‐PHI " (p.486). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
Risk of bias for analysis 2.1 Repetition of SH by post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 2.1.1 Comparator: TAU | ||||||||||||
| Linehan 1991 | Low risk of bias | "...randomized” (p. 1060). Correspondence with authors clarified that they used a computer programme to generate the random sequence. Additionally, correspondence with authors further clarified that allocation had been concealed. "No significant pretreatment between‐group differences appeared on lifetime parasuicides, psychiatric hospitalizations, Diagnostic Interview for Borderlines scores, depression, hopelessness, suicide ideation, reasons for living age, employment, or marital status" (p.1062). | Some concerns | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. There was no information as to whether intention‐to‐treat analyses had been conducted. Subsequent analyses appear to be based on those participants with available information suggesting modified intention to treat analyses were used. |
High risk of bias | "Ten subjects dropped out of the study during the pretreatment assessment…seven subjects were dropped following pretreatment assessment for refusal or inability to meet study conditions…Two subjects...were dropped from all analyses [due to treatment non‐adherence]" (p.1061). Therefore, data were available for 69.8% of those randomised. Sensitivity analyses were not undertaken. Data were available for 68.7% of those randomised to the intervention arm, and 71.0% of those randomised to the comparator arm. Additionally, data for 24/63 (38.1%) participants were deliberately not included in the 24‐month follow‐up assessment. |
High risk of bias | "The PHI obtained information about all parasuicide behavior" (p.1061). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. As the intervention was found to be significant, this is possible. |
Some concerns | "The treatment lasted 1 year, with assessment every 4 months" (p.1060). All eligible reported results for repetition of SH correspond to all intended outcome. "The PHI obtained information about all parasuicide behavior" (p.1061). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
High risk of bias | Overall, this trial was rated as high risk of bias as unblinded personnel were acting as outcome assessors which may have influenced assessment of the outcome. As the intervention was found to be significant this is possible, particularly given that no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| McMain 2009 | Low risk of bias | "Eligible participants were randomly assigned to treatment arms using a pre‐generated block randomization scheme developed and held by the statistician who prepared 45 sealed envelopes, each containing the group allocations in random order for four participants" (p. 1366). "...there were no between‐group differences on baseline demographic characteristics, diagnostic variables, or suicidal and nonsuicidal self‐injurious behaviors" (p.1371). |
Low risk of bias | This was a single‐blind study and only "[a]ssessors...were...blind to treatment assignment" (p. 1366). Participants were therefore not blind to treatment allocation. Additionally, "[t]he study coordinator...was not blind to treatment assignment" (p. 1366). There were no apparent deviations from the intended intervention. "All results were analysed using an intent‐to‐treat analysis..." (p.1370). |
Low risk of bias | Data were available for 82.2% of those randomised. "...participants with missing data were still included in the model. Each model was reanalyzed using preselected covariates that are known or theorized to affect the outcome" (p.1371). |
Low risk of bias | "The primary outcome measures were frequency and severity of suicidal and nonsuicidal self‐injurious behavior episodes, as assessed by the Suicide Attempt Self‐Injury Interview" (p.1370). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Participants were not blind to treatment allocation. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. However, as the intervention was not found to be significant, this is unlikely. |
Some concerns | Referring back to the trial protocol (NCT00154154), no specific information was reported. "The primary outcome measures, assessed at baseline and every 4 months over the treatment period, were frequency and severity of suicidal and nonsuicidal self‐harm episodes" (p.1365). All eligible reported results for repetition of SH correspond to all intended outcome measurements. "The primary outcome measures were frequency and severity of suicidal and nonsuicidal self‐injurious behavior episodes, as assessed by the Suicide Attempt Self‐Injury Interview..." (p.1370). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Priebe 2012 | Some concerns | "Randomisation was computer generated with a 1:1 allocation...using 6 blocks of 12 randomly permuted treatment allocation sequences, with a final block of 8" (p. 358). However, no information on allocation concealment reported. There were no significant differences between the intervention and comparator arms for any of the demographic characteristics and clinical variables measured (Table 1, p.360). |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "[M]issing covariate values were...[estimated using] maximum likelihood estimation [to] ensure...unbiased parameter estimates. We...[also] conducted a sensitivity analysis with last observation carried forward" (p.358). |
Low risk of bias | Data were available for 93.7% of those randomised. "[M]issing covariate values were...[estimated using] maximum likelihood estimation [to] ensure...unbiased parameter estimates. We...[also] conducted a sensitivity analysis with last observation carried forward" (p.358). Moreover, for the primary outcome, "[t]he sensitivity analysis with last observation carried forward showed a very similar result..." (p.360). |
Some concerns | "The primary outcome was self‐harm...recorded in an interview on a structured form" (p.358). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. However, as the intervention was not found to be significant, this is unlikely. |
Some concerns | "The primary outcome was self‐harm...[t]his was assessed...at each 2‐month follow‐up thereafter" (p.358). All eligible reported results for repetition of SH correspond to all intended outcome. "The primary outcome was self‐harm...recorded in an interview on a structured form" (p.358). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Subgroup 2.1.2 Comparator: Alternative psychotherapy | ||||||||||||
| Linehan 2006 | Some concerns | "Computerized adaptive minimization randomization procedure" (p. 758). No information on allocation concealment reported. "The treatment groups did not significantly differ on demographic characteristics, diagnoses, or pretreatment number of suicide attempts or nonsuicidal self‐injuries" (p.760). |
Some concerns | "Initial assessments were done before informing subjects of treatment assignment" (p. 758), suggesting that participants were made aware of treatment assignment during the trial. Additionally, given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. There was no information as to whether intention‐to‐treat analyses had been conducted. Subsequent analyses appear to be based on those participants with available information suggesting modified intention to treat analyses were used. Moreover, "we examined the effects of differential missing data and treatment dropout on each of our major outcome variables and found no evidence that the findings were biased by these differences" (p. 760). |
Low risk of bias | Data were available for 96% of those randomised. | Low risk of bias | "The Suicide Attempt Self‐Injury Interview measured...suicide intent, and medical severity of each suicide attempt and nonsuicidal self‐injury" (p.758). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "Initial assessments were done before informing subjects of treatment assignment" (p. 758), suggesting that participants were made aware of treatment assignment during the trial. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. However, as the intervention was not found to be significant, this is unlikely. |
Some concerns | "Our primary method for analyzing repeated‐measures data (pretreatment through the 24‐month assessment)..." (p.760). All eligible reported results for repetition of SH correspond to all intended outcome. "The Suicide Attempt Self‐Injury Interview measured...suicide intent, and medical severity of each suicide attempt and nonsuicidal self‐injury" (p.758). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias no specific information on allocation concealment was reported. Additionally, no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Turner 2000 | Some concerns | "Participants [were] randomly assigned..." (p. 414). However, without further specific information on the method used it is difficult to ascertain whether the randomisation sequence was adequate. Additionally, no information on allocation concealment reported. "To determine if the random assignment procedure worked, we examined the pretreatment values of the dependent variables for each...outcome...there were no significant differences between the groups" (pp.416‐7). However, information on any differences in demographic characteristics at baseline was not reported. |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "All 24 patients participated in the 6 month and 12 month assessments and composed the intention‐to‐treat sample for the analyses" (p. 414). |
Low risk of bias | Data were available for 100% of those randomised. | High risk of bias | "Patients...maintained daily logs of suicidal urges and attempts" (p.415). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. As the intervention was found to be significant, this is possible, and given the magnitude of the effect size, this is likely. |
Some concerns | "Outcome assessment was conducted at pretreatment, 6 months, and 12 months" (p.415). All eligible reported results for repetition of SH correspond to all intended outcome. "Patients...maintained daily logs of suicidal urges and attempts" (p.415). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
High risk of bias | Overall, this trial was rated as high risk of bias as unblinded personnel were acting as outcome assessors. They may have influenced assessment of the outcome. As the intervention was found to be significant, this is possible, and given the magnitude of the effect size, this is likely. |
| Walton 2020 | Low risk of bias | "A stratified randomisation procedure was used to maximise the likelihood of comparable distributions across groups for gender and antidepressant use. A computerised formula with blocked randomisation (blocks of 4) was used by an independent research manager of the health service. A sealed, opaque envelope containing randomisation status was given to participants at the end of their assessment" (p.3). "The two groups showed no imbalances at baseline after randomisation with regard to sociodemographic and clinical characteristics" (p.7). |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. Referring back to the trial protocol (ACTRN12612001187831), there was no apparent deviation from the intended intervention. "Intent‐to‐treat analyses..." (p.7). All patients who were randomised and attended a minimum of one treatment session after the baseline assessment were included in the analysis. |
Low risk of bias | Data were available for 74.7% of those randomised. "To take into account missing data and maximise usage of all available data, major analyses comprised a series of generalised linear models (and, where appropriate, GEE analyses), together with some supplementary sensitivity analyses (e.g. restricted to participants completing posttreatment assessments)" (p.7). |
Some concerns | "Combined outcome of any episode of suicidal and non‐suicidal self‐injury [using] the SASI‐Count" (p.4). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. However, given that data obtained by correspondence indicated the intervention was not found to be significant, this is unlikely. |
Some concerns | "This study utilised an adapted time frame of behaviour occurring within the past 7 months" (p.4). All eligible reported results for repetition of SH correspond to all intended outcome. "Combined outcome of any episode of suicidal and non‐suicidal self‐injury [using] the SASI‐Count" (p.4). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
Risk of bias for analysis 3.1 Repetition of SH at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Gratz 2006 | Some concerns | "Random assignment" (p. 30). However, without further specific information on the method used it is difficult to ascertain whether the randomisation sequence was adequate. Additionally, no information on allocation concealment reported. "A series of...were conducted on demographic and clinical characteristic variables to determine equivalence across conditions. Results indicate no significant between‐group differences on any of these variables" (p.30). |
Some concerns | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. There was no information as to whether intention‐to‐treat analyses had been conducted. "Two participants dropped out of the study (one from each condition)" (p.27). Subsequent analyses appear to be based on those participants with available information suggesting modified intention to treat analyses were used. |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "The following self‐report measures...were used to assess outcome:
Deliberate self‐harm inventory" (p.29). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. However, as the intervention was not found to be significant, this is unlikely. |
Some concerns | "...self‐report measures [were] administered before and after treatment, were used to assess outcome" (p.29). All eligible reported results for repetition of SH correspond to all intended outcome. "The following self‐report measures...were used to assess outcome: Deliberate self‐harm inventory" (p.29). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information on randomisation or allocation concealment was reported. Additionally, no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Gratz 2014 | Some concerns | "Participants...were matched on four prognostic variables [emotion dysregulation, number of lifetime incidents of SH, global assessment of functioning (GAF) scores, and age] and randomly assigned...using a stratified randomization procedure" (p. 2100). However, without further specific information on the method used it is difficult to ascertain whether the randomisation sequence was adequate. Additionally, no information on allocation concealment reported. There were no significant differences between the intervention and comparator arms for any of the demographic characteristics and clinical variables measured (Table 1, p.2101). Furthermore, the trial authors undertook a series of tests "...on pre‐treatment scores on outcome measures to determine equivalence across conditions. The results indicate no significant between‐group differences...with one exception: the [intervention group] had significantly lower scores...on the DERS lack of clarity subscale...(p <0.05)" (p.2104). However, this may have been compatible with chance. |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "We adopted a Bayesian approach...using the Markov chain Monte Carlo routines...This approach implements a multiple imputation strategy to handle missing data...enabling an analysis of the intent‐to‐treat (ITT) sample" (p. 2104). |
Low risk of bias | Data were available for 100% of those randomised. | Some concerns | "The following measures were administered...to assess treatment efficacy...The DSHI [and] The Self‐Harm Inventory..." (pp.2100‐2). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. As the intervention was found to be significant, this is possible, but given the magnitude of the effect size, this is unlikely. |
Some concerns | "...measures were administered pre and post‐treatment or ‐waitlist to assess treatment efficacy, and at 3 and 9 months post‐treatment" (p.2100). All eligible reported results for repetition of SH correspond to all intended outcome. "The following measures were administered...to assess treatment efficacy...The DSHI [and] The Self‐Harm Inventory..." (pp.2100‐2). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information on randomisation or allocation concealment was reported. Additionally, no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
Risk of bias for analysis 4.1 Repetition of SH at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 4.1.1 TAU (whole sample) | ||||||||||||
| Clarke 2002 | Low risk of bias | "Randomisation was conducted using random numbered lists, stratified for sex and admitting hospital..." (p.169). Additionally, "[t]he random number lists were constructed independently of the research team and they did not have sight of them....The researchers were required to telephone an administrator with possible candidates’ details and were then informed of the treatment group" (p. 169). There were no significant differences between the intervention and comparator arms for any of the demographic characteristics and clinical variables measured (Table 1, p.172). |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "Data analysis proceeded on an intention to treat basis..." (p.170). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | Repetition of self‐harm was ascertained from readmission to hospital. However, only repeat episodes of self‐harm resulting in presentation to the study hospital were counted. Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. In this trial, researchers also acted as case managers. Repetition of SH as determined by clinical and hospital records represents an observer‐reported outcome. |
Some concerns | "The main outcome measure was readmission to A&E as a result of self‐harm within 12 months" (p.186). All eligible reported results for repetition of SH correspond to all intended outcome. "The main outcome measure was readmission to A&E as a result of self‐harm..." (p.186). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Hvid 2011 | Low risk of bias | "We applied a stratified randomization procedure...this stratified randomization procedure...created eight categories and randomization was performed for each independently" (p. 293). Without further specific information on the method used it is difficult to ascertain whether the randomisation sequence was adequate. However, "[r]andomisation was performed by an independent office" (p. 293). There were "no significant differences with respect to age, sex, method, type (violent/non‐violent), alcohol influence, psychiatric assessment, earlier psychiatric contact, earlier suicide attempt and reason (problem type)" (p.294). |
Low risk of bias | "The patient...knew who was a case and who was a control" (p. 293). Additionally, "...intervention staff knew who was a case and who was a control" (p. 293). There were no apparent deviations from the intended intervention. "Outcomes were measured by an intent‐to‐treat design in which all patients were followed until the end of the trial, irrespective of whether the patient was still receiving or complying with the assigned treatment" (p. 294). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "...information about suicidal behaviour...was obtained by our team through interview, public registrations, health records and staff" (p.293). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "[I]ndependent assessors (three psychiatrists) who reviewed all incidents did not have this information" (p. 294) on participants' treatment allocation. |
Some concerns | "Outcome data were obtained...in a 1‐year period, including 6 months after the completion of the 6‐month intervention period" (p.294). All eligible reported results for repetition of SH correspond to all intended outcome. "...information about suicidal behaviour...was obtained by our team through interview, public registrations, health records and staff" (p.293). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Subgroup 4.1.2 Enhanced usual care (whole sample) | ||||||||||||
| Kawanishi 2014 | Low risk of bias | "Participants were randomly assigned (1:1) by and Internet‐based system...to either the intervention group (assertive case management) or the control group (enhanced usual care). Assignment was by the minimisation method,with four factors: participating hospital, sex, age...and history of previous suicide attempts before the current episode..." (p. 194). Additionally, "[p]articipants were randomly assigned...by an Internet‐based system operated by a central, independent data centre" (p. 194). "Baseline characteristics were well balanced between the groups" (p.197). |
Low risk of bias | "...patients and case managers who provided the interventions were not [blind to treatment allocation]" (p. 194). There were no apparent deviations from the intended intervention. "Analyses were done in accordance with the intention‐to‐treat principle" (p.196). The sample was biased towards more compliant patients who were willing and able to attend a psychoeducation session seminar at the commencement of treatment and were able to attend hospital regularly for face‐to‐face interviews and case management sessions. |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "The primary outcome measure was the incidence of first recurrent suicidal behaviour" (p.196). However, even after referring to the trial protocol (NCT00736918) it is unclear how repetition of self‐harm was ascertained. It is likely that repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "Outcome assessors were masked to group assignment...The assessors did not know the participants’ assigned groups, the status of implementation of the intervention or information about events obtained by other on‐site staff" (p. 194). |
Some concerns | Referring back to the trial protocol (NCT00736918 and UMIN‐CTR C000000444), no specific information was reported. Referring back to the trial protocol (NCT00736918 and UMIN‐CTR C000000444), all eligible reported results for repetition of SH correspond to all intended outcome measurements. Referring back to the trial protocol (NCT00736918 and UMIN‐CTR C000000444), all eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Morthorst 2012 | Low risk of bias | "Computer randomisation was done by an independent research assistant stratified by whether the patient had previously attempted suicide (first attempt v previous attempt), previous psychiatric contacts or hospitalisations (none v previous contacts), and alcohol consumption at the time of suicide attempt (none v alcohol consumption)...The randomisation procedure ensured adequate...allocation concealment" (p.3). "The only differences between participants at baseline were that patients in the intervention group were more frequently being treated with antidepressants at inclusion [OR 1.99, 95% CI 1.18 to 3.55] and more frequently used narcotics as method of suicide attempt" (p.3). However, data on the proportion using narcotics at the index attempt were not reported making it difficult to determine whether this difference could have been compatible with chance. |
Low risk of bias | "[P]articipants were immediately informed of the outcome [i.e., allocation]" (p. 3). Additionally, "[o]wing to the nature of the study design, the intervention staff were not blinded" (p. 3) There were no apparent deviations from the intended intervention. "All participants were included in the analysis regardless of subsequent adherence to treatment, according to the intention to treat principle" (p.3). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "The outcomes of interest were repeated suicide attempt...We obtained information on these events through ICD‐10 diagnoses (recorded as part of standardised hospital registration procedure) and review of medical records. Additionally, we collected self reported data on events...through telephone interviews with patients" (p.3). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "An external medical evaluation committee conducted a blinded outcome assessment using medical records" (p. 3). However, trial authors later state "[t]he researcher conducting the analyses on self‐reported outcomes was...not blinded" (p.3). Repetition of SH as determined by clinical and hospital records represents an observer‐reported outcome. |
Some concerns | "Main outcome...[was r]epeated suicide attempt and death by suicide...at 1‐year follow‐up" (p.1). All eligible reported results for repetition of SH correspond to all intended outcome. "The outcomes of interest were repeated suicide attempt...We obtained information on these events through ICD‐10 diagnoses (recorded as part of standardised hospital registration procedure) and review of medical records. Additionally, we collected self reported data on events...through telephone interviews with patients" (p.3). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
Risk of bias for analysis 5.1 Repetition of SH at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Evans 1999a | Low risk of bias | "Randomised on a 1:1 basis...using the sealed envelope technique, ensuring that it was impossible to tell from feeling or looking at the envelopes whether they contained a green card or a ’dummy card’ (which was not given out)" (p. 23). However, without further specific information on the method used it is difficult to ascertain whether the randomisation sequence was adequate. "These [demographic and clinical] characteristics were simllar in the two groups, although there were slighily more males in the control group [OR 0.80, 95% CI 0.61 to 1.06]" (p.25). This may be compatible with chance. |
Low risk of bias | "Those randomised to receive a green card were offered the card immediately after the psychiatric assessment" (p.23). Given this, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "...all analyses were conducted on an intention‐to‐treat basis" (p. 24). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "All subiects' repeat hospital attendanccs for DSH...were monitored (blind to their study group) by means of a computerised case register based on routine accident and emergency and admission data for each of the three general hospitals" (p.24). Whilst only repeat episodes of self‐harm resulting in presentation to the study hospitals were counted, the authors do note that "...other accident and emergency departments were at least 13 miles away" (p.24). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "All subjects’ repeat hospital attendances for SH...were monitored (blind to their study group)..." (p. 24). |
Some concerns | "All subjects' repeat hospital attendanccs for DSH within six months of randomisation were monitored..." (p.24). All eligible reported results for repetition of SH correspond to all intended outcome. "All subiects' repeat hospital attendanccs for DSH...were monitored (blind to their study group) by means of a computerised case register..." (p.24). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as high risk of bias as there was a higher incidence of personality disorders as well as a higher number of subjects with multiple suicide attempts at baseline amongst those allocated to the intervention arm, suggesting there may have been a problem with the randomisation process. |
| Morgan 1993 | Some concerns | "Allocation to experimental or control group was carried out by random selection from a supply of closed envelopes, half of which contained the green card" (p.111). However, it is unclear whether these were opaque. Additionally, no information on allocation concealment reported. "The groups were similar in age...ethnic origin, marital, and occupational status. In both groups, depressive disorder was the most common diagnostic category" (p.111). |
Low risk of bias | "[Patients] receive[ed] the green card" (p. 111). Additionally, "GPs were also sent copies of the green card" (p. 111), suggesting that both participants and clinical personnel were aware of treatment allocation. There were no apparent deviations from the intended intervention. "Data concerning outcome were obtained for all patients included in the study" (p. 111). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "...follow up data were obtained by review of medical and psychiatric notes, as well as OP [outpatient] records of all patients" (p.111). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. No specific information on whether outcome assessors were aware of participants' treatment allocation was reported. Repetition of SH as determined by clinical and hospital records represents an observer‐reported outcome. |
Some concerns | "One year later, follow up data were obtained..." (p.111). All eligible reported results for repetition of SH correspond to all intended outcome. "...follow up data were obtained by review of medical and psychiatric notes, as well as OP [outpatient] records of all patients" (p.111). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
Risk of bias for analysis 6.1 Repetition of SH at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 6.1.1 Postcards (whole sample) | ||||||||||||
| Beautrais 2010 | Low risk of bias | “Participants were randomised 1:1...using predetermined computer‐generated random numbers...using a uniform distribution to generate a sequence of random numbers between 0 and 1. Numbers of 0.5 or above were classified as the intervention group; numbers below 0.5 were classified as the control group" (p. 56). Additionally, "[r]andomisation was performed...by research staff who were not involved in the recruitment or clinical care of participants" (p.56). "There were no significant differences between the intervention and control groups in age, gender, marital status, method of self‐harm, length of hospital stay or history of attendance for self‐harm in the 12 months prior to the index presentation" (p.57) However, whilst the trial authors state "...there was a significant difference between the groups in the number of prior attendances for self‐harm in the previous 12 months...with the number of prior attendances being lower in the intervention than in the control group" (p.57), this may have been compatible with chance. |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. However, "[p]articipants’ randomisation status was not conveyed to clinical...staff" (p.56). There were no apparent deviations from the intended intervention. "...results of the trial were analysed using the intention‐to‐treat design" (p. 56). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "Re‐presentations for self‐harm were assessed by monitoring two sources of re‐presentation information. First, psychiatric emergency service records were checked...to identify attendances by study participants. Second, participants’ hospital medical records were reviewed..." (p.56). However, only repeat episodes of self‐harm resulting in presentation to the study hospital were counted. Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "Participants’ randomisation status was not conveyed to...data‐collection staff" (p. 56). |
Some concerns | "Outcome measures were the proportion of participants re‐presenting with self‐harm and the number of re‐presentations for self‐harm in the 12 months following the initial presentation" (p.55). All eligible reported results for repetition of SH correspond to all intended outcome. "Re‐presentations for self‐harm were assessed by monitoring two sources of re‐presentation information. First, psychiatric emergency service records were checked...Second, participants’ hospital medical records were reviewed..." (p.56). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Carter 2005 | Some concerns | "Randomisation was by database (HanDBase, version 2.0, DDH Softwards, FL, USA) on a personal digital assistant (Palm III, Palm, CA, USA) that was populated with a pre‐generated randomisation schedule (in blocks of 10)..." (p. 2). This trial implemented Zelen’s post‐consent method. Therefore, following allocation participants were given the option to change treatment arms. Referring to Table 1 (p.3), there was a lower proportion of females assigned to the intervention as compared to the comparator arm (OR 0.57, 95% CI 0.42 to 0.77). This is unlikely to have been compatible with chance. However, there were no other significant differences between the intervention and comparator arms for any of the other demographic characteristics and clinical variables measured (Table 1, p.3). |
High risk of bias | "We used a randomised consent design, using the single consent version (Zelen’s design). This design is a variation on the standard randomised controlled experimental design, where participants are randomised...before consent is sought" (p.2). Additionally, "...the secretary responsible for managing the mailing database and postcards [was] not blind to allocation status" (p. 4). As clinical personnel knew whether or not a postcard had been sent, they could not have been blinded to allocation status. "Twenty participants in the control group received the intervention due to clerical errors but were included in the control group for the intention to treat analyses" (p.2). The proportion of participants crossing over was modest (6.6%). However, the proportion of participants crossing over was not balanced (i.e., 0% in the intervention arm compared with 6.6% in the comparator arm). "We assessed the outcomes by an intention to treat analysis on the basis of allocation" (p. 2). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "We extracted the descriptive variables of the sample from the toxicology service’s database, which were derived from the standardised clinical assessment of patients with deliberate self poisoning" (p.1). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "...research staff remained blinded to allocation" (p. 2). |
Some concerns | "Main outcome measures [were the p]roportion of patients with one or more repeat episodes of deliberate self poisoning and the number of repeat episodes for deliberate self poisoning per person in 12 months" (p.1). All eligible reported results for repetition of SH correspond to all intended outcome. "We extracted the descriptive variables of the sample from the toxicology service’s database, which were derived from the standardised clinical assessment of patients with deliberate self poisoning" (p.1). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
High risk of bias | Overall, this trial was rated as high risk of bias as there deviations from the intended intervention that arose because of the trial context that may have affected the outcome. Specifically, a number of participants assigned to the control group received the intervention due to clerical errors. |
| Hassanian‐Moghaddam 2011 | Low risk of bias | "Block randomisation (blocks of 100) was undertaken using a random digit table” (p. 310). Furthermore, "[t]o maintain masking to allocation, randomisation was not revealed to the recruiting toxicologist until all information was entered and eligibility determined" (p.310). The trial authors note that although "...this older form of randomisation is potentially liable to interference...no imbalances at baseline suggest that the randomisation was likely to have been successful" (p.314). |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. However, "[o]ther staff were masked to allocation status during hospital treatment” (p.310). There were no apparent deviations from the intended intervention. "All outcomes were analysed on randomisation status at baseline for 12‐month follow‐up" (p. 311). |
Low risk of bias | Data were available for 91.9% of those randomised. Sensitivity analyses were not undertaken. Data were available for 90.7% of those randomised to the intervention arm, and 93.0% of those randomised to the comparator arm. Additionally, the trial authors report "[there were no significant differences for gender, age, employment status or previous suicide attempt...[and] a small, significant difference for marital status...for missing versus study group respectively" (p.313). |
Some concerns | "Outcomes were determined by direct questions, for example ‘Did you have any self‐mutilation (self‐cutting) during the study period?'" (p.310). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If unblinded personnel were acting as outcome assessors, they may have influenced assessment of the outcome. As the intervention was found to be significant, this is possible, but given the magnitude of the effect size, this is unlikely. |
Some concerns | "All outcomes were analysed on randomisation status at baseline for 12‐month follow‐up" (p.311). All eligible reported results for repetition of SH correspond to all intended outcome. "Outcomes were determined by direct questions..." (p.310). |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Kapur 2013 | Some concerns | "Randomisation was conducted via a remote Internet‐based service (www.sealedenvelope.com)" (p. 73). However, no information on allocation concealment reported. Information on any differences in demographic characteristics and clinical variables between the intervention and control groups at baseline was not reported. |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "Primary analysis was on an intention‐to‐treat basis" (p. 73). |
Low risk of bias | Data were available for 98.5% of those randomised. | Low risk of bias | "We investigated the proportion of patients with at least one repeat episode of self‐harm resulting in hospital attendance...identified from the hospital information systems" (p.73). However, only repeat episodes of self‐harm resulting in presentation to the study hospital were counted. Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "All outcome data were collected by researchers masked to allocation status" (p.73). |
Some concerns | We investigated the proportion of patients with at least one repeat episode of self‐harm resulting in hospital attendance within 12 months" (p.73). All eligible reported results for repetition of SH correspond to all intended outcome. "We investigated the proportion of patients with at least one repeat episode of self‐harm resulting in hospital attendance...identified from the hospital information systems" (p.73). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Subgroup 6.1.2 Postcards (males) | ||||||||||||
| Carter 2005 | Some concerns | "Randomisation was by database (HanDBase, version 2.0, DDH Softwards, FL, USA) on a personal digital assistant (Palm III, Palm, CA, USA) that was populated with a pre‐generated randomisation schedule (in blocks of 10)..." (p. 2). This trial implemented Zelen’s post‐consent method. Therefore, following allocation participants were given the option to change treatment arms. Referring to Table 1 (p.3), there was a lower proportion of females assigned to the intervention as compared to the comparator arm (OR 0.57, 95% CI 0.42 to 0.77). This is unlikely to have been compatible with chance. However, there were no other significant differences between the intervention and comparator arms for any of the other demographic characteristics and clinical variables measured (Table 1, p.3). |
High risk of bias | "We used a randomised consent design, using the single consent version (Zelen’s design). This design is a variation on the standard randomised controlled experimental design, where participants are randomised...before consent is sought" (p.2). Additionally, "...the secretary responsible for managing the mailing database and postcards [was] not blind to allocation status" (p. 4). As clinical personnel knew whether or not a postcard had been sent, they could not have been blinded to allocation status. "Twenty participants in the control group received the intervention due to clerical errors but were included in the control group for the intention to treat analyses" (p.2). The proportion of participants crossing over was modest (6.6%). However, the proportion of participants crossing over was not balanced (i.e., 0% in the intervention arm compared with 6.6% in the comparator arm). "We assessed the outcomes by an intention to treat analysis on the basis of allocation" (p. 2). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "We extracted the descriptive variables of the sample from the toxicology service’s database, which were derived from the standardised clinical assessment of patients with deliberate self poisoning" (p.1). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "...research staff remained blinded to allocation" (p. 2). |
Some concerns | "Main outcome measures [were the p]roportion of patients with one or more repeat episodes of deliberate self poisoning and the number of repeat episodes for deliberate self poisoning per person in 12 months" (p.1). All eligible reported results for repetition of SH correspond to all intended outcome. "We extracted the descriptive variables of the sample from the toxicology service’s database, which were derived from the standardised clinical assessment of patients with deliberate self poisoning" (p.1). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
High risk of bias | Overall, this trial was rated as high risk of bias as there deviations from the intended intervention that arose because of the trial context that may have affected the outcome. Specifically, a number of participants assigned to the control group received the intervention due to clerical errors. |
| Subgroup 6.1.3 Postcards (females) | ||||||||||||
| Carter 2005 | Some concerns | "Randomisation was by database (HanDBase, version 2.0, DDH Softwards, FL, USA) on a personal digital assistant (Palm III, Palm, CA, USA) that was populated with a pre‐generated randomisation schedule (in blocks of 10)..." (p. 2). This trial implemented Zelen’s post‐consent method. Therefore, following allocation participants were given the option to change treatment arms. Referring to Table 1 (p.3), there was a lower proportion of females assigned to the intervention as compared to the comparator arm (OR 0.57, 95% CI 0.42 to 0.77). This is unlikely to have been compatible with chance. However, there were no other significant differences between the intervention and comparator arms for any of the other demographic characteristics and clinical variables measured (Table 1, p.3). |
High risk of bias | "We used a randomised consent design, using the single consent version (Zelen’s design). This design is a variation on the standard randomised controlled experimental design, where participants are randomised...before consent is sought" (p.2). Additionally, "...the secretary responsible for managing the mailing database and postcards [was] not blind to allocation status" (p. 4). As clinical personnel knew whether or not a postcard had been sent, they could not have been blinded to allocation status. "Twenty participants in the control group received the intervention due to clerical errors but were included in the control group for the intention to treat analyses" (p.2). The proportion of participants crossing over was modest (6.6%). However, the proportion of participants crossing over was not balanced (i.e., 0% in the intervention arm compared with 6.6% in the comparator arm). "We assessed the outcomes by an intention to treat analysis on the basis of allocation" (p. 2). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "We extracted the descriptive variables of the sample from the toxicology service’s database, which were derived from the standardised clinical assessment of patients with deliberate self poisoning" (p.1). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "...research staff remained blinded to allocation" (p. 2). |
Some concerns | "Main outcome measures [were the p]roportion of patients with one or more repeat episodes of deliberate self poisoning and the number of repeat episodes for deliberate self poisoning per person in 12 months" (p.1). All eligible reported results for repetition of SH correspond to all intended outcome. "We extracted the descriptive variables of the sample from the toxicology service’s database, which were derived from the standardised clinical assessment of patients with deliberate self poisoning" (p.1). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
High risk of bias | Overall, this trial was rated as high risk of bias as there deviations from the intended intervention that arose because of the trial context that may have affected the outcome. Specifically, a number of participants assigned to the control group received the intervention due to clerical errors. |
Risk of bias for analysis 7.1 Repetition of SH at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Marasinghe 2012 | Some concerns | "The participants were randomly allocated" (p. 152). However, without further specific information on the method used it is difficult to ascertain whether the randomisation sequence was adequate. Additionally, no information on allocation concealment reported. "There were no significant differences between the groups at baseline" (p.152). |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "Intention to treat analyses..." (p.152) |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | No specific information on how repeat self‐harm was ascertained was reported. It is likely that repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "The assessor was blind to the treatment” (p. 152). |
Some concerns | "At six months, an independent assessor repeated the baseline measures with the participants...[a]t the end of 12 months another independent assessor assessed the outcomes" (p.152). All eligible reported results for repetition of SH correspond to all intended outcome. No specific information on how repeat self‐harm was ascertained was reported. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias no specific information on randomistion or allocation concealment was reported. Additionally, no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Wei 2013 | Some concerns | "[P]articipants...were randomly assigned...using a computerized randomization program" (p. 109). However, no information on allocation concealment reported. "The three groups did not significantly differ on age, education, minority race, marriage, sex, occupation, and mental disorder diagnosis" (p.110). |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "All analyses were conducted using the intent‐to‐treat (ITT) principle..." (p.110). |
High risk of bias | Data were available for 72.0% of those randomised. Sensitivity analyses were not undertaken. "...the cumulative dropout rate [at post‐intervention] was 32.9% (n = 27) for the cognitive therapy group, 30.0% (n = 24) for the telephone intervention group, and 20.8% (n = 16) for the control group; the proportion of participants with missed assessment of three groups was not significantly different" (p.110). No other information on causes of missingness reported. |
Some concerns | "...research assessors followed up patients by telephone using measures of a detailed structured questionnaire...[to assess] suicidal history of patients" (p.110). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant blinding could have been convincingly achieved. If clinical personnel were acting as outcome assessors, they may have influenced assessment of the outcome. However, as the intervention was not found to be significant, this is unlikely. |
Some concerns | "At the 3 months, 6 months, and 12 months postbaseline assessments, the research assessors followed up patients..." (p.110). All eligible reported results for repetition of SH correspond to all intended outcome. "...research assessors followed up patients by telephone using measures of a detailed structured questionnaire...[to assess] suicidal history of patients" (p.110). All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
High risk of bias | Overall, this trial was rated as some concerns for risk of bias as missingness in the outcome could have depended on its true value and analyses did not correct for bias, nor were sensitivity analyses undertaken to investigate the potential effect of missing data. |
Risk of bias for analysis 8.1 Repetition of SH at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Amadéo 2015 | Some concerns | "A sequence based on a random procedure (block randomization) was used to assign all enrolled subjects" (p.49). However, detail on the randomisaton method was not reported. Additionally, no information on allocation concealment reported. "Over half of subjects in the [intervention] group had a diagnosis of mood disorder. A large proportion of cases (63% in the [intervention], 72% in [control] group) had previous history of suicidal behaviors before the index episode" (p.49). These differences may have been compatible with chance. |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant or clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. Analyses were made "...using intention to treat approach" (p.52). |
Low risk of bias | Data were available for 95.0% of those randomised. | Low risk of bias | Repetition of SH was ascertained from "several self‐report scales" (p.49). "Additional information from the hospital emergency department was obtained because participants may fail to report new episodes of non‐fatal suicidal behavior" (p.49). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. No specific information on whether outcome assessors were aware of participants' treatment allocation was reported. Repetition of SH as determined by clinical and hospital records represents an observer‐reported outcome. |
Some concerns | "This randomized controlled trial used number of suicides and repeated non‐fatal suicidal behavior (NFSB), as primary outcome measures [at 18 months]" (p.49). Repetition of self‐harm was ascertained from participant self‐report. All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as at some concerns for risk of bias as no specific information on randomisation or allocation concealment was reported. Additionally, no specific information was reported as to whether the data that produced this result analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis. |
| Fleischmann 2008 | Low risk of bias | "An allocation sequence based on a random‐number table was used to randomly assign all enrolled subjects....the allocation sequence was maintained in a separate location to prevent...bias" (p. 704). "No differences in the sociodemographic variables and items related to the current attempt between the TAU and [intervention] groups were found among the subjects analysed" (p.705). |
Some concerns | "The subjects were blinded as to their assignment" (p. 704). No information was reported on clinical personnel blinding, however, given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. There was no information as to whether intention‐to‐treat analyses had been conducted. Subsequent analyses appear to be based on those participants with available information suggesting modified intention to treat analyses were used. |
High risk of bias | Data were available for 89.1% of those randomised (by the 18‐month assessment). Sensitivity analyses were not undertaken. Data were available for 93.6% of those randomised to the intervention arm, and 84.6% of those randomised to the comparator arm. However, the authors do note that "[n]o subjects at all were lost during follow‐up in Yuncheng; 3%, 4%, 11%, and 15% were lost at the final follow‐up in Campinas, Karaj, Colombo, and Chennai respectively" (p.705), suggesting there may have also been regional differences. |
Low risk of bias | "The questionnaire for the comprehensive assessment of all suicide attempters enrolled was commonly applied across all sites, translated into the local language of each site, adapted to take into account cultural specificities, and pilot‐tested to assess face and content validity. It was largely based on the European Parasuicide Study Interview Schedule (EPSIS), which had been applied in the WHO/EURO Multicentre Study on Suicidal Behaviour" (p.705). However, previous work has demonstrated that self‐harm prevalence estimates derived from self‐report may be underestimated, and supplementing prevalence estimates with medical or clinical record information is advisable (Mars 2016). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "The subjects were blinded as to their assignment" (p. 704). |
Some concerns | "The primary study outcome measurement was...at 18‐month follow‐up" (p.703). All eligible reported results for repetition of SH correspond to all intended outcome. Repetition of self‐harm was ascertained from participant self‐report. All eligible reported results for repetition of SH correspond to all intended analyses of the data. |
High risk of bias | Overall, this trial was rated as high risk of bias as missingness in the outcome likely depended on its true value and analyses did not correct for bias, nor were sensitivity analyses undertaken to investigate the potential effect of missing data. |
Risk of bias for analysis 9.1 Repetition of SH at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 9.1.1 Whole sample | ||||||||||||
| Gysin‐Maillart 2016 | Low risk of bias | "Simple randomization was carried out using shuffled unmarked sealed envelopes. Similar to a modified Zelen design...participants were contacted following randomization and informed that they had been allocated to one of the two groups...Written informed consent was obtained from participants of both groups after detailed description of the study" (p.3). Referring to Table 1 (p.9), those assigned to the intervention arm were less likely to have engaged in multiple episodes of SH (i.e., ≥1) (OR 0.58, 95% CI 0.28 to 1.20) but had attended a greater number of outpatient treatment sessions in the six months preceding trial entry (i.e., 8 versus 2.5, p<0.01). This is may have been compatible with chance. |
Low risk of bias | Given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that participant and clinical personnel blinding could have been convincingly achieved. Referring back to the trial protocol (NCT02505373), there was no apparent deviation from the intended intervention. "Analysis was conducted on the intention‐to‐treat (ITT) population to ensure unbiased comparisons between the two groups and to address concerns regarding withdrawal and noncompliance. To address the issue of missing data, multiple imputations by chained equations were implemented" (p.6). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "The questions related to suicidal behavior and self‐harm were as follows: (1) 'Did you in the past 6 months try to take your own life?'; (2) 'How often did you in the past 6 months have thoughts about taking your own life?'; and (3) 'How often did you in the past 6 months physically harm yourself (e.g., cutting, burning, hitting)?'...we [also] searched hospital records and contacted the responsible general practitioners and therapists to check for suicide attempts..." (p.6). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. This was an open label trial. Self‐reported repetition of self‐harm was supplemented with clinical and hospital records which represents an observer‐reported outcome. |
Low risk of bias | Referring back to the trial protocol (NCT02505373), there were no apparent departures from the analysis plan. Referring back to the trial protocol (NCT02505373), all eligible reported results for repetition of SH correspond to all intended outcome measurements. Referring back to the trial protocol (NCT02505373), all eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Low risk of bias | Overall, this trial was rated as at low risk of bias as all domains were rated as at low risk of bias. |
| Hatcher 2015 | Low risk of bias | "All eligible participants were allocated randomly to the intervention or usual care groups using a central computerised randomisation system at the Clinical Trials Research Unit (subsequently the National Institute for Health Innovation)...Stratified minimisation randomization was used to ensure a balance in key prognostic factors between the study groups" (p.231). This trial implemented Zelen’s post‐consent method. Therefore, following allocation participants were given the option to change treatment arms. "There were no significant differences between those allocated to the two groups who provided consent to be in the study" (p.232). |
Low risk of bias | As this trial implemented Zelen’s post‐consent method, participants were given the option to change treatment arms following allocation.Therefore, participants cannot have been blind to treatment allocation. Additionally, given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "Analysis of the primary outcome was in everyone who was randomised..." (p.232). "Analysis of the primary outcome was in everyone who was randomised... The secondary outcomes were analysed only in those people who had consented to be in the study” |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "The primary outcome measure was re‐presentation to any hospital in New Zealand for self‐harm...This was assessed by interrogating district health board electronic systems and Ministry Of Health Information Directorate data" (p.230). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "The research assistants were masked to treatment allocation" (p.231). |
Low risk of bias | Referring back to the trial protocol (ACTRN12609000641291), there were no apparent departures from the analysis plan. Referring back to the trial protocol (ACTRN12609000641291), all eligible reported results for repetition of SH correspond to all intended outcome measurements. Referring back to the trial protocol (ACTRN12609000641291), all eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Low risk of bias | Overall, this trial was rated as at low risk of bias as all domains were rated as at low risk of bias. |
| Hatcher 2016 | Some concerns | "All eligible participants were allocated randomly to the intervention or usual care groups using a central computerised randomization system at the Clinical Trials Research Unit (subsequently the National Institute for Health Innovation)...Stratified minimisation randomization was used to ensure a balance in key prognostic factors..." (p.888). This trial implemented Zelen’s post‐consent method. Therefore, following allocation participants were given the option to change treatment arms. "Comparing participants who consented there were no significant differences between those randomised to the intervention and control groups except for the Beck Hopelessness Scores which were significantly lower in the controls [MD ‐3.00, 95% CI ‐5.19 to ‐1.41]" (p.888). This is unlikely to have been compatible with chance. |
Low risk of bias | As this trial implemented Zelen’s post‐consent method, participants were given the option to change treatment arms following allocation.Therefore, participants cannot have been blind to treatment allocation. Additionally, "the introduction to the study differed depending on which arm of the trial [the participant was] randomised to" (p.3, unpublished manuscript). Given the difference in therapeutic intensity between the intervention and comparator arms, it is also unlikely that clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "The intention to treat analyses consisted of all patients that were randomized..." (p.892). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | Repetition of self‐harm was ascertained from "a review of DHB records; and by using the National Minimum Dataset from the Ministry of Health Information Directory to record hospital contacts...[and t]he National Minimum Dataset [which] contains routinely collected information on all hospital discharges in New Zealand linked to a patient’s individual National Health Index number" (pp.887‐8). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "The research assistants were blind to treatment allocation" (p.888). |
Low risk of bias | Referring back to the trial protocol (ACTRN12609000952246), there were no apparent departures from the analysis plan. Referring back to the trial protocol (ACTRN12609000952246), all eligible reported results for repetition of SH correspond to all intended outcome measurements. Referring back to the trial protocol (ACTRN12609000952246), all eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as some concerns for risk of bias as there was a higher severity of hopelessness at baseline amongst those allocated to the comparator arm, suggesting there may have been a problem with the randomisation process. |
| Subgroup 9.1.2 First SH episode | ||||||||||||
| Hatcher 2015 | Low risk of bias | "All eligible participants were allocated randomly to the intervention or usual care groups using a central computerised randomisation system at the Clinical Trials Research Unit (subsequently the National Institute for Health Innovation)...Stratified minimisation randomization was used to ensure a balance in key prognostic factors between the study groups" (p.231). This trial implemented Zelen’s post‐consent method. Therefore, following allocation participants were given the option to change treatment arms. "There were no significant differences between those allocated to the two groups who provided consent to be in the study" (p.232). |
Low risk of bias | As this trial implemented Zelen’s post‐consent method, participants were given the option to change treatment arms following allocation.Therefore, participants cannot have been blind to treatment allocation. Additionally, given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "Analysis of the primary outcome was in everyone who was randomised..." (p.232). "Analysis of the primary outcome was in everyone who was randomised... The secondary outcomes were analysed only in those people who had consented to be in the study” |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "The primary outcome measure was re‐presentation to any hospital in New Zealand for self‐harm...This was assessed by interrogating district health board electronic systems and Ministry Of Health Information Directorate data" (p.230). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "The research assistants were masked to treatment allocation" (p.231). |
Low risk of bias | Referring back to the trial protocol (ACTRN12609000641291), there were no apparent departures from the analysis plan. Referring back to the trial protocol (ACTRN12609000641291), all eligible reported results for repetition of SH correspond to all intended outcome measurements. Referring back to the trial protocol (ACTRN12609000641291), all eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Low risk of bias | Overall, this trial was rated as at low risk of bias as all domains were rated as at low risk of bias. |
| Hatcher 2016 | Some concerns | "All eligible participants were allocated randomly to the intervention or usual care groups using a central computerised randomization system at the Clinical Trials Research Unit (subsequently the National Institute for Health Innovation)...Stratified minimisation randomization was used to ensure a balance in key prognostic factors..." (p.888). This trial implemented Zelen’s post‐consent method. Therefore, following allocation participants were given the option to change treatment arms. "Comparing participants who consented there were no significant differences between those randomised to the intervention and control groups except for the Beck Hopelessness Scores which were significantly lower in the controls [MD ‐3.00, 95% CI ‐5.19 to ‐1.41]" (p.888). This is unlikely to have been compatible with chance. |
Low risk of bias | As this trial implemented Zelen’s post‐consent method, participants were given the option to change treatment arms following allocation.Therefore, participants cannot have been blind to treatment allocation. Additionally, "the introduction to the study differed depending on which arm of the trial [the participant was] randomised to" (p.3, unpublished manuscript). Given the difference in therapeutic intensity between the intervention and comparator arms, it is also unlikely that clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "The intention to treat analyses consisted of all patients that were randomized..." (p.892). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | Repetition of self‐harm was ascertained from "a review of DHB records; and by using the National Minimum Dataset from the Ministry of Health Information Directory to record hospital contacts...[and t]he National Minimum Dataset [which] contains routinely collected information on all hospital discharges in New Zealand linked to a patient’s individual National Health Index number" (pp.887‐8). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "The research assistants were blind to treatment allocation" (p.888). |
Low risk of bias | Referring back to the trial protocol (ACTRN12609000952246), there were no apparent departures from the analysis plan. Referring back to the trial protocol (ACTRN12609000952246), all eligible reported results for repetition of SH correspond to all intended outcome measurements. Referring back to the trial protocol (ACTRN12609000952246), all eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as some concerns for risk of bias as there was a higher severity of hopelessness at baseline amongst those allocated to the comparator arm, suggesting there may have been a problem with the randomisation process. |
| Subgroup 9.1.3 Repeat SH episode | ||||||||||||
| Hatcher 2015 | Low risk of bias | "All eligible participants were allocated randomly to the intervention or usual care groups using a central computerised randomisation system at the Clinical Trials Research Unit (subsequently the National Institute for Health Innovation)...Stratified minimisation randomization was used to ensure a balance in key prognostic factors between the study groups" (p.231). This trial implemented Zelen’s post‐consent method. Therefore, following allocation participants were given the option to change treatment arms. "There were no significant differences between those allocated to the two groups who provided consent to be in the study" (p.232). |
Low risk of bias | As this trial implemented Zelen’s post‐consent method, participants were given the option to change treatment arms following allocation.Therefore, participants cannot have been blind to treatment allocation. Additionally, given the difference in therapeutic intensity between the intervention and comparator arms, it is unlikely that clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "Analysis of the primary outcome was in everyone who was randomised..." (p.232). "Analysis of the primary outcome was in everyone who was randomised... The secondary outcomes were analysed only in those people who had consented to be in the study” |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | "The primary outcome measure was re‐presentation to any hospital in New Zealand for self‐harm...This was assessed by interrogating district health board electronic systems and Ministry Of Health Information Directorate data" (p.230). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "The research assistants were masked to treatment allocation" (p.231). |
Low risk of bias | Referring back to the trial protocol (ACTRN12609000641291), there were no apparent departures from the analysis plan. Referring back to the trial protocol (ACTRN12609000641291), all eligible reported results for repetition of SH correspond to all intended outcome measurements. Referring back to the trial protocol (ACTRN12609000641291), all eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Low risk of bias | Overall, this trial was rated as at low risk of bias as all domains were rated as at low risk of bias. |
| Hatcher 2016 | Some concerns | "All eligible participants were allocated randomly to the intervention or usual care groups using a central computerised randomization system at the Clinical Trials Research Unit (subsequently the National Institute for Health Innovation)...Stratified minimisation randomization was used to ensure a balance in key prognostic factors..." (p.888). This trial implemented Zelen’s post‐consent method. Therefore, following allocation participants were given the option to change treatment arms. "Comparing participants who consented there were no significant differences between those randomised to the intervention and control groups except for the Beck Hopelessness Scores which were significantly lower in the controls [MD ‐3.00, 95% CI ‐5.19 to ‐1.41]" (p.888). This is unlikely to have been compatible with chance. |
Low risk of bias | As this trial implemented Zelen’s post‐consent method, participants were given the option to change treatment arms following allocation.Therefore, participants cannot have been blind to treatment allocation. Additionally, "the introduction to the study differed depending on which arm of the trial [the participant was] randomised to" (p.3, unpublished manuscript). Given the difference in therapeutic intensity between the intervention and comparator arms, it is also unlikely that clinical personnel blinding could have been convincingly achieved. There were no apparent deviations from the intended intervention. "The intention to treat analyses consisted of all patients that were randomized..." (p.892). |
Low risk of bias | Data were available for 100% of those randomised. | Low risk of bias | Repetition of self‐harm was ascertained from "a review of DHB records; and by using the National Minimum Dataset from the Ministry of Health Information Directory to record hospital contacts...[and t]he National Minimum Dataset [which] contains routinely collected information on all hospital discharges in New Zealand linked to a patient’s individual National Health Index number" (pp.887‐8). Repetition of self‐harm was ascertained in the same way between the intervention and comparator arms in this trial. "The research assistants were blind to treatment allocation" (p.888). |
Low risk of bias | Referring back to the trial protocol (ACTRN12609000952246), there were no apparent departures from the analysis plan. Referring back to the trial protocol (ACTRN12609000952246), all eligible reported results for repetition of SH correspond to all intended outcome measurements. Referring back to the trial protocol (ACTRN12609000952246), all eligible reported results for repetition of SH correspond to all intended analyses of the data. |
Some concerns | Overall, this trial was rated as some concerns for risk of bias as there was a higher severity of hopelessness at baseline amongst those allocated to the comparator arm, suggesting there may have been a problem with the randomisation process. |
Acknowledgements
The authors thank the following trial authors for providing us with unpublished data: Anthony Bateman, Ryan Barnhart, Kirsten Barnicot, Annette Beautrais, Ram Pratap Beniwal, Olive Bennewith, Greg Carter, Marie Cedereke, Tom Clarke, Mike Crawford, Kate Davidson, Elspeth Guthrie, Tony Fitzgerald, Alexandra Fleischmann, Peter Fonagy, Kim Gratz, Anja Gysin‐Maillart, Melanie Harned, Simon Hatcher, Nusrat Husain, Nav Kapur, Chiaki Kawanishi, Marsha Linehan, Rohana Marasinghe, Shelley McMain, David Owens, Stefan Priebe, Simon Schwab, Nadja Slee, Priya Sreedaran, Carmen Stewart, Vojna Tapolaa, Barbara Tomenson, Peter Tyrer, Guillaume Vaiva, Lakshmi Vijayakumar, Carla Walton, August Wang, Igor Weinberg, and Dong Xu.
The authors and the CCMD Editorial Team are also grateful to the following peer reviewers for their time and comments: Kerry Dwan, Sarah Fortune, Nick Meader and Jean Sellar‐Edmunds. They would also like to thank Cochrane Copy Edit Support for the team's help and Phil Roberts from the University of York for graphic design support in the production of Figure 2 and 3.
This project was previously supported by the National Co‐ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO). KH is funded by Oxford Health NHS Foundation Trust. He is a National Institute for Health Research (NIHR) Senior Investigator, and personal funding from NIHR helped support this update.
The NIHR is the largest single funder of the CCMD Group.
The views expressed are those of the authors, and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
Appendices
Appendix 1. Cochrane Common Mental Disorders Specialised Register
The Cochrane Common Mental Disorders Group (CCMD) maintains an archived controlled trials register known as the CCMDCTR. This specialised register contains over 40,000 reference records (reports of RCTs) for anxiety disorders, depression, bipolar disorder, eating disorders, self‐harm, and other mental disorders within the scope of this Group. The CCMDCTR is a partially studies‐based register with more than 50% of reference records tagged to around 12,500 individually PICO‐coded study records. Reports of studies for inclusion in the register were collated from (weekly) generic searches of key bibliographic databases to June 2016, which included: MEDLINE (1950 onwards), Embase (1974 onwards), PsycINFO (1967 onwards), quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), and review‐specific searches of additional databases. Reports of studies were also sourced from international trials registries, drug companies, the handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses. Details of CCMD's core search strategies (used to identify RCTs) are on the Group's website, with an example of the core MEDLINE search displayed below.
[MeSH Headings]: eating disorders/ or anorexia nervosa/ or binge‐eating disorder/ or bulimia nervosa/ or female athlete triad syndrome/ or pica/ or hyperphagia/ or bulimia/ or self‐injurious behavior/ or self mutilation/ or suicide/ or suicidal ideation/ or suicide, attempted/ or mood disorders/ or affective disorders, psychotic/ or bipolar disorder/ or cyclothymic disorder/ or depressive disorder/ or depression, postpartum/ or depressive disorder, major/ or depressive disorder, treatment‐resistant/ or dysthymic disorder/ or seasonal affective disorder/ or neurotic disorders/ or depression/ or adjustment disorders/ or exp antidepressive agents/ or anxiety disorders/ or agoraphobia/ or neurocirculatory asthenia/ or obsessive‐compulsive disorder/ or obsessive hoarding/ or panic disorder/ or phobic disorders/ or stress disorders, traumatic/ or combat disorders/ or stress disorders, post‐traumatic/ or stress disorders, traumatic, acute/ or anxiety/ or anxiety, castration/ or koro/ or anxiety, separation/ or panic/ or exp anti‐anxiety agents/ or somatoform disorders/ or body dysmorphic disorders/ or conversion disorder/ or hypochondriasis/ or neurasthenia/ or hysteria/ or munchausen syndrome by proxy/ or munchausen syndrome/ or fatigue syndrome, chronic/ or obsessive behavior/ or compulsive behavior/ or behavior, addictive/ or impulse control disorders/ or firesetting behavior/ or gambling/ or trichotillomania/ or stress, psychological/ or burnout, professional/ or sexual dysfunctions, psychological/ or vaginismus/ or Anhedonia/ or Affective Symptoms/ or *Mental Disorders/ OR [Title/ Author Keywords]: (eating disorder* or anorexia nervosa or bulimi* or binge eat* or (self adj (injur* or mutilat*)) or suicide* or suicidal or parasuicid* or mood disorder* or affective disorder* or bipolar i or bipolar ii or (bipolar and (affective or disorder*)) or mania or manic or cyclothymic* or depression or depressive or dysthymi* or neurotic or neurosis or adjustment disorder* or antidepress* or anxiety disorder* or agoraphobia or obsess* or compulsi* or panic or phobi* or ptsd or posttrauma* or post trauma* or combat or somatoform or somati#ation or medical* unexplained or body dysmorphi* or conversion disorder or hypochondria* or neurastheni* or hysteria or munchausen or chronic fatigue* or gambling or trichotillomania or vaginismus or anhedoni* or affective symptoms or mental disorder* or mental health).tw,kf. AND [RCT filter]: (controlled clinical trial.pt. or randomised controlled trial.pt. or (randomi#ed or randomi#ation).ab,ti. or randomly.ab. or (random* adj3 (administ* or allocat* or assign* or class* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*)).ab. or placebo*.ab,ti. or drug therapy.fs. or trial.ab,ti. or groups.ab. or (control* adj3 (trial* or study or studies)).ab,ti. or ((singl* or doubl* or tripl* or trebl*) adj3 (blind* or mask* or dummy*)).mp. or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or randomised controlled trial/ or pragmatic clinical trial/ or (quasi adj (experimental or random*)).ti,ab. or ((waitlist* or wait* list* or treatment as usual or TAU) adj3 (control or group)).ab.)
Records were screened for reports of RCTs within the scope of the Cochrane Common Mental Disorders Group. Secondary reports of RCTs were tagged to the appropriate study record
An information specialist with CCMD will cross‐search the CCMDCTR‐Studies and References register using the following terms (all fields):
(suicid* or parasuicid* or "auto mutilat*" or automutilat* or "self destruct*" or selfdestruct* or self‐harm* or selfharm* or "self immolat*" or selfimmolat* or "self inflict*" or selfinflict* or "self injur*" or selfinjur* or selfmutilat* or "self mutilat*" or "self poison*" or selfpoison* or (self adj2 (cut or cuts or cutting or cutter? or burn or burns or burning or bite or bites or biting or hit or hits or hitting)) or "head bang*" or headbang* or "over dose*" or overdos* or NSSI* or nonsuicid* or non‐suicid*) (2015‐June‐2016) n = 29
Appendix 2. MEDLINE, Embase, PsycINFO Ovid search strategy
An information specialist with CCMD searched the main biomedical databases using the terms listed below from January 2015 to 4‐July‐2020. [N.B. CCMDCTR is current to June 2016 only]
Search summary
Date‐of‐search: 4‐July‐2020
Cochrane Library (CDSR) Systematic Reviews, n = 38
Cochrane Library (CDSR) Protocols, n = 12
Cochrane Library CENTRAL, n = 2727
Cochrane Specialised Register (CCMDCTR), n = 291
Ovid MEDLINE, PsycINFO (cross‐search), n = 2743
Ovid Embase (precise), n = 1375
Total = 7186 Duplicates removed, n = 2483 To screen, n = 4703 [Cochrane Library CENTRAL‐Trial Register Records (removed) n = 1969] Cochrane Library (Issue 7 of 12, 2020) [Date limited, 2015 onwards] #1 MeSH descriptor: [Self‐Injurious Behavior] explode all trees #2 (overdose* and prevent*):kw or (overdos* near/3 prevent*):ti,ab #3 ((nonfatal or non‐fatal) near/2 (overdose* or over dose*)):ti,ab,kw #4 (NSSI* or ((nonsuicid* or non‐suicid*) near/2 (self* or injur*))):ti,ab #5 (suicid* or parasuicid* or (auto next mutilat*) or automutilat* or (self next destruct*) or selfdestruct* or self‐harm* or selfharm* or (self next harm*) or (self next immolat*) or selfimmolat* or (self next inflict*) or selfinflict* or (self next injur*) or selfinjur* or selfmutilat* or (self next mutilat*) or (self next poison*) or selfpoison* or (self near/2 (cut or cuts or cutting or cutter* or burn or burns or burning or bite or bites or biting or hit or hits or hitting)) or (head next bang*) or headbang*):ti,ab,kw #6 (#1 or #2 or #3 or #4 or #5) Limited 2015 to date CDSR‐reviews (38); CDSR‐protocols (12); CENTRAL (2727); CENTRAL‐TR (1969) *************************** PsycINFO/MEDLINE cross‐search
Ovid APA PsycInfo <1806 to June Week 5 2020>, Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations and Daily <1946 to July 02, 2020> [Date limited, 2015 onwards] Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 Automutilation/ or Self‐injurious Behavior/ or Self‐destructive Behavior/ or Self‐mutilation/ or Self‐inflicted Wounds/ (19601) 2 Suicidal Behavior/ or Suicide/ or Suicidal Ideation/ or Attempted Suicide/ or Suicide, Attempted/ or Self Poisoning/ or Suicide Prevention/ or Suicide Prevention Centers/ or Suicidology/ (97875) 3 (suicid* or parasuicid* or auto mutilat* or automutilat* or self destruct* or selfdestruct* or self‐harm* or selfharm* or self immolat* or selfimmolat* or self inflict* or selfinflict* or self injur* or selfinjur* or selfmutilat* or self mutilat* or self poison* or selfpoison* or (self adj2 (cut or cuts or cutting or cutter? or burn or burns or burning or bite or bites or biting or hit or hits or hitting)) or head bang* or headbang*).ti,ab,kf,kw,id. (164244) 4 (NSSI? or ((nonsuicid* or non‐suicid*) adj2 (self* or injur*))).ti,ab,kf,kw,id. (3469) 5 (Overdose/ or Drug Overdose/ or Drug Overdoses/) and prevent*.af. (3529) 6 ((nonfatal or non‐fatal) adj2 (overdose? or over dose?)).mp. (571) 7 or/1‐6 (183505) 8 Randomized Controlled Trial/ (509272) 9 Randomized Controlled Trial.pt. (508805) 10 Randomization/ (103117) 11 Random Allocation/ (103117) 12 Controlled Clinical Trial/ (93744) 13 Controlled Clinical Trial.pt. (93744) 14 Double‐blind Method/ or Single‐blind Method/ (186347) 15 (randomi#ed or randomi#ation or randomi#ing).ti,ab,kf,kw,id. (726423) 16 (RCT or "at random" or (random* adj3 (administ* or allocat* or assign* or class* or cluster or crossover or cross‐over or control* or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic or quasi or recruit* or split or subsitut* or treat*))).ti,ab,kf,kw,id. (667814) 17 trial.ti. (251482) 18 placebo/ or (placebo and (allocat* or assign* or control* or group*)).ti,ab,kf,kw,id. (204672) 19 (control* adj3 group*).ab. (634930) 20 (control* and (trial or study or group*) and (waitlist* or wait* list* or ((treatment or care) adj2 usual))).ti,ab,kf,kw,id. (32182) 21 ((single or double or triple or treble) adj2 (blind* or mask* or dummy)).ti,ab,kf,kw,id. (200109) 22 treatment effectiveness evaluation/ (24511) 23 or/8‐22 (1833008) 24 7 and 23 (9906) 25 (2015* or 2016* or 2017* or 2018* or 2019* or 2020*).yr,dc,dp,dt,ep,ez. (7909383) 26 24 and 25 (3732) 27 remove duplicates from 26 (2743) *************************** Ovid Embase <1974 to 2020 Week 26> [Date limited, 2015 onwards] Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 Automutilation/ (17795) 2 suicidal behavior/ or self immolation/ or self poisoning/ or suicidal ideation/ or suicide/ or suicide attempt/ (101066) 3 Drug Overdose/ and prevent*.af. (4897) 4 (suicid* or parasuicid* or auto mutilat* or automutilat* or self destruct* or selfdestruct* or self‐harm* or selfharm* or self immolat* or selfimmolat* or self inflict* or selfinflict* or self injur* or selfinjur* or selfmutilat* or self mutilat* or self poison* or selfpoison* or (self adj2 (cut or cuts or cutting or cutter? or burn or burns or burning or bite or bites or biting or hit or hits or hitting)) or head bang* or headbang*).ti,kw. (62383) 5 (NSSI? or ((nonsuicid* or non‐suicid*) adj2 (self* or injur*))).ti,ab,kw. (1786) 6 ((nonfatal or non‐fatal) adj2 (overdose? or over dose?)).mp. (418) 7 or/1‐6 (125188) 8 randomized controlled trial/ (608057) 9 randomization.de. (87068) 10 controlled clinical trial/ and (Disease Management or Drug Therapy or Prevention or Rehabilitation or Therapy).fs. (253859) 11 *clinical trial/ (17606) 12 placebo.de. (351476) 13 placebo.ti,ab. (307193) 14 trial.ti. (301646) 15 (randomi#ed or randomi#ation or randomi#ing).ti,ab,kw. (917476) 16 (RCT or "at random" or (random* adj3 (administ* or allocat* or assign* or class* or cluster or control* or crossover or cross‐over or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic or quasi or recruit* or split or subsitut* or treat*))).ti,ab,kw. (769731) 17 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. (309225) 18 (control* and (study or group?) and (waitlist* or wait* list* or ((treatment or care) adj2 usual))).ti,ab,kw,hw. (39665) 19 or/8‐18 (1732296) 20 ((animal or nonhuman) not (human and (animal or nonhuman))).de. (5683745) 21 19 not 20 (1575127) 22 7 and 21 (8502) 23 (2015* or 2016* or 2017* or 2018* or 2019* or 2020*).yr,dc,dp. (9329153) 24 22 and 23 (3277) 25 limit 24 to exclude medline journals (353) 26 *Automutilation/ (7770) 27 *suicidal behavior/ or *self immolation/ or *self poisoning/ or *suicidal ideation/ or *suicide/ or *suicide attempt/ (49956) 28 *Drug Overdose/ and prevent*.af. (984) 29 4 or 5 or 6 or 26 or 27 or 28 (72349) 30 21 and 29 (2692) 31 23 and 30 (1132) 32 25 or 31 (1375) ***************************
Data and analyses
Comparison 1. CBT‐based psychotherapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Repetition of SH at post‐intervention | 4 | 238 | Odds Ratio (M‐H, Random, 95% CI) | 0.35 [0.12, 1.02] |
| 1.2 Repetition of SH at six months | 12 | 1260 | Odds Ratio (M‐H, Random, 95% CI) | 0.52 [0.38, 0.70] |
| 1.3 Repetition of SH at 12 months | 9 | 2458 | Odds Ratio (M‐H, Random, 95% CI) | 0.81 [0.66, 0.99] |
| 1.4 Repetition of SH at 24 months | 2 | 105 | Odds Ratio (M‐H, Random, 95% CI) | 0.31 [0.14, 0.69] |
| 1.5 Frequency of SH at post‐intervention | 4 | 149 | Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.67, 0.61] |
| 1.6 Frequency of SH at six months | 4 | 118 | Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.32, ‐0.11] |
| 1.7 Time to SH repetition | 3 | Hazard Ratio (IV, Random, 95% CI) | 0.81 [0.61, 1.08] | |
| 1.8 Depression scores at post‐intervention | 5 | 953 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.54, ‐0.02] |
| 1.9 Depression scores at six months | 8 | 934 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.50, 0.01] |
| 1.10 Depression scores at 12 months | 7 | 1130 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.64, ‐0.07] |
| 1.11 Depression scores at 24 months | 2 | 225 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.48, 0.05] |
| 1.12 Hopelessness scores at post‐intervention | 5 | 803 | Mean Difference (IV, Random, 95% CI) | ‐2.99 [‐3.91, ‐2.07] |
| 1.13 Hopelessness scores at six months | 2 | 315 | Mean Difference (IV, Random, 95% CI) | ‐3.14 [‐4.78, ‐1.49] |
| 1.14 Hopelessness scores at 12 months | 3 | 539 | Mean Difference (IV, Random, 95% CI) | ‐1.89 [‐2.97, ‐0.81] |
| 1.15 Suicidal ideation scores at post‐intervention | 5 | 718 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.68, ‐0.28] |
| 1.16 Suicidal ideation scores at six months | 4 | 353 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.60, ‐0.17] |
| 1.17 Proportion reporting suicidal ideation | 2 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.17.1 Post‐intervention | 2 | 219 | Odds Ratio (M‐H, Random, 95% CI) | 0.44 [0.08, 2.26] |
| 1.17.2 Six months | 1 | 159 | Odds Ratio (M‐H, Random, 95% CI) | 1.27 [0.66, 2.46] |
| 1.17.3 12 months | 1 | 159 | Odds Ratio (M‐H, Random, 95% CI) | 1.20 [0.62, 2.31] |
| 1.18 Suicide deaths by final follow‐up | 16 | 2130 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.34, 1.80] |
| 1.19 Repetition of SH at 12 months (by repeater status) | 2 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.19.1 History of prior SH | 2 | 508 | Odds Ratio (M‐H, Random, 95% CI) | 0.56 [0.36, 0.88] |
| 1.19.2 No history of prior SH | 2 | 733 | Odds Ratio (M‐H, Random, 95% CI) | 1.10 [0.48, 2.52] |
Comparison 2. DBT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Repetition of SH by post‐intervention | 6 | 502 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.32, 1.55] |
| 2.1.1 Comparator: TAU | 3 | 267 | Odds Ratio (M‐H, Random, 95% CI) | 0.59 [0.16, 2.15] |
| 2.1.2 Comparator: Alternative psychotherapy | 3 | 235 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.16, 2.78] |
| 2.2 Repetition of SH by 12 months | 3 | 269 | Odds Ratio (M‐H, Random, 95% CI) | 0.65 [0.24, 1.72] |
| 2.2.1 Comparator: TAU | 2 | 172 | Odds Ratio (M‐H, Random, 95% CI) | 0.36 [0.05, 2.47] |
| 2.2.2 Comparator: Alternative psychotherapy | 1 | 97 | Odds Ratio (M‐H, Random, 95% CI) | 1.18 [0.35, 3.95] |
| 2.3 Frequency of SH by post‐intervention | 7 | 659 | Mean Difference (IV, Random, 95% CI) | ‐5.00 [‐8.92, ‐1.08] |
| 2.3.1 Comparator: TAU | 4 | 376 | Mean Difference (IV, Random, 95% CI) | ‐10.09 [‐21.57, 1.40] |
| 2.3.2 Comparator: Alternative psychotherapy | 3 | 283 | Mean Difference (IV, Random, 95% CI) | ‐5.00 [‐7.91, ‐2.09] |
| 2.4 Treatment adherence: Proportion completing treatment | 4 | 467 | Odds Ratio (M‐H, Random, 95% CI) | 1.40 [0.73, 2.67] |
| 2.4.1 Comparator: TAU | 1 | 180 | Odds Ratio (M‐H, Random, 95% CI) | 0.95 [0.52, 1.74] |
| 2.4.2 Comparator: Alternative psychotherapy | 3 | 287 | Odds Ratio (M‐H, Random, 95% CI) | 1.79 [0.65, 4.89] |
| 2.5 Depression scores by post‐intervention | 6 | 557 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.58, ‐0.17] |
| 2.5.1 Comparator: TAU | 3 | 282 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.50, ‐0.03] |
| 2.5.2 Comparator: Alternative psychotherapy | 3 | 275 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.85, ‐0.14] |
| 2.6 Suicidal ideation scores by post‐intervention | 3 | 194 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.64, 0.02] |
| 2.6.1 Comparator: TAU | 1 | 81 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.78, 0.10] |
| 2.6.2 Comparator: Alternative psychotherapy | 2 | 113 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐1.11, 0.31] |
| 2.7 Suicide deaths by post‐intervention | 5 | 563 | Odds Ratio (M‐H, Random, 95% CI) | 3.00 [0.12, 76.49] |
| 2.7.1 Comparator: TAU | 4 | 401 | Odds Ratio (M‐H, Random, 95% CI) | 3.00 [0.12, 76.49] |
| 2.7.2 Comparator: Alternative psychotherapy | 1 | 162 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.8 Suicide deaths by 12 months | 2 | 254 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.8.1 Comparator: TAU | 2 | 254 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.8.2 Comparator: Alternative psychotherapy | 0 | 0 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.9 Suicide deaths by 24 months | 2 | 254 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.9.1 Comparator: TAU | 2 | 254 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.9.2 Comparator: Alternative psychotherapy | 0 | 0 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
Comparison 3. Group‐based emotion‐regulation psychotherapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Repetition of SH at post‐intervention | 2 | 83 | Odds Ratio (M‐H, Random, 95% CI) | 0.34 [0.13, 0.88] |
| 3.2 Frequency of repetition of SH at post‐intervention | 2 | 83 | Mean Difference (IV, Random, 95% CI) | ‐12.76 [‐34.92, 9.40] |
| 3.3 Depression scores at post‐intervention | 2 | 83 | Mean Difference (IV, Random, 95% CI) | ‐9.59 [‐13.43, ‐5.75] |
Comparison 4. Case management.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Repetition of SH at post‐intervention | 4 | 1608 | Odds Ratio (M‐H, Random, 95% CI) | 0.78 [0.47, 1.30] |
| 4.1.1 TAU (whole sample) | 2 | 600 | Odds Ratio (M‐H, Random, 95% CI) | 0.59 [0.25, 1.40] |
| 4.1.2 Enhanced usual care (whole sample) | 2 | 1008 | Odds Ratio (M‐H, Random, 95% CI) | 0.99 [0.42, 2.31] |
| 4.2 Suicide deaths at post‐intervention | 4 | 1757 | Odds Ratio (M‐H, Random, 95% CI) | 0.95 [0.57, 1.57] |
| 4.2.1 TAU | 2 | 600 | Odds Ratio (M‐H, Random, 95% CI) | 1.50 [0.24, 9.35] |
| 4.2.2 Enhanced usual care | 2 | 1157 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.54, 1.55] |
Comparison 5. Remote contact interventions: Emergency cards.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Repetition of SH at post‐intervention | 2 | 1039 | Odds Ratio (M‐H, Random, 95% CI) | 0.82 [0.31, 2.14] |
| 5.2 Repetition of SH at 12 months | 1 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.2.1 Emergency cards (whole sample) | 1 | 827 | Odds Ratio (M‐H, Random, 95% CI) | 1.19 [0.85, 1.67] |
| 5.2.2 Emergency cards (history of prior SH) | 1 | 394 | Odds Ratio (M‐H, Random, 95% CI) | 1.85 [1.14, 3.03] |
| 5.2.3 Emergency cards (no history of prior SH) | 1 | 427 | Odds Ratio (M‐H, Random, 95% CI) | 0.64 [0.34, 1.22] |
Comparison 6. Remote contact interventions: Postcards.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Repetition of SH at post‐intervention | 4 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1.1 Postcards (whole sample) | 4 | 3277 | Odds Ratio (M‐H, Random, 95% CI) | 0.87 [0.62, 1.23] |
| 6.1.2 Postcards (males) | 1 | 247 | Odds Ratio (M‐H, Random, 95% CI) | 0.86 [0.42, 1.75] |
| 6.1.3 Postcards (females) | 1 | 524 | Odds Ratio (M‐H, Random, 95% CI) | 0.89 [0.56, 1.41] |
| 6.2 Repetition of SH at 12 months | 2 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.2.1 Postcards (whole sample) | 2 | 2885 | Odds Ratio (M‐H, Random, 95% CI) | 0.76 [0.57, 1.02] |
| 6.2.2 Postcards (males) | 1 | 247 | Odds Ratio (M‐H, Random, 95% CI) | 0.95 [0.50, 1.84] |
| 6.2.3 Postcards (females) | 1 | 524 | Odds Ratio (M‐H, Random, 95% CI) | 1.19 [0.78, 1.80] |
| 6.3 Frequency of SH at post‐intervention | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.3.1 Postcards (whole sample) | 3 | 1097 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.32, 0.18] |
| 6.3.2 Postcards (males) | 3 | 401 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.13, 0.12] |
| 6.3.3 Postcards (females) | 3 | 695 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.29, 0.20] |
| 6.3.4 Postcards (history of prior SH) | 3 | 339 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.68, 0.51] |
| 6.3.5 Postcards (no history of prior SH) | 3 | 758 | Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.32, 0.77] |
| 6.4 Frequency of SH at 12 months | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.4.1 Postcards (whole sample) | 2 | 984 | Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.58, 0.20] |
| 6.4.2 Postcards (males) | 2 | 336 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.11, 0.16] |
| 6.4.3 Postcards (females) | 2 | 647 | Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.62, 0.18] |
| 6.4.4 Postcards (history of prior SH) | 2 | 296 | Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐2.07, 0.80] |
| 6.4.5 Postcards (no history of prior SH) | 2 | 688 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.22, 0.09] |
| 6.5 Frequency of SH at 24 months | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.5.1 Postcards (whole sample) | 1 | 472 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.16, 0.10] |
| 6.5.2 Postcards (males) | 1 | 220 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.21, 0.29] |
| 6.5.3 Postcards (females) | 1 | 252 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.21, 0.07] |
| 6.5.4 Postcards (history of prior SH) | 1 | 338 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.31, 0.13] |
| 6.5.5 Postcards (no history of prior SH) | 1 | 134 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.16, 0.14] |
| 6.6 Suicide deaths at post‐intervention | 4 | 3464 | Odds Ratio (M‐H, Random, 95% CI) | 1.86 [0.61, 5.72] |
| 6.6.1 Postcards (whole sample) | 4 | 3464 | Odds Ratio (M‐H, Random, 95% CI) | 1.86 [0.61, 5.72] |
Comparison 7. Remote contact interventions: Telephone‐based psychotherapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Repetition of SH at post‐intervention | 2 | 185 | Odds Ratio (M‐H, Random, 95% CI) | 0.36 [0.01, 8.94] |
| 7.2 Depression scores at post‐intervention | 2 | 185 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐1.39, 0.59] |
| 7.3 Suicide deaths at post‐intervention | 3 | 240 | Odds Ratio (M‐H, Random, 95% CI) | 3.09 [0.12, 78.55] |
Comparison 8. Provision of information and support.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Repetition of SH at post‐intervention | 2 | 1853 | Odds Ratio (M‐H, Random, 95% CI) | 1.09 [0.79, 1.50] |
| 8.2 Suicide deaths at post‐intervention | 3 | 2577 | Odds Ratio (M‐H, Random, 95% CI) | 0.15 [0.05, 0.48] |
| 8.2.1 Provision of information and support | 2 | 1889 | Odds Ratio (M‐H, Random, 95% CI) | 0.12 [0.03, 0.44] |
| 8.2.2 Provision of information and support with peer support | 1 | 688 | Odds Ratio (M‐H, Random, 95% CI) | 0.33 [0.03, 3.20] |
Comparison 9. Other multimodal interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Repetition of SH at post‐intervention | 3 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1.1 Whole sample | 3 | 1937 | Odds Ratio (M‐H, Random, 95% CI) | 0.69 [0.37, 1.30] |
| 9.1.2 First SH episode | 2 | 901 | Odds Ratio (M‐H, Random, 95% CI) | 1.02 [0.70, 1.47] |
| 9.1.3 Repeat SH episode | 2 | 938 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.52, 1.62] |
| 9.2 Time to SH repetition | 2 | Hazard Ratio (IV, Random, 95% CI) | 0.39 [0.09, 1.76] | |
| 9.3 Depression scores at post‐intervention | 3 | 651 | Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐2.08, 1.05] |
| 9.4 Hopelessness scores at post‐intervention | 2 | 556 | Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐1.27, 0.69] |
| 9.5 Suicide deaths at post‐intervention | 3 | 971 | Odds Ratio (M‐H, Random, 95% CI) | 0.63 [0.13, 3.06] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allard 1992.
| Study characteristics | ||
| Methods | Participants were individually randomised using sealed and numbered envelopes to intensive outpatient treatment or TAU. N lost to follow‐up: 24/150 (16.0%) for repetition of SH by the 24‐month assessment. Location: Montreal, Canada. |
|
| Participants |
Number of total participants: 150 participants were randomised, 76 were allocated to intensive outpatient treatment and 74 were allocated to TAU. Profile of participants: mean (SD) age not reported. Just over half (n = 83; 55.3%) were female. Half (n = 75; 50.0%) had a history of SH (i.e. multiple episodes of SH). The majority were diagnosed with MDD (n = 131; 87.3%), followed by SUD (n = 80; 53.3%), and any personality disorder (n = 68; 45.3%). Source of participants: patients presenting to hospital following a suicide attempt (i.e. SH with suicidal intent). Inclusion criteria: i) resident in the catchment area; ii) sufficient language ability (French or English); iii) no physical handicap preventing attendance; iv) not already in institutional care; v) able to provide informed consent; vi) not sociopathic; vii) suicide attempt within one week prior to trial entry. Exclusion criteria: i) no fixed address; ii) moving out of the catchment area; iii) in the care of an institution that ensures follow‐up after all suicide attempts; iv) diagnosed with a physical disability that would prevent attendance at follow‐up sessions; v) unable to provide informed consent; vi) diagnosed with sociopathy and presents a physical threat to hospital personnel; vii) suicide attempt occurred over one week preceding trial entry. |
|
| Interventions |
Intervention: intensive outpatient treatment consisting of 18 sessions (duration not reported), including one delivered in the participants' home (delivered by a social worker). Sessions were weekly for the first month, fortnightly for the next three months, and monthly for the remaining eight months. Therapeutic content included: developing a collaborative treatment plan and other various therapeutic approaches including psychoanalytically oriented psychotherapy, psychosocial therapy, AOD treatment, or behavioural therapy as needed. At the conclusion of the 12‐month treatment period, participants were referred to usual psychiatric care. Sessions were delivered by a social worker (information on experience not reported). Comparator: TAU consisting of treatment by the regular personnel within the same hospital (number and duration of sessions not reported). Further information on therapeutic content not reported. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to hospital records, Coroner's records, and/or collateral informant report. Secondary outcome(s): i) treatment adherence as measured by the number of sessions attended; ii) suicide as ascertained from Coroner's records and collateral informant report. |
|
| Notes |
Source(s) of funding: no information on funding reported. Conflict(s) of interest: no information on conflicts of interest reported. |
|
Amadéo 2015.
| Study characteristics | ||
| Methods | Participants were individually randomised using a block randomisation procedure. N lost to follow‐up: 10/200 (5.0%) by the post‐intervention assessment. Location: Papeete, Tahiti, French Polynesia. |
|
| Participants |
Number of total participants: 200 participants were randomised, 100 were allocated to provision of information and support and 100 were allocated to TAU. Profile of participants: mean age 32.2 years (SD not reported, range not reported). Over half (n = 122; 64.2%) were female. Just over half (n = 97; 51.0%) were diagnosed with any mood disorder, followed by any anxiety/adjustment disorder (n = 33; 17.4%), psychosis (n = 10; 5.3%), alcohol use disorder (n = 5; 2.6%), any personality disorder (n = 4; 2.1%), and cannabis use disorder (n = 2; 1.0%). Source of participants: patients presenting to the ED following an episode of SH. Inclusion criteria: i) presenting to ED following an episode of SH. Exclusion criteria: none reported. |
|
| Interventions |
Intervention: based on the SUPRE‐MISS model (Fleischmann 2008), the intervention consisted of a brief inpatient psychiatric admission (≥ 24 hours), a brief (one‐hour) information session, and nine follow‐up telephone contacts (duration not reported) at weeks one, two, four, seven, 11, and months four, six, 12, and 18 months post‐discharge. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: TAU consisting of a brief inpatient psychiatric admission (≥ 24 hours), a single psychiatric assessment (duration not reported), and then either hospitalisation, outpatient follow‐up, or no care at all. Length of treatment: 18 months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH as ascertained from self‐report using the European Parasuicide Study Interview Schedule (EPSIS); ii) suicide (as determined from Coroner's records). | |
| Notes | Source(s) of funding: "[T]he study was funded by the French Polynesia Ministry of Health and the Centre Hospitalier de Polynésie Française" (Amadéo 2015, p.48). Conflict(s) of interest: "[T]he authors declare no potential conflict of interest" (Amadéo 2015, p.48). | |
Andreoli 2015.
| Study characteristics | ||
| Methods | Participants were individually randomised using a pre‐generated block randomisation procedure via envelopes to either three months of abandonment psychotherapy delivered by certified psychotherapists, abandonment psychotherapy delivered by trained nurses, or TAU. N lost to follow‐up: 0/170 (0%) for repetition of SH at post‐intervention. Location: Geneva, Switzerland. |
|
| Participants |
Number of total participants: 170 participants were randomised, 70 were allocated to abandonment psychotherapy delivered by certified psychotherapists, 70 were allocated to abandonment psychotherapy delivered by trained nurses, and 30 were allocated to TAU. Profile of participants: mean age 31.9 ± 10.1 years (range: 18 to 60 years). The majority (n = 143; 84.1%) were female. All (n = 170; 100%) were diagnosed with BPD. The majority (n = 138; 81.2%) were also diagnosed with comorbid MDD, followed by SUD (n = 62; 36.5%). Source of participants: patients presenting to the ED following an episode of SH requiring immediate medical/surgical treatment. Inclusion criteria: i) 18‐60 years of age; ii) diagnosed with comorbid MDD and BPD according to DSM‐IV criteria. Exclusion criteria: i) diagnosed with psychosis, bipolar I disorder, or severe SUD according to DSM‐IV criteria; ii) diagnosed with an intellectual disability; iii) diagnosed with an medical condition contraindicated for antidepressant medication or likely to significantly alter clinical outcome(s); iv) insufficient language ability. |
|
| Interventions |
Intervention 1: manualised abandonment psychotherapy delivered by certified psychotherapists. Abandonment psychotherapy consists of twice weekly sessions (duration not reported) incorporating principles from cognitive/psychodynamic therapy (e.g. cognitive restructuring), DBT (e.g. distress tolerance), MBT (e.g. identification and labelling of different affective states), and family therapy. Sessions focus on difficulties in romantic relationships. Participants also had access to a 24‐hour crisis hotline as required. Sessions were delivered by certified psychotherapists (information on experience was not reported). Intervention 2: manualised abandonment psychotherapy (as above) delivered by trained nurses with experience in the management of patients diagnosed with BPD. Sessions were delivered by nurses with considerable experience in managing patient with BPD. Comparator: TAU. Consisting of as many nurse visits (duration not reported) as needed over a two‐week period, followed by biweekly nurse visits (duration not reported), weekly clinical and medication review sessions (duration not reported), weekly group‐therapy sessions (duration not reported), and as many partial hospitalisations and family therapy sessions (duration not reported) as required for the remainder of the treatment period. Concomitant medications: were permitted. The majority (n = 125, 89.3%) were prescribed venlafaxine. However, the proportion of participants prescribed an any antidepressant medication was lower in the comparator arm (76.7%) compared with either of the intervention arms (97.1% and 97.1%, respectively). Length of treatment: three months. |
|
| Outcomes |
Primary outcome(s): i) clinical remission as measured by a Global Assessment Scale (GAS; Endicott 1976) score of > 60. Secondary outcome(s): i) repetition of SH as ascertained from medical records; ii) symptom severity as measured by a scores on the severity subscale of the Clinical Global Impression (CGI; Guy 1976); iii) depression as measured by the HDRS; iv) remission from depression as ascertained from whether the participant still meets DSM‐IV criteria; iv) psychosocial outcome as measured by the HSRS; v) treatment adherence as measured by the number of days retained in treatment and dropouts; vi) suicidal ideation (unclear how ascertained); vii) all‐cause hospitalisations as ascertained from medical records; viii) suicide (unclear how ascertained). |
|
| Notes |
Source(s) of funding: no details on funding reported. Conflict(s) of interest: no details on conflicts of interest reported. |
|
Armitage 2016.
| Study characteristics | ||
| Methods | Participants were individually randomised using web‐based software to either a guided implementation‐focused intervention based on the volitional help‐sheet model (Armitage 2016a), a self‐directed implementation intention‐focused intervention (Armitage 2016b), or TAU. N lost to follow‐up: 0/226 (0%) for repetition of SH by the three‐month assessment. Location: Kuala Lumpur, Malaysia. |
|
| Participants |
Number of total participants: 226 participants were randomised, 78 were allocated to a brief, self‐directed implementation intention intervention, 75 were allocated to a brief volitional help sheet intervention, and 73 were allocated to TAU. Profile of participants: mean age 30.0 ± 13.4 years (range: 15 to 65 years). The majority (n = 158; 69.9%) were female. Source of participants: admitted to a general hospital following an episode of SH. Inclusion criteria: i) admitted to a general hospital following an episode of SH. Exclusion criteria: none reported. |
|
| Interventions | See Armitage 2016a and Armitage 2016b for a detailed description. | |
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from self‐report using the Suicidal Behaviours Questionnaire; ii) suicidal ideation ascertained from self‐report using the Suicidal Behaviours Questionnaire. Secondary outcome(s): i) depression measured using the BDI; ii) motivation to avoid SH measured using an idiosyncratic scale. |
|
| Notes |
Source(s) of funding: no information on sources of funding reported. Conflict(s) of interest: none reported. |
|
Armitage 2016a.
| Study characteristics | ||
| Methods | See Armitage 2016 for a detailed description. | |
| Participants | See Armitage 2016 for a detailed description. | |
| Interventions |
Intervention (guided volitional help‐sheet): one‐off (duration not reported) session. Participants are provided with a list of common situations in which they may be tempted to engage in SH together with a list of potential alternative behaviours. Participants then draw links between any situation that applies to them and any one of the listed alterative behaviours. Participants can make as many links as desired. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: TAU. No further information reported. Length of treatment: one‐off session (duration not reported). |
|
| Outcomes | See Armitage 2016 for a detailed description. | |
| Notes | See Armitage 2016 for a detailed description. | |
Armitage 2016b.
| Study characteristics | ||
| Methods | See Armitage 2016 for a detailed description. | |
| Participants | See Armitage 2016 for a detailed description. | |
| Interventions |
Intervention (self‐directed implementation intention): one‐off (duration not reported) session in which participants were free to formulate their own safety plan. Sessions were self‐delivered. Comparator: TAU. No further information reported. Length of treatment: one‐off session (duration not reported). |
|
| Outcomes | See Armitage 2016 for a detailed description. | |
| Notes | See Armitage 2016 for a detailed description. | |
Bateman 2009.
| Study characteristics | ||
| Methods | Participants were individually randomised using a stochastic minimisation programme
(MINIM) balanced for age (18‐25, 26‐30, and > 30 years), sex, and diagnosis of ASPD to MBT or structured case management. N lost to follow‐up: 2/136 (1.5%) for repetition data at post‐intervention. Location: London, UK. |
|
| Participants |
Number of total participants: 134 participants were randomised, 71 were allocated to MBT and 63 were allocated to structured case management. Profile of participants: mean age 31.1 ± 7.7 years (range: 18‐65 years). The majority (n = 107; 79.9%) were female. All (n = 134; 100%) had a history of SH (i.e. multiple episodes of SH). Just over three‐quarters (n = 103; 76.9%) were diagnosed with a milder depressive disorder such as dysthymia, followed by any anxiety disorder (n = 82; 61.2%), SUD (n = 72; 53.7%), any eating disorder (n = 37; 27.6%), PTSD (n = 19; 14.2%), and somatoform disorder (n = 17; 12.7%). Just over one‐quarter (n = 37; 27.6%) were diagnosed with comorbid ASPD. Source of participants: consecutive referrals to one of two community outpatient psychiatric facilities, one of which provides specialist treatment for PD. Inclusion criteria: i) 18‐65 years of age; ii) diagnosed with BPD; iii) engaged in SH within six months prior to trial entry. Exclusion criteria: i) currently in long‐term psychotherapeutic treatment; ii) diagnosed with any psychosis or bipolar I disorder according to DSM‐IV criteria; iii) dependent on any opiate to such a degree that specialist AOD treatment is indicated; iv) diagnosed with a mental impairment or evidence of an organic brain disorder. |
|
| Interventions |
Intervention: manualised MBT consisting of up to 140 sessions (duration not reported) of weekly individual and group therapy. Therapeutic content also included: collaborative crisis planning, a general psychiatric review every three months, case management, advocacy support, and problem‐oriented psychotherapy. Sessions were delivered by therapists (no further information on expertise or experience was reported). Comparator: structured case management designed to analogue TAU consisting of three‐monthly individual and group therapy (duration not reported). Therapeutic content was based on a counselling model resembling a supportive approach and included: counselling, case management, and problem‐oriented psychotherapy. Concomitant medication(s): participants were prescribed medication (e.g. antidepressants, antipsychotics, mood stabilisers, minor tranquillisers), as needed. As baseline, just under three‐quarters (n = 98; 73.1%) were prescribed concomitant medications (mean number of medications prescribed at baseline: 1.1 ± 0.9). Length of treatment: 18 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH (unclear how ascertained); ii) repetition of suicide attempts (unclear how ascertained); iii) hospital readmission (unclear how ascertained). Secondary outcome(s): i) general functioning as measured by the GAF; ii) distress as measured by the Global Severity Index (GSI); iii) depression as measured by the BDI; iv) social functioning as measured by the Social Adjustment Scale (SAS); v) interpersonal functioning as measured by the Inventory of Interpersonal Problems (IIP); vi) medication use (unclear how ascertained). |
|
| Notes | Source(s) of funding: “Supported by a grant from the Borderline Personality Disorder Research Foundation” (Bateman 2009, p. 1363). Conflict(s) of interest: none reported. Other: data on repetition of SH, suicide attempts, and suicides were obtained via correspondence with trial authors. | |
Beautrais 2010.
| Study characteristics | ||
| Methods | Participants were individually randomised using a predetermined computer‐generated random number procedure to a remote contact intervention (postcards) or TAU. N lost to follow‐up: 0/327 (0) for repetition of SH data. Location: Christchurch, New Zealand. |
|
| Participants |
Number of total participants: 327 participants were randomised, 153 were allocated to the remote contact intervention and 174 were allocated to TAU. Profile of participants: mean age 33.8 (SD: not reported; range: 18‐65 years). Two thirds (n = 216; 66.0%) were female. Fifty‐eight (17.7%) had a history of SH (i.e. multiple episodes of SH). No information on psychiatric diagnoses was reported. Source of participants: patients admitted to a psychiatric emergency service following an episode of SH or attempted suicide. Inclusion criteria: i) 16 years of age or older; ii) admitted to a psychiatric emergency service following an episode of SH or attempted suicide; iii) resident in New Zealand; iv) sufficient language ability. Exclusion criteria: none reported. Length of treatment: 12 months. |
|
| Interventions |
Intervention: remote contact intervention consisting of postcards mailed at two and six weeks and three, six, nine, and 12 months post‐discharge in addition to TAU. Postcards encouraged participants to make contact with the service if required. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: TAU consisting of crisis assessment and referral to inpatient community‐based mental health services as required. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from emergency service records and medical records; ii) representation to psychiatric emergency services as ascertained from emergency service records and medical records. Secondary outcome(s): i) suicide (unclear how ascertained). |
|
| Notes |
Source(s) of funding: "This study was supported by grants from the Canterbury District Health Board and the Accident Compensation Corporation (ACC). S.J.G. was supported by a University of Otago Postgraduate Publishing Bursary" (Beautrais 2010, p. 59). Conflict(s) of interest: none reported. Other: data on suicides were obtained via correspondence with trial authors. |
|
Bennewith 2002.
| Study characteristics | ||
| Methods | cRCT. GP practices were randomised, stratified by rate of SH, via a random numbers trial to either a GP letter or TAU. N lost to follow‐up: 0/1932 (0%) for repetition of SH data. Location: Avon, Wiltshire, and Somerset, UK. |
|
| Participants |
Number of total participants: 1932 participants were allocated, 964 were allocated to GP management and 968 were allocated to TAU. Profile of participants: mean age 32.5 ± 13.2 years (range: 16‐95 years). Just over half (n = 1140; 59.0%) were female. A minority (n = 244; 12.6%) had a history of SH (i.e. multiple episodes of SH) according to case register information. No information on psychiatric diagnoses was reported. Source of participants: patients presenting to hospital following an episode of SH and who were also registered with one of the participating primary care practices. Inclusion criteria (for GP practices): i) located in catchment area (i.e. within catchment area of the four recruitment general hospitals). Inclusion criteria (for participants): i) aged 16 years and older; ii) data able to be found in general hospital case register; iii) recruitment data able to be collected weekly from hospitals’ A&E sites; iv) fixed residence. Exclusion criteria: i) engaged in an alcohol only or illicit drug overdose (except where casualty officer felt purpose was SH or suicide); ii) imprisoned; iii) made a request that no one be informed of SH episode; iv) SH occurred in direct response to a hallucination or delusion; v) SH episode managed entirely in primary care. |
|
| Interventions |
Intervention: letter from GP inviting patient to a consultation with GP (provided with management guideline). Sessions were delivered by GPs (no information on experience was reported). Comparator: TAU consisting of GP management, psychiatric, or other referral, as required. Length of treatment: one‐off consultation. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from hospital case registers. Secondary outcome(s): i) frequency of SH repetition ascertained from hospital case registers; ii) time to first repeat SH episode ascertained from hospital case registers; iii) contact with services (unclear how ascertained). |
|
| Notes | Source(s) of funding: "National Health Service South West Research and Development Directorate" (Bennewith 2002, p. 1260). Conflict(s) of interests: none reported. | |
Brown 2005.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated sequence (designed to prohibit more than seven consecutive assignments to the same treatment group) to either CBT or EUC. N lost to follow‐up: 18/120 (15.0%) for repetition by the six‐month follow‐up assessment. Location: Pennsylvania, USA. |
|
| Participants |
Number of total participants: 120 participants were allocated, 60 were allocated to CBT and 60 were allocated to TAU. Profile of participants: mean age 35.0 ± 10.2 years (range: 18‐66 years). Over half (n = 73; 60.8%) were female. The majority (n = 87; 72.5%) had a history of SH (i.e. multiple episodes of SH). Just over three‐quarters were diagnosed with MDD (n = 92; 76.7%), followed by SUD (n = 82; 68.3%). Source of participants: patients presenting to hospital following a suicide attempt. Inclusion criteria: i) 16 years of age or older; ii) engaged in a suicide attempt and received medical/psychiatric evaluation within 48 hours of the attempt; iii) able to provide at least two verifiable contacts; iv) sufficient language ability; v) able to complete baseline assessment; vi) able to provide informed consent. Exclusion criteria: i) diagnosed with any medical condition that would prevent participation in an outpatient clinical trial. |
|
| Interventions |
Intervention: CBT‐based psychotherapy consisting of 10 weekly/biweekly sessions (duration not reported) in addition to TAU. Therapeutic content included: identification of proximal thoughts, core beliefs, development of alternative coping strategies, and relapse prevention. Therapy focused on hopelessness, deficits in problem‐solving, treatment noncompliance, and social isolation. Sessions were delivered by trial therapists (no further information on expertise or experience was reported). Comparator: TAU, including referral to other services, as required. Length of treatment: 10‐20 weeks (exact duration not clearly reported). |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from self‐report; ii) depression as measured using the HDRS and BDI; iii) hopelessness as measured by the BHS; iv) suicidal ideation as measured by the BSSI. Secondary outcome(s): i) treatment adherence (this outcome had to be excluded from the review due to the nature of the data reported). |
|
| Notes | Source(s) of funding: "This research was supported by grants R01 MH60915 and P20 MH71905 from the National Institute of Mental Health and grant R37 CCR316866 from the Centers for Disease Control and prevention" (Brown 2005, p. 570). Conflict(s) of interest: none reported. | |
Carter 2005.
| Study characteristics | ||
| Methods | Participants were individually randomised using Zelen's post‐consent design to a remote contact intervention in addition to TAU or TAU alone. N lost to follow‐up: 0/772 (0%) for repetition of SH data. Location: Hunter Valley, NSW, Australia. |
|
| Participants |
Number of total participants: 772 participants were allocated, 378 were allocated to a remote contact intervention (postcards) in addition to TAU and 394 were allocated to TAU alone. Profile of participants: median age 33.0 years (IQR: 24.0 to 44.0 years; range: not reported). Over two‐thirds (n = 525; 68.0%) were female. A minority (n = 131; 17.0%) had a history of SH (i.e. multiple episodes of SH). Just under half (n = 333; 43.1%) were diagnosed with any mood disorder, followed by SUD (n = 311; 40.3%), and any PD (n = 169; 21.9%). Source of participants: patients presenting to hospital toxicology service following an episode of self‐poisoning. Inclusion criteria: i) 16 years of age or older; ii) presented to a toxicology service following an episode of deliberate self‐poisoning; iii) able to provide informed consent; iv) fixed address; v) sufficient language ability; vi) did not pose a potential threat to the interviewer. Exclusion criteria: none reported. |
|
| Interventions |
Intervention: remote contact intervention consisting of a series of postcards mailed at one, two, three, four, six, eight, 10 and 12 months' post‐discharge in addition to TAU. Postcards encouraged participants to make contact with the service if required. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: TAU. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from electronic hospital records. Secondary outcome(s): i) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: “KC is funded by the NSW Health, Burdekin Mental Health Enhancement Strategy” (Carter 2005, p. 4). Conflict(s) of interest: none reported. Other: data on suicides obtained following correspondence with the trial authors. Additionally, 20 control group participants received intervention due to clerical errors but were included by the authors in the control group for all intention‐to‐treat analyses. | |
Cedereke 2002.
| Study characteristics | ||
| Methods | Participants were individually randomised using sealed envelopes to a remote contact intervention (telephone contact) in addition to TAU or TAU alone. N lost to follow‐up: 44/216 (20.4%) for repetition of SH by the 12‐month follow‐up assessment. Location: Lund, Sweden. |
|
| Participants |
Number of total participants: 216 participants were allocated, 107 were allocated to a remote contact intervention (telephone contact) in addition to TAU and 109 were allocated to TAU alone. Profile of participants: mean age 41.0 ± 18.0 years (range: not reported). Almost two‐thirds (n = 143; 66.2%) were female. Just over half (n = 112; 51.8%) had a history of SH (i.e. multiple episodes of SH). The majority (n = 197; 91.2%) were diagnosed with a mood disorder. Source of participants: patients treated in hospital following a suicide attempt (i.e. with evidence of suicidal intent). Inclusion criteria: i) received treatment in a general hospital following a suicide attempt. Exclusion criteria: none reported. |
|
| Interventions |
Intervention: remote contact intervention consisting of a two telephone contacts (20‐45 minutes) at four and eight months' post‐discharge in addition to TAU. Telephone calls were designed to offer motivational therapy and to encourage participants to remain adherent to TAU. Sessions were delivered by therapists (no information on expertise reported) with a minimum of 10 years' experience working with suicidal persons. Comparator: TAU. Length of treatment: eight months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from self‐report and medical records; ii) suicide as ascertained from mortality registers. Secondary outcomes: i) general functioning as measured by the GAF; ii) distress as measured by the Symptom Check List‐90 (SCL‐90) and the GSI; iii) suicidal ideation as measured by the BSSI; iv) treatment adherence as measured by the number of telephone contacts made. |
|
| Notes | Source(s) of funding: “This study was supported by grants from The Axson Johnsons foundation and from the Vardal Foundation (V97 341)” (Cedereke 2002, p. 90). Conflict(s) of interest: no information reported. | |
Clarke 2002.
| Study characteristics | ||
| Methods | Participants were individually randomised using a random numbers list, stratified by sex and admitting hospital, to case management in addition to TAU or TAU alone. N lost to follow‐up: 0/467 (0%) for repetition of SH at post‐intervention. Location: East London and Essex, UK. |
|
| Participants |
Number of total participants: 467 participants were allocated, 220 were allocated to case management in addition to TAU and 247 were allocated to TAU alone. Profile of participants: mean age 33.0 (SD not reported; range: not reported). Over half (n = 263; 56.3%) were female. One in five (n = 104; 22.3%) had a history of SH (i.e. multiple episodes of SH). A minority were diagnosed with any psychiatric disorder (n = 80; 17.1%); most commonly AUD (n = 60; 75.0%) followed by schizoaffective disorder (n = 12; 2.5%). Source of participants: patients presenting to hospital following SH. Inclusion criteria: i) aged 16 years or older; ii) resident in the catchment area; iii) overdose attributable to recreational or problematic substance use. Exclusion criteria: i) aged less than 16 years; ii) between 16 and 19 years and still in full‐time secondary education; overdose attributable to recreational or problematic substance use. |
|
| Interventions |
Intervention: case management comprising a comprehensive assessment of individual needs, development of an individualised package of care, arrangement of access to services, monitoring of quality of services provided, and long‐term, flexible support. Number of sessions and their duration not reported. Participants also received TAU. Sessions were delivered by a case manager (no further information on expertise or experience was reported). Comparator: TAU comprising triage, and medical and psychosocial treatment, as required. Length of treatment: up to six months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH according to hospital admission records; ii) suicide (unclear how ascertained). | |
| Notes |
Source(s) of funding: "Funded by the participating health authority” (Clarke 2002, p. 167). Conflict(s) of interest: none reported. Other: data on suicides obtained following correspondence with trial authors. |
|
Crawford 2010.
| Study characteristics | ||
| Methods | Participants were individually randomised using a random numbers table to a brief, alcohol‐focused intervention or TAU. N lost to follow‐up: 0/103 (0%) for repetition of SH by the six‐month assessment; 65/103 (63.1%) for secondary outcomes not included in this review (e.g. alcohol consumption, mental health problems, and satisfaction with treatment). Location: London, UK. |
|
| Participants |
Number of total participants: 103 participants were allocated, 51 were allocated to the brief alcohol‐focused intervention and 52 were allocated to TAU alone. Profile of participants: mean age 37.2 ± 12.0 years (range: 18‐65 years). Almost half (n = 50; 48.5%) were female. All (n = 103; 100%) were diagnosed with AUD. Source of participants: consecutive admissions to an ED following an episode of SH and who were diagnosed with alcohol misuse according to scores on the Paddington Alcohol Test. Inclusion criteria: i) aged 18 years or older; ii) admitted to an ED following an episode of SH; iii) diagnosed with alcohol misuse according to scores on the Paddington Alcohol Test. Exclusion criteria: i) unwilling to provide informed consent; ii) unable to provide informed consent (e.g. due to insufficient language ability or impaired consciousness); iii) no fixed address in the greater London area; iv) already receiving treatment from AOD services; v) made a specific request to receive treatment from AOD services at the index presentation. |
|
| Interventions |
Intervention: one‐off appointment (~30 minutes) with an alcohol nurse specialist involving assessment and discussion of both current and previous drinking behaviours delivered according to the FRAMES approach in addition to a health information leaflet advising on the damaging effects of excessive alcohol consumption, recommended limits of alcohol consumption, and the contact details of nationally‐based alcohol misuse help lines (Miller 1993). Participants could also be referred by the alcohol nurse specialist to individual alcohol counselling or detoxification services as required. Sessions were delivered by an alcohol nurse specialist (no further information on experience was reported). Comparator: TAU comprising a health information leaflet advising on the damaging effects of excessive alcohol consumption, recommended limits of alcohol consumption, and the contact details of nationally‐based alcohol misuse help lines. Length of treatment: 30 minutes. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to hospital records. Secondary outcome(s): i) levels of alcohol consumption as measured by the Alcohol Use Disorders Identification Test (AUDIT); ii) diagnosis of probable personality disorder as ascertained by a score of ≥ 3 on the Standardised Assessment of Personality ‐ Abbreviated Scale (SAPAS); iii) general mental health as measured by the General Health Questionnaire‐12 (GHQ‐12); iv) satisfaction with treatment as measured by the Client Satisfaction Questionnaire; v) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: “This study was funded by St Mary’s Paddington Charitable Trust” (Crawford 2010, p. 1827). Conflict(s) of interest: none stated. Other: data on suicides were obtained following correspondence with trial authors. | |
Davidson 2014.
| Study characteristics | ||
| Methods | Participants were individually randomised (2:1 ratio) using a random numbers table to manualised CBT‐based psychotherapy or TAU. N lost to follow‐up: 6/20 (30.0%) for repetition of SH by the three‐month assessment. Location: Glasgow, UK. |
|
| Participants |
Number of total participants: 20 participants were allocated, 14 were allocated to CBT‐based psychotherapy and 6 were allocated to TAU. Profile of participants: mean (SD) age not reported (range: 18‐65 years). Proportion female not reported. All (n = 20; 100%) were diagnosed with a personality disorder; most commonly BPD (n = 17; 85.0%), followed by avoidant PD (n = 13; 65.0%), and paranoid PD (n = 8; 40.0%). Almost half (n = 9; 45.0%) were diagnosed with a comorbid SUD. Source of participants: patients admitted to the medical receiving ward of the A&E department following an episode of SH. Inclusion criteria: i) aged 18‐65 years; ii) diagnosed with any PD according to the SCID‐II; iii) score of ≥ 3 on the Standardised Assessment of Personality Abbreviated Scale. Exclusion criteria: i) unwilling or unable to provide informed consent. |
|
| Interventions |
Intervention: brief, manualised CBT‐based psychotherapy consisting of six sessions (duration not reported). Therapeutic content included: psychoeducation, development of alternatives to resolving problems, and referral to appropriate mental health services, where required. Sessions were delivered either by a doctoral‐level clinical psychologist or a psychiatrist who received training (duration not reported) in manualised CBT‐based psychotherapy and ongoing weekly supervision. Comparator: TAU consisting of referral to community mental health teams, appointments with psychiatrists and a community psychiatric nurse, and inpatient psychiatric treatment, as required. Information on both the number and duration of sessions was not reported. Length of treatment: not reported. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to self‐report using the Acts of Deliberate Self‐Harm Inventory (DSHI); ii) suicidal ideation as measured by the BSS; iii) depression as measured by the HADS; iv) alcohol consumption as measured by the AUDIT; v) psychiatric treatment as ascertained from electronic medical records. Secondary outcome(s): i) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: "This work was supported by NHS Greater Glasgow and the Scottish Mental Health Research Network” (Davidson 2014, p. 4). Conflict(s) of interests: none reported. | |
Dubois 1999.
| Study characteristics | ||
| Methods | Participants were individually randomised; however, the method used was not reported. N lost to follow‐up: 18/102 (17.6%) for repetition of SH by the 12‐month assessment. Location: Bohars, France. |
|
| Participants |
Number of total participants: 102 participants were allocated, 51 were allocated to CBT‐based psychotherapy and 51 were allocated to TAU. Profile of participants: mean age 22.4 ± 5.8 years (range: not reported). The majority (n = 82; 80.4%) were female. Over half (n = 57; 55.9%) were diagnosed with any mood disorder, followed by any anxiety disorder (n = 44; 43.1%), psychosis (n = 43; 42.1%), and SUD (n = 14; 13.7%). A minority were not diagnosed with any psychiatric disorder (n = 13; 12.7). Source of participants: patients attending the ED following a suicide attempt. Inclusion criteria: i) aged 15‐34 years; ii) presented to the ED following a suicide attempt. Exclusion criteria: i) hospitalised for more than 24 hours; ii) currently being treated by a psychiatrist. |
|
| Interventions |
Intervention: brief CBT‐based psychotherapy consisting of five sessions (duration not reported). Whilst these sessions followed a specific therapeutic model, the therapeutic content was not reported. Sessions were delivered by the same therapist who initially saw them in the hospital (no further information on who delivered the intervention, their expertise, or their experience was reported). Comparator: TAU involving an assessment and follow‐up by a clinical psychiatrist. Length of treatment: one month. |
|
| Outcomes | Primary outcome(s): i) repetition of SH (unclear how ascertained); ii) suicide (unclear how ascertained); iii) treatment adherence as measured by the number of sessions attended. | |
| Notes |
Source(s) of funding: no information reported. Conflict(s) of interest: no information reported. Other: As data on treatment adherence were not reported for the control group, this outcome had to be excluded from subsequent analyses. |
|
Evans 1999a.
| Study characteristics | ||
| Methods | Participants were individually randomised using sealed envelopes to either a remote contact intervention (emergency card) or TAU. N lost to follow‐up: 0/827 (0%) for repetition of SH at post‐intervention. Location: Bristol, UK. |
|
| Participants |
Number of total participants: 827 participants were allocated, 417 were allocated to a remote contact intervention and 410 were allocated to TAU. Profile of participants: mean age 33.3 ± 13.0 years (range: not reported). Just over half (n = 458; 55.4%) were female. Just under half (n = 349; 42.2%) had a history of SH (i.e. multiple episodes of SH). The majority (n = 707; 85.5%) were diagnosed with a psychiatric disorder; however, no specific information on these diagnoses was reported. One hundred and twenty (14.5%) did not have a psychiatric diagnosis. Source of participants: patients admitted to general hospital following an episode of SH. Inclusion criteria: i) admitted to the ED following an episode of SH; ii) referred for routine psychiatric evaluation; iii) resident in catchment area; iv) judged likely to use intervention appropriately; v) made contact with and used mental health services; vi) acceptable level of aggressive behaviour. Exclusion criteria: i) inappropriate substance abuse leading to repetitive presentation in which the participant was aggressive; ii) unable to engage in treatment. |
|
| Interventions |
Intervention: remote contact intervention (emergency card) in addition to TAU. Participants were provided with an emergency card offering 24‐hour service for crisis telephone consultation with an on‐call psychiatrist. Sessions were delivered by the duty trainee psychiatrist (no further information on experience was reported). Comparator: TAU. Length of treatment: six months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from A&E and hospital records; ii) suicide (unclear how ascertained). | |
| Notes | Source(s) of funding: “Funding was provided by a grant from the Department of Health” (Evans 1999a, p. 23). Conflict(s) of interest: none stated. | |
Evans 1999b.
| Study characteristics | ||
| Methods | Participants were individually randomised using sealed envelopes opened sequentially to either CBT‐based psychotherapy or TAU. N lost to follow‐up: 2/34 (5.9%) for repetition of SH by the six‐month assessment. Location: London, UK. |
|
| Participants |
Number of total participants: 34 participants were allocated, 18 were allocated to CBT‐based psychotherapy and 16 were allocated to TAU. Profile of participants: mean (SD) not reported (range: 16 to 50 years). Over half (n = 21; 61.8%) were female. All (n = 34; 100%) had a history of SH (i.e. multiple episodes of SH). All (n = 34; 100%) were diagnosed with a PD. Source of participants: patients admitted to 1 of 2 hospitals in the London area (Paddington and Chelsea, Westminster) following an episode of SH. Inclusion criteria: i) diagnosed with any PD (ASPD, dissocial, impulsive or BPD); ii) ≥ 1 episode of SH in 12 months preceding trial entry. Exclusion criteria: i) diagnosed with alcohol or drug dependence, schizophrenia, or organic psychiatric disorder. |
|
| Interventions |
Intervention: two to six sessions (duration not reported) of manual‐assisted CBT. Therapeutic content included: basic cognitive techniques (e.g. cognitive restructuring), problem‐solving, distress tolerance, identification and management of emotions and thoughts, identification of alternative coping strategies, and relapse prevention. Sessions were delivered by a psychiatrist, community mental health team member, or social workers with experience (duration not reported) working with persons who engage in SH. Comparator: TAU. Five participants had contact with a psychiatrist, three saw a community mental health team, four saw a specialist social worker, and two saw no mental health professional. Length of treatment: varied. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from self‐report and hospital records. Secondary outcome(s): i) time to repetition of SH as ascertained from self‐report and hospital records; ii) social functioning as measured by the Social Functioning Questionnaire; iii) depression as measured by the depression subscale of the HADS; iv) anxiety as measured by the anxiety subscale of the HADS; v) treatment adherence as measured by the number of sessions attended; vi) health economics evaluation. |
|
| Notes | Source(s) of funding: “This work was supported by a grant from the North Thames Regional Health Authority” (Evans 1999b, p. 24). Conflict(s) of interest: no information on author interests reported. Other: five participants in the intervention arm did not see a therapist and instead received therapy from the booklets. One participant in the intervention arm did not receive any intervention. | |
Fleischmann 2008.
| Study characteristics | ||
| Methods | Participants were individually randomised using a random numbers table to either provision of information and support or TAU. N lost to follow‐up: 204/1867 (10.9%) for repetition of SH by the post‐intervention assessment. Locations: Campinas, Brazil; Chennai, India; Colombo, Sri Lanka; Karaj, Iran; Yuncheng, China. |
|
| Participants |
Number of total participants: 1867 participants were allocated, 922 were allocated to information and support and 945 were allocated to TAU. Profile of participants: median 23.0 years (IQR not reported; range: not reported). Over half (n = 1086; 58.2%) were female. Around one in five (n = 394; 21.1%) had a history of SH (i.e. multiple episodes of SH). No information reported on psychiatric diagnoses. Source of participants: patients presenting to emergency care settings following an episode of SH/self‐poisoning within a defined catchment area with a population of at least 250,000 persons. Inclusion criteria: i) presenting to services following an episode of SH/self‐poisoning as determined by medical staff. Exclusion criteria: i) died on the ward; ii) presence of a clinical condition that would preclude interview; iii) left hospital against medical advice; iv) resident in a different catchment area; v) insufficient language ability. |
|
| Interventions |
Intervention: brief, one‐off intervention involving “information about suicidal behaviour as a sign of psychological and/or social distress, risk and protective factors, basic epidemiology, repetition, alternatives to suicidal behaviours, and referral options” (Fleischmann 2008, p. 705) (duration: one hour) and contact via telephone or home visits to provide referral support in addition to TAU for up to 18 months. The number and duration of these telephone contacts was not reported. Sessions were delivered by trained psychiatrists, medical doctors, psychologists, or psychiatric nurses (no information on experience was reported). Comparator: TAU “according to the norms prevailing in the respective emergency departments” (Fleischmann 2008, p. 704). This typically involved only acute treatment for somatic problems only. Length of treatment: 18 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from self‐report using the European Parasuicide Study Interview Schedule (EPSIS); ii) suicide (unclear how ascertained). Secondary outcome(s): i) anger as measured by the Spielberger Trait‐Anger Scale; ii) depression as measured by the BDI; iii) hopelessness as measured by the BHS; iv) impulsiveness as measured by the Eysenck Impulsiveness Scale; v) social support as measured by the Bille‐Brahe Measurement of Social Support; vi) suicidal intent as measured by the Beck Suicide Intent Scale; vii) treatment adherence as measured by the number of sessions attended; viii) well‐being as measured by the WHO Well‐Being Index. |
|
| Notes | Source(s) of funding: “The study was funded by the Department of Mental Health and Substance Abuse, WHO. Some field research sites obtained additional funding from the following agencies: Campinas: Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), grant no 02/08288‐9, São Paulo, Brazil; Durban: Medical Research Council (MRC), Tygerberg, Cape Town, South Africa; Karaj: Tehran Psychiatric Institute, Mental Health Research Centre (IUMS), Tehran, Iran; Tallinn: Estonian Health Insurance Fund, Tallinn, Estonia; the Swedish National and Stockholm County Centre for Suicide Research and Prevention of Mental Ill‐Health (NASP), WHO Collaborating Centre for Research and Training in Suicide Prevention, Department of Public Health Sciences, Karolinska Institute, Stockholm, Sweden” (Fleischmann 2008, p. 708). Conflict(s) of interest: none reported. | |
Gibbons 1978.
| Study characteristics | ||
| Methods | Correspondence with trial authors confirmed participants were individually randomised using sequentially numbered envelopes to either CBT‐based psychotherapy or TAU. N lost to follow‐up: 0/400 (0%) for repetition of SH by the 12‐month follow‐up assessment. Location: Southampton, UK. |
|
| Participants |
Number of total participants: 400 participants were allocated, 200 were allocated to CBT‐based psychotherapy and 200 were allocated to TAU. Profile of participants: mean (SD) age not reported (range: not reported). The majority (n = 284; 71.0%) were female. A mix of both first‐time and those with a history of multiple episodes of SH were included, however, information on the proportion of each was not reported. Under half (n = 176; 44.0%) were diagnosed with a depressive disorder, followed by an anxiety disorder (n = 8; 2.0%), affective psychosis (n = 8; 2.0%), and schizophrenia (n = 4; 1.0%). Diagnoses for the remaining four (1.0%) participants not reported. Source of participants: patients presenting to A&E following an episode of self‐poisoning, Inclusion criteria: i) 17 years of age or older; ii) presented to A&E following an episode of self‐poisoning. Exclusion criteria: i) at immediate suicide risk; ii) not formally diagnosed with a psychiatric disorder. |
|
| Interventions |
Intervention: CBT‐based psychotherapy consisting of sessions (both the number and duration not reported) of a time‐limited, crisis‐oriented, task‐entered programme delivered by social workers. Therapeutic content involved problem‐solving focused on personal and social relationships, identifying alternative coping strategies, and distress tolerance. Sessions were delivered by qualified and experienced (duration not reported) social workers. Comparator: TAU. Just over half (n = 108; 54.0%) were referred to their GP, one‐third (n = 66; 33.0%) were referred to psychiatric services, and 26 (13.0%) received an unspecified referral. Length of treatment: three months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH as according to hospital records; ii) depression as measured by the BDI; iii) social functioning as measured by an idiosyncratic scale; iv) treatment satisfaction according to self‐report. | |
| Notes | Source(s) of funding: “The study was supported by the Department of Health and Social Security, and the Wessex Regional Health Authority” (Gibbons 1978, p. 117). Conflict(s) of interests: no information reported. | |
Gratz 2006.
| Study characteristics | ||
| Methods | Participants were individually randomised using an unspecified method to either group‐based emotion regulation therapy or TAU. N lost to follow‐up: 2/24 (8.3%) for repetition of SH data by the post‐intervention assessment. Location: Boston, MA, USA. |
|
| Participants |
Number of total participants: 24 participants were allocated, 13 were allocated to group‐based emotion regulation therapy and 11 were allocated to TAU. Profile of participants: mean age 33.3 ± 12.2 (range: 18 to 60 years). All (n = 24; 100%) were female, had a history of SH (i.e. multiple episodes of SH), and were diagnosed with BPD. Source of participants: clinician referrals and self referrals from advertisements posted at a hospital and on two websites. All had engaged in an episode of SH presenting to clinical services within the six months preceding trial entry. Inclusion criteria: i) diagnosed with BPD; ii) history of SH resulting in presentation to clinical services, with ≥ 1 episode in the six months preceding trial entry; iii) have an individual therapist; iv) aged 18 to 60 years; v) female. Exclusion criteria: i) diagnosed with psychosis, bipolar I disorder, or SUD; ii) at immediate suicide risk (i.e. made a suicide attempt rated as having a ’high’ risk of death or greater within the six months preceding trial entry); iii) at risk of attempting suicide within the next year; iv) received DBT in the six months preceding trial entry. |
|
| Interventions |
Intervention: group‐based emotion regulation psychotherapy consisting of weekly (duration not reported) sessions. Therapeutic content is drawn from Acceptance and Commitment Therapy (ACT), DBT, and emotion‐focused therapy and includes: psychoeducation, identification of emotions, distress tolerance, emotional acceptance, behavioural activation, developing alternative coping strategies, impulse control, and identifying and clarifying valued directions. Participants also received weekly (one hour) sessions of individual therapy and TAU. The average number of hours spent in TAU per week was 2.1 ± 1.6. Sessions were delivered by therapists (no further information on expertise or experience was reported). Comparator: TAU consisting of weekly (more than one hour) sessions of individual therapy. In addition to individual therapy almost two‐thirds (32%) attended group‐based psychotherapy, and 9% attended self‐help groups (e.g. AA, NA). The average number of hours spent in TAU per week was 2.9 ± 2.8. Length of treatment: 14 weeks. |
|
| Outcomes | Primary outcome(s): i) repetition of SH according to self‐report using the DSHI; ii) anxiety as measured by the anxiety subscale of the DASS; iii) BPD symptomatology as measured by the Borderline Evaluation of Severity over Time (BEST); iv) depression as measured by the depression subscale of the DASS; v) emotion regulation as measured by the DERS; vi) emotional avoidance as measured by the Acceptance and Action Questionnaire (AAQ); vii) stress as measured by the stress subscale of the DASS. | |
| Notes | Source(s) of funding: ”This research was supported by the Psychosocial Fellowship of McLean Hospital, awarded to the first author“ (Gratz 2006, p. 25). Conflict(s) of interests: Although no author interests were reported, Prof Gratz developed emotion regulation group therapy. | |
Gratz 2014.
| Study characteristics | ||
| Methods | Participants were individually randomised, stratified by age, emotion dysregulation, number of lifetime episodes of SH, and GAF scores to either group‐based emotion regulation therapy or TAU. N lost to follow‐up: 0/61 (23.5%) for repetition of SH data by the post‐intervention assessment. Location: Jackson, MS, USA. |
|
| Participants |
Number of total participants: 61 participants were allocated, 31 were allocated to group‐based emotion regulation therapy and 30 were allocated to TAU. Profile of participants: mean age 33.2 ± 10.9 (range: 18 to 60 years). All (n = 61; 100%) were female, and had a history of SH. Over half (n = 38; 62.3%) were diagnosed with any anxiety disorder, half (n = 31; 50.0%) were diagnosed with any mood disorder, followed by PTSD (n = 22; 36.0%), any eating disorder (n = 8; 13.3%), and SUD (n = 1; 1.6%). Source of participants: referrals from clinicians to the emotion regulation group therapy and from self referrals in response to an advertisement posed both online and in the community. All had engaged in an episode of SH presenting to clinical services within the six months preceding trial entry. Inclusion criteria: i) aged 18‐60 years; ii) females; iii) diagnosed with threshold or subthreshold BPD; iv) history of repeated SH with ≥ 1 episode in the six months prior to trial entry; v) have one or more of the following: individual therapist, psychiatrist, case manager. Exclusion criteria: i) diagnosed with psychosis or bipolar I disorder; ii) current (past month) substance use. |
|
| Interventions |
Intervention: manualised group‐based (maximum of six participants per group) emotion regulation psychotherapy consisting of weekly (90 minutes) sessions. Therapeutic content is drawn from Acceptance and Commitment Therapy (ACT), DBT, and emotion‐focused therapy and includes: psychoeducation, identification of emotions, distress tolerance, emotional acceptance, behavioural activation, developing alternative coping strategies, impulse control, and identifying and clarifying valued directions. Participants also received weekly (one hour) sessions of individual therapy and TAU. The average number of hours spent in TAU per week was 2.1 ± 1.6. Sessions were delivered by doctoral‐level therapists who received a minimum of four months training in delivering group‐based emotion regulation psychotherapy. Comparator: TAU consisting of weekly (more than one hour) sessions of individual or group‐based therapy. Few participants (18%) received group‐based therapy, however. Most (> 70%) were receiving supportive or dynamic individual therapy, 19% were receiving CBT, none were receiving DBT. Length of treatment: 14 weeks. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to self‐report using the DSHI and the Self‐Harm Inventory (SHI); ii) BPD symptomatology as measured by the Zanarini Rating Scale for Borderline Personality Disorder (ZAN‐BPD) and the BEST; iii) depression as measured by the BDI and the depression subscale of the DASS. Secondary outcome(s): i) emotion regulation as measured by the DERS; ii) emotional avoidance as measured by the AAQ; iii) interpersonal problems as measured by the BPD‐related composite of the Inventory of Interpersonal Problems (IIP‐BPD); iv) quality of life as measured by the Quality of Life Inventory; v) social functioning as measured by the Sheehan Disability Scale (SDS). |
|
| Notes | Source(s) of funding: “This research was supported by National Institute of Mental Health Grant R34 MH079248, awarded to Dr. Gratz” (Gratz 2014, p. 2110). Conflict(s) of interests: Although no author interests were reported, Prof Gratz developed emotion regulation group therapy. | |
Grimholt 2015.
| Study characteristics | ||
| Methods | Participants were individually randomised to either structured GP management or TAU. N lost to follow‐up: 6/149 (4.0%) for repetition of SH at the post‐intervention assessment according to hospital records, or 26/149 (17.5%) according to emergency department records. Location: Oslo and Akershus County, Norway. |
|
| Participants |
Number of total participants: 202 participants were randomised, 101 were allocated to structured GP follow‐up and 101 were allocated to TAU. However, data on repetition of SH were only available for analysis for up to 59.4% of those allocated to the intervention arm and 82.2% of those allocated to TAU. Profile of participants: mean age 38.2 (SD not reported; range: 18 to 75 years). Just under three‐quarters (n = 111; 74.5%) were female. Over one‐third (n = 58; 38.9%) had a history of SH (i.e. multiple episodes of SH). Information on psychiatric diagnoses were not reported. Source of participants: patients admitted to the acute medical wards of any of five hospitals following an episode of self‐poisoning. Inclusion criteria: i) 18‐75 years of age; ii) admitted to the acute medical ward following an episode of self‐poisoning. Exclusion criteria: i) diagnosed with psychosis, an intellectual disability, or organic cognitive impairment; ii) insufficient language ability; iii) not registered with a GP (includes non‐native citizens); iv) referred for inpatient psychiatric or other (e.g. AOD) treatment. |
|
| Interventions |
Intervention: structured GP follow‐up consisting of one follow‐up GP appointment within one‐week post‐discharge, one GP consultation per month for the first three months of the intervention (i.e. months one to three), and two further GP consultations in the final three months of the intervention (i.e. months four to six). Sessions were delivered by GPs (no further information on experience reported). Comparator: referral to outpatient psychiatric, AOD, and/or family counselling, as needed. TAU did not preclude GP management. Length of treatment: six months. |
|
| Outcomes |
Primary outcome(s): i) suicidal ideation as measured by the BSSI. Secondary outcome(s): i) depression as measured by the BDI; ii) hopelessness as measured by the BHS; iii) repetition of SH as ascertained from self‐report supplemented by medical records. |
|
| Notes |
Source(s) of funding: "The trial was funded by the Norwegian Southern Eastern Health Authority and the Regional Centre of Traumatic Stress and Suicide Prevention, Eastern Norway" (Grimholt 2015, pp.1‐2). Conflict(s) of interest: "The authors have declared that no competing interests exist" (Grimholt 2015, p.2). |
|
Guthrie 2001.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated list to either CBT‐based psychotherapy or TAU. N lost to follow‐up: 0/119 (0%) for repetition of SH by the six‐month assessment. Location: Manchester, UK. |
|
| Participants |
Number of total participants: 119 participants were allocated, 58 were allocated to CBT‐based psychotherapy and 61 were allocated to TAU. Profile of participants: mean age 31.2 ± 1.5 (range: not reported). Just over half (n = 66; 55.5%) were female, had a history of SH (i.e. multiple episodes of SH) (n = 71; 59.7%), and a history of previous psychiatric treatment (n = 65; 54.6%); however, information on psychiatric diagnoses was not reported. Source of participants: patients presenting to hospital after an episode of self‐poisoning most commonly involving acetaminophen/paracetamol (n = 43; 36.1%). Inclusion criteria: i) aged 18‐65 years; ii) presenting with episode of self‐poisoning; iii) sufficient language ability; iv) living in the catchment area; v) registered with a GP. Exclusion criteria: i) requiring immediate psychiatric treatment. |
|
| Interventions |
Intervention: individual CBT‐based psychotherapy consisting of weekly (50 minute) sessions of home‐based psychodynamic interpersonal therapy. Therapeutic content included: resolving interpersonal difficulties causing distress through a conversational approach, identification of feelings and relating these to problems and relationships, and developing shared understanding and approaches to resolving family problems. Sessions were delivered by nurse therapists (no further information on experience was reported). Comparator: TAU. In most cases, this involved assessment by doctor in the ED and referral to psychiatry outpatient treatment, addiction services, or GP, where required. Length of treatment: 4 weeks. |
|
| Outcomes |
Primary outcome(s): i) suicidal ideation as measured using the BSSI. Secondary outcome(s): i) repetition of SH as ascertained by self‐report supplemented by hospital records; ii) depression as measured using the BDI; iii) service use as ascertained from records; iv) treatment satisfaction as measured by an idiosyncratic scale; v) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: “North West Regional Health Authority and the NHS Research and Development Levy” (Guthrie 2001, p. 4). Conflict(s) of interest: none reported. | |
Gysin‐Maillart 2016.
| Study characteristics | ||
| Methods | Participants were individually randomised using Zelen's post‐consent method to either 24 months of a CBT‐based program (ASSIP) in addition to a remote contact intervention or TAU. N lost to follow‐up: 0/120 (0%) for repetition of SH at post‐intervention. Location: Bern, Switzerland. |
|
| Participants |
Number of total participants: 120 participants were randomised, 60 were allocated to the multi‐component ASSIP program and 60 were allocated to TAU. Profile of participants: mean age 38.2 ± 14.0 years; range: 18 to 75 years). Over half (n = 66; 55.0%) were female. Half (n = 60; 50.0%) had a history of SH (i.e. multiple episodes of SH). Most (n = 76; 63.3%) were diagnosed with any mood disorder, followed by SUD (n = 30; 25.0%), and any PD (n = 20; 16.7%). Source of participants: patients admitted to the ED for an episode of SH. Inclusion criteria: i) referred for in‐ or outpatient treatment; ii) sufficient language ability; iii) able to provide written informed consent. Exclusion criteria: i) diagnosed with psychosis; ii) in custody or imprisoned; iii) insufficient language ability. |
|
| Interventions |
Intervention: mixed multimodal intervention (CBT‐based program together with a remote contact). The Attempted Suicide Short Intervention Program (ASSIP) comprises three weekly sessions (60‐90 minutes) comprising cognitive case conceptualisation based on a vulnerability‐trigger model, psychoeducation, collaborative safety planning, and relapse prevention. A fourth session (60‐90 mins) can be added as necessary. Participants also receive personalised letters at 1, 3, 6, 9, 12, 18, and 24 months' post‐discharge. Sessions were delivered by psychiatrists, psychologists, and other therapists with an average of two years experience working with suicidal persons and who received training (one week) in delivering ASSIP. Comparator: TAU comprising a one‐off structured risk assessment, a summary of which was sent to the participant's usual care coordinator. Concomitant medications: were permitted. Around half were prescribed antidepressants (n = 56; 46.7%), followed by antipsychotics (n = 21; 17.5%), tranquillisers (both major and minor; n = 15; 12.5%), and other medications (not specified; n = 13; 10.8%). Length of treatment: 24 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from self‐report supplemented by collateral informants (e.g. GPs) and medical records. Secondary outcome(s): i) suicidal ideation as measured by the BSSI; ii) healthcare utilisation (unclear how measured); iii) depression as measured by the BDI; iv) therapeutic alliance as measured by the Penn Helping Alliance Questionnaire; v) suicide as ascertained from collateral informants (e.g. GPs) and medical records. |
|
| Notes |
Source(s) of funding: "The authors received no specific funding for this work (Gysin‐Maillart 2016, p.1). Conflict(s) of interest: "KM and AGM received royalties from Hogrefe Publishing for "ASSIP—Attempted Suicide Short Intervention Program: A Manual for Clinicians. K. Michel & A. Gysin‐Maillart (2015)" (Gysin‐Maillart 2016, p.1). |
|
Harned 2014.
| Study characteristics | ||
| Methods | Participants were individually randomised using a minimisation procedure stratified for number of suicide attempts/episodes of NSSI (past year), PTSD symptom severity, dissociative symptom severity, and current use of any SSRI to either DBT (prolonged‐exposure protocol) or DBT (standard protocol). N lost to follow‐up: 8/26 (30.8%) for repetition of SH data at the post‐intervention assessment. Location: Seattle, WA, USA. |
|
| Participants |
Number of total participants: 26 participants were allocated, 19 were allocated to DBT (prolonged protocol) and 7 were allocated to DBT (standard protocol). Profile of participants: mean age 32.6 ± 12.0 (range: 19‐55 years). All (n = 26; 100%) were female, and were diagnosed with comorbid PTSD and BPD. Source of participants: patients seeking treatment from a specialist treatment service for suicidal individuals with comorbid BPD and PTSD. Inclusion criteria: i) female; ii) aged 18‐60 years; iii) diagnosed with BPD; iv) diagnosed with PTSD; v) has satisfactory recall of at least part of the index trauma; vi) recent and recurrent SH (i.e. ≥ 2 suicide attempts or episodes of NSSI in the previous five years, with ≥ 1 within the eight weeks preceding trial entry); vii) lives within commuting distance. Exclusion criteria: i) diagnosed with psychosis, bipolar disorder, or mental retardation; ii) receiving treatment under legal mandate; iii) require treatment for another life‐threatening condition (e.g. anorexia nervosa). |
|
| Interventions |
Intervention: DBT (prolonged‐exposure protocol) consisting of either one combined individual therapy session per week (90 minutes) or two individual therapy sessions per week delivered by the same therapist (90 min), one group‐based skills session (60 minutes), and telephone consultation, as required. Therapeutic content was the same as standard DBT and included: identification of emotions, targeting problems that may occur during or as a result of exposure to trauma, targeting trauma‐related shame, dialectics, irreverence, self‐disclosure, and validation. Sessions were delivered by masters‐level clinicians (doctoral‐level students in training, licensed professionals, or postdoctoral fellows) with an average of two years of clinical experience and who received training (one day) in delivering DBT. Comparator: standard DBT consisting of either one combined individual therapy session per week (30 minutes) or two individual therapy sessions per week delivered by the same therapist (60 minutes), one group‐based skills session (60 minutes), and telephone consultation, as required. Therapeutic content was the same as above. Concomitant medication(s): were permitted, however, "...patients on SSRIs were asked to either taper off the medication before starting...or remain at a constant dose..." (Harned 2014, p.10). Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from self‐report using the SASII; ii) PTSD symptoms as measured by the PSS‐I. Secondary outcome(s): i) anxiety as measured by the Hamilton Rating Scale for Anxiety (HRSA); ii) depression as measured by the HDRS; iii) dissociative experiences as measured by the Dissociative Experiences Scale‐Taxon (DES‐T); iv) general psychological well‐being as measured by the GSI; v) shame as measured by the Experience of Shame Scale (ESS); vi) trauma‐related guilt cognitions as measured by the Trauma‐ Related Guilt Inventory (TRGI). |
|
| Notes | Source(s) of funding: “This work was supported by grant R34MH082143 from the National Institute of Mental Health” (Harned 2014, p. 16). Conflict(s) of interest: “Drs. Harned, Korslund, and Linehan are trainers and consultants for Behavioral Tech, LLC” (Harned 2014, p. 16). | |
Hassanian‐Moghaddam 2011.
| Study characteristics | ||
| Methods | Participants were individually randomised using a blocking procedure and a random numbers table to either a remote contact intervention (postcards) in addition to TAU or TAU alone. N lost to follow‐up: 187/2300 (8.1%) for repetition of SH at post‐intervention. Location: Tehran, Iran. |
|
| Participants |
Number of total participants: 2300 participants were allocated, 1150 were allocated to the remote contact intervention (postcards) and 1150 were allocated to TAU. Profile of participants: mean age 24.1 ± 8.1 years (range: not reported). Over half (n = 1402; 66.4%) were female. Just under one‐third (n = 723; 31.4%) had a history of SH (i.e. multiple episodes of SH). No information was reported on psychiatric diagnoses. Source of participants: patients admitted or transferred to a specialist hospital for the treatment of poisoning following an episode of self‐poisoning. Inclusion criteria: i) aged 12 years or older; ii) admitted or transferred to a specialist hospital for the treatment of poisoning following an episode of self‐poisoning. Exclusion criteria: i) treated in the ED of a general hospital; ii) diagnosed with psychosis; iii) unable to provide informed consent (e.g. due to insufficient language ability); iv) no fixed address; v) posed a potential threat to interviewers; vi) episode of self‐poisoning was classified by the attending toxicologist as recreational, habitual, accidental, or iatrogenic. |
|
| Interventions |
Intervention: remote contact intervention consisting of a series of postcards mailed at one, two, three, four, six, eight, 10 and 12 months' post‐discharge in addition to TAU. Postcards encouraged participants to make contact with the service, if required. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: TAU. Although no specific details were provided, the authors noted that “[f ]ollow‐up care for self‐poisoning in Tehran is generally poor...Contact is mainly hospital‐ or office‐based, and community‐based programs are almost non‐existent. Psychiatric beds are often at 100% occupancy, with short admissions and frequent readmissions.” (Hassanian‐Moghaddam 2011, pp. 310‐311). Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to self‐report supplemented by hospital records; ii) suicidal ideation (according to self‐report). Secondary outcome(s): i) suicide (unclear how ascertained); ii) treatment adherence as ascertained by the number receiving the postcard; iii) satisfaction with treatment as ascertained by the number reporting the postcard was useful in the prevention of SH; iv) all‐cause mortality (unclear how ascertained). |
|
| Notes | Source(s) of funding: “This study was supported by a grant from the Legal Medicine Organization of Iran and the Loghman‐Hakim Research Development Unit, Shahid Beheshti Medical University” (Hassanian‐Moghaddam 2011, p. 315). Conflict(s) of interest: none reported. | |
Hatcher 2011.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated numbers list and Zelen's method to either CBT‐based psychotherapy in addition to TAU or TAU alone. N lost to follow‐up: 0/552 (0%) (of those consenting) by for repetition of SH by the 12‐month assessment. Location: Auckland and Wellington, New Zealand. |
|
| Participants |
Number of total participants: 552 participants were allocated, 253 were allocated to CBT‐based psychotherapy and 299 were allocated to TAU. Profile of participants: mean age 33.7 ± 12.9 years (range: not reported). Over two‐thirds (n = 380; 68.8%) were female. Just under half (n = 247; 44.7%) had a history of SH (i.e. multiple episodes of SH). Source of participants: patients admitted to hospital following an episode of SH. Inclusion criteria: i) aged 16 years or older; ii) admitted to hospital following an episode of SH. Exclusion criteria: i) enrolled full time in school; ii) receiving DBT for the treatment of BPD; iii) have a treatment management plan which precludes short‐term therapy; iv) cognitively impaired; v) admitted to a psychiatric care unit following the index episode of SH for a minimum period of 48 hours. |
|
| Interventions |
Intervention: manualised CBT‐based psychotherapy based on D'Zurilla 1971 consisting of up to nine (60 minutes) sessions of PST. Therapeutic content included: problem orientation, problem listing and definition, brainstorming, devising an action plan, and reviewing the plan. Sessions were delivered by clinicians (social workers, psychotherapists, counselling and health psychologists) who did not have extensive experience working in mental health settings and who received training (one week) in delivering problem‐solving psychotherapy. Comparator: TAU involving a one‐off psychosocial assessment by a mental health professional, as well as referral to multidisciplinary teams for psychiatric or psychological intervention, referral to mental health crisis teams, recommendations for engagement with AOD centres or other health and non‐health services, as required. Length of treatment: three months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to hospital records; ii) time to repetition of SH according to hospital records. Secondary outcome(s): i) anxiety as measured by the anxiety subscale of the HADS; ii) depression as measured by the depression subscale of the HADS; iii) hopelessness as measured by the BHS; iv) social functioning as measured by the Social Problem‐Solving Inventory Scale (SPSI); v) suicidal ideation as measured by the BSS: vi) suicide (ascertained from Coroner's records). |
|
| Notes | Source(s) of funding: “This study was funded by the Accident Compensation Corporation of New Zealand” (Hatcher 2011, p. 316). Conflict(s) of interest: none reported. | |
Hatcher 2015.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated sequence, stratified by history of SH and method of SH, using Zelen's method, to either a multimodal intervention or TAU. N lost to follow‐up: 0/1474 (0%) (of those consenting) for repetition of SH by the post‐intervention assessment. Location: Waitemata, Manukau, Northland, and Waikato regions, New Zealand. |
|
| Participants |
Number of total participants: 684 participants were allocated, 327 were allocated to the multimodal intervention and 357 were allocated to TAU. Profile of participants: mean age 36.8 ± 14.4 (range: not reported). Over half (n = 464; 67.8%) were female and had a history of SH (i.e. multiple episodes of SH) (n = 370; 54.1%). Information on psychiatric diagnoses not reported. Source of participants: patients admitted to hospital following an episode of SH. Inclusion criteria: i) presented to the ED following an episode of SH. Exclusion criteria: i) aged less than 17 years; ii) enrolled full time in school; iii) unable to provide informed consent; iv) self‐identifies as Māori (these participants were instead invited to participate in the Hatcher 2016 trial). |
|
| Interventions |
Intervention: multimodel intervention consisting of one to two face‐to‐face or telephone patient support sessions (duration not reported) over the fortnight following discharge from hospital to ensure patients were adhering to their agreed discharge plan; four to six sessions (duration not reported) of PST (based on D'Zurilla 1971) in the four weeks following the index SH episode; postcards mailed at one, two, three, four, six, eight, 10 and 12 months following the index SH episode; improved access to primary care via the provision of a voucher that could be used to access one free GP consultation (duration not reported); development of a risk management strategy; and a cultural assessment focused on identifying patients’ sense of belonging and identification with their ethnic group. Sessions were delivered by research clinicians (no further information on their expertise or experience was reported). Comparator: TAU consisting of referral to multidisciplinary teams for psychiatric/psychological assessment, intervention, or both; referral to crisis teams; or referral to community‐based AOD treatment teams, as required. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from electronic medical records. Secondary outcome(s): i) repetition of SH as ascertained from self‐report; ii) anxiety as measured by the anxiety subscale of the HADS; ii) belonging as measured by the Sense of Belonging Instrument; iii) depression as measured by the depression subscale of the HADS; iv) hopelessness as measured by the BHS; v) quality of life as measured by the EQ‐5D; vi) service use as measured by self‐report supplemented by electronic medical records; vii) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: none reported. Conflict(s) of interests: none reported. | |
Hatcher 2016.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated sequence, stratified by history of SH and method of SH, using Zelen's method, to either a multimodal intervention or TAU. N lost to follow‐up: 0/365 (0%) for repetition of SH by the post‐intervention assessment. Location: Waitemata, Manukau, and Northland regions, New Zealand. |
|
| Participants |
Number of total participants: 365 participants were allocated, 182 were allocated to the multimodal intervention and 183 were allocated to TAU. Profile of participants: mean age 32.3 ± 10.7 (range: not reported). Over two‐thirds (n = 109; 65.3%) were female, and over half (n = 100; 59.9%) had a history of SH (i.e. multiple episodes of SH). Information on psychiatric diagnoses not reported. Source of participants: patients admitted to hospital following an episode of SH. Inclusion criteria: i) presented to the ED following an episode of SH; ii) self‐identifies as Māori; iii) sufficient language ability to communicate in te reo Maori (Māori language). Exclusion criteria: i) aged less than 17 years; ii) enrolled full time in school; iii) unable to provide informed consent. |
|
| Interventions |
Intervention: culturally‐adapted multimodel intervention consisting of one to two face‐to‐face or telephone patient support sessions (duration not reported) over the fortnight following discharge from hospital to ensure patients were adhering to their agreed discharge plan; four to six sessions (duration not reported) of PST (based on D'Zurilla 1971) in the four weeks following the index SH episode; postcards mailed at one, two, three, four, six, eight, 10 and 12 months following the index SH episode; improved access to primary care via the provision of a voucher that could be used to access one free GP consultation (duration not reported); development of a risk management strategy; and a cultural assessment focused on identifying patients’ sense of belonging and identification with Māori culture. Sessions were delivered by research clinicians (no further information on their expertise or experience was reported). Comparator: TAU consisting of referral to multidisciplinary teams for psychiatric/psychological assessment, intervention, or both; referral to crisis teams; or referral to community‐based AOD treatment teams, as required. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from electronic medical records. Secondary outcome(s): i) repetition of SH as ascertained from self‐report; ii) anxiety as measured by the anxiety subscale of the HADS; ii) belonging as measured by the Sense of Belonging Instrument; iii) depression as measured by the depression subscale of the HADS; iv) cultural identity as measured by the Cultural Impact Profile (CIP) which is a Maori‐specific measure of cultural knowledge and practice; v) hopelessness as measured by the BHS; vi) quality of life as measured by the EQ‐5D and the Social Functioning‐36 item (SF‐36); vii) service use as measured by self‐report supplemented by electronic medical records; viii) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: none reported. Conflict(s) of interests: none reported. | |
Hawton 1981.
| Study characteristics | ||
| Methods | Participants were individually randomised using sealed, opaque envelopes to either home‐based psychotherapy and telephone contact or an alternative form of psychotherapy. N lost to follow‐up: 0/96 (0%) for repetition of SH by the 12‐month assessment. Location: Oxford, UK. |
|
| Participants |
Number of total participants: 96 participants were allocated, 48 were allocated to home‐based psychotherapy and telephone contact and 48 were allocated to alternative psychotherapy. Profile of participants: mean age 25.2 ± 8.2 (range: not reported). The majority (n = 67; 69.8%) were female, and just under one‐third (n = 31; 32.3%).and had a history of SH (i.e. multiple episodes of SH). Information on psychiatric diagnoses not reported. Source of participants: patients admitted to a general hospital following an episode of self‐poisoning. Inclusion criteria: i) aged over 16 years; ii) suitable for randomisation (e.g. fixed address). Exclusion criteria: i) in psychiatric care; ii) residing outside the catchment area; iii) requiring treatment for AOD addiction; iv) referred for inpatient psychiatric care. |
|
| Interventions |
Intervention: mixed domiciliary (home‐based) therapy where the frequency of treatment sessions was flexible (i.e. according to therapists’ ’assessment of needs’). Mean number of sessions was 4.3 (range: one to eight). Mean duration of sessions was 45.0 ± 7.8 minutes. Open telephone access to the general hospital service was also available, as required. Therapeutic content included: brief problem‐oriented counselling, problem‐solving, and family involvement (as appropriate). Sessions were delivered by junior psychiatrists, psychiatric nurses, or social workers (no further information on experience was reported). Comparator: alternative psychotherapy consisting of weekly sessions (mean 4.9, range: one to ten) of outpatient therapy. Mean duration of sessions was 47.0 ± 8.3 minutes. Concomitant medication(s): were permitted "...although this was rarely necessary" (Hawton 1981, p.170). Specific information on the medication(s) prescribed was not reported. Length of treatment: up to three months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to hospital records, self‐report, and from a GP questionnaire. Secondary outcome(s): i) depression as measured using a modification of the Lorr and McNair Mood Scale; ii) improvement in problems as measured by an idiosyncratic scale; iii) social functioning as measured using a modification of the Social Adjustment Scale; iv) treatment adherence as measured by the number that completed treatment; v) suicidal ideation as measured by the BSSI. Tertiary outcome(s): i) number of GP visits as ascertained from a questionnaire sent to GPs. |
|
| Notes | Source(s) of funding: “The project was supported by a grant from the Department of Health and Social Security” (Hawton 1981, p. 177). Conflict(s) of interest: none reported. | |
Hawton 1987.
| Study characteristics | ||
| Methods | Participants were individually randomised using a random numbers table to either CBT‐based psychotherapy or TAU. N lost to follow‐up: 0/80 (0%) for repetition of SH by the 12‐month assessment. Location: Oxford, UK. |
|
| Participants |
Number of total participants: 80 participants were allocated, 41 were allocated to CBT‐based psychotherapy and 39 were allocated to TAU. Profile of participants: mean age 29.3 years (SD not reported; range: not reported). Almost two thirds (n = 53; 66.3%) were female, and just under one‐third (n = 25; 31.3%).and had a history of SH (i.e. multiple episodes of SH). Information on psychiatric diagnoses not reported. Source of participants: patients admitted to a general hospital following an episode of self‐poisoning. Inclusion criteria: i) aged 16 years or older; ii) registered with a GP; iii) living up to 15 miles away from hospital; iv) suitable for outpatient counselling; iv) willing to accept aftercare offered. Exclusion criteria: i) in need of psychiatric care (day‐patient or inpatient); ii) currently receiving psychiatric care. |
|
| Interventions |
Intervention: outpatient CBT‐based psychotherapy consisting of up to eight sessions (54 minutes) of PST. No specific detail on therapeutic content reported. Sessions were delivered by counsellors from the clinical team in the general hospital psychiatric service (no further information on experience was reported). Comparator: GP management consisting of individual support, marriage counselling, and/or psychiatric referral, as required. No information on the number of sessions or their duration reported. Length of treatment: not reported. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to hospital records, self report, collateral informant report, and/or from a GP questionnaire. Secondary outcome(s): i) depression as measured by the BDI; ii) improvement in problems as measured by an idiosyncratic scale; iii) social functioning as measured by the Social Adjustment Scale; iv) symptomatology as measured by the GHQ; v) treatment adherence as measured by the number that completed treatment; vi) treatment attitudes as measured by self‐report; vii) suicide (unclear how ascertained). Tertiary outcome(s): i) number of GP visits as ascertained from a questionnaire sent to GPs. |
|
| Notes | Sources of funding: “This study was supported by a grant from the Medical Research Council” (Hawton 1987, p. 760). Conflict(s) of interest: none reported. Other: As compliance data were not reported for the comparator arm, this outcome had to be excluded from subsequent analyses. | |
Husain 2014.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated list to either culturally adapted CBT‐based psychotherapy or TAU. N lost to follow‐up: 8/221 (3.6%) for repetition of SH by the six‐month assessment. Location: Karachi, Sindh province, Pakistan. |
|
| Participants |
Number of total participants: 221 participants were allocated, 108 were allocated to CBT‐based psychotherapy and 113 were allocated to TAU. Profile of participants: mean age 23.1 ± 5.5 (range: 16‐64 years). Over two‐thirds (n = 53; 66.3%) were female. A minority (n = 9; 4.1%) had a history of SH (i.e. multiple episodes of SH). Information on psychiatric diagnoses not reported. Source of participants: patients admitted to the medical unit at university hospitals following an episode of SH. Inclusion criteria: i) aged 16‐64 years; ii) living within the catchment area. Exclusion criteria: i) referred for inpatient psychiatric treatment; ii) temporarily resident in the catchment area; iii) diagnosed with a psychiatric disorder due to a general medical condition, substance misuse, dementia, delirium, substance dependence, schizophrenia, bipolar disorder, or an intellectual disability according to DSM‐IV criteria. |
|
| Interventions |
Intervention: manualised, culturally‐adapted CBT‐based psychotherapy consisting of six sessions (50 minutes). The first two sessions were held weekly, followed by fortnightly. Therapeutic content included: an evaluation of the SH episode, development of crisis management skills, use of problem‐solving and cognitive‐behavioural techniques to improve emotion regulation skills, negative thinking, interpersonal relationships, and relapse prevention. Sessions were delivered by qualified, masters‐level psychologists with a minimum of three years post‐qualifying clinical experience and who also received training (duration not reported) in delivering the intervention. Comparator: TAU. The authors further clarified that “[p]atients are not routinely referred to psychiatric or psychological services” (Husain 2014, p. 464). Length of treatment: three months. |
|
| Outcomes |
Primary outcome(s): i) suicidal ideation as measured by the BSSI. Secondary outcome(s): i) repetition of SH as ascertained from self‐report using the SASII; ii) coping as measured by the Coping Resource Inventory; iii) depression as measured by the BDI; iv) hopelessness as measured by the BHS; v) quality of life as measured by the EQ‐5D; vi) service use as measured by the Client Service Receipt Inventory; vii) treatment adherence as measured by the number of sessions attended; viii) days spent in inpatient treatment; ix) attendances at outpatient clinics; x) GP consultations; xi) consultations with any other doctors; xii) consultations with non‐medical religious healers; xiii) consultations with non‐medical homeopathic healers. |
|
| Notes | Source(s) of funding: “This study was jointly funded by the University of Manchester and Pakistan Institute of Learning and Living” (Husain 2014, p. 469). Conflict(s) of interest: none reported. | |
Hvid 2011.
| Study characteristics | ||
| Methods | Participants were individually randomised, stratified by sex, history of SH, history of previous psychiatric treatment, and use of alcohol during the index SH to either case management or TAU. N lost to follow‐up: 0/133 (0.0%) for repetition of SH by the post‐intervention assessment. Location: Amager, Denmark. |
|
| Participants |
Number of total participants: 133 participants were allocated, 69 were allocated to assertive outreach and 64 were allocated to TAU. Profile of participants: mean age 37.5 ± 18.2 (range: not reported). Almost three‐quarters (n = 95; 71.4%) were female. Over one‐third (n = 51; 38.3%) had a history of SH (i.e. multiple episodes of SH) and a history of previous psychiatric treatment (n = 49; 36.8%); however, information on psychiatric diagnoses was not reported. Source of participants: patients admitted to an emergency or clinical department following an episode of SH. Inclusion criteria: i) admitted to an emergency department or clinical department following an episode of SH. Exclusion criteria: i) less than 12 years old; ii) diagnosed with any major psychiatric illness, including: schizophrenia, other psychoses, bipolar disorder, major depression, psychotic depression, mental retardation, and severe dementia; iii) insufficient language ability. |
|
| Interventions |
Intervention: case management consisting of assertive outreach delivered according to the Baerum model, involving: assertive outreach via home visits (mean number of home visits was eight, range three to 22), telephone calls, email messages, and text messages (range five to 36), sessions (number and duration not reported) of solution‐focused PST, adherence therapy, and treatment continuity as participants were contacted by the same psychiatric nurse (as far as practical) throughout the course of treatment. Sessions were delivered by consultant‐level psychiatrists or psychiatric nurses (no further information on experience was reported). Comparator: TAU involving encouraging participants to contact their GP who could, where required, refer the participant on to further psychiatric or psychological treatment. Length of treatment: maximum period of six months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH according to clinical records; ii) suicide according to Coroner's records. | |
| Notes | Source(s) of funding: “The trial has been funded by a grant from the Danish Ministry of Social Affairs, the Lundbeck Foundation and the Health Insurance Foundation” (Hvid 2011, p. 297). Conflict(s) of interests: none reported. | |
Kapur 2013.
| Study characteristics | ||
| Methods | Participants were individually randomised using web‐based software to a remote contact intervention (postcards) or TAU. N lost to follow‐up: 1/66 (1.5%) at post‐intervention. Location: Manchester, UK. |
|
| Participants |
Number of total participants: 66 participants were allocated, 33 were allocated to the remote contact intervention (postcards) and 33 were allocated to TAU. Profile of participants: not reported, although the authors noted “[i]ntervention and usual treatment groups were similar in terms of age, gender” (Kapur 2013, p. 73). Just over half (n = 39; 59.1%) had a history of SH (i.e. multiple episodes of SH prior to trial entry). Source of participants: patients presenting to ED following an episode of SH. Inclusion criteria: i) i) aged 18 or older; ii) resident in the catchment area; iii) presenting to ED following an episode of SH. Exclusion criteria: i) referred for admission to a psychiatric unit; ii) without a telephone; iii) admitted to a general hospital for a period of greater than seven days; iv) living outside of the catchment area; v) deterioration in psychosis symptoms; vi) denies SH; vii) declined to participate. |
|
| Interventions |
Intervention: remote contact intervention consisting of a series of postcards mailed at one, two, four, six, eight, and 12 months post‐discharge, an information leaflet listing both local and national sources of support, and two semi‐structured telephone calls to facilitate referral to appropriate specialist treatment, as required, in addition to TAU. Postcards encouraged participants to make contact with the service, if required. Sessions were delivered by clinical researchers (no further information on expertise or experience was reported). Comparator: TAU consisting of referral to mental health services, social services, or voluntary sector services, as required. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from hospital records; ii) frequency of SH as ascertained from hospital records. Secondary outcome(s): i) number of ED attendances; ii) number of days on a medical inpatient ward; iii) number of face‐to‐face contacts with mental health services; iv) number of admissions to psychiatric inpatient services; v) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: “commissioned by the National Institute for Health Research (NIHR) under its Program Grants for Applied Research scheme (RP‐PG‐0606‐1247)” (Kapur 2013, p. 74) Conflict(s) of interest: “N.K. chaired the National Institute for Health and Clinical Excellence (NICE) guideline development group and evidence for the longer‐term management of self‐harm. N.K., D.G., K.H. are members of the National Suicide Prevention Strategy Advisory Group” (Kapur 2013, p. 73). | |
Kawanishi 2014.
| Study characteristics | ||
| Methods | Participants were individually randomised using web‐based software using minimisation stratified by site, age, and history of SH to either assertive outreach and case management or EUC. N lost to follow‐up: 0/914 (0%) for repetition of SH by the 18‐month assessment. Location: various sites, Japan. |
|
| Participants |
Number of total participants: 914 participants were allocated, 460 were allocated to case management and assertive outreach and 454 were allocated to EUC. Profile of participants: mean age 42.3 ± 14.9 years (range: not reported). Over half (n = 514; 56.2%) were female, and just under half (n = 450; 49.2%) had a history of SH (i.e. multiple episodes of SH). Information on psychiatric diagnoses reported in a separate publication (Furuno 2018); under half (n = 426; 46.6%) were diagnosed with any mood disorder, adjustment disorder (n = 191; 20.9%), psychosis (n = 179; 19.6%), SUD (n = 45; 4.9%), and other disorders (unspecified) (n = 73; 8.0%). Source of participants: patients admitted to EDs following a suicide attempt. Inclusion criteria: i) aged 20 years or older; ii) admitted to EDs following a suicide attempt; iii) ≥ 2 previous suicide attempts rated as having definite suicidal intent as determined by scores on the Suicide Intent Scale; iv) diagnosed with any Axis I psychiatric disorder according to DSM‐IV‐TR criteria; v) able to understand the trial procedure; vi) able to provide informed consent; vii) able to attend a face‐to‐face interview; viii) able attend a psychoeducation session during the hospital admission. Exclusion criteria: i) diagnosed with any psychiatric disorder which did not meet DSM‐IV‐TR criteria. |
|
| Interventions |
Intervention: assertive outreach and case management involving contact with patients at week one and one, two, three, six, 12, and 18 months after the index suicide attempt with a view to collecting information about the participant’s treatment status and any problems that could interfere with treatment adherence. Therapeutic content included: providing encouragement to remain adherent with treatment, coordination and referral to appointments with psychiatrists and any other primary care physicians, outreach for those who had dropped out of treatment, referral to social services and other support organisations, as needed, psychoeducation, and access to a dedicated website designed to provide participants with information and resources. Sessions were delivered by psychiatrists, clinical psychologists, nurses, and social workers (no further information on experience was reported). Comparator: EUC. No further details on treatment content provided. Length of treatment: 18 months. |
|
| Outcomes |
Primary outcome(s): i) time to SH repetition (unclear how ascertained); ii) repetition of SH (unclear how ascertained); iii) suicide as ascertained from a mortality register; iv) all‐cause morality as ascertained from a mortality register. Secondary outcome(s): i) hopelessness as measured by the BHS; ii) quality of life as measured by the SF‐36; iii) service contacts as ascertained from records; iv) physical functioning (unclear how ascertained). |
|
| Notes |
Source(s) of funding: “This study was funded by the Ministry of Health, Labour, and Welfare of Japan” (Kawanishi 2014, p. 200).
Conflict(s) of interest: none reported. Other: The authors stated that for "[o]ther protocol‐specified secondary outcomes...We plan to publish results for all these outcomes in a separate report" (Kawanishi 2014, p. 196). |
|
Liberman 1981.
| Study characteristics | ||
| Methods | Participants were individually randomised (method not reported) to either a mixed intervention or alternative psychotherapy. N lost to follow‐up: 0/24 (0%) for repetition of SH at post‐intervention (including up to the 24‐month assessment). Location: Los Angeles, CA, USA. |
|
| Participants |
Number of total participants: 24 participants were allocated, 12 were allocated to a mixed intervention and 12 were allocated to alternative psychotherapy. Profile of participants: mean age 29.7 ± 8.8 years (range: 18‐47 years). Two thirds (n = 16; 66.6%) were female. All (n = 24; 100%) had a history of SH (i.e. multiple episodes of SH). Whilst all (n = 24; 100%) had previously received psychiatric treatment, information on psychiatric diagnoses was not reported. Source of participants: patients referred by psychiatric emergency services or hospital A&E following an episode of SH. Inclusion criteria: i) ≥ 1 suicide attempt preceding trial entry. Exclusion criteria: i) diagnosed with psychosis; ii) addicted to drugs and alcohol; ii) diagnosed with organic brain syndrome. |
|
| Interventions |
Intervention: inpatient treatment consisting of daily sessions (duration not reported). Therapeutic content included: behaviour therapy, social skills training, anxiety management, and family therapy. A therapeutic milieu with a token economy was also established. Aftercare at a community mental health centre or with a private therapist was also used, as required. Sessions were delivered by psychologists assisted by bachelors‐level technicians (no further information on experience was reported). Comparator: alternative psychotherapy (inpatient treatment involving insight‐oriented therapy) consisting of daily sessions (duration not reported). Therapeutic content included: individual therapy, group therapy and psychodrama, and family therapy. A therapeutic milieu with a token economy was also established. Aftercare at a community mental health centre or with a private therapist was also used, as required. Length of treatment: 10 days. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained by self‐report; ii) depression as measured by the Zung Self‐rating Depression Scale, the BDI, and the depression subscale of the Minnesota Multiphasic Personality Inventory (MMPI); iii) suicidal ideation as ascertained by self‐report. Secondary outcome(s): i) assertiveness as measured by the Assertiveness Questionnaire; ii) fear as measured by the Fear Survey Schedule; iii) reinforcement as measured by the Reinforcement Survey Schedule. |
|
| Notes | Source(s) of funding: “The project was made possible by grant MH 22804 from the Clinical Research Branch of the National Institute of Mental Health to Michael Serber, MD, and R.P.L., the co‐principal investigators” (Liberman 1981, p. 1130). Conflict(s) of interests: no information on interests reported. | |
Lin 2020.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computerised blocking procedure to either CBT‐based psychotherapy and standard case management or TAU. N lost to follow‐up: 3/150 (2.0%) for repetition of SH by the six‐ and 12‐month assessment. Location: Taipei and New Taipei City, Taiwan. |
|
| Participants |
Number of total participants: 147 participants were randomised, 75 were allocated to brief CBT‐based psychotherapy and standard case management, and 75 were allocated to TAU. Profile of participants: mean age 33.0 ± NR years (range: 18‐81 years). The majority (n = 106; 72.1%) were female. Over half had a history of SH (i.e. multiple episodes of SH) (n = 88; 59.9%). Most were diagnosed with an alcohol use disorder (n = 52; 38.2%), followed by major depression (n = 54; 36.7%), and bipolar disorder (n = 20; 14.0%). Source of participants: patients presenting to EDs following a suicide attempt. Inclusion criteria: i) 18 years of age or older; ii) reporting current suicidal ideation; iii) sufficient language ability; iv) able to provide informed consent; v) able to be contacted via mail or telephone. Exclusion criteria: i) medically or cognitively incapable of participating in the study procedure; ii) insufficient language ability; iii) receiving other research or psychotherapy. |
|
| Interventions |
Intervention: brief CBT‐based psychotherapy in addition to standard case management, consisting of up to six sessions (in person or via telephone) at weeks' one, two, four, seven, 11, and 15 post‐discharge. Session frequency could be increased to up to one per week, depending on risk. Mean duration of face‐to‐face sessions was 45.6 ± 14.9 minutes (range: 15‐70 minutes), whilst the mean duration of telephone sessions was 26.2 ± 10.5 minutes (range 13‐55 minutes). Therapeutic content included: a suicide risk assessment, safety planning, chain analysis, problem‐solving skills training, distress tolerance, and seeking resources. Sessions were delivered by case managers (no further information on expertise or experience was reported). Comparator: TAU consisting of admission to a general medical/surgical ward or a psychiatric ward (as needed), followed by referral to a specialist suicide prevention centre for ongoing outpatient psychiatric treatment (as required). Participants were not routinely referred for psychotherapy from this centre. Length of treatment: four months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from self‐report supplemented by information from medical records. Secondary outcome(s): i) psychiatric service use, as measured by the number of service contacts; ii) depression, as measured by the HAMD‐24; iii) hopelessness, as measured by the BHS; iv) suicidal ideation, as measured by the BSSI. |
|
| Notes |
Source(s) of funding: "This study was funded by the National Science Council of the Republic of China, Taiwan" (Lin 2020, pp. 693‐4). Conflict(s) of interest: none reported. |
|
Linehan 1991.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computerised procedure to either manualised DBT or TAU. N lost to follow‐up: 19/63 (30.2%) for repetition of SH by the post‐intervention assessment. Additionally, data for 24/63 (38.1%) participants were deliberately not included in the 24‐month follow‐up assessment. Location: Seattle, WA, USA. |
|
| Participants |
Number of total participants: 63 participants were randomised, 31 were allocated to DBT and 31 were allocated to TAU. Profile of participants: mean age not reported (range: 18‐45 years). All (n = 63; 100%) were female and had a history of SH (i.e. multiple episodes of SH). Source of participants: referred patients with ≥ 1 episode of SH in the 8 weeks preceding trial entry. Inclusion criteria: i) female; ii) aged 18‐45 years; iii) diagnosed with BPD; iv) ≥ 2 suicide attempts in the five years preceding trial entry with ≥ 1 in the eight weeks preceding trial entry; v) agree to trial conditions. Exclusion criteria: none reported. |
|
| Interventions |
Intervention: manualised DBT consisting of weekly (60 minutes) sessions of individual psychotherapy, and weekly (2.5 hours) sessions of group skills training, as well as telephone consultation, as required (within each therapists’ limitations), and weekly therapist team meetings. Therapeutic content included: DBT developed specifically for the treatment of suicidal patients with BPD, which targeted increasing behavioural capabilities and motivation for treatment whilst also reinforcing functional behaviour. Sessions were delivered by psychiatrists, psychologists, or clinical psychology graduates (no further information on experience was reported). Comparator: TAU consisting of referral to alternative therapy. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to self‐report using the Parasuicide History Interview. Secondary outcome(s): i) coping as measured by the Survival and Coping Scale; ii) depression as measured by the BDI; iii) hopelessness as measured by the BHS and the Reasons for Living Inventory; iv) service usage as ascertained from self‐report using the Treatment History Interview; v) suicidal ideation as measured by the BSSI; vi) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: ”This research was supported by grant MH34486 from the National Institute of Mental Health, Bethesda, Md (Dr Linehan)" (Linehan 1991, p.1064). Conflict(s) of interests: Although no information on conflicts of interests were reported, Dr. Linehan has developed dialectical behaviour therapy. Other: Half (50%) of the self‐reported episodes of SH were checked against medical records, therapist records, and observer/nurse/physician ratings. | |
Linehan 2006.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computerised adaptive minimisation procedure to either manualised DBT or alternative psychotherapy (treatment by experts). N lost to follow‐up: 4/101 (4.0%) for repetition of SH by the post‐intervention assessment. Location: Seattle, WA, USA. |
|
| Participants |
Number of total participants: 101 participants were randomised, 52 were allocated to DBT and 49 were allocated to alternative psychotherapy (treatment by experts). Profile of participants: mean age 29.3 ± 7.5 years (range: 18‐45 years). All (n = 101; 100%) were female and were diagnosed with BPD. Almost all (n = 97; 96.0%) were also diagnosed with MDD, followed by SUD (n = 88; 87.1%), any anxiety disorder (n = 54; 55.4%), any eating disorder (n = 40; 39.6%), avoidant PD (n = 21; 20.8%), and ASPD (n = 11; 10.9%). Source of participants: clinical referrals and individuals attending inpatient units, emergency rooms and outpatient clinics. Inclusion criteria: i) 18‐45 years; ii) female; iii) meets criteria for BPD; iv) ≥ 2 suicide attempts or episodes of SH in the five years preceding trial entry, with ≥ 1 in the eight weeks preceding trial entry. Exclusion criteria: i) lifetime diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder, psychotic disorder not otherwise specified, or mental retardation; ii) seizure disorder requiring medication; iii) legally mandated to treatment; iv) requiring primary treatment for another debilitating condition. |
|
| Interventions |
Intervention: manualised DBT consisting of weekly (60 minutes) sessions of individual psychotherapy, and weekly (2.5 hours) sessions of group skills training, as well as telephone consultation, as required (within each therapists’ limitations), and weekly therapist team meetings. Therapeutic content included: CBT developed specifically for the treatment of for suicidal patients with BPD which targeted increasing behavioural capabilities and motivation for treatment whilst also reinforcing functional behaviour. Sessions were delivered by trained doctoral‐level therapists (one‐quarter had over 10 years experience working with suicidal persons). Comparator: TAU consisting of community treatment by experts specifically designed for the trial to control for factors previously uncontrolled in DBT trials. Whilst similar to TAU, as therapists were free to decide on type and dose of therapy they believed was most suited to the patient (minimum of one scheduled individual session per week; duration not reported), the characteristics of therapists were controlled via selection of therapists and supervisory arrangements. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH according to self‐report using the SASII. Secondary outcome(s): i) medical severity of SH according to self‐report using the SASII; iii) hopelessness as measured by the Reasons for Living Inventory; iv) service usage as ascertained from self‐report. |
|
| Notes | Source(s) of funding: “This study was supported by grants MH34486 and MH01593 from the National Institute of Mental Health” (Linehan 2006; p. 765). Conflict(s) of interests: although no information on conflicts of interests were reported, Dr Linehan developed dialectical behaviour therapy. | |
Linehan 2015.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computerised adaptive procedure stratified by age, number of previous suicide attempts, number of previous episodes of NSSI, psychiatric hospitalisations (past year), and depression severity to either DBT plus group‐based skills training (Linehan 2015a), individual‐based DBT (Linehan 2015b), or standard manualised DBT. N lost to follow‐up: 0/99 (0%) for repetition of SH by the 12‐month assessment. Location: Seattle, WA, USA. |
|
| Participants |
Number of total participants: 99 participants were randomised, 33 were allocated to DBT plus group‐based skills therapy, 33 were allocated to individual‐based DBT, and 33 were allocated to standard DBT. Profile of participants: mean age 30.3 ± 8.9 years (range: 18‐60 years). All (n = 99; 100%) were female. The majority were diagnosed with any anxiety disorder (n = 81; 96.4%), followed by MDD (n = 70; 70.7%), any SUD (n = 37; 37.4%), and any eating disorder (n = 15; 15.1%). Almost three‐quarters (n = 73; 73.7%) were also diagnosed with a personality disorder; commonly avoidant personality disorder (n = 26; 26.3%). Source of participants: patients currently receiving treatment from outpatient mental health services. Inclusion criteria: i) 18 to 60 years of age; ii) diagnosed with BPD according to DSM‐IV criteria; iii) ≥ 2 episodes of suicide attempt/NSSI in the five years preceding trial entry with ≥ 1 of these episodes in the year preceding trial entry and ≥ 1 of these episodes in the eight weeks preceding trial entry. Exclusion criteria: i) IQ score < 70 on the Peabody Picture Vocabulary Test‐Revised; ii) diagnosed with psychosis or bipolar disorder; iii) diagnosed with a seizure disorder requiring medication; iv) requiring treatment for another life‐threatening condition (e.g. severe anorexia nervosa). |
|
| Interventions | See Linehan 2015a and Linehan 2015b for a detailed description. | |
| Outcomes |
Primary outcome(s): i) repetition of SH according to self‐report using the SASII; ii) frequency of SH according to self‐report using the SASII. Secondary outcome(s): i) hopelessness as measured using the Reasons for Living Inventory (reverse scored); ii) depression as measured using the HRSD; iii) anxiety as measured using the Hamilton Rating Scale for Anxiety. |
|
| Notes |
Source(s) of funding: "This study was supported by grant R01MH034486 from the National Institute of Mental Health for the design and conduct of the study and for collection, management, analysis, and interpretation of the data" (Linehan 2015, p.8). Conflict(s) of interest: "Dr Linehan receives royalties from Guilford Press for books she has written on Dialectical Behavior Therapy (DBT) and from Behavioral Tech, LLC, for DBT training materials she has developed; she owns Behavioral Tech Research, Inc, a company that develops online learning and clinical applications that include products for DBT. Drs Linehan, Korslund, Harned, Neacsiu, and Comtois are compensated for providing DBT training and consultation. No other disclosures were reported" (Linehan 2015, p.8). |
|
Linehan 2015a.
| Study characteristics | ||
| Methods | See Linehan 2015 for a detailed description. | |
| Participants | See Linehan 2015 for a detailed description. | |
| Interventions |
Intervention (DBT plus group skills training): comprising manualised case management (duration not reported), weekly group skills training (2.5 hours), DBT consultation team meeting (1 hour), and telephone coaching, as needed. Participants did not receive individual therapy. Sessions were delivered by therapists (one‐third were doctoral‐level therapists), the majority of whom had over 10 years clinical experience working with suicidal persons and who received training (duration not reported) in delivering the intervention and ongoing supervision. Comparator: comprising weekly sessions of individual therapy (1 hour), group skills training (2.5 hours), DBT consultation team meeting (1 hour), and telephone coaching, as needed. Concomitant medications: were permitted. The average number of psychotropic medications prescribed at baseline was 3.1 ± 2.7. Length of treatment: 12 months. |
|
| Outcomes | See Linehan 2015 for a detailed description. | |
| Notes | See Linehan 2015 for a detailed description. | |
Linehan 2015b.
| Study characteristics | ||
| Methods | See Linehan 2015 for a detailed description. | |
| Participants | See Linehan 2015 for a detailed description. | |
| Interventions |
Intervention (individual‐based DBT): comprising weekly sessions of individual therapy (1 hour), DBT consultation team meeting (1 hour), and telephone coaching, as needed. Participants did not receive group skills training. Sessions were delivered by therapists (93% were doctoral‐level therapists), the majority of whom had over 10 years clinical experience working with suicidal persons and who received training (duration not reported) in delivering the intervention and ongoing supervision. Comparator: comprising weekly sessions of individual therapy (1 hour), group skills training (2.5 hours), DBT consultation team meeting (1 hour), and telephone coaching, as needed. Concomitant medications: were permitted. The average number of psychotropic medications prescribed at baseline was 3.1 ± 2.7. Length of treatment: 12 months. |
|
| Outcomes | See Linehan 2015 for a detailed description. | |
| Notes | See Linehan 2015 for a detailed description. | |
Marasinghe 2012.
| Study characteristics | ||
| Methods | Participants were individually randomised using an unknown method to either a remote contact intervention (brief psychotherapy delivered by mobile phone) or waiting list. N lost to follow‐up: 0/68 (0%) for repetition of SH at post‐intervention. Location: Colombo, Sri Lanka. |
|
| Participants |
Number of total participants: 68 participants were randomised; 34 were allocated to the mobile phone based psychotherapy, and 34 were allocated to waiting list. Profile of participants: mean age 31.0 ± 14.8 years (range: 15‐74 years). Half (n = 34; 50.0%) were female. No information on psychiatric diagnoses reported. Source of participants: patients admitted to hospital following an episode of SH. Inclusion criteria: i) aged 15‐74 years; ii) admitted to hospital following an episode of SH; iii) episode of SH was associated with significant suicidal intent as reported either at the intake interview or according to scores on BSS; iv) considered likely to be discharged from hospital within 2 days or able to be re‐approached if admitted for longer than 2 days; v) able to provide informed consent. Exclusion criteria: i) currently receiving ongoing psychiatric treatment; ii) diagnosed with psychosis; iii) diagnosed with dementia. |
|
| Interventions |
Intervention: brief mobile intervention consisting of an assessment of mental health, meditation, PST, interventions to increase social support, interventions to address alcohol or other substance misuse problems, a series of 10 telephone calls to reaffirm techniques learnt during treatment, the ability to access telephone messages to reaffirm techniques learnt during treatment, and a series of up to 26 text messages to encourage the participant to practice meditation techniques, problem‐solving skills, to seek social support, to avoid alcohol and other drugs, and to use the telephone helpline to get individual support in times of crisis. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: waiting list. Length of treatment: up to 26 weeks. |
|
| Outcomes | Primary outcome(s): i) repetition of SH (unclear how ascertained); ii) AOD use as measured by the AUDIT and the Drug Check Problem List; iii) depression as measured by the BDI; iv) social support as measured by the Medical Outcomes Study; v) suicidal ideation as measured by the BSSI; v) suicide (unclear how ascertained). | |
| Notes | Source(s) of funding: “We are grateful for funding from the Improving Relevance and Quality of Undergraduate Education (IRQUE) project of the University of Jeyewardenepura, Sri Lanka” (Marasinghe 2012, p. 155). Conflict(s) of author interests: no information on author interests reported. | |
McAuliffe 2014.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated sequence of numbers stratified by sex, SH repeater status, and trial site to either manualised, group‐based CBT‐based psychotherapy or TAU. N lost to follow‐up: 313/433 (27.7%) for repetition of SH at post‐intervention. Location: Cork and Limerick, Republic of Ireland. |
|
| Participants |
Number of total participants: 433 participants were randomised; 222 were allocated to the group‐based CBT‐based psychotherapy, and 211 were allocated to TAU. Profile of participants: mean age 33.5 ± 11.8 years (range: 18‐64 years). Almost two‐thirds (n = 279; 64.4%) were female. Just under one‐third (n = 127; 29.3%) had a history of SH (i.e. multiple episodes of SH). No information on psychiatric diagnoses reported. Source of participants: patients presenting to the ED following an episode of SH, or patients engaging in SH in acute psychiatric facilities even if this did not necessitate admission to the ED. Inclusion criteria: i) aged 18‐64 years; ii) engaged in SH in the three days preceding trial entry. Exclusion criteria: i) diagnosed with psychosis, intellectual disability, sensory disability, or an organic cognitive impairment; ii) currently substance dependent according to scores on the Short Alcohol Dependent Data questionnaire; iii) imprisoned; iv) no fixed address. |
|
| Interventions |
Intervention: manualised problem‐solving skills training consisting of six (two hour) sessions facilitated by a trained therapist and a co‐therapist. Therapeutic content involved problem‐solving skills training. Sessions were delivered by therapists (expertise and experience not reported) who received training (duration not reported) in delivering the intervention. Comparator: TAU consisting of an assessment by mental health professional staff and by crisis staff, and referral to acute mental health or community‐based services, psychotherapy, and pharmacotherapy, as necessary. Length of treatment: six weeks. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH (as ascertained from self‐report for the 6‐week and 6‐month follow‐up assessment and from hospital records for the 12‐month assessment); ii) suicide as ascertained from hospital records. Secondary outcome(s): i) anxiety as measured by the Beck Anxiety Inventory (BAI); ii) depression as measured by the BDI; iii) hopelessness as measured by the BHS; iv) impulsivity as measured by BIS; v) problem‐solving skills as measured by the Means‐Ends Problem‐Solving Procedure (MEPS) and the Self‐Rating Problem‐Solving Scale; vi) self‐efficacy as measured by the Generalised Self‐efficacy Scale; vii) social functioning as measured by the Social Life Scale; vii) suicidal ideation as measured by the BSSI. |
|
| Notes | Source(s) of funding: “This work was supported by funding from the Health Service Executive (HSE) South, HSE Mid‐West, the HSE National Office for Suicide Prevention, the Health Research Board and Pobal‐Dormant Accounts Fund in Ireland” (McAuliffe 2014, p. 389). Conflict(s) of interests: none reported. | |
McLeavey 1994.
| Study characteristics | ||
| Methods | Participants were individually randomised using an open numbers table to either interpersonal problem‐solving skills training or alternative psychotherapy (brief PST). N lost to follow‐up: 6/39 (15.4%) for repetition of SH by the 12‐month assessment. Location: Cork, Republic of Ireland. |
|
| Participants |
Number of total participants: 39 participants were randomised, 19 were allocated to interpersonal problem‐solving skills, and 20 were allocated to alternative psychotherapy. Profile of participants: mean age 23.9 ± 7.2 years (range: 15‐45 years). Just under three‐quarters (n = 29; 74.3%) were female. Over one‐third (n = 14; 35.9%) had a history of SH (i.e. multiple episodes of SH). Almost one‐quarter (n = 9; 23.1%) were diagnosed with dysthymia, followed by dependent PD (n = 6; 15.4%), and AUD (n = 5; 12.8%). Source of participants: patients admitted to an A&E department following an episode of self‐poisoning. Inclusion criteria: i) aged 15‐45 years; ii) score ≥ 80 on the Mill Hill Vocabulary Scale. Exclusion criteria: i) history of psychosis, mental retardation, or organic cognitive impairment; ii) referred for psychiatric treatment (day care or inpatient). |
|
| Interventions |
Intervention: manualised interpersonal problem‐solving skills training (number and duration of sessions not reported). Therapeutic content involved instruction, active discussion, reflective listening, modelling, coping strategy, role playing, sentence completion, and prompting. Sessions were delivered by psychiatry registrars and clinical psychologists (no further information on experience was reported). Comparator: alternative psychotherapy (brief problem‐solving therapy) (number and duration of sessions not reported). Therapeutic content involved focusing on patients’ current problems and prevention by helping patients gain insight into problems. No specific skills training was provided, however. Length of treatment: five weeks. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from hospital records and a GP questionnaire. Secondary outcome(s): i) hopelessness as measured by the BHS; ii) problem‐solving as measured by the MEPS, the Optional Thinking Test, the Awareness of Consequences Test, the Self‐Rating Problem‐Solving Scale, and the Problems Questionnaire; iii) self‐concept as measured by the Self‐Perception Scale; iv) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: no information on funding sources reported. Conflict(s) of interest: Although no conflicts of interest were reported, Dr McLeavey was the developer of interpersonal problem‐solving skills training. | |
McMain 2009.
| Study characteristics | ||
| Methods | Participants were individually randomised using a pre‐generated blocking procedure to either interpersonal DBT or TAU. N lost to follow‐up: 32/180 (17.8%) for repetition of SH by the post‐intervention assessment. Location: Toronto, ON, Canada. |
|
| Participants |
Number of total participants: 180 participants were randomised, 90 were allocated to DBT, and 90 were allocated to TAU. Profile of participants: mean age 30.4 ± 9.9 years (range: 18‐60 years). The majority (n = 155; 86.1%) were female. All (n = 180; 100%) had a history of SH (i.e. multiple episodes of SH), and were diagnosed with BPD. Three‐quarters (n = 135; 75.0%) were diagnosed with any anxiety disorder, just under half (n = 88; 48.9%) were diagnosed with MDD, followed by PTSD (n = 71; 37.4%), panic disorder (n = 39; 21.7%), and SUD (n = 17; 9.4%). Source of participants: patients attending a specialised Centre for Addiction and Mental Health, hospital or both. Inclusion criteria: i) aged 18‐60 years; ii) met DSM‐IV criteria for BPD; iii) ≥ 2 episodes of suicide attempts and/or NSSI in the past five years with ≥ 1 in the three months preceding trial entry. Exclusion criteria: i) met DSM‐IV criteria for a psychotic disorder, bipolar I disorder, delirium, dementia, or mental retardation; ii) diagnosed with substance dependence in the 30 days preceding trial entry; iii) did not live within communing distance; iv) diagnosed with a serious medical condition likely to require hospitalisation within one year (e.g. cancer); v) planning to move out of the catchment area within two years. |
|
| Interventions |
Intervention: manualised DBT consisting of weekly (60 minutes) sessions of individual therapy, group‐based skills training (two hours), and telephone‐based coaching (2 hours). Number of sessions not reported. Therapeutic content involved: psychoeducation, validation and empathy, mindfulness, exposure, contingency management, and behavioural analysis with an explicit focus on SH and suicidal behaviour. Additionally, therapists attended weekly therapist team meetings. Sessions were delivered by board‐certified psychiatrists and doctoral‐level clinicians (no further information on experience was reported). Comparator: TAU (general psychiatric management) consisting of weekly (60 minutes) sessions of individual therapy focused on improving medication management through the use of a structured drug algorithm. Participants also received psychoeducation, providing validation and empathy within a ’here and now’ focus. Additionally, therapists attended weekly therapist team meetings. Number of sessions not reported. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH as ascertained from self‐report using the SASII; ii) frequency of SH as ascertained from self‐report using the SASII; iii) severity of SH as ascertained from self‐report using the SASII. Secondary outcome(s): i) anger as measured by the STAXI; ii) BPD symptomatology as measured by the Zanarini Rating Scale for Borderline Personality Disorder; iii) depression as measured by the BDI; iv) general symptomatology as measured by the SCL‐90; v) interpersonal problems as measured by the Inventory of Interpersonal Problems, 64‐item version; vi) quality of life as measured by the EQ‐5D; vii) service use as ascertained from self‐report; viii) reasons for dropout as measured by the Reasons for Early Termination From Treatment Questionnaire; ix) treatment adherence as measured by the number of sessions attended; x) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: “Supported by grant 200204MCT‐101123 from the Canadian Institutes for Health Research” (McMain 2009, p. 1373) Conflict(s) of interest: “Dr. Links has received an unrestricted educational grant from Eli Lilly Canada Inc. All other authors report no competing interests” (McMain 2009, p. 1373). Other: data on hospital admissions for self‐harm obtained from self‐report following clinician interview. | |
McMain 2017.
| Study characteristics | ||
| Methods | Participants were individually randomised via a blocking procedure either to 20 weeks of a DBT skills training program or active waiting list. N lost to follow‐up: 0/84 (0%) for repetition of SH at post‐intervention. Location: Toronto, Canada. |
|
| Participants |
Number of total participants: 84 participants were randomised, 42 were allocated DBT plus group skills therapy and 42 were allocated to waiting‐list control. Profile of participants: mean age 29.7 ± 8.6 years (range: 18‐60 years). Over three‐quarters (n = 66; 78.6%) were female. The majority (n = 51; 60.7%) were diagnosed with any anxiety disorder, followed by SUD (n = 47 56.0%), MDD (n = 43; 51.2%), PTSD (n = 19; 22.6%), any eating disorder (n = 13; 15.5%), and panic disorder (n = 12; 14.3%). Source of participants: patients currently receiving treatment from outpatient mental health services. Inclusion criteria: i) 18‐60 years of age; ii) diagnosed with BPD according to DSM‐IV criteria; iii) ≥ 2 episodes of SH in the five years preceding trial entry with ≥ 1 episode in the 10 weeks preceding trial entry; iv) sufficient language ability. Exclusion criteria: i) diagnosed with psychosis, bipolar disorder, or dementia according to DSM‐IV criteria; ii) diagnosed with an organic disorder or intellectual disability; iii) received DBT within the year preceding trial entry. |
|
| Interventions |
Intervention: manualised DBT plus group skills therapy consisting of a single (90 minute) individual orientation session followed by weekly sessions (two hours) of group skills training comprising mindfulness, emotion regulation, distress tolerance, interpersonal effectiveness, and dialectics. Participants were also provided with the numbers for 24‐hour crisis lines. Comparator: waiting‐list control. Concomitant medications: 71 participants (84.5%) were prescribed psychotropic medications (mean 1.8 ± 1.4 medications per participant). Length of treatment: 20 weeks. |
|
| Outcomes |
Primary outcome(s): i) frequency of SH as ascertained from the clinician‐report using the Lifetime Suicide Attempt Self‐Injury Interview (LSASI) together with self‐report using the Deliberate Self‐Harm Inventory (DSHI). Secondary outcome(s): i) healthcare utilisation as measured using the Treatment History Interview‐2 (THI‐2); ii) number of ED visits as measured using the THI‐2; iii) number of psychiatric hospital admissions as measured using the THI‐2; iv) use of medications as measured using the THI‐2; v) borderline personality symptoms as measured using the Borderline Symptoms List‐23; vi) anger as measured by the State‐Trait Anger Expression Inventory; vii) general symptoms as measured by the Symptom Checklist‐90‐Revised; viii) impulsiveness as measured by the Barrett Impulsiveness Scale‐11; ix) depression as measured by the BDI; x) social functioning as measured by the Social Adjustment Scale‐Self‐Report; xi) emotion regulation as measured by the Difficulties in Emotion Regulation Scale; xii) distress as measured by the Distress Tolerance Scale; xiii) mindfulness skills as measured by the Kentucky Inventory of Mindfulness Scale; xiv) treatment adherence as measured by the Reasons for Early Termination from Treatment Questionnaire (for dropouts). |
|
| Notes |
Source(s) of funding: "The study was funded by the Ontario Mental Health Foundation (McMain 2017, p. 147). Conflict(s) of interest: "The authors report no conflict of interests in relationship to this study" (McMain 2017, p. 147). |
|
Morgan 1993.
| Study characteristics | ||
| Methods | Participants were individually randomised using sealed envelopes to a remote contact intervention (emergency card) or TAU. N lost to follow‐up: 0/212 (0%) for repetition of SH at post‐intervention. Location: Bristol, UK. |
|
| Participants |
Number of total participants: 212 participants were randomised, 101 were allocated to the remote contact intervention (emergency card), and 111 were allocated to TAU. Profile of participants: mean age 30.1 years (SD: not reported; range: not reported). Proportion female not reported. All (n = 212; 100%) had engaged in SH for the first time. One‐quarter (n = 53; 25.0%) were diagnosed with a depressive disorder. Source of participants: patients admitted to hospital following first episode of SH. Inclusion criteria: i) no previous episode of SH; ii) resident within the catchment area. Exclusion criteria: none reported. |
|
| Interventions |
Intervention: remote contact intervention (emergency card) in addition to TAU. The green card outlined that a doctor was available by telephone and provided their contact information and enabled participants to on‐demand admission to hospital. Sessions were delivered by duty doctors (no further information on expertise or experience was reported). Comparator: TAU consisting of referral to the primary healthcare team, and psychiatric or inpatient admissions, if required. No information on the number or duration of sessions was reported. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from hospital, psychiatric, and GP records. Secondary outcome(s): i) use of the emergency card ascertained from hospital, psychiatric, and GP records; ii) admission to psychiatric hospital ascertained from records ascertained from hospital, psychiatric, and GP records; iii) service use ascertained from hospital, psychiatric, and GP records. |
|
| Notes | Source(s) of funding: no sources of funding were reported. Conflict(s) of interest: no conflicts of interest were reported. | |
Morthorst 2012.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐based software stratified by history of suicide attempts, history of psychiatric treatment or hospitalisation, and alcohol consumption at the index attempt to either case management or EUC. N lost to follow‐up: 0/243 for repetition of SH at post‐intervention. Location: Copenhagen, Denmark. |
|
| Participants |
Number of total participants: 243 participants were randomised, 123 were allocated to case management and assertive outreach, and 120 were allocated to TAU. Profile of participants: mean age 31.0 ± 13.3 years (range: 11‐69 years). Three‐quarters (n = 184; 75.7%) were female. Over half (n = 130; 53.5%) had a history of SH (i.e. multiple episodes of SH). Whilst just under half (n = 109; 44.8%) had a history of psychiatric treatment prior to the index attempt, no information on psychiatric diagnoses was reported. Source of participants: patients admitted to acute emergency units, intensive care units, paediatric units, or psychiatric emergency room units following a suicide attempt. Inclusion criteria: i) aged 12 years or older; ii) admitted to acute emergency units, intensive care units, paediatric units, or psychiatric emergency room units following a suicide attempt. Exclusion criteria: i) living in an institution; ii) admitted to a psychiatric unit for > 14 days; iii) diagnosed with a schizophrenia‐spectrum disorder; iv) diagnosed with severe depression, bipolar disorder, or dementia; v) currently receiving outreach services from social service agencies. |
|
| Interventions |
Intervention: between eight to 20 sessions (duration not reported) of an assertive intervention involving case management, crisis intervention, as required, problem‐solving therapy, and assertive outreach based on motivational support to encourage patients to attend treatment sessions, assist patients to attend these sessions, and to improve adherence to after‐treatment in addition to TAU. Sessions were delivered by psychiatric nurses (experience not reported) who received further training (duration not reported) in suicidology. Comparator: EUC consisting of six to eight sessions (duration not reported), including a psychiatric assessment and referral to AOD treatment, psychological therapy, and GP treatment, as required. Pharmacological treatment was also provided, where necessary, through the Centre for Excellence. Length of treatment: six months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report in addition to medical and hospital records; ii) suicide ascertained from self‐report in addition to medical and hospital records. | |
| Notes | Source(s) of funding: “This study received funding from the Ministry of Health and Internal Affairs, Denmark, the National Board of Social Services, and independent subdivision of The Ministry of Social Affairs and Integration, TrygFoden, and Aase og Ejnar Danielsens Foundation” (Morthorst 2012, p. 6). Conflict(s) of interests: none reported. | |
Mouaffak 2015.
| Study characteristics | ||
| Methods | Participants were individually randomised (procedure not reported) stratified by history of suicide attempts to either a remote contact intervention (telephone contact combined with emergency cards and letters) or TAU. N lost to follow‐up: 0/303 (0.0%) for repetition of SH at post‐intervention. Location: Bicêtre, France. |
|
| Participants |
Number of total participants: 303 participants were randomised, 152 were allocated to a remote contact intervention (letters and telephone contact), and 151 were allocated to TAU. Profile of participants: mean age 38.8 ± 13.1 years (range: not reported). Almost three‐quarters (n = 224; 73.9%) were female. Just under half (n = 151; 49.8%) had a history of SH (i.e. multiple episodes of SH). Almost one‐third were diagnosed with a depressive disorder (n = 87; 28.7%) or PTSD (n = 87; 28.7%), followed by AUD (n = 18; 5.9%). A minority were diagnosed with a comorbid PD (n = 50; 16.5%). Source of participants: patients admitted to a psychiatric ED following a suicide attempt. Inclusion criteria: i) aged 18 years or older; ii) discharged from the ED within 72 hours with a referral to an outpatient follow‐up programme; iii) able to provide consent; iv) able to be contacted by telephone; v) sufficient language ability. Exclusion criteria: i) unable to be contacted by telephone (e.g. homeless, incarcerated); ii) insufficient language ability. |
|
| Interventions |
Intervention: remote contact intervention (letters and telephone contact) consisting of a letter sent within days post‐discharge providing information on scheduled interventions, and a resource card providing the contact information of a senior psychiatrist available 24 hours. Participants received further letters one, six, and 11 months' post‐discharge. Participants also received telephone contact (duration not reported) at two weeks, and months one and three post‐discharge. The purpose of these calls was to facilitate collaborative management and foster treatment engagement. PST, crisis management, and hospital treatment were also provided, if required. Sessions were delivered by psychiatrists (no further information on experience was reported). Comparator: TAU (no further details reported) as well as reminder letters one, six, and 11 months' post‐discharge. Length of treatment: 12 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from self‐report, collateral informant report, and/or hospital reports; ii) time to repetition of SH ascertained from self‐report, collateral informant report, and/or hospital reports. Secondary outcome(s): i) service use ascertained from self‐report, collateral informant report, and/or hospital reports; ii) suicide as ascertained from mortality registers; iii) all‐cause mortality as ascertained from mortality registers. |
|
| Notes |
Source(s) of funding: none reported. Conflict(s) of interest: none reported. |
|
Mousavi 2015.
| Study characteristics | ||
| Methods | Participants were individually randomised (procedure not reported) to either a remote contact intervention (telephone contact) or alternative psychotherapy. N lost to follow‐up: 8/55 (14.5%) for repetition of SH at post‐intervention. Location: Isfahan, Iran. |
|
| Participants |
Number of total participants: 55 participants were randomised, 29 were allocated to a remote contact intervention (telephone contact), and 26 were allocated to TAU. Profile of participants: mean age 28.3 ± 7.8 years (range: not reported). The majority (n = 48; 87.3%) were female. All (n = 55; 100%) had a history of SH (i.e. multiple episodes of SH). No information on psychiatric diagnoses was reported. Source of participants: patients admitted to the ED of a general hospital following a suicide attempt. Inclusion criteria: i) aged 20 years or older; ii) ≥ 2 previous suicide attempts (time‐frame not reported); iii) able to understand the trial procedure; iv) able to provide informed consent; v) sufficient language ability. Exclusion criteria: i) diagnosed with dementia or other cognitive impairment according to DSM‐IV‐TR criteria; ii) required immediate medical intervention (e.g. emergency surgery); iii) no known contact information; iv) those unable to be contacted post‐intervention; v) those who die during the follow‐up period (other than by suicide). |
|
| Interventions |
Intervention: remote contact intervention (telephone contact) consisting of up to eight telephone calls (20 minutes) at weeks two and four, and at months two, three, four, five, six, and eight post‐discharge. Therapeutic content included psychoeducation, identification of problems, problem appraisal, stress management, and referral to a psychiatrist, psychologist, or social worker, as required. Sessions were delivered by assistant psychiatrists (no further information on experience was reported). Comparator: face‐to‐face contact consisting of up to eight sessions (20 minutes) at weeks two and four, and at months two, three, four, five, six, and eight post‐discharge. Therapeutic content included psychoeducation, identification of problems, problem appraisal, stress management, and referral to a psychiatrist, psychologist, or social worker, as required. Length of treatment: eight months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report; ii) hopefulness as ascertained from self‐report (reverse coded); iii) interest as ascertained from self‐report; iv) problem resolution as ascertained from self‐report; v) suicidal ideation as ascertained from self‐report; vi) suicide (unclear how ascertained). | |
| Notes |
Source(s) of funding: none reported. Conflict(s) of interest: none reported. |
|
Mousavi 2017.
| Study characteristics | ||
| Methods | Participants were individually randomised (procedure not reported) to either CBT‐based psychotherapy in addition to TAU or TAU alone. N lost to follow‐up: 0/60 (0%) for repetition of SH at post‐intervention. Location: Isfahan, Iran. |
|
| Participants |
Number of total participants: 60 participants were randomised, 30 were allocated to brief CBT‐based psychotherapy in addition to TAU, and 30 were allocated to TAU alone. Profile of participants: mean age not reported (range: not reported). The majority (n = 42; 70.0%) were female. All (n = 60; 100%) had a history of SH (i.e. multiple episodes of SH). No information on psychiatric diagnoses was reported. Source of participants: patients hospitalised following a suicide attempt. Inclusion criteria: i) sufficient language ability; ii) able to provide informed consent. Exclusion criteria: i) diagnosed with dementia or other cognitive impairment according to DSM‐IV‐TR criteria; ii) required immediate medical intervention (e.g. emergency surgery); iii) no known contact information; iv) those unable to be contacted post‐intervention; v) those who died during the follow‐up period (other than by suicide). |
|
| Interventions |
Intervention: brief psychotherapy based on principles of ACT and CBT in addition to TAU. Therapy consisted of 10 face‐to‐face visits in weeks one and two and months two, three, four, five, six, seven, eight, 10, and 12 post‐discharge. Therapeutic content included identifying and recognising thoughts that interfered with problem‐solving (e.g. all‐or‐nothing thinking), cognitive restructuring, coping with problems, acceptance of problems, and cognitive diffusion. Participants were also referred to treatment by a psychologist, psychiatrist, or social worker, as required. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: TAU consisting of referral to the psychiatric emergency unit for review, further referral to treatment by a psychologist, psychiatrist, or social worker, as required, and telephone contact at months two, four, six, five, six, seven, eight, 10 and 12 post‐discharge. Length of treatment: 12 months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report; ii) hopelessness as ascertained from self‐report; iii) satisfaction with life as ascertained from self‐report; iv) suicidal ideation as ascertained from self‐report. | |
| Notes |
Source(s) of funding: none reported. Conflict(s) of interest: none reported. |
|
Naidoo 2014.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer generated process to either provision of information and support or TAU. N lost to follow‐up: unclear. Location: Durban, South Africa. |
|
| Participants |
Number of total participants: 688 participants were randomised, 344 were allocated to provision of information and support and 344 were allocated to TAU. Profile of participants: mean age 35.0 years (SD not reported, range: 20‐29 years). Three‐quarters (n = 516; 75.0%) were female. Information on psychiatric diagnoses was not reported. Source of participants: patients presenting to the ED and/or admitted to the short‐ or long‐stay wards of one of two general hospitals following an episode of SH. Inclusion criteria: i) aged 18 years and older; ii) presenting to the ED and/or admitted to the short‐ or long‐stay wards of one of two general hospitals following an episode of SH. Exclusion criteria: none reported. |
|
| Interventions |
Intervention: based on the SUPRE‐MISS model (Fleischmann 2008) consisting of a brief (one hour) information and psychoeducation session, and nine follow‐up contacts (duration not reported, also modality not reported) at weeks one, two, four, seven, 11, and months four, six, 12, and 18 months post‐discharge. Participants were also paired with a nominated support person who received training (three sessions of four hours' duration each) in basic counselling and gate‐keeping skills. No further information on who delivered the intervention, their expertise, or their experience was reported. Comparator: SUPRE‐MISS intervention without support persons. Based on the SUPRE‐MISS model (Fleischmann 2008), this consisted of a brief (one hour) information ad psychoeducation session, and nine follow‐up contacts (duration not reported, also modality not reported) at weeks one, two, four, seven, 11, and months four, six, 12, and 18 months post‐discharge. Length of treatment: 18 months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH as ascertained from self‐report using a tool developed for the SUPRE‐MISS trial; ii) suicide (unclear how determined); iii) all‐cause mortality (unclear how determined). | |
| Notes |
Source(s) of funding: no source(s) of funding reported. Conflict(s) of interest: no conflict(s) of interest reported. |
|
O'Connor 2015.
| Study characteristics | ||
| Methods | Participants were individually randomised (method not reported) to either a brief ED‐based Collaborative Assessment and Management of Suicidality (CAMS)‐based intervention or TAU. N lost to follow‐up: data on repetition of SH not reported. However the authors reported "[w]e completed 80% of the 1‐month follow‐up interviews. The 20% who were lost to follow‐up did not respond to our efforts at contacting them through telephone, mail, or email contacts" (O'Connor 2015, p.430). Location: unclear (USA). |
|
| Participants |
Number of total participants: 30 participants were randomised, 15 were allocated to a brief intervention (based on principles of CAMS and DBT), and 15 were allocated to TAU. Profile of participants: mean age 41.3 ± 13.8 years (range: not reported). Just over one‐quarter (n = 8; 26.7%) were female. No information on psychiatric diagnoses was reported. Source of participants: patients medically admitted to a medical or surgical ward of a trauma hospital following a suicide attempt. Inclusion criteria: i) 15 years of age or older; ii) medically admitted to a medical or surgical ward of a trauma hospital following a suicide attempt; iii) sufficient language ability; iv) able to provide informed consent. Exclusion criteria: i) denied making an index attempt; ii) insufficient language ability; iii) imprisoned; iv) assessed as either too cognitively impaired, delirious, or psychotic to respond to a psychosocial intervention by clinical personnel. |
|
| Interventions |
Intervention: brief, one‐off intervention (average duration 43.98 ± 12.87 minutes) based on principles from CAMS. Therapeutic content involved collaborative assessment and planning, rapport building, guided discovery, functional analysis, crisis planning, and linkage to outpatient mental health services, as required. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: TAU. No specific information on TAU content was reported. Length of treatment: one‐off consultation. |
|
| Outcomes |
Primary outcome(s): i) satisfaction with treatment as measured by the Patient Satisfaction Questionnaire. Secondary outcome(s): i) suicidal ideation as measured by the BSS; ii) motivation to change as measured by the Stages of Change Questionnaire; iii) hopelessness as measured by the Reasons for Living Inventory (reverse scored). |
|
| Notes |
Source(s) of funding: "The current study was supported by grants T32HD057822 (PI: Rivara) from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and K24MH086814 (PI: Zatzick) from the National Institutes of Mental Health" (O'Connor 2015, p.432). Conflict(s) of interest: none reported. |
|
O'Connor 2017.
| Study characteristics | ||
| Methods | Participants were individually randomised (1:1) using a web‐based, minimisation procedure to either a brief ED‐based guided integrated motivational‐volitional‐focused intervention or TAU. N lost to follow‐up: 6/518 (1.2%) for repetition of SH by the six‐month follow‐up assessment. Location: Edinburgh, UK. |
|
| Participants |
Number of total participants: 518 participants were randomised, 259 were allocated to a brief intervention (volitional help sheet), and 259 were allocated to TAU. Profile of participants: mean age 36.3 ± 13.7 years (range: not reported). Over half (n = 324; 62.5%) were female and had a history of SH (i.e. multiple episodes of SH (n = 329; 63.5%). No information on psychiatric diagnoses was reported. Source of participants: patients admitted overnight to an acute medical unit of a general hospital following a suicide attempt. Inclusion criteria: i) 16 years of age or older; ii) ≥ 1 self‐reported episode of SH. Exclusion criteria: i) assessed as medically unfit for interview; ii) insufficient language ability; iii) already participating in other trials being conducted within the hospital; iv) were treated within the ED without an admission. |
|
| Interventions |
Intervention: brief, volitional help‐sheet (VHS) intervention consisting of a one‐off assessment (duration not reported) in addition to TAU. Participants were provided with a list of common situations in which they may be tempted to engage in SH together with a list of potential alternative behaviours. Participants then drew links between any situation that applied to them and any one of the listed alternative behaviours. Participants could make as many links as desired. At the conclusion of the assessment, participants took a copy of the VHS home. At approximately two months' post‐discharge, participants received a booster VHS by mail. Sessions were delivered by clinical staff (no further information on their expertise or experience was reported). Comparator: TAU consisting of a one‐off psychosocial assessment (duration not reported) undertaken by the liaison psychiatry service. Following this, participants were either transferred to inpatient psychiatric care, or referred for outpatient psychiatric treatment, voluntary sector follow‐up, or primary care follow‐up, as required. Length of treatment: one‐off consultation. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from medical records; ii) number of repeat SH episodes ascertained from medical records; iii) incremental cost per SH event averted. Secondary outcome(s): i) time to SH repetition ascertained from medical records. |
|
| Notes |
Source(s) of funding: "The trial was funded by a grant from the Chief Scientist Office, Scotland (CZH/4/704)" (O'Connor 2017, p.459). Conflict(s) of interest: "We declare no competing interests" (O'Connor 2017, p.459). |
|
O'Connor 2020.
| Study characteristics | ||
| Methods | Participants were individually randomised using a minimisation procedure, stratified by sex and history of SH to either a brief ED‐based intervention (teachable moment brief intervention) or TAU. N lost to follow‐up: 25/48 (52.1%) for repetition of SH by the 12‐month assessment. Location: Nashville, TN, USA. |
|
| Participants |
Number of total participants: 48 participants were randomised, 23 were allocated to a brief intervention (teachable moment brief intervention), and 25 were allocated to TAU. Profile of participants: mean age 42.6 ± 2.6 years (range: not reported). Over half (n = 26; 54.2%) were female. No information on psychiatric diagnoses was reported. Source of participants: patients admitted to an acute medical unit of a general hospital following a suicide attempt. Inclusion criteria: i) aged 18 years or older; ii) admitted to an acute medical unit of a general hospital following a suicide attempt; iii) sufficient language ability; iv) able to provide informed consent. Exclusion criteria: i) insufficient language ability; ii) imprisoned; iii) assessed as either too cognitively impaired, delirious, or psychotic to respond to a psychosocial intervention by clinical personnel. |
|
| Interventions |
Intervention: brief intervention based on principles of CAMS, consisting of nine components (30 minutes' duration in total). Therapeutic content involved collaborative assessment and planning, rapport building, guided discovery, functional analysis, crisis planning, and linkage to outpatient mental health services, as required. Sessions were delivered by clinicians (no further information on expertise or experience was reported). Comparator: TAU. No specific information on TAU content was reported. Length of treatment: 30 minutes. |
|
| Outcomes |
Primary outcome(s): i) satisfaction with treatment as measured by the Client Satisfaction Questionnaire. Secondary outcome(s): i) repetition of SH according to self‐report using the SASII; ii) interpersonal functioning as measured by the Interpersonal Needs Questionnaire; iii) motivation to change as measured by the Stages of Change Questionnaire; iv) hopelessness as measured by the Reasons for Living Inventory (reverse scored); v) services use ascertained from the Health Services and Medication Use measure; vi) suicidal ideation as measured by the BSSI. |
|
| Notes |
Source(s) of funding: "This work was supported by the American Foundation for Suicide Prevention [grant number YIG‐0‐098‐13]" (O'Connor 2020, p.117). Conflict(s) of interest: none reported. |
|
Owens 2020.
| Study characteristics | ||
| Methods | Participants were individually randomised (1:1) using a computer adaptive minimisation procedure balanced for: i) number of previous episode of SH leading to hospital treatment prior to study entry (i.e. one vs. > 1); ii) method of SH at the index episode (i.e. self‐poisoning vs. self‐injury vs. both combined); iii) sex (i.e. male vs. female); iv) age (i.e. < 30 years vs. 30–59 years vs. ≥ 60 years) to either CBT‐based psychotherapy or TAU. N lost to follow‐up: 0/62 (0%) for repetition of SH at six months (as ascertained from hospital records). Location: Leeds and York, UK. |
|
| Participants |
Number of total participants: 62 participants were randomised, 30 were allocated to PST, and 32 were allocated to TAU. Profile of participants: mean age 35.2 ± 13.8 years (range: 18 to 65 years). Over half (n = 40; 64.5%) were female. Over three‐quarters (n = 48; 77.4%) and had a history of SH (i.e. multiple episodes of SH). Whilst the majority (n = 52; 83.9%) had received mental health treatment, no specific information on psychiatric diagnoses was reported. Source of participants: patients presenting to EDs following an episode of self‐harm. Inclusion criteria: i) 18 years of age or older; ii) living within the catchment area; iii) presented to one of two EDs following an episode of SH within six weeks prior to trial entry. Exclusion criteria: i) currently receiving treatment that may interfere with PST; ii) insufficient cognitive capacity; iii) insufficient language ability; iv) known risk of violence to others; v) unable to be contacted within eight weeks of the index episode of SH. |
|
| Interventions |
Intervention: manualised PST adapted from Hatcher 2015 and Hatcher 2016, comprising six weekly to fortnightly sessions (1 hour). Participants could also receive a single booster session (1 hour) between six to eight weeks following the acute phase. Therapeutic content involved problem orientation, recognising and identifying problems, selecting and defining a problem, generating alternative solutions, decision‐making, implementing a SMART (Specific, Measurable, Achievable, Relevant, and Time‐bound) plan, and reviewing progress. Sessions were delivered by mental health nurses or occupational therapists who received training (two days) in delivering the intervention together with ongoing fortnightly supervision. Comparator: TAU. This could vary widely, from telephone contact to remind participants of appointments, to follow‐up psychosocial assessments, referral to other services (e.g. AOD), as required, and participation in group‐based therapy. Any form of TAU was received by 69%, most commonly, community mental health contacts. Concomitant medications: no information on concomitant medications reported. Length of treatment: up to 12 weeks (for the acute phase), up to 20 weeks (including ‘booster’ phase). |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from self‐report and hospital records. Secondary outcome(s): i) repetition of SH ascertained from self‐report; ii) other serious adverse events ascertained from hospital records; iii) treatment adherence as measured by the number of sessions attended; iv) health‐related quality of life as measured by the SF‐36; v) health economics data. |
|
| Notes |
Source(s) of funding: "This work represents independent research funded by the UK National Institute for Health Research in the form of a Research for Patient Benefit grant (NIHR Project Number PB‐PG‐0610‐22267). The treatment costs of the PST were funded by the Leeds and York Partnership NHS Foundation Trust" (Owens 2020, p.13). Conflict(s) of interest: "The authors declare that they have no competing interests" (Owens 2020, p.13). Other: It should be noted that one of the authors (SH) wrote the therapeutic manual, and has been involved in two further trials of this therapeutic approach. |
|
Patsiokas 1985.
| Study characteristics | ||
| Methods | Participants were individually randomised (method not reported) to either cognitive restructuring, PST, or TAU. N lost to follow‐up: not reported. Location: Charleston, SC, USA. |
|
| Participants |
Number of total participants: 15 participants were randomised, 5 were allocated to cognitive restructuring, 5 were allocated to PST, and 5 were allocated to TAU. Profile of participants: not reported. Source of participants: patients admitted to a psychiatric ward following a suicide attempt. Inclusion criteria: i) admitted to a psychiatric ward following a suicide attempt. Exclusion criteria: i) diagnosed with psychosis; ii) diagnosed with substance abuse. |
|
| Interventions |
Intervention (cognitive restructuring): up to 10 sessions (60 minutes) of cognitive restructuring delivered according to the model by Beck 1976. Therapeutic content included identifying automatic thoughts, cognitive distortions, and discussing the validity of assumptions, beliefs, and attitudes that led to their suicide attempt. Sessions were delivered by the same therapist for all three conditions (no further information on expertise or experience was reported). Intervention (PST): up to 10 sessions (60 minutes) of PST according to D'Zurilla 1971. Therapeutic content included orientation, problem definition and formulation, generation of alternatives, decision‐making, and verification. Sessions were delivered by the same therapist for all three conditions (no further information on expertise or experience was reported). Comparator: TAU (number and duration of sessions not reported) involving open discussions about suicidal behaviour, problems, and daily life. Length of treatment: 3 weeks. |
|
| Outcomes | Primary outcome(s): i) repetition of SH (unclear how ascertained); ii) cognitive flexibility as measured by the Alternative Uses Test; iii) hopelessness as measured by the BHS; iv) problem‐solving as measured by the MEPS; v) suicidal ideation as measured from self‐report using the Self‐Monitoring of Suicidal Ideation and the BSSI. | |
| Notes |
Source(s) of funding: no sources of funding reported. Conflict(s) of interest: no conflicts of interest reported. |
|
Priebe 2012.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated algorithm to either DBT or TAU. N lost to follow‐up: 5/80 (6.3%) for repetition of SH by the post‐intervention assessment. Location: London, UK. |
|
| Participants |
Number of total participants: 80 participants were randomised, 40 were allocated to DBT, and 40 were allocated to TAU. Profile of participants: mean age 32.2 ± 10.8 years (range: not reported). The majority (n = 70; 87.5%) were female. Source of participants: referrals to a specialist DBT service. Inclusion criteria: i) aged 16 years or older; ii) engaged in SH on ≥ 5 days in the year prior to trial entry; iii) diagnosed with ≥ 1 PD. Exclusion criteria: i) diagnosed with a severe learning disability that would interfere with the ability to benefit from DBT; ii) insufficient language ability. |
|
| Interventions |
Intervention: DBT delivered according to Linehan 1993, involving weekly individual (60 minutes) and group‐based skills training (2 hours). Out‐of‐hours telephone skills training was also available, as required. Therapeutic content involved CBT, mindfulness, validation, supportive therapeutic techniques, and skills training. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: TAU involving referral back to the referee agency where the participant was encouraged to engage with any treatment other than DBT, including psychotherapy, referral to psychiatrists, mental health teams, counsellors, GPs, or other user‐run support services, as required. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from self‐report. Secondary outcome(s): i) BPD symptoms as measured by the Zanarini Rating Scale for Borderline Personality Disorder; ii) quality of life as measured by the Manchester Short Assessment of Quality of Life; iii) symptoms as measured by the Brief Psychiatric Rating Scale and the BSI; iv) services use as measured by the Client Service Receipt Inventory; v) treatment adherence as measured by the number of sessions attended. |
|
| Notes | Source(s) of funding: “This paper... [was] funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit Programme (grant reference No. PB‐PG‐0906‐10540). All authors were funded by this grant with the exception of K.B. whose contribution was funded by the NIHR Doctoral Research Fellowship Scheme” (Priebe 2012, p. 364). Conflict(s) of interests: no conflicts of interests reported. | |
Sahin 2018.
| Study characteristics | ||
| Methods | Participants were individually randomised (method not reported) to either DBT, psychodynamic psychotherapy, or TAU. N lost to follow‐up: data on repetition of SH not reported. Location: Stockholm, Sweden. |
|
| Participants |
Number of total participants: 106 participants were randomised, 35 were allocated to DBT, 36 were allocated to object‐relational psychotherapy (psychodynamic psychotherapy), and 35 were allocated to TAU. Profile of participants: mean age 29.5 ± 7.7 years (range: 19‐50 years). All (n = 106; 100%) were female, had a history of SH (i.e. multiple episodes of SH), and were diagnosed with BPD. A minority were also diagnosed with the following comorbid psychiatric disorders: major depression (n = 40; 37.7%), panic disorder (n = 40; 37.7%), PTSD (n = 28; 26.4%), avoidant PD (n = 20; 18.9%), paranoid PD (n = 13; 12.3%), dependent PD (n = 9; 8.5%), and obsessive‐compulsive PD (n = 9; 8.5%). Source of participants: patients receiving outpatient psychiatric treatment who self‐reported a history of engaging in multiple episodes of SH. Inclusion criteria: i) female; ii) aged 19‐50 years; iii) diagnosed with BPD according to DSM‐IV criteria; iv) ≥ 2 suicide attempts with ≥ 1 of these within the six months preceding trial entry. Exclusion criteria: i) diagnosed with SUD, psychosis, major depression with melancholic features, a life‐threatening eating disorder, dementia, or other neurological disorder. |
|
| Interventions |
Intervention (DBT): DBT delivered according to Linehan 1993, comprising sessions of both individual therapy and group‐based therapy. Mean number of sessions 44.5 ± 33.4 (range: 0‐155). No specific information on therapeutic content reported. Sessions were delivered by masters‐level psychiatrists, psychologists, psychiatric social workers, psychiatric nurses, psychiatric nurse assistants, nurses, or occupational therapists who received training (duration not reported) in delivering DBT, who reached a minimum score of 3.7 or higher on the DBT Global Rating Scale, who had an average of 22 years clinical experience, and who received ongoing supervision (duration not reported). Intervention (object‐relational psychotherapy): consisting of psychodynamic psychotherapy. Mean number of sessions 58.0 ± 65.1 (range: 0‐236). Therapeutic content included: structural interview according to Clarkin 1999, comprising establishing the therapeutic contract, setting the framework of treatment, techniques to explore mental imagery, and interpersonal relationship therapy. Sessions were delivered by masters‐level psychiatrists, psychologists, psychiatric social workers, psychiatric nurses, psychiatric nurse assistants, nurses, or occupational therapists who received training (duration not reported) in delivering the intervention, who had an average of 22 years clinical experience, and who received ongoing supervision (duration not reported). Comparator: TAU. Consisted of maintenance therapy. No specific detail was reported. Length of treatment: 12 months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH as ascertained from self‐report using the PHI; ii) BPD symptoms as measured by the DSM‐IV and ICD‐10 Personality Disorders Interview; iii) general functioning as measured by the GAF; iv) general psychiatric symptoms as measured by the SCL‐90. | |
| Notes |
Source(s) of funding: no sources of funding reported. Conflict(s) of interest: no conflicts of interest reported. |
|
Salkovskis 1990.
| Study characteristics | ||
| Methods | Participants were individually randomised using a predetermined method of sampling without replacement and sealed envelopes to either CBT‐based psychotherapy or TAU. N lost to follow‐up: 0/20 (0%) for repetition of SH by the six‐month assessment. Location: Leeds, UK. |
|
| Participants |
Number of total participants: 20 participants were randomised, 12 were allocated to CBT‐based psychotherapy, and 8 were allocated to TAU. Profile of participants: mean age 27.2 ± 6.7 years (range: 16‐65 years). Half (n = 10; 50.0%) were female. All (n = 20; 100%) had a history of SH (i.e. multiple episodes of SH). Whilst the majority (n = 19; 95.0%) had previous psychiatric treatment (inpatient: n = 7, 35.0%; outpatient: n = 12, 60.0%), no information on psychiatric diagnoses was reported. Source of participants: patients referred by the duty psychiatrist following an episode of self‐poisoning using antidepressants, and who were assessed in an A&E department following this episode. Inclusion criteria: i) aged 16‐65 years; ii) of fixed abode and living within the catchment area; iii) antidepressants were taken as part of the self‐poisoning episode; iv) ≥ 2 or more suicide attempts preceding trial entry; v) Buglass and Horton Risk of Repetition Scale score ≥ 4. Participants had to fulfil at least 2 criteria to be included. Exclusion criteria: i) not requiring immediate psychiatric treatment; ii) diagnosed with psychosis; iii) diagnosed with a serious organic illness. |
|
| Interventions |
Intervention: domiciliary (home‐based) CBT‐based problem‐solving psychotherapy consisting of five (60 minutes) sessions. Therapeutic content involved identifying problems, priority setting, generating alternative solutions, and goal‐setting. Sessions were delivered by community psychiatric nurses (no further information on experience was reported). Comparator: TAU. No further information on number, duration, or therapeutic content reported. Length of treatment: one month. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from hospital records; ii) anxiety, tension, and fatigue measured by the Profile of Mood State; iii) depression measured by the BDI; iv) hopelessness measured by the BHS; v) problem‐solving measured by the Personal Questionnaire Rapid Scaling Technique; vi) suicidal ideation measured by the BSSI; vii) suicide (unclear how ascertained). | |
| Notes | Source(s) of funding: no sources of funding reported. Conflict(s) of interests: no conflicts of interest reported. | |
Slee 2008.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐based random number generator to either CBT‐based psychotherapy in addition to TAU or TAU alone. N lost to follow‐up: 8/90 (8.9%) for repetition of SH data by the six‐month assessment. Location: Leiden, the Netherlands. |
|
| Participants |
Number of total participants: 90 participants were randomised, 48 were allocated to CBT‐based psychotherapy in addition to TAU, and 42 were allocated to TAU. Profile of participants: mean age 24.6 ± 5.6 years (range: 15‐35 years). The majority (n = 77; 93.9%) were female, and were diagnosed with any mood disorder (n = 73; 89.0%), followed by any anxiety disorder (n = 45; 54.9%), any eating disorder (n = 14; 17.1%), alcohol/drug misuse (n = 14; 17.1%), and somatoform disorder (n = 3; 3.7%). Three‐quarters (n = 62; 75.6%) had a history of SH (i.e. multiple episodes of SH prior to trial entry). Source of participants: patients presenting to hospital/mental health centre following an episode of SH. Inclusion criteria: i) recently engaged in SH; ii) aged 15‐35; iii) sufficient language ability; iv) residing within the catchment area. Exclusion criteria: i) diagnosed with a psychiatric disorder requiring intensive inpatient treatment; ii) diagnosed with a cognitive impairment. |
|
| Interventions |
Intervention: CBT‐based psychotherapy consisting of 12 sessions (duration not reported) in addition to TAU. Therapeutic content included cognitive restructuring, problem‐solving skills, and behavioural activation. Sessions were delivered by experienced CBT practitioners (no further information on expertise was reported). Comparator: TAU consisting of medication, psychotherapy, or hospitalisation, as required. Length of treatment: 5.5 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from self‐report. Secondary outcome(s): i) anxiety as measured by the anxiety subscale of the SCL‐90; ii) depression as measured by the BDI; iii) problem‐solving as measured by the Coping Inventory for Stressful Situations; iv) self‐esteem as measured by the Robson Self‐Concept Questionnaire, Short version; v) suicidal cognitions as measured by the Suicide Cognition Scale; vi) treatment adherence as measured by the number of sessions attended; vii) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: “Support for the study was provided by The Netherlands Organisation for Health Research and Development (AonMw) (contract grant number: 2100.0068)" (Slee 2008, p. 210). Conflict(s) of interests: none reported. Other: Repetition of SH data provided by participants was subjected to reliability analysis by comparing self reports to hospital records and information from treatment sessions. | |
Sreedaran 2020.
| Study characteristics | ||
| Methods | Participants were individually randomised (1:1) using a computer‐based procedure in blocks of ten to either telephone‐based psychotherapy or a remote contact intervention (telephone contact). N lost to follow‐up: 13/28 (46.4%) for repetition of SH at post‐intervention. Location: Bangalore and New Delhi, India. |
|
| Participants |
Number of total participants: 28 participants were randomised, 15 were allocated to telephone‐based psychotherapy in addition to TAU, and 13 were allocated to a remote contact intervention (telephone contact). Profile of participants: median age 33.7 years (range: 18‐55 years). Three‐quarters (n = 21; 75.0%) were female. Just under one‐third (n = 9; 32.1%) were diagnosed with a common psychiatric disorder (e.g. MDD, any anxiety disorder, adjustment disorder). A minority (n = 1; 3.6%) were diagnosed with a personality disorder. Just under one‐third (n = 9; 32.1%) were not diagnosed with a psychiatric disorder. Source of participants: patients presenting to a general hospital and who had made a recent (within one month) suicide attempt. Inclusion criteria: i) aged 18‐55 years; ii) those with a history of SH (i.e. multiple episodes of attempted suicide); iii) sufficient language ability (English, Hindi, Kannada, Telugu, or Tamil); iv) recent (within one month preceding trial entry) suicide attempt. Exclusion criteria: i) diagnosed with psychosis or SUD according to the MINI, version 6, criteria; ii) diagnosed with an unstable medical illness; iii) diagnosed with a cognitive impairment. |
|
| Interventions |
Intervention: manualised telephone‐based psychosocial intervention consisting of three telephone calls (12‐15 minutes) incorporating principles from supportive therapy, CBT‐based psychotherapy, and DBT. Therapeutic content involved mental status examination, reflective listening, problem‐solving, counselling, and treatment adherence. Sessions were delivered by postgraduate psychologists who received training (duration not reported) in delivering the intervention and ongoing supervision. Comparator: remote contact intervention consisting of three telephone calls (two to five minutes) designed to encourage follow‐up with mental health and other services, as required. Length of treatment: 24 days. |
|
| Outcomes |
Primary outcome(s): i) treatment adherence as measured by dropout rates; ii) satisfaction with treatment as measured by an idiosyncratic scale. Secondary outcome(s): i) repetition of SH (unclear how ascertained); ii) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: "This study was funded by the Indian Council of Medical Research (ICMR), with research oversight by a National Coordination Unit, under Capacity Building Projects of National Mental Health Program, ICMR‐NMHP" (Sreedaran 2020, p.5). Conflict(s) of interest: "The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article" (Sreedaran 2020, p.5). |
|
Stewart 2009.
| Study characteristics | ||
| Methods | Participants were individually randomised by drawing names from a hat to either CBT‐ or PST‐based psychotherapy or TAU. N lost to follow‐up: 0/32 (0%) for repetition of SH at post‐intervention. Location: Brisbane, QLD, Australia. |
|
| Participants |
Number of total participants: 32 participants were randomised, 11 were allocated to CBT‐based psychotherapy, 12 were allocated to PST, and 9 were allocated to TAU. Profile of participants: mean (SD) age not reported (range: 20‐58 years). Just over half (n = 17; 53.1%) were female. No information on psychiatric diagnoses were reported. Source of participants: patients admitted a general hospital following a suicide attempt. Inclusion criteria: i) suicide attempt with self‐reported suicide intent; ii) admitted to hospital. Exclusion criteria: i) diagnosed with an intellectual disability; ii) current diagnosis of mania, psychosis, or both; iii) under 18 years. Correspondence with authors further clarified that one participant was subsequently excluded after randomisation due to being a frequent repeater of SH, possibly in the context of BPD. |
|
| Interventions |
Intervention (CBT‐ or PST‐based psychotherapy): consisting of four weekly individual sessions of cognitive‐behavioural therapy (60 minutes) or seven weekly sessions of PST (60 minutes). CBT‐based psychotherapy was manualised and based on elements of both Beck’s CBT (Beck 1976) and Ellis’ theory of rational emotive therapy (Ellis 1986). PST was also manualised and was based on the 6‐step model of D'Zurilla 1971. Specific information on therapeutic content was not reported, however. Sessions were delivered by "the researcher" (Stewart 2009, p.542) (no further information on expertise or experience was reported). Comparator: TAU consisting of treatment by the hospitals' acute care teams. Length of treatment: two months. |
|
| Outcomes | Primary outcome(s): i) hopelessness as measured by the BHS; ii) problem‐solving as measured by the Social Problem‐Solving Inventory Revised; iii) treatment adherence as measured by the number of sessions attended; iv) satisfaction with treatment as measured by the CSQ‐8; v) suicidal ideation as measured by the BSSI; vi) suicide (unclear how ascertained). | |
| Notes | Source(s) of funding: no sources of funding reported. Conflict(s) of interests: no conflicts of interest reported. | |
Tapolaa 2010.
| Study characteristics | ||
| Methods | Participants were individually randomised using a coin toss to either CBT‐based psychotherapy or TAU. N lost to follow‐up: 0/16 (0%) for repetition of SH by the six‐month follow‐up assessment (following correspondence). Location: Jyväskylä, Finland. |
|
| Participants |
Number of total participants: 16 participants were randomised, 9 were allocated to CBT‐based psychotherapy, and 7 were allocated to TAU. Profile of participants: average age 33.2 years (unclear if mean or median) (range: 18‐65 years). All (n = 16; 100%) were female. Although no information on psychiatric diagnoses were reported, all (n = 16; 100%) were prescribed medication. Source of participants: admissions to an ED following an episode of SH. Inclusion criteria: i) aged 18‐65 years; ii) sufficient language ability; iii) living within the catchment area. Exclusion criteria: none reported. |
|
| Interventions |
Intervention: ACT solution‐focused brief therapy consisting of four weekly sessions (duration not reported) in addition to TAU. Therapeutic content involved meditation, identification of problems, strategies to solve these problems, reflection on alternative methods of problem‐solving, providing motivation to solve these problems, frustration tolerance exercises, and identity assimilation exercises. Sessions were delivered by advanced level psychology students who received 36 hours of training in delivering ACT. Comparator: TAU consisting of four weekly sessions (duration not reported). Correspondence with trial authors clarified that TAU involved psychiatric outpatient treatment in the form of supportive sessions with a mental health nurse in addition to pharmacological treatment, as required. Length of treatment: four weeks. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from self‐report using the SASII. Secondary outcome(s): i) anxiety measured by the BAI; ii) depression measured by the BDI; iii) emotional avoidance measured by the AAQ; iv) emotional regulation measured by the DERS; v) health‐related quality of life measured by the 15D; vi) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: no information on sources of funding reported. Conflict(s) of interests: no information on conflicts of interest reported. | |
Torhorst 1987.
| Study characteristics | ||
| Methods | Participants were individually randomised (method not reported) to either continuity of care by the same therapist or alternative psychotherapy (treatment by a different therapist). N lost to follow‐up: 5/141 (3.5%) for repetition of SH data by the 12 month follow‐up assessment. Location: Munich, Germany. |
|
| Participants |
Number of total participants: 141 participants were randomised, 68 were allocated to crisis intervention followed by outpatient follow‐up by the same therapist, and 73 were allocated to crisis intervention followed by outpatient follow‐up by a different therapist. Profile of participants: average age not reported, range: 18‐65 years. Over half (n = 98; 63.1%) were female. Just under half (n = 68; 48.2%) had a history of SH (i.e. multiple episodes of SH). Source of participants: patients hospitalised following a suicide attempt by self‐poisoning. Inclusion criteria: i) admitted to the toxicology department of a hospital following a suicide attempt by acute intoxication. Exclusion criteria: i) diagnosed with psychosis. |
|
| Interventions |
Intervention: short crisis intervention during hospital stay followed by 12 weekly outpatient appointments with the same therapist (duration not reported). Therapeutic content involved a motivational interview, as well as a letter and assessment of motivation towards therapy delivered by the same therapist. Sessions were delivered by therapists trained (duration not reported) in psychotherapy or behaviour therapy (further information on expertise not reported). Comparator: short crisis intervention during hospital stay followed by outpatient appointments with a different therapist (both the number and duration of these appointments were not reported). Therapeutic content involved a motivational interview, as well as a letter and assessment of motivation towards therapy delivered by different therapists. Length of treatment: three months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report; ii) depression (unclear how measured); iii) treatment adherence as measured by the number of sessions attended; iv) suicide (unclear how ascertained). | |
| Notes | Source(s) of funding: no information on sources of funding reported. Conflict(s) of interests: no information on conflicts of interest reported. Other: in the first phase of this trial, the efficacy of standard care was assessed in terms of compliance. 85 participants were not randomly assigned to this group but were instead “referred routinely” (Torhorst 1987, p. 53). | |
Torhorst 1988.
| Study characteristics | ||
| Methods | Participants were individually randomised (method not reported) to either long‐term (over 12 months) or short‐term (over 12 weeks) psychotherapy. N lost to follow‐up: 0/80 (0%) for repetition of SH at post‐intervention. Location: Munich, Germany. |
|
| Participants |
Number of total participants: 80 participants were randomised, 40 were allocated to long‐term psychotherapy, and 40 were allocated to short‐term psychotherapy. Profile of participants: average age not reported, range: 18‐65 years. All (n = 80; 100%) had a history of SH (i.e. multiple episodes of SH). Source of participants: patients hospitalised following an episode of self‐poisoning and who were referred to the liaison service of a toxicological ward. Inclusion criteria: i) sufficient language ability; ii) living within commuting distance; iii) ≥ 1 suicide attempt preceding trial entry. Exclusion criteria: i) diagnosed with endogenous psychosis; ii) already receiving psychotherapeutic treatment (in‐ or outpatient); iii) overdose involving use of illicit drugs. |
|
| Interventions |
Intervention: long‐term psychotherapy involving one session (duration not reported) per month over a period of 12 months in addition to a brief crisis intervention (duration not reported) delivered three days after admission. Sessions were delivered by psychiatric attendants (no further information on experience was reported). Comparator: short‐term psychotherapy involving 12 weekly sessions (duration not reported) over a period of three months in addition to a brief crisis intervention (duration not reported) delivered three days after admission. Length of treatment: for the experimental arm, 12 months; for the control arm, 3 months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH (unclear how ascertained); ii) depression (unclear how measured); iii) general symptomatology (unclear how measured); iv) treatment adherence as measured by the number of sessions attended. | |
| Notes | Source(s) of funding: “Supported by a grant from the FRG Ministry for Research and Technology” (Torhorst 1988; p. 419). Conflict(s) of interests: no information on conflicts of interest reported. | |
Turner 2000.
| Study characteristics | ||
| Methods | Participants were individually randomised (method not reported) to either DBT or alternative psychotherapy. N lost to follow‐up: 0/24 (0%) for repetition of SH by the post‐intervention assessment. Location: Philadelphia, PA, USA. |
|
| Participants |
Number of total participants: 24 participants were randomised, 12 were allocated to DBT, and 12 were allocated to alternative psychotherapy (client‐centred psychotherapy). Profile of participants: average age 22.0 years (SD not reported) (range: 18‐27 years). The majority (n = 19; 79.2%) were female. Almost all (n = 23; 95.8%) were diagnosed with an Axis I disorder, including: dysthymia with a comorbid generalised anxiety disorder (n = 17), MDD (n = 3), and dysthymia (n = 3). Almost all (n = 23; 95.8%) were also diagnosed with a comorbid Axis II disorder, including: dependent PD (n = 9), histrionic PD (n = 6), narcissistic PD (n = 6), schizotypal PD (n = 3), ASPD (n = 2), paranoid PD (n = 2), and compulsive PD (n = 1). Three‐quarters (n = 18; 75.0%) were also diagnosed with AUD misuse, 83.3% (n = 20) were diagnosed with SUD. Source of participants: patients admitted to hospital following a suicide attempt. Inclusion criteria: i) diagnosed with BPD according to both the Diagnostic Interview for Borderlines and the Personality Disorders Examination criteria; ii) admitted to hospital following a suicide attempt; iii) able to provide written informed consent; iv) consented to randomised assignment. Exclusion criteria: i) diagnosed with schizophrenia, schizoaffective disorder, bipolar disorder, organic mental disorder, or mental retardation. |
|
| Interventions |
Intervention: DBT delivered according to Linehan’s manualised protocol (Linehan 1993) modified to include psychodynamic techniques to conceptualise patients’ behavioural, emotional, and relationship schema. Additionally, no group skills training sessions were provided. Instead, participants received six sessions (duration not reported) of individual therapy to provide interpersonal skills training focusing on the identification of significant persons in the participants’ environment, including problems in relationships and with family. Sessions were delivered by therapists with an average of 22 years clinical experience working in family systems, and in delivering client‐centred and psychodynamic therapy. Therapists also received 12 sessions of training in delivering DBT over three months. Comparator: client‐centred therapy based on Carkhuff 1969. Therapeutic content involved a SH/suicide contract, emphatic understanding, provision of a supportive atmosphere to enable individuation, stress management, and relapse prevention. Participants also received six sessions (duration not reported) of interpersonal skills training focusing on the identification of significant persons in the participants’ environment, including problems in relationships and with family. Concomitant medications: were permitted. The majority (n = 19, 71.2%) were prescribed some form of psychiatric medication. A slightly greater proportion of those allocated to TAU were prescribed medication (91.7% and 66.7%, respectively). Length of treatment: 12 months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report; ii) anger measured by the Target Behavior Ratings; iii) anxiety measured by the Beck Anxiety Inventory; iv) depression as measured by the BDI; v) general symptomatology measured by the Brief Psychiatric Rating Scale; vi) impulsiveness measured by the Target Behavior Ratings; vii) suicidal ideation measured by the BSSI. | |
| Notes | Source(s) of funding: no information on sources of funding reported. Conflict(s) of interests: no information on conflicts of interest reported. | |
Tyrer 2003.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐based allocation sequence with a random blocking procedure stratified by hospital and parasuicide risk to either CBT‐based psychotherapy or TAU. N lost to follow‐up: 50/480 (10.4%) for repetition of SH data at post‐intervention. Location: Glasgow, Edinburgh, Nottingham, West London, and South London, UK. |
|
| Participants |
Number of total participants: 480 participants were randomised, 239 were allocated to manual‐assisted CBT‐based psychotherapy, and 241 were allocated to TAU. Profile of participants: average age 32.0 ± 11.0 years (range: 16‐65 years). The majority (n = 326; 67.9%) were female. Just under half (n = 202; 42.1%) were diagnosed with any PD. Source of participants: patients presenting to hospital following an episode of SH. Inclusion criteria: i) aged 16‐65 years; ii) history of SH prior to trial entry; iii) able to provide informed consent; iv) sufficient language ability; v) lives in the catchment area; vi) available for follow‐up. Exclusion criteria: i) diagnosed with an organic disorder, AOD dependence, schizophrenia or bipolar affective disorder group of according to ICD‐10 diagnostic codes; ii) required psychiatric hospitalisation. |
|
| Interventions |
Intervention: manual‐assisted CBT‐based psychotherapy consisting of up to seven sessions (five sessions during the acute phase, and two further 'booster' sessions; duration not reported). Therapeutic content involved an evaluation of the most recent suicide attempt, crisis skills, PST, cognitive techniques for emotional, and negative thinking management, and the development of relapse prevention strategies. Sessions were delivered by duty therapists (no further information on expertise or experience was reported). Comparator: TAU involving psychiatric assessment, outpatient care, occasional day‐patient care, referral to GP, or a combination of these. Length of treatment: up to 3 months (for the acute phase); up to 6 months (including ‘booster’ phase). |
|
| Outcomes | Primary outcome(s): i) repetition of SH according to SH and as supplemented by GP notes, hospital records or both; ii) anxiety as measured by the HADS; iii) depression as measured by the HADS; iv) hopelessness as measured by the BHS; v) general functioning as measured by the GAS; vi) social functioning as measured by the SFQ; vii) quality of life as measured by the EuroQoL; viii) symptomatology, including personality disorder symptomatology, as measured by the CSRI; ix) suicide (unclear how ascertained). | |
| Notes | Source(s) of funding: “The POPMACT study is funded by the Medical Research Council of the United Kingdom” (Tyrer 2003, p. 67). Conflict(s) of interests: no conflicts of interest reported. | |
Vaiva 2006.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐based pseudo‐random numbers list in opaque sealed envelopes to either a remote contact intervention (telephone contact) or TAU. N lost to follow‐up: 0/605 (0%) for repetition of SH by the 24‐month assessment. Location: Lille, France. |
|
| Participants |
Number of total participants: 605 participants were randomised, 293 were allocated to a remote contact intervention (telephone contact) in addition to TAU, and 312 were allocated to TAU. Profile of participants: mean age 35.7 ± 11.3 years (range: 18‐65 years). The majority (n = 441; 72.9%) were female. A minority (n = 54; 9.0%) had a history of SH (i.e. multiple episodes of SH). No information on psychiatric diagnoses reported. Source of participants: patients presenting to hospital following a drug overdose. Inclusion criteria: i) aged 18‐65 years; ii) hospitalised following a suicide attempt by drug overdose; iii) examined by a psychiatrist who agreed to patients’ discharge; iv) able to provide name of GP; v) able to be contacted by phone; vi) able to provide written consent. Exclusion criteria: i) homeless; ii) addicted to illicit drugs. |
|
| Interventions |
Intervention: remote contact intervention (telephone contact) consisting of a single telephone call (either at one or three months' post‐discharge; duration not reported) to review the ED‐recommended treatment in addition to TAU. Where participants found the treatment recommended during their hospitalisation too difficult to follow, a new regimen was suggested. For those at high risk of suicide, an urgent appointment was made at the emergency department where the patient initially received treatment. No therapy other than support was provided. Sessions were delivered by psychiatrists with a minimum of 5 years experience working with suicidal persons. Comparator: TAU typically involving referral to the participants’ GP. Length of treatment: single telephone call at one or three months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report and hospital records; ii) suicide (unclear how ascertained). | |
| Notes |
Source(s) of funding: “This study was funded by a hospital clinical research grant (PHRC98), a state region contract plan, a subsidy from the regional hospitalization agency” (Vaiva 2006, p. 1245). Conflict(s) of interests: no conflicts of interest reported. |
|
Vaiva 2018.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐based pseudo‐random numbers list using a blocking procedure to either a remote contact intervention (telephone contact combined with emergency cards and letters) or TAU. N lost to follow‐up: data on repetition of SH not reported. Location: various locations, France. |
|
| Participants |
Number of total participants: 987 participants were randomised, 493 were allocated to a remote contact intervention (crisis card, postcards and/or telephone contact) in addition to TAU, and 943 were allocated to TAU. Profile of participants: mean age 38.3 ± 13.3 years (range not reported). Almost two‐thirds (n = 361; 63.4%) were female. Just under half (n = 452; 45.8%) had a history of SH (i.e. multiple episodes of SH). Almost half (n = 481; 48.7%) were diagnosed with MDD, followed by GAD (n = 136; 13.8%), panic disorder (n = 110; 11.1%), dysthymia (n = 103; 10.4%), PTSD (n = 75; 7.6%), any eating disorder (n = 47; 4.8%), social phobia (n = 44; 4.5%), and mania (n = 36; 3.6%). Source of participants: patients presenting to the ED following a suicide attempt. Inclusion criteria: i) presenting to the ED following a suicide attempt. Exclusion criteria: i) admitted to hospital for ≥ 7 days following the index suicide attempt; ii) unable to be contacted by telephone; iii) homeless; iv) under guardianship; v) engaged in ≥ 4 suicide attempts within the three years preceding trial entry. |
|
| Interventions |
Intervention: remote contact intervention consisting of either a crisis card delivered within 24 hours' post‐discharge (for those whose index attempt represented their first episode), telephone contact at days 10 and 21 post‐discharge, or for those who were unable to be contacted by telephone, a series of postcards mailed at two, three, four, and five months post‐discharge (for those who had engaged in multiple episodes of SH). Participants in addition received TAU. Crisis, telephone contacts, and postcards encouraged participants to make contact with the service, if required. No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: TAU consisting of a follow‐up appointment within 24‐48 hours' post‐discharge, and referral to a psychiatrist or physician, as required. Length of treatment: six months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH (at post‐intervention) ascertained from self‐report and electronic medical records. Secondary outcome(s): i) repetition of SH (at 13 months follow‐up) ascertained from self‐report and electronic medical records; ; ii) frequency of repeated SH ascertained from self‐report and electronic medical records; iii) time to SH repetition ascertained from self‐report and electronic medical records; iv) adverse events (i.e. repetition of SH, suicide, and/or loss to follow‐up). |
|
| Notes |
Source(s) of funding: "This study received a Hospital Clinical Research Grant (PHRC 2009) from the French Health Ministry" (Vaiva 2018, p.7). Conflict(s) of interest: "The authors have no conflict of interest to disclose" (Vaiva 2018, p.7). |
|
Van der Sande 1997.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated series of random numbers to either intensive in‐ and outpatient treatment or TAU. N lost to follow‐up: 0/274 (0%) for repetition of SH data by the 12‐month assessment. Location: Utrecht, the Netherlands. |
|
| Participants |
Number of total participants: 274 participants were randomised, 140 were allocated to brief CBT‐based psychotherapy, and 134 were allocated to TAU. Profile of participants: mean age 36.3 ± 15.1 years (range not reported). Just over half (n = 158; 57.7%) were female. Over half (n = 175; 63.9%) also had a history of SH (i.e. multiple episodes of SH). Just over one quarter (n = 77; 28.1%) were diagnosed with a mood disorder. Source of participants: patients admitted to hospital following a suicide attempt. Inclusion criteria :i) admitted to hospital following a suicide attempt; ii) sufficient language ability; iii) lived in catchment area. Exclusion criteria: i) engaged in habitual wrist cutting of minor severity; ii) referred for psychiatric inpatient treatment; iii) imprisoned; iv) diagnosed with a substance addiction; v) required recurrent consultations with a liaison psychiatrist during a stay > 2 days on a somatic ward. |
|
| Interventions |
Intervention: brief psychiatric unit admission to a specialist unit for the treatment of suicide attempters for a period of one to four days. Participants were then offered outpatient treatment based on Hawton and Catalan’s problem‐solving approach (Hawton 1987b) (number and duration of sessions not reported). Therapeutic content involved discussing the reasons behind the current suicide attempt, discussing these reasons with family, partner or both, if required, and changing the ability to cope with future problems. 24‐hour emergency access to the unit was offered throughout the duration of outpatient treatment. Sessions were delivered by psychiatrists, community psychiatric nurses, and psychiatric nurses (no further information on experience was reported). Comparator: TAU. For around one quarter (n = 34) this involved admission to an inpatient unit, whilst for the remaining three‐quarters (n = 100), this involved referral to outpatient services. Length of treatment: unclear. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH ascertained from self‐report, hospital records, or both. Secondary outcome(s): i) hopelessness measured by the BHS; ii) general symptoms measured by the SCL‐90; iii) service use ascertained from self‐report; iv) suicide (unclear how ascertained). |
|
| Notes | Source(s) of funding: “This study was supported by grant OG 92‐023 of the National Health Insurance Council (Ziekenfonds‐Raad)” (Van der Sande 1997, p. 40). Conflict(s) of interests: none reported. | |
Van Heeringen 1995.
| Study characteristics | ||
| Methods | Participants were individually randomised using an open randomisation list to either case management or TAU. N lost to follow‐up: 125/516 (24%) for repetition of SH data by the 12‐month assessment. Location: Ghent, Belgium. |
|
| Participants |
Number of total participants: 516 participants were randomised, 258 were allocated to a compliance enhancement intervention, and 258 were allocated to TAU. Profile of participants: mean (SD) age not reported (range not reported). Just under half (n = 222; 43.0%) were female. Just under one third (n = 155; 30.0%) had a history of SH (i.e. multiple episodes of SH). A minority (n = 77; 14.9%) were diagnosed with any mood disorder, followed by any anxiety disorder (n = 14; 2.7%). Source of participants: patients treated in an A&E department following a suicide attempt. Inclusion criteria: i) aged 15 years of age or older; ii) lived in the catchment area. Exclusion criteria: i) currently receiving inpatient medical treatment. |
|
| Interventions |
Intervention: case management and compliance enhancement involving home visits (number and duration not reported) to those participants who did not keep to scheduled outpatient appointments in addition to TAU. Therapeutic content involved discussing reasons for not attending appointments and the patient was encouraged to attend future treatment sessions. Sessions were delivered by community nurses (no further information on experience was reported). Comparator: TAU consisting of outpatient appointments only (number and duration not reported). Non‐compliant participants did not receive home visits. Length of treatment: not reported. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report supplemented by collateral report from GPs, relatives, or both; ii) treatment adherence measured by the number of sessions attended; iii) suicide (unclear how ascertained). | |
| Notes | Source(s) of funding: “This study was supported by a grant from the National Fund for Scientific Research (NFWO, grant no. 3.0061.86)” (Van Heeringen 1995, p. 969). Conflict(s) of interests: no information on conflicts of interest reported. | |
Walton 2020.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated sequence and a blocking procedure stratified by sex and antidepressant use at baseline, to either DBT or alternative psychotherapy. N lost to follow‐up: 48/162 (25.3%) for repetition of SH by the post‐intervention assessment (data obtained by correspondence). Location: Newcastle, NSW, Australia. |
|
| Participants |
Number of total participants: 162 participants were randomised, 81 were allocated to DBT, and 81 were allocated to alternative psychotherapy (conversational model). Profile of participants: mean age 22.6 ± 7.8 years (range: 18‐65 years). Just over three‐quarters (n = 125; 77.2%) were female. All (n = 162; 100%) were diagnosed with BPD. Just over half (n = 89; 54.9%) were diagnosed with any anxiety disorder, followed by MDD (n = 84; 51.8%), and SUD (n = 45; 27.8%). Source of participants: patients referred to a specialist DBT service. Correspondence with trial authors also revealed that all had engaged in SH resulting in presentation to clinical services within six months preceding trial entry. Inclusion criteria: i) aged 18‐65 years of age; ii) diagnosed with BPD according to DSM‐IV criteria; iii) ≥ 3 episodes of suicide attempts and/or NSSI in the 12 months preceding trial entry. Exclusion criteria: i) diagnosed with an organic disorder, psychosis, or a developmental disability; ii) engaging in antisocial behaviour that posed a significant threat to staff and fellow patients; iii) lived outside the catchment area; iv) insufficient language ability; v) substance dependant (other than nicotine); vi) previously treatment with BDT or conversational psychotherapy. |
|
| Interventions |
Intervention: DBT consisting of 52 weekly individual therapy sessions (60 minutes) and 52 weekly group‐based skills sessions (2.5 hours). Participants also had access to telephone coaching, as required. DBT therapists also participated in weekly consultation team meetings (duration not reported). Therapeutic content involved directive, problem‐oriented techniques (including behavioural skill training, contingency management and cognitive modification) alongside supportive techniques. Sessions were delivered by psychiatrists, psychologists, psychiatric trainees, mental health nurses, social workers, or occupational therapists with a minimum of two years clinical experience and who had received training (duration not reported) in delivering the intervention. Over one‐third (37.5%) delivered both the intervention and comparator conditions. Comparator: manualised conversational model psychotherapy consisting of twice weekly sessions (60 minutes) based on Meares 2004. Therapeutic content was nondirective and included a focus on emotional misunderstanding, mutual self‐reflection, repair of the moment of disconnection in the therapeutic relationship, and the development of an authentic personal narrative. Length of treatment: 14 months. |
|
| Outcomes |
Primary outcome(s): i) frequency of SH ascertained from self‐report using the SASII; ii) depression as measured by the BDI. Secondary outcome(s): i) BPD symptoms as measured by the Borderline Personality Disorder Severity Index (BPDSI‐IV); ii) dissociation as measured by the DES; iii) emotion regulation as measured by the DERS; iv) interpersonal problems as measured by the IIP; v) mindfulness skills as measured by the Kentucky Inventory of Mindfulness Skills (KIMS); vi) sense of self as measured by the Sense of Self Inventory (SSI). |
|
| Notes |
Source(s) of funding: "No external research funding was obtained for this project. We acknowledge the support of Hunter New England Mental Health Service and thank the Centre for Brain and Mental Health Research (University of Newcastle) for providing a small grant specifically to cover the cost of adherence coding" (Walton 2020, p.13). Conflict(s) of interest: "The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article" (Walton 2020, p.13). |
|
Wang 2016.
| Study characteristics | ||
| Methods | Participants were individually randomised "according to the order of their documented suicide report number received...Report numbers with an odd number were grouped into the TAU group, while even numbered reports were grouped into the coping card group" (Wang 2016, p.108). N lost to follow‐up: 0/64 (0.0%) for repetition of SH by the post‐intervention assessment. Location: Chia‐Yi City, Taiwan. |
|
| Participants |
Number of total participants: 64 participants were randomised, 32 were allocated to a remote contact intervention (emergency card), and 32 were allocated to TAU. Profile of participants: mean age 37.9 ± 11.1 years (range: not reported). Almost three‐quarters (n = 47; 73.4%) were female. Just over one third (n = 23; 35.9%) had a history of SH (i.e. multiple episodes of SH). Although over half (n = 39; 60.9%) had previously received psychiatric treatment, no information on psychiatric diagnoses was reported. Source of participants: patients referred by gatekeepers for case management provided by a suicide prevention service following a suicide attempt. Inclusion criteria: i) referred by gatekeepers for case management provided by a suicide prevention service following a suicide attempt; ii) sufficient language ability. Exclusion criteria: i) moved outside of the catchment area; ii) refused a follow‐up visit on ≥ 3 separate occasions; iii) admitted to hospital, another institution, and/or imprisoned for ≥ 1 month; iv) pregnant. |
|
| Interventions |
Intervention: remote contact intervention (crisis card). Participants received a 180 x 108 mm paper folded into a business card size small enough to fit into a wallet. The card provided contact details for a 24‐hour crisis hotline telephone number and local contact details for local medical services. Additionally, participants received a series of six weekly "training sessions" (duration not reported) provided during home visits. Sessions were delivered by clinical psychologists, graduate psychologists, or social workers who received training (30 minutes) in delivering the intervention. Comparator: TAU consisting of a crisis assessment, emotional support, psychological support, and referral for other resources (i.e. community‐based mental health services, social welfare, and vocational training). Length of treatment: 14 months. |
|
| Outcomes |
Primary outcome(s): i) repetition of SH (unclear how ascertained); ii) time to SH repetition (unclear how ascertained). Secondary outcome(s): i) suicide risk measured by the Suicide Risk Inventory (SRI); ii) suicidal ideation measured by the suicidal ideation subscale of the SRI; iii) hopelessness measured by the BHS; iv) general symptoms measured by the BSRS. |
|
| Notes | Source(s) of funding: no information on sources of funding reported. Conflict(s) of interests: no information on conflicts of interest reported. | |
Waterhouse 1990.
| Study characteristics | ||
| Methods | Participants were individually randomised using sequentially numbered sealed envelopes to either general hospital admission or discharge. N lost to follow‐up: 0/77 (0%) for repetition of SH data at post‐intervention. Location: York, UK. |
|
| Participants |
Number of total participants: 77 participants were randomised, 38 were allocated to a short‐stay hospital admission, and 39 were allocated to alternative psychotherapy (discharge from hospital). Profile of participants: mean age 30.0 years (SD not reported; range: not reported). Over half (n = 48; 62.3%) were female. Over one third (n = 28; 36.4%) had a history of SH (i.e. multiple episodes of SH). Source of participants: patients admitted to an A&E department following an episode of SH. Inclusion criteria: i) aged 16 years or older. Exclusion criteria: i) had immediate medical and/or psychiatric treatment needs. |
|
| Interventions |
Intervention: general hospital admission excluding additional treatment or counselling. “Hospital admission consisted of little more than a bed, without further referral to other helping agencies” (Waterhouse 1990, p. 238). No information on who delivered the intervention, their expertise, or their experience was reported. Comparator: discharge from hospital. Length of treatment: median length of admission was 17 hours. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from collateral informant report (GPs), hospital records, or both; ii) social functioning as measured by the Social Behaviour Assessment Schedule; iii) depression and anxiety (unclear how ascertained); iv) hopelessness measured by the BHS; iv) social isolation (unclear how ascertained); v) suicidal ideation as measured by the BSSI. | |
| Notes | Source(s) of funding: no specific sources of funding were reported. Conflict(s) of interests: “John Waterhouse was in receipt of a research grant from the Yorkshire Regional Health Authority” (Waterhouse 1990, pg. 241). Other: As depression data had been combined with anxiety data in this trial, this outcome could not be included in the present review. | |
Wei 2013.
| Study characteristics | ||
| Methods | Participants were individually randomised using a computer‐generated sequence to either a CBT‐based psychotherapy, a telephone intervention, or TAU. N lost to follow‐up: 67/239 (28.0%) for repetition of SH at post‐intervention; 123/239 (51.5%) at the six‐month follow‐up; 151/239 (63.2%) at the 12‐month follow‐up. Location: Shenyang, Liaoning Province, China. |
|
| Participants |
Number of total participants: 239 participants were randomised, 82 were allocated to CBT‐based psychotherapy, 80 were allocated to a telephone intervention, and 77 were allocated to TAU. Profile of participants: mean age 32.7 ± 14.0 (range: not reported). Just over three‐quarters (n = 182; 76.1%) were female. Just under half (n = 108; 45.2%) were diagnosed with any psychiatric disorder. Source of participants: patients admitted to ED following a suicide attempt. Inclusion criteria: i) older than 15 years; ii) admitted to ED following a suicide attempt; iii) ≥ 1 contact person to provide collateral reports on suicidal behaviour; iv) able to understand the trial procedures; v) able to provide written informed consent. Exclusion criteria: none reported. |
|
| Interventions |
Intervention: there were two experimental arms in this trial: i) CBT‐based psychotherapy, and ii) telephone intervention. CBT‐based psychotherapy consisted of 10 weekly/biweekly/monthly sessions (45‐60 minutes). The telephone intervention involved 12 psychological support calls (20‐40 minutes). Therapeutic content involved reassurance, emphatic reasoning, collaborative PST, stress management, and encouraging participants to increase contact with existing social supports (e.g. family, friends). Sessions were delivered by therapists (no further information on expertise) with a minimum of five years clinical work experience. Comparator: "[P]atients in the control group did not receive any interventions” (Wei 2013, p. 109). Length of treatment: three months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report and/or collateral informant report; ii) depression measured by the HDRS; iii) quality of life measured by an idiosyncratic scale; iv) suicidal ideation measured by the BSSI; v) suicide (unclear how ascertained). | |
| Notes | Source(s) of funding: “This project was part of the Small Grants Program to Improve the Quality and Implementation of Suicide Research in China’ which was supported by the China Medical Board of New York (grant number 05‐813)” (Wei 2013, p. 113). Conflict(s) of interests: no conflicts of interest reported. | |
Weinberg 2006.
| Study characteristics | ||
| Methods | Participants were individually randomised by asking participants to choose between two similar envelopes to either CBT‐based psychotherapy or TAU. N lost to follow‐up: 0/30 (0%) for repetition of SH data by the six‐month assessment. Location: Boston, MA, USA. |
|
| Participants |
Number of total participants: 30 participants were randomised, 15 were allocated to manual assisted CBT‐based psychotherapy, and 15 were allocated to TAU. Profile of participants: mean age 28.2 ± 8.2 (range: 18‐40 years). All (n = 30; 100%) were female. Source of participants: recruited from the community via advertisements in local newspapers, clinical services at a hospital, and from individuals participating in a longitudinal study. Inclusion criteria: i) female; ii) aged 18‐40 years; iii) diagnosed with BPD; iv) history of repetitive SH with at ≥ 1 episode during the month prior to trial entry. Exclusion criteria: i) diagnosed with comorbid psychosis; ii) judged to be at an elevated risk of suicide; iii) diagnosed with substance abuse; iv) history of attempted suicide (only those engaging in repetitive SH were eligible for inclusion in this trial). |
|
| Interventions |
Intervention: manual assisted CBT‐based psychotherapy consisting of six sessions (duration not reported). Therapeutic content included evaluation of the attempt, developing crisis skills problem‐solving skills, developing cognitive techniques for emotional and negative thinking management, and relapse prevention. The primary investigator acted as the therapist (no further information on expertise or experience was reported). Comparator: TAU. Length of treatment: two months. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report using the PHI; ii) borderline symptoms measured by the Revised Diagnostic Interview for Borderlines; iii) suicidal ideation measured by the Suicide Behaviors Questionnaire; iv) service use measured by the Treatment Utilization Interview; v) suicide (unclear how ascertained). | |
| Notes | Source(s) of funding: ”This study was supported by a Young Investigator Award from the Borderline Personality Disorder Research Foundation (I.W.)“ (Weinberg 2006, p. 482). Conflict(s) of interests: no conflict of interest reported. Other: All participants were also simultaneously participating in additional treatment throughout the duration of this trial. | |
Welu 1977.
| Study characteristics | ||
| Methods | Participants were individually randomised using a random numbers table to either intensive outpatient treatment or TAU. N lost to follow‐up: 1/120 (0.8%) for repetition of SH data by the four‐month assessment. Location: Pittsburgh, PA, USA. |
|
| Participants |
Number of total participants: 120 participants were randomised, 63 were allocated to intensive outpatient treatment, and 57 were allocated to TAU. Profile of participants: average age 29.0 years (IQR/SD not reported; range: not reported). Information on sex not reported. Over half (n = 72; 60.0%) had a history of SH (i.e. multiple episodes of SH). Source of participants: patients admitted to an A&E department following an episode of SH. Inclusion criteria: i) over 16 years of age. Exclusion criteria: i) student living in university accommodation; ii) resident in a care‐giving institution or institutionalised at the time of the index episode of SH. |
|
| Interventions |
Intervention: outreach programme involving a community mental health team contacting participants immediately after discharge to arrange weekly/biweekly home visits. Sessions were delivered by nurses, social workers, and community workers (further information on experience was not reported). Comparator: TAU involving a psychiatric consultation at request of the treating physician. Participants were also given a next day appointment for evaluation at the community mental health team centre. Any further contact after discharge was at the participant’s request. Length of treatment: unclear. |
|
| Outcomes | Primary outcome(s): i) repetition of SH ascertained from self‐report, hospital records, and/or collateral informant report; ii) AOD use ascertained from self‐report, hospital records, and/or collateral informant report; iii) adverse events (purposive accidents) ascertained from self‐report, hospital records, and/or collateral informant report; iv) service use ascertained from records. | |
| Notes | Source(s) of funding: “This investigation was supported by Research Grant MH19491 from the National Institute of Mental Health” (Welu 1977, p. 17). Conflict(s) of interests: no conflicts of interest reported. | |
AA: alcoholics anonymous AAQ: Acceptance and Action Questionnaire ACT: Acceptance and Commitment Therapy A&E: Accident and Emergency AOD: alcohol and other drug ASPD: antisocial personality disorder ASSIP: Attempted Suicide Short Intervention Program AUD: Alcohol use disorder AUDIT: Alcohol Use Disorders Identification Test BAI: Beck Anxiety Inventory BDI: Beck Depression Inventory BEST: Brief Education Supported Treatment BHS: Beck Hopelessness Scale BIS: Barratt Impulsiveness Scale BPD: borderline personality disorder BPDSI‐IV: Borderline Personality Disorder Severity Index, 4th revision BSRS: Brief Symptom Rating Scale BSSI: Beck Scale for Suicidal Ideation CAMS: Collaborative Assessment and Management of Suicidality CBT: Cognitive Behavioural Therapy CGI: Clinical Global Impression CIP: Cultural Impact Profile cRCT: cluster randomised controlled trial CSQ‐8: Client Satisfaction Questionnaire (8 item) CSRI: Client Services Receipt Inventory DASS: Depression Anxiety Stress Scale DBT: Dialectical Behaviour Therapy DERS: Difficulties in Emotion Regulation Scale DES(‐T): Dissociative Experiences Scale (‐Taxon) DSHI: Deliberate Self‐Harm Inventory DSM‐IV(‐TR): Diagnostic and Statistical Manual for mental disorders, version IV (Text Revision) ED: emergency department EPSIS: European Parasuicide Study Interview Schedule EQ‐5D: European Quality of Life‐5 Dimension ESS: Experience of Shame Scale EUC: enhanced usual care EuroQoL: European Quality of Life FRAMES: Feedback, Responsibility, Advice, Menu, Empathic, and Self‐efficacy GAD: Generalized Anxiety Disorder GAF: General Assessment of Functioning GAS: Global Assessment Scale GHQ(‐12): General Health Questionnaire (12 item) GP: general practitioner GSI: Global Severity Index HADS: Hospital Anxiety and Depression Scale HAMD‐24: Hamilton Rating Scale, 24‐item HDRS: Hamilton Depression Rating Scale HRSA: Health Resources and Services HRSD: Hamilton Rating Scale for Depression HSRS: Health Sickness Rating Scale ICD‐10: International Classification of Diseases, 10th Revision IIP: Inventory of Interpersonal Problems IQ: intelligence quotient IQR: interquartile range KIMS: Kentucky Inventory of Mindfulness Skills LSASI: Lifetime Suicide Attempt Self‐Injury Interview MBT: Mentalisation‐Based Therapy MDD: Major Depressive Disorder MEPS: Means‐Ends Problem‐Solving procedure MINIM: minimisation programme MMPI: Minnesota Multiphasic Personality Inventory NA: narcotics anonymous NR: not reported NSSI: non‐suicidal self‐injury PD: personality disorder p.: page PHI: Parasuicide History Inventory PSS‐I: PTSD Symptom Scale ‐ Interview PST: problem‐solving therapy PTSD: Post‐traumatic stress disorder SAPAS: Standardised Assessment of Personality ‐ Abbreviated Scale SAS: Social Assessment Scale SASII: Suicide Attempt‐Self‐Injury Interview SCID‐II: Structured Clinical Interview for DSM‐IV Axis II Personality Disorders SCL‐90: Symptom Check List‐90 SD: standard deviation SF‐36: Social Functioning ‐ 36 item SFQ: Social Functioning Questionnaire SH: self‐harm SHI: Self‐Harm Inventory SMART: Specific, Measurable, Achievable, Relevant, and Time‐bound SPSI: Social Problem‐Solving Inventory SRI: Suicide‐Resilience Inventory SSRI: Selective Serotonin Reuptake Inhibitor STAXI: State‐Trait Anxiety Inventory SUD: substance use disorder SUPRE‐MISS: SUicide‐PREvention Multisite Intervention Study on Suicidal behaviours TAU: Treatment‐as‐usual THI‐2: Treatment History Interview‐2 TRGI: Trauma‐Related Guilt Interview VHS: Volitional Help Sheet vs.: versus WHO: World Health Organization ZAN‐BPD: Zanarini Rating Scale for Borderline Personality Disorder 15D: 15D measure of health‐related quality of life
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agyapong 2016 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Ahmed 2016 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Albuixech‐García 2020 | Non‐RCT |
| Andover 2015 | Non‐RCT |
| Andover 2017 | At baseline, 78.8% of the sample had engaged in SH. |
| Andreasson 2016 | Due to difficulties in recruitment, inclusion criteria for recency of SH was changed from within one month of trial entry to within five years of trial entry. At baseline, 96% of the sample had engaged in SH. |
| Andreoli 2019 | Reported on outcomes ≥ 3 years post‐intervention. Data for earlier follow‐up assessments were included in this review, however. |
| Barnes 2018 | At baseline, 25.0% of the sample had engaged in SH. |
| Barnhofer 2015 | Participants engaging in regular SH were excluded. |
| Bateman 2020 | Reported on outcomes ≥ 8 years post‐intervention. Data for earlier follow‐up assessments were included in this review, however. |
| Bentley 2017 | At baseline, mean number of SH episodes per participant was < 1, suggesting that not all some participants had engaged in SH. |
| Berrouiguet 2019 | Study protocol. However, non‐RCT |
| Betz 2020 | Correspondence with trial authors indicated information on SH within six months of trial entry was not recorded. However, at baseline, 6.1% of the sample had presented to the ED with SH. |
| Bryan 2017a | At baseline, 56.0% of the sample had engaged in SH. |
| Bryan 2017b | At baseline, 44.0% of the sample had engaged in SH. |
| Cebria 2015 | Non‐RCT |
| Celano 2017 | Correspondence with trial authors indicated information on SH within six months of trial entry was not recorded. However, at baseline, 41.5% had engaged in SH. |
| Currier 2015 | Study protocol. However, non‐RCT |
| Dassa 2018 | We were unable to locate full text despite correspondence. |
| Davidson 2006 | Information on SH within six months of trial entry was not recorded. However, at baseline, 70.7% had engaged SH. |
| Dimeff 2020 | Non‐RCT |
| Di Simplicio 2020 | Participants were recruited from non‐clinical settings. |
| Dixon‐Gordon 2015 | Participants were recruited from non‐clinical settings. |
| Doering 2010 | At baseline, 61.5% of the sample had engaged in SH. |
| Ducasse 2018 | We were unable to obtain data on the proportion of participants with an episode of SH within six months of trial entry from trial authors. However, at baseline, 27.5% had engaged in SH within one month of trial entry. |
| Exbrayat 2017 | Non‐RCT |
| Franklin 2016 | Participants were recruited from non‐clinical settings. |
| Gabilondo 2020 | Non‐RCT |
| Galfalvy 2017 | We were unable to locate full text despite correspondence. |
| Gooding 2020 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Goodman 2016 | We were unable to obtain data on the proportion of participants with an episode of SH within six months of trial entry from trial authors. |
| Goodman 2020 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Haddock 2019 | We were unable to obtain data on the proportion of participants with an episode of SH within six months of trial entry from trial authors. |
| Hashemi‐Aliabadi 2020 | Non‐RCT |
| Hooley 2014 | At baseline, 74.6% of the sample had engaged in SH. |
| Hooley 2018 | Participants were recruited from non‐clinical settings. |
| Hurtado‐Santiago 2018 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Inder 2015 | At baseline, 50.0% of the sample had engaged in SH. |
| ISRCTN10115835 | Recruitment into this trial has suspended. |
| ISRCTN16003313 | Trial paused. Recruitment into this trial has suspended due to COVID‐19 restrictions. |
| ISRCTN16049211 | Trial paused. Recruitment into this trial has suspended due to COVID‐19 restrictions. |
| ISRCTN16862589 | Trial paused. Recruitment into this trial has suspended due to COVID‐19 restrictions. |
| ISRCTN18761534 | Trial registration record last updated 12 December 2017. Current status therefore unknown |
| Jardon 2019 | Non‐RCT |
| Jobes 2017 | At baseline, 50.0% of the sample had engaged in SH. |
| Johnson 2018 | SH did not occur within six months of trial entry. |
| Kawanishi 2018 | Study protocol for a cohort follow‐up study of an RCT. Data from the RCT were included in this review, however. |
| Kennedy 2018 | Participants were recruited from non‐clinical settings. |
| Kholodkov 2015 | Participants were recruited from non‐clinical settings. |
| Kim 2020 | Non‐RCT |
| Kline 2016 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Korczak 2020 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| LaCroix 2018 | Correspondence with trial authors indicated that, at baseline, 86.1% of the sample had engaged in SH. |
| Lahoz 2016 | Reported on outcomes ≥ 5 years post‐intervention. |
| Lin 2019 | Participants were recruited from non‐clinical settings. |
| Luxton 2014 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Mackie 2017 | Non‐RCT (qualitative investigation) |
| Marriott 2016 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Matsubara 2019 | Non‐RCT |
| McCall 2019 | At baseline, 30.1% of the sample had engaged in SH. |
| McManama O'Brien 2018 | Correspondence with trial authors indicated information on SH within six months of trial entry not recorded. However, at baseline, 80.4% had a lifetime history of SH. |
| Miller 2016 | At baseline, 74.5% had engaged in SH. |
| Morley 2014 | At baseline, 55.1% had engaged in SH within six months of trial entry. |
| Navarro‐Haro 2018 | Correspondence with trial authors indicated that, at baseline, 38.9% had engaged in NSSI and 38.9% had made a suicide attempt. |
| NCT00218725 | Correspondence with trial authors indicated the trial was terminated early due to feasibility problems in identifying and recruiting participants. |
| NCT00601939 | Trial paused. Recruitment into this trial has suspended due to COVID‐19 restrictions. |
| NCT00603421 | We were unable to locate full text despite correspondence. |
| NCT00641498 | We were unable to locate full text despite correspondence. |
| NCT00980824 | Trial registration record last updated 28 June 2010. Current trial status therefore unknown |
| NCT01359761 | Sample overlapped with LaCroix 2018. |
| NCT01823120 | Correspondence with trial authors indicated the trial was terminated early due to a lack of funding and resignation of critical trial staff. |
| NCT01952405 | We were unable to locate full text despite correspondence. |
| NCT02227160 | Trial was withdrawn due to a lack of funding. |
| NCT02299440 | We were unable to obtain data on the proportion of participants with an episode of SH within six months of trial entry from trial authors. |
| NCT02522143 | Trial was withdrawn due to a lack of funding. |
| NCT02742922 | Trial registration record last updated 1 February 2018. Current trial status therefore unknown |
| NCT03300596 | We were unable to locate full text despite correspondence. |
| NCT03376113 | Trial registration record last updated 1 December 2018. Current trial status therefore unknown |
| NCT03489382 | Trial registration record last updated 1 June 2018. Current trial status therefore unknown |
| NCT03533075 | Trial registration record last updated 1 August 2019. Current trial status therefore unknown |
| NCT03600532 | Trial terminated early due to feasibility problems in identifying and recruiting participants |
| NCT03943862 | Trial terminated early due to feasibility problems in identifying and recruiting participants |
| O'Toole 2019 | At baseline, 16.3% of the sample had engaged in SH. |
| Pearce 2017 | At baseline, 66.7% of the sample had engaged in SH. |
| Pfeiffer 2019 | At baseline, 77.1% of the same had engaged in SH. |
| Philips 2018 | Participants were recruited from non‐clinical settings. |
| Pistorello 2020 | At baseline, 30.6% of the sample had engaged in SH. |
| Pratt 2015 | At baseline, 85.5% of the sample had engaged in SH. |
| Rees 2015 | Trial terminated early due to feasibility problems in identifying and recruiting participants |
| Rompogren 2018 | Participants were recruited from non‐clinical settings. |
| Rudd 2015 | At baseline, 59.3% of the sample had engaged in SH. |
| Ryberg 2019 | At baseline, 69.2% of the sample had engaged in SH. |
| Sáiz 2014 | Correspondence with trial authors indicated that not all participants were randomised to the intervention or control arms; some could choose to receive the intervention (i.e. non‐RCT). |
| Santel 2020 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Sayal 2019 | Trial terminated early due to to feasibility problems in identifying and recruiting participants. Additionally, at baseline, 81.8% of the sample had engaged in SH. |
| Sequeira 2016 | At baseline, 15.4% of the sample had engaged in SH. |
| Simon 2016 | Study protocol. However, unlikely that all participants would have engaged in SH at baseline |
| Sinnaeve 2018 | Correspondence with trial authors indicated information on SH within six months of trial entry was not recorded. However, at baseline, 91.7% of the sample had engaged in SH. |
| Slesnick 2020 | At baseline, 80.0% of the sample had engaged in SH. |
| Smits 2020 | At baseline, 42.1% had engaged in NSSI and 16.7% had made a suicide attempt. |
| Taha 2015 | SH did not occur within six months of trial entry. |
| Tejedor 2011 | Correspondence with trial authors indicated information in SH within six months of trial entry was not recorded. However, at baseline, 39.0% had engaged in SH. |
| Vaiva 2016 | Book chapter |
| Van Spijker 2018 | At baseline, 54.3% of the sample had engaged in SH. |
| Ward‐Ciesielski 2016 | Participants were recruited from non‐clinical settings. |
| Westling 2019 | At baseline, 80.0% of the sample had engaged in SH. |
| Wilks 2018 | Participants were recruited from non‐clinical settings. |
| Wittouck 2014 | Participants were those bereaved by suicide. |
| Yang 2020 | Participants were recruited from non‐clinical settings. |
ED: emergency department; NSSI: non‐suicidal self‐injury; RCT: randomised controlled trial; SH: self‐harm.
Characteristics of studies awaiting classification [ordered by study ID]
NCT00533117.
| Methods | Triple (participant, investigator, outcome assessor)‐blind RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged between 18 and 55 years; ii) diagnosed with borderline personality disorder; iii) at least one suicide attempt in the two months preceding trial entry; iv) at least one further suicide attempt in the year preceding trial entry; v) experiences continued SH urges; vi) stable living situation; vii) clinically stable enough to undergo a wash‐out of all psychotropic medications; viii) not participating in other forms of treatment; ix) women of child‐bearing age must also be using effective birth control Exclusion criteria: i) diagnosed with any organic mental disorder (current); ii) lifetime diagnosis of schizophrenia, another psychosis, bipolar disorder, or mental retardation; iii) unable and/or unwilling to complete a psychiatric interview; iv) unable to tolerate DBT or fluoxetine; v) currently receiving treatment for an acute medical illness, including substance abuse or anorexia nervosa; vi) history of major depression lasting longer than three months; vii) Hamilton Depression Score > 22; viii) pregnant or breastfeeding |
| Interventions |
Intervention 1 (DBT plus fluoxetine): DBT consisting of twice weekly individual therapy sessions (60 minutes' duration) and once weekly group therapy sessions (90 minutes' duration) for 12 months in addition to fluoxetine administered with a starting dose of 20 mg/day increasing by 20 mg/day in monthly increments to one month, depending on tolerability, to up to 80 mg/day Intervention 2 (Supportive psychotherapy plus fluoxetine): Supportive psychotherapy consisting of weekly individual therapy sessions (50 minutes' duration) for 12 months in addition to fluoxetine administered with a starting dose of 20 mg/day increasing by 20 mg/day in monthly increments to one month, depending on tolerability, to up to 80 mg/day Comparator 1 (DBT plus placebo): DBT consisting of twice weekly individual therapy sessions (60 minutes' duration) and once weekly group therapy sessions (90 minutes' duration) for 12 months in addition to placebo Comparator 2 (Supportive psychotherapy plus placebo): Supportive psychotherapy consisting of weekly individual therapy sessions (50 minutes' duration) for 12 months in addition to placebo |
| Outcomes | Primary outcome(s): i) repetition of SH as ascertained from self‐report |
| Notes |
NCT00834834.
| Methods | Single‐blind RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) meets DSM‐IV criteria for borderline personality disorder; ii) at least one suicide attempt in the two months preceding trial entry; iii) at least one further suicide attempt in the year preceding trial entry; iv) current suicidal ideation; v) not currently receiving optimum psychiatric treatment; vi) has a stable living arrangement; v) sufficient language ability; vi) clinically stable enough to undergo a washout of all psychotropic medications with the exception of benzodiazepines; viii) women of child‐bearing age must also be using effective birth control Exclusion criteria: i) diagnosed with an intellectual disability, bipolar disorder, schizophrenia, delusional disorder; schizophreniform disorder, schizoaffective disorder, or a psychotic disorder not otherwise specified; ii) severe psychiatric disorder or medical condition requiring acute treatment; iii) clinically too unstable to be treated as an outpatient; iv) failed two adequate trials of fluoxetine and citalopram within the two years preceding trial entry; v) history of severe allergies, adverse drug reactions, or known allergy to fluoxetine or citalopram; vi) has a heart pacemaker body implant, other metal implants, shrapnel or surgical prostheses that may present a risk to the participant or interfere with the fMRI scan; vii) diagnosed with Raynaud's disorder; viii) history of hypertension, cardiovascular disease, or abnormal electrocardiograms; ix) claustrophobia or significant discomfort in enclosed space; x) pregnant |
| Interventions |
Psychosocial: DBT consisting of weekly individual therapy sessions (60 minutes' duration) and group therapy sessions (90 minutes' duration) for six months Pharmacological: fluoxetine. Starting dose of 20 mg/day increasing to over four weeks, depending on tolerability, to up to 40 mg/day. Treatment will last six months. |
| Outcomes |
Primary outcome(s): i) SH, as measured by the Columbia Suicide History Interview (CSHI) Secondary outcome(s): i) number of participants with SH, as measured by the CSHI |
| Notes |
CSHI: Columbia Suicide History Interview; DBT: dialectical behaviour therapy; DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, fourth revision; fMRI: functional magnetic resonance imaging; mg: milligram; RCT: randomised controlled trial; SH: self‐harm.
Characteristics of ongoing studies [ordered by study ID]
ACTRN12617000529347.
| Study name | Will prisoners who self‐harm reduce their frequency of self‐harming after going through the dialectical behaviour therapy intervention? |
| Methods | Open‐label RCT Allocation: parallel‐group, blocked, individual‐level |
| Participants |
Inclusion criteria: i) males; ii) between 14 and 21 years of age; iii) convicted of any offence and currently serving a term of imprisonment; iv) remaining length of sentence of six months or greater; v) able to understand trial procedures (but not necessarily how to read or write) Exclusion criteria: i) females; ii) insufficient language ability; iii) foreign nationality; iv) diagnosed with a psychiatric disorder, alcohol, drug, or other physical health condition that would interfere with participation |
| Interventions |
Intervention: group‐based DBT. Twice weekly sessions (two hours' duration) of manualised, group‐based DBT for 12 weeks Comparator. TAU, consisting of psychoeducation and ongoing monitoring by prison medical staff |
| Outcomes |
Primary outcome(s): i) SH, as measured by the Inventory of Statements about Self‐Injury (ISAS); ii) borderline personality disorder symptoms, as measured by the Structured Clinical Interview for Borderline Personality Disorder (SCID‐BPD) Secondary outcome(s): i) well‐being, as measured by the Well‐being Survey; ii) emotion regulation, as measured by the Difficulties in Emotion Regulation Scale (DERS) |
| Starting date | 26 April, 2017 |
| Contact information |
Principal investigator: Prof. Brin Grenyer, University of Wollongong, Wollongong, New South Wales, Australia (grenyer@uow.edu.au) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
Berrouiguet 2014.
| Study name | SIAM (Suicide Intervention Assisted by Messages): The development of a post‐acute crisis text messaging outreach for suicide prevention |
| Methods | Open‐label RCT Assignment: parallel‐group, blocked, individual‐level |
| Participants |
Inclusion criteria: i) aged 18 years and older; ii) discharged from the emergency department and/or psychiatric unit following a presentation for attempted suicide; iii) hospitalised for < 7 days; iv) able to provide informed consent; v) able to be contacted by telephone Exclusion criteria: i) unwilling or unable to provide informed consent; ii) under guardianship; iii) incarcerated; iv) enrolled in other trials; v) not in possession of a mobile (cell) telephone |
| Interventions |
Intervention: a series of nine text messages sent within 48 hours post‐discharge, at days 8, 15, and at months 1, 2, 3, 4, 5, and 6. Message content will provide validation, reminders of discharge agreements, and will also include information on how to access support from the participants’ managing doctor (i.e. psychiatrist or general practitioner, as appropriate), as well as appointment reminders. Comparator: TAU |
| Outcomes |
Primary outcome(s): i) repetition of SH as measured by the Columbia Scale Secondary outcome(s): i) suicidal ideation as measured by the Columbia Scale; ii) satisfaction with treatment as measured using a study‐specific scale |
| Starting date | 8 April, 2014 |
| Contact information |
Principal investigator: Dr. Sofian Berrouiguet, Brest Medical University Hospital, Brest, France (sofian.berrouiguet@gmail.com) |
| Notes |
Chaïb 2020.
| Study name | Group post‐admission cognitive therapy for suicidality vs individual support therapy for the prevention of repeat suicide attempts: a randomized controlled trial |
| Methods | Single (assessor)‐blind RCT Allocation: parallel‐group, blocked, individual‐level |
| Participants |
Inclusion criteria: i) aged 18 years and older; ii) hospitalised for the prevention of suicide; iii) high suicide risk score, as measured by the MINI; iv) suicide attempt within the month prior to trial entry; v) available to attend mid‐week appointments; vi) insured or beneficiary of a health insurance plan; vii) sufficient language ability; viii) able to provide informed consent Exclusion criteria: i) participated in another interventional trial within the three months prior to trial entry; ii) under an exclusion period as a consequence of participating in another trial; iii) under judicial protection or is an adult under legal guardianship; vi) unable and/or unwilling to provide informed consent; v) diagnosed with schizophrenia or another psychotic disorder according to the MINI; vi) diagnosed with a severe cognitive impairment on clinical observation; vii) diagnosed with a severe AOD dependence |
| Interventions |
Intervention: group‐based CBT consisting of six weekly sessions (90‐120 minutes' duration) over six weeks. Therapeutic content is based on the Post‐Admission Cognitive Therapy model (Ghahramanlou‐Holloway 2012). Therapeutic content includes: i) psychoeducation; ii) problem identification; iii) cognitive restructuring; iv) behavioural activation; v) identification of reasons for living; vi) hope box; vii) emotion regulation; viii) development of coping strategies; ix) problem‐solving; x) relapse prevention; xi) safety planning. Comparator: individual supportive therapy consisting of six weekly sessions (60‐90 minutes' duration) over six weeks. Therapeutic content includes: i) providing a supportive, non‐judgemental and empathetic environment in which the participant can explore reasons for SH. Therapists are specifically told to avoid applying any principles of CBT‐based psychotherapy. Length of treatment: six weeks |
| Outcomes |
Primary outcome(s): i) time to SH repetition (unclear how ascertained) Secondary outcome(s): i) suicidal ideation, as measured by the C‐SSRS and the BSSI; ii) depression, as measured by the BDI; iii) hopelessness, as measured by the BHS; iv) general symptoms, as measured by the MINI‐7; v) suicide attempt lethality, as measured by the Risk Rescue Rating Scale (RRRS) |
| Starting date | 1 November, 2017 |
| Contact information |
Pincipal investigator: Dr. Laurent Chaïb, Centre Hospitalier Université de Nîmes, Nîmes, France (laurent.chaib@chu-nimes.fr) |
| Notes |
McMain 2018.
| Study name | The effectiveness of 6 versus 12‐months of dialectical behaviour therapy for borderline personality disorder: the feasibility of a shorter treatment and evaluating responses (FASTER) trial protocol |
| Methods | Multisite, single (assessor)‐blind RCT Allocation: parallel‐group, blocked, individual‐level |
| Participants |
Inclusion criteria: i) aged between 18 and 65 years; ii) diagnosed with BPD according to DSM‐IV criteria and the International Personality Disorders Examination; iii) ≥ 2 episodes of SH in the five years prior to trial entry, including ≥ 1 episode in the eight weeks prior to trial entry; iv) sufficient language ability; v) able to provide informed consent; vi) have either Ontario Health Insurance Plan (OHIP) coverage or BC Medical Services Plan (MSP) health insurance for ≥ 1 year Exclusion criteria: i) received > 8 weeks of DBT in the 12 months prior to trial entry; ii) diagnosed with psychosis, bipolar disorder, or dementia according to DSM‐IV criteria; iii) estimated IQ ≤ 70; iv) diagnosed with a chronic physical health condition expected to require periods of hospitalisation within the next 12 months (e.g. cancer); v) plan to move outside of the catchment area within the next two years |
| Interventions |
Intervention 1: manualised DBT (12‐month protocol) consisting of weekly sessions (one hour) of individual therapy, weekly sessions (2 hours) of group skills training, access to 24/7 telephone consultation, as needed, and weekly (duration not reported) therapist consultation meetings. Therapeutic content involves: i) acceptance‐based techniques; ii) problem‐solving; iii) behavioural analysis; iv) contingency management; v) skills training. Intervention 2: manualised DBT (six‐month protocol) consisting of weekly sessions (one hour) of individual therapy, weekly sessions (2 hours) of group skills training, access to 24/7 telephone consultation as needed, and weekly (duration not reported) therapist consultation meetings. Therapeutic content involves: i) acceptance‐based techniques; ii) problem‐solving; iii) behavioural analysis; iv) contingency management; v) skills training. |
| Outcomes |
Primary outcome(s): i) frequency of SH, as measured by the SASII; ii) severity of SH, as measured by the SASII Secondary outcome(s): i) characteristics of SH, as measured by the L‐SASI; ii) service use, as measured by the Treatment History Interview, version 2; iii) borderline symptoms, as measured by the Borderline Symptom List‐23; iv) impulsivity, as measured by the Barratt Impulsiveness Scale‐11; v) depression, as measured by the BDI; anger, as measured by the State‐Trait Anger Expression Inventory‐2; vi) general symptomatology, as measured by the Symptom Checklist‐90 Revised; vii) interpersonal functioning, as measured by the Inventory of Interpersonal Problems‐64; viii) social functioning, as measured by the Social Adjustment Scale Self‐Report; ix) health‐related quality of life, as measured by the EQ‐5D‐5L and the SF‐36; x) alcohol use, as measured by the AUDIT; xi) drug use, as measured by the Drug Abuse Screening Test; xii) NSSI, as measured by the Inventory of Statements About Self‐Injury; xiii) suicidal ideation, as measured by the BSSI; xiv) post‐traumatic symptoms, as measured by the PTSD Checklist for DSM‐5; xv) emotion regulation, as measured by the DERS; xvi) mindfulness, as measured by the Kentucky Inventory of Mindfulness; xvii) coping during stressful situations, as measured by the Dialectical Behavior Therapy‐Ways of Coping Checklist Tertiary outcome(s): i) personality, as measured by the NEO‐Five Factor Inventory; ii) experiences of trauma, as measured by the Childhood Trauma Questionnaire‐Short Form and the Credibility/Expectancy Questionnaire; iii) therapeutic alliance, as measured by the Working Alliance Inventory‐Short Form (therapist and client versions); iv) reasons for treatment discontinuation, as measured by the Reasons for Early Termination from Treatment Questionnaire |
| Starting date | 1 February 2015 |
| Contact information |
Principal investigator: Dr. Shelley McMain, Centre for Addiction and Mental Health, Department of Psychiatry, University of Toronto, Toronto, Canada (shelley.mcmain@camh.ca) |
| Notes |
NCT02060448.
| Study name | Exploring two emotion‐focused treatment modules in non‐suicidal self‐injury |
| Methods | Single‐case experimental design. Participants are randomly allocated to receive either mindful emotion awareness training or cognitive reappraisal and then, depending on improvement, are permitted to cross over to receive the alternate module. Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged 18 years and older; ii) current NSSI; iii) meets DSM‐5 criteria for NSSI; iv) either not taking psychotropic medications, or taking stable doses likely to be maintained throughout the duration of the trial Exclusion criteria: i) current suicidal ideation with a plan; ii) currently receiving CBT or any other psychotherapy to reduce NSSI, anxiety, depression, or other Axis I disorder; iii) unwilling to refrain from initiating additional treatment throughout the duration of the trial; iv) current or recent (within three months) history of a substance use disorder; v) experiencing emotional symptoms due to a medical/physical condition |
| Interventions |
Intervention (mindful emotion awareness training): consisting of four 50‐minute weekly sessions of mindful emotion awareness training Intervention (cognitive reappraisal): consisting of four 50‐minute weekly sessions of cognitive reappraisal |
| Outcomes |
Primary outcome(s): i) frequency of urges and acts of NSSI, as ascertained from self‐report Secondary outcome(s): i) anxiety, as measured by the OASIS and BAI; ii) depression as measured by the ODSIS and BDI; iii) emotion regulation, as measured by the Deficits in Emotion Regulation Scale (DERS) and the Emotion Regulation Questionnaire (ERQ); iv) mindfulness, as measured by the Southampton Mindfulness Questionnaire (SMQ); v) experiential avoidance, as measured by the Multi‐dimensional Experiential Avoidance Questionnaire (MEAQ); vi) sleep problems, as measured by the Insomnia Severity Index (ISI); vii) subjective symptomatology, as measured by the Subjective Symptoms Scale (SSS) Tertiary outcome(s): i) self‐injury implicit associations, as measured by the Self‐Injury Implicit Association Test (SI‐IAT) |
| Starting date | 1 November, 2013 End date: 31 December, 2015 |
| Contact information |
Principal investigators: Prof. David Barlow, Boston University, Boston, MA, USA (dhbarlow@bu.edu) Assistant Prof. Kate Bentley, Harvard Medical School, Harvard University, Cambridge, MA, USA (KBENTLEY@mgh.harvard.edu) |
| Notes | We are grateful to Assistant Prof. Kate Bentley for confirming the above details were correct, 21 October, 2020. |
NCT02354183.
| Study name | Commitment and motivation in a brief DBT intervention for self harm |
| Methods | Single‐blind RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged between 18 and 80 years; ii) ≥ 3 episodes of SH in the five year preceding trial entry, including ≥ 1 in the preceding eight weeks; iii) received no more than four weeks of DBT in the one year preceding trial entry; iv) self‐reports no knowledge of core DBT skills; v) has a valid Canadian healthcare card; vi) sufficient language ability Exclusion criteria: i) diagnosed with an organic brain disorder and/or intellectual disability |
| Interventions |
Intervention: DBT. Single one‐hour session of DBT core skills, including wise mind, distraction, mindfulness of the current emotion, and opposite to emotion action skills, in addition to psychoeducation Comparator: Psychoeducation. Single one‐hour session of psychoeducation |
| Outcomes |
Primary outcome(s): i) motivation, as measured by the Autonomous and Controlled Motivation for Treatment Questionnaire Secondary outcome(s): i) frequency of SH, as measured by the DSHI; ii) severity of SH, as measured by the DSHI |
| Starting date | 1 April, 2015 |
| Contact information |
Principal investigator: Dr Michelle Leybman, McGill University, Montreal, Quebec, Canada (Michelle.leybman@mail.mcgill.ca) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT03081078.
| Study name | Effects of community‐based caring contact on post‐discharge young adults with self‐harm ‐ a multi‐center randomized controlled trial |
| Methods | Open‐label RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged between 18 and 45 years; ii) ≥ 1 episode of SH, ascertained from ICD‐10 assigned codes, leading to admission to the ED; iii) received mental health assessment by a psychiatrist or consultation liaison nurse; iv) able to provide written informed consent Exclusion criteria: i) diagnosis of any DSM‐IV‐TR axis II personality disorder; iii) diagnosed with psychosis or bipolar disorder |
| Interventions |
Intervention 1: Mobile (cell) telephone app with remote contact intervention in addition to TAU. Participants receive access to the app (no further details on content or therapeutic focus provided) and remote contact (≥ 2 telephone contacts and/or text messages) by volunteers over a two‐month period in addition to TAU. Intervention 2: Mobile (cell) telephone app in addition to TAU. Participants receive access to the app (no further details on content or therapeutic focus provided) in addition to TAU. Control: TAU |
| Outcomes |
Primary outcome(s): i) suicidal ideation, as measured by the Chinese language translation of the ASIQ; ii) hopelessness, as measured by the Chinese language translation of the BHS‐4; iii) thwarted belongingness, as measured by the Thwarted Belongingness subscale of the Interpersonal Needs Questionnaire (INQ‐15); iv) perceived burdensomeness as measured by the Perceived Burdensomeness subscale of the INQ‐15; v) service use, as measured by the self‐reported compliance with any prescribed treatment(s); vi) SH, as measured by a four‐item scale for levels of suicidality developed by the authors Secondary outcome(s): i) depression, as measured by the Center for Epidemiologic Studies Depression Scale (CES‐D); ii) frequency of SH, according to self‐report and medical records; iii) suicide, as verified by records retrieved from the Hong Kong Special Administrative Region (HKSAR) Coroner's Court; iv) time spent engaging with the mobile app, as measured by time‐stamp logs; v) time spent engaging with remote contacts, as measured by time‐stamp logs and volunteer service records |
| Starting date | 1 June 2017 |
| Contact information |
Principal investigator: Associate Prof. Yik‐Wa Law, The Univesrity of Hong Kong, Hong Kong (flawhk@hku.hk) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT03185026.
| Study name | Effectiveness of the first French psychoeducational program for suicidal behavior: a randomized controlled trial |
| Methods | Single‐blind RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged between 18 and 65 years; ii) diagnosed with suicidal behaviour disorder (DSM‐5) (i.e. ≥ 1 suicide attempt in 12 months preceding trial entry); iii) sufficient language ability; iv) able to provide written informed consent; iv) belongs to a social safety system Exclusion criteria: i) current or past diagnosis of an organic mental disorder; ii) lifetime history of schizophrenia; iii) diagnosed with an intellectual disability; iv) unable to comply with the study visit procedures |
| Interventions |
Intervention: relaxation training consisting of 10 weekly sessions (two hours' duration) of a standardised relaxation programme Comparator: psychoeducation consisting of 10 weekly sessions (two hours' duration) of a psychoeducation programme focused on providing education on suicidal behaviour, identification of patterns, and self‐assessment of suicidal ideation, and presentation of a stress‐diathesis model of suicidal behaviour |
| Outcomes |
Primary outcome(s): i) SH, as measured by the C‐SSRS Secondary outcomes(s): i) suicide attempt (both interrupted and aborted) rate reduction, as measured by the C‐SSRS; ii) suicidal ideation, as measured by the C‐SSRS; iii) intensity of suicidal ideation, as measured by the C‐SSRS; iv) treatment adherence, as measured by the Medication Adherence Rating Scale; v) service use, as measured by an idiosyncratic scale; vi) depression, as measured by the Inventory of Depressive Symptomatology; vii) anxiety, as measured using the State‐Trait Anxiety Inventory; viii) psychological pain, as measured by an idiosyncratic scale; ix) hopelessness, as measured by the BHS; x) general functioning, as measured by the Functioning Assessment Short Test; xi) quality of life, as measured by the World Health Organization Quality Of Life measure (WHOQOL‐BREF); xii) social support, as measured by an idiosyncratic scale; xiii) emergency service use; xiv) acceptance, as measured by the Acceptance and Action questionnaire; xv) mindfulness, as measured by the Mindful Attention Awareness Scale; xvi) meaning in life, as measured by the Life Regard Index; xvii) treatment adherence, as measured by the number of sessions attended |
| Starting date | 6 September, 2017 |
| Contact information |
Principal investigator: Dr. Deborah Ducasse, University Hospital, Montpellier, France (d-ducasse@chu-montpellier.fr) |
| Notes | We are grateful to Dr. Deborah Ducasse for confirming the above details were correct, 28 October, 2020. |
NCT03427190.
| Study name | Suicide prevention algorithm in the French Overseas Territories (APSOM) |
| Methods | Open‐label, RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged 16 years and older; ii) discharged from hospital within 15 days of an index suicide attempt; iii) has healthcare insurance; iv) able to be contacted via telephone and mail; v) resident of one of the French overseas territories participating in the trial (i.e. Guadeloupe, French Guyana, Martinique, or Reunion Island); vi) sufficient language ability; vii) willing and able to provide oral informed consent Exclusion criteria: i) homeless; ii) disabled, under judicial/court protection, and/or legally incompetent; iii) unable to understand the study protocol |
| Interventions |
Intervention: remote contact intervention (telephone contact and/or postcards), in addition to GP management. Participants will receive telephone contact within 21 days' post‐discharge. If participants are unable to be contacted via telephone, postcards will be sent at months' 2, 3, 4, and 5 post‐discharge. Participants will also be contacted by their GP within 21 days' post‐discharge to organise a consultation within 21 to 45 days' post‐discharge. Two additional GP contacts will be made at months 6 and 13 post‐discharge. Comparator: remote contact intervention (telephone contact and/or postcards) consisting of telephone contact within 21 days' post‐discharge. If participants are unable to be contacted via telephone, postcards will be sent at months' 2, 3, 4, and 5 post‐discharge. |
| Outcomes |
Primary outcome(s): i) repetition of SH (unclear how ascertained); ii) suicide (unclear how ascertained) Secondary outcome(s): i) frequency of SH repetition (unclear how ascertained); ii) anxiety and depression as measured by the HADS; iii) suicide risk as measured by the C‐SSRS |
| Starting date | 9 February, 2018 |
| Contact information |
Principal investigator: Dr. Louis Jehel, University Hospital Martinique, Fort‐de‐France, Martinique (louis.jehel@chu-martinique.fr) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT03463980.
| Study name | Compassion meditation and ReliefLink app for suicidal, low‐income, African‐Americans |
| Methods | Open‐label, RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged between 18 and 64 years; ii) self‐identifies as black or African‐American; iii) presents to the medical or psychiatric department of a general hospital following a suicide attempt; iv) at least moderate suicidal intent, as defined by a BSSI score of ≥ 8; v) Mini Mental Status Examination (MMSE) score ≥ 22 Exclusion criteria: i) significant cognitive impairment, as defined by a MMSE score < 22; ii) psychosis symptoms; iii) diagnosed with an imminently life‐threatening medical condition |
| Interventions |
Intervention: compassion meditation consisting of six weekly sessions (120 minutes' duration) of compassion meditation. Participants will also be encouraged to meditate at least 30 minutes a day and will be asked to track their daily meditation time. Comparator: supportive group therapy consisting of six weekly sessions (90 minutes' duration) of supportive group therapy |
| Outcomes |
Primary outcome(s): i) suicidal ideation, as measured by the BSSI Secondary outcome(s): i) depression, as measured by the BDI; ii) shame, as measured by the Experience of Shame Scale (ESS); iii) self‐criticism, as measured by the Self‐Criticism Scale; iv) interpersonal connectedness, as measured by the Social Support Behaviors Scale (SSB); v) self‐compassion, as measured by the Self‐Compassion Scale (SCS); vi) mindfulness, as measured by the Five Facet Mindfulness Questionnaire (FFMQ); vii) behavioural monitoring, as measured by the Behavior Monitoring Form (BMF) |
| Starting date | 13 May, 2010 |
| Contact information |
Principal investigator: Prof. Nadine Kaslow, Emory University, Atlanta, GA, USA (nkaslow@emory.edu) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT03541824.
| Study name | Reducing suicide risk associated with weight loss |
| Methods | Single‐blind RCT Allocation: cross‐over, individual‐level |
| Participants |
Inclusion criteria: i) aged between 18 and 65 years; ii) males and females; iii) ≥ 1 episode of NSSI within the one month prior to trial entry; iv) > 5 pounds weight suppression Exclusion criteria: i) indicating being "sure" of suicide attempt on a trial‐specific screening questionnaire; ii) lives outside of the USA; iii) pregnant |
| Interventions |
Intervention: Body Acceptance Program (BAP), an internet‐based intervention designed to challenge the appearance‐ideal Comparator: waiting‐list control |
| Outcomes |
Primary outcome(s): i) frequency of SH, as measured by the Self‐Injurious Thoughts and Behaviors Interview‐Short Form Secondary outcome(s): i) body self‐esteem, as measured by the appearance subscale of the Body Esteem Scale; iii) body weight esteem, as measured by the weight subscale of the Body Esteem Scale; iv) body attribution, as measured by the attribution subscale of the Body Esteem Scale; v) body shape, as measured by the Body Shape Questionnaire‐8; vi) depression, as measured by the BDI; vii) positive and negative affect, as measured by the Positive and Negative Affect Schedule |
| Starting date | 1 July 2016 |
| Contact information |
Principal investigator: Prof. Pamela Keel, Florida State University, Tallahassee, FL, USA (keel@psy.fsu.edu ) |
| Notes | We are grateful to Prof. Pamela Keel for confirming the above details were correct, 29 October, 2020. |
NCT03732300.
| Study name | Evaluation of ASSIP ‐ Attempted Suicide Short Intervention Program: a randomized controlled trial |
| Methods | Single‐blind RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged 18 years and older; ii) suicide attempt in the six months preceding trial entry; iii) able and willing to provide written informed consent; iv) received treatment in an in/outpatient psychiatric facility; v) able and willing to comply with the trial procedures Exclusion criteria: i) acute psychosis; ii) insufficient language ability; iii) diagnosed with dementia; iv) engaging in chronic SH without suicidal intent; v) receiving current ECT; vi) previously enrolled in the trial; vii) study investigators, their family members and other dependants, and employees are also excluded from participation |
| Interventions |
Intervention: Attempted Suicide Short Intervention Program (ASSIP) in addition to TAU. Three sessions (duration not reported) of ASSIP, in addition to up to 12 remote contact interventions (letters) Comparator: TAU |
| Outcomes | Primary outcome(s): i) suicide deaths (unclear how ascertained); ii) repetition of SH (unclear how ascertained); iii) duration of hospital admissions (days) ascertained from records; iv) costs of hospital admissions ascertained from records; v) electrophysiological wakefulness regulation, as measured by a standardised algorithm; vi) electrophysiological heart rate variability, as measured by a standardised algorithm |
| Starting date | 1 December 2018 |
| Contact information |
Principal investigator: Prof. Sebastian Olbrich, University of Zurich, Zurich, Switzerland (sebastian.olbrich@puk.zh.ch) |
| Notes | We are grateful to Prof. Sebastian Olbrich for confirming the above details were correct, 8 October, 2020. |
NCT03853382.
| Study name | Cognitive Analytic Therapy‐informed Containment for self‐Harm (CATCH) |
| Methods | RCT (feasibility) Assignment: parallel‐group, individual‐level |
| Participants | Inclusion criteria: i) aged 16 years and older; ii) access to email and Internet (necessary for completing study measures); iii) currently in receipt of clinical support from National Health Service (NHS) or private health services; iv) ≥ 5 or more episodes of NSSI in the year preceding trial entry; v) able to provide written informed consent in English; vi) capable of providing written informed consent Exclusion criteria: i) currently receiving any form of psychological therapy; ii) received any form of psychological therapy in the month preceding trial entry; iii) previously received Cognitive Analytic Therapy; iv) diagnosed with a learning disability and/or autistic spectrum disorder; v) currently at high risk of suicidal behaviour; vi) hospitalised for SH in the one month preceding trial entry |
| Interventions | Intervention: brief Cognitive Analytic Therapy‐informed Containment for self‐Harm (CATCH) consisting of two sessions, each lasting approximately 90 minutes Comparator: TAU. No further details provided |
| Outcomes |
Primary outcome(s): i) acceptability, as measured by the proportion of participants who complete both sessions and from qualitative interviews with participants; ii) safety, as measured by the Adverse Effects in Psychotherapy; iii) feasibility, as measured by the proportion of participants attending a post‐therapy follow‐up assessment Secondary outcome(s): i) NSSI, as measured by the Self‐Injurious Thoughts and Behaviors Inventory Short‐Form; ii) self‐compassion, as measured by the Self‐Compassion Scale; iii) depression, as measured by the PHQ‐9; iv) self‐injury urges, as measured by the Alexian Brothers Urges to Self‐Injury Scale. Assessments for secondary outcomes were not completed at comparable time points for the two arms. |
| Starting date | 1 April, 2019 |
| Contact information |
Prinicpal investigator: Dr Peter Taylor, University of Manchester, Manchester, UK (peter.taylor-2@manchester.ac.uk) |
| Notes | We are grateful to Dr. Peter Taylor for confirming the above details were correct, 9 October, 2020. |
NCT03894462.
| Study name | Effectiveness of a targeted brief intervention for recent suicide attempt survivors |
| Methods | Single‐blind RCT Assignment: parallel‐group, individual‐level (N = 400) |
| Participants |
Inclusion criteria: i) aged 18 years and older; ii) attempted suicide in the 60 days preceding trial entry; iii) able and willing to provide written informed consent; iv) have at least one contact person who can promote participant’s safety and who can be contacted in the event of missed follow‐up appointments Exclusion criteria: i) acute psychosis; ii) insufficient language ability |
| Interventions |
Intervention: Attempted Suicide Short Intervention Program (ASSIP) in addition to TAU. Three outpatient sessions (approximately one hours' duration each) of ASSIP. All three ASSIP sessions will be completed within six weeks. Participants have the choice to receive the intervention in person or via telehealth. Comparator: TAU from providers that have adopted the Zero Suicide model, incorporating enhanced clinical care protocols, improved clinical coding for suicidal behaviour, and the adoption of common protocols |
| Outcomes | Primary outcome(s): i) time to SH, as ascertained from the C‐SSRS and electronic medical records |
| Starting date | 1 October 2020 |
| Contact information |
Principal investigator: A/Prof. Anthony R. Pisani, PhD, University of Rochester Medical Center, Rochester, NY, USA (anthony_pisani@urmc.rochester.edu) |
| Notes | We are grateful to Caroline Kelberman for confirming the above details were correct, 8 October, 2020. |
NCT04072666.
| Study name | Investigations of psychological interventions in suicide prevention: a comparison of brief cognitive behavioural therapy and the attempted suicide short intervention program |
| Methods | Double‐blind RCT Assignment: parallel=group, block randomisation, individual‐level |
| Participants |
Inclusion criteria: i) aged 16 years and older; ii) presenting to a general hospital following a recent (duration not reported) suicide attempt; iii) referred to the Suicide Prevention Pathway Exclusion criteria: i) unable or unwilling to provide consent; ii) receiving any other psychosocial intervention. Those taking stable doses of any psychotropic medications will not be excluded. |
| Interventions |
Intervention 1: Attempted Suicide Short Intervention Program (ASSIP) plus Suicide Prevention Pathway (SPP) consisting of three sessions (60 minutes' duration each) manualised ASSIP along with a remote contact intervention over a 24‐month period plus SPP Intervention 2: CBT plus SPP. Five sessions (60 minutes' duration each) of manualised individual‐level CBT plus SPP Comparator: SPP. Seven sessions (duration not reported) of a blended face‐to‐face and online programme incorporating a psychosocial assessment, formulation of suicide risk, collaborative safety planning, counselling on access to lethal means, development of a transition care plan, and a remote contact intervention (letters and/or text messages) for a 24‐month period |
| Outcomes |
Primary outcome(s): i) SH, as ascertained from representations to hospital; ii) suicide, as ascertained from official records Secondary outcome(s): i) coping, as measured by the Coping Inventory for Stressful Situations (CISS); ii) resilience, as measured by the Resilience Scale for Adults (RSA) or the Resilience Scale for Adolescents (READ) (as appropriate for age); iii) therapeutic alliance, as measured by the revised Helping Alliance Questionnaire – II; iv) interpersonal problem‐solving, as measured by the Independent‐Interdependent Problem Solving Scale (IIPSS) |
| Starting date | 1 October 2019 |
| Contact information |
Principal investigator: Prof. Chris Stapelberg, Bond University, Gold Coast, Queensland, Australia (chris.stapelberg@health.qld.gov.au) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT04168645.
| Study name | Inpatient cognitive‐behavioral therapy to reduce suicide risk post‐discharge |
| Methods | Single‐blind RCT Assignment: parallel=group, stratified block randomisation, individual‐level |
| Participants |
Inclusion criteria: i) aged between 18 and 65 years; ii) at least one suicide attempt in the week preceding trial entry; iii) admitted to either a medical or psychiatric inpatient ward Exclusion criteria: i) diagnosed with a schizophrenia spectrum disorder; ii) diagnosed with an organic brain disorder and/or intellectual disability; iii) acute mania; iv) diagnosed with any other psychiatric and/or medical condition that would preclude the participant being able to provide informed consent; v) referred for ECT |
| Interventions |
Intervention: CBT. Up to four sessions of CBT (between 1 to 1.5 hours' duration) Comparator: TAU |
| Outcomes | Primary outcome(s): i) SH, as measured by the C‐SSRS; ii) suicidal ideation, as measured by the C‐SSRS; iii) number of readmissions, as ascertained from electronic medical records |
| Starting date | 15 October 2019 |
| Contact information |
Principal investigator: Prof. David Tolin, Yale University, New Haven, CT, USA (David.Tolin@hhchealth.org) |
| Notes | We are grateful to Prof. David Tolin for confirming the above details were correct, 7 October, 2020. |
NCT04191122.
| Study name | Community Outpatient Psychotherapy Engagement Service for Self‐harm (COPESS): a feasibility study |
| Methods | Double‐blind RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged 16 years and older; ii) ≥ 1 episode of SH in the six months preceding trial entry; iii) presented to GPs Exclusion criteria: i) diagnosed with an intellectual disability; ii) alcohol and/or drug dependant; iii) severe suicidal ideation; iv) currently experiencing symptoms of psychosis or treatment‐resistant depression; iv) unwilling or unable to provide written informed consent; v) insufficient language ability |
| Interventions |
Intervention: Psychodynamic psychotherapy consisting of five sessions (50 minutes' duration each) of psychotherapy based on a psychodynamic and cognitive analytic approach in addition to TAU Comparator: TAU based on NICE 2011 principles |
| Outcomes |
Primary outcome(s): i) treatment acceptability, as measured by the proportion of participants completing treatment; ii) adverse events, as measured by the AEP; iii) feasibility, as measured by the number of assessments completed by participants Secondary outcome(s): i) depression, as measured by the BDI; ii) frequency of NSSI, as measured by the Self‐Injurious Thoughts and Behaviors Interview (SITBI); iii) severity of NSSI, as measured by the SITBI; iv) intensity of SH urges, as measured by the SITBI; v) emotion regulation, as measured by the Emotion Regulation Questionnaire (ERQ); vi) clinical outcomes, as measured by the Clinical Outcomes in Routine Evaluation (CORE‐10); vii) help‐seeking attitudes, as measured by the General Help‐Seeking Questionnaire (GHSQ) and the Actual Help Seeking Questionnaire (AHSQ); viii) therapeutic alliance, as measured by the Helping Relationship Questionnaire (HRQ) |
| Starting date | 2 May 2020 |
| Contact information |
Principal investigator: Dr Pooja Saini, Liverpool John Moores University, Liverpool, UK (poojasaini@hotmail.co.uk) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT04244786.
| Study name | Treating self injurious behavior: a novel brain stimulation approach |
| Methods | Quadruple‐blind RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged between 18 and 60 years; ii) engages in frequent NSSI (defined as ≥ 2 episodes of NSSI in the two months prior to trial entry); iii) able to provide informed consent; iv) if diagnosed with bipolar I or II disorder, taking a stable therapeutic dose of a mood stabiliser Exclusion criteria: i) diagnosed with an unstable medical condition; ii) diagnosed with psychosis, mania, hypomania, or an intellectual disability; iii) current suicidal ideation with a plan that cannot be managed safely in an outpatient setting; iv) pregnant, lactating, or planning to conceive during the trial duration; v) diagnosed with a neurological disease or prior head trauma with evidence of cognitive impairment (defined as scoring ≥ 1.5 standard deviations below the mean on the Trailmaking A&B Test); vi) current moderate to severe alcohol or substance use disorder; v) those whose dose of any current psychiatric medications (including antidepressants, anxiolytics, antipsychotic medications, mood stabilisers, and benzodiazepines) was increased within two weeks prior to trial entry; vi) received any form of psychotherapy within two weeks prior to trial entry; vii) any metal implants or paramagnetic objects contained within the body (including heart pacemaker, shrapnel, or surgical prostheses) which may present a risk to the participant and/or interfere with the MRI scan; viii) claustrophobia significant enough to interfere with MRI scanning; ix) weight that exceeds 325 pounds or inability to fit into MRI scanner |
| Interventions |
Intervention: Transcranial magnetic stimulation. Six 20‐minute sessions of transcranial direct current stimulation (1.5 milliamp) delivered to the right ventrolateral prefrontal cortex Comparator: Sham. Six 20‐minute sessions where an electrode montage is applied to the right ventrolateral prefrontal cortex |
| Outcomes |
Primary outcome(s): i) adverse effects, as measured by the Transcranial Direct Current Stimulation Adverse Effects Questionnaire; ii) social processing, as measured by changes in brain responses whilst undertaking a social processing task during an fMRI scan; iii) NSSI urges and behaviours, as measured by ecological momentary assessment (EMA) Secondary outcome(s): i) mood state, as measured by a task during an fMRI scan and EMA |
| Starting date | 1 October 2019 |
| Contact information |
Principal investigator: Dr Jeffrey M. Miller, New York State Psychiatric Institute and Columbia University, NYC, NY, USA Public contact: Young Cho, New York State Psychiatric Institute and Columbia University, NYC, NY, USA (mailto:young.cho%40nyspi.columbia.edu?subject=NCT04244786,%20#7170, Treating Self Injurious Behavior: A Novel Brain Stimulation Approach) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT04284085.
| Study name | Evaluation of a psychoeducational intervention for people with suicidal behaviour in the penitentiary environment: N'VIU project |
| Methods | Single‐blind RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged 18 years and older; ii) history of attempted suicide (unclear the time frame over which this will be assessed) Exclusion criteria: i) diagnosis of any psychiatric disorder in an acute phase; ii) intellectual disability; iii) cognitive impairment |
| Interventions |
Intervention: psychoeducation consisting of 13 sessions (90 minutes' each), of a group‐based psychoeducation programme Comparator: fact‐sheet on the risks of suicide, along with tips for reducing suicidal ideation |
| Outcomes |
Primary outcome(s): i) frequency of SH (unclear how ascertained) Secondary outcome(s): i) suicidal ideation, as measured by the C‐SSRS; ii) anxiety, as measured by the HARS; iii) depression, as measured by the HDRS; iv) quality of life, as measured by the EuroQoL‐5D Health Questionnaire |
| Starting date | 15 October 2019 |
| Contact information |
Principal investigator: Dr. Pere Roura‐Poch, Consorci Hospitalari de Vic, Barcelona, Spain (tac.vhc@aruorp) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT04343703.
| Study name | Suicide prevention and intervention (SURVIVE): cohort study and nested randomized controlled trials of secondary prevention programs for suicide attempts |
| Methods | Single‐blind RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged 12 years and older; ii) presented to an ED following a suicide attempt; iii) willing and able to provide written informed consent, and able to comply with the trial procedures Exclusion criteria: i) unable to provide written informed consent; ii) insufficient language ability; iii) currently participating in another clinical trial of psychosocial therapy for SH |
| Interventions |
Intervention 1: telephone management consisting of three telephone consultations (between 5‐45 minutes' duration each). Therapeutic content includes: 1) assessment; 2) crisis management. Intervention 2: internet‐based CBT. Participants will receive access to an internet‐based CBT programme consisting of seven modules. Whilst the intervention can be self‐paced, each module should be worked through over a week‐long period. Therapeutic content includes: i) behavioural activation; ii) cognitive restructuring; iii) sleep regulation; iv) mood monitoring; v) establishing healthy lifestyle habits. Comparator: TAU, consisting of any nonspecific intervention to address suicidal behavior or to prevent suicide |
| Outcomes |
Primary outcome(s): i) SH (unclear how ascertained); ii) suicide (unclear how ascertained) Secondary outcomes(s): i) general symptoms, as measured by the BSI; ii) depression, as measured by the PHQ‐9; iii) anxiety, as measured by the GAD‐7; iv) quality of life, as measured by the EQ‐5D; v) impulsivity, as measured by the BIS; vi) acquired capability, as measured by the Acquired Capability for Suicide Scale‐Fearlessness about Death (ACSS‐FAD); vii) mentalising skills, as measured by the Reflective Functioning Questionnaire‐8; viii) suicidal ideation, as measured by the C‐SSRS; ix) strengths and difficulties, as measured by the SDQ |
| Starting date | 17 June 2020 |
| Contact information |
Principal investigator: Dr. Victor Pérez, Parc de Salut Mar, Barcelona, Spain (vperezsola@parcdesalutmar.cat) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT04366466.
| Study name | Program to promote Engagement in care for the Prevention of Suicidal recidivism (PEPS) |
| Methods | Open‐label RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged 18 years and older; ii) admitted to a general hospital following a suicide attempt; iii) referred for outpatient follow‐up; iv) able and willing to provide written informed consent Exclusion criteria: i) not in receipt of social security and/or state medical care; ii) diagnosed with cognitive or delusional disorders; iii) hospitalised for > 72 hours following the index suicide attempt; iv) currently under psychiatric care; v) unable to be reached by telephone (e.g. without a telephone, homeless, or incarcerated); vi) insufficient language ability |
| Interventions |
Intervention: consisting of a series of telephone contacts (both the number and duration not reported) delivered over a 12‐month period. Therapeutic content not reported Comparator: TAU |
| Outcomes | Primary outcome(s): i) repetition of SH (unclear how ascertained); ii) feasibility, as measured by the percentage of participants fulfilling the inclusion and exclusion criteria and the proportion of participants who received the treatment in full |
| Starting date | 29 April, 2020 |
| Contact information |
Principal investigator: Dr Fayçal Mouaffak, Centre Hospitalier de Ville‐Evrard, Paris, France (mouaffakf@yahoo.fr) |
| Notes | We were unable to confirm the above details were correct despite correspondence. |
NCT04420546.
| Study name | Using implementation intentions to reduce self‐harm |
| Methods | Double‐blind, RCT Assignment: parallel‐group, individual‐level |
| Participants |
Inclusion criteria: i) aged 18 years and older; ii) have a history of SH (lifetime); iii) sufficient language ability Exclusion criteria: i) not currently residing in an inpatient psychiatric facility |
| Interventions |
Intervention: electronic volitional help sheet. Participants read a brief statement designed to encourage them to avoid self‐harming by forming implementation intentions by linking critical situations with appropriate alternative responses for each critical situation. Comparator: analogue volitional help sheet |
| Outcomes |
Primary outcome(s): i) NSSI, as ascertained from self‐report; ii) suicidal ideation, as ascertained from self‐report; iii) suicide attempts, as ascertained from self‐report Secondary outcome(s): i) exposure to suicide and mental imagery about death, as measured by a seven‐point scale adapted from Dhingra 2015; ii) capability, opportunity, and motivation, as measured by the Capability, Opportunity, Motivation Questionnaire; iii) habit, as measured by a self‐reported scale; iv) self‐regulation, as measured by items adapted from Sniehotta 2005; v) frequency with which critical situations were encountered and appropriate responses were used |
| Starting date | 1 June, 2020 |
| Contact information |
Principal investigator: Dr. Chris Keyworth, University of Manchester, Manchester, UK (chris.keyworth@manchester.ac.uk) |
| Notes | We are grateful to Dr. Chris Keyworth for confirming the above details were correct, 9 October, 2020. |
O'Connor 2019.
| Study name | SAFETEL randomised controlled feasibility trial of a safety planning intervention with follow‐up telephone contact to reduce suicidal behaviour: study protocol |
| Methods | Open‐label, RCT Assignment: 2:1 allocation, individual‐level |
| Participants |
Included: i) aged 18 years and older; ii) admitted to hospital following a suicide attempt; iii) assessed by the Liaison Psychiatry team; iv) sufficient language ability Excluded: i) no suicidal intent; ii) medically unfit for interview; iii) unable to provide informed consent; iv) insufficient language ability; v) participating in another psychological intervention study within the trial hospital; vi) no access to a telephone |
| Interventions |
Intervention: SAFETEL consisting of collaborative safety planning and five structured telephone calls (around 15 minutes' duration each) over a period of four weeks. Therapeutic content involves: i) safety planning; ii) suicide risk assessment; iii) mood monitoring; iv) reviewing and revising the safety plan (as needed); v) treatment engagement enhancement; vi) motivational enhancement; vii) problem‐solving. Comparator: TAU consisting of referral to any one of the following services as needed (e.g. primary care, community psychiatric service, third sector services, specialist mental health services, intensive home treatment, outpatient services, transfer to inpatient care, social work, or no further treatment) |
| Outcomes | Primary outcome(s): i) repetition of SH, as measured by the C‐SSRS and medical records; ii) feelings of entrapment, as measured by the Entrapment Scale; iii) interpersonal functioning, as measured by the Interpersonal Needs Questionnaire; iv) social functioning, as measured by the ENRICHD Social Support Instrument; v) coping skills, as measured by the Suicide‐Related Coping Scale |
| Starting date | 5 May, 2017 |
| Contact information |
Principal investigator: Prof. Rory O'Connor, University of Glasgow, Glasgow, UK (Rory.OConnor@glasgow.ac.uk) |
| Notes |
SLCTR/2017/008.
| Study name | A pilot randomised controlled trial to evaluate the acceptability and feasibility of a counselling intervention, delivered by nurses, for those who have attempted self‐poisoning in Sri Lanka |
| Methods | Open‐label RCT Assignment: parallel‐group, blocked, individual‐level |
| Participants |
Inclusion criteria: i) aged 16 years and older; ii) admitted to hospital for medical management following an episode of self‐poisoning Exclusion criteria: i) diagnosed with schizophrenia, any psychosis, bipolar disorder, dementia, intellectual disability, or cognitive impairment; ii) physically too unwell to comply with the study procedures |
| Interventions |
Intervention: brief Culturally‐adapted Manually Assisted Problem‐solving training (C‐MAP) consisting of one session (20‐30 minutes' duration) of an adapted form of C‐MAP Comparator: TAU |
| Outcomes |
Primary outcome(s): i) coping skills, as measured by the Brief‐COPE inventory; ii) alcohol use, as measured by the Alcohol Use Disorders Identification Test (AUDIT); iii) depression, as measured by the Patient Health Questionnaire 9 (PHQ‐9) and the Peradeniya Depression Scale; iv) anxiety, as measured by the Generalised Anxiety Disorder 7‐item scale (GAD‐7); v) suicidal intent, as measured by the Pierce Suicide Intent Scale (PSIS) Secondary outcome(s): acceptability, feasibility, and utility, as ascertained from qualitative interviews with participants |
| Starting date | 27 March, 2017 |
| Contact information |
Principal investigator: Dr. Thillini Rajapakse, University of Peradeniya, Sri Lanka (gemba471@gmail.com) |
| Notes | We are grateful to Dr. Thillini Rajapakse for confirming the above details were correct, 29 October, 2020. |
Stevens 2019.
| Study name | SMS SOS: using SMS text messages to prevent SH |
| Methods | Open‐label Zelen RCT Assignment: parallel‐group, individual‐level, blocked randomisation stratified by multiple SH status |
| Participants |
Inclusion criteria: i) aged 16 years of age or older; ii) assessed in participating EDs following an episode of SH; iii) sufficient language ability; iv) owns a mobile (cell) telephone Exclusion criteria: i) no fixed address; ii) do not own a mobile (cell) telephone; iii) unable or unwilling to provide informed consent |
| Interventions |
Intervention: series of nine SMS text messages delivered via mobile (cell) telephone at 1, 2, 3, 4, 5, 6, 8, 10, and 12 months' post‐discharge. Messages are designed to express concern for participants' well‐being and to encourage them to make contact with local crisis services, if needed. Participants will also receive TAU. Comparator: TAU consisting of in‐ or outpatient mental health treatment, referral to other services (e.g. AOD services), and/or GP management (as appropriate) |
| Outcomes |
Primary outcome(s): i) frequency of SH as ascertained from hospital records; ii) time to SH repetition as ascertained from hospital records Secondary outcome(s): i) repetition of SH as ascertained from hospital records; ii) suicide as ascertained from mortality registers; iii) all‐cause mortality as ascertained from mortality registers |
| Starting date | 8 May, 2017 |
| Contact information |
Principal investigator: Dr. Garry Stevens, Western Sydney University, Sydney, New South Wales, Australia (g.stevens@westernsydney.edu.au) |
| Notes |
ACSS‐FAD: Acquired Capability for Suicide Scale‐Fearlessness about Death AEP: AHSQ: Actual Help Seeking Questionnaire AOD: alcohol and other drug app: application APSOM: ASIQ: Adult Suicidal Ideation Questionnaire ASSIP: Attempted Suicide Short Intervention Program AUDIT: Alcohol Use Disorders Identification Test BAI: Beck Anxiety Inventory BAP: BDI: Beck Depression Inventory BHQ: Beck Hopelessness Scale BHS(‐4): BIS: Barratt Impulsiveness Scale BMF: Behavior Monitoring Form BPD: Brief‐COPE: BSI: Brief Symptom Inventory BSSI: CATCH: CBT: cognitive behavioural therapy CES‐D: Center for Epidemiologic Studies Depression Scale CISS: Coping Inventory for Stressful Situations COPESS: CORE‐10: Clinical Outcomes in Routine Evaluation‐10 C‐MAP: Culturally‐adapted Manually Assisted Problem‐solving training C‐SSRS: Columbia‐Suicide Severity Rating Scale DBT: Dialectical Behaviour Therapy DERS: Difficulties in Emotion Regulation Scale DSH: deliberate self‐harm DSHI: Deliberate Self‐Harm Interview DSM‐IV‐TR: Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision DSM‐5: Diagnostic and Statistical Manual of Mental Disorders, 5th Edition ECT: electroconvulsive therapy ED: emergency department ENRICHD: EQ‐5D: European Quality of Life‐5 Dimension EMA: ecological momentary assessment ERQ: Emotion Regulation Questionnaire ESS: Experience of Shame Scale EuroQoL‐5D: European Quality of Life‐5 Dimension FASTER: FFMQ: Five Facet Mindfulness Questionnaire fMRI: functional magnetic resonance imaging GAD‐7: GHSQ: General Help‐Seeking Questionnaire GP: general practitioner HADS: HARS: Hamilton Anxiety Rating Scale HDRS: Hamilton Depression Rating Scale HKSAR: Hong Kong Special Administrative Region HRQ: Helping Relationship Questionnaire ICD‐10: International Classification of Diseases, 10th Revision INQ‐15: Interpersonal Needs Questionnaire‐15 IIPSS: Independent‐Interdependent Problem Solving Scale IQ: intelligence quotient ISAS: ISI: Insomnia Severity Index L‐SASI: MEAQ: Multi‐dimensional Experiential Avoidance Questionnaire MINI(‐7): MMSE: Mini Mental Status Examination MRI: magnetic resonance imaging MSP: NEO: NHS: National Health Service NSSI: non‐suicidal self‐injury N'VIU: OASIS: Overall Anxiety Severity and Impairment Scale ODSIS: Overall Depression Severity and Impairment Scale OHIP: PEPS: PHQ‐9: Patient Health Questionnaire 9 PSIS: Pierce Suicide Intent Scale PTSD: RCT: randomised controlled trial READ: Resilience Scale for Adolescents RRRS: RSA: Resilience Scale for Adults SAFETEL: SASII: SCID‐BPD: Structured Clinical Interview for Borderline Personality Disorder SCS: Self‐Compassion Scale SDQ: SF‐36: SH: self‐harm SIAM: SI‐IAT: Self‐Injury Implicit Association Test SITBI: Self‐Injurious Thoughts and Behaviors Interview SMQ: Southampton Mindfulness Questionnaire SMS: short messaging service SOS: SPP: Suicide Prevention Pathway SSB: Social Support Behaviours Scale SSS: Subjective Symptoms Scale SURVIVE: TAU: treatment‐as‐usual vs: WHOQOL‐BREF:
Differences between protocol and review
Following consensus discussions with review authors, we combined one comparison with case management:
Treatment adherence enhancement approaches.
We added three further comparisons to reflect approaches used in new trials of psychosocial interventions for SH in adults identified by this update:
Psychodynamic psychotherapy;
Structured general practitioner (GP) follow‐up;
Brief emergency department‐based interventions.
Contributions of authors
KH had the idea for the review. All authors screened studies for inclusion. KGW, SEH, GR, and KH extracted data and assessed risk of bias for included studies. KGW, SEH, and TLTS conducted the statistical analyses. KGW and KH wrote the initial version of the review and all authors contributed to the writing of drafts. All authors approved the final version of the review for publication.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Health and Medical Research Council, Australia
KW is supported by an Emerging Leadership 1 Fellowship awarded by the NHMRC (APP1177787).
-
National Institute of Health Research (NIHR), UK
KW received support from the NIHR (Award number: NIHR 131986)
Declarations of interest
KGW: is an editor for the Cochrane Common Mental Disorders Group, and senior editor for the Self‐Harm and Suicide Satellite of the group. SEH: is the joint co‐ordinating editor of the Cochrane Common Mental Disorders Group. She is funded by an Auckland Medical Research Foundation Douglas Goodfellow Repatriation Fellowship to develop and test a digital intervention for young people who engage in self‐harm. She is the Principal Clinical Advisor of the Suicide Prevention Office of the Ministry of Health for the New Zealand Government. GR: no declarations of interest to report in relation to this review PH: no declarations of interest to report in relation to this review TLTS: no declarations of interest to report in relation to this review ET: no declarations of interest to report in relation to this review KH: no declarations of interest to report in relation to this review
New
References
References to studies included in this review
Allard 1992 {published data only}
- Allard R, Marshall M, Plante MC. Intensive follow-up does not decrease the risk of repeat suicide attempts. Suicide and Life-Threatening Behavior 1992;22:303-14. [PubMed] [Google Scholar]
Amadéo 2015 {published data only}
- Amadéo S, Rereao M, Malogne A, Favro P, Nguyen NL, Milner A, et al. Testing brief intervention and phone contact among subjects with suicidal behavior: a randomized controlled trial in French Polynesia in the frames of the World Health Organization/Suicide Trends in At-Risk Territories study. Mental Illness 2015;7:5818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Leo D, Milner A. The WHO/START Study: promoting suicide prevention for a diverse range of cultural contexts. Suicide and Life-Threatening Behavior 2010;40:99-106. [DOI] [PubMed] [Google Scholar]
Andreoli 2015 {published data only}
- Andreoli A, Burnand Y, Cochennec M-F, Ohlendorf P, Frambati L, Gaudry-Maire D. Disapointed love and suicide: a randomized controlled trial of "abandonment psychotherapy" among borderline patients. Journal of Personality Disorders 2015;29:1-17. [DOI] [PubMed] [Google Scholar]
Armitage 2016 {published data only (unpublished sought but not used)}
- Armitage CJ, Rahim WA, Rowe R, O'Connor RC. An exploratory randomised trial of a simple, brief psychological intervention to reduce subsequent suicidal ideation and behaviour in patients admitted to hospital for self-harm. British Journal of Psychiatry 2016;208:470-6. [DOI] [PubMed] [Google Scholar]
Armitage 2016a {published data only (unpublished sought but not used)}
- Armitage CJ, Rahim WA, Rowe R, O'Connor RC. An exploratory randomised trial of a simple, brief psychological intervention to reduce subsequent suicidal ideation and behaviour in patients admitted to hospital for self-harm. British Journal of Psychiatry 2016;208:470-6. [DOI] [PubMed] [Google Scholar]
Armitage 2016b {published data only (unpublished sought but not used)}
- Armitage CJ, Rahim WA, Rowe R, O'Connor RC. An exploratory randomised trial of a simple, brief psychological intervention to reduce subsequent suicidal ideation and behaviour in patients admitted to hospital for self-harm. British Journal of Psychiatry 2016;208:470-6. [DOI] [PubMed] [Google Scholar]
Bateman 2009 {published and unpublished data}ISRCTN27660668
- Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. American Journal of Psychiatry 2009;166:1355-64. [DOI] [PubMed] [Google Scholar]
- Bateman A, O'Connell J, Lorenzini N, Gardner T, Fonagy P. A randomised controlled trial of mentalization-based treatment versus structured clinical management for patients with comorbid borderline personality disorder and antisocial personality disorder. BMC Psychiatry 2016;16:304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beautrais 2010 {published and unpublished data}
- Beautrais AL, Gibb SJ, Faulkner A, Fergusson DM, Mulder RT. Postcard intervention for repeat self-harm: randomised controlled trial. British Journal of Psychiatry 2010;197:55-60. [DOI] [PubMed] [Google Scholar]
Bennewith 2002 {published data only}
- Bennewith O, Stocks N, Gunnell D, Peters TJ, Evans MO, Sharp DJ. General practice based intervention to prevent repeat episodes of deliberate self-harm: cluster randomised controlled trial. British Medical Journal 2002;324:1254-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2005 {published data only}
- Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Journal of the American Medical Association 2005;294:563-70. [DOI] [PubMed] [Google Scholar]
- Ghahramanlou-Holloway M, Bhar SS, Brown GK, Olsen C, Beck AT. Changes in problem-solving appraisal after cognitive therapy for the prevention of suicide. Psychological Medicine 2012;42:1185-93. [DOI] [PubMed] [Google Scholar]
- Stirman SW, Brown GK, Ghahramanlou-Holloway M, Fox AJ, Chohan MZ, Beck AT. Participation bias among suicidal adults in a randomized controlled trial. Suicide and Life-Threatening Behavior 2011;41:203-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carter 2005 {published and unpublished data}
- Carter GL, Clover K, Whyte IM, Dawson AH, D’este C. Postcards from the EDge: 24-month outcomes of a randomised controlled trial for hospital-treatment self-poisoning. British Journal of Psychiatry 2007;191:548-53. [DOI] [PubMed] [Google Scholar]
- Carter GL, Clover K, Whyte IM, Dawson AH, D’este C. Postcards from the EDge project: randomised controlled trial of an intervention using postcards to reduce repetition of hospital treated deliberate self-poisoning. British Medical Journal 2005;331:805-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cedereke 2002 {published data only}
- Cedereke M, Monti K, Ojehagen A. Telephone contact with patients in the year after a suicide attempt: does it affect treatment attendance and outcome? A randomised controlled study. European Psychiatry 2002;17:82-91. [DOI] [PubMed] [Google Scholar]
Clarke 2002 {published data only}
- Clarke T, Baker P, Watts CJ, Williams K, Feldman RA, Sherr L. Self-harm in adults: a randomised controlled trial of nurse-led case management versus routine care only. Journal of Mental Health 2002;11:167-76. [Google Scholar]
Crawford 2010 {published and unpublished data}
- Crawford MJ, Csipke E, Brown A, Reid S, Nilsen K, Redhead J, et al. The effect of referral for brief intervention for alcohol misuse on repetition of deliberate self-harm: an exploratory randomized controlled trial. Psychological Medicine 2010;40:1821-8. [DOI] [PubMed] [Google Scholar]
Davidson 2014 {published and unpublished data}
- Davidson KM, Brown TM, James V, Kirk J, Richardson J. Manual-assisted cognitive therapy for self-harm in personality disorder and substance misuse: a feasibility trial. Psychiatric Bulletin 2014;38:108-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dubois 1999 {published data only}
- Dubois L, Walter M, Bleton L, Genest P, Lemonnier E, Lachevre G. Evaluation of a comparative and prospective protocol for suicidal youth: analysis of psychiatric diagnosis, therapeutic compliance and rate of recurrence over one year (preliminary results) [Evaluation comparative et prospective d’un protocole de prise en charge specifique de jeunes suicidants: analyse du diagnostic psychiatrique initial, de l’observance therapeutique et du taux de recidive a un an (resultats preliminaires)]. Annales Médico-Psychologiques 1999;157:557-61. [Google Scholar]
Evans 1999a {published data only}
- Evans J, Evans M, Morgan HG, Hayward A, Gunnell, D. Crisis card following self-harm: 12-month follow-up of a randomised controlled trial. British Journal of Psychiatry 2005;187:186-7. [DOI] [PubMed] [Google Scholar]
- Evans MO, Morgan HG, Hayward A, Gunnell DJ. Crisis telephone consultation for deliberate self-harm patients: effects on repetition. British Journal of Psychiatry 1999;175:23-7. [DOI] [PubMed] [Google Scholar]
Evans 1999b {published data only}
- Evans K, Tyrer P, Catalan J, Schmidt U, Davidson K, Dent J, et al. Manual-assisted cognitive-behaviour therapy (MACT): a randomized controlled trial of a brief intervention with bibliotherapy in the treatment of recurrent deliberate self-harm. Psychological Medicine 1999;29:19-25. [DOI] [PubMed] [Google Scholar]
Fleischmann 2008 {published and unpublished data}
- Bertolote JM, Fleischmann A, De Leo D, Phillips MR, Botega NJ, Vijayakumar L, et al. Repetition of suicide attempts: data from five culturally different low- and middle-income country emergency care settings participating in the WHO SUPRE-MISS study. Crisis 2010;31:194-201. [DOI] [PubMed] [Google Scholar]
- Da Silva Cais CF, Stefanello S, Fabricio M, Marisa L, Vaz Scavacini de Freitas G, Botega NJ. Factors associated with repeated suicide attempts: preliminary results of the WHO Multisite Intervention Study on Suicidal Behavior (SUPRE-MISS) from Capinas, Brazil. Crisis 2009;30:73-8. [DOI] [PubMed] [Google Scholar]
- Fleischmann A, Bertolote JM, Wasserman D, De Leo D, Bolhari J, Botega NJ, et al. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bulletin of the World Health Organisation 2008;86:703-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischmann A, Bertolote JM. Multisite Intervention Study on Suicidal Behaviours - SUPRE-MISS: protocol of SUPRE-MISS. citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.174.5140&rep=rep1&type=pdf (accessed 31 October 2020).
- Hassanzadeh M, Khajeddin N, Nojomi M, Fleischmann A, Eshrati T. Brief intervention and contact after deliberate self-harm: an Iranian randomised controlled trial. Iranian Journal of Psychiatry and Behavioral Sciences 2010;4:5-12. [Google Scholar]
- Stefanello S, Filinto da Silva Cais C, Mauro MLF, Scavacini de Freitas GV, Botega NJ. Gender differences in suicide attempts: preliminary results of the multisite intervention study on suicidal behavior (SUPRE-MISS) from Campinas, Brazil. Brazilian Journal of Psychiatry 2008;30:139-43. [DOI] [PubMed] [Google Scholar]
- Vijayakumar L, Umamaheswari C, Shujaath Ali ZS, Devaraj P, Kesavan K. Intervention for suicide attempters: a randomized controlled study. Indian Journal of Psychiatry 2011;53:244-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu D, Zhang X-L, Li X-Y, Niu Y-J, Zhang Y-P, Wang S-L, et al. Effectiveness of 18-month psychosocial intervention for suicide attempters. Zhongguo Xinli Weisheng Zazhi [Chinese Mental Health Journal] 2012;26:24-9. [Google Scholar]
Gibbons 1978 {published data only}
- Gibbons JS, Butler J, Urwin P, Gibbons JL. Evaluation of a social work service for self-poisoning patients. British Journal of Psychiatry 1978;133:111-8. [DOI] [PubMed] [Google Scholar]
Gratz 2006 {published and unpublished data}
- Gratz KL, Gunderson JG. Preliminary data on an acceptance-based emotion regulation group intervention for deliberate self-harm among women with borderline personality disorder. Behavior Therapy 2006;37:25-35. [DOI] [PubMed] [Google Scholar]
Gratz 2014 {published and unpublished data}
- Gratz KL, Bardeen JR, Levy R, Dixon-Gordon KL, Tull MT. Mechanisms of change in an emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Behaviour Research and Therapy 2015;65:29-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Dixon-Gordon KL, Tull MT. Predictors of treatment response to an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Personality disorders: Theory, Research, and Treatment 2014;5:97-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Levy R. Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychological Medicine 2013;44:2099-122. [DOI] [PubMed] [Google Scholar]
Grimholt 2015 {published data only}
- Grimholt TK, Jacobsen D, Haavet OR, Sandvik L, Jorgensen T, Norheim AB, et al. Structured follow-up by general practitioners after deliberate self-poisoning: A randomised controlled trial. BMC Psychiatry 2015;15:245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimholt TK, Jacobsen D, Haavet OR, Sandvik L, Jorgensen T, Norheim AB. Effect of systematic follow-up by general practitioners after deliberate self-poisoning: a randomised controlled trial. PLOS One 2015;10:e0143934. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guthrie 2001 {published data only}
- Guthrie E, Kapur N, Kway-Jones K, Chew-Graham C, Moorey J, Mendel E, et al. Randomised controlled trial of brief psychological intervention after deliberate self-poisoning. British Medical Journal 2001;323:135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gysin‐Maillart 2016 {published data only}
- Gysin-Maillart A, Schwab S, Soravia L, Megert M, Michel K. A novel brief therapy for patients who attempt suicide: a 24-months follow-up randomized controlled study of the Attempted Suicide Short Intervention Program (ASSIP). PLOS One 2016;13:e1001968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gysin-Maillart A, Soravia L, Schwab S. Attempted suicide short intervention program influences coping among patients with a history of attempted suicide. Journal of Affective Disorders 2020;264:393-9. [DOI] [PubMed] [Google Scholar]
- Michel K, Valach L, Gysin-Maillart A. A novel therapy for people who attempt suicide and why we need new models of suicide. International Journal Environmental Research and Public Health 2017;14:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park A-L, Gysin-Maillart A, Müller TJ, Exadaktylos A, Michel K. Cost-effectiveness of a brief structured intervention program aimed at preventing repeat suicide attempts among those who previously attempted suicide: a secondary analysis of the ASSIP randomized clinical trial. JAMA Open 2018;1:e183680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ring M, Gysin-Maillart A. Patients' satisfaction with the therapeutic relationship and therapeutic outcome is related to suicidal ideation in the Attempted Suicide Short Intervention Program (ASSIP). Crisis 2020;41(5):337-43. [DOI] [PubMed] [Google Scholar]
Harned 2014 {published and unpublished data}
- Harned MS, Fitzpatrick S, Schmidt SC. Identifying change targets for posttraumatic stress disorder among suicidal and self-injuring women with borderline personality disorder. Journal of Traumatic Studies 2020;33(4):610-16. [DOI: 10.1002/jts.22504] [DOI] [PubMed] [Google Scholar]
- Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of dialectical behavior therapy with and without the dialectical behavior therapy prolonged exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behaviour Research and Therapy 2014;55:7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hassanian‐Moghaddam 2011 {published and unpublished data}
- Hassanian-Moghaddam H, Sarjami S, Kolahi A-A, Carter GL. Postcards in Persia: randomised controlled trial to reduce suicidal behaviours 12 months after hospital-treated self-poisoning. British Journal of Psychiatry 2011;198:309-16. [DOI] [PubMed] [Google Scholar]
- Hassanian-Moghaddam H, Sarjami S, Kolahi A-A, Lewin T, Carter G. Postcards in Persia: a twelve to twenty-four month follow-up of a randomized controlled trial for hospital-treated deliberate self-poisoning. Archives of Suicide Research 2017;21:138-54. [DOI] [PubMed] [Google Scholar]
Hatcher 2011 {published and unpublished data}
- Hatcher S, Sharon C, Parag V, Collins N. Problem-solving therapy for people who present to hospital with self-harm: Zelen randomised controlled trial. British Journal of Psychiatry 2011;199:310-6. [DOI] [PubMed] [Google Scholar]
Hatcher 2015 {published and unpublished data}
- Hatcher S, Sharon C, House A, Collins N, Collings S, Pillai A. The ACCESS study: Zelen randomised controlled after self-harm. British Journal of Psychiatry 2015;206:229-36. [DOI] [PubMed] [Google Scholar]
Hatcher 2016 {published and unpublished data}
- Hatcher S, Coupe N, Wikiriwhi K, Durie M, Pillai A. Te Ira Tangata: a Zelen randomised controlled trial of a culturally informed treatment compared to treatment as usual in Māori who present to hospital after self-harm. Social Psychiatry and Psychiatric Epidemiology 2016;51:885-94. [DOI] [PubMed] [Google Scholar]
Hawton 1981 {published and unpublished data}
- Hawton K, Bancroft J, Catalan J, Kingston B, Stedeford A. Domiciliary and out-patient treatment of self-poisoning patients by medical and non-medical staff. Psychological Medicine 1981;11:169-77. [DOI] [PubMed] [Google Scholar]
Hawton 1987 {published and unpublished data}
- Hawton K, McKeown S, Day A, Martin P, O’Connor M, Yule J. Evaluation of out-patient counselling compared with general practitioner care following overdoses. Psychological Medicine 1987;17:751-61. [DOI] [PubMed] [Google Scholar]
Husain 2014 {published and unpublished data}
- Husain N, Afsar S, Ara J, Fayyaz H, Ur Rahman R, Tomenson B, et al. Brief psychological intervention after self-harm: randomised controlled trial from Pakistan. British Journal of Psychiatry 2014;204:462-70. [DOI] [PubMed] [Google Scholar]
Hvid 2011 {published and unpublished data}
- Hvid M, Vangborg K, Sørensen HJ, Nielsen IK, Stenborg JM, Wang AG. Preventing repetition of attempted suicide- II: the Amager Project, a randomized controlled trial. Nordic Journal of Psychiatry 2011;65:292-8. [DOI] [PubMed] [Google Scholar]
Kapur 2013 {published and unpublished data}
- Kapur N, Gunnell D, Hawton K, Nadeem S, Khalil S, Longson D, et al. Messages from Manchester: pilot randomised controlled trial following self-harm. British Journal of Psychiatry 2013;203:73-4. [DOI] [PubMed] [Google Scholar]
Kawanishi 2014 {published and unpublished data}
- Furuno T, Nakagawa M, Hinto K, Tamada T, Kawashima Y, Matsuoka Y, et al. Effectiveness of assertive case management on repeat self-harm in patients admitted for suicide attempt: findings from ACTION-J study. Journal of Affective Disorders 2018;225:460-5. [DOI] [PubMed] [Google Scholar]
- Kawanishi C, Aruga T, Ishizuka N, Yonemoto N, Otsuka K, Kamijo Y, et al. Assertive case management versus enhanced usual care for people with mental health problems who had attempted suicide and were admitted to hospital emergency departments in Japan (ACTIONJ): a multicentre, randomised controlled trial. Lancet Psychiatry 2014;1:193-201. [DOI] [PubMed] [Google Scholar]
- Norimoto K, Ikeshita K, Kishimoto T, Okuchi K, Yonemoto N, Sugimoto T, et al. Effect of assertive case management intervention on suicide attempters with comorbid Axis I and II psychiatric diagnoses: secondary analysis of a randomised controlled trial. BMC Psychiatry 2020;20:311. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liberman 1981 {published data only}
- Liberman RP, Eckman T. Behavior therapy vs insight-oriented therapy for repeated suicide attempters. Archives of General Psychiatry 1981;38:1126-30. [DOI] [PubMed] [Google Scholar]
Lin 2020 {published data only (unpublished sought but not used)}
- Lin Y-C, Liu S-I, Chen S-C, Sun F-J, Huang H-C, Huang C-R, et al. Brief cognitive-based psychosocial intervention and case management for suicide attempters discharged from the emergency department in Taipei, Taiwan: a randomized controlled study. Suicide and Life-Threatening Behavior 2020;50:688-705. [DOI] [PubMed] [Google Scholar]
Linehan 1991 {published data only}
- Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of General Psychiatry 1991;48:1060-4. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Heard HL, Armstrong HE. Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Archives of GeneralPsychiatry 1993;50:971-4. [DOI] [PubMed] [Google Scholar]
Linehan 2006 {published and unpublished data}
- Bedics JD, Atkins DC, Comtois JA, Linehan MM. Treatment differences in the therapeutic relationship and introject during a 2-year randomized controlled trial of dialectical behavior therapy versus non-behavioral psychotherapy experts for borderline personality disorder. Journal of Consulting and Clinical Psychology 2012;80:66-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedics JD, Atkins DC, Harned MS, Linehan MM. The therapeutic alliance as a predictor of outcome in dialectical behavior therapy versus nonbehavioral psychotherapy by experts for borderline personality disorder. Psychotherapy: Theory, Research and Practice 2015;52:67-77. [DOI] [PubMed] [Google Scholar]
- Coyle TN, Shaver JA, Linehan MM. On the potential for iatrogenic effects of psychiatric crisis services: the example of dialectical behavior therapy for adult women with borderline personality disorder. Journal of Consulting and Clinical Psychology 2018;86:116-24. [DOI] [PubMed] [Google Scholar]
- Harned MS, Chapman AL, Dexter-Mazza ET, Murray A, Comtois KA, Linehan MM. Treating co-occurring axis I disorders in recurrently suicidal women with borderline personality disorder: a 2-year randomized trial of dialectical behavior therapy versus community treatment by experts. Journal of Consulting and Clinical Psychology 2008;76:1068-75. [DOI] [PubMed] [Google Scholar]
- Harned MS, Chapman AL, Dexter-Mazza ET, Murray A, Comtois KA, Linehan MM. Treating co-occurring axis I disorders in recurrently suicidal women with borderline personality disorder: a 2-year randomized trial of dialectical behavior therapy versus community treatment by experts. Personality Disorders: Theory, Research and Treatment 2009;5:35-45. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry 2006;63:757-66. [DOI] [PubMed] [Google Scholar]
- Neacsiu AD, Lungu A, Harned MS, Rizvi SL, Linehan MM. Impact of dialectical behavior therapy versus community treatment by experts on emotional experience, expression,and acceptance in borderline personality disorder. Behaviour Research and Therapy 2014;53:47-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secrist CD. The Role of Executive Functioning in the Treatment of Borderline Personality Disorder. Seattle, WA: Department of Clinical Psychology, University of Washington, 2014. [Google Scholar]
Linehan 2015 {published data only}
- Kuehn KS, King KM, Linehan MM, Harned MS. Modeling the suicidal behavior cycle: understanding repeated suicide attempts among individuals with borderline personality disorder and a history of attempting suicide. Journal of Consulting and Clinical Psychology 2020;88:570-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: a randomized clinical trial and component analysis. JAMA Psychiatry 2015;72:475-82. [DOI] [PubMed] [Google Scholar]
- Wilks CR, Korslund KE, Harned M, Linehan MM. Dialectical behavior therapy and domains of functioning over two years. Behaviour Research and Therapy 2016;77:162-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Linehan 2015a {published data only}
- Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: a randomized clinical trial and component analysis. JAMA Psychiatry 2015;72:475-82. [DOI] [PubMed] [Google Scholar]
- Kuehn KS, King KM, Linehan MM, Harned MS. Modeling the suicidal behavior cycle: understanding repeated suicide attempts among individuals with borderline personality disorder and a history of attempting suicide. Journal of Consulting and Clinical Psychology 2020;88:570-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilks CR, Korslund KE, Harned M, Linehan MM. Dialectical behavior therapy and domains of functioning over two years. Behaviour Research and Therapy 2016;77:162-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Linehan 2015b {published data only}
- Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: a randomized clinical trial and component analysis. JAMA Psychiatry 2015;72:475-82. [DOI] [PubMed] [Google Scholar]
- Kuehn KS, King KM, Linehan MM, Harned MS. Modeling the suicidal behavior cycle: understanding repeated suicide attempts among individuals with borderline personality disorder and a history of attempting suicide. Journal of Consulting and Clinical Psychology 2020;88:570-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilks CR, Korslund KE, Harned M, Linehan MM. Dialectical behavior therapy and domains of functioning over two years. Behaviour Research and Therapy 2016;77:162-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marasinghe 2012 {published and unpublished data}
- Marasinghe RB, Edirippulige S, Kavanagh D, Smith A, Jiffry MTM. Effect of mobile phone-based psychotherapy in suicide prevention: a randomized controlled trial in Sri Lanka. Journal of Telemedicine and Telecare 2012;18:151-5. [DOI] [PubMed] [Google Scholar]
- Marasinghe RB. Evaluation of a Brief Inpatient and Community Intervention to Address Suicide Risk in Sri Lanka Using Mobile Phones [PhD thesis]. Brisbane, QLD: The University of Queensland, School of Medicine, 2012. [Google Scholar]
McAuliffe 2014 {published and unpublished data}
- McAuliffe C, McLeavey BC, Fitzgerald T, Corcoran P, Carroll B, Ryan L, et al. Group problem-solving skills training for self-harm: randomised controlled trial. British Journal of Psychiatry 2014;204:383-90. [DOI] [PubMed] [Google Scholar]
McLeavey 1994 {published data only}
- McLeavey B, Daly R, Ludgate J, Murray C. Interpersonal problem-solving skills training in the treatment of self-poisoning patients. Suicide and Life-Threatening Behavior 1994;24:382-94. [PubMed] [Google Scholar]
McMain 2009 {published and unpublished data}
- Boritz T, Barnhart R, McMain SF. The influence of posttraumatic stress disorder on treatment outcomes of patients with borderline personality disorder. Journal of Personality Disorders 2016;30:395-407. [DOI] [PubMed] [Google Scholar]
- Case BG. Dialectical behavior therapy versus general psychiatric management in the treatment of borderline personality disorder. American Journal of Psychiatry 2010;167:475. [DOI] [PubMed] [Google Scholar]
- McMain SF, Fitzpatrick S, Boritz T, Barnhart R, Links P, Streiner DL. Outcome trajectories and prognostic factors for suicide and self-harm behaviors in patients with borderline personality disorder following one year of outpatient psychotherapy. Journal of Personality Disorders 2018;32:497-512. [DOI] [PubMed] [Google Scholar]
- McMain SF, Guimond T, Streiner DL, Cardish RJ, Links PS. Dialectical behavior therapy compared with general psychiatric management for borderline personality disorder: clinical outcomes and functioning over a 2-year follow-up. American Journal of Psychiatry 2012;169:650-61. [DOI] [PubMed] [Google Scholar]
- McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, et al. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. American Journal of Psychiatry 2009;166:1365-74. [DOI] [PubMed] [Google Scholar]
McMain 2017 {published data only}
- Krantz LH, McMain S, Kuo JR. The unique contribution of acceptance without judgment in predicting nonsuicidal self-injury after 20-weeks of dialectical behaviour therapy group skills training. Behaviour Research and Therapy 2018;104:44-50. [DOI] [PubMed] [Google Scholar]
- McMain SF, Guimond T, Barnhart R, Habinski L, Streiner DL. A randomized trial of brief dialectical behaviour therapy skills training in suicide patients suffering from borderline disorder. Acta Psychiatrica Scandinavica 2017;135:138-48. [DOI] [PubMed] [Google Scholar]
- Stratton N, Mendoza Alvarez M, Labrish C, Barnhart R, McMain S. Predictors of dropout from a 20-week dialectical behavior therapy skills group for suicidal behaviors and borderline personality disorder. Journal of Personality Disorders 2018;32:391-406. [DOI] [PubMed] [Google Scholar]
Morgan 1993 {published data only}
- Morgan HG, Jones EM, Owen JH. Secondary prevention of non-fatal deliberate self-harm. The green card study. British Journal of Psychiatry 1993;163:111-2. [DOI] [PubMed] [Google Scholar]
Morthorst 2012 {published data only}
- Morthorst B, Krogh J, Erlangsen A, Alberdi F, Nordentoft M. Effect of assertive outreach after suicide attempt in the AID (Assertive Intervention for Deliberate self-harm) trial: randomised controlled trial. British Medical Journal 2012;345:e4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mouaffak 2015 {published data only}
- Mouaffak F, Marchand A, Castaigne E, Arnoux A, Hardy P. OSTA program: a French follow up intervention program for suicide prevention. Psychiatry Research 2015;230:913-8. [DOI] [PubMed] [Google Scholar]
Mousavi 2015 {published data only}
- Mousavi SG, Amini M, Mahaki B, Bagherian-Sarariudi R. Effect of phone call versus face-to-face follow-up on recurrent suicide prevention in individuals with a history of multiple suicide attempts. Advanced Biomedical Research 2016;5:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mousavi 2017 {published data only}
- Mousavi SG, Tehrani MN, Maracy M. The effect of active treatment and visit compared to conventional treatment, on preventing recurrent suicidal attempts: a randomized controlled clinical trial. Advanced Biomedical Research 2017;6:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Naidoo 2014 {published data only}
- Naidoo SS, Gathiram P, Schlebusch L. Effectiveness of a buddy intervention support programme for suicidal behaviour in a primary care setting. South African Family Practice 2014;56:263-70. [Google Scholar]
O'Connor 2015 {published data only}
- O'Connor SS, Comtois KA, Wang J, Russo J, Peterson R, Lapping-Carr L, et al. The development and implementation of a brief intervention for medically admitted suicide attempt survivors. General Hospital Psychiatry 2015;37:427-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Connor 2017 {published data only}ISRCTN99488269
- O'Connor RC, Ferguson E, Scott F, Smyth R, McDaid D, Park A-L. A brief psychological intervention to reduce repetition of self-harm in patient admitted to hospital following a suicide attempt: a randomised controlled trial. Lancet Psychiatry 2017;4:451-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Connor 2020 {published data only}
- O'Connor SS, McClay MM, Choudhry S, Shields AD, Carlson R, Alonso Y. Pilot randomized clinical trial of the teachable moment brief intervention for hospitalized suicide attempt survivors. General Hospital Psychiatry 2020;63:111-8. [DOI] [PubMed] [Google Scholar]
Owens 2020 {published data only}ISRCTN54036115
- Collinson M, Owens D, Blenkiron P, Burton K, Graham L, Hatcher S, et al. MIDSHIPS: Multicentre Intervention Designed for Self-Harm using Interpersonal Problem-Solving: protocol for a randomised controlled feasibility study. Trials 2014;15:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens D, Wright-Hughes A, Graham L, Blenkiron P, Burton K, Collinson M, et al. Problem-solving therapy rather than treatment as usual for adults after self-harm: a pragmatic, feasibility, randomised controlled trial (the MIDSHIPS trial). Pilot and Feasibility Studies 2020;6:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patsiokas 1985 {published data only}
- Patsiokas AT, Clum GA. Effects of psychotherapeutic strategies in the treatment of suicide attempters. Psychotherapy: Theory, Research and Practice 1985;22:281-90. [Google Scholar]
Priebe 2012 {published and unpublished data}
- Priebe S, Bhatti N, Barnicot K, Bremner S, Gaglia A, Katsakou C, et al. Effectiveness and cost-effectiveness of dialectical behaviour therapy for self-harming patients with personality disorder: a pragmatic randomised controlled trial. Psychotherapy and Psychosomatic 2012;81:356-65. [DOI] [PubMed] [Google Scholar]
Sahin 2018 {published data only}
- Sahin Z, Vinnars B, Gorman BS, Wilczek A, Åsberg M, Barber JP. Clinical severity as a moderator of outcome in psychodynamic and dialectical behavior therapies for borderline personality disorder. Personality Disorders 2018;9:437-46. [DOI] [PubMed] [Google Scholar]
Salkovskis 1990 {published data only}
- Salkovskis PM, Atha C, Storer D. Cognitive-behavioural problem solving in the treatment of patients who repeatedly attempt suicide. A controlled trial. British Journal of Psychiatry 1990;157:871–6. [DOI] [PubMed] [Google Scholar]
Slee 2008 {published and unpublished data}
- Slee N, Garnefski N, Van der Leeden R, Arensman E, Spinhoven P. Cognitive-behavioural intervention for self-harm: randomised controlled trial. British Journal of Psychiatry 2008;192:202-11. [DOI] [PubMed] [Google Scholar]
Sreedaran 2020 {published data only}
- Sreedaran P, Beniwal RP, Chari U, Smitha TS, Vidhya SSV, Gupta V, et al. A randomized controlled trial to assess feasibility and acceptability of telephone-based psychosocial interventions in individuals who attempted suicide. Indian Journal of Psychological Medicine 2020;42:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stewart 2009 {published and unpublished data}
- Stewart CD, Quinn A, Plever S, Emmerson B. Comparing cognitive behavior therapy, problem solving therapy, and treatment as usual in a high risk population. Suicide and Life-Threatening Behavior 2009;39:538-47. [DOI] [PubMed] [Google Scholar]
Tapolaa 2010 {published and unpublished data}
- Tapolaa V, Lappalainen R, Wahlström J. Brief intervention for deliberate self-harm: an exploratory study. Suicidology Online 2010;1:95-108. [Google Scholar]
Torhorst 1987 {published data only}
- Möller HJ. Efficacy of different strategies of aftercare for patients who have attempted suicide. Journal of the Royal Society of Medicine 1989;82:643-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torhorst A, Möller HJ, Bürk F, Kurz A, Wächtler C, Lauter H. The psychiatric management of parasuicide patients: a controlled clinical study comparing different strategies of outpatient treatment. Crisis 1987;8:53-61. [PubMed] [Google Scholar]
Torhorst 1988 {published data only}
- Torhorst A, Möller HJ, Kurz A, Schmid-Bode W, Lauter H. Comparing a 3-month and a 12-month-outpatient aftercare program for parasuicide repeaters. In: Möller HJ, Schmidtke A, Welz R, editors(s). Current Issues of Suicidology. Berlin, Germany: Springer-Verlag, 1988:419–24. [Google Scholar]
Turner 2000 {published data only}
- Turner RM. Naturalistic evaluation of dialectical behavior therapy-oriented treatment for borderline personality disorder. Cognitive and Behavioral Practice 2000;7:413-9. [Google Scholar]
Tyrer 2003 {published data only}
- Tyrer P, Thompson S, Schmidt U, Jones V, Knapp M, Davidson K, et al. Randomized controlled trial of brief cognitive behaviour therapy versus treatment as usual in recurrent deliberate self-harm: the POPMACT study. Psychological Medicine 2003;33:969-76. [DOI] [PubMed] [Google Scholar]
Vaiva 2006 {published data only}
- Vaiva G, Ducrocq F, Meyer P, Mathieu D, Philippe A, Libersa C, et al. Effect of telephone contact on further suicide attempts in patients discharged from an emergency department: randomised controlled study. British Medical Journal 2006;332:1241-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaiva 2018 {published data only}
- Demesmaeker A, Benard V, Leroy A, Vaiva G. Impacts of a brief contact intervention in suicide prevention on medical care consumptions [Impacts d'un système de veille en prévention du suicide sur les consommations de soins]. L'Encéphale 2019;45:S27-31. [DOI] [PubMed] [Google Scholar]
- Messiah A, Notredame C-E, Demarty A-L, Duhem S, Vaiva G. Combining green cards, telephone calls and postcards into an intervention algorithm to reduce suicide reattempt (AlgoS): p-hoc analyses of an inconclusive randomized controlled trial. PLOS One 2019;14:e0210778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaiva G, Berrouiguet S, Walter M, Courtet P, Ducrocq F, Jardon V, et al. Combining postcards, crisis cards, and telephone contact into a decision-making algorithm to reduce suicide reattempt: a randomized clinical trial of a personalized brief contact intervention. Journal of Clinical Psychiatry 2018;79:17m11631. [DOI] [PubMed] [Google Scholar]
Van der Sande 1997 {published data only}
- Van der Sande R, Buskens E, Van der Graaf Y, Van Rooijen E, Allart E, Van Engeland H. No measurable effect from general socio-psychiatric care for those attempting suicide: a randomized experiment [Geen meetbaar effect van algemene sociaal–psychiatrische nazorg voor suicidepogers; een gerandomiseerd experiment]. Nederlands Tijdschriftvoor de Geneeskunde 1998;142:2356. [Google Scholar]
- Van der Sande R, Van Rooijen L, Buskens E, Allart E, Hawton K, Van der Graaf Y, et al. Intensive in-patient and community intervention versus routine care after attempted suicide. A randomised controlled intervention study. British Journal of Psychiatry 1997;171:35-41. [DOI] [PubMed] [Google Scholar]
Van Heeringen 1995 {published data only}
- Van Heeringen C, Jannes S, Buylaert W, Hendrick H, De Bacquer D, Van Remoortel J. The management of noncompliance with referral to out-patient after-care among attempted suicide patients: a controlled intervention study. Psychological Medicine 1995;25:963-70. [DOI] [PubMed] [Google Scholar]
Walton 2020 {published and unpublished data}
- Walton CJ, Bendit N, Baker AL, Carter GL, Lewin TJ. A randomised trial of dialectical behaviour therapy and the conversational model for the treatment of borderline personality disorder with recent suicidal and/or non-suicidal self-injury: an effectiveness study in an Australian public mental health service. Australian and New Zealand Journal of Psychiatry 2020;54:1020-34. [DOI] [PubMed] [Google Scholar]
Wang 2016 {published data only}
- Wang Y-C, Hsieh L-Y, Wang M-Y, Chou C-H, Huang M-W, Ko H-C. Coping card usage can further reduce suicide reattempt in suicide attempter case management within 3-month intervention. Suicide and Life-Threatening Behavior 2016;46:106-20. [DOI] [PubMed] [Google Scholar]
Waterhouse 1990 {published data only}
- Waterhouse J, Platt S. General hospital admission in the management of parasuicide. A randomised controlled trial. British Journal of Psychiatry 1990;156:236–42. [DOI] [PubMed] [Google Scholar]
Wei 2013 {published data only}
- Wei S, Liu L, Bi B, Li H, Hou J, Tan S, et al. An intervention and follow-up study following a suicide attempt in the emergency departments of four general hospitals in Shenyang, China. Crisis 2013;34:107-15. [DOI] [PubMed] [Google Scholar]
Weinberg 2006 {published data only}
- Weinberg I, Gunderson JG, Hennen J, Cutter CJ. Manual assisted cognitive treatment for deliberate self-harm in borderline personality disorder patients. Journal of Personality Disorders 2006;20:482-92. [DOI] [PubMed] [Google Scholar]
Welu 1977 {published data only}
- Welu T. A follow-up program for suicide attempters: evaluation of effectiveness. Suicide and Life-Threatening Behavior 1977;7:17-30. [PubMed] [Google Scholar]
References to studies excluded from this review
Agyapong 2016 {published data only}
- Agyapong V, Behre T, Juhas M, Greenshaw A. Preventing self-harm and reducing suicidal ideation through an expediated regular supportive psychotherapy and assertive case management - protocol for a three-armed partial randomised controlled trial. European Psychiatry 2016;33S:S440. [Google Scholar]
Ahmed 2016 {published data only}ISRCTN76914248
- Ahmed N, John A, Islam S, Jones R, Anderson P, Davies C, et al. Investigating the feasibility of an enhanced contact intervention in self-harm and suicidal behaviour: a protocol for a randomised controlled trial delivering a Social support and Wellbeing Intervention following Self-Harm (SWISH). British Medical Journal Open 2016;6:e012043. [DOI] [PMC free article] [PubMed] [Google Scholar]
Albuixech‐García 2020 {published data only}
- Albuixech-García R, Juliá-Sanchis R, Molina MAF, Escribano S. Impact of the mental health care continuity-chain among individuals expressing suicidal behaviour in a Spanish sample. Issues in Mental Health Nursing 2020;41:602-7. [DOI] [PubMed] [Google Scholar]
Andover 2015 {published data only}
- Andover MS, Schatten HT, Morris BW, Miller IW. Development of an intervention for nonsuicidal self-injury in young adults: an open pilot trial. Cognitive and Behavioral Practice 2015;22:491-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andover 2017 {published data only}
- Andover MS, Schatten HT, Morris BW, Holman CS, Miller IW. An intervention for non-suicidal self-injury in young adults: a pilot randomized controlled trial. Journal of Consulting and Clinical Psychology 2017;85:620-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andreasson 2016 {published data only}
- Andreasson K, Krough J, Rosenbaum B, Gluud C, Jobes DA, Nordentoft M. The DiaS trial: Dialectical behavior therapy versus collaborative assessment and management of Suicidality on self-harm in patients with a recent suicide attempt and borderline personality disorder traits - study protocol for a randomized controlled trial. Trials 2014;15:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreasson K, Krough J, Wenneberg C, Jessen HKL, Krakauer K, Gluud C, et al. Effectiveness of dialectical behavior therapy versus collaborative assessment and management of suicidality treatment for reduction of self-harm in adults with borderline personality traits and disorder - randomized observer-blinded clinical trial. Depression and Anxiety 2016;33:520-30. [DOI] [PubMed] [Google Scholar]
Andreoli 2019 {published data only}
- Andreoli A, Burnand Y, Frambati L, Manning D, Frances A. Abandonment psychotherapy and psychosocial functioning among suicidal patients with borderline personality disorder: a 3-year naturalistic follow-up. Journal of Personality Disorders 2019;33:423-36. [DOI] [PubMed] [Google Scholar]
Barnes 2018 {published data only}
- Barnes MC, Haase AM, Bard AM, Donovan JL, Davies R, Dursley S, et al. HOPE: Help fOr PEople with money, employment, benefit or housing problems: study protocol for a randomised controlled trial. Pilot and Feasibility Studies 2017;3:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes MC, Haase AM, Scott LJ, Linton M-J, Bard AM, Donovan JL, et al. The Help fOr PEople with money, employment, benefit or housing problems (HOPE) intervention: pilot randomised trial with mixed methods feasibility research. Pilot and Feasibility Studies 2018;4:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barnhofer 2015 {published data only}ISRCTN97185214
- Barnhofer T, Crane C, Brennan K, Duggan DS, Crane RS, Eames C, et al. Mindfulness-based cognitive therapy (MBCT) reduces the association between depressive symptoms and suicidal cognitions in patients with a history of suicidal depression. Journal of Consulting and Clinical Psychology 2015;83:1013-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane C, Barnhofer T, Duggan DS, Eames C, Hepburn S, Shah D, et al. Comfort from suicidal cognition in recurrently depressed patients. Journal of Affective Disorders 2014;155:241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radford S, Eames C, Brennan K, Lambert G, Crane C, Williams JMG, et al. Trait mindfulness as a limiting factor for residual depressive symptoms: an explorative study using quantile regression. PLOS One 2014;9:e100022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG, Russell IT, Crane C, Russell D, Whitaker CJ, Duggan DS. Staying well after depression: trial design and protocol. BMC Psychiatry 2010;10:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bateman 2020 {published data only}
- Bateman A, Constantinou MP, Fonagy P, Holzer S. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personality Disorders: Theory, Research, and Treatment 2020 Jun 25 [EPub ahead of print]. [DOI: 10.1037/per0000422] [DOI] [PubMed]
Bentley 2017 {published data only}
- Bentley KH, Sauer-Zavala S, Cassiello-Robbins CF, Conklin LR, Vento S, Homer D. Treating suicidal thoughts and behaviors within an emotional disorders framework: acceptability and feasibility of the unified protocol in an inpatient setting. Behavior Modification 2017;41:529-57. [DOI] [PubMed] [Google Scholar]
Berrouiguet 2019 {published data only}
- Berrouiguet S, Barrigón ML, Castroman JL, Courtet P, Artés-Rodríguez A, Baca-García E. Combining mobile-health (mHealth) and artificial intelligence (AI) methods to avoid suicide attempts: the Smartcrises study protocol. BMC Psychiatry 2019;19:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
Betz 2020 {published and unpublished data}
- Betz ME, Knoepke CE, Simpson S, Siry BJ, Clement A, Saunders T, et al. An interactive web-based lethal means safety decision aid for suicidal adults (Lock to Live): pilot randomized controlled trial. Journal of Medical Internet Research 2020;22:e16253. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bryan 2017a {published data only (unpublished sought but not used)}
- Bryan CJ, May AM, Rozek DC, Williams SR, Clemans TA, Mintz J, et al. Use of crisis management interventions among suicidal patients: results of a randomized controlled trial. Depression and Anxiety 2018;35:619-28. [DOI] [PubMed] [Google Scholar]
Bryan 2017b {published data only}
- Bryan CJ, Mintz J, Clemans TA, Leeson B, Burch S, Williams SR, et al. Effect of crisis response planning vs. contracts for safety on suicide risk in U.S. army soldiers: a randomized clinical trial. Journal of Affective Disorders 2017;212:64-72. [DOI] [PubMed] [Google Scholar]
Cebria 2015 {published data only}
- Cebrià AI, Pérez-Bonaventura I, Cuijpers P, Kerkhof A, Parra I, Escayola A, et al. Telephone management program for patients discharged from an emergency department after a suicide attempt: a 5-year follow-up study in a Spanish population. Crisis 2015;36(5):345-52. [DOI] [PubMed] [Google Scholar]
- Cebrià AI, Parra I, Pàmias M, Escayola A, García-Parés G, Puntí J, et al. Effectiveness of a telephone management programme for patients discharged from an emergency department after a suicide attempt: controlled study in a Spanish population. Journal of Affective Disorders 2013;147:269-76. [DOI] [PubMed] [Google Scholar]
Celano 2017 {published and unpublished data}
- Celano CM, Beale EE, Mastromauro CA, Stewart JG, Millstein RA, Auerbach RP, et al. Psychological interventions to reduce suicidality in high-risk patients with major depression: a randomized controlled trial. Psychological Medicine 2017;47(5):810-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Currier 2015 {published data only}
- Currier GW, Brown GK, Brenner LA, Chesin M, Knox KL, Ghahramanlou-Holloway M, et al. Rationale and study protocol for a two-part intervention: safety planning and structured follow-up among veterans at risk for suicide and discharged from the emergency department. Contemporary Clinical Trials 2015;43:179-84. [DOI] [PubMed] [Google Scholar]
Dassa 2018 {published data only (unpublished sought but not used)}
- Dassa D, Olie E, Courtet P, Ducasse D. Positive psychology for management of suicidal patients: a controlled trial. European Psychiatry 2018;48S:S446. [Google Scholar]
Davidson 2006 {published and unpublished data}
- Davidson K, Norrie J, Tyrer P, Gumley A, Tata P, Murray H, et al. The effectiveness of cognitive behavior therapy for borderline personality disorder: results from the borderline personality disorder study of cognitive therapy (BOSCOT) trial. Journal of Personality Disorders 2006;20:450-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson K, Tyrer P, Gumley A, Tata P, Norrie J, Palmer S, et al. A randomized controlled trial of cognitive behavior therapy for borderline personality disorder: rationale for trial, method, and description of sample. Journal of Personality Disorders 2006;20:431-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson KM, Tyrer P, Norrie J, Palmer SJ, Tyrer H. Cognitive therapy v. usual treatment for borderline personality disorder: prospective 6-year follow-up. British Journal of Psychiatry 2010;197:456-62. [DOI] [PubMed] [Google Scholar]
- Norrie J, Davidson K, Tata P, Gumley A. Influence of therapist competence and quantity of cognitive behavioural therapy on suicidal behaviour and inpatient hospitalisation in a randomised controlled trial in borderline personality disorder: further analyses of treatment effects in the BOSCOT study. Psychology and Psychotherapy: Theory, Research and Practice 2013;86:280-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer S, Davidson K, Tyrer P, Gumley A, Tata P, Norrie J, et al. The cost-effectiveness of cognitive behavior therapy for borderline personality disorder: results from the BOSCOT trial. Journal of Personality Disorders 2006;20:466-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dimeff 2020 {published data only}
- Dimeff LA, Jobes DA, Chalker SA, Piehl BM, Duvivier LL, Lok BC, et al. A novel engagement of suicidality in the emergency department: Virtual Collaborative Assessment and Management of Suicidality. General Hospital Psychiatry 2020;63:119-26. [DOI] [PubMed] [Google Scholar]
Di Simplicio 2020 {published data only}
- Di Simplicio M, Appiah-Kusi E, Wilkinson P, Watson P, Meiser-Stedman C, Kavanagh DJ, et al. Imaginator: a proof-of-concept feasibility trial of a brief imagery-based psychological intervention for young people who self-harm. Suicide and Life-Threatening Behavior 2020;50:724-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dixon‐Gordon 2015 {published data only}
- Dixon KL, Chapman AL, Turner BJ. A preliminary pilot study comparing dialectical behavior therapy emotion regulation skills with interpersonal effectiveness skills and a control group treatment. Journal of Experimental Psychopathology 2015;6:369-88. [Google Scholar]
Doering 2010 {published data only}
- Buchheim A, Hörz-Sagstetter S, Doering S, Rentrop M, Schuster P, Buchheim P, et al. Change of unresolved attachment in borderline personality disorder: RCT study of transference-focused psychotherapy. Psychotherapy and Psychosomatics 2017;86:314-6. [DOI] [PubMed] [Google Scholar]
- Doering S, Hörz S, Rentrop M, Fischer-Kern M, Schuster P, Benecke C, et al. Transference-focused psychotherapy v. treatment by community psychotherapists for borderline personality disorder: randomised controlled trial. British Journal of Psychiatry 2010;196:389-95. [DOI] [PubMed] [Google Scholar]
Ducasse 2018 {published data only (unpublished sought but not used)}
- Ducasse D, Jaussent I, Arpon-Brand V, Vienot M, Laglaoui C, Béziat S, et al. Acceptance and commitment therapy for the management of suicidal patients: a randomized controlled trial. Psychotherapy and Psychosomatics 2018;87:1-12. [DOI] [PubMed] [Google Scholar]
Exbrayat 2017 {published data only}
- Exbrayat S, Coudrot C, Gourdon X, Gay A, Sevos J, Pellet J, et al. Effect of telephone follow-up on repeated suicide attempt in patients discharged from an emergency psychiatry department: a controlled study. BMC Psychiatry 2017;17:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Franklin 2016 {published data only}
- Franklin JC, Fox KR, Franklin CR, Kleiman EM, Ribeiro JD, Jaroszewski AC, et al. A brief mobile app reduces nonsuicidal and suicidal self-injury: evidence from three randomized controlled trials. Journal of Consulting and Clinical Psychology 2016;84:544-57. [DOI] [PubMed] [Google Scholar]
Gabilondo 2020 {published data only}
- Gabilondo A, Aristegi E, Gonzalez-Pinto A, Zurimendi JM, Mateos del Pinto M, Roca R, et al. Prevention of suicidal behaviour with telemedicine in patients with a recent suicide attempt: is a 6-month intervention long enough? Suicide and Life-Threatening Behavior 2020;50:211-9. [DOI] [PubMed] [Google Scholar]
Galfalvy 2017 {published data only (unpublished sought but not used)}
- Galfalvy H, Brodsky B, Oquendo M, Stanley B. Childhood maltreatment moderates antidepressant treatment response for self-injury in borderline personality disorder. Biological Psychiatry 2017;81:S74. [Google Scholar]
Gooding 2020 {published data only}ISRCTN17776666
- Gooding PA, Pratt D, Awenat Y, Drake R, Elliott R, Emsley R, et al. A psychological intervention for suicide applied to non-affective psychosis: the CARMS (Cognitive AppRoaches to coMbatting Suicidality) randomised controlled trial protocol. BMC Psychiatry 2020;20:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodman 2016 {published data only (unpublished sought but not used)}
- Goodman M, Banthin D, Blair NJ, Mascitelli KA, Wilsnack J, Chen J, et al. A randomized trial of dialectical behavior therapy in high-risk suicidal veterans. Journal of Clinical Psychiatry 2016;77:e1591-600. [DOI] [PubMed] [Google Scholar]
Goodman 2020 {published data only}
- Goodman M, Brown GK, Galfalvy HC, Page Spears A, Sullivan SR, Kapil-Pair KN, et al. Group ("Project Life Force") versus individual suicide safety planning: a randomized clinical trial. Contemporary Clinical Trials Communications 2020;17:100520. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haddock 2019 {published data only (unpublished sought but not used)}ISRCTN17890126
- Awenat YF, Peters S, Gooding PA, Pratt D, Shaw-Núñez E, Harris K, et al. A qualitative analysis of suicidal psychiatric inpatients views and expectations of psychological therapy to counter suicidal thoughts, acts and deaths. BMC Psychiatry 2018;18:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock G, Davies L, Evans E, Emsley R, Gooding P, Heaney L, et al. Investigating the feasibility and acceptability of a cognitive behavioural suicide prevention therapy for people in acute psychiatric wards (the 'INSITE' trial): study protocol for a randomised controlled trial. Trials 2016;17:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock G, Pratt D, Gooding PA, Peters S, Emsley R, Evans E, et al. Feasibility and acceptability of suicide prevention therapy on acute psychiatric wards: randomised controlled trial. British Journal of Psychiatry Open 2019;5:e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hashemi‐Aliabadi 2020 {published data only}
- Hashemi-Aliabadi S, Jalali A, Rahmati M, Salari N. Group reminiscence for hope and resilience in care-seekers who have attempted suicide. Annals of General Psychiatry 2020;19:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hooley 2014 {published data only}
- Hooley JM, St Germain SA. Nonsuicidal self-injury, pain, and self-criticism: does changing self-worth change pain endurance in people who engage in self-injury. Clinical Psychological Science 2014;2:297-305. [Google Scholar]
Hooley 2018 {published data only}ISRCTN12276176
- Hooley JM, Fox KR, Wang SB, Kwashie AND. Novel online daily diary interventions for nonsuicidal self-injury: a randomized controlled trial. BMC Psychiatry 2018;18:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hurtado‐Santiago 2018 {published data only}
- Hurtado-Santiago S, Guzmán-Parra J, Bersabé RM, Mayoral F. Effectiveness of iconic therapy for the reduction of borderline personality disorder symptoms among suicidal youth: study protocol for a randomised controlled trial. BMC Psychiatry 2018;18:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
Inder 2015 {published data only}
- Inder ML, Crowe MT, Luty SE, Carter JD, Moor S, Frampton CM, et al. Randomized, controlled trial of interpersonal and social rhythm therapy for young people with bipolar disorder. Bipolar Disorder 2015;17:128-38. [DOI] [PubMed] [Google Scholar]
- Inder ML, Crowe MT, Luty SE, Carter JD, Moor S, Frampton CM. Prospective rates of suicide attempts and nonsuicidal self-injury by young people with bipolar disorder participating in a psychotherapy study. Australian and New Zealand Journal of Psychiatry 2015;50:167-73. [DOI] [PubMed] [Google Scholar]
ISRCTN10115835 {unpublished data only}10115835
- ISRCTN10115835. Is a talking therapy, called psychodynamic interpersonal therapy, clinically and cost effective for women who self-harm in prison? [Women Offenders Repeat Self-Harm Intervention Pragmatic Trial (WORSHIP III)]. doi.org/10.1186/ISRCTN10115835 (first received 11 February 2019). [DOI: 10.1186/ISRCTN10115835] [DOI]
ISRCTN16003313 {unpublished data only}16003313
- ISRCTN16003313. A brief psychological intervention for self-harm in emergency departments [ASsuRED: Improving outcomes in patients who self-harm. Adapting and evaluating a brief pSychological inteRvention in Emergency Departments]. doi.org/10.1186/ISRCTN16003313 (first received 27 January 2020).
ISRCTN16049211 {unpublished data only}16049211
- ISRCTN16049211. FReSH START feasibility study [Function REplacement in repeated Self-Harm: Standardising Therapeutic Assessment and the Related Therapy (FRESH START): feasibility study]. doi.org/10.1186/ISRCTN16049211 (first received 9 December 2019).
ISRCTN16862589 {unpublished data only}16862589
- ISRCTN16862589. Brief education supported treatment for adolescent borderline personality disorder [Brief Education Supported Treatment (BEST) for adolescent borderline personality disorder: a feasibility study of delivery of specialised early intervention for borderline personality disorder through collaboration with education providers, incorporating a feasibility randomised controlled trial]. doi.org/10.1186/ISRCTN16862589 (first received 28 January 2019).
ISRCTN18761534 {unpublished data only}18761534
- ISRCTN18761534. Women Offenders Repeat Self-Harm Intervention Pilot II (WORSHIP II). doi.org/10.1186/ISRCTN18761534 (first received 19 December 2012).
Jardon 2019 {published data only}
- Jardon V, Debien C, Duhem S, Morgiève M, Ducrocq F, Vaiva G. An example of post-discharge monitoring after a suicide attempt: VigilanS [Un example de système de veille post-hospitalière des suicidants: VigilanS]. L'Éncéphale 2019;45:S13-21. [DOI] [PubMed] [Google Scholar]
Jobes 2017 {published data only}
- Huh D, Jobes DA, Comtois KA, Kerbrat AH, Chalker SA, Gutierrez PM, et al. The Collaborative Assessment and Management of Suicidality (CAMS) versus Enhanced Care As Usual (E-CAU) with suicidal soldiers: moderator analyses from a randomized controlled trial. Military Psychology 2018;30:495-506. [Google Scholar]
- Jobes DA, Comtois KA, Gutierrez PM, Brenner LA, Huh D, Chalker SA, et al. A randomized controlled trial of the Collaborative Assessment and Management of Suicidality versus Enhanced Care As Usual with suicidal soldiers. Psychiatry 2017;80:339-56. [DOI] [PubMed] [Google Scholar]
Johnson 2018 {published data only}
- Johnson SB, Goodnight BL, Zhang H, Daboin I, Patterson B, Kaslow NJ. Compassion-based mediation in African Americans: self-criticism mediates changes in depression. Suicide and Life-Threatening Behavior 2018;48:160-8. [DOI] [PubMed] [Google Scholar]
Kawanishi 2018 {published data only}
- Kawanishi C, Ishii T, Yonemoto N, Yamada M, Tachikawa H, Kishimoto T, et al. Protocol for a prospective multicentre registry cohort study on suicide attempters given the assertive case management intervention after admission to an emergency department in Japan: Post-ACtion-J Study (PACS). British Medical Journal Open 2018;8:e020517. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kennedy 2018 {published data only}
- Kennedy GA, Forney KJ, Pinner D, Martinez KM, Buchman-Schmitt JM, Keel PK. Reducing anticipated non-suicidal self-injury by improving body esteem in individuals with weight suppression: a proof of concept study. International Journal of Eating Disorders 2018;52:206-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kholodkov 2015 {published data only}
- Kholodkov T. Mindfulness-Based Relapse Prevention for Non-Suicidal Self-Injury [Doctor of Philosophy thesis]. Laramie, WY: University of Wyoming, 2015. [Google Scholar]
Kim 2020 {published data only}
- Kim M-H, Lee J, Noh H, Hong J-P, Kim P, Cha YS, et al. Effectiveness of a flexible and continuous case management program for suicide attempters. International Journal of Environmental Research and Public Health 2020;17:2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kline 2016 {published data only}
- Kline A, Chesin M, Latorre M, Miller R, St Hill L, Shcherbakov A, et al. Rationale and study design of a trial of mindfulness-based cognitive therapy for preventing suicidal behavior (MBCT-S) in military veterans. Contemporary Clinical Trials 2016;50:245-52. [DOI] [PubMed] [Google Scholar]
Korczak 2020 {published data only}
- Korczak DJ, Finkelstein Y, Barwick M, Chaim G, Cleverley K, Henderson J, et al. A suicide prevention strategy for youth presenting to the emergency department with suicide related behaviour: protocol for a randomized controlled trial. BMC Psychiatry 2020;20:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
LaCroix 2018 {published and unpublished data}
- Ghahramanlou-Holloway M, LaCroix JM, Perera KU, Neely L, Grammer G, Weaver J, et al. Inpatient psychiatric care following a suicide-related hospitalization: a pilot trial of post-admission cognitive therapy in a military medical center. General Hospital Psychiatry 2020;63:46-53. [DOI] [PubMed] [Google Scholar]
- LaCroix JM, Perera KU, Neely LL, Grammer G, Weaver J, Ghahramanlou-Holloway M. Pilot trial of post-admission cognitive therapy: inpatient program for suicide prevention. Psychological Services 2018;15:279-88. [DOI] [PubMed] [Google Scholar]
- Neely L, Irwin K, Carreno Ponce JT, Perera K, Grammer G, Ghahramanlou-Holloway M. Post Admission Cognitive Therapy (PACT) for the prevention of suicide in military personnel with histories of trauma: treatment development and case example. Clinical Case Studies 2013;12:457-73. [Google Scholar]
Lahoz 2016 {published data only}
- Lahoz T, Hvid M, Wang AG. Preventing repetition of attempted suicide - III. The Amager Project, 5-year follow-up of a randomized controlled trial. Nordic Journal of Psychiatry 2017;70:547-53. [DOI] [PubMed] [Google Scholar]
Lin 2019 {published data only}
- Lin T-J, Ko H-C, Wu KY-W, Oei TP, Lane H-Y, Chen C-H. The effectiveness of dialectical behavior therapy skills training group vs. cognitive therapy group on reducing depression and suicide attempts for borderline personality disorder in Taiwan. Archives of Suicide Research 2019;23:82-99. [DOI] [PubMed] [Google Scholar]
Luxton 2014 {published data only}
- Luxton DD, Thomas EK, Chipps J, Relova RM, Brown D, McLay R, et al. Caring letters for suicide prevention: implementation of a multi-site randomized clinical trial in the U.S. military and veteran affairs healthcare systems. Contemporary Clinical Trials 2014;37:252-60. [DOI] [PubMed] [Google Scholar]
Mackie 2017 {published data only}
- Mackie C, Dunn N, MacLean S, Testa V, Heisel M, Hatcher S. A qualitative study of a blended therapy using problem solving therapy with a customised smartphone app in men who present to hospital with intentional self-harm. Evidence Based Mental Health 2017;20:118-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marriott 2016 {published data only}
- Marriott BP, Hibbeln JR, Killeen TK, Magruder KM, Holes-Lewis K, Tolliver BK, et al. Design and methods for the Better Resiliency Among Veterans and non-Veterans with Omega-3's (BRAVO) study: A double-blind, placebo-controlled trial of omega-3 fatty acid supplementation among adult individuals at risk of suicide. Contemporary Clinical Trials 2016;47:325-33. [DOI] [PubMed] [Google Scholar]
Matsubara 2019 {published data only}
- Matsubara T, Matsuo K, Matsuda A, Ogino Y, Hobara T, Wakabayashi Y, et al. Combining phone and postcard brief contact interventions for preventing suicide reattempts: a quasi-randomized controlled trial. Psychiatry Research 2019;279:395-6. [DOI] [PubMed] [Google Scholar]
McCall 2019 {published data only}
- McCall WV, Ahn E, Benca R, Krystal A, Rosenquist PB, Rumble M, et al. 0960. A preliminary report from the "REST-IT" study: insomnia severity and hypersomnia severity each independently predict the intensity of suicidal ideation. Sleep 2015;38:A339. [Google Scholar]
- McCall WV, Benca RM, Rosenquist PB, Youssef NA, McCloud L, Newman JC, et al. REducing Suicidal ideation Through Insomnia Treatment (REST-IT): a randomized clinical trial. American Journal of Psychiatry 2019;176:957-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
McManama O'Brien 2018 {published data only}
- McManama O'Brien KH, Sellers CM, Battalen AW, Ryan CA, Maneta EK, Aguinaldo LD, et al. Feasibility, acceptability, and preliminary effects of a brief alcohol intervention for suicidal adolescents in inpatient psychiatric treatment. Journal of Substance Abuse Treatment 2018;94:105-12. [DOI] [PubMed] [Google Scholar]
Miller 2016 {published data only}
- Miller IW, Gaudiano BA, Weinstock LM. The Coping Long Term with Active Suicide Program: description and pilot data. Suicide and Life-Threatening Behavior 2016;46:752-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morley 2014 {published data only}
- Morley KC, Sitharthan G, Haber PS, Tucker P, Sitharthan T. The efficacy of an Opportunistic Cognitive Behavioral intervention package (OCB) on substance use and comorbid suicide risk: a multisite randomized controlled trial. Journal of Consulting and Clinical Psychology 2014;82:130-40. [DOI] [PubMed] [Google Scholar]
Navarro‐Haro 2018 {published and unpublished data}
- Navarro-Haro MV, Botella C, Guillen V, Moliner R, Marco H, Jorquera M, et al. Dialectical behavior therapy in the treatment of borderline personality disorder and eating disorders comorbidity: a pilot study in a naturalistic setting. Cognitive Therapy and Research 2018;42:636-49. [Google Scholar]
NCT00218725 {unpublished data only}
- NCT00218725. Cognitive therapy for suicide attempters with drug dependence disorder. clinicaltrials.gov/ct2/show/NCT00218725 (first received 22 September 2005).
NCT00601939 {unpublished data only}
- NCT00601939. Group interventions for abused, suicidal black women. clinicaltrials.gov/ct2/show/NCT00601939 (first received 28 January 2008).
NCT00603421 {unpublished data only}
- NCT00603421. Effectiveness of a 24 hour phone line on the rate of suicide attempts in borderline patients. clinicaltrials.gov/ct2/show/NCT00603421 (first received 29 January 2008).
NCT00641498 {unpublished data only}
- NCT00641498. Effectiveness of standard emergency department psychiatric treatment compared with effectiveness of standard emergency department psychiatric treatment associated with treatment delivery by a suicide prevention center. clinicaltrials.gov/ct2/show/NCT00641498 (first received 24 March 2008).
NCT00980824 {published data only (unpublished sought but not used)}
- NCT00980824. ENGAGE - Meeting mental health needs of complex comorbid patients. clinicaltrials.gov/ct2/show/NCT00980824 (first received 21 September 2009).
NCT01359761 {unpublished data only}
- NCT01359761. Post Admission Cognitive Therapy (PACT) for the inpatient treatment of military personnel with suicidal behaviors: a multi-site randomized controlled trial. clinicaltrials.gov/ct2/show/NCT01359761 (first received 25 May 2011).
NCT01823120 {unpublished data only}
- NCT01823120. Text message intervention to reduce repeat self-harm in patients presenting to the emergency department. clinicaltrials.gov/ct2/show/NCT01823120 (first received 4 April 2013).
NCT01952405 {unpublished data only}
- NCT01952405. Efficacy of dialectical behavior therapy in patients with borderline personality disorder: a controlled trial in Taiwan. clinicaltrials.gov/ct2/show/NCT01952405 (first received 30 September 2013).
NCT02227160 {unpublished data only}
- NCT02227160. Group interventions for suicidal African Americans. clinicaltrials.gov/ct2/show/NCT02227160 (first received 27 August 2014).
NCT02299440 {unpublished data only}
- NCT02299440. Effects of ketamine in the acute phase of suicidal ideation (KETIS). clinicaltrials.gov/ct2/show/NCT02299440 (first received 24 November 2014).
NCT02522143 {unpublished data only}
- NCT02522143. College students who self-harm: an intervention study. clinicaltrials.gov/ct2/show/NCT02522143 (first received 13 August 2015).
NCT02742922 {unpublished data only}
- NCT02742922. Multicenter RCT to evaluate the clinical and cost-effectiveness of a culturally adapted therapy (C-MAP) in patients with a history of self-harm. clinicaltrials.gov/ct2/show/NCT02742922 (first received 19 April 2016).
NCT03300596 {unpublished data only}
- NCT03300596. Suicidal adults with alcohol or drug use problems: a new hospital-based treatment. clinicaltrials.gov/ct2/show/NCT03300596 (first received 3 October 2017).
NCT03376113 {unpublished data only}
- NCT03376113. The effect of a brief psychological intervention on reducing self-harm repetition: feasibility study. clinicaltrials.gov/ct2/show/NCT03376113 (first received 18 December 2017).
NCT03489382 {unpublished data only}
- NCT03489382. The BEACON Study: protocol for cluster RCT of a service to deliver smartphone-assisted problem-solving therapy compared to usual care in men who present with intentional self-harm to the ED in Ontario (protocol A). clinicaltrials.gov/ct2/show/NCT03489382 (first received 5 April 2018).
NCT03533075 {unpublished data only}
- NCT03533075. A pilot effectiveness trial of the Teachable Moment Brief Intervention (TMBI) for veterans hospitalized following a suicide attempt. clinicaltrials.gov/ct2/show/NCT03533075 (first received 22 May 2018).
NCT03600532 {unpublished data only}
- NCT03600532. Testing the efficacy of the Teachable Moment Brief Intervention for suicide attempt survivors in an inpatient setting: effects on psychosocial and experimental pain outcomes. clinicaltrials.gov/ct2/show/NCT03600532 (first received 26 July 2018).
NCT03943862 {unpublished data only}
- NCT03943862. To Share or not to Share (2Share): group intervention to support disclosure decisions after suicide attempt. clinicaltrials.gov/ct2/show/NCT03943862 (first received 9 May 2019).
O'Toole 2019 {published data only}
- O'Toole MS, Arendt MB, Pedersen CM. Testing an app-assisted treatment for suicide prevention in a randomized controlled trial: effect on suicide risk and depression. Behavior Therapy 2019;50:421-9. [DOI] [PubMed] [Google Scholar]
Pearce 2017 {published data only}
- Pearce S, Scott L, Attwood G, Saunders K, Dean M, De Ridder R, et al. Democratic therapeutic community treatment for personality disorder: randomised controlled trial. British Journal of Psychiatry 2017;210:149-56. [DOI] [PubMed] [Google Scholar]
Pfeiffer 2019 {published data only}
- Lapidos A, Abraham KM, Jagusch J, Garlick J, Walters H, Kim HM, et al. Peer mentorship to reduce suicide attempts among high-risk adults (PREVAIL): rationale and design of a randomized controlled effectiveness-implementation trial. Contemporary Clinical Trials 2019;87:105850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer PN, King C, Ilgen M, Ganoczy D, Clive R, Garlick J, et al. Development and pilot study of a suicide prevention intervention delivered by peer support specialists. Psychological Services 2019;16:360-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Philips 2018 {published data only}ISRCTN98982683
- Philips B, Wennberg P, Konradsson P, Frank J. Mentalization-based treatment for concurrent borderline personality disorder and substance use disorder: a randomized controlled feasibility study. European Addiction Research 2018;24:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pistorello 2020 {published data only}
- Pistorello J, Jobes D, Compton S, Locey NS, Walloch JC, Gallop R, et al. Developing adaptive treatment strategies to address suicidal risk in college students: a pilot sequential, multiple assignment, randomized trial (SMART). Archives of Suicide Research 2017;22:644-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pistorello J, Jobes DA, Gallop R, Compton SN, Locey NS, Au JS, et al. A randomized controlled trial of the Collaborative Assessment and Management of Suicidality (CAMS) versus Treatment As Usual (TAU) for suicidal college students. Archives of Suicide Research 2020 [ePub ahead of print]. [DOI: 10.1080/13811118.2020.1749742] [DOI] [PMC free article] [PubMed]
Pratt 2015 {published data only}
- Pratt D, Tarrier N, Dunn G, Awenat Y, Shaw J, Ulph F, et al. Cognitive-behavioural suicide prevention for male prisoners: a pilot randomized controlled trial. Psychological Medicine 2015;45:3441-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rees 2015 {published data only}
- Rees CS, Hasking P, Breen LJ, Lipp OV, Marmotte C. Group mindfulness based cognitive therapy vs group support for self-injury among young people: study protocol for a randomised controlled trial. BMC Psychiatry 2015;15:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rompogren 2018 {published data only}
- Rompogren JR. Using Resonance Frequency Breathing to Improve Distress Tolerance in Females who Engage in Non-Suicidal Self-Injury [Doctor of Philosophy thesis]. San Diego, CA: Alliant International University, 2018. [Google Scholar]
Rudd 2015 {published data only}
- Bryan CJ, Peterson AL, Rudd MD. Differential effects of brief CBT versus treatment as usual on posttreatment suicide attempts among groups of suicidal patients. Psychiatric Services 2018;69:703-9. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Rudd MD, Peterson AL, Young-McCaughan S, Wertenberger EG. The ebb and flow of the wish to live and the wish to die among suicidal military personnel. Journal of Affective Disorders 2016;202:58-66. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Wood DS, May A, Peterson AL, Wertenberger E, Rudd MD. 2017. Mechanisms of action contributing to reductions in suicide attempts following brief cognitive behavioral therapy for military personnel: a test of the interpersonal-psychological theory of suicide 2017;22:241-53. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Bryan CJ, Wertenberger EG, Peterson AL, Young-McCaughan S, Mintz J, et al. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. American Journal of Psychiatry 2015;172:441-9. [DOI] [PubMed] [Google Scholar]
Ryberg 2019 {published data only}
- Ryberg W, Diep LM, Landrø NI, Fosse R. Effects of the Collaborative Assessment and Management of Suicidality (CAMS) model: a secondary analysis of moderation and influencing factors. Archives of Suicide Research 2019 [ePub ahead of print]. [DOI: 10.1080/13811118.2019.1650143] [DOI] [PubMed]
- Ryberg W, Fosse R, Zahl P-H, Brorson I, Moller P, Landrø NI, et al. Collaborative Assessment and Management of Suicidality (CAMS) compared to Treatment As Usual (TAU) for suicidal patients: study protocol for a randomized controlled trial. Trials 2016;17:481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryberg W, Zahl P-H, Diep LM, Landrø NI, Fosse R. Managing suicidality within specialized care: a randomized controlled trial. Journal of Affective Disorders 2019;249:112-20. [DOI] [PubMed] [Google Scholar]
Sáiz 2014 {published and unpublished data}
- Sáiz PA, Rodriguez-Revulta J, González-Blanco L, Burón P, Al-Halabi S, Garrido M, et al. Study protocol of a prevention of recurrent suicidal behavior program based on case management (PSyMAC). Revista de Psiquiatría y Salud Mental 2014;7:131-8. [DOI] [PubMed] [Google Scholar]
Santel 2020 {published data only}
- Santel M, Beblo T, Neuner F, Berg M, Hennig-Fast K, Jobes DA, et al. Collaborative Assessment and Management of Suicidality (CAMS) compared to Enhanced Treatment As Usual (E-TAU) for suicidal patients in an inpatient setting: study protocol for a randomized controlled trial. BMC Psychiatry 2020;20:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sayal 2019 {published and unpublished data}
- Sayal K, Roe J, Atha C, Kaylor-Hughes C, Guo B, Townsend E, et al. Feasibility of a randomised controlled trial of remotely delivered problem-solving cognitive behaviour therapy versus usual care for young people with depression and repeat self-harm: Lessons learnt (e-DASH). BMC Psychiatry 2019;19:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sequeira 2016 {published data only}
- Sequeira E, Field C, Wagler A, Avila A. The moderation effect of mental health indicators on the efficacy of three brief alcohol interventions. Alcoholism 2016;40:69A. [Google Scholar]
Simon 2016 {published data only}
- Simon GE, Beck A, Rossom R, Richards J, Kirlin B, King D, et al. Population-based outreach versus care as usual to prevent suicide attempt: study protocol for a randomized controlled trial. Trials 2016;17:452. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinnaeve 2018 {published and unpublished data}
- Hakkaart-van Roijen L, Sinnaeve R, Bouwmans C, Van den Bosch L. Cost-effectiveness and cost-utility of short-term inpatient dialectical behavior therapy for chronically parasuicidal BPD (young) adults. Journal of Mental Health Policy and Economics 2015;1:S19. [Google Scholar]
- Sinnaeve R, Van den Bosch LMC, Hakkaart-van Roijen L, Vansteelandt K. Effectiveness of step-down versus outpatient dialectical behaviour therapy for patients with severe levels of borderline personality disorder: a pragmatic randomized controlled trial. Borderline Personality Disorder and Emotion Dysregulation 2018;5:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Bosch LMC, Sinnaeve R, Hakkaart-van Roijen L, Van Furth EF. Efficacy and cost-effectiveness of an experimental short-term inpatient dialectical behavior therapy (DBT) program: study protocol for a randomized controlled trial. Trials 2014;15:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Slesnick 2020 {published data only}
- Slesnick N, Zhang J, Feng X, Wu Q, Walsh L, Granello DH. Cognitive therapy for suicide prevention: a randomized pilot with suicidal youth experiencing homelessness. Cognitive Therapy and Research 2020;44:402-11. [Google Scholar]
Smits 2020 {published data only}
- Laurenssen EMP, Smits ML, Bales DL, Feenstra DJ, Eeren HV, Noom MJ, et al. Day hospital mentalization-based treatment versus intensive outpatient mentalization-based treatment for patients with severe borderline personality disorder: protocol of a multicentre randomized clinical trial. BMC Psychiatry 2014;14:301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurenssen EMP, Westra D, Kikkert MJ, Noom MJ, Eeren HV, Van Broekhuyzen AJ, et al. Day hospital mentalization-based treatment (MBT-DH) versus treatment as usual in the treatment of severe borderline personality disorder: protocol or a randomized controlled trial. BMC Psychiatry 2014;14:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits ML, Feenstra DJ, Bales DL, Blankers M, Dekker JJM, Lucas Z, et al. Day hospital versus intensive outpatient mentalization-based treatment: 3-year follow-up of patients treated for borderline personality disorder in a multicentre randomized clinical trial. Psychological Medicine 2020;216:79-84. [DOI] [PubMed] [Google Scholar]
- Smits ML, Feenstra DJ, Eeren HV, Bales DL, Laurenssen EMP, Blankers M, et al. Day hospital versus intensive out-patient mentalisation-based treatment for borderline personality disorder: multicentre randomised clinical trial. British Journal of Psychiatry 2020;216:79-84. [DOI] [PubMed] [Google Scholar]
Taha 2015 {published data only}
- Taha F, Zhang H, Snead K, Jones AD, Blackmon B, Bryant RJ, et al. Effects of a culturally informed intervention on abused, suicidal African American women. Cultural Diversity and Ethnic Minority Psychology 2015;21:560-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tejedor 2011 {published and unpublished data}
- Farré A, Portella MJ, De Angel L, Díaz A, De Diego-Adeliño J, Vegué J, et al. Benefits of a secondary prevention program in suicide: a 1-year follow-up experimental study compared with a treatment-as-usual control group. Crisis 2016;37:281-9. [DOI] [PubMed] [Google Scholar]
- Tejedor C, Díaz A, Faus G, Pérez V, Solà I. Results of the prevention program of suicidal behavior: eixample district of Barcelona [Resultados del programa de prevención de la conducta suicida: Distrito de la Dreta de l’Eixample de Barcelona]. Actas Españolas de Psiquiatria 2011;39:280-7. [PubMed] [Google Scholar]
Vaiva 2016 {published data only}
- Vaiva G, Jardon V, Ducrocq F, Grandgenèvre P, Debien C, Berrouiguet S, et al. Surveillance is a powerful took to prevent suicidal acts. In: Courtet P, editors(s). Understanding Suicide: From Diagnosis to Personalized Treatment. Cham, Switzerland: Springer International Publishing, 2016:269-79. [Google Scholar]
Van Spijker 2018 {published data only}
- Van Spijker BAJ, Werner-Seidler A, Batterham PJ, Mackinnon A, Calear AL, Gosling JA, et al. Effectiveness of a web-based self-help program for suicidal thinking in an Australian community sample: randomized controlled trial. Journal of Medical Internet Research 2018;20:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ward‐Ciesielski 2016 {published data only}
- Ward-Ciesielski EF, Jones CB, Wielgus MD, Wilks CR, Linehan MM. Single-session dialectical behavior therapy skills training versus relaxation training for non-treatment-engaged suicidal adults: a randomized controlled trial. BMC Psychology 2016;4:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Westling 2019 {published data only}
- Liljedahl SI, Helleman M, Daukantaité D, Westrin Å, Westling S. A standardized crisis management model for self-harming and suicidal individuals with three or more diagnostic criteria of borderline personality disorder: the Brief Admission Skåne Randomized Controlled Trial protocol (BASRCT). BMC Psychiatry 2017;17:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westling S, Daukantaitė D, Liljedahl SI, Oh Y, Westrin Å, Flyckt L, et al. Effect of brief admission to hospital by self-referral for individuals who self-harm and are at risk of suicide: a randomized clinical trial. JAMA Network Open 2019;2:e195463. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilks 2018 {published data only}
- Wilks CR, Lungu A, Ang SY, Matsumiya B, Yin Q, Linehan MM. A randomized controlled trial of an internet delivered dialectical behavior therapy skills training for suicidal and heavy episodic drinkers. Journal of Affective Disorders 2018;232:219-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wittouck 2014 {published data only}
- Wittouck C, Van Autreve S, Portzky G, Van Heeringen K. A CBT-based psychoeducational intervention for suicide survivors: a cluster randomized controlled study. Crisis 2014;35:193-201. [DOI] [PubMed] [Google Scholar]
Yang 2020 {published data only}
- Yang X, Liu D, Wang Y, Chen Y, Chen W, Yang C, et al. Effectiveness of Zhong-Yong thinking based dialectical behavior therapy group skills training versus supportive group therapy for lowering suicidal risks in Chinese young adults: a randomized controlled trial with a 6-month follow-up. Brain and Behavior 2020;10:e01621. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
NCT00533117 {published data only (unpublished sought but not used)}
- NCT00533117. Treating suicidal behavior and self-mutilation in people with borderline personality disorder. clinicaltrials.gov/ct2/show/NCT00533117 (first received 21 September 2007).
NCT00834834 {unpublished data only}
- NCT00834834. Comparing treatments for self-injury and suicidal behavior in people with borderline personality disorder. clinicaltrials.gov/ct2/show/NCT00834834 (first received 3 February 2009).
References to ongoing studies
ACTRN12617000529347 {unpublished data only}
- ACTRN12617000529347. Will prisoners who self-harm reduce their frequency of self-harming after going through the Dialectical Behaviour Therapy intervention? www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=372437&isReview=true (first received 27 February 2017).
Berrouiguet 2014 {published and unpublished data}
- Berrouiguet S, Alavi Z, Vaiva G, Courtet P, Baca-García E, Vidailhet P, et al. SIAM (Suicide Intervention Assisted by Messages): the development of a post-acute crisis text messaging outreach for suicide prevention. BMC Psychiatry 2014;14:294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrouiguet S, Larsen ME, Mesmeur C, Gravey M, Billot R, Walter M, et al. Toward mHealth brief contact intervention in suicide prevention: case series from the Suicide Intervention Assisted by Messages (SIAM) randomized controlled trial. Journal of Medical Internet Research mHealth and uHealth 2018;6:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaïb 2020 {published data only (unpublished sought but not used)}
- Chaïb LS, Lopez-Castroman J, Abbar M. Group post-admission cognitive therapy for suicidality vs individual supportive therapy for the prevention of repeat suicide attempts: a randomized controlled trial. Trials 2020;21:889. [DOI] [PMC free article] [PubMed] [Google Scholar]
McMain 2018 {published and unpublished data}
- McMain SF, Chapman AL, Kuo JR, Guimond T, Streiner DL, Dixon-Gordon KL, et al. The effectiveness of 6 versus 12-months of dialectical behaviour therapy for borderline personality disorder: the Feasibility of A Shorter Treatment and Evaluating Responses (FASTER) trial protocol. BMC Psychiatry 2018;18:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02060448 {unpublished data only}
- NCT02060448. Exploring two emotion-focused treatment modules in non-suicidal self-injury. clinicaltrials.gov/ct2/show/NCT02060448 (first received 12 february 2014).
NCT02354183 {unpublished data only}
- NCT02354183. Commitment and motivation in a brief DBT intervention for self harm. clinicaltrials.gov/ct2/show/NCT02354183 (first received 3 February 2015).
NCT03081078 {unpublished data only}
- NCT03081078. Effects of community-based caring contact on post-discharge young adults with self-harm. clinicaltrials.gov/ct2/show/NCT03081078 (first received 15 March 2017).
NCT03185026 {unpublished data only}
- NCT03185026. Effectiveness of the first French psychoeducational program for suicidal behavior: a randomized controlled trial. clinicaltrials.gov/ct2/show/NCT03185026 (first received 14 June 2017).
NCT03427190 {unpublished data only}
- NCT03427190. Assessment of preventive efficacy of an algorithm taking place after suicide attempts among attempters admitted to hospital in the French Overseas Territories. clinicaltrials.gov/ct2/show/NCT03427190 (first received 9 February 2018).
NCT03463980 {unpublished data only}
- NCT03463980. Compassion meditation and ReliefLink app for suicidal, low-income, African Americans. clinicaltrials.gov/ct2/show/NCT03463980 (first received 13 March 2018).
NCT03541824 {unpublished data only}
- NCT03541824. Reducing suicide risk associated with weight loss. clinicaltrials.gov/ct2/show/NCT03541824 (first received 31 May 2018).
NCT03732300 {unpublished data only}
- NCT03732300. Evaluation of ASSIP - Attempted Suicide Short Intervention Program: a randomized controlled trial. clinicaltrials.gov/ct2/show/NCT03732300 (first received 6 November 2018).
NCT03853382 {unpublished data only}
- NCT03853382. Cognitive Analytic Therapy-informed Containment for self-Harm (CATCH). clinicaltrials.gov/ct2/show/NCT03853382 (first received 25 February 2019).
NCT03894462 {unpublished data only}
- NCT03894462. Effectiveness of a targeted brief intervention for recent suicide attempt survivors. clinicaltrials.gov/ct2/show/NCT03894462 (first received 28 March 2019).
NCT04072666 {unpublished data only}
- NCT04072666. Investigations of psychological interventions in suicide prevention: a comparison of brief cognitive behavioural therapy and the attempted suicide short intervention program. clinicaltrials.gov/ct2/show/NCT04072666 (first received 28 August 2019).
NCT04168645 {unpublished data only}
- NCT04168645. Inpatient cognitive-behavioral therapy to reduce suicide risk post-discharge. clinicaltrials.gov/ct2/show/NCT04168645 (first received 19 November 2019).
NCT04191122 {unpublished data only}
- NCT04191122. Community Outpatient Psychotherapy Engagement Service for Self-harm (COPESS): a feasibility study. clinicaltrials.gov/ct2/show/NCT04191122 (first received 9 December 2019).
NCT04244786 {unpublished data only}
- NCT04244786. Treating self injurious behavior: a novel brain stimulation approach. clinicaltrials.gov/ct2/show/NCT04244786 (first received 28 January 2020).
NCT04284085 {unpublished data only}
- NCT04284085. Evaluation of a psychoeducational intervention for people with suicidal behaviour in the penitentiary environment: N'VIU project. clinicaltrials.gov/ct2/show/NCT04284085 (first received 25 February 2020).
NCT04343703 {unpublished data only}
- NCT04343703. Suicide prevention and intervention (SURVIVE): cohort study and nested randomized controlled trials of secondary prevention programs for suicide attempts. clinicaltrials.gov/ct2/show/NCT04343703 (first received 13 April 2020).
NCT04366466 {published data only (unpublished sought but not used)}
- NCT04366466. Program to Promote Engagement in care for the Prevention of Suicide recidivism (PEPS). clinicaltrials.gov/ct2/show/NCT04366466 (first received 29 April 2020).
NCT04420546 {unpublished data only}
- NCT04420546. Using implementation intentions to reduce self-harm. clinicaltrials.gov/ct2/show/NCT04420546 (first received 9 June 2020).
O'Connor 2019 {published data only}ISRCTN62181241
- O'Connor RC, Lundy J-M, Stewart C, Smillie S, McClelland H, Syrett S, et al. SAFETEL randomised controlled feasibility trial of a safety planning intervention with follow-up telephone contact to reduce suicidal behaviour: study protocol. BMJ Open 2019;9:e025591. [DOI] [PMC free article] [PubMed] [Google Scholar]
SLCTR/2017/008 {unpublished data only}
- SLCTR/2017/008. A brief intervention for prevention of repetition of self-harm, among those who have recently attempted self-poisoning: a randomized controlled trial. slctr.lk/trials/slctr-2017-008 (first received 23 March 2017).
Stevens 2019 {published and unpublished data}
- Stevens GJ, Hammond TE, Brownhill S, Anand M, De la Riva A, Hawkins J, et al. SMS SOS: a randomized controlled trial to reduce self-harm and suicide attempts using SMS text messaging. BMC Psychiatry 2019;19:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Allen 2008
- Allen JG, Fonagy P, Bateman AW. Mentalizing in Clinical Practice. Washington DC, USA: American Psychiatric Publishing, 2008. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric Association, 2000. [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561. [DOI] [PubMed] [Google Scholar]
Beck 1974
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the Hopelessness Scale. Journal of Consulting and Clinical Psychology 1974;42:861-5. [DOI] [PubMed] [Google Scholar]
Beck 1976
- Beck AT. Cognitive Therapy and Emotional Disorders. New York, NY: International Universities Press, 1976. [Google Scholar]
Beck 1988
- Beck AT, Steer RA, Ranieri WF. Scale for Suicide Ideation: psychometric properties of a self-report version. Journal of Clinical Psychology 1988;44:499-505. [DOI] [PubMed] [Google Scholar]
Bergen 2010
- Bergen H, Hawton K, Waters K, Cooper J, Kapur N. Epidemiology and trends in non-fatal self-harm in three centres in England, 2000-2007. British Journal of Psychiatry 2010;197:493-8. [DOI] [PubMed] [Google Scholar]
Bertolote 2010
- Bertolote JM, Fleischmann A, De Leo D, Phillips MR, Botega NJ, Vijayakumar L, et al. Repetition of suicide attempts: data from five culturally different low- and middle-income country emergency care settings participating in the WHO SUPRE-MISS study. Crisis 2010;31:194-201. [DOI] [PubMed] [Google Scholar]
Bornheimer 2020
- Bornheimer LA, Zhang A, Li J, Hiller M, Tarrier N. Effectiveness of suicide-focused psychosocial interventions in psychosis: a systematic review and meta-analysis. Psychiatric Services 2020;71:829-38. [DOI] [PubMed] [Google Scholar]
Briggs 2019
- Briggs S, Netuveli G, Gould N, Gkaravella A, Gluckman NS, Kangogyere P, et al. The effectiveness of psychoanalytic/psychodynamic psychotherapy for reducing suicide attempts and self-harm: systematic review and meta-analysis. British Journal of Psychiatry 2019;214:320-8. [DOI] [PubMed] [Google Scholar]
Bustamante‐Madsen 2018
- Bustamante-Madsen L, Eddleston M, Schultz-Hansen K, Konradsen F. Quality assessment of economic evaluations of suicide and self-harm interventions. Crisis 2018;39:82-95. [DOI] [PubMed] [Google Scholar]
Calati 2016
- Calati R, Courtet P. Is psychotherapy effective for reducing suicide attempt and non-suicidal self-injury rates? Meta-analysis and meta-regression of literature data. Journal of Psychiatric Research 2016;79:8-20. [DOI] [PubMed] [Google Scholar]
Canner 2018
- Canner JK, Giuliano K, Selvaraiah S, Hammond ER, Schneider EB. Emergency department visits for attempted suicide and self harm in the USA, 2006-2013. Epidemiology and Psychiatric Sciences 2018;27:94-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carkhuff 1969
- Carkhuff RR. Helping and Human Relations. New York, NY: Holt, Rinehart, & Winston, 1969. [Google Scholar]
Carroll 2014
- Carroll R, Metcalfe C, Gunnell D. Hospital presenting self-harm and risk of fatal and non-fatal repetition: systematic review and meta-analysis. PL0S One 2014;9:e89944. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carter 2016
- Carter G, Page A, Large M, Hetrick S, Milner AJ, Bendit N, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guideline for the management of deliberate self-harm. Australian and New Zealand Journal of Psychiatry 2006;50:939-1000. [DOI] [PubMed] [Google Scholar]
Claes 2007
- Claes L, Wandereycken W, Vertommen H. Self-injury in female versus male psychiatric patients: a comparison of characteristics, psychopathology and aggression regulation. Personality and Individual Differences 2007;42:611-21. [Google Scholar]
Clarkin 1999
- Clarkin JF, Yeomans FE, Kernberg OF. Psychotherapy for Borderline Personality. New York, NY: Wiley, 1999. [Google Scholar]
Corcoran 2015
- Corcoran P, Griffin E, O'Carroll A, Cassidy L, Bonner B. Hospital-treated deliberate self-harm in the western area of Northern Ireland. Crisis 2015;36:83-90. [DOI] [PubMed] [Google Scholar]
Courtney 2019
- Courtney DB, Duda S, Szatmari P, Henderson J, Bennett K. Systematic review and quality appraisal of practice guidelines for self-harm in children and adolescents. Suicide & Life-threatening Behavior 2019;49:707-23. [DOI] [PubMed] [Google Scholar]
Cristea 2017
- Cristea IA, Gentili C, Cotét CD, Palomba D, Barbui C, Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: a systematic review and meta-analysis. JAMA Psychiatry 2017;74:319-28. [DOI] [PubMed] [Google Scholar]
Curtin 2002a
- Curtin F, Elbourne D, Altman DG. Meta-analysis combining parallel and cross-over clinical trials. III: the issue of carry-over. Statistics in Medicine 2002;21:2161-73. [DOI] [PubMed] [Google Scholar]
Curtin 2002b
- Curtin F, Altman DG, Elbourne D. Meta-analysis combining parallel and cross-over trials. I. Continuous outcomes. Statistics in Medicine 2002;21:2131-44. [DOI] [PubMed] [Google Scholar]
D'Anci 2019
- D'Anci KE, Uhl S, Giradi G, Martin C. Treatments for the prevention and management of suicide: a systematic review. Annals of Internal Medicine 2019;171:334-42. [DOI] [PubMed] [Google Scholar]
D'Zurilla 1971
- D’Zurilla TJ, Goldfried MR. Problem solving and behaviour modification. Journal of Abnormal Psychology 1971;78:107-26. [DOI] [PubMed] [Google Scholar]
D'Zurilla 2010
- D'Zurilla TJ, Nezu AM. Problem-solving therapy. In: Dobson KS, editors(s). Handbook of Cognitive-Behavioral Therapies. New York, NY: Guilford Press, 2010. [Google Scholar]
De Beurs 2018
- De Beurs D, Vancayseele N, Van Borkulo C, Portzky G, Van Heeringen K. The association between motives, perceived problems and current thoughts of self-harm following an episode of self-harm: a network analysis. Journal of Affective Disorders 2018;240:262-70. [DOI] [PubMed] [Google Scholar]
DeCou 2019
- DeCou CR, Comtois KA, Landes SJ. Dialectical behavior therapy is effective for the treatment of suicidal behavior: a meta-analysis. Behavior Therapy 2019;50:60-72. [DOI] [PubMed] [Google Scholar]
Deeks 2019
- Deeks JJ, Higgins JPT, Altman DG, editor(s). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
De Leo 2013
- De Leo D, Milner A, Fleischmann A, Bertolote J, Collings S, Amadeo S, et al. The WHO START Study: suicidal behaviours across different areas of the world. Crisis 2013;34:156-63. [DOI] [PubMed] [Google Scholar]
Dhingra 2015
- Dhingra K, Boduszek D, O'Connor RC. Differentiating suicide attempters from suicide ideators using the Integrated Motivational-Volitional Model of Suicidal Behaviour. Journal of Affective Disorders 2015;186:211-8. [DOI] [PubMed] [Google Scholar]
Donner 2002
- Donner A, Klar N. Issues in the meta-analysis of cluster randomized trials. Statistics in Medicine 2002;21:2971-80. [DOI] [PubMed] [Google Scholar]
Easterbrook 1991
- Easterbrook PJ, Gopalan R, Berlin JA, Matthews DR. Publication bias in clinical research. Lancet 1991;337:867-72. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Christoph M. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629. [DOI: 10.1136/bmj.315.7109.629] [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JPT, Curtin F, Worthington HV, Vail A. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2002;31:140-9. [DOI] [PubMed] [Google Scholar]
Ellis 1986
- Ellis A, Grieger R. Handbook of Rational-Emotive Therapy. New York, NY: Springer, 1986. [Google Scholar]
Endicott 1976
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale. A procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry 1976;33:766-71. [DOI] [PubMed] [Google Scholar]
Erez 1996
- Erez A, Bloom MC, Wells MT. Using random rather than fixed effects models in meta-analysis: implications for situation specificity and validity generalization. Personnel Psychology 1996;49:275-306. [Google Scholar]
Evans 2005
- Evans J, Evans M, Morgan HG, Hayward A, Gunnell D. Crisis card following self-harm: 12-month follow-up of a randomised controlled trial. British Journal of Psychiatry 2005;187:186-7. [DOI] [PubMed] [Google Scholar]
Ferrari 2014
- Ferrari AJ, Norman RE, Freedman G, Baxter AJ, Pirkis JE, Harris MG, et al. The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the Global Burden of Disease Study 2010. PL0S One 2014;9:e91936. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fleischmann 2002
- Fleischmann A, Bertolote JM. Multisite intervention study on suicidal behaviours - SUPRE-MISS: protocol of SUPRE-MISS. citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.174.5140&rep=rep1&type=pdf (accessed 31 October 2020).
Fleiss 1994
- Fleiss JL. Measures of effect size for categorical data. In: Cooper H, Hedges LV, editors(s). The Handbook of Research Synthesis. New York, NY: Russell Sage Foundation, 1994. [Google Scholar]
Forte 2019
- Forte A, Buscaioni A, Fiorillo A, Pompii A, Baldessarini R. Suicidal risk following hospital discharge: a review. Harvard Review of Psychiatry 2019;27:209-16. [DOI] [PubMed] [Google Scholar]
Furuno 2018
- Furuno T, Nakagawa M, Hinto K, Yamada T, Kawashima Y, Matsuoka Y, et al. Effectiveness of assertive case management on repeat self-harm in patients admitted for suicide attempt: findings from ACTION-J study. Journal of Affective Disorders 2018;225:460-5. [DOI] [PubMed] [Google Scholar]
Geulayov 2016
- Geulayov G, Kapur N, Turnbull P, Clements C, Waters K, Ness J, et al. Epidemiology and trends in non-fatal self-harm in three centres in England, 2000-2012: findings from the Multicentre Study of Self-harm in England. BMJ Open 2016;6:e010538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Geulayov 2019
- Geulayov G, Casey D, Bale L, Brand F, Clements C, Farooq B, et al. Suicide following presentation to hospital for non-fatal self-harm in the Multicentre Study of Self-Harm: a long-term follow-up study. Lancet Psychiatry 2019;6:1021-30. [DOI] [PubMed] [Google Scholar]
Ghahramanlou‐Holloway 2012
- Ghahramanlou-Holloway M, Cox DW, Greene FN. Post-Admission Cognitive Therapy: a brief intervention for psychiatric inpatients admitted after a suicide attempt. Cognitive and Behavioral Practice 2012;19:233-44. [Google Scholar]
Ghanbari 2015
- Ghanbari B, Malakouti SK, Nojomi M, Alavi K, Khaleghparast S. Suicide prevention and follow-up services: a narrative review. Global Journal of Health Sciences 2015;8:145-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gilbody 1997
- Gillbody S, House A, Owens D. The early repetition of deliberate self-harm. Journal of the Royal College of Physicians in London 1997;31:171-2. [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- GRADEpro GDT. Version accessed 26 June 2020. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available at gradepro.org.
Griffin 2014
- Griffin E, Arensman E, Corcoran P, Wall A, Williamson E, Perry I. National Register of Deliberate Self Harm Annual Report. Cork, Ireland: National Suicide Research Foundation, 2014. [Google Scholar]
Gunnell 2008
- Gunnell D, Hawton K, Ho D, Evans J, O'Connor S, Potokar J, et al. Hospital admissions for self harm after discharge from psychiatric inpatient care: cohort study. British Medical Journal 2008;337:a2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guy 1976
- Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD, USA: US Department of Heath, Education, and Welfare Public Health Service Alcohol, Drug Abuse, and Mental Health Administration, 1976. [Google Scholar]
Gøtzsche 2017
- Gøtzsche PC, Gøtzsche PK. Cognitive behavioural therapy halves the risk of repeated suicide attempts: systematic review. Journal of the Royal Society of Medicine 2017;110:404-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry 1960;32:56-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hanratty 2019
- Hanratty D, Kilicaslan J, Wilding H, Castle D. A systematic review of efficacy of Collaborative Assessment and Management of Suicidality (CAMS) in managing suicide risk and deliberate self-harm in adult populations. Australasian Psychiatry 2019;27:559-64. [DOI] [PubMed] [Google Scholar]
Harrison 2014
- Harrison JE, Henley G, AIHW. Suicide and hospitalised self-harm in Australia: trends and analysis. 2014. Injury research and statistics series no. 93. Cat. no. INJCAT 169. Canberra: AIHW. Available at www.aihw.gov.au/getmedia/b70c6e73-40dd-41ce-9aa4-b72b2a3dd152/18303.pdf.aspx?inline=true.
Hassanian‐Moghaddam 2017
- Hassanian-Moghaddam H, Sarjami S, Kolahi A-A, Lewin T, Carter G. Postcards in Persia: a twelve to twenty-four month follow-up of a randomized controlled trial for hospital-treated deliberate self-poisoning. Archives of Suicide Research 2017;21:138-54. [DOI] [PubMed] [Google Scholar]
Hassanzadeh 2010
- Hassanzadeh M, Khajeddin N, Nojomi M, Fleischmann A, Eshrati T. Brief intervention and contact after deliberate self-harm: an Iranian randomised controlled trial. Iranian Journal of Psychiatry and Behavioral Sciences 2010;4:5-12. [Google Scholar]
Hawton 1987b
- Hawton K, Catalan J. Attempted Suicide: A Practical Guide to its Nature and Management. Oxford, UK: Oxford University Press, 1987. [Google Scholar]
Hawton 2003
- Hawton K, Hariss L, Hall S, Simkin S, Bale E, Bond A. Deliberate self-harm in Oxford, 1990-2000: a time of change in patient characteristics. Psychological Medicine 2003;33:987-96. [DOI] [PubMed] [Google Scholar]
Hawton 2004
- Hawton K, Harriss L, Simkin S, Bale E, Bond A. Self-cutting: patient characteristics compared with self-poisoners. Suicide and Life-Threatening Behavior 2004;34:199-208. [DOI] [PubMed] [Google Scholar]
Hawton 2007
- Hawton K, Bergen H, Casey D, Simkin S, Palmer B, Cooper J, et al. Self-harm in England: a tale of three cities. Multicentre study of self-harm. Social Psychiatry and Psychiatric Epidemiology 2007;42:513-21. [DOI] [PubMed] [Google Scholar]
Hawton 2008
- Hawton K, Harriss L. The changing gender ratio in occurrence of deliberate self-harm across the lifecycle. Crisis 2008;29:4-10. [DOI] [PubMed] [Google Scholar]
Hawton 2013
- Hawton K, Saunders KEA, Topiwala A, Haw C. Psychiatric disorders in patients presenting to hospital following self-harm: a systematic review. Journal of Affective Disorders 2013;151:821-30. [DOI] [PubMed] [Google Scholar]
Hetrick 2016
- Hetrick SE, Robinson J, Spittal MJ, Carter G. Effective psychological and psychosocial approaches to reduce repetition of self-harm: a systematic review, meta-analysis and meta-regression. British Medical Journal Open 2016;6:e011024. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Deeks JJ. Chapter 7: Selecting studies and collecting data. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1.
Higgins 2019a
- Higgins JPT, Eldridge S, Li T, editor(s). Chapter 23: Including variants on randomized trials. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Higgins 2019b
- Higgins JPT, Li T, Deeks JJ, editor(s). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Högberg 2008
- Högberg G, Hällström T. Active multimodal psychotherapy in children and adolescents with suicidality: description, evaluation and clinical profile. Clinical Child Psychology and Psychiatry 2008;13:435-48. [DOI] [PubMed] [Google Scholar]
Hopewell 2009
- Hopewell S, Loudon K, Clarke MJ, Oxman A, Dickersin K. Publication bias in clinical trials due to statistical significance or direction of trial results. Cochrane Database of Systematic Reviews 2009, Issue 1. Art. No: MR000006. [DOI: 10.1002/14651858.MR000006.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hsu 1997
- Hsu WY, Chung JM. Constructing a scale of suicide risk and testing its reliability and validity. Formosa Journal of Mental Health 1997;10:1-17. [Google Scholar]
Hunt 2013
- Hunt GE, Siegfried N, Morley K, Sitharthan T, Cleary M. Psychosocial interventions for people with both severe mental illness and substance misuse. Cochrane Database of Systematic Reviews 2013, Issue 10. Art. No: CD001088. [DOI: 10.1002/14651858.CD001088.pub3] [DOI] [PubMed] [Google Scholar]
Inagaki 2019
- Inagaki M, Kawashima Y, Yonemoto N, Yamada M. Active contact and follow-up interventions to prevent repeat suicide attempts during high-risk periods among patients admitted to emergency departments for suicidal behavior: a systematic review and meta-analysis. BMC Psychiatry 2019;19:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jobes 2012
- Jobes DA. The Collaborative Assessment and Management of Suicidality (CAMS): an evolving evidence-based clinical approach to suicidal risk. Suicide and Life Threatening Behavior 2012;42:640-53. [DOI] [PubMed] [Google Scholar]
Jones 2012
- Jones C, Hacker D, Cormac I, Meaden A, Irving CB. Cognitive behavioural therapy versus other psychological treatments for schizophrenia. Cochrane Database of Systematic Reviews 2012, Issue 4. Art. No: CD008712. [DOI: 10.1002/14651858.CD008712.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kerry 1998
- Kerry SM, Bland JM. Analysis of a trial randomised in clusters. BMJ 1998;316:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klonsky 2011
- Klonsky ED. Non-suicidal self-injury in United States adults: prevalence, socio-demographics, topography and functions. Psychological Medicine 2011;41:1981-6. [DOI] [PubMed] [Google Scholar]
Knipe 2019
- Knipe D, Metcalfe C, Hawton K, Pearson M, Dawson A, Jayamanne S, et al. Risk of suicide and repeat self-harm after hospital attendance for non-fatal self-harm in Sri Lanka: a cohort study. Lancet Psychiatry 2019;6:659-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Krysinska 2016
- Krysinska K, Batterham PJ, Christensen H. Differences in the effectiveness of psychosocial interventions for suicidal ideation and behaviour in women and men: a systematic review of randomised controlled trials. Archives of Suicide Research 2016;21:12-32. [DOI] [PubMed] [Google Scholar]
Krysinska 2017
- Krysinska K, Batterham PJ, Christensen H. Differences in the effectiveness of psychosocial interventions for suicidal ideation and behaviour in women and men: a systematic review of randomised controlled trials. Archives of Suicide Research 2017;21:12-32. [DOI] [PubMed] [Google Scholar]
Larkin 2014
- Larkin C, Di Blasi Z, Arensman E. Risk factors for repetition of self-harm: a systematic review of prospective hospital-based studies. PLOS One 2014;9:e84282. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Medicine 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lilley 2008
- Lilley R, Owens D, Horrocks J, House A, Noble R, Bergen H, et al. Hospital care and repetition following self-harm: multicentre comparison of self-poisoning and self-injury. British Journal of Psychiatry 2008;192:440-5. [DOI] [PubMed] [Google Scholar]
Linehan 1981
- Linehan MM, Nielsen SL. Assessment of suicide ideation and parasuicide: hopelessness and social desirability. Journal of Consulting and Clinical Psychology 1981;49:773-5. [DOI] [PubMed] [Google Scholar]
Linehan 1993
- Linehan MM. Skills Training Manual for Treating Borderline Personality Disorder. New York, NY: Guilford Press, 1993. [Google Scholar]
Liu 2020
- Liu B-P, Lunde KB, Jia C-X, Qin P. The short-term rate of non-fatal and fatal repetition of deliberate self-harm: A systematic review and meta-analysis of longitudinal studies. J Affective Disord 2020;273:597-603. [DOI] [PubMed] [Google Scholar]
Lizardi 2010
- Lizardi D, Stanley B. Treatment engagement: a neglected aspect in the psychiatric care of suicidal patients. Psychiatric Services 2010;61:1183-91. [DOI] [PubMed] [Google Scholar]
Lovibond 1995
- Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy 1995;33:335-42. [DOI] [PubMed] [Google Scholar]
Lynch 2006
- Lynch TR, Chapman Al, Rosenthal MZ, Kuo JR, Linehan MM. Mechanisms of change in dialectical behavior therapy: theoretical and empirical observations. Journal of Clinical Psychology 2006;62:459-80. [DOI] [PubMed] [Google Scholar]
Marshall 2000a
- Marshall M, Gray A, Lockwood A, Green R. Case management for people with severe mental disorders. Cochrane Database of Systematic Reviews 2000, Issue 2. Art. No: CD000050. [DOI: 10.1002/14651858.CD000050.pub2] [DOI] [PubMed] [Google Scholar]
Marshall 2000b
- Marshall M, Lockwood A, Bradley C, Adams C, Joy C, Fenton M. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. British Journal of Psychiatry 2000;176:249-52. [DOI] [PubMed] [Google Scholar]
Masiran 2017
- Masiran R, Haniff J, Ali NH, Amid AMA. Rates and profiles of self-harm presenting to Malaysian general hospitals: data from the Ministry of Health in 2011. Malaysian Journal of Medicine and Health Sciences 2017;13:39-45. [Google Scholar]
McNair 1964
- McNair DM, Lorr M. An analysis of mood in neurotics. Journal of Abnormal and Social Psychology 1964;69:620-7. [DOI] [PubMed] [Google Scholar]
Meares 2004
- Meares R. The conversational model: an outline. American Journal of Psychotherapy 2004;58:51-66. [DOI] [PubMed] [Google Scholar]
Meerwijk 2016
- Meerwijk EL, Parekh A, Oquendo MA, Allen IE, Franck LS, Lee KA. Direct versus indirect psychosocial and behavioural interventions to prevent suicide and suicide attempts: a systematic review and meta-analysis. Lancet Psychiatry 2016;3:544-54. [DOI] [PubMed] [Google Scholar]
Microsoft Excel RoB2 Macro [Computer program]
- RoB2 Macro. Risk of Bias 2 Development Group, Version accessed prior to 24 March 2021. Microsoft, 2019. sites.google.com/site/riskofbiastool/welcome/rob-2-0-tool/current-version-of-rob-2.
Miller 1993
- Miller WR, Sanchez VC. Motivating young adults for treatment and lifestyle change. In: Howard G, editors(s). Issues in Alcohol Use and Misuse in Young Adults. South Bend, IN, USA: University of Notre Dame Press, 1993:55-82. [Google Scholar]
Milner 2015
- Milner AJ, Carter G, Pirkis J, Robinson J, Spittal MJ. Letters, green cards, telephone calls and postcards: systematic and meta-analytic review of brief contact interventions for reducing self-harm, suicide attempts and suicide. British Journal of Psychiatry 2015;206:184-90. [DOI] [PubMed] [Google Scholar]
Milner 2016
- Milner A, Spittal MJ, Kapur N, Witt K, Pirkis J, Carter G. Mechanisms of brief contact interventions in clinical populations: a systematic review. BMC Psychiatry 2016;16:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mitchell 2016
- Mitchell AJ, Hussain S, Leaver J, Rajan C, Jones A, Malcolm N, et al. Is there a difference between hospital-verified and self-reported self-harm? Implications for repetition. General Hospital Psychiatry 2016;43:12-6. [DOI] [PubMed] [Google Scholar]
Moher 1998
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998;352:609-13. [DOI] [PubMed] [Google Scholar]
Montgomery 1979
- Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry 1979;134:382-9. [DOI] [PubMed] [Google Scholar]
Morthorst 2016
- Morthorst BT, Soegaard B, Nordentoft M, Erlangsen A. Incidence rates of deliberate self-harm in Denmark, 1994-2011: a nationwide register study. Crisis 2016;37:256-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Müller 2016
- Müller A, Claes L, Brähler E, De Zwann M. Prevalence and correlates of self-harm in the German general population. PLOS One 2016;11:e0157928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 2012
- Murphy E, Kapur N, Webb R, Purandare N, Hawton K, Bergen H, et al. Risk factors for repetition and suicide following self-harm in older adults: multicentre cohort study. British Journal of Psychiatry 2012;200:399-404. [DOI] [PubMed] [Google Scholar]
NCCMH 2004
- National Collaborating Centre for Mental Health. Clinical Guideline 16. Self-Harm: The Short-Term Physical and Psychological Management and Secondary Prevention of Self-Harm in Primary and Secondary Care. London, UK: National Institute for Clinical Excellence, 2004. [Google Scholar]
Newcomb 2020
- Newcomb ME, Hill R, Buehler K, Ryan DT , Whitton SW, Mustanski B. High burden of mental health problems, substance use, violence, and related psychosocial factors in transgender, non‑binary, and gender diverse youth and young adults. Archives of Sexual Behavior 2020;49:645-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nezu 2010
- Nezu AM, Nezu CM, D'Zurilla TJ. Problem-solving therapy. In: Kazantzis N, Reinecke MA, Freeman A, editors(s). Cognitive and Behavioral Theories in Clinical Practice. New York, NY: Guilford Press, 2010. [Google Scholar]
NICE 2011
- National Institute for Health and Clinical Excellence. Self-harm: Longer-Term Management [National Clincial Practice Guideline Number 133]. London, UK: National Institute for Health and Clinical Excellence, 2011. [Google Scholar]
O'Connor 2011
- O'Connor RC. The integrated motivational-volitional model of suicidal behavior. Crisis 2011;32:295-8. [DOI] [PubMed] [Google Scholar]
Oliver 2010
- Oliver C, Richards C. Self-injurious behavior in people with intellectual disability. Current Opinion in Psychiatry 2010;23:412-6. [DOI] [PubMed] [Google Scholar]
Osman 1992
- Osman A, Gregg CL, Osman JR, Jones K. Factor structure and reliability of the Reasons for Living Inventory. Psychological Reports 1992;70:107-12. [DOI] [PubMed] [Google Scholar]
Owens 2002
- Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm: systematic review. British Journal of Psychiatry 2002;181:193-9. [DOI] [PubMed] [Google Scholar]
Owens 2020b
- Owens C, Fox F, Redwood S, Davies R, Foote L, Salisbury N, et al. Measuring outcomes in trials of interventions for people who self-harm: qualitative study of service users' views. British Journal of Psychiatry Open 2020;6:e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Padmanathan 2020
- Padmanathan P, Hall K, Moran P, Jones HE, Gunnell D, Carlisle V, et al. Prevention of suicide and reduction of self-harm among people with substance use disorder: a systematic review and meta-analysis of randomised controlled trials. Comprehensive Psychiatry 2020;96:152135. [DOI] [PubMed] [Google Scholar]
Perry 2012
- Perry IJ, Corcoran P, Fitzgerald AP, Keeley HS, Reulback U, Arensman E. The incidence and repetition of hospital-treated deliberate self-harm: findings from the world's first national registry. PLOS One 2012;7:e31663. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pirkis 2020
- Pirkis J, Amadeo S, Beautrais A, Phillips M, Yip PSF. Suicide prevention in the Western Pacific region. Crisis 2020;41:s80-98. [DOI] [PubMed] [Google Scholar]
Platt 1983
- Platt S, Weyman A, Hirsch S. Social Behaviour Assessment Schedule. 3rd edition. Windsor, UK: NFER-Nelson, 1983. [Google Scholar]
Plener 2016
- Plener PL, Brunner R, Fegert JM, Groschwitz RC, In-Albon T, Kaess M, et al. Treating nonsuicidal self-injury in adolescents: consensus based German guidelines. Child and Adolescent Psychiatry and Mental Health 2016;10:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pridemore 2005
- Pridemore WA, Damphousse KR, Moore RK. Obtaining sensitive information from a wary population: a comparison of telephone and face-to-face surveys of welfare recipients in the United States. Social Science and Medicine 2005;61:976-84. [DOI] [PubMed] [Google Scholar]
Review Manager 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2020.
Reynolds 1998
- Reynolds W. Suicidal Ideation Questionnaire: Professional Manual. Odessa, FL: Psychological Assessment Resources, 1998. [Google Scholar]
Riblet 2017
- Riblet NBV, Shiner B, Young-Xu Y, Watts BV. Strategies to prevent death by suicide: meta-analysis of randomised controlled trials. British Journal of Psychiatry 2017;210:396-402. [DOI] [PubMed] [Google Scholar]
Royal College of Psychiatrists 2014
- Royal College of Psychiatrists. Managing Self-Harm in Young People (Guideline number CR192). London, UK: Royal College of Psychiatrists, 2014. [Google Scholar]
Schotte 1982
- Schotte DE, Clum GA. Suicide ideation in a college population. Journal of Consulting and Clinical Psychology 1982;50:690-6. [DOI] [PubMed] [Google Scholar]
Schünemann 2019
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Selph 2014
- Selph SS, Ginsburg AD, Chou R. Impact of contacting study authors to obtain additional data for systematic reviews: diagnostic accuracy studies for hepatic fibrosis. Systematic Reviews 2014;3:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinclair 2011
- Sinclair JMA, Gray A, Rivero-Arias O, Saunders KEA, Hawton K. Healthcare and social services resource use and costs of self-harm patients. Social Psychiatry and Psychiatric Epidemiology 2011;46:263-71. [DOI] [PubMed] [Google Scholar]
Sniehotta 2005
- Sniehotta FF, Scholz U, Schwarzer R. Bridging the intention–behaviour gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychology and Health 2005;20:143-60. [Google Scholar]
Spitzer 1970
- Spitzer R, Endicott J, Fleiss JL, Cohen J. The Psychiatric Status Schedule: a technique for evaluating psychopathology and impairment in role functioning. Archives of General Psychiatry 1970;23:41-55. [DOI] [PubMed] [Google Scholar]
Sterne 2019
- Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:I4898. [DOI] [PubMed] [Google Scholar]
Tighe 2018
- Tighe J, Nicholas J, Shand F, Christensen H. Efficacy of acceptance and commitment therapy in reducing suicidal ideation and deliberate self-harm: systematic review. Journal of Medical Internet Research Mental Health 2018;5:e10732. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ting 2012
- Ting SA, Sulivan AF, Boudreaux ED, Miller I, Camargo CA. Trends in US emergency department visits for attempted suicide and self-inflicted injury, 1993-2008. General Hospital Psychiatry 2012;34:557-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Torgerson 2004
- Torgerson D. The use of Zelen's design in randomised trials. British Journal of Obstetrics and Gynaecology 2004;111:2. [DOI] [PubMed] [Google Scholar]
Tsiachristas 2017
- Tsiachristas A, McDaid D, Casey D, Brand F, Lead J, Park A-L, et al. General hospital costs in England of medical and psychiatric care for patients who self-harm: a retrospective analysis. Lancet 2017;4:759-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tyrer 1990
- Tyrer P. Personality disorder and social functioning. In: Peck DF, Shapiro CM, editors(s). Measuring Human Problems: A Practical Guide. Chichester, UK: John Wiley & Sons, 1990:119–42. [Google Scholar]
Van Heeringen 2014
- Van Heeringen K, Mann JJ. The neurobiology of suicide. Lancet 2014;1:63-72. [DOI] [PubMed] [Google Scholar]
Viechtbauer 2020
- Viechtbauer W, Cheung MW-L. Outlier and influence diagnostics for meta-analysis. Research Synthesis Methods 2020;1:112-25. [DOI] [PubMed] [Google Scholar]
Vijayakumar 2011
- Vijayakumar L, Umamaheswari C, Shujaath Ali ZS, Devaraj P, Kesavan K. Intervention for suicide attempters: a randomized controlled study. Indian Journal of Psychiatry 2011;53:244-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weissman 1999
- Weissman MM, Staff MHS. Social Adjustment Scale - Self-Report (SAS-SR) User's Manual. North Tonawanda, NY: Multi-Health Systems, 1999. [Google Scholar]
Westbrook 2008
- Westbrook D, Kennerley H, Kirk J. An introduction to cognitive behaviour therapy: skills and applications. In: An Introduction to Cognitive Behaviour Therapy: Skills and Applications. London, UK: SAGE Publications, 2008. [Google Scholar]
WHO 2014
- World Health Organization. Preventing Suicide: A Global Imperative. Geneva, Switzerland: World Health Organization, 2014. [Google Scholar]
WHO 2019
- WHO. Psychiatrists and nurses working in the mental health sector (per 100,000 population), 2014-2016. gamapserver.who.int/gho/interactive_charts/mental_health/psychiatrists_nurses/atlas.html (accessed 19 November 2020).
Wilkinson 2002
- Wilkinson S, Taylor G, Templeton L, Mistral W, Salter E, Bennett P. Admissions to hospital for deliberate self-harm in England 1995-2000: an analysis of Hospital Episode Statistics. Journal of Public Health 2002;24:179-83. [DOI] [PubMed] [Google Scholar]
Witt 2018
- Witt K, Pache de Moraes D, Taylor Salisbury T, Arensman E, Gunnell D, Hazell P, et al. Treatment as usual (TAU) as a control condition in trials of cognitive behavioural-based psychotherapy for self-harm: impact of content and quality on outcomes in a systematic review. Journal of Affective Disorders 2018;235:434-47. [DOI] [PubMed] [Google Scholar]
Witt 2019
- Witt K, Daly C, Arensman E, Pirkis J, Lubman D. Patterns of self-harm methods over time and the association with methods used a repeat episodes of non-fatal self-harm and suicide: a systematic review. Journal of Affective Disorders 2019;245:250-64. [DOI] [PubMed] [Google Scholar]
Witt 2020a
- Witt K, Townsend E, Arensman E, Gunnell D, Hazell P, Taylor Salisbury T, et al. Psychosocial interventions for people who self-harm: methodological issues involved in trials to evaluate effectiveness. Archives of Suicide Research 2020;24(sup2):S32-93. [DOI: 10.1080/13811118.2019.1592043] [DOI] [PubMed]
Witt 2021a
- Witt KG, Hetrick SE, Rajaram G, Hazell P, Taylor Salisbury TL, Townsend E, et al. Pharmacological interventions for self‐harm in adults. Cochrane Database of Systematic Reviews 2021, Issue 1. Art. No: CD013669. [DOI: 10.1002/14651858.CD013669.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Witt 2021b
- Witt KG, Hetrick SE, Rajaram G, Hazell P, Taylor Salisbury TL, Townsend E, et al. Interventions for self‐harm in children and adolescents. Cochrane Database of Systematic Reviews 2021, Issue 3. Art. No: CD013667. [DOI: 10.1002/14651858.CD013667.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2012
- Xu D, Zhang X-L, Li X-Y, Niu Y-J, Zhang Y-P, Wang SL. Effectiveness of 18-month psychosocial intervention for suicide attempters. Zhongguo Xinli Weisheng Zazhi [Chinese Mental Health Journal] 2012;26:24-9. [Google Scholar]
Yakeley 2018
- Yakeley J, Burbridge-James W. Psychodynamic approaches to suicide and self-harm. B J Psych Advances 2018;24:37-45. [Google Scholar]
Zahl 2004
- Zahl DL, Hawton K. Repetition of deliberate self-harm and subsequent suicide risk: long-term follow-up study of 11 583 patients. British Journal of Psychiatry 2004;185:70-5. [DOI] [PubMed] [Google Scholar]
Zelen 1979
- Zelen M. A new design for randomized clinical trial. New England Journal of Medicine 1979;300:1242-5. [DOI] [PubMed] [Google Scholar]
Zigmond 1983
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica 1983;67:361-70. [DOI] [PubMed] [Google Scholar]
Zung 1965
- Zung WWK. A self-rating depression scale. Archives of General Psychiatry 1965;12:63-70. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Hawton 2016
- Hawton K, Witt KG, Taylor Salisbury Tl, Arensman E, Gunnell D, Hazell P, et al. Psychosocial interventions for self-harm in adults. Cochrane Database of Systematic Reviews 2016, Issue 5. Art. No: CD012189. [DOI: 10.1002/14651858.CD012189] [DOI] [PMC free article] [PubMed] [Google Scholar]
Witt 2020b
- Witt KG, Hawton K, Hetrick SE, Taylor Salisbury TL, Townsend E, Hazell P. Psychosocial interventions for self-harm in adults. Cochrane Database of Systematic Reviews 2020, Issue 7. Art. No: CD013668. [DOI: 10.1002/14651858.CD013668] [DOI] [PMC free article] [PubMed] [Google Scholar]